West Nile virus and other mosquito-borne diseases surveillance report: Annual edition 2019
Download in PDF format
(2 MB, 12 pages)
Organization: Public Health Agency of Canada
Date published: August 2023
ISBN: 2816-8038
Cat: HP37-33E-PDF
Pub.: 230016
On this page
- Surveillance highlights
- Introduction
- Methods
- West Nile virus
- California serogroup viruses
- Eastern equine encephalitis virus
- Discussion
- Public health conclusions
- Acknowledgements
- Erratum
- References
Surveillance highlights
West Nile virus (WNV)
- A total of 45 human infections of West Nile virus were reported: 33 clinical cases acquired in Canada, eight travel-associated clinical cases, and four asymptomatic cases.
- 64% of locally-acquired WNV clinical cases were classified as neurological. Two deaths associated with WNV neurological syndrome were reported.
- A lower number of WNV-positive birds, mosquitoes and horses were observed when compared to the previous five years.
Eastern equine encephalitis virus (EEEV)
- Seven equine cases of Eastern equine encephalitis virus were reported.
California serogroup viruses (CSGV)
- Eighteen infections of California serogroup viruses were reported: two infections identified by the National Microbiology Laboratory (NML), and 16 were reported by Quebec.
Introduction
West Nile virus (WNV), Eastern equine encephalitis virus (EEEV), and the California serogroup viruses (CSGV), specifically the Jamestown Canyon and snowshoe hare virus, are known to cause human infection in North America. All four mosquito-borne diseases are endemic in parts of Canada with a 10% increase in incidence observed over last 20 years, largely attributed to climate changeFootnote1. Canada’s endemic mosquito-borne diseases have complex transmission cycles with viruses circulating between specific avian or mammal hosts and competent mosquito vectors. However, a broad range of other animals, including humans and horses, can also be infected. Recognizing that the health of humans is interconnected with that of animals and the environment, mosquito-borne disease surveillance requires a One Health approach. This report therefore integrates findings from human and animal health surveillance, conducted in collaboration with multi-disciplinary health partners, with the goal of achieving optimal human health outcomes.
Methods
West Nile virus has been a nationally notifiable disease since 2003 and human cases in Canada are reported voluntarily to the Public Health Agency of Canada (PHAC) by provincial and territorial health authorities via the Canadian WNV Surveillance Program. Although symptoms of WNV can be severe, they are usually mild, and most individuals may not be aware of their infections. Human infections include both clinical cases and asymptomatic infections. In this report, human cases are classified according to the national surveillance case definition. During spring, summer and fall, blood donations are also routinely screened using a nucleic acid amplification test (NAAT) by Canadian Blood Services and Hema-Quebec using a risk-based approach. Positive blood donors, most commonly asymptomatic, then get reported to provincial/territorial health agencies. Except for Figure 5, cases that reported travel within Canada and internationally, are excluded from overall epidemiological analyses.
Other indicators of WNV activity in Canada include information from animals and mosquitoes. In 2019, information on WNV-positive dead wild birds was largely provided by the Canadian Wildlife Health Cooperative (CWHC); however, some provinces also provide this data directly to the Canadian WNV Surveillance Program. The Canadian Food Inspection Agency (CFIA) provides nationwide data on WNV veterinary cases, while mosquito surveillance data are collected and provided by four participating provinces: Saskatchewan, Manitoba, Ontario, and Québec.
Unlike WNV, CSGV and EEEV infections in humans are not nationally notifiable diseases in Canada, and therefore, the true burden of cases is unknown. Some provincial/territorial laboratory partners perform their own testing and there may be differences among their respective case definitions, which can lead to discrepancies in reported numbers. In addition, when requested by other laboratories, the National Microbiology Laboratory (NML) within PHAC, tests for EEEV and CSGV in patients who present with symptoms consistent with an arboviral infectionFootnote 1.
The findings in this report are subject to several limitations. First, the West Nile virus surveillance system is a passive surveillance system; therefore, it is likely that the actual incidence of WNV infections in humans is under-diagnosed. Moreover, only approximately 20% of WNV infections are symptomatic, therefore it is suspected that many cases would go undetected. Detection and reporting of WNV neurological syndrome are considered more complete than that of WNV non-neurological syndrome. Second, data collection methods and case definitions vary within Canada, leading to challenges with interpretation. Of note, Saskatchewan reports WNV neurological syndrome cases only. In addition, provincial and territorial disease reporting systems may receive updated case information, which can result in differences between what is presented in this report and provincial and territorial reports. This report is based on the latest data provided to PHAC for the 2019 transmission season (data as of: 2020/11/13). Modifications and updates to case information made after this date may not be captured in this report.
West Nile virus
Human case surveillance
A total of 45 WNV human infections were reported to PHAC during the 2019 season. Of these, 33 were locally acquired clinical cases, eight travel associated cases and four asymptomatic cases. The locally acquired clinical cases were reported across four provinces: Ontario (n=17), Québec (n=12), Alberta (n=2) and Manitoba (n=2). The majority of cases were geographically distributed in the southern regions of these provinces (Figure 1). The four asymptomatic infections were reported by Ontario (n=2) and Québec (n=2).
Figure 1. Geographic distribution of West Nile virus human infections (clinical and asymptomatic cases) and positive birds reported in Canada by public health region, 2019
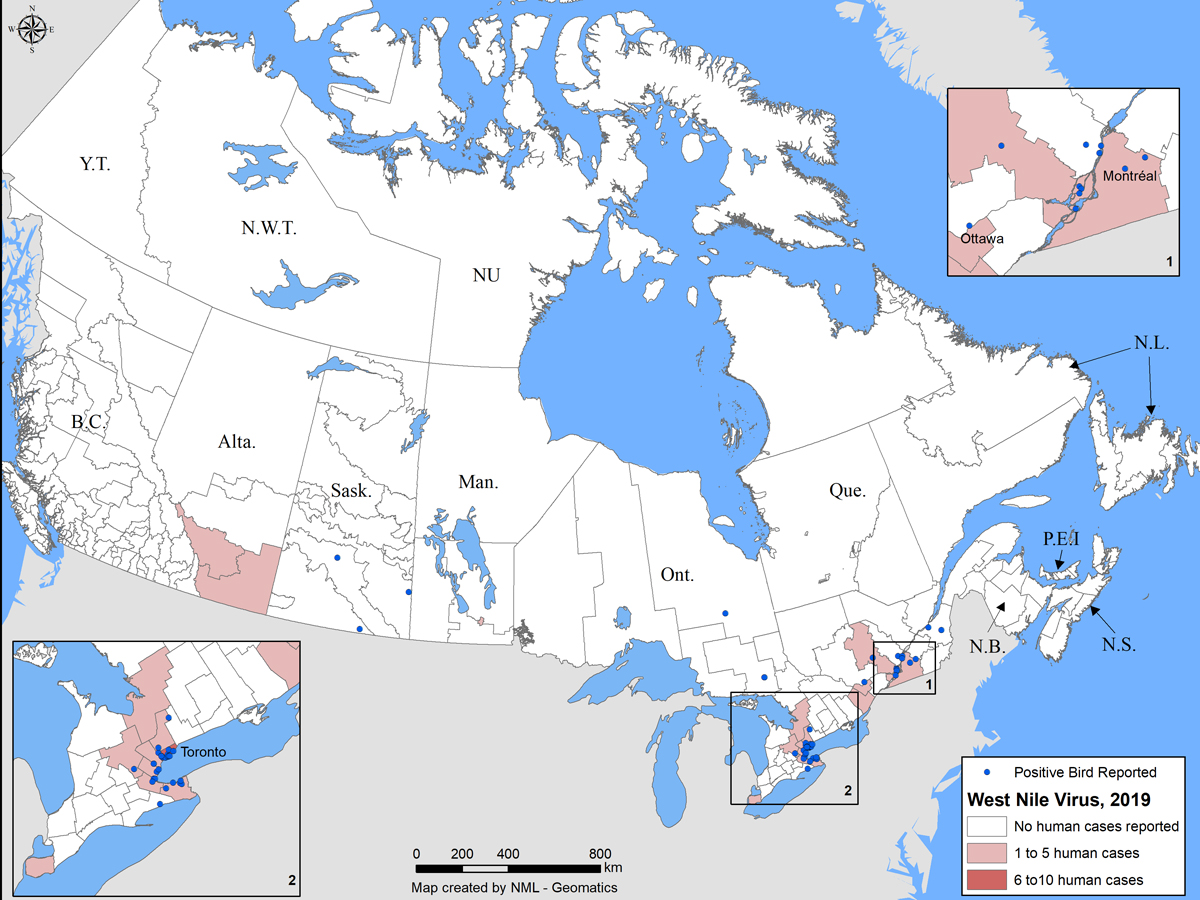
Figure 1 - Text description
This figure shows a map of Canada, indicating distribution of human infections reported across four provinces: Alberta, Manitoba, Ontario and Québec. Furthermore, 46 WNV-positive birds were reported in Saskatchewan, Ontario and Québec.
| Province/Territory | Human Infections (n) | Positive birds (n) |
|---|---|---|
| Alberta | 2 | 0 |
| Saskatchewan | 0 | 3 |
| Manitoba | 2 | 0 |
| Ontario | 19 | 30 |
| Québec | 14 | 12 |
| Total | 37 | 45 |
The earliest onset date for a WNV human case in 2019 was July 3 in Ontario (surveillance week 27). Most (99%) of reported cases occurred with an onset date between surveillance weeks 27 and 41 (early July to mid October), with a peak in early September (Figure 2). Typically, the peak weeks vary from year to year, ranging from week 32 to 36 (early August to early September) (Figure 3). The number of human cases observed in 2019 represents the lowest number of cases reported since 2015 ( Figures 3 and 5).
Figure 2. West Nile virus human infections (clinicalFootnote *) reported by province and episode week in Canada, 2019 from surveillance week 25 to 44Figure 2 Footnote a
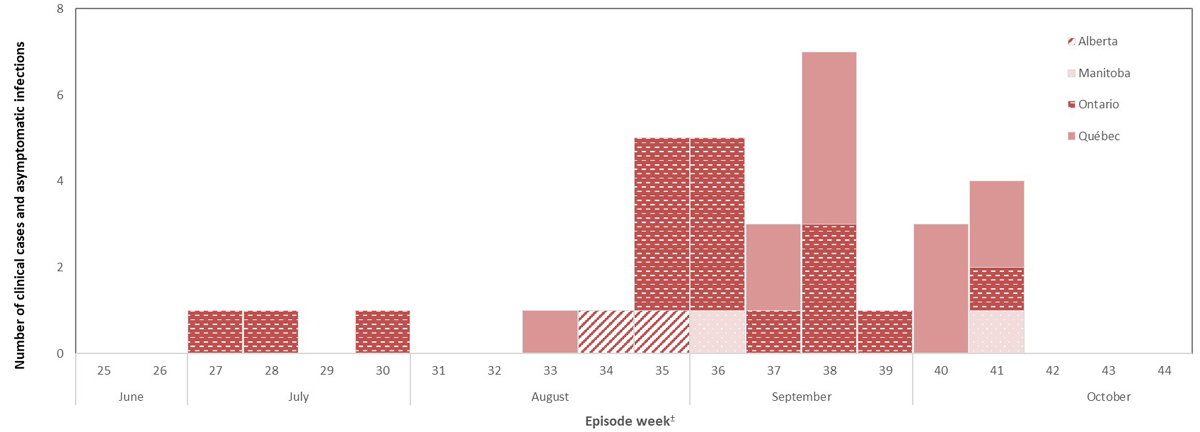
- Footnote 1
-
Saskatchewan’s WNV surveillance system monitors neurological syndrome cases only.
- Footnote 2
-
WNV cases are grouped based on episode date. Episode week is calculated using the earliest available date based on the following hierarchy: symptom onset date, diagnosis date, laboratory sample date or reporting date.
Figure 2 - Text Description
In 2019, between mid-June and end of October, 37 human infections (clinical cases) of West Nile virus were reported to the Public Health Agency of Canada.
| Episode (surveillance) WeekFigure 2 Footnote a | Province | ||||
|---|---|---|---|---|---|
| Ontario | Québec | Alberta | Manitoba | ||
| June | 25 | 0 | 0 | 0 | 0 |
| 26 | 0 | 0 | 0 | 0 | |
| July | 27 | 1 | 0 | 0 | 0 |
| 28 | 1 | 0 | 0 | 0 | |
| 29 | 0 | 0 | 0 | 0 | |
| 30 | 1 | 0 | 0 | 0 | |
| August | 31 | 0 | 0 | 0 | 0 |
| 32 | 0 | 0 | 0 | 0 | |
| 33 | 0 | 1 | 0 | 0 | |
| 34 | 0 | 0 | 1 | 0 | |
| 35 | 4 | 0 | 1 | 0 | |
| September | 36 | 4 | 0 | 0 | 1 |
| 37 | 1 | 2 | 0 | 0 | |
| 38 | 3 | 4 | 0 | 0 | |
| 39 | 1 | 0 | 0 | 0 | |
| October | 40 | 0 | 3 | 0 | 0 |
| 41 | 1 | 0 | 0 | 1 | |
| 42 | 0 | 2 | 0 | 0 | |
| 43 | 0 | 0 | 0 | 0 | |
| 44 | 0 | 0 | 0 | 0 | |
| Total | 17 | 12 | 2 | 2 | |
|
|||||
Figure 3. West Nile virus human infections (clinicalFigure 3 Footnote * and asymptomatic cases) reported by episode week in Canada, 2014-2019Footnote a
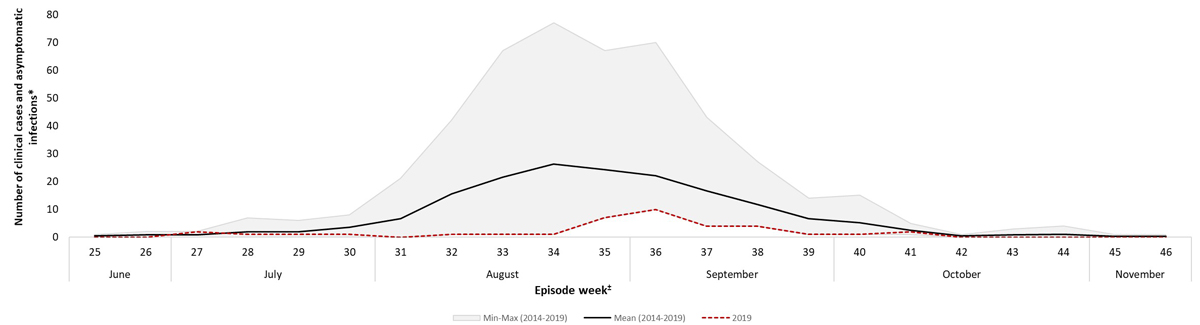
- Figure 3 Footnote *
-
Saskatchewan's WNV surveillance system monitors neurological syndrome cases only.
- Footnote a
-
WNV cases are grouped based on episode date. Episode week is calculated using the earliest available date based on the following hierarchy: symptom onset date, diagnosis date, laboratory sample date or reporting date.
Figure 3 - Text Description
This graph shows the number of the West Nile virus human infections (clinicalFigure 3 Footnote * and asymptomatic cases) reported in 2019, which are below the average of the five preceding seasons (2014-2019).
| Episode (surveillance) WeekFigure 3 Footnote b | Mean (2014 - 2019) |
Min-Max (2014 -2019) |
2019 | |
|---|---|---|---|---|
| June | 25 | 0.4 | 1 | 0 |
| 26 | 0.8 | 2 | 0 | |
| July | 27 | 0.8 | 2 | 2 |
| 28 | 2 | 7 | 1 | |
| 29 | 2 | 6 | 1 | |
| 30 | 3.6 | 8 | 1 | |
| August | 31 | 6.6 | 21 | 0 |
| 32 | 15.6 | 41 | 1 | |
| 33 | 21.6 | 66 | 1 | |
| 34 | 26.2 | 76 | 1 | |
| 35 | 24.2 | 60 | 7 | |
| September | 36 | 22 | 60 | 10 |
| 37 | 16.6 | 39 | 4 | |
| 38 | 11.8 | 23 | 4 | |
| 39 | 6.6 | 13 | 1 | |
| October | 40 | 5.2 | 14 | 1 |
| 41 | 2.4 | 4 | 2 | |
| 42 | 0.4 | 1 | 0 | |
| 43 | 0.8 | 3 | 0 | |
| 44 | 1 | 4 | 0 | |
|
||||
Of the 33 human infections (confirmed and probable), 64% (n=21) were reported as WNV neurological syndrome, 30% (n=10) as WNV non-neurological syndrome and 6% (n=2) as unclassified/unspecified (Table 1). Among the clinical cases classified as neurological, two deaths were reported. In addition, four WNV asymptomatic infections were reported.
| Province | Clinical cases | Total Clinical Cases | Asymptomatic infectionsTable 1 Footnote c | Rate (per 100,000)Table 1 Footnote d | ||
|---|---|---|---|---|---|---|
| Neurological | Non-neurological | Unclassified/Unspecified | ||||
| Ontario | 9 | 7 | 1 | 17 | 2 | 0.12 |
| Québec | 10 | 2 | 0 | 12 | 2 | 0.14 |
| Alberta | 2 | 0 | 0 | 2 | 0 | 0.15 |
| Manitoba | 0 | 1 | 1 | 2 | 0 | 0.05 |
| Canada | 21 | 10 | 2 | 33 | 4 | 0.09 |
|
||||||
In 2019, the incidence rate of reported infections (clinical and asymptomatic) increased with age; incidence was higher for females than males in the 50-59 age group, and lower in those 0-19, 20-29, 40-49 and over 60 years old (Figure 4). It is important to interpret these differences with caution, given the low number of human infections in 2019.
Figure 4. Age- and sex-specific incidence rateFigure 4 Footnote * (per 100,000 population) of reported West Nile virus human infections (clinical and asymptomatic cases) in Canada, 2019
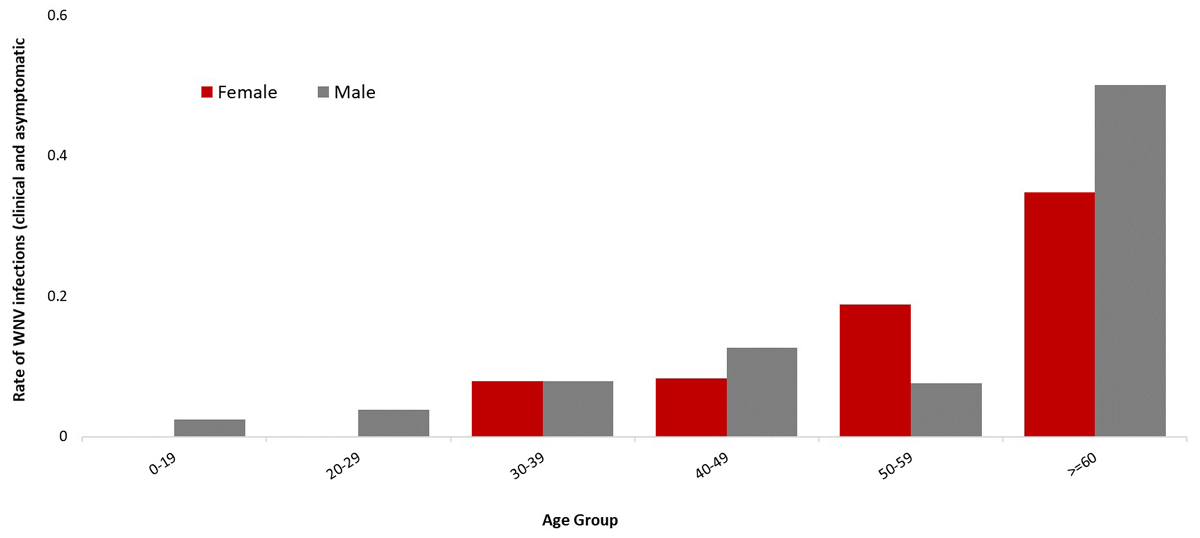
- Figure 4 Footnote *
-
Incidence was calculated using Q4 2019 Statistics Canada population estimates.
Figure 4 – Text Description
This figure shows that the incidence rateFigure 4 Footnote * of reported infections (clinical and asymptomatic) increased with age; incidence was higher for females than males in the 50-59 age group, and lower in those 0-19, 20-29, 40-49 and over 60 years old.
| Age group | Female incidence rate | Male incidence rate |
|---|---|---|
| 0-19 | 0.00 | 0.02 |
| 20-29 | 0.00 | 0.04 |
| 30-39 | 0.08 | 0.08 |
| 40-49 | 0.08 | 0.13 |
| 50-59 | 0.19 | 0.08 |
| Over 60 | 0.35 | 0.51 |
|
||
Travel-related cases
Between January 2 and November 22, 2019, a total of eight travel-related clinical cases were reported from Ontario (n=5), Alberta (n=2) and British Columbia (n=1). Of these, 12.5% (n=1) were reported as WNV neurological syndrome, 75% (n=6) as WNV non-neurological syndrome and 12.5% (n=1) as unclassified/unspecified. The median age of cases was 56 (range: 35-71). International travel locations included United States, Mexico, Cuba, Barbados and Ireland. These cases were excluded from analyses in this report.
Mosquito, wild bird and equine surveillance
During the 2019 transmission season, 11,586 mosquito pools were tested for WNV in four provinces: Ontario (n=8,400), Québec (n=1,820), Manitoba (n=1,166) and Saskatchewan (n=200). Of these, 96 (<1%) tested positive for WNV: 71 in Ontario, 19 in Québec, and 6 in Manitoba (Table 2). In 2019, the percent of mosquito pools positive for WNV infection was highest in Québec (1.0%). Similar to human cases, percent positivity for tested mosquito pools was low (<1%), compared to the average of the previous five years (1.9%) (Figure 5).
The CWHC tested 220 dead wild birds for WNV. Of these, 45 (21%) were positive for WNV across three provinces (Table 3, Figures 1 and 5). Overall, WNV activity was detected in birds from June to late October. Despite maintaining rigorous surveillance activities, fewer WNV-positive birds were identified than previous years (Figure 5).
The CFIA was notified of eight cases of WNV in domestic horses in the following five provinces: Alberta (n=3), Saskatchewan (n=2), British Columbia (n=1), Ontario (n=1) and Québec (n=1) (Table 3). This is the lowest number observed in Canada in a six-year span (Figure 5).
| Province | Number of positive pools | Total pools tested | Percent of positive pools |
|---|---|---|---|
| Ontario | 71 | 8,400 | 0.8 % |
| Québec | 19 | 1,820 | 1.0 % |
| Manitoba | 6 | 1,166 | 0.5 % |
| Saskatchewan | 0 | 200 | 0 % |
| Total | 96 | 11,586 | 0.8 % |
|
|||
| Province | Number of positive birds | Number of positive horses |
|---|---|---|
| Ontario | 30 | 1 |
| Québec | 12 | 1 |
| Saskatchewan | 3 | 2 |
| British Columbia | 0 | 1 |
| Alberta | 0 | 3 |
| Total | 45 | 8 |
Figure 5. Reported number of West Nile virus positive infections in humans (clinical, asymptomatic and travel-related cases), birds, horses and percent positive mosquito pools in Canada, 2014-2019
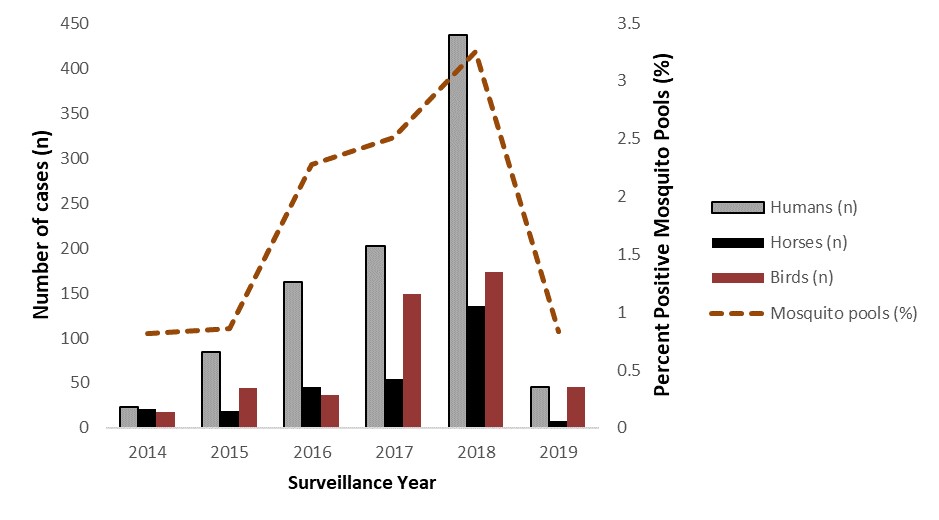
Figure 5 – Text Description
This figure shows that in 2019, the lowest number of human infections, (clinical, asymptomatic and travel-related cases), birds, horses and percent positive mosquito pools was observed in Canada, 2014-2019.
| Year | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|
| Humans (n) | 23 | 84 | 162 | 202 | 437 | 45 |
| Horses (n) | 21 | 19 | 46 | 54 | 123 | 8 |
| Birds (n) | 18 | 44 | 37 | 149 | 173 | 45 |
| Positive mosquito pools (%) | 0.81 | 0.86 | 2.28 | 2.51 | 3.25 | 0.84 |
California serogroup viruses
The NML confirmed two infections of CSGV in Québec (n=1) and Northwest Territories (n=1), of which the latter may be associated with travel outside the territory. Additionally, the province of Québec reported 16 infections of CSGV, however these infections were determined using a different case definitionFootnote 2 than the two infections reported nationally.
Eastern equine encephalitis virus
In 2019, the CFIA reported seven equine cases of EEEV with either clinical or laboratory diagnosis in Ontario. No human cases of EEEV were reported in Canada.
Discussion
The 2019 year marks the second lowest incidence of WNV cases reported in the last six years. Recurring fluctuations in the number of WNV human infections are expected. The low incidence of WNV in people was accompanied by low evidence of WNV infection in birds, horses, and mosquitoes across multiple jurisdictions in Canada during the 2019 transmission season.
Climate is one of the main dictators of yearly WNV fluctuations, affecting mosquito population dynamics in a given geographic areaFootnote 3. Lower winter temperatures are associated with poorer mosquito abundance and decreased transmission activityFootnote 3,Footnote 4. The changeability of the climate across Canada, combined with species lifecycles and habitat preferences, lead to differences in disease transmission patterns. This can be seen in the difference observed in 2019, between Eastern Canada, where Culex pipiens and Culex restuans are established, and Western Canada, where Culex tarsalis is foundFootnote 5,Footnote 6.
Low numbers of human WNV cases have also been observed in jurisdictions outside of Canada. The United States Centers for Disease Control and Prevention (CDC) reported a low number of cases of WNV infections in humans in 2019 (n=971), with 60 deathsFootnote 7. Similarly, incidence rates for locally acquired cases in Europe in 2019 decreased when compared to 2018, with the European Centre for Disease Control (ECDC) reporting 463 cases of WNV infections in humans, and 50 deathsFootnote 8. Despite this decrease, both Germany and Slovakia reported their first autochthonous WNV infection in humans in 20198.
In Canada, two confirmed infections of human CSGV were reported in 2019. CSGV, such as Jamestown Canyon virus and snowshoe hare virus, are endemic in Canada, and evidence suggests that they are not only more common than previously thought, but their incidence might increase with climate changeFootnote 3. As CSGV infections are not nationally notifiable diseases in Canada, there is no formal surveillance system in place to monitor, track and report cases. Furthermore, CSGV infections are likely under-diagnosed due to low-level of awareness among healthcare professionals in CanadaFootnote 1.
There were no reports of human EEEV cases in Canada in 2019, despite seven horse cases. The last report of a human EEEV case occurred in Ontario in 2016. However, as with CSGV, EEEV is not nationally notifiable in humans and there is no formal surveillance system in place.
Public health conclusions
Climate change can result in modified weather patterns and an increase in extreme events that can affect disease outbreaks and may contribute to an increase in the risk of the pathogen being carried to humans. Many vector-borne zoonotic diseases are climate sensitive and ecological shifts associated with climate change are expected to impact the distribution and incidences of these diseases. However, there are no vaccines or specific treatments for WNV, EEEV and CSGV human infections. Therefore, prevention strategies including education and promotion of personal protection (i.e., long-sleeved clothing, permethrin treated clothing, window screens and mosquito repellents) from mosquito bites, as well as mosquito control, are critical for decreasing the risk of mosquito-borne infections in people. Ongoing national surveillance is needed to help target prevention and control efforts, and increase awareness among healthcare professionals, especially of CSGV and EEEV.
For more information including populations-at-risk, symptoms and treatment, please refer to Canada.ca.
Acknowledgements
The Public Health Agency of Canada would like to acknowledge the provincial and territorial WNV and other mosquito-borne disease programs, Canadian Blood Services, Héma-Québec, the Canadian Wildlife Health Cooperative, and the Canadian Food Inspection Agency for their participation to the Canadian WNV Surveillance Program.
Erratum
The authors would like to correct the following information in the publication of the original report, West Nile virus and other mosquito-borne diseases surveillance report: Annual edition (2018):
The CSGV human infection counts were reported as “cases”; however, retrospective review of the data indicates these should in fact be considered “infections”, since the timeframe of these illnesses could not be determined. Furthermore, the correct number of equine cases in 2018 should be 123.
References
- Footnote 1
-
Ludwig A, Zheng H, Vrbova L, Drebot MA, Iranpour M, Lindsay LR. Increased risk of endemic mosquito-borne diseases in Canada due to climate change. Can Commun Dis Rep. 2019;45(4):90-7
- Footnote 2
-
Surveillance des maladies à déclaration obligatoire au Québec [Internet]. July 2019 [cited on 10 September 2021]. Available from: https://publications.msss.gouv.qc.ca/msss/fichiers/2019/19-268-05W.pdf
- Footnote 3
-
Ogden NH, Lindsay LR, Ludwig A, Morse AP, Zheng H, Zhu H. Weather-based forecasting of mosquito-borne disease outbreaks in Canada. Can Commun Dis Rep. 2019;45(5):127-32
- Footnote 4
-
Wang G, Minnis RB, Belant JL, Wax CL. Dry weather induces outbreaks of human West Nile virus infections. BMC Inf Dis. 2010;10:38
- Footnote 5
-
Kulkarni MA, Berrang-Ford L, Buck PA, Lindsay LR, Ogden NH. Major emerging vector-borne zoonotic diseases of public health importance in Canada. Emerg Microbes Infect. 2019;4(6): e33
- Footnote 6
-
Giordano BV, Kaur S, Hunter FF. West Nile virus in Ontario, Canada: A twelve-year analysis of human case prevalence, mosquito surveillance, and climate data. PLoS ONE. 2017;12(8): e0183568
- Footnote 7
-
Center for Disease Control. Final Cumulative maps and Data for 1999-2019 [Internet]. 24 November 2020 [cited on 07 December 2020]. Available from: https://www.cdc.gov/westnile/statsmaps/cumMapsData.html
- Footnote 8
-
European Centre for Disease Prevention and Control. Epidemiological Update: West Nile virus transmission season in Europe, 2019 [Internet]. 05 December 2019 [cited on 07 December 2020]. Available from: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-west-nile-virus-transmission-season-europe-2019
