A Dementia Strategy for Canada: Together We Achieve - 2022 Annual Report
Download in PDF format
(5.5 MB, 102 pages)
Organization: Public Health Agency of Canada
Date published: January 2023
Cat.: HP22-1E-PDF
ISSN: 2652-7805
Pub.: 220451
On this page
- Minister's message
- Introduction
- State of dementia in Canada
- Public Health Agency of Canada: Dementia investments
- Advancing dementia prevention
- Priorities for dementia research and innovation
- New directions for dementia research priorities for Canada
- Informing research with lived experience
- Sharing high-quality research results through guidance and training for care providers
- Assessment of dementia guidance available in Canada on treatment and care
- Dementia research efforts across Canada
- Strengthening efforts on quality of life
- Dementia and populations at higher risk
- Conclusion
- Appendix A: Overview of the national dementia strategy
- Appendix B: Aspirations for Canada's efforts on dementia from the national dementia strategy
- Appendix C: Map of PHAC investments – project details
- Bibliography
- Endnotes
Minister's message
It is my pleasure to share the 2022 annual report on the national dementia strategy with Canadians. Despite the continued challenges of the past year related to the COVID-19 pandemic and climate change-related emergencies, many organizations and individuals across our country continue to dedicate themselves to efforts that support progress on the strategy's three national objectives. These objectives remain central to the Government of Canada's investments in dementia-related initiatives: to move toward prevention, to advance therapies and find a cure, and to improve the quality of life of people living with dementia and caregivers.
In January 2022, the Government of Canada launched a successful national advertising campaign as part of our national public education initiative on dementia under the Dementia Strategic Fund. Awareness-raising activities focused on reducing stigma by helping Canadians to better understand dementia and to learn how to be supportive when interacting with a person living with this condition. This knowledge is essential to making our communities more inclusive and welcoming. Advertisements ran on television and digital platforms and in newspapers, with the digital ads shown more than 50 million times. Two well-known Canadians who have personal experience with dementia in their families supported the campaign through media interviews, resulting in a combined reach of over 21.5 million impressions across Canada.
Over the past few years, the Government of Canada has continued to develop new dementia-focused programs that support the strategy's national objectives. For example, the Dementia Community Investment has to date supported 21 community-based projects designed to improve the wellbeing of people living with dementia and caregivers and to increase knowledge about the dementia risk factors. These projects also undertake intervention research, enabling assessment of their effectiveness. This program also supports a knowledge hub to share lessons and results and enable collaboration to expand impact. The Dementia Strategic Fund (DSF) has supported 15 awareness raising projects to date across the country which are focused on risk reduction and making communities more dementia-inclusive including through addressing stigma. In this year's report, you will find details about these and other projects that are underway.
Recent public opinion research conducted for the Public Health Agency of Canada is providing greater insight into topics such as the experiences and knowledge of dementia care providers, what quality of life means in the context of dementia, and the knowledge, perceptions, motivations and actions of Canadians related to risk reduction. Some highlights from the results are shared throughout this year's report.
The Government of Canada continues to invest in surveillance projects that gather data to deepen our understanding of dementia in Canada and its impact. Through the Enhanced Dementia Surveillance Initiative, 10 projects have been funded to support new approaches to strengthen data on areas such as when dementia co-exists with other chronic conditions, dementia in long-term care settings, and risk factors. The data and evidence produced by these projects is expected to inform future public health actions to better support those living with dementia and caregivers.
Investment in research and innovation is essential to advancing progress in Canada on the national dementia strategy. In Budget 2022, the Government announced a new $20 million investment for the Canadian Institutes of Health Research to ramp up efforts to learn more about dementia and brain health, to improve treatment and outcomes for persons living with dementia, and to evaluate and address mental health consequences for caregivers and different models of care. Budget 2022 also provides $30 million for the Centre for Aging and Brain Health Innovation to accelerate innovations in brain health and aging. Combined with ongoing investments, Canada is continuing to contribute to global progress on building the research base in dementia as well as innovations that allow research results to support concrete outcomes.
The Government of Canada continues to support efforts to strengthen our health care system, including long-term care, incorporating lessons learned. It is a priority for Canada to be well-prepared for the next public health emergency by strengthening international collaboration and by improving our response systems at home. We also must strengthen preparations for the impacts of climate change, which has been shown to disproportionately impact older adults and people with pre-existing medical conditions that may impact mobility and cognition, such as dementia.
I will close by thanking all those who are focusing their efforts on dementia, whether it is through caring for and supporting those living with the condition, advancing more effective therapies and moving us closer to a cure or expanding risk reduction efforts. Together and every day, across all of our work and investments, we are making progress on the objectives of our national dementia strategy.
Introduction
A variety of efforts across Canada support progress toward the national dementia strategy's objectives on prevention, improved therapies and quality of life. These efforts are made by many different organizations and individuals. They include: community-based programming; many aspects of health care including guidance; research and innovation; data gathering; and, health promotion efforts that reduce the risk of developing dementia. As part of Canada's effort, increased federal investments in dementia-related initiatives are translating into activity that aligns with the strategy's national objectives. The chapter in this report on investments managed by the Public Health Agency of Canada provides a glimpse of projects now underway across the country.
Dementia is a term used to describe symptoms affecting brain function. It may be characterized by a decline in cognitive (thinking) abilities such as: memory; planning; judgement; basic math skills; and awareness of person, place and time. Dementia can also affect language, mood and behaviour, and the ability to maintain activities of daily living. Dementia is not an inevitable part of aging.
Dementia is a chronic and progressive condition that may be caused by neurodegenerative diseases (affecting nerve cells in the brain), vascular diseases (affecting blood vessels like arteries and veins) or injuries. Types of dementia include vascular, Lewy body, frontotemporal, Alzheimer's disease and mixed (a combination of more than one type). In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease.
Action to pursue the national objectives requires high-quality data and evidence and needs to be informed by lived experience to ensure it responds to notable gaps and reflects Canadians' priorities. This report shares the results of public opinion research Footnote 1 that have deepened knowledge about dementia in Canada, including about quality of life when living with dementia, dementia guidance and Indigenous peoples, and the perspectives and experiences of health care providers Footnote 2 who work with people living with dementia. The report also provides results from a 2022 dementia prevention study and includes key findings from analytical work on dementia guidance. A focus on populations identified as being likely to be at higher risk of developing dementia and/or to face barriers to dementia care continues this year, which includes information about Indigenous peoples and dementia guidance.
This year's report also provides an overview of the impact of the COVID-19 pandemic on people living with dementia as well as on the ability to maintain healthy behaviours associated with a reduced risk of developing dementia. It notes the need to improve the capacity to support people living with dementia during times of climate-change related emergencies such as extreme weather events. People living with dementia are likely to be at higher risk of adverse outcomes in both pandemic situations and climate change-related emergencies and efforts are underway to better understand how to mitigate these impacts and develop necessary resources. This annual report shares information that was current as of June 2022.Footnote 3
State of dementia in Canada
A Dementia Strategy for Canada: Together We Aspire includes ambitious aspirations for the future of dementia in Canada to inspire action from all Canadians to work toward achieving its national objectives. The 2020 annual report to Parliament was the first to present data points selected to shed light on key aspects of the state of dementia in Canada; this year, data points for all three objectives are together in a single chapter to provide insight into movement toward the objectives.
Objective: Prevent dementia
The data points on dementia prevention monitor risk factors among Canadians over time along with the rate of new cases (incidence). Later in the report, the prevalence of risk factors is broken down across provinces and territories. As well, these data points include responses from a 2021 public opinion survey of health care professionals related to their knowledge and access to information about dementia risk reduction. Footnote 4 Health care professionals such as family doctors and nurses have the opportunity to provide guidance related to risk reduction to their patients, making it important to understand their level of knowledge and whether there is adequate access to the tools and resources they need.
Dementia risk factors among Canadians
As rates among Canadians for modifiable dementia risk factors decrease and protective factors increase, the rate of new cases of dementia in Canada may continue to decrease. The data points below outline the age-standardized Footnote 5 prevalence of known dementia risk and protective factors among Canadians over two time points including the most recently available data (see Table 1). This year, one additional risk factor (drinking) is now moving in a better direction, while two risk factors (obesity and diabetes) are still trending in a worse direction. A neutral trend suggests that the risk or protective factor has not changed in a statistically significant way from one time point to the other.
| Dementia risk or protective factor | Percentage (%) of Canadians with factor (Year 1) | Percentage (%) of Canadians with factor (Year 2) | Trend | Source |
|---|---|---|---|---|
| % of population (aged 18+) that reports heavy drinkingFootnote 7 | 20.7 (2015) | 17.8 (2020) | BetterFootnote 8 | Canadian Community Health Survey, 2020; 2015 (custom analysis) |
| % of population (aged 20+) that reports having less than a high school education | 12.0 (2015) | 8.4 (2020) | Better | Canadian Community Health Survey, 2020; 2015 |
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | 24.2 (2012–13) | 23.5 (2017–18) | Better | Canadian Chronic Disease Surveillance System, 2017–18; 2012–13 |
| % of population (aged 18+) that reports being current smokers (daily or occasional) | 18.7 (2015) | 13.4 (2020) | Better | Canadian Community Health Survey, 2020; 2015 |
| % of population (aged 18–79) with elevated blood cholesterol | 18.4 (2014–15) | 14.0 (2018–19) | No significant change | Canadian Health Measures Survey, 2018-2019; 2014-2015 |
| % of population (aged 18–79) who meet physical activity recommendations by accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or moreFootnote 9 | 22.4 (2012–13) | 21.7 (2018–19) |
No significant change | Canadian Health Measures Survey, 2018-2019; 2012-2013 |
| % of population (aged 18–79) that reports obtaining the recommended amount of daily sleep | 61.8 (2009–11) | 64.9 (2014–15) | No significant change | Canadian Health Measures Survey, 2014-2015; 2009-2011 |
| % of population (aged 12+) that reports a "very strong" or "somewhat strong" sense of belonging to their local community (social isolation is a dementia risk factor)Footnote 10 | 68.0 (2015) | 69.7 (2020) | No significant change | Canadian Community Health Survey, 2020; 2015 |
| % of population (aged 20+) with diagnosed stroke | 2.6 (2012–13) | 2.6 (2017–18) | No significant change | Canadian Chronic Disease Surveillance System, 2017–18; 2012–13 |
| % of population (aged 20+) with diagnosed diabetes | 9.7 (2012–13) | 10.3 (2017–18) | Worse | Canadian Chronic Disease Surveillance System, 2017–18; 2012–13 |
| % of adults (aged 18–79) that are obeseFootnote 11(self-reported, adjusted BMI) | 25.7 (2015) | 27.8 (2020) | Worse | Canadian Community Health Survey, 2020; 2015 |
Dementia incidence
The age-standardized data shows that the rate of newly diagnosed cases of dementia has decreased between 2008–2009 and 2017–2018. However, as the population of Canadians over the age of 65 grows, the number of Canadians living with dementia is expected to rise. As of 2017–2018, almost 452,000 Canadians aged 65 years and older were living with diagnosed dementia, an increase of almost 10,000 since 2016–2017.Footnote 12
- In 2008–2009 there were 1,576 new cases per 100,000 Canadians aged 65+ years
- In 2017–2018 there were 1,418 new cases per 100,000 Canadians aged 65+ yearsFootnote 13
Health care professionals and dementia risk reduction
Health care professionals such as nurses and family doctors are often the first point of contact for people seeking more information on dementia risk reduction. Recent data suggests the majority of health care professionals in Canada consider themselves knowledgeable about dementia prevention and know where to find resources. Drawn from a 2021 survey, these data points provide a sense of the degree of understanding among health care professionals about the factors linked to dementia, their knowledge about resources and their awareness of actions that reduce the risk of dementia.Footnote 4
Overall, health care professionals assess themselves as more knowledgeable regarding dementia risk reduction compared with other categories of care providers such as personal care workers or caregivers.Footnote 14
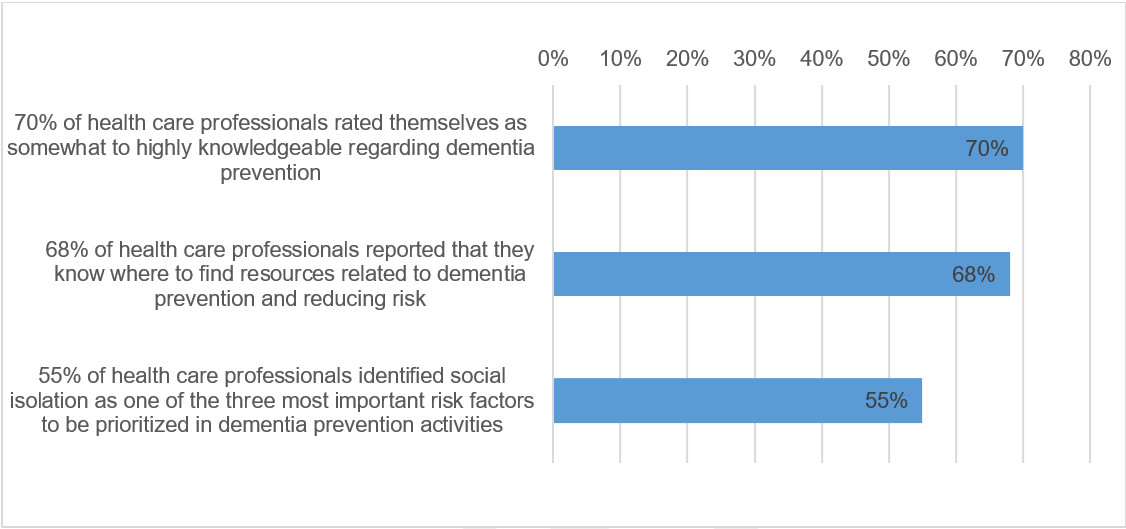
Figure 1 - Text description
- 70% of health care professionals rated themselves as somewhat to highly knowledgeable regarding dementia prevention
- 68% of health care professionals reported that they know where to find resources related to dementia prevention and reducing risk
- 55% of health care professionals identified social isolation as one of the three most important risk factors to be prioritized in dementia prevention activities
When asked to identify three risk factors to prioritize for prevention, health care professionals most often identified social isolation (55%), physical inactivity (38%) and depression (28%). These three factors, along with several others, are associated with an increased relative risk of dementia, see Table 4a. On a global scale, it has been estimated that people older than 65 who experience social isolation are about 60% more likely to develop dementia than those who do not. Similarly, the increased relative risk for dementia for people older than 65 who are physically inactive is 40%; and those over age 65 who experience depression are 90% more likely to develop dementia compared with those who do not.
Other dementia risk factors identified by health care professionals as being important across the lifespan include a low level of education (26%), alcohol consumption (25%) and traumatic brain injury (23%). Risk factors identified by health care professionals less frequently included hearing loss (12%), diabetes (9%), smoking (9%), hypertension (9%), obesity (7%) and air pollution (1%). (Livingston, 2020)
Objective: Advance therapies and find a cure
Investments in innovation and research help advance improved therapies and deepen understanding of potential causes of dementia. Data points for this national objective track dementia research spending by the Canadian Institutes of Health Research (CIHR) and the number of dementia research trainees supported by CIHR.
Dementia research spending
The CIHR is Canada's federal funding agency for health research and has 13 Institutes, including the Institute of Aging, that collaborate with partners and researchers to improve health and strengthen the health care system. This data point reports on CIHR's total investment in dementia research, including investigator-initiated research (e.g. funded through the Project Grant competition), research in priority areas (e.g. the Canadian Consortium on Neurodegeneration in Aging), and training and career support programs (e.g. fellowships). Canada's investments in research support all three objectives of the national dementia strategy.
| Year | Spending ($) |
|---|---|
| 2020–21 | approximately $49 million |
| 2019–20 | approximately $42 million |
| 2018–19 | approximately $40.8 million |
Dementia research trainees
Supporting and training the next generation of researchers is critical to advancing what we know about dementia. This data point reports on the approximate number of students/trainees engaged in dementia research through CIHR funding. This includes students and fellows who either received a training award (direct trainees), or received a stipend paid through researcher grants (indirect trainees).
| Year | Trainees (number) |
|---|---|
| 2020–21 | 389 |
| 2019–20 | 375 |
| 2018–19 | 359 |
Objective: Improve the quality of life of people living with dementia and caregivers
The data points below report on ratings of quality of life by people living with dementia and dementia caregivers, and on care provider perspectives related to stigma. They include levels of pain, depression and social interaction among people living with dementia receiving home care, as well as a comparison of distress between dementia caregivers and caregivers for those with other conditions.
Quality of life rating
A 2021 public opinion research project focused on deepening understanding of what quality of life means for people living with dementia. Footnote 16 The more than 500 respondents who participated were people living with dementia responding on their own or with the assistance of a caregiver, or current or recent caregivers responding on behalf of a person living with dementia to ensure the results were informed by lived experience.
Just over half of respondents rated quality of life positively. Almost a third responded neutrally, rating quality of life as "fair" and 13% responded that it was poor.
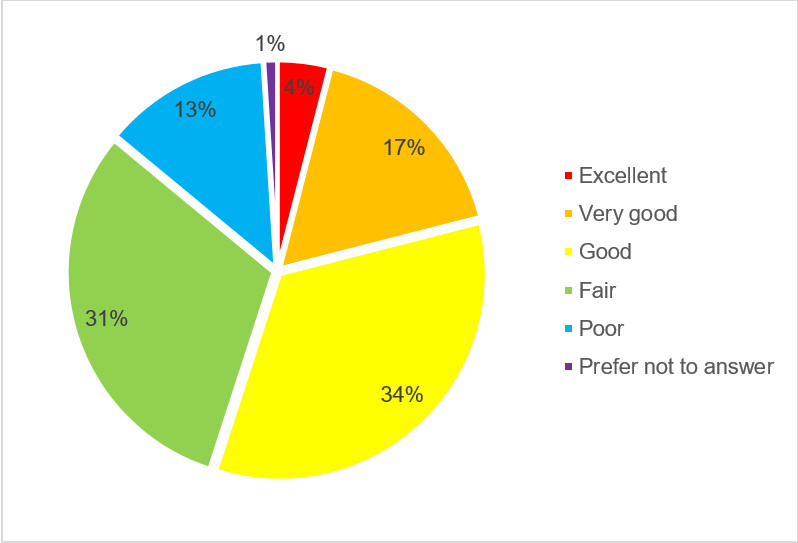
Figure 2 - Text description
- 4% responded with "excellent"
- 17% responded with "very good"
- 34% responded with "good"
- 31% responded with "fair""
- 13% responded with "poor"
- 1% responded with "prefer not to answer"
Care provider perspectives and experiences with stigma related to dementia
The perspectives of care providers Footnote 17 provide insight into the degree of stigma related to dementia in the health care system and the community. Stigma can come from inaccurate assumptions about the capacity of a person diagnosed with dementia and being unaware that symptoms can vary widely by individual and even by day. Care provider perspectives captured below include views about the ability of people living with dementia to work and remain independent.
- 51% of care providers agree that negative stereotypes about dementia are common within the health care system.
- 47% of care providers agree that someone living with dementia can sometimes continue to work for years following diagnosis.
- 73% of care providers agree that someone living with dementia can sometimes continue to live in their own home for years following diagnosis.
Depression, pain, and social interaction among people living with dementia in home care settings and caregiver distress
The 2022 report continues to track data points on depression, pain, and social interaction for people living with dementia receiving home care and on caregiver distress. Footnote 18 They suggest that most people living with dementia receiving home care engaged in activities of interest and had social interactions in 2020–21. However, nearly 34% experienced daily pain and nearly 25% showed signs of depression. Footnote 19 These statistics stayed relatively stable in 2020–21 compared with 2019–20, with the exception of the percentage of people living with dementia receiving home care experiencing reduced social interaction, which increased.Footnote 20
- 21.1% exhibit withdrawal from activities of interest and/or reduced social interaction.
- 24.9% display a potential or actual problem with depression, based on a depression rating scale.
- 33.8% experience daily pain (severe and not severe).
| Data point | Percentage (%) in 2018–19 | Percentage (%) in 2019–20 | Percentage (%) in 2020–21 |
|---|---|---|---|
| Exhibiting withdrawal from activities of interest and/or reduced social interaction | 18.3 | 19.1 | 21.1 |
| Displaying a potential or actual problem with depression, based on a depression rating scale | 24 | 24.8 | 24.9 |
| Experiencing daily pain (severe and not severe) | 34.6 | 34.6 | 33.8 |
Caregivers play a key role in supporting the quality of life of people living with dementia. However, this role is often demanding and can lead to distress, impacting physical, mental and emotional health. The data point below from 2020–21 measures distress encountered by caregivers Footnote 21 of people living with dementia who receive home care in contrast to caregivers who provided care to people without dementia who receive home care. Footnote 22 This statistic stayed relatively stable in 2020–21 compared with 2019–20.
- 36.6% of caregivers providing home care to people living with dementia experienced distress, compared with 18.5% of caregivers who provided care for someone without dementia.Footnote 19
Public Health Agency of Canada: Dementia investments
The Public Health Agency of Canada (PHAC) directly funds the implementation of key elements of A Dementia Strategy for Canada: Together We Aspire through the Dementia Strategic Fund, the Dementia Community Investment and the Enhanced Dementia Surveillance Initiative.
Dementia Strategic Fund
The Dementia Strategic Fund (DSF) supports efforts designed to pursue the strategy's national objectives on prevention and quality of life. These efforts include awareness-raising projects by organizations across Canada, work to improve access to and use of high-quality dementia guidance and information, and a national public education/awareness campaign.
DSF projects raising awareness about dementia across Canada
As of June 2022, the DSF was supporting 15 projects focused on raising awareness of actions that help prevent dementia, reduce stigma and support communities in becoming more dementia-inclusive. Additional projects are expected to be funded in 2022–23.
Some of the DSF projects encourage Canadians to adopt healthier behaviours to reduce their risk of developing dementia. Through the Luci program, a web-based application, Canadians can learn about dementia risk and protective factors and receive advice from counsellors to engage in a brain-healthy lifestyle. A project with Women's Brain Health Initiative is raising awareness through a brain health campaign that includes an interactive application focused on dementia prevention, alongside a podcast series and educational videos. Another risk reduction project led by S.U.C.C.E.S.S. is developing and delivering a culturally appropriate awareness and educational workshop series in Mandarin, Cantonese, Korean and Farsi to immigrant communities in Metro Vancouver.
Some of the efforts funded by the DSF are focused on dementia-inclusive communities in urban and rural areas, including one project led by the Rural Development Network that is piloting the implementation of dementia-inclusive initiatives and producing guides for rural communities in Alberta. Another led by Simon Fraser University is developing knowledge sharing resources to assess and create dementia-inclusive neighbourhood environments in Metro Vancouver and Prince George, British Columbia. As well, a team led by the Centre collégial d'expertise en gérontologie du Cégep de Drummondville in Quebec is identifying best practices for stigma reduction and dementia-inclusive communities. These best practices will be shared through videos and online training for the general population in St-Jean-sur-Richelieu.
Building capacity for awareness-raising initiatives
For some organizations, capacity building is a necessary first step to dementia awareness raising initiatives. In 2020–21, the Native Women's Association of Canada (NWAC) received funding from PHAC to undertake capacity building. NWAC successfully developed a distinctions-based understanding of the needs, attitudes and behaviours of First Nations, Inuit and Métis communities surrounding stigma and dementia, including the identification of existing community strengths and resources to address dementia.
This additional capacity enabled NWAC to work next toward developing and delivering a strengths-based photobook that illustrates the experiences of Indigenous people living with dementia and a toolkit for people living with dementia and caregivers with culturally specific information on stigma, its effects and tips to overcome it. The photobook and toolkit will be delivered through in-person and virtual workshops/webinars, with the toolkit also being made available in print.
Making a community more dementia-inclusive also means supporting people living with dementia in continuing activities they enjoy. Canada's National Ballet School's Sharing Dance with People with Dementia project, including its Dancer Not Dementia campaign, is increasing opportunities across Canada to participate in dance. Through dance, the project challenges dementia-related stigma while highlighting the creativity, joy, playfulness, community and connection of dancers living with dementia and their caregivers. Similarly, the Art Gallery of Hamilton is building on its Artful Moments program to share best practices and approaches that can be adopted by other museums and galleries to help them become more accessible and welcoming for people living with dementia.
How others interact with and perceive people living with dementia is a core aspect of dementia-inclusive communities. The Open Minds, Open Hearts project led by the Conestoga College Institute of Technology and Advanced Learning is fostering a sense of belonging among college students, people living with dementia and caregivers through guided intergenerational activities in educational institutions in British Columbia, Ontario and Quebec. As well, the Regional Geriatric Program of Toronto is delivering a multi-site education and coaching program on person-centred language to health care professionals working in acute care settings in Ontario to help reduce stigma linked to language, attitudes and practices, including how patients are described in medical records.
Some of the projects funded by the DSF focus on both risk reduction and quality of life for those living with dementia. The Cyber-Seniors intergenerational technology-training program in Ontario and New Brunswick is developing an online educational webinar series, a dementia awareness app and active learning centres where seniors can try out the latest techniques designed to facilitate the adoption of healthier behaviours to reduce the risk of dementia. The ABCs of a Healthy Brain project led by RésoSanté Colombie-Britannique is conducting awareness campaigns and providing information resources to Francophone minorities living in the Yukon, British Columbia, Alberta and Saskatchewan. A project led by the Dementia Society of Ottawa and Renfrew County is enhancing and evaluating an existing dementia-inclusive program that could serve as a model elsewhere in Canada. Activities include an interactive media campaign focused on brain health and dementia risk reduction. The project will use interactive virtual reality to complement existing training and an app to locate and rate dementia-inclusive businesses in the region.
Improving dementia guidance
To improve access to and use of high-quality dementia guidance in Canada, the DSF includes funding for the Dementia Guidelines and Best Practices Initiative. Dementia guidance refers to recommendations and advice in various formats including formal guidelines and best practice statements. A call for proposals for projects was launched in December 2021. As of the preparation of this report, proposals were under review. Applicants were encouraged to focus on populations identified as being likely to be at higher risk and/or facing barriers to equitable dementia care. The themes for the 2021 call were informed by analysis of the quality of dementia guidance available in Canada and engagement with dementia guidance users. Applicants were asked to focus on at least one of these themes:
- Dementia prevention
- Reduce stigma and encourage dementia-inclusive communities
- Person-centred support, communication and care
- Support in times of emergency such as pandemics and natural disasters
- Indigenous-led
The national awareness campaign
A national public education campaign in 2021–22 involved a variety of efforts to reach and educate Canadians about dementia, such as a national advertising campaign and a public relations tour with two public figures as spokespeople. The national advertising campaign, with a focus on reducing stigma, took place in early 2022. This multimedia campaign included a video ad highlighting how to interact in a supportive way with someone living with dementia while out in the community. The advertisements ran from January 17 to March 13 on television, digital platforms and newspapers across Canada. During this period, digital ads were shown 50.4 million times and users clicked on the ads a total of 137,600 times. Results from a survey following the campaign showed that 76% of participants felt the ad helped reduce negative perceptions of people living with dementia, 68% felt it clearly conveyed how to support people who live with dementia, and 63% felt that it provided new information. Average daily visits to the website increased from 79 before the advertising campaign to 2,441 during the advertising period. During the advertising period, there were a total of 136,700 visits to the Canada.ca/dementia website.
Two well-known spokespersons, Jay Ingram and François Morency, supported the campaign through media interviews and other activities. Both spokespeople have family-related experience with dementia. Their speaking tours resulted in 99 interviews and the resulting content appeared in media outlets with a combined reach of over 21.5 million impressions across Canada.
To further raise awareness about dementia in Canada, news articles and a radio spot about risk reduction and healthy lifestyle behaviours as well as an animated video to help reduce stigma have been available to media outlets since January 2021. Between January 2021 and March 2022, these awareness-raising products were integrated into local and national media channels with a reach of 15.5 million impressions across Canada.
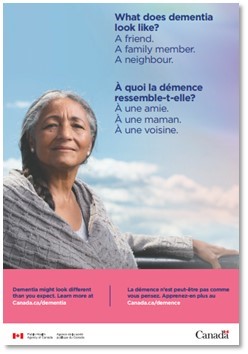
Figure 5 - Text description
What does dementia look like?
A friend.
A family member.
A neighbour.
À quoi la démence ressemble-t-elle?
À une amie.
À une maman.
À une voisine.
Dementia might look different than you expect. Learn more at Canada.ca/dementia
La démence n'est peut-être pas comme vous pensez. Apprenez-en plus au Canada.ca/demence
"Addressing misconceptions about dementia is an important step in reducing stigma, which can contribute to social isolation for people living with dementia and can lead to poorer health outcomes. Through initiatives such as the national dementia awareness campaign, we can create more supportive communities where people living with dementia are actively engaged and feel valued and respected as individuals."
— Theresa Tam, Chief Public Health Officer of Canada
As PHAC continues to create a variety of tools to support its efforts to raise awareness about dementia, a video portrait series featuring people living with dementia and their personal stories is being developed as part of a digital engagement campaign. PHAC is also developing a risk reduction campaign for next year.
Dementia Community Investment
PHAC's Dementia Community Investment (DCI) funds community-based projects that develop, test and scale up resources, information, and programs to improve the wellbeing of people living with dementia and caregivers, and to increase knowledge about dementia and its risk and protective factors. All projects funded by the DCI undertake intervention research to assess the effectiveness of the initiative and develop knowledge transfer and sustainability plans to help mobilize and share results.
The DCI has funded 21 community-based projects to date, which have undertaken a variety of initiatives such as developing a model for education and support for caregivers of people living with dementia that reflects participants' cultural heritage, beliefs, values and preferences, as well as promoting inclusive approaches that decrease barriers and increase support for 2SLGBTQI+ people living with dementia and their caregivers.
The DCI funded three new community-based projects from its 2020 solicitation, focused on providing virtual supports to address the impacts of social isolation experienced by people living with dementia and caregivers in the context of the COVID-19 pandemic. The Alzheimer Society of Ontario is adapting its Minds in Motion bilingual programming from in-person to include virtual delivery to better support people living with dementia and caregivers in Ontario. This includes increasing access to those living in rural areas. The eight-week, evidence-based program will be shared with all Alzheimer Societies across Canada. Similarly, McGill University's bilingual Dementia Education Program is being adapted into a virtual platform to educate and support caregivers of people living with dementia, including those living in diverse communities across Montreal and remote communities in Quebec. A third project is adapting an existing virtual intervention from the United Kingdom, the Computer Interactive Reminiscing and Conversation Aid (CIRCA). This intervention provides social engagement and meaningful activities for people living with dementia and caregivers and has been shown to enhance speech and recall from long-term memory while minimizing the impact of challenges related to short-term memory losses. This virtual intervention will reach urban, rural and remote communities across Ontario, Saskatchewan and British Columbia.
Two projects under the DCI have recently been completed. The BC Centre for Palliative Care's project focused on mobilizing and equipping community-based organizations to promote the engagement of people at risk of dementia, people living with dementia, and caregivers in Advance Care Planning (ACP). Tools, resources and training materials were developed to support 28 unique community-based organizations in British Columbia to deliver ACP activities for people living with early stages of dementia and their family and friends. This project involved the training of 131 staff and volunteers, with 85% of public participants reporting increased awareness and knowledge about ACP. SE Health's Research Centre focused on developing tools and processes to build stronger and more effective relationships among people living with dementia, caregivers and care providers. A tool called Our Dementia Journey Journal (ODJJ) was adapted collaboratively with Indigenous, rural and urban communities in British Columbia and Ontario into three versions (English, French and Indigenous) and a mobile app to improve communication, quality of life and relationships throughout the dementia journey.
Knowledge hub spotlight
The DCI also supports a knowledge hub, the Canadian Dementia Learning and Resource Network (CDLRN), led by the Schlegel-UW Research Institute for Aging (RIA). This hub facilitates a community of practice for all DCI projects, enabling them to build capacity, share findings, learn from each other and support collaboration. It is guided by a community advisory committee, which includes people living with dementia and caregivers, to ensure that lived experience is integrated into the work of CDLRN. The CDLRN website offers resources and information about each of the community-based projects.
CDLRN shares key findings from individual projects and broader lessons learned to inform dementia policy and programming across Canada (e.g. through newsletters, working groups, website resources, webinars and workshops). Building these connections will help ensure learnings from DCI investments are shared broadly with partners across Canada to benefit more Canadians living with dementia, caregivers, and the communities in which they live.
Key lessons learned from DCI projects
The CDLRN supports mutual learning among DCI projects and the wider community through sharing at events and annual reporting by DCI projects. Some key themes of lessons learned and best practices have emerged, such as developing tailored approaches in collaboration with diverse communities, as well as understanding how language and stigma can influence recruitment and participation in dementia projects.
- Several DCI projects have highlighted the importance of paying attention to language and culture. Notably, recent findings from an environmental scan (led by COSTI Immigration Services in Toronto) indicate that the ethnocultural and linguistic needs of people living with dementia and caregivers are significantly under-addressed in current dementia care and intervention practices. Incorporating cultural traditions has been highlighted as an effective way to help people living with dementia from diverse cultures feel comfortable and experience positive memories.
- Some DCI projects have also emphasized that the term "dementia" often does not exist in Indigenous languages. Instead, words that describe symptoms associated with dementia are often used. This can be a contributing factor to not accessing health and social services for those in the early stages of dementia. It can also contribute to a lack of Indigenous participation in community-based dementia projects. This underscores the need to raise awareness and to learn about and integrate Indigenous language, concepts, and perspectives in dementia-related projects, specific to each community, as well as the need for Indigenous community members to play a central role in designing, developing and delivering projects.
- Stigma has also been highlighted as an important theme among projects. While addressing ageism and stigma related to dementia is a responsibility of all Canadians, paying attention to privacy and confidentiality when working directly with people living with dementia and caregivers is critical to building trusting relationships with project participants.
- Some best practices have been highlighted for creating inclusive and safe spaces when engaging 2SLGBTQI+ people living with dementia and caregivers, such as leveraging existing 2SLGBTQI+ networks, using inclusive imagery, avoiding gendered language and not making unwarranted assumptions about gender and sexual orientation. It is also helpful to work directly with researchers and partners who identify as 2SLGBTQI+ to improve participation, recognizing that some 2SLGBTQI+ people living with dementia and caregivers may not trust organizations and institutions because of previous experiences of discrimination.
Enhanced Dementia Surveillance Initiative: Strengthening Canada's data
The Enhanced Dementia Surveillance Initiative (EDSI) funds projects that support the surveillance and data pillar of the national dementia strategy (see Appendix A, which provides an overview of the dementia strategy and its pillars). Surveillance and data offer insights into groups within the general population that are more impacted or more at risk to develop dementia. This information is key to guiding prevention efforts. It can also be used to inform the development of policies and programs, health care planning, and service delivery to meet the needs of people living with dementia and their caregivers.
Ten projects have been supported since the start of the EDSI, six of which are highlighted below. Through collaboration between PHAC, provincial and federal partners, as well as academic stakeholders, new approaches are being explored to collect and analyze data on topics such as risk factors for dementia, co-occurrence of dementia and other chronic conditions (i.e. comorbidities), and dementia in long-term care (LTC) settings.
Most of the EDSI projects will ultimately feed into the first and third objectives of the strategy. For example a project led by the Canadian Primary Care Sentinel Surveillance Network (Queen's University) resulted in a public access dashboard that presents valuable data on people living with dementia, including demographics, comorbidities, medications, health care use, to support researchers and public health professionals conducting dementia prevention and health care planning activities.
Improving data to support dementia prevention
Many of the ongoing EDSI projects aim to collect, analyze and report data on specific populations living with dementia as well as risk and protective factors. These data will help inform initiatives to prevent dementia or delay its progression.
Improving Indigenous data on dementia (McMaster University)
A first step to help prevent a condition at the population level is to know who develops it and what factors are associated with its development. A team at McMaster University has undertaken an extensive review of the literature and an environmental scan. They highlighted important limitations with existing strategies and data sources which make data-gathering about dementia in Indigenous populations in Canada more difficult. These limitations include incomplete coverage of older Indigenous populations, the lack of culturally safe cognitive assessment tools to appropriately diagnose dementia in Indigenous populations, and barriers to accessing health care. These limitations impact the ability to use existing data sources for surveillance, and this work will set the stage for future surveillance tools to more accurately identify Indigenous peoples living with dementia and inform community-based prevention and treatment.
A comprehensive and holistic approach to dementia surveillance in Canada (University of Waterloo)
A University of Waterloo project has developed a comprehensive and holistic model of dementia to inform surveillance. This model encompasses factors affecting the health and wellbeing of older adults across three levels: individual (e.g. age and sex), social (e.g. social support and family structure), and broader (e.g. public policies). Focus groups that informed the development of this model reflected diverse populations, inclusive of those with different cultural backgrounds, who identify as 2SLGBTQI+, or are from rural or remote areas in eight provinces and one territory. The components of this model will be compared with existing data sources across Canada to identify where new ones are needed to support future prevention efforts as well as treatment and care.
A microsimulation model for dementia projections (Statistics Canada)
In collaboration with PHAC, Statistics Canada is developing a microsimulation model of dementia, Footnote 23 a complex tool that produces long-term projections of the number of new and existing cases of dementia, mortality, risk factors, and associated health care costs among Canadians living with the condition. Projected estimates produced by this tool will enable policy-makers not only to investigate modifiable risk factors, but also to evaluate the impact of potential interventions and policy options. Statistics Canada will be publishing findings from this work, in addition to publicly releasing an application to showcase these projections and the impacts of interventions.
Improving data to support the quality of life of people living with dementia
A series of projects will build on the Canadian Chronic Disease Surveillance System (CCDSS), a collaborative network of provincial and territorial surveillance systems that is supported by PHAC and used to produce national surveillance data on dementia. Footnote 24 These projects will leverage the CCDSS data infrastructure to expand and enhance dementia surveillance and generate evidence for public health action aimed at improving the quality of life of people living with dementia.
Using health administrative data to describe comorbidities in people living with dementia (Institute for Clinical and Evaluative Science [IC/ES] in Ontario and three participating provinces)
Comorbidities add to the complexity of care and the overall health impacts associated with dementia. This project, led by IC/ES with the support of British Columbia, Prince Edward Island and Quebec, focuses on developing a common method to identify the presence and the sequence in time of other chronic conditions occurring among people living with dementia (comorbidities). Currently, there is little information on the subject. Early findings from Ontario indicate that adults over the age of 65 with dementia have more comorbidities than those without dementia and that there are important differences in the profile of specific comorbidities by age, sex and setting of care. This project will also assess the association between having multiple comorbidities and subsequent health care use and mortality. These data will help enable optimal management of dementia comorbidities to aid individuals to achieve a higher quality of life by potentially lessening the health impact of these comorbidities.
Collecting data on where people with dementia are living (independently led by three provinces)
This series of projects will examine where people with dementia live, what factors may predict the transition from the community to other settings, and finally, identify the possible data sources to enhance ongoing surveillance of dementia in LTC settings. Each province (British Columbia, Ontario, Quebec) will lead their own work and explore different approaches, given the databases available in their jurisdiction.
People with dementia may live within the community and in LTC settings. In fact, early findings from Ontario (IC/ES) indicate that approximately 80% of older adults (aged 65 years and older) have a history of dementia when admitted to LTC. Currently, routinely collected surveillance data cannot distinguish cases in the community versus cases in LTC, and the extent to which the CCDSS is able to identify all cases of dementia in LTC is not well documented. Early findings from British Columbia suggest that around 80% of those living with dementia in LTC are identified in both the CCDSS and a LTC database (Continuing Care Reporting System Footnote 25) in this jurisdiction, but that a portion of these people remains undetected in the CCDSS. To support jurisdictions where linking to other data sources to improve the identification of dementia cases in LTC is not currently possible, Quebec is piloting a "proxy" approach that will rely only on available information contained in the CCDSS.Footnote 26
Understanding the characteristics of individuals transitioning to LTC and establishing how many people with dementia live in the community compared with LTC is crucial for health system planning. Such data are also important from a quality of life perspective, to ensure appropriate resources are available to ensure optimal quality of life in each setting.
Public Health Agency of Canada investments across Canada
PHAC has funded many dementia-related projects supporting the national dementia strategy across Canada over the last several years. The map in Figure 6 highlights the broad spread of these initiatives supported through the Dementia Strategic Fund (DSF), the Dementia Community Investment (DCI), and the Enhanced Dementia Surveillance Initiative (EDSI). They include provincial and national surveillance projects along with community-based projects. They also include projects that raise awareness of dementia and promote dementia-inclusive communities, and projects that accelerate innovation in aging and brain health. The dots on the map represent areas of activity from 36 projects whose scope is focused on one or more provinces or territories but whose scope is not national. PHAC also supports 11 projects that are national in scope. See Appendix C for a list of projects.
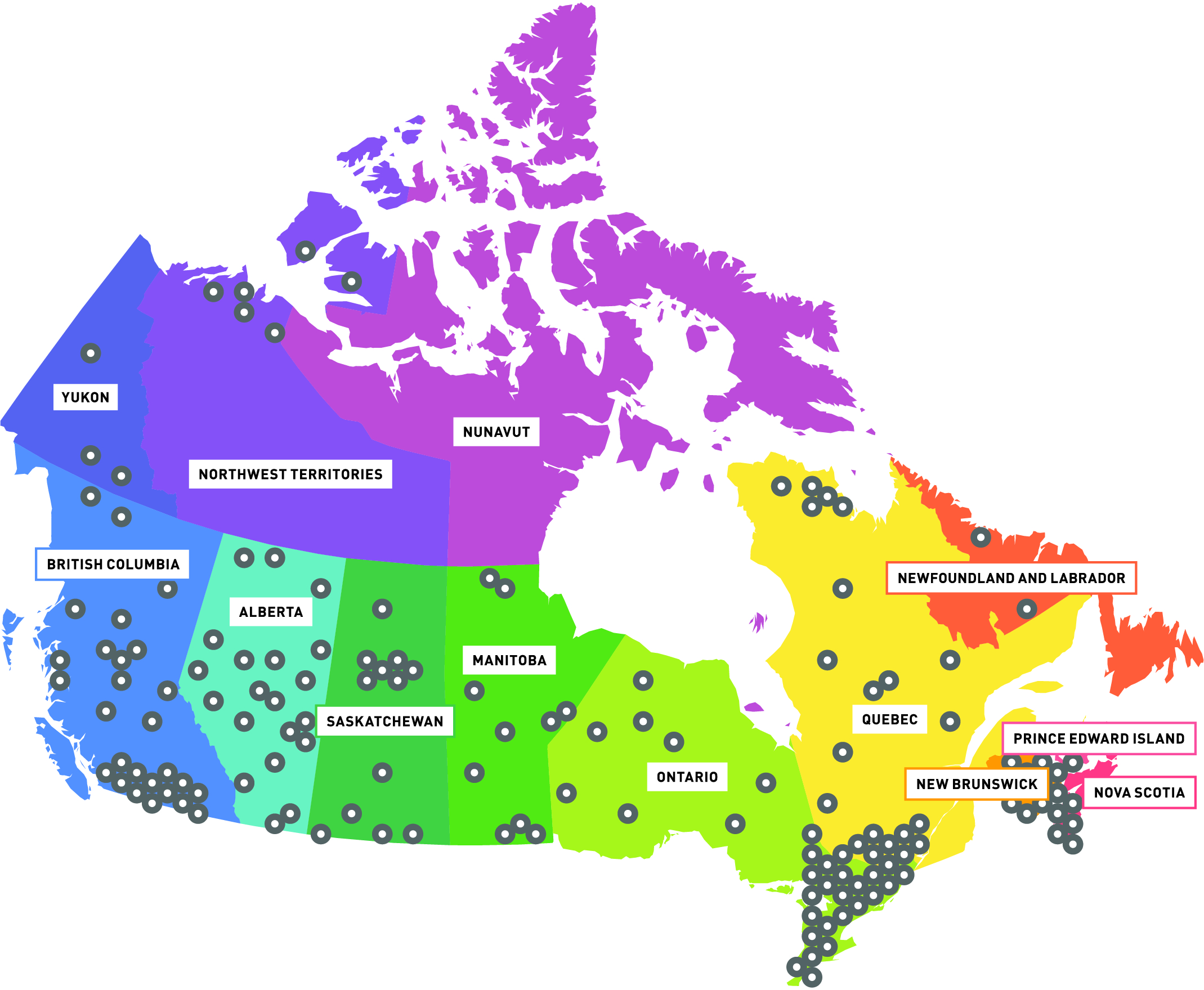
Description: Map of Canada with indicators on provinces/territories where PHAC has invested in a project (numbers seen in table 3 below).
| Total projects funded | National projects | Provincial projects | Number of project sites | |
|---|---|---|---|---|
| DSF | 15 | 3 | 12 | 54 |
| DCI | 22 | 4 | 18 | 68 |
| EDSI | 10 | 4 | 6 | 29 |
| Total | 47 | 11 | 36 | 151 |
| NL | PEI | NS | NB | QC | ON | MB | SK | AB | BC | YT | NWT | NU | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSF | 1 | 0 | 1 | 1 | 4 | 10 | 1 | 9 | 16 | 9 | 2 | 0 | 0 |
| DCI | 0 | 0 | 2 | 6 | 13 | 16 | 9 | 1 | 2 | 13 | 0 | 6 | 0 |
| EDSI | 1 | 1 | 2 | 2 | 6 | 5 | 2 | 2 | 2 | 5 | 1 | 0 | 0 |
| Total | 2 | 1 | 5 | 9 | 23 | 31 | 12 | 12 | 20 | 27 | 3 | 6 | 0 |
Advancing dementia prevention
As knowledge about dementia risk factors grows, efforts to reduce risk must be evidence-based to be effective. Examining the rates of these factors across Canada provides insight into where efforts may be most needed. Similarly, a better understanding the views and actions of Canadians about dementia risk and how knowledgeable and equipped care providers are about risk reduction will help to focus efforts and lead to a greater impact.
Dementia risk factors across Canada
Table 4 shows the levels of dementia risk and protective factors in Canada, broken down by province and territory compared with the overall national average. Some factors such as heavy alcohol drinking, education, obesity, smoking, physical activity and social isolation vary widely in some provinces and territories compared with the national average. For example:
- Diabetes prevalence estimates were higher in Manitoba, New Brunswick, Newfoundland and Labrador, Nova Scotia, and Ontario and lower in Alberta, British Columbia, Prince Edward Island, Quebec and the Yukon.
- Heavy alcohol drinking prevalence estimates were higher in Newfoundland and Labrador, the Northwest Territories, and Quebec and lower in Manitoba.
- Less than high school education prevalence estimates were higher in Manitoba, New Brunswick, Newfoundland and Labrador, the Northwest Territories, Nunavut, Prince Edward Island, and Quebec and lower in Alberta, British Columbia, and Ontario.
- Hypertension prevalence estimates were higher in Alberta, Manitoba, New Brunswick, Newfoundland and Labrador, Nova Scotia, Prince Edward Island, and Saskatchewan and lower in British Columbia, Quebec and the Yukon.
- Obesity prevalence estimates were higher in all the territories, New Brunswick, Newfoundland and Labrador, Nova Scotia, Prince Edward Island, and Saskatchewan and lower in British Columbia.
- Smoking prevalence estimates were higher in all the territories, Newfoundland and Labrador, Nova Scotia, Quebec, and Saskatchewan and lower in British Columbia.
- Stroke prevalence estimates were higher in Manitoba, Ontario, Prince Edward Island, and Saskatchewan and lower in Alberta, New Brunswick, Newfoundland and Labrador, Nova Scotia, Quebec and the Yukon.
The prevalence of some dementia protective factors differ in the following provinces and territories compared with the national average:
- Physical activity prevalence estimates were higher in Alberta, British Columbia, and the Yukon and lower in New Brunswick, Newfoundland and Labrador, Nunavut, Prince Edward Island, and Quebec.
- Strong social wellbeing prevalence estimates were higher in all the territories, Manitoba, New Brunswick, Newfoundland and Labrador, Nova Scotia, Prince Edward Island, and Saskatchewan and lower in Quebec. Social isolation is associated with a higher risk of developing dementia.
| Dementia risk factor | Source | National | AB | BC | MB | NB | NFL | NWT | NS | NU | ON | PEI | QC | SK | YK |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of population (aged 20+) with diagnosed diabetes | CCDSS (2017–18) | 10.3 | 9.6 | 10.0 | 11.7 | 11.3 | 11.5 | N/A | 10.5 | N/A | 11.2 | 9.9 | 8.6 | 10.3 | 8.4 |
| % of population (aged 18+) that reports heavy drinkingFootnote 7 | CCHS (2017–18) | 22.9 | 22.2 | 22.5 | 19.2 | 22.7 | 32.1 | 31.7 | 24.5 | 25.5 | 21.4 | 20.2 | 25.3 | 24.4 | 28.7 |
| % of population (aged 20+) that reports having less than a high school education | CCHS (2017–18) | 10.7 | 9.1 | 7.8 | 12.9 | 12.5 | 15.8 | 23.4 | 12.0 | 50.0 | 9.1 | 14.8 | 14.2 | 11.7 | 13.1 |
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | CCDSS (2017–18) | 23.5 | 24.7 | 22.3 | 27.4 | 27.4 | 30.6 | N/A | 26.5 | N/A | 24.0 | 24.4 | 20.5 | 25.4 | 21.1 |
| % of population (aged 18–79) that are obeseFootnote 11 (self-reported, adjusted BMI) | CCHS (2017–18) | 26.9 | 29.4 | 22.9 | 30.0 | 36.1 | 39.6 | 41.7 | 33.9 | 37.8 | 26.0 | 33.9 | 25.4 | 35.1 | 33.8 |
| % of population (aged 18+) that reports being current smokers (daily or occasional) | CCHS (2017–18) | 17.1 | 17.1 | 13.4 | 17.7 | 16.2 | 22.2 | 35.8 | 19.3 | 59.5 | 16.6 | 18.4 | 18.7 | 21.5 | 21.6 |
| % of population (aged 20+) with diagnosed stroke | CCDSS (2017–18) | 2.6 | 2.5 | 2.6 | 3.1 | 2.2 | 2.1 | N/A | 2.0 | N/A | 2.7 | 3.1 | 2.4 | 2.9 | 1.9 |
Note: For tables 4a and 4b, provincial and territorial differences observed with the CCDSS should be interpreted with caution. Even though differences are statistically significant, methodological differences may explain the patterns observed in addition to actual differences in the health status of the populations. For instance, differences in detection and treatment practices, as well as differences in data coding, remuneration models and shadow billing practices likely play a role in the patterns observed.
| Dementia protective factor | Source | National | AB | BC | MB | NB | NFL | NWT | NS | NU | ON | PEI | QC | SK | YK |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % of population (aged 18+) that report accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or moreFootnote 9 | CCHS (2017–18) | 56.8 | 58.8 | 65.7 | 54.4 | 52.2 | 51.5 | 57.1 | 56.0 | 45.9 | 55.8 | 52.1 | 53.8 | 57.0 | 69.6 |
| % of population (aged 12+) that reports a "very strong" or "somewhat strong" sense of belonging to their local community (social isolation is a dementia risk factor)Footnote 10 | CCHS (2017–18) | 68.9 | 69.8 | 70.5 | 73.6 | 75.5 | 77.4 | 81.4 | 71.8 | 80.8 | 70.7 | 73.4 | 61.4 | 74.4 | 80.2 |
The Weston Family Foundation awarded a $12-million research grant to the Canadian Longitudinal Study on Aging (CLSA) hosted at McMaster University, for a new initiative that will shed light on the many factors that influence brain health as we age, including lifestyle and the human microbiome. The human microbiome is the collection of microorganisms (for example, the bacteria, bacteriophage, fungi, protozoa and viruses) that live inside and on the human body.
The Healthy Brains, Healthy Aging Initiative will feature a cohort of 6,000 research participants currently enrolled in the CLSA. It marks the first time a national study of aging in Canada has introduced both brain imaging and microbiome analyses to investigate cognitive aging in the population over time. The goal of the six-year Healthy Brains, Healthy Aging Initiative is to enhance the CLSA platform with longitudinal data from magnetic resonance imaging (MRI) of the brain and microbiome analyses of the gut, to help researchers examine how diverse lifestyle, medical, psychosocial, economic and environmental factors as well as changes in the microbiome correlate with healthy aging outcomes. This data will be critical to the future development of screening and prevention strategies that promote brain health for aging Canadians.
Building our understanding of dementia risk reduction in Canada
Perceptions of dementia risk and action to reduce risk among Canadians
Public opinion research undertaken by the Public Health Agency of Canada (PHAC) in 2022 provides greater insight into the views and actions of Canadians related to dementia risk reduction. Footnote 28 These results suggest that over half of Canadians (52%) would rate their personal risk of developing dementia as moderate to high. Individuals belonging to groups identified as likely to be at higher risk rate their own risk as moderate to high slightly more often than all respondents, with Indigenous individuals at 57% and 2SLGBTQI+ individuals at 61% for example, while those with existing health conditions are at 61%. Common reasons among respondents for rating their risk as moderate to high include having family members who have or have had dementia (61%), lack of exercise (41%), or having one or more ongoing health conditions (34%).
Almost one in three Canadians (32%) rate their personal risk of developing dementia as low. Common reasons among respondents for rating their risk of developing dementia as low (32%) include challenging their brain regularly (72%), no one in their family having or have had dementia (64%) and maintaining healthy eating habits (58%). Common risk factors identified by all respondents to be likely to increase their own risk include sleep disruption (41%), loneliness/social isolation (42%), and depression (41%).
Despite more than half of Canadians rating their personal dementia risk moderate or higher, more than two-thirds (69%) of all respondents have not taken any steps to intentionally reduce that risk in the last 12 months. However, many did report healthy behaviours associated with a reduced risk such as challenging their brain (68%), eating healthy foods (62%) and being physically active (54%), although less than half of respondents reported being socially active (44%). About 60% feel they would like to be able to or need to do more to reduce their dementia risk. Of those (27%) who indicated they would not do more to reduce their risk, reasons include not knowing enough about what actions to take (33%), feeling it would not have an impact (13%), lacking the time to take steps (12%), and having health challenges that prevent them from taking steps (11%).Footnote 28
| Risk factor | Relative increased risk of developing dementia compared with someone without this risk factor |
|---|---|
| Early life (under 45 years old) | |
| Lower levels of education | 60% |
| Midlife (45 to 65 years old) | |
| Hearing loss | 90% |
| Traumatic brain injury | 80% |
| Hypertension | 60% |
| Obesity | 60% |
| Alcohol use (over 21 units per week) | 20% |
| Later life (over 65 years of age) | |
| Depression | 90% |
| Smoking | 60% |
| Social isolation | 60% |
| Diabetes | 50% |
| Physical inactivity | 40% |
| Air pollution | 10% |
Care providers and risk reduction
Health care providers may have the opportunity in their work to provide guidance about dementia risk factors. A 2021 survey of 1593 care providers Footnote 31 who interact with people living with dementia asked which three risk factors should be prioritized. Care providers most often selected well-recognized risk factors although there was some variation among different groups of care providers. Among all respondents, social isolation was the most common risk factor identified (59%). It was also highlighted as a risk factor by most of the care providers who participated in the individual interviews that were another part of this public opinion research project.
In the 2021 survey, health care professionals such as family doctors and nurses Footnote 32 identified social isolation (55%), physical inactivity (38%) and depression (28%) most often as risk factors to prioritize. These three factors have been identified as associated with dementia (see Table 5).Footnote 29 It is important to note that alternatively dementia may be a risk factor for depression; as well dementia and depression may have similar risk factors. Health care professionals were more likely to identify obesity (7%), smoking (9%), diabetes (9%) and alcohol consumption (25%) as risk factors to prioritize compared with other dementia care providers.
Depression was often selected by developmental service workers and personal care workers (41% each) as a priority risk factor while caregivers were more likely to identify social isolation (66%), physical inactivity (51%), hearing loss (17%) and hypertension (11%) compared with other care providers. Developmental service workers were most likely to identify traumatic brain injury (31%). Only 1% of health care professionals and personal care workers identified air pollution Footnote 33 as a risk factor for prioritization.
Availability and use of guidance related to dementia risk reduction
Another recent PHAC study gathered insights from dementia guidance users and those otherwise familiar with this guidance Footnote 34 through a questionnaire, roundtables and interviews. Most roundtable and interview participants Footnote 35 indicated in self-reporting that there is a lack of awareness among health care professionals and the public related to risk reduction and a need for more education. Among questionnaire participants, 60% were familiar with or use dementia guidance on risk reduction. Almost all of this guidance was related to healthy habits (e.g. diet, physical activity and cognitive stimulation) (88%), reducing risk factors like smoking and sleep disorders (83%), and managing chronic conditions linked to dementia (70%). Participants in approximately half of the roundtables indicated that more public education and resources are needed on this topic. Conducting public health campaigns, providing education in schools, and having an accessible educational toolkit and supportive resources were noted as ways to address gaps and barriers, and improve awareness, access and training regarding dementia risk reduction guidance
The study of dementia guidance users found that health care professionals need access to practical and efficient on-the-job training and quick reference information in one convenient location (such as fact sheets or an app), both of which need to include case examples and clear recommendations relevant to their practice. Education was highlighted as a key component to successfully disseminating guidance across Canada for all audiences, including the general public. Dementia guidance users also noted that it is important that evidence-based information is available in plain language, provided in multiple formats, located all in one spot, and tailored to various contexts and audiences. These strategies were noted as particularly important for dementia guidance related to prevention.
To inform effective action to reduce the risk of dementia, high-quality evidence-based guidance must be easy to access. A 2021 survey focused on care providers found that almost half of caregivers (48%), who are often family and friends, reported that they would not know where to find resources related to dementia risk reduction.Footnote 4 About one-quarter of health care professionals (23%) and personal care workers (27%) reported a similar lack of knowledge. The majority of developmental service workers (60%) and personal care workers (52%) felt they could use more preparation or training in reducing dementia risk. Almost half (46%) of health care professionals, who may be the most likely to need this information in their day-to-day work, felt the same.
As part of a recent analysis of existing dementia guidance in Canada, expert panel members suggested that additional efforts to improve knowledge about risk reduction could include knowledge translation activities Footnote 36 aimed at educating care providers about new and existing guidance to support the adoption and consistency of guidance use across Canada. These activities could take place in schools and through continued education and awareness raising efforts targeted at professionals throughout their careers.
Indigenous perspectives on dementia risk reduction
Indigenous individuals in Canada have been identified as likely to be at higher risk for developing dementia and facing barriers to care. In a 2021 survey that gathered Indigenous perspectives on dementia guidance, 34% of Indigenous participants who were not living with dementia and had not cared for someone living with dementia said they were somewhat to very knowledgeable about ways to reduce the risk. Footnote 37 Approximately three in five (62%) said they were a little to not at all knowledgeable about ways to reduce the risk. A third (39%) said that they have taken steps to reduce their own risk. Of those who had not taken any steps, the most common barrier identified to reducing risk was being unaware of what steps to take (57%). These respondents less frequently said the reason they have not taken any steps is because they do not consider themselves at risk (10%), they are not sure it will make a difference (8%), and they are not personally concerned about developing dementia (7%). Respondents to this survey commonly identified a diet lacking in healthy foods, social isolation, a lack of physical activity and harmful alcohol use as factors that come to mind that could increase their chances of developing dementia.
Care providers to an Indigenous person living with dementia more often than not said they were relatively knowledgeable about ways to reduce the risk of developing dementia with 51% and 73% of unpaid and paid care providers respectively identifying as somewhat to very knowledgeable. Almost half of unpaid care providers (45%) and 27% of paid care providers said they were a little to not at all knowledgeable about ways to reduce the risk of developing dementia. Over two-thirds of both paid and unpaid care providers (68%) agreed that there were gaps or barriers in dementia risk reduction recommendations and advice for Indigenous populations.
When looking for dementia guidance, recommendations or advice online, nearly two-thirds (64%) of Indigenous respondents who were not living with dementia and had not provided care to someone living with dementia said they would be likely or very likely to refer to advocacy organization websites and over half (53%) would likely or very likely go to health care expert websites. Slightly less than half of this segment would be likely or very likely to use federal government websites (49%), provincial or territorial websites (43%), or regional or local Indigenous health authority websites (41%). Most unpaid and paid care providers are likely to very likely to use advocacy organizations (67% and 74% respectively) and health care expert websites (51% and 68% respectively).
Dementia and the genetic link
In Canada and globally, genetic factors are known to play one of two roles in the emergence of dementia. The less common role is when genetic inheritance determines a dementia outcome. The more common role is when genetic factors elevate the risk of developing a dementia-causing disease. In the latter case, genetic risk is one of many dementia risk factors, including several that can be modified through healthy lifestyles and behaviours. Recent studies have shown that taking action on some of these lifestyle risk factors can have a notable impact on dementia risk reduction. Footnote 38, Footnote 39, Footnote 40 A study in 2019 exploring the link between genetic risk and lifestyle found that overall only 1.23% of those with a high genetic risk eventually developed dementia compared with 0.63% with a low genetic risk. Footnote 41 However, those with a high genetic risk and a lower level of healthy behaviours were almost three times as likely to develop dementia. In other words, while genetics may heighten the risk of developing dementia, evidence suggests that acting to reduce other risk factors can still have an impact on lowering risk.Footnote 29 Regardless of one's genetic risk, having a healthy lifestyle such as not smoking, regular physical activity, healthy diet, and moderating alcohol consumption along with a good level of cognitive reserve (i.e. early life education, mid-life substantive work complexity, late life leisure activities, and late life social networks) is associated with a lower risk of developing dementia. Footnote 42, Footnote 43
PHAC's 2022 public opinion research on dementia prevention found that genetics is the risk factor most likely to come to mind for respondents when asked what may increase the likelihood of developing dementia (34%).Footnote 28 Further, when asked about their own perceived level of risk and the reasons for that perception, genetics was commonly mentioned. Among the 52% of respondents who felt their own risk of developing dementia is moderate to high, having family members who have or have had dementia was given as a reason by 61%. Among the 32% of respondents who felt their risk of developing dementia is low, almost two-thirds (64%) selected having no one in their family having or having had dementia as a reason. Similarly, a 2021 study found that almost one in four Indigenous respondents (23%) identified genetics as one of the first three risk factors that come to mind when asked about what increases their chances of developing dementia.Footnote 37
While genetic risk was a common reason identified by participants as informing their rating of their own personal risk in a 2022 survey,Footnote 28 studies suggest that it is not a direct cause in most cases of dementia.
- Alzheimer's disease (AD) is the most common form of dementia, accounting for 60-80% of all dementia cases in Canada. Footnote 44 It is estimated that between 15–25% of the general population carries at least one copy of the APOE ɛ4 gene (which increases the chance of developing AD three to fourfold) Footnote 45 and 2–3% are estimated to carry two copies of that gene (which further increases the risk of developing AD nine to fifteenfold). Footnote 46, Footnote 47
- The second most common form of dementia is vascular dementia which accounts for 15-20% of all cases in North America. Footnote 48 This form is typically not inherited. However, underlying conditions, such as high blood pressure or diabetes, may be inherited along with genes that increase the risk of conditions that lead to vascular dementia, like heart disease or stroke.Footnote 29
- Other types of dementia are much rarer in Canada. For these types, genetic risk may play a larger role. However, the likelihood of them being inherited is never more than 50% (rarer types of dementia such as Huntington's disease can be up to 50%),Footnote 38 behavioural variant frontotemporal dementia is 40%, Footnote 49 dementia with Lewy bodies is 10%, Footnote 50 semantic dementia is less than 5% Footnote 51 and young-onset AD is less than 1%.Footnote 52
The impact of the COVID-19 pandemic on dementia risk factors among Canadians
Research is exploring how the COVID-19 pandemic has reduced opportunities for exercise and social activity and increased feelings of loneliness, isolation, anxiety and stress that have challenged Canadians' abilities to maintain positive mental health. Alcohol use, which is linked to depression, has been identified as a common coping mechanism during the COVID-19 pandemic. A lack of physical activity, social isolation, harmful levels of alcohol consumption and depression are risk factors for developing dementia.
Physical activity
Physical activity in children and youth can have life-long benefits by helping to maintain a healthy weight, develop cardiovascular fitness, and reduce the risk of developing chronic conditions in later life, such as dementia. Footnote 53, Footnote 54, Footnote 55 In the early weeks of the COVID-19 pandemic, physical activity levels declined among some populations and increased in others. As of April 2020, 4.8% of children aged 5–11 and 0.6% of youth aged 12–17 were found to be meeting Canada's 24-hour movement guidelines. This represents a significant drop in physical activity levels compared with pre-pandemic, when the proportion of Canadian children and youth aged 5–17 who met physical activity recommendations had been between 12.7% and 17.1%. Footnote 56 As of October 2020, during the second COVID-19 wave, the number of children aged 5–11 who met the guidelines dropped further to 4.5%. Footnote 57 For youth aged 12–17, 37.2% met the Canadian physical activity recommendations in fall 2020, compared with 50.8% of youth in fall 2018.Footnote 58
Physical activity recommendations
Children aged 5–11
- At least one hour of moderate to vigorous intensity physical activity daily
- Vigorous intensity activities at least three days per week
- Activities that strengthen muscle and bone at least three days per week (Public Health Agency of Canada, 2019a)
Youth aged 12–17
- An hour every day of moderate to vigorous intensity activity
- Vigorous intensity activities at least three days a week
- Activities that build muscles and bones at least three days a week (Public Health Agency of Canada, 2019b)
There were no significant changes in physical activity noted among adults aged 18–64 overall, though results varied depending on whether individuals were working from home.Footnote 58 While those working at home due to the COVID-19 pandemic appeared to be able to transition to other forms of physical activity, such as at-home workouts or recreational walks, total physical activity minutes remained less than those who did not work from home (40.7 minutes per day compared with 49.8 minutes per day). For adults aged 65 and over, physical activity levels increased by almost 5% in 2020 compared with 2018 (from 35.4% to 40.3%).
Social isolation
Some Canadians have reported a sense of loneliness during the COVID-19 pandemic, particularly younger Canadians. Data on loneliness among Canadians aged 15 and older during the COVID-19 pandemic (collected for the first time between August and September 2021) indicates that 23% of youth aged 15–24 experienced loneliness, compared with 15% of those between the ages of 25 and 34. Footnote 59 Women were particularly susceptible, with almost a third (29%) of women aged 15–24 experiencing loneliness compared with 18% of men aged 15–24. Among those aged 25–34, 16% of women reported feelings of loneliness compared with 15% of men. Adults aged 65–75 were least likely to report experiences of loneliness (9%), followed by 14% of those aged 75 and older.
Alcohol consumption
Researchers have been exploring links between social isolation and alcohol consumption as there is evidence of alcohol consumption being used during the COVID-19 pandemic as a coping strategy for feelings of loneliness, isolation, stress, and boredom. Footnote 60, Footnote 61, Footnote 62 Excessive alcohol use in mid-life is a risk factor for developing dementia.
About one-quarter (24%) of Canadians reported increased alcohol consumption during the COVID-19 pandemic, with stress, boredom and loneliness contributing to the increase, while 22% said their consumption had decreased.Footnote 60 CIHR's COVID-19 and Mental Health (CMH) Initiative found that more Canadians (especially those aged 40–49, those reporting increased anxiety, and those reporting feelings of loneliness) reported an increase in alcohol use (23%) than those that reported a decrease in alcohol use (11%). Footnote 63 The number of Canadians reporting no change in alcohol use was slightly higher, at 65%. As well, the number of hospital stays for harm caused by substances such as alcohol, opioids, stimulants and cannabis between March and September 2020 increased by 4,000 stays across Canada, compared with the same period in 2019. Footnote 64 The relationship between stress, loneliness and increased alcohol use was also noted among Canadians living in New Brunswick and Nova Scotia, where research indicates that about 12% of respondents reported more frequent drinking during the COVID-19 pandemic, and 25%–40% reported increased stress, loneliness and hopelessness.Footnote 65
Depression
For several years up to 2016, approximately 5.4% of Canadians aged 18 and over experienced a major depressive episode each year. Footnote 66 Findings released in September 2021 from the Survey on COVID-19 and Mental Health (SCMH) indicate a substantial increase in depression among Canadians during the COVID-19 pandemic: 25% of Canadians aged 18 and older experienced symptoms of depression, anxiety or posttraumatic stress disorder (PTSD) in spring 2021, rising from 21% in fall 2020. Footnote 67 The majority (94%) of those experiencing depression, anxiety or PTSD also reported having feelings of loneliness or isolation, physical health problems, and/or challenges in personal relationships. These results were consistent between spring 2021 and fall 2020, and were reported more often among those aged 18–24 (83%), 25–44 (80%) and 45–64 (70%) compared with those aged 65 and older (54%).
Poorer mental health outcomes have also been noted for older adults who were unable to participate in social and physical activities during the COVID-19 pandemic. Footnote 68 Adults (45 and older) were found to be twice as likely to develop depressive symptoms during the COVID-19 pandemic, mainly due to loneliness and COVID-19 stressors. Footnote 69 Among caregivers (including but not exclusive to those providing care to someone living with dementia), more frequent depressive symptoms were reported during the COVID-19 pandemic, particularly among those providing care at home versus those who cared for someone in a healthcare institution or who cared for someone in another household. Footnote 70 A study from the Canadian Longitudinal Survey on Aging Footnote 71 suggests that efforts to respond to challenges and stresses related to the COVID-19 pandemic should include, for example, increased opportunities for safe social participation and access to telemedicine, as well as online and telephone support services.
Budget 2021 provided $100 million over three years to support the mental health of Canadians affected by the COVID-19 pandemic. In addition, an investment of $9.2M was announced to support a range of distress centres across the country, including in rural and remote areas. This investment will support centres that provide crisis support for specific populations, including seniors, Indigenous communities, 2SLGBTQI+ populations and racially and linguistically diverse communities. The Government of Canada also released a fact sheet entitled Coronavirus Disease (COVID-19): Taking Care of Your Mental Health with tips as well as contact information for the Hope for Wellness line and Talk Suicide Canada.
"Being alone to do everything is hard physically and mentally…during COVID. Very isolating."
- Family/friend caregiverFootnote 4
COVID-19 and cognitive health
Globally, research is underway to explore the link between COVID-19 infection and potential consequences on brain health, including increased dementia risk. Evidence has been found of elevated blood biomarkers of brain degeneration in COVID-19 patients, Footnote 72 as well as changes to brain structure, Footnote 73 brain inflammation and impaired "brain circuitry", Footnote 74 in some cases similar to those with Alzheimer's disease. It has been suggested that one in three of those who contract COVID-19 (particularly severe COVID-19) will eventually be diagnosed with a psychiatric or neurological condition. Footnote 75, Footnote 76 Cognitive deficits were experienced by approximately 17.6% of COVID-19 patients, loss of memory by approximately 28.3%, and reports of difficulty concentrating ranged from 22–28%.Footnote 77
Delirium and dementia have an interconnected relationship, where people living with dementia have a higher risk of developing delirium, and the occurrence of delirium is a risk factor for developing dementia. Delirium is also one of the most common early symptoms of coronavirus infection in people living with dementia. A small study of 148 patients with COVID-19 admitted to an intensive care unit at Michigan Medicine from March 1 to May 31, 2020 found that almost a quarter (24%) of those experiencing delirium during hospitalization later screened positive for delirium at home, 23% demonstrated signs of cognitive impairment and 12% screened positive for depression within two months after discharge. Footnote 78 For those with severe COVID-19, delirium appears to be a common complication experienced by approximately 65%–80% of those in intensive care. More recently, a study investigating brain changes in 785 UK Biobank participants (aged 51–81) found a greater reduction in grey matter thickness and greater changes in markers of tissue damage, as well as greater reduction in global brain size, with infected participants showing greater cognitive decline compared with those who were not infected with COVID-19 during the study.Footnote 73 While some changes in grey matter thickness or volume are normal over time as people age, they can also be a feature of dementia. Footnote 79 Researchers are also exploring the link between tissue damage to the regions of the brain responsible for smell (resulting in a loss of smell) and the development of dementia.Footnote 80
Budget 2022 included approximately $4 million over three years to detect and understand the wider impacts of the COVID-19 pandemic in relation to chronic disease surveillance; the long-term effects of post COVID-19 condition; impacts on health care utilization; and the interactions between infectious diseases and chronic conditions. Budget 2022 also committed $20 million over five years, starting in 2022–23, for the Canadian Institutes of Health Research to support additional research on the long-term effects of COVID-19 infections on Canadians, as well as the wider impacts of the COVID-19 pandemic on health and health care systems.
Furthering dementia risk reduction across Canada
Examples of the variety of efforts underway across Canada to reduce Canadians' risk of developing dementia include non-pharmacological methods to improve cognitive function, such as encouraging daily exercise during periods of bed rest, and using web-based tools and other innovative approaches (e.g. wrist-worn devices).
- Researchers at the Ottawa Hospital Research Institute and the Bruyère Research Institute are raising awareness of dementia risk through the Project Big Life Dementia Calculator. This web-based tool is designed to help community-dwelling adults who are 55 years of age and older to better understand their brain health and what they can do to reduce the risk of developing dementia. Since its launch in June 2021, this online calculator has been used by more than 900,000 unique visitors nationally and internationally. The tool consists of an interactive online questionnaire followed by a personalized report of the respondent's dementia risk and the modifiable risk factors contributing to their risk.
- Sleep-wake disturbances are associated with increased cognitive decline and dementia risk. Those who are at risk of developing dementia and those living with dementia commonly have these disturbances. Ryan Falck from the University of British Columbia is using machine learning and data from the United Kingdom Biobank to assess dementia risk from the 24-hour sleep-wake cycle, using a wrist-worn actigraphy, which is similar to a wristwatch that records movement. This initiative is expected to benefit those at greater risk for cognitive decline and dementia through earlier detection, identifying the need to increase risk reduction efforts and possibly slow the pace of cognitive decline.
- Older adults may experience prolonged bed rest as a result of injury, surgery, or hospitalization. This period of bed rest may have a negative impact on cognitive and physical abilities. Ensuring daily exercise during bed rest may counteract these negative consequences. Teresa Liu-Ambrose and Guilherme Moraes Balbim from the University of British Columbia are undertaking a project to promote the development of novel interventions and rehabilitation strategies to support cognitive health among older adults during transitions in care.
- Benoit Mulsant and his team from the Centre for Addiction and Mental Health and the University of Toronto have been working on a randomized controlled trial using a combination of cognitive remediation and brain stimulation on 250 older adults with major depression since 2015. The goal of this study is to improve cognitive function, slow decline, and ultimately prevent the onset of mild cognitive impairment or Alzheimer's disease.
Priorities for dementia research and innovation
Canada's researchers are continuing to advance our understanding of dementia therapies, both domestically and internationally. Since its inception in 2000, the federal organization Canadian Institutes of Health Research (CIHR) has supported research on dementia-related topics, including research on the latest preventive, diagnostic and treatment approaches. Importantly, provincial health research organizations and other key health charities and foundations such as the Alzheimer Society of Canada also support research on dementia. Over the past several months, CIHR has been consulting on priorities for dementia research to renew the vision for its future.
New directions for dementia research priorities for Canada
In fall 2020, the CIHR Institute of Aging embarked on an extensive consultation process to assess the evolution of the dementia research landscape and identify new directions and bolder horizons for dementia research.
The CIHR Institute of Aging consulted with more than 550 diverse stakeholders, including the Alzheimer Society of Canada, Heart and Stroke Foundation, Weston Family Foundation, national and international dementia researchers, Indigenous health researchers, and other key partners. These public consultations involved people living with dementia and caregivers, reflecting the national dementia strategy's aspiration that people living with dementia and caregivers are active participants and partners in dementia research. The consultation process allowed for a more inclusive approach to defining research priorities.
Highlights of the key priorities that emerged:
- Ensuring issues related to health equity are considered throughout the research process is critical. This will help to ensure that findings from dementia research support the breadth of individuals who are diagnosed so that they can 'live well with dementia'.
- Advancing the health and wellbeing of First Nations, Inuit, and Métis Peoples, particularly ensuring that all dementia research studies are culturally safe and accessible.
- Supporting effective and innovative approaches for knowledge mobilization and implementation of research findings should be a priority to enable the rapid translation of dementia research findings into new treatment and care options.
- Increasing the amount of research on the identification and reduction of risks that can result in age-related cognitive impairment to inform the development of programs to mitigate risk and improve brain health.
- Including people with lived experience of dementia and their caregivers in every stage of the research process so their needs are prioritized.
The insights gleaned from the process will be used to inform the future directions and work in this area.
New federal investments in brain health and dementia
Budget 2022 announced a new $20 million investment over five years, starting in 2022–23, for CIHR to ramp up efforts to learn more about dementia and brain health, to improve treatment and outcomes for persons living with dementia, and to evaluate and address mental health consequences for caregivers and different models of care.
Budget 2022 also announced an additional investment of $30 million over three years, starting in 2022–23, to the Public Health Agency of Canada, for the Centre for Aging and Brain Health Innovation (CABHI) to help accelerate innovations in brain health and aging. This builds on a previous federal investment of $44M to establish CABHI from 2015–21. CABHI is a collaboration of health care, science, industry, not-for-profit and government partners who seek to support the cognitive, emotional and physical wellbeing of aging populations. It offers an integrated suite of programs to help accelerate the innovation-to-commercialization process by providing financial support for promising innovation projects, facilitating co-development with end-users (e.g. patients, caregivers, health care providers) and offering tailored services for innovators (e.g. scientific advice, training in innovation and health systems, developing procurement options and marketing plans). CABHI-supported innovation projects cover a range of issues including supporting aging at home, cognitive health, caregiver support, care coordination, financial health and wellness, as well as cross-cutting themes focusing on the health and wellbeing of Indigenous, diverse, official language minority and rural communities, promoting social inclusion, and preventing stigma and elder abuse.
Informing research with lived experience
Along with recent CIHR consultations, public opinion research continues to confirm that people living with dementia and dementia caregivers are interested in learning more about current treatments for dementia, as well as about dementia research, both in Canada and abroad. Footnote 81 To contribute to the effectiveness of therapies, people living with dementia and dementia caregivers should be active participants throughout research projects. Stigma can sometimes be a barrier to participation in research, including negative and perhaps inaccurate perceptions about the abilities of people living with dementia among researchers themselves.
Enhancing the participation of people living with dementia and caregivers in research
The Flipping Stigma on its Ear Toolkit enables people living with dementia, caregivers, health care professionals and researchers to recognize and respond to stigma and discrimination. The toolkit was designed by people living with dementia as part of a participatory action research project. By tailoring content to researchers, this initiative is helping to address stigma within the research community with the goal of increasing involvement of people living with dementia in all stages of research.
"People living with dementia have led our project, providing unique insight and perspective and showing the importance of the research process itself being more inclusive."
– Jim Mann, Advocate living with dementia
"The Flipping Stigma on its Ear Toolkit is being shared across Canada and internationally with community centres, church groups, family doctors and nurses, and others. People are excited by the toolkit, saying it has made them more confident and more committed to engaging with people living with dementia."
– Alison Phinney, UBC researcher
The Alzheimer Society of Canada Research Portal and Citizen Reviewer programs help connect people with lived experience to research studies and develop therapies and programs, allowing for active engagement and development using a person-centred, human rights lens. The Research Portal lists active projects across Canada that are recruiting participants. The Citizen Reviewer program gives people living with dementia an equal voice in assessing the relevance of dementia research that is funded through the Alzheimer Society of Canada Research Program.
Jennifer Bethell and Katherine McGilton from the University Health Network in Toronto are leading the Engagement of People with Lived Experience of Dementia (EPLED) program in association with the Canadian Consortium on Neurodegeneration in Aging (CCNA). This program seeks to enable meaningful and active involvement of people living with dementia and dementia caregivers in all aspects of CCNA research. An advisory group of people living with dementia with diverse backgrounds from across Canada informs this effort.
Sharing high-quality research results through guidance and training for care providers
To be put into action, research results must be translated into guidance and tools that are easily accessible for care providers and others. Current evidence-based information on therapies and treatments can be difficult to find for people living with dementia, caregivers and other dementia care providers.Footnote 4, Footnote 82 Additionally, research findings indicate that more resources are required to train health care professionals regarding best practices in treatment and management as well as the need for more time and supports to implement dementia guidance.
In a 2021 engagement of dementia guidance users, most of the caregivers who participated reported that dementia guidance related to treatment and management is not easy to obtain and that people living with dementia and caregivers often do not know where to go to get reliable information regarding treatment and management of dementia, especially right after receiving a diagnosis.
During the roundtable and interviews that were part of the 2021 study, participants noted a lack of time and human resources to effectively train health care professionals and implement best practices (e.g. in both community practice and long-term care), leading to inconsistent treatment and management of dementia across the country. Almost a quarter (24%) of questionnaire participants reported a lack of dementia guidance for specific emergency situations such as pandemics, evacuations, and for first responders (i.e. paramedics, firefighters, police) and 37% of questionnaire participants reported that they have adapted their services and programs to better handle emergencies.
Public opinion research conducted in 2021 also found that many care providers, including caregivers, believe they could benefit from more training. The 2021 survey found that more than half (54%) of personal care workers feel they could use more training on the treatment and care of someone living with dementia. As well, about four in ten developmental service workers, first responders, or health care professionals reported they could use more training on treatment and care. These findings suggest that making evidence-based guidance more available to health care providers is key to improving therapies and treatment, ensuring those living with dementia are benefitting from the timely integration and adoption of research findings in clinical practices and community supports.
To contribute to improving access to and use of high-quality dementia guidance, the Public Health Agency of Canada launched a call for proposals through the Dementia Guidance and Best Practices Initiative in December 2021 for projects to address gaps in dementia guidance by developing, adapting or updating high-quality guidance and/or improve its access, understanding and implementation.
Assessment of dementia guidance available in Canada on treatment and care
A recent assessment of the quality of the development processes for dementia guidance available in Canada for treatment and care developed between 2010 and August 2020 has helped to identify areas where there are notable gaps in guidance. Footnote 83 Topics for which moderate and significant gaps were identified are represented in the table below.
Guidance elements were included in the assessment of the availability of high-quality guidance if they met the AGREE Global Rating Scale criteria, which indicates the overall quality of the guideline development methods and completeness of reporting. Footnote 84 The assessment concluded that there is ample guidance for: pharmacological management strategies; providing information and communicating with people living with dementia and caregivers in care-related decisions; considerations for administering antidepressants or drugs when one or more comorbidities are present; when to recommend changes in medication, changes in dosing or stopping medications to evaluate a patient's response; when to co-manage a patient's care with dementia specialists; and involving people living with dementia and clinicians in advanced care planning.
A number of moderate gaps in guidance were identified, including: non-pharmacological management strategies; input and coordination for people living with dementia and caregivers in care-related decisions; insomnia and sleep disorder management strategies when one or more comorbidities are present; assessment tools and considerations to evaluate a patient's response to treatment and management; holistic and individual care plans for advanced care planning; swallowing and feeding assessments; medication and symptom management during palliative or end of life care; and risk mitigation strategies to avoid common risks.
Significant gaps in the guidance identified included: pharmacological and non-pharmacological management strategies when one or more comorbidities are present; aspects of evaluating a patient's response to treatment and management; managing transitions to different settings; aspects of advanced care planning; supporting people living with dementia when admitted to the hospital; some considerations for care strategies during palliative or end of life care; and needs considerations during services and facilities design to avoid common risks such as falls, negligence and abuse.
| Topics | Moderate gap | Significant gap |
|---|---|---|
| Optimal non-pharmacological management strategies | ||
| Cognitive, sensory and recreational activities | ✔ | N/A |
| Dementia-friendly community/environment setting | ✔ | N/A |
| Exercise | ✔ | N/A |
| Group activities | ✔ | N/A |
| Art therapy, music and/or dancing | ✔ | N/A |
| Non-pharmacological approaches should be used first | ✔ | N/A |
| Occupational and/or rehabilitation therapy | ✔ | N/A |
| Person-centred approaches | ✔ | N/A |
| Other (dental and oral health, practice programs, proper nourishment and balanced diet, sleep management) | ✔ | N/A |
| How people living with dementia and caregivers should be involved in decisions related to their care | ||
| Advanced planning and decision-making | ✔ | N/A |
| Supports for them | ✔ | N/A |
| Their input and coordination | ✔ | N/A |
| Key considerations for pharmacological and non-pharmacological management strategies when one or more comorbidities are present | ||
| Diagnosis and assessment | N/A | ✔ |
| Other (strategies for individuals with depression) | N/A | ✔ |
| Insomnia/sleep disorder management | ✔ | N/A |
| Hospital admission | N/A | ✔ |
| Palliative or end of life care management | N/A | ✔ |
| How and when a patient's response to treatment and management should be evaluated | ||
| Follow-up visits time and frequency | N/A | ✔ |
| Assessment tools and considerations | ✔ | N/A |
| Caregiver's burden assessment and monitoring | N/A | ✔ |
| Care plan creation | N/A | ✔ |
| Most effective ways of managing the transition between different settings | ||
| Managing transition between care settings | N/A | ✔ |
| Needs and wishes during transitions | N/A | ✔ |
| Key considerations for advanced care planning | ||
| Holistic and individual care plan | ✔ | N/A |
| Other (quality of life and supports for caregivers) | N/A | ✔ |
| Key considerations for supporting people living with dementia when they are admitted to the hospital | ||
| Key considerations for supporting people living with dementia when they are admitted to the hospital | N/A | ✔ |
| Most effective care strategies during palliative or end of life care | ||
| Anticipatory healthcare planning | N/A | ✔ |
| Swallowing and feeding assessment | ✔ | N/A |
| Best-interest decision-making | N/A | ✔ |
| Other (general palliative care management and ensure flexibility) | N/A | ✔ |
| Medication and symptom management | ✔ | N/A |
| Most effective risk mitigation strategies that can be taken to avoid common risks | ||
| Needs considerations during services and facilities design | N/A | ✔ |
| Driving assessments and recommendations | ✔ | N/A |
| Other (pain assessment, risk of falls management, and negligence and signs of abuse) | ✔ | N/A |
| Admission to hospital planning | ✔ | N/A |
| Protection (incapacitated) requirement | ✔ | N/A |
Dementia research efforts across Canada
Efforts to advance dementia research include the exploration of innovative solutions and improved measures of the impact of dementia that incorporate lived experience.
- Falls and fear of falling are common among those living with dementia. Erica Dove at the University of Toronto is developing an engaging and accessible exercise video game ("exergame") for people living with dementia or mild cognitive impairment. The aim of the game is to improve balance and reduce fear of falling, which keeps people living with dementia active and engaged. People with dementia, caregivers, health care professionals, and game developers are helping to create the new game, with work beginning in June 2022. The project will benefit people living with dementia or mild cognitive impairment, families, and service providers by raising awareness about fall rehabilitation for people living with dementia.
- A new measure that will incorporate the preferences of caregivers when evaluating dementia impact is being developed and will be available in English, French and Spanish. Ayse Kuspinar from McMaster University is working alongside caregivers of people living with dementia from Canada and the United States to create a CAregiver REported and weighted Dementia outcome measure (CARED). Guidelines for this measure will integrate the experiences of caregivers, building on their knowledge of the person living with dementia and their experience observing the progression of dementia symptoms.
Strengthening efforts on quality of life
The national objective to improve the quality of life for people living with dementia and caregivers has become even more important as the impacts of the COVID-19 pandemic continue. Exploring the concept and experience of quality of life by seeking the perspectives of those living with dementia and dementia caregivers informs and helps to focus efforts in this area. This chapter shares results from recent public opinion research along with an overview of some of the lessons learned and responses to the COVID-19 pandemic.
Deepening our understanding of quality of life
As the World Health Organization notes, individual assessments of quality of life are subjective and made in the context of diverse cultural and value systems and are informed by individual goals, expectations, standards and concerns. Footnote 85 To inform our understanding of what quality of life means for people living with dementia through lived experience, PHAC conducted public opinion research in 2021.Footnote 16 Participants were people living with dementia (some assisted by caregivers) and current or former caregivers. This research was designed to capture a first-hand perspective. Results reflect the perspectives of people living with dementia and/or caregivers gathered through 40 in-depth interviews and 556 survey responses. The results also capture perspectives within the COVID-19 pandemic context.
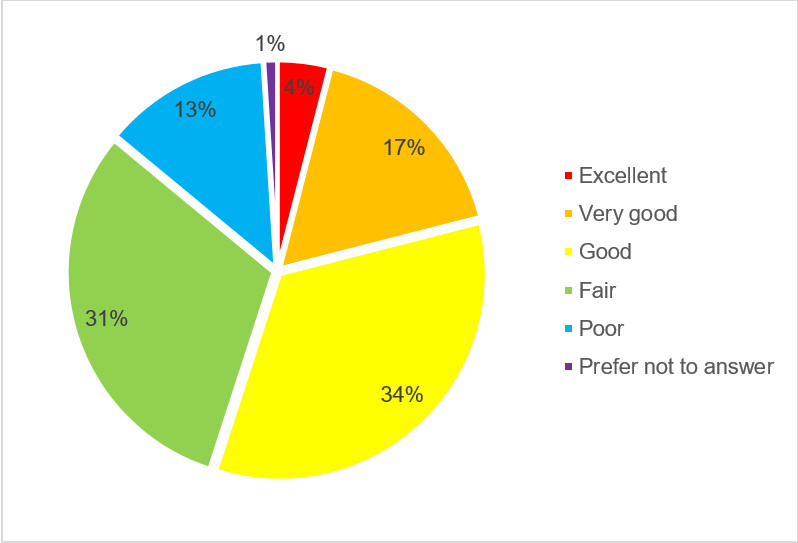
Figure 7 - Text description
- 4% responded with "excellent"
- 17% responded with "very good"
- 34% responded with "good"
- 31% responded with "fair""
- 13% responded with "poor"
- 1% responded with "prefer not to answer"
Quality of life ratings and factors
Rating quality of life
A majority rated quality of life as good or better (55%), while slightly less than half rated it as less than good (44%). People living with dementia who completed the survey on their own were more likely to rate their quality of life as good or better (70%). Conversely, current caregivers (48%) and former caregivers who provided care before the COVID-19 pandemic (46%) were more likely to rate the quality of life as fair or poor.
Factors contributing to quality of life
When asked to identify factors they see as generally having the most impact on quality of life, approximately half of respondents noted good physical health (51%), having frequent support and visits with family and friends (51%), and feeling comfortable in their surroundings (51%).
Additional factors mentioned include:
- Good mental health (48%)
- Being able to stay in their own home for as long as possible (48%)
- Being independent in their daily living needs such as preparing food and doing laundry (47%)
- Having a sense of purpose (45%)
- Living with loved ones such as family and friends (43%)
- Not having to worry about money (42%)
- Being able to move around their community as much as they want or need (41%)
- Being able to be close to nature or enjoy the outdoors (35%)
- Feeling like they belong to a community (27%)
- Being able to participate in religious or spiritual activities (21%)
"The lack of community, I guess, is the thing that detracted me most from my quality of life."
– Person living with dementia
A few interview participants suggested that quality of life is largely influenced by interaction with care providers, not just for physical care, but also as a means of engagement. Sufficient education and training for care providers, including caregivers, can help.
"The best thing they could possibly do for patients, especially for people who take care of their own [family] at home as long as possible, is more education as to the severity of the disease and the unpredictability of it. If I would have known a lot more about dementia, let's say two years ago, I would have been better prepared to give [her] a better quality [of life]."
– Caregiver assisting an individual living with dementia as a participant in the interview
Interview participants also highlighted the importance of safety and security, freedom, pets, participating in activities, sleep and travel. Some interview participants also talked about the stigma and negative perceptions associated with dementia.
"We have purposely kept it quiet. I feel that you can't help start to act differently. I don't want friends to suddenly be looking for problems. So, I have just told my sister and a close friend because I need that support. I have asked everybody to keep quiet. I don't think there's any need to know until other people notice something."
- Person living with dementia
Survey respondents were also asked to rate the current status of eleven different aspects of their own situation that are important to quality of life while living with dementia. The most positively rated factors were the relationship with family and friends (42%), access to health services (35%) and finances (29%). Of the aspects rated, those related to autonomy tend to be rated the lowest, such as the ability to move around freely in their community (16%), socialize with others (15%) and engage in hobbies and leisure (14%) along with physical health (17%) and mental health (16%).
Quality of life and the COVID-19 pandemic
When this study took place, the COVID-19 pandemic had been affecting the lives of Canadians for more than a year. The vast majority of respondents reported that the pandemic had had a negative impact on quality of life while living with dementia (84%), including one-third (32%) who describe the effect as very negative.
Among survey respondents who said the person living with dementia was aware of the COVID-19 pandemic and had an unpaid caregiver, almost seven in ten (69%) said the caregiver was not seen any less as a result of the pandemic. However, interview participants said the most important change since the COVID-19 pandemic seemed to be the decrease in physical contact and in-person visits.
"Dementia is making her world smaller. COVID has made it even smaller. But we're trying to keep her in her home and the world is opening as big as possible using technology."
- Current caregiver (interview)
Many of those interviewed described the disruption of services and activities, including missing the regular support group meetings and church services they attended. Most of all, they missed the opportunity these activities provided to socialize in a setting that was comfortable.
Challenges faced by care providers during the COVID-19 pandemic
As care providers (both paid and unpaid) play an integral role in supporting people living with dementia, the Public Health Agency of Canada (PHAC) conducted public opinion research to better understand their perspectives, experiences and knowledge.
When asked about the impact of the COVID-19 pandemic on the care or support provided to people living with dementia, communications and in-person care were noted as among the areas most affected. Half of the health care professionals (51%) and developmental service workers (50%) reported changing how they communicated with patients, typically moving to virtual methods.
A lack of staff was most often noted as the most challenging part of providing care or support to people living with dementia during COVID-19. This was identified by 49% of personal care workers, 45% of health care professionals, 41% of developmental service workers and 38% of first responders. Further, health care professionals (36%) reported having less time to spend with the person receiving care (e.g. due to increased workload, changes in staffing). In long-term care and acute care settings, understaffing and related burnout were described by interview participants as significant and compromising to the quality of care – leaving little to no time to connect with dementia residents or patients. The absence of family and volunteers to assist with care also contributed to the challenge.
Among caregivers, approximately half reported that visitation restrictions (54%) and the loss of activities available to the person they provide care to (49%) were among the most challenging parts of providing care during the COVID-19 pandemic. Interview participants described the impacts on support programs that provided stimulation for those living with dementia and respite programs for caregivers. These restrictions limited options for participation, making it difficult to maintain the usual activities that provided enjoyment and daily structure pre-pandemic.
"The separation from family was terrible. Patients lost their only connection to the world, their engagement and stimulation, and the presence of people who care about them. It contributed significantly to the decline of many."
- Physician
"I am limited to when and how often I can see her. With her living in a centre, I was hoping she would have more interaction [with those around her], but with COVID they can't [interact in that way]."
- Caregiver
"All outings are gone and that is so unfortunate since it is an activity, and stimulates [those living with dementia] and adds structure and they enjoy it."
- Direct case manager
The majority (87%) of respondents reported about the person living with dementia having had negative feelings (for two weeks or more at a time) or experiences in the year prior to this 2021 survey. Over half felt isolated (59%), sad (55%), or anxious (54%) for an extended period of time.
"I think it's changed gradually over the 10 years, but I noticed other people pulling away from my mom more than the other way around… that became very isolating."
- Caregiver assisting an individual living with dementia as a participant in the interview
Most respondents (85%) also reported challenges and difficult experiences in the past year. Over half (53%) reported difficulty communicating needs to others and four in ten reported people talking to the caregiver rather than to the person living with dementia even though the latter individual was present (39%). (Ekos Research Associates Inc., 2021)
Finance Canada Budget 2022 tax credits for home accessibility/home renovations
Tax measures proposed in Budget 2022 support housing options for seniors and persons with disabilities Budget 2022 proposes to:
- Double the qualifying expense limit of the Home Accessibility Tax Credit to $20,000 for 2022 and subsequent tax years. This will mean a tax credit of up to $3,000—an increase from the previous tax credit of up to $1,500—for qualifying accessibility renovations or alterations for seniors and eligible persons with disabilities.
- Introduce a Multigenerational Home Renovation Tax Credit, which would provide up to $7,500 in support for constructing a secondary suite for a senior or an eligible adult with a disability. Starting in 2023, this refundable credit would allow families to claim 15% of up to $50,000 in qualifying renovation and construction costs incurred in order to construct a secondary suite.
Care provider perspectives on quality of life
Another recent PHAC research project focused on the perspectives of care providers also explored the concept of quality of life through in-depth interviews.Footnote 16 These discussions confirmed that quality of life is likely to mean different things to different people and that its elements can be expected to vary depending on the nature of symptoms. For those living with milder symptoms, the important aspects of a good quality of life may include staying active, such as continued engagement in physical and recreational activities and social connection. Most participants suggested that a higher quality of life may include living among familiar surroundings and remaining at home as long as possible. For some people living with more advanced symptoms, participants described quality of life as coming from activities such as sitting by a window or outside, or hearing their favourite music.
Many care providers in the study perceive quality of life to be associated with the quality of dementia care provided. It was often noted that the best situation is when the person living with dementia has caregivers who are able to support them appropriately at their current stage of dementia. This might mean family checking in on and bringing food to an individual during the early stages of dementia, as well as monitoring the situation closely for the progression of symptoms. This might also mean caring for them in the same home, keeping them in an environment they are comfortable in and know well, and taking them to participate in social activities.
"(It's) about meeting them where they are. If their dementia is mild, and they have a good support system, they can have a good quality of life. [For] someone with more [severe] dementia [who] needs more care, [this could mean] a place with more recreation activities … [with] people who are well trained and understand their needs so that they are not trying to reorient them … causing them stress. You want to see that they are happy, engaged in activities or the people around them, and have a bit of a social life, be it family or friends."
- Personal care worker
Some participants noted that the broader community has a role to play in the engagement of people living with dementia. This would require a more widespread and deeper understanding of the nature of dementia and how to communicate in a supportive way with people living with dementia.
"They won't reach out and do that (engage) for themselves, someone else has to do it for them. That is why community is so important and has so much of a role to play. Everyone in the community can play a role in keeping people [living] with dementia engaged and active, but you also have to understand [how] to communicate appropriately."
- Caregiver (interview)
Forward with Dementia
Forward with Dementia is an initiative that seeks to support people living with dementia and caregivers following diagnosis, and the health and social care providers who care for them. It includes a website (in English and French) and an awareness raising campaign created to address stigma by challenging negative perceptions surrounding dementia. The website has three main goals: to offer suggestions for health care providers on how to communicate a diagnosis, to provide a sense of hope that people with dementia can live well, and to enhance supports for people following a dementia diagnosis. A positive diagnosis experience can impact how well people living with dementia and caregivers can move forward with adjusting to the diagnosis and enjoy quality of life.
Co-designed in collaboration with people living with dementia and those who support them, the website's content is tailored for three distinct audiences: people living with dementia, caregivers, and health and social care providers. Among the resources offered by the website are articles to break down the stigma surrounding dementia, practical resources such as checklists and worksheets, and stories from people with lived experience. The Forward with Dementia campaign focuses on how to live well with dementia and promotes the website through webinars and presentations, media such as radio and newspapers, and social media.
Forward with Dementia is currently being tested in parts of Ontario as well as Quebec and New Brunswick. It is the result of a three-year international research project with Australia, the Netherlands, the United Kingdom, and Poland.
Lessons emerging from the COVID-19 pandemic
In recent years, Canadians have faced many unexpected and unprecedented changes to their daily lives, resulting from evolving public health recommendations in response to the COVID-19 pandemic. Such changes can be particularly challenging for some populations, including those living with dementia. The pandemic has also had a significant impact on Canada's health care system and workforce, especially those living and working in long-term care, where the majority of residents as of 2015–16 (69%) are living with dementia. Footnote 86, Footnote 87 The mortality rate among long-term care residents resulting from the COVID-19 pandemic has been high compared with that of the general population, Footnote 88 particularly in the initial months and those providing care in long-term care settings have reported exhaustion and burnout.Footnote 89
People living with dementia were particularly impacted by the COVID-19 pandemic: From March through August 2020, long-term care residents, the majority of whom are people living with dementia, accounted for more than 80% of all reported COVID-19 deaths, Footnote 90 and more than 10% of Canada's total cases were resulting from infections among long-term care staff. Footnote 91 Between January 2020 and February 2021, dementia was listed as a pre-existing condition on the death certificate of 41% of the women and 31% of the men who died due to COVID-19, higher than any other pre-existing condition. Footnote 92 As of early March 2021, long-term care homes continued to account for the greatest proportion of outbreak-related cases and deaths (7% of all cases and more than 50% of all deaths).Footnote 93
Learning from challenges: Long-term care
While provinces and territories are primarily responsible for delivering long-term care, the federal government is working collaboratively with these governments to improve the quality and availability of long-term care and to support training and better wages for personal care workers. For example, the Government of Canada announced a $3 billion investment, starting in 2022–23, to support provinces and territories in their efforts to ensure standards for long-term care are applied and permanent changes are made.
In spring 2021, the Standards Council of Canada (SCC), Canadian Standards Association (CSA Group) and Health Standards Organization (HSO) announced a collaboration to develop two complementary National Standards of Canada for long-term care (LTC). Developed by these expert standards development organizations and arms-length from government, these new standards will take into account lessons learned from the COVID-19 pandemic and incorporate the latest evidence-informed, people-centred requirements of quality care and services. The standards will also address both the delivery of safe, reliable and high-quality care (HSO), and the safe operating practices and infection prevention and control measures in LTC homes (CSA Group). HSO and the CSA Group have completed extensive consultations, including a 60-day public review period of their draft LTC standards. Both organizations expect to release their final LTC standards by late 2022.
The federal government has also provided funding to Healthcare Excellence Canada for its LTC+ initiative. The goal of this initiative is to better position participating LTC facilities and retirement homes to prevent and manage any future outbreaks. Participating teams receive seed funding to support needed improvements, access to training sessions and materials, and coaching on the implementation of the program's key components. The Government of Canada's funding has helped meet the demand for the program, which now covers more than 1,500 facilities.
The Government of Canada committed up to $1 billion for a Safe Long-term Care Fund to help provinces and territories protect people in long-term care and support infection prevention and control. Provinces and territories are able to use this funding to improve infection prevention and control in facilities, including to assess infection prevention and control readiness, infrastructure improvements (e.g. making improvements to ventilation) and hiring additional staff or raising wages. This funding is conditional on the development and publication of clear action plans by provinces and territories that include performance metrics and list specific investments in infection prevention and control measures, with an emphasis on three priority areas: wages, infrastructure, and readiness assessments. A list of signed agreements can be found online.
The health care workforce and the COVID-19 pandemic
One of the largest burdens of the COVID-19 pandemic has fallen on Canada's health care workforce, with related impacts on people living with dementia and caregivers. For example, preliminary results of Statistic Canada's 2020 Nursing and Residential Care Facility Survey Footnote 94 indicate that long-term care homes have experienced more staffing challenges than other facilities: 77% reported an increase in the number of overtime hours; 71% reported an increase in absenteeism; and 85% reported other staffing challenges. Footnote 95 Over 50% of long-term care homes reported staffing shortages in key roles (e.g. directors of care, nurses or personal care workers) and one-third reported shortages in personal protective equipment (PPE) in 2020. In recognition of exhaustion and burnout in Canada's healthcare workforce, the HESA Standing Committee on Health adopted a motion in February 2022 to study how the federal government can facilitate the recruitment and retention of physicians, nurses, nurse practitioners and other health care providers for the public healthcare system; including a focus on rural and northern communities. Footnote 96 As of July 2022, 22 briefs have been submitted to the committee, including a brief by the Neurological Health Charities Canada.
Many people living with dementia who reside in long-term care rely on caregivers to provide essential support through daily care tasks, emotional support and advocacy. In addition to the staffing challenges experienced by long-term care homes, COVID-19 visitor restrictions prohibited access of caregivers to long-term care facilities to help with these essential supports. A Calgary-based study of caregivers for people living with dementia living in long-term care in Canada conducted in June–July 2020 found that the majority (83%) of caregivers indicated that the restrictions made it difficult, if not impossible, to maintain the level of care they had been providing prior to the COVID-19 pandemic. Footnote 97 Visitor restrictions have also been associated with accelerated cognitive decline and increased responsive behaviours. Footnote 98, Footnote 99
Healthcare Excellence Canada's Essential Together project promotes supportive, open access programming with curated evidence-informed tools and resources and multi-modal learning opportunities for health and care organizations to help support the safe re-integration of caregivers in health and care settings, such as long-term care. From Healthcare Excellence Canada's Essential Together website, organizations can:
- Access Learning Bundles with tools and resources that can be adapted to implement policy guidance
- Fill out an organizational self-assessment to identify strengths and areas for improvement to safely welcome caregivers
- Join Essential Together Huddles that create an open and safe space to support learning from and connecting with others who are facing similar challenges
- Access dedicated coaching and other supports (for organizations that formally join the program)
- Link to the latest evidence and environmental policy scans for what is happening across Canada
- Commit to the Essential Together pledge and be recognized for their commitment to the values of person- and family-centred care and partnership in care
Protecting people living with dementia during climate change-related emergencies
Older adults and those living with disabilities, including people with dementia, are at increased risk during climate change-related emergencies and natural disasters, such as heat waves, wild fires, flooding and ice storms, and experience high mortality rates associated with extreme weather. This may be due to mobility issues and difficulties communicating and remembering information, which could impede their ability to take precautions, follow instructions or express their concerns. Footnote 100, Footnote 101
Between 2014 and 2018, rapid warming contributed a 58.4% increase in heat-related deaths of people over 65 in Canada, compared with the 2000–2004 baseline. Footnote 102 Between June 25 and July 1, 2021, record high temperatures above 40 Celsius occurred in many areas of British Columbia. The Coroner's Report found that "most of the deceased were older adults with compromised health due to multiple chronic diseases and who lived alone." Footnote 103 Almost all (90%) of those who died were aged 60 and older, and more than two-thirds (69%) had chronic illnesses or conditions that could impact mobility, such as heart failure, arthritis or Parkinson's disease. Just under two-thirds (64%) of those who died were living with chronic illnesses or conditions that could impact cognition, such as dementia. The Coroner's panel identified several recommendations including to identify and support populations most at risk of dying during extreme heat emergencies and to implement extreme heat prevention and long-term risk mitigation strategies. More research is needed to evaluate the effects of conditions such as dementia on risks, including mortality, during a climate change-related emergency. Footnote 104 In addition, air pollution from an increasing severity and frequency of wildfires, for example, could contribute to an increased risk of developing dementia. Footnote 105, Footnote 106
British Columbia also saw high levels of flooding in 2021 that caused disruption and dangerous conditions for many. While there is limited information available about the impact of these floods on people living with dementia, anecdotal reports describe difficulties related to walking when evacuating during similar events. An American study following floods from Hurricane Katrina in 2005 recommends further training for families, first responders, and healthcare providers to better prepare them to assist persons with dementia as a distinct population. Footnote 107, Footnote 108 The study also recommends training for caregivers of people living with dementia on how to respond and prepare for disaster and recovery.
In March 2022, the international advocacy organization Alzheimer's Disease International issued advice for caregivers, humanitarian agencies, communities and people living with dementia during times of crisis. This resource can be adapted to different emergency situations and provides advice on methods to easily identify a person living with dementia, locate essential information about them such as emergency contacts, how to communicate with them, as well as how to be patient and supportive when approaching them during an emergency. Other topics in this resource include mobility, how to handle disruptions to daily tasks, and self-care practices for caregivers.
Recognizing the need to improve access to dementia guidance related to people living with dementia in times of emergencies, such as climate change-related emergencies, PHAC's Dementia Guidelines and Best Practices Initiative launched a funding opportunity in December 2021 that encouraged applications focused on this issue.
Contributions to quality of life from across Canada
Canadians benefit from many efforts across the country intended to improve the quality of life of people living with dementia and caregivers. The few noted below highlight examples focused on early diagnosis and improving access to quality care and support, as well as innovative approaches to combat dementia-related stigma through art.
- A project in Nova Scotia is exploring how collaborative family practice teams in Nova Scotia are addressing the needs of people living with dementia. Elaine Moody from Dalhousie University and her team are seeking to improve patient engagement and patient-oriented research. By examining three clinics that differ on characteristics such as rural/urban settings, dementia expertise, and number of people with dementia served, they are gathering evidence about accessing care informed by the lived experiences of people living with dementia and caregivers. The assessment will identify gaps and ways to better care for people living with dementia while maintaining a focus of diversity and inclusion.
- Through a project in which people living with dementia and their care partners created art depicting what it means to live well with dementia, Susan Cox and Gloria Puurveen from the University of British Columbia are exploring how care for those living with dementia could become empowering in a way that reflects unique life experiences. A collection of the art has been displayed in a virtual exhibit titled In There Out Here: Art Making Space to Live Well With Dementia. This exhibit has had 3,100 visitors from more than 42 countries as of June 2022, and is being incorporated into gerontology and aging courses at several universities.
- Between 5% and 15% of people living with a dementia have a rare dementia, this can include young onset Alzheimer's disease, frontotemporal dementia, Lewy body dementia, and posterior cortical atrophy. Rare Dementia Support (RDS) Canada offers access to information, tailored individual and group support and guidance, and connection with others living with similar conditions.
- The Toronto Dementia Research Alliance, led by Tarek Rajji, created the first city-wide standard magnetic resonance imaging (MRI) brain scan protocol for imaging patients for dementia. The protocol provides a high quality image that captures relevant information to assist with diagnosis and tracking disease progression. Training is in development to train radiologists on this protocol and provide a standardized reporting framework. As of June 2022, three clinical dementia imaging sites in Toronto have agreed to use this protocol. The overall goal is to adopt standardized MRI protocols at sites across Canada.
- Efforts are being made to improve the measurement of social connection for people living with dementia to better their health, care and quality of life. The SONNET Study led by Jennifer Bethell (University Health Network in Toronto) and Andrew Summerland (University College in London, England) will incorporate information from interviews and focus groups of people with lived experience and test an approach to measure social connection in long-term care (LTC). Findings from this research will help assess person-centred care to improve the health and quality of life of LTC residents.
- A free educational resource to assist individuals living with dementia and dementia caregivers provides information on the science and progression of dementia as well as practical advice on safety and self-care. It is available in English, French and Spanish and it is expected to be available in Portuguese, Greek, Italian, Chinese and Punjabi in the future. Dementia, Your Companion Guide was created by a multidisciplinary team at the McGill University Dementia Education Program.
Dementia and populations at higher risk
Ethnic and cultural communities and dementia in Canada
Current evidence suggests that some ethnic and cultural communities are likely to be at higher risk of developing dementia. Some may also face barriers to equitable care. This may be due to genetic factors, unequal access to health services, higher risk for certain chronic diseases or limited resources in their first languages. Footnote 109, Footnote 110 While the prevalence of dementia within Canada's ethnic and cultural communities is unknown, expanding data about their health-related issues could assist in understanding ways in which their vulnerabilities to dementia could be reduced. Recent public opinion research, along with analysis of the status of dementia guidance in Canada, is providing a deeper understanding about ethnic and cultural communities and dementia.
As of 2016, slightly more than one-fifth of Canadians (22%) identified as belonging to a visible minority population, as defined by the Employment Equity Act. Of these almost 8 million individuals, the largest groups are South Asian (1.9 million individuals), Chinese (1.6 million) and Black (1.2 million). According to the Employment Equity Act, members of visible minorities means persons, other than Aboriginal peoples, who are non-Caucasian in race or non-white in colour. (Statistics Canada, 2017)
This section of the report shares some recent findings about knowledge of dementia and perceptions about community support for people living with dementia among ethnic and cultural communities.
Knowledge and impact of dementia
The Public Health Agency of Canada (PHAC)'s 2020 dementia baseline public opinion research study included a focus on respondents identifying as Black, Southeast Asian, South American and South Asian, which are populations identified as being likely to be at higher risk of developing dementia. Footnote 111 About one-third of those identifying as South American (35%) or Black Canadian (34%) rated themselves as highly knowledgeable about dementia, compared with 24% of all respondents. In contrast, respondents identifying as Southeast Asian and South American were more likely to rate themselves as being not knowledgeable about dementia (33% and 32% respectively) compared with all respondents (25%). Respondents of South American descent are more likely to rate the impact of dementia on society as high (46%), compared with the overall response of 35%. Meanwhile, respondents of Southeast Asian descent were less likely to rate the impact of dementia on society as high (23%).
Risk of developing dementia and effective treatments for dementia
Some evidence suggests that ethnic and cultural communities may be at an increased risk of developing dementia. For example, Black Canadians are more likely than Caucasian Canadians to report diabetes and hypertension Footnote 112 and Canadians of South Asian descent have been found to have higher rates of diabetes than Caucasian Canadians. Footnote 113 Diabetes and hypertension are both identified as factors associated with increased risk of developing dementia. When asked in the 2020 study whether some ethnic/cultural groups have a higher risk of developing dementia, one-third (32%) of all respondents indicated (as is accurate) that they believe this is true while the same proportion (32%) indicated that they do not believe this to be the case.Footnote 111 A slightly higher proportion of respondents (36%) were unsure. By comparison, 46% of respondents identifying as South Asian and 42% of those identifying as Black Canadian indicated that they believe the risk is higher among some ethnic groups.
Respondents of South American and South Asian descent (47% and 50% respectively) are more likely than all respondents (37%) to the 2020 survey to believe that the risk of developing dementia is higher among those with chronic health conditions. Respondents identifying as Black Canadians or of South American descent were more likely to indicate that there is no increased risk of dementia associated with chronic health conditions (45% and 44% respectively compared with 29% for all respondents). The 2020 study also found that the inaccurate belief that dementia is an inevitable part of aging was shared by 34% of Black Canadian respondents; 28% of South American Canadian respondents; and 27% of South and Southeast Asian Canadian respondents, compared with 16% of all respondents.
Effective treatments to delay the onset of symptoms and slow the progression of dementia have yet to be developed. However, two-thirds (67%) of all respondents to the 2020 public opinion research study indicated that they believe that there are effective treatments that can delay the onset of symptoms and slow the progression of dementia. This belief was slightly higher among South American Canadian respondents (75%) and South Asian Canadian respondents (74%).
Perceptions of health care and the level of community support for those living with dementia
As part of PHAC's 2020 dementia public opinion research study, respondents were asked to rate access to and the quality of health care as well as the level of support in their respective communities for people living with dementia.Footnote 114
| POR Data point: level of support in community for people living with dementia | Rating | General population (%) | Black Canadians (%) | South American (%) | South Asian (%) | Southeast Asian (%) |
|---|---|---|---|---|---|---|
| Access to health care | Good (4–5) | 42 | 55 | 44 | 47 | 33 |
| Moderate (3) | 28 | 17 | 24 | 30 | 30 | |
| Poor (1–2) | 12 | 8 | 16 | 10 | 12 | |
| Quality of health care provided to those living with dementia | Good (4–5) | 35 | 43 | 30 | 39 | 20 |
| Moderate (3) | 31 | 27 | 27 | 28 | 39 | |
| Poor (1–2) | 13 | 10 | 21 | 14 | 13 | |
| Opportunities for social engagement/social connection | Good (4–5) | 20 | 37 | 11 | 19 | 13 |
| Moderate (3) | 31 | 26 | 44 | 36 | 36 | |
| Poor (1–2) | 25 | 13 | 19 | 24 | 21 | |
| Overall support from the community | Good (4–5) | 18 | 31 | 14 | 24 | 10 |
| Moderate (3) | 35 | 32 | 49 | 30 | 36 | |
| Poor (1–2) | 23 | 13 | 14 | 25 | 22 | |
| Efforts to make the community safer for those living with dementia | Good (4–5) | 16 | 29 | 19 | 22 | 11 |
| Moderate (3) | 30 | 30 | 31 | 29 | 31 | |
| Poor (1–2) | 27 | 14 | 25 | 23 | 25 |
Culturally appropriate dementia guidance
The initial phases of PHAC's Dementia Guidelines and Best Practices Initiative under the Dementia Strategic Fund included an examination of the availability and use of dementia guidance tailored for groups in Canada considered to be at higher risk of developing dementia or facing barriers to equitable care. Footnote 115 Guidance topics for this examination included prevention, screening and diagnosis, treatment and management, stigma, dementia-inclusive communities, and emergency preparedness and response.
Culturally appropriate guidance and training is informed by consideration of an individual's cultural background, personal experiences and norms, and is best developed through engagement and co-creation with members from the specific population (e.g. health leaders from different cultural/ethnic communities, advocacy organizations, and those from the local community or with lived experience) to better understand their perceptions and ensure relevancy of the information. Cultural competency has been defined as "the ability to understand, appreciate, and interact with people from cultures or belief systems other than one's own." Footnote 116
Familiarity with dementia guidance tailored to specific populations
Approximately half of questionnaire respondents (52%) reported not being familiar with dementia guidance tailored to those with young onset dementia (60%), individuals with existing health issues (52%), rural communities (47%) and those with intellectual disabilities (41%). Fewer indicated familiarity with dementia guidance tailored to individuals from ethnic and cultural minority communities (26%), LGBTQ2+ (23%), and official language minority communities (18%).
Availability of culturally appropriate dementia guidance
When asked whether the dementia guidance that they use and/or are familiar with is culturally appropriate for specific populations, more than half of the questionnaire respondents indicated that there is culturally appropriate dementia guidance for rural communities (69%) and individuals with young onset dementia (66%), and official language minority communities (57%). Fewer reported that there is culturally appropriate guidance for ethnic and cultural minority communities (40%), LGBTQ2+ communities (40%), Indigenous communities (42%), and remote communities (44%). Slightly more identified challenges than those who did not when finding dementia guidance that takes into account cultural context (35% compared with 25%). Approximately half reported gaps or barriers across dementia guidance topics for higher risk populations, although many (74%) reported that their organization had adapted services or programs to better serve these populations.
Participants identified gaps in guidance for these specific populations related to dementia-inclusive communities (57%), stigma (57%), transitions in care (54%), treatment and management (45%), screening and diagnosis (44%), emergency preparedness and response (41%), and dementia prevention (41%). When asked to describe specific gaps or barriers for those at higher risk of developing dementia and/or facing barriers to equitable care, respondents cited a lack of culturally appropriate tailored guidance and limited resources to implement guidance for these populations (e.g. limited health care provider time and lack of educational opportunities) (11%).
Most participants in the roundtables and interviews that were part of this study noted that they do not have access to the necessary tools to provide culturally appropriate dementia care. They identified a need for more culturally appropriate dementia guidance tools and resources that are tailored to, for example, newcomers to Canada, 2SLGBTQI+ individuals, and individuals dealing with trauma.
Cultural competency of dementia guidance and care
When asked about the status of cultural competency in Canada as it relates to dementia guidance, most of the roundtable and interview participants indicated that improvements are needed. Where there is dementia guidance available related to cultural competency, it was reported that it is fragmented across multiple sources and is not being implemented consistently. Participants noted a lack of specific and practical information on how to consider cultural factors for implementation of guidance. It was also suggested that care providers and leaders in particular need greater exposure to different populations. Further, more education is needed to improve the cultural competency of dementia care, possibly through mandatory cultural training embedded into the workplace, as well as through the promotion of person-centred approaches.
Deepening the understanding of dementia care experiences in Canada
To better understand the care experiences of people living with dementia, with a focus on Black, Indigenous, and People of Colour (BIPOC) communities in Canada, the Alzheimer Society of Canada launched the national Dementia Journey Survey in 2021. Many respondents to an online survey that gathered almost 500 responses, including 100 from BIPOC communities, identified barriers that prevented them from seeking a diagnosis, accessing dementia care, and reinforced stigma and isolation. These barriers include gaps in education and support for health care providers, lack of culturally relevant community resources, lack of access to specialists, and communication barriers around care and diagnosis. Further analysis of the experiences of the BIPOC survey respondents is underway and a report is expected to be available within the next year. The experiences shared by people living with dementia are informing the development of new resources, including accessible and culturally sensitive information, and shaping programs provided by Alzheimer societies across Canada.
Another project, the L'Abécédaire d'un cerveau en santé, is an initiative led by RésoSanté Colombie-Britannique in partnership with the Réseaux santé en français de l'Alberta, de la Saskatchewan et du Yukon. It is intended for Francophones whose language of communication is primarily French and will particularly try to reach those who live in remote areas and have less access to health resources. The project is documenting the state of dementia in the participating communities to provide a better understanding of the challenges of accessing resources in French as well as the needs of people with dementia and their caregivers. It will also include awareness campaigns and peer coaching aimed at improving cognitive health literacy.
Dementia and Indigenous peoples
Information on dementia and Indigenous peoples in Canada is limited. There is some evidence that suggests the proportion of individuals living with dementia is rising more quickly in First Nations populations and the onset of dementia may be occurring earlier. Footnote 117, Footnote 118 As well, a lack of access to health care in remote, rural and isolated communities and a lack of cultural safety in the health care system may create barriers to equitable and culturally appropriate care. Additional barriers may include linguistic differences, racism and poverty. Footnote 119, Footnote 120 These barriers and challenges can lead to undiagnosed dementia and delays in diagnosis, impacting the quality of life of Indigenous individuals living with dementia.
Indigenous perspectives, experiences and priorities related to dementia
Shortly after the launch of the national dementia strategy in 2019, PHAC commissioned a national public opinion survey to better understand awareness about and knowledge of dementia among Canadians, as well as their views on the abilities of people living with dementia and experiences providing care. Among the 4,207 respondents, the survey gathered the perspectives of 596 Indigenous individuals, of which 54% identified as First Nations, 35% as Métis, and 3% as Inuk. Footnote 121 The survey found that during the experience of providing care to someone living with dementia, Indigenous respondents (21%) were less likely to feel they were able to provide the care needed compared with the overall result of 16%. Among the Indigenous respondents the most common reasons for this response were a lack of time (68%), a lack of information (55%), and a lack of support (54%).Footnote 111
In 2021, PHAC undertook additional public opinion research to focus on Indigenous perspectives, experiences and priorities regarding dementia guidance, including guidelines and best practices on prevention, diagnosis, treatment and management, stigma reduction, creating dementia-inclusive communities, and emergency preparedness and response. Areas where responses from First Nations, Métis and Inuk respondents varied significantly with each other are highlighted in the summary below.Footnote 37
Of the 1,008 respondents, 693 were Indigenous people without dementia who have not cared for an Indigenous person living with dementia in the last 10 years (this group is referred to below as Indigenous), 111 were paid care providers for one or more Indigenous individuals living with dementia and 176 were unpaid care providers who have cared for an Indigenous person living with dementia in the last 10 years who may or may not be Indigenous themselves (see Figure 8). There was also a small group of 28 people who participated as Indigenous people living with dementia. Footnote 122 A breakdown of First Nations, Métis, Inuk and non-Indigenous respondents can be found in Figure 9 and a breakdown of Indigenous and non-Indigenous paid and unpaid care provider respondents is shown in Figure 10.
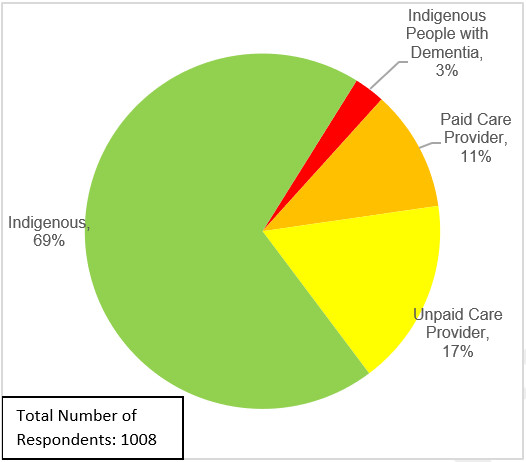
Figure 8 - Text description
- 3% of respondents are Indigenous people with dementia
- 11% of respondents are paid care providers
- 17% of respondents are unpaid care providers
- 69% of respondents are Indigenous
- Total number of respondents: 1008
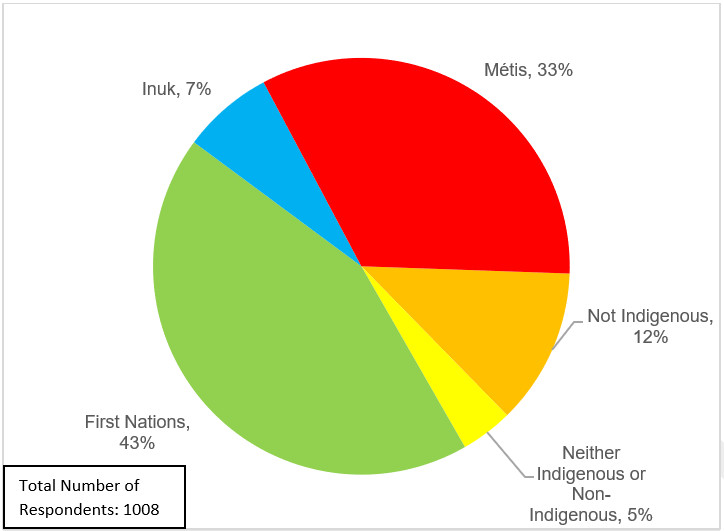
Total Number of Respondents: 1008
Figure 9 - Text description
- 33% of respondents self-identify as Métis
- 12% of respondents self-identify as not Indigenous
- 5% of respondents self-identify as neither Indigenous or non-Indigenous
- 43% of respondents self-identify as First Nations
- 7% of respondents self-identify as Inuk
- Total number of respondents: 1008
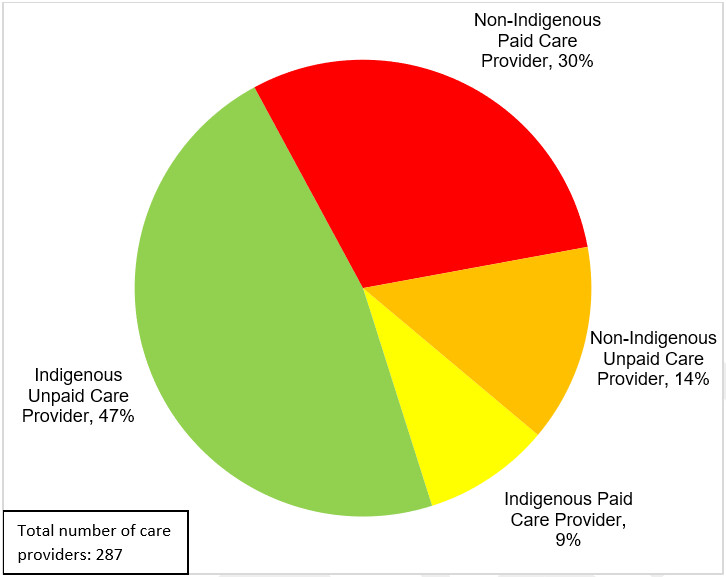
Figure 10 - Text description
- 30% of respondents are non-Indigenous paid care providers
- 14% of respondents are non-Indigenous unpaid care providers
- 9% of respondents are Indigenous paid care providers
- 47% of respondents are Indigenous unpaid care providers
- Total number of care providers: 287
Supporting Indigenous-led work on dementia
PHAC has invested in efforts to deepen its understanding of dementia among Indigenous peoples and to enable the implementation of Indigenous-led initiatives. For example, the agency is supporting a project with the Native Women's Association of Canada (NWAC) that has gathered distinctions-based information about Indigenous peoples, with a focus on stigma. NWAC first completed a project that explored the lived experiences, understandings and behaviours of dementia within Indigenous communities and is now implementing an awareness initiative focusing on stigma.
PHAC is funding several community-based projects that focus on developing culturally appropriate tools, resources and supports for people living with dementia and caregivers living in Indigenous communities. For example, NWAC is also advancing a project titled, Supporting the Circle of Care: A Culturally Informed Support Group and Toolkit for Caregivers of Indigenous People Living with Dementia, which is enabling access to trauma-informed tools and supports for rural and remote Indigenous communities to improve access to caregiver supports, reduce social isolation and caregiver burnout, and increase knowledge and awareness of dementia.
Data gathering about Indigenous perspectives and experiences related to dementia informs funding opportunities such as the December 2021 solicitation under the Dementia Strategic Fund: Dementia Guidelines and Best Practices Initiative. One theme of this funding opportunity is focused on addressing gaps in guidance on dementia for Indigenous peoples. Proposals under this theme must be Indigenous-led and demonstrate how they will consider and reflect Indigenous perspectives about aging well, Indigenous ways of knowing, the historical experiences of Indigenous peoples, geography of the population(s), be distinctions-based, and, as appropriate, involve Indigenous communities, Elders, Healers, Medicine Men/Women, and/or Knowledge Keepers.
PHAC is also funding a surveillance project that is working with Indigenous partner organizations to conduct a feasibility study to develop appropriate approaches for dementia surveillance in Indigenous populations. This work will help inform future surveillance tools to better identify Indigenous people living with dementia and develop culturally safe dementia prevention and treatment options.
Dementia risk reduction among Indigenous peoples
While about half of Indigenous respondents to the 2021 survey (52% of First Nations, 50% of Métis, and 41% of Inuk)Footnote 121 were worried about personally developing dementia, fewer (38% of First Nations, 50% of Métis, and 20% of Inuk) had taken steps to reduce their own risk. This is similar to results from a 2020 survey, which showed that almost half of Indigenous respondents (46%) were personally worried about developing dementia with a smaller number (28%) taking steps to reduce their risk.Footnote 111
In the 2021 survey, the most common reason among Indigenous respondents for not taking steps to reduce dementia risk was a lack of awareness of what to do.Footnote 37 When asked in 2021 about the first three things that come to mind when thinking about what factors increase personal chances of developing dementia, the following items were selected:
- a diet lacking in healthy foods (24% of First Nations, 31% of Métis, and 21% of Inuk respondents)
- loneliness and social isolation (20% of First Nations, 24% of Métis, and 9% of Inuk respondents)
- genetics (19% of First Nations, 32% of Métis, and 8% of Inuk respondents)
- a lack of physical activity (18% of First Nations, 26% of Métis, and 15% of Inuk respondents)
- harmful alcohol use (18% of First Nations, 20% of Métis, and 11% of Inuk respondents)
- hypertension (6% of First Nations, 4% of Métis, and 1% of Inuk respondents)
- mental health (e.g. stress, depression, PTSD) (6% of First Nations, 6% of Métis, and 3% of Inuk respondents)
- smoking (5% of First Nations, 5% of Métis, and 6% of Inuk respondents)
- hearing loss (2% of First Nations respondents, 3% of Métis, and 1% of Inuk respondents)
Respondents who live in urban areas (54%) were more likely to have taken steps to reduce their risk of developing dementia than those who live in rural areas (40%), and approximately 50% of those between the ages of 55 and 74 were more likely to have taken steps compared with 38% under the age of 55.
Dementia guidance and Indigenous peoples
Dementia guidance used by Indigenous peoples across Canada must incorporate the needs, experiences, knowledge, attitudes and behaviours of these individuals and communities, including community strengths, resources, traditional healing practices and ways of knowing. Footnote 123 Many Indigenous individuals in Canada have some experience with dementia. About two-thirds of Indigenous respondents to the 2021 survey knew someone who is living or has lived with dementia, and that person was likely to be an extended family member (42%), friend, neighbour or colleague (19%), or a community member (14%). However, almost half of Inuk respondents (42%)Footnote 37 reported not knowing anyone living with dementia, compared with First Nations (33%) and Métis (27%) respondents.
Dementia guidance for Indigenous peoples: Gaps and barriers
When paid care providers working with Indigenous individuals living with dementia were asked which dementia guidance topics they were using regularly, the most common topics were treatment and management (77%), prevention (56%), and screening and diagnosis (50%). Many care providers reported finding gaps or barriers. More than half of unpaid care providers noted gaps or barriers regarding the day-to-day care of someone living with dementia (76%), screening and diagnosis (69%), ways to reduce the risk of developing dementia (68%), transitions in care (65%), dementia-inclusive communities and reducing inaccurate negative perceptions (i.e. stigma) (64%). Paid care providers, such as primary health care providers, specialists and personal care workers, reported gaps or barriers related to treatment and management of dementia (70%), safe and supportive interactions (69%), transitions in care (68%), ways to reduce the risk of developing dementia (68%), and advanced care planning and end-of-life care (64%).
Just under one-quarter (23%) of paid care providers reported no challenges when accessing or using dementia guidance for Indigenous peoples. However, almost one-third (34%) indicated that guidance is not culturally appropriate or culturally safe, Footnote 124 is too complicated (15%), is not in the right language (14%), is too expensive (10%), or they do not know where to look for the guidance, it is not readily available, or it is hard to access (12%).
Guidance on dementia-inclusive communities
In a dementia-inclusive community, measures are in place that make it more possible for people living with dementia to protect and improve their health and wellbeing, live independently, safely navigate and access local activities, and maintain social networks. Guidance on how to reduce stigma related to dementia and to be more dementia-inclusive can help everyone contribute to these types of communities. This guidance is particularly useful for those likely to interact with people living with dementia in the community, such as health care professionals, first responders, and those working in banks, retail stores, restaurants, and providing public transit. Of those Indigenous respondents from the general public (not a person living with dementia or a care provider), one-third (34%) reported in the 2021 survey that they believe their community is knowledgeable, respectful and supportive of people living with dementia and a fifth (17–19%) have knowledge on how to make a community more welcoming and supportive.Footnote 37
Developing culturally appropriate and culturally safe dementia guidance
The 2021 public opinion research study focused on Indigenous peoples and dementia guidance also investigated access to culturally safe and appropriate tools. Cultural safety has been defined as "an outcome based on respectful engagement that recognizes and strives to address power imbalances inherent in the health care system. It results in an environment free of racism and discrimination, where people feel safe when receiving health care." Footnote 125 About half (47%) of paid care providers indicated that the guidance on dementia and related tools they use to provide care and support to Indigenous people living with dementia are culturally appropriate and safe, while a third (34%) of paid care providers reported the opposite. The remaining 20% of paid care providers either did not know (17%) or did not respond to this question (3%). Those living in Ontario (64%) and Atlantic Canada (60%) were more likely than those in other regions of Canada to say they have culturally appropriate tools for Indigenous peoples.
In addition, survey participants were also asked what should be done to ensure that recommendations or advice about dementia are culturally appropriate and culturally safe for Indigenous populations. Responses indicate a desire for engagement of Indigenous peoples during the development process to ensure that advice reflects the lived experience and perspectives of Indigenous peoples and considers the different strengths and needs of Indigenous communities across Canada (see Figures 11 and 12).
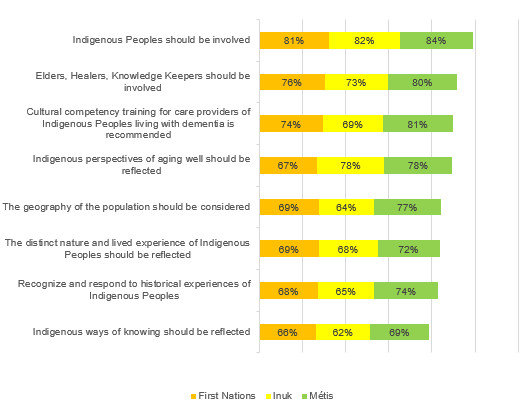
Figure 11 - Text description
| To ensure that recommendations or advice about dementia are culturally appropriate and culturally safe for Indigenous populations | First Nations | Inuk | Métis |
|---|---|---|---|
| Indigenous Peoples should be involved | 81% | 82% | 84% |
| Elders, Healers, Knowledge Keepers should be involved | 76% | 73% | 80% |
| Cultural competency training for care providers of Indigenous Peoples living with dementia is recommended | 74% | 69% | 81% |
| Indigenous perspectives of aging well should be reflected | 67% | 78% | 78% |
| The geography of the population should be considered | 69% | 64% | 77% |
| The distinct nature and lived experience of Indigenous Peoples should be reflected | 69% | 68% | 72% |
| Recognize and respond to historical experiences of Indigenous Peoples | 68% | 65% | 74% |
| Indigenous ways of knowing should be reflected | 66% | 62% | 69% |

Figure 12 - Text description
| To ensure that recommendations or advice about dementia are culturally appropriate and culturally safe for Indigenous populations | Indigenous people without dementia not providing care to an Indigenous person in a paid or unpaid capacity in the last 10 years | Paid care providers that have care for an Indigenous person living with dementia within the last 10 years | Unpaid care providers that have provided unpaid care and support to an Indigenous person living with dementia within the last 10 years |
|---|---|---|---|
| Indigenous Peoples should be involved | 79% | 84% | 82% |
| Elders, Healers, Knowledge Keepers should be involved | 75% | 79% | 81% |
| Cultural competency training for care providers of Indigenous Peoples living with dementia is recommended | 77% | 79% | 75% |
| Indigenous perspectives of aging well should be reflected | 70% | 78% | 73% |
| The geography of the population should be considered | 70% | 75% | 73% |
| The distinct nature and lived experience of Indigenous Peoples should be reflected | 68% | 76% | 74% |
| Recognize and respond to historical experiences of Indigenous Peoples | 69% | 78% | 69% |
| Indigenous ways of knowing should be reflected | 66% | 76% | 69% |
Respondents include Indigenous people without dementia who have not cared for an Indigenous person living with dementia in the last 10 years, paid care providers for one or more Indigenous individuals living with dementia and caregivers who have cared for an Indigenous person living with dementia in the last 10 years who may or may not be Indigenous themselves. Please use caution when interpreting Inuit data due to the smaller sample size (74 of the respondents identified themselves as Inuk).
Gaps and barriers have been identified in terms of finding and using culturally appropriate and safe dementia guidance in Canada. For example, another recent PHAC study found that participants familiar with dementia guidance in the North (i.e. Northwest Territories, Yukon and Nunavut) were more likely to identify challenges with finding guidance that considers cultural context (86%) and with obtaining guidance in a preferred language (71%), compared with guidance users in all other regions in Canada (13% – 46%). As well, when asked about the availability of culturally appropriate dementia guidance for distinct groups, just over 40% of all participants across Canada indicated that such guidance is available for Indigenous peoples.
Seeking dementia guidance
People may look to multiple sources when seeking recommendations or advice about dementia although some sources may be considered more trustworthy, accessible or credible than others. When asked who they would talk to first to get recommendations or advice on dementia for Indigenous peoples:Footnote 121
- Indigenous peoples and paid care providers most often indicated that they would be likely to ask health care professionals and other care providers (83%), followed by unpaid care providers at 78%. This was particularly true among Métis (88%) and First Nations (80%) respondents, compared with Inuk respondents (76%).
- 13% of unpaid care providers and Indigenous, and 14% of paid care providers, would also ask people they know, particularly among First Nations (16%) and Inuk (15%) respondents, compared with Métis (10%) respondents.
- 17% of paid care providers, 10% of unpaid care providers, and 8% of Indigenous would ask local/community health groups, particularly among Inuk (12%) and First Nations (10%) respondents compared with Métis (7%) respondents.
- 17% of paid care providers, 8% of unpaid care providers and 8% of Indigenous would ask someone in their community that holds traditional knowledge (i.e. an Elder, Healer, Medicine Man/Woman, Clan Mother or Knowledge Keeper). More First Nations respondents selected this option (12%) than Métis (4%) or Inuk (3%) respondents.
Formatting is also an important consideration, as it can make guidance resources more accessible and appealing to the user. Online text resources were identified as a preferred format (67%) and more often among Métis respondents (74%) than First Nations (65%) and Inuk (53%) respondents. This was followed by printed copies, such as brochures, pamphlets and information sheets (56%), online videos (33%) and telephone helplines (29%). More Métis (32%) respondents preferred telephone hotlines than First Nations (27%) and Inuk (24%). Delivery of guidance through an in-person meeting or from a health care professional was the least preferred format to receive health recommendations or advice.
Knowing where people go online to find advice about dementia can help with dissemination strategies and ensure that those looking for the information are able to find it easily. When looking for dementia advice, two-thirds of respondents indicated they would use dementia advocacy organizations' websites (66%). About half would seek information from a variety of sources including health care expert websites (55%), federal government websites (48%), provincial or territorial government websites (44%) and regional/local Indigenous health authority websites (43%). Métis respondents were more likely (74%) than First Nations or Inuk respondents (both at 59%) to seek information from dementia advocacy organizations' websites. Only 17% of Métis respondents would seek information from a health care expert website, compared with 36% of Inuk respondents and 23% of First Nations respondents.
Language is another important factor to consider when developing dementia guidance, recommendations and/or advice. When looking for dementia guidance tools to provide care, the majority of respondents indicated that resources are preferred in English (87%) or French (12%) Footnote 126 although 12% of paid care providers indicated a preference for information to be available in Cree. Language preference differed by region. More Métis (92%) respondents preferred resources in English than First Nations (85%) and Inuk (80%) respondents. First Nations (11%) and Métis (10%) respondents were more likely to prefer resources in French than Inuk (6%) respondents. Inuk respondents were the only respondents among the First Nations, Métis and Inuk categories to select Unuinnaqtun (6%), Inuktitut (Baffin) (9%), Inuktitut (Nunatsiatvut) (9%), and Inuktitut (Nunavik) (9%) as preferred languages. In Manitoba and Saskatchewan, 12% indicated that they preferred Cree. In the territories, Inuktitut was preferred by 13%, especially from those living in Nunavut.
Conclusion
The 2022 annual report to Parliament on the national dementia strategy provides a glimpse of the growing number of dementia-related initiatives across Canada resulting from federal investments and highlights some of the results from recent public opinion research and other data-gathering recently undertaken by the Public Health Agency of Canada (PHAC). As activity grows and results are reported, resources and tools that support progress on the strategy's national objectives are becoming more available, including those designed to be culturally appropriate and culturally safe for diverse populations. Increased research funding announced in Budget 2022 will further efforts on brain health, improved treatments, and support for dementia caregivers. The report also highlights a few of the many efforts underway by partners and stakeholders across the country that are addressing some of the challenges of dementia in Canada. Looking ahead, more work is needed on the many challenges dementia presents including continuing to assess and act on the impact of the COVID-19 pandemic, as well as the need to develop responses for climate change-related emergencies tailored to the needs of people living with dementia.
We thank all those who contributed information in this year's report, including several organizations across Canada working on a variety of dementia-related initiatives. We also thank all those individuals who participated in or otherwise supported the data-gathering projects over the past year, including PHAC's public opinion research studies, which have deepened our understanding of dementia in Canada. This report shares just a few of the results; all of the public opinion research conducted on behalf of PHAC can be accessed through Library and Archives Canada. If you would like to receive communications about the national dementia strategy and funding opportunities or provide information about relevant dementia-related activities, please contact the PHAC Dementia Policy Secretariat.
Appendix A: Overview of the national dementia strategy
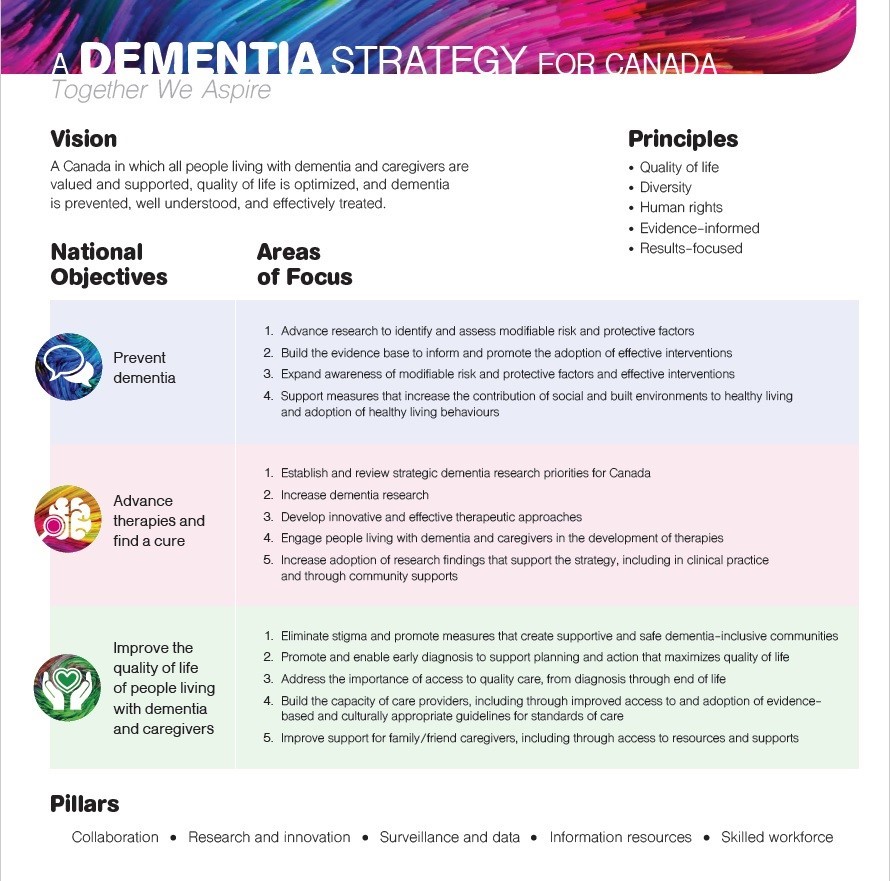
Appendix A - Text description
A Dementia Strategy for Canada: Together We Aspire
Vision: a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated.
Principles:
- Quality of life
- Diversity
- Human rights
- Evidence-informed
- Results-focused
| National objectives | Areas of focus |
|---|---|
| Prevent dementia |
|
| Advance therapies and find a cure |
|
| Improve the quality of life of people living with dementia and caregivers |
|
Pillars:
- Collaboration
- Research
- Innovation
- Surveillance and data
- Information resources
- Skilled workforce
Appendix B: Aspirations for Canada's efforts on dementia from the national dementia strategy
| Current status | Aspiration | |
|---|---|---|
| Prevent dementia | ||
| 1 | Incomplete understanding of risk and protective factors linked with dementia, with some factors not yet identified and insufficient evidence on the link between factors and dementia. | A complete understanding of the risk and protective factors linked to dementia, their impacts and interactions. |
| 2 | Limited evidence about effective interventions to reduce risk for dementia and insufficient information resources. | Availability of effective prevention resources and interventions, supported by a strong evidence base. |
| 3 | A lack of awareness among the general public and care providers about actions that may help prevent dementia. | All people living in Canada are aware of actions that prevent dementia. |
| 4 | Barriers related to built and social environments limit the ability of individuals to pursue healthy living in ways that may reduce the risk of developing dementia. | All people living in Canada have access to built and social environments that support their ability to pursue healthy living in ways that may reduce their risk of developing dementia. |
| Advance therapies and find a cure | ||
| 1 | Limited broad stakeholder input when setting research priorities and insufficient engagement of people living with dementia and caregivers. | Research priorities established in an inclusive manner with broad stakeholder input, with the participation of those living with dementia and caregivers. |
| 2 | Annual investment in dementia research in Canada is less than one percent of dementia care costs. | Annual investment in dementia research in Canada exceeds one percent of dementia care costs. |
| 3 | Options for evidence-informed therapies remain limited and often are not person-centred. | New evidence-informed person-centred therapies are more readily available. |
| 4 | People living with dementia and caregivers are predominantly the subject of research to develop new therapies and find a cure. | People living with dementia and caregivers are active participants and partners in research to develop new therapies and find a cure. |
| 5 | Research findings tend to stay within academic settings and journals and are not broadly known, accepted, or brought into clinical practice. | Research design always includes efforts that ensure findings can be understood, adopted and quickly put into practice. |
| Improve quality of life of people living with dementia and caregivers | ||
| 1 | Widespread stigma within communities and a lack of understanding of dementia. | All people living in Canada understand dementia and stigma no longer exists in Canada. |
| 2 | Individuals are unable to receive an early or timely diagnosis, or feel unsupported when receiving a diagnosis. | A timely diagnosis, provided in a compassionate manner, is available to all people living in Canada, along with immediate availability of resources and supports. |
| 3 | Lack of access to, awareness or understanding of health and social services that provide integrated and person-centred care. | Integrated, person-centered quality care based on evidence-informed best practices across all settings and that people feel welcomed and well-cared for when hospitalization or admission to long-term care is necessary. |
| 4 | Lack of information and resources for care providers, reducing the capacity to provide quality care. | Care providers have access to the resources and training needed to deliver quality care. |
| 5 | Caregivers experiencing burnout, financial hardship, isolation and depression while caring for someone living with dementia. | All caregivers have access to the resources and supports required to protect their own wellbeing and to care for someone living with dementia, including being equipped to navigate health care and other support systems. |
Appendix C: Map of PHAC investments – project details
Note: Projects marked with an asterisk (*) indicate that they are national in scope
Dementia Strategic Fund projects
- Abécédaire d'un cerveau en santé – Sensibilisation à la démence dans l'Ouest et le Nord (Réso-Santé Colombie-Britannique)
- Acquainting Canadian Seniors with State of the Art Dementia Prevention Strategies: Up Close and Personal (Cyber-Seniors: Connecting Generations)
- Artful Moments: Shared Learning (Art Gallery of Hamilton)
- Awareness Builds Connections in Dementia-Friendly Communities (ABCD Initiative) (Rural Development Network)
- Culturally-Appropriate Dementia Awareness and Education Project for Diverse Immigrant Communities (S.U.C.C.E.S.S.)
- Dementia-inclusive Streets and Community Access, Participation, and Engagement (DemSCAPE) (Simon Fraser University)
- *Luci : une application mobile personnalisée, accompagnée par un entraîneur, servant à adopter et à conserver des habitudes de vie saine pour réduire le risque de la démence chez les personnes d'âge moyen et les jeunes aînés présentant des facteurs de risque modifiables. (Lucilab Inc.)
- Mesures visant à prévenir ou combattre la stigmatisation des personnes âgées atteintes de démence dans leurs collectivités et promouvoir leur inclusion (Centre collégial d'expertise en gérontologie du Cégep de Drummondville)
- *Mind Over Matter®– A Comprehensive Brain Health Awareness Campaign (Women's Brain Health Initiative)
- Open Minds, Open Hearts (Conestoga College Institute of Technology and Advanced Learning)
- Partnering for Dementia Friendly Communities (Department of Health and Community Services, Newfoundland and Labrador)
- Reducing dementia-related stigma by using person-centred language to describe responsive behaviours in hospital admissions (Regional Geriatric Program of Toronto)
- Sharing Dance with People with Dementia (Canada's National Ballet School)
- *Stigma: An Exploration of Lived Experience, Understandings and Behaviours of Dementia within Indigenous Communities (Native Women's Association of Canada)
- Stronger Together: Making Ottawa and Renfrew County Dementia Inclusive (Dementia Society of Ottawa and Renfrew County)
Dementia Community Investment projects
- Building Capacity for Meaningful Participation by People Living with Dementia (University of British Columbia)
- Cummings Centre Therapeutic Dementia Care Program (Cummings Jewish Centre for Seniors)
- Dementia Dialogue Podcast Network (Lakehead University)
- *Dementia-Friendly Canada (Alzheimer Society of Canada)
- Des collectivités en soutien à la trajectoire de vie des personnes allochtones et autochtones atteintes de démence (Centre de recherche sur le vieillissement de Sherbrooke)
- Enhancing Minds in Motion®as a Virtual Program Delivery Model for People Living with Dementia and Their Care Partners (Alzheimer Society of Ontario)
- Ethno-Cultural and Linguistically Based Support Services to People Living with Dementia (COSTI Immigrant Services)
- Evaluating co-designed tools for strong partnerships in the dementia care triad (Saint Elizabeth Health Care)
- Implementing Computer Interactive Reminiscing and Conversation Aid in Canada (CIRCA-CA) (University Health Network)
- Empowering Dementia Friendly Communities – Hamilton and Haldimand (Hamilton Council on Aging)
- Inuvialuit Settlement Region Dementia Awareness and Intervention (Inuvialuit Regional Corporation)
- L'approche par le plaisir en milieu communautaire : créer des environnements accueillants pour les personnes avec des atteintes cognitives (Société Alzheimer de Granby et région)
- Living with Dementia in Rural First Nations Communities: A Health and Wellness Project (University of Manitoba)
- Mobilizing and Equipping Community Based Organizations to Promote Awareness and Support for Person-Centered Care for People Living with Dementia and their Caregivers (BC Centre for Palliative Care)
- Moving, Eating, and Living Well (University of Waterloo)
- *Supporting a Circle of Care: A Culturally Informed Support Group and Toolkit for Indigenous Caregivers of People Living with Dementia (Native Women's Association of Canada)
- Supporting Family Caregivers of Persons Living with Dementia: Effectiveness and Sustainability of My Tools 4 Care-In Care (University of Alberta)
- Ten Online Modules Over Ten Weeks for Adult Learners (TOTAL) eLearning for Family/Friend Caregivers of Persons Living with Dementia (PLWD) (McGill University)
- *The Canadian Dementia Learning and Resource Network (CDLRN) (Schlegel UW- Research Institute for the Aging)
- *The Integration, Optimization and Promotion of Inclusive Approaches for LGBTQI2S People Living With Dementia and their Caregivers (Egale)
- New Brunswick Dementia Friendly Initiative (The New Brunswick Association of Nursing Homes)
- Ce qui nous lie ~ What connects us: A mixed methods ethnography to evaluate an intersectoral participatory approach for sustainable community-based initiatives to destigmatize dementia (CIUSSS du Centre-Ouest-de-L'île de Montréal)
Enhanced Dementia Surveillance Initiative projects
- A comprehensive and holistic approach to dementia surveillance in Canada (Schlegel-University of Waterloo Research Institute for Aging)
- *A National Indigenous dementia surveillance initiative – A feasibility study (McMaster University)
- *Ascertaining dementia and surveillance of risk factors in the Canadian Longitudinal Study on Aging (McMaster University)
- Canadian Chronic Disease Surveillance System case capture and dementia prevalence in long-term care settings (Participants: British Columbia, Ontario and Quebec)
- Disease and mortality trajectory among Canadians with dementia (Participants: British Columbia, Ontario, Prince Edward Island and Quebec)
- Exploring linkage opportunities to enrich Canadian Chronic Disease Surveillance System data (Participants: British Columbia and Quebec)
- Health surveillance of community-dwelling, person-with-dementia and caregiver dyads (LIFE Research Institute, University of Ottawa)
- National Dementia Caregiver Surveillance through First Link®: A Pilot Project (The Alzheimer Society of Canada)
- *Population Health Model (POHEM), a microsimulation model for dementia projections (Health Analysis Division,Statistics Canada)
- *The implementation of the 'Canadian Primary Care Sentinel Surveillance Network Data Presentation Tool' in primary care clinics to enhance the surveillance, prevention and management of chronic disease: Phase 3 (Queen's University)
Bibliography
Alzheimer's Association. 2008 Alzheimer's disease facts and figures. Alzheimer's & Dementia. 2008;4(2):110–33. Available from: https://doi.org/10.1016/j.jalz.2008.02.005
Alzheimer's Association. Is Alzheimer's Genetic? Alzheimer's Association. Available from: https://www.alz.org/alzheimers-dementia/what-is-alzheimers/causes-and-risk-factors/genetics
Alzheimer Society of Canada. Dementia with Lewy bodies. Alzheimer's Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/other-types-dementia/dementia-lewy-bodies
Alzheimer Society of Canada. Risk factors for dementia. Alzheimer Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/how-can-i-prevent-dementia/risk-factors-dementia
Alzheimer Society of Canada. What is Alzheimer's disease? Alzheimer Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/what-alzheimers-disease
Alzheimer's Society (UK). Is dementia hereditary? Alzheimer's Society (UK). Available from: https://www.alzheimers.org.uk/about-dementia/risk-factors-and-prevention/is-dementia-hereditary
Alzheimer's Society (UK). Delirium - symptoms, diagnosis and treatment. Available from: https://www.alzheimers.org.uk/get-support/daily-living/delirium
Bellenguez C, Küçükali F, Jansen IE, et al. New insights into the genetic etiology of Alzheimer's disease and related dementias. Nature Genetics. 2022;54:412–436. Available from: https://doi.org/10.1038/s41588-022-01024-z
Bourassa C. Addressing the Duality of Access to Healthcare for Indigenous Communities: Racism and Geographical Barriers to Safe Care. HealthcarePapers. 2018;17(3):6–10. Available from: https://doi.org/10.12927/hcpap.2018.25507
British Columbia Coroners Service. Extreme Heat and Human Mortality: A Review of Heat-Related Deaths in B.C. in Summer 2021. British Columbia Coroners Service. 2022. Available from: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-panel/extreme_heat_death_review_panel_report.pdf
Canadian Institute for Health Information. COVID-19's impact on long-term care. Canadian Institute for Health Information. 2021. Available from: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care
Canadian Institute for Health Information. Continuing Care Metadata. Canadian Institute for Health Information. Available from: https://www.cihi.ca/en/continuing-care-metadata
Canadian Institute for Health Information. Dementia in long-term care. Canadian Institute for Health Information. Available from: https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-care
Canadian Institute for Health Information. Hospital stays for substance use harms increased during the first months of the COVID-19 pandemic. Canadian Institute for Health Information. 2021. Available from: https://www.cihi.ca/en/hospital-stays-for-substance-use-harms-increased-during-the-first-months-of-the-covid-19-pandemic
Canadian Institute for Health Information. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months. Canadian Institute for Health Information. 2021. Available from: https://www.cihi.ca/sites/default/files/document/impact-covid-19-long-term-care-canada-first-6-months-report-en.pdf
Clair R, Gordon M, Kroon M, Reilly C. The effects of social isolation on well-being and life satisfaction during pandemic. Humanities and Social Sciences Communications. 2021;8:28. Available from: https://doi.org/10.1057/s41599-021-00710-3
Clarke J. Impacts of the COVID-19 pandemic in nursing and residential care facilities in Canada. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00025-eng.htm
Coogan SCP, Robinne FN, Jain P, Flannigan MD. Scientists' warning on wildfire — a Canadian perspective. Canadian Journal of Forest Research. 2019;49(9):1015–1023. https://doi.org/10.1139/cjfr-2019-0094
Cosco TD, Wister A, Riadi I, Kervin L, Best J, Raina P. Reduced ability to engage in social and physical activity and mental health of older adults during the COVID-19 pandemic: longitudinal analysis from the Canadian Longitudinal Study on Aging. The Lancet. 2021;398:S35. https://doi.org/10.1016/S0140-6736(21)02578-2
Dekhtyar S, Marseglia A, Xu W, Darin-Mattsson A, Wang HX, Fratiglioni L. Genetic risk of dementia mitigated by cognitive reserve: A cohort study. Annals of Neurology. 2019;86(1):68–78. Available from: https://doi.org/10.1002/ana.25501
Dobson KG, Vigod SN, Mustard C, Smith PM. Trends in the prevalence of depression and anxiety disorders among Canadian working-age adults between 2000 and 2016. Health Reports. 2020; 31(12): 12–23. Available from: https://doi.org/10.25318/82-003-x202001200002-eng
Douaud G, Lee S, Alfaro-Almagro F, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604(7907):697–707. Available from: https://doi.org/10.1038/s41586-022-04569-5
Earnscliffe Strategy Group for the Public Health Agency of Canada. Quality of Life and Dementia Quality and Quantitative Research: Final Report. Government of Canada. 2020. Available from: https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2021/081-20-e/POR081-20-Report-FINAL-EN.pdf
Ekos Research Associates Inc. for the Public Health Agency of Canada. Dementia Guidance and Indigenous Populations in Canada: Findings Report. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-374-2021-eng.pdf
Ekos Research Associates Inc. for the Public Health Agency of Canada. Dementia Survey: Final Report. Government of Canada. 2020. Available from: https://publications.gc.ca/collections/collection_2020/aspc-phac/HP10-36-2020-eng.pdf
Ekos Research Associates Inc. for the Public Health Agency of Canada. Knowledge, Perspectives and Experience of Dementia Care Providers: Final Report. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-380-2021-eng.pdf
Ekos Research Associates Inc. for the Public Health Agency of Canada. Survey of Canadians Regarding Dementia Prevention: Final Report. Government of Canada. 2022. Available from: https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2022/104-21-e/POR104-21-Final-Report.pdf
First Nations Health Authority. Cultural Safety and Humility. First Nations Health Authority. Available from: https://www.fnha.ca/wellness/wellness-and-the-first-nations-health-authority/cultural-safety-and-humility
Fong, T.G., Inouye, S.K. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat Rev Neurol (2022). https://doi.org/10.1038/s41582-022-00698-7
Frontera JA, Boutajangout A, Masurkar AV, et al. Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer's dementia. Alzheimer's & Dementia. 2022;18(5):899–910. Available from: https://doi.org/10.1002/alz.12556
Gibson A. Stories from the Flood: Dementia Caregivers' Disaster Response Training Recommendations. The Gerontologist. 2016;56(3):285. Available from: https://doi.org/10.1093/geront/gnw162.1154
Gibson A, Walsh J, Brown LM. A perfect storm: Challenges encountered by family caregivers of persons with Alzheimer's disease during natural disasters. Journal of Gerontological Social Work. 2018;61(7):775–789. Available from: https://doi.org/10.1080/01634372.2018.1474158
Godard-Sebillotte C., Sourial N., Hardouin M., Rochette L., Pelletier E., Gamache P., Jean S., Strumpf E., Vedel I. Development of two hierarchical algorithms identifying the 65+ community dwelling population in the provincial administrative database in Quebec. CAHSPR Annual conference, May 27-31 2019; Halifax NS. Poster.
Hakala JO, Rovio SP, Pahkala K, et al. Physical Activity from Childhood to Adulthood and Cognitive Performance in Midlife. Medicine and Science in Sports and Exercise. 2019;51(5):882–890. Available from: https://doi.org/10.1249/mss.0000000000001862
Heerema E. What Causes Lewy Body Dementia? Verywell Health. 2022. Available from: https://www.verywellhealth.com/lewy-body-dementia-risks-98761
Henderson SB, McLean KE, Lee MJ, Kosatsky T. Analysis of community deaths during the catastrophic 2021 heat dome: Early evidence to inform the public health response during subsequent events in greater Vancouver, Canada. Environmental Epidemiology. 2022;6(1):e189. Available from: https://doi.org/10.1097/ee9.0000000000000189
Hindmarch W, McGhan G, Flemons K, McCaughey D. COVID-19 and Long-Term Care: the Essential Role of Family Caregivers. Canadian Geriatrics Journal. 2021;24(3):195–199. Available from: https://doi.org/10.5770/cgj.24.508
Hodges JR, Piguet O. Progress and Challenges in Frontotemporal Dementia Research: A 20-Year Review. Journal of Alzheimer's disease. 2018;62(3):1467–1480. Available from: https://doi.org/10.3233/jad-171087
House of Commons. HESA Committee Meeting. Parliament of Canada. 2022. Available from: https://www.ourcommons.ca/DocumentViewer/en/44-1/HESA/meeting-6/minutes
Iaccarino L, La Joie R, Lesman-Segev OH, et al. Association Between Ambient Air Pollution and Amyloid Positron Emission Tomography Positivity in Older Adults With Cognitive Impairment. JAMA Neurology. 2021;78(2):197–207. Available from: https://doi.org/10.1001/jamaneurol.2020.3962
Ikeda M, Mori E, Hirono N, et al. Amnestic people with Alzheimer's disease who remembered the Kobe earthquake. The British Journal of Psychiatry. 1998;172:425–8. Available from: https://doi.org/10.1192/bjp.172.5.425
Jacklin KM, Walker JD, Shawande M. The emergence of dementia as a health concern among First Nations populations in Alberta, Canada. Canadian Journal of Public Health. 2021;104(1):e39–e44. Available from: https://doi.org/10.1007/bf03405652
Khan M, Kobayashi K, Lee SM, Vang Z. (In)Visible Minorities in Canadian Health Data and Research. Population Change and Lifecourse Strategic Knowledge Cluster Discussion Paper Series. 2015; 3(1): 5. Available from: https://ir.lib.uwo.ca/pclc/vol3/iss1/5
Lancet Countdown, Canadian Medical Association, Canadian Public Health Association. The Lancet Countdown on Health and Climate Change: Policy Brief for Canada. Lancet Countdown, Canadian Medical Association, Canadian Public Health Association. 2021. Available from: https://www.cpha.ca/sites/default/files/uploads/advocacy/2021_lancet/2021_Lancet_Countdown_Canada_Policy_Brief_e.pdf
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413–446. Available from: https://doi.org/10.1016/S0140-6736(20)30367-6
Lourida I, Hannon E, Littlejohns TJ, et al. Association of Lifestyle and Genetic Risk With Incidence of Dementia. JAMA. 2019;322(5):430–437. Available from: https://doi.org/10.1001/jama.2019.9879
Manly JJ, Mayeux R. Ethnic Differences in Dementia and Alzheimer's Disease. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Available from: https://www.ncbi.nlm.nih.gov/books/NBK25535/
Marin C, Vilas D, Langdon C, et al. Olfactory Dysfunction in Neurodegenerative Diseases. Current Allergy and Asthma Reports. 2018;18(8):42. Available from: https://doi.org/10.1007/s11882-018-0796-4
Mayo Clinic. Alzheimer's genes: Are you at risk? Mayo Clinic. 2021. Available from: https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-genes/art-20046552
McGraw-Hill Concise Dictionary of Modern Medicine. Cultural Competency. McGraw-Hill Concise Dictionary of Modern Medicine. 2002. Available from: https://medical-dictionary.thefreedictionary.com/Cultural+Competency
Middleton LE, Barnes DE, Lui L-Y, Yaffe K. Physical Activity Over the Life Course and Its Association with Cognitive Performance and Impairment in Old Age. Journal of the American Geriatrics Society. 2010;58(7):1322–6. Available from: https://doi.org/10.1111/j.1532-5415.2010.02903.x
Moore SA, Faulkner G, Rhodes RE, et al. Few Canadian children and youth were meeting the 24-hour movement behaviour guidelines 6-months into the COVID-19 pandemic: Follow-up from a national study. Applied Physiology, Nutrition, and Metabolism. 2021;46(10):1225–1240. Available from: https://doi.org/10.1139/apnm-2021-0354
Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. International Journal of Behavioral Nutrition and Physical Activity. 2020;17:85. Available from: https://doi.org/10.1186/s12966-020-00987-8
Nakazawa T, Ohara T, Hirabayashi N, et al. Multiple-region grey matter atrophy as a predictor for the development of dementia in a community: the Hisayama Study. Journal of Neurology, Neurosurgery & Psychiatry. 2021;93:263–271. Available from: http://dx.doi.org/10.1136/jnnp-2021-326611
Narrative Research for the Public Health Agency of Canada. Priorities for an Information Portal on Dementia. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/sc-hc/H14-378-2021-2-eng.pdf
Nasserie T, Hittle M, Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: A Systematic Review. JAMA Network Open. 2021;4(5):e2111417. Available from: https://doi.org/10.1001/jamanetworkopen.2021.11417
National Institute on Ageing. Alzheimer's Disease Genetics Fact Sheet. National Institute on Aging. 2019. Available from: https://www.nia.nih.gov/health/alzheimers-disease-genetics-fact-sheet
National Institute on Ageing. Closing the Gaps: Advancing Emergency Preparedness, Response and Recovery for Older Adults. National Institute on Ageing. 2020. Available from: https://www.nia-ryerson.ca/commentary-posts/2020/12/14/closing-the-gaps-advancing-emergency-preparedness-response-and-recovery-for-older-adults
Office of Indigenous Initiatives. Ways of Knowing. Queen's University. Available from: https://www.queensu.ca/indigenous/ways-knowing/about
Petrasek MacDonald J, Ward V, Halseth R. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and Risk Factors. National Collaborating Centre for Aboriginal Health. 2018. Available from: https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf
Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS). Government of Canada. 2021. Available from: https://health-infobase.canada.ca/ccdss/Index
Public Health Agency of Canada. Dementia Strategic Fund: Dementia Guidelines and Best Practices Initiative. Government of Canada. 2021. Available from: https://www.canada.ca/en/public-health/services/funding-opportunities/grant-contribution-funding-opportunities/dementia-strategic-fund-dementia-guidelines-best-practices-initiative.html
Public Health Agency of Canada. Physical Activity Tips for Children (5-11 years). Government of Canada. 2019. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/physical-activity-tips-children-5-11-years.html
Public Health Agency of Canada. Physical Activity Tips for Youth (12-17 years). Government of Canada. 2019. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/physical-activity-tips-youth-12-17-years.html
Ragheb J, McKinney A, Zierau M, et al. Delirium and neuropsychological outcomes in critically ill patients with COVID-19: a cohort study. BMJ Open. 2021;11 (9):e050045. Available from: https://doi.org/10.1136/bmjopen-2021-050045
Raina P, Wolfson C, Griffith L, et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nature Aging. 2021;1:1137–1147. Available from: https://doi.org/10.1038/s43587-021-00128-1
Rana A, de Souza RJ, Kandasamy S, Lear SA, Anand SS. Cardiovascular risk among South Asians living in Canada: a systematic review and meta-analysis. CMAJ Open. 2014;2(3):E183–91. Available from: https://doi.org/10.9778/cmajo.20130064
Shield K, Wells S, Rehm J, et al. Alcohol consumption and the COVID-19 pandemic: synthesizing knowledge for policy action. 2020. Canadian Institutes of Health Research. Available from: https://cihr-irsc.gc.ca/e/documents/SHIELD_CMH-KS-Knowledge-Synthesis__2020-09-22.pdf
Sims R, Hill M, Williams J. The multiplex model of the genetics of Alzheimer's disease. Nature Neuroscience. 2020;23:311–322. Available from: https://doi.org/10.1038/s41593-020-0599-5
Stall NM, Johnstone J, McGreer AJ, Dhuper M, Dunning J, Sinha SK. Finding the Right Balance: An Evidence-Informed Guidance Document to Support the Re-Opening of Canadian Nursing Homes to Family Caregivers and Visitors during the Coronavirus Disease 2019 Pandemic. Journal of the American Medical Directors Association. 2020;21(10):1365–1370.e7. Available from: https://doi.org/10.1016/j.jamda.2020.07.038
Statistics Canada. Alcohol and cannabis use during the pandemic: Canadian Perspectives Survey Series 6. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/210304/dq210304a-eng.htm
Statistics Canada. Canadian Social Survey: Loneliness in Canada. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/211124/dq211124e-eng.htm
Statistics Canada. Experiences of health care workers during the COVID-19 pandemic, September to November 2021. Statistics Canada. 2022. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/220603/dq220603a-eng.htm
Statistics Canada. Table 13-10-0096-01 Health characteristics, annual estimates DOI: https://doi.org/10.25318/1310009601-eng
Statistics Canada. Health models. Statistics Canada. 2021. Available from: https://www.statcan.gc.ca/en/microsimulation/health/health
Statistics Canada. Immigration and ethnocultural diversity: Key results from the 2016 Census. Statistics Canada. 2017. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025b-eng.htm
Statistics Canada. Survey on COVID-19 and Mental Health, February to May 2021. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm
Tait JL, Collyer TA, Gall SL, et al. Longitudinal associations of childhood fitness and obesity profiles with midlife cognitive function: an Australian cohort study. Journal of Science and Medicine in Sport. 2022;25(8):667–672. Available from: https://doi.org/10.1016/j.jsams.2022.05.009
Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021;8(5):416–427. Available from: https://doi.org/10.1016/S2215-0366(21)00084-5
Thompson K, Dutton DJ, MacNabb K, Liu T, Blades S, Asbridge M. Changes in alcohol consumption during the COVID-19 pandemic: exploring gender differences and the role of emotional distress. Health Promotion and Chronic Disease Prevention in Canada. 2021;41(9):254–63. Available from: https://doi.org/10.24095/hpcdp.41.9.02
Veenstra G, Patterson AC. Black–White Health Inequalities in Canada. Journal of Immigrant and Minority Health. 2016;18(1),51–7. Available from: https://doi.org/10.1007/s10903-014-0140-6
Watt J, Colley RC. Youth—but not adults—reported less physical activity during the COVID-19 pandemic. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/en/pub/45-28-0001/2021001/article/00032-eng.pdf?st=JxVe1Qht
Wister A, Li L, Mitchell B, et al. Levels of depression and anxiety among informal caregivers during the COVID-19 pandemic: A study based on the Canadian Longitudinal Study on Aging. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2022;gbac035. Available from: https://doi.org/10.1093/geronb/gbac035
Wolters FJ, Ikram MA. Epidemiology of Vascular Dementia. Arteriosclerosis, Thrombosis, and Vascular Biology. 2019;39:1542–1549. Available from: https://doi.org/10.1161/ATVBAHA.119.311908
World Health Organization. WHOQOL: Measuring Quality of Life. World Health Organization. Available from: https://www.who.int/tools/whoqol
Xu S, Park M, Kang UG, Choi JS, Koo JW. Problematic Use of Alcohol and Online Gaming as Coping Strategies During the COVID-19 Pandemic: A Mini Review. Front Psychiatry. 2021;12:685964. Available from: https://www.doi.org/10.3389/fpsyt.2021.685964
Yamazaki Y, Zhao N, Caulfield TR, Liu CC, Bu G. Apolipoprotein E and Alzheimer disease: pathobiology and targeting strategies. Nature Reviews Neurology. 2019;15:501–518. Available from: https://doi.org/10.1038/s41582-019-0228-7
Yang AC, Kern F, Losada PM, et al. Dysregulation of brain and choroid plexus cell types in severe COVID-19. Nature. 2021;595:565–571. Available from: https://doi.org/10.1038/s41586-021-03710-0
Endnotes
- Footnote 1
-
When interpreting the public opinion research presented in this report, please refer to the methodologies included in the reports that are posted on Library and Archives Canada.
- Footnote 2
-
A care provider is a person who provides care and support to a person living with dementia in a paid or unpaid role.
- Footnote 3
-
Please note that some of the websites this report links to may not have content in both English and French.
- Footnote 4
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Knowledge, Perspectives and Experience of Dementia Care Providers: Final Report. Government of Canada. 2021. Available from:
https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-380-2021-eng.pdf - Footnote 5
-
Age-standardized rates account for the differences in the age structure of the populations being compared. In the calculation of the age-standardized rate, either one population is mathematically adjusted to have the same age structure as the other; or both populations are mathematically adjusted to have the same age structure as a third population, called the standard population. In this way, the two groups are given the same age distribution structure so that a more representative picture of the characteristic in question is provided. (https://www.statcan.gc.ca/en/dai/btd/asr)
- Footnote 6
-
All rates are age-standardized to the Canadian population. All data from the Canadian Community Health Survey and Canadian Health Measures Survey are representative of Canada, excluding the territories. Please use caution when interpreting data collected in 2020 from the Canadian Community Health Survey. Data collection was halted on account of the COVID-19 pandemic from mid-March until September 2020. Statistics Canada notes that the "impossibility of conducting in-person interviews, the shorter collection periods and collection capacity issues resulted in a significant decrease in the response rates" and that "users are advised to use the CCHS 2020 data with caution, especially when creating estimates for small sub-populations or when comparing to other CCHS years." In this table, CCHS 2020 data are from the collection period between September-December 2020. Statistics Canada. Table 13-10-0096-01 Health characteristics, annual estimates DOI: https://doi.org/10.25318/1310009601-eng and Centre for Surveillance and Applied Research, Public Health Agency of Canada. Canadian Chronic Disease Indicators Data Tool, 2021 Edition. Public Health Infobase. Ottawa (ON): Public Health Agency of Canada, 2021.
- Footnote 7
-
Heavy alcohol drinking is defined as binge drinking (i.e. five or more drinks for males and four or more drinks for females, on a single occasion) at least once a month in the past year.
- Footnote 8
-
Examining trends in heavy drinking from 2015 to 2020, the 2020 data point is the first data point in which a significant difference is seen. Given limitations of the data collected in 2020, please use caution when interpreting this apparent change.
- Footnote 9
-
This physical activity measure uses device-measured physical activity data from the Canadian Health Measures Survey (CHMS). It is used to report on adherence to the Canadian 24-Hour Movement Guidelines recommendations for physical activity by PHAC. Self-reported estimates of physical activity, which report perceived time, are often significantly higher than device-based measures, which measure actual movement. Self-report and device-measured data provide complementary information about different aspects of physical activity but should not be used interchangeably.
- Footnote 10
-
Sense of belonging to a local community illustrates the social attachment of individuals with communities. Social isolation tends to be detrimental to health, while social engagement and attachments are associated with positive health outcomes (both physical and mental).
- Footnote 11
-
Obesity among adults is defined as a BMI ≥ 30.0 kg/m2. This indicator is based on self-reported weight and height. BMI calculations are adjusted to respondent bias to more closely approximate measured values. Pregnant women excluded.
- Footnote 12
-
Government of Canada. Dementia: Overview. Available from:
https://www.canada.ca/en/public-health/services/diseases/dementia.html - Footnote 13
-
Public Health Agency of Canada. 2017-2018 estimates in Canadian Chronic Disease Surveillance System (CCDSS) Data Tool 2019. Canada.ca. https://health-infobase.canada.ca/ccdss/data-tool/
- Footnote 14
-
A caregiver is defined as a person who provides unpaid care and support to someone living with dementia. A caregiver is likely to be a relative, close friend, neighbour or volunteer. Support may include assisting with the activities of daily living and helping with advance care planning.
- Footnote 15
-
This number includes an estimate of indirect trainees for applications where number of trainees were not directly reported. The estimate is calculated based on the amount spent on students divided by average students salaries, based on recent Canadian Institutes of Health Research internal data.
- Footnote 16
-
Earnscliffe Strategy Group for the Public Health Agency of Canada. Quality of Life and Dementia Quality and Quantitative Research: Final Report. Government of Canada. 2020. Available from: https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por-ef/public_health_agency_canada/2021/081-20-e/POR081-20-Report-FINAL-EN.pdf
- Footnote 17
-
The care provider categories for this study included health care professionals, developmental service workers, personal care workers and unpaid caregivers from each provincial region of the country. Ekos Research Associates Inc. for the Public Health Agency of Canada. Knowledge, Perspectives and Experience of Dementia Care Providers: Final Report. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-380-2021-eng.pdf
- Footnote 18
-
These data points are about people living with dementia who are receiving home care in the Yukon, British Columbia, Alberta and Newfoundland and Labrador in 2020–21. Data from 2020–2021 should be interpreted with care. The number of home care clients with dementia decreased by about 3% between 2019–20 and 2020–21, which may reflect the impact of the COVID-19 pandemic on the provision of home care services.
- Footnote 19
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the Resident Assessment Instrument - Home Care (RAI HC)©- Home Care Reporting System (HCRS), fiscal year 2020-21. It is representative of people living with dementia receiving home care in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.
- Footnote 20
-
There has been a significant increase in the percentage of people living with dementia receiving home care experiencing reduced social interaction from 2019–20 to 2020–21. A similar increase was also seen for home care clients without dementia, which suggests that the change likely reflects the impact of COVID-19 public health restrictions (such as stay-at-home orders). The percentage of people living with dementia receiving home care experiencing withdrawal from activities of interest or a potential or actual problem with depression or experiencing daily pain (severe and not severe) have stayed relatively stable from 2019–20 to 2020–21. Data was collected up to March 31, 2021.
- Footnote 21
-
Caregivers who are distressed are defined as primary caregivers who express feelings of distress, anger or depression and/or any caregiver who is unable to continue in their caring activities.
- Footnote 22
-
These data points are from the Yukon, British Columbia, Alberta and Newfoundland and Labrador in 2020–21.
- Footnote 23
-
"The Population Health Model (POHEM) is a microsimulation model of diseases and risk factors in which the basic unit of analysis is the individual person. The simulation creates and ages a large sample population representative of Canada, one individual at a time, until death. The life trajectory of each simulated person unfolds by exposure to different life-like events, such as smoking initiation and cessation, changes in weight and/or leisure time physical activity, and incidence of diseases such as osteoarthritis, diabetes, cardiovascular disease, and dementia." Statistics Canada. Health Models. Statistics Canada. 2021. https://www.statcan.gc.ca/en/microsimulation/health/health
- Footnote 24
-
'The CCDSS collects data on all residents who are eligible for provincial or territorial health insurance. It can generate national estimates and trends over time for over 20 chronic diseases and conditions, and other selected health outcomes. To identify people with chronic diseases and conditions, provincial and territorial health insurance registry records are linked using a unique personal identifier to the corresponding physician billing claims, hospital discharge abstract records and prescription drug records." Public Health Agency of Canada. Canadian Chronic Disease Surveillance System (CCDSS). Government of Canada, 2021. https://health-infobase.canada.ca/ccdss/Index
- Footnote 25
-
The Continuing Care Reporting System is a database that covers populations living in LTC across Canada; British Columbia linked it to the CCDSS for this project.
- Footnote 26
-
This project is building on previous work: Godard-Sebillotte C, et al. Development of two hierarchical algorithms identifying the 65+ community dwelling population in the provincial administrative database in Quebec. CAHSPR Annual conference.
- Footnote 27
-
All rates are age-standardized to the 2011 Canadian population. Provincial and territorial data for blood cholesterol and daily sleep are not available.
- Footnote 28
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Survey of Canadians Regarding Dementia Prevention: Final Report. Government of Canada. 2022. Available from: https://epe.lac-bac.gc.ca/100/200/301/pwgsc-tpsgc/por- ef/public_health_agency_canada/2022/104-21-e/POR104-21-Final-Report.pdf
- Footnote 29
-
Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413-446. Available from: https://doi.org/10.1016/S0140-6736(20)30367-6
- Footnote 30
-
This table describes the increased dementia risk associated with the 12 potentially modifiable risk factors from a global perspective. For example, someone who experiences hypertension in midlife could be 60% more likely to be diagnosed with dementia than someone who does not have hypertension. Limiting these risk factors may have a significant impact on reducing the risk overall of dementia and improving one's health.
- Footnote 31
-
The Knowledge, Perspectives and Experience of Dementia Care Providers public opinion research project surveyed 1593 dementia care providers including family and friend caregivers, health care professionals, developmental services workers, personal care workers and first responders. Ekos Research Associates Inc. for the Public Health Agency of Canada. Knowledge, Perspectives and Experience of Dementia Care Providers: Final Report. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-380-2021-eng.pdf
- Footnote 32
-
Healthcare professionals in this context include physicians, nurses, technicians, and social workers.
- Footnote 33
-
There is some evidence that air pollution is associated with an increased risk of dementia and this link continues to be investigated. Examples of air pollution could include high nitrogen dioxide concentrations, carbon monoxide and other chemicals. The 2020 report of the Lancet Commission estimates that people over the age of 65 exposed to air pollution are 10% more likely to be diagnosed with dementia, compared with someone who is not exposed.
- Footnote 34
-
Guidance refers to evidence-based recommendations in various formats, including formal guidelines and best practices.
- Footnote 35
-
Participants include specialized dementia care providers (e.g. health care providers), staff and management providing care to people living with dementia in various settings (e.g. long-term care, home care, etc.), health care providers that do not regularly provide care to people living with dementia, family/ friend caregivers, researchers familiar with dementia, government representatives, people providing non-care related services to people living with dementia, people living with dementia and employers.
- Footnote 36
-
Knowledge translation is the exchange, synthesis and ethically-sound application of knowledge to accelerate the capture of the benefits of research for Canadians (https://cihr-irsc.gc.ca/e/29418.html#2)
- Footnote 37
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Dementia Guidance and Indigenous Populations in Canada:
Findings Report. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/aspc-phac/H14-374-2021-eng.pdf - Footnote 38
-
Alzheimer's Society (UK). Is dementia hereditary? Alzheimer's Society (UK). Available from: https://www.alzheimers.org.uk/about-dementia/risk-factors-and-prevention/is-dementia-hereditary
- Footnote 39
-
Alzheimer Society of Canada. Risk factors for dementia. Alzheimer Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/how-can-i-prevent-dementia/risk-factors-dementia
- Footnote 40
-
Sims R, Hill M, Williams J. The multiplex model of the genetics of Alzheimer's disease. Nature Neuroscience. 2020;23:311–322. Available from: https://doi.org/10.1038/s41593-020-0599-5
- Footnote 41
-
Lourida I, Hannon E, Littlejohns TJ, et al. Association of Lifestyle and Genetic Risk With Incidence of Dementia. JAMA. 2019;322(5):430–437. Available from: https://doi.org/10.1001/jama.2019.9879
- Footnote 42
-
Lourida I, Hannon E, Littlejohns TJ, et al. Association of Lifestyle and Genetic Risk With Incidence of Dementia. JAMA. 2019;322(5):430–437. Available from: https://doi.org/10.1001/jama.2019.9879
- Footnote 43
-
Dekhtyar S, Marseglia A, Xu W, Darin-Mattsson A, Wang HX, Fratiglioni L. Genetic risk of dementia mitigated by cognitive reserve: A cohort study. Annals of Neurology. 2019;86(1):68-78. Available from: https://doi.org/10.1002/ana.25501
- Footnote 44
-
Alzheimer Society of Canada. What is Alzheimer's disease? Alzheimer Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/what-alzheimers-disease
- Footnote 45
-
Yamazaki Y, Zhao N, Caulfield TR, Liu CC, Bu G. Apolipoprotein E and Alzheimer disease: pathobiology and targeting strategies. Nature Reviews Neurology. 2019;15:501-518. Available from: https://doi.org/10.1038/s41582-019-0228-7
- Footnote 46
-
National Institute on Aging. Alzheimer's Disease Genetics Fact Sheet. National Institute on Aging. 2019. Available from: https://www.nia.nih.gov/health/alzheimers-disease-genetics-fact-sheet
- Footnote 47
-
Mayo Clinic. Alzheimer's genes: Are you at risk? Mayo Clinic. 2021. Available from:
https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-genes/art-20046552 - Footnote 48
-
Wolters FJ, Ikram MA. Epidemiology of Vascular Dementia. Arteriosclerosis, Thrombosis, and Vascular Biology. 2019;39:1542-1549. Available from: https://doi.org/10.1161/ATVBAHA.119.311908
- Footnote 49
-
Hodges JR, Piguet O. Progress and Challenges in Frontotemporal Dementia Research: A 20-Year Review. Journal of Alzheimer's disease. 2018;62(3):1467-1480. Available from: https://doi.org/10.3233/jad-171087
- Footnote 50
-
Heerema E. What Causes Lewy Body Dementia? Verywell Health. 2022. Available from: https://www.verywellhealth.com/lewy-body-dementia-risks-98761
- Footnote 51
-
Alzheimer Society of Canada. Dementia with Lewy bodies. Alzheimer's Society of Canada. Available from: https://alzheimer.ca/en/about-dementia/other-types-dementia/dementia-lewy-bodies
- Footnote 52
-
Alzheimer's Association. Is Alzheimer's Genetic? Alzheimer's Association. Available from:: https://www.alz.org/alzheimers-dementia/what-is-alzheimers/causes-and-risk-factors/genetics
- Footnote 53
-
Tait JL, Collyer TA, Gall SL, et al. Longitudinal associations of childhood fitness and obesity profiles with midlife cognitive function: an Australian cohort study. Journal of Science and Medicine in Sport. 2022;25(8):667-672. Available from: https://doi.org/10.1016/j.jsams.2022.05.009
- Footnote 54
-
Hakala JO, Rovio SP, Pahkala K, et al. Physical Activity from Childhood to Adulthood and Cognitive Performance in Midlife. Medicine and Science in Sports and Exercise. 2019;51(5):882-890. Available from: https://doi.org/10.1249/mss.0000000000001862
- Footnote 55
-
Middleton LE, Barnes DE, Lui L-Y, Yaffe K. Physical Activity Over the Life Course and Its Association with Cognitive Performance and Impairment in Old Age. Journal of the American Geriatrics Society. 2010;58(7):1322-6. Available from: https://doi.org/10.1111/j.1532-5415.2010.02903.x
- Footnote 56
-
Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. International Journal of Behavioral Nutrition and Physical Activity. 2020;17:85. Available from: https://doi.org/10.1186/s12966-020-00987-8
- Footnote 57
-
Moore SA, Faulkner G, Rhodes RE, et al. Few Canadian children and youth were meeting the 24-hour movement behaviour guidelines 6-months into the COVID-19 pandemic: Follow-up from a national study. Applied Physiology, Nutrition, and Metabolism. 2021;46(10):1225-1240. Available from: https://doi.org/10.1139/apnm-2021-0354
- Footnote 58
-
Watt J, Colley RC. Youth—but not adults—reported less physical activity during the COVID-19 pandemic. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/en/pub/45-28-0001/2021001/article/00032-eng.pdf?st=JxVe1Qht
- Footnote 59
-
Statistics Canada. Canadian Social Survey: Loneliness in Canada. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/211124/dq211124e-eng.htm
- Footnote 60
-
Statistics Canada. Alcohol and cannabis use during the pandemic: Canadian Perspectives Survey Series 6. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/210304/dq210304a-eng.htm
- Footnote 61
-
Clair R, Gordon M, Kroon M, Reilly C. The effects of social isolation on well-being and life satisfaction during pandemic. Humanities and Social Sciences Communications. 2021;8:28. Available from: https://doi.org/10.1057/s41599-021-00710-3
- Footnote 62
-
Xu S, Park M, Kang UG, Choi JS, Koo JW. Problematic Use of Alcohol and Online Gaming as Coping Strategies During the COVID-19 Pandemic: A Mini Review. Front Psychiatry. 2021;12:685964. Available from: https://www.doi.org/10.3389/fpsyt.2021.685964
- Footnote 63
-
Shield K, Wells S, Rehm J, et al. Alcohol consumption and the COVID-19 pandemic: synthesizing knowledge for policy action. 2020. Canadian Institutes of Health Research. Available from::
https://cihr-irsc.gc.ca/e/documents/SHIELD_CMH-KS-Knowledge-Synthesis__2020-09-22.pdf - Footnote 64
-
This includes all jurisdictions except Quebec. Canadian Institute for Health Information. Hospital stays for substance use harms increased during the first months of the COVID-19 pandemic. Canadian Institutes for Health Information. 2021. Available from::
https://www.cihi.ca/en/hospital-stays-for-substance-use-harms-increased-during-the-first-months-of-the-covid-19-pandemic - Footnote 65
-
Thompson K, Dutton DJ, MacNabb K, Liu T, Blades S, Asbridge M. Changes in alcohol consumption during the COVID-19 pandemic: exploring gender differences and the role of emotional distress. Health Promotion and Chronic Disease Prevention in Canada. 2021;41(9):254-63. Available from: https://doi.org/10.24095/hpcdp.41.9.02
- Footnote 66
-
Dobson KG, Vigod SN, Mustard C, Smith PM. Trends in the prevalence of depression and anxiety disorders among Canadian working age adults between 2000 and 2016. Health Reports. 2020; 31(12): 12-23. Available from::
https://doi.org/10.25318/82-003-x202001200002-eng - Footnote 67
-
Statistics Canada. Survey on COVID-19 and Mental Health, February to May 2021. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm
- Footnote 68
-
Cosco TD, Wister A, Riadi I, Kervin L, Best J, Raina P. Reduced ability to engage in social and physical activity and mental health of older adults during the COVID-19 pandemic: longitudinal analysis from the Canadian Longitudinal Study on Aging. The Lancet. 2021;398:S35. https://doi.org/10.1016/S0140-6736(21)02578-2
- Footnote 69
-
Raina P, Wolfson C, Griffith L, et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle- aged and older adults from the Canadian Longitudinal Study on Aging. Nature Aging. 2021;1:1137–1147. Available from: https://doi.org/10.1038/s43587-021-00128-1
- Footnote 70
-
Wister A, Li L, Mitchell B, et al. Levels of depression and anxiety among informal caregivers during the COVID-19 pandemic: A study based on the Canadian Longitudinal Study on Aging. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2022;gbac035. Available from: https://doi.org/10.1093/geronb/gbac035
- Footnote 71
-
The Canadian Longitudinal Study on Aging (CLSA) is a large, national, long-term study that collects a range of health-related data on approximately 50,000 individuals over approximately 20 years; individuals were between the ages of 45 and 85 years when recruited into the study in 2009. This existing research platform was leveraged to address evidence needs presented by the COVID-19 pandemic. Raina, P., Wolfson, C., Griffith, L. et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nat Aging 1, 1137–1147 (2021). https://doi.org/10.1038/s43587-021-00128-1
- Footnote 72
-
Frontera JA, Boutajangout A, Masurkar AV, et al. Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer's dementia. Alzheimer's & Dementia. 2022;18(5):899-910. Available from: https://doi.org/10.1002/alz.12556
- Footnote 73
-
Douaud G, Lee S, Alfaro-Almagro F, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604(7907):697-707. Available from: https://doi.org/10.1038/s41586-022-04569-5
- Footnote 74
-
Yang AC, Kern F, Losada PM, et al. Dysregulation of brain and choroid plexus cell types in severe COVID-19. Nature. 2021;595:565- 571. Available from: https://doi.org/10.1038/s41586-021-03710-0
- Footnote 75
-
The cohorts included all patients older than 10 years who had an index event on or after Jan 20, 2020 (the date of the first recorded COVID-19 case in the USA), and who were still alive at the time of the main analysis (Dec 13, 2020).
- Footnote 76
-
Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021;8(5):416–427. Available from: https://doi.org/10.1016/S2215-0366(21)00084-5
- Footnote 77
-
Nasserie T, Hittle M, Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID- 19: A Systematic Review. JAMA Network Open. 2021;4(5):e2111417. Available from: https://doi.org/10.1001/jamanetworkopen.2021.11417
- Footnote 78
-
Ragheb J, McKinney A, Zierau M, et al. Delirium and neuropsychological outcomes in critically ill patients with COVID-19: a cohort study. BMJ Open. 2021;11 (9):e050045. Available from: https://doi.org/10.1136/bmjopen-2021-050045
- Footnote 79
-
Nakazawa T, Ohara T, Hirabayashi N, et al. Multiple-region grey matter atrophy as a predictor for the development of dementia in a community: the Hisayama Study. Journal of Neurology, Neurosurgery & Psychiatry. 2021;93:263-271. Available from: http://dx.doi.org/10.1136/jnnp-2021-326611
- Footnote 80
-
Marin C, Vilas D, Langdon C, et al. Olfactory Dysfunction in Neurodegenerative Diseases. Current Allergy and Asthma Reports. 2018;18(8):42. Available from: https://doi.org/10.1007/s11882-018-0796-4
- Footnote 81
-
Narrative Research for the Public Health Agency of Canada. Priorities for an Information Portal on Dementia. Government of Canada. 2021. Available from: https://publications.gc.ca/collections/collection_2021/sc-hc/H14-378-2021-2-eng.pdf
- Footnote 82
-
Phase II questionnaire participants (n=125) were asked whether they feel that dementia guidance related to treatment and management is sufficiently easy to obtain for caregivers. Most (n=75; 60%) said no, with a greater proportion of caregiver questionnaire participants answering no (77%), compared with other participant types (30% - 60%). Of the questionnaire participants who said no, they indicated that people living with dementia and caregivers do not know where to go to get reliable information regarding treatment and management of dementia, especially right after receiving a diagnosis (n=37). Accessibility issues were also noted by these participants for people living with dementia and caregivers trying to access dementia guidance related to treatment and management (n=15).
- Footnote 83
-
The summary includes both guidance developed outside Canada and inside Canada. Guidance elements are individual recommendations, guidelines, best practices, or considerations on dementia found in a guidance document.
- Footnote 84
-
The AGREE Global Rating Scale is an evaluation framework used to assess the quality of a guidance document.
- Footnote 85
-
World Health Organization. WHOQOL: Measuring Quality of Life. World Health Organization. Available from: https://www.who.int/tools/whoqol
- Footnote 86
-
Canadian Institute for Health Information. Dementia in long-term care. Canadian Institutes for Health Information. Available from: https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-care
- Footnote 87
-
Canadian Institute for Health Information. COVID-19's impact on long-term care. Canadian Institutes for Health Information. 2021. Available from: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care
- Footnote 88
-
Canadian Institute for Health Information. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months. Canadian Institutes for Health Information. 2021. Available from::
https://www.cihi.ca/sites/default/files/document/impact-covid-19-long-term-care-canada-first-6-months-report-en.pdf - Footnote 89
-
Statistics Canada. Experiences of health care workers during the COVID-19 pandemic, September to November 2021. Statistics Canada. 2022. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/220603/dq220603a-eng.htm
- Footnote 90
-
Canadian Institute for Health Information. Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare With Other Countries?. Ottawa, ON: CIHI; 2020.
- Footnote 91
-
Canadian Institute for Health Information. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months. Ottawa, ON: CIHI; 2021.
- Footnote 92
-
Statistics Canada. Provisional death counts and excess mortality, January 2020 to February 2021. 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210514/dq210514c-eng.htm
- Footnote 93
-
Statistics Canada. Impacts of the COVID-19 pandemic in nursing and residential care facilities in Canada. 2021. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00025-eng.htm
- Footnote 94
-
The residential care facilities included in this survey were long-term care homes, retirement homes or assisted living facilities, mental health facilities and other residential care facilities (such as group homes for persons with disabilities or addictions, homes for women, etc.). Results are from 4,217 residential care facilities and data was collected up to December 31, 2020.
- Footnote 95
-
Clarke J. Impacts of the COVID-19 pandemic in nursing and residential care facilities in Canada. Statistics Canada. 2021. Available from: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00025-eng.htm
- Footnote 96
-
House of Commons. HESA Committee Meeting. Parliament of Canada. 2022. Available from: https://www.ourcommons.ca/DocumentViewer/en/44-1/HESA/meeting-6/minutes
- Footnote 97
-
Hindmarch W, McGhan G, Flemons K, McCaughey D. COVID-19 and Long-Term Care: the Essential Role of Family Caregivers. Canadian Geriatrics Journal. 2021;24(3):195-199. Available from: https://doi.org/10.5770/cgj.24.508
- Footnote 98
-
Responsive behaviours are actions, words or gestures presented by a person living with dementia as a way of responding to something negative, frustrating or confusing in their social and physical environment.
- Footnote 99
-
Stall NM, Johnstone J, McGreer AJ, Dhuper M, Dunning J, Sinha SK. Finding the Right Balance: An Evidence-Informed Guidance Document to Support the Re-Opening of Canadian Nursing Homes to Family Caregivers and Visitors during the Coronavirus Disease 2019 Pandemic. Journal of the American Medical Directors Association. 2020;21(10):1365-1370.e7. Available from: https://doi.org/10.1016/j.jamda.2020.07.038
- Footnote 100
-
Ikeda M, Mori E, Hirono N, et al. Amnestic people with Alzheimer's disease who remembered the Kobe earthquake. The British Journal of Psychiatry. 1998;172:425-8. Available from: https://doi.org/10.1192/bjp.172.5.425
- Footnote 101
-
National Institute on Ageing. Closing the Gaps: Advancing Emergency Preparedness, Response and Recovery for Older Adults. National Institute on Ageing. 2020. Available from: https://www.nia-ryerson.ca/commentary-posts/2020/12/14/closing-the-gaps-advancing-emergency-preparedness-response-and-recovery-for-older-adults
- Footnote 102
-
Lancet Countdown, Canadian Medical Association, Canadian Public Health Association. The Lancet Countdown on Health and Climate Change: Policy Brief for Canada. Lancet Countdown, Canadian Medical Association, Canadian Public Health Association. 2021. Available from: https://www.cpha.ca/sites/default/files/uploads/advocacy/2021_lancet/2021_Lancet_Countdown_Canada_Policy_Brief_e.pdf
- Footnote 103
-
British Columbia Coroners Service. Extreme Heat and Human Mortality: A Review of Heat-Related Deaths in B.C. in Summer 2021. British Columbia Coroners Service. 2022. Available from: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-panel/extreme_heat_death_review_panel_report.pdf
- Footnote 104
-
Henderson SB, McLean KE, Lee MJ, Kosatsky T. Analysis of community deaths during the catastrophic 2021 heat dome: Early evidence to inform the public health response during subsequent events in greater Vancouver, Canada. Environmental Epidemiology. 2022;6(1):e189. Available from: https://doi.org/10.1097/ee9.0000000000000189
- Footnote 105
-
Laccarino L, La Joie R, Lesman-Segev OH, et al. Association Between Ambient Air Pollution and Amyloid Positron Emission Tomography Positivity in Older Adults With Cognitive Impairment. JAMA Neurology. 2021;78(2):197–207. Available from: https://doi.org/10.1001/jamaneurol.2020.3962
- Footnote 106
-
Coogan SCP, Robinne FN, Jain P, Flannigan MD. Scientists' warning on wildfire — a Canadian perspective. Canadian Journal of Forest Research. 2019;49(9):1015-1023. https://doi.org/10.1139/cjfr-2019-0094
- Footnote 107
-
Gibson A. Stories from the Flood: Dementia Caregivers' Disaster Response Training Recommendations. The Gerontologist. 2016;56(3):285. Available from: https://doi.org/10.1093/geront/gnw162.1154
- Footnote 108
-
Gibson A, Walsh J, Brown LM. A perfect storm: Challenges encountered by family caregivers of persons with Alzheimer's disease during natural disasters. Journal of Gerontological Social Work. 2018;61(7):775-789. Available from: https://doi.org/10.1080/01634372.2018.1474158
- Footnote 109
-
Manly JJ, Mayeux R. Ethnic Differences in Dementia and Alzheimer's Disease. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Available from: https://www.ncbi.nlm.nih.gov/books/NBK25535/
- Footnote 110
-
Khan M, Kobayashi K, Lee SM, Vang Z. (In)Visible Minorities in Canadian Health Data and Research. Population Change and Lifecourse Strategic Knowledge Cluster Discussion Paper Series. 2015; 3(1): 5. Available from: https://ir.lib.uwo.ca/pclc/vol3/iss1/5
- Footnote 111
-
Ekos Research Associates Inc. for the Public Health Agency of Canada. Dementia Survey: Final Report. Government of Canada. 2020.:
Available from: https://publications.gc.ca/collections/collection_2020/aspc-phac/HP10-36-2020-eng.pdf - Footnote 112
-
Veenstra G, Patterson AC. Black–White Health Inequalities in Canada. Journal of Immigrant and Minority Health. 2016;18(1),51–7. Available from: https://doi.org/10.1007/s10903-014-0140-6
- Footnote 113
-
Rana A, de Souza RJ, Kandasamy S, Lear SA, Anand SS. Cardiovascular risk among South Asians living in Canada: a systematic review and meta-analysis. CMAJ Open. 2014;2(3):E183-91. Available from: https://doi.org/10.9778/cmajo.20130064
- Footnote 114
-
Across all respondents, most (75%) reported knowing or having known someone living with dementia, compared with a smaller proportion (66–70%) of Black, South American, South Asian, and Southeast Asian Canadian respondents saying they know or have known someone living with dementia.
- Footnote 115
-
Populations focused on for this study included: Indigenous peoples, individuals with intellectual disabilities, individuals with existing health issues, older adults, ethnic and cultural minority communities, LGBTQ2 individuals, official language minority communities, rural and remote communities, and individuals with young onset dementia.
- Footnote 116
-
McGraw-Hill Concise Dictionary of Modern Medicine. Cultural Competency. McGraw-Hill Concise Dictionary of Modern Medicine. 2002. Available from: https://medical-dictionary.thefreedictionary.com/Cultural+Competency
- Footnote 117
-
Evidence suggests that rates of dementia have been increasing more rapidly among Indigenous Peoples compared with the general population, and that dementia onset may be earlier among Indigenous Peoples. (Jacklin & Walker, 2012). Petrasek MacDonald J, Ward V, Halseth R. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and risk factors. National Collaborating Centre for Aboriginal Health. 2018. Available from: https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf
- Footnote 118
-
The age-standardized prevalence of dementia in 2009 in First Nations in Alberta was 7.5 per 1,000 compared with non-First Nations, at 5.6 per 1,000, which indicates that the prevalence of dementia rose more quickly for First Nations. Jacklin KM, Walker JD, Shawande M. The emergence of dementia as a health concern among First Nations populations in Alberta, Canada. Canadian Journal of Public Health. 2021;104:e39-e44. Available from: https://doi.org/10.1007/bf03405652
- Footnote 119
-
Bourassa C. Addressing the Duality of Access to Healthcare for Indigenous Communities: Racism and Geographical Barriers to Safe Care. Healthcare Papers. 2018;17(3):6-10. Available from: https://doi.org/10.12927/hcpap.2018.25507
- Footnote 120
-
Petrasek MacDonald J, Ward V, Halseth R. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and Risk Factors. National Collaborating Centre for Aboriginal Health. 2018. Available from:
https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf - Footnote 121
-
Due to the small sample size, caution should be used when interpreting Inuk data.
- Footnote 122
-
While results from this group are not shared here due to the small size of the group, they are available in report at the Library and
Archives Canada website: https://bac-lac.on.worldcat.org/oclc/1289930909?lang=en&q=Indigenous%20dementia - Footnote 123
-
Indigenous ways of knowing recognizes the complexity and diversity of Indigenous ways of learning and teaching, and refers to the vast variety of knowledge that exists across diverse Indigenous communities, including all elements of creation. Available from: https://www.queensu.ca/indigenous/ways-knowing/about
- Footnote 124
-
Culturally appropriate and culturally safe guidance acknowledge and include an understanding of cultural differences (e.g.
Indigenous perspectives of aging well), personal experiences, norms and power imbalances in the health care system to help make health related advice easier and safer for Indigenous populations. - Footnote 125
-
First Nations Health Authority. Cultural Safety and Humility. First Nations Health Authority. Available from: https://www.fnha.ca/wellness/wellness-and-the-first-nations-health-authority/cultural-safety-and-humility
- Footnote 126
-
It should be considered that the survey was only conducted in English and French which may have biased the results.