Chlamydia among young women: A resource for population-specific prevention
Table of contents
- Acknowledgements
- Introduction
- 1. What is chlamydia?
- 2. Risk factors and determinants of health
- 3. Theory of STBBI prevention
- 4. Promising practices in chlamydia prevention among young women
- Conclusion
- Endnotes
Acknowledgements
The Public Health Agency of Canada would like to acknowledge the individuals, community representatives, researchers and government officials who contributed their time, expertise and experience to the development of this resource. Of note are the individuals who provided advice and guidance during the external review process:
Barbara Beattie, Department of Health, Government of Nunavut (Iqaluit, Nunavut)
Alex McKay, Sex Information and Education Council of Canada (Toronto, Ontario)
Gina McKay, Sexuality Education Resource Centre Manitoba (Winnipeg, Manitoba)
Introduction
Sexually transmitted and blood borne infections (STBBIs) continue to be a significant public health concern in Canada. In particular, chlamydia is the most commonly reported STBBI in Canada and rates have increased substantially since it became a notifiable infection in 1991. Improvements in testing technology have likely contributed to rising reported rates; however, it is also clear that the more than 40,000 young women diagnosed with chlamydia each year in Canada represent only a fraction of the number of young women with the infection. In a majority of cases in both women and men, chlamydia is an asymptomatic infection. Due to its asymptomatic nature, women who have chlamydia are less likely to recognize that they are infected and are therefore highly vulnerable to the health consequences of infection.
This resource was developed to support health professionals and community organizations in the development of evidence-based strategies for the prevention of chlamydia among young women aged 30 and under. For the purpose of this resource, young women include transwomen and transmen with female reproductive parts who have not yet had sex reassignment surgery. A comprehensive review of the existing evidence on chlamydia and other STBBI prevention interventions was conducted to inform the development of this resource.
The following sections provide a summary of key issues related to the prevention, diagnosis, treatment and management of chlamydia. Consult the Canadian Guidelines on Sexually Transmitted InfectionsFootnote1 for detailed information and guidance on the natural history, transmission, prevention, testing, and treatment of chlamydia.
1. What is chlamydia?
1.1 Natural history
Natural history
Chlamydia is an infection caused by the bacterium Chlamydia trachomatis. Chlamydia infection is commonly underdiagnosed because the majority of infected individuals do not have any symptoms. When symptoms do occur, they are usually more severe for women than for men. The period of time between exposure to infection (e.g., transmission through sexual contact) to when symptoms appear is typically two to three weeks but can be as long as six weeksFootnote2. If left untreated, chlamydia infection can lead to serious health consequences, particularly for women.
Health consequences
In women, untreated chlamydia infection can lead to pelvic inflammatory disease (PID), ectopic pregnancy, infertility, and chronic pelvic pain. Chlamydia infection can make those who have it at increased risk for HIV infection due to inflammation and recruitment of immune cells to the site of chlamydia infectionFootnote3.
1.2 Testing and treatment
Chlamydia infection can be diagnosed through a urine sample. In some cases, testing for chlamydia is done through a swab of the infected area. Chlamydia can be treated and cured with antibiotics.
Testing and, if necessary, treating the sex partner(s) of an individual diagnosed with chlamydia is important to prevent reinfection. Individuals who are sexually active or have risk factors for chlamydia infection should get tested regularly. Testing for other STBBIs, such as gonorrhea, may be done at the same time since both chlamydia and gonorrhea can be detected using the same urine or swab sampleFootnote4. Blood tests for syphilis, hepatitis B (if not immunized), hepatitis C and HIV can also be done at the same time.
1.3 Partner notification
Chlamydia is reportable to local public health authorities in all provinces and territories. This means that personal information regarding the diagnosis of chlamydia will be provided to the relevant government health agencies. However, these agencies are responsible for keeping the name of the infected individual confidentialFootnote5.
Like other reportable STBBIs, chlamydia is also subject to partner notification regulations within provincial/territorial public health acts. These regulations require that an attempt is made to locate, test, and treat all those who have had sexual contact with the person with the infection. There are different ways that individuals can tell their partners that they need to get tested for STBBIs, including telling their partners themselves or sending anonymous electronic postcards. Local public health nurses are also available to help with partner notification and appropriate referral for testing and treatment.
1.4 Epidemiology of chlamydia in Canada
Chlamydia has been a nationally notifiableNote i infection in Canada since 1991. Reported rates of the infection are based on the number of newly diagnosed cases reported to provincial/territorial health ministries and then to the Public Health Agency of Canada (the Agency). However, as chlamydia may not show symptoms, many cases may be undiagnosed and therefore not reported.
Chlamydia is most frequently diagnosed among young women aged 15 to 19 and 20 to 24. Women in these age groups are more than twice as likely to be diagnosed with the infection as similarly aged men. Because reported rates are based only on diagnosed cases, testing is key to monitoring rates.
Figure 1 illustrates the dramatic rise in reported rates of chlamydia among young women in Canada since 1991 when the infection first became a nationally notifiable infection. Reported rates of chlamydia have increased in recent years after declining from 1992 to 1997. According to data from the Agency, from 1997 to 2011, the reported rate of chlamydia among 15 to 19 year-old females rose from 971.3 per 100,000 to 1881.6, an increase of 93.7%Footnote6. Among females aged 20 to 24 years, the rate rose from 924.1 to 2113.0, an increase of 128.6%.
Figure 1: Reported rates per 100,000 of chlamydia among females aged 15-19, 20-24, 25-29, 1991-2011, Canada
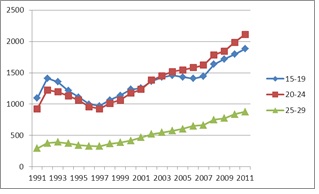
Figure 1: Reported rates per 100,000 of chlamydia among females aged 15-19, 20-24, 25-29, 1991-2011, CanadaFootnote7
| Year | Age 15-19 | Age 20-24 | Age 25-29 |
|---|---|---|---|
| 1991 | 1095.1 | 925.0 | 295.6 |
| 1992 | 1412.1 | 1225.6 | 378.7 |
| 1993 | 1355.0 | 1194.2 | 394.4 |
| 1994 | 1215.5 | 1131.8 | 373.6 |
| 1995 | 1111.1 | 1060.2 | 345.4 |
| 1996 | 997.1 | 956.7 | 331.7 |
| 1997 | 971.3 | 924.1 | 325.8 |
| 1998 | 1063.7 | 1011.8 | 366.4 |
| 1999 | 1138.3 | 1064.6 | 386.1 |
| 2000 | 1234.3 | 1175.7 | 417.9 |
| 2001 | 1256.0 | 1235.1 | 466.2 |
| 2002 | 1366.2 | 1382.4 | 522.5 |
| 2003 | 1429.6 | 1453.3 | 546.8 |
| 2004 | 1458.0 | 1518.3 | 574.9 |
| 2005 | 1431.3 | 1545.0 | 602.6 |
| 2006 | 1407.2 | 1582.8 | 649.3 |
| 2007 | 1440.8 | 1622.3 | 664.3 |
| 2008 | 1636.6 | 1783.9 | 750.2 |
| 2009 | 1718.4 | 1845.0 | 773.8 |
| 2010 | 1794.1 | 1983.9 | 838.8 |
| 2011 | 1881.6 | 2113.0 | 878.3 |
- Footnote i
-
Notifiable STBBI include chlamydia, gonorrhea, syphilis, and HIV. Common non-notifiable STBBI include Human papilloma virus (HPV) and Herpes simplex virus (HSV).
2. Risk factors and determinants of health
There are multiple factors that can influence what make young women vulnerable to or resilient against chlamydia. These factors, or determinants of health, can be experienced at various levels (Figure 2). While individual behaviours such as inconsistent condom use and multiple sex partners are major drivers of STBBI transmission and acquisition, these behaviours are directly and indirectly influenced by many social, structural or economic factorsFootnote 8. These conditions may increase STBBI vulnerability by increasing the likelihood of high risk behaviours and exposure to and acquisition of an STBBIFootnote 9.
| Individual | Micro (relational) | Meso (community) | Macro (structural) |
|---|---|---|---|
|
|
|
|
An understanding of the underlying causes or determinants of health that impact the health of young women is important for effective chlamydia prevention among this population. For detailed information on the factors that impact resilience and vulnerability to STBBIs among young women, consult the Population-specific HIV/AIDS Status Report: WomenFootnote 10.
2.1 Gender
Gender is a key determinant that impacts vulnerability to STBBIs, including chlamydia. Gender norms related to masculinity and femininity can contribute to an imbalance of power in relationships and affect sexual risk behaviours by limiting women's ability to negotiate safer sexFootnote 11. Experiences of gendered physical or emotional violence in relationships can also increase a woman's vulnerability to STBBIsFootnote 12. Transgender women face multiple barriers to accessing health services due to experiences of discrimination and fear of judgment. These barriers can contribute to their marginalization and increase their vulnerability to STBBIsFootnote 13.
2.2 Biology
Biological differences can influence what makes women vulnerable to STBBI transmission. For example, female anatomy such as the large surface area and delicate tissue of the genital tract makes women more vulnerable to tissue damage during vaginal intercourse, which may contribute to increased risk of certain STBBIs such as HIV and chlamydiaFootnote 14. Also, due to the asymptomatic nature of chlamydia infection, symptoms of vaginal discharge may be misinterpreted by young women and their health care providers as having a different cause. This may be particularly relevant if health care providers are not aware of their patient's sexual historyFootnote 15.
2.3 Social environments and social support networks
Lack of social power and status directly affect women and increase vulnerability to sexual, physical and emotional violence, which can have a negative impact on their mental and physical healthFootnote 16. A history of intimate partner violence and childhood sexual abuse is associated with higher risk behaviours such as inconsistent condom use and multiple sex partners, which can increase vulnerability to STBBIsFootnote 17. Women who face multiple forms of stigma and discrimination, such as racism and homophobia, are particularly vulnerable to STBBIs because they are more likely to be excluded from support networks and servicesFootnote 18. Support from families, friends and communities is important in helping young women maintain control over life circumstances and build resilience in the face of adversityFootnote 19.
2.4 Culture
Cultural factors, including attitudes, beliefs, values and practices that are shaped by historical, socioeconomic and political contexts, are key determinants that can make young ethnocultural minority and Aboriginal women more vulnerable to chlamydia infectionFootnote 20. An historical context of cultural disruptions, multiple disconnections with family and experiences of poverty, violence and exploitation has led to Aboriginal women's low self-esteem and mistrust of non-Aboriginal health care providers and servicesFootnote 21. These factors are barriers to negotiating safer sex and to accessing health care. A lack of knowledge and lack of defence against violence and abuse further increases their vulnerability to STBBIs and to potential violence and abuseFootnote 22.
For newcomers to Canada, many health promotion and STBBI prevention campaigns or messages may not be available in their native language. In some instances there may not be a safe space where women can discuss such issues openly and confidentially. Being unaware of where or how to access STBBI services in the community may further contribute to STBBI vulnerabilityFootnote 23. While in some cases cultural factors can serve as a barrier to open discussions about sexuality and access to services, culture can also be a source of strength and resilience. For example, studies have found that Aboriginal persons' connection to their culture and traditional spirituality can help them to cope with adverse life circumstancesFootnote 24.
2.5 Socioeconomic status
Lower socioeconomic status, typically measured by poverty level or income, has been clearly associated with vulnerability to STBBIs through high risk sexual encounters among adolescents and young adultsFootnote 25. Young women who have lower incomes or who may live below the poverty line may be at greater risk for contracting STBBIs through participation in survival sex as a source of income. They may face additional financial concerns related to accessing condoms for STBBI prevention, and costs associated with accessing testing and treatment services.
2.6 Physical environment
Among youth in particular, there is a relationship between homelessness, housing insecurity and exposure to violence in the community, and increased risk for STBBIsFootnote 26. For some young women, the lack of access to housing and safe spaces may increase the risk of survival sex and partner violence and reduce their ability to practice or negotiate ways to protect themselves against STBBIsFootnote 27.
3. Theory of STBBI prevention
3.1 Upstream, primary, secondary and tertiary STBBI prevention
STBBI prevention activities can take many forms. Prevention activities are usually identified as upstream, primary, secondary or tertiary. A comprehensive STBBI prevention approach will address most or all four categories of prevention if it is to be effective in substantially reducing the burden of STBBIs.
Upstream prevention activities address the determinants of health (e.g., stigma and discrimination, gender norms, socioeconomic status) that influence vulnerability to and resilience against STBBIs. Primary prevention activities are aimed at preventing STBBIs among individuals who are currently uninfected. These programs provide recipients with information and skills to enable them to reduce their risk of acquiring an STBBI. Secondary prevention activities seek to identify and treat individuals who are infected with an STBBI. STBBI testing and partner notification are the key elements of secondary prevention. Tertiary prevention activities focus on providing care and support to individuals living with an STBBI. The goal is to limit disease progression and improve the quality of life of those living with chronic STBBIs.
3.2 A model to guide primary and secondary chlamydia prevention
One approach which has been proven to be effective for health professionals in modifying high risk sexual behaviour among multiple populations is the Information, Motivation, Behavioural Skills (IMB) modelFootnote 28. As its name suggests, the IMB model specifies that effective STBBI prevention programs are based on three essential elements. This model can be used to guide educators and health professionals in the development and evaluation of effective STBBI prevention programs. Application of these three elements specifically to chlamydia prevention is outlined below.
Information
The information component of an effective IMB-based chlamydia prevention intervention provides participants with relevant knowledge and information regarding the transmission of chlamydia and ways to prevent chlamydia infection (e.g., condom use, reducing numbers of sexual partners) as prerequisites for reducing risk behaviours. It is important that the information provided is tailored to the age and literacy level of the recipientsFootnote 29.
Motivation
Information by itself is not sufficient to achieve behaviour change (e.g. condom use negotiation). Intervention participants must also be motivated to act on the information they have learned. With respect to reducing sexual risk and increasing STBBI testing, it is important that interventions take into account the specific needs and motivations of audiences, address barriers to prevention and testing and emphasize positive behaviour (e.g., self-care)Footnote 30.
Behavioural skills
STBBI prevention programs are significantly less likely to reach their objectives without incorporating the necessary behavioural skills (e.g. how to use a condom, how to negotiate safer sex with partners) to adopt the desired behaviour change (e.g. condom use)Footnote 31. The third component of an effective chlamydia prevention intervention focuses on the skills necessary to reduce sexual risk behaviour as well as those required to seek out testing and treatment. It is important to equip individuals with practical skills to carry out the desired behaviour. This includes the person's belief and confidence that they have the ability to perform the behaviour (known as self-efficacy) and the opportunity to rehearse it.
4. Promising practices in chlamydia prevention among young women
Strategies to reduce the burden of chlamydia among adolescent and young adult women have typically focused on a combination of primary and secondary prevention. Developing new knowledge and expanding both the scope and understanding of emerging public health evidence and promising practices is important for an effective response to chlamydia infection over the long-term. This includes the systematic use of knowledge and rigorous program evaluation to identify knowledge gaps for researchers and to inform future cycles of program development to improve public health results.
4.1 Primary prevention interventions to reduce sexual risk for chlamydia infection
This section provides a synthesis of peer-reviewed literature which has evaluated primary prevention interventions to reduce sexual risk for STBBIs. Practice points and case studies are provided that outline key strategies to guide program planners in the development and implementation of effective chlamydia prevention interventions.
Interactive strategies
Interventions to encourage safer sex behaviour among youth have used a variety of interactive strategies. A survey of 83 programs designed to reduce sexual risk behaviour among youth found that more than 90% of all the interventions used at least two or more interactive strategiesFootnote 32.
Key practice point:
- Consider interventions that use a variety of interactive strategies to deliver information, teach skills, and promote behavioural change. For example: role playing with or without scripts; group discussions and brain-storming sessions to help students overcome barriers to safer sex behaviour; homework assignments about selected topics that involve discussions with parents or other adults; small group work; question boxes; video presentations; and skits that reflect real life issues and present different responses to challenging situations.
Upstream intervention
Case study #1 — FOXY: Fostering Open eXpression among YouthFootnote 33
Goal of intervention: To increase knowledge on the determinants of HIV and other STBBIs among First Nations, Inuit, and Métis youth in Northern Canada to prevent the acquisition of new HIV infection and other STBBIs.
Description of Intervention: The intervention takes a participatory arts-based approach to improving sexual health knowledge, self-efficacy and sexual health decision-making among young women aged 13-17 years old in the Northwest Territories. The project includes workshops in schools and a peer leadership retreat.
Key Strategies: The program builds capacity through self-exploration, relationship-building and exercises in confidence using arts- and drama-based workshops (e.g. body mapping, photography, creative writing, music and Aboriginal arts and crafts) in schools and during a six-day leadership retreat.
Results: Based on participant and parent feedback and project staff observations, the project has produced meaningful impacts on the sexual health needs and HIV/STBBI knowledge of the target population. Participants discussed the impact of gaining personal skills such as communication, knowledge of personal strengths, respect and confidence in addition to increasing capacity to adopt healthy sexual behaviours such as knowing how to put on a condom.
Behaviour change and STBBI risk:
There are many factors that increase an individual's vulnerability to STBBIs. The challenge in creating an effective intervention is to understand why certain risk behaviours occur and what factors may increase or decrease this behaviourFootnote 34. Interventions that address a range of factors that influence sexual behaviour and include more than one component (e.g., combining skills training and motivation for behaviour change with basic sexual health information) have been shown to be effective in reducing sexual risk behaviour and increasing preventive behaviour over the long-termFootnote 35.
Key practice points:
- Develop STBBI prevention interventions that address individual, societal, and cultural factors that influence sexual behaviour.
- Consider interventions delivered in small groups to enhance positive behaviour change in the short term.
- Provide information about the transmission and prevention of STBBIs, motivation for positive behaviour change, and behavioural skills training to reduce sexual risk behaviour over the long-term.
Primary prevention
Case study #2 — HORIZONS: “Stay safe for yourself and your community”Footnote 36
Goal of intervention: To reduce rates of STBBI/HIV among young African American women, decrease sexual risk behaviour and increase preventive behaviour.
Description of Intervention: African American women aged 15 to 21 were recruited from three sexual health clinics in Atlanta, Georgia. Participants (715) were randomly assigned either to the intervention or a control group. The intervention consisted of two four- hour sessions with small groups of eight participants on average. Upon completion of the sessions, follow-up phone calls were made to reinforce information and skills learned in the small group sessions. Participants were assessed before the intervention and at six- and 12-month intervals following completion of the study.
Key Strategies: The sessions included group discussions and interactive sessions to encourage risk reduction behaviour. Program content also focused on enhancing gender and cultural pride. Women discussed the accomplishments of African American women, read poetry and framed art work by African American women. By focusing on broader cultural issues, a link was made between personal sexual health and the overall health and strength of the community. Role play was used to enhance HIV-preventive behaviour, including helping women become comfortable with informing partners about their STBBI status and encouraging partners to seek testing.
Results: Individuals in the intervention group had lower rates of chlamydia infection and higher rates of condom usage over the 12 month follow-up period.
Longer-term interventions to support sustained behaviour change
Long-term interventions are important to support and encourage sustained behaviour change as participants move through different phases of their sexual lives. It is also important to delay follow-up evaluations of an intervention to allow participants adequate time to integrate STBBI preventive behaviour into their livesFootnote37.
Key practice points:
- Support longer-term interventions to ensure continued behaviour change.
- Provide periodic booster sessions to reinforce original prevention messages and extend the benefits of an intervention.
- Incorporate an evaluation component into all interventions and allow participants time to process information and implement prevention strategies.
Tailored messages
STBBI prevention messages that are customized for individual health behaviour profiles are more likely to have a positive influence on behavioural change than social media campaigns that rely on generic messagingFootnote38.
Key practice points:
- Tailor prevention messages to reflect individual age, race, culture, gender, sexual orientation and linguistic characteristics.
Online interventions
Online media has been used to disseminate prevention information to reduce rates of STBBIs in specific communitiesFootnote39. However, the outcomes associated with using various websites are not always measured. Web-based approaches to STBBI prevention and education include using Facebook pages, websites, texting, partner notification e-cards, and online ordering of self-testing kits. While social media has the capability to reach a large segment of the population, the mode of delivery and relevance of information presented must be assessed on a regular basis and notifications to users about content updates are recommended as one way to prevent loss of interest in a site.
Key practice points:
- Update online STBBI prevention content on a regular basis to reflect changes in testing and treatment information and available resources.
- Integrate healthy living messages with STBBI prevention messages. STBBI prevention messaging on its own is not always enough to encourage users to visit a website.
- Link prevention information sites with other health related sites, especially sites that will appeal to youth.
Interventions and administrative issues
The structural and administrative nature of prevention interventions plays an important role in program effectivenessFootnote40. A study of chlamydia prevention interventions in Sweden found that well-resourced, collaborative and coordinated programs were associated with reduced rates of infection and increased rates of condom useFootnote41.
Key practice point:
- Support and build capacity of interventions through adequate resourcing, strong leadership, and collaborative partnerships.
- Engage multiple stakeholders in STBBI prevention including community-based organizations, community leaders, public health promoters, schools, government agencies, non-governmental organizations, researchers and family members.
4.2 Secondary prevention interventions to reduce sexual risk for chlamydia infection
This section provides a synthesis of peer-reviewed literature evaluating secondary prevention interventions to increase rates of chlamydia testing, and focuses on interventions carried out in non-clinical settings.
Attitudes towards chlamydia testing
Studies on the attitudes and perceptions of youth towards chlamydia testing show that youth experiences of STBBI testing or diagnosis often result in feelings of shame and embarrassmentFootnote42.
Key practice points:
- Challenge social stigma and societal beliefs that promote feelings of shame and embarrassment related to STBBIs and STBBI testing.
- Emphasize STBBI prevention and testing as a key component of healthy behaviour, so that individuals do not feel judged by peers, family and health care providers when they are tested.
Barriers to testing
Barriers to chlamydia testing can be physical such as issues related to accessibility and convenience, as well as psychological, such as issues related to negative perceptions and feelings of fear, shame and embarrassmentFootnote43. Young women are more likely to seek testing for chlamydia if they have positive attitudes towards STBBI services, less concern about sexual disclosure, greater STBBI knowledge and an increased perception of risk for infectionFootnote44.
Key practice points:
- Provide young women with information about chlamydia testing and dispel myths associated with STBBI testing, and address concerns about confidentiality.
Risk appraisal
Risk appraisal, or the perception of risk and severity of possible outcomes, is significantly associated with intention to be tested and the adoption of preventive behaviour. Young people often underestimate their personal risk of chlamydia infection and the severity of consequences associated with an infectionFootnote45. Individuals who are concerned about the negative outcomes of a condition (i.e., chlamydia infection) will pay more attention to an intervention. On the other hand, if they do not perceive a personal risk to their health, then attempts to promote preventive behaviour and increased testing among the population will not be as effectiveFootnote46. Furthermore, many youth are unaware that chlamydia often displays no symptoms. This is a key point to address, since perception of risk is often associated with obvious physical symptoms of infection. As well, young adults often make assumptions about the health status of their partners based on physical appearance and reputation.
Key practice points:
- Address individual awareness and perception of personal risk to have a positive impact on preventive behaviour including STBBI testing.
- Provide information about STBBIs and risk factors for infection that help individuals develop a realistic sense of their risk for chlamydia.
Fear and anxiety
Some individuals may avoid testing due to fear and anxiety when an intervention over-emphasizes negative consequencesFootnote47. Studies of attitudes and perceptions of young adults toward chlamydia have observed that prevention campaigns that create fear and anxiety may serve to deter rather than encourage youth to take control of their own sexual health and adopt preventive strategies to avoid infectionFootnote48.
Key practice points:
- Reinforce positive messaging (rather than fear-based) to encourage STBBI testing and promote preventive behaviour.
- Encourage preventive strategies that strengthen decision-making skills as well as those that support positive coping skills.
Positive messages related to testing
Video presentations and posters have been used to increase positive attitudes and counter negative attitudes towards chlamydia testingFootnote49. Positive messages position testing as part of a healthy lifestyle for all sexually active adults, regardless of age, sex, gender, sexual orientation, and ethnicity.
Key practice points:
- Encourage prevention messages that promote chlamydia testing as part of a responsible, sexually healthy lifestyle for all adults.
Secondary prevention
Case study #3 — Get tested. Why not?Footnote50
Goal of Intervention: Increase access to chlamydia and gonorrhea testing among youth in the Ottawa area. Raise awareness of personal risk factors for infection and provide basic information about STBBIs.
Description of Intervention: Get tested. Why not? is a bilingual Internet-based campaign developed by Ottawa Public Health to encourage chlamydia and gonorrhea testing among all youth aged 15 to 29 years who live in Ottawa. The Get tested. Why Not? website provides information about chlamydia and gonorrhea, basic sexual and reproductive information as well as information about where and how to get tested.
Key Strategies: Ottawa area youth participated in focus groups to help identify issues and strategies to be included in the campaign. Youth recommended that the site be advertised on Facebook, through posters, billboards, and newspaper and bus ads. The site features downloadable requisition forms for urine-based chlamydia and gonorrhea testing which can be taken to participating laboratories identified on the website. There is also a texting function, Get Texted, which provides 24 hour access to information about sexual health services in the community and general sexual health information.
Results: The campaign has expanded access to testing in the Ottawa area. During the first year of operation (March 2011 to March 2012) the site had more than 13,000 hits. There were 104 requisitions submitted for testing, with four positive results for asymptomatic cases of chlamydia.
Community-based interventions
Chlamydia testing has been offered in a variety of settings such as sports and entertainment events, community centres, beaches, courts of law and on the street. High participation rates in community and social settings suggest that people feel most comfortable in an environment that openly encourages testing, and among others who are also getting tested. Studies have also validated the effectiveness of monetary and other incentives (i.e., food vouchers, condoms, movie tickets, cash) to increase testing ratesFootnote51.
Key practice points:
- Offer outreach-based chlamydia testing programs in a variety of settings.
- Consider use of incentives to increase testing rates.
Conclusion
In Canada, chlamydia is the most commonly reported STBBI. Reported rates of chlamydia continue to increase among young people aged 15 to 24, especially women. Untreated chlamydia infection can result in numerous negative health outcomes.
There are a number of factors at the individual, micro (relational), meso (community) and macro (structural) levels that influence vulnerability to and resilience against STBBIs, including chlamydia. Research literature has highlighted a number of effective approaches for the design and implementation of STBBI and chlamydia prevention interventions. Elements of the Information, Motivation, Behavioural Skills (IMB) model can be applied to chlamydia prevention programming among young women. A comprehensive approach to chlamydia prevention includes a combination of upstream, primary and secondary prevention interventions. Moreover, the systematic use of knowledge and rigorous program evaluation is important to identify knowledge gaps for researchers and to inform future cycles of program development to improve public health results.