The Canadian Chronic Disease Surveillance System – An Overview
The Canadian Chronic Disease Surveillance System (CCDSS) is a collaborative network of provincial and territorial surveillance systems, supported by the Public Health Agency of Canada (PHAC). The CCDSS enhances the scope of data on chronic diseases in Canada and supports the planning of health resources and the development of health policies and programs. It collects data on all residents who are eligible for provincial or territorial health insurance and can generate national estimates and trends over time for over 20 chronic diseases (see the textbox “Chronic diseases included in the CCDSS”).Footnote 1
Chronic diseases included in the CCDSS |
|
Cardiovascular diseases
Chronic respiratory diseases
Mental illnesses
|
Diabetes Musculoskeletal disorders
Neurological conditions
|
More information on these diseases is available at: https://www.canada.ca/en/public-health/services/chronic-diseases.html.
Download the alternative format
(PDF format, 922 KB, 5 pages)
Organization: Public Health Agency of Canada
What are CCDSS data sources?
To identify people with chronic diseases, provincial and territorial health insurance registry records are linked using a unique personal identifier to the corresponding physician billing claims, hospital discharge abstract records and prescription drug records.
Data are collected by fiscal year since 1995–1996 in most provinces and territories.Footnote 2 However, the start year for reporting CCDSS data is determined on a case-by-case basis for each disease to allow enough time to capture all prevalent cases as well as to ensure that previously prevalent cases are excluded from incident cases.
Under this distributed model, CCDSS data extraction is conducted in each jurisdiction using a standardized analytical protocol developed by PHAC.Footnote 3,Footnote 4 Using this protocol, case definitions are applied to these linked databases and individual data are aggregated at the provincial or territorial level before being submitted to PHAC for analysis and reporting. Throughout the process, data are managed by the relevant authorities according to custodial obligations to protect patient privacy.
Each database (Figure 1) provides a specific piece of information contributing to case identification. The databases also provide additional health information such as:
- demographic data (age, sex, province or territory of residence);
- mortality data; and
- use of health care services (hospitalization, visit to a specialist, visit to a physician).
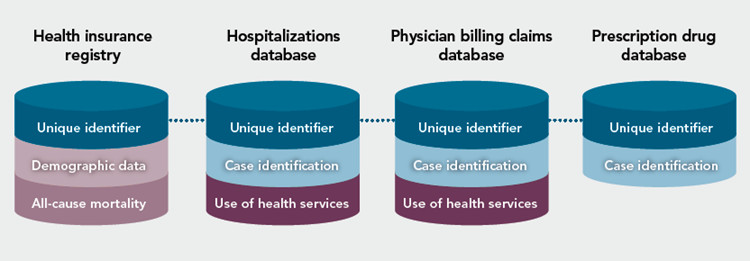
Figure 1 - Text description
The health insurance registry is linked to the hospitalizations database and the physician billing claims database for case identification using a unique case identifier. In some instances, the prescription drug database is also linked to the former databases for case identification. Each database provides a specific piece of information contributing to case identification. The databases also provide additional health information. The health insurance registry provides demographic data, such as age, sex, and province or territory of residence, as well as mortality data. The other databases provide information on the use of health care services, such as hospitalizations, visit to a specialist, or visit to a physician.
Health insurance registry: The health insurance registry contains records for each person entitled to provincial or territorial health insurance.
Hospitalizations database: Provinces and territories record acute care hospital information using either the Discharge Abstract Database (DAD) or in Quebec, the “Maintenance et exploitation des données pour l'étude de la clientèle hospitalière” database (MED-ÉCHO). Hospital diagnoses are coded using the International Statistical Classification of Diseases and Related Health Problems (ICD).Footnote 5, Footnote 6, Footnote 7, Footnote 8
Physician billing claims database: Most physician activity in Canada is captured by physician billing claims,Footnote 9, Footnote 10 either through fee-for-service or shadow billing claims,Footnote 11 using ICD codes or diagnostic text, depending on the province or territory.
Prescription drug database: The comprehensiveness of the provincial or territorial prescription drug databases and their accessibility by the CCDSS partners vary across the country. For example in some provinces and territories, data are only available for the population aged 65 years and older. The drug dispensed is coded using a drug identification number (DIN) issued by Health Canada.Footnote 12 Currently, only the case definition for dementia, including Alzheimer’s disease, uses this data source for reporting purposes.
What are CCDSS case definitions?
A CCDSS case definition (see the textbox “CCDSS case definition using diabetes as an example”) is a set of rules that enables the identification of cases of a disease in a given population. The majority of CCDSS case definitions are validated through comparison against clinical diagnoses. The list of case definitions and diagnostic codes used for conditions included in the CCDSS is available online.Footnote 13
CCDSS case definitions are developed through a rigorous process, led by disease-specific working groups which are comprised of representatives from PHAC, provincial and territorial governments, epidemiologists and clinical experts. The development of a new case definition is comprised of four main steps, with examples of publications listed in the references: 1) literature review,Footnote 14 2) validation studies,Footnote 15, Footnote 16 3) feasibility studies,Footnote 17, Footnote 18 4) and a national pilot.Footnote 19 The evidence generated throughout this process is carefully analyzed to select a case definition for the purposes of national surveillance.
CCDSS case definition using diabetes as an example
Canadians aged 1 year and older are identified as having diagnosed diabetes (type 1 or type 2 combined) if they have at least one hospitalization record or at least two physician claims in a two-year period with an ICD code for diabetes.
To exclude gestational diabetes cases, evidence from women aged 10-54 is removed 120 days preceding or 180 days following an hospitalization with a record containing selected pregnancy-related and obstetrical codes.
What do CCDSS data provide?
CCDSS data can be used to report national estimates and trends over time of:
- incidence and prevalence;Footnote 20
- all-cause mortality (death due to any cause);
- health care utilization, such as hospitalizations and physician visits; and
- multimorbidity and comorbidity.
Other estimates on economic costs of chronic diseases can be produced using the CCDSS data infrastructure, when additional databases are linked to the system.
CCDSS data can be stratified by:
- age group;
- sex;
- province or territory;
- year; and
- disease status.
Where to find CCDSS data and more surveillance information on chronic diseases?
- Data tools, indicator frameworks, and data lab: Public Health Infobase
- CCDSS datasets: Government of Canada – Open Data
- PHAC reports, fact sheets, and infographics: Canada.ca – Publications
Acknowledgements
The CCDSS is a collaboration between PHAC and all Canadian provincial and territorial governments. This fact sheet was developed by PHAC; no endorsement by the provinces and territories is intended or should be inferred.
References
- Footnote 1
In this document, the term ‘chronic diseases’ is also used to refer to chronic conditions, disorders, or health related consequences or events.
- Footnote 2
Except in Quebec where the data collection starts in 1996–1997 and in Nunavut where data can only be reported as of 2005–2006.
- Footnote 3
Lix LM, Ayles J, Cooke CA, et al. The Canadian Chronic Disease Surveillance System: A model for collaborative surveillance. International Journal of Population Data Science. 2018; 3(3):5.
- Footnote 4
Lix LM, Reimer, K. The Canadian Chronic Disease Surveillance System: A Distributed Surveillance Model. OJPHI Public Health Informatics. 2017;9(1):e140.
- Footnote 5
World Health Organization. Classifications [Internet]. Geneva: WHO [updated 2018 Feb 23; cited 2018 June 7]. Available from: www.who.int/classifications/icd/en/
- Footnote 6
Canadian Institute for Health Information. Canadian Coding Standards for Version 2012 ICD-10-CA and CCI [Internet]. Ottawa (ON): CIHI; 2012 Sep 3 [cited 2017 Aug 1]. Available from: https://secure.cihi.ca/estore/productFamily. htm?pf=PFC1708&lang=en&media=0
- Footnote 7
World Health Organization. International Statistical Classification of Diseases, Ninth Revision. Geneva: WHO; 1978.
- Footnote 8
World Health Organization. International Statistical Classification of Diseases, Ninth Revision, Clinical Modification. Geneva: WHO; 1978.
- Footnote 9
Lix LM, Walker R, Quan H, et al. CHEP-ORTF Hypertension Outcomes and Surveillance Team. Features of physician services databases in Canada. Chronic Dis Inj Can. 2012 Sep;32(4):186–93.
- Footnote 10
Canadian Institute for Health Information. National Physician Database – Payments Data, 2015-2016 [Internet]. Ottawa (ON): CIHI; 2017 Sep [cited 2018 June 13]. Available from: www.cihi.ca/en/physicians
- Footnote 11
An administrative process whereby physicians remunerated via various alternative payment plans submit claims using provincial and territorial fee codes, even though they are reimbursed by other means of payment.
- Footnote 12
Health Canada. Drug Identification Number (DIN) [Internet]. Ottawa (ON): Health Canada; [updated 2018 Jan 8; cited 2018 Feb 6]. Available from: www.canada.ca/en/health-canada/ services/drugs-health-products/drug-products/fact-sheets/drugidentification- number.html.
- Footnote 13
Public Health Agency of Canada. Public Health Infobase: Canadian Chronic Disease Surveillance System (CCDSS). [Internet]. Ottawa (ON): PHAC [updated 2018 Apr 26; cited 2018 July 17]. Available from: https://infobase.phac-aspc.gc.ca/ccdss-scsmc/data-tool/
- Footnote 14
Fiest KM, Sauro, KM, Wiebe, S, et al. Prevalence and incidence of epilepsy: A systematic review and meta-analysis of international studies. Neurology. 2017 Jan 17;88(3):296–303.
- Footnote 15
Butt DA, Tu K, Young J, et al. A validation study of administrative data algorithms to identify patients with parkinsonism with prevalence and incidence trends. Neuroepidemiology. 2014;43(1):28–37.
- Footnote 16
Tu K, Mitiku T, Lee DS, et al. Validation of physician billing and hospitalization data to identify patients with ischemic heart disease using data from the Electronic Medical Record Administrative data Linked Database (EMRALD). Can J Cardiol 2010; Aug-Sep;26(7):e225-8.
- Footnote 17
Robitaille C, Bancej C, Dai S, et al. Surveillance of ischemic heart disease should include physician billing claims: Population-based evidence from administrative health data across seven Canadian provinces. BMC Cardiovasc Disord 2013;13:88.
- Footnote 18
Blais C, Dai S, Waters C, et al. Assessing the burden of hospitalized and community-care heart failure in Canada. Can J Cardiol. 2014 Mar;30(3):352–8.
- Footnote 19
Robitaille C, Dai S, Waters C, et al. Diagnosed hypertension in Canada: Incidence, prevalence and associated mortality. CMAJ. 2012 Jan 10;184(1):E49–56.
- Footnote 20
For mental illness and mood and anxiety disorders, annual use of health services is reported instead of prevalence.