A Dementia Strategy for Canada: Together We Aspire
Download the alternative format
(3.8 MB, 110 pages)
Organization: Public Health Agency of Canada
Published: 2019-06-17
Related topics
A summary of the strategy, A Dementia Strategy for Canada: Together We Aspire: In Brief, is also available.
Table of contents
- Minister's message
- Executive summary
- Chapter 1: Introduction
- Chapter 2: National objective: Prevent dementia
- 2.1 Advance research to identify and assess modifiable risk and protective factors
- 2.2 Build the evidence base to inform and promote the adoption of effective interventions
- 2.3 Expand awareness of modifiable risk and protective factors and effective interventions
- 2.4 Support measures that increase the contribution of social and built environments to healthy living and adoption of healthy living behaviours
- Chapter 3: National objective: Advance therapies and find a cure
- 3.1 Establish and review strategic dementia research priorities for Canada
- 3.2 Increase dementia research
- 3.3 Develop innovative and effective therapeutic approaches
- 3.4 Engage people living with dementia and caregivers in the development of therapies
- 3.5 Increase adoption of research findings that support the strategy, including in clinical practice and through community supports
- Chapter 4: National objective: Improve the quality of life of people living with dementia and caregivers
- 4.1 Eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities
- 4.2 Promote and enable early diagnosis to support planning and action that maximizes quality of life
- 4.3 Address the importance of access to quality care, from diagnosis through end of life
- 4.4 Build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care
- 4.5 Improve support for family/friend caregivers, including through access to resources and supports
- Chapter 5: Pillars
- Chapter 6: Focus on higher-risk and equitable care
- Chapter 7: Moving towards implementation
- Appendices
- Appendix A: Federal government dementia-related initiatives
- Appendix B: Overview of provincial and territorial dementia-related initiatives
- Appendix C: Examples of non-governmental, not-for-profit, and international organizations working on dementia-related initiatives
- Appendix D: Engaging on dementia: learning about challenges, opportunities and solutions
- Appendix E: Glossary
- Endnotes
- Bibliography
Minister's message
I am pleased to be sharing with you Canada's first national strategy on dementia. Developing and funding this strategy has been a priority for the Government of Canada, but it is also a deeply personal priority. My first experience with dementia was during my time as a social worker; now I have a very different experience with dementia care following my mother's diagnosis. I know very well the impact that dementia can have on those living with this condition, their family members and caregivers.
Dementia has a significant and growing impact in Canada. We know that there are more than 419,000 Canadians aged 65 and older diagnosed with dementia, but this is only part of the story. This number does not capture those under the age of 65 with a diagnosis of dementia and those who, possibly due to stigma or other barriers, remain undiagnosed. This strategy is not just for those living with or caring for someone with dementia. It is a strategy for all Canadians. There is a growing body of evidence that healthy living is key to preventing dementia. Whether as a caregiver to a family member or friend, as a person living with dementia or in interactions at work or community involvement, many of us will encounter dementia at some point in our daily lives.
The release of this strategy marks a key milestone in our efforts to create a Canada where all people living with dementia and caregivers are valued and supported, and experience an optimal quality of life and where dementia is prevented, effectively treated and better understood. Canada now joins those in the international community who have already developed national dementia strategies, supporting the first target in the WHO Global Action Plan on the Public Health Response to Dementia (2017-2025).
At the opening of the National Dementia Conference in May 2018, I encouraged participants to dream big when sharing their thoughts and advice with us about the focus for our national dementia strategy. I believe we have achieved a strategy with an aspirational vision that will inspire and motivate us to work together towards our national objectives.
As we move forward, we will continue to collaborate with all those interested in addressing the challenges of dementia, including our partners in other governments, people living with dementia, caregivers, advocacy groups, health care providers and researchers. This strategy has been designed to evolve over time so that we can integrate new evidence and priorities. The Government of Canada will report to Parliament each year on the effectiveness of this strategy. New federal investments of $70 million over 5 years will also help to ensure we make meaningful progress on the national objectives of this strategy.
Many people have helped us get to this point. I would like to extend a thank you to all the individuals and organizations who shared their experiences and advice as well as their hopes and priorities for the strategy. Aging does not cause dementia, but advanced age increases risk. In her role as Minister of Seniors, Minister Filomena Tassi has been a strong supporter of the development of this national dementia strategy. Her conversations with seniors and caregivers are reflected in the strategy. I would like to thank Minister Tassi for her leadership in making dementia a priority in Canada by highlighting issues associated with this condition. I would also like to thank our provincial and territorial partners who have been generous in sharing the lessons learned from their work on dementia and who have welcomed the opportunity to collaborate. Lastly, I would especially like to thank the members of the Ministerial Advisory Board on Dementia. Led by co-chairs Pauline Tardif and Dr. William Reichman, members volunteered their time and energy to ensure that we got this strategy right. The many hours that these members dedicated to reviewing the draft strategy during its development and attending meetings to share their knowledge and expertise with us is something for which I am personally very grateful and have enriched the strategy.
The Honourable Ginette Petitpas Taylor, P.C., M.P.
Minister of Health
Executive summary
Canada's first national dementia strategy sets out a vision for the future and identifies common principles and national objectives to help guide actions by all levels of government, non-governmental organizations, communities, families and individuals. In developing the strategy, we sought at all times to ensure that people living with dementia and the family and friends who provide care to them were at the heart of these efforts.
Dementia is a term used to describe symptoms affecting the brain that include a decline in cognitive abilities such as memory; awareness of person, place, and time; language; basic math skills; judgement; and planning. Mood and behavior may also change as a result of this decline. Dementia is a progressive condition that, over time, can reduce the ability to independently maintain activities of daily life.
The National Strategy for Alzheimer's Disease and Other Dementias Act (the Act) was passed in June 2017 and followed a comprehensive report on dementia from the Senate in 2016. This Act requires the federal Minister of Health to develop a national dementia strategy, host a national conference and establish a Ministerial Advisory Board on Dementia.
The Minister held a national conference on dementia in May 2018, which brought together a diverse group of Canadians to identify and discuss challenges related to dementia, identify opportunities for collaboration and action, and share ideas for a national strategy. Participants at the conference included people living with dementia, caregivers, advocacy groups, health professionals, researchers and representatives from provincial and territorial governments.
Discussions were also held in March 2018 at 4 stakeholder roundtables across the country organized by the Alzheimer Society of Canada. Two further roundtables were held in Toronto to specifically discuss research and innovation. The roundtable on research was facilitated by the Weston Brain Institute and was attended primarily by researchers. The roundtable on innovation was facilitated by the Centre for Aging + Brain Health Innovation and attended by a diverse group of stakeholders. The strategy has also been informed by the guidance of the Ministerial Advisory Board, as well as ongoing engagement with provincial and territorial governments and other federal organizations. Footnote 1
The vision for this strategy is bold and reflects the aspirations of the many individuals and organizations who contributed to its development. The actions undertaken to achieve the strategy's national objectives may evolve over time, but every action will bring Canada closer to the vision of a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated.
Key to achieving this vision are 5 principles setting out values to guide the implementation of efforts in support of the national objectives and their areas of focus. In implementing the strategy, governments, non-governmental organizations, community organizations and others working on dementia should:
- Prioritize quality of life for people living with dementia and caregivers;
- Respect and value diversity to ensure an inclusive approach, with a focus on those most at risk or with distinct needs;
- Respect the human rights of people living with dementia to support their autonomy and dignity;
- Engage in evidence-informed decision making, taking a broad approach to gathering and sharing best available knowledge and data; and
- Maintain a results-focused approach to tracking progress, including evaluating and adjusting actions as needed.
Building on the vision and guided by these principles, the strategy identifies 3 national objectives:
- Prevent dementia
- Advance therapies and find a cure
- Improve the quality of life of people living with dementia and caregivers
Areas of focus are set out for each of these national objectives, to guide efforts toward meaningful progress.
Finally, the strategy identifies 5 underlying pillars that are essential for implementation, for upholding the principles and achieving the national objectives.
- Collaboration — Achieving progress on the strategy is a shared responsibility among governments, researchers, community organizations, people living with dementia, caregivers and many others
- Research and innovation — Promoting research and innovation will address knowledge gaps and develop therapies that will improve the quality of life of people with dementia and caregivers, and move us towards a cure
- Surveillance and data — Enhanced surveillance and data will help us to understand the scope of dementia in Canada, and focus our efforts and resources where they are most needed and will be most effective
- Information resources — The development of culturally appropriate and culturally safe information resources on dementia will facilitate the work of care providers to provide quality care and will help all Canadians to better understand dementia
- Skilled workforce — Having a sufficient and skilled workforce will support dementia research efforts and provide evidence-informed care, which will improve the quality of life of people living with dementia and caregivers
The strategy places emphasis on those groups who are at a higher risk of dementia as well as those who face barriers to equitable care. These groups include but are not limited to Indigenous peoples, individuals with intellectual disabilities, individuals with existing health issues such as hypertension and type 2 diabetes, older adults, women, ethnic and cultural minority communities, LGBTQ2 individuals, official language minority communities, rural and remote communities, and those with young onset dementia.
The final chapter of the strategy outlines next steps toward implementation including the development of indicators, identification of opportunities for focused collaboration between partners, and reporting. It concludes with the recognition that advancement of the strategy will require the collective action of many organizations and individuals, as well as the flexibility to evolve and respond to new ideas and emerging needs over time. The Government of Canada will report annually on the effectiveness of this strategy, as required by the Act, beginning in 2019.
Chapter 1: Introduction
A Dementia Strategy for Canada
Canada's first national dementia strategy places people living with dementia and the family and friends who provide care to them at its centre. Footnote 2 It provides a focused vision and direction for advancing dementia prevention, care and support in Canada.
Building on existing efforts — including provincial and territorial dementia-related initiatives as well as federal investments in dementia — the strategy sets out 3 national objectives. The implementation of this strategy relies on collaboration toward common goals across federal, provincial, territorial and local governments, as well as with many other organizations and individuals.
Text box 1: What is dementia?
Dementia is an umbrella term used to describe a set of symptoms affecting brain function that are caused by neurodegenerative and vascular diseases or injuries. It is characterized by a decline in cognitive abilities. These abilities include: memory; awareness of person, place, and time; language, basic math skills; judgement; and planning. Dementia can also affect mood and behaviour.
As a chronic and progressive condition, dementia can significantly interfere with the ability to maintain activities of daily living (PDF), such as eating, bathing, toileting and dressing.
Alzheimer's disease, vascular disease and other types of disease all contribute to dementia. Other common types of dementia include Lewy body dementia, frontotemporal dementia and mixed dementias. In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease.
This strategy includes a commitment to raise awareness of dementia across Canada. This is important, not only to help reduce stigma, but also because the strategy is for all people living in Canada regardless of whether they are currently affected by dementia. There is growing persuasive scientific evidence that healthy living from an early age may prevent or delay the onset of dementia. This strategy promotes healthy lifestyle choices and includes an emphasis on populations that are more at risk of developing dementia and those that may be facing barriers to equitable care. More information about these populations can be found in Chapter 6.
All Canadians can contribute to supporting the quality of life of those living with dementia and caregivers by better understanding dementia and helping to eliminate stigma. While most people receiving a diagnosis of dementia are in later life, dementia also affects individuals at a much younger age. The strategy will encourage dementia-inclusive communities that support people living with dementia and caregivers in staying involved in their communities and at work for as long as possible.
The strategy identifies gaps in knowledge about preventing dementia to help focus efforts by researchers and funders both nationally and internationally. There is also a need to advance efforts that improve the ability to identify, test and share effective therapies that support healthy living after a diagnosis. The strategy will encourage initiatives that broaden access to and adoption of those therapies, including in rural and remote communities and by making them culturally safe and culturally appropriate.
While the national objectives are deliberately broad in scope so that priorities and areas of focus can evolve as new knowledge and new issues emerge, the principles and pillars of the strategy are designed to be constant over time to help guide and support that evolution. The strategy will be implemented through activities such as those undertaken by governments, researchers and other partners, and its impact will be tracked through annual reports to Parliament. Canada's strategy also responds to the call for action in the World Health Organization's (WHO) Global Action Plan on the Public Health Response to Dementia (2017-2025) and its designation of dementia as a public health priority. The scope of the Canadian strategy responds to all 7 action areas identified by the WHO plan and aligns with its cross-cutting principles.
Impact of dementia on Canadians
Dementia has a significant and growing impact on Canadians. In 2015–16, more than 419,000 Canadians (6.9%) aged 65 years and older were living with diagnosed dementia. Footnote 3 As this number does not include those under age 65 who may have a young onset diagnosis nor those that have not been diagnosed, the true picture of dementia in Canada may be somewhat larger. See Text box 2 for some key statistics on dementia in Canada.
Text box 2: Key statistics on dementia in Canada
- More than 419,000: the number of Canadians aged 65 years of age and older who are living with diagnosed dementia
- 78,600: the number of new cases of dementia in Canada diagnosed per year among people aged 65 years of age and older
- 63%: the percentage of those aged 65 years of age and older living with diagnosed dementia in Canada who are women
- 9: the approximate number of seniors who are diagnosed with dementia every hour in Canada
- 26 hours: the average number of hours that family/friend caregivers spend per week supporting a person with dementia
- $8.3 billion: the total health care costs and out-of-pocket caregiver costs of dementia in Canada in 2011
- $16.6 billion: the projected total health care costs and out-of-pocket caregiver costs of dementia in Canada by 2031
While dementia is not an inevitable part of aging, age is the most important risk factor. As a result, with a growing and aging population, the number of Canadians living with dementia is expected to increase in future decades.Footnote 4 Estimates suggest 50 million people are living with dementia worldwide.Footnote 5 As the proportion of the population aged 65 years and older continues to rise, countries around the world are expected to experience similar increases in the number of individuals living with dementia.Footnote 6
Of those aged 65 years and older living with diagnosed dementia in Canada in 2015–16, almost two-thirds (63%) were women.Footnote 7 Women have higher rates of Alzheimer's disease, while men have higher rates of other types of dementia, such as frontotemporal and Lewy body dementias.Footnote 8 The number of women in long-term care with dementia also greatly exceeds the number of men, which is only partially due to longer life expectancy among women.Footnote 9
A wide range of care providers are involved in meeting the needs of people living with dementia. These needs can fluctuate as the condition progresses. Care providers include but are not limited to physicians, personal care workers, nurses, and first responders. They also include family and friend caregivers. The majority of these caregivers are female, most commonly female intimate partners and daughters.Footnote 10 On average, family and friend caregivers spend 20 hours a week caring for and supporting a person living with dementia.Footnote 11
The impact of dementia on the health care system is significant. Currently there is no cure or effective therapy to stop the progression of dementia. Direct health care costs for people living with dementia have been estimated to be 3 times higher than for those without dementia. It has been projected that the total annual health care costs and out-of-pocket caregiver costs for Canadians with dementia will double from $8.3 billion in 2011 to $16.6 billion by 2031, while indirect economic costs due to working-age death and disability are projected to increase from $0.6 billion to $0.7 billion during the same period.Footnote 12 Globally, dementia is also a major cause of disability and dependency among older adults.Footnote 13
A dialogue with Canadians
Since the passage of the National Strategy for Alzheimer's Disease and Other Dementias Act in June 2017 that formally put the development of the first national dementia strategy for Canada in motion, the Government of Canada has heard from many individuals and organizations.
This strategy reflects the valuable input and guidance received from a broad range of stakeholders. It has been informed by consultations and engagement with people living with dementia, caregivers, researchers, health professionals and other care providers, and representatives of dementia-related advocacy groups from across Canada. The strategy also reflects advice resulting from the work of the Ministerial Advisory Board on Dementia, regular meetings with provincial and territorial officials, and the engagement of officials from federal organizations whose activities fall within the scope of the strategy.
The National Dementia Conference in May 2018 was a key step in developing the strategy. It brought together close to 200 participants, including people living with dementia and caregivers, to identify challenges, solutions, and opportunities related to dementia. Prior to the conference, 4 roundtables were organized by the Alzheimer Society of Canada and held across the country in March 2018, in Vancouver, Montreal, Saint John, and Fredericton. They brought together nearly 160 participants, including 15 people living with dementia, to discuss what living well with dementia looks like. Two additional roundtables on research and innovation were facilitated by the Weston Brain Institute and the Centre for Aging + Brain Health Innovation. These roundtables brought together researchers, people living with dementia, advocacy groups, health care professionals, and provincial and territorial representatives. They provided feedback on how innovation can best support living well with dementia and possible ways to break through existing barriers, and identified priorities for dementia research and innovation.
The Public Health Agency of Canada commissioned expert reports to inform the strategy, including an assessment by the Canadian Academy of Health Sciences of the state and strength of the evidence on dementia and a review of sex, gender, diversity and equity considerations related to dementia. Development of the strategy also considered the findings of several other reports and surveys related to dementia, including submissions received from organizations.
The Government of Canada recognizes that Indigenous communities and individuals have distinct dementia experiences and distinct needs. Engagement with Indigenous organizations, communities and governments will continue as the strategy is implemented to better understand these needs and facilitate Indigenous-led efforts to improve the quality of life for people living with dementia and caregivers in those communities.
The Government of Canada was challenged to be bold and ambitious with Canada's first national dementia strategy. We heard that the strategy should encompass both the importance of immediate efforts to improve the quality of life of people living with dementia and caregivers, as well as longer-term efforts to prevent dementia, advance therapies and find a cure. As the strategy moves into implementation, the Government of Canada will continue collaborating with all those committed to making progress on the vision and national objectives. This dialogue will ensure the strategy evolves as new priorities emerge.
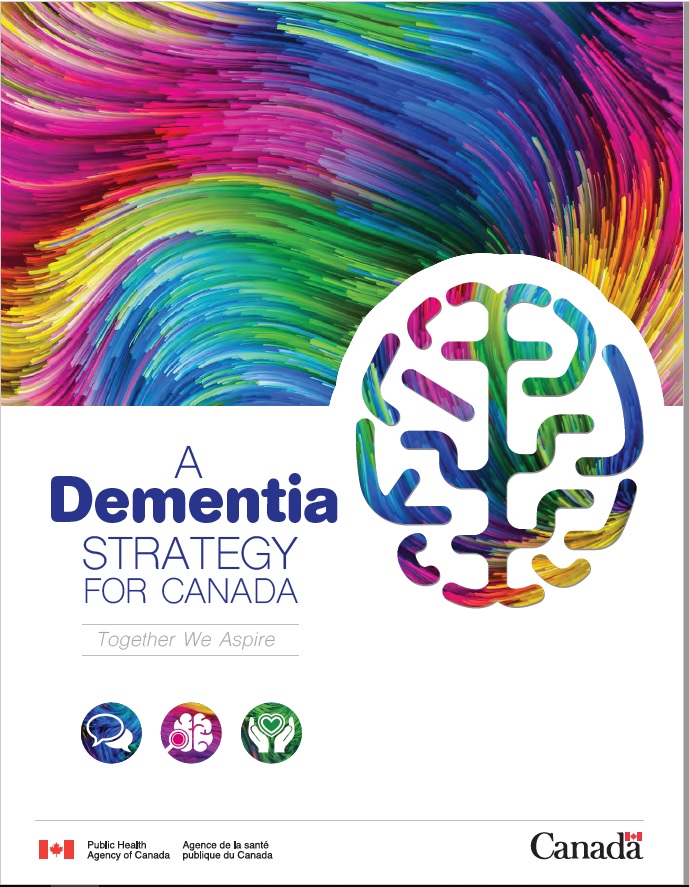
Figure 1: Canada's dementia strategy
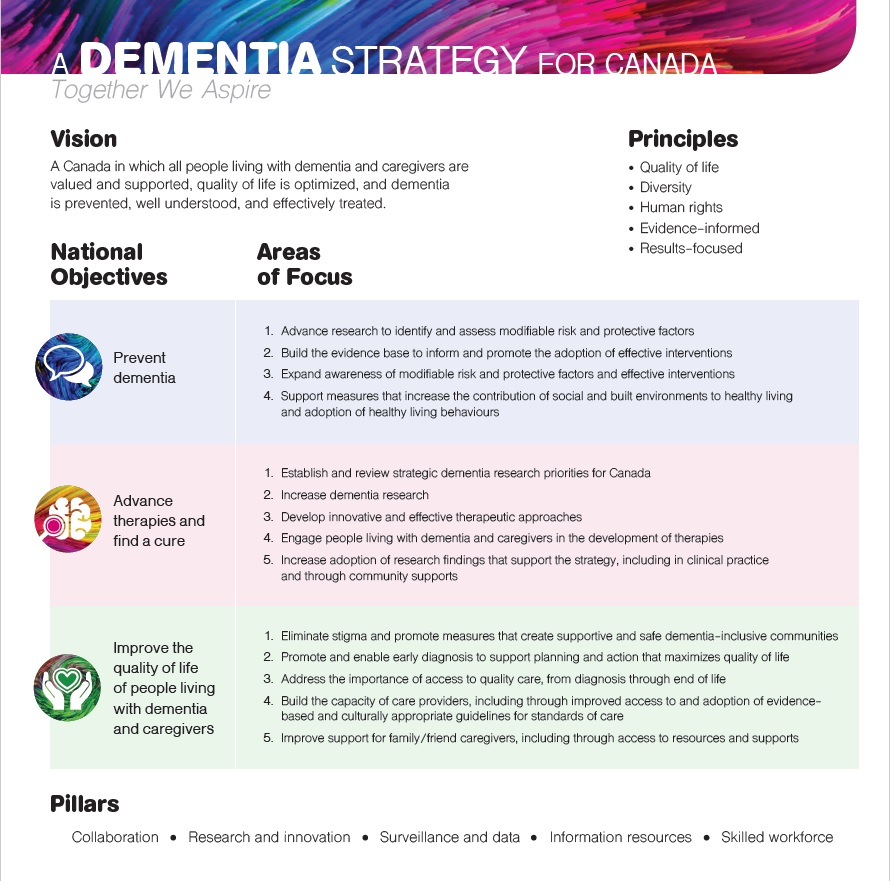
Figure 1 - Text description
Canada's dementia strategy
This image is a visual depiction of the core elements of the strategy.
The title of the strategy appears at the top "A dementia strategy for Canada: Together We Aspire".
Below this the Vision is stated which is "A Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated".
Next to the vision the principles are displayed in a bulleted list: Quality of life, Diversity, Human rights, Evidence-informed, and Results-focused.
Below the principles are a table with a row for each of the National Objectives and their corresponding Areas of Focus.
In the second row is the objective of "Advance therapies and find a cure".
- Advance research to identify and assess modifiable risk and protective factors,
- Build the evidence base to inform and promote the adoption of effective interventions,
- Expand awareness of modifiable risk and protective factors and effective interventions,
- Support measures that increase the contribution of social and built environments to healthy living and adoption of healthy living behaviours.
In the second row is the objective of "Advance therapies and find a cure".
The corresponding Areas of Focus are:
- Establish and review strategic dementia research priorities for Canada,
- Increase dementia research,
- Develop innovative and effective therapeutic approaches,
- Engage people living with dementia and dementia caregivers in the development of therapies,
- Increase adoption of research findings that support the strategy, including in clinical practice and through community supports.
In the third row is the objective of "Improve the quality of life of people living with dementia and caregivers". The corresponding Areas of Focus are:
- Eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities,
- Promote and enable early diagnosis to support planning and action that maximizes quality of life,
- Address the importance of access to quality care, from diagnosis through end of life,
- Build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care,
- Improve support for family/friend caregivers, including through access to resources and supports.
At the bottom of the image (underneath the National Objectives/Areas of Focus table), the Pillars of the strategy are listed in one line separated by dots. The pillars are:
- Collaboration
- Research
- Innovation
- Surveillance and data
- Information resources
- Skilled workforce
Vision: Setting a clear path forward
The vision we hope to achieve is a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood and effectively treated.
Achieving the best quality of life for people living with dementia and caregivers is at the centre of the strategy. The vision prioritizes the need to support and value people living with dementia to make it easier to live well for as long as possible, to deepen the understanding of dementia, and to raise awareness of dementia and of stigmatizing behaviours. It also recognizes the importance of improving therapies and investing in efforts towards prevention and a cure, including through research.
Principles
Five principles set out values to direct and guide action on dementia in Canada. These principles are intended to inform all elements of the strategy, including when evaluating options for policies and programs with a direct impact on dementia-related issues. This strategy calls on all governments in Canada and other stakeholders to consider and support these principles through their own work on dementia.
Prioritizing quality of life: Actions taken to implement the strategy prioritize the wellbeing of people living with dementia and caregivers.
- Living well for as long as possible: It is widely recognized and accepted that greater understanding and better access to supports Footnote 14 and tools will enable living well with dementia.
- Access to quality care and supports: The availability and quality of care and supports helps people live as well as possible each day and make choices that are important to them.
- Supportive communities: Community leaders and the general public are knowledgeable and committed to initiatives that make their communities more dementia-inclusive, including by raising awareness and making it easier for people living with dementia to participate.
Respect and value diversity: Actions and initiatives undertaken by all partners maintain an inclusive approach, with special consideration given to those most at risk or with distinct needs in support of greater health equity.
- Inclusive: All forms of diversity are considered in developing and implementing initiatives.
- Most at risk: Initiatives are tailored as needed and when appropriate to reach those most at risk in order to support health equity.
- Distinct Indigenous needs: The distinct needs of Indigenous communities and individuals are identified by Indigenous peoples and recognized by others. Indigenous communities and organizations are supported in addressing dementia in culturally appropriate and culturally safe ways, including through a distinctions-based approach that recognizes differences among First Nations, Inuit and Métis cultures.
- Community involvement: Community input is gathered to support community-based and community-led initiatives, and local capacity building is leveraged to reflect the diversity within Canada.
Respect human rights: Actions taken under the strategy respect the human rights of those living with dementia and reflect and reinforce Canada's domestic and international commitments to human rights.
- Human rights lens: A person-centred approach that focuses on respecting and preserving an individual's rights, autonomy and dignity in alignment with Canada's human rights commitments.
- Inclusion: Steps are taken to enable the participation of people living with dementia.
- Respects choice: The rights of individuals living with dementia to make their own decisions are broadly understood and facilitated.
- Hears the voices of those living with dementia: Actively including and consulting those living with dementia on matters that affect their quality of life.
- Caregiver perspectives: Consideration is given to the needs of the family and friends who care for people living with dementia.
Evidence-informed: Partners implementing the strategy engage in evidence-informed decision making, taking a broad approach to gathering and sharing the best available knowledge and data.
- Best evidence: Identification, creation and access to the best available research findings, data and knowledge.
- All forms of knowledge: A broad approach is taken when gathering evidence, including scientific data, traditional knowledge and the experiences of those living with dementia and of those caring for people living with dementia.
- Working together: Collaboration is used to build evidence and knowledge, including sharing research results.
- Informed decision-making: Policies and programs are informed by a thorough and rigorous examination of the evidence.
Results-focused: Partners maintain a results-focused approach to implementing the strategy and tracking progress, including evaluating and adjusting actions as needed.
- Initiatives that support reporting: Implementation activities are clearly linked to the areas of focus and national objectives, and are designed to support reporting on results.
- Enabling evaluation: Data and evidence are gathered to support evaluation and inform future efforts, both on activities undertaken and their impacts.
- Measurement: Indicators are identified and developed to support tracking of progress.
- Accountability: Annual reports to Parliament demonstrate accountability by sharing the results gathered from monitoring and evaluation.
- Flexibility to evolve: A flexible approach enables priorities to evolve as needed through continued dialogue, ongoing collaboration, and consideration of new evidence and information.
National objectives
Each of the 3 national objectives provides a broad scope for initiatives and activities. Under each national objective, areas of focus are identified where greater efforts are required to make progress on dementia in Canada. The 3 national objectives are:
- Prevent dementia
- Advance therapies and find a cure
- Improve the quality of life of people living with dementia and caregivers
Pillars
Five cross-cutting pillars are essential for implementation of the strategy.
Collaboration
The implementation of the strategy depends on continuing to build on key partnerships and collaboration on dementia, including with people living with dementia, caregivers, and communities. All governments in Canada and many stakeholders, including care providers, community and social service organizations, researchers and advocacy groups have a role to play in contributing to achievement of the strategy's national objectives.
Research and innovation
High quality, collaborative research and innovation are essential to the implementation of the strategy. While Canada is making significant investments in dementia research and advancing our understanding of dementia, there is still much to be learned and tested about prevention, new and better approaches to therapies, and supporting the quality of life of those living with dementia and caregivers. To continue and build Canada's contribution to dementia research, it is important to recruit young researchers.
Canada remains committed to its national and international collaborations and to supporting research towards a cure. It will continue to evaluate research findings and promote adoption of the most effective approaches as best practices across the country. Putting research findings into practice requires awareness and understanding, along with acceptance and sharing. Effort is required to reduce barriers for the adoption of research findings.
Surveillance and data
Optimizing dementia surveillance will provide a more accurate picture of the impact of dementia in Canada. This will give us insight into groups within the general population that are more affected and more at risk, and will support better identification of their health needs and those of caregivers. High quality surveillance data helps ensure that activities taken to support the strategy are well-informed and appropriately targeted. It also enables evaluation of progress resulting from activities undertaken in support of the strategy.
Information resources
Valuable information resources about dementia are available both in Canada and around the world. Efforts to improve public access to information about dementia, best practices in care and prevention, and social supports along with other key resources will broaden awareness and understanding of dementia and support greater health equity. Innovative ways to improve access to information will be explored, along with options for providing information resources in multiple languages and making them culturally appropriate.
Skilled workforce
Canada's dementia workforce is diverse. It includes researchers who are exploring the development of therapies and seeking a cure, as well as health professionals and other care providers who interact with people living with dementia and caregivers. Having a sufficient workforce that is well-equipped to pursue dementia research and provide quality dementia care is essential.
As our population grows and ages and the expected number of people living with dementia increases, Canada is likely to need more care providers. Post-secondary institutions will need to provide programs that include more dementia training for care providers and practitioners across the care pathway, to ensure the workforce is informed about dementia from diagnosis through to end of life. It is critical that these care providers have the necessary knowledge and skills to provide quality care.
Chapter 2: National objective: Prevent dementia
Developing a better understanding of how dementia can be prevented and sharing information about how Canadians can reduce their risk of developing dementia or delay its onset is critical to keeping Canadians healthy and improving quality of life.
There are individual health behaviours and other factors that can reduce or increase our chances of developing dementia (see Text box 3). For example, protective factors include healthy eating and physical activity, while smoking and hypertension may put Canadians at higher risk of developing dementia.
Text box 3: Risk factors for dementia
While there is currently no clear consensus, some evidence suggests that about one third of dementia cases could be prevented by addressing 9 risk factors:
- lower levels of early life education (up to 12 years of age)
- midlife hypertension (45-65 years of age)
- obesity
- hearing loss
- smoking in later life (over age 65)
- depression
- physical inactivity
- diabetes
- social isolation*
While certain factors may be more closely associated with specific stages of life, such as early life education, midlife hypertension and smoking in later life, reducing individual risk may be beneficial at any age when it comes to prevention. For people living with dementia, taking action focused on these factors could improve quality of life and reduce the risk of developing other chronic diseases, such as type 2 diabetes.Footnote 15
The environments we live in, including both social and built environments, can significantly influence our overall health and wellbeing. Dementia prevention efforts include sharing knowledge about the links between the design of our environments and dementia risk factors. The social environment is the space in which we engage in social activity within our communities, including recreation and education. Footnote 16 The built environment refers to the physical environment around us, including buildings, roads, green spaces and public transit — the places where we live, learn, work and play. Footnote 17 The natural environment, from plants and animals to water and air, also plays an important role in our lives, particularly for those who live in rural and remote communities across Canada. In these communities, geography may amplify both positive and negative impacts of the social and built environment on healthy living.
To support progress on preventing dementia, the strategy encourages researchers to continue working to better understand the factors already associated with developing dementia and assess additional factors that may be linked, such as traumatic brain injury, gum disease and inadequate sleep. Footnote 18 By furthering our knowledge of how these risk factors are linked to dementia, we can move beyond a list of risk factors to more effectively manage those risks and reduce their impact. This work will build a solid foundation for developing ways to prevent dementia.
Studies also suggest that delaying the onset of dementia could significantly reduce the total number of dementia cases in subsequent years. It is estimated that delaying onset by a few years could reduce the number of individuals with dementia by up to one third a few decades later. Footnote 19, Footnote 20 For those at increased risk of developing dementia, delaying its onset may also improve quality of life and reduce the personal, family and societal costs of care. Footnote 21 Some developed countries have already begun to report reduced incidence rates of dementia that appear linked to healthy living and higher education levels. Footnote 22 Canadian data suggests a possible decline in incidence rates of diagnosed dementia, Footnote 23 consistent with trends observed in other developed countries including the United States and the United Kingdom.Footnote 24
Four areas of focus will support preventing dementia:
- 2.1 Advance research to identify and assess modifiable risk and protective factors
- 2.2 Build the evidence base to inform and promote the adoption of effective interventions
- 2.3 Expand awareness of modifiable risk and protective factors and effective interventions
- 2.4 Support measures that increase the contribution of social and built environments to healthy living and adoption of healthy living behaviours
Area of focus 2.1: Advance research to identify and assess modifiable risk and protective factors
Advancing work to better understand which factors are linked to the increased risk of developing dementia, how important a factor is in comparison to other factors, and how these factors influence each other will build a foundation for preventing dementia. Although age is the strongest known risk factor for the onset of dementia, dementia is not an inevitable consequence of aging.
Research has shown a relationship between cognitive impairment (problems with memory, learning, thinking and judgement greater than normal age-related changes) and lifestyle risk factors common to several chronic conditions. Unhealthy lifestyle behaviours linked with conditions such as type 2 diabetes, cardiovascular disease and hypertension also appear to be associated with a higher risk of developing dementia. As a result, lifestyle changes focused on healthy living behaviours, like healthy eating and regular physical activity (protective factors) may reduce the number of dementia cases in the future. As well, an increase in unhealthy behaviours such as smoking and harmful alcohol use Footnote 25 (risk factors) could be expected to increase the risk of dementia.Footnote 26
Evidence also suggests that building the brain's ability to resist, offset and cope with damage or decline may contribute to prevention or delay the onset of dementia. Higher levels of education are associated with lower rates of dementia in later life, possibly due to greater flexibility and ability for the brain to adapt or overcome challenges (known as cognitive reserve).Footnote 27
Activities to advance research to identify and assess modifiable risk and protective factors may include:
- Promoting research that deepens evidence related to a more accurate assessment of risk and protective factors already linked to dementia
- Encouraging research on and identification of additional potential risk and protective factors to move toward a more comprehensive understanding of dementia
| Current status | Aspiration |
|---|---|
| Incomplete understanding of risk and protective factors linked with dementia, with some factors not yet identified and insufficient evidence on the link between factors and dementia. | A complete understanding of the risk and protective factors linked to dementia, their impacts and interactions. |
Area of focus 2.2: Build the evidence base to inform and promote the adoption of effective interventions
Given emerging evidence about factors that affect the risk of developing dementia, building the evidence base about effective interventions is an essential step in increasing the success of prevention efforts. Recent research has shown that interventions that promote healthy living can reduce the risk of developing dementia. Footnote 28 Healthy living includes embracing actions that maintain health such as physical activity and healthy eating, and avoiding behaviours that may harm health such as smoking.
Building on the work that is already underway, more research is needed to gather evidence on and increase understanding of interventions focused on these factors to determine which are effective in preventing dementia, and in what dose and what combination. Some evidence from prevention research is encouraging, but further research on larger and more diverse populations over longer timeframes is required. Footnote 29 Work is also needed to design interventions that are culturally safe and culturally appropriate to increase the adoption of healthy behaviours. Interventions need to be adapted in ways that best address the unique needs of individuals, particularly within higher-risk populations and for those facing barriers to care.
Interventions that address a number of factors at the same time, rather than those with a sole focus, could potentially be a more effective way to reduce the risk of developing dementia and to prevent chronic diseases. An example of encouraging research on prevention is the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Footnote 30 It examined the effectiveness of changing lifestyle factors such as nutrition, physical activity, cognitive training, social activities and monitoring vascular risk for those at risk of developing dementia. Interaction of these types of lifestyle factors is showing promising results of reduced risk of cognitive decline. This study has since expanded to the United States, China, Singapore and Australia.
Activities to build the evidence base to inform and promote the adoption of effective interventions may include:
- Investing in research to study and test interventions that prevent dementia
- Scaling-up and/or integrating promising interventions that enable and change behaviour focusing on modifiable risk and protective factors for dementia
- Sharing Canadian research results on prevention-focused interventions
- Including assessment of brain health and function in healthy living intervention research
| Current status | Aspiration |
|---|---|
| Limited evidence about effective interventions to reduce risk for dementia and insufficient information resources. | Availability of effective prevention resources and interventions, supported by a strong evidence base. |
Area of focus 2.3: Expand awareness of modifiable risk and protective factors and effective interventions
As our understanding of factors that affect the risk of developing dementia grows and we learn more about interventions that are most effective in reducing risk, creating effective ways of sharing this knowledge broadly in a way that Canadians can understand will be important. By increasing awareness among both care providers and the general population, Canadians will be empowered to take action to protect their own health and reduce their risk of developing dementia. To be effective in our diverse country, awareness activities will need to be multi-lingual and culturally appropriate.
The development of dementia can begin as early as 20 years before symptoms can be observed to permit diagnosis. Footnote 31 As a result, a focus on health promotion that expands awareness and promotes lifestyle changes that can delay or reduce risk of dementia should start as early as possible.
In Canada and internationally, the development, implementation and adoption of healthy living interventions is ongoing. Researchers and health professionals are encouraged to seek opportunities to build on and integrate dementia into existing efforts.
Activities to expand awareness of modifiable risk and protective factors and effective interventions may include:
- Putting in place educational awareness activities and campaigns for preventing dementia among people of all ages in Canada with a focus on those most at risk
- Raising awareness among Canadians about brain health promotion and dementia prevention through messaging targeted at other chronic conditions with similar risk and protective factors
- Encouraging care providers to integrate brain health and dementia prevention information with information about other chronic conditions with similar risk and protective factors
| Current status | Aspiration |
|---|---|
| A lack of awareness among the general public and care providers about actions that may help prevent dementia. | All people living in Canada are aware of actions that prevent dementia. |
Area of focus 2.4: Support measures that increase the contribution of social and built environments to healthy living and adoption of healthy living behaviours
While it is important for people to be aware of risk and protective factors, this knowledge alone cannot prevent or delay the onset of dementia. People must also be supported by their environments — the people, places and social contexts that impact their daily lives. These environments, if appropriately designed, can make it easier to adopt healthy living behaviours, which may reduce the risk of developing dementia.
Social environments can have a significant impact on health, particularly mental health and wellbeing, as well as stress levels. A strong and stable social network and a built environment that supports active living can reduce the risk of social isolation that is often associated with aging, and is a risk factor for dementia.
While it can be difficult to identify the extent to which neighbourhood features influence healthy living, we know that the communities we live in can often be better designed to support our health. Footnote 32 For example, neighbourhood features such as walkable destinations, green spaces and gathering places have been linked to a greater sense of community and positive social interaction. Footnote 33 Neighbourhoods with complete streets (streets designed to be safe for people of all ages and abilities, regardless of their mode of transportation) can better support physical activity, while greater availability of healthy food (such as through community gardens) helps people make healthier food choices. Poor health, including obesity, is more common in areas where it is more difficult to access healthy food and where there are many unhealthy food options.Footnote 34
The built environment (which includes buildings, roads, green spaces, and public transit) varies across urban, rural and remote communities. Challenges in accessing transportation may greatly impact the ability to maintain healthy living behaviours, including access to healthy foods and maintaining social networks. For example, in rural and remote communities, public transportation may not be available or accessible. As a result, interventions and solutions may need to be different than those used in urban areas. Other factors in the built environment may contribute to the risk of developing dementia, such as those that also make it more challenging to be physically active and exposure to environmental risks including air pollution.Footnote 35
The World Health Organization's age-friendly communities model, adopted in Canada by over 1200 communities, is an example of an approach that seeks to support healthy and active aging. This approach helps older adults to live safely, enjoy good health and remain involved in their communitiesFootnote 36 (see Text box 4).
Text box 4: Age-friendly communities
There are 8 areas in which communities can take action to become more age-friendly:
- housing
- transportation
- outdoor spaces and buildings
- social participation
- respect and social inclusion
- civic participation and employment
- communication and information
- community support and health services*
Activities to support measures that increase the contribution of social and built environments to healthy living and the adoption of healthy living behaviours may include:
- Raising awareness of the impacts of social and built environments on the risk of developing dementia to foster greater support for initiatives to create healthy environments
- Encouraging programs and initiatives that support healthy social and built environments, including those that contribute to healthy aging and support older adults to age in place
- Delivering community-based programs that increase the adoption of healthy living behaviours related to modifiable risk and protective factors for dementia that are also linked to our environments, including targeted activities for higher-risk populations
- Evaluating best practices to make age-friendly communities more dementia-inclusive
| Current status | Aspiration |
|---|---|
| Barriers related to built and social environments limit the ability of individuals to pursue healthy living in ways that may reduce the risk of developing dementia. | All people living in Canada have access to built and social environments that support their ability to pursue healthy living in ways that may reduce their risk of developing dementia. |
Chapter 3: National objective: Advance therapies and find a cure
In 2013, Canada committed to support efforts to increase research funding for dementia with the aim of finding a disease-modifying treatment or cure by 2025 as a member of the Group of Eight nations (G8). Footnote 37 Canada is also committed to supporting the World Health Organization's Global action plan on the public health response to dementia (2017–2025), Footnote 38 which identifies "dementia research and innovation" as 1 of 7 priority areas of action.
While improving our understanding of dementia and finding possible ways to prevent or cure this condition requires a collective international effort, Canada boasts a strong brain health and dementia research community and is home to many internationally recognized researchers. As awareness of dementia has grown over the years, so has funding for dementia research by governments and other organizations in Canada. However, much more work remains to enhance our fundamental understanding of dementia and its root causes, and to use that knowledge to develop therapies and find a cure. Producing new knowledge and evaluating novel approaches for how best to treat dementia to support those with dementia to live well and advancing efforts towards finding a cure is one of the strategy's 3 national objectives.
Five areas of focus will support advancing therapies and finding a cure:
- 3.1 Establish and review strategic dementia research priorities for Canada
- 3.2 Increase dementia research
- 3.3 Develop innovative and effective therapeutic approaches
- 3.4 Engage people living with dementia and caregivers in the development of therapies
- 3.5 Increase adoption of research findings that support the strategy, including in clinical practice and through community supports
Area of focus 3.1: Establish and review strategic dementia research priorities for Canada
The strategy will encourage efforts to support an inclusive approach to the selection of dementia research priorities, one that is informed by engagement with key stakeholders including people living with dementia and caregivers.
Priority setting also allows us to build on Canadian strengths, support international commitments, and advance Canadian priorities including the strategy's 3 national objectives of preventing dementia, advancing therapies and finding a cure, and improving the quality of life of people living with dementia and caregivers. In addition, regular review of research priorities related to therapies and finding a cure will ensure these priorities remain relevant in addressing gaps in knowledge and are responsive to new research findings.
Priority setting for dementia research is best accomplished with input from diverse stakeholders and populations (e.g. researchers, academics, care providers, industry, organizations, cultural minorities, First Nations, Métis and Inuit) and, most importantly, people living with dementia and caregivers. A broad approach ensures research includes a focus on issues that affect those living with dementia and those who provide care.
Building on the work done through the Canadian Institutes for Health Research (CIHR) Dementia Research Strategy, the CIHR and partner funded Canadian Consortium on Neurodegeneration in Aging (CCNA) funding will continue to address dementia research across the 3 themes of primary prevention, secondary prevention, and quality of life (see Text box 5), which are well aligned with the 3 national objectives of the national dementia strategy. Additionally, CIHR will continue to work with international partners to identify and address research priorities.
Text box 5: Research themes of the Canadian Consortium on Neurodegeneration in Aging (Phase II)
Primary prevention: To examine the basic mechanisms to prevent cognitive impairment and dementia.
Treatment and secondary prevention: To improve early detection (diagnostics) and treatment of dementia.
Quality of life: improving the management of dementia and the quality of life for those living with dementia and caregivers.
Another example of a stakeholder-engaged priority setting approach comes from a collaborative effort among the Alzheimer Society of Canada, the Toronto Rehabilitation Institute, and the CCNA. The Canadian Dementia Priority Setting PartnershipFootnote 39 initiative was undertaken to better understand research priorities of those living with dementia, caregivers, families, health and social care providers and the general public. The Partnership questions focused on living with dementia, dementia prevention, treatment and diagnosis. Questions on cure and the biological mechanisms of dementia were not included in this prioritization exercise. The outcome of this priority setting process differs from those dementia research priorities outlined by the World Health Organization in 2016, which was informed by researchers, clinicians, and health and care workers (see Table 1). For example, stigma, and early treatment were prioritized by the Partnership while the WHO priorities included a strong focus on prevention, diagnosis and therapies. These differences demonstrate the importance of dialogue with multiple stakeholders when setting and reviewing research priorities.
International research priorities for dementia identified by the WHO in 2016 fell into 59 thematic research areas which were organized into the top 7 thematic research domainsFootnote 40 (see Text box 6). Research priorities were identified for each thematic research domain.
Text box 6: 2016 World Health Organization dementia thematic research domains:
- Prevention, identification and risk reduction
- Quality of care for people with dementia and their caregivers
- Delivery of care for people with dementia and their caregivers
- Diagnosis, biomarker development, and disease monitoring
- Drug and non-drug clinical-translational research
- Public awareness and understanding
- Physiology and progression of normal ageing and disease development*
* Research Priorities to Reduce the Global Burden of Dementia by 2025
| 2017 The Canadian Dementia Priority Setting Partnership Initiative - Research priorities | 2016 World Health Organization's dementia research priorities |
|---|---|
| (Participants were Canadians affected by dementia including people with dementia, care partners, family, friends and health and social care providers) | (Participants were researchers, clinicians and health and care workers) |
| 1. Addressing stigma | 1. Prevention and risk reduction; relationship with chronic diseases |
| 2. Emotional wellbeing | 2. Identify clinical practices and interventions to promote timely and accurate diagnosis |
| 3. Impact of early treatment | 3. Diversify therapeutic approaches (drug and non-drug) |
| 4. Health system capacity | 4. Brain health promotion and dementia prevention communication strategies |
| 5. Caregiver support | 5. Understand contributions of vascular conditions |
| 6. Access to information and services post-diagnosis | 6. Influence and interactions of non-modifiable and modifiable risk and protective factors |
| 7. Care provider education | 7. Interventions to address risk factors |
| 8. Dementia-friendly communities | 8. Models of care and support in the community |
| 9. Implementing best practices for care | 9. Educating, training and supporting formal and informal carers |
| 10. Non-drug approaches to managing symptoms | 10. Later-life and end-of-life care, including advance care planning |
Activities to support efforts to establish and review strategic dementia research priorities for Canada may include:
- Enabling consideration of diverse perspectives when setting and reviewing strategic dementia research priorities in Canada
- Exploring ways to bring together those working in different disciplines of dementia research to leverage and align efforts
- Supporting dementia research priority setting summits that are open to a broad range of stakeholders
| Current status | Aspiration |
|---|---|
| Limited broad stakeholder input when setting research priorities and insufficient engagement of people living with dementia and caregivers. | Research priorities established in an inclusive manner with broad stakeholder input, with the participation of those living with dementia and caregivers. |
Area of focus 3.2: Increase dementia research
There is a wealth of dementia-related research supported through different funding mechanisms and a variety of national and international organizations. This research addresses many aspects of dementia, including but not limited to: biomedical, clinical, health systems and population health research. Investing in research that explores these elements is critical for the advancement of our understanding of dementia and our ability to treat and manage it as a society. However, there is much more to be explored and learned to find more effective approaches to treat dementia.
Biomedical research aims to understand at the cellular level what changes are occurring in the brain and why. For example, there has been a focus over the last thirty years on two proteins in the brain that are linked to dementia: beta-amyloid and tauFootnote 42. These two proteins reach abnormally high levels in the brain of someone with dementia. Clinical research examines the safety and effectiveness of medications, devices, tools for diagnosis, and therapies. Other types of research include health systems research which examines how people access health services, health professionals, care costs and outcomes. Population health research aims to examine the health of an entire population, understanding how social, cultural, environmental, occupational and economic factors can influence health status.
Moving forward, there is an opportunity to harness Canada's broad and rich foundation of research through strategic partnerships and initiatives to focus efforts on advancing therapies that can prevent, slow or stop the changes underway in the brain that are associated with dementia, as well as working towards the ultimate goal of finding a cure. Using a variety of approaches to fund dementia research may enable us to leverage research investments for greater impact. For example, public-private partnerships allow government and the private sector to work towards common goals while sharing risk and expertise. There may be potential to match funding to increase impact; an example is the partnership between Health Canada and Brain Canada for the Canada Brain Research Fund where non-governmental funding is matched by the Government of Canada.
Strategic and targeted research investments for chronic diseases, such as cancer, heart disease and stroke have had a significant positive impact in Canada. For example, cancer prevention and control efforts and the importance of maintaining heart health by addressing risk factors have resulted in advancements in prevention, diagnosis and treatments for these diseases. Focusing on strategic and targeted investments may result in similar impacts for dementia in Canada.
The federal government, through the CIHR, applies a dual approach in supporting research on dementia. CIHR investments in dementia research totalled close to $200 million between 2013–14 and 2017–18. This investment is both fundamental and strategic in nature, and includes both domestic and international components of the CIHR Dementia Research Strategy. Additionally, the Government of Canada funds dementia-relevant research and innovation networks — AGE-WELL, the Centre for Aging + Brain Health Innovation (CABHI), and the Canadian Frailty Network. Canada's research efforts are spread across provinces, territories and many organizations, and are often collaborative (see examples in Text box 7).
Text box 7: Highlights of non-federal dementia research investments in Canada
The following are examples of investments in dementia research from provincial governments, academia, health charities and other organizations.
Over the past 6 years, Alberta Innovates, the largest research and innovation agency in Alberta, has invested over $2.9 million in Alzheimer's research. Alberta Innovates co-funds the Alberta Alzheimer Research Program through the Alberta Prion Research Institute which helps researchers better understand the fundamental mechanisms of the disease and improve the quality of life of those living with dementia.
Since 1989, the Alzheimer Society of Canada's Alzheimer Research Program has funded $53 million in grants and awards in biomedical and quality of life research.
Through the Fonds de recherche du Québec - Santé, the Government of Quebec funds research on the causes, prevention, screening, diagnosis and treatment of age-related conditions, including dementia.
Ontario Brain Institute is a research centre that maximizes the impact of neuroscience through translational research (applied research) aimed at developing therapeutics for the prevention and/or treatment of human disease. For example, through the ONtrepreneurs program, the company RetiSpec was awarded $50K to develop a non-invasive eye scanner for early detection of Alzheimer's disease, which will dramatically reduce diagnostic costs and advance the detection of Alzheimer's disease.
The Pacific Alzheimer Research Foundation focuses exclusively on funding scientific research and investigation into the cause, prevention and treatment of dementia. The Foundation received a $15 million grant from the British Columbia government in 2006 and this endowment has been supplemented by private donations.
Research Manitoba and the Centre for Aging + Brain Health Innovation launched a funding opportunity through the Accelerating Innovations for Aging and Brain Health program (2018-2019) focused on priority innovation themes. In particular, the Aging in Place theme is advancing solutions that enable older adults with dementia to maximize their independence and quality of life.
In 2017, the Weston Brain Institute announced $30 million in grants for researchers to fight neurodegenerative diseases including dementia. This is in addition to the $100M announced in 2016 by the Weston Brain Institute for high-risk, high-reward translational research projects with the potential to help speed up the development of treatments.
Activities to increase dementia research may include:
- Continuing to leverage existing federal investments and working with potential funding organizations to increase overall Canadian investment in dementia research
- Pursuing international opportunities to expand investments including through new funding models
| Current status | Aspiration |
|---|---|
| Annual investment in dementia research in Canada is less than 1% of dementia care costs. | Annual investment in dementia research in Canada exceeds 1% of dementia care costs. |
Area of focus 3.3: Develop innovative and effective therapeutic approaches
The development of innovative approaches to therapies across all stages of dementia, from before symptoms appear to early and advanced symptoms, will be encouraged. Therapies can include any intervention that rehabilitates, provides positive social adjustment and improves quality of life.
Types of innovation could include new technologies, along with social and biomedical innovations such as assistive technologies, individualized cognitive training, drug and non-drug therapies. Assistive technologies can include devices or systems that support a person with dementia to maintain or improve their independence, safety and overall wellbeing. Examples include clocks to assist with telling time, including whether it is day or night, communication aids, electric appliance monitors, picture phones, reminder devices, as well as in-home cameras and home monitoring devices that help caregivers and care providers properly and safely care for people living with dementia. Cognitive training has been shown to improve skills and quality of life for people with dementia through activities such as categorization, word association and discussions of current affairs, which can improve mood and concentration. Further scientific testing of these and other promising therapeutic approaches is needed before wide-scale adoption by the medical community.
There is currently no cure for dementia; however, some drug therapies have been proven to have modest benefits on cognitive abilities such as improving memory and thinking. Current guidance suggests that drug therapies should not be the first choice for managing behavioural and psychological symptoms associated with dementia because their effectiveness is modest and there is a risk of harm associated with use. Footnote 43, Footnote 44 In addition, better understanding is required with some drug therapies due to the increased complexity of care when an individual is receiving treatment for dementia along with medications for other chronic conditions, particularly if the person is of an advanced age. Limited progress on drug therapies highlights the need to support innovative and effective non-drug therapies. These non-drug options can include music therapy, aromatherapy, pet therapy and massage therapy. While still requiring scientific validation, Footnote 45, Footnote 46 these therapies have shown promising benefits for people with dementia.
Activities to develop innovative and effective therapeutic approaches may include:
- Strategically focusing investments on developing innovative and effective therapeutic approaches
- Enhancing Canadian efforts at the international level to promote innovation in dementia research
- Ensuring that the federal regulatory framework for approval of new drugs is flexible and responds to the need for timely access to novel and innovative therapies
- Fostering interdisciplinary approaches to innovation that bring together stakeholders and researchers to develop and identify effective and timely therapies
- Encouraging opportunities for hospitals and associated academic institutions to adopt innovative approaches to therapies — many of these institutions are teaching hospitals where health professionals in training can test and apply new approaches
- Exploring the feasibility of expanding the use of a tailored person-centred care model rather than a focus on the condition
| Current status | Aspiration |
|---|---|
| Options for evidence-informed therapies remain limited and often are not person-centred. | New evidence-informed person-centred therapies are more readily available. |
Area of focus 3.4: Engage people living with dementia and caregivers in the development of therapies
For research on dementia therapies to be effective and culturally appropriate, people living with dementia as well as their families and caregivers must be meaningfully involved as active participants and partners. Their voluntary participation is a vital contribution to our understanding of which therapies are effective, as well as a core tenet of ethical research practice.
For example, Canada's Strategy for Patient-Oriented Research (SPOR), a CIHR-partnered initiative, funds research that fosters evidence-informed health care by bringing innovative diagnostic and therapeutic approaches to the point of care. SPOR's Patient Engagement Framework Footnote 47 is based on a vision where patients are active partners in health research which leads to improved health outcomes and an enhanced health care system. Through a collaborative and stakeholder-partnered approach, SPOR builds capacity in patient-oriented research and promotes patient engagement (see Text box 8). Such a model can be drawn upon to guide future patient-centric approaches in dementia.
Text box 8: Canadian Strategy for Patient-Oriented Research
“Patients bring the perspective as ‘experts' from their unique experience and knowledge gained through living with a condition or illness, as well as their experiences with treatments and the health care system.”*
By encouraging a diversity of patients to tell their stories, new themes may emerge to guide research. Patients gain many benefits through their involvement in research including increased confidence, new skills, greater access to useable information, and a feeling of accomplishment from contributing to research relevant to their needs.
* Strategy for Patient-Oriented Research: Patient Engagement Framework (PDF)
Activities to engage people living with dementia and caregivers in the development of therapies may include:
- Leveraging collaborative work already underway that engages people living with dementia
- Providing financial supports to caregivers so they can assist people living with dementia in participating in research activities
| Current status | Aspiration |
|---|---|
| People living with dementia and caregivers are predominantly the subject of research to develop new therapies and find a cure. | People living with dementia and caregivers are active participants and partners in research to develop new therapies and find a cure. |
Area of focus 3.5: Increase adoption of research findings that support the strategy, including in clinical practice and through community supports.
Research has shown that there is a gap between health research findings and their practical use in clinical settings. Footnote 48 Traditionally, researchers publish findings in academic journals and other researchers consider this new evidence. However, more can be done to turn research findings on therapies for people living with dementia more quickly into relevant information that can be adapted and adopted in clinical, community and family settings.
Barriers to putting research findings into practice may reduce the ability of health professionals to make informed decisions and prevent patients from benefitting from promising therapies. These barriers include a lack of mechanisms to assist researchers and practitioners in moving research findings toward adoption, uncertainty of researchers about their roles in facilitating adoption, and difficulty in gaining access to clinical settings to test new interventions.
"If the incidence of dementia is to be reduced and the lives of people with dementia are to be improved, research and innovation are crucial, as is their translation into daily practice."*
* WHO Global Action Plan on the Public Health Response to Dementia (2017-2025)
To enable broad adoption by all those who could benefit, research findings need to be turned into practical information in ways that are affordable. It is also important that research findings are communicated in ways that increase accessibility and are culturally appropriate across diverse communities such as Indigenous peoples, immigrant and minority language communities, LGBTQ2 individuals, people with intellectual disabilities, as well as those who live in rural and remote settings or in federal and provincial custody.
Activities to increase adoption of research findings that support the strategy, including in clinical practice and through community supports may include:
- Supporting projects that generate knowledge on how to effectively and quickly test research findings that can then be used in real-world settings
- Encouraging research design that includes an approach to share research results and encourage their adoption
- Developing mechanisms that support the sharing of best available research findings and potential innovations in ways that make them easier to adopt
| Current status | Aspiration |
|---|---|
| Research findings tend to stay within academic settings and journals and are not broadly known, accepted, or brought into clinical practice. | Research design always includes efforts that ensure findings can be understood, adopted and quickly put into practice. |
Chapter 4: National objective: Improve the quality of life of people living with dementia and caregivers
The quality of life of those living with dementia and caregivers is the motivation for the national dementia strategy. In 2015–16, over 419,000 (6.9%) Canadians aged 65 years and older were living with diagnosed dementia. Footnote 49 In 2012, approximately 8.1 million individuals, or 28% of Canadians aged 15 years and older, were family/friend caregivers for a person with a long-term health condition, disability or aging needs. Footnote 50 Of these caregivers, approximately 486,000 (or 6%) were caring for an individual with dementia. Footnote 51 With the aging population, the number of caregivers is expected to grow.
While recognizing the importance of funding for health care, social services and other types of resources, 5 areas of focus will support improving the quality of life of people living with dementia and caregivers.
- 4.1 Eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities
- 4.2 Promote and enable early diagnosis to support planning and action that maximizes quality of life
- 4.3 Address the importance of access to quality care, from diagnosis through end of life
- 4.4 Build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care
- 4.5 Improve support for family/friend caregivers, including through access to resources and supports
Area of focus 4.1: Eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities
Creating supportive, safe and inclusive communities across Canada for people living with dementia and caregivers is essential to maximizing their quality of life. In dementia-inclusive communities (see Text box 9), the participation and contribution of people living with dementia is encouraged, supported, and valued, and the care and support provided within the community is culturally safe, culturally appropriate, and mindful of diversity.
Everyone can contribute to a dementia-inclusive community, including health professionals, first responders, and those working in banks, retail stores, restaurants, public transit, rail transit and air transit.
These communities also consider the proper planning of space, to help people living with dementia to navigate and support social engagement. For example, multigenerational housing offers opportunities for connections to be formed across generations. Some multigenerational facilities are being developed in Canada that include assisted living units, which allow couples and their families to stay together longer and provide more opportunities for people living with dementia to engage in meaningful activities.
Where possible, dementia-inclusive community initiatives should complement and build upon work already underway, such as the development of age-friendly communities. The model for age-friendly communities set out by the World Health Organization to support healthy and active aging brings together all aspects of the physical and social environment, to help older adults live safely, enjoy good health and remain involved in their communities.
Text box 9: A dementia-inclusive community
"Allows people living with dementia and their caregivers to: optimize their health and wellbeing; live as independently as possible and remain part of their community; be understood and supported; safely navigate and access their local communities, including banks, shops, restaurants, entertainment and transportation; and maintain or expand their social networks"*. Examples of dementia-inclusive efforts can include:
- Training for those interacting with people living with dementia on how they can best provide service or assistance
- Public walkways that are clear, uncluttered and pattern-free
- Safe and engaging gathering spaces for people living with dementia and their caregivers
- Simplified transit schedules with clear language and easy-to-follow signage
* Dementia-inclusive communities (State Government of Victoria, Australia)
Dementia-inclusive communities help to reduce and eliminate barriers, including those resulting from stigma that can lead to social isolation. Stigmatizing language and behaviours related to dementia may include: making uninformed assumptions about a person's abilities; age-related stereotyping and discrimination; and dementia-related jokes. Language may include implying that dementia is a normal part of aging and referring to an individual as "demented", "senile" or "crazy". In dementia-inclusive communities, people living with dementia feel safe and supported to live well, interact comfortably with community members and participate in community activities.
Stigmatization and discrimination sometimes occur within the health system, including in primary care, hospitals and home and long-term care settings, where they can delay or create barriers to diagnosis, treatment and care, including end-of-life care. Footnote 52 Experiences reported during consultations to inform the strategy include: physicians not speaking directly to the person being diagnosed but instead to caregivers; health care practitioners withholding diagnosis based on the belief that nothing can be done and a desire to spare the person the stress and anxiety of receiving the diagnosis; and being less likely to be offered available services and supports, including palliative care. In addition, first responders (paramedics, police, etc.) may come into contact with people living with dementia and caregivers and these situations are often stressful for all involved. Compassionate and respectful interactions require an understanding of how to recognize, communicate with and respond to people living with dementia.
Activities to eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities may include:
- Delivering culturally appropriate awareness campaigns that are respectful of diversity and focus on stigma reduction
- Educating service providers, including retail, service and transportation industries, to increase age-friendliness and dementia-inclusive environments
- Building a better understanding of dementia-inclusive communities and evaluating their effectiveness
- Creating, collecting and sharing knowledge about dementia-inclusive communities that can be easily accessed by people living with dementia, caregivers, and the general public
- Learning more about how age-friendly communities can be leveraged to be dementia-inclusive
- Increasing access to community-based initiatives and/or programming that will help communities become more dementia-inclusive
| Current status | Aspiration |
|---|---|
| Widespread stigma within communities and a lack of understanding of dementia. | All people living in Canada understand dementia and stigma no longer exists in Canada. |
Area of focus 4.2: Promote and enable early diagnosis to support planning and action that maximizes quality of life
Timely communication of symptoms to health professionals together with greater confidence among primary care practitioners in diagnosing dementia early are key to maximizing the quality of life for people living with dementia. The many benefits of receiving an early diagnosis include:
- Individuals and their friends and family members can seek information sooner to better understand what to expect and how to prepare. This learning process can help to reduce stress levels and provide a sense of control and direction.
- Therapies, services and supports can be accessed earlier, which can help to reduce the severity of symptoms. For example, having access to proper visual or hearing aids has been associated with improved cognitive function in those diagnosed with dementia. Footnote 53, Footnote 54 Support groups can help individuals feel socially connected, give a sense of belonging and purpose, and provide a safe place to seek advice and encouragement.
- Increased time for individuals to develop advance care plans, and communicate their preferences for care to their families and care providers.
Activities to promote and enable early diagnosis to support planning and action that maximizes quality of life may include:
- Reviewing and addressing gaps in existing Canadian guidelines for diagnosing dementia Footnote 55 including barriers to uptake (see Text box 10)
- Working with provincial and territorial governments to support the efforts of health professionals in primary care to recognize, diagnose and communicate a dementia diagnosis in a compassionate manner that includes information on available supports and services
- Developing and/or updating evidence-informed and culturally appropriate diagnostic resources and tools for health professionals
- Collecting data on diagnosis rates, including when the diagnosis is made
| Current status | Aspiration |
|---|---|
| Individuals are unable to receive an early or timely diagnosis, or feel unsupported when receiving a diagnosis. | A timely diagnosis, provided in a compassionate manner, is available to all people living in Canada, along with immediate availability of resources and supports. |
Text box 10: Guidelines for diagnosing dementia in Canada
Canadian guidelines on the diagnosis and treatment of dementia recommend that the initial assessment for memory problems or dementia be performed in primary care. Primary care practitioners are optimally placed as an individual's first point of contact with the health care system to detect changes in thinking and behaviour.
Exception: The guidelines recommend that all individuals with young onset dementia (i.e., prior to age 65) should be referred to a memory clinic, ideally with access to genetic counseling and testing. Those with rapidly progressive dementia (i.e. dementia that develops within 12 months of the appearance of the first cognitive symptoms) also require a consultation with a specialist.
Area of focus 4.3: Address the importance of access to quality care, from diagnosis through end of life
Access to care that is holistic, culturally safe, culturally appropriate and respectful of diversity and dignity will help improve quality of life. Dementia care can range from therapies that manage or reduce the severity of symptoms, to services and/or programs including rehabilitation, to social, behavioural and psychological supports. The types of care needed and care settings can fluctuate as the condition progresses. Services may be delivered in a variety of health care settings, in the home and in the community (see Text box 11). Assistive technologies and community-based services can also help people living with dementia stay at home longer, reduce hospital visits, and delay entry to long-term care.
Information relating to dementia services and supports is not always easy to find, access or coordinate. People living with dementia and caregivers would benefit from easier access to care and supports available in their community.
Text box 11: Federal funding for care
In 2017, the Government of Canada provided provinces and territories with an additional $11 billion over 10 years specifically targeted to improve home and community care, including palliative care, and mental health and addiction services.
Care settings and care coordination
For many people, living well means living independently or in their homes and participating in their community for as long as possible. As dementia progresses, individuals can require more assistance with activities of daily living, which is often provided by a family member or friend.
Caregivers may require additional resources and training to provide optimal support. As caregiving needs become more complex, a paid care provider may be needed to provide additional assistance with home care or the person living with dementia may choose a supportive housing option where on-site personal care and support services are provided. When it is no longer possible to live independently, individuals living with dementia may need to transition to long-term care. Footnote 56 It is anticipated that access to higher levels of care will become even more challenging given that the number of older adults in the population is increasing and the availability of this care will possibly be reduced as a result. Footnote 57
People aged 65 years and older living with dementia are more likely to be hospitalized than those without dementia, which often results in feelings of distress due to the variety of treatments, tests and changes to their daily routines. The cause of hospitalization is often a fall-related injury. Footnote 58 Emergency department stays are often longer, and after the stay in acute care is completed, it is 3 times more likely that the individual will stay in an alternative level of care before being released. Footnote 59
Effective care coordination with a case manager who advocates for the patient is essential to ensure good communication among care settings and to avoid gaps in continuity of care, as well as costly and disruptive transitions that can lead to serious health consequences. Footnote 60
Decision making is an important part of care coordination. While people with dementia have the right to make decisions about their care, they may need to consider putting in place other decision-making approaches as the condition progresses. Many are familiar only with the substitute decision-making model which gives decision-making authority to someone else. Using a human rights lens allows for additional decision-making models to be considered such as the supportive decision-making model which allows people with dementia to make their own decisions about care with the support of people they know and trust. Should a substitute decision-maker be required, advance care planning allows individuals to identify someone to take on this role and plan future health care in line with their beliefs and values. This can reduce distress and ensure that the care received aligns with their wishes throughout all stages of the condition.
Palliative care
In Canada, people living with dementia are less likely to be referred to palliative care teams, are prescribed fewer palliative care medications, and have more difficulty accessing end-of-life care than those diagnosed with other life-limiting illnesses. This could be due to difficulties assessing needs as dementia progresses, limited access to palliative care programs, poor communication between care providers, and the mistaken view that palliative care is not relevant to dementia among some families, patients, and health professionals. Footnote 61 Palliative care (see Text box 12) can begin at the time of a dementia diagnosis and aims to reduce suffering and improve quality of life through pain and symptom management, psychological, social, emotional, spiritual and practical support, as well as support for caregivers throughout the trajectory of the condition, including after death. It focuses on comfort, respect, and dignity and complements other therapies intended to prolong life.
The lack of a palliative approach for people living with dementia can result in poor management of symptoms toward the end of life, especially pain, which has been linked to reduced quality of life, depression, increased agitation and other behavioural and psychological symptoms. Footnote 62,Footnote 63
Text box 12: A Framework For Palliative Care
In December 2018, the Government of Canada released a Framework on Palliative Care to help support improved access to palliative care by providing a useful reference point for governments, stakeholders, caregivers and communities to help identify common directions and opportunities, address gaps, and share best practices.
Activities to address the importance of access to quality care, from diagnosis through end of life, may include:
- Building evidence on effective innovative and alternative care models that support quality of life to address the needs of people living with dementia and caregivers, including a focus on removing barriers to care
- Identifying and adopting best practices, proven innovations and strategies that enhance integrated dementia care, focused on the safety, quality of care and quality of life of people living with dementia in long-term care
- Developing and sharing evidence-informed services, information and resources related to dementia care and advance care planning, and adapting them to different cultures, populations and languages
- Exploring and evaluating the use of affordable assistive technologies that can help people living with dementia to live safely, more economically, and independently
- Providing information and learning events to increase the understanding of the legal capacity and rights of people living with dementia, including the different decision-making models that are available to them
| Current status | Aspiration |
|---|---|
| Lack of access to, awareness or understanding of health and social services that provide integrated and person-centred care. | Integrated, person-centred quality care based on evidence-informed best practices across all settings and that people feel welcomed and well-cared for when hospitalization or admission to long-term care is necessary. |
Area of focus 4.4: Build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care
Delivering quality dementia care requires a wide range of care providers to meet the varying needs of people living with dementia and caregivers (see Figure 2). Employed care providers include nurses, family physicians, psychiatrists, and other health professionals (for example, social workers, psychologists, dental hygienists, pharmacists, occupational therapists, physical therapists, and speech language pathologists), and personal care workers. Collaborative care teams that bring these providers together and include people living with dementia and family/friend caregivers in decision-making have been shown to improve the quality of dementia care and reduce some symptoms of dementia.Footnote 64
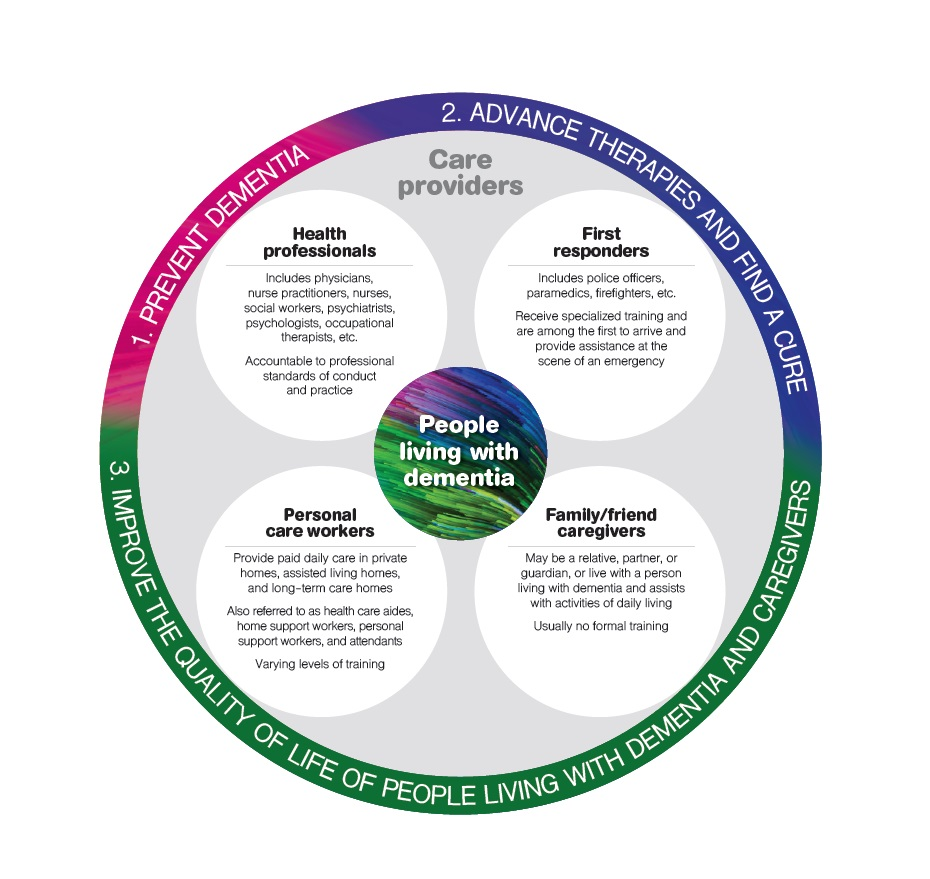
Figure 2 - Text description
This image explains 4 broad categories of care providers. It is a large circle with the 3 national objectives written around the perimeter (1. Prevent Dementia, 2. Advance therapies and find a cure, 3. Improve the quality of life of people living with dementia and caregivers).
Inside the circle are 4 smaller circles which name and describe the 4 types of care providers. These 4 smaller circles are:
- Health professionals - includes physicians, nurse practitioners, nurses, social workers, psychiatrists, psychologists, occupational therapists, etc. Health professionals are accountable to professional standards of conduct and practice.
- First responders - includes police officers, paramedics, firefighters, etc. First responders receive specialized training and are among the first to arrive and provide assistance at the scene of an emergency.
- Personal care workers - provide paid daily care in private homes, assisted living homes, and long-term care homes. Personal care workers are also referred to as health care aides, home support workers, personal support workers and attendants. They receive varying levels of training.
- Family/friend caregivers - may be a relative, partner, or guardian, or live with a person living with dementia and assists with activities of daily living. Family/friend caregivers usually receive no formal training. At the very center of the large circle is a small circle with text inside that says 'people living with dementia'.
Aside from family/friend caregivers, the majority of day-to-day hands-on care of people living with dementia is performed by personal care workers. Personal care workers work in private homes, within the community in assisted living homes, and in long-term care homes. Given the amount of time spent with the person living with dementia and the tasks they perform, personal care workers are an integral part of the care team who are well-positioned to notice changes in symptoms or behaviours and to be an active participant in discussions about care. However, staffing shortages, low wages with limited benefits and a lack of regular or guaranteed hours of work pose considerable challenges for these workers, who sometimes face discrimination, racism, and unsafe conditions that impact their health. Footnote 65, Footnote 66
Challenging working conditions, organizational challenges, and a lack of training can lead to burnout and high turnover rates, which can impact the quality of care that is provided. Footnote 67, Footnote 68 Improved access to evidence-informed, culturally safe and culturally appropriate guidelines for standards of care and best practices, such as through education and training, can improve the quality of care provided.
Health professionals also face challenges when providing care for a person living with dementia. Limited access to specialists (particularly in rural and remote areas), a lack of connection with community-based resources, time constraints, difficulties in coordinating care, and lack of access to interdisciplinary teams all present barriers to the provision of quality care. As a result, only 2 out of 5 Canadian family physicians feel well-prepared to manage community dementia care. Footnote 69,Footnote 70
Activities to build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care, may include:
- Assessing the availability and effectiveness of dementia care guidelines and best practices, including for standards of care, evaluating new evidence and identifying gaps
- Understanding barriers to using guidelines and best practices as a first step toward developing strategies to make them more accessible and to encourage wider use
- Evaluating the effectiveness of efforts to implement guidelines
- Determining what additional tools, beyond guidelines and best practices, may be necessary for care providers to complete their work
| Current status | Aspiration |
|---|---|
| Lack of information and resources for care providers, reducing the capacity to provide quality care. | Care providers have access to the resources and training needed to deliver quality care. |
Area of focus 4.5: Improve support for family/friend caregivers, including through access to resources and supports
Often, family members, neighbours and friends care for someone living with dementia, and organize the care delivered by others. These caregivers help with the essential activities of daily living and help keep the person living with dementia engaged in activities. Caregivers can spend approximately 26 hours per week caring for a person living with dementia. Footnote 71 This represents a significant amount of the caregiver's time, and often their own needs go unnoticed or unmet. Footnote 72
The significant physical, mental and financial impacts of caring for an individual living with dementia must be addressed. Caregivers experience high levels of stress and are at higher risk of injury and depression. They are susceptible to financial and employment difficulties, particularly those caring for a person diagnosed with young onset dementia. Some men may view themselves as being in a reversal of a traditional gender role as a caregiver and may be reluctant to seek help. Caregivers are essential members of the care team; improving support for them is integral to improving the quality of life of the person they are caring for and to ensuring their own health.
Mental and physical health
As dementia progresses, the needs of the person living with dementia increase which can result in the caregiver experiencing additional stress. Behavioural and psychological symptoms of people living with dementia can become more challenging to manage and have a significant impact on a caregiver's health. Footnote 73, Footnote 74 In cases where the person living with dementia needs to transition to a long-term care home or another facility, feelings of guilt can arise for caregivers. Some caregivers may not know when they need extra supports or how to access or use available resources, such as adult day programs, respite programs (see Text box 13) and education programs. Footnote 75
Text box 13: Respite care
Respite care provides caregivers with mental and physical relief. It allows the caregiver some time to themselves for self-care. This period of rejuvenation allows them to continue providing quality care for the person living with dementia when they return.
Respite can be provided in-home. Trained individuals will come to a home to provide care or companionship and assistance with the activities of daily living, offering a break to the caregiver.
Long-term care homes can also provide respite for caregivers by allowing short stays for people living with dementia.
Additionally, adult day programs can bring respite to caregivers, as they provide an opportunity for the person living with dementia to participate in activities and socialize with others in ways that do not require the usual caregiver to be present.
Finance and employment
Caregivers are often responsible for significant out-of-pocket costs, including costs for home modifications, help with activities of daily living, support for recreation, transportation, travel or accommodation, specialized aids or devices and medications, and rehabilitation services. On average, caregivers spend $4,600 out-of-pocket annually for each person under their care who is living with dementia. Footnote 76
For the approximately 60% of Canadian caregivers who are employed, Footnote 77 caregiving may have serious negative financial consequences, such as lost income due to reduced hours of work, leading to reduced pension and retirement income. Some may need to adjust work schedules, if they are able to find employment that will allow for an appropriate balance between work and caregiving, while others may need to leave the workforce entirely. Caregivers of persons with young onset dementia tend to be younger, provide more hours of care, and may experience greater financial impacts as a result of caregiving, as do those caregivers who already have a low income. Federal tax measures are in place to recognize the impact caregiving expenses have on the ability to pay tax. Footnote 78, Footnote 79 Provinces and territories provide similar credits. In terms of direct support for caregivers, provinces and territories offer a variety of financial supports. For example, the provinces of Quebec and Manitoba offer tax credits and Nova Scotia offers financial benefit payments to caregivers. Other jurisdictions, such as Newfoundland and Labrador, allow the care recipient to pay a family member to provide care.
Activities to improve support for family/friend caregivers, including through access to resources and supports, may include:
Mental and physical health
- Supporting the mental and physical health and wellbeing of caregivers by identifying, and sharing evidence-informed, culturally safe and culturally appropriate information, tools and resources on, for example: self-care; how to navigate the health care system; approaching primary care practitioners about symptoms or concerns; how to provide care for a person living with dementia; and how to support transitions to long-term care
- Continuing to fund community-based projects on mental health supports and information about self-care for caregivers as well as promoting the use of available respite services and community support groups
- Supporting the ongoing assessment of caregiver needs in addition to those of the person living with dementia
Finance and employment
- Continuing to provide tax relief/credits for caregivers and promote awareness of their availability
- Raising awareness among employers of the need for flexible workplaces that can accommodate the needs of caregivers to balance work and caregiving
- Examining the needs of caregivers who are still in the workforce to inform policy and program design
| Current status | Aspiration |
|---|---|
| Caregivers experiencing burnout, financial hardship, isolation and depression while caring for someone living with dementia. | All caregivers have access to the resources and supports required to protect their own wellbeing and to care for someone living with dementia, including being equipped to navigate health care and other support systems. |
Chapter 5: Pillars
Five pillars are essential for effective implementation of the national strategy for dementia:
- Collaboration among all governments in Canada and all organizations working on dementia-related initiatives
- Research and innovation on prevention, therapies and a cure, and quality of life
- Surveillance and data to improve understanding of the impact of dementia in Canada and to identify and support efforts that are effective
- Information resources that are accessible and evidence-based
- A skilled workforce now and into the future to provide quality dementia care and pursue the research and innovation priorities ahead
A concentrated effort and investment in these 5 areas will enable Canada to achieve the 3 national objectives related to prevention; therapies and a cure; and quality of life for those living with dementia and caregivers.
Collaboration
A collaborative approach provides an opportunity to learn from one another and enables a broader understanding of dementia, rooted in both knowledge and experience. Collaboration can take many forms, including working together to design and develop dementia policies and programs, engaging in research, and sharing data, knowledge and best practices. Many different organizations and individuals are engaged in dementia-related activities, including those in research, health and social care, and communities (see Figure 3). Each brings a unique set of expertise and experiences. Ensuring that dementia initiatives are informed by a broad range of perspectives increases the chances of these initiatives being effective and widely adopted.
The Public Health Agency of Canada will continue to work collaboratively with others in support of achieving the national objectives of the national dementia strategy, including people living with dementia, researchers, health professionals, caregivers, advocacy groups, academia, provincial and territorial governments, other federal organizations, international organizations and governments, non-governmental organizations, and populations who are at higher risk and face barriers to equitable care.
Figure 3: Together we achieve dementia objectives
Figure 3 - Text Description
This image shows all the stakeholders who will be instrumental in achieving dementia strategy objectives.
The image depicts a large cog wheel on the left representing Canada and a smaller interconnecting cog wheel on the upper right representing the international community.
Within the Canada cog, there are smaller cogs representing each of the stakeholders.
Cogs for 'People living with dementia' and 'Family/friend caregivers' are at the centre of the Canada cog.
Other smaller cogs within the Canada cog include: Care providers, Advocacy groups, Academia, Researchers, Provincial/territorial/local governments and the Government of Canada. Within the International cog, there are 2 smaller cogs: International organizations and International governments.
The Ministerial Advisory Board on Dementia, established in 2018, will continue its work to provide evidence-informed advice on current and emerging issues to help improve the lives of people living with dementia and caregivers.
Federal government
Several federal departments and agencies (see Appendix A) have mandates for policies, programs and services that have an impact on the quality of life of people living with dementia and caregivers, in areas such as housing, palliative care, and healthy eating. Continued collaboration through a whole-of-government approach will encourage consideration of how these federal initiatives could better support the strategy's national objectives.
Provincial and territorial governments
Provincial governments in Canada have shown leadership through dementia strategies and initiatives over the past 2 decades (see Text box 14 and Appendix B). Canada's dementia strategy builds on and complements this valuable work and will continue to do so as it moves into the implementation phase. The Federal/Provincial/Territorial Coordinating Committee on Dementia was established in 2017 to encourage collaboration among provincial and territorial health officials. This committee will continue to serve as an important mechanism to share information and best practices, as governments across Canada implement dementia-related activities and initiatives.
Text box 14: Examples of provincial dementia initiatives
British Columbia: The Provincial Guide to Dementia Care in British Columbia (2016)
Alberta: The Alberta Dementia Strategy and Action Plan (2017)
Manitoba: Manitoba's Framework for Alzheimer's Disease and Other Dementias (2014)
Ontario: Ontario's Investments in Dementia Care in the Community (2018)
Quebec: Meeting the Challenge of Alzheimer's Disease and Related Disorders: A Vision Focused on the Individual, Humanism, and Excellence (2009 - expert report)
Nova Scotia: Towards Understanding: A Dementia Strategy for Nova Scotia (2015)
International
The challenges related to dementia are too large for one country to tackle alone. As this strategy is implemented, knowledge will be created and gathered globally on dementia prevention, therapies, care, quality of life and a cure. Canada will seek ways to learn from international experiences and knowledge. Canada adopted the World Health Organization's (WHO) Global action plan on the public health response to dementia (2017–2025), and will use Canada's strategy to support progress toward the WHO goals outlined for member states.
Canada also supports and provides data to the World Health Organization's Global Dementia Observatory to enable information sharing and tracking of progress on dementia issues across countries. Canadian participation in the World Dementia Council also supports collaboration at the international level and helps create a strong global network for the exchange of knowledge and best practices.
Priorities for collaboration:
- Support research initiatives that promote collaboration among researchers and other stakeholders
- Leverage the work of federal, provincial and territorial governments by promoting collaboration in areas of shared jurisdiction and in support of common priorities as well as by exchanging information on best practices through the Federal/Provincial/Territorial Coordinating Committee on Dementia
- Work collaboratively across the federal government to build greater understanding and align actions
- Continue learning from members of the Ministerial Advisory Board on Dementia, who represent a broad range of dementia stakeholders
- Further support Canada's participation in international collaborative efforts, including supporting progress on goals in the World Health Organization's Global action plan on the public health response to dementia (2017–2025), and the World Dementia Council
- Engage with Indigenous governments, organizations and communities to better understand unique dementia challenges and to facilitate the development of distinction-based dementia solutions for First Nations, Métis and Inuit
Research and innovation
Many gaps in our knowledge of dementia still exist. It is essential to ensure that research addresses these gaps and provides the greatest impact possible for people living with dementia in Canada and around the world.
Collaborative, multidisciplinary research efforts will: advance our understanding of the biological causes of dementia and risk and protective factors to support prevention; allow for identification of effective new therapies; improve dementia care and supports; and support quality of life for those living with dementia and caregivers. Research and innovation efforts will also move us closer to a cure. Innovation, including social and technological advancements, will create new tools, devices, methods, processes, and approaches to improve the lives of Canadians living with dementia and caregivers.
Canada remains active in national and international research initiatives, and will continue to pursue opportunities to collaborate across borders, and benefit from the expertise of researchers located in multiple regions. Through this international research collaboration, dementia researchers are able to leverage complementary strengths from other countries in order to maximize the impact of research.
Advancing research and innovation is only the beginning. Turning research findings into useful information that can be put into practice in programs and services is key to providing solutions for real-world settings. More work is needed to move dementia research into practice, to make it easier to evaluate and adopt results. These efforts should include greater engagement of people living with dementia and caregivers to ensure that research findings and innovative supports meet their needs in practical, culturally safe, culturally appropriate and meaningful ways.
Priorities for research and innovation:
- Invest in preventing dementia, delaying the onset of symptoms, enhancing dementia care and therapies, and improving the quality of life of those living with dementia
- Support and strengthen knowledge sharing mechanisms that expand understanding and access among a broad range of stakeholders
- Enable dialogue toward identifying solutions and evaluating effective approaches to overcome barriers that impede moving innovation and research into practice
- Encourage the active involvement of people living with dementia and caregivers at all stages of the research process, and build our knowledge base on how best to do that
Surveillance and data
In Canada, dementia surveillance is a shared responsibility among the federal, provincial and territorial governments. Others, including the Canadian Institute for Health Information, Indigenous organizations, other non-governmental organizations and academia, also play a role at the local, provincial and national levels through their collection, analysis and sharing of data.
Surveillance of dementia is the ongoing collection, analysis and sharing of data to inform public health actions. Optimizing dementia surveillance will provide a more accurate picture of its impact in Canada and a better identification of health needs. Surveillance provides data to inform policies, programs and research as well as health care planning and service delivery to meet the needs of people living with dementia and caregivers. High-quality data help ensure that activities taken to support this strategy are well-informed and appropriately targeted.
Public health data can give us insight into groups within the general population that are more impacted and more at risk. For example, evidence on where these groups are located and whether the number of people impacted is increasing or decreasing helps to support planning for dementia policies, programs and services. Surveillance data are being collected on several risk factors of dementia to offer insights on the effectiveness of dementia prevention efforts in lowering these risks. Surveillance data will also help to track progress on the strategy, assess the impact of activities, and help plan future efforts.
Priorities for surveillance and data:
- Regularly assess and review priorities for data collection to ensure alignment with emerging evidence and the strategy's national objectives, as well as to develop innovative solutions
- Continue to work with or seek engagement from the provinces and territories, governments, non-governmental organizations, and Indigenous organizations to conduct and strengthen ongoing surveillance of dementia
- Share data within Canada and internationally, in a timely manner and in ways that make it accessible for all stakeholders, including people living with dementia and caregivers
- Contribute data on dementia in Canada to the World Health Organization's Global Dementia Observatory
Information resources
Broad access to evidence-based information resources is key to meeting the national objectives of the dementia strategy. Information about dementia comes from diverse sources, including research findings, surveillance and clinical data, and individual lived experiences. Information resources can take many forms, such as written materials, informal discussions, awareness campaigns, social media, online content and training programs. Development of these resources must be done in ways that ensure accessibility across cultures, languages and different geographic areas (such as rural/remote communities). Information resources can include tools that assist with daily living and therapies, or written materials, such as guidelines for care providers on how to diagnose and treat dementia, and platforms that help share information.
For example, many Canadians are not aware of how certain lifestyle choices could influence their chances of developing dementia. Evidence-based resources that educate the general public on ways to reduce their personal risk will help support prevention.
Better resources about day-to-day care can help people living with dementia and caregivers. Equipping care providers with evidence-based information resources benefits both those receiving and those providing care. Useful topics for caregivers could include: learning where to go for help; how to assist someone receiving news of a diagnosis; how to respond to and prevent challenging or violent behaviour; and how to locate sources of respite. Information resources can also be geared toward deepening understanding so that those in the community who interact with people living with dementia are able to do so with compassion, ease and confidence, resulting in a more positive experience for all and a reduction in stigma that might otherwise occur during these interactions.
Priorities for information resources:
- Update and develop information resources as new knowledge becomes available, in collaboration with stakeholders and partners (see Appendix C)
- Promote easy access to reliable, evidence-based information, research, educational resources and tools that are culturally safe and culturally appropriate
- Create mechanisms for tailoring information resources to the needs of specific stakeholders, and populations including people living with dementia and caregivers, as well as care providers and policy makers
Skilled workforce
The dementia workforce is diverse and includes researchers who are studying dementia, exploring the development of therapies and seeking a cure as well as care providers who interact with people living with dementia. Care providers in the workforce can include physicians, medical specialists, nurses, nurse practitioners, and personal care workers.
To find a cure and effective therapies for dementia, we need to ensure we have enough researchers working in this field. Many would argue that we do not currently have enough dementia care providers and that the quality of life for care providers and the people living with dementia they support is negatively impacted as a result. This challenge will only intensify as our population ages and if the number of people living with dementia increases as expected. Canada will need more care providers to meet this demand, requiring an increase in the number of students choosing careers in dementia care, geriatrics and home care as well as an increase in the number of post-secondary opportunities and work placements that provide this training.
Professional care providers need to be informed about dementia across the care pathway from diagnosis through to end of life to reduce stigma and improve the quality of care. Currently, some professionals may receive very little training on dementia. As a result, challenges may include: negative diagnosis experiences, misdiagnosis, difficult experiences in acute care settings such as hospitals, and a lack of access to geriatricians for people living with young onset dementia. Having professionals who are aware of the latest information about dementia, and available supports will allow for a diagnosis experience, specialist care, and acute care that are compassionate and provide hope.
Personal care workers often spend a lot of time with people living with dementia. When these workers are aware of evidence-informed dementia interventions, best practices and therapies, such as through training, there can be a direct improvement to the daily quality of life for people living with dementia.
Priorities for skilled workforce:
- Encourage recruitment to dementia-related training programs to increase the supply of professional care providers equipped to work with people with dementia and help reduce wait times for care
- Integrate a dementia lens within existing curricula (including palliative care for people living with dementia)
- Develop and share information on non-pharmacological, evidence-informed interventions, best practices and therapies for dementia with professional care providers
- Support strategies to lower injury and turnover rates, especially among personal care workers
- Explore what additional tools (e.g. training webinars, workshops), are necessary for professional care providers to provide the best care possible
Chapter 6: Focus on higher-risk and equitable care
Health equity is achieved when everyone has an equal opportunity to reach their fullest health potential regardless of factors such as social class, gender, or ethnicity. Footnote 80 Integrating health equity into Government of Canada policies, programs and practices is achieved in part through Sex and Gender-based Analysis Plus (SGBA+). The SGBA+ for this strategy identified individuals at higher risk of developing dementia and/or who experience significant barriers to diagnosis and access to dementia supports and services. Considerations for the following populations and individuals are detailed below: Indigenous peoples, individuals with intellectual disabilities, individuals with existing health issues, older adults, women, ethnic and cultural minority communities, LGBTQ2 individuals, official language minority communities, rural and remote communities, and young onset individuals. Further research is required to determine whether there are other populations at risk or facing barriers to equitable care. As activities in support of the strategy are developed, consideration will be given to the groups listed below as well as other groups that may be identified.
Populations who face barriers to equitable care and are at higher risk:
Indigenous peoples
Dementia is an emerging health issue among Indigenous populations. While there are limited data and research related to dementia in Indigenous populations, evidence suggests that the proportion of the population living with dementia is increasing more rapidly among First Nations populations compared with the general Canadian population, and that dementia onset may be occurring earlier. Footnote 81 While risk factors such as obesity, hypertension, and diabetes can be considered modifiable for the general population, for Indigenous peoples, these risk factors can be a result of long-term socio-economic marginalization and cannot be viewed through the same lens.Footnote 82
Standardized cognitive testing has been shown to be less accurate for Indigenous peoples, possibly resulting in misdiagnosis, and highlights the need to work collaboratively with Indigenous communities to develop culturally safe and culturally appropriate tools for diagnosis. For those who live on reserve, lack of access to health professionals and services on reserve, especially in rural and remote communities, as well as a lack of cultural safety in the health system create barriers to equitable care. Additional barriers, regardless of where people live, may include linguistic differences, racism and poverty. Footnote 83,Footnote 84
Intellectual disabilities
Studies suggest that 50 to 70% of adults with Down syndrome over the age of 60 are likely to develop dementia and that symptom onset tends to occur earlier. Footnote 85, Footnote 86, Footnote 87 However, assessment of dementia in individuals with intellectual disabilities can be challenging as these individuals may not be able to report dementia symptoms and commonly used dementia assessment tools are not relevant or effective.
Adults with intellectual disabilities have experienced stigma, discrimination and exclusion that can continue following a dementia diagnosis. Those with intellectual disabilities may also have unique care and support needs, arising from the combination of their previous disability with the overlay of dementia symptoms.
Furthermore, the service systems in place may not be well-equipped to address these needs: developmental service workers are sometimes not trained to support people with dementia and care providers are sometimes not trained to support people with intellectual disabilities.
There is currently a shift toward community housing for people with intellectual disabilities rather than traditional institutional housing. This change makes research, education, and training specific to the diagnostic and support needs of this population all the more important as well as greater community and public education and awareness.
Higher-risk populations:
Individuals with existing health issues or health behaviours known to be risk factors for dementia
People with certain existing health issues, such as mid-life hearing loss, and hypertension as well as depression and diabetes in later life, have a higher risk of developing dementia. We also know that people who have experienced stroke, heart failure and heart disease are at a higher risk of developing dementia. Footnote 88 Physical inactivity and smoking are examples of health behaviours that can put people at a higher risk of developing dementia.Footnote 89
Older adults
While dementia is not an inevitable part of aging, age is the greatest known risk factor for dementia. The number of Canadians with dementia more than doubles every 5 years after the age of 65. While less than 1% of Canadians between the ages of 65 and 69 are living with dementia, this number increases to 25% for those aged 85 and over.Footnote 90
Women
Of those over 65 years of age and living with diagnosed dementia in 2015–16, two-thirds were women. Footnote 91 The number of women in long-term care with dementia substantially exceeds the number of men with dementia. Footnote 92 Emerging research indicates that non-modifiable risk factors for dementia, such as genetics, impact women significantly more than men. As well, the majority of caregivers for people living with dementia are women and they are usually daughters and female intimate partners.Footnote 93
Populations facing barriers to equitable care:
Ethnic and cultural minority communities
Cultural differences in the understanding of and views toward dementia can result in a reluctance to talk about symptoms and may lead to under-diagnosis and difficulty connecting with networks of support that are useful following diagnosis. Understanding the impacts of dementia among ethnic minority populations is limited in Canada; however, studies from other countries have shown that ethnic minority people living with dementia and caregivers face difficulties in accessing care and support due to systemic racism and socio-economic marginalization. Footnote 94 A lack of information about dementia in their first language, as well as insufficient access to culturally safe and culturally appropriate dementia care can be barriers to diagnosis and treatment.Footnote 95
Lesbian, gay, bisexual, transgender, queer, two-spirit (LGBTQ2)
Some evidence indicates that LGB adults may experience delays in dementia diagnosis and difficulties finding supports due to stigma and social marginalization. Footnote 96 Transgender people face additional barriers to health services with a survey showing that 23% did not see a doctor or seek medical care for fear of being mistreated. Footnote 97 Concerns have been raised by LGBTQ2 adults about possible stigma and discrimination in assisted living and long-term care homes as well as the challenges around trust and disclosure of sexual orientation with rotating home care workers. Footnote 98 LGBT individuals are twice as likely to live alone and 3 to 4 times less likely to have children, which may limit their opportunities for support.Footnote 99
Official language minority communities (OLMCs)
Official language minority communities consist of Francophones who reside outside of Quebec and English-speaking residents of Quebec. Individuals living in these communities are more likely to face barriers to accessing services and/or information in their first language, including being able to communicate with health professionals. Footnote 100 The lack of information on dementia in the official minority language, as well as the lack of access to care for people living with dementia and their families that are culturally appropriate for OLMCs, can have an impact on the quality of care received, diagnosis, treatment and patient safety. It is also recognized that bilingual people living with dementia often revert to their first language resulting in challenges in being understood.
Rural and remote communities
Evidence shows that rural populations are aging more rapidly than urban populations due to youth outmigration and seniors retiring to rural communities. Footnote 101 People living in rural and remote communities may face social and geographical isolation.
Health and social supports are typically more sparse in rural and remote regions compared with urban communities, which can result in people living with dementia having to leave their communities or travel long distances for care and supports. In addition, caregivers may face limited access to adequate and appropriate health and social supports, making them more susceptible to stress and burnout.
Young onset dementia
Young onset dementia occurs when dementia is diagnosed before age 65 and represents approximately 3% of all dementia cases in Canada. Footnote 102 A lack of awareness of young onset dementia can lead to delays in diagnosis which result in delays in accessing needed supports and treatments. Footnote 103 A lack of age-appropriate services is a significant barrier to the quality of life for people living with young onset dementia and caregivers. Those with young onset dementia and those who provide care may also face additional challenges related to caring for young children, being in mid-career and/or having major financial commitments.
Federal dementia-related activities with a focus on higher-risk and equitable care
Dementia Community Investment
Through the Dementia Community Investment, the federal government supports community-based projects that: develop, test and share information, programs, best practices, and/or tools to optimize the wellbeing of people living with dementia and caregivers, who are predominately women. The Dementia Community Investment will prioritize projects targeting various populations such as women and Indigenous populations who are more at risk of developing dementia or experiencing barriers to care and supports.
First Nations and Inuit Home and Community Care Program
The Government of Canada supports the delivery of primary and public health services to First Nations and Inuit communities, including in rural, remote and isolated areas where provincial and territorial services are not readily available. For those who do not require medical assistance, the Assisted Living Program provides funding for non-medical, social support services to seniors, adults with chronic illness, and children and adults with disabilities (including conditions like dementia), to help them maintain their independence. Care can be provided at home or in an institutional setting such as assisted living or long-term care. First Nations people living off-reserve are generally not included in this program.
Healthy living and chronic disease prevention - multisectoral partnerships
The Government of Canada supports collaborative action across all sectors of society to promote healthy living and prevent chronic disease in Canada including among those experiencing health inequality. Since 2013, funding has been invested and leveraged to support prevention interventions that promote healthy living and healthy weights, and prevent chronic disease by focusing on modifiable risk factors such as unhealthy eating, physical inactivity and tobacco use.
Research
The Government of Canada funds dementia-related health research through efforts such as the Challenge of Dementia in Indigenous Populations, the Wilfred and Joyce Posluns Chair in Women's Brain Health and Aging, and activities undertaken through the Canadian Consortium on Neurodegeneration in Aging (CCNA) (see Text box 15) that support research for those at higher risk of developing dementia and/or experiencing barriers to accessing care and support services. Many of these efforts are collaborative and funded in partnership with other organizations.
Text box 15: The Canadian Consortium on Neurodegeneration in Aging (CCNA)
The CCNA includes researchers focused on issues in dementia care within rural and Indigenous populations. In 2017, team members worked closely with elder Jerry Otowadjiwan, an Indigenous-owned graphic design agency, and First Nations home care staff to enrich a series of factsheets about dementia, memory loss, and healthy aging. The factsheets are available on the I-CAARE website. The team also developed the Canadian Indigenous Cognitive Assessment, which is a culturally-appropriate tool to screen for dementia among Indigenous people in Canada.
A more complete list of federal government dementia-related initiatives can be found in Appendix A.
Chapter 7: Moving towards implementation
Annual reports will be tabled in Parliament by the Minister of Health that will share progress on efforts to advance on the national objectives of the strategy, starting in June 2019. These reports will identify federal efforts contributing to the strategy. They will also note collaborative efforts with provincial, territorial and local governments and with dementia stakeholders. Indicators will be developed to measure the effectiveness of the strategy.
The reports will reflect new activities supported by the Budget 2019 funding announcement of $50 million over 5 years, starting in 2019–20, as well as Budget 2018 funding of $20 million over 5 years, and $4 million per year ongoing. These investments will be used to achieve the following:
- Increase awareness in Canada about actions that may prevent dementia or delay its onset, and ways to reduce stigma. Reducing stigma is central to the quality of life of people living with dementia, to ensure that they are able to stay active and involved in their workplaces and communities for as long as possible, and are able to maintain dignity and autonomy.
- Develop treatment guidelines and best practices for early diagnosis to support quality care and move toward a Canada where a dementia diagnosis is timely, provided compassionately and supported through access to resources and other forms of assistance.
- Improve our understanding of the effects of dementia on our communities. We have some information about rates of dementia in Canada, but much more data is needed to ensure that efforts to achieve the strategy's national objectives are as effective as possible and that our resources are focused on the right priorities.
- Support and evaluate the impact of community-based projects that seek to optimize the wellbeing of people living with dementia and/or the family members and friends who care for them and measure the projects' effectiveness.
The strategy is designed to foster meaningful progress on each national objective in the years to come by setting out clear areas of focus to concentrate efforts and define what we hope to achieve through these efforts. The table below sets out the aspirations for each area of focus. Some of these aspirations may be achieved sooner than others.
Current status |
Aspiration |
|
|---|---|---|
| Prevent dementia | ||
| 1 | Incomplete understanding of risk and protective factors linked with dementia, with some factors not yet identified and insufficient evidence on the link between factors and dementia. | A complete understanding of the risk and protective factors linked to dementia, their impacts and interactions. |
| 2 | Limited evidence about effective interventions to reduce risk for dementia and insufficient information resources. | Availability of effective prevention resources and interventions, supported by a strong evidence base. |
| 3 | A lack of awareness among the general public and care providers about actions that may help prevent dementia. | All people living in Canada are aware of actions that prevent dementia. |
| 4 | Barriers related to built and social environments limit the ability of individuals to pursue healthy living in ways that may reduce the risk of developing dementia. | All people living in Canada have access to built and social environments that support their ability to pursue healthy living in ways that may reduce their risk of developing dementia. |
| Advance therapies and find a cure | ||
| 1 | Limited broad stakeholder input when setting research priorities and insufficient engagement of people living with dementia and caregivers. | Research priorities established in an inclusive manner with broad stakeholder input, with the participation of those living with dementia and caregivers. |
| 2 | Annual investment in dementia research in Canada is less than 1% of dementia care costs. | Annual investment in dementia research in Canada exceeds 1% of dementia care costs. |
| 3 | Options for evidence-informed therapies remain limited and often are not person-centred. | New evidence-informed person-centred therapies are more readily available. |
| 4 | People living with dementia and caregivers are predominantly the subject of research to develop new therapies and find a cure. | People living with dementia and caregivers are active participants and partners in research to develop new therapies and find a cure. |
| 5 | Research findings tend to stay within academic settings and journals and are not broadly known, accepted, or brought into clinical practice. | Research design always includes efforts that ensure findings can be understood, adopted and quickly put into practice. |
| Improve the quality of life of people living with dementia and caregivers | ||
| 1 | Widespread stigma within communities and a lack of understanding of dementia. | All people living in Canada understand dementia and stigma no longer exists in Canada. |
| 2 | Individuals are unable to receive an early or timely diagnosis, or feel unsupported when receiving a diagnosis. | A timely diagnosis, provided in a compassionate manner, is available to all people living in Canada, along with immediate availability of resources and supports. |
| 3 | Lack of access to, awareness or understanding of health and social services that provide integrated and person-centred care. | Integrated, person-centred quality care based on evidence-informed best practices across all settings and that people feel welcomed and well-cared for when hospitalization or admission to long-term care is necessary. |
| 4 | Lack of information and resources for care providers, reducing the capacity to provide quality care. | Care providers have access to the resources and training needed to deliver quality care. |
| 5 | Caregivers experiencing burnout, financial hardship, isolation and depression while caring for someone living with dementia. | All caregivers have access to the resources and supports required to protect their own wellbeing and to care for someone living with dementia, including being equipped to navigate health care and other support systems. |
The strategy provides a broad framework for dementia-related activities across Canada and can be tailored by individual communities, organizations and local governments to support their distinct needs. Individual organizations are encouraged to keep this in mind as they undertake their work on dementia.
Though the strategy is meant to be implemented broadly, it also recognizes that Indigenous communities and individuals have distinct dementia experiences and distinct needs. The principles, national objectives, and activities are designed to facilitate Indigenous-led efforts to prevent dementia and improve the quality of life for people living with dementia and caregivers in Indigenous communities. Ongoing dialogue and engagement with First Nations, Métis and Inuit governments, organizations and communities is important as the strategy moves toward implementation. This engagement is key to understanding how to develop dementia resources and supports that are culturally safe and culturally appropriate.
Our success in moving toward the vision of this strategy will be a result of the efforts of all governments in Canada as well as of many organizations and individuals whose work touches on dementia-related challenges. In fact, all Canadians can support the national objectives of the strategy by adopting healthy behaviours to prevent dementia and by taking steps to make our communities more inclusive of those living with dementia.
Appendices
Appendix A: Federal government dementia-related initiatives
Active engagement across federal government departments was instrumental in the development of this strategy. An Interdepartmental Committee on Dementia was put in place to inform, engage and gather balanced input from across the federal government.
The dementia strategy for Canada is based on a whole-of-government approach given the many federal initiatives that support people living with dementia and caregivers. The following snapshots highlight some of these federal initiatives.
Canadian Institutes of Health Research
As Canada's federal funding agency for health research, Canadian Institutes of Health Research (CIHR) supports the creation of research evidence and its translation into improved health outcomes for Canadians, more effective health services and products and a strengthened Canadian health care system. CIHR is part of the federal Health Portfolio, which supports the federal Minister of Health in maintaining and improving the health of Canadians.
Between 2013-14 and 2017-18, CIHR invested close to $200 million in dementia-related research through its investigator-initiated and priority-driven research funding programs. These research investments span the areas of biomedical, clinical and health services research as well as population and public health research that aims to better understand the ways in which social, cultural and environmental factors influence the health of Canadians.
The CIHR Dementia Research Strategy supports research on the latest preventive, diagnostic and treatment approaches to Alzheimer's disease and other neurodegenerative diseases causing dementia. The CIHR Dementia Research Strategy consists of both international and national components, which together allow the Government of Canada to support world-class research on dementia. For example, the Canadian Consortium on Neurodegeneration in Aging (CCNA), supported by CIHR and many partners, is a research hub that brings together over 350 researchers as well as partners from across Canada to help accelerate the development of dementia treatments and care. CIHR also facilitates the participation of Canadian dementia researchers in international research activities through its engagement in strategic international research partnerships.
Through the Networks of Centres of Excellence program, supported jointly by CIHR, the Natural Sciences and Engineering Research Council and the Social Sciences and Humanities Research Council, the Government of Canada is supporting dementia-relevant research and innovation efforts. This includes the Canadian Frailty Network which aims to have an impact in 4 areas: improved care of the sick elderly; improved efficiency of the health care system; evidence-informed policy and practice; and reduced moral distress for patients, families, and caregivers. In addition, the Aging Gracefully across Environments using Technology to Support Wellness, Engagement and Long Life (AGE-WELL) research network aims to accelerate the delivery of technology-based solutions to improve health outcomes and increase independence and quality of life for seniors.
Correctional Service Canada
Responding to the unique needs of older persons in custody, including those who may have dementia, while maintaining safety and security, is complex. In May 2018, Correctional Service Canada (CSC) approved the policy framework Promoting Wellness and Independence - Older Persons in CSC Custody. The framework is comprehensive and identifies priority areas for action. It was informed by domestic and international research and consultation with expert stakeholders in the fields of geriatrics, gerontology, law, culture, Indigenous health and correctional health.
CSC is mandated, under the Corrections and Conditional Release Act, to provide every inmate with essential health care that conforms to professionally accepted practices, and reasonable access to non-essential mental health care that will contribute to the inmate's rehabilitation and successful reintegration into the community. Within CSC, the provision of health services is governed by the Health Sector. Consistent with health services in the wider Canadian community, CSC's health services are accredited by Accreditation Canada.
Department for Women and Gender Equality
There is a complex relationship between dementia and domestic violence; people with dementia are at increased risk of different forms of abuse (e.g. verbal, physical, sexual, financial, and psychological abuse as well as neglect) due to their cognitive impairment, loss of or limited capacity, and/or communication challenges as well as increased dependence on caregivers. The person with dementia may also abuse the caregiver, due either to lifelong habits or to the impacts of dementia. Given the prevalence of dementia among women and the gendered nature of caregiving, this violence may be considered gender-based violence.
It's Time: Canada's Strategy to Prevent and Address Gender-Based Violence is the Government of Canada's response to gender-based violence (GBV). The strategy takes a whole-of-government approach, building on and aligning with current GBV efforts by federal departments as well as provincial and territorial governments. The strategy's initiatives are organized across 3 pillars: Preventing GBV; Supporting Survivors and their Families; and Promoting Responsive Legal and Justice Systems. It is coordinated by the GBV Knowledge Centre at the Department for Women and Gender Equality. The strategy fills gaps in programs and supports for at-risk and vulnerable populations, including senior women and women living with disabilities, such as dementia.
Employment and Social Development Canada
The New Horizons for Seniors Program (NHSP) provides funding for projects that make a difference in the lives of seniors and in their communities. Projects relevant to dementia issues include promoting the inclusion of seniors with dementia, reducing caregiver burden through the provision of supports, education, and interventions and working to address awareness about dementia and the isolation that is often experienced both by persons with dementia and by people caring for family members or friends living with dementia. The 2019 NHSP Community-based Annual Call for Proposals identifies 3 national priorities: supporting healthy aging in community; addressing dementia, including supports; and intergenerational housing. The 2018–2019 Pan-Canadian Call for Concepts focuses on increasing the social inclusion of vulnerable seniors' subpopulations, including those with dementia.
The Workforce Development Agreements (WDAs) provide funding to provinces and territories (P/Ts) to support them in their efforts to offer employment assistance and skills training with the flexibility to respond to the diverse needs of their respective clients. Programs delivered under the WDAs seek to help individuals who are further removed from the labour market, unemployed, underemployed, or seeking to upskill, to either find and maintain good jobs or reorient their careers. These agreements include specific funding targeted for persons with disabilities, which may include persons with dementia. They can also be used to support members of underrepresented groups (e.g., older workers) and employers seeking to train current or future employees. This may include supporting training for individuals who work or wish to work in professions that support persons with dementia.
When in force, amendments to the Canada Labour Code, passed as part of the Budget Implementation Act, 2017, No.2, will provide federally regulated private-sector employees with the right to request flexible work arrangements from their employer, such as a change to the number of hours they must work, their work schedule or their location of work. Additional changes will provide for 5 days of personal leave per year (3 of them paid) to deal with family and other responsibilities as well as measures to improve the predictability of hours of work. These changes may support employees with caregiving responsibilities.
Employment and Social Development Canada (ESDC) also provides funding to help persons with disabilities prepare for, obtain and maintain employment through the Opportunities Fund for Persons with Disabilities ("Opportunities Fund") program. The Opportunities Fund program provides employment support to persons who self-identify as having a disability, including cognitive and memory disabilities, such as dementia.
Canada Pension Plan (CPP) Disability Benefits is a legislative program that provides partial income replacement to working age individuals between 18 and 64 who are not in receipt of a CPP retirement pension, and who meet the contributory and medical (cannot work due to a severe and prolonged disability) criteria.
Finance Canada
Finance Canada provides tax assistance in recognition of the fact that individuals living with dementia and those who care for them may have a reduced ability to pay tax. For example, individuals who provide support to an infirm family member may be eligible for tax relief through the Canada caregiver credit (CCC), introduced in 2017. Individuals may claim a non-refundable tax credit on an amount of up to either $7,140 (in 2019) (a maximum tax relief of $1,071) or $2,230 (a maximum tax relief of $335), depending on the infirm dependant for whom the CCC is being claimed and whether other dependency-related credits are being claimed in respect of that person. The amount is also reduced by the infirm dependant's net income above a specific threshold.
In addition, tax relief is available in respect of above-average medical expenses, including disability-related expenses, through the medical expense tax credit and for non-itemizable disability-related expenses through the disability tax credit.
Health Canada
Budget 2017 confirmed $11 billion over 10 years for provinces and territories to improve access to mental health ($5 billion) and home care services ($6 billion). In August 2017, federal, provincial, and territorial (FPT) governments endorsed A Common Statement of Principles on Shared Health Priorities that sets out pan-Canadian objectives for home and community care, including palliative care, as well as mental health and addiction services. Specific priorities for home and community care include spreading and scaling evidence-based models that are more integrated and connected with primary health care; enhancing access to palliative and end-of-life care at home or in hospices; increasing support for caregivers; and enhancing home care infrastructure, such as digital connectivity, remote monitoring technology and facilities for community-based service delivery. The federal government has now concluded bilateral agreements with all provinces and territories which provide details on how the federal funding will be spent within these priorities. Some jurisdictions such as Nova Scotia and Newfoundland have identified initiatives and activities focused on dementia.
Health Canada consulted with Canadians, including provinces and territories, people with life-limiting illnesses, caregivers, palliative care experts and care providers to inform the Framework on Palliative Care in Canada which was publicly released in December 2018. Palliative care is an approach that aims to reduce suffering and improve the quality of life of individuals with life-limiting illnesses such as dementia, and of their families and caregivers.
The Health Products and Food Branch of Health Canada is the national authority that regulates, evaluates and monitors the safety, efficacy, and quality of therapeutic and diagnostic products available to Canadians as well as medical devices and natural health products. Under the Regulatory Review of Drugs and Devices initiative, Health Canada is establishing a new division within the Therapeutic Products Directorate's Medical Devices Bureau to allow for a more targeted pre-market review of digital health technologies, to adapt to rapidly changing technologies in digital health, and to respond to fast innovation cycles.
Indigenous Services Canada
The First Nations and Inuit Home and Community Care Program provides a continuum of basic home and community care services that enable First Nations and Inuit of all ages, including vulnerable seniors and those living with disabilities, or with acute or chronic illness, to receive the care they need in their homes in their respective communities. The program invested approximately $142 million in Indigenous communities in 2017-18.
The Assisted Living Program provides funding for non-medical, social support services to seniors, adults with chronic illness, and children and adults with disabilities usually living on reserve, to help them maintain their independence. Care can be provided in-home or in an institutional setting to populations including clients living with dementia, depending on the person's needs.
Justice Canada
The Justice Canada component of the federal Family Violence Initiative (FVI) supports the development, implementation, testing and assessment of models, strategies and tools to improve the criminal justice system's response to family violence. Funding is administered through the Justice Partnership and Innovation Program. The Justice FVI includes a focus on elder abuse which is relevant to individuals with dementia who may be suffering from abuse by someone they know, such as an intimate partner, spouse, family member or caregiver.
The Federal Victims Strategy (FVS) is a horizontal initiative led by Justice Canada. Its objective is to give victims a more effective voice in the criminal justice system, including older adult victims and victims with disabilities/conditions, such as those living with dementia. The Victims Fund, through the FVS, is available to provincial and territorial governments and non-governmental organizations to support projects that address the needs of victims and survivors of crime in the criminal justice system. The Victims Fund can support projects that meet the needs of older adult victims and victims with disabilities.
Public Health Agency of Canada
The Public Health Agency of Canada (PHAC) has led the development of the national dementia strategy and will coordinate its implementation. PHAC initiatives support all 3 national objectives of the strategy. Examples include the following:
The federal government has a convening and coordination role in surveillance of dementia. PHAC conducts ongoing surveillance of dementia through the Canadian Chronic Disease Surveillance System (CCDSS). This system is a collaborative network of provincial and territorial surveillance systems. PHAC works with the provinces and territories to collect data on all residents who are eligible for provincial or territorial health insurance. It can generate national estimates and trends over time for more than 20 chronic diseases, including dementia prevalence, incidence and all-cause mortality.
In 2018, PHAC launched the Dementia Community Investment, a $4 million per year ongoing investment, which funds community-based projects that seek to optimize the wellbeing of people living with dementia and/or the family members and friends who care for them; increase knowledge of dementia and its risk factors; and undertake intervention research to assess the effectiveness of the program or initiative and apply that knowledge to support expansion of the project's reach to new communities, sectors, populations and/or jurisdictions.
Budget 2019 provides $50 million over 5 years, starting in 2019-20, to support the implementation of the national dementia strategy and to work with key stakeholders to: increase awareness about dementia through targeted campaigns and activities that focus on prevention, reducing risk and stigma; develop treatment guidelines and best practices for early diagnosis; and improve our understanding of the prevalence and effects of dementia on our communities.
PHAC provided $42 million over 5 years (2015-2020) to help establish the Centre for Aging + Brain Health Innovation. Funding for the Centre supports the development, testing, and scale-up of products and services to support brain health and aging, with a focus on dementia.
PHAC is facilitating the creation of new partnerships, ideas and interventions through its healthy living and chronic disease prevention multi-sectoral partnerships program. This program has invested $112 million and leveraged an additional $92 million in non-governmental funding from partners since its 2013 launch, to promote healthy living and prevent chronic disease. It aims to advance innovative solutions to public health challenges by providing the co-investment needed to test and/or scale-up the most promising interventions. Priority areas of this program include addressing common risk factors, such as physical inactivity, unhealthy eating, unhealthy weights and tobacco use, which underlie many major chronic diseases, including those linked with dementia, such as cardiovascular disease and type 2 diabetes.
Veterans Affairs Canada
Veterans Affairs Canada (VAC) compensates Veterans with approved disabilities related to their military service. VAC will cover necessary health care for eligible Veterans and other eligible clients across a wide range of health benefits which extends to treatment for those with dementia. For Veterans, this may include treatment benefits, home care supports through the Veterans Independence Program or long-term care. In addition, the Caregiver Recognition Benefit (CRB) was introduced in April 2018 to recognize the integral role an informal caregiver plays in the health and wellbeing of Veterans living with physical and/or mental health conditions (for which disability benefits under the Veterans Wellbeing Act have been approved) and who require ongoing provision of care or supervision. The CRB recognizes the important role of caregivers, who are often the spouse or common-law partner, of Veterans eligible exclusively under the Veterans Wellbeing Act and provides them with $1,024 per month (2019 rate), tax free.
Appendix B: Overview of provincial and territorial dementia-related initiatives
Provincial and territorial governments are responsible for health care delivery within their jurisdictions. The provinces and territories bring together unique perspectives from across the country and have been crucial to the development of Canada's dementia strategy.
In December 2017, the Federal/Provincial/Territorial Coordinating Committee on Dementia (FPT-CCD) was established to provide FPT governments with a forum for collaboration, information sharing, and discussion of programs, policies and issues related to dementia. This committee helps to strengthen FPT relationships for the purpose of addressing the public health challenge of dementia. The FPT-CCD is co-chaired by 1 federal representative and 1 provincial/territorial representative. Continued dialogue through this committee will enable implementation of the strategy. Membership of the committee includes all jurisdictions with the exception of Quebec which has opted to engage through bilateral discussions.
The following snapshots highlight some of the significant provincial and territorial dementia-related work underway:
British Columbia
British Columbia (B.C.) released the Provincial Guide to Dementia Care (PDF) in 2016. This guide built on earlier province-wide directions including the Dementia Action Plan in 2012 and the Dementia Services Framework in 2007. The Guide has 4 priorities:
- Increase public awareness and early recognition of cognitive changes
- Support people with dementia to live safely at home for as long as possible, including caregiver support
- Improve the quality of dementia care in residential care, including palliative and end-of-life care
- Increase system supports and adoption of best practices in dementia care
Guidelines have been developed to support quality dementia care in British Columbia. Among these, the B.C. Guideline: Cognitive Impairment - Recognition, Diagnosis and Management in Primary Care provides clinical practice guideline recommendations to practitioners on delivering quality, appropriate care for people with cognitive impairment.
The province is building on investments to support people with dementia to live safely at home for as long as possible, including caregiver support. The province has recently expanded respite care and adult day programs, helping both seniors and caregivers. The province is also increasing the number of direct care hours seniors receive in long-term care. This is part of a larger strategy to ensure that B.C. seniors are getting the quality care they need.
Alberta
Alberta's first dementia strategy was released in 2002 to provide information and advice to support the planning of continuing care services for individuals with Alzheimer's disease and other dementias. Since then, the Government of Alberta has broadened its focus to address the changing needs of people living with dementia and caregivers within society. The Alberta Dementia Strategy and Action Plan, released in 2017, was developed in partnership with people living with dementia, caregivers and families, Alberta Health Services, Alzheimer's Societies operating in Alberta, care providers and community organizations. It focuses on brain health, timely diagnosis, accessible services and providing supports for families from the onset of dementia through to end-of-life. Alberta takes a person-centred approach to care that recognizes the importance and input of people living with dementia and caregivers, and focuses on enabling care and support within the community, for as long as possible.
Alberta has invested in a number of initiatives to advance the implementation of its Strategy, including, but not limited to the following:
- Supporting the province-wide implementation of the First Link® program by the Alzheimer Society of Alberta and Northwest Territories
- Providing telephone access to clinical dementia support across Alberta, through specially trained Dementia Advice nurses, a service available through Health Link 811
- Offering short-term grants to community and health service providers to test innovations designed to optimize independence and quality of life for people living with dementia and caregivers
- Increasing primary care capacity to recognize, diagnose and provide ongoing care for people with dementia (accomplished through activities like the Primary Health Care Integrated Geriatric Services Initiative)
- Reducing the inappropriate use of antipsychotics in continuing care facilities
Saskatchewan
People with Alzheimer's disease and related dementias, along with their families, have access to a number of services delivered through the Saskatchewan Health Authority, its affiliated agencies and other community-based organizations. The Government of Saskatchewan has recently committed a significant increase in funding to the Alzheimer Society of Saskatchewan (ASOS) to enhance its programming. Funding will be used to: expand the First Link® program, which refers physicians, health care providers and other community service providers to the ASOS for services and supports; add system navigators to connect clients with appropriate services outside of the ASOS; implement a chronic disease management program for people living with dementia; implement an "early diagnosis and lowering the risk" awareness campaign; and, enhance support to rural areas of the province through a Dementia Helpline.
The Rural and Remote Memory Clinic at the University of Saskatchewan streamlines assessment and diagnosis of atypical and complex cases of suspected dementia where an interdisciplinary team assessment is most needed. This clinic provides rural and remote communities with in-person dementia assessment services from an interdisciplinary team of health care providers in one day. This one-stop clinic reduces repeated travel over long distances and shortens the time to diagnosis, while also providing telephone follow-ups.
Two provincial Dementia Assessment Units assist in assessing the needs of clients and residents who have challenges that cannot be managed in the community or in long-term care. The goal is to stabilize these residents, develop a care plan in order to better manage their care, and return the individual to the home community. Each Unit also has a resource team (consisting of various team members) that provides screening for admission to the Unit, offers assistance to staff in the client's existing environment, and provides support upon discharge back to the home environment.
Saskatchewan is focusing on a provincial Connected Care Strategy (PDF). Connected Care focuses on providing safe, seamless care for patients as they move from one care setting to another, ensuring that patients receive care in the setting that best matches their needs. It is a collaborative, team-based approach designed so that patients are supported to manage their care in the community, whenever possible. Community Health Centers, that have a target population of frail seniors with multiple chronic conditions, are also being supported.
Additional services and supports in the community and the health care system include the following:
- Provision of geriatric services through the Saskatchewan Health Authority by a range of health care providers, including physicians, geriatricians, nurses, nurse practitioners, home care services, occupational and physical therapists
- Investments in staff training and infrastructure to support residents in long-term care facilities and provide a safer environment
- Monitoring of inappropriate use of anti-psychotics in long-term care
- Provision of adult day programs and respite programs in some long-term care facilities
- Loan of mobility aids to assist people with physical disabilities to live more independently at home
- A cap on prescription drugs for eligible seniors
- A provincial recognition program for communities that have taken steps to be age-friendly and inclusive of seniors
Manitoba
Manitoba's first dementia strategy was released in 2002 and resulted in initiatives that enhanced care and support for Manitobans living with dementia and caregivers. Manitoba Health released Manitoba's Framework for Alzheimer's Disease and Other Dementias (PDF) in 2014. This 5-year framework is focused on raising awareness, early recognition, initial assessment and diagnosis, management, care and support, end-of-life care, and research and evaluation. It is informed by consultations with caregivers and care/service providers in Winnipeg and rural communities. Manitoba prioritizes a collaborative approach to dementia care that includes government departments, health regions, social services and community-based partners.
The province is developing new initiatives in health care delivery including My Health Teams. These teams will support a more integrated primary care system and ensure access to earlier diagnosis and treatment, while promoting improved service coordination and outreach for all health conditions. They will bring together different health care providers such as doctors, nurses, nurse practitioners and others to provide high-quality primary care. In regards to dementia, each team member will use his or her expert knowledge and skills to offer the best care possible for people living with dementia.
Other current investments include: funding dementia education in personal care homes, funding the First Link® program, co-sponsoring a Provincial Dementia Research Chair, increased funds for geriatricians who choose to practise in Manitoba, and establishing the Caregiver Recognition Act and caregiver tax credit.
Ontario
The Ontario Ministry of Health and Long-Term Care's dementia care in the community investments help build a more integrated and enhanced suite of dementia services for people living with dementia and their care partners.
The dementia care in the community investments support the expansion, enhancement and coordination of services in the home and community sector, including the following:
- Behavioural supports for older adults in the community presenting with or at risk of responsive behaviours associated with dementia, complex mental health, substance use and/or other neurological conditions
- Education, training and ongoing supports through the Enhancing Care program, which provides therapeutic skills training to family or other care partners who provide care to individuals living with dementia
- The expansion and enhancement of community dementia programs and in-home respite, which provide activation for people living with dementia and reduce burnout for care partners
- Improved care coordination through a patient navigation service that connects newly diagnosed people living with dementia and their care partners to local community supports and services
- Improving timely access to specialists through initiatives such as GeriMedRisk, which is a rapid eConsult service that prevents adverse drug events, preventing unnecessary hospitalizations and delaying the need for long-term care home placement
The ministry's dementia care in the community investments build clinician capacity and expand local front-line services, creating a more patient-centred system that helps people live well with dementia as active members of their communities.
Quebec
In 2007, an expert panel, chaired by Dr. Howard Bergman, was created by Quebec's Ministry of Health and Social Services to set out the required guidelines and actions on Alzheimer's disease and other major cognitive disorders. The panel's report, Meeting the Challenge of Alzheimer's Disease and Related Disorders: A Vision Focused on the Individual, Humanism, and Excellence (PDF), was published in 2009 and contained 24 recommendations, with 6 priority targets driving further work:
- Increase access to front line health and social services with tangible second- and third line support, particularly through outpatient care teams managing behavioural and psychological symptoms associated with dementia (BPSD) and through memory clinics
- Develop and provide access to evidence based practice support tools
- Develop and implement education and training programs for stakeholders
- Develop the required communication tools
- Offer a comfortable stay during acute care hospitalization
- Gradually consolidate the range of services for caregivers, in collaboration with organizations involved in this business line
Quebec's approach focuses on the dignity of individuals with dementia and respect for their choices, as well as on enhancing front line services.
In 2013, to help reach the targets established in the expert panel's report, Quebec launched 19 pilot projects in 14 health regions. These projects were carried out in family medicine groups and involved interdisciplinary outreach services teams, supported by memory clinics. This integrated approach improved detection, diagnosis and the quality of follow up visits for individuals with dementia. The project's second phase, launched in 2016, enabled provincial scale up under the responsibility of all institutions.
Quebec is working with various partners to develop phase 3, which is focused on enhancing support for caregivers, among other things.
New Brunswick
The Government of New Brunswick committed in the 2017 document We Are All in This Together: An Aging Strategy for New Brunswick (PDF) to developing a provincial dementia plan to align with Canada's national dementia strategy. The aging strategy's goals are to (1) enable seniors to live independently, (2) achieve sustainability and innovation, and (3) embrace a provincial culture of person-centred care and support. Dementia care in New Brunswick is moving toward a more integrated/coordinated continuum of care and support to persons living with dementia and the people supporting them.
The Healthy Active Living Program provides information on lifestyle choices designed to help seniors make more informed choices about their health and wellbeing through education, personal empowerment and prevention/delay onset.
Currently, the Department of Health is developing a dementia strategy and action plan with its partners, the Department of Social Development, Horizon Health Network, Vitalité Health Network and Extra Mural/Ambulance New Brunswick with support from the Alzheimer Society of New Brunswick.
Engaging with stakeholders in all sectors and especially with persons living with dementia and caregivers has been the foundation of the approach in developing the strategy and action plan. New Brunswick is in an advantageous position to leverage the work done in other jurisdictions and at the national level that can be adapted to its environment.
Key themes are emerging from the work, which also align closely with objectives of the national strategy:
- Prevention and risk reduction
- Public awareness and education
- Supports for persons living with dementia and caregivers
- Trained workforce
- Enhanced quality of dementia care and services
- Enabling elements
Prince Edward Island
Prince Edward Island (PEI) released its Provincial Action Plan for Seniors, Near Seniors, and Caregivers Living on Prince Edward Island in 2018. This action plan responds to issues facing citizens as they age, including dementia. The vision for the action plan highlights an age-friendly health and social system that promotes wellness and preserves health. The plan's priorities include: (1) age-in-place initiatives, (2) age-friendly communities, (3) addressing ageism and supporting active aging, and (4) upstream endeavours that address the social determinants of health. These priorities are addressed in part through dementia-specific actions of improving support for people living with dementia and caregivers, enhancing training for health care providers and increasing public awareness of dementia risk factors.
PEI initiatives that focus on dementia include the Let's Talk Memory Campaign which includes targeted local and social media, posters, feature stories about Islanders and educational components to increase awareness (e.g. about risk factors and early signs of dementia) and reduce stigma.
Nova Scotia
In 2015, Towards Understanding: A Dementia Strategy for Nova Scotia was released to:
- Ensure access to timely and accurate diagnosis
- Provide better supports for families and caregivers
- Improve the coordination of person-centred and culturally relevant dementia care across the health system
- Increase public education and awareness
The strategy was developed using a broad consultative process that included input from more than 700 contributors, including those living with dementia, those caring for them, local and international researchers, health care providers, and community support agencies.
Notable strategy actions implemented since 2015 include the following:
- Revision of 811 tele-health dementia protocols
- A strengthened link between the Alzheimer Society of Nova Scotia (ASNS) and the provincial Health Authority to create improvements in end-of-life care
- Enhanced pathways for referrals to community support agencies
- Expanded eligibility criteria for Nova Scotia's Supportive Care and caregiver benefit programs, to include more clients with dementia
- Development of a primary health provider practice tool kit focused on diagnosis, treatment, and long-term care planning for dementia patients
- Provision of public awareness, education, and training for families, caregivers, and health care providers
The relationship between the provincial government and ASNS has included ongoing investment for some core services. In addition, Nova Scotia has funded ASNS to develop cultural competence training for staff in the delivery of culturally specific programs and services to groups such as: Francophones, First Nations and African Nova Scotians. Culturally diverse resources help in reaching all citizens of Nova Scotia living with dementia and caregivers.
Newfoundland and Labrador
Newfoundland and Labrador has adopted a Home First Initiative which aims to provide community-based supports and services to individuals with complex care needs to support them to remain at home in their communities and avoid hospitalization and premature long-term care placement. Dementia care is a priority within the Home First Initiative.
Priorities in Newfoundland and Labrador include a focus on education and awareness, improving programs and services to better support individuals with dementia in the community, and increasing support to families and caregivers. This work focuses on improving care coordination, health system integration for people living with dementia throughout their care journey and increasing public knowledge of dementia to reduce stigma. Enhancements to the HealthLine (811) including the addition of dementia-related resources and training for staff support, increased awareness and health system navigation. The Home Dementia Program will provide intensive case management led by a physician and a nurse practitioner to support clients with moderate to advanced dementia at home. The project aims to reduce falls, reduce inappropriate medications and help families manage the complex responsive behaviours often associated with dementia.
Long-term care homes in Newfoundland and Labrador are collaborating with the Canadian Foundation for Healthcare Improvement on the Appropriate Use of Antipsychotics to improve quality of life through a resident-centred approach.
The province works closely with the local chapter of the Alzheimer Society and provides funding to support First Link® and Dementia Passport, an electronic training platform. Newfoundland and Labrador is developing a provincial Dementia Care Action Plan in alignment with the national strategy.
Newfoundland and Labrador is supporting work on creating age-friendly communities (AFCs). AFCs promote health, remove barriers, and provide support for people to age in place and contribute to their communities, regardless of ability. These communities benefit people living with dementia, allowing more independence and supporting a better quality of life.
Nunavut
The Government of Nunavut released the Strategic Framework: Addressing the Needs of Nunavut Seniors (PDF) in 2016. This strategy provides an overview of programs and services for seniors and a comprehensive framework for seniors. Components of the framework relevant to dementia include (1) increased capacity of residential long-term care, including creating a secure dementia care unit in Nunavut, (2) family caregiver support, and (3) specialized dementia care training. Nunavut seniors face unique challenges in receiving care because their communities are fly-in only and complex care needs often require seniors to leave their home community for further treatment. The seniors' strategy is looking to address these challenges.
The Government of Nunavut's Department of Health delivers home care services through the Home and Community Care Program. These services are made available in all communities throughout Nunavut and provide support to Nunavummiut with assessed needs, as well as to their caregivers. These services include home support, personal care, and home nursing support to individuals with a dementia-related illness, as well as respite services to support the caregivers. There are also 5 long-term care facilities in Nunavut that can provide support to Nunavummiut at the early stages of a dementia-related illness, and are equipped with a wander guard system to provide safe care.
Included in the Home and Continuing Care Certificate program supported by the Government of Nunavut and facilitated by Nunavut Arctic College is a 10-day Dementia Care course to educate and support home and continuing care workers in providing dementia care to Nunavummiut. Additionally, over the last year, several deliveries of the Gentle Persuasive Approach (GPA) were provided across the territory and included train the trainer sessions, which helps support dementia care in the territory.
Northwest Territories
The Northwest Territories (NWT) released its Continuing Care Services Action Plan (PDF) in 2017. The plan includes recommendations and activities focused on aging in place, and it highlights caregiver support, training nurses in long-term care, and enabling staff to consistently apply a person-centred approach in dementia care. The NWT continues to build upon its evidence base and programs to expand dementia care services to support all NWT seniors and elders.
The Alzheimer Society of Alberta and NWT are involved in the Alzheimer's Champions program to train champions who will help advocate for caregivers to have access to information and supports. An Alzheimer champion is someone who has experience with Alzheimer's disease and other dementias and works as an advocate, giving a voice to others living with dementia when it comes to care and services. The Alzheimer Society is also responsible for disseminating research and best practice evidence to the Department of Health and Social Services of NWT staff. This program works to better the quality of life for people living with dementia and caregivers by increasing understanding and support in the broader community.
All new long-term care facilities in the NWT are designed and constructed to accommodate residents with dementia. The NWT has one 28-bed territorial dementia care facility that provides a high quality of therapeutic care through the Supportive Pathways care philosophy for residents with moderate to severe dementia. This client-centred approach provides individualized care to residents with dementia in a supportive, homelike environment. Each resident has a unique journey through the dementia process, which results in differing "pathways" of care. The Supportive Pathways program and other skills-based training strives to ensure that skilled staff, specially-designed environments and a partnership with families provide each resident with the highest quality of life possible.
Yukon
The Forward Together: Yukon Mental Wellness Strategy (PDF) was released in 2016. It is a 10-year plan developed in close partnership with First Nations communities. The strategy mentions the rising prevalence of dementia as one of the reasons for a mental wellness strategy. Resources for people living with dementia and caregivers, such as support groups for caregivers and families, are provided by both the territorial Department of Health and Social Services as well as community agencies.
Yukon aims to enhance the quality of life of people living with dementia. One Yukon initiative is to improve dementia accessibility of signage in long-term care facilities, using pictograms and colours, to facilitate navigation and service access for people living with dementia. As well, Virtual Reality Elder Care, a joint project of Kluane First Nation and Yukon Health and Social Services, reconnects home-bound and bed-bound Elders to the land, their community and their culturally significant activities. Yukon believes that providing on-the-land experiences through virtual reality can improve the quality of life for Elders.
Appendix C: Examples of non-governmental, non-profit and international organizations contributing to dementia-related initiatives
Across Canada, and internationally, there are many organizations that contribute to dementia-related initiatives in many ways. These organizations collaborate with one another or work alongside governments to improve the lives of people living with dementia and caregivers every day. While there are a number of organizations that contribute to dementia work in Canada, a few examples are listed below:
Alzheimer Society of Canada
The Alzheimer Society of Canada is the leading nationwide not-for-profit organization dedicated to enhancing the quality of life and care for people living with Alzheimer's disease and other forms of dementias, their caregivers and their families. Active in communities across Canada, the Society provides information, support and programs, from diagnosis to end of life. First Link® is an Alzheimer Society information and referral program that provides support and quickly connects individuals receiving a diagnosis with relevant health and social resources in their community. The Society also raises awareness and understanding about dementia and advocates for policy change within all levels of government. Through the Alzheimer Society Research Program, the Society funds research to improve diagnosis, advance treatment and care and to find cures.
Canadian Foundation for Healthcare Improvement
The Canadian Foundation for Healthcare Improvement (CFHI) is a not-for-profit organization funded by Health Canada. As part of its work, CFHI is improving elder care by incubating, spreading and scaling the Appropriate Use of Antipsychotics (AUA) approach across Canada. Antipsychotic medications are often prescribed to help manage symptoms related to dementia, such as agitation and aggression. However, there is a lack of evidence to support their effectiveness and a risk that they can cause significant side effects. AUA is a person-centred approach to care that engages all staff, along with the resident's family, to develop approaches to care that consider the preference of the resident and understand what triggers behaviours and provide more personalized care. In February 2019, CFHI, the New Brunswick Association of Nursing Homes and the Government of New Brunswick announced the results of a successful province-wide expansion of person-centred dementia care to 68 nursing home organizations in New Brunswick. CFHI is also supporting Quebec's own provincial expansion through the Optimizing Practices, Care, Use and Services—Antipsychotics initiative, as well as similar collaborations in Newfoundland and Labrador and in Prince Edward Island.
Canadian Geriatrics Society
The Canadian Geriatrics Society (CGS) is the national organization that represents specialists in Geriatric Medicine and Care of the Elderly. CGS members approach the care of persons with dementia through the holistic lens of the GERIATRIC 5Ms (PDF). Applied to dementia, the 5Ms are: Mind (diagnosis and treatment of dementia and delirium), Mobility (prevention of falls and injuries that lead to long hospitalizations and alternate level of care), Medications (deprescribing medications that worsen dementia by causing delirium and falls), Multi-complexity (care of persons with dementia who also have multiple other interacting diseases such as heart failure, diabetes, chronic lung disease leading to hospitalizations) and Matters Most (establishing Goals of Care and Advance Care Planning). As the medical specialists in the care of persons with dementia, CGS members are key to keeping persons with dementia safely at home and out of hospital or long-term care.
Canadian Institute for Health Information
The Canadian Institute for Health Information (CIHI) is an independent, not-for-profit organization that provides essential information on Canada's health systems and the health of Canadians. CIHI provides comparable and actionable data and information that are used to accelerate improvements in health care, health system performance and population health across Canada. CIHI works with a broad range of health organizations and partners across the country, including ministries of health, Statistics Canada, the Public Health Agency of Canada and Health Canada. Stakeholders use CIHI's broad range of health system databases, measurements and standards, together with evidence-based reports and analyses, in their decision-making processes. The CIHI Strategic Plan, (2016-2021) (PDF) focuses on a number of vulnerable populations, including seniors.
Canadian Home Care Association/Carers Canada
Carers Canada (formally known as the Canadian Caregiver Coalition), established in 2000, is an alliance of diverse partner organizations that work collectively and autonomously to identify and respond to the needs of carers in Canada. Under the leadership of the Canadian Home Care Association, Carers Canada enhances the quality of life for carers through synergistic partnerships and global advocacy.
In 2008, Carers Canada released the Canadian Carer Strategy (PDF) (updated in 2014) that outlines the 5 universal priorities to mobilize actions for carers across Canada. This strategy focuses on safeguarding the health and wellbeing of carers; minimizing the financial burden placed on family carers; enabling access to user-friendly information and education; creating flexible workplace/educational environments that respect caregiving obligations and investing in research on unpaid caregiving as a foundation for evidence-informed decision making.
Canadian Medical Association
The Canadian Medical Association (CMA) unites the medical profession in Canada to improve the health of Canadians and strengthen the health care system. It focuses on engaging collaborative dialogue and advocacy, consistently brings a patient perspective to its work, and seeks to inform and shape public policy with the perspective of Canada's physicians. Insights from its members and CMA policy specialists help to advance initiatives and policies to address some of the most pressing health issues in Canada. The CMA hosted its first-ever CMA Health Summit in Winnipeg in 2018 and has created a patient-engagement campaign (Demand a Plan) to support a national seniors care strategy. The CMA also works to advance initiatives and policies for the aging population, people living with dementia, and caregivers.
Canadian Nurses Association
The Canadian Nurses Association (CNA) provides a unified voice for Canada's nurses. It represents nurses from 10 provincial and territorial nursing associations and colleges, independent registered nurse members from Ontario and Quebec and retired registered nurses from across the country. The CNA advances the practice and profession of nursing to improve health outcomes and strengthen Canada's publicly funded, not-for-profit health system. The CNA advocates for many health-related issues, including dementia care. The CNA has provided recommendations to the federal government about dementia in Canada and works to use the nursing perspective to help shape public policy.
CNA recognizes the contributions of nurses to the care of Canada's aging population. CNA offers gerontological nursing certification and recently published a Choosing Wisely Canada nursing list, both of which address dementia care. CNA will continue to work to advance dementia care and will support the work of the federal government.
Dementia Alliance International
Dementia Alliance International (DAI) is a registered not-for-profit organization, and provides a global voice of dementia. Eight people diagnosed with dementia from 3 countries established DAI in 2014. It now has members in 49 countries, and it continues to be an organization exclusively for people diagnosed with dementia, working as an advocacy and support group of, by and for people with dementia. DAI's global work helps to provide a unified voice of collaboration and cooperation with other international organizations such as Alzheimer's Disease International, the Conference of State Parties, the United Nations (UN) and the World Health Organization (WHO) for a human rights approach to dementia. DAI advocates for individual autonomy for people with dementia, and for proactive disability assessment and support, aligned to the Convention on the Rights of People with Disabilities. It is 1 of 14 founding members of the Global Rehabilitation Alliance, which was launched at the World Health Assembly in 2018. DAI promotes education and awareness about dementia toward reducing stigma and discrimination and to improve the quality of the lives of people with dementia. This organization is also heavily involved with international UN and WHO working groups and committees, and produces reports about dementia-related topics. DAI hosts a monthly webinar series, “A Meeting of the Minds”, with international speakers on topics relevant to the dementia community. DAI also continues to provide support through its online peer-to-peer support groups, online cafes and other meetings. Its activities remain free for all people with dementia.
Health Standards Organization and Accreditation Canada
Health Standards Organization (HSO) develops world-class standards, innovative assessment programs and quality improvement support in the form of toolkits, consulting and training. HSO works with accreditation bodies, governments, patients, health and social service providers, researchers and associations.
Accreditation Canada (AC), an affiliate of HSO, delivers HSO's assessment programs to care providers such as health regions, long-term care, mental health and addictions, primary care, community care, residential seniors care and hospitals.
AC and HSO are not-for-profit organizations and deliver services in over 10,000 locations in 38 countries in every part of the health ecosystem. The team includes 200+ staff and more than 1,000 specialized surveyors, faculty and technical committee members. Both organizations are unified by the ambition to unleash the power and potential of people around the world who share the passion for achieving quality health services for all.
Heart & Stroke
Heart & Stroke is dedicated to reducing the burden of heart disease, stroke and vascular cognitive impairment. It is a leading funder of life-saving research, including breakthroughs such as heart transplant surgery and a revolutionary stroke treatment. The link between heart conditions, stroke and dementia is profound. There is an imperative for aggressive prevention to reduce the incidence of dementia. In response, Heart & Stroke funded a landmark study, called the Pure-Mind study, which is the first in Canada to look at strokes and dementia at a population level. This work will help identify people in midlife who might be at risk for memory and thinking problems later in life, and potentially prevent those problems from happening. In addition, the 2019 Heart & Stroke Report (PDF) on the connections between these conditions calls for policies that enable and support healthy environments, such as built environments that promote physical activity.
Neurological Health Charities Canada
Neurological Health Charities Canada (NHCC) is a coalition of neurological health charities that represent people with brain diseases, disorders and injuries in Canada. It provides leadership in advancing new opportunities for collaboration regarding advocacy, education and research to improve the quality of life for people affected by brain conditions. NHCC recognizes that dementia can be caused by a number of brain conditions and that research, health care and policy responses must be flexible to meaningfully serve the largest number of Canadians living with dementia. NHCC believes public education and awareness activities must be expanded to dispel stigma for people living with all types of dementia. NHCC works with its member organizations to promote awareness, education, research and services for all Canadians affected by brain conditions.
Ontario Dementia Advisory Group
Ontario Dementia Advisory Group (ODAG) is a group of people living with dementia in Ontario formed with the purpose of influencing policies, practices, and people to ensure that they, people living with dementia, are included in every decision that affects their lives. ODAG is involved in many ways to advocate for dementia care such as appearing as a witness before Canada's Standing Senate Committee on Social Affairs, Science and Technology on its study on dementia in Canadian society and playing a key role in Ontario's dementia strategy by being on its many planning groups. It provides education through webinars, interviews, submissions and presentations highlighting human rights for people living with dementia, rehabilitation, stigma and living well with dementia.
Speech-Language & Audiology Canada
Speech-Language & Audiology Canada (SAC) is a national organization that supports and represents speech-language pathologists, audiologists and communication health assistants inclusively. Through this support, they champion the needs of people with communication disorders and help ensure all people of Canada achieve optimal communication health. Speech, language, communication, swallowing, hearing and balance disorders are prevalent in people living with dementia. As such, speech-language pathologists and audiologists are integral to achieving optimal care and quality of life for people living with dementia and, in turn, their families and caregivers. In 2017 SAC released a position statement on the role of the professions in dementia care. Last year, SAC prepared an evidence-informed submission: Speech-Language & Audiology Canada (SAC): Submission to the Public Health Agency of Canada to Inform the National Dementia Strategy. SAC continues to advocate on this issue.
Weston Brain Institute
The Weston Brain Institute (WBI) funds translational research on prevention and treatment strategies for brain diseases of aging such as Alzheimer's and other forms of dementia. It addresses gaps and challenges in scientific research by supporting high-risk, high-reward projects while leveraging world-class business and scientific expertise, and tries to drive innovation in funding processes. Projects range from target validation to Phase 2 clinical trials, and can be on treatments directly, or tools such as biomarkers that help other researchers speed up treatment development. WBI commits approximately $10 million each year to projects led by Canadian-based researchers through a range of programs, ranging from $200,000 Rapid Response grants to $20 million Big Ideas grants. Recent changes to programs include modifiable risk factors and lifestyle interventions (e.g., diet, exercise) becoming eligible for funding, and reducing the amount of grant management for Rapid Response grants.
World Dementia Council
The World Dementia Council (WDC) helps change the lives of people with dementia by securing change internationally, working with international governmental and non-governmental organizations. The role of the WDC is to challenge and support international governmental organizations to work toward developing therapies for dementia. The WDC enacts change through global advocacy, global leadership and global networks. It advocates for an international effort to collaborate to defeat dementia, provides leadership by developing evidence of best practices through hosting conferences and performing research, and builds global collaborative networks to share common goals and targets.
World Health Organization
The World Health Organization (WHO) is made up of 194 member-state countries that pledge to work toward global targets on public health. The WHO works worldwide to promote health, keep the world safe, and serve the vulnerable. Dementia is one its major focuses and the WHO has recently released its Global Action Plan on the Public Health Response to Dementia (2017-2025) which signals an important step forward in achieving physical, mental and social wellbeing for people living with dementia, caregivers and families. The plan's vision is of a world in which dementia is prevented and people living with dementia and caregivers receive the care and support they need to live a life with meaning and dignity.
Appendix D: Engaging on dementia: learning about challenges, opportunities and solutions
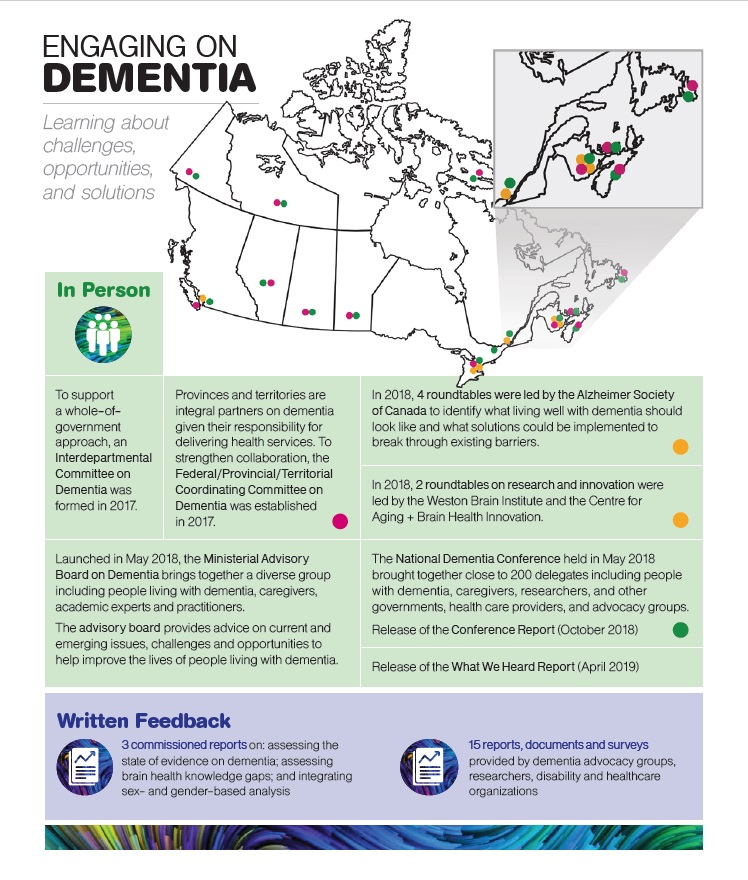
Text description - Engaging on Dementia
This image explains the ways in which Canadians were engaged in the development of this strategy.
The title "Engaging on Dementia: Learning about challenges opportunities and solutions" appears at the top along with a map of Canada which shows the places where engagements happened or where people who participated in engagements live. The map shows that there were roundtables led by the Alzheimer Society in Vancouver, Montreal, Saint John and Fredericton, and that the roundtables led by the Weston Brain Institute and the Centre for Aging and Brain Health Innovation were held in Toronto.
The map shows that there were participants for the National Dementia Conference from all the provinces and territories. The map shows that there are members of the Federal/Provincial/Territorial Coordinating Committee on Dementia from: Yukon, Northwest Territories, Nunavut, British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, New Brunswick, Nova Scotia, PEI and Newfoundland.
Below the map is a description of the In Person Engagement activities. These activities are described in boxes with a green background. From left to right they read:
- To support a whole-of-government approach, an Interdepartmental Committee on Dementia was formed in 2017.
- Provinces and territories are integral partners on dementia given their responsibility for delivering health services. To strengthen collaboration, the Federal/Provincial/Territorial Coordinating Committee on Dementia was established in 2017.
- In 2018, 4 roundtables were led by the Alzheimer Society of Canada to identify what living well with dementia should look like and what solutions could be implemented to break through existing barriers.
- In 2018, 2 roundtables on research and innovation were led by the Weston Brain Institute and the Centre for Aging and Brain Health Innovation.
- Launched in May 2018, the Ministerial Advisory Board on Dementia brings together a diverse group including people living with dementia, caregivers, academic experts and practitioners. The advisory board provides advice on current and emerging issues, challenges and opportunities to help improve the lives of people living with dementia.
- The National Dementia Conference held in May 2018 brought together close to 200 delegates including people with dementia, caregivers, researchers, and other governments, health care providers, and advocacy groups. Release of the Conference Report (October 2018).
- Release of the What We Heard Report (April 2019).
Across the bottom of the image is a description of the Written Feedback that was received for the development of this strategy. This feedback is described as follows:
- 3 commissioned reports on: assessing the state of evidence on dementia; assessing brain health knowledge gaps; and integrating sex-and gender-based analysis.
- 15 reports, documents and surveys provided by dementia advocacy groups, researchers, disability and healthcare organizations.
Appendix E: Glossary
For the purpose of this strategy, the following definitions are used.
- Advance care planning:
- A process of reflecting on personal values and having discussions with your substitute decision maker about the care that you would want to receive should you become unable to make decisions for yourself.
- Age-friendly communities:
- In an age-friendly community, the policies, services and structures related to the physical and social environment are designed in ways that allow seniors to be involved and active. In other words, the community is responsive to vulnerable groups' need to live safely and stay involved in their communities. There are 8 domains through which communities can become more age-friendly: housing, transportation, outdoor spaces and buildings, social participation, respect and social inclusion, civic participation and employment, communication and information, and community support and health services.
- Alternate level of care:
- The designation given by a physician to a patient who is occupying a bed in a hospital who no longer needs the same level of resources or services provided in that particular care setting (e.g. may no longer need treatment or hospital care) but still requires some form of care, such as in a long-term care home or home care. These people must wait for a space to become available in a setting that provides the appropriate care.
- Assisted living:
- An establishment that provides accommodation and care for older or disabled persons who need support to live independently, but do not need nursing care. Residents are provided with assistance with meals, laundry, and related personal care.
- Assistive technology:
- An umbrella term used to describe any device or system that allows individuals to perform tasks they would otherwise be unable to do on their own. Assistive technologies can increase the ease and safety with which daily tasks are performed.
- Basic or biomedical research:
- Research that aims to understand, at the cellular level, the changes occurring in the body and why they are occurring.
- Canadian:
- A Canadian refers to a person living in Canada.
- Care:
- Care takes place across a variety of settings: in the home and/or community, and in primary, acute, or long-term care settings.
- Care provider:
- A person who provides care and support to a person with dementia, in a paid or unpaid role. Includes, but is not limited to, the following groups:
- Caregiver:
- A caregiver is defined as a person who provides care and support to a person with dementia, and who is not a paid care professional or personal care worker. A caregiver is likely to be a relative, close friend, neighbour or volunteer. Support provided by a caregiver may include assisting with the activities of daily living and helping with advance care planning.
- Developmental service worker:
- Provides support to individuals who have intellectual or developmental disabilities. Support can be provided in homes, at work, in schools and to families.
- First responder:
- A person who goes immediately to the scene of an accident or emergency to provide assistance, and is often the first to provide care. First responders include police, paramedics, and/or firefighters.
- Health professional:
- Includes but is not limited to, physicians (including family doctors and specialists such as psychiatrists and geriatricians), nurse practitioners, nurses, social workers, psychologists, chaplains, pharmacists, and physical or occupational therapists.
- Personal care worker (PCW):
- A paid caregiver who assists people with daily personal care needs that may arise from the effects of aging, injury or illness. PCWs may work in private homes, assisted living homes, and long-term care homes. PCWs in home care or long-term care may be referred to as health care aides, home support workers, personal support workers, or attendants and their work is mostly unregulated in Canada.
- Clinical practice:
- Any work undertaken by a health professional, such as a physician or nurse, that relates to the care of a patient.
- Cognitive impairment:
- Challenges associated with memory, language, thinking or judgement.
- Community-based care:
- The blend of health and social services provided to an individual or family in his/her place of residence and/or community to minimize the effects of illness and disability.
- Culturally appropriate care:
- Involves giving consideration to a patient's cultural background, personal experiences and norms.
- Culturally safe care:
- Involves paying attention to the cause of health and health care inequities, by developing an ongoing personal practice of critical self-reflection, and by paying attention to how social and historical contexts shape health and health care systems, power and privilege, especially as these relate to Indigenous peoples.
- Dementia:
- Dementia is an umbrella term used to describe a set of symptoms affecting brain function that are caused by neurodegenerative and vascular diseases or injuries. It is characterized by a decline in cognitive abilities such as memory; awareness of person, place, and time; language, basic math skills; judgement; and planning. Dementia can also affect mood and behaviour. As a chronic and progressive condition, dementia can significantly interfere with the ability to maintain activities of daily living, such as eating, bathing, toileting and dressing. Alzheimer's disease, vascular disease and other types of disease all contribute to dementia. Other common types of dementia include Lewy body dementia, frontotemporal dementia and mixed dementias. In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease.Footnote 104
- Dementia-inclusive communities:
- Communities that allow people living with dementia and caregivers to optimize their health and wellbeing; live as independently as possible; be understood and supported; safely navigate and access their local communities; and maintain their social networks.
- Evidence-based:
- The thorough, clear and careful use of existing evidence, for example, in developing guidelines, implementing interventions and making decisions about the types of care and therapies that an individual receives.
- Evidence-informed:
- Emphasizes flexibility regarding the nature of the evidence and its use. It implies that many different types of evidence are needed and used to support decisions and using the right evidence that matches the context.
- Guidelines:
- Evidence- or consensus-based information or recommendations intended to support a higher-quality result. Guidelines may be followed by care providers interacting with people living with dementia and can encompass various aspects of care including, for example, prevention, diagnosis and treatment.
- Health equity:
- Achieved when everyone has an equal opportunity to reach their fullest health potential regardless of factors such as social class, gender, or ethnicity.
- Health innovation:
- New and/or improved health policies, systems, products and technologies, and delivery methods designed to improve people's health and wellbeing. Health innovation responds to unmet health needs by creating new ways of thinking and working with a focus on the needs of person being served. Health innovation can occur in preventive, promotive, curative and rehabilitative and/or assistive care.
- Home care services:
- Assistance such as nursing and personal care provided to people who have physical health problems, to support them to live independently in the community. These services often prevent or delay the need for care in institutions such as hospitals or long-term care homes. Home care clients often benefit from community services such as Meals on Wheels, and informal care given by family and friends.
- Human rights:
- Includes the right to life and liberty, freedom from slavery and torture, freedom of opinion and expression, work and education, and many more. Human rights are inherent to all human beings, regardless of race, sex, nationality, ethnicity, language, religion or any other social status.
- Hypertension:
- A medical condition in which the blood pressure in the arteries is continuously elevated; also referred to as high blood pressure.
- Incidence:
- The rate of occurrence of new disease cases during a period of time (new cases).
- Intervention:
- An activity or set of activities aimed at modifying a process, course of action or sequence of events, in order to change one or several characteristics such as performance and/or expected outcome.
- Knowledge translation:
- Adapting the learnings from research into easy to understand information, best practices and tools, then sharing this information widely with patients, caregivers, clinicians, other researchers and governments so that it can be used to improve clinical practice, health policy and the quality of life of people living with dementia and caregivers.
- Long-term care:
- In general, long-term care provides living accommodation for people who require supervised care 24 hours a day, 7 days a week, including professional health services, personal care, and services such as meals, laundry and housekeeping.
- Multisectoral collaboration:
- Collaboration of different groups, such as governments, nongovernmental organizations, the private for-profit sector, and academia.
- Palliative care:
- "A type of care that can be offered along the full time continuum of any life-limiting illness, including bereavement of family, friends and caregivers. It includes services such as pain and symptom management, addresses psychological and spiritual concerns, supports family and caregivers, and enhances quality of life. It is provided by primary health care providers, disease specialists, and palliative care specialists."Footnote 105
- Patient:
- A person seeking health care and attention within the health system.
- Person-centred:
- An approach to the planning and delivery of health care founded on mutually beneficial partnerships among care providers and the people receiving care. Person-centred care is respectful of, and responsive to, the preferences, needs and values of the care recipient.
- Prevalence:
- the proportion of the population that has the disease during a period of time or at a specific point in time (existing cases). This can indicate how widespread the disease is.
- Prevention:
- Actions taken to promote and preserve health and to reduce the chance of developing dementia. Prevention activities can include the following:
- Primary prevention:
- Protection of health through personal and community-wide efforts. Primary prevention includes informing individuals of measures to take to prevent the development of dementia (e.g. healthy diet and exercise).
- Secondary prevention:
- Involves focused activities that lead to early detection (diagnostics) and timely treatment of dementia.
- Primary care:
- Basic or general health care provided at the point where an individual first seeks assistance from the medical care system, usually delivered by a physician. It is the basis for referrals to secondary- and tertiary-level care.
- Protective factors:
- Factors associated with a reduced chance of developing dementia. They include healthy lifestyle, social, economic, biological, behavioural and environmental influences.
- Public private partnership (P3):
- A contractual arrangement between public and private sectors in which mutual benefits are sought.
- Quality of life:
- The ability of individuals to do the things they value, such as maintain their physical health, mental wellbeing, level of independence, social relationships, and personal beliefs.
- Risk factors:
- Factors associated with an increased chance of developing dementia; they include lifestyle, social, economic, biological, behavioural and environmental influences.
- Modifiable risk factors:
- Factors that can be changed which reduce the risk of developing dementia, such as unhealthy eating, physical inactivity, and tobacco use.
- Non-modifiable risk factors:
- Factors that cannot be changed which affects the risk of developing dementia, such as an inherited trait (genetics).
- Standard of care:
- Refers to informal or formal guidelines generally accepted in the medical community regarding the approach to care, including diagnosis and treatment. Standards of care are sometimes called best practices and may vary across settings.
- Stakeholders:
- Individuals and organizations who have a shared interest through their involvement in a program, or may be affected by the program.
- Stigma:
- A negative stereotype often influenced by public attitudes, misconceptions and fear. Stigmatizing language and behaviours related to dementia may include: making assumptions about a person's abilities; ageism or implying that dementia is a normal part of aging; and dementia-related jokes.
- Supports:
- Types of support for people living with dementia and caregivers that may include, but are not limited to, assistance with activities of daily living, financial assistance, information and training, and assistive devices.
- Surveillance:
- Ongoing monitoring and collection of data to further understand dementia and other areas of public health.
- Therapy:
- Any intervention that aims to rehabilitate, provide positive social adjustment and improve quality of life.
Endnotes
- Footnote 1
-
Quebec did not participate in the Federal Provincial Territorial Coordinating Committee on Dementia as it does not participate in a national strategy in an area within its exclusive jurisdiction. However, it has shared information and best practices with the federal government which are found in this document.
- Footnote 2
-
Throughout this document the term 'caregivers' will be used to refer to this group.
- Footnote 3
-
Public Health Infobase. Canadian chronic disease surveillance system data on dementia, excluding Saskatchewan and Yukon. Government of Canada. 2018; https://infobase.phac-aspc.gc.ca/CCDSS-SCSMC/data-tool/?l=eng&HRs=00&DDLV=16&DDLM=ASIR&CBVS=on&1=M&2=F&DDLFrm=1999&DDLTo=2012&=10&VIEW=0
- Footnote 4
-
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian chronic disease surveillance system. Government of Canada. 2017; http://publications.gc.ca/collections/collection_2018/aspc-phac/HP35-84-2017-eng.pdf
- Footnote 5
-
World Health Organization. Towards a dementia plan: a WHO guide. World Health Organization. 2018; https://apps.who.int/iris/bitstream/handle/10665/272642/9789241514132-eng.pdf?ua=1
- Footnote 6
-
Standing Senate Committee on Social Affairs, Science and Technology. Dementia in Canada: A national strategy for dementia-friendly communities. 2016; https://sencanada.ca/content/sen/committee/421/SOCI/Reports/SOCI_6thReport_DementiaInCanada-WEB_e.pdf
- Footnote 7
-
Public Health Infobase. Canadian chronic disease surveillance system data on dementia, excluding Saskatchewan and Yukon. Government of Canada. 2018; https://infobase.phac-aspc.gc.ca/CCDSS-SCSMC/data-tool/?l=eng&HRs=00&DDLV=16&DDLM=ASIR&CBVS=on&1=M&2=F&DDLFrm=1999&DDLTo=2012&=10&VIEW=0
- Footnote 8
-
Clow B. A narrative review of sex, gender, diversity and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 9
-
Wong SL, Gilmour H and Ramage-Morin PL. Alzheimer's disease and other dementias in Canada. Statistics Canada. 2016; https://www150.statcan.gc.ca/n1/en/pub/82-003-x/2016005/article/14613-eng.pdf?st=gwU3mB_V
- Footnote 10
-
Clow B. A narrative review of sex, gender, diversity and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 11
-
Canadian Home Care Association. Informing the national strategy for Alzheimer's disease and other dementias: National survey findings. Canadian Home Care Association. 2018; www.virtualhospice.ca/Assets/CHCA_Survey_Report-_Informing_ the_National_Strategy_for_Alzheimers%20-%202018_20180720151139.pdf
- Footnote 12
-
Public Health Agency of Canada. Mapping Connections: An understanding of neurological conditions in Canada. Government of Canada. 2014; https://www.canada.ca/en/public-health/services/reports-publications/mapping-connections-understanding-neurological-conditions.html
- Footnote 13
-
World Health Organization. Dementia: Key facts. World Health Organization. 2017; https://www.who.int/news-room/fact-sheets/detail/dementia
- Footnote 14
-
"Supports" in this document refers to a variety of ways that support can be provided to people living with dementia and caregivers such as assistance with activities of daily living, financial assistance, information and training, and assistive devices.
- Footnote 15
-
Savica R and Petersen RC. Prevention of dementia. The Psychiatric Clinics of North America. 2011; 34(1) 127-45. https://www.ncbi.nlm.nih.gov/pubmed/21333844
- Footnote 16
-
Natural Resource Canada. Quality of life - social environment index. Government of Canada. 2010; 6(6779). https://open.canada.ca/data/en/dataset/eed6a7cf-8893-11e0-bb58-6cf049291510
- Footnote 17
-
Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 - Designing healthy living. Government of Canada. 2018; https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 18
-
Nordström A and Nordström P. Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study. PLoS Medicine. 2018; 15(1). https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002496
- Footnote 19
-
Vickland V, et al. A computer model of dementia prevalence in Australia: Foreseeing outcomes of delaying dementia onset, slowing disease progression, and eradicating dementia types. Dementia and Geriatric Cognitive Disorders. 2010; 29(2):123-30. https://www.ncbi.nlm.nih.gov/pubmed/20145398
- Footnote 20
-
Lewis F, et al. The trajectory of dementia in the UK - Making a difference. Alzheimer's Research UK. 2014; https://www.alzheimersresearchuk.org/wp-content/uploads/2015/01/OHE-report-Full.pdf
- Footnote 21
-
Vickland V, et al. Modelling the impact of interventions to delay the onset of dementia in Australia. Alzheimer's Australia. 2012; https://www.dementia.org.au/files/201212_NAT_AAnumberedPub_Paper30final.pdf
- Footnote 22
-
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017; https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-highlights-canadian-chronic-disease-surveillance.html
- Footnote 23
-
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017; https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-highlights-canadian-chronic-disease-surveillance.html
- Footnote 24
-
Livingston G, et al. Dementia prevention, intervention, and care. The Lancet. 2017; 390: 2673-734. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31363-6.pdf
- Footnote 25
-
Schwarzinger M, et al. Contribution of alcohol use disorders to the burden of dementia in France 2008-13: A nationwide retrospective cohort study. The Lancet. 2018; (3)3. https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(18)30022-7/fulltext
- Footnote 26
-
Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 - Designing healthy living. Government of Canada. 2018; https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 27
-
Livingston G, et al. Dementia prevention, intervention, and care. The Lancet. 2017; 390: 2673-734. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31363-6.pdf
- Footnote 28
-
Ngandu T, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. The Lancet. 2015; 385(9984) 2255-63. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60461-5/fulltext
- Footnote 29
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 30
-
Ngandu T, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. The Lancet. 2015; 385(9984) 2255-63. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60461-5/fulltext
- Footnote 31
-
Beason-Held LL, et al. Changes in brain function occur years before the onset of cognitive impairment. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2013; 33(46), 18008–014. www.jneurosci.org/content/ jneuro/33/46/18008.full.pdf
- Footnote 32
-
Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 - Designing healthy living. Government of Canada. 2018; https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 33
-
Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 - Designing healthy living. Government of Canada. 2018; https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 34
-
Hilmers A, Hilmers DC and Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health. 2012; 102(9), 1644-54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3482049/
- Footnote 35
-
Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 - Designing healthy living. Government of Canada. 2018; https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Footnote 36
-
World Health Organization. Global age-friendly cities: A guide. World Health Organization. 2007; https://apps.who.int/iris/bitstream/handle/10665/43755/9789241547307_eng.pdf;jsessionid=D74A47B2D68649A4DCD98936FEA73B81?sequence=1
- Footnote 37
-
The G8 was made up of industrialized nations of Canada, France, Germany, Italy, Japan, Russia, the United Kingdom and the United States of America. Annual meetings are held that aim at tackling global problems by discussing big issues and planning what action to take. In 2013, the UK held the presidency and dementia was a key issue addressed.
- Footnote 38
-
World Health Organization. Global action plan on the public health response to dementia 2017 - 2025. World Health Organization. 2017; www.who.int/mental_health/neurology/dementia/action_plan_2017_2025/en/1
- Footnote 39
-
Canadian Dementia Priority Setting Partnership. 2018 Canadian dementia research priorities report. Canadian Dementia Priority Setting Partnership. 2018; https://alzheimer.ca/sites/default/files/2018-01/Dementia%20PSP%20Report%20ENG%20Dec%20Final%20SCREEN_0.pdf
- Footnote 40
-
Shah H, et al. Research priorities to reduce the global burden of dementia by 2025. The Lancet. 2016; 15(12) 1285-94. https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(16)30235-6/fulltext
- Footnote 41
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; p. 57. https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 42
-
Alzheimer's Disease International. The state of the art of dementia research: New Frontiers - World Alzheimer Report 2018. Alzheimer's Disease International. 2018; 8-9. https://www.alz.co.uk/research/world-report-2018
- Footnote 43
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; p. 52. https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 44
-
Masopust J, et al. Treatment of behavioral and psychological symptoms of dementias with psychopharmaceuticals: A review. Neuropsychiatric Disease and Treatments. 2018; 1211-20. https://www.ncbi.nlm.nih.gov/pubmed/29785112
- Footnote 45
-
McDermitt O, et al. Music therapy in dementia: A narrative synthesis systematic review. International Journal of Geriatric Psychiatry. 2012; 28(8) 781-94. https://onlinelibrary.wiley.com/doi/full/10.1002/gps.3895
- Footnote 46
-
Dyer SM, et al. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. International Psychogeriatrics. 2018; 30(3) 295-309. www.cambridge.org/core/services/aop-cambridge-core/content/view/DCA87B8BC78047977CB92427BF3F4FC3/ S1041610217002344a.pdf/an_overview_of_systematic_reviews_of_pharmacological_and_nonpharmacological_ interventions_for_the_treatment_of_behavioral_and_psychological_symptoms_of_dementia.pdf
- Footnote 47
-
Canadian Institutes of Health Research. Strategy for patient-oriented research - Patient engagement framework. Government of Canada. 2014; p. 6. http://www.cihr-irsc.gc.ca/e/documents/spor_framework-en.pdf
- Footnote 48
-
Draper B, et al. Translating dementia research into practice. International Psychogeriatrics. 2009; 21(1) 72-80. https://www.cambridge.org/core/journals/international-psychogeriatrics/article/translating-dementia-research-into-practice/7971965AC3163BBAC383640F2A98D53F
- Footnote 49
-
Public Health Infobase. Canadian chronic disease surveillance system data on dementia from 2015-16, excluding Saskatchewan and Yukon. Government of Canada. 2018; https://infobase.phac-aspc.gc.ca/CCDSS-SCSMC/data-tool/?l=eng&HRs=00&DDLV=16&DDLM=ASIR&CBVS=on&1=M&2=F&DDLFrm=1999&DDLTo=2012&=10&VIEW=0
- Footnote 50
-
Sinha M. Portrait of caregivers, 2012. Statistics Canada. 2013; (1). www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2013001-eng.pdf
- Footnote 51
-
Sinha M. Portrait of caregivers, 2012. Statistics Canada. 2013; (1). www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2013001-eng.pdf
- Footnote 52
-
Public Health Agency of Canada. Inspiring and informing a national dementia strategy for Canada: Conference Report. Government of Canada. 2018; https://www.canada.ca/en/services/health/publications/diseases-conditions/national-dementia-conference-report.html
- Footnote 53
-
Spierer O, et al. Correlation between vision and cognitive function in the elderly: A cross-sectional study. Medicine, 2016; 95(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998246/
- Footnote 54
-
University of North Texas. Hearing aids, auditory training may provide dementia patients with increases in cognitive abilities, UNT study says. University of North Texas. 2016; https://news.unt.edu/news-releases/hearing-aids-auditory-training-may-provide-dementia-patients-increases-cognitive-abili
- Footnote 55
-
Moore A, et al. Fourth Canadian consensus conference on the diagnosis and treatment of dementia: Recommendations for family physicians. Canadian Family Physician.2014; 60(5):433-8. http://www.cfp.ca/content/60/5/433
- Footnote 56
-
Danila O, et al. Prevalence of neurological conditions across the continuum of care based on interRAI assessments. BMC Health Serv Res. 2014; 14(1):1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3906754/
- Footnote 57
-
Gibbard R. Sizing up the challenge: meeting the demand for long-term care in Canada. The Conference Board of Canada. 2017; https://www.conferenceboard.ca/e-library/abstract.aspx?did=9228&AspxAutoDetectCookieSupport=1
- Footnote 58
-
Canadian Institute for Health Information. Dementia and falls. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/dementia-and-falls
- Footnote 59
-
Canadian Institute for Health Information. Dementia in hospitals. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/dementia-across-the-health-system/dementia-in-hospitals
- Footnote 60
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 61
-
Tanuseputro P, et al. Palliative care delivery across health sectors: A population-level observational study. Palliative Medicine. 2017; 31(3): 247-57. https://journals.sagepub.com/doi/full/10.1177/0269216316653524?url_ver=Z39.88-2003&rfr_id=oripercent3Aridpercent3Acrossref.org&rfr_dat=cr_pubpercent3Dpubmed
- Footnote 62
-
Canadian Institute for Health Information. Palliative and end-of-life care. Canadian Institute for Health Information. 2018; https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/palliative-and-end-of-life-care
- Footnote 63
-
Livingston G, et al. Dementia prevention, intervention, and care. The Lancet. 2017; 390: 2673-734. https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31363-6.pdf
- Footnote 64
-
Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care. JAMA. 2006;295(18):2148–2157. https://jamanetwork.com/journals/jama/fullarticle/202837
- Footnote 65
-
Keefe JM, et al. Key issues in human resource planning for home support workers in Canada. Work. 2011; 40(1) 21-8. http://www.msvu.ca/site/media/msvu/Key%20issues%20in%20human%20resource%20planning%20for%20home%20 support%20workers%20in%20Canada.pdf
- Footnote 66
-
Zagrodney K, and Saks M. Personal support workers in Canada: the new precariat? Healthcare Policy. 2017; 13(2):31-9. www.ncbi.nlm.nih.gov/pmc/articles/PMC5749522
- Footnote 67
-
Hoben M, et al. Health of health care workers in Canadian nursing homes and pediatric hospitals: A cross-sectional study. CMAJ Open. 2017; 5(4):791-99. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5741427/
- Footnote 68
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 69
-
Canadian Institute for Health Information. Family doctor preparedness. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/family-doctor-preparedness
- Footnote 70
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 71
-
Canadian Institute for Health Information. Unpaid caregiver challenges and supports. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports
- Footnote 72
-
National Institute on Ageing. Why Canada needs to better care for its working caregivers. National Institute on Ageing. 2018; https://www.ryerson.ca/content/dam/nia/white-papers/working-caregivers.pdf
- Footnote 73
-
Canadian Institute for Health Information. Dementia in Canada. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports
- Footnote 74
-
Tremont G. Family caregiving in dementia. Med Health R I. 2011; 94(2): 36-38; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3487163/
- Footnote 75
-
Canadian Home Care Association. Informing the national strategy for Alzheimer's disease and other dementias: national survey findings. Canadian Home Care Association. 2018; www.virtualhospice.ca/Assets/CHCA_Survey_Report-_Informing_ the_National_Strategy_for_Alzheimers%20-%202018_20180720151139.pdf
- Footnote 76
-
Public Health Agency of Canada, Neurological Health Charities Canada. Mapping connections: An understanding of neurological conditions in Canada - Chapter 2. Government of Canada. 2014; http://www.phac-aspc.gc.ca/publicat/cd-mc/mc-ec/section-2-eng.php.
- Footnote 77
-
Sinha M. Portrait of caregivers, 2012. Statistics Canada. 2013; (1); www150.statcan.gc.ca/n1/pub/89-652-x/89-652- x2013001-eng.pdf
- Footnote 78
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Footnote 79
-
Canadian Institute for Health Information. Unpaid caregiver challenges and supports. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports
- Footnote 80
-
Ontario Agency for Health Protection and Promotion. Health Equity. Public Health Ontario. 2019; https://www.publichealthontario.ca/en/health-topics/health-equity
- Footnote 81
-
Petrasek-MacDonald J, et al. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and risk factors. National Collaborating Centre for Aboriginal Health. 2018; https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf
- Footnote 82
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 83
-
Bourassa C. Addressing the duality of access to healthcare for indigenous communities: racism and geographical barriers to safe care. HealthcarePapers. 2018; 17(3) 6-10. https://www.ncbi.nlm.nih.gov/pubmed/30052180
- Footnote 84
-
Petrasek-MacDonald J, et al. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and risk factors. National Collaborating Centre for Aboriginal Health. 2018; https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf
- Footnote 85
-
National Institute on Aging. Alzheimer's disease in people with down syndrome. U.S. Department of Health & Human Services. 2017; https://www.nia.nih.gov/health/alzheimers-disease-people-down-syndrome
- Footnote 86
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 87
-
University of Hertfordshire. Alzheimer's dementia: what you need to know, what you need to do. University of Hertfordshire. 2019; http://www.intellectualdisability.info/mental-health/articles/alzheimers-dementia-what-you-need-to-know,-what-you-need-to-do
- Footnote 88
-
Heart & Stroke. (Dis)connected: how unseen links are putting us at risk. Report on heart, stroke and vascular cognitive impairment. Heart & Stroke. 2019; https://www.heartandstroke.ca/-/media/pdf-files/canada/2019-report/heartandstrokereport2019.ashx
- Footnote 89
-
The Lancet. Risk factors for dementia. [PDF]. The Lancet. 2017; https://www.thelancet.com/pb/assets/raw/Lancet/infographics/dementia-2017/Risk_factors_for_dementia.pdf
- Footnote 90
-
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017; https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-highlights-canadian-chronic-disease-surveillance.html
- Footnote 91
-
Canadian Institute for Health Information. Dementia in Canada. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/dementia-in-canada-summary
- Footnote 92
-
Statistics Canada. Neurological conditions in institutions. Government of Canada. 2019; https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310046801
- Footnote 93
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 94
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 95
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 96
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 97
-
SAGE. Issues Brief: LGBT and dementia. Diverse Elders Coalition. 2018; https://www.diverseelders.org/resource/issues-brief-lgbt-and-dementia/
- Footnote 98
-
Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report-Addendum.pdf
- Footnote 99
-
SAGE. Issues Brief: LGBT and dementia. Diverse Elders Coalition. 2018; https://www.diverseelders.org/resource/issues-brief-lgbt-and-dementia/
- Footnote 100
-
Garcia LJ, McCleary L, et al. The pathway to diagnosis of dementia for Francophones living in a minority situation. The Gerontologist. 2014; 54(6) 964-75. https://academic.oup.com/gerontologist/article/54/6/964/564464
- Footnote 101
-
Clow B. Narrative review of sex, gender, diversity, and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Footnote 102
-
Canadian Institute for Health Information. Young-onset dementia. Canadian Institute for Health Information. 2019; https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/young-onset-dementia
- Footnote 103
-
Alzheimer Society Canada. Young onset dementia. Alzheimer Society Canada. 2019; https://alzheimer.ca/en/Home/About-dementia/Dementias/young-onset-dementia
- Footnote 104
-
This definition of dementia is based on a combination of commonly used sources.
- Footnote 105
-
Health Canada. Framework for palliative care in Canada. Government of Canada. 2018; https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/palliative-care/framework-palliative-care-canada.html#appf
Bibliography
- Alfakhri AS, Alshudukhi AW, Alqahtani AA, Alhumaid AM, Alhathlol OA, Almojali AI, et al. Depression among caregivers of patients with dementia. Inquiry. 2018; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5798670/
- Alzheimer's Disease International. The state of the art of dementia research: New frontiers –World Alzheimer Report 2018. Alzheimer's Disease International. 2018; 8-9. Available from: https://www.alz.co.uk/research/world-report-2018
- Alzheimer Society Canada. Young onset dementia. Alzheimer Society Canada. 2019; Available from: https://alzheimer.ca/en/Home/About-dementia/Dementias/young-onset-dementia
- Beason-Held LL, Goh JO, An Y, Kraut MA, O'Brien RJ, Ferrucci L, et al. Changes in brain function occur years before the onset of cognitive impairment. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2013; 33(46), 18008–014. Available from: www.jneurosci.org/content/jneuro/33/46/18008. full.pdf
- Bourassa C. Addressing the duality of access to healthcare for indigenous communities: Racism and geographical barriers to safe care. HealthcarePapers. 2018; 17(3) 6-10. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30052180
- Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, Perkins AJ, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care. JAMA. 2006; 295(18):2148–57. Available from: https://jamanetwork.com/journals/jama/fullarticle/202837
- Canadian Academy of Health Sciences. Improving the quality of life and care of persons living with dementia and their caregivers. Canadian Academy of Health Sciences. 2019; Available from: https://www.cahs-acss.ca/wp-content/uploads/2019/01/Report.pdf
- Canadian Dementia Priority Setting Partnership Steering Committee. Canadian dementia research priorities report. Canadian Dementia Priority Setting Partnership. 2018; Available from: https://alzheimer.ca/sites/default/files/2018-01/Dementia%20PSP%20Report%20ENG%20Dec%20Final%20SCREEN_0.pdf
- Canadian Home Care Association. Informing the national strategy for Alzheimer's disease and other dementias: National survey findings. Canadian Home Care Association. 2018; Available from: www.virtualhospice.ca/Assets/CHCA_Survey_Report-_Informing_the_National_Strategy_for_ Alzheimers%20-%202018_20180720151139.pdf
- Canadian Institute for Health Information. Dementia in Canada: Summary. Canadian Institute for Health Information. 2019; Available from: www.cihi.ca/en/dementia-in-canada/how-dementia-impacts-canadians
- Canadian Institute for Health Information. Dementia and falls. Canadian Institute for Health Information. 2019; Available from: https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/dementia-and-falls
- Canadian Institute for Health Information. Dementia in hospitals. Canadian Institute for Health Information. 2019; Available from: https://www.cihi.ca/en/dementia-in-canada/dementia-across-the-health-system/dementia-in-hospitals
- Canadian Institute for Health Information. Family doctor preparedness. Canadian Institute for Health Information. 2019; Available from: https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/family-doctor-preparedness
- Canadian Institute for Health Information. Palliative and end-of-life care. Canadian Institute for Health Information. 2018; Available from: https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/palliative-and-end-of-life-care
- Canadian Institute for Health Information. Unpaid caregiver challenges and supports. Canadian Institute for Health Information. 2019; Available from: https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports
- Canadian Institute for Health Information. Young-onset dementia. Canadian Institute for Health Information. 2019; Available from: https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/young-onset-dementia
- Canadian Institutes of Health Research. Strategy for patient-oriented research - Patient engagement framework. Government of Canada. 2014; Available from: http://www.cihr-irsc.gc.ca/e/documents/spor_framework-en.pdf
- Chertkow H. Canadian consortium on neurodegeneration in aging. The CCNA Phase II (2019-2024). Internal document. 2019.
- Clow B. A narrative review of sex, gender, diversity and equity considerations related to Alzheimer's Disease and other dementias in Canada. 2018.
- Danila O, Hirdes JP, Maxwell CJ, Marrie RA, Patten S, Pringsheim T, and Jetté N. Prevalence of neurological conditions across the continuum of care based on interRAI assessments. BMC Health Serv Res. 2014; 14(1):1. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3906754/
- Department of Health & Human Services. Dementia-inclusive communities. State Government of Victoria, Australia. 2018; Available from: https://www2.health.vic.gov.au/ageing-and-aged-care/wellbeing-and-participation/age-friendly-victoria/dementia-inclusive-communities
- Draper B, Low LF, Withall A, Vickland V, et al. Translating dementia research into practice. International Psychogeriatrics. 2009; 21(1) 72-80. Available from: https://www.cambridge.org/core/journals/international-psychogeriatrics/article/translating-dementia-research-into-practice/7971965AC3163BBAC383640F2A98D53F
- Dyer SM, Harrison SL, Laver K, Whitehead C and Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. International Psychogeriatrics. 2018; 30(3) 295-309. Available from:
www.cambridge.org/core/services/ aop-cambridge-core/content/view/DCA87B8BC78047977CB92427BF3F4FC3/S1041610217002344 .pdf/ an_overview_of_systematic_reviews_of_pharmacological_and_nonpharmacological_interventions_for_the_ treatment_of_behavioral_and_psychological_symptoms_of_dementia.pdf - Garcia LJ, McCleary L, et al. The pathway to diagnosis of dementia for Francophones living in a minority situation. The Gerontologist. 2014; 54(6) 964-75. Available from: https://academic.oup.com/gerontologist/article/54/6/964/564464
- Gibbard R. Sizing up the challenge: Meeting the demand for long-term care in Canada. The Conference Board of Canada. 2017; Available from: https://www.conferenceboard.ca/e-library/abstract.aspx?did=9228&AspxAutoDetectCookieSupport=1
- Health Canada. Framework on palliative care in Canada. Government of Canada. 2018; Available from: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/palliative-care/framework-palliative-care-canada.html
- Heart & Stroke. (Dis)connected: how unseen links are putting us at risk. Report on heart, stroke and vascular cognitive impairment. Heart & Stroke. 2019; Available from: https://www.heartandstroke.ca/-/media/pdf-files/canada/2019-report/heartandstrokereport2019.ashx
- Hilmers A, Hilmers DC and Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health. 2012; 102(9), 1644-54. Available from: www.ncbi. nlm.nih.gov/pmc/articles/PMC3482049/
- Hoben M, Knopp-Sihota JA, Nesari M, Chamberlain SA, Squires JE, Norton PG, et al. Health of health care workers in Canadian nursing homes and pediatric hospitals: A cross-sectional study. CMAJ Open. 2017; 5(4):791-99. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5741427/
- Keefe JM, Knight L, Martin-Matthews A, and Légaré J. Key issues in human resource planning for home support workers in Canada. Work. 2011; 40(1) 21-8. Available from: https://www.msvu.ca/site/media/msvu/Key%20issues%20in%20human%20resource%20planning%20for%20home%20support%20workers%20in%20Canada.pdf
- Lewis F, Schaffer S, Sussex J, O'Neill P, and Cockcroft L. The trajectory of dementia in the UK – Making a difference. Alzheimer's Research UK. 2014; Available from: https://www.alzheimersresearchuk.org/wp-content/uploads/2015/01/OHE-report-Full.pdf
- Livingston G, Sommerlad A, Orgeta V, Costafreda S, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. The Lancet. 2017; 390: 2673–734. Available from: https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)31363-6.pdf
- Masopust J, Protopopova D, Valis M, Pavelek Z and Kilmova B. Treatment of behavioral and psychological symptoms of dementias with psychopharmaceuticals: A review. Neuropsychiatric Disease and Treatments. 2018; 1211-20. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29785112
- McDermitt O, Crellin N, Mette Ridder H and Orrell M. Music therapy in dementia: A narrative synthesis systematic review. International Journal of Geriatric Psychiatry. 2012; 28(8) 781-94. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/gps.3895
- Moore A, Patterson C, Lee L, Vedel I, and Bergman H. Fourth Canadian consensus conference on the diagnosis and treatment of dementia: Recommendations for family physicians. Canadian Family Physician.2014; 60(5):433–8. Available from: http://www.cfp.ca/content/60/5/433
- National Institute on Aging. Alzheimer's disease in people with Down syndrome. U.S. Department of Health & Human Services. 2017; Available from: https://www.nia.nih.gov/health/alzheimers-disease-people-down-syndrome
- National Institute on Ageing. Why Canada needs to better care for its working caregivers. Toronto, ON: National Institute on Ageing White Paper. 2018; Available from: https://www.ryerson.ca/content/dam/nia/white-papers/working-caregivers.pdf
- Natural Resource Canada. Quality of life - Social environment index. Government of Canada. 2010; 6(6779). Available from: https://open.canada.ca/data/en/dataset/eed6a7cf-8893-11e0-bb58-6cf049291510
- Ngandu T, Lehtisalo J, Soloman A, Levalahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. The Lancet. 2015; 385(9984) 2255-63. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60461-5/fulltext
- Nordström A and Nordström P. Traumatic brain injury and the risk of dementia diagnosis: A nationwide cohort study. PLoS Medicine. 2018; 15(1). Available from: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002496
- Ontario Agency for Health Protection and Promotion. Health Equity. Public Health Ontario. 2019; Available from: https://www.publichealthontario.ca/en/health-topics/health-equity
- Petrasek-MacDonald J, Ward V and Halseth R. Alzheimer's disease and related dementias in indigenous populations in Canada: Prevalence and risk factors. National Collaborating Centre for Aboriginal Health. 2018; Available from: https://www.ccnsa-nccah.ca/docs/emerging/RPT-Alzheimer-Dementia-MacDonald-Ward-Halseth-EN.pdf
- Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017; Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-highlights-canadian-chronic-disease-surveillance.html
- Public Health Agency of Canada. Inspiring and informing a national dementia strategy for Canada: Conference report. Government of Canada. 2018; Available from: https://www.canada.ca/en/services/health/publications/diseases-conditions/national-dementia-conference-report.html
- Public Health Agency of Canada. Mapping Connections: An understanding of neurological conditions in Canada. Government of Canada. 2014; Available from: https://www.canada.ca/en/public-health/services/reports-publications/mapping-connections-understanding-neurological-conditions.html
- Public Health Agency of Canada. The chief public health officer's report on the state of public health in Canada 2017 – Designing healthy living. Government of Canada. 2018; Available from: https://www.canada.ca/en/public-health/services/publications/chief-public-health-officer-reports-state-public-health-canada/2017-designing-healthy-living.html
- Public Health Infobase. Canadian chronic disease surveillance system data on dementia, excluding Saskatchewan and Yukon. Government of Canada. 2018; Available from: https://infobase.phac-aspc.gc.ca/CCDSS-SCSMC/data-tool/?l=eng&HRs=00&DDLV=16&DDLM=ASIR&CBVS=on&1=M&2=F&DDLFrm=1999&DDLTo=2012&=10&VIEW=0
- SAGE. Issues Brief: LGBT and dementia. Diverse Elders Coalition. 2018; Available from: https://www.diverseelders.org/resource/issues-brief-lgbt-and-dementia/
- Savica R and Petersen RC. Prevention of dementia. The Psychiatric Clinics of North America. 2011; 34(1) 127–45. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21333844
- Schwarzinger M, Pollock BG, Dufouil C and Rehm J. Contribution of alcohol use disorders to the burden of dementia in France 2008-13: A nationwide retrospective cohort study. Lancet. 2018; (3)3. Available from: https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(18)30022-7/fulltext
- Shah H, Albanese E, Duggan C, Rudan I, Langa KM, Carrillo MC, et al. Research priorities to reduce the global burden of dementia by 2025. The Lancet. 2016; 15(12) 1285-94. Available from: https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(16)30235-6/fulltext
- Sinha M. Portrait of caregivers, 2012. Statistics Canada. 2013; (1). Available from: www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2013001-eng.pdf
- Spierer O, Fischer N, Barak A, and Belkin M. Correlation between vision and cognitive function in the elderly: A cross-sectional study. Medicine, 2016; 95(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998246/
- Standing Senate Committee on Social Affairs, Science and Technology. Dementia in Canada: A national strategy for dementia-friendly communities. 2016; Available from: https://sencanada.ca/content/sen/committee/421/SOCI/Reports/SOCI_6thReport_DementiaInCanada-WEB_e.pdf
- Statistics Canada. Neurological conditions in institutions. Government of Canada. 2019; Available from: https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310046801
- Tanuseputro P, Budhwani S, Qing Bai Y and Wodchis WP. Palliative care delivery across health sectors: A population-level observational study. Palliative Medicine. 2017; 31(3): 247–57. Available from: https://journals.sagepub.com/doi/full/10.1177/0269216316653524?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed
- The Lancet. Risk factors for dementia. [PDF]. The Lancet. 2017; Available from: https://www.thelancet.com/pb/assets/raw/Lancet/infographics/dementia-2017/Risk_factors_for_dementia.pdf
- Tremont G. Family caregiving in dementia. Med Health R I. 2011; 94(2): 36–38. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3487163/
- University of Hertfordshire. Alzheimer's dementia: What you need to know, what you need to do. University of Hertfordshire. 2019; Available from: http://www.intellectualdisability.info/mental-health/articles/alzheimers-dementia-what-you-need-to-know,-what-you-need-to-do
- University of North Texas. Hearing aids, auditory training may provide dementia patients with increases in cognitive abilities, UNT study says. University of North Texas. 2016; Available from: https://news.unt.edu/news-releases/hearing-aids-auditory-training-may-provide-dementia-patients-increases-cognitive-abili
- Vickland V, McDonnell G, Werner J, Draper B, Low LF, and Brodaty H. A computer model of dementia prevalence in Australia: Foreseeing outcomes of delaying dementia onset, slowing disease progression, and eradicating dementia types. Dementia and Geriatric Cognitive Disorders. 2010; 29(2):123-30. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20145398
- Vickland V, Morris T, Draper B, Low LF and Brodaty H. Modelling the impact of interventions to delay the onset of dementia in Australia. Alzheimer's Australia. 2012; Available from: https://www.dementia.org.au/files/201212_NAT_AAnumberedPub_Paper30final.pdf
- Wong SL, Gilmour H and Ramage-Morin PL. Alzheimer's disease and other dementias in Canada. Statistics Canada. 2016; Available from: https://www150.statcan.gc.ca/n1/en/pub/82-003-x/2016005/article/14613-eng.pdf?st=gwU3mB_V
- World Health Organization. Current and future long-term care needs. World Health Organization. 2002; Available from: https://www.who.int/chp/knowledge/publications/ltc_needs.pdf
- World Health Organization. Dementia: Key facts. World Health Organization. 2017; Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
- World Health Organization. Global age-friendly cities: A guide. World Health Organization. 2007; Available from: https://apps.who.int/iris/bitstream/handle/10665/43755/9789241547307_eng.pdf;jsessionid=D74A47B2D68649A4DCD98936FEA73B81?sequence=1
- World Health Organization. Global action plan on the public health response to dementia 2017 - 2025. World Health Organization. 2017; Available from: www.who.int/mental_health/neurology/dementia/action_ plan_2017_2025/en/
- World Health Organization. Risk reduction of cognitive decline and dementia: WHO guidelines. World Health Organization. 2019; Available from: https://www.who.int/mental_health/neurology/dementia/guidelines_risk_reduction/en/
- World Health Organization. Towards a dementia plan: A WHO guide. World Health Organization. 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/272642/9789241514132-eng.pdf?ua=1
- Zagrodney K, and Saks M. Personal support workers in Canada: The new precariat? Healthcare Policy. 2017; 13(2):31-9. Available from: www.ncbi.nlm.nih.gov/pmc/articles/PMC5749522