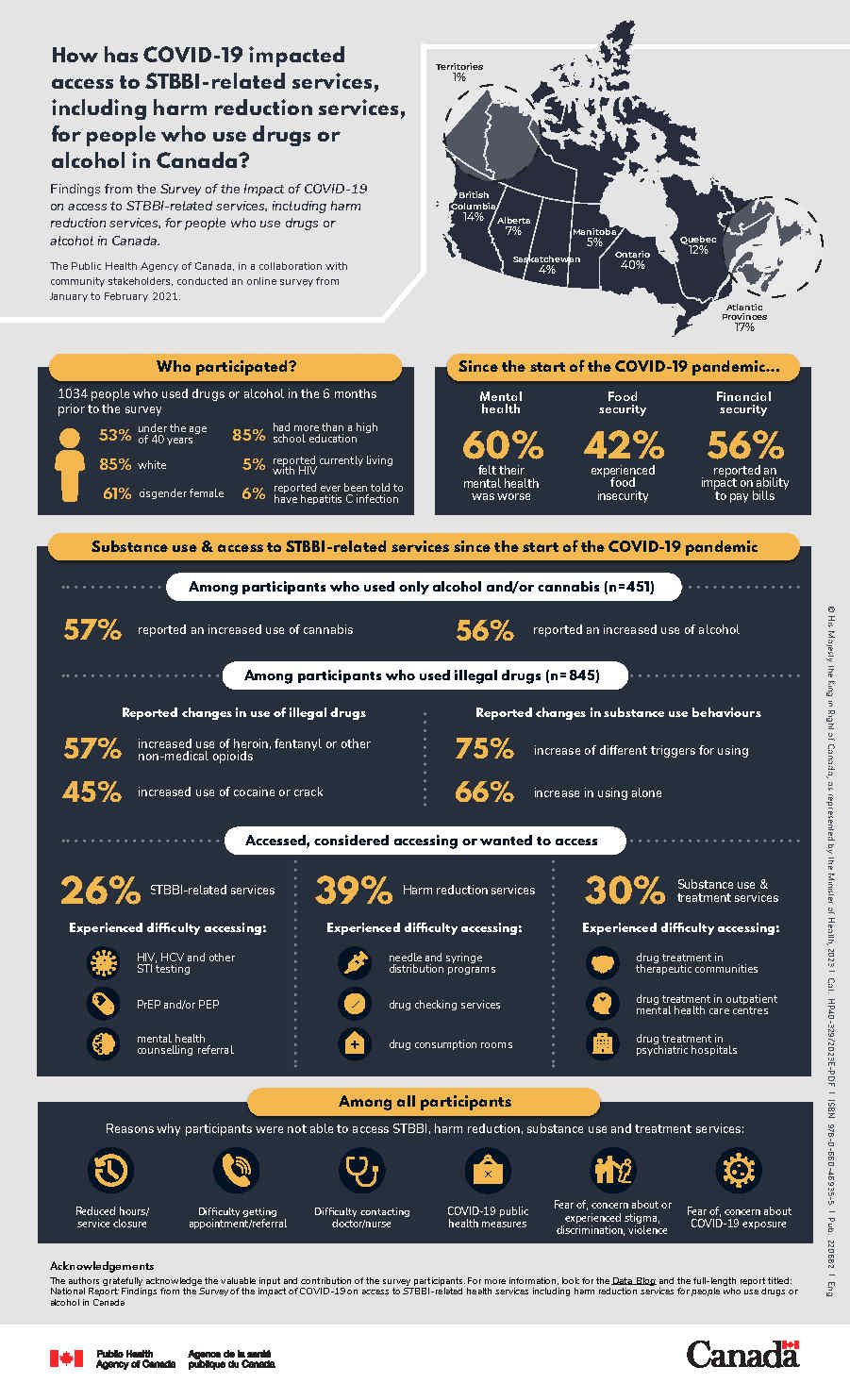
Impact of COVID-19 on the delivery of STBBI-related services in Canada, including harm reduction services, for people who use drugs or alcohol
Download in PDF format
(336 KB, 1 page)
Organization: Public Health Agency of Canada
Date published: 2023-03-27
Cat.: HP40-329/2023E-PDF
ISBN: 978-0-660-46935-5
Pub.: 220682
Findings from the Survey of the impact of COVID-19 on access to sexually transmitted and blood borne infection (STBBI)-related health services, including harm reduction services, for people who use drugs or alcohol in Canada.
The Public Health Agency of Canada, in a collaboration with community stakeholders, conducted an online survey from January to February 2021.
- Territories: 1%
- British Columbia: 17%
- Alberta: 7%
- Saskatchewan: 4%
- Manitoba: 5%
- Ontario: 40%
- Quebec: 12%
- Atlantic: 17%
Who participated
1,034 people who used drugs or alcohol in the 6 months prior to the survey:
- 53% were under the age of 40
- 85% white
- 61% cisgender female
- 85% have more than high school education
- 5% reported currently living with HIV
- 6% reported ever been told to have hepatitis C infection
Since the start of the COVID-19 pandemic
- Mental health: 60% felt their mental health was worse
- Food security: 42% experienced food insecurity
- Financial security: 56% reported a major or moderate impact on ability to pay bills
Substance use since the start of the COVID-19 pandemic
Among participants who used only alcohol and/or cannabis (n=451)
- 57% reported an increased use of cannabis
- 56% reported an increased use of alcohol
Among participants who used illegal drugs (n=845)
- Reported changed in use of illegal drugs:
- 57% increased use of heroin, fentanyl or other non-medical opioids
- 45% increased used of cocaine or crack
- Reported changes in substance use behaviours:
- 75% increase of different triggers for using
- 66% increase in using alone
Accessed, considered accessing or wanted to access
26% STBBI-related services
Experienced difficulty accessing:
- HIV, hepatitis C and other sexually transmitted infection (STI) testing
- pre-exposure prophylaxis (PrEP) and/or post-exposure prophylaxis (PEP)
- mental health counselling referral
39% harm reduction services
Experienced difficulty accessing:
- needle and syringe distribution programs
- drug checking services
- drug consumption rooms
30% substance use and treatment services
Experienced difficulty accessing:
- drug treatment in therapeutic communities
- drug treatment in outpatient mental health care centres
- drug treatment in psychiatric hospitals
Among all participants
Reasons why participants were not able to access STBBI, harm reduction, substance use and treatment services:
- Reduced hours or service closure
- Difficulty getting appointment or referral
- Difficulty contacting doctor or nurse
- COVID-19 public health measures
- Fear of, concern about or experienced stigma, discrimination, violence
- Fear of, concern about COVID-19 exposure
Acknowledgements
The authors gratefully acknowledge the valuable input and contribution of the survey participants. For more information, look for the Data Blog and the full-length report titled National Report: Findings from the Survey of the impact of COVID-19 on access to STBBI-related health services including harm reduction services for people who use drugs or alcohol in Canada.