The Chief Public Health Officer’s Report on the State of Public Health in Canada 2017 – Designing Healthy Living
A message from Canada's Chief Public Health Officer
Without being aware of it, our neighbourhoods and how they are built influence how healthy we are.
I chose designing healthy living as the topic for my first report as Canada’s Chief Public Health Officer because of the tremendous potential that changing our built environment has for helping Canadians live healthier lives.
Chronic diseases like diabetes, cancer and cardiovascular disease are the leading causes of death in Canada. It is alarming that in 2011, almost 2.7 million or 1 in 10 Canadians 20 years and older were living with diabetes. Rising rates of type II diabetes can be considered a red flag for poor health as they are associated with higher rates of other diseases and conditions and linked to an unhealthy diet, low physical activity and higher rates of overweight and obesity. Rates of type II diabetes and other chronic diseases in Canada could be reduced by seamlessly integrating healthy living into our daily lives which can be achieved, in part, by designing and redesigning our communities.
Improving public health and preventing disease through changes to our environment is a well-founded concept. For example, infectious disease rates in the last century were reduced not just through scientific innovation and vaccination, but also through infrastructure planning by improving sanitation and addressing overcrowding in residential neighbourhoods.
This report answers many questions but also raises several others. We need better information if we are to measure the health impacts of community design to incorporate evidence-based strategies into community planning. This report will raise awareness among Canadians about the unique aspects of their communities that they could take advantage of to improve their health. It will also encourage more dialogue across the many disciplines involved in community planning and health promotion so that neighbourhood design considers and promotes physical activity, healthy diets and mental wellness.
Dr. Theresa Tam
Chief Public Health Officer of Canada
Table of Contents

Download the alternative format
(PDF format, 7 MB, 74 pages)
Organization: Public Health Agency of Canada
Date published: 2018-07-20
Acknowledgements
Many individuals and organizations have contributed to the development of The Chief Public Health Officer's Report on the State of Public Health in Canada, 2017: Designing Healthy Living.
I would like to express my appreciation to the consultants who provided invaluable expert advice:
- Dr. Cory Neudorf, Chief Medical Health Officer, Saskatoon Health Region, University of Saskatchewan
- Dr. David Mowat, Canadian Partnership Against Cancer
- Dr. Daryl Pullman, Memorial University
- Dr. Elizabeth Saewyc, University of British Columbia
- Dr. Jeff Reading, Simon Fraser University
- Dr. John Frank, University of Edinburgh
- Dr. Margo Greenwood, University of Northern British Columbia, National Collaborating Centre for Aboriginal Health
- Dr. Michael Routledge, Medical Officer of Health, Manitoba
- Dr. Peter Donnelly, President and Chief Executive Officer of Public Health Ontario
I would like to extend a special thank you to Dr. Mowat for sharing his expertise in reviewing many drafts. In addition, I would also like to recognize contributions made by partners and stakeholders who were consulted on the report under tight timelines, including Health Canada, Dr. Steven Hoffman at the Canadian Institutes of Health Research, Dr. Jim Dunn at the McMaster University, Dr. Meghan Winters at Simon Fraser University and Nathan Taylor at Memorial University.
I would also like to sincerely thank the many individuals and groups within the Public Health Agency of Canada for all of their efforts related to the development of my report, including John Cuningham and representatives from the Health Promotion and Chronic Disease Prevention Branch: Simone Powell, Dawn Sheppard, Greg Butler, Ahalya Mahendra, Wendy Thompson, Dr. Margaret de Groh and Christine Soon.
I appreciate the excellence and dedication of my support staff and CPHO Reports Unit in researching, consulting on and developing this report: Dr. Stephanie Rees-Tregunno, Anne-Marie Robert, Dr. Hong-Xing Wu, Michael Halucha, Judith O’Brien, Rhonda Fraser, Meheria Arya, Benjamin Jiaming Wang, Aimée Campeau, Stephanie Davies and Lori Engler-Todd.
Key messages
This Report raises awareness about how our built environment provides a foundation for healthy living and ultimately our health.
It is possible to improve or worsen the health of populations by changing our physical world. Conditions and chronic diseases linked to unhealthy living are increasing in Canada. For example, over 7.8 million Canadians 18 years and older were living with obesity in 2015, which is more than a quarter of this population. Obesity increases the risk for premature death and chronic diseases, such as cardiovascular disease, cancer and diabetes.
The relationship between the built environment, healthy living, people’s behaviour and health status is complex. Even so, cities and communities can be designed and built to set people up for success so that healthy choices are the easier choices.
The majority of Canadians – about 80% – live in urban or suburban areas. While there are trends, the health of a population varies within the same geographic area. The rise of urban sprawl is a concern as it has been linked to sedentary lifestyles, easy access to unhealthy food, more time spent driving, less physical activity and higher rates of obesity.
While we know that changing the built environment can be a cost-effective way to increase physical activity, less is known about how to improve healthy diets and mental wellness through neighbourhood design as these are newer fields of study.
Improving the opportunity to cycle, walk or take public transit to work or school by changing the built environment is a growing area of research. Changing the built environment could significantly influence people’s daily physical activity. Community design features, such as connected streets, a mix of residential, commercial, educational and employment areas, bike paths, and good public transit can support being active to get to work or other places; whereas green spaces, waterways, walking paths, trails and recreation facilities can promote recreational physical activity.
Neighbourhoods with easy access to healthier food options appear to be linked to better diets and better health. Those with a higher ratio of unhealthy to healthy food options appear to be linked to poor diets and worse health. However, there are significant gaps in our knowledge and other factors, such as affordability, may have a bigger influence on diet than the built environment.
Neighbourhoods may not be set up to address social isolation and loneliness. Communities with houses that have front yards or that are close to the street, have destinations to walk to and have places for people to gather could encourage social interaction. Studies suggest that green spaces are linked to a variety of health benefits including lower risk for premature death. Ties to the land, water, family, community and identity, as well as a holistic, interconnected view of health and well-being are important components of Indigenous culture that can provide insight into healthy neighbourhood design.
Going forward, decision-makers and planners at all levels should take a multi-sectoral, collaborative approach and consider health as an important outcome as appropriate when making infrastructure planning decisions. More targeted and hypothesis-driven research, standardized data collection, and systematic evaluations of the health impact of community design features are needed. With the diversity of communities and cities across Canada, considering context and engaging citizens are important for ensuring that a community’s unique needs are met when designing for healthy living.
Understanding the complexities of the link between the built environment and health
Recognizing the complexity of the link between the built environment, healthy living and people’s behaviour is essential when designing communities to improve health. For example Footnote 1-10
It is important to consider where a neighbourhood is situated and who lives there: Neighbourhoods are situated within a bigger context and are impacted by many factors beyond the built environment including laws, policies, socioeconomic factors, culture, beliefs and attitudes. Neighbourhoods are also dynamic and change over time. For example, people move in and out of neighbourhoods for many reasons, including due to their current state of health. People tend to live in neighbourhoods with others who are similar to them, often having similar characteristics, such as culture, values or socioeconomic status.
People’s behaviour and health are affected by many factors: Where we live is one factor among many that influences behaviour and health. Where people live, work, study, shop, play and are active can involve many neighbourhoods. Because it can take time for a neighbourhood to impact the health of its residents, it is difficult to identify which features or which neighbourhoods create a health impact on a population – for example, effects on health could be due to features that no longer exist or neighbourhoods that people lived in as children.
Applying research can be challenging: Research in the area of health and the built environment is rapidly evolving. To date, most studies have been observational and cross-sectional (comparing different groups of people at a specific point in time), making our ability to determine which neighbourhood features cause changes in health challenging. More targeted and hypothesis-driven research and evaluations of the health impact of community design features are needed.
Researchers also use a variety of definitions, methods and measures, which has led to some contradictory results. This limits our ability to draw conclusions and to develop effective initiatives based on existing evidence. Each community is unique with different characteristics, behavioural norms and needs. It can be difficult to directly apply findings from one community to another, including the application of findings from the United States or Europe to the Canadian context. Standardized, open data collection would support knowledge sharing and identification of approaches that can be effective across different communities. Within Canada, much of the research is situated in large urban settings, meaning there is a gap in our knowledge of the role of the built environment in small, rural, remote and Indigenous communities.
Section 1: What this report is about
This Report raises awareness about how our built environment provides a foundation for healthy living and ultimately our health.
It is possible to improve or worsen the health of populations by changing our physical world. The percentage of Canadians who report they are obese, living with diabetes, or a mood disorder has been increasing in Canada.Footnote 11,Footnote 12 These health issues have a serious impact on quality of life and are linked to some of the leading causes of death, including cancer, cardiovascular disease and respiratory disease.Footnote 13
Lifestyle factors, such as a lack of physical activity, sedentary behaviour, poor diet and lack of social connection can increase the risk for poor health outcomes.Footnote 14-18 For example, evidence suggests that about 30% of cancers can be prevented by adopting a healthy lifestyle.Footnote 19 While healthy behaviour is shaped by many forces, these lifestyle factors are all influenced by our built environment.
What is the built environment? For the purposes of this report, the built environment is defined as the external physical environment where we live, work, study and play. It includes buildings, roads, public transit systems, parks, and other types of infrastructure. It is linked to how we design, plan and build our communities.Footnote 20
This report focusses on the built environment and healthy living in terms of physical activity, healthy diets and mental wellness (including social connectedness). Although this report addresses these topics separately, it is recognized that they interact and influence health together. For example, a healthy diet and physical activity can lead to weight loss and reduced risk for obesity separately, but are more effective in combination.Footnote 21
There are many other ways that the built environment can impact health including through its role in air pollution, safety (e.g., injuries), housing, heat, UV exposure, climate change and natural disasters.
Healthy cities and communities are also defined by more than their built environment. Examples of other factors that are important to consider include inequity in terms of health and poverty, community engagement, social factors, cultural factors, economic factors and factors linked to the natural environment.
Changing Canadian lifestyles
In the 1940s, the split between urban-rural living was about 50-50; now about 80% of Canadians live in an urban or suburban area.Footnote 22Our communities are changing and often expanding through urban sprawl rather than by building compact and complete communities.Footnote 23-26 Urban sprawl has been linked to sedentary lifestyles, easy access to unhealthy food, less physical activity and higher rates of obesity.Footnote 27-36 One of the key results of urban sprawl that may explain some of these impacts is more time spent driving.Footnote 34-36 From 1999 to 2016, the number of registered light motor vehicles including cars and SUVs in Canada has increased at a faster rate than Canada’s population, at 36% compared to 19%. This suggests that Canadians are increasingly relying on driving.Footnote 37,Footnote 38
What is urban sprawl? Urban sprawl refers to urban areas expanding beyond their core, often into rural areas to form suburbs. This frequently results in different land use design than in urban centres, a lack of diversity in land use across suburbs and the need for more roads and infrastructure.Footnote 27 Footnote 39
Physical activity and sedentary behaviour:Although they appear to be the same, lack of physical activity and sedentary behaviour are two separate concepts. Lack of physical activity involves not being active enough to meet physical activity guidelines. Sedentary behaviour is any behaviour that involves low energy expenditure, such as sitting or lying down. Based on these definitions, an individual can be both active and sedentary.
Neighbourhoods to support healthy living
Figure 1 explains how neighbourhoods can be designed and built to provide a foundation for healthy living by promoting physical activity, healthy diets and supportive environments. These can be simple, practical measures, such as having stores that sell fresh fruit and vegetables near to where people live.
Figure 1: Examples of potential pathways from a neighbourhood’s built environment to good health. e.g.,Footnote 42-59
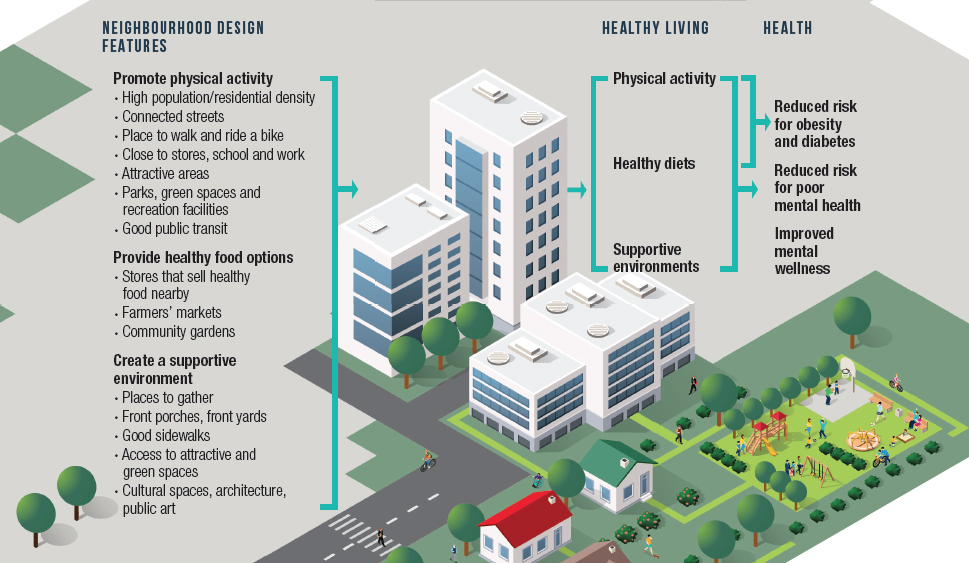
Figure 1 - Text Equivalent
This image depicts how neighbourhood features may lead to good health through healthy living. Examples of neighbourhood design features that may promote physical activity include high population/residential density, connected streets, places to walk and ride a bike, living close to stores, school and work, attractive areas, parks, green spaces and recreation facilities, and good public transit. Examples of neighbourhood design features that may provide healthy food options include stores that sell healthy food nearby, farmers’ markets and community gardens. Examples of neighbourhood design features that may create a supportive environment include: places to gather, front porches, front yards, good sidewalks, access to attractive and green spaces, cultural spaces, architecture, and public art. Features that promote physical activity may lead to a reduced risk for obesity, diabetes and poor mental health as well as improved mental wellness. Features that provide healthy food options may lead to healthy diets which may reduce the risk for obesity, diabetes and poor mental health as well as improve mental wellness. Features that create a supportive environment may lead to a reduced risk for poor mental health and improve mental wellness.
We do not yet know how to quantify the extent to which the built environment affects healthy living, but we know enough to say with confidence that neighbourhoods that are built with health in mind are important for making healthy choices the easiest choices. For example, this could involve designing communities so that people live close enough to walk or bike to work or school.
The most developed area of research related to the built environment and healthy living is about the impact on physical activity. Research has shown that changing the built environment is a cost-effective way to increase physical activity in large populations. Examples include building multi-use trails on the bed of former railway tracks, equipment in parks, new bike and walking paths and easy access to recreation facilities.Footnote 40,Footnote 41 The roles of the built environment in healthy diets and mental health and wellness are still relatively new fields of study. Our knowledge is growing.
Building healthier Canadian neighbourhoods
Many Canadian cities are changing our built environment for the better. The concept of designing healthy cities as a global issue emerged from an initial healthy cities workshop held in Toronto in 1986.Footnote 60,Footnote 61 Today, there are many promising approaches available to improve communities with most focusing on urban settings.Footnote 62 Multiple sectors working together with community planners is essential to building healthy communities and supporting healthier Canadians.Footnote 62,Footnote 64
Snapshot of what Canada’s largest cities are doing:
- Vancouver’s Healthy City Strategy
- Toronto’s Complete Streets Guidelines
- Montreal’s structuring efficient transportation networks to fully integrate into the urban fabric(in French only)
Figure 2 captures the complexity of the built environment’s link to behaviour and health outcomes. It outlines how the built environment and other mediating factors can influence human behaviour which can lead to different health outcomes. This complex relationship exists within a multi-dimensional context defined by other determinants of health, such as age, genetics, gender, social environment, culture and health care.
Figure 2 : Overview of how the built environment might influence health. (adapted fromFootnote 72)
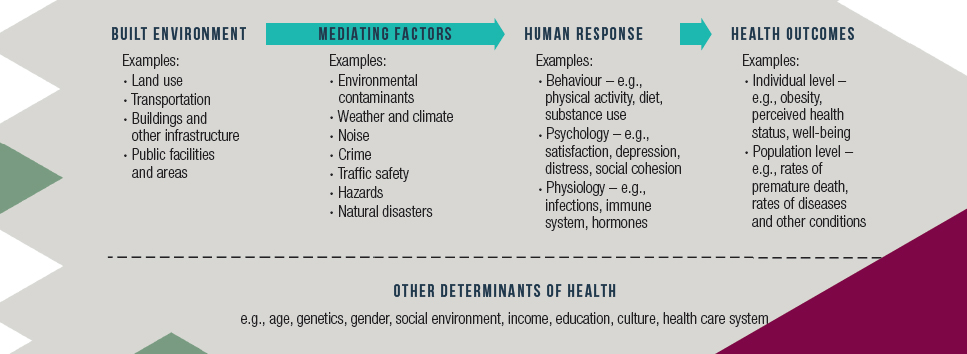
Figure 2 - Text Equivalent
This image depicts how the built environment may lead to various health outcomes based on human responses to the environment and the influence of various mediating factors and other determinants of health. Examples of features in the built environment that may impact health include land use, transportation, buildings and other infrastructure, and public facilities and areas. Examples of mediating factors include environmental contaminants, weather, climate, noise, crime, traffic safety, hazards and natural disasters. Examples of possible human responses to the built environment include behaviours such as physical activity, diet and substance use, psychological responses including satisfaction, depression, distress and social cohesion, and physiological response such as infections, activated immune system and hormones. Examples of possible health outcomes that are influenced by mediating factors and that result from human responses to the built environment include outcomes at the individual level, such as obesity, perceived health status and well-being and outcomes at the population level, such as premature death and rates of disease and other conditions. This complex interaction between the built environment and mediating factors that lead to human responses and health outcomes are all influenced by other determinants of health such as age, genetics, gender, social environment, income, education, culture and the health care system.
The history of public health and urban planning: Public health and urban planning have a long history of working together to tackle disease. In the early 1900s, the focus of this collaboration was on improving sanitation, reducing overcrowding to reduce infectious disease and moving people away from areas with high pollution. However, separating residential areas from areas of employment has likely contributed to our reliance on motor vehicles and urban sprawl.Footnote 31,Footnote 70,Footnote 71 More recently, public health professionals and urban planners are working together to tackle health issues linked to urban sprawl, such as low levels of physical activity and high rates of chronic diseases and conditions, such as obesity and diabetes.Footnote 70,Footnote 71
What this report covers
This report brings together evidence to explore how we can design Canadian communities to serve as a foundation for healthy living. Included in this report are the following sections
- Canadian communities – This section provides an overview of the Canadian context through a snapshot of trends in health, data on Canada’s population and urban, suburban and rural health.
- Building blocks of healthy living – This section explores how the built environment can create active neighbourhoods, influence healthy diets and lead to supportive environments.
- Design features and specific populations – This section covers how the built environment can affect health in different populations by focusing on children, youth and older adults, as well as populations experiencing health inequity.
- Designing communities for healthy living in Canada – This section provides an overview of how different sectors work together to design healthy communities in Canada and also provides examples of initiatives and approaches underway in some Canadian cities.
- A call to action – This section aims to provide guidance on how we can better harness the impact of the built environment to improve the health and well-being of Canadians.
Section 2: Canadian communities
This section provides a snapshot of broad factors that differ across Canada and that also relate to the built environment.
While the majority of Canadians, about 80%, live in urban areas, Canada’s considerable geographic expanse creates communities with unique characteristics and needs. This diversity and how it is changing are important to consider when thinking about the built environment and its impacts on health.
Trends in Canadian health
Canadians are generally healthy, but some Canadians are healthier than others.Footnote 11 Diseases and conditions that are linked to unhealthy living have been increasing in Canada. For example, the percentage of Canadians
- Aged 20 years and older living with diabetes has increased from 6% in 2000 to 10% in 2011 (based on hospitalization and physician claims).Footnote 11
- Who were obese increased from 21% in 2003 to 25% in 2012.Footnote 12 Data from a revised survey on Canadians ages 18 years and older showed that rates of obesity have increased from 23% in 2004 to 27% in 2015.Footnote 73 Obesity in younger children appears to be decreasing from 14% in 2004 to 10% in 2015.Footnote 74
- Who said they had been diagnosed with a mood disorder increased from 5% in 2003 to 8% in 2014.Footnote 11
Diabetes, obesity and mental health issues are all linked to a wide variety of other diseases and conditions, making them proxies for overall health.Footnote 11,Footnote 19,Footnote 690-692
Canada’s population is aging: The 2016 Census showed that for the first time, there are more adults over the age of 65 years (5.9 million) than children under the age of 15 years (5.8 million). The number of Canadians over the age of 85 years is growing four times more quickly than the overall Canadian population.Footnote 75,Footnote 76
However, the Prairie Provinces, the Territories and Indigenous populations have proportionally more children than older adults. Ontario has a similar proportion of each age group.Footnote 75
Large urban areas are aging less quickly than rural areas. The suburbs have even younger populations than urban centres.Footnote 75
Where Canadians are living in 2016
In 2016, Canada’s population reached more than 35 million people. Canada has one of the lowest population densities in the world at four people per square kilometre (km2); however, its population is largely clustered in a smaller area, mostly in urban centres and along the southern border with the United States.Footnote 23,Footnote 77
In 2016, it was estimated that
- 27 million or 76% of Canadians lived in areas with more than 100,000 residents.Footnote 24
- 86% of Canada’s population resided in four provinces: Ontario (38%), Quebec (23%), British Columbia (13%) and Alberta (12%).Footnote 23
- 12.5 million or almost 36% of Canadians lived in one of Canada’s three largest urban centres, namely Toronto, Montreal or Vancouver.Footnote 23
- The population of Canada’s three territories was 2% the size of Toronto’s population.Footnote 78
Defining urban and rural areas: There are many definitions used to categorize urban and rural areas.Generally, urban areas have large populations in relatively small areas. Rural areas have small populations and are defined as any settlement lying outside urban or suburban areas.Footnote 25,Footnote 39,Footnote 80-82
Statistics Canada defines an urban area or population centre as having a population of at least 1000 and a population density of at least 400 people per km2. Rural areas are those that are outside an urban area.Footnote 82
Rural areas can include small towns, villages and other settlement of fewer than 1000 people and areas that contain estate lots, agricultural land, undeveloped areas and remote and wilderness areas.Footnote 82
For First Nations communities, Indigenous and Northern Affairs Canada defines urban, rural, remote and special access by proximity and access to nearest service centre:Footnote 83
- Urban – within 50km and having road access; just over 34% of communities.
- Rural – between 50 to 350 km and having road access; 44% of communities.
- Remote – over 350 km and having road access; almost 4% of communities.
- Special access – no year-round road access; 17% of communities.
Suburban living
By the 1960s, many Canadians lived in what we recognize today as suburbs.Footnote 63 Evidence shows that suburbs are not a new phenomenon, reaching back to at least medieval times. Their form and function as well as the characteristics of their residents have changed over time, affected by various events such as the Great Depression and the World Wars.Footnote 63 Compared to urban areas that have compact, walkable neighbourhoods, suburban living is often viewed as having an over-reliance on driving and fewer places to walk to, which can lead to less physical activity and more sedentary behaviour.Footnote 27-32,Footnote 34-36
There is no universal definition of what constitutes a suburb. Suburbs can be defined in many ways, including through administrative or political boundaries, boundaries of a city’s central core, distance from city centre or population density.Footnote 39 How many Canadians live in the suburbs depends on the definition used. Canadian data show that
- When defining suburbs by administrative or political boundaries, a greater proportion of people lived in the suburbs in Toronto (51%), Montreal (55%) and Vancouver (73%) in 2006. A smaller proportion of people lived in the suburbs in Ottawa (28%), Calgary (8%), Edmonton (29%), Quebec City (31%) and Winnipeg (9%).Footnote 39
- In 2016, the population of municipalities that were located near large urban centres continued to grow at a faster pace (7%) than the large urban centres (6%). An example of a municipality located near a large urban centre is Whistler, British Columbia which is located near Vancouver. Municipalities that were located farther away from any size of urban centre were less likely to have a growing population.Footnote 25
- For municipalities located within large urban areas, 31 had a population growth that was more than three times the Canadian average of 5%. Almost 26% of these municipalities were located in Montreal. Examples of municipalities located within large urban areas include Mirabel which is part of the greater Montreal and Cochrane which is part of the greater Calgary area.Footnote 25
- The proportion of Canadians living in single-detached homes, which is a common characteristic of suburban areas, has been decreasing over the last 30 years, although more than half of Canadians lived in single-detached houses in 2016. Among Canada’s top ten most populated cities, multiple family dwellings (e.g., apartment buildings) were more common in Toronto, Montreal, Vancouver and Quebec City while single-detached homes were more common in Calgary, Edmonton, Ottawa-Gatineau, Winnipeg, Hamilton and Kitchener-Cambridge-Waterloo.Footnote 79
Urban and rural communities have different characteristics, needs and built environments. Although most Canadians live in or near urban areas, 20% of Canadians live in rural areas. Most research on the built environment and its influence on health has focused on urban areas. Existing research on rural areas suggests that they may need a tailored approach.e.g.,Footnote 84,Footnote 85
Urban, suburban and rural health
Health differs across and within urban, suburban and rural areas.Footnote 86 Factors such as age, gender, income, education, employment, population mobility, health care access and other characteristics likely play a role.Footnote 86-91,Footnote 98-100
Determining which areas are healthier and why is challenging due to
- Multiple definitions of urban, suburban and rural areas.
- Large variation in health status within urban, suburban and rural areas. For example, within urban areas, poor health can cluster in disadvantaged neighbourhoods.e.g.,Footnote 94,Footnote 101-104
- Differences in how communities are designed in urban, suburban and rural areas.
- Variations of socio-demographic factors across communities, such as age and income that influence health.
- Mobility of populations, particularly people moving from rural to urban areas.
- Changes in determinants of health across communities over time.
Typically, data on urban, suburban and rural differences provide only a snapshot of the health of current residents. Data from the United States suggest it is important to track changes over time. For example, urban areas in the United States have experienced a larger decrease in mortality rates for many diseases and conditions than rural areas, creating a widening gap in health inequity.Footnote 89
Older Canadian data show that which area is healthier depends on the health outcome being measured. People living in urban areas tend to have lower mortality rates for injury, poisoning, suicide and motor vehicle accidents as well as lower rates of smoking, arthritis and being overweight or obese and higher rates of people eating recommended amounts of fruit and vegetables than rural or suburban areas.Footnote 86 Urban areas also tend to have higher rates of cancer, infectious disease, stress and a weaker sense of community belonging. Urban residents are also more likely to be exposed to poor air quality.Footnote 86,Footnote 93-97
People living in rural areas were more likely to report they were in poor or fair health, were less stressed and had a stronger sense of community belonging than people living in urban or suburban areas. Residents of rural areas also tended to have the highest rates of mortality from all causes as well as from respiratory disease, the latter of which may be linked to smoking patterns. Generally, the more rural the area, the worse the health outcome for these measures, but the stronger the sense of community belonging.Footnote 86
Determining how healthy suburbs are is complicated and sometimes contradictory. Urban sprawl has been linked to sedentary lifestyles, easy access to unhealthy food, less physical activity and higher rates of being overweight or obese.Footnote 27-36,Footnote 86Yet when suburban areas are defined based on the proportion of residents who commuted to work in larger urban centres, those areas with the highest proportion had the lowest rates of people living with any chronic disease or dying from all causes, circulatory disease, respiratory disease, cancer or diabetes. Men living in these areas also had longer life expectancies than all other areas.Footnote 86 Suburbs with a strong connection to urban centres may benefit more from a range of employment opportunities and services.
Where people grow up may affect their health differently than where they live as adults. For example, some evidence has shown that people who grow up in an urban area react more strongly to stressful social situations than those who grow up outside urban areas.Footnote 113,Footnote 114How long an individual has lived in an area may also have an effect. For example, living or growing up in urban areas has been linked to a higher risk for poor mental health, a difference that cannot be fully explained by socio-demographic factors, such as age, gender, marital status, socioeconomic status or ethnicity.Footnote 105-112 This risk may be “dose-dependent” - the longer someone has lived in an urban environment or the “more urban the environment” (e.g., higher population density), the higher the risk.Footnote 110-112
Section 3: Building blocks for healthy living
3A: Active neighbourhoods
This section explores research on how we can build active communities to improve health.
The majority of Canadians do not get enough exercise.Footnote 115 Being physically active is an essential component to good health, yet Canadians are generally not active enough to gain optimal health benefits. How can we increase physical activity? Building communities that make being active an easy choice is an important step. Figure 3 shows how the complexity of neighbourhood features is likely linked to better health by increasing physical activity.
Figure 3: Overview of how the built environment influences physical activity to influence health. (adapted fromFootnote 72)
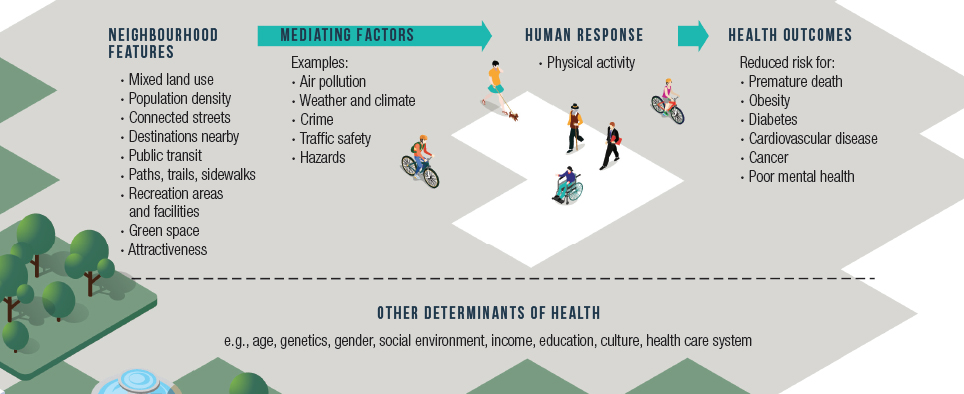
Figure 3 - Text Equivalent
This image depicts how the built environment may lead to various health outcomes based on increasing physical activity and the influence of various mediating factors and other determinants of health. Examples of features in the built environment that may increase physical activity include mixed land use, population density, connected streets, destinations nearby, public transit, paths, trails, sidewalks, recreation areas and facilities, green space and attractiveness. Examples of mediating factors include air pollution, weather and climate, crime, traffic safety and hazards. Examples of possible health outcomes include reduced risk for premature death, obesity, diabetes, cardiovascular disease, cancer and poor mental health. These complex interactions between the built environment and mediating factors that lead to human response and health outcomes are all influenced by other determinants of health, such as age, genetics, gender, social environment, income, education, culture and the health care system.
Physical activity and health
Globally, physical inactivity is thought to cause 6% to 10% of non-communicable diseases.Footnote 117 At least 30 minutes of moderate physical activity a day can decrease the risk of premature death by at least 19%.Footnote 118 Being physically active is strongly linked toFootnote 119-145
- Better muscle strength, cardiovascular function and mental health.
- Healthy development in children and youth.
- Healthy aging.
- Reduced risk for premature death, even with a small increase in physical activity.
- Reduced risk of diseases and conditions such as obesity, heart disease, some types of cancer, diabetes, dementia, osteoporosis, and cardiovascular issues.
- Better health in people who are living with various diseases and conditions (e.g., cancer, diabetes, mood disorders).
Did you know? In 2013, only 10% of Canadian children and youth and 20% of Canadian adults met the Canadian Physical Activity Guidelines when their activity levels were measured via accelerometers.Footnote 115
The Guidelines recommend that:
Toddlers should do at least three hours of physical activity over each day of any intensity.
Children and youth should do:
- At least one hour a day of moderate to vigorous aerobic activity.
- Muscle and bone strengthening exercise at least three times a week.
- Several hours of light activity per day.
Adults should do:
- At least 150 minutes of moderate to vigorous aerobic activity per week.
- Muscle and bone strengthening exercise at least twice a week.
These are recommended levels; however, people can still achieve health benefits from lower levels of activity. Health benefits of increasing activity may be greatest for those who are inactive.Footnote 116
Building neighbourhoods that promote physical activity
Neighbourhoods can be designed to promote utilitarian (activity to get somewhere or do something), recreational (activity during leisure time) physical activity or both. Both types of activity can be important contributors for meeting physical activity guidelines and are linked to similar and different types of neighbourhood features.
At a population level, efforts have focused on harnessing the built environment to build communities that encourage active transportation in the forms of walking, cycling and using public transit, as well as recreational physical activity. In some situations, the relationship between the built environment and physical activity has been linked to better health, such as lower body mass index and body fat; improved cardiovascular disease risk factors; lower risk for cancer; lower risk for premature death from all causes; better mental health; and a stronger sense of community belonging.Footnote 146-168
Encouraging active transportation: Walking and cycling are common forms of physical activity and active transportation
- Walking is popular and considered to be a great way to be physically active for all ages. It is often a better choice in busy, dense areas.Footnote 169-170
- Cycling is an efficient way of being moderately to vigorously active and allows people to travel farther distances than walking. It often has less infrastructure to support it than has walking.Footnote 169,Footnote 177
What is active transportation? Active transportation is the use of human powered transportation to get places. Examples include biking or walking to work.Footnote 171 Public transit is also a form of active transportation as people walk to access public transit or to their destination at the end of their trip.Footnote 172-176
Active transportation can contribute to people’s daily physical activity.Footnote 178 Not many people currently use active transportation.Footnote 167 At a population level, active transportation has good potential to increase people’s activity levels and improve their health.Footnote 168 It is one way to
- Address people’s lack of time to be physically active.
- Reduce the amount of time Canadians spend driving.
- Help people reach recommended levels of physical activity.
The built environment can play an important role in active transportation. Generally, areas with higher population density, a mix of residential, commercial, educational and employment areas, connected streets, good access to destinations, good public transit and attractiveness have been linked to more active transportation or reduced driving, although the strength of this link is unclear.Footnote 179-187 In Canada, active transportation has been linked to havingFootnote 179,Footnote 188,Footnote 189-192
- A public transit stop nearby.
- A choice of destinations within a reasonable distance.
- Well-maintained sidewalks.
- Dedicated areas for cycling.
- Affordable recreation facilities.
- Safe traffic.
For cycling, examples of features that have been linked to active transportation include bike paths close to where people live; bike paths that provide access to a variety of destinations in a short distance; good connections between roads and routes; safe cycling routes; safe places to park bikes, including near railway or bus stations; available short-term bike rentals; signals and traffic lights for cyclists; and routes with fewer hills and safer traffic. Footnote 49,Footnote 169,Footnote 177,Footnote 193-205
Examples of initiatives on active transportation in Canada can be found here: Public Health Agency of Canada.
Did you know? In 2011Footnote 188
- 62% of Canadians said there were stores within walking distance of their home.
- 78% had free or low-cost recreational facilities and areas nearby.
- 72% had a transit stop within a 15 minute walk of their home.
- 70% said they lived in an attractive neighbourhood.
Canadians were more likely to be active if their neighbourhoods had places to walk to (e.g., stores), free or low cost recreational facilities or areas specifically for cycling, good sidewalks, interesting features and a higher level of safety.Footnote 188
There are other factors to consider in terms of active transportation. For example, providing employment opportunities closer to where people live and making driving a less appealing choice than active transportation.Footnote 180,Footnote 181,Footnote 200 Examples of strategies that have led to less traffic on the roads include car free zones or days, increasing the cost of driving and free or low cost public transit.Footnote 209-216 Places like Canada where residents can have long distances to travel and rely heavily on motor vehicles may have difficulty implementing some of these strategies.
Promoting recreational physical activity: Physical activity during leisure time is not always linked to the same neighbourhood features as active transportation.Footnote 166,Footnote 191,Footnote 217 Some evidence also suggests that people who live in walkable neighbourhoods and are more likely to use active transportation may be less likely to be active during their leisure time.Footnote 185,Footnote 190
Recreational walking is linked to neighbourhood features such as destinations (e.g., lakes, waterways, sports and cultural destinations), attractiveness, good street lighting, good sidewalks, paths and trails, nearby recreational areas and facilities and green space.Footnote 54,Footnote 217-223 Canadians who live in neighbourhoods with these features were more likely to be active during their leisure time. Traffic and safety can also influence leisure time activity.Footnote 188
A role for raising awareness: Believing that a neighbourhood is walkable, whether or not it actually is, is linked to more walking and better health.Footnote 206-208 This suggests that raising awareness about a neighbourhood’s walkability could be an important way to increase physical activity.
Mediating factors affecting the link between the built environment, physical activity and health
The built environment can impact people’s physical activity and their health. However, there are factors that can affect this link and that should be considered when designing communities. Examples that are relevant in Canada include traffic safety, air pollution, weather, climate and daylight.
Population density: Estimates from the United States suggest that neighbourhoods with a population density of around 360 to 1540 people per km2 are linked to more walking. Less time driving is linked to neighbourhoods with a population density of 1160 people per km2 or more.Footnote 229 In 2016, there were 32 urban areas in Canada with a population density of at least 360 people per km2 and one with a population density of at least 1160 people. About 43% of Canada’s population lived in these urban areas.Footnote 230 Within Canadian urban areas, population density differs across neighbourhoods with those closest to the city’s centre often being most dense (e.g., TorontoFootnote 231) .
Traffic safety: Evidence suggests that the health benefits of walking or cycling are greater than the risk for injury from traffic.Footnote 232 People are more likely to choose active travel when they feel it is a safe alternative. There are many ways to build infrastructure to make roads safer for motor vehicles, pedestrians and cyclists. Effective approaches to influence traffic safety involve reducing speed (e.g., speed bumps, speed limits, narrowing lanes), decreasing points of conflict with pedestrians and cyclists, increasing visibility of pedestrians (e.g., curb extensions) and diverting traffic away from residential areas.Footnote 45,Footnote 56,Footnote 233,Footnote 234
Pedestrian safety can also be increased through pedestrian signals, traffic lights, signs to remind pedestrians to look for vehicles, pedestrian islands, overpasses, underpasses, barriers, fences, sidewalks and good streetlights.Footnote 236,Footnote 237 Collisions between pedestrians and vehicles are more likely to occur near schools and in commercial areas and are linked to higher population density, traffic volume, pedestrian volume, road density and number of intersections.Footnote 237Canadian research has shown that people will choose to walk or bike if their route is safe and attractive. Some evidence suggests that cyclists will pick a safer, more attractive route over a shorter, more direct route.Footnote 232,Footnote 238-242
Cycling safety can influence the likelihood that people will use their bikes. People cycle more when they feel safe and dedicated infrastructure for cycling is available. This may be particularly important for those who are less confident on a bicycle.Footnote 55,Footnote 243 Approaches such as having dedicated cycling routes, paths and lanes, reducing speed limits for motor vehicles, having places to cycle to, having access to public transit and having good street connectivity have been linked to more cycling. More traffic, highways and congestion are linked to less active travel, including less cycling. Some approaches for reducing the number of motor vehicles on the road, such as increasing costs of motor vehicle ownership, limiting parking and car-free areas might also help increase walking and cycling.Footnote 243
Cycling – global comparisons: Cycling on a regular basis is popular in several European countries, particularly the Netherlands, Denmark, Germany, Finland, Sweden and Belgium. Cycling is also safer in these countries.Footnote 224 It is supported through widespread dedicated cycling infrastructure, traffic calming in residential neighbourhoods, bike parking, integration with public transit, traffic education for both drivers and cyclists and events that promote cycling and increase public support. In these cities, mixed land use and high population density ensures there are many places that are accessible by bike. Owning a car is also expensive, and driving to get places is challenging, although some countries like the Netherlands and Germany have high levels of car ownership and cycling.Footnote 200,Footnote 225
Cycling on a regular basis is not nearly as popular in North America. In 2013/2014, about 12 million or 41% of Canadians said they had cycled at least once in the previous year. Younger Canadians were more likely to use their bikes than older Canadians, and men were more likely to use their bikes than women. Men living in urban areas were more likely to cycle than men in rural areas; however, the opposite pattern was seen for women. Canadians are less likely to ride their bikes than in the past, a trend that is likely not due to the aging population. It may be at least partially due to increases in other activities such as running.Footnote 226
Canadians are more likely to use their bikes than Americans. This difference is thought to be due to a more supportive built environment for cycling in Canada (e.g., mixed land use, short distances to destinations, higher costs of driving, safer cycling, more dedicated cycling infrastructure and training related to cycling).Footnote 227,Footnote 228
Air pollution: Being active (e.g., running, cycling) in high traffic areas can increase the risk for exposure to air pollution.Footnote 244 Exercise may increase the amount of pollution that enters the lungs. Air pollutants can irritate the lungs, changing breathing patterns and heart rate during exercise.Footnote 247Particulate matter can increase blood pressure and heart rate as well as activate the immune system.Footnote 248In Canada, this is less of an issue than in other countries because generally, Canada’s air quality is relatively good.Footnote 245,Footnote 246
Did you know? In 2014,90% of people worldwide were living in places where air quality did not meet the World Health Organization’s air quality guidelines (for fine particulate matter).Footnote 263 As a whole, Canada’s air quality meets these standards, although air quality does vary across the country.Footnote 263,Footnote 264
What are the risks? Footnote 168,Footnote 249-254
- There are more health benefits from exercise than there are health impacts from exposure to air pollution, except in areas with high levels of air pollution.
- There are many harmful pollutants inside motor vehicles, sometimes at levels that are higher than outside the vehicle.
People can reduce their exposure to air pollution while being active outside by using roads that are less busy or paths and trails without motor vehicle traffic as well as by avoiding exercise or exercising less intensely on days when air quality is poor.Footnote 271,Footnote 272
Information on daily air quality in Canada can be found at the Air Quality Health Index.
Exposure to air pollution is linked to an increased risk forFootnote 254-270
- Premature death from diseases and conditions such as heart disease, stroke, respiratory disease, lung cancer, diabetes, and respiratory infections in children.
- Poor respiratory and cardiovascular health even at low levels of exposure, especially among people at greater risk, such as those with asthma and other lung conditions, children and older adults.
- Living with respiratory disease, asthma, pneumonia and otitis media in children, sudden infant death syndrome, adverse birth outcomes (particularly in mothers with pre-existing medical conditions), atherosclerosis, hypertension, diabetes and neurological conditions such as dementia.
Weather, climate and daylight: It is no surprise that bad weather, unsafe conditions due to weather, extreme temperatures and lack of daylight all reduce the likelihood that people will be active outdoors.Footnote 273-292 Even in Nordic countries like Finland where many people use active transportation, the proportion of those who do so in the winter is lower than in warmer months.Footnote 293
This is an important consideration in Canada due to our diverse climate. However, it also provides an opportunity for innovation in the built environment to support physical activity across seasons and different types of weather. For example, suggestions to increase physical activity in colder months include having better access to more and better indoor recreation facilities (e.g., swimming pools, gyms) and promoting facilities for outdoor winter recreation (e.g., skating, snowshoeing, skiing).Footnote 281 Well-lit neighbourhoods and access to indoor recreation facilities could also encourage physical activity during periods of shorter daylight.Footnote 291-295
3B: Access to healthy food
This section explores research that relates to how we can design communities that promote healthy eating.
A healthy diet is a key component of good health and involves eating healthy food and avoiding unhealthy food. What we choose to eat is influenced by many factors, including what food is available and accessible in our communities and beyond. Figure 4 shows how the complexity of neighbourhood features is likely linked to better health through healthy diets.
Figure 4: Overview of how the built environment influences diets to influence health. (adapted fromFootnote 72)
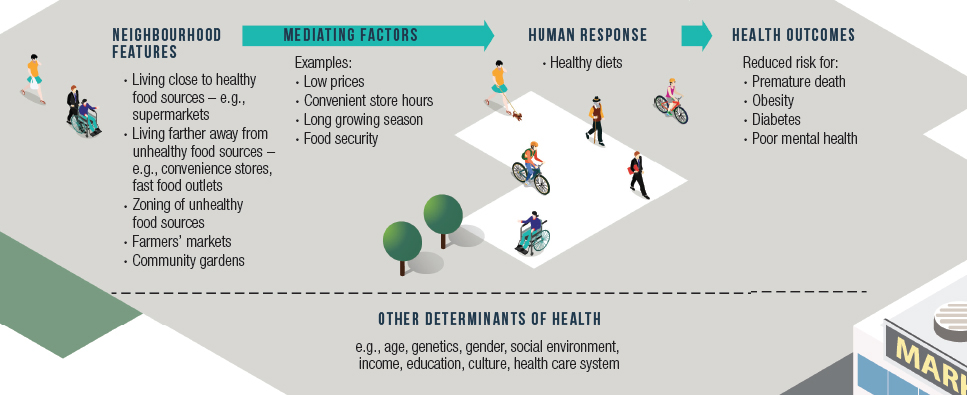
Figure 4 - Text Equivalent
This image depicts how the built environment may lead to various health outcomes based on promoting healthy diets and the influence of various mediating factors and other determinants of health. Examples of features in the built environment that may lead to healthy diets include: living close to healthy food sources, such as supermarkets; living farther away from unhealthy food sources, such as convenience stores and fast food outlets; and zoning of unhealthy food sources, farmers' markets and community gardens. Examples of possible health outcomes include reduced risk for premature death, obesity, diabetes and poor mental health. These complex interactions between the built environment and mediating factors that lead to human responses and health outcomes are all influenced by other determinants of health, such as age, genetics, gender, social environment, income, education, culture and the health care system.
Did you know? Many Canadians do not consume a healthy diet.Footnote 296 Canadian diets have been changing – the percent of daily energy intake from carbohydrates has been decreasing for Canadian adults while the intake of fat and protein has increased from 2004 to 2015.Footnote 297 Sugars account for just over 20% of Canadians’ total intake.Footnote 298,Footnote 299 Many Canadians do not meet recommendations for vitamin and mineral intake.Footnote 297
Diet and health
There is little doubt that a healthy diet is linked to better health. Generally speaking, there are certain foods that are considered to be healthy and that together, form a balanced, healthy diet. Examples include vegetables, fruit, grain products, low fat milk, fish and lean meat as well as traditional or country food for Indigenous populations. A balanced, healthy diet also involves eating regularly, consuming appropriate portions and minimizing how much food we eat that is high in saturated fat, sugar and salt.Footnote 300
Access to healthy food at work: Many people spend most of their waking day at work. Some evidence suggests that bringing food to work from home is linked to a healthier diet than buying food at work or near work.Footnote 301 Access to healthier food choices at or near work has also been linked to a healthier diet, but not necessarily to weight loss.Footnote 302-304 Workers in rural areas may face limited food choices.Footnote 305
There are many factors that influence what people choose to eat. Currently, many places that sell food offer a wide variety of choices that includes food that is high in calories, fat, sodium and sugar. This can create challenges for healthy eating. Information about food and nutrition is constantly evolving, often presenting conflicting messages about what to eat and what to avoid.Footnote 306 What constitutes a healthy diet and identifying how it contributes to better health can vary across individuals. People differ in how they digest and metabolize food, meaning not everyone reacts to food in the same way.Footnote 307,Footnote 308 Personalized diets are an emerging area of research that could lead to dietary advice that is based on individual differences.Footnote 309,Footnote 310
Building neighbourhoods that promote a healthy diet
We choose the food we eat based on many interconnected factors, including access to healthy food in our neighbourhoods. The built environment can play a role although results from research are mixed and sometimes conflicting.Footnote 311-313 Experts believe that current food environments are set up so that it is easy for people to eat unhealthy food.Footnote 314
Food or nutrition environments include a wide variety of factors that influence diet, such as government and industry policies, community environment (e.g., accessibility to and type and location of stores and restaurants), organizational environment (e.g., home, school, work, other), consumer environment (e.g., available food options, price, promotion, placement, nutrition information), media, advertising and individual characteristics (e.g., socio-demographic characteristics, psychosocial factors, perceived nutrition environment).Footnote 324 The built environment is part of this overall picture with its main focus being access to healthy and unhealthy food. There are gaps in our knowledge about the role of the built environment in healthy diets in Canada, particularly in rural and remote communities.Footnote 325
Examples of mediating factors that influence food choicesFootnote 58,Footnote 102,Footnote 148,Footnote 306,Footnote 315-323
- Food prices can have a bigger influence on diet and health than distance to a food source, particularly for low income families.
- Many people do not always shop for food in their home neighbourhoods and have access to transportation so they can buy food elsewhere.
- People tend to establish a routine and buy from the same stores most of the time.
- Many stores sell both healthy and unhealthy food. Store hours can affect access to healthy food.
- Access to healthy food differs across countries and municipalities. It can also differ across urban, suburban and rural areas.
Access to healthy and unhealthy food: Neighbourhoods that promote a healthy diet should aim to increase the availability and accessibility of healthy food for all residents. Affordability and food quality are also key factors.Footnote 325 Whether or not living near places that sell healthy and unhealthy food affects health is not clear. Some evidence suggests that when people have better access to sources of healthy food than they do to sources of unhealthy food, they are more likely to have healthier diets, are less likely to be obese and have a reduced risk for early death, but not all research has shown a link between access and health.Footnote 58,Footnote 316,Footnote 326-338
Access to alcohol: Easy access to alcohol is linked to increased alcohol consumption and negative health impacts. For example, neighbourhoods that have a higher density of places that sell alcohol were more likely to have incidents of violent crime, including family violence and motor vehicle accidents.Footnote 91,Footnote 340-345 A higher density of liquor stores was also linked to lower prices for alcohol, problem drinking and bigger impacts on health (e.g., alcohol-related hospital admissions, mental health).Footnote 346-351
Access is also an important factor to consider for other drugs, including for the public health implications of the legalization of cannabis.
Food deserts and food swamps: Food deserts are areas with limited access to nutritious and affordable healthy foods. Some evidence has shown that there is a link between food deserts and poor health, although not all research has found this effect.Footnote 148,Footnote 315,Footnote 327,Footnote 338,Footnote 339Food swamps are areas with many unhealthy food options. Evidence suggests that there is a link between food swamps and poor health (e.g., unhealthy diets, higher BMI, obesity, diabetes).Footnote 323,Footnote 339,Footnote 352-361
Food deserts and food swamps can co-exist in the same community. However, research suggests that in Canada and particularly in urban areas, food swamps are more common than food deserts.Footnote 362-364 Stores that sell food in rural areas can differ from stores that sell food in urban areas. Food deserts may be more common in rural areas.Footnote 320 Food deserts also tend to be common in remote communities, especially those without grocery stores.Footnote 325
Creating policies and legislation that restrict access to fast food by influencing where fast food restaurants are built and limiting unhealthy food sources (e.g., convenience stores) nears schools are approaches that have been considered to address unhealthy diets and obesity.Footnote 363-365 Zoning could also be used to support healthy diets (e.g., zoning that increases access to places that sell fruit and vegetables in rural communities).Footnote 363,Footnote 366
Farmers’ markets and community gardens: Cities and communities are using various approaches to bring healthy food options to their residents. Two examples include farmers’ markets and community gardens. Currently, our knowledge of their effectiveness is limited.
Farmers’ markets: To help provide their residents with better access to healthy food, some municipalities are supporting or considering farmers’ markets. Their impact appears to be localized, improving access to healthy food options for those who live nearby and in some cases, improving diets.Footnote 367-378 The variety of food is not always better at farmers’ markets than at supermarkets, and certain food can be more expensive.Footnote 379
Community gardens: Similar to farmers’ markets, community gardens are another approach being supported or considered. Some studies have found that community gardens have been linked to better diets, mental health and well-being, as well as lower BMI.Footnote 380-387 Community gardens tend to be found in areas with supermarkets, meaning people already have healthy food options available.Footnote 371 This can make it difficult to assess the impact of community gardens independently of supermarkets. Community gardens are also linked to community belonging and in some cases, social support.Footnote 388,Footnote 389
Mediating factors affecting the link between the built environment and diet
The impact of the characteristics of a particular neighbourhood on diet is often linked to access to healthy or unhealthy food. There are many factors that can influence or are related to food access, including seasons and food insecurity.
Seasons: Canada experiences distinct seasons and fluctuating growing seasons, with both affecting food growth and production as well as availability of traditional or country food. Although a wide variety of food is available all year for many areas in Canada due to food imports, the availability and price of fruit and vegetables in stores fluctuate across seasons.Footnote 390 Farmers markets and community gardens are also seasonal, providing fresh produce based on the growing season. Despite its short growing season, Canada produces a good amount of fruit and vegetables, and production has generally increased.Footnote 391,Footnote 392
Food insecurity: Access to food to form a healthy diet can be difficult for families experiencing food insecurity.Footnote 393 In 2014, about 12% of Canadian households were living with food insecurity at some point in the previous year. Not all provinces and territories collect information on food insecurity, so this is not a full estimate of the issue.Footnote 394
What is food security? Food security occurs when people can afford and have access to enough safe and nutritious food for a healthy diet and life. Lack of food security or food insecurity is linked to poor physical and mental health and wellness.Footnote 394,Footnote 395
Food security does not appear to be strongly related to living close to stores that sell food or to community food programs.Footnote 396,Footnote 397 Some evidence suggests that food insecurity is lower in rural areas, particularly for those areas with many farms.Footnote 394,Footnote 396
Food insecurity and food prices are much higher in the territories. In 2014, Nunavut reported that almost 47% of households experienced food insecurity in the previous year, and the Northwest Territories reported just over 24%.Footnote 394 In Nunavut, food insecurity was higher in smaller communities than in the capital, Iqaluit.Footnote 398 Examples of approaches that may help address food insecurity in the North include food sharing networks, better access to country food and community greenhouses.Footnote 399,Footnote 400
3C: Supportive environments
This section explores research that relates to how we can build communities that promote mental wellness.
Mental wellness is a key component of daily well-being and a healthy life. Many factors play a role in the risk for poor mental health, including where we live, work, study and play. Figure 5 shows how the complexity of neighbourhood features is likely linked to better health through social support, reduced stress and community belonging.
Figure 5: Overview of how the built environment influences social support, stress and community belonging to influence health. (adapted fromFootnote 72)
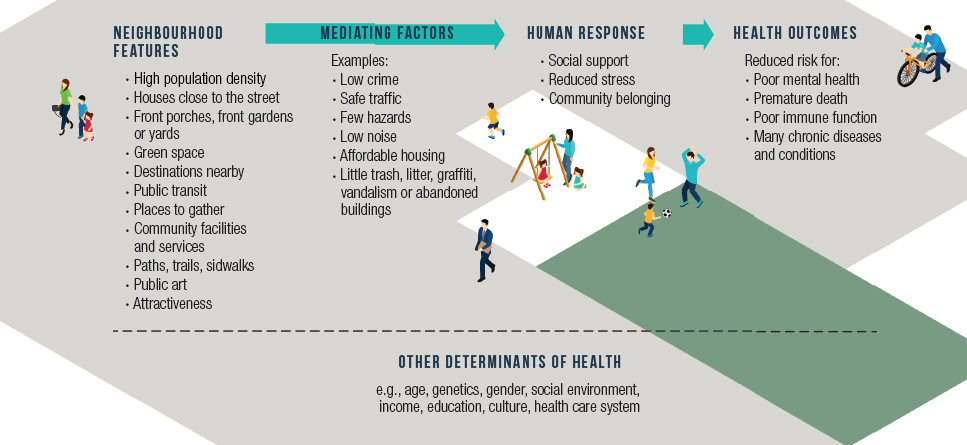
Figure 5 - Text Equivalent
This image depicts how the built environment may lead to various health outcomes based on creating supportive environments and the influence of various mediating factors and other determinants of health. Examples of features in the built environment that may create supportive environments include high population density, houses close to the street, front porches, front gardens, front yards, green space, destinations nearby, public transit, places to gather, community facilities and services, paths, trails, sidewalks, public art and attractiveness. Examples of possible health outcomes include improved mental wellness and reduced risk for poor mental health, premature death, poor immune function and many chronic diseases and conditions. These complex interactions between the built environment and mediating factors that lead to human response and health outcomes are all influenced by other determinants of health, such as age, genetics, gender, social environment, income, education, culture and the health care system.
Social support, stress and health
Social support and low stress have been strongly linked to good health.
Social support: Social support can decrease the risk for premature death and poor health in the form of cardiovascular disease, stress, poor mental health and other health issues such as cancer and infectious disease, likely linked to factors such as impaired immune function or delayed access to health care.Footnote 401-403 Canadians with more family and friends were more likely to report being in very good or excellent physical and mental health at all ages.Footnote 404 It is thought that social support is linked to better health because it promotes healthy behaviours and helps people deal with difficult situations.Footnote 403
Social isolation and loneliness: Feeling socially isolated or lonely can increase the risk for premature death and poor health in the form of increased risk for depression, poor sleep, difficulties paying attention, impaired decision making, problem solving and memory, cognitive decline, poor cardiovascular function, poor immune function and stress.Footnote 406-409
Did you know? In 2013Footnote 404,Footnote 405
Friends and neighbours
- 6% of Canadians said they had no close friends. This is higher for Canadians 75 years and older at 15%.
- 75% of Canadians said they had three or more close friends, which is an increase from 70% in 2003. This is higher for Canadians ages 15 to 24 years at 88%.
- About 40% of Canadians said they knew many or most of their neighbours.
- 44% of Canadians see their friends at least a few times a week, which is lower than in 2003 at 56%.
Family
- 55% of Canadians said they felt close to at least five family members.
- 26% of Canadians see relatives at least a few times a week, which is lower than in 2003 at 38%.
- 86% of Canadians with close ties to at least five relatives were satisfied with their lives compared to 75% with one or two close relatives and 69% with no close relatives.
Why do we feel lonely? Loneliness is often temporary and is thought to be a motivator for people to seek out social support.Footnote 407 When loneliness becomes a long-term situation, there are risks to health.Footnote 407,Footnote 417 Loneliness can happen at any age, but it is triggered by different factors across the lifespan.Footnote 417 Loneliness appears to be highest in adolescence when teenagers are seeking to establish their own identity and in old age when people begin losing loved ones and have poorer health.Footnote 417
Community belonging: In Canada, people who have a strong sense of community belonging are more likely to report having excellent or very good physical and mental health.Footnote 410,Footnote 411 In 2014, almost 19.4 million or 66% of Canadians age 12 years and older felt a very strong or somewhat strong sense of community belonging.Footnote 412
Stress: Chronic stress has a wide range of impacts on health, increasing the risk for early death and poor physical and mental health. e.g.,Footnote 413-416 In 2014, almost 6.7 million or 23% of Canadians over the age of 15 years said they had experienced quite a lot of life stress in the previous year.Footnote 412
Building neighbourhoods that promote mental wellness
Neighbourhoods can be built to increase social interactions and reduce stress.
Social interactions: Neighbourhoods can affect social interactions by increasing the probability of meeting others and by providing places to gather.Footnote 418,Footnote 419 Neighbourhoods that are linked to higher levels of neighbourliness, social capital (defined as social networks and interactions that increase trust and support among neighbours) or a sense of communityFootnote 419-433
- Have houses close to the street and with front porches, front gardens or yards.
- Have green spaces.
- Are pedestrian friendly.
- Have walkable destinations and accessible public transit.
- Are clean.
- Have low traffic and parking.
- Have places where people gather (e.g., places of worship, local tavern, coffee shops, restaurants, parks, recreation areas and facilities, community centres, libraries).
- Are places where people walk for leisure and people see each other out and about.
- Create feelings of safety.
Areas with these features can have drawbacks that need to be considered when building communities for mental wellness. For example, neighbourhoods that are linked to higher levels of sense of community and social capital may not be affordable for everyone, may not be diverse or may not be what some people prefer.Footnote 435-440 Areas with many stores and restaurants may draw in people from other neighbourhoods, leading to a lower sense of community for residents.Footnote 419
Stress and poor mental health: Neighbourhood features and characteristics linked to an increase risk for stress and poor mental health includeFootnote 441-450
- Hazards (e.g., uneven sidewalks, potholes in roads, debris)
- Noise
- Trash and litter
- Poor quality housing
- Lack of places to gather
- Lack of services
- Low walkability
- Unattractiveness
- Lack of access to green spaces and community facilities
- Negative characteristics like abandoned buildings
- Unsafe neighbourhoods.
Getting from home to work or school is a regular routine for many Canadians. In Canada, the majority of people work in the municipality in which they live. For example, 55% of commuters who live in Mississauga work in Mississauga and 81% of commuters who live in Toronto work in Toronto. A similar pattern can be seen in and near Montreal and Vancouver.Footnote 451
Long commute times can be a source of stress, particularly when commuters feel they lack control over conditions, traffic and time.Footnote 452-461 This can also result when travelling by public transit. Improvements in public transit infrastructure (e.g., fewer stops to reach destination) can reduce commuters’ stress in some situations.Footnote 454,Footnote 462-465 Some drivers enjoy their commute and find it is a good buffer between work and home.Footnote 466,Footnote 467 Over the long-term, stressful or long commutes have been linked to poor health in some situations but not others.Footnote 485,Footnote 500-502
Did you know? Commuting varies greatly across Canada,Footnote 451 likely due to factors such as differences in the infrastructure available for commuting, commuting distances and climate.
In 2011, over 15 million Canadians commuted to work. About 80% of these commuters used a private vehicle, while about 12% used public transit and 7% walked or biked.Footnote 451 In 2011, about 27% of Canadians said they had used active transport in the previous three months.Footnote 188
In 2011, Canadians who commuted to work spent about 25 minutes to travel from home to work. About 17% of Canadians spend at least 45 minutes commuting to work.Footnote 451
Taking public transit took longer on average than driving to work – Canadians who drove to work took about 24 minutes to do so while those who took the bus took 40 minutes, those who took the subway took 45 minutes and those who took light rail, a streetcar or commuter train took almost 53 minutes. For public transit, this includes the time to walk to public transit stops and waiting time.Footnote 451
Canadians who commuted by walking or cycling spent less time commuting – people who walked spent about 13 minutes commuting while those who cycled spent about 20 minutes.Footnote 451 This could be because people who choose to commute via active transportation live closer to work.
Mediating factors affecting the link between the built environment and mental wellness
Currently, experts do not agree on how to build crime-free or low crime communities, but safety is considered a key element of healthy communities.Footnote 500
Crime: Being a victim of a crime or a fear of crime can lead to long-lasting effects on mental health and wellness.Footnote 501-505 A fear of crime can lead people to change their behaviour as a response to their fears. This can lead to unhealthy outcomes like physical inactivity and mistrust.Footnote 502,Footnote 506,Footnote 507
Did you know? In 2014, 20% of Canadians over the age of 15 years said they had been victim of at least one crime (e.g., assault, robbery, breaking and entering, theft of personal property, vandalism) in the previous year.Footnote 509
Understanding local crime patterns and neighbourhood features that may promote crime appears to be important for reducing crime.Footnote 508 Two examples of promising strategies that look at the built environment to prevent crime are
- Crime Prevention through Environmental Design (CPTED): Supported by the United Nations and countries across the world, CPTED aims to decrease crime by reducing opportunity. It supports clear identification of public and private areas (e.g., through signs and fences), removing litter and graffiti, reducing unused or underused spaces, improving surveillance (e.g., improve visibility, strategic placement of windows, good street lighting) and controlling access.Footnote 510
- Situational Crime Prevention (SCP): This approachaims to understand where, why and when crime happens in a neighbourhood and to reduce opportunities for crime by increasing its risks and decreasing its rewards. This involves tailored solutions that can include changing neighbourhood features to reduce crime.Footnote 508,Footnote 511
Evidence suggests that these approaches are effective in some situations, but may address only the symptoms of crime and not its causes. In some situations, they may potentially increase or displace crime.Footnote 508,Footnote 510,Footnote 512-518 There is some evidence that neighbourhood interventions may reduce fear of crime. Reducing physical disorder (e.g., litter, graffiti, vandalism) and improving the maintenance of properties and public areas appear to increase feelings of safety to some extent.Footnote 519
Improving mental wellness: Research on how to harness the built environment to improve mental wellness is limited and weak but growing. Examples of approaches that could be targeted include
Increasing green spaces: Looking at the impact of green spaces on health is a relatively new area of research. Green spaces have been linked to better mental and physical healthFootnote 44,Footnote 51,Footnote 52,Footnote 468-481 It is thought that their availability may lead to better health through increased physical activity, less exposure to air pollution, more social interactions and/or feeling less stressed.Footnote 471,Footnote 482,Footnote 483 How green spaces are linked to mental wellness may change across the lifespan and differ by gender.Footnote 470,Footnote 484
Reducing noise: Noise in our neighbourhoods can come from sources such as motor vehicles, airplanes, trains, industrial areas, construction and noisy neighbours. The World Health Organization estimates that among environmental factors that influence health, noise pollution is second to air pollution in terms of its impacts in Europe.Footnote 485 Living in a noisy neighbourhood has been linked to an increased risk for health issues such asFootnote 486-491
- Hearing loss.
- Stress as well as poorer quality of life, mental health and sleep.
- Hypertension, cardiovascular disease, diabetes and respiratory disease.
- Poorer memory and reading skills in children.
Creating public art: The attractiveness of a space can affect how people feel, think and behave. For example, art in public places has been shown to have a calming effect.Footnote 492-494 Art can reflect culture and also build social and community connections.Footnote 495 Some evidence suggests that art projects that involve a community can improve the health and well-being of its residents as well as build a better sense of community.Footnote 496-499
Section 4: Design features for specific populations
This section explores how design features of the built environment impact healthy living in children, youth and older adults as well as their role in health inequities.
Most research on the impact of the built environment on healthy living, and health in general has focused on adults. Research on children, youth, older adults and marginalized groups is limited despite known health risks and inequities for these groups. There is also limited research on how the built environment may affect gender differently. Some research suggests that there may be gender differences, but results are mixed and overall conclusions remain elusive.Footnote 520
Children and Youth
Physical activity: In 2014, Canadian data showed that 31% of boys and 22% of girls in Grade 6 were physically active every day for at least 60 minutes. This dropped to 22% of boys and 10% of girls by Grade 10. Students in Grades 6 to 10 are more likely to participate in team sports than individual sports.Footnote 521 It appears that a greater proportion of Canadian students in Grades 6 to 10 are spending more of their leisure time playing video games and on the computer than in the past.Footnote 521,Footnote 522
The presence of parks and green spaces may play an important role in increasing physical activity in children in urban areas, although some evidence shows that neighbourhoods with destinations, such as recreation facilities, parks, playgrounds and features linked to walking are associated with lower levels of physical activity in children.Footnote 523,Footnote 524 A key factor for physical activity may be the availability of undeveloped areas that allow for unstructured play.Footnote 525
The need for challenging play: Challenging play is important for children’s development as well as their physical and mental health. This type of play encourages children to evaluate their environment and its challenges before taking action. It has also been linked to helping children learn about assessing and managing risks, to be more independent and to develop better learning and judgment skills.Footnote 526 Footnote 527
Living in suburbs or small towns was linked to the highest levels of physical activity in children while living in urban areas was linked to the lowest. Children living in rural areas were more likely to spend time outdoors and in unstructured play than children living in urban areas.Footnote 528 This may be linked to how safe rural neighbourhoods, in terms of both traffic and crime, are perceived to be.
Parents’ concerns about safety are linked to their willingness to allow their children be active outside.Footnote 529-534 Like other age groups, children who walk or cycle are more likely to get injured than children who travel in a motor vehicle.Footnote 535 Measures to increase safety such as traffic calming and having recreation areas nearby were linked to more physical activity and fewer injuries among children. Features such as higher road density, having schools and other services nearby and crosswalks were linked to more walking, but not increased safety.Footnote 536-539 Crime is also an issue. Children living in neighbourhoods with less crime are more likely to be physically active.Footnote 540
Walking, cycling or using public transit to get to school can increase children’s and teenagers’ physical activity levels, yet many Canadian students are not using active transportation.Footnote 541-544 It appears that using active transportation in Canada is decreasing. Among students in Grades 6 to 10, rates appear to be decreasing, particularly in lower grades (see Table 1).Footnote 521,Footnote 522A survey of Canadian parents in 2012 showed that 58% walked to school as children while 28% of their own children walk to school today.Footnote 545
|
Grade 6 |
Grade 7 |
Grade 8 |
Grade 9 |
Grade 10 |
|---|---|---|---|---|---|
2014 |
|||||
Boys |
31% |
25% |
27% |
28% |
26% |
Girls |
29% |
25% |
26% |
24% |
19% |
2011 |
|||||
Boys |
41% |
36% |
39% |
27% |
31% |
Girls |
36% |
32% |
36% |
25% |
22% |
Distance and safety are two key factors - children are more likely to use active transportation if their school is nearby and the route to get there is safe.Footnote 546-556 They are also more likely to use active transportation in areas experiencing urban sprawl.Footnote 557 Parents are important role models for their children in terms of physical activity. For example, for every 20 minutes of activity a parent did on weekends or during evenings, their children’s activity increased by five to ten minutes.Footnote 558 Children whose parents use active transportation are also more likely to do so.Footnote 559,Footnote 560
Healthy diets: Research in this area is still evolving, but generally, access to healthy or unhealthy food has the same effect on children and teenagers as it does on adults.Footnote 561 One aspect that differs is the fact that children and teenagers can also be influenced by food access near schools or on route to school. Recent findings suggest that children and teenagers who live or go to school in neighbourhoods with many places that sell unhealthy food are more likely to have an unhealthy diet and be overweight, be obese, have higher insulin resistance and have poor bone density.Footnote 561-565
Mental wellness: Green spaces may have a positive influence on children’s brain, behavioural and physical development.Footnote 566-571 In Canada, children who spend more time outdoors are more likely to be physically active, have fewer problems with their friends and have better psychosocial health.Footnote 571
Physical activity, healthy eating and pregnant/postpartum women: There is a lack of research on the role of the built environment on the health of pregnant and postpartum women. However, they may benefit from a neighbourhood that encourages physical activity and healthy eating. Evidence suggests that healthy diets and physical activity are important for appropriate weight gain during pregnancy, although they may have no effect on issues such as preeclampsia, gestational diabetes and induction of labour.Footnote 572,Footnote 573 Weight gain during pregnancy is also linked to a child’s health, including the risk of high birth weight and being overweight in childhood.Footnote 574-576
Research is mixed, but some evidence suggests that exercise and healthy diets in the postpartum period are linked to weight loss and improvement in postpartum depression symptoms.Footnote 577-581 Many women have trouble losing weight during the postpartum period, suggesting a need for specific interventions for this group.Footnote 582,Footnote 583
Older adults
Communities are not always built to support aging. Most older adults want to stay in their homes and neighbourhoods as they get older. As they age, older adults are also more likely to spend more time in their neighbourhoods and to be more sensitive to changes in their environment.Footnote 584 Canada’s population is aging.Footnote 11 Ensuring that the built environment supports healthy aging is becoming increasingly important.
Older adults and falls: In Canada, about 20% to 30% of older adults fall every year. Falls are also the leading cause of hospitalization among older Canadians.Footnote 608,Footnote 609
Older adults who felt that they were part of their community and that people would help them were less likely to experience falls. Neighbourhoods that were thought to be cleaner and safer were linked to fewer falls.Footnote 610
Outdoor hazards increase the risk or the perceived risk for falls among older adults. Examples include uneven surfaces, curbs, lack of street, sidewalk and path maintenance, poor lighting, potholes, cluttered areas, unsafe traffic, unclear signs and crossings that are perceived to be unsafe.611,612
Physical activity: Even older adults who are already in poor health can benefit from being active.Footnote 585,Footnote 586 Many neighbourhood features (e.g., attractiveness, living near stores, services or friends) that are linked to more utilitarian walking in other age groups are also linked to more utilitarian walking in older adults, although research is mixed and likely influenced by other factors like mobility, income and attitudes.Footnote 587-607 Some research suggests that walkable neighbourhoods are linked to more walking even among older adults with mobility issues.Footnote 605
Some of the biggest barriers to being active for older adults include how accessible and safe their neighbourhood is (e.g., access to services, public transit, safety of sidewalks, weather, noise, lighting, street curbs, attractiveness, challenging street crossings due to short traffic lights or wide streets, proximity to destinations).Footnote 588,Footnote 611,Footnote 613,Footnote 614 Living in the suburbs is linked to many of these factors and can create a challenging situation for older adults, particularly for those who no longer drive. Concerns about safety include worries about crowds, crime, violence and traffic.Footnote 615
For older adults who have health and mobility issues, having benches in neighbourhoods is important. They function as rest stops during longer trips and can be good places for older adults to better enjoy green spaces and areas near water.Footnote 616
Social isolation: Neighbourhoods may not be set up to address the risk for social isolation associated with aging. Loneliness is an important public health issue for Canada’s aging population. Risk factors for being lonely at an older age include not being married, being in poor health, having a declining income and having a low education.Footnote 617 Limited research has addressed how the built environment can support social interactions and reduce social isolation for older adults.Footnote 618 Walkable neighbourhoods and physical activity itself are linked to increased activity and being more social in older adults.Footnote 614,Footnote 618
Populations experiencing health inequity
Building a healthy community addresses the needs and improves the health of all of its residents, including those who are marginalized.Footnote 1 Access to food, clean water and housing are basic needs. It makes sense that some approaches to improve healthy living, such as building more recreational areas or cycling infrastructure, may not have a positive impact on community health before these basic needs are met.
Accessibility for people living with a disability: The needs of people living with a disability are not always considered when designing and building communities.Footnote 619-622 In 2012, 3.8 million or 14% of Canadians 15 years and older reported living with a disability that limited their daily activities.Footnote 623
Evidence suggests that neighbourhoods with good accessibility, high quality and safe streets, lower traffic density as well as uncrowded and open spaces increase the likelihood that people with a disability can be mobile, productive and social.Footnote 613,Footnote 621,Footnote 622,Footnote 624-626 Winter can further reduce accessibility for people living with a physical disability, leading to increased risks to health and for being isolated.Footnote 620,Footnote 627-630
Certain features can worsen health inequity, particularly in disadvantaged neighbourhoods. Examples of these features includeFootnote 631,Footnote 632
- Lack of transportation options
- Limited access to healthy food, housing and health care
- Lack of parks and recreation facilities
- Empty buildings and vacant lots
- Poor air or water quality
- Lack of safety, higher crime
- Increased social isolation
- Residential segregation
Affordability is an important factor that influences where people decide to live. For those living with a low income, access to affordable housing is linked to better health and more income being available to support health and well-being.Footnote 633-639
Gentrification: Gentrification is the transformation of areas into middle class or affluent neighbourhoods. There is limited evidence and some debate about whether or not gentrification benefits or harms a neighbourhood’s original residents, particularly those with a low income.Footnote 640,Footnote 641
Limited research is available on the role of the built environment for Indigenous populations, people living in poverty, the homeless and people with a disability, and no evident research is available on people who identify as lesbian, gay, bisexual, transgendered, queer, questioning, intersex and two-spirited (LGBTQQI2S).
Indigenous communities: About 50% of Canada’s Indigenous population live in an urban area, a proportion that has grown over time. About 34% of the urban Indigenous population live in Winnipeg, Edmonton, Vancouver, Calgary and Toronto.Footnote 642 Whether Indigenous Peoples live in an urban, rural or remote area varies by Indigenous population:
- In 2006, about 70% of Metis lived in an urban area.Footnote 643
- In 2006, about 40% of First Nations lived on-reserve while 60% lived off reserve. Among those who lived off reserve, 47% lived in major urban centres, 31% lived in smaller urban areas and 21% lived in rural areas.Footnote 644
- In 2011, about 75% of Inuit lived in four northern regions that span the Territories and Labrador.Footnote 645
For First Nations and Inuit populations, particularly those living in remote and isolated communities, there are challenges and opportunities for harnessing the built environment to support healthy living. Challenges can include lack of infrastructure and jurisdictional barriers. From a built environment perspective, some of the more pressing health concerns for remote Indigenous communities are related to safe drinking water, food availability, security and safety, access to health care and housing quality, affordability, accessibility and crowding.Footnote 646-653
Like Canada as a whole, Indigenous populations are also dealing with a shift to sedentary lifestyles, physical inactivity, unhealthy diets and resulting impacts on health.Footnote 653,Footnote 654 This is linked to a shift from traditional built environments. Traditionally, Indigenous communities and camps were designed and located with purpose and to address community needs, well-being and geographic realities. In some cases, communities were temporary and moved in response to changes in season and food availability. With colonization and assimilation, communities were displaced and relocated, often away from traditional lands and practices.Footnote 83
For healthy living, there is limited research on the impact of the built environment on Indigenous communities.Footnote 83 Examples of barriers to physical activity that have been identified include isolation, an environment that does not make being physical active easy (e.g., weather, hazardous roads, safety, aggressive animals) and a lack of time, opportunities, support, programs, facilities and equipment.Footnote 83,Footnote 654-657
There are also opportunities to learn from Indigenous populations. Ties to the land, water, family, community and identity are important components of Indigenous culture that also emphasizes wholeness, connectedness and balance.Footnote 653,Footnote 658 For Indigenous communities, place is an important source of health and is seen as part of a holistic, interconnected view of health and well-being. 658 Many Indigenous communities have developed or are interested in developing land-based programs to support improved wellness outcomes.
Section 5: Designing Canadian communities for healthy living
This section provides a brief overview of some of the approaches that are used to design communities in Canada to improve healthy living. Communities that effectively support, promote and inspire healthy living take a collaborative, multidisciplinary effort that includes expertise not traditionally linked to health, such as economics and transportation. They involve all levels of government and engage at the community level.Footnote 659
Multi-sectoral collaboration: Currently, public health professionals are working closely with urban planners, traffic engineers, architects and policy makers at all levels across Canada to varying degrees. Building these relationships is seen as a particularly important step for moving initiatives forward.Footnote 659
Health in All Policies is an important approach that encourages decision makers across all sectors to consider the health implications of public policies.Footnote 67-69 This has been noted as an important approach for planning, development and equity. 1,2 For public health, designing healthy communities is truly a population health approach. It involves finding a balance to
- Improve the health of all Canadians and reduce health inequities.
- Prevent unhealthy behaviours and poor physical and mental health.
- Consider the influence of the social determinants of health.
Much of what drives this work happens at the local level; however, provincial, territorial and federal laws, regulations and policies can have an impact. Examples include investments in various sectors such as public transportation and the establishment of policies for municipal planning.
Tackling urban sprawl: While some cities are working to proactively address or prevent urban sprawl, the response to urban sprawl is often reactive happening once its effects are already being felt. Urban sprawl is often characterized as living in the suburbs. Although suburbs are linked to unhealthy behavioursFootnote 27-32, they often provide attractive options at affordable prices for some Canadians. Many Canadians want to live in the suburbs and enjoy doing so.Footnote 65,Footnote 66 This suggests that there is a need for innovative thinking to tackle the unhealthy aspects of suburban living.
Examples of proactive approaches can be found in Ontario and Metro Vancouver where growth plans have been developed to address urban sprawl. In southern Ontario, this included establishing density targets for development and protection of green spaces. The goals of the Metro Vancouver plan include
- Having its population concentrated in compact communities with access to a range of housing choices, employment, amenities and services.
- Protecting industrial and agricultural land.
- Protecting natural areas for clean air, water and food as well as diverse recreational activities.
- Developing complete communities with a range of housing choices, good distribution of employment, access to services and amenities and support for walking, cycling and public transit to foster healthy lifestyles.
- Having a compact, transit-oriented urban setting that supports a range of sustainable transportation choices.
Examples of Canadian guidelines and other resources: There are many guidelines on promising practices for building healthy communities. Below are some examples
- Canadian Institute of Planners - Healthy Communities Practice Guide
- Built Environment Readiness Assessment Tool
- Planning by Design: a healthy communities handbook
- Healthy Built Environment Linkages Toolkit
- Healthy Development Assessment - User Guide
- Active Design Guidelines
Local planning
All cities in Canada have plans, policies and laws in place to guide the design and building of their communities. Active transportation is now the most addressed issue by planners, followed by access to public spaces, social networks and meeting areas. Lack of government or political support is the most often cited barrier for making sure planning considers health implications.Footnote 660
The built environment is something that can be tangibly changed. It is important for understanding population-level physical barriers and incentives for making healthy choices. e.g.,Footnote 72 To help people maximize health benefits from their built environment, public health can support the evaluation of initiatives or approaches to determine what works and what does not, and in what settings. It can also maximize the effectiveness of the built environment through policies and programs focused on designing healthy living. Improving health should be a goal of all community planning.
The story of Portland: Portland, Oregon is often used as an example of a city that changed its built environment and improved its citizens’ health by containing urban sprawl. Since 1979, the city has put in place many approaches
- Limiting development outside of its urban boundaries.
- Keeping its population closer to the city’s centre in dense, mixed-use neighbourhoods.
- Developing a well-connected light rail system that services many areas of the city.
Mortality rates decreased from almost 9,000 per million people per year in 1989-1994 to almost 8,000 per million people per year in 1995-2000. This change has been linked to the city’s approach to containing urban sprawl.Footnote 72
Examples from Canada’s three largest cities
Many of Canada’s larger cities have initiatives in place to help design and build communities that promote healthy living. Vancouver, Toronto and Montreal are used below as examples of multi-sectoral planning at a large scale for large populations. It should be noted that multi-sectoral community planning is happening in many areas, including planning that covers the suburbs and smaller communities. What works in larger cities may not work for the suburbs, smaller cities and communities or rural or remote communities.
The shift to a focus on the impact of the built environment on healthy living has taken time. Making widespread changes is difficult and often starts as smaller changes at the community level. Evidence is important, but so is context. Evidence needs to match a community’s needs, situation and characteristics to be considered relevant. This makes local knowledge and community engagement important. Seeing the effects of change also takes time, particularly on the health of a population. Together, these challenges show that harnessing the built environment to improve health is no easy task.Footnote 661
Vancouver
Population in 2016: 2.5 million
For many years, the City of Vancouver has focused on developing a sustainable city and on improving the health and well-being of its residents through policies, planning and related initiatives. In 2006, the Vancouver Coastal Health Authority implemented a collaborative focus on the built environment. The Health Authority has worked closely with communities on their Official Community Plans to ensure that the built environment is considered in their development.Footnote 661
Information on planning, zoning, development, community building and public health can be found at:
- Urban planning, sustainable zoning and development
- Building community(e.g., neighbourhood planning, improving public spaces, Indigenous communities, accessibility, seniors, women, youth)
- Public health
Healthy City Strategy: Vancouver’s Healthy City Strategy presents a long-term, integrated plan for healthier people, healthier places and a healthier planet. Champions from a range of sectors are guiding the adoption of the Strategy’s Healthy City for All vision.
Below are examples of the Strategy’s themes related to the built environment and healthy living.
Theme |
Goals and targets |
Working towards goals and targets |
|---|---|---|
Goal: All residents are engaged in active living and have incomparable access to nature Targets:
|
Vancouver Board of Parks and Recreation Strategic Framework |
|
Goal: Safe, active and accessible ways of getting around Targets:
|
||
Goal: Residents have the right to a healthy environment and equitable access to a livable environment in which they can thrive Targets:
|
Building community |
|
Goal: A healthy, just and sustainable food system Target:
|
||
Other city websites and resources:
- Parks, recreation and culture
- Home, property and development
- Streets and transportation
- Green Vancouver
- Resilient city
Citizen engagement and involvement: In Vancouver, citizens can be involved in many aspects of city government and municipal affairs. The City promotes engagement through Talk Vancouver, an on-line forum and public consultations. They also hold open City Council meetings and provide opportunities for members of the public to speak at City Council meetings, for citizens to serve on boards and committees and for citizens to volunteer. They also use various means, including social media, to reach out to citizens.
More information on how to become involved can be found here: Citizen involvement.
Toronto
Population in 2016: 5.9 million
Toronto was one of the first cities to adopt the concept of Healthy Cities. This concept defines a healthy city as one that is continually working to enhance its environments and communities to improve its citizens’ health and well-being.Footnote 662,Footnote 663 Toronto Public Health has been heavily involved in the development of various plans and strategies and in working with other municipal sectors on the built environment.Footnote 661
Information on city planning and public health in Toronto can be found at:
Below are examples of innovative approaches, best practices, activities and projects taking place in Toronto to improve healthy living by focusing on the built environment.
Activities |
Goals |
Working towards goals and targets |
|---|---|---|
Complete Streets involve the following components: Streets for People
Streets as Placemaking
Streets for Prosperity
|
Develop and implement guidelines Examples of complete streets in Toronto:
|
|
|
Examples of projects :
|
|
Examples: |
||
Examples: |
||
Other city websites and resources:
- Toronto Public Health - Built Environment
- Healthy Toronto by Design
- Improving Health by Design in the Greater Toronto-Hamilton Area
Citizen engagement and involvement: Get Involved Toronto aims to create opportunities for Toronto’s residents to shape a vision for the City’s future, plan changes in its neighbourhoods, provide information and insight on issues being tackled by City Council and serve on boards, advisory groups or volunteer in other ways.
The City of Toronto holds Council and committee meetings that are open to the public, undertakes various public consultations and provides many engagement opportunities to its citizens. A recent pilot project asked citizens to propose and vote on projects to improve their neighbourhoods through the Participatory Budgeting Pilot Project.
Toronto also engages citizens through social media. The City’s chief planner has a blog to discuss and engage citizens on various planning projects and issues.
Montreal
Population in 2016: 4.1 million
Montreal has many initiatives and projects in place that address the built environment. For many years, the City has involved neighbourhoods and non-governmental organizations in addressing issues related to the built environment.Footnote 664 The Direction de santé publique de Montréal has also been involved in policy development and in supporting various projects on the built environment for the past 30 years. Since the early 2000s, it has focused on transportation and health.Footnote 661
Information on planning, health and public safety can be found at:
- Planning (in French only)
- Health and public safety
Urban plan (in French only): The city of Montreal’s urban plan was adopted in 2004 and significantly modified in early 2016.
Theme |
Goals |
Supporting actions, principles and programs |
|---|---|---|
Structuring efficient transportation networks to fully integrate into the urban fabric(in French only) |
Goal: Consolidate and develop Montreal’s territory in relation to existing and planned transportation networks |
Actions:
Other: |
An enhanced architectural, archaeological and natural heritage(in French only) |
Goal: Preserve and enhance the built and archaeological heritage |
Actions:
Other: |
A healthy environment(in French only) |
Goal:
|
Actions:
Other: |
Other city websites and resources:
- Community life and education
- Transportation and public works
- Environment and sustainable development
- Housing and taxation
- Activities and recreation
Citizen engagement and involvement: In Montreal, citizens can be involved in many aspects of city government and municipal affairs. The City undertakes consultations on various issues and holds open City Council meetings. They also use various means, including social media, to reach out to citizens.
More information on how to become involved can be found here: Democratic participation.
Community planning and Indigenous populations: Planning has always been a part of Indigenous communities and included many traditional and historical practices. Over time, these practices have been ignored, particularly in urban centres. However, there are examples that this is changing.
- Today, there are a growing number of examples in Indigenous communities of community-based planning with strong participation, recognition of community needs, collaborative processes and inclusion of traditional knowledge.Footnote 83,Footnote 665-667
- Indigenous communities have unique factors that need to be considered when undertaking community planning. Examples include Indigenous culture, traditional knowledge, colonization, residential schools, self-determination, language and geography.Footnote 668
- The federal government supports communities in collaboration with community members for planning that takes place on-reserve.Footnote 83
- Some planners, municipalities and communities in Canada have strengthened relationships with urban Indigenous populations. Examples of promising practices include involving First Nations, tribal or band councils in decision making and strategic planning as well as recognizing Indigenous history and heritage in planning projects.Footnote 665-667
- Tools are available that aim to help build collaborative land use planning between First Nations and municipalities in urban settings. Relationship building is important. Treaties, First Nations laws and legal traditions as well as legislation and policies at all levels of government play a role in planning in First Nations reserves.Footnote 668-670
Perspectives from provinces and territories
Based on a survey of planners from Canadian provinces in 2013, strong provincial leadership through policies, legislation and regulations that recognizes the role of the built environment in health can greatly benefit municipalities and communities in planning, designing and building healthy communities. Currently, approaches, policies, regulations and legislation that consider health in the design and building of communities vary considerably across Canada.Footnote 671
Although different sectors do work together to develop healthy communities, the need for better collaboration has been noted at both the provincial and municipal level. Leaders from the health sector, academics and non-governmental organizations are seen as important supporters of healthy communities.Footnote 671
British Columbia, Ontario, Quebec and New Brunswick are provinces where strong healthy community networks exist. The principles that guide these networks include community engagement, political commitment, multi-sectoral collaborations, asset-based community development and healthy public policy. Important factors for this approach include recognizing the social determinants of health, diversity, social justice and equity, empowerment and community ownership, research and evaluation, and creativity and innovation.Footnote 672,Footnote 673 More details on these networks, including their governance and organizational profiles, can be found here and here.
In its Land Use and Sustainability Framework, the Government of the Northwest Territories has noted that “land is life” and has recognized the need to consider spiritual, cultural, physical, economic and social factors when managing lands, waters and natural resource. It also supports many initiatives that help develop healthy communities, including Community Wellness Initiatives and On the Land Healing programs.
Federal programs
The Public Health Agency of Canada (PHAC) supports work on the link between the built environment and healthy living through surveillance, research, knowledge mobilization, collaborations and funded interventions:
- Surveillance and research activities include the development of the Physical Activity, Sedentary Behaviour and Sleep Indicators Framework.
- PHAC also supports six National Collaborating Centres for Public Health. The Centres for Healthy Public Policy, Environmental Health and Aboriginal Health all have publications on the built environment.
- As part of its Innovation Strategy, PHAC is funding initiatives that foster active communities. Examples include Active Neighbourhoods Canada and other initiatives to support school environments and food-secure communities.
- Through its Multi-sectoral Partnerships to Promote Healthy Living and Prevent Chronic Disease, PHAC is supporting interventions that target the built environment. Examples include Creating Connections in St. Thomas, Ontario and Healthy by Design: Active Apartment Neighbourhoods in Toronto.
The Canadian Institutes of Health Research (CIHR) is supporting research on health and the built environment including $17.7 million for nine Intersectoral Prevention Research Grants that focus on healthier cities and communities.
Healthy Canada by Design
This initiative began in 2009 and was funded by the Canadian Partnership Against Cancer and Health Canada. Its aim was to move evidence into action and build collaborations that harness the built environment to improve health. Members of this initiative include the Urban Public Health Network, the Heart and Stroke Foundation, the Canadian Institute of Planners, the National Collaborating Centre for Healthy Public Policy, the Canadian Institute of Transportation Engineers and several universities.Footnote 62,Footnote 674,Footnote 675
About 163 government policies related to the built environment and increasing physical activity were influenced by the Healthy Canada by Design and the related Children’s Mobility, Health and Happiness projects.Footnote 659
International initiatives
Many countries are looking to the built environment to improve health. Covering all the examples that exist is outside the scope of this report. Outlined below are two examples of World Health Organization initiatives.
Healthy Cities: The concept of building a healthy city has a long history. As an international movement, it grew in part from an initial health city workshop held in Toronto in 1984 and aligns with the Ottawa Charter for Health Promotion. In 1986, the World Health Organization Healthy Cities project began with the involvement of representatives from 21 cities and seven countries in Europe.Footnote 60,Footnote 61 This project focuses on clean and safe environments, community connections, interaction and engagement, stable and sustainable ecosystems, meeting basic needs of all citizens, diverse, vital and innovative local economies and good health.Footnote 60,Footnote 61,Footnote 662 Today, there are approximately 30 national Healthy Cities networks with more than 1400 cities involved.Footnote 61,Footnote 676
In Canada, the healthy communities movement has developed on a different path with a broader approach that looks beyond urban areas and involves several separate networks rather than a pan-Canadian approach. Initiatives tend to be more local and built on existing community capacity. Across Canada, this has led to a wide variety of strategies that reflect individual community needs and have led to a broad range of results.Footnote 677
Age-Friendly Communities: In 2006, the World Health Organization started its Global Age-Friendly Cities project and in 2007, published a guide for developing age-friendly cities. Since that time, its Global Network for Age-friendly Cities and Communities has grown to include 287 communities in 33 countries with Canada being a key partner. This project focuses on eight areas for making communities age-friendly: outdoor spaces and buildings; transportation; housing; social participation; respect and social inclusion; civic participation and employment; communication and information; and community support and health services.Footnote 678,Footnote 679
In Canada, communities in all provinces are implementing age-friendly initiatives. PHAC recently developed a set of indicators to help communities evaluate the implementation of these initiatives, as did the World Health Organization.Footnote 679-681
Most work on age-friendly communities focuses on aging in urban areas, but there is a need to consider what age-friendly communities look like in rural settings.Footnote 682-685 In 2007, a report called Age-Friendly Rural and Remote Communities: A Guide was developed in Canada and endorsed by federal, provincial and territorial Ministers responsible for seniors. Its purpose was to raise awareness of the needs of older adults and to present a practical guide for rural and remote communities in Canada.
Moving research and evaluation into planning
Taking research that links a design feature to a health outcome, such as walkable communities and diabetes, and translating it into community action is challenging. Policies and programs need to be developed and implemented using the most relevant and up-to-date evidence, but they also need to be evaluated to determine their effectiveness.
Many projects and initiatives related to the built environment have taken place or are underway in Canada, but many are not evaluated or if they are, evaluation findings may not be accessible. In addition, cities and communities already collect data on various built environment initiatives, but data are not collected in a standardized way, limiting their use for researchers and planners in other communities. Systematically sharing data, knowledge and lessons learned about the effectiveness of initiatives is important to improve the health of Canadians in all communities.
Doing research that is policy and program relevant and engages stakeholders is a good step towards ensuring that community and neighbourhood planning is evidence-based.Footnote 686-688 This type of research can help create traction with decision-makers and help generate public awareness and community support.Footnote 689
Section 6: Call to action
We can do more to help Canadians take charge of their own health. We have an exciting opportunity to consciously design our communities to support healthy living and help Canadians unconsciously improve their own health and the health of generations to come.
Changing behaviour is complicated. Why people do what they do is based on a wide variety of connected factors. These include age, physical and mental health, socioeconomic status, culture, and genetics as well as how we react to our physical and social environments. The built environment is only one piece of this much larger puzzle.
Designing the built environment for healthy living is about supporting social connection and seamlessly providing access to features that promote physical activity, healthy eating and mental wellness. It can include simple things like connected streets, access to healthy food and places to gather with family and friends.
We know that communities are not all designed the same way and that they evolve over time. In addition, most of us spend our lives in many different neighbourhoods at any given time and across our lifespan. This makes it challenging to quantify how the built environment impacts health.
However, we know that where you live can matter. For example:
- For someone with a life-threatening chronic disease, being closer to urgent care and specialized health services can be a key consideration for good health.
- For young families, neighbourhood features that support challenging play, active transportation and parents’ opportunities to be healthy role models can provide the whole family with a foundation for healthy living.
- Living in smaller communities can foster a strong sense of community belonging.
While many cities in Canada are already considering health in their community planning, there is much that remains to be explored. Research in this area is relatively young and moving findings into action is still a challenge. This means that we can be proactive and now is the time for public health to work closely with other sectors to take advantage of this growing domain.
Public health can influence the way forward and ensure that community planning and infrastructure initiatives, as well as sustainable, economic and technological development are based on integrated evidence and consider good health as a key outcome. Unravelling the complexity of the impact of the built environment on population health lies in precision public health, which uses data to guide interventions to benefit populations more effectively.
Six actions
Going forward, I call on domestic and international partners, all levels of government including municipal, provincial, and federal leaders, political decision makers, community planners and entrepreneurs to take action in the following six ways:
- Consider the health of populations when designing and re-designing communities and developing and implementing major infrastructure projects, especially in cities given that most of us live in urban or suburban areas. As much as possible, proactively examine projects for their health promotion potential.
- Avoid worsening health inequity when designing and re-designing communities by considering the needs and circumstances of populations experiencing these inequities.
- Evaluate the health impacts of community design features by enlisting public health expertise. Make the findings from these evaluations openly accessible.
- Strengthen existing approaches, share lessons learned and best practices. For all communities, learn from each other in terms of both successful and less successful approaches. Build on existing Canadian networks to foster a pan-Canadian dialogue.
- Collaborate to collect standardized data and engage citizens. Support a better understanding of community needs and the health impact of community design on populations.
- Innovate so that the healthy choices are the easy choices. Bring together ideas and concepts from across disciplines and sectors. Combine strategies that promote healthy living with those that improve the built environment to optimise impact and investment.
All of these actions could improve the lives of millions of Canadians. As Canada’s Chief Public Health Officer, this is an easy goal for me to stand behind.
References
- Footnote 1
-
Corburn, J. (2017). Urban place and health equity: critical issues and practices. International Journal of Environmental Research & Public Health, 14(2), 117.
- Footnote 2
-
Greaves, L.J., Bialystok, L.R. (2011). Health in All Policies – All talk and little action? Canadian Journal of Public Health, 102(6), 407-409.
- Footnote 3
-
Chaix, B., Billaudeau, N., Thomas, F., Havard, S., Evans, D., Kestens, Y., Bean, K. (2011). Neighborhood effects on health: correcting bias from neighborhood effects on participation. Epidemiology, 22(1), 18-26.
- Footnote 4
-
Clarke, P., Neiuwenhuijsen, E.R. (2009). Environment for healthy ageing: a critical review. Maturitas, 64(1), 14-19.
- Footnote 5
-
Diez Roux, A.V., Mair, C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125-145.
- Footnote 6
-
Frohlich, K.L., Dunn, J.R. McLaren, L., Shiell, A., Potvin, L., Hawe, P., Dassa, C., Thurston, W.E. (2007). Understanding place and health: a heuristic for using administrative data. Health and Place, 13(2), 299-309.
- Footnote 7
-
Geneletti, S., Mason, A., Best, N. (2011). Adjusting for selection effects in epidemiologic studies: why sensitivity analysis is the only "solution". Epidemiology, 22(1), 36-39.
- Footnote 8
-
Healy, M.A., Gilliland, J.A. (2012). Quantifying the magnitude of environmental exposure misclassification when using imprecise address proxies in public health research. Spatial Spatiotemporal Epidemiology, 3(1), 55-67.
- Footnote 9
-
Riggs, W. (2014). Steps toward validity in active living research: research design that limits accusations of physical determinism. Health and Place, 26, 7-13.
- Footnote 10
-
Terashim, M., Kephart, G. (2016). Misclassification errors from postal code-based geocoding to assign census geography in Nova Scotia, Canada. Canadian Journal of Public Health, 107(4-5), 424-430.
What this Report is about
- Footnote 11
-
11. The Chief Public Health Officer's Report (2016). Health Status of Canadians 2016: Report of the Chief Public Health Officer.
- Footnote 12
-
Navaneelan, T., Janz, T. (2014). Adjusting the scales: Obesity in the Canadian population after correcting for respondent bias. Health at a Glance, 82-624-X. Statistics Canada.
- Footnote 13
-
Statistics Canada (2013). Table 102-0561: Leading causes of death, by sex. Statistics Canada.
- Footnote 14
-
Faienza, M.F., Wang, D.Q., Furhbeck, G., Garruti, G., Portincasa, P. (2016). The dangerous link between childhood and adulthood predictors of obesity and metabolic syndrome. Internal & Emergency Medicine, 11(2), 175-182.
- Footnote 15
-
Hidaka, B.H. (2012). Depression as a disease of modernity : explanations for increasing prevalence. Journal of Affective Disorders, 140(3), 205-214.
- Footnote 16
-
Hu, F.B. (2003). Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids, 39(2), 103-108.
- Footnote 17
-
Chaput, J.P., Carson, V., Gray, C.E., Tremblay, M.S. (2014). Importance of all movement behaviors in a 24 hour period for overall health. International Journal of Environmental Research & Public Health, 11(12), 12575-12581.
- Footnote 18
-
Whisman, M.A. (2010). Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychology, 29(5), 550-554.
- Footnote 19
-
Tomasetti, C., Li, L., Vogelstein, B. (2017). Stem cell divisions, somatic mutations, cancer etiology, and cancer prevention. Science, 355(6331), 1330-1334.
- Footnote 20
-
Public Health Agency of Canada (2014). Supportive environments for physical activity: how the built environment affects our health. Public Health Agency of Canada.
- Footnote 21
-
Washburn, R. A., Szabo, A. N., Lambourne, K., Willis, E. A., Ptomey, L. T., Honas, J. J., Herrmann, S.D., Donnelly, J. E. (2014). Does the method of weight loss effect long-term changes in weight, body composition or chronic disease risk factors in overweight or obese adults? A systematic review. PLoS One, 9(10).
- Footnote 22
-
Statistics Canada (2015). Canada's rural population since 1851. Census in Brief. Statistics Canada.
- Footnote 23
-
Statistics Canada (2017). Population size and growth in Canada: key results from the 2016 Census. Statistics Canada.
- Footnote 24
-
Statistics Canada (2017). Population and dwelling count highlight tables, 2016 Census. Statistics Canada.
- Footnote 25
-
Statistics Canada (2017). Municipalities in Canada with the largest and fastest-growing populations between 2011 and 2016. Statistics Canada.
- Footnote 26
-
Statistics Canada (2017). Municipalities in Canada with population decreases between 2011 and 2016. Statistics Canada.
- Footnote 27
-
Frumkin, H.(2002). Urban sprawl and public health. Public Health Reports, 117, 201-217.
- Footnote 28
-
Pohanka, M., Fitzgerald, S. (2004). Urban sprawl and you: how sprawl adversely affects worker health. American Association of Occupational Health Nurses Journal, 52(6), 242-246.
- Footnote 29
-
Thompson, S. (2014). Healthy built environments supporting everyday occupations: current thinking in urban planning. Journal of Occupational Science, 21(1), 25-41.
- Footnote 30
-
Turcotte, M. (2008). Dependence on cars in urban neighbourhoods. Canadian Social Trends, 11-008-XWE. Statistics Canada.
- Footnote 31
-
Vlahov, D., Galea, S. (2002). Urbanization, urbanicity and health. Journal of Urban Health, 79(Suppl 1), S1-S12.
- Footnote 32
-
Mackenbach, J.D., Rutter, H., Compernolle, S., Glonti, K., Oppert, J.M., Charreire, H., De Bourdeaudhuij, I., Brug, J., Nijpels, G., Lakerveld, J. (2014). Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health, 14, 233.
- Footnote 33
-
Owen, N., Sparling, P.B., Healy, G.N., Dunstan, D.W., Matthews, C.E. (2010). Sedentary behavior: emerging evidence for a new health risk. Mayo Clinic Proceedings, 85(12), 1138-1141.
- Footnote 34
-
Bento, A.M., Cropper, M.L. Mobarak, A.M., Vinha, K. (2005). The effects of urban spatial structure on travel demand in the United States. Review of Economics and Statistics, 87(3), 466-478.
- Footnote 35
-
Ewing, R., Cervero, R. (2010). Travel and the built environment: a meta-analysis. Journal of American Planning Association, 3, 265-294.
- Footnote 36
-
Trowbridge, M.J., McDonald, N.C. (2008). Urban sprawl and miles driven daily by teenagers in the United States. American Journal of Preventive Medicine, 34(3), 202-206.
- Footnote 37
-
Statistics Canada. Table 405-0004: Vehicle registrations (annual (number)). Statistics Canada.
- Footnote 38
-
Statistics Canada. Table 051-0001. Estimates of population, by age group and sex for July 1, Canada, provinces and territories. (annual (persons unless otherwise noted)). Statistics Canada.
- Footnote 39
-
Statistics Canada (2008). The city/suburb contrast: how can we measure it? Statistics Canada.
- Footnote 40
-
Laine, J., Kuvaja-Kollner, V., Pietila, E., Koivuneva, M., Valtonen, H., Kankaanpaa, E. (2014). Cost-effectiveness of population-level physical activity interventions: a systematic review. American Journal of Health Promotion, 29(2), 71-80.
- Footnote 41
-
McKinnon, R.A., Siddiqi, S.M., Chaloupka, F.J., Mancino, L. Prasad, K. (2016). Obesity-related policy/environmental interventions: a systematic review of economic analyses. American Journal of Preventative Medicine, 50(4), 543-549.
- Footnote 42
-
Adams, E.J., Goodman, A., Sahlqvist, S., Bull, F.C., Ogilvie, D., iConnect consortium. (2013). Correlates of walking and cycling for transport and recreation : factor structure, reliability and behavioural associations of the perceptions of the environment in the neighbourhood scale (PENS). International Journal of Behavioral Nutrition & Physical Activity, 10, 87.
- Footnote 43
-
Bancroft, C., Joshi, S., Rundle, A., Hutson, M., Chong, C., Weiss, C.C., Genkinger, J., Neckerman, K., Lovasi, G. (2015). Association of proximity and density of parks and objectively measured physical activity in the United States: A systematic review. Social Science & Medicine, 138, 22-30.
- Footnote 44
-
Bowler, D.E., Buyung-Ali, L.M., Knight, T.M., Pullin, A.S. (2010). A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health, 10, 456.
- Footnote 45
-
Bunn, F., Collier, T., Frost, C., Ker, K., Steinbach, R., Roberts, I., Wentz, R. (2003). Area-wide traffic calming for preventing traffic related injuries (Review). Cochrane Database of Systematic Reviews.
- Footnote 46
-
Cerin, E., Leslie, E., du Toit, L., Owen, N., Frank, L.D. (2007). Destinations that matter : Associations with walking for transport. Health and Place, 13(3), 713-724.
- Footnote 47
-
Child, S.T., Schollfman, D.E., Kaczynski, A. T., Forthofer, M., Wilcox, S., Baruth, M. (2016). Neighbourhood attributes associated with the social environment. American Journal of Health Promotion, 30(8), 634-637.
- Footnote 48
-
Eriksson, U., Arvidsson, D., Gebel, K., Ohlsson, H., Sundquist, K. (2012). Walkability parameters, active transportation and objective physical activity: moderating and mediating effects of motor vehicle ownership in a cross-sectional study. International Journal of Behavioral Nutrition & Physical Activity, 9, 123.
- Footnote 49
-
Fraser, S.D., Locke, K. (2011). Cycling for transport and public health: a systematic review of the effect of the environment on cycling. European Journal of Public Health, 21(6), 738-743.
- Footnote 50
-
Hassen, N., Kaufman, P. (2016 ). Examining the role of urban street design in enhancing community engagement: a literature review. Health and Place, 41, 119-132.
- Footnote 51
-
Lachowycz, K., Jones, A.P. (2011). Greenspace and obesity: a systematic review of the evidence. Obesity Reviews, 12(5), 183-189.
- Footnote 52
-
Lee, A.C., Maheswaran, R. (2011). The health benefits of urban green spaces: a review of the evidence. Journal of Public Health (Oxf), 33(2), 212-222.
- Footnote 53
-
Matson-Koffman, D.M., Brownstein, J.N., Neiner, J.A., Greaney, M.L. (2005). A site-specific literature review of policy and environmental interventions that promote physical activity and nutrition for cardiovascular health: what works? American Journal of Health Promotion, 19(3), 167-193.
- Footnote 54
-
McCormack, G.R., Shiell, A. (2011). In search of causality: a systematic review of the relationship between the built environment and physical activity among adults. International Journal of Behavioral Nutrition & Physical Activity, 8, 125.
- Footnote 55
-
Mulvaney, C.A., Smith, S., Watson, M.C., Parkin, J., Coupland, C., Miller, P., Kendrick, D., McClintock, H. (2015). Cycling infrastructure for reducing cycling injuries in cyclists. Cochrane Database of Systematic Reviews.
- Footnote 56
-
National Collaborating Centre for Healthy Public Policy (2012). Urban traffic calming and health. National Collaborating Centre for Healthy Public Policy.
- Footnote 57
-
Owen, N., Cerin, E., Leslie, E., duToit, L., Coffee, N., Frank, L.D., Baumann, A.E., Hugo, G. (2007). Neighborhood walkability and the walking behavior of Australian adults. American Journal of Preventive Medicine, 33(5), 387-395.
- Footnote 58
-
Rahmanian, E., Gasevic, D., Vukmirovich, I., Lear, S.A. (2014). The association between the built environment and dietary intake: a systematic review. Asia Pacific Journal of Clinical Nutrition, 23(2), 183-196.
- Footnote 59
-
Winters, M., Brauer, M., Setton, E.M., Teschke, K. (2010). Built environment influences on healthy transportation choices: bicycling versus driving. Journal of Urban Health, 87(6), 969-993.
- Footnote 60
-
Ashton, J. (1991). The Healthy Cities project: a challenge for health education. Health Education Quarterly, 18(1) 39-48.
- Footnote 61
-
Hancock, T. (1997). Healthy cities and communities: past, present, and future. National Civic Review, 86(1), 11-21.
- Footnote 62
-
Mowat, D. (2014). Healthy Canada by Design: translating science in action and prevention. Canadian Journal of Public Health, 106(1 Suppl 1), S3-4.
- Footnote 63
-
Harris, R. (2004). Creeping conformity: how Canada became suburban, 1900-1960. Toronto: University of Toronto Press Incorporated.
- Footnote 64
-
Canadian Institute of Planners (2011). Healthy Communities Practice Guide. Canadian Institute of Planners.
- Footnote 65
-
Harris, R. (2004). Creeping conformity: how Canada became suburban, 1900-1960. Toronto: University of Toronto Press Incorporated.
- Footnote 66
-
Harris, R., Larkham, P. (2004). Changing suburbs: foundation, form and function. New York: Taylor and Francis.
- Footnote 67
-
Organisation mondiale de la Santé (2013). Health in All Policies: Framework for Country Action. Organisation mondiale de la Santé.
- Footnote 68
-
St-Pierre, L., Gauvin, F.P. (2011). Intersectoral governance for Health in All Policies: an integrated framework. Government of South Australia, Health SA.
- Footnote 69
-
Frelier, A., Muntaner, C., Shankardass, K., Mah, C.L., Molnar, A., Renahy, E., O'Campo, P. (2013). Glossary for the implementation of Health in All Policies (HiAP). Journal of Epidemiology and Community Health, 67(12), 1068-1072.
- Footnote 70
-
Frank, L.D., Kavage, S. (2008). Urban planning and public health: a story of separation and reconnection. Journal of Public Health Management and Practice, 14(3), 214-220.
- Footnote 71
-
Sarkar, C., Webster, C. (2017). Health cities of tomorrow: the case for large scale built environment-health studies. Journal of Urban Health, 94(1), 4-19.
- Footnote 72
-
Fan, Y., Song, Y. (2009). Is sprawl associated with a widening urban-suburban mortality gap? Journal of Urban Health, 86(5), 708-728.
Canadian communities
- Footnote 73
-
Statistics Canada. Table 105-2023: Measured adult body mass index (BMI) (World Health Organization classification), by age group and sex, Canada and provinces, Canadian Community Health Survey – Nutrition (occasional). Statistics Canada.
- Footnote 74
-
Statistics Canada. Table 105-2024: Measured children and youth body mass index (BMI) (World Health Organization classification), by age group and sex, Canada and provinces, Canadian Community Health Survey – Nutrition (occasional). Statistics Canada.
- Footnote 75
-
Statistics Canada (2017). Age and sex, and type of dwelling data: key results from the 2016 Census. Statistics Canada.
- Footnote 76
-
Statistics Canada (2017). A portrait of the population aged 85 and older in 2016 in Canada. Census in Brief. Statistics Canada.
- Footnote 77
-
The World Bank (2015). Population density. The World Bank.
- Footnote 78
-
Statistics Canada (2017). Population size and growth rate, Canada, provinces and territories, 2006 to 2011 and 2011 to 2016. Statistics Canada.
- Footnote 79
-
Statistics Canada (2017). Dwellings in Canada. Census in Brief. Statistics Canada.
- Footnote 80
-
Alberta Health Services (2011). Towards an understanding of healthy equity: glossary. Alberta Health Services.
- Footnote 81
-
Public Health Agency of Canada (2005). The Rural Think Tank 2005 – understanding issues families face living in rural and remote communities. Public Health Agency of Canada.
- Footnote 82
-
Statistics Canada (2015). Rural area (RA). Statistics Canada.
- Footnote 83
-
Stout, R. (in press). The built environment: understanding how physical environments influence the health and well-being of First Nations peoples living on-reserve. National Collaborating Centre for Aboriginal Health.
- Footnote 84
-
Frost, S.S., Goins, R.T., Hunter, R.H., Hooker, S.P., Bryant, L.L., Kruger, J., Pluto, D. (2010). Effects of the built environment on physical activity of adults living in rural settings. American Journal of Health Promotion, 24(4), 267-283.
- Footnote 85
-
Hansen, A.Y., Umstattd Meyer, M.R., Lenardson, J.D., Hartley, D. (2015). Built environments and active living in rural and remote areas: a review of the literature. Current Obesity Reports, 4(4), 484-493.
- Footnote 86
-
Canadian Institute for Health Information (2006). How healthy are rural Canadians? An assessment of their health status and health determinants. Canadian Institute for Health Information.
- Footnote 87
-
Lavergne, M.R., Kephart, G. (2012). Examining variations in health within rural Canada. Rural Remote Health, 12, 1848.
- Footnote 88
-
Sibley, L.M., Weiner, J.P. (2011). An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Services Research, 11, 20.
- Footnote 89
-
Singh, G.K., Siahpush, M. (2013). Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. Journal of Urban Health, 91(2), 272-292.
- Footnote 90
-
Song, X., MacKnight, C., Latta, R., Mithitkski, A.B., Rockwood, K. (2007). Frailty and survival of rural and urban seniors: results from the Canadian Study of Health and Aging. Aging Clinical and Experimental Research, 19(2), 145-153.
- Footnote 91
-
Morrison, C., Ponicki, W. R., Gruenewald, P. J., Wiebe, D. J., Smith, K. (2016). Spatial relationships between alcohol-related road crashes and retail alcohol availability. Drug & Alcohol Dependence, 162, 241-244.
- Footnote 92
-
Vafaei, A., Rosenberg, M.W., Pickett, W. (2010). Relationships between income inequality and health: a study on rural and urban regions of Canada. Rural Remote Health, 10(2), 1430.
- Footnote 93
-
Alirol, E., Getaz, L., Stoll, B., Chappuis, F., Loutan, L. (2011). Urbanisation and infectious diseases in a globalised world. The Lancet infectious diseases, 11(2), 131-141.
- Footnote 94
-
Berry, H.L. (2007). 'Crowded suburbs' and 'killer cities': a brief review of the relationship between urban environments and mental health. New South Whales Public Health Bulletin, 18(11-12), 222-2227.
- Footnote 95
-
Harner, T., Shoeib, M., Diamond, M., Stern, G., Rosenberg, B. (2004). Using passive air samplers to assess urban-rural trends for persistent organic pollutants. 1. Polychlorinated biphenyls and organochlorine pesticides. Environmental Science and Technology, 38(17), 4474-4483.
- Footnote 96
-
Kundu, S, Stone, E.A. (2014). Composition and sources of fine particulate matter across urban and rural sites in the Midwestern United States. Environmental Sciences: Processes & Impacts, 16, 1360-1370.
- Footnote 97
-
Neiderud, C.J. (2015). How urbanization affects the epidemiology of emerging infectious diseases. Infection Ecology & Epidemiology.
- Footnote 98
-
Pickett, K.E., Wilkonson, R.G. (2015). Income inequality and health: a causal review. Social Science & Medicine, 128, 316-326.
- Footnote 99
-
Wilkinson, R.G., Pickett, K.E. (2006). Income inequality and population health: a review and explanation of the evidence. Social Science & Medicine, 62(7), 1768-1784.
- Footnote 100
-
Macinko, J.A., Shi, L., Starfield, B., Wulu Jr., J.T., (2003). Income inequality and health: a critical review of the literature. Medical Care Research & Review, 60(4), 407-452.
- Footnote 101
-
Grant, T.L., Edwards, N., Sveistrup, H., Andrew, C., Egan, M. (2010). Inequitable walking conditions among older people: examining the interrelationship of neighbourhood socio-economic status and urban form using a comparative case study. BMC Public Health, 10, 677.
- Footnote 102
-
Larsen, K., Gilliland, J. (2008). Mapping the evolution of 'food deserts; in a Canadian city : Supermarket accessibility in London, Ontario, 1961-2005. International Journal of Health Geographics, 7, 16.
- Footnote 103
-
Kheirbek, I., Haney, J., Douglas, S., Ito, K., Matte, T. (2016). The contribution of motor vehicle emissions to ambient fine particulate matter public health impacts in New York City: a health burden assessment. Environmental Health, 15(1), 89.
- Footnote 104
-
Sugiyama, T., Howard, N.J., Paquet, C., Coffee, N.T., Taylor, A.W., Daniel, M. (2015). Do relationships between environmental attributes and recreational walking vary according to area-level socioeconomic status? Journal of Urban Health, 92(2), 253-264.
- Footnote 105
-
Clark, C., Myron, R., Stansfeld, S., Candy, B. (2007). A systematic review of the evidence on the built and physical environment on mental health. Journal of Public Mental Health, 6(2), 14-27.
- Footnote 106
-
Haddad, L., Schafer, A., Streit, F., Lederbogen, F., Grimm, O., Wust, S., Deuschle, M., Kirsch, P., Tost, H., Meyer-Lindenberg, A. (2015). Brain structure correlates with urban upbringing, an environment risk factor for schizophrenia. Schizophrenia Bulletin, 41(1), 115-122.
- Footnote 107
-
Hirsch, J.K. (2006). A review of the literature on rural suicide: risk and protective factors, incidence and prevention. Crisis, 27(4), 189-199.
- Footnote 108
-
Krabbendam, L., van Os, J. (2005). Schizophrenia and urbanicity: a major environmental influence – conditional on genetic risk. Schizophrenia Bulletin, 31(4), 795-799.
- Footnote 109
-
Peen, J., Schoevers, R.A., Beekman, A.T., Dekker, J. (2010). The current status of urban-rural differences in psychiatric disorders. Acta Psychiatrica Scandinavica, 121(2), 84-93.
- Footnote 110
-
Pedersen, C.B., Mortensen, P.B. (2001). Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Archives of General Psychiatry, 58(11), 1039-1045.
- Footnote 111
-
Sundquist, K., Frank, G. (2004). Urbanization and hospital admission rates for alcohol and drug abuse: a follow-up study of 4.5 million women and men in Sweden. Addiction, 99(10), 1298-1305.
- Footnote 112
-
Van Son, G.E., van Hoeken, D., Bartelds, A.I., van Furth, E.F., Hoek, H.W. (2006). Urbanisation and the incidence of eating disorders. British Journal of Psychiatry, 189, 562-563.
- Footnote 113
-
Lederbogen, F., Kirsch, P., Haddad, L., Streit, F., Tost, H. Schuch, P., Wust, S., Pruessner, J.C., Rietschel, M., Deuschel, M., Meyer-Lindenberg, A. (2011). City living and urban upbringing affect neural social stress processing in humans. Nature, 474(7352), 498-501.
- Footnote 114
-
Steinheuser, V., Ackermann, K., Schofeld, P., Schwabe, L. (2014). Stress and the city: impact of urban upbringing on the (re)activity of the hypothalamus-pituitary-adrenal axis. Psychosomatic Medicine, 76(9), 678-685.
Building blocks of Canadian communities
Active neighbourhoods
- Footnote 115
-
Statistics Canada. Table 117-0019 - Distribution of the household population meeting/not meeting the Canadian physical activity guidelines, by sex and age group (occasional (percentage)). Statistics Canada.
- Footnote 116
-
Kelly, P., Kahlmeier, S., Gotschi, T., Orsini, N., Richards, J., Roberts, N., Scarborough, P., Foster, C. (2014). Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. International Journal of Behavioral Nutrition & Physical Activity, 11, 132.
- Footnote 117
-
Lee, I. M., Shiroma, E. J., Lobelo, F., Puska, P., Blair, S. N., Katzmarzyk, P. T., Lancet Physical Activity Series Working Group. (2012). Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet, 380(9838), 219-229.
- Footnote 118
-
Woodcock, J., Franco, O. H., Orsini, N., Roberts, I. (2011). Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. International Journal of Epidemiology, 40(1), 121-138.
- Footnote 119
-
Bauman, A., Merom, D., Bull, F. C., Buchner, D. M., Fiatarone Singh, M. A. (2016). Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote "Active Aging". The Gerontologist, 56(Suppl_2), S268-S280.
- Footnote 120
-
Bouaziz, W., Vogel, T., Schmitt, E., Kaltenbach, G., Geny, B., Lang, P. O. (2017). Health benefits of aerobic training programs in adults aged 70 and over: a systematic review. Archives of Gerontology and Geriatrics, 69, 110-127.
- Footnote 121
-
Costigan, S. A., Eather, N., Plotnikoff, R. C., Taaffe, D. R., Lubans, D. R. (2015). High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. British Journal of Sports Medicine, 39(19), 1253-1261.
- Footnote 122
-
García‐Hermoso, A., Cerrillo‐Urbina, A. J., Herrera‐Valenzuela, T., Cristi‐Montero, C., Saavedra, J. M., Martínez‐Vizcaíno, V. (2016). Is high‐intensity interval training more effective on improving cardiometabolic risk and aerobic capacity than other forms of exercise in overweight and obese youth? A meta‐analysis. Obesity Reviews, 17(6), 531-540.
- Footnote 123
-
Jelleyman, C., Yates, T., O'Donovan, G., Gray, L. J., King, J. A., Khunti, K., Davies, M. J. (2015). The effects of high‐intensity interval training on glucose regulation and insulin resistance: a meta‐analysis. Obesity Reviews, 16(11), 942-961.
- Footnote 124
-
Kruk, J., Czerniak, U. (2013). Physical activity and its relation to cancer risk: updating the evidence. Asian Pacific Journal of Cancer Prevention, 14(7) 399-4003.
- Footnote 125
-
Liou, K., Ho, S., Fildes, J., Ooi, S. Y. (2016). High intensity interval versus moderate intensity continuous training in patients with coronary artery disease: a meta-analysis of physiological and clinical parameters. Heart, Lung and Circulation, 25(2), 166-174.
- Footnote 126
-
Loprinzi, P. D., Cardinal, B. J., Loprinzi, K. L., Lee, H. (2012). Benefits and environmental determinants of physical activity in children and adolescents. Obesity Facts, 5(4), 597-610.
- Footnote 127
-
Melo, M. C. A., Daher, E. D. F., Albuquerque, S. G. C., de Bruin, V. M. S. (2016). Exercise in bipolar patients: a systematic review. Journal of Affective Disorders, 198, 32-38.
- Footnote 128
-
O'Donovan, G., Lee, I. M., Hamer, M., Stamatakis, E. (2017). Association of "weekend warrior" and other leisure time physical activity patterns with risks for all-cause, cardiovascular disease, and cancer mortality. JAMA Internal Medicine, 177(3), 335-342.
- Footnote 129
-
Petriz, B. A., Gomes, C. P., Almeida, J. A., de Oliveira, G. P., Ribeiro, F. M., Pereira, R. W., Franco, O. L. (2017). The effects of acute and chronic exercise on skeletal muscle proteome. Journal of Cellular Physiology, 232(2), 257-269.
- Footnote 130
-
Poitras, V. J., Gray, C. E., Borghese, M. M., Carson, V., Chaput, J. P., Janssen, I., Katzmarzyk, P.T., Pate, R.R., Connor Gorber, S., Kho, M.E., Sampson, M. (2016). Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41(6), S197-S239.
- Footnote 131
-
Radovic, S., Gordon, M. S., Melvin, G. A. (2017). Should we recommend exercise to adolescents with depressive symptoms? A meta‐analysis. Journal of Paediatrics and Child Health, 53(3), 214-220.
- Footnote 132
-
Ramos, J. S., Dalleck, L. C., Tjonna, A. E., Beetham, K. S., Coombes, J. S. (2015). The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports Medicine, 45(5), 679.
- Footnote 133
-
Rimes, R.R., de Souza Moura, A.M., Khede Lamego, M., Souza de Sa Filho, A., Manochio, J., Paes, F., Giovanni Carta, M., Mura, G., Wegner, M., Budde, H. Barbosa Ferreira Rocha, N. (2015). Effects of exercise on physical and mental health, and cognitive and brain functions in schizophrenia: clinical and experimental evidence. CNS and Neurological Disorders-Drug Targets, 14(10), 1244-1254.
- Footnote 134
-
Rosenbaum, S., Tiedemann, A., Stanton, R., Parker, A., Waterreus, A., Curtis, J., Ward, P. B. (2016). Implementing evidence-based physical activity interventions for people with mental illness: an Australian perspective. Australasian Psychiatry, 24(1), 49-54.
- Footnote 135
-
Stubbs, B., Vancampfort, D., Rosenbaum, S., Firth, J., Cosco, T., Veronese, N., Salum, G. A., Schuch, F. B. (2017). An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Research, 249, 102-108.
- Footnote 136
-
Warburton, D. E., Katzmarzyk, P. T., Rhodes, R. E., Shephard, R. J. (2007). Evidence informed physical activity guidelines for Canadian adults. Canadian Journal of Public Health, 96 (Suppl 2), S16-68.
- Footnote 137
-
World Cancer Research Fund/American Institute for Cancer Research. (2007). Food, nutrition, physical activity and the prevention of cancer. A global perspective. Washington DC: AICR.
- Footnote 138
-
Zhao, W., Ukawa, S., Kawamura, T., Wakai, K., Ando, M., Tsushita, K., Tamakoshi, A. (2015). Health benefits of daily walking on mortality among younger-elderly men with or without major critical diseases in the new integrated suburban seniority investigation project: a prospective cohort study. Journal of Epidemiology, 25(10), 609-616.
- Footnote 139
-
Hilfiker, R., Meichtry, A., Eicher, M., Nilsson, B. L., Knols, R. H., Verra, M. L., Taeymans, J. (2017). Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. British Journal of Sports Medicine, epub.
- Footnote 140
-
Cormie, P., Zopf, E. M., Zhang, X., Schmitz, K. H. (2017). The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiologic Reviews, 39(1), 71-92.
- Footnote 141
-
Zanuso, S., Sacchetti, M., Sundberg, C. J., Orlando, G., Benvenuti, P., Balducci, S. (2017). Exercise in type 2 diabetes: genetic, metabolic and neuromuscular adaptations. A review of the evidence. British Journal of Sports Medicine, epub.
- Footnote 142
-
Baptista, L. C., Machado-Rodrigues, A. M., Martins, R. A. (2017). Exercise but not metformin improves health-related quality of life and mood states in older adults with type 2 diabetes. European Journal of Sport Science, 17(6), 794-804.
- Footnote 143
-
Melling, C. W. J., Grisé, K. N., Hasilo, C. P., Fier, B., Milne, K. J., Karmazyn, M., Noble, E. G. (2013). A model of poorly controlled type 1 diabetes mellitus and its treatment with aerobic exercise training. Diabetes and Metabolism, 39(3), 226-235.
- Footnote 144
-
O'Gorman, D. J., Krook, A. (2011). Exercise and the treatment of diabetes and obesity. Medical Clinics of North America, 95(5), 953-969.
- Footnote 145
-
Sanz, C., Gautier, J. F., Hanaire, H. (2010). Physical exercise for the prevention and treatment of type 2 diabetes. Diabetes and Metabolism, 36(5), 346-351.
- Footnote 146
-
Berry, T. R., Spence, J. C., Blanchard, C., Cutumisu, N., Edwards, J., Nykiforuk, C. (2010). Changes in BMI over 6 years: the role of demographic and neighborhood characteristics. International Journal of Obesity, 34(8), 1275-1283.
- Footnote 147
-
Berry, T. R., Spence, J. C., Blanchard, C. M., Cutumisu, N., Edwards, J., Selfridge, G. (2010). A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 57.
- Footnote 148
-
Casazza, K., Brown, A., Astrup, A., Bertz, F., Baum, C., Brown, M. B., Dawson, J., Durant, N., Dutton, G., Fields, D.A., Fontaine, K. R. (2015). Weighing the evidence of common beliefs in obesity research. Critical Reviews in Food Science and Nutrition, 55(14), 2014-2053.
- Footnote 149
-
Ferdinand, A.O., Sen, B., Rahurkar, S., Engler, S., Menachemi, N. (2012). The relationship between built environments and physical activity: a systematic review. American Journal of Public Health, 102(10), e7-e13
- Footnote 150
-
Feng, J., Glass, T. A., Curriero, F. C., Stewart, W. F., Schwartz, B. S. (2010). The built environment and obesity: a systematic review of the epidemiologic evidence. Health and Place, 16(2), 175-190.
- Footnote 151
-
Booth, K. M., Pinkston, M. M., Poston, W. S. C. (2005). Obesity and the built environment. Journal of the American Dietetic Association, 105(5), 110-117.
- Footnote 152
-
Durand, C. P., Andalib, M., Dunton, G. F., Wolch, J., Pentz, M. A. (2011). A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obesity Reviews, 12(5), e173-e182.
- Footnote 153
-
Ewing, R., Meakins, G., Hamidi, S., Nelson, A. C. (2014). Relationship between urban sprawl and physical activity, obesity, and morbidity–update and refinement. Health and Place, 26, 118-126.
- Footnote 154
-
Hipp, J. A., Chalise, N. (2015). Spatial analysis and correlates of county-level diabetes prevalence, 2009–2010. Preventing Chronic Disease, 12.
- Footnote 155
-
Malambo, P., Kengne, A. P., De Villiers, A., Lambert, E. V., Puoane, T. (2016). Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review. PloS One, 11(11), e0166846.
- Footnote 156
-
Renalds, A., Smith, T. H., Hale, P. J. (2010). A systematic review of built environment and health. Family and Community Health, 33(1), 68-78.
- Footnote 157
-
Zick, C. D., Hanson, H., Fan, J. X., Smith, K. R., Kowaleski-Jones, L., Brown, B. B., Yamada, I. (2013). Re-visiting the relationship between neighbourhood environment and BMI: an instrumental variables approach to correcting for residential selection bias. International Journal of Behavioral Nutrition and Physical Activity, 10(1), 27.
- Footnote 158
-
Kligerman, M., Sallis, J. F., Ryan, S., Frank, L. D., Nader, P. R. (2007). Association of neighborhood design and recreation environment variables with physical activity and body mass index in adolescents. American Journal of Health Promotion, 21(4), 274-277.
- Footnote 159
-
Saelens, B. E., Sallis, J. F., Frank, L. D., Couch, S. C., Zhou, C., Colburn, T., Cain, K.L., Chapman, J., Glanz, K. (2012). Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. American Journal of Preventive Medicine, 42(5), e57-e64.
- Footnote 160
-
Sugiyama, T., Koohsari, M. J., Mavoa, S., Owen, N. (2014). Activity-friendly built environment attributes and adult adiposity. Current Obesity Reports, 3(2), 183-198.
- Footnote 161
-
Creatore, M. I., Glazier, R. H., Moineddin, R., Fazli, G. S., Johns, A., Gozdyra, P., Matheson, F.I., Kaufman-Shriqui, V., Rosella, L.C., Manuel, D.G., Booth, G. L. (2016). Association of neighborhood walkability with change in overweight, obesity, and diabetes. JAMA, 315(20), 2211-2220.
- Footnote 162
-
Glazier, R. H., Creatore, M. I., Weyman, J. T., Fazli, G., Matheson, F. I., Gozdyra, P., Moineddin, R., Shriqui, V.K., Booth, G. L. (2014). Density, destinations or both? A comparison of measures of walkability in relation to transportation behaviors, obesity and diabetes in Toronto, Canada. PloS One, 9(1), e85295.
- Footnote 163
-
Booth, G. L., Creatore, M. I., Moineddin, R., Gozdyra, P., Weyman, J. T., Matheson, F. I., Glazier, R. H. (2013). Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care, 36(2), 302-308.
- Footnote 164
-
Loo, C. J., Greiver, M., Aliarzadeh, B., Lewis, D. (2017). Association between neighbourhood walkability and metabolic risk factors influenced by physical activity: a cross-sectional study of adults in Toronto, Canada. BMJ Open, 7(4), e013889.
- Footnote 165
-
Booth, G.L. (2016). Built environment and health. Canada Communicable Disease Report, 42, 10.
- Footnote 166
-
Kaczynski, A. (2010). Neighborhood walkability perceptions: associations with amount of neighborhood-based physical activity by intensity and purpose. Journal of Physical Activity & Health, 7(1), 3-10.
- Footnote 167
-
Wojan, T.R., Hamrick, K.S. (2015). Can walking or biking to work really make a difference? Compact development, observed commuter choice and body mass index. PLoS One, 10(7).
- Footnote 168
-
Mueller, N., Rojas-Rueda, D., Cole-Hunter, T., de Nazelle, A., Dons, E., Gerike, R., Goetschi, T., Panis, L.I., Kahlmeier, S., Nieuwenhuijsen, M. (2015). Health impact assessment of active transportation: a systematic review. Preventive Medicine, 76, 103-114.
- Footnote 169
-
Butler, G.P., Orpana, H.M., Wiens, A.J. (2007). By your own two feet: factors associated with active transportation in Canada. Canadian Journal of Public Health, 98(4), 259-264.
- Footnote 170
-
Ogilvie, D., Foster, C.E., Rothnie, H., Cavill, N., Hamilton, V., Fitzsimons, C.F., Mutrie, N., Scottish Physical Activity Research Collaboration. (2007). Interventions to promote walking: systematic review. BMJ, 334(7605), 1204.
- Footnote 171
-
Public Health Agency of Canada (2014). What is Active Transportation? Public Health Agency of Canada.
- Footnote 172
-
Besser, L. M., Dannenberg, A. L. (2005). Walking to public transit: steps to help meet physical activity recommendations. American Journal of Preventive Medicine, 29(4), 273-280.
- Footnote 173
-
Lachapelle, U., Frank, L. D. (2009). Transit and health: mode of transport, employer-sponsored public transit pass programs, and physical activity. Journal of Public Health Policy, 30(1), S73-S94.
- Footnote 174
-
Chaix, B., Kestens, Y., Duncan, S., Merrien, C., Thierry, B., Pannier, B., Brondeel, R., Lewin, A., Karusisi, N., Perchoux, C., Thomas, F. (2014). Active transportation and public transportation use to achieve physical activity recommendations? A combined GPS, accelerometer, and mobility survey study. International Journal of Behavioral Nutrition and Physical Activity, 11(1), 124.
- Footnote 175
-
Rissel, C., Curac, N., Greenaway, M., Bauman, A. (2012). Physical activity associated with public transport use—a review and modelling of potential benefits. International Journal of Environmental Research and Public Health, 9(7), 2454-2478.
- Footnote 176
-
Lachapelle, U., Frank, L., Saelens, B. E., Sallis, J. F., Conway, T. L. (2011). Commuting by public transit and physical activity: where you live, where you work, and how you get there. Journal of Physical Activity and Health, 8(Suppl 1), S72-S82.
- Footnote 177
-
Yang, L., Sahlqvist, S., McMinn, A., Griffin, S.J., Ogilvie, D. (2010). Interventions to promote cycling : systematic review. BMJ, 341, c5293.
- Footnote 178
-
New York City Department of Health and Mental Hygiene. (2011). Health benefits of active transportation in New York City. NYC Vital Signs, 10(3).
- Footnote 179
-
Canadian Institute of Planners (2012). Active transportation, health and community design: What is the Canadian evidence saying? Canadian Institute of Planners.
- Footnote 180
-
Handy, S. L., Boarnet, M. G., Ewing, R., Killingsworth, R. E. (2002). How the built environment affects physical activity: views from urban planning. American Journal of Preventive Medicine, 23(2), 64-73.
- Footnote 181
-
Stevens, M. R. (2017). Does compact development make people drive less?. Journal of the American Planning Association, 83(1), 7-18.
- Footnote 182
-
Giles-Corti, B., Vernez-Moudon, A., Reis, R., Turrell, G., Dannenberg, A.L., Badland, H., Foster, S., Lowe, M., Sallis, J.F., Stevenson, M., Owen, N. (2016). City planning and population health : a global challenge. The Lancet, 388(10062), 2912-2924.
- Footnote 183
-
Sallis, J.F., Bull., F., Burdett, R., Frank, L.D., Griffiths, P., Giles-Corti, B., Stevenson, M. (2016 ). Use of science to guide city planning policy and practice : how to achieve healthy and sustainable future cities. The Lancet, 388(10062), 2936-2947.
- Footnote 184
-
Sallis, J.F., Cerin, E., Conway, T.L., Adams, M.A., Frank, L.D., Pratt, M., Salvo, D., Schipperijn, J., Smith G., Cain, K.L., Davey, R., Kerr, J., Lai, P.C., Mitas, J., Reis, R., Sarmiento, O.L., Schofield, G., Troelsen, J., Van Dyck, D., De Bourdeaudhuij, I., Owen, N. (2016). Physical activity in relation to urban environments in 14 cities worldwide: a cross-sectional study. The Lancet, 387(10034), 2207-2217.
- Footnote 185
-
Hajna, S., Ross, N. A., Brazeau, A. S., Bélisle, P., Joseph, L., Dasgupta, K. (2015). Associations between neighbourhood walkability and daily steps in adults: a systematic review and meta-analysis. BMC Public Health, 15(1), 768.
- Footnote 186
-
Kelly, C., Lian, M., Struthers, J., Kammrath, A. (2015). Walking to work: The roles of neighborhood walkability and socioeconomic deprivation. Journal of Physical Activity and Health, 12(Suppl 1), S70-S75.
- Footnote 187
-
Thielman, J., Manson, H., Chiu, M., Copes, R., Rosella, L. C. (2016). Residents of highly walkable neighbourhoods in Canadian urban areas do substantially more physical activity: a cross-sectional analysis. Canadian Medical Association Journal Open, 4(4), e720.
- Footnote 188
-
Public Health Agency of Canada (2011). Fast facts about Canada's neighbourhoods and physical activity. Public Health Agency of Canada.
- Footnote 189
-
Hajna, S., Ross, N. A., Joseph, L., Harper, S., Dasgupta, K. (2015). Neighbourhood walkability, daily steps and utilitarian walking in Canadian adults. BMJ Open, 5(11), e008964.
- Footnote 190
-
Jack, E., McCormack, G. R. (2014). The associations between objectively-determined and self-reported urban form characteristics and neighborhood-based walking in adults. International Journal of Behavioral Nutrition and Physical Activity, 11(1), 71.
- Footnote 191
-
Thielman, J., Rosella, L., Copes, R., Lebenbaum, M., Manson, H. (2015). Neighborhood walkability: differential associations with self-reported transport walking and leisure-time physical activity in Canadian towns and cities of all sizes. Preventive Medicine, 77, 174-180.
- Footnote 192
-
Wasfi, R. A., Ross, N. A., El-Geneidy, A. M. (2013). Achieving recommended daily physical activity levels through commuting by public transportation: Unpacking individual and contextual influences. Health and Place, 23, 18-25.
- Footnote 193
-
Winters, M., Brauer, M., Setton, E. M., Teschke, K. (2010). Built environment influences on healthy transportation choices: bicycling versus driving. Journal of Urban Health, 87(6), 969-993.
- Footnote 194
-
Brown, B. B., Tharp, D., Tribby, C. P., Smith, K. R., Miller, H. J., Werner, C. M. (2016). Changes in bicycling over time associated with a new bike lane: relations with kilocalories energy expenditure and body mass index. Journal of Transport and Health, 3(3), 357-365.
- Footnote 195
-
Fuller, D., Gauvin, L., Kestens, Y., Daniel, M., Fournier, M., Morency, P., Drouin, L. (2013). Impact evaluation of a public bicycle share program on cycling: a case example of BIXI in Montreal, Quebec. American Journal of Public Health, 103(3), e85-e92.
- Footnote 196
-
Goodman, A., Sahlqvist, S., Ogilvie, D., iConnect Consortium. (2014). New walking and cycling routes and increased physical activity: one-and 2-year findings from the UK iConnect Study. American Journal of Public Health, 104(9), e38-e46.
- Footnote 197
-
Panter, J., Ogilvie, D. (2015). Theorising and testing environmental pathways to behaviour change: natural experimental study of the perception and use of new infrastructure to promote walking and cycling in local communities. BMJ open, 5(9), e007593.
- Footnote 198
-
Parker, K. M., Gustat, J., Rice, J. C. (2011). Installation of bicycle lanes and increased ridership in an urban, mixed-income setting in New Orleans, Louisiana. Journal of Physical Activity and Health, 8(Suppl 1), S98-S102.
- Footnote 199
-
Parker, K. M., Rice, J., Gustat, J., Ruley, J., Spriggs, A., Johnson, C. (2013). Effect of bike lane infrastructure improvements on ridership in one New Orleans neighborhood. Annals of Behavioral Medicine, 45(1), 101-107.
- Footnote 200
-
Pucher, J., Buehler, R. (2008). Making cycling irresistible: lessons from the Netherlands, Denmark and Germany. Transport Reviews, 28(4), 495-528.
- Footnote 201
-
Pucher, J., Dill, J., Handy, S. (2010). Infrastructure, programs, and policies to increase bicycling: an international review. Preventive Medicine, 50, S106-S125.
- Footnote 202
-
Rissel, C., Greaves, S., Wen, L. M., Crane, M., Standen, C. (2015). Use of and short-term impacts of new cycling infrastructure in inner-Sydney, Australia: a quasi-experimental design. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 129.
- Footnote 203
-
Stewart, G., Anokye, N. K., Pokhrel, S. (2015). What interventions increase commuter cycling? A systematic review. BMJ Open, 5(8), e007945.
- Footnote 204
-
Winters, M., Teschke, K., Brauer, M., Fuller, D. (2016). Bike Score®: Associations between urban bikeability and cycling behavior in 24 cities. International Journal of Behavioral Nutrition and Physical Activity, 13(1), 18.
- Footnote 205
-
Reynolds, C. C., Harris, M. A., Teschke, K., Cripton, P. A., Winters, M. (2009). The impact of transportation infrastructure on bicycling injuries and crashes: a review of the literature. Environmental Health, 8(1), 47.
- Footnote 206
-
Arvidsson, D., Kawakami, N., Ohlsson, H., Sundquist, K. (2012). Physical activity and concordance between objective and perceived walkability. Medicine and Science in Sports and Exercise, 44(2), 280-287.
- Footnote 207
-
Gebel, K., Bauman, A. E., Sugiyama, T., Owen, N. (2011). Mismatch between perceived and objectively assessed neighborhood walkability attributes: prospective relationships with walking and weight gain. Health and Place, 17(2), 519-524.
- Footnote 208
-
Gebel, K., Bauman, A., Owen, N. (2009). Correlates of non-concordance between perceived and objective measures of walkability. Annals of Behavioral Medicine, 37(2), 228-238.
- Footnote 209
-
Nieuwenhuijsen, M. J., Khreis, H. (2016). Car free cities: pathway to healthy urban living. Environment International, 94, 251-262.
- Footnote 210
-
Manville, M., King, D. A., Smart, M. J. (2017). The Driving Downturn: A Preliminary Assessment. Journal of the American Planning Association, 83(1), 42-55.
- Footnote 211
-
Coronini-Cronberg, S., Millett, C., Laverty, A. A., Webb, E. (2012). The impact of a free older persons' bus pass on active travel and regular walking in England. American Journal of Public Health, 102(11), 2141-2148.
- Footnote 212
-
Edwards, P., Steinbach, R., Green, J., Petticrew, M., Goodman, A., Jones, A., Roberts, H., Kelly, C., Nellthorp, J., Wilkinson, P. (2013). Health impacts of free bus travel for young people: evaluation of a natural experiment in London. Journal of Epidemiology and Community Health, jech-2012.
- Footnote 213
-
Green, J., Steinbach, R., Jones, A., Edwards, P., Kelly, C., Nellthorp, J., Goodman, A., Roberts, H., Petticrew, M., Wilkinson, P. (2014). On the buses: a mixed-method evaluation of the impact of free bus travel for young people on the public health. Public Health Research, 2(1).
- Footnote 214
-
Menai, M., Charreire, H., Feuillet, T., Salze, P., Weber, C., Enaux, C., Andreeva, V.A., Hercberg, S., Nazare, J.A., Perchoux, C., Simon, C. (2015). Walking and cycling for commuting, leisure and errands: relations with individual characteristics and leisure-time physical activity in a cross-sectional survey (the ACTI-Cités project). International Journal of Behavioral Nutrition and Physical Activity, 12(1), 150.
- Footnote 215
-
Stepaniuk, J. A., Tuokko, H., McGee, P., Garrett, D. D., Benner, E. L. (2008). Impact of transit training and free bus pass on public transportation use by older drivers. Preventive Medicine, 47(3), 335-337.
- Footnote 216
-
Webb, E., Laverty, A., Mindell, J., Millett, C. (2016). Free bus travel and physical activity, gait speed, and adiposity in the English Longitudinal Study of Ageing. American Journal of Public Health, 106(1), 136-142.
- Footnote 217
-
Adams, E. J., Goodman, A., Sahlqvist, S., Bull, F. C., Ogilvie, D. (2013). Correlates of walking and cycling for transport and recreation: factor structure, reliability and behavioural associations of the perceptions of the environment in the neighbourhood scale (PENS). International Journal of Behavioral Nutrition and Physical Activity, 10(1), 87.
- Footnote 218
-
Addy, C. L., Wilson, D. K., Kirtland, K. A., Ainsworth, B. E., Sharpe, P., Kimsey, D. (2004). Associations of perceived social and physical environmental supports with physical activity and walking behavior. American Journal of Public Health, 94(3), 440-443.
- Footnote 219
-
Giles-Corti, B., Bull, F., Knuiman, M., McCormack, G., Van Niel, K., Timperio, A., Christian, H., Foster, S., Divitini, M., Middleton, N., Boruff, B. (2013). The influence of urban design on neighbourhood walking following residential relocation: longitudinal results from the RESIDE study. Social Science and Medicine, 77, 20-30.
- Footnote 220
-
McCormack, G. R., Friedenreich, C. M., Giles-Corti, B., Doyle-Baker, P. K., Shiell, A. (2013). Do motivation-related cognitions explain the relationship between perceptions of urban form and neighborhood walking? Journal of Physical Activity and Health, 10(7), 961-973.
- Footnote 221
-
Merom, D., Bauman, A., Phongsavan, P., Cerin, E., Kassis, M., Brown, W., Smith, B.J. Rissel, C. (2009). Can a motivational intervention overcome an unsupportive environment for walking—findings from the Step-by-Step Study. Annals of Behavioral Medicine, 38(2), 137-146.
- Footnote 222
-
Perchoux, C., Kestens, Y., Brondeel, R., Chaix, B. (2015). Accounting for the daily locations visited in the study of the built environment correlates of recreational walking (the RECORD Cohort Study). Preventive Medicine, 81, 142-149.
- Footnote 223
-
Chaix, B., Simon, C., Charreire, H., Thomas, F., Kestens, Y., Karusisi, N., Vallée, J., Oppert, J.M., Weber, C. Pannier, B. (2014). The environmental correlates of overall and neighborhood based recreational walking (a cross-sectional analysis of the RECORD Study). International Journal of Behavioral Nutrition and Physical Activity, 11(1), 20.
- Footnote 224
-
Buehler, R., Pucher, J. (2012). International Overview: Cycling Trends in Western Europe, North America, and Australia. City Cycling, 9-29.
- Footnote 225
-
Ebert, A. K. (2004). Cycling towards the nation: The use of the bicycle in Germany and the Netherlands, 1880–1940. European Review of History, 11(3), 347-364.
- Footnote 226
-
Statistique Canada (2017). La pratique de la bicyclette au Canada. Rapports sur la santé. Statistique Canada.
- Footnote 227
-
Pucher, J., Buehler, R. (2006). Why Canadians cycle more than Americans: a comparative analysis of bicycling trends and policies. Transport Policy, 13(3), 265-279.
- Footnote 228
-
Pucher, J., Buehler, R., Seinen, M. (2011). Bicycling renaissance in North America? An update and re-appraisal of cycling trends and policies. Transportation Research Part A: Policy and Practice, 45(6), 451-475.
- Footnote 229
-
Lopez, R., Hynes, H. P. (2003). Sprawl in the 1990s: measurement, distribution, and trends. Urban Affairs Review, 38(3), 325-355.
- Footnote 230
-
Statistics Canada (2017). Population and dwelling count highlight tables, 2016 Census. Statistics Canada.
- Footnote 231
-
City of Toronto (2017). Ward Profiles.
- Footnote 232
-
Mueller, N., Rojas-Rueda, D., Cole-Hunter, T., De Nazelle, A., Dons, E., Gerike, R., Gotschi, T., Int Panis, L., Kahlmeier, S., Neiuwenhuijsen, M. (2015). Health impact assessment of active transportation: a systematic review. Preventative Medicine, 76, 103-104.
- Footnote 233
-
Cairns, J., Warren, J., Garthwaite, K., Greig, G., Bambra, C. (2015). Go slow: an umbrella review of the effects of 20 mph zones and limits on health and health inequalities. Journal of Public Health, 37(3), 515-520.
- Footnote 234
-
Elvik, R. (2001). Area-wide urban traffic calming schemes: a meta-analysis of safety effects. Accident Analysis and Prevention, 33(3), 327-336.
- Footnote 235
-
Pulugurtha, S. S., Desai, A., Pulugurtha, N. M. (2010). Are pedestrian countdown signals effective in reducing crashes?. Traffic Injury Prevention, 11(6), 632-641.
- Footnote 236
-
Retting, R. A., Ferguson, S. A., McCartt, A. T. (2003). A review of evidence-based traffic engineering measures designed to reduce pedestrian–motor vehicle crashes. American Journal of Public Health, 93(9), 1456-1463.
- Footnote 237
-
Moradi, A., Soori, H., Kavousi, A., Eshghabadi, F., Jamshidi, E. (2016). Spatial factors affecting the frequency of pedestrian traffic crashes: a systematic review. Archives of Trauma Research, 5(4).
- Footnote 238
-
Brown, B.B., Tharp, D., Tribby, C.P., Smith, K.R., Miller, H.J., Werner, C.M. (2016). Changes in bicycling over time associated with a new bike lane: relationship with kilocalories energy expenditure and body mass index. Journal of Transportation & Health, 3(3), 357-365.
- Footnote 239
-
Fuller, D., Guavin, L., Kestens, Y., Daniel, M., Fournier, M., Morency, P., Drouin, L. (2013) Impact evaluation of a public bicycle share program on cycling: a case example of BIXI in Montreal, Quebec. American Journal of Public Health, 103(3), e85-e92.
- Footnote 240
-
Goodman, A., Sahlqvist, S., Ogilivie, D., iConnect Consortium (2014). New walking and cycling routes and increased physical activity: one- and 2-year findings from the UK iConnect Study. Am J Public Health, 104(9), e38-e46.
- Footnote 241
-
Winters, M., Teschke, K., Grant, M., Setton, E., Brauer, M. (2014). How far out of the way will we travel? Built environment influences on route selection for bicycle and car travel. Transportation Research Record, 2190.
- Footnote 242
-
Winters, M., Brauer, M., Setton, E.M., Teschke, K. (2010). Built environment influences on healthy transportation choices : bicycling versus driving. Journal of Urban Health, 87(6), 969-993.
- Footnote 243
-
Winters, M., Buehler, R., Gotschi, T. (2017). Policies to promote active travel: evidence from reviews of literature. Current Environmental Health Reports, epub.
- Footnote 244
-
Jarjour, S., Jerrett, M., Westerdahl, D., de Nazelle, A., Hanning, C., Daly, L., Lipsitt, J., Balmes, J. (2013). Cyclist route choice, traffic-related air pollution, and lung function: a scripted exposure study. Environmental Health, 12(1), 14.
- Footnote 245
-
Organisation mondiale de la Santé (2016). Ambient air pollution: a global assessment of exposure and burden of disease. Organisation mondiale de la Santé.
- Footnote 246
-
Environment and Climate Change Canada (2016). Your Local Air Quality Health Index Conditions. Environment and Climate Change Canada.
- Footnote 247
-
Brook, R. D., Bard, R. L., Morishita, M., Dvonch, J. T., Wang, L., Yang, H. Y., Spino, C., Mukherjee, B., Kaplan, M.J., Yalavarthi, S., Oral, E. A. (2014). Hemodynamic, autonomic, and vascular effects of exposure to coarse particulate matter air pollution from a rural location. Environmental Health Perspectives, 122(6), 624.
- Footnote 248
-
Urch, B., Speck, M., Corey, P., Wasserstein, D., Manno, M., Lukic, K. Z., Brook, J.R., Liu, L., Coull, B., Schwartz, J., Gold, D. R. (2010). Concentrated ambient fine particles and not ozone induce a systemic interleukin-6 response in humans. Inhalation Toxicology, 22(3), 210-218.
- Footnote 249
-
Betts, K.S. (2012). Heart Disease Tradeoffs: The Built Environment, Air Pollution, and Activity. Environmental Health Perspectives, 120(2), a77.
- Footnote 250
-
De Nazelle, A., Rodríguez, D. A., Crawford-Brown, D. (2009). The built environment and health: impacts of pedestrian-friendly designs on air pollution exposure. Science of the Total Environment, 407(8), 2525-2535.
- Footnote 251
-
Hankey, S., Marshall, J. D., Brauer, M. (2012). Health impacts of the built environment: within-urban variability in physical inactivity, air pollution, and ischemic heart disease mortality. Environmental Health Perspectives, 120(2), 247.
- Footnote 252
-
Sattar, S. A., Wright, K. E., Zargar, B., Rubino, J. R., Ijaz, M. K. (2016). Airborne infectious agents and other pollutants in automobiles for domestic use: potential health impacts and approaches to risk mitigation. Journal of Environmental and Public Health.
- Footnote 253
-
Tainio, M., de Nazelle, A. J., Götschi, T., Kahlmeier, S., Rojas-Rueda, D., Nieuwenhuijsen, M. J., de Sá, T.H., Kelly, P., Woodcock, J. (2016). Can air pollution negate the health benefits of cycling and walking?. Preventive Medicine, 87, 233-236.
- Footnote 254
-
Giles, L. V., Koehle, M. S. (2014). The health effects of exercising in air pollution. Sports Medicine, 44(2), 223-249.
- Footnote 255
-
Chen, H., Kwong, J.C., Copes, R., Tu, K., Villenevue, P.J., van Donkelaar, A., Hystad, P., Martin, R.V., Murray, B.J., Jessiman, B., Wilton, A.S., Kopp, A., Burnett, R.T. (2017). Living near major roads and the incidence of dementia, Parkinson's disease and multiple sclerosis: a population-based cohort study. The Lancet, 389(10070), 718-726.
- Footnote 256
-
Kelly, F.J., Fussell, J.C. (2015). Air pollution and public health : emerging hazards and improved understanding risk. Environmental Geochemistry & Health, 37(4), 631-649.
- Footnote 257
-
Khreis, H., Kelly, C., Tate, J., Parslow, R., Lucas, K., Niewenhuijsen, M. (2017). Exposure to traffic-related air pollution and risk of development of childhood asthma: a systematic review and meta-analysis. Environment International, 100, 1-31.
- Footnote 258
-
Stieb, D.M., Chen, L., Eshoul, M., Judek, S. (2012). Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environmental Research, 1117, 100-111.
- Footnote 259
-
Stieb, D. M., Beveridge, R. C., Brook, J. R., Smith-Doiron, M. A. R. C., Burnett, R. T., Dales, R. E., Beaulieu, S., Judek, S., Mamedov, A. (2000). Air pollution, aeroallergens and cardiorespiratory emergency department visits in Saint John, Canada. Journal of Exposure Science and Environmental Epidemiology, 10(5), 461.
- Footnote 260
-
Beckerman, B. S., Jerrett, M., Finkelstein, M., Kanaroglou, P., Brook, J. R., Arain, M. A., Sears, M.R., Stieb, D., Balmes, J., Chapman, K. (2012). The association between chronic exposure to traffic-related air pollution and ischemic heart disease. Journal of Toxicology and Environmental Health, Part A, 75(7), 402-411.
- Footnote 261
-
Brook, R. D., Jerrett, M., Brook, J. R., Bard, R. L., Finkelstein, M. M. (2008). The relationship between diabetes mellitus and traffic-related air pollution. Journal of Occupational and Environmental Medicine, 50(1), 32-38.
- Footnote 262
-
Brook, R. D., Cakmak, S., Turner, M. C., Brook, J. R., Crouse, D. L., Peters, P. A., Van Donkelaar, A., Villeneuve, P.J., Brion, O., Jerrett, M., Martin, R. V. (2013). Long-term fine particulate matter exposure and mortality from diabetes in Canada. Diabetes Care, 36(10), 3313-3320.
- Footnote 263
-
Chen, H., Burnett, R. T., Kwong, J. C., Villeneuve, P. J., Goldberg, M. S., Brook, R. D., van Donkelaar, A., Jerrett, M., Martin, R.V., Brook, J.R., Copes, R. (2013). Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environmental Health Perspectives, 121(7), 804.
- Footnote 264
-
Chen, H., Burnett, R. T., Kwong, J. C., Villeneuve, P. J., Goldberg, M. S., Brook, R. D., van Donkelaar, A., Jerrett, M., Martin, R.V., Kopp, A., Brook, J. R. (2014). Spatial association between ambient fine particulate matter and incident hypertension. Circulation, 129 (5), 562-569.
- Footnote 265
-
Chen, H., Burnett, R. T., Copes, R., Kwong, J. C., Villeneuve, P. J., Goldberg, M. S., Brook, R.D., van Donkelaar, A., Jerrett, M., Martin, R.V., Brook, J. R. (2016). Ambient fine particulate matter and mortality among survivors of myocardial infarction: population-based cohort study. Environmental Health Perspectives, 124(9), 1421.
- Footnote 266
-
Crouse, D. L., Peters, P. A., van Donkelaar, A., Goldberg, M. S., Villeneuve, P. J., Brion, O., Khan, S., Atari, D.O., Jerrett, M., Pope III, C.A., Brauer, M. (2012). Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environmental Health Perspectives, 120(5), 708.
- Footnote 267
-
Crouse, D. L., Peters, P. A., Hystad, P., Brook, J. R., van Donkelaar, A., Martin, R. V., Villeneuve, P.J., Jerrett, M., Goldberg, M.S., Pope III, C.A., Brauer, M. (2015). Ambient PM2. 5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environmental Health Perspectives, 123(11), 1180.
- Footnote 268
-
Crouse, D. L., Peters, P. A., Villeneuve, P. J., Proux, M. O., Shin, H. H., Goldberg, M. S., Johnson, M., Wheeler, A.J., Allen, R.W., Atari, D.O., Jerrett, M. (2015). Within-and between-city contrasts in nitrogen dioxide and mortality in 10 Canadian cities; a subset of the Canadian Census Health and Environment Cohort (CanCHEC). Journal of Exposure Science and Environmental Epidemiology, 25(5), 482.
- Footnote 269
-
Dales, R., Burnett, R. T., Smith-Doiron, M., Stieb, D. M., Brook, J. R. (2004). Air pollution and sudden infant death syndrome. Pediatrics, 113(6), e628-e631.
- Footnote 270
-
Lavigne, E., Yasseen, A. S., Stieb, D. M., Hystad, P., Van Donkelaar, A., Martin, R. V., Brook, J.R., Crouse, D.L., Burnett, R.T., Chen, H., Weichenthal, S. (2016). Ambient air pollution and adverse birth outcomes: Differences by maternal comorbidities. Environmental Research, 148, 457-466.
- Footnote 271
-
Giles L.V., Barn P., Künzli N., Romieu I., Mittleman M.A., van Eeden S., Allen R., Carlsten C., Stieb D., Noonan C., Smargiassi A, Kaufman J.D., Hajat S., Kosatsky T., Brauer M. (2011). From good intentions to proven interventions: effectiveness of actions to reduce the health impacts of air pollution. Environmental Health Perspectives, 119(1), 29.
- Footnote 272
-
Laumbach, R., Meng, Q., Kipen, H. (2015). What can individuals do to reduce personal health risks from air pollution?. Journal of Thoracic Disease, 7(1), 96.
- Footnote 273
-
Böcker, L., Dijst, M., Prillwitz, J. (2013). Impact of everyday weather on individual daily travel behaviours in perspective: a literature review. Transport Reviews, 33(1), 71-91.
- Footnote 274
-
Bopp, M., Gayah, V. V., Campbell, M. E. (2015). Examining the link between public transit use and active commuting. International Journal of Environmental Research and Public Health, 12(4), 4256-4274.
- Footnote 275
-
Chan, C. B., Ryan, D. A. (2009). Assessing the effects of weather conditions on physical activity participation using objective measures. International Journal of Environmental Research and Public Health, 6(10), 2639-2654.
- Footnote 276
-
Dill, J., McNeil, N., Broach, J., Ma, L. (2014). Bicycle boulevards and changes in physical activity and active transportation: Findings from a natural experiment. Preventive Medicine, 69, S74-S78.
- Footnote 277
-
Fishman, E., Böcker, L., Helbich, M. (2015). Adult active transport in the Netherlands: An analysis of its contribution to physical activity requirements. PloS One, 10(4), e0121871.
- Footnote 278
-
Gebhart, K., Noland, R. B. (2014). The impact of weather conditions on bike share trips in Washington, DC. Transportation, 41(6), 1205-1225.
- Footnote 279
-
Miranda-Moreno, L. F., Lahti, A. C. (2013). Temporal trends and the effect of weather on pedestrian volumes: A case study of Montreal, Canada. Transportation Research Part D: Transport and Environment, 22, 54-59.
- Footnote 280
-
Owen, N., Humpel, N., Leslie, E., Bauman, A., Sallis, J. F. (2004). Understanding environmental influences on walking: review and research agenda. American Journal of Preventive Medicine, 27(1), 67-76.
- Footnote 281
-
Tucker, P., Gilliland, J. (2007). The effect of season and weather on physical activity: a systematic review. Public Health, 121(12), 909-922.
- Footnote 282
-
Winters, M., Friesen, M. C., Koehoorn, M., Teschke, K. (2007). Utilitarian bicycling: a multilevel analysis of climate and personal influences. American Journal of Preventive Medicine, 32(1), 52-58.
- Footnote 283
-
Wolff, D., Fitzhugh, E. C. (2011). The relationships between weather-related factors and daily outdoor physical activity counts on an urban greenway. International Journal of Environmental Research and Public Health, 8(2), 579-589.
- Footnote 284
-
Collins, P. A., Mayer, D. (2015). Active transportation in Kingston, Ontario: an analysis of mode, destination, duration, and season among walkers and cyclists. Journal of Physical Activity and Health, 12(Suppl 1), S76-S83.
- Footnote 285
-
Dalton, M. A., Longacre, M. R., Drake, K. M., Gibson, L., Adachi-Mejia, A. M., Swain, K., Xie, H., Owens, P. M. (2011). Built environment predictors of active travel to school among rural adolescents. American Journal of Preventive Medicine, 40(3), 312-319.
- Footnote 286
-
Katapally, T. R., Rainham, D., Muhajarine, N. (2016). A methodology to leverage cross-sectional accelerometry to capture weather's influence in active living research. Canadian Journal of Public Health, 107(1), 30-36.
- Footnote 287
-
Merchant, A. T., Dehghan, M., Akhtar-Danesh, N. (2007). Seasonal variation in leisure time physical activity among Canadians. Canadian Journal of Public Health, 203-208.
- Footnote 288
-
Winters, M., Davidson, G., Kao, D., Teschke, K. (2011). Motivators and deterrents of bicycling: comparing influences on decisions to ride. Transportation, 38(1), 153-168.
- Footnote 289
-
Winters, M., Friesen, M. C., Koehoorn, M., Teschke, K. (2007). Utilitarian bicycling: a multilevel analysis of climate and personal influences. American Journal of Preventive Medicine, 32(1), 52-58.
- Footnote 290
-
Helbich, M., Böcker, L., Dijst, M. (2014). Geographic heterogeneity in cycling under various weather conditions: Evidence from Greater Rotterdam. Journal of Transport Geography, 38, 38-47.
- Footnote 291
-
Witham, M. D., Donnan, P. T., Vadiveloo, T., Sniehotta, F. F., Crombie, I. K., Feng, Z., McMurdo, M. E. (2014). Association of day length and weather conditions with physical activity levels in older community dwelling people. PloS One, 9(1), e85331.
- Footnote 292
-
Goodman, A., Page, A. S., Cooper, A. R. (2014). Daylight saving time as a potential public health intervention: an observational study of evening daylight and objectively-measured physical activity among 23,000 children from 9 countries. International Journal of Behavioral Nutrition & Physical Activity, 11(1), 84.
- Footnote 293
-
Kallio, J., Turpeinen, S., Hakonen, H., Tammelin, T. (2016). Active commuting to school in Finland, the potential for physical activity increase in different seasons. International Journal of Circumpolar Health, 75(1), 33319.
- Footnote 294
-
Reynolds, K.D., Wolch, J., Byrne, J., Chou, C.P., Feng, G., Weaver, S., Jerrett, M. (2007). Trail characteristics as correlates of urban trail use. American Journal of Health Promotion, 21(4_suppl), 335-345.
- Footnote 295
-
Wilson, L.A.M., Giles-Corti, B., Burton, N.W., Giskes, K., Haynes, M., Turrell, G. (2011). The association between objectively measured neighborhood features and walking in middle-aged adults. American Journal of Health Promotion, 25(4), e12-e21.
Healthy food options
- Footnote 296
-
Garriguet, D. (2009). Diet quality in Canada. Health Reports, 20(3), 41.
- Footnote 297
-
Health Canada (2012). Do Canadian adults meet their nutrient requirements through food intake alone? Health Canada.
- Footnote 298
-
Brisbois, T.D., Marsden, S.L., Anderson, G.H., Sievenpiper, J.L. (2014). Estimated intakes and sources of total and added sugars in the Canadian diet. Nutrients, 6(5), 1899-1912.
- Footnote 299
-
Langlois, K., Garriguet, D. (2011). Sugar consumption among Canadians of all ages. Health Reports, 22(3), 23-27.
- Footnote 300
-
Canada's Food Guides (2016).
- Footnote 301
-
Strickland, J.R., Pizzorno, G., Kinghorn, A.M., Evanoff, B.A. (2015). Worksite influences on obesogenic behaviors in low-wage workers in St Louis, Missouri, 2013-2014. Preventing Chronic Disease, 12, epub.
- Footnote 302
-
Linde, J.A., Nygaard, K.E., MacLehose, R.F., Mitchell, N.R., Harnack, L.J., Cousins, J.M., Graham, D.J., Jeffery, R.W. (2012). HealthWorks: results of a multi-component group-randomized worksite environmental intervention trial for weight gain prevention. International Journal of Behavioral Nutrition & Physical Activity, 9, 14.
- Footnote 303
-
Thornton, L.E., Lamb, K.E., Ball, K. (2013). Employment status, residential and workplace food environments: associations with women's eating behaviours. Health and Place, 24, 80-89.
- Footnote 304
-
Backman, D., Gonzaga, G., Sugerman, S., Francis, D., Cook, S. (2011). Effect of fresh fruit availability at worksites on fruit and vegetable consumption of low-wage employees. Journal of Nutrition Education & Behavior, 43(4 Suppl 2), S113-S121.
- Footnote 305
-
Escovvery, C., Kegler, M.C., Alcantara, I., Wilson, M., Glanz, K. (2011). A qualitative examination of the role of small, rural worksites in obesity prevention. Preventing Chronic Disease, 8(4), A75.
- Footnote 306
-
Health Canada (2016). Healthy eating strategy. Health Canada.
- Footnote 307
-
Shoaie, S., Ghaffari, P., Kovatcheva-Datchary, P., Mardinoglu, A., Sen, P., Pujos-Guillot, E., de Wouters, T., Juste, C., Rizkalla, S., Chilloux, J., Hoyles, L. (2015). Quantifying diet-induced metabolic changes of the human gut microbiome. Cell Metabolism, 22(2), 320-331.
- Footnote 308
-
Zeevi, D., Korem, T., Zmora, N., Israeli, D., Rothschild, D., Weinberger, A., Ben-Yacov, O., Lador, D., Avnit-Sagi, T., Lotan-Pompan, M., Suez, J. (2015). Personalized nutrition by prediction of glycemic responses. Cell, 163(5), 1079-1094.
- Footnote 309
-
Celis-Morales, C., Livingstone, K. M., Marsaux, C. F., Macready, A. L., Fallaize, R., O'Donovan, C. B., Woolhead, C., Forster, H., Walsh, M.C., Navas-Carretero, S., San-Cristobal, R. (2017). Effect of personalized nutrition on health-related behaviour change: evidence from the Food4me European randomized controlled trial. International Journal of Epidemiology, 46(2).
- Footnote 310
-
Nielsen, D. E., El-Sohemy, A. (2014). Disclosure of genetic information and change in dietary intake: a randomized controlled trial. PloS One, 9(11), e112665.
- Footnote 311
-
Townshend, T., Lake, A. (2017). Obesogenic environments: current evidence of the built and food environments. Perspectives in Public Health, 137(1), 38-44.
- Footnote 312
-
Lipek, T., Igel, U., Gausche, R., Kiess, W., Grande, G. (2015). Obesogenic environments: environmental approaches to obesity prevention. Journal of Pediatric Endocrinology and Metabolism, 28(5-6), 485-495.
- Footnote 313
-
Caspi, C. E., Sorensen, G., Subramanian, S. V., Kawachi, I. (2012). The local food environment and diet: a systematic review. Health and Place, 18(5), 1172-1187.
- Footnote 314
-
Roberto, C. A., Swinburn, B., Hawkes, C., Huang, T. T., Costa, S. A., Ashe, M., Zwicker, L., Cawley, J.H., Brownell, K. D. (2015). Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. The Lancet, 385(9985), 2400-2409.
- Footnote 315
-
Block, J. P., Subramanian, S. V. (2015). Moving beyond "food deserts": reorienting United States policies to reduce disparities in diet quality. PLoS Medicine, 12(12), e1001914.
- Footnote 316
-
Clary, C., Matthews, S. A., Kestens, Y. (2017). Between exposure, access and use: Reconsidering foodscape influences on dietary behaviours. Health and Place, 44, 1-7.
- Footnote 317
-
Brown, D. R., Brewster, L. G. (2015). The food environment is a complex social network. Social Science and Medicine, 133, 202-204.
- Footnote 318
-
Dubowitz, T., Zenk, S. N., Ghosh-Dastidar, B., Cohen, D. A., Beckman, R., Hunter, G., Steiner, E.D., Collins, R. L. (2015). Healthy food access for urban food desert residents: examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutrition, 18(12), pp.2220-2230.
- Footnote 319
-
Ghosh-Dastidar, B., Cohen, D., Hunter, G., Zenk, S. N., Huang, C., Beckman, R., Dubowitz, T. (2014). Distance to store, food prices, and obesity in urban food deserts. American Journal of Preventive Medicine, 47(5), 587-595.
- Footnote 320
-
Lebel, A., Noreau, D., Tremblay, L., Oberlé, C., Girard-Gadreau, M., Duquay, M., Block, J. P. (2016). Identifying rural food deserts: Methodological considerations for food environment interventions. Canadian Journal of Public Health, 107(1), e521.
- Footnote 321
-
Mejia, N., Lightstone, A. S., Basurto-Davila, R., Morales, D. M., Sturm, R. (2015). Neighborhood Food Environment, Diet, and Obesity Among Los Angeles County Adults, 2011. Preventing Chronic Disease, 12, e143.
- Footnote 322
-
Minaker, L. M., Olstad, D. L., Thompson, M. E., Raine, K. D., Fisher, P., Frank, L. D. (2016). Associations between frequency of food shopping at different store types and diet and weight outcomes: findings from the NEWPATH study. Public Health Nutrition, 19(12), 2268-2277.
- Footnote 323
-
Sadler, R. C., Gilliland, J. A., Arku, G. (2011). An application of the edge effect in measuring accessibility to multiple food retailer types in Southwestern Ontario, Canada. International Journal of Health Geographics, 10(1), 34.
- Footnote 324
-
Glanz, K., Sallis, J.F., Saelens, B.E., Frank, L.D. (2005). Healthy nutrition environments : concepts and measures. American Journal of Health Promotion, 19(5), 330-333
- Footnote 325
-
Health Canada (2013). Measuring the food environment in Canada. Health Canada.
- Footnote 326
-
Cobb, L. K., Appel, L. J., Franco, M., Jones‐Smith, J. C., Nur, A., Anderson, C. (2015). The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity, 23(7), 1331-1344.A.
- Footnote 327
-
Zenk, S.N., Tarlov, E., Wing, C., Matthews, S.A., Jones, K., Tong, H., Powell, L.M. (2017). Geographic accessibility of food outlets not associated with body mass index change among veterans, 2009-2014. Health Affairs, 36(8), 1433.
- Footnote 328
-
Rahman, T., Cushing, R. A., Jackson, R. J. (2011). Contributions of built environment to childhood obesity. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine, 78(1), 49-57.
- Footnote 329
-
Thornton, L. E., Kavanagh, A. M. (2012). Association between fast food purchasing and the local food environment. Nutrition and Diabetes, 2(12), e53.
- Footnote 330
-
Zenk, S. N., Thatcher, E., Reina, M., Odoms-Young, A. (2015). 6 Local Food Environments and Diet-Related Health Outcomes. Local Food Environments: Food Access in America, 167.
- Footnote 331
-
Daniel, M., Paquet, C., Auger, N., Zang, G., Kestens, Y. (2010). Association of fast-food restaurant and fruit and vegetables tore densities with cardiovascular mortality in a metropolitan population. European Journal of Epidemiology, 25(10), 711-719.
- Footnote 332
-
Prince, S. A., Kristjansson, E. A., Russell, K., Billette, J. M., Sawada, M. C., Ali, A.,Tremblay, M.S., Prud'homme, D. (2012). Relationships between neighborhoods, physical activity, and obesity: a multilevel analysis of a large Canadian city. Obesity, 20(10), 2093-2100.
- Footnote 333
-
Minaker, L. M., Raine, K. D., Wild, T. C., Nykiforuk, C. I., Thompson, M. E., Frank, L. D. (2013). Objective food environments and health outcomes. American Journal of Preventive Medicine, 45(3), 289-296.
- Footnote 334
-
Prince, S. A., Kristjansson, E. A., Russell, K., Billette, J. M., Sawada, M., Ali, A.,Tremblay, M.S., Prud'homme, D. (2011). A multilevel analysis of neighbourhood built and social environments and adult self-reported physical activity and body mass index in Ottawa, Canada. International Journal of Environmental Research and Public Health, 8(10), 3953-3978.
- Footnote 335
-
Kruger, D. J., Greenberg, E., Murphy, J. B., DiFazio, L. A., Youra, K. R. (2014). Local concentration of fast-food outlets is associated with poor nutrition and obesity. American Journal of Health Promotion, 28(5), 340-343.
- Footnote 336
-
Fraser, L. K., Edwards, K. L., Cade, J., Clarke, G. P. (2010). The geography of fast food outlets: a review. International Journal of Environmental Research and Public Health, 7(5), 2290-2308.
- Footnote 337
-
Dubowitz, T., Ghosh‐Dastidar, M. B., Steiner, E., Escarce, J. J., Collins, R. L. (2013). Are our actions aligned with our evidence? The skinny on changing the landscape of obesity. Obesity, 21(3), 419-420.
- Footnote 338
-
Chen, D., Jaenicke, E. C., Volpe, R. J. (2016). Food environments and obesity: household diet expenditure versus food deserts. American Journal of Public Health, 106(5), 881-888.
- Footnote 339
-
Widener, M. J., Shannon, J. (2014). When are food deserts? Integrating time into research on food accessibility. Health and Place, 30, 1-3.
- Footnote 340
-
Fitterer, J.L., Nelson, T.A., Stockwell, T. (2015). A review of existing studies reporting the negative effects of alcohol access and positive effects of alcohol control policies on interpersonal violence. Front Public Health, 3, 253.
- Footnote 341
-
Badland, H., Mavoa, S., Linvingston, M., David, S., Giles-Corti, B. (2016). Testing spatial measures of alcohol outlet density with self-rated health in the Australian context: implications for policy and practice. Drug & Alcohol Review, 35(3), 298-306.
- Footnote 342
-
Fone, D., Morgan, J., Fry, R., Rodgers, S., Orford, S., Farewell, D., Dunstan, F., White, J., Sivarajasingam, V., Trefan, L., Brennan, I., Lee, S., Shiode, N., Weightman, A., Webster, C., Lyons, R. (2016). Change in alcohol outlet density and alcohol-related harm to population health (CHALICE): a comprehensive record-linked database study in Wales. NIHB Journal Library.
- Footnote 343
-
Morrison, C., Smith, K., Gruenewald, P.J., Ponicki, W.R., Lee, J.P., Cameron, P. (2015). Relating off-premises alcohol outlet density to intentional and unintentional injuries. Addiction, 111(1), 56-64.
- Footnote 344
-
Morrison, C.N., Dong, B., BRanas, C.C., Richmond, T.S., Wiebe, D.J. (2017). A momentary exposures analysis of proximity to alcohol outlets and risk for assault. Addiction, 112(2), 269-278.
- Footnote 345
-
Snowden, A.J. (2016). Alcohol outlet density and intimate partner violence in a nonmetropolitan college town: accounting for neighborhood characteristics and alcohol outlet types. Violence & Victims, 31(1), 111-123.
- Footnote 346
-
Ahem, J., Balzer, L., Galea, S. (2015). The roles of outlet density and norms in alcohol use disorder. Drug & Alcohol Dependence, 151, 144-150.
- Footnote 347
-
Bryden, A. Roberts, B., McKee, M., Petticrew, M. (2012). A systematic review of the influence on alcohol use of community level availability and marketing of alcohol, Health and Place, 18(2), 349-357.
- Footnote 348
-
Stockwell, T., Zhao, J., Martin, G., Macdonald, S., Vallance, K., Treno, A., Ponicki, W., Tu, A., Buxton, J. (2013). Minimum alcohol prices and outlet densities in British Columbia, Canada: estimated impacts on alcohol-attributable hospital admissions. American Journal of Public Health, 103(11), 2014-2020.
- Footnote 349
-
Pereira, G., Wood, L., Foster, S., Haggar, F. (2013). Access to alcohol outlets, alcohol consumption and mental health. PLoS One, 8(1), e53461.
- Footnote 350
-
Popova, S., Giesbrecht, N., Bekmuradov, D., Patra, J. (2009). Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol & Alcoholism, 44(5), 500-516.
- Footnote 351
-
Treno, A.J., Ponicki, W.R., Stockwell, T., Macdonald, S., Gruenewald, P.J., Zhao, J., Martin, G., Greer, A. (2013). Alcohol outlet densities and alcohol price: the British Columbia experiment in the partial privatization of alcohol sales off-premise. Alcoholism: Clinical & Experimental Research, 37(5), 854-859.
- Footnote 352
-
Gilliland, J. A., Rangel, C. Y., Healy, M. A., Tucker, P., Loebach, J. E., Hess, P. M., He, M., Irwin, J.D., Wilk, P. (2012). Linking childhood obesity to the built environment: a multi-level analysis of home and school neighbourhood factors associated with body mass index. Canadian Journal of Public Health, 103(9), 15-21.
- Footnote 353
-
Hollands, S., Campbell, M. K., Gilliland, J., Sarma, S. (2013). A spatial analysis of the association between restaurant density and body mass index in Canadian adults. Preventive Medicine, 57(4), 258-264.
- Footnote 354
-
Hollands, S., Campbell, M. K., Gilliland, J., Sarma, S. (2014). Association between neighbourhood fast-food and full-service restaurant density and body mass index: a cross-sectional study of Canadian adults. Canadian Journal of Public Health, 105(3), 172-178.
- Footnote 355
-
Polsky, J.Y, Moineddin R., Glazier, R. H., Dunn J.R., Booth, G. L. (2016). Relative and absolute availability of fast-food restaurants in relation to the development of diabetes: A population-based cohort study. Canadian Journal of Public Health, 107(1), e527.
- Footnote 356
-
Polsky, J. Y., Moineddin, R., Dunn, J. R., Glazier, R. H., Booth, G. L. (2016). Absolute and relative densities of fast-food versus other restaurants in relation to weight status: Does restaurant mix matter? Preventive Medicine, 82, 28-34.
- Footnote 357
-
Boone-Heinonen, J., Gordon-Larsen, P., Kiefe, C. I., Shikany, J. M., Lewis, C. E., Popkin, B. M. (2011). Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Archives of Internal Medicine, 171(13), 1162-1170.
- Footnote 358
-
Hager, E. R., Cockerham, A., O'Reilly, N., Harrington, D., Harding, J., Hurley, K. M., Black, M. M. (2016). Food swamps and food deserts in Baltimore City, MD, USA: associations with dietary behaviours among urban adolescent girls. Public Health Nutrition, 1-10.
- Footnote 359
-
Hollands, S., Campbell, M. K., Gilliland, J., Sarma, S. (2014). Association between neighbourhood fast-food and full-service restaurant density and body mass index: a cross-sectional study of Canadian adults. Canadian Journal of Public Health, 105(3), 172-178.
- Footnote 360
-
Mezuk, B., Li, X., Cederin, K., Rice, K., Sundquist, J., Sundquist, K. (2016). Beyond Access: Characteristics of the Food Environment and Risk of Diabetes. American Journal of Epidemiology, 183(12), 1129-1137.
- Footnote 361
-
Minaker, L. M., Raine, K. D., Wild, T. C., Nykiforuk, C. I., Thompson, M. E., Frank, L. D. (2013). Objective food environments and health outcomes. American Journal of Preventive Medicine, 45(3), 289-296.
- Footnote 362
-
Luan, H., Law, J., Quick, M. (2015). Identifying food deserts and swamps based on relative healthy food access: a spatio-temporal Bayesian approach. International Journal of Health Geographics, 14(1), 37.
- Footnote 363
-
Centers for Disease Control and Prevention (2010). Healthy Places: Zoning. Centers for Disease Control and Prevention.
- Footnote 364
-
Raine, K. D., Muhajarine, N., Spence, J. C., Neary, N. E., Nykiforuk, C. I. (2012). Coming to consensus on policy to create supportive built environments and community design. Canadian Journal of Public Health, 103(Suppl 3), S5-S8.
- Footnote 365
-
Quebec en Forme (2012). Modifying the built environment to promote healthy eating among youth. Highlights of Research, 2011-2012.
- Footnote 366
-
Mayo, M. L., Pitts, S. B. J., Chriqui, J. F. (2013). Associations between county and municipality zoning ordinances and access to fruit and vegetable outlets in rural North Carolina, 2012. Preventing Chronic Disease, 10, e203.
- Footnote 367
-
McCormack, L. A., Laska, M. N., Larson, N. I., Story, M. (2010). Review of the nutritional implications of farmers' markets and community gardens: a call for evaluation and research efforts. Journal of the American Dietetic Association, 110(3), 399-408.
- Footnote 368
-
Jilcott Pitts, S. B., Wu, Q., Demarest, C. L., Dixon, C. E., Dortche, C. J., Bullock, S. L., McGuirt, J., Ward, R., Ammerman, A. S. (2015). Farmers' market shopping and dietary behaviours among Supplemental Nutrition Assistance Program participants. Public Health Nutrition, 18(13), 2407-2414.
- Footnote 369
-
Leone, L. A., Beth, D., Ickes, S. B., MacGuire, K., Nelson, E., Smith, R. A., Tate, D.F., Ammerman, A. S. (2012). Attitudes toward fruit and vegetable consumption and farmers' market usage among low-income North Carolinians. Journal of Hunger and Environmental Nutrition, 7(1), 64-76.
- Footnote 370
-
McGuirt, J. T., Pitts, S. B. J., Ward, R., Crawford, T. W., Keyserling, T. C., Ammerman, A. S. (2014). Examining the influence of price and accessibility on willingness to shop at farmers' markets among low-income eastern North Carolina women. Journal of Nutrition Education and Behavior, 46(1), 26-33.
- Footnote 371
-
Wang, H., Qiu, F., Swallow, B. (2014). Can community gardens and farmers' markets relieve food desert problems? A study of Edmonton, Canada. Applied Geography, 55, 127-137.
- Footnote 372
-
Bowling, A. B., Moretti, M., Ringelheim, K., Tran, A., Davison, K. (2016). Healthy Foods, Healthy Families: combining incentives and exposure interventions at urban farmers' markets to improve nutrition among recipients of US federal food assistance. Health Promotion Perspectives, 6(1), 10.
- Footnote 373
-
Jilcott Pitts, S. B., Wu, Q., McGuirt, J. T., Crawford, T. W., Keyserling, T. C., Ammerman, A. S. (2013). Associations between access to farmers' markets and supermarkets, shopping patterns, fruit and vegetable consumption and health indicators among women of reproductive age in eastern North Carolina, USA. Public Health Nutrition, 16(11), 1944-1952.
- Footnote 374
-
Jilcott Pitts, S. B., Gustafson, A., Wu, Q., Mayo, M. L., Ward, R. K., McGuirt, J. T., Rafferty, A.P., Lancaster, M.F., Evenson, K.R., Keyserling, T.C., Ammerman, A. S. (2014). Farmers' market use is associated with fruit and vegetable consumption in diverse southern rural communities. Nutrition Journal, 13(1), 1.
- Footnote 375
-
Jilcott Pitts, S. B., Acheson, M. L. M., Ward, R. K., Wu, Q., McGuirt, J. T., Bullock, S. L., Lancaster, M.F., Raines, J., Ammerman, A. S. (2015). Disparities in healthy food zoning, farmers' market availability, and fruit and vegetable consumption among North Carolina residents. Archives of Public Health, 73(1), 35.
- Footnote 376
-
Jilcott Pitts, S. B., Hinkley, J., Wu, Q., McGuirt, J. T., Lyonnais, M. J., Rafferty, A. P., Whitt, O.R., Winterbauer, N., Phillips, L. (2017). A possible dose–response association between distance to farmers' markets and roadside produce stands, frequency of shopping, fruit and vegetable consumption, and body mass index among customers in the Southern United States. BMC Public Health, 17(1), 65.
- Footnote 377
-
Payne, G. H., Wethington, H., Olsho, L., Jernigan, J., Farris, R., Walker, D. K. (2013). Implementing a Farmers' Market Incentive Program: Perspectives on the New York City Health Bucks Program. Preventing Chronic Disease, 10, e145.
- Footnote 378
-
Robles, B., Montes, C. E., Nobari, T. Z., Wang, M. C., Kuo, T. (2017). Dietary Behaviors among Public Health Center Clients with Electronic Benefit Transfer Access at Farmers' Markets. Journal of the Academy of Nutrition and Dietetics, 117(1), 58-68.
- Footnote 379
-
Lucan, S. C., Maroko, A. R., Sanon, O., Frias, R., Schechter, C. B. (2015). Urban farmers' markets: Accessibility, offerings, and produce variety, quality, and price compared to nearby stores. Appetite, 90, 23-30.
- Footnote 380
-
Alaimo, K., Beavers, A. W., Crawford, C., Snyder, E. H., Litt, J. S. (2016). Amplifying health through community gardens: A framework for advancing multicomponent, behaviorally based neighborhood interventions. Current Environmental Health Reports, 3(3), 302-312.
- Footnote 381
-
Alaimo, K., Packnett, E., Miles, R.A., Kruger, D.J. (2008). Fruit and vegetable intake among urban community gardeners. Journal of Nutrition Education & Behavior, 40(2), 94-101.
- Footnote 382
-
Barnidge, E. K., Baker, E. A., Schootman, M., Motton, F., Sawicki, M., Rose, F. (2015). The effect of education plus access on perceived fruit and vegetable consumption in a rural African American community intervention. Health Education Research, 30(5), 773-785.
- Footnote 383
-
Carney, P. A., Hamada, J. L., Rdesinski, R., Sprager, L., Nichols, K. R., Liu, B. Y., Pelayo, J., Sanchez, M.A., Shannon, J. (2012). Impact of a community gardening project on vegetable intake, food security and family relationships: a community-based participatory research study. Journal of Community Health, 37(4), 874-881.
- Footnote 384
-
Castro, D. C., Samuels, M., Harman, A. E. (2013). Growing healthy kids: a community garden–based obesity prevention program. American Journal of Preventive Medicine, 44(3), S193-S199.
- Footnote 385
-
Egli, V., Oliver, M., Tautolo, E. S. (2016). The development of a model of community garden benefits to wellbeing. Preventive Medicine Reports, 3, 348-352.
- Footnote 386
-
Litt, J. S., Soobader, M. J., Turbin, M. S., Hale, J. W., Buchenau, M., Marshall, J. A. (2011). The influence of social involvement, neighborhood aesthetics, and community garden participation on fruit and vegetable consumption. American Journal of Public Health, 101(8), 1466-1473.
- Footnote 387
-
Soga, M., Gaston, K. J., Yamaura, Y. (2016). Gardening is beneficial for health: A meta-analysis. Preventive Medicine Reports. 5, 92-99.
- Footnote 388
-
Alaimo, K., Reischl, T.M., Allen, J.O. (2010). Community gardening, neighborhood meetings, and social capital. Journal of Community Psychology, 38(4), 497-514.
- Footnote 389
-
Teig, E., Amulya, J., Bardwell, L., Buchenau, M., Marshall, J.A., Litt, J.S. (2009). Collective efficacy in Denver, Colorado: Strengthening neighborhoods and health through community gardens. Health and Place, 15(4), 1155-1122.
- Footnote 390
-
Statistics Canada. Table 326-0012: Average retail prices for food and other selected items (monthly (dollars)). Statistics Canada.
- Footnote 391
-
Statistics Canada (2014). The changing face of the Canadian fruit and vegetable sector: 1941 to 2011. Statistics Canada.
- Footnote 392
-
Statistics Canada (2017). Fruit and vegetable production, 2016. Statistics Canada.
- Footnote 393
-
Tarasuk, V. (2010). Policy directions to promote healthy dietary patterns in Canada. Applied Physiology Nutrition & Metabolism, 35, 229-233.
- Footnote 394
-
Tarasuk, V., Mitchell, A., Dachner, N. (2014). Household food insecurity in Canada, 2014. PROOF: Food insecurity policy research.
- Footnote 395
-
Food and Agriculture Organization of the United Nations. (2017). Food security statistics. Food and Agriculture Organization of the United Nations.
- Footnote 396
-
Carter, M. A., Dubois, L., Tremblay, M. S. (2014). Place and food insecurity: a critical review and synthesis of the literature. Public Health Nutrition, 17(1), 94-112.
- Footnote 397
-
Kirkpatrick, S. I., Tarasuk, V. (2010). Assessing the relevance of neighbourhood characteristics to the household food security of low-income Toronto families. Public Health Nutrition, 13(7), 1139-1148.
- Footnote 398
-
Guo, Y., Berrang-Ford, L., Ford, J., Lardeau, M. P., Edge, V., Patterson, K., IHACC Research Team, Harper, S. L. (2015). Seasonal prevalence and determinants of food insecurity in Iqaluit, Nunavut. International Journal of Circumpolar Health, 74(1), 27284.
- Footnote 399
-
Collings, P., Marten, M. G., Pearce, T., Young, A. G. (2016). Country food sharing networks, household structure, and implications for understanding food insecurity in Arctic Canada. Ecology of Food and Nutrition, 55(1), 30-49.
- Footnote 400
-
Skinner, K., Hanning, R. M., Metatawabin, J., Tsuji, L. J. (2014). Implementation of a community greenhouse in a remote, sub-Arctic First Nations community in Ontario, Canada: a descriptive case study. Rural and Remote Health, 14(2), 2545.
Supportive environments
- Footnote 401
-
Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan III, C. A., Charney, D., Southwick, S. (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont), 4(5), 35-40.
- Footnote 402
-
Reblin, M., Uchino, B. N. (2008). Social and emotional support and its implication for health. Current Opinion in Psychiatry, 21(2), 201.
- Footnote 403
-
Uchino, B. N. (2006). Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377-387.
- Footnote 404
-
Sinha, M. (2015). Canadians' connections with family and friends. Statistics Canada.
- Footnote 405
-
Turcotte, M. (2015). Trends in social capital in Canada. Statistics Canada.
- Footnote 406
-
Cacioppo, J. T., Cacioppo, S., Capitanio, J. P., Cole, S. W. (2015). The neuroendocrinology of social isolation. Annual Review of Psychology, 66, 733-767.
- Footnote 407
-
Cacioppo, J. T., Cacioppo, S., Cole, S. W., Capitanio, J. P., Goossens, L., Boomsma, D. I. (2015). Loneliness across phylogeny and a call for comparative studies and animal models. Perspectives on Psychological Science, 10(2), 202-212.
- Footnote 408
-
Hawkley, L. C., Capitanio, J. P. (2015). Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Philosophical Transactions of the Royal Society of London: Series B, Biological Sciences, 370(1669).
- Footnote 409
-
Masi, C. M., Chen, H. Y., Hawkley, L. C., Cacioppo, J. T. (2011). A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review, 15(3), 219-266.
- Footnote 410
-
Shields, M. (2008). Community belonging and self-perceived health. Statistics Canada: Catalogue no. 82-003-X Health Reports.
- Footnote 411
-
Statistics Canada (2002). Community belonging and health. Statistics Canada.
- Footnote 412
-
Statistics Canada. Table 105-0501 - Health indicator profile, annual estimates, by age group and sex, Canada, provinces, territories, health regions (2013 boundaries) and peer groups, occasional. Statistics Canada.
- Footnote 413
-
Brosschot, J. F., Gerin, W., Thayer, J. F. (2006). The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research, 60(2), 113-124.
- Footnote 414
-
Glaser, R., Kiecolt-Glaser, J. K. (2005). Stress-induced immune dysfunction: implications for health. Nature Reviews Immunology, 5(3), 243-251.
- Footnote 415
-
Juster, R. P., McEwen, B. S., Lupien, S. J. (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews, 35(1), 2-16.
- Footnote 416
-
Marin, M. F., Lord, C., Andrews, J., Juster, R. P., Sindi, S., Arsenault-Lapierre, G., Fiocco, A.J., Lupien, S. J. (2011). Chronic stress, cognitive functioning and mental health. Neurobiology of Learning and Memory, 96(4), 583-595.
- Footnote 417
-
Qualter, P., Vanhalst, J., Harris, R., Van Roekel, E., Lodder, G., Bangee, M., Maes, M., Verhagen, M. (2015). Loneliness across the life span. Perspectives on Psychological Science, 10(2), 250-264.
- Footnote 418
-
Child, S. T., Schoffman, D. E., Kaczynski, A. T., Forthofer, M., Wilcox, S., Baruth, M. (2016). Neighborhood attributes associated with the social environment. American Journal of Health Promotion, 30(8), 634-637.
- Footnote 419
-
Wood, L., Frank, L. D., Giles-Corti, B. (2010). Sense of community and its relationship with walking and neighborhood design. Social Science and Medicine, 70(9), 1381-1390.
- Footnote 420
-
Brown, S.C., Mason, C.A., Lombard, J.L., Martinez, F., Plater-Zyberk, E., Spokane, A.R., Newman, F.L., Pantin, H., Szapocznik, J. (2009). The relationships of built environment to perceived social support and psychological distress in Hispanic elders: the role of "eyes on the street". Journal of Gerontology: series B Psychological Sciences & Social Sciences, 64B(2), 234-246.
- Footnote 421
-
Brown, B. B., Cropper, V. L. (2001). New urban and standard suburban subdivisions: Evaluating psychological and social goals. Journal of the American Planning Association, 67(4), 402-419.
- Footnote 422
-
Cabrera, J.F. (2013). New urbanism and selection bias in the formation of social capital. Housing Policy Debate, 23(2), 376-394.
- Footnote 423
-
Cabrera, J. F., Najarian, J. C. (2015). How the built environment shapes spatial bridging ties and social capital. Environment and Behavior, 47(3), 239-267.
- Footnote 424
-
Hassen, N., Kaufman, P. (2016). Examining the role of urban street design in enhancing community engagement: A literature review. Health and Place, 41, 119-132.
- Footnote 425
-
Kim, J., Kaplan, R. (2004). Physical and psychological factors in sense of community: New urbanist Kentlands and nearby Orchard Village. Environment and Behavior, 36(3), 313-340.
- Footnote 426
-
Mazumdar, S., Learnihan, V., Cochrane, T., Davey, R. (2017). The Built Environment and Social Capital: A Systematic Review. Environment and Behavior.
- Footnote 427
-
Leyden, K. M. (2003). Social capital and the built environment: the importance of walkable neighborhoods. American Journal of Public Health, 93(9), 1546-1551.
- Footnote 428
-
Lund, H. (2002). Pedestrian environments and sense of community. Journal of Planning Education and Research, 21(3), 301-312.
- Footnote 429
-
Mazumdar, S., Learnihan, V., Cochrane, T., Davey, R. (2017). The Built Environment and Social Capital: A Systematic Review. Environment and Behavior.
- Footnote 430
-
Podobnik 2002; Podobnik, B. 2002. New urbanism and the generation of social capital: Evidence from Orenco station. National Civic Review, 91(3), 245–255.
- Footnote 431
-
Rogers, G. O., Sukolratanametee, S. (2009). Neighborhood design and sense of community: Comparing suburban neighborhoods in Houston Texas. Landscape and Urban Planning, 92(3), 325-334.
- Footnote 432
-
Torres, A., Sarmiento, O. L., Stauber, C., Zarama, R. (2013). The Ciclovia and Cicloruta programs: promising interventions to promote physical activity and social capital in Bogotá, Colombia. American Journal of Public Health, 103(2), e23-e30.
- Footnote 433
-
Wilkerson, A., Carlson, N. E., Yen, I. H., Michael, Y. L. (2012). Neighborhood physical features and relationships with neighbors: does positive physical environment increase neighborliness?. Environment and Behavior, 44(5), 595-615.
- Footnote 434
-
Audirac, I. (1999). Stated preference for pedestrian proximity: an assessment of new urbanist sense of community. Journal of Planning Education and Research, 19(1), 53-66.
- Footnote 435
-
Grant, J., Perrott, K. (2009). Producing diversity in a new urbanism community: Policy and practice. Town Planning Review, 80(3), 267-289.
- Footnote 436
-
Talen, E. (1999). Sense of community and neighbourhood form: An assessment of the social doctrine of new urbanism. Urban Studies, 36(8), 1361-1379.
- Footnote 437
-
Talen, E. (2005). Land use zoning and human diversity: Exploring the connection. Journal of Urban Planning and Development, 131(4), 214-232.
- Footnote 438
-
Talen, E. (2010). Affordability in new urbanist development: Principle, practice, and strategy. Journal of Urban Affairs, 32(4), 489-510.
- Footnote 439
-
Tu, C. C., Eppli, M. J. (1999). Valuing new urbanism: The case of Kentlands. Real Estate Economics, 27(3), 425-451.
- Footnote 440
-
Tu, C. C., Eppli, M. J. (2001). An empirical examination of traditional neighborhood development. Real Estate Economics, 29(3), 485-501.
- Footnote 441
-
Dreger, S., Buck, C., Bolte, G. (2014). Material, psychosocial and sociodemographic determinants are associated with positive mental health in Europe: a cross-sectional study. BMJ Open, 4(5), e005095.
- Footnote 442
-
Evans, G. W. (2003). The built environment and mental health. Journal of Urban Health, 80(4), 536-555.
- Footnote 443
-
Francis, J., Wood, L. J., Knuiman, M., Giles-Corti, B. (2012). Quality or quantity? Exploring the relationship between Public Open Space attributes and mental health in Perth, Western Australia. Social Science and Medicine, 74(10), 1570-1577.
- Footnote 444
-
Guite, H. F., Clark, C., Ackrill, G. (2006). The impact of the physical and urban environment on mental well-being. Public Health, 120(12), 1117-1126.
- Footnote 445
-
Mair, C. F., Roux, A. V. D., Galea, S. (2008). Are neighborhood characteristics associated with depressive symptoms? A critical review. Journal of Epidemiology and Community Health, 62(11), 940-946.
- Footnote 446
-
Roe, J. J., Thompson, C. W., Aspinall, P. A., Brewer, M. J., Duff, E. I., Miller, D., Mitchell, R. Clow, A. (2013). Green space and stress: evidence from cortisol measures in deprived urban communities. International Journal of Environmental Research and Public Health, 10(9), 4086-4103.
- Footnote 447
-
Sugiyama, T., Leslie, E., Giles-Corti, B., Owen, N. (2008). Associations of neighbourhood greenness with physical and mental health: do walking, social coherence and local social interaction explain the relationships?. Journal of Epidemiology and Community Health, 62(5), e9.
- Footnote 448
-
Gariepy, G., Kaufman, J. S., Blair, A., Kestens, Y., Schmitz, N. (2015). Place and health in diabetes: the neighbourhood environment and risk of depression in adults with Type 2 diabetes. Diabetic Medicine, 32(7), 944-950.
- Footnote 449
-
Gariepy, G., Thombs, B. D., Kestens, Y., Kaufman, J. S., Blair, A., Schmitz, N. (2015). The neighbourhood built environment and trajectories of depression symptom episodes in adults: A latent class growth analysis. PloS One, 10(7), e0133603.
- Footnote 450
-
Gariepy, G., Blair, A., Kestens, Y., Schmitz, N. (2014). Neighbourhood characteristics and 10-year risk of depression in Canadian adults with and without a chronic illness. Health and Place, 30, 279-286.
- Footnote 451
-
Statistics Canada (2011). Commuting to work. NHS in Brief. Statistics Canada.
- Footnote 452
-
Cassidy, T. (1992). Commuting-relating stress: consequences and implications. Employee Counselling Today, 4(2), 15-21.
- Footnote 453
-
Costa, G., Pickup, L., Di Martino, V. (1988). Commuting – a further stress factor for working people : evidence from the European community. I. A review. International Archives of Occupational and Environmental Health, 60(5), 371-376.
- Footnote 454
-
Costa, G., Pickup, L., Di Martino, V. (1988). Commuting – a further stress factor for working people : evidence from the European Community. II. An empirical study. International Archives of Occupational and Environmental Health, 60(5), 377-385.
- Footnote 455
-
Evans, G.W., Wener, R.E., Phillips, D. (2002). The morning rush hour: predictability and commuter stress. Environment and Behavior, 34(4).
- Footnote 456
-
Gottholmseder, G., Nowotny, K., Pruckner, G.J., Theurl, E. (2008). Stress perception and commuting. Health Economics, 18(5), 559-576.
- Footnote 457
-
Lucas, J.L., Heady, R.B. (2002). Flextime commuters and their driver stress, feelings of time urgency, and commute satisfaction. Journal of Business and Psychology, 16(4), 565-571.
- Footnote 458
-
Milner, A., Badland, H., Kavanagh, A., LaMontagne, A.D. (2017). Time spent commuting to work and mental health: evidence from 13 waves of an Australian cohort study. American Journal of Epidemiology, 27, 1-9.
- Footnote 459
-
Novaco, R.W., Stokols, D., Campbell, J., Stokols, J. (1979). Transportation, stress and community psychology. American Journal of Community Psychology, 7(4), 361-380.
- Footnote 460
-
Novaco, R.W., Stokols, D., Milanesi, L. (1990). Objective and subjective dimensions of travel impedance as determinants of commuting stress. American Journal of Community Psychology, 18(2), 231-257.
- Footnote 461
-
Schaeffer, M.H., Street, S.W., Singer, J.E., Baum, A. (1988). Effects of control on the stress reaction of commuters. Journal of Applied Social Psychology, 18(11), 944-957.
- Footnote 462
-
Cantwell, M., Caulfield, B., O'Mahony, M. (2009). Examining the factors that impact public transport commuting satisfaction. Journal of Public Transportation, 12(2).
- Footnote 463
-
Lundberg, U. (2010). Urban commuting : crowdedness and catecholamine excretion. Journal of Human Stress, 2(3), 26-32.
- Footnote 464
-
Wener, R., Evans, G., Boately, P. (2014). Commuting stress: psychophysiological effects of a trip and spillover into the workplace. Transportation Research Record, 1924.
- Footnote 465
-
Wener, R.E., Evans, G.W., Phillips, D., Nadler, N. (2003). Running for the 7:45: the effects of public transit improvements on commuter stress. Transportation, 30(2), 203-220.
- Footnote 466
-
Olsson, L.E., Garling, T., Ettema, D., Friman, M., Fujii, S. (2013). Happiness and satisfaction with work commute. Social Indicators Research, 111(1), 255-263.
- Footnote 467
-
Van Hooff, M.L. (2015). The daily commute from work to home: examining employees' experiences in relation to their recovery status. Stress Health, 31(2), 124-137.
- Footnote 468
-
Gascon, M., Triguero-Mas, M., Martínez, D., Dadvand, P., Rojas-Rueda, D., Plasència, A., Nieuwenhuijsen, M. J. (2016). Residential green spaces and mortality: a systematic review. Environment International, 86, 60-67.
- Footnote 469
-
Kabisch, N., Qureshi, S., Haase, D. (2015). Human–environment interactions in urban green spaces—A systematic review of contemporary issues and prospects for future research. Environmental Impact Assessment Review, 50, 25-34.
- Footnote 470
-
Maas, J., Verheij, R. A., de Vries, S., Spreeuwenberg, P., Schellevis, F. G., Groenewegen, P. P. (2008). Morbidity is related to a green living environment. Journal of Epidemiology and Community Health, 63(12), 967-973.
- Footnote 471
-
Van den Berg, A. E., Maas, J., Verheij, R. A., Groenewegen, P. P. (2010). Green space as a buffer between stressful life events and health. Social Science and Medicine, 70(8), 1203-1210.
- Footnote 472
-
van den Berg, M., Wendel-Vos, W., van Poppel, M., Kemper, H., van Mechelen, W., Maas, J. (2015). Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban Forestry and Urban Greening, 14(4), 806-816.
- Footnote 473
-
Villeneuve, P. J., Jerrett, M., Su, J. G., Burnett, R. T., Chen, H., Wheeler, A. J., Goldberg, M. S. (2012). A cohort study relating urban green space with mortality in Ontario, Canada. Environmental Research, 115, 51-58.
- Footnote 474
-
Dadvand, P., de Nazelle, A., Triguero-Mas, M., Schembari, A., Cirach, M., Amoly, E., Figueras, F., Basagaña, X., Ostro, B., Nieuwenhuijsen, M. (2012). Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environmental Health Perspectives, 120(9), 1286.
- Footnote 475
-
Demoury, C., Thierry, B., Richard, H., Sigler, B., Kestens, Y., Parent, M. E. (2017). Residential greenness and risk of prostate cancer: A case-control study in Montreal, Canada. Environment International, 98, 129-136.
- Footnote 476
-
Hystad, P., Davies, H. W., Frank, L., Van Loon, J., Gehring, U., Tamburic, L., Brauer, M. (2014). Residential greenness and birth outcomes: evaluating the influence of spatially correlated built-environment factors. Environmental Health Perspectives, 122(10), 1095.
- Footnote 477
-
Laurent, O., Wu, J., Li, L., Milesi, C. (2013). Green spaces and pregnancy outcomes in Southern California. Health and Place, 24, 190-195.
- Footnote 478
-
Markevych, I., Thiering, E., Fuertes, E., Sugiri, D., Berdel, D., Koletzko, S., von Berg, A., Bauer, C.P., Heinrich, J. (2014). A cross-sectional analysis of the effects of residential greenness on blood pressure in 10-year old children: results from the GINIplus and LISAplus studies. BMC Public Health, 14(1), 477.
- Footnote 479
-
Markevych, I., Fuertes, E., Tiesler, C. M., Birk, M., Bauer, C. P., Koletzko, S., von Berg, A., Berdel, D., Heinrich, J. (2014). Surrounding greenness and birth weight: results from the GINIplus and LISAplus birth cohorts in Munich. Health and Place, 26, 39-46.
- Footnote 480
-
McMorris, O., Villeneuve, P. J., Su, J., Jerrett, M. (2015). Urban greenness and physical activity in a national survey of Canadians. Environmental Research, 137, 94-100.
- Footnote 481
-
Pereira, G., Foster, S., Martin, K., Christian, H., Boruff, B. J., Knuiman, M., Giles-Corti, B. (2012). The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health, 12, 466.
- Footnote 482
-
Bell, S. L., Phoenix, C., Lovell, R., Wheeler, B. W. (2014). Green space, health and wellbeing: Making space for individual agency. Health and Place, 30, 287-292.
- Footnote 483
-
Maas, J., van Dillen, S.M.E., Verheij, R.A., Groenewegen, P.P. (2009). Social contacts as a possible mechanism behind the relation between green space and health. Health and Place, 15(2), 586-595.
- Footnote 484
-
Astell-Burt, T., Mitchell, R., Hartig, T. (2014). The association between green space and mental health varies across the lifecourse. A longitudinal study. Journal of Epidemiology and Community Health, 68(6), 578-583.
- Footnote 485
-
Organisation mondiale de la Santé (2011). Burden of disease from environmental noise. Organisation mondiale de la Santé, Bureau régional de l'Europe.
- Footnote 486
-
Clark, C., Crombie, R., Head, J., Van Kamp, I., Van Kempen, E., Stansfeld, S. A. (2012). Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children's health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. American Journal of Epidemiology, 176(4), 327-337.
- Footnote 487
-
Hammer, M. S., Swinburn, T. K., Neitzel, R. L. (2014). Environmental noise pollution in the United States: developing an effective public health response. Environmental Health Perspectives, 122(2), 115.
- Footnote 488
-
Holzman, D.C. (2014). Fighting noise pollution: a public health strategy. Environmental Health Perspectives, 122(2), A58.
- Footnote 489
-
Stansfeld, S.A., Matheson, M.P. (2003). Noise pollution: non-auditory effects on health. British Medical Bulletin, 68, 243-257.
- Footnote 490
-
Tétreault, L. F., Perron, S., Smargiassi, A. (2013). Cardiovascular health, traffic-related air pollution and noise: are associations mutually confounded? A systematic review. International Journal of Public Health, 58(5), 649-666.
- Footnote 491
-
Vienneau, D., Perez, L., Schindler, C., Lieb, C., Sommer, H., Probst-Hensch, N., Künzli, N., Röösli, M. (2015). Years of life lost and morbidity cases attributable to transportation noise and air pollution: A comparative health risk assessment for Switzerland in 2010. International Journal of Hygiene and Environmental Health, 218(6), 514-521.
- Footnote 492
-
Nanda, U., Eisen, S., Zadeh, R. S., Owen, D. (2011). Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. Journal of Psychiatric and Mental Health Nursing, 18(5), 386-393.
- Footnote 493
-
Nanda, U., Chanaud, C., Nelson, M., Zhu, X., Bajema, R., Jansen, B. H. (2012). Impact of visual art on patient behavior in the emergency department waiting room. The Journal of Emergency Medicine, 43(1), 172-181.
- Footnote 494
-
Nanda, U., Pati, D., McCurry, K. (2009). Neuroesthetics and healthcare design. HERD: Health Environments Research and Design Journal, 2(2), 116-133.
- Footnote 495
-
Clift, S. (2012). Creative arts as a public health resource: moving from practice-based research to evidence-based practice. Perspectives in Public Health, 132(3), 120-127.
- Footnote 496
-
Cameron, M., Crane, N., Ings, R., Taylor, K. (2013). Promoting well-being through creativity: how arts and public health can learn from each other. Perspectives in Public Health, 133(1), 52-59.
- Footnote 497
-
Mohatt, N. V., Singer, J. B., Evans, A. C., Matlin, S. L., Golden, J., Harris, C., Burns, J., Siciliano, C., Kiernan, G., Pelleritti, M., Tebes, J. K. (2013). A community's response to suicide through public art: Stakeholder perspectives from the Finding the Light Within project. American Journal of Community Psychology, 52(1-2), 197-209.
- Footnote 498
-
Mohatt, N. V., Hunter, B. A., Matlin, S. L., Golden, J., Evans, A. C., Tebes, J. K. (2015). From recovery-oriented care to public health: Case studies of participatory public art as a pathway to wellness for persons with behavioral health challenges. Journal of Psychosocial Rehabilitation and Mental Health, 2(1), 9-18.
- Footnote 499
-
Semenza, J. C. (2003). The intersection of urban planning, art and public health : the Sunnyside Piazza. AJPH, 93(9), 1439-1441.
- Footnote 500
-
Dempsey, N. (2008). Quality of the built environment in urban neighbourhoods. Planning, Practice and Research, 23(2), 249-264.
- Footnote 501
-
Ivey, S. L., Kealey, M., Kurtovich, E., Hunter, R. H., Prohaska, T. R., Bayles, C. M., Satariano, W. A. (2015). Neighborhood characteristics and depressive symptoms in an older population. Aging and Mental Health, 19(8), 713-722.
- Footnote 502
-
Stafford, M., Chandola T., Marmot M. (2007). Association between fear of crime and mental health and physical functioning. American Journal of Public Health, 97 (11), 2076-2018.
- Footnote 503
-
Foster, S., Hooper, P., Knuiman, M., Giles-Corti, B. (2016). Does heightened fear of crime lead to poorer mental health in new suburbs, or vice versa?. Social Science and Medicine, 168, 30-34.
- Footnote 504
-
Lorenc, T., Clayton, S., Neary, D., Whitehead, M., Petticrew, M., Thomson, H., Cummins, S., Sowden, A., Renton, A. (2012). Crime, fear of crime, environment, and mental health and wellbeing: mapping review of theories and causal pathways. Health and Place, 18(4), 757-765.
- Footnote 505
-
Lorenc, T., Petticrew, M., Whitehead, M., Neary, D., Clayton, S., Wright, K., Thomson, H., Cummins, S., Sowden, A., Renton, A. (2014). Crime, fear of crime and mental health: synthesis of theory and systematic reviews of interventions and qualitative evidence. Public Health Research, 2(2).
- Footnote 506
-
Foster, S., Giles-Corti, B. (2008). The built environment, neighborhood crime and constrained physical activity: an exploration of inconsistent findings. Preventive Medicine, 47(3), 241-251.
- Footnote 507
-
Ross, C. E., Jang, S. J. (2000). Neighborhood disorder, fear, and mistrust: The buffering role of social ties with neighbors. American Journal of Community Psychology, 28(4), 401-420.
- Footnote 508
-
Cozens, P. M. (2011). Urban planning and environmental criminology: Towards a new perspective for safer cities. Planning Practice and Research, 26(4), 481-508.
- Footnote 509
-
Statistics Canada (2015). Self-reported victimization, 2014. The Daily. Statistics Canada.
- Footnote 510
-
Cozens, P., Love, T. (2015). A review and current status of Crime Prevention through Environmental Design (CPTED). Journal of Planning Literature, 30(4).
- Footnote 511
-
Shariati, A., Guerette, R. T. (2017). Situational Crime Prevention. In Preventing Crime and Violence (pp. 261-268). Springer International Publishing.
- Footnote 512
-
Cozens, P. (2007). Public health and the potential benefits of crime prevention through environmental design. New South Wales Public Health Bulletin, 18(12), 232-237.
- Footnote 513
-
Cozens, P.M. (2008). New urbanism, crime and the suburbs: A review of the evidence. Urban Policy and Research, 26(4), 429-444.
- Footnote 514
-
Carter, S. P., Carter, S. L., Dannenberg, A. L. (2003). Zoning out crime and improving community health in Sarasota, Florida:"crime prevention through environmental design". American Journal of Public Health, 93(9), 1442-1445.
- Footnote 515
-
Casteel, C., Peek-Asa, C., Howard, J., Kraus, J. F. (2004). Effectiveness of crime prevention through environmental design in reducing criminal activity in liquor stores: a pilot study. Journal of Occupational and Environmental Medicine, 46(5), 450-458.
- Footnote 516
-
Casteel, C., Peek-Asa, C. (2000). Effectiveness of crime prevention through environmental design (CPTED) in reducing robberies. American Journal of Preventive Medicine, 18(4), 99-115.
- Footnote 517
-
Freilich, J.D. (2014). Beccaria and situational crime prevention. Criminal Justice Review, 40(2), 131-150.
- Footnote 518
-
Huisman, W., van Erp, J. (2013). Opportunities for environmental crime: A test of situational crime prevention theory. British Journal of Criminology, 53(6), 1178-1200.
- Footnote 519
-
Lorenc, T., Petticrew, M., Whitehead, M., Neary, D., Clayton, S., Wright, K., Thomson, H., Cummins, S., Sowden, A., Renton, A. (2013). Environmental interventions to reduce fear of crime: systematic review of effectiveness. Systematic Reviews, 2(1), 30.
Design features for specific populations
- Footnote 520
-
Durand, C.P., Andalib, M., Dunton, G.F. , Wolch, J., Pentz, M.A. (2011). A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obesity Reviews, 12(501), e173-e182.
- Footnote 521
-
Public Health Agency of Canada (2015). Health behaviour in school-aged children in Canada: focus on relationships. Public Health Agency of Canada.
- Footnote 522
-
Freeman, J.G., King, M., Pickett, W., Craig, W., Elgar, F., Janssen, I., Klinger, D. (2011). The health of Canada's young people: a mental health focus. Public Health Agency of Canada.
- Footnote 523
-
Janssen, I., Rosu, A. (2015). Undeveloped green space and free-time physical activity in 11 to 13-year-old children. International Journal of Behavioral Nutrition & Physical Activity, 12, 26.
- Footnote 524
-
McGrath, L. J., Hopkins, W. G., Hinckson, E. A. (2015). Associations of objectively measured built-environment attributes with youth moderate–vigorous physical activity: a systematic review and meta-analysis. Sports Medicine, 45(6), 841-865.
- Footnote 525
-
Janssen, I., King, N. (2015). Walkable school neighborhoods are not playable neighborhoods. Health and Place, 35, 66-69.
- Footnote 526
-
Brussoni, M., Olsen, L.L., Pike, I., Sleet, D.A. (2012). Risky play and children's safety: balancing priorities for optimal child development. International Journal of Environmental Research & Public Health, 9(9), 3134-3148.
- Footnote 527
-
Brussoni, M., Gibbons, R., Gray, C., Ishikawa, T., Sandseter, E.B., Bienenstock, A., Chabot, G., Fuselli, P., Herrington, S., Janssen, I., Pickett, W., Power, M., Sanger, N., Sampson, M., Tremblay M.S. (2015). What is the relationship between risky outdoor play and health in children? A systematic review. International Journal of Environmental Research & Public Health, 12(6), 6423-6454.
- Footnote 528
-
Sandercock, G., Angus, C., Barton, J. (2010). Physical activity levels of children living in different built environments. Preventive Medicine, 50(4), 193-198.
- Footnote 529
-
Esteban-Cornejo, I., Carlson, J. A., Conway, T. L., Cain, K. L., Saelens, B. E., Frank, L. D., Glanz, K., Roman, C.G., Sallis, J. F. (2016). Parental and adolescent perceptions of neighborhood safety related to adolescents' physical activity in their neighborhood. Research Quarterly for Exercise and Sport, 87(2), 191-199.
- Footnote 530
-
Carver, A., Timperio, A., Hesketh, K., Crawford, D. (2010). Are children and adolescents less active if parents restrict their physical activity and active transport due to perceived risk?. Social Science and Medicine, 70(11), 1799-1805.
- Footnote 531
-
Cutumisu, N., Bélanger-Gravel, A., Laferté, M., Lagarde, F., Lemay, J. F., Gauvin, L. (2014). Influence of area deprivation and perceived neighbourhood safety on active transport to school among urban Quebec preadolescents. Canadian Journal of Public Health, 105(5), e376-e382.
- Footnote 532
-
Giles-Corti, B., Kelty, S. F., Zubrick, S. R., Villanueva, K. P. (2009). Encouraging walking for transport and physical activity in children and adolescents. Sports Medicine, 39(12), 995-1009.
- Footnote 533
-
Loptson, K., Ridalls, T. (2012). Walkable for whom? Examining the role of the built environment on the neighbourhood-based physical activity of children. Canadian Journal of Public Health, 103(Suppl 3), S29.
- Footnote 534
-
Tappe, K. A., Glanz, K., Sallis, J. F., Zhou, C., Saelens, B. E. (2013). Children's physical activity and parents' perception of the neighborhood environment: neighborhood impact on kids study. International Journal of Behavioral Nutrition and Physical Activity, 10(1), 39.
- Footnote 535
-
Lavoie, M., Burigusa, G., Maurice, P., Hamel, D., Turmel, É. (2014). Active and safe transportation of elementary-school students: comparative analysis of the risks of injury associated with children travelling by car, walking and cycling between home and school. Chronic Diseases and Injuries in Canada, 34(4), 195-202.
- Footnote 536
-
van Loon, J., Frank, L. D., Nettlefold, L., Naylor, P. J. (2014). Youth physical activity and the neighbourhood environment: examining correlates and the role of neighbourhood definition. Social Science and Medicine, 104, 107-115.
- Footnote 537
-
Audrey, S., Batista-Ferrer, H. (2015). Healthy urban environments for children and young people: a systematic review of intervention studies. Health and Place, 36, 97-117.
- Footnote 538
-
Carver, A., Timperio, A., Hesketh, K., Crawford, D. (2010). Are safety-related features of the road environment associated with smaller declines in physical activity among youth?. Journal of Urban Health, 87(1), 29-43.
- Footnote 539
-
Rothman, L., Buliung, R., Macarthur, C., To, T., Howard, A. (2014). Walking and child pedestrian injury: a systematic review of built environment correlates of safe walking. Injury Prevention, 20(1), 41-49.
- Footnote 540
-
Kneeshaw-Price, S. H., Saelens, B. E., Sallis, J. F., Frank, L. D., Grembowski, D. E., Hannon, P. A., Smith, N.L., Chan, K. G. (2015). Neighborhood crime-related safety and its relation to children's physical activity. Journal of Urban Health, 92(3), 472-489.
- Footnote 541
-
Barnes, J. D., Cameron, C., Carson, V., Chaput, J. P., Faulkner, G. E., Janson, K., Kramers, R., LeBlanc, A.G., Spence, J.C., Tremblay, M. S. (2016). Results from Canada's 2016 ParticipACTION report card on physical activity for children and youth. Journal of Physical Activity and Health, 13(11 Suppl 2), S110-S116.
- Footnote 542
-
Faulkner, G. E., Buliung, R. N., Flora, P. K., Fusco, C. (2009). Active school transport, physical activity levels and body weight of children and youth: a systematic review. Preventive Medicine, 48(1), 3-8.
- Footnote 543
-
Lee, M. C., Orenstein, M. R., Richardson, M. J. (2008). Systematic review of active commuting to school and children's physical activity and weight. Journal of Physical Activity and Health, 5(6), 930-949.
- Footnote 544
-
Voss, C., Winters, M., Frazer, A., and McKay, H. (2015). School-travel by public transit: rethinking active transportation. Preventive Medicine Reports, 2, 65-70.
- Footnote 545
-
Coalitions Linking Action and Science for Prevention (2012). Children's Mobility, Health and Happiness: a Canadian School Travel Planning Model: 2012 national results – executive summary. Coalitions Linking Action and Science for Prevention.
- Footnote 546
-
Larouche, R. (2015). Built environment features that promote cycling in school-aged children. Current Obesity Reports, 4(4), 494-503.
- Footnote 547
-
Larouche, R., Barnes, J., Tremblay, M. S. (2013). Too far to walk or bike?. Canadian Journal of Public Health, 104(7), 487-489.
- Footnote 548
-
Larouche, R., Chaput, J. P., Leduc, G., Boyer, C., Bélanger, P., LeBlanc, A. G., Borghese, M.M., Tremblay, M. S. (2014). A cross-sectional examination of socio-demographic and school-level correlates of children's school travel mode in Ottawa, Canada. BMC Public Health, 14(1), 497.
- Footnote 549
-
Faulkner, G. E., Richichi, V., Buliung, R. N., Fusco, C., Moola, F. (2010). What's "quickest and easiest?": parental decision making about school trip mode. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 62.
- Footnote 550
-
Gropp, K. M., Pickett, W., Janssen, I. (2012). Multi-level examination of correlates of active transportation to school among youth living within 1 mile of their school. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 124.
- Footnote 551
-
Gropp, K., Janssen, I., Pickett, W. (2013). Active transportation to school in Canadian youth: should injury be a concern?. Injury Prevention, 19(1), 64-67.
- Footnote 552
-
Larsen, K., Gilliland, J., Hess, P. M. (2011). Route-based analysis to capture the environmental influences on a child's mode of travel between home and school. Annals of the Association of American Geographers, 102(6), 1348-1365.
- Footnote 553
-
Mitra, R., Buliung, R. N. (2012). Built environment correlates of active school transportation: neighborhood and the modifiable areal unit problem. Journal of Transport Geography, 20(1), 51-61.
- Footnote 554
-
Oliver, M., Badland, H., Mavoa, S., Witten, K., Kearns, R., Ellaway, A., Hinckson, E., Mackay, L., Schluter, P. J. (2014). Environmental and socio-demographic associates of children's active transport to school: a cross-sectional investigation from the URBAN Study. International Journal of Behavioral Nutrition and Physical Activity, 11(1), 70.
- Footnote 555
-
Trapp, G. S., Giles-Corti, B., Christian, H. E., Bulsara, M., Timperio, A. F., McCormack, G. R., Villaneuva, K. P. (2011). On your bike! a cross-sectional study of the individual, social and environmental correlates of cycling to school. International Journal of Behavioral Nutrition and Physical Activity, 8(1), 123.
- Footnote 556
-
Wong, B. Y. M., Faulkner, G., Buliung, R. (2011). GIS measured environmental correlates of active school transport: a systematic review of 14 studies. International Journal of Behavioral Nutrition and Physical Activity, 8(1), 39.
- Footnote 557
-
Seliske, L., Pickett, W., Janssen, I. (2012). Urban sprawl and its relationship with active transportation, physical activity and obesity in Canadian youth. Health Reports, 23(2), 17-25.
- Footnote 558
-
Garriguet, D., Colley, R., Bushnik, T. (2017). Parent-child association in physical activity and sedentary behaviour. Health Reports. Statistics Canada.
- Footnote 559
-
Carlson, J. A., Sallis, J. F., Kerr, J., Conway, T. L., Cain, K., Frank, L. D., Saelens, B. E. (2014). Built environment characteristics and parent active transportation are associated with active travel to school in youth age 12–15. British Journal of Sports Medicine, 48(22), 1634-1639.
- Footnote 560
-
Henne, H. M., Tandon, P. S., Frank, L. D., Saelens, B. E. (2014). Parental factors in children's active transport to school. Public Health, 128(7), 643-646.
- Footnote 561
-
Cutumisu, N., Traoré, I., Paquette, M. C., Cazale, L., Camirand, H., Lalonde, B., Robitaille, E. (2017). Association between junk food consumption and fast-food outlet access near school among Quebec secondary-school children: findings from the Quebec Health Survey of High School Students (QHSHSS) 2010–11. Public Health Nutrition, 20(5), 927-937.
- Footnote 562
-
Van Hulst, A., Barnett, T. A., Gauvin, L., Daniel, M., Kestens, Y., Bird, M., Gray-Donald, K., Lambert, M. (2012). Associations between children's diets and features of their residential and school neighbourhood food environments. Canadian Journal of Public Health, 103(9), 48-54.
- Footnote 563
-
He, M., Tucker, P., Irwin, J. D., Gilliland, J., Larsen, K., Hess, P. (2012). Obesogenic neighbourhoods: the impact of neighbourhood restaurants and convenience stores on adolescents' food consumption behaviours. Public Health Nutrition, 15(12), 2331-2339.
- Footnote 564
-
He, M., Tucker, P., Gilliland, J., Irwin, J. D., Larsen, K., Hess, P. (2012). The influence of local food environments on adolescents' food purchasing behaviors. International Journal of Environmental Research and Public Health, 9(4), 1458-1471.
- Footnote 565
-
Sadler, R. C., Clark, A. F., Wilk, P., O'Connor, C., Gilliland, J. A. (2016). Using GPS and activity tracking to reveal the influence of adolescents' food environment exposure on junk food purchasing. Canadian Journal of Public Health, 107, 14-20.
- Footnote 566
-
Christian, H., Zubrick, S. R., Foster, S., Giles-Corti, B., Bull, F., Wood, L., Knuiman, M., Brinkman, S., Houghton, S., Boruff, B. (2015). The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health and Place, 33, 25-36.
- Footnote 567
-
Villanueva, K., Badland, H., Kvalsvig, A., O'Connor, M., Christian, H., Woolcock, G., Giles-Corti, B., Goldfeld, S. (2016). Can the neighborhood built environment make a difference in children's development? Building the research agenda to create evidence for place-based children's policy. Academic Pediatrics, 16(1), 10-19.
- Footnote 568
-
Agay-Shay, K., Peled, A., Crespo, A. V., Peretz, C., Amitai, Y., Linn, S., Friger, M., Nieuwenhuijsen, M. J. (2014). Green spaces and adverse pregnancy outcomes. Occupational and Environmental Medicine, 71(8), 562-569.
- Footnote 569
-
Ebisu, K., Holford, T. R., Bell, M. L. (2016). Association between greenness, urbanicity, and birth weight. Science of The Total Environment, 542, 750-756.
- Footnote 570
-
Mitchell, C. A., Clark, A. F., Gilliland, J. A. (2016). Built environment influences of children's physical activity: examining differences by neighbourhood size and sex. International Journal of Environmental Research and Public Health, 13(1), 130.
- Footnote 571
-
Larouche, R., Garriguet, D., Gunnell, K.E., Goldfield, G.S., Tremblay, M.S. (2016). Outdoor time, physical activity, sedentary time, and health indicators at ages 7 to 14: 2012/2013 Canadian Health Measures Survey. Health Reports. Statistics Canada.
- Footnote 572
-
International Weight Management in Pregnancy Collaborative Group (2017). Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ, 358, j3119.
- Footnote 573
-
Ruifrok, A.E., van Poppel, M.N., van Wely, M., Rogozinska, E., Khan, K.S., de Groot, C.J., Thangaratinam, S., Mol, B.W. (2014). Association between weight gain during pregnancy and pregnancy outcomes after dietary and lifestyle interventions: a meta-analysis. American Journal of Perinatology, 31(5), 353-364.
- Footnote 574
-
Margerison Zilko, C.E., Rehkopf, D., Arbams, B. (2010). Association of maternal gestational weight gain with short- and long-term maternal and child health outcomes. American Journal of Obstetrics & Gynecology, 202(6), 574.
- Footnote 575
-
Siega-Riz, A.M., Viswanathan, M., Moos, M.K., Deierlein, A., Mumford, S., Knaack, J., Thieda, P., Lux, L.J., Lohr, K.N. (2009). A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: birthweight, fetal growth, and postpartum weight retention. American Journal of Obstetrics & Gynecology, 201(4), 339.
- Footnote 576
-
Lau, E.Y., Liu, J., Archer, E., McDonald, S.M., Liu, J. (2014). Maternal weight gain in pregnancy and risk of obesity among offspring: a systematic review. Journal of Obesity, 524939.
- Footnote 577
-
Saligheh, M., Hackett, D., Boyce, P. Cobley, S. (2017). Can exercise or physical activity help improve postnatal depression and weight loss? A systematic review. Archives of Women's Mental Health, epub.
- Footnote 578
-
Poyatos-Leon, R., Garcia-Hermoso, A., Sanabria-Martinez, G., Alvarez-Bueno, C., Cavero-Redondo, I., Martinez-Vizcaino, V. (2017). Effects of exercise-based interventions on postpartum depression: a meta-analysis of randomized controlled trials. Birth, epub.
- Footnote 579
-
McCurdy, A.P., Boule, N.G., Sivak, A., Davenport, M.H. (2017). Effects of exercise on mild-to-moderate depressive symptoms in the postpartum period: a meta-analysis. Obstetrics & Gynecology, 129(6), 1087-1097.
- Footnote 580
-
Lim, S., O'Reilly, S., Behrens, J., Skinner, T., Ellis, I., Dunbar, J.A. (2015). Effective strategies for weight loss in post-partum women: a systematic review and meta-analysis. Obesity Reviews, 16(11), 972-987.
- Footnote 581
-
Baskin, R., Hill, B., Jacka, F.N., O'Neil, A. Skouteris, H. (2015). The association between diet quality and mental health during the perinatal period. a systematic review. Appetite, 91, 41-47.
- Footnote 582
-
Endres, L.K., Straub, H., McKinney, C., Plunkett, B., Minkovitz, C.S., Schetter, C.D., Ramey, S., Wang, C., Hobel, C., Raju, T., Shalowitz, M.U. (2015). Postpartum weight retention risk factors and relationship to obesity at one year. Obstetrics & Gynecology, 125(1), 144-152.
- Footnote 583
-
Nehring, I., Schmoll, S., Beyerlein, A., Hauner, H., von Kries, R. (2011). Gestational weight gain and long-term postpartum weight retention: a meta-analysis. American Journal of Clinical Nutrition, 94(5), 1225-1231.
- Footnote 584
-
Lord, S., Luxembourg, N. (2008). The mobility of elderly residents living in suburban territories: mobility experiences in Canada and France. Journal of Housing for the Elderly, 20(4), 103-121.
- Footnote 585
-
McPhee, J. S., French, D. P., Jackson, D., Nazroo, J., Pendleton, N., Degens, H. (2016). Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology, 17(3), 567-580.
- Footnote 586
-
Vogel, T., Brechat, P. H., Leprêtre, P. M., Kaltenbach, G., Berthel, M., Lonsdorfer, J. (2009). Health benefits of physical activity in older patients: a review. International Journal of Clinical Practice, 63(2), 303-320.
- Footnote 587
-
Yen, I. H., Michael, Y. L., Perdue, L. (2009). Neighborhood environment in studies of health of older adults: a systematic review. American Journal of Preventive Medicine, 37(5), 455-463.
- Footnote 588
-
Yen, I. H., Fandel Flood, J., Thompson, H., Anderson, L. A., Wong, G. (2014). How design of places promotes or inhibits mobility of older adults: Realist synthesis of 20 years of research. Journal of Aging and Health, 26(8), 1340-1372.
- Footnote 589
-
Rosso, A. L., Auchincloss, A. H., Michael, Y. L. (2011). The urban built environment and mobility in older adults: a comprehensive review. Journal of Aging Research.
- Footnote 590
-
Frank, L., Kerr, J., Rosenberg, D., King, A. (2010). Healthy aging and where you live: community design relationships with physical activity and body weight in older Americans. Journal of Physical Activity and Health, 7(Suppl 1), S82-S90.
- Footnote 591
-
Adams, M. A., Sallis, J. F., Conway, T. L., Frank, L. D., Saelens, B. E., Kerr, J., Cain, K.L., King, A. C. (2012). Neighborhood environment profiles for physical activity among older adults. American Journal of Health Behavior, 36(6), 757-769.
- Footnote 592
-
Chudyk, A. M., Winters, M., Moniruzzaman, M., Ashe, M. C., Gould, J. S., McKay, H. (2015). Destinations matter: The association between where older adults live and their travel behavior. Journal of Transport and Health, 2(1), 50-57.
- Footnote 593
-
King, A. C., Sallis, J. F., Frank, L. D., Saelens, B. E., Cain, K., Conway, T. L., Chapman, J.E., Ahn, D.K., Kerr, J. (2011). Aging in neighborhoods differing in walkability and income: associations with physical activity and obesity in older adults. Social Science and Medicine, 73(10), 1525-1533.
- Footnote 594
-
Levasseur, M., Généreux, M., Bruneau, J. F., Vanasse, A., Chabot, É., Beaulac, C., Bédard, M. M. (2015). Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: results from a scoping study. BMC Public Health, 15(1), 503.
- Footnote 595
-
Mitra, R., Siva, H., Kehler, M. (2015). Walk-friendly suburbs for older adults? Exploring the enablers and barriers to walking in a large suburban municipality in Canada. Journal of Aging Studies, 35, 10-19.
- Footnote 596
-
Thornton, C. M., Kerr, J., Conway, T. L., Saelens, B. E., Sallis, J. F., Ahn, D. K., Frank, L.D., Cain, K.L., King, A. C. (2016). Physical activity in older adults: An ecological approach. Annals of Behavioral Medicine, 51(2), 159-169.
- Footnote 597
-
Todd, M., Adams, M. A., Kurka, J., Conway, T. L., Cain, K. L., Buman, M. P., Frank, L.D., Sallis, J.F., King, A. C. (2016). GIS-measured walkability, transit, and recreation environments in relation to older Adults' physical activity: a latent profile analysis. Preventive Medicine, 93, 57-63.
- Footnote 598
-
Van Holle, V., Van Cauwenberg, J., Van Dyck, D., Deforche, B., Van de Weghe, N., De Bourdeaudhuij, I. (2014). Relationship between neighborhood walkability and older adults' physical activity: results from the Belgian Environmental Physical Activity Study in Seniors (BEPAS Seniors). International Journal of Behavioral Nutrition and Physical Activity, 11(1), 110.
- Footnote 599
-
Van Holle, V., Van Cauwenberg, J., Gheysen, F., Van Dyck, D., Deforche, B., Van de Weghe, N., De Bourdeaudhuij, I. (2016). The association between Belgian older adults' physical functioning and physical activity: what is the moderating role of the physical environment?. PLoS One, 11(2), e0148398.
- Footnote 600
-
Winters, M., Voss, C., Ashe, M. C., Gutteridge, K., McKay, H., Sims-Gould, J. (2015). Where do they go and how do they get there? Older adults' travel behaviour in a highly walkable environment. Social Science and Medicine, 133, 304-312.
- Footnote 601
-
Chudyk, A. M., Winters, M., Moniruzzaman, M., Ashe, M. C., Gould, J. S., McKay, H. (2015). Destinations matter: The association between where older adults live and their travel behavior. Journal of Transport and Health, 2(1), 50-57.
- Footnote 602
-
Chudyk, A. M., McKay, H. A., Winters, M., Sims-Gould, J., Ashe, M. C. (2017). Neighborhood walkability, physical activity, and walking for transportation: A cross-sectional study of older adults living on low income. BMC Geriatrics, 17(1), 82.
- Footnote 603
-
Frank, L., Kerr, J., Rosenberg, D., King, A. (2010). Healthy aging and where you live: community design relationships with physical activity and body weight in older Americans. Journal of Physical Activity and Health, 7(Suppl 1), S82-S90.
- Footnote 604
-
Gauvin, L., Richard, L., Kestens, Y., Shatenstein, B., Daniel, M., Moore, S. D., Mercille, G., Payette, H. (2012). Living in a well-serviced urban area is associated with maintenance of frequent walking among seniors in the VoisiNuAge study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67(1), 76-88.
- Footnote 605
-
Gell, N. M., Rosenberg, D. E., Carlson, J., Kerr, J., Belza, B. (2015). Built environment attributes related to GPS measured active trips in mid-life and older adults with mobility disabilities. Disability and Health Journal, 8(2), 290-295.
- Footnote 606
-
Marquet, O., Miralles-Guasch, C. (2015). Neighbourhood vitality and physical activity among the elderly: The role of walkable environments on active ageing in Barcelona, Spain. Social Science and Medicine, 135, 24-30.
- Footnote 607
-
Rosso, A. L., Auchincloss, A. H., Michael, Y. L. (2011). The urban built environment and mobility in older adults: a comprehensive review. Journal of Aging Research, 2011.
- Footnote 608
-
Public Health Agency of Canada. (2014). Seniors' Falls in Canada: Second Report. Public Health Agency of Canada.
- Footnote 609
-
Canadian Institute for Health Information. National Trauma Registry Metadata.
- Footnote 610
-
Nicklett, E. J., Lohman, M. C., Smith, M. L. (2017). Neighborhood environment and falls among community-dwelling older adults. International Journal of Environmental Research and Public Health, 14(2), 175.
- Footnote 611
-
Chippendale, T., Boltz, M. (2015). The neighborhood environment: Perceived fall risk, resources, and strategies for fall prevention. The Gerontologist, 55(4), 575-583.
- Footnote 612
-
Li, W., Keegan, T. H., Sternfeld, B., Sidney, S., Quesenberry Jr, C. P., Kelsey, J. L. (2006). Outdoor falls among middle-aged and older adults: a neglected public health problem. American Journal of Public Health, 96(7), 1192-1200.
- Footnote 613
-
Clarke, P., Gallagher, N.A. (2013). Optimizing mobility in later life: the role of the urban built environment for older adults aging in place. Journal of Urban Health, 90(6), 997-1009.
- Footnote 614
-
Hanson, H. M., Ashe, M., McKay, H. A., Winters, M. (2012). Intersection between the built and social environments and older adults' mobility: an evidence review. National Collaborating Centre for Environmental Health.
- Footnote 615
-
Clarke, P., Hirsch, J. A., Melendez, R., Winters, M., Gould, J. S., Ashe, M., Furst, S., McKay, H. (2017). Snow and Rain Modify Neighbourhood Walkability for Older Adults. Canadian Journal on Aging, 36(2), 159-169.
- Footnote 616
-
Ottoni, C. A., Sims-Gould, J., Winters, M., Heijnen, M., McKay, H. A. (2016). "Benches become like porches": Built and social environment influences on older adults' experiences of mobility and well-being. Social Science and Medicine, 169, 33-41.
- Footnote 617
-
Emerson, K.G., Jayawardhana, J. (2016). Risk factors for loneliness in elderly adults. Journal of American Geriatrics Society, 64(4), 886-887.
- Footnote 618
-
Richard, L., Gauvin, L., Kestens, Y., Shatenstein, B., Payette, H., Daniel, M., Moore, S., Levasseur, M., Mercille, G. (2013). Neighborhood resouces and social participation among older adults: results from the VoisiNuage study. Journal of Aging & Health, 25(2), 296-318.
- Footnote 619
-
Gray, J.A., Zimmerman, J.L., Rimmer, J.H. (2012). Built environment instruments for walkability, bikeability and recreation: disability and universal design relevant? Disability & Health Journal, 5(2), 87-101.
- Footnote 620
-
Morales, E., Lindsay, S., Edwards, G., Howell, L., Vincent, C., Yantzi, N., Gauthier, V. (2016). Addressing challenges for youths with mobility devices in winter conditions. Disability & Rehabilitation, 7, 1-7.
- Footnote 621
-
Spivock, M., Gauvin, L., Brodeur, J.M. (2007). Neighborhood-level active living buoys for individuals with physical disabilities. American Journal of Preventive Medicine, 32(3), 224-230.
- Footnote 622
-
Spivock, M., Gauvin, L., Riva, M., Brodeur, J.M. (2008). Promoting active living among people with physical disabilities. American Journal of Preventive Medicine, 34(4), 291-298.
- Footnote 623
-
Statistics Canada (2015). A profile of persons with disabilities among Canadians aged 15 years or older, 2012. Canadian Survey on Disability, 2012. Statistics Canada.
- Footnote 624
-
Botticello, A.L., Rohorbach, T., Cobbold, N. (2014). Disability and the built environment: an investigation of community and neighborhood land uses and participation for physically impaired adults. Annals of Epidemiology, 24(7), 545-550.
- Footnote 625
-
Clarke, P. Aiolshire, J.A., Bader, M., Morenoff, J.D., House, J.S. (2008). Mobility disability and the urban built environment. American Journal of Epidemiology, 168(5), 506-513.
- Footnote 626
-
Shumway-Cook, A., Patla, A., Stewart, A., Ferrucci, L., Ciol, M.A., Guralnik, J.M. (2003). Environmental components of mobility disability in community-living older persons. Journal of the American Geriatrics Society, 51(3), 393-398.
- Footnote 627
-
Lindsay, S., Morales, E., Yantzi, N., Vincent, C., Howell, L., Edwards, G. (2015). The experiences of participating in winter among youths with a physical disability compared with their typically developing peers. Child: Care, Health & Development, 41(6), 980-988.
- Footnote 628
-
Lindsay, S., Yantzi, N. (2014). Weather, disability, vulnerability, and resilience: exploring how youth with physical disabilities experience winter. Disability & Rehabilitation, 36(26), 2195-2204.
- Footnote 629
-
Ripat, J., Colatruglio, A. (2016). Exploring winter community participation among wheelchair users : an online focus group. Occupational Therapy in Health Care, 30(1), 95-106.
- Footnote 630
-
Ripat, J.D., Brown, C.L., Ethans, K.D. (2015). Barriers to wheelchair use in the winter. Archives of Physical Medicine & Rehabilitation, 96(6), 1117-1122.
- Footnote 631
-
Friel, S., Akerman, M., Hancock, T., Kumaresan, J., Marmot, M., Melin, T., Valhov, D., GRNUHE members (2011). Addressing the social and environmental determinants of urban health equity: evidence for action and a research agenda. Journal of Urban Health, 88(5), 860-874.
- Footnote 632
-
Hutch, D.J., Bouye, K.E., Skillen, E. Lee, C., Whitehead, L., Rashid, J.R. (2011). Potential strategies to eliminate built environment disparities for disadvantaged and vulnerable communities. American Journal of Public Health, 101(4), 587-595.
- Footnote 633
-
Badland, H., Foster, S., Bentley, R., Higgs, C., Roberts, R., Pettit, C., Giles-Corti, B. (2017). Examining associations between aera-level spatial measures of housing with selected health and wellbeing behaviours and outcomes in an urban context. Health and Place, 43, 17-24.
- Footnote 634
-
Downing, J. (2016). The health effects of the foreclosure crisis and unaffordable housing: a systematic review and explanation of evidence. Social Science and Medicine, 162, 88-96.
- Footnote 635
-
Maqbool, N., Viveiros, J., Ault, M. (2015). The impacts of affordable housing on health : a research summary. Insights from Housing Policy Research. Center for Housing Policy.
- Footnote 636
-
Mason, K.E., Baker, E., Blakely, T., Bentley, R.J. (2013). Housing affordability and mental health: does the relationship differ for renters and home purchasers? Social Science and Medicine, 94, 91-97.
- Footnote 637
-
Meltzer, R., Schwartz, A. (2015). Housing affordability and health: evidence from New York City. Housing Policy Debate, 26(1), 80-104.
- Footnote 638
-
Novoa, A.M., Ward, J., Malmusi, D., Diaz, F., Darnell, M., Trilla, C., Bosch, J. Borrell, C. (2015). How substandard dwellings and housing affordability problems are associated with poor health in a vulnerable population during the economic recession of the late 2000s. International Journal for Equity in Health, 14, 120.
- Footnote 639
-
Vasquez-Vera, H., Palencia, L., Magna, I., Mena, C., Neira, J., Borrell, C. (2017). The threat of home eviction and its effects on health through the equity lens : a systematic review. Social Science and Medicine, 175, 188-208.
- Footnote 640
-
Atkinson, R. (2010). The evidence on the impact of gentrification: new lessons for the urban renaissance? International Journal of Housing Policy, 4(1), 107-131.
- Footnote 641
-
Shaw, K.S., Hagemans, I.W. (2015). "Gentrification without displacement" and the consequent loss of place: the effects of class transition on low-income residents of secure housing in gentrifying areas. International Journal of Urban and Regional Research, 39(2), 323-341.
- Footnote 642
-
Indigenous and Northern Affairs Canada (2010). Fact sheet – Urban Aboriginal population in Canada. Indigenous and Northern Affairs Canada.
- Footnote 643
-
Gionet, L. (2009). Métis in Canada: selected findings of the 2006 Census. Statistics Canada.
- Footnote 644
-
Statistics Canada (2010). 2006 Census: Aboriginal Peoples in Canada in 2006: Inuit Métis and First Nations, 2006 Census: First Nations people. Statistics Canada.
- Footnote 645
-
Statistics Canada (2016). Aboriginal Peoples in Canada: First Nations People, Métis and Inuit. Statistics Canada.
- Footnote 646
-
Brown, B., Wachowiak-Smolíková, R., Spence, N. D., Wachowiak, M. P., Walters, D. F. (2016). Why Do Some First Nations Communities Have Safe Water and Others Not? Socioeconomic Determinants of Drinking Water Risk. Global Journal of Health Science, 8(9), 99.
- Footnote 647
-
Galway, L.P. (2016). Boiling over: A Descriptive Analysis of Drinking Water Advisories in First Nations Communities in Ontario, Canada. International Journal of Environmental Research and Public Health, 13(5), 505.
- Footnote 648
-
Patrick, R.J. (2011). Uneven access to safe drinking water for First Nations in Canada: Connecting health and place through source water protection. Health and Place, 17(1), 386-389.
- Footnote 649
-
Sarkar, A., Hanrahan, M., Hudson, A. (2015). Water insecurity in Canadian Indigenous communities: some inconvenient truths. Rural and Remote Health, 15(3354), 1-14.
- Footnote 650
-
Donaldson, S. G., Van Oostdam, J., Tikhonov, C., Feeley, M., Armstrong, B., Ayotte, P., Boucher, O., Bowers, W., Chan, L., Dallaire, F., Dallaire, R. (2010). Environmental contaminants and human health in the Canadian Arctic. Science of the Total Environment, 408(22), 5165-5234.
- Footnote 651
-
Hlimi, T., Skinner, K., Hanning, R., Martin, I. D., Tsuji, L. S. (2012). Traditional food consumption behaviour and concern with environmental contaminants among Cree schoolchildren of the Mushkegowuk territory. International Journal of Circumpolar Health, 71(1), 17344.
- Footnote 652
-
Johnson-Down, L., Egeland, G. M. (2010). Adequate nutrient intakes are associated with traditional food consumption in Nunavut Inuit children aged 3–5 years. The Journal of Nutrition, 140(7), 1311-1316.
- Footnote 653
-
Reading, J., Halseth, R. (2013). Pathways to Improving Well-Being for Indigenous Peoples: How Living Conditions Decide Health. Prince George, BC: National Collaborating Centre for Aboriginal Health.
- Footnote 654
-
Akande, V. O., Hendriks, A. M., Ruiter, R. A., Kremers, S. P. (2015). Determinants of dietary behavior and physical activity among Canadian Inuit: a systematic review. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 84.
- Footnote 655
-
Bruner, B., Chad, K. (2013). Physical activity attitudes, beliefs, and practices among women in a Woodland Cree community. Journal of Physical Activity and Health, 10(8), 1119-1127.
- Footnote 656
-
Gates, M., Hanning, R., Gates, A., Stephen, J., Fehst, A., Tsuji, L. (2016). Physical activity and fitness of First Nations youth in a remote and isolated northern Ontario community: a needs assessment. Journal of Community Health, 41(1), 46.
- Footnote 657
-
Lévesque, L., Janssen, I., Xu, F. (2015). Correlates of physical activity in First Nations youth residing in First Nations and northern communities in Canada. Canadian Journal of Public Health, 106(2), 29-35.
- Footnote 658
-
Parks, M.W. (2010). Ecohealth and Aboriginal Health: A Review of Common Ground. National Collaborating Centre for Aboriginal Health.
Designing Canadian communities for healthy living
- Footnote 659
-
Politis, C.E., Mowat, D., Keen, D. (2017). Pathways to policy: lessons learned in multisecctoral collaboration for physical activity and built environment policy development from the Coalitions Linking Action and Science for Prevention (CLASP) initiative. Canadian Journal of Public Health, 108(2), e192-e198.
- Footnote 660
-
Kishchuk, N. (2014). "Taking the Pulse 2": Comparative analysis: planning for healthier communities. Questionnaire results, June 2014. Institut canadien des urbanistes.
- Footnote 661
-
Centre de collaboration nationale sur les politiques publique et la santé (2012). Health authorities and the built environment: actions to influence public policies: interview report, November 2012. Centre de collaboration nationale sur les politiques publique et la santé.
- Footnote 662
-
de Leeuw, E., Simos, J. (eds.). (2017). Healthy Cities: The Theory, Policy, and Practice of Value-Based Urban Planning. Springer.
- Footnote 663
-
Macfarlane, R. G., Wood, L. P., Campbell, M. E. (2015). Healthy Toronto by Design: Promoting a healthier built environment. Canadian Journal of Public Health, 106(1), 5-8.
- Footnote 664
-
Dube, A. S., Beausoleil, M., Gosselin, C., Beaulne, G., Paquin, S., Pelletier, A., Goudreau, S., Poirier, M. H., Drouin, L., Gauvin, Li. (2014). Grassroots projects aimed at the built environment: Association with neighbourhood deprivation, land-use mix and injury risk to road users. Canadian Journal of Public Health, 106(1), e521.
- Footnote 665
-
Plan Canada (2013). Indigenizing Planning/Planning to Indigenize. Canadian Institute of Planners.
- Footnote 666
-
Walker, R., Jojola, T., Natcher, N. (eds.). (2013). Reclaiming indigenous planning (Vol. 70). McGill-Queen's Press-MQUP.
- Footnote 667
-
Plan Canada (2008). Indigenizing Planning/Planning to Indigenize. Canadian Institute of Planners.
- Footnote 668
-
Federation of Canadian Municipalities. First Nation-Municipal land use planning tool. Federation of Canadian Municipalities.
- Footnote 669
-
Federation of Canadian Municipalities (2015). Stronger together toolkit. Federation of Canadian Municipalities.
- Footnote 670
-
National Collaborating Centre for Environment Health (2016). Integrating Indigenous community planning into a healthy built environment. National Collaborating Centre for Environment Health.
- Footnote 671
-
Canadian Institute of Planners (2013). Healthy communities: Legislative comparison survey report. Canadian Institute of Planners.
- Footnote 672
-
BC Healthy Communities, Mouvement Acadien des communautés en santé du Nouveau-Brunswick, Ontario Healthy Communities Coalition, Réseau Québecois de villes et villages en santé. The Healthy Communities approach : a framework for action on the determinants of health. Communautés en santé du Canada.
- Footnote 673
-
Canadian Healthy Communities. A survey of Canadian Healthy Communities initiatives. Canadian Healthy Communities.
- Footnote 674
-
Miro, A., Kishchuk, N. A., Perrotta, K., & Swinkels, H. M. (2015). Healthy Canada by Design CLASP: Lessons learned from the first phase of an intersectoral, cross-provincial, built environment initiative. Canadian Journal of Public Health, 106(1), 50-58.
- Footnote 675
-
Perrotta, K. (2015). Building a community of practice: Healthy Canada by Design CLASP Renewal–Postscript. Canadian Journal of Public Health, 106(1), 59-61.
- Footnote 676
-
World Health Organization. Healthy Cities. World Health Organization, Regional Office for Europe.
- Footnote 677
-
Canadian Healthy Communities. An integrated approach for chronic disease prevention. Canadian Healthy Communities.
- Footnote 678
-
Jeste, D. V., Blazer, D. G., Buckwalter, K. C., Cassidy, K. L. K., Fishman, L., Gwyther, L. P., Levin, S.M., Phillipson, C., Rao, R.R., Schmeding, E., Vega, W. A. (2016). Age-friendly communities initiative: public health approach to promoting successful aging. The American Journal of Geriatric Psychiatry, 24(12), 1158-1170.
- Footnote 679
-
Plouffe, L. A., Kalache, A. (2011). Making communities age friendly: state and municipal initiatives in Canada and other countries. Gaceta Sanitaria, 25, 131-137.
- Footnote 680
-
Orpana, H., Chawla, M., Gallagher, E., Escaravage, E. (2016). Developing indicators for evaluation of age-friendly communities in Canada: process and results. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 36(10), 214.
- Footnote 681
-
World Health Organization. (2015). Measuring the age-friendliness of cities: A guide to using core indicators. World Health Organization.
- Footnote 682
-
Keating, N., Eales, J., Phillips, J. E. (2013). Age-friendly rural communities: Conceptualizing 'best-fit'. Canadian Journal on Aging, 32(4), 319-332.
- Footnote 683
-
Menec, V., Bell, S., Novek, S., Minnigaleeva, G. A., Morales, E., Ouma, T., Parodi, J.F., Winterton, R. (2015). Making rural and remote communities more age-friendly: experts' perspectives on issues, challenges, and priorities. Journal of Aging & Social Policy, 27(2), 173-191.
- Footnote 684
-
Neville, S., Napier, S., Adams, J., Wham, C., Jackson, D. (2016). An integrative review of the factors related to building age‐friendly rural communities. Journal of Clinical Nursing, 25(17-18), 2402-2412.
- Footnote 685
-
Spina, J., Menec, V. H. (2015). What community characteristics help or hinder rural communities in becoming age-friendly? Perspectives from a Canadian prairie province. Journal of Applied Gerontology, 34(4), 444-464.
- Footnote 686
-
Gagnon, F., Bellefleur, O. (2015). Influencing public policies: Two (very good) reasons to look toward scientific knowledge in public policy. Canadian Journal of Public Health, 106(1), 9-11.
- Footnote 687
-
Raine, K. D., Muhajarine, N., Spence, J. C., Neary, N. E., Nykiforuk, C. I. (2012). Coming to consensus on policy to create supportive built environments and community design. Canadian Journal of Public Health, 103(Suppl 3), S5-S8.
- Footnote 688
-
Sallis, J. F., Bull, F., Burdett, R., Frank, L. D., Griffiths, P., Giles-Corti, B., Stevenson, M. (2016). Use of science to guide city planning policy and practice: how to achieve healthy and sustainable future cities. The Lancet, 388(10062), 2936-2947.
- Footnote 689
-
Fazli, G.S., Creatore, M.I., Matheson, F.I., Guilcher, S., Kaufman-Shriqui, V., Manson, H., Johns, A., Booth, G.L. (2017). Identifying mechanisms for facilitating knowledge to action strategies targeting the built environment. BMC Public Health, 17(1), 1.
- Footnote 690
-
Kovacic, J. C., Castellano, J. M., Farkouh, M. E., Fuster, V. (2014). The relationships between cardiovascular disease and diabetes: focus on pathogenesis. Endocrinology and Metabolism Clinics of North America, 43(1), 41-57.
- Footnote 691
-
Rössner, S. (2002). Obesity: the disease of the twenty-first century. International Journal of Obesity, 26(S4), S2.
- Footnote 692
-
McCloughen, A., Foster, K., Huws Thomas, M., Delgado, C. (2012). Physical health and wellbeing of emerging and young adults with mental illness: An integrative review of international literature. International Journal of Mental Health Nursing, 21(3), 274-288.