Recommendation on the Use of Live Attenuated Influenza Vaccine (LAIV) in HIV-Infected Individuals
An Advisory Committee Statement (ACS) | National Advisory Committee on Immunization (NACI)
Preamble
The National Advisory Committee on Immunization (NACI) provides the Public Health Agency of Canada (hereafter referred to as PHAC) with ongoing and timely medical, scientific, and public health advice relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Over the coming years NACI will be refining methodological approaches to include these factors. Not all NACI Statements will require in-depth analyses of all programmatic factors. As NACI works towards full implementation of the expanded mandate, select Statements will include varying degrees of programmatic analyses for public health programs.
PHAC acknowledges that the advice and recommendations set out in this statement are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC's Policy on Conflict of Interest, including yearly declaration of potential conflict of interest.
Download the alternative format
(PDF format, 1.52 MB, 42 pages)
Organization: Public Health Agency of Canada
Publication Date: 2020-08-13
Cat.: HP40-268/2020E-PDF
ISBN: 978-0-660-35127-8
Pub.: 200073
Related topics
Table of contents
- Summary of the information contained in this NACI statement
- I. Introduction
- II. Methods
- III. Use of LAIV in HIV-infected individuals
- IV. Discussion
- V. Recommendations
- Tables
- List of abbreviations
- Acknowledgments
- References
- Appendix A: PRISMA flow diagram
Summary of the information contained in this NACI statement
The following highlights key information for immunization providers. Please refer to the remainder of this statement for details.
1. What
Annual influenza vaccination is recommended for all individuals 6 months of age and older, including those with human immunodeficiency virus (HIV) infection. Prior to this statement, NACI recommended that live attenuated influenza vaccine (LAIV) was contraindicated for all individuals with HIV infection.
2. Who
This statement updates NACI's guidance on the use of LAIV for HIV-infected individuals.
3. How
LAIV may be considered as an option for annual vaccination of children 2–17 years of age with stable HIV infection on highly active antiretroviral therapy (HAART) and with adequate immune function. LAIV remains contraindicated for adults with HIV. LAIV should only be considered in children with HIV who meet the following criteria:
- Receiving HAART for ≥4 months;
- CD4 count ≥500/µL if 2–5 years of age, or ≥200/µL if 6–17 years of age (measured within 100 days before administration of LAIV); and
- HIV plasma RNA <10,000 copies/mL (measured within 100 days before administration of LAIV).
Intramuscular (IM) influenza vaccination still is considered the standard for children living with HIV by NACI and the Canadian Pediatric & Perinatal HIV/AIDS Research Group (CPARG), particularly for those without HIV viral load suppression (i.e. plasma HIV RNA >40 copies/mL). However, if IM vaccination is not accepted by the patient or substitute decision maker, LAIV would be reasonable for children meeting the criteria outlined above.
4. Why
LAIV is considered immunogenic in HIV-infected children 2–17 years of age with stable HIV infection on HAART and with adequate immune function. LAIV has a comparable immunogenicity profile to inactivated influenza vaccine for this population. No concerns regarding safety have been demonstrated, but there is currently insufficient evidence to draw a conclusion on the rate of uncommon, rare, and very rare adverse events (AE) after vaccination with LAIV in individuals with HIV. Intranasal administration of the influenza vaccine may be preferable to intramuscular injection for some children. There is insufficient evidence at this time to recommend LAIV for adults with HIV.
I. Introduction
Annual vaccination against influenza is recommended for all individuals 6 months of age and older, including those with human immunodeficiency virus (HIV) infectionFootnote 1. Acquired immunodeficiency syndrome is associated with increased influenza-related morbidity and mortality. However, data on the burden of influenza illness in individuals living with HIV who have less severe immunosuppression are sparse and likely influenced by the degree of immunosuppression, effectiveness of antiretroviral therapy, and comorbiditiesFootnote 2Footnote 3Footnote 4. Although data are limited, influenza vaccination is immunogenic and efficacious in a substantial proportion of individuals with HIVFootnote 5Footnote 6Footnote 7.
Live attenuated influenza vaccine (LAIV) is a type of seasonal influenza vaccine that is administered as an intranasal spray. The influenza viruses contained in LAIV are attenuated so that they do not cause influenza and are cold-adapted and temperature sensitive, so that they replicate in the nasal mucosa rather than the lower respiratory tract. A quadrivalent formulation of LAIV (FluMist® Quadrivalent, AstraZeneca) is currently authorized for use in Canada for individuals 2–59 years of age. There are several LAIV-specific contraindications, including for children and adults with immune compromising conditions. For these populations, inactivated influenza vaccine (IIV) has been recommended. NACI's previous recommendation against LAIV use for individuals with immune compromising conditions was based on expert opinion and the small number of studies in children and adults with mild to moderate immune suppression due to HIV infection and cancer (NACI Recommendation Grade D)Footnote 8.
Live vaccines are generally contraindicated in persons with immunodeficiency, out of concern that the live virus may cause disease in the host. However, for infections for which the disease burden is significant and live vaccines are the only option (e.g., measles), criteria have been established to permit vaccination when immune function is not severely impaired. Live attenuated vaccines, such as measles-mumps-rubella (MMR) and varicella vaccines, have been shown to be safe and are recommended for persons with HIV if the infection is controlled and immune function is satisfactory.
An environmental scan of recommendations on LAIV use in HIV-infected individuals from Canadian provinces and territories and from selected high income countries revealed that LAIV is contraindicated for HIV-infected individuals in British Columbia, Alberta, Manitoba, Saskatchewan, New Brunswick and in the United States (US)Footnote 1Footnote 2,Footnote 9Footnote 10Footnote 11Footnote 12Footnote 13Footnote 14, and for immunocompromised individuals in Ontario, Newfoundland and Labrador, YukonFootnote 15Footnote 16Footnote 17. Some jurisdictions, such as Quebec, the United Kingdom, and FranceFootnote 18Footnote 19Footnote 20 and professional organizations including the Infectious Diseases Society of America and the British Children's HIV AssociationFootnote 21Footnote 22 state that LAIV may be given to individuals with HIV who meet specific criteria. The product monograph for FluMist® Quadrivalent cautions that the administration of the vaccine to immunosuppressed individuals should be based on careful consideration of potential benefits and risks, but does not explicitly identify this vaccine as being contraindicated for this populationFootnote 23.
Guidance objective
The objective of this advisory committee statement is to review the efficacy and effectiveness, immunogenicity, and safety evidence on LAIV use in HIV-infected individuals and to provide updated guidance on the use of LAIV in this population.
II. Methods
The systematic review's methodology was specified a priori in a written protocol that included review questions, search strategy, inclusion and exclusion criteria, and quality assessment. NACI's Influenza Working Group (IWG) reviewed and approved the protocol.
Research question
What are the efficacy and effectiveness, immunogenicity, and safety of LAIV in HIV-infected individuals?
- P (population)
- HIV-infected individuals
- I (intervention)
- Live attenuated influenza vaccine
- C (comparison)
- Inactivated influenza vaccine or placebo given to HIV-infected individuals, LAIV given to individuals without HIV, or no comparator
- O (outcomes)
- Efficacy and effectiveness, immunogenicity, safety, and vaccine virus shedding
The search strategy was developed based on the research question and PICO in consultation with a librarian of the Health Library of Health Canada and PHAC (search strategy available upon request). The EMBASE, MEDLINE, Scopus, ProQuest Public Health, ClinicalTrials.gov, and PROSPERO electronic databases were searched for primary research articles and case reports from inception until April 13, 2018, using search terms for LAIV and HIV. Searches were restricted to articles published in English and French. In addition, hand searching of included studies was performed by checking reference lists to identify additional relevant publications. Hand searching of reference lists was also performed for any relevant retrieved secondary research articles. Two reviewers independently screened the records retrieved from database searches for relevance. They were initially screened by title and abstract for potential eligibility. The full-text of records deemed potentially eligible were obtained and further reviewed by both reviewers for potential inclusion in the review. Appendix A shows the PRISMA Flow Diagram. One reviewer extracted data and a second reviewer independently validated the extracted data. Two reviewers independently appraised study's quality using the criteria outlined by Harris et alFootnote 24. Any disagreements or discrepancies were resolved by discussion and consensus. The knowledge synthesis was performed by two NACI members, DM and ND, and was supervised by NACI's IWG.
Studies were included if they met the following criteria:
- The study population or subpopulation consisted of HIV-infected individuals; and
- The study assessed efficacy or effectiveness, immunogenicity, safety (including impact on markers of HIV infection), or vaccine virus shedding following LAIV receipt.
Studies were excluded if they met one or more of the following criteria:
- The study did not present data on any of: efficacy and effectiveness, immunogenicity, safety or vaccine virus shedding outcomes for LAIV;
- The study was in a language other than English or French;
- The study was a non-human or in vitro study;
- The article was an editorial, opinion, or news report;
- The study presented only secondary research (e.g., literature review, systematic review, meta-analysis); or
- The LAIV investigated was not a seasonal LAIV based on the Ann Arbor backbone.
Canadian Adverse Events Following Immunization Surveillance System
AE following immunization are monitored through the Canadian Adverse Events Following Immunization Surveillance System (CAEFISS). A search was performed through CAEFISS to identify reports on AE following vaccination with LAIV in HIV-infected individuals. Reports with a vaccine trade name of FluMist® or FluMist® Quadrivalent and mention of keywords (e.g. HIV, HIV infection, AIDS, etc.) in medical history or supplementary information were returned.
Recommendation Development
Following critical appraisal of individual studies, summary tables with ratings of the quality of evidence using NACI's methodological hierarchy (Table 3, table 4 and table 5) were prepared, and proposed recommendations for vaccine use developed. Following thorough review of the evidence, NACI approved the recommendation contained in this statement on June 5, 2019. The description of relevant considerations, rationale for specific decisions, and knowledge gaps are described in the following sections.
III. Use of LAIV in HIV-infected individuals
III.1 LAIV preparation authorized for use in Canada
LAIV is given as an intranasal spray. The influenza viruses contained in LAIV are attenuated so that they do not cause influenza and are cold-adapted and temperature sensitive, so that they replicate in the nasal mucosa, rather than the lower respiratory tract. A quadrivalent LAIV (LAIV4; FluMist® Quadrivalent) is authorized for use in Canada for individuals 2–59 years of age. The trivalent LAIV (LAIV3; FluMist®, AstraZeneca) is no longer available in Canada.
| Route of administration | Dosage | Clinically relevant non-medicinal ingredients |
|---|---|---|
| Intranasal | Each 0.2 mL dose contains 106.5-7.5 fluorescent focus units of live attenuated reassortants given as 0.1 mL in each nostril. |
|
III.2 Vaccine efficacy and effectiveness
No studies on the efficacy or effectiveness of LAIV in HIV-infected individuals were identified.
III.3 Vaccine immunogenicity
III.3.1 Correlates of Protection against Influenza Infection
For hemagglutination inhibition (HI) serological assessments, an HI titre of 1:40 has been suggested to correlate with an efficacy of 50–70% against clinical symptoms of influenza in healthy adults, but may vary, depending on individual characteristics, population, age, and vaccine typeFootnote 25. A similar correlate for protection between antibody titre and vaccine efficacy has not been determined for children. The concentration of observed serum HI antibodies is calculated as the geometric mean titre (GMT), which is the mean of the logarithmic values of serum antibody titres. Seroprotection rate is the proportion of subjects achieving an HI titre of ≥1:40 post-vaccination. Seroconversion rate is the proportion of subjects achieving significant increase from pre- to post-vaccination HI titres (≤1:10 to ≥1:40 or ≥4-fold rise in HI titres). Fold rise is the ratio of post- and pre-vaccination HI titres. Correlates of protection against influenza have not been well-established for other assessments of humoral immunity, such as microneutralization (MN) assayFootnote 26, and assessments of cell-mediated immunity.
III.3.2 Characteristics of Immunogenicity Studies
Three studies investigated the immunogenicity of LAIV in a total of 191 HIV-infected children and young adults 2–25 years of ageFootnote 27Footnote 28Footnote 29 and one study investigated the immunogenicity in 28 HIV-infected adults 18 years of age and olderFootnote 30. All four studies were of good quality according to ratings of Harris et al (2001)Footnote 24. Key study characteristics are summarized in table 2. Additional details on the studies assessing immunogenicity can be found in table 7.
| Author | Study design (vaccine administered) | Study population | Outcomes |
|---|---|---|---|
| King et al. (2000)Table 2: Tablenote 1 | RCT (LAIV3 vs. placebo) | Adults 18–58 years of age with HIV (n=57 total; 28 received LAIV3) and without HIV (n=54 total; 27 received LAIV3) Eligibility criteria for HIV-infected subject: Immune class A1-2, plasma HIV RNA <10,000 copies/mL, and >200 CD4 cells/µL (and if ≤500 CD4 cells/µL, be on stable antiretroviral regimen) within three months prior to vaccination. |
HI antibody response |
| King et al. (2001)Table 2: Tablenote 2 | RCT (LAIV3) | Children less than 8 years of age with HIV (n=24) and without HIV (n=25) Eligibility criteria for HIV-infected subject: Immune class N1-2 or A1-2 and plasma HIV RNA <10,000 copies/mL within 100 days prior to enrolment. |
HI antibody response |
Levin et al. (2008)Table 2: Tablenote 3 Weinberg et al. (2010a)Table 2: Tablenote 4 Weinberg et al. (2010b)Table 2: Tablenote 5 |
RCT (LAIV3 vs. IIV3) | Children 5 to less than 18 years of age with HIV (n=243 total; 122 received LAIV3 and 121 received IIV3) Eligibility criteria for HIV-infected subject: Stable HIV on HAART for ≥16 weeks and with HIV-1 plasma HIV RNA <60,000 copies/mL within 60 days prior to vaccination. All subjects had received IIV3 in at least one of the prior two years. |
HI and MN antibody response; Salivary mucosal IgA and IgG antibody response; T cell response. |
Curtis et al. (2015)Table 2: Tablenote 6 Weinberg et al. (2016) |
Prospective cohort study (LAIV4) | Children and young adults 2–25 years of age with HIV (n=45) and without HIV (n=55) Eligibility criteria for HIV-infected subject: CD4 >15% or >200 cells/µL on cART, or >25% or >500 cells/µL if not on cART. All subjects had received influenza vaccine in one or more previous seasons. |
HI and MN antibody response; Nasal mucosal IgA response; IgA and IgG memory B cell response; T cell response. |
| Abbreviations: cART, combination antiretroviral therapy; HAART, highly active antiretroviral therapy; HI, hemagglutination inhibition; HIV, human immunodeficiency virus; IgA: immunoglobulin A; IgG: immunoglobulin G; IIV3, trivalent inactivated influenza vaccine; LAIV3, trivalent live attenuated influenza vaccine; LAIV4, quadrivalent live attenuated influenza vaccine; MN, Microneutralization; RCT, randomized controlled trial; RNA, ribonucleic acid.
Table 2: Tablenotes
|
|||
III.3.3 Hemagglutination Inhibition Antibody Response
Three studies looked at HI antibody response to LAIV in HIV-infected children and young adultsFootnote 27Footnote 28Footnote 29 and one looked at the response to LAIV in HIV-infected adultsFootnote 30.
Response by HIV infection status
The King et al. (2001) RCT on LAIV3 in children with and without HIV found that after one dose of LAIV, 59% of the HIV-infected and 76% of the non-HIV infected children achieved seroprotection against at least one of the three vaccine strainsFootnote 27. Seroprotection against at least one of the three vaccine strains increased to 77% for HIV-infected and 83% for non-HIV infected children 28–35 days after administration of the second LAIV dose. There was no statistically significant difference between the rate and magnitude of serologic responses of the HIV-infected and non-HIV infected children.
In the Curtis et al. (2015) prospective cohort study, pre- and post-vaccination seroprotection rates were not statistically different between the HIV-infected and non-HIV infected children and young adults for all four vaccine strains contained in LAIV4Footnote 29. HI antibody responses were modest, such that the proportions of subjects with titres ≥1:40 at 14–21 day post-vaccination did not differ from baseline for A(H1N1), A(H3N2), and B/Victoria in either group. For B/Yamagata, seroprotection rate significantly increased in the HIV-infected group (p=0.03), but not in the non-HIV infected group.
In the King et al. (2000) RCT on LAIV3 vs. placebo in adults with and without HIV, the level of seroprotection before vaccination was high and very few individuals in any group showed a ≥4-fold rise in HI titres after vaccinationFootnote 30. GMT pre- and 28–35 days post-vaccination did not differ significantly among trial groups.
Response by vaccine type
The Levin et al. (2008) RCT on LAIV3 vs. trivalent IIV (IIV3) in children with HIV found that the proportions with HI titres ≥1:40 at baseline and at 4 and 24 weeks post-vaccination were similar in the two groups for A(H1N1) and A(H3N2), but higher with IIV3 for influenza BFootnote 28 at all three time points. The proportions with a 4-fold increase in titer for A(H1N1) were similar for LAIV3 and IIV3; however, significantly more IIV3 recipients had a 4-fold increase in titer against A(H3N2) and B. GMT after receipt of LAIV3 and IIV3 were similar for A(H1N1), but were significantly higher after receipt of IIV3 for A(H3N2) and B. Multivariate linear regression analyses showed direct relationships between pre- and 4 weeks post-vaccination GMT for all three strains with both LAIV3 and IIV3.
Response to mismatched strains
The Levin et al. (2008) RCT found that HI antibody responses to mismatched A(H3N2) and B strains not contained in the vaccines administered were increased with both LAIV3 and IIV3 at 4 and 24 weeks post-vaccination. However, IIV3 recipients had statistically significantly higher HI titres compared with LAIV3 recipients against the mismatched A(H3N2) and B strains at 4 and 24 weeks post-vaccination (p<0.0003 for the comparisons)Footnote 31.
The Curtis et al. (2015) retrospective cohort study looked at HI antibody responses in HIV-infected and non-HIV infected children and young adults following LAIV4 to the A(H1N1) and B/Yamagata vaccine strains, and additionally the drifted circulating A(H1N1) strain for the 2013–2014 seasonFootnote 33. HI titres significantly increased 14–21 days post-vaccination against all three viruses (p≤0.02) and pre- and post-vaccination titres did not differ by HIV status pre- and post-vaccination and significantly increased 14–21 days post-vaccination against all three viruses (p≤0.02).
III.3.4 Microneutralization Antibody Response
Two studies looked at MN antibody response to LAIV in HIV-infected individualsFootnote 28Footnote 29.
Response by vaccine type
In the Levin et al. (2008) RCT, the proportion of HIV-infected children with MN titres of ≥1:40 were similar for LAIV3 and IIV3 at baseline and at 4 and 24 weeks post-vaccination for all three vaccine strainsFootnote 28Footnote 31. At 4 and 24 weeks post-vaccination, there were statistically significant increases in MN titres against all vaccine strains in LAIV3 and IIV3 recipients, but MN titres at 4 weeks post-vaccination were 2–3 fold higher with IIV3 than with LAIV3 (p≤0.002). In multivariate analysis, only the plasma HIV viral load was inversely associated with MN responses to all three vaccine strains in IIV3 recipients and to A(H1N1) in LAIV3 recipients.
Response to a mismatched strain
MN titres against the vaccine A(H1N1) strain and a mismatched circulating A(H1N1) strain were measured 14-21 days after vaccination with LAIV4. Titres increased significantly for both strains in non-HIV infected children and young adults. However, in HIV-infected children and young adults, the increase was only significant for the mismatched circulating A(H1N1) strainFootnote 33.
III.3.5 Mucosal Immunoglobulin A and Immunoglobulin G Antibody Response
Two studies looked at mucosal immunoglobulin A (IgA) antibody responseFootnote 28Footnote 29 and one study looked at mucosal immunoglobulin G (IgG) antibody responseFootnote 28 in HIV-infected children and young adults. There were no studies that looked at these responses in HIV-infected adults over 25 years of age.
Response by HIV infection status
Nasal IgA antibody concentrations against the vaccine strains contained in LAIV4 were found in the Curtis et al. (2015) study to have significantly increased post-vaccination in HIV-infected and non-infected children and young adults (p<0.05). Post-vaccination there was also an increase in antibody concentration against the drifted circulating A(H1N1) strain in HIV-infected children but not in the non-HIV infected groupFootnote 29Footnote 33. There were no significant differences in nasal IgA concentrations against any strain by HIV status, with the exception of post-vaccination IgA levels for B/Victoria, which were significantly higher in the HIV-infected group. IgA response occurred earlier and, for influenza A strains, persisted longer in the non-HIV infected group compared with the HIV-infected group.
No study looked at mucosal IgG antibody response in HIV-infected individuals compared to non-HIV infected individuals.
Response by vaccine type
In the Levin et al. (2008) RCT, both LAIV3 and IIV3 were found to increase salivary IgG antibodies in HIV-infected children. The increase was significantly higher with IIV3 than with LAIV3 at 4 weeks post-vaccination, but there was no significant difference between the groups at 24 weeks post-vaccination. Multivariate analysis showed that salivary IgG responses at 4 weeks post-vaccination to either vaccine were directly associated with baseline salivary IgG antibody concentrations and inversely associated with baseline plasma HIV viral loadFootnote 28Footnote 31. Salivary IgA antibody responses were detected only in a minority of participants and therefore no meaningful findings were reportedFootnote 28Footnote 31.
III.3.6 IgA/IgG memory B Cell Response
Only one study investigated IgA/IgG memory B cell response to LAIV in HIV-infected children and young adultsFootnote 29. None of the studies investigated this response in HIV-infected adults aged over 25 years.
Response by HIV infection status
The Curtis et al. (2015) prospective cohort study, supplemented with data from Weinberg at al. (2016), of children and young adults found that HIV status was not associated with any differences in IgG memory B cell pre-LAIV4 vaccination responses to the A(H1N1) and B/Yamagata vaccine strains or to the drifted circulating A(H1N1) strain. There were no significant differences in responses at 14–21 days post-vaccination by HIV status for the A(H1N1) vaccine strain or the A(H1N1) drifted strain; however, IgG memory B cell response for B/Yamagata vaccine strain was lower in the HIV-infected group than in the non-HIV infected group (p=0.04)Footnote 33. Most study subjects did not have detectable IgA memory B cells before or after vaccination for any of the influenza strains, regardless of HIV statusFootnote 33.
III.3.7 T cell Response
Two studies investigated T cell response to LAIV in HIV-infected children and young adultsFootnote 28Footnote 29. None of the studies investigated T cell response to LAIV in HIV-infected adults aged over 25 years.
Response by HIV infection status
HIV-infected children and young adults in the Curtis et al. (2015) study had lower T cell responses than non-HIV infected participants to all vaccine strains contained in LAIV4 pre-vaccination (p≤0.06) and lower responses at 14–21 days post-vaccination to the vaccine and drifted circulating A(H1N1) strains (p≤0.04), but not to B/Yamagata. The fold-rise in T cell responses from pre- to post-vaccination did not differ by HIV statusFootnote 33.
Response by vaccine type
In a sub-analysis of the Levin et al. (2008) RCT of children with HIV, an unexpected decrease in T cell response was found for both LAIV3 and IIV3. At 4 and 24 weeks post-vaccination, IIV3 resulted in a significantly greater decrease in T cell response for the all influenza strains compared to LAIV3 (p≤0.02). Nonspecific responses to phytohemagglutinin also tended to decrease at 4 weeks after receipt of IIV3 compared with LAIV3 (p=0.07), but rebounded at 24 weeksFootnote 32.
III.4 Vaccine safety
Five studies reported AE following LAIV; three in HIV-infected children and young adultsFootnote 27Footnote 28Footnote 29 and two in HIV-infected adultsFootnote 30Footnote 34. Effects on HIV infection following receipt of LAIV were assessed in three studies; two in HIV-infected childrenFootnote 27Footnote 28 and one in HIV-infected adultsFootnote 30. Four of the studies were of good quality, and one was rated as fair. Additional details on the studies assessing vaccine safety can be found in table 8.
III.4.1 Adverse Events Following Immunization
Adverse events by HIV infection status
A RCT of children with HIV (n=24) and without HIV (n=25) who received two doses of LAIV3 found no significant difference in number or duration of AE, including fever events and influenza-like illness (ILI), by HIV statusFootnote 27. There was one episode of ILI after 38 doses of LAIV in children with HIV and two episodes of ILI after 49 doses in children without HIV.
In a prospective cohort study of children and young adults aged 2–25 years with HIV (n=45) or without HIV (n=55) who received LAIV4, muscle aches and decreased energy occurred significantly more frequently in the HIV-infected group compared to the non-HIV infected group (17.8% vs. 3.6%, p=0.04 and 24.4% vs. 5.4%, p=0.01, respectively)Footnote 29. No other expected or unsolicited AE, including runny nose and nasal congestion, differed between the two groups.
In a placebo-controlled RCT of LAIV3 use in adults with HIV (n=57 total; 28 received LAIV3) and without HIV (n=54 total; 27 received LAIV3), the rate of runny nose/nasal congestion was statistically significantly higher in LAIV3 recipients than placebo overall, but did not differ between the HIV-infected and non-HIV infected recipients of LAIV3 (61% vs. 78%)Footnote 30. There were no significant differences in rates of other AE between LAIV and placebo recipients, or by HIV status.
Adverse events by vaccine type
In an RCT of children with HIV who received LAIV3 (n=122) or IIV3 (n=121), AE within 28 days of vaccination were similar for the two groups except for injection site reactions after IIV3 (23%) and more frequent nasopharyngeal symptoms after LAIV3 than IIV3 (52% vs. 31%, p=0.002)Footnote 28. Pulmonary signs and symptoms, including asthma, wheezing, cough, chest pain and pneumonia, were not significantly different after LAIV3 than IIV3 (32% vs. 26%). Severity of reactions was also similar for the two groups.
Menegay et al. (2017) conducted a retrospective cohort study on ILI occurring within 30 days after vaccination with IIV or LAIV in HIV-infected US Air Force members. Of all active Air Force members diagnosed with HIV infection who received influenza vaccines over a ten year period, only one of 121 LAIV vaccinations (0.8%) was followed by an ILI diagnosis (defined as visits with an ICD-09 code for fever, an included acute respiratory code, or unspecified viral illness) within the 30-day post-vaccination period, compared to 16 ILI diagnoses associated with IIV. The number of IIV vaccinations was not statedFootnote 34.
No serious or severe AE attributable to LAIV were reported in any study.
Canadian Adverse Events Following Immunization Surveillance System
Since 2010 when LAIV was first licensed for use in Canada, there have been no reports of AE following vaccination with LAIV in HIV-infected individuals of any age.
III.4.2 Effects on HIV Infection
In two studies of children with HIV (n=146 total), LAIV3 had no significant effect on HIV RNA viral load or CD4 countFootnote 27Footnote 28. One placebo-controlled study of adults with HIV who received LAIV3 (n=28) also showed no significant effect on HIV RNA viral load or CD4 count compared to placebo recipients (n=29)Footnote 30.
III.4.3 Vaccine Virus Shedding
Four studies reported on the effect of HIV status on LAIV vaccine virus shedding; three in HIV-infected children and young adultsFootnote 27Footnote 28Footnote 29 and one in HIV-infected adultsFootnote 30.
Vaccine virus shedding by HIV infection status
In two studies that looked for LAIV vaccine virus shedding in a total of 65 children and young adults with HIV and 80 without, there were no significant differences by HIV status in the proportions of subjects who shed vaccine virus, the quantity of virus shedFootnote 27Footnote 29, the types of virus shed, or the timing or duration of sheddingFootnote 29. In a study of adults, shedding of LAIV vaccine virus was infrequent; one of 28 HIV-infected adults shed vaccine virus while none of the 27 non-HIV infected adults shed vaccine virusFootnote 30. While another study did not report how many HIV-infected children shed vaccine virus, the authors stated that the frequency of shedding of vaccine virus was similar to that previously reported in both HIV-infected and non-HIV infected children, as well as in HIV-infected adultsFootnote 28.
Immunologic predictors of vaccine virus shedding
Two studies investigated associations between various baseline immunologic parameters and vaccine virus sheddingFootnote 28Footnote 29.
In a study of 113 HIV-infected children who received LAIV3Footnote 28, shedders of A(H1N1) had significantly lower HI and MN titres at baseline than children without shedding (p<0.001 for both)Footnote 31. A similar but non-significant trend was also seen for HI and MN titres with shedding of BFootnote 31 and for HI titres with A(H3N2)Footnote 28. There were increased concentrations of salivary IgG and IgA at baseline in non-shedders compared to shedders of any influenza vaccine strain (p=0.05 and 0.02, respectively). Neither HI nor MN baseline titres of ≥1:40 were completely protective against sheddingFootnote 31.
A study of LAIV4 in children and young adults found no significant association between pre-vaccination serum HI or mucosal IgA antibody levels and vaccine virus shedding in 45 HIV-infected recipientsFootnote 29. In non-HIV infected recipients, high pre-vaccination serum HI titres were found to be significantly associated with low shedding of B/Victoria and B/Yamagata (p<0.001), and high baseline nasal IgA concentrations were significantly associated with low B/Yamagata shedding (p=0.01)Footnote 29.
IV. Discussion
The present systematic review identified eight articlesFootnote 27Footnote 28Footnote 29Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34 that reported on five studies investigating the immunogenicity, the safety or both, of the administration of LAIV in HIV-infected individuals. Of the five studies identified, four were of good quality and one was fair. Common methodological concerns included small sample sizeFootnote 27Footnote 30 and differences between study groups at baselineFootnote 28Footnote 29Footnote 31Footnote 32Footnote 33.
Immunogenicity was studied in a total of 191 children and adults aged <25 years plus 28 adults over 18 years of ageFootnote 27Footnote 28Footnote 29Footnote 30Footnote 31Footnote 32Footnote 33. For serological responses, there were no major differences in HI antibody responses following receipt of LAIV between individuals with and without HIVFootnote 27Footnote 29Footnote 30. In the study of Curtis et al. (2015), HI response to influenza B/Yamagata was better in the group with HIV than in the HIV negative control group. The HIV positive group was significantly older than the HIV negative group, which should have biased the results towards a lower response in this groupFootnote 29Footnote 33.
Significant increase in MN titres was observed against mismatched, but not the vaccine A(H1N1) strain in a study of HIV-infected children and young adultsFootnote 29Footnote 33.
The proportions of HIV-infected individuals with HI titers of ≥40 to LAIV and IIV were similar for influenza A(H1N1) and A(H3N2) but higher with IIV for influenza B and antibody titers were statistically significantly higher with IIV for influenza A(H3N2) and B vaccine strainsFootnote 28 and for mismatched strainsFootnote 31.
The proportion of HIV-infected individuals with MN titres ≥1:40 was similar post-vaccination for LAIV and IIV, but the magnitude of response was higher for IIV than LAIVFootnote 31. As noted earlier, immunologic correlates of protection against influenza are relatively well established for HI antibodies for adults, but not for MN antibodies for adults and not for any serological response for children.
LAIV induces humoral and mucosal antibody responses as well as T cell responses, mimicking to some extent infection with wild strain influenza virus. Correlates of protection have not been established for LAIV, and HI titre may underestimate protectionFootnote 35. Mucosal IgA response or cell-mediated immunity have been suggested as contributing to protection after LAIV but have not been validated as correlates of protection (Weinberg 2016).
Only two studies looked at mucosal antibody responses. The available data suggest that there is no important difference in nasal IgA antibody response to LAIV by HIV statusFootnote 29Footnote 33, or in salivary IgG antibody response to LAIV and IIV in HIV-infected individualsFootnote 28Footnote 31.
There is a paucity of evidence for cell-mediated responses. One study investigated memory B cell responses and T cell responses in children and young adults. IgG memory B cell responses did not significantly differ by HIV status for influenza A(H1N1) or A(H3N2); however, a lower absolute response to B/Yamagata post-vaccination was observed in the HIV-infected groupFootnote 29Footnote 33. The magnitude of the rise in T cell response did not differ by HIV statusFootnote 29Footnote 33. An earlier study in children with HIV found that, contrary to previous results in healthy children, T cell responses to both LAIV and IIV decreased below baseline post-vaccination, more so with IIV than with LAIVFootnote 28Footnote 32. Similar results have not been reported elsewhere. Note that the immunologic correlates of cell-mediated responses for protection against influenza have not been well established.
AE following LAIV were studied in a total of 191 children and young adults (<25 years of age) and in 28 adults (with another 61 adults investigated only for vaccine-associated ILI)Footnote 27Footnote 28Footnote 29Footnote 30Footnote 34. In both children and adults with HIV, rates of AE, including fever events and ILI, following receipt of LAIV were comparable to rates observed in individuals without HIV receiving LAIV except for more muscle aches and decreased energy in those with HIVFootnote 27Footnote 29Footnote 30. Rates of AE in individuals with HIV receiving LAIV or IIV were also similarFootnote 28Footnote 34, with the exception of more frequent but expected nasopharyngeal symptoms (runny nose and nasal congestion) after LAIVFootnote 28.
Reports of ILI post-LAIV were rare. There were no serious adverse events (SAE) attributable to LAIV reported in HIV-infected subjects in any of the studies. However, the total number of subjects assessed is insufficient to detect uncommon or rare AEFootnote 36. No AE were reported through CAEFISS. Given the small number of HIV-infected children in Canada, LAIV use would likely not have been sufficient to detect rare AE. It should also be noted that prior to the release of this Statement, NACI considered the use of LAIV in individuals infected with HIV to be contraindicated. LAIV also had no significant impact on HIV RNA viral load or CD4 countFootnote 27Footnote 28Footnote 30. Vaccine virus shedding was studied in 191 children and young adults and 28 adults with HIV and did not differ by HIV infection statusFootnote 27Footnote 28Footnote 29Footnote 30.
No studies were identified on the efficacy or effectiveness of LAIV in children or adults with HIV infection. However, studies with sufficient sample size required to address this evidence gap may not be feasible, particularly in children, given the limited numbers of children with HIV in high income countries where LAIV is used.
V. Recommendations
The following section outlines the recommendations that NACI has made regarding the use of LAIV in HIV-infected individuals. Additional information on the strength of NACI recommendations and the grading of evidence is available in table 4.
V.1 Recommendations for individual level decision-making
- NACI recommends that LAIV may be considered as an option for children 2–17 years of age with stable HIV infection on highly active antiretroviral therapy (HAART) and with adequate immune functionFootnote * (Discretionary NACI recommendation).
- NACI concludes that there is fair evidence (based on immunogenicity data) to recommend the use of LAIV vaccine as an option for children 2–17 years of age with stable HIV infection on HAART and adequate immune function (Grade B Evidence).
- NACI concludes that there is insufficient evidence to detect uncommon AE related to the use of LAIV in HIV infected children. LAIV appears to have a similar safety profile to IIV (Grade I Evidence).
Endnotes
- Endnote *
-
LAIV should only be considered in children with HIV who meet the following criteria:
- Receiving HAART for ≥4 months;
- CD4 count ≥500/µL if 2–5 years of age, or ≥200/µL if 6–17 years of age (measured within 100 days before administration of LAIV); and
- HIV plasma RNA <10,000 copies/mL (measured within 100 days before administration of LAIV).
These criteria were based upon those used in the studies of LAIV in children with HIVFootnote 27Footnote 28Footnote 29, relevant guidance from reputable international organizationsFootnote 19Footnote 20Footnote 21, NACI's guidance regarding the use of live attenuated MMR and varicella vaccines in individuals with HIV infectionFootnote 37, and the revised United States Centers for Disease Control and Prevention (CDC) immune classification criteria for pediatric HIV infectionFootnote 38. Where thresholds from these sources differed, the most stringent criteria were selected.
Intramuscular (IM) influenza vaccination still is considered the standard for children living with HIV by NACI and CPARG, particularly for those without HIV viral load suppression (i.e. plasma HIV RNA >40 copies/mL). However, if IM vaccination is not accepted by the patient or substitute decision maker, LAIV would be reasonable for children meeting the criteria outlined above.
Summary of evidence and rationale
NACI concludes that LAIV is immunogenic in children on HAART with stable HIV infection and adequate immune function. This recommendation is "discretionary"; therefore, the decision to use LAIV in children with stable HIV should be made on a case-by-case basis. The evidence is considered Grade B as there is no direct evidence on the efficacy or effectiveness of LAIV in HIV-infected individuals and the sample size for the evidence base is small.
- There is evidence that LAIV is immunogenic in children 2–17 years of age with stable HIV infection on HAART and with adequate immune function
- LAIV appears to have a similar safety profile to IIV; however, the evidence base is too small to effectively detect uncommon, rare, and very rare AE related to the use of LAIV in HIV-infected children.
- Children with HIV receive all the routine childhood vaccines and additional parenteral vaccines warranted by their actual or potential immunocompromised stateFootnote 37 Therefore, offering intranasal LAIV instead of IIV avoids one IM injection annually, and may improve acceptance of the seasonal influenza vaccineFootnote 39Footnote 40.
NACI concluded that the quantity of evidence available on the immunogenicity and safety of LAIV in adults with HIV is insufficient to justify a recommendation for the use of LAIV in this group. (Grade I Evidence). This recommendation is based on expert opinion. In addition, NACI considered that most studies have found LAIV to have similar or slightly lower efficacy than IIV in adultsFootnote 8 and consequently recommends IIV for adults with chronic conditions. Therefore, IIV remains the recommended formulation of influenza vaccine for adults with HIV and LAIV remains contraindicated in this population.
V.2 Management options
With the publication of this NACI Statement, there are two influenza vaccines that may be used in children with HIV infection. The decision on which vaccine option is preferable depends on availability and key considerations for each vaccine. The relative merits of both vaccines are summarized in table 3.
| Options | Factors for consideration | Decision points |
|---|---|---|
| 1. IIV | Immunogenicity IIV may be immunogenic in immunocompromised individuals depending on the degree of immune compromise. Safety IIV has been shown to be safe for HIV-infected individuals, and inactivated vaccines in general are safe for immunocompromised individuals. Acceptability IIV is given as an IM injection, which still is considered the standard for influenza vaccination in this group by NACI and CPARG. |
Immunogenicity Both vaccines are immunogenic but stimulate different types of immune responses. Safety Both vaccines appear to have similar safety profiles with regard to frequency and severity of AE, although injection site reactions were seen only with IIV and nasal symptoms were more common with LAIV. Although no safety concerns have been identified, the presence of uncommon AE related to LAIV in individuals with HIV is not known. Acceptability Some children and their parents may prefer intranasal vaccination; however, individual preferences vary. Therefore, a discussion with the patient or substitute decision maker on their preference for route of administration should take place prior to vaccination. |
| 2. LAIV | Immunogenicity LAIV is immunogenic in HIV-infected children with mild or moderate immunosuppression. Safety The sample sizes from studies assessing safety are not sufficient to detect uncommon AE. Acceptability LAIV is given intranasally, into both nostrils. Influenza vaccine given intranasally may be preferred to IM injection by some children and their parents. |
Tables
Table 4. NACI recommendations: Strength of recommendation and grade of evidence
Strength of NACI recommendation
Based on factors not isolated to strength of evidence (e.g. public health need)
Strong
"should/should not be offered"
-
Known/Anticipated advantages outweigh known/anticipated disadvantages ("should"),
OR Known/Anticipated disadvantages outweigh known/anticipated advantages ("should not")
- Implication: A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present
Discretionary
"may be considered"
- Known/Anticipated advantages closely balanced with known/anticipated disadvantages, OR uncertainty in the evidence of advantages and disadvantages exists
- Implication: A discretionary recommendation may be considered for some populations/individuals in some circumstances. Alternative approaches may be reasonable
Grade of evidence
Based on assessment of the body of evidence
- A: good evidence to recommend
- B: fair evidence to recommend
- C: conflicting evidence, however other factors may influence decision-making
- D: fair evidence to recommend against
- E: good evidence to recommend against
- I: insufficient evidence (in quality or quantity), however other factors may influence decision-making
| Level | Description |
|---|---|
| I | Evidence from randomized controlled trial(s). |
| II-1 | Evidence from controlled trial(s) without randomization. |
| II-2 | Evidence from cohort or case-control analytic studies, preferably from more than one centre or research group using clinical outcome measures of vaccine efficacy. |
| II-3 | Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence. |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees. |
| Quality Rating | Description |
|---|---|
| Good | A study (including meta-analyses or systematic reviews) that meets all design- specific criteriaTable 6 tablenote * well. |
| Fair | A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criterionTable 6 tablenote * but has no known "fatal flaw". |
| Poor | A study (including meta-analyses or systematic reviews) that has at least one design-specificTable 6 tablenote * "fatal flaw", or an accumulation of lesser flaws to the extent that the results of the study are not deemed able to inform recommendations. |
Table 6 Tablenotes
|
|
| Study details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study design | Participants | Summary of key findings | Level of evidence | Quality |
| King JC, Treanor J, Fast PE, Wolff M, Yan L, Iacuzio D, Readmond B, O'Brien D, Mallon K, Highsmith WE, Lambert JS, Belshe RB. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)–infected and non–HIV-infected adults. J Infect Dis 2000;181:725-8Table7: tablenote 1 | LAIV3 | RCT US multicentre Influenza season unknown Funded by the NIH and Aviron (Mountain View, CA) |
Adults 18–58 years of age HIV+: 51% female mean age, 40 years 28 vaccinated with LAIV3 29 received placebo HIV-: 65% female mean age, 34 years 27 vaccinated with LAIV3 27 received placebo HIV+ adults were considered eligible if they met the following criteria: CDC class A1-2, plasma HIV RNA PCR <10,000 copies/mL, >200 CD4 cells/µL within 3 months prior to vaccination and on stable antiretroviral regimen if CD4 ≤500 cells/µL. |
Pre-vaccine: % with HI titre <1:8: Sub-table-1 View data Seroconversion rate 28–35 days post-vaccination: Sub-table-2 View data There were no important differences in HI GMT titres before and 28–35 post-vaccination in any participant group. |
I | Good Small sample size. |
King JC, Fast PE, Zangwill KM, Weinberg GA, Wolff M, Yan L, Newman F, Belshe RB, Kovacs A, Deville JG, Jelonek M. Safety, vaccine virus shedding and immunogenicity of trivalent, cold- adapted, live attenuated influenza vaccine administered to human immunodeficiency virus-infected and noninfected children. Pediatric Infect Dis J 2001; 20(12):1124-113Table7: tablenote 2 |
LAIV3 | RCT US multicentre 1999–2000 influenza season Funded by the NIH and Aviron (Mountain View, CA) |
Children 1–7 years of age HIV+: 24 children were vaccinated following schedule 1 or 2 46% female mean age, 4.7 years age range 1.0–7.9 years HIV-: 25 children were vaccinated following schedule 1 or 2 40% female mean age, 4.3 years age range 1.0–7.8 years Schedule 1: Day 0: LAIV3 (1st dose) Day 28–35: placebo Day 56–70: LAIV3 (2nd dose) Schedule 2: Day 0: placebo Day 28–35: LAIV3 (1st dose) Day 56–70: LAIV3 (2nd dose) HIV+ children were considered eligible if they met the following criteria: CDC class N1-2 or A1-2, HIV plasma RNA <10,000copies/mL, CD4 measured <100 days of enrolment. |
HI seroconversion rate 28–35 post-vaccination with 2nd dose of LAIV: Sub-table-3 View data Seroconversion rate 28–35 post-vaccination with 2nd dose of LAIV in children seronegative† at baseline: Sub-table-4 View data |
I | Good Small sample size. |
Levin MJ, Song LY, Fenton T, Nachman S, Patterson J, Walker R, Kemble G, Allende M, Hultquist M, Yi T, Nowak B. Shedding of live vaccine virus, comparative safety, and influenza-specific antibody responses after administration of live attenuated and inactivated trivalent influenza vaccines to HIV-infected children. Vaccine. 2008; 26: 4210–4217Table7: tablenote 3 Supplemented with additional details from Weinberg et al. (2010a) for MNTable7: tablenote 4 and Weinberg et al. (2010b) for CMI outcomesTable7: tablenote 5. |
LAIV3 | RCT US multicentre 2004–2005 influenza season Funded by the NIH |
HIV-infected children 5–18 years of age LAIV3: 122 HIV+ children vaccinated with LAIV3; 47% female; mean age, 11.4 years IIV3: 121 HIV+ children vaccinated with IIV3 (Fluzone®, Aventis Pasteur, Inc.); 47% female; mean age, 11.9 year Children were considered eligible if they met the following criteria: on stable HAART regimen for ≥16 weeks and HIV-1 plasma RNA <60,000 copies/mL within 60 days prior to screening. Must have received IIV in at least one of the previous 2 years Stratified into three groups by immunological status |
Pre-vaccine % with HI titre ≥40: Sub-table-5 View data HI GMT LAIV3/IIV3 ratios at 4 weeks and 24 weeks post-vaccination (LAIV3/IIV3): Sub-table-6 View data HI seroprotection rates post-vaccination: Sub-table-7 View data Difference in seroprotection rates post-vaccination (%IIV3-%LAIV3): Sub-table-8 View data HI seroconversion rates post-vaccination: Sub-table-9 View data Difference in seroconversion rates post-vaccination (%IIV3-%LAIV3): Sub-table-10 View data The antibody responses to LAIV3 and IIV3 were similar regardless of the HIV immunological group. HI GMT at 4 weeks post-vaccination were inversely related to baseline HIV RNA levels for LAIV3 for one strain [A(H3N2), p=0.02] and for IIV3 for all strains [A(H1N1), p=0.03; A(H3N2), p=0.05; B, p=0.004]. IIV3 HIV+ recipients had significantly higher GMT compared with LAIV3 recipients against mismatched A(H3N2) and B viruses at 4 and 24 weeks post-vaccination. HI titres against mismatched influenza strains: Sub-table-11 View data At 4 weeks post-vaccination, HI titres against A/Sydney (H3N2) and B/Yamanashi (not included in the vaccines administered), were increased with both LAIV3 and IIV3. IIV3 recipients had significantly higher HI titres compared with LAIV3 recipients at 4 and 24 weeks post-vaccination. Proportion of HIV-infected individuals with anti-influenza MN titres post-vaccination ≥1:40: Sub-table-12 View data Baseline MN titers were similar in the two arms. There were no significant differences between LAIV3 and IIV3 at p<0.05 level. The magnitude of MN response was significantly related to baseline MN titres and plasma HIV RNA in multivariate regression analysis. Both vaccines increased salivary IgG antibody levels. The increase in salivary IgG GMT was significantly higher in IIV3 than LAIV3 HIV+ recipients at week 4 (p=0.05), but not at week 24 (p>0.05). Magnitude of IgG response was significantly related to baseline IgG GMT in multivariate regression analysis. Salivary IgA antibodies detected only in a minority of participants. There were no significant increases in IgA GMT at 4 weeks post-vaccination. At 24 weeks post-vaccination IgA GMT were significantly higher compared to baseline in IIV3 recipients (p<0.01), but not in LAIV3 recipients (p>0.05). T cell response to A(H3N2) and B vaccine virus decreased significantly by 1.4 fold at 4 weeks post-vaccination with LAIV3 (p≤0.03), but was not significantly different from baseline at 24 weeks. T cell response to circulating and vaccine viruses decreased significantly by 1.5–3 fold at 4 weeks post-vaccination with IIV3 (p<0.001). IIV3 resulted in a significantly greater decrease in T cell response for influenza A strains compared to LAIV3 at 4 and 24 weeks post-vaccination (p≤0.02). There was no significant difference in T cell response for influenza B strains. IIV3 also resulted in a decrease in non-specific response to phytohemagglutinin. There were no differences by HIV immunologic status. |
I | Good HI test used cold-adapted antigen, which may underestimate HI response to A(H1N1) with IIVTable7: tablenote 3. Baseline higher proportion with titer of ≥40 for AHN2 and B in IIV vs LAIV groupTable7: tablenote 3. Salivary antibody may not reflect antibody production in the respiratory tractTable7: tablenote 4. |
Curtis D, Ning MF, Armon C, Li S, Weinberg A. Safety, immunogenicity and shedding of LAIV4 in HIV-infected and uninfected children. Vaccine. 2015; 33: 4790–4797Table7: tablenote 6 Supplemented with additional details from Weinberg et al. (2016) for CMI outcomesTable7: tablenote 7. |
LAIV4 | Prospective cohort study US Single centre 2013–2014 influenza season Funded by MedImmune and Colorado Clinical and Translational Sciences Institute |
Children and young adults 2–25 years of age HIV+: 45 subjects were vaccinated with LAIV4 37.8% female median age, 18 years; 22% < 9 years old HIV-: 55 subjects were vaccinated with LAIV4 45.5% female median age, 10 years; 40% <9 years old HIV+ individuals were eligible if they met the following criteria: CD4 >15% or >200 cells/µL on cART or >25% and >500/µL if not on cART All received influenza vaccine in previous season(s) |
HI seroprotection rates 14–21 days post-vaccination: Sub-table-13 View data There was no significant difference between HIV+ and HIV- individuals in pre- or post-vaccination seroprotection rates. HIV+ individuals had a significantly higher seroprotection rate to B/Yamagata (p=0.03) at 14–21 days post-vaccination than at baseline, but this was not significant when subdivided by <9 and ≥9 years of age. No other group was significantly different from baseline at 14–21 days. At baseline, ≥58% of participants had seroprotective titres against A(H1N1) and A(H3N2), while <10% had seroprotective titres against B. MN titres against the vaccine and circulating A(H1N1) strains were significantly increased in HIV- individuals at 14–21 days post-vaccination whereas only titres against the circulating A(H1N1) strain were significantly increased in HIV+ individuals. Baseline nasal mucosal IgA antibody levels were significantly higher in the HIV+ group for A(H1N1), A(H3N2), B/Victoria (p≤0.01), but not for B/Yamagata Significant increases from pre- to post-vaccination were noted for all strains by day 2–5 in HIV- individuals and by day 7–10 in HIV+ individuals. A(H1N1) IgA concentration was no longer significant at day 14–21 in HIV+ individuals. There were no significant differences in IgA antibody concentrations by HIV status. Median fold-increase in T cell response 14–21 days post-vaccination: Sub-table-14 View data HIV+ individuals had significantly lower T cell responses to the A(H1N1) vaccine strain and circulating strain than HIV- individuals before vaccination and at 14–21 days post-vaccination (p≤0.04). The difference in T cell response from pre-vaccination to post-vaccination did not differ by HIV status. There were no significant differences in IgG memory B-cell response at 14–21 days to A(H1N1) vaccine or circulating strain by HIV status but response to B/Yamagata in HIV+ individuals was significantly lower than in HIV- individuals [median interquartile range of 9 (0; 21) vs. 14 (6; 28); p=0.04]. |
II-2 | Good HIV+ group were older; this may have biased towards better responses in the HIV- group. HIV+ group had higher baseline nasal IgA antibody levels to three of the four viruses and would have biased towards a better response in the HIV- group. |
| Abbreviations: cART: combination antiretroviral therapy; CDC: Centers for Disease Control and Prevention (United States); CI: confidence interval; CMI: cell-mediated immunity; GMT: geometric mean titre; HAART: highly active antiretroviral therapy; HI: hemagglutination inhibition; HIV: human immunodeficiency virus; HIV+: HIV-infected; HIV-: non-HIV infected; IgA: immunoglobulin A; IgG: immunoglobulin G; IIV3: trivalent inactivated influenza vaccine; LAIV: live attenuated influenza vaccine; LAIV3: trivalent live attenuated influenza vaccine; LAIV4: quadrivalent live attenuated influenza vaccine; MN: microneutralization; NIH: National Institutes of Health (United States); RCT: randomized controlled trial; RNA: ribonucleic acid; US: United States.
Table 7: Tablenotes
|
||||||
| Study details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study design | Participants | Summary of key findings | Level of evidence | Quality |
| King JC, Treanor J, Fast PE, Wolff M, Yan L, Iacuzio D, Readmond B, O'Brien D, Mallon K, Highsmith WE, Lambert JS, Belshe RB. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)–infected and non–HIV-infected adults. J Infect Dis 2000;181:725-8Table 8: tablenote 1 | LAIV3 | RCT US multicentre Influenza season unknown Funded by the NIH and Aviron (Mountain View, CA) |
Adults 18–58 years of age HIV+: 51% female mean age, 40 years 28 vaccinated with LAIV3 29 received placebo HIV-: 65% female mean age, 34 years 27 vaccinated with LAIV3 27 received placebo HIV+ adults were considered eligible if they met the following criteria: CDC class A1-2, plasma HIV RNA PCR <10,000 copies/mL, >200 CD4 cells/µL within 3 months prior to vaccination and on stable antiretroviral regimen if CD4 ≤500 cells/µL. |
Proportion experiencing AE within 10 days:Sub-table-15 View data Runny nose/nasal congestion was higher with LAIV3 than placebo, but there was no significant difference based on HIV infection status. No SAE were attributable to LAIV3. Four possibly vaccine-related AE occurred 28–35 days after vaccination (clinical sinusitis and wheezing in HIV+ LAIV recipients; wheezing in an HIV+ placebo recipient; and bronchitis in an HIV- placebo recipient). All resolved without sequelae. Effects on HIV replication: No significant differences in plasma HIV RNA levels between LAIV3 and placebo recipients or between pre-vaccination levels and post-vaccination levels on days 7–10, 28–35, or 3 or 6 months. Three LAIV3 recipients had transient increases of ≥10-fold rise in HIV RNA levels that returned to baseline by the 90-day post-vaccination visit, and one placebo recipient had an increase which persisted to 90 days post-vaccination. No significant differences in CD4 cell counts between LAIV3 and placebo recipients or between pre-vaccination and post-vaccination (days 28–35 or 3 or 6 months) CD4 cell counts. No CD4 cell counts fell below 200 cells/µL within 1 month of vaccination. Vaccine virus shedding: One HIV+ LAIV3 recipient had a positive culture for vaccine virus (influenza B) 5 days after receiving LAIV3. No other LAIV shedding was detected. |
I | Good Small sample size. The paucity of AE could have been due to failure of LAIV to replicate in this group with high level of seroprotection pre- vaccine |
| King JC, Fast PE, Zangwill KM, Weinberg GA, Wolff M, Yan L, Newman F, Belshe RB, Kovacs A, Deville JG, Jelonek M. Safety, vaccine virus shedding and immunogenicity of trivalent, cold- adapted, live attenuated influenza vaccine administered to human immunodeficiency virus-infected and noninfected children. Pediatric Infect Dis J 2001; 20(12):1124-113Table 8: tablenote 2 | LAIV3 | RCT US multicentre 1999–2000 influenza season Funded by the NIH and Aviron (Mountain View, CA) |
Children 1–7 years of age HIV+: 24 children were vaccinated following schedule 1 or 2 46% female mean age, 4.7 years age range 1.0–7.9 years HIV-: 25 children were vaccinated following schedule 1 or 2 40% female mean age, 4.3 years age range 1.0–7.8 years Schedule 1: Day 0: LAIV3 (1st dose) Day 28–35: placebo Day 56–70: LAIV3 (2nd dose) Schedule 2: Day 0: placebo Day 28–35: LAIV3 (1st dose) Day 56–70: LAIV3 (2nd dose) HIV+ children were considered eligible if they met the following criteria: CDC class N1-2 or A1-2 and HIV plasma RNA <10,000 copies/mL. CD4 measured <100 days of enrolment. |
Proportion experiencing AE within 10 days of vaccination:Sub-table-16 View data Dose-related AE**: Sub-table-17 View data The following AE were reported 28-35 days following a dose of LAIV or placebo: 1st LAIV dose: HIV+ otitis media (2), upper respiratory infection (URI) (2), sinusitis; HIV- nasal irritation, and nasal congestion. 2nd LAIV dose: HIV+ URI (2); HIV- none. Placebo: HIV+ wheezing, cough, URI, otitis media; HIV- nasal burning. There were no significant differences in rates of AE, or AE reported as study dose-related, between HIV+ and HIV- children after LAIV dose 1 or 2 or after placebo. None of the AE identified were judged to be severe. SAE: 3 SAE occurred after LAIV in 2 HIV+ children, but none judged vaccine-related by the blinded clinical investigator. All resolved without sequelae. Effects on HIV replication: No significant changes in plasma HIV RNA levels, CD4 cell counts, or CD4% in HIV+ children after receiving either LAIV3 dose. Vaccine virus shedding: No significant prolonged or increased quantity of LAIV virus shedding occurred in HIV+ vs. HIV- children after receiving either LAIV3 dose. Three (13%) HIV+ LAIV3 recipients shed LAIV B virus and 7 (28%) HIV- LAIV3 recipients shed LAIV A, B, or both viruses. No shedding was detected after day 10 after receiving either LAIV3 dose. |
I | Good Small sample size. |
| Levin MJ, Song LY, Fenton T, Nachman S, Patterson J, Walker R, Kemble G, Allende M, Hultquist M, Yi T, Nowak B. Shedding of live vaccine virus, comparative safety, and influenza-specific antibody responses after administration of live attenuated and inactivated trivalent influenza vaccines to HIV-infected children. Vaccine. 2008; 26: 4210–4217Table 8: tablenote 3 | LAIV3 | RCT US multicentre 2004–2005 influenza season Funded by the NIH |
HIV-infected children 5–18 years of age LAIV3: 122 HIV+ children vaccinated with LAIV3; 47% female; mean age, 11.4 years IIV3: 121 HIV+ children vaccinated with IIV3 (Fluzone®, Aventis Pasteur, Inc.); 47% female; mean age, 11.9 years Children were considered eligible if they met the following criteria: on stable HAART regimen for ≥16 weeks and HIV-1 plasma RNA <60,000 copies/mL within 60 days prior to screening Stratified into three groups by immunological status Must have received IIV in at least one of the prior 2 years |
Proportion experiencing AE within 28 days:Sub-table-18 View data AE within 28 days of vaccination were similar after LAIV3 and IIV3 except for injection site reactions after IIV3 (23% overall) and nasopharyngeal symptoms after LAIV3 (52% vs. 31% after IIV3; p=0.002). AE did not differ by immunological group. No significant differences between immunological groups for toxicity grade 2 events (occurring in 16–31% of subjects) regardless of vaccine administered. There were 3 subjects with grade 3 events following LAIV3 (malaise, finger pain, and leg boil; one considered vaccine related) and 2 grade 3 events following IIV3 (fever, injection site lump; both considered vaccine related). No grade 4 events were reported. Effects on HIV replication: No significant increases from baseline in plasma HIV RNA levels 28 days or 6 months after LAIV3 or IIV3 in any of the immunological groups. CD4% did not change significantly at 28 days or 6 months after vaccination. Vaccine virus shedding: Influenza vaccine strains isolated from 347 specimens from 122 LAIV3 recipients: A(H1N1): 23 (6.6% of specimens); B: 11 (3.2%); A(H3N2): 3 (<1%). Five specimens contained two vaccine strains. No shedding was detected later than day 15 after LAIV3. HIV+ children who shed A(H1N1) had significantly lower baseline HI (p<0.001) and MN (p<0.001) titres than children without shedding post-vaccination. HIV+ children who shed B had non-significantly lower baseline HI and MN titres. Analysis of A(H3N2) shedding was not performed. influenza A(H1N1) shedders had significantly lower proportions of subjects with baseline protective HI or MN titres compared with non-shedders (p≤0.01). There was a trend towards lower prevalence of MN titres ≥1:40 among B shedders compared with non-shedders (p=0.06), but no difference in the proportions of subjects with HI titres ≥1:40. Neither baseline HI nor MN titres ≥1:40 were completely protective against vaccine virus shedding. Baseline salivary IgG and IgA antibody titres were significantly higher in HIV+ children who did not shed any strain compared to children who shed at least one strain (p=0.05 and 0.02, respectively). |
I | Good Unblinded RCT and more frequent clinic visits required for LAIV3 recipients could have contributed to reporting bias with respect to nasopharyngeal symptoms. |
| Curtis D, Ning MF, Armon C, Li S, Weinberg A. Safety, immunogenicity and shedding of LAIV4 in HIV-infected and uninfected children. Vaccine. 2015; 33: 4790–4797Table 8: tablenote 4 | LAIV4 | Prospective cohort study US single centre 2013–2014 influenza season Funded by MedImmune and Colorado Clinical and Translational Sciences Institute All received influenza vaccine in a previous season |
Children and young adults 2–25 years of age. HIV+: 45 children were vaccinated with LAIV4 37.8% female median age, 18 years; 22% <9 years HIV-: 55 children were vaccinated with LAIV4 45.5% female median age, 10 years; 40% <9 years Individuals were considered HIV+ if they met the following criteria: CD4 >15% or >200 cells/µL on cART or >25% and >500/µL if not on cART |
Proportion experiencing AE within 6 weeks:Sub-table-19 View data SAE: There were no vaccine-related SAE. Vaccine virus shedding: No difference between HIV+ and HIV- in type or number of LAIV viruses shed, timing or duration of shedding, or amount of LAIV virus shed. Shedding of any LAIV virus on day 7–10 was detected in 13 (31%) HIV+ and 11 (21%) HIV- subjects (p=0.4). Overall, 30 (67%) HIV+ and 28 (55%) HIV- subjects shed any LAIV virus up to 14–21 days post-vaccination (p=0.14). In HIV+, there were no significant associations between pre-vaccination HI or nasal IgA antibody levels and vaccine viral shedding. In HIV-, high pre-vaccination HI titres were associated with low shedding of B/Victoria and B/Yamagata (ρ≤-0.52, p<0.001) and high baseline nasal IgA concentrations were associated with low B/Yamagata shedding (ρ=-0.33, p=0.01). |
II-2 | Good HIV+ group significantly older than HIV- group. |
| Menegay JL, Xu X, Sunil TS, Okulicz JF. Live versus attenuated influenza vaccine uptake and post-vaccination influenza-like illness outcomes in HIV-infected US Air Force members. J Clin Virol. 2017; 95:72-75Table 8: tablenote 5 | LAIV (formulation not stated) IIV (formulation not stated) |
Retrospective cohort study No funding declared 2005–2015 |
All active duty US Air Force members diagnosed with HIV (n=437) 2% female 61 received LAIV at least once after HIV diagnosis (121 doses) 376 received only IIV after HIV diagnosis. (number of doses not stated) |
Post-vaccination ILI: There was one report of post-vaccination ILI after 121 doses of LAIV (0.8%). There were 17 cases of ILI within 30 days of vaccination with 16 cases occurring after IIV compared to 1 case after LAIV. IIV was associated with ILI diagnosis (p=0.032). | II-2 | Fair Discrepancies between data in text and tables; do not affect conclusion of 1 case of ILI after 121 doses of LAIV |
| Abbreviations: AE: adverse event; cART: combination antiretroviral therapy; CDC: Centers for Disease Control and Prevention (United States); HAART: highly active antiretroviral therapy; HIV: human immunodeficiency virus; HIV+: HIV-infected; HIV-: non-HIV infected; IIV3: trivalent inactivated influenza vaccine; ILI: influenza-like illness; LAIV: live attenuated influenza vaccine; LAIV3: trivalent live attenuated influenza vaccine; LAIV4: quadrivalent live attenuated influenza vaccine; NIH: National Institutes of Health (United States); RCT: randomized controlled trial; RNA: ribonucleic acid; SAE: serious adverse event; URI: upper respiratory infection; US: United States.
Table 8: Tablenotes
|
||||||
List of abbreviations
- AE
- Adverse event
- CAEFISS
- Canadian Adverse Events Following Immunization Surveillance System
- cART
- Combination antiretroviral therapy
- CDC
- Centers for Disease Control and Prevention (United States)
- CI
- Confidence interval
- CMI
- Cell-mediated immunity
- CPARG
- Canadian Pediatric & Perinatal HIV/AIDS Research Group
- GMT
- Geometric mean titre
- HAART
- Highly active antiretroviral therapy
- HI
- Hemagglutination inhibition
- HIV
- Human immunodeficiency virus
- HIV+
- HIV-infected
- HIV-
- Non-HIV infected
- IgA
- Immunoglobulin A
- IgG
- Immunoglobulin G
- IIV
- Inactivated influenza vaccine
- IIV3
- Trivalent inactivated influenza vaccine
- ILI
- Influenza-like illness
- IM
- Intramuscular
- IWG
- Influenza Working Group
- LAIV
- Live attenuated influenza vaccine
- LAIV3
- Trivalent live attenuated influenza vaccine
- LAIV4
- Quadrivalent live attenuated influenza vaccine
- MMR
- Measles-mumps-rubella
- MN
- Microneutralization
- NACI
- National Advisory Committee on Immunization
- NIH
- National Institutes of Health (United States)
- PCR
- Polymerase chain reaction
- PHAC
- Public Health Agency of Canada
- RCT
- Randomized controlled trial
- RNA
- Ribonucleic acid
- SAE
- Serious adverse event
- US
- United States
- URI
- Upper respiratory infection
Acknowledgments
This statement was prepared by: D Moore, N Dayneka, L Zhao, A Sinilaite, K Young, and I Gemmill, on behalf of the NACI Influenza Working Group and was approved by NACI.
NACI gratefully acknowledges the contribution of: A House, M Laplante, S Ismail, M Tunis, and the Canadian Paediatric & Perinatal HIV/AIDS Research Group.
NACI Influenza Working Group
Members: I Gemmill (Chair), L Cochrane, N Dayneka, R Harrison, K Klein, D Kumar, J Langley, J McElhaney, A McGeer, D Moore, S Smith, and B Warshawsky.
Former working group members: M Lavoie.
Liaison representatives: L Grohskopf (Centers for Disease Control and Prevention [CDC], United States)
Ex-officio representatives: C Bancej (Centre for Immunization and Respiratory Infectious Diseases [CIRID], PHAC), P Wolfe-Roberge (First Nations and Inuit Health Branch [FNIHB], Indigenous Services Canada [ISC]), and J Xiong (Biologics and Genetic Therapies Directorate [BGTD], Health Canada [HC]).
Former ex-officio representatives: K Watkins (CIRID, PHAC).
NACI
Members: C Quach (Chair), S Deeks (Vice-Chair), N Dayneka, P De Wals, V Dubey, R Harrison, K Hildebrand, C Rotstein, M Salvadori, B Sander, N Sicard, and S Smith.
Former NACI members: W Vaudry (Vice-Chair) and M Lavoie.
Liaison representatives: LM Bucci (Canadian Public Health Association), E Castillo (Society of Obstetricians and Gynaecologists of Canada), A Cohn (CDC, United States), M Naus (Canadian Immunization Committee), J Emili (College of Family Physicians of Canada), K Klein (Council of Chief Medical Officers of Health), D Moore (Canadian Paediatric Society), and A Pham-Huy (Association of Medical Microbiology and Infectious Disease Canada).
Former liaison representatives: J Brophy (Canadian Association for Immunization Research and Evaluation), T Cole (Canadian Immunization Committee), and C Mah (Canadian Public Health Association).
Ex-officio representatives: J Gallivan (Marketed Health Products Directorate, HC), E Henry (CIRID, PHAC), M Lacroix (Public Health Ethics Consultative Group, PHAC), J Pennock (CIRID, PHAC), R Pless (BGTD, HC), G Poliquin (National Microbiology Laboratory, PHAC), and T Wong (FNIHB, ISC).
Former ex-officio representatives: K Barnes (National Defence and the Canadian Armed Forces).
References
Footnotes
- Footnote 1
-
National Advisory Committee on Immunization. Canadian Immunization Guide Chapter on Influenza and Statement on Seasonal Influenza Vaccine for 2019–2020. 2019; Available at https://www.canada.ca/en/public-health/services/publications/vaccines-immunization/canadian-immunization-guide-statement-seasonal-influenza-vaccine-2019-2020.html. Accessed February 17, 2020.
- Footnote 2
-
AIDS Info. Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Exposed and HIV-Infected Children. 2019; Available at: https://aidsinfo.nih.gov/guidelines/brief-html/5/pediatric-opportunistic-infection/0. Accessed February 17, 2020.
- Footnote 3
-
Sheth AN, Althoff KN, Brooks JT. Influenza susceptibility, severity, and shedding in HIV-infected adults: a review of the literature. Clinical Infectious Diseases. 2011;52(2):219-27.
- Footnote 4
-
Cohen C, Simonsen L, Sample J, et al. Influenza-related mortality among adults aged 25–54 years with AIDS in South Africa and the United States of America. Clinical infectious diseases. 2012;55(7):996-1003.
- Footnote 5
-
Anema A, Mills E, Montaner J, et al. Efficacy of influenza vaccination in HIV‐positive patients: a systematic review and meta‐analysis. HIV medicine. 2008;9(1):57-61.
- Footnote 6
-
Cooper C, Hutton B, Fergusson D, et al. A review of influenza vaccine immunogenicity and efficacy in HIV-infected adults. Canadian Journal of Infectious Diseases and Medical Microbiology. 2008;19(6):419-23.
- Footnote 7
-
Remschmidt C, Wichmann O, Harder T. Influenza vaccination in HIV-infected individuals: systematic review and assessment of quality of evidence related to vaccine efficacy, effectiveness and safety. Vaccine. 2014;32(43):5585-92.
- Footnote 8
-
National Advisory Committee on Immunization. Recommendations on the use of live, attenuated influenza vaccine (FluMist®). Supplemental Statement on Seasonal Influenza Vaccine for 2011-2012. CCDR. 2011;37(ACS-7):1-77.
- Footnote 9
-
BC Centre for Disease Control. Human Immunodeficiency Virus (HIV) Infection. 2018; Available at: http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Epid/CD%20Manual/Chapter%202%20-%20Imms/Part2/HIV.pdf. Accessed February 17, 2020
- Footnote 10
-
Alberta Health. Immunization of Specific Populations (Immunosuppressed and Chronic Health Conditions). 2019; Available at: https://open.alberta.ca/dataset/aip/resource/8a92b77b-351b-4f1e-9d4d-31aaa9effdb3/download/AIP-Specific-Populations-Immunocompromised.pdf. Accessed February 17, 2020.
- Footnote 11
-
Manitoba Health. Seasonal Influenza Immunization Program: Live Attenuated Influenza Vaccine (LAIV) (FluMist®Quadrivalent): Questions and Answers for Health Care Providers. 2018; Available at: https://www.gov.mb.ca/health/flu/docs/flumist_hcp.pdf. Accessed November 1, 2018.
- Footnote 12
-
Government of New Brunswick. 2013-2014 FluMist®,Live Attenuated Influenza Vaccine, Information for Immunization Providers. 2014; Available at: https://www2.gnb.ca/content/dam/gnb/Departments/h-s/pdf/en/CDC/vaccines/FLUMISTInformationForImmunizationProviders.pdf. Accessed February 17, 2020.
- Footnote 13
-
Government of Saskatchewan. Saskatchewan Immunization Manual. Chapter 7 – Immunization of Special Populations. 2015. https://www.ehealthsask.ca/services/manuals/Documents/sim-chapter7.pdf. Accessed February 17, 2020.
- Footnote 14
-
Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices-United States, 2018-19 Influenza Season. MMWR Recomm Rep. 2018;67(3):1-20.
- Footnote 15
-
Public Health Ontario. Influenza Vaccines available for Children and Older Adults for the 2018-19 Influenza Season. 2018; Available at: http://files.clickdimensions.com/publichealthontarioca-agulw/files/influenzavaccinesseptember142018.pdf?1537538243479&_cldee=Y293YW5lQHRpbWlza2FtaW5naHUuY29t&recipientid=contact-cfb775dc749fe611837d0050569e0009-a0769aa716c646eda2719c3d48e2477d&esid=d1f64a90-05bd-e811-aea7-0050569e0009. Accessed February 17, 2020.
- Footnote 16
-
Newfoundland and Labrador Health and Community Services. Newfoundland and Labrador Immunization Manual: Section 3: Routine Immunization Products. 2018; Available at: https://www.health.gov.nl.ca/health/publichealth/cdc/Section3_Routine_Immunization_Products_May_2018.pdf. Accessed February 17, 2020.
- Footnote 17
-
Yukon Health and Social Services. Community Health Programs: Yukon Immunization Program: Section 8 - Biological Products. 2018; Available at: http://www.hss.gov.yk.ca/pdf/im_manual_section8.pdf. Accessed November 1, 2018.
- Footnote 18
-
Ministère de la Santé et des Services sociaux (MSSS). Vaccinologie pratique : Immunodépression. 2019; Available at: http://www.msss.gouv.qc.ca/professionnels/vaccination/piq-vaccinologie-pratique/immunodepression/. Accessed February 17, 2020.
- Footnote 19
-
Public Health England. Influenza: the green book, chapter 19. 2018; Available at: https://www.gov.uk/government/publications/influenza-the-green-book-chapter-19. Accessed February 17, 2020.
- Footnote 20
-
Haut Conseil de la santé publique (HCSP). Vaccination des personnes immunodéprimées ou aspléniques. Recommandations actualisées. 2014; Available at: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=504. Accessed February 17, 2020.
- Footnote 21
-
Rubin LG, Levin MJ, Ljungman P, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clinical Infectious Diseases. 2013;58(3):e44-e100.
- Footnote 22
-
Children's HIV Association (CHIVA). Vaccination of HIV infected children 2018. Available at: https://www.chiva.org.uk/files/8315/4453/4519/Vaccination_of_HIV_infected_children_2018.pdf. Accessed February 17, 2020.
- Footnote 23
-
AstraZeneca. Product Monograph: FluMist®Quadrivalent. 2018; Available at: https://pdf.hres.ca/dpd_pm/00047438.PDF. Accessed November 1, 2018.
- Footnote 24
-
Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3):21-35.
- Footnote 25
-
European Medicines Agency. Guideline on influenza vaccines: Non-clinical and clinical module. 2014; Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/07/WC500170300.pdf. Accessed February 17, 2020.
- Footnote 26
-
Verschoor CP, Singh P, Russell ML, et al. Microneutralization assay titres correlate with protection against seasonal influenza H1N1 and H3N2 in children. PLoS One. 2015;10(6):e0131531.
- Footnote 27
-
King Jr JC, Fast PE, Zangwill KM, et al. Safety, vaccine virus shedding and immunogenicity of trivalent, cold-adapted, live attenuated influenza vaccine administered to human immunodeficiency virus-infected and noninfected children. Pediatr Infect Dis J. 2001;20(12):1124-31.
- Footnote 28
-
Levin MJ, Song L, Fenton T, et al. Shedding of live vaccine virus, comparative safety, and influenza-specific antibody responses after administration of live attenuated and inactivated trivalent influenza vaccines to HIV-infected children. Vaccine. 2008;26(33):4210-7.
- Footnote 29
-
Curtis D, Ning MF, Armon C, et al. Safety, immunogenicity and shedding of LAIV4 in HIV-infected and uninfected children. Vaccine. 2015;33(38):4790-7.
- Footnote 30
-
King Jr JC, Treanor J, Fast PE, et al. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)-infected and non-HIV-infected adults. J Infect Dis. 2000;181(2):725-8.
- Footnote 31
-
Weinberg A, Song L, Walker R, et al. Anti-influenza serum and mucosal antibody responses after administration of live attenuated or inactivated influenza vaccines to HIV-infected children. J Acquir Immune Defic Syndr. 2010;55(2):189.
- Footnote 32
-
Weinberg A, Song L, Fenton T, et al. T cell responses of HIV-infected children after administration of inactivated or live attenuated influenza vaccines. AIDS Res Hum Retroviruses. 2010;26(1):51-9.
- Footnote 33
-
Weinberg A, Curtis D, Ning MF, et al. Immune Responses to Circulating and Vaccine Viral Strains in HIV-Infected and Uninfected Children and Youth Who Received the 2013/2014 Quadrivalent Live-Attenuated Influenza Vaccine. Frontiers in immunology. 2016;7:142.
- Footnote 34
-
Menegay JL, Xu X, Sunil T, et al. Live versus attenuated influenza vaccine uptake and post-vaccination influenza-like illness outcomes in HIV-infected US Air Force members. Journal of Clinical Virology. 2017;95:72-5.
- Footnote 35
-
Mohn KG, Smith I, Sjursen H, et al. Immune responses after live attenuated influenza vaccination. Human vaccines & immunotherapeutics. 2018;14(3):571-8.
- Footnote 36
-
Public Health Agency of Canada. Page 2: Canadian Immunization Guide: Part 2 – Vaccine Safety. 2019; Available at: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-2-vaccine-safety/page-2-vaccine-safety.html. Accessed February 17, 2020.
- Footnote 37
-
Public Health Agency of Canada. Page 8: Canadian Immunization Guide: Part 3 - Vaccination of Specific Populations. 2018; Available at: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-3-vaccination-specific-populations/page-8-immunization-immunocompromised-persons.html. Accessed February 17, 2020.
- Footnote 38
-
Selik RM, Mokotoff ED, Branson B, et al. Revised surveillance case definition for HIV infection—United States, 2014. Morbidity and Mortality Weekly Report: Recommendations and Reports. 2014;63(3):1-10.
- Footnote 39
-
Marien AG, Hochart A, Lagrée M, Diallo D, Martinot A, Dubos F. Parental acceptance of an intranasal vaccine: Example of influenza vaccine. Archives de Pédiatrie. 2019; 26:71-4.
- Footnote 40
-
Santibanez TA, Kahn KE, Bridges CB. Do parents prefer inactivated or live attenuated influenza vaccine for their children? Vaccine. 2018;36(48):7300-5.
Appendix A: PRISMA flow diagram
Efficacy, effectiveness, immunogenicity, and safety of LAIV in HIV infected individuals. April 13, 2018
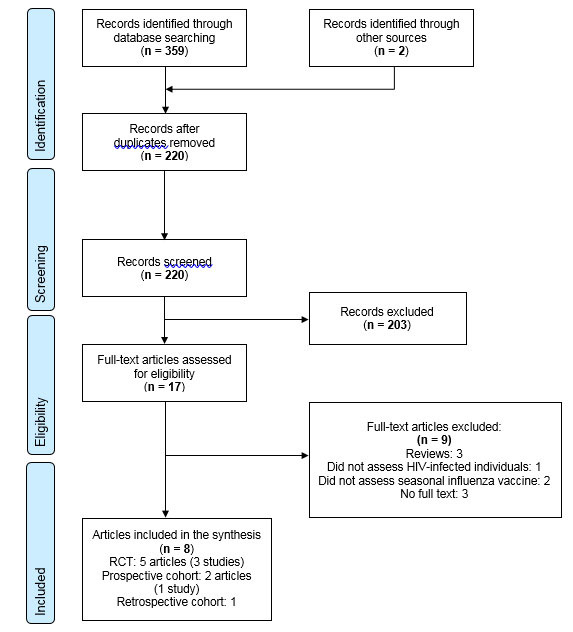
PRISMA flow diagram: Text description
The PRISMA flow diagram describes the process by which articles were selected for the literature review. The process is broken down into four stages: Identification, Screening, Eligibility and Included.
Stage 1: Identification
- 359 records were identified through the April 13, 2018 database search and 2 records were identified through additional sources.
- 220 records remained after duplicates were removed.
Stage 2: Screening
- 220 records were then screened.
- Of these 220 records, 203 records were excluded.
Stage 3: Eligibility
- 17 full-text articles were assessed for eligibility.
- Of these 17 full-text articles, 9 were excluded. The exclusion breakdown is as follows: 3 were reviews, 1 did not assess HIV-infected individuals, 2 did not assess seasonal influenza vaccine and 3 had no full-text.
Stage 4: Included
- 8 articles were included in the final synthesis: 5 RCTs (3 studies), 2 prospective cohort articles (1 study) and 1 retrospective cohort.