National Lyme Disease Surveillance in Canada 2009–2012
Table of contents:
- Introduction
- A summary of Lyme disease cases
- Traveled-acquired Lyme disease cases
- Lyme disease cases by age and gender
- Seasonal variation in Lyme disease risk
- Where in Canada Lyme disease cases were acquired
- The symptoms of Lyme disease are being reported in Canada
- Interpretation and conclusions
- Acknowledgments
- References
- Technical notes
Introduction
Lyme disease became nationally notifiable in 2009 and surveillance data are provided by every province and territory through the National Notifiable Disease Surveillance System (NNDSS). Some provinces (Alberta, Manitoba, Ontario, New Brunswick, Nova Scotia and Prince Edward Island) participate in the Lyme disease enhanced surveillance (LDES) system, which aims to better identify Canadians at risk by analysis of information on reported human cases that is additional to information normally transferred to the NNDSS. Through collection of these data we aim to track the incidence of Lyme disease in Canada, and better understand how incidence is changing from year to year, where Lyme disease cases are occurring in Canada, age and gender groups most at risk, and what clinical manifestations are being seen in Canada. Collection and analysis of National Lyme disease surveillance data provides information that has two aims: i) supporting prevention of Lyme disease by helping to target control and prevention activities to the population most at risk; and ii) supporting improved diagnosis and treatment of affected Canadians by informing health care workers of the clinical manifestations of Lyme disease most frequently reported in Canada. Together these objectives aim to minimise the impact of Lyme disease in Canada.
A summary of Lyme disease cases
In 2012, 338 probable and confirmed cases were reported by 8 provinces (British Columbia, Alberta, Manitoba, Ontario, Quebec, New-Brunswick, Nova Scotia and Prince Edward Island: Figure 1). The number of cases reported in Canada has more than doubled in four years, from 144 in 2009 to 338 in 2012 (Table 1, Figure 2: but see the technical notes regarding these data), which is an increase in incidence from 0.4 to 1.0 cases per 100,000 population. Increasing incidence was mostly due to an increase in the number of cases that were most likely acquired in Canada, which comprised 65% of cases in 2009 and 82% of cases in 2012 (Figure 2). For all cases from 2009-2012, 62.2% of domestically-acquired cases were reported as confirmed (i.e. were mostly disseminated Lyme disease with serological laboratory evidence of infection and were acquired in a known endemic area) and 37.8% were reported as probable according to the surveillance case definition (i.e. were early Lyme disease acquired in a known endemic area or were disseminated Lyme disease with laboratory evidence of infection, but no contact with a known endemic area: Public Health Agency of Canada, 2009).
Figure 1. The numbers of reported Lyme disease cases by province in Canada in 2012.

Figure 1 description
The numbers of reported Lyme disease cases by province in Canada in 2012. This figure is a bar graph with vertical bars showing the numbers of cases of confirmed (light grey bars), probable (light gray cross hatched bars) and all (dark grey bars) Lyme disease cases reported by each province (from left to right, British Columbia, Alberta, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia and Prince Edward Island) and, on the right hand side, the totals (338 for all cases) for Canada. The numbers of cases are detailed in the following table:
| Province | Case classification | Total | |||
|---|---|---|---|---|---|
| Confirmed | % confirmed | Probable | % probable | ||
| British Columbia | 18 | 100.0 | 0 | 0.0 | 18 |
| Alberta | 7 | 87.5 | 1 | 12.5 | 8 |
| Manitoba | 8 | 42.1 | 11 | 57.9 | 19 |
| Ontario | 114 | 59.7 | 77 | 40.3 | 191 |
| Quebec | 42 | 100.0 | 0 | 0.0 | 42 |
| New Brunswick | 7 | 100.0 | 0 | 0.0 | 7 |
| Nova Scotia | 34 | 66.7 | 17 | 33.3 | 51 |
| Prince Edward Island | 2 | 100.0 | 0 | 0.0 | 2 |
| Canada | 227 | 67.2 | 111 | 32.8 | 338 |
Note that all cases acquired in Alberta were acquired on travel outside the province. British Columbia, Quebec and New Brunswick report only confirmed cases.
| Province | Year | |||
|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | |
Table 1 Footnotes
|
||||
| All cases | ||||
| British ColumbiaFootnote 1 | 0.2 | 0.2 | 0.4 | 0.4 |
| AlbertaFootnote 2 | 0.0 | 0.0 | 0.2 | 0.2 |
| SaskatchewanFootnote 2 | 0.0 | 0.0 | 0.1 | 0.0 |
| Manitoba | 0.4 | 1.0 | 1.0 | 1.5 |
| Ontario | 0.8 | 0.7 | 1.0 | 1.4 |
| QuebecFootnote 1 | 0.2 | 0.1 | 0.4 | 0.5 |
| New Brunswick | 0.0 | 0.3 | 0.7 | 0.9 |
| Nova Scotia | 1.7 | 1.8 | 5.7 | 5.4 |
| Prince Edward Island | 0.0 | 0.0 | 0.7 | 1.4 |
| Newfoundland and LabradorFootnote 2 | 0.0 | 0.2 | 0.0 | 0.0 |
| Canada | 0.4 | 0.4 | 0.8 | 1.0 |
| Cases acquired in Canada for Provinces that provide information on location of acquisition | ||||
| Manitoba | 0.3 | 0.6 | 0.6 | 1.0 |
| Ontario | 0.5 | 0.5 | 0.8 | 0.8 |
| New Brunswick | 0.0 | 0.3 | 0.4 | 0.7 |
| Nova Scotia | 1.5 | 1.5 | 5.2 | 5.3 |
| Prince Edward Island | 0.0 | 0.0 | 0.0 | 0.7 |
Figure 2. The numbers of reported Lyme disease cases in Canada 2009-2012.
Figure 2 description
This is a bar chart with vertical bars showing the numbers of cases reported in each year, from left to right, from 2009 to 2012. There are two bars for each year. Unfilled bars show the numbers of all reported cases (from 144, 143, 266 and 338 respectively for the years 2009 to 2012), while cross-hatched bars show the numbers of cases that were known to have been acquired in Canada (which increase from 79 in 2009, through 86 in 2010, 160 in 2011, to 220 in 2012). Above the cross-hatched bars are percentage figures which show, for each year, the proportions of the reported cases for which information on location of infection was provided that were acquired in Canada (65%, 69%, 78%, 82% for the years 2009 to 2012).
| Year | Cases acquired in Canada | All reported cases | Proportions of cases acquired in Canada |
|---|---|---|---|
| 2009 | 79 | 144 | 65% |
| 2010 | 86 | 143 | 69% |
| 2011 | 160 | 266 | 78% |
| 2012 | 220 | 338 | 82% |
The number of "cases acquired in Canada" reflects the numbers of cases reported to have been acquired in Canada. Whether or not Lyme disease cases are acquired in Canada or abroad is not recorded and reported by all provinces. The percentage values above the cross-hatched columns indicate, for each year, the proportions of cases for which information on location of infection was provided that were acquired in Canada.
| Case classification | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | Total | ||||||
| N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | |
Table 2 Footnotes
|
||||||||||
| All cases | ||||||||||
| Confirmed | 115 | (79.9) | 107 | (74.8) | 188 | (70.7) | 227 | (67.2) | 637 | (71.5) |
| Probable | 29 | (20.1) | 36 | (25.2) | 78 | (29.3) | 111 | (32.8) | 254 | (28.5) |
| Total | 144 | n/a | 143 | n/a | 266 | n/a | 338 | n/a | 891 | n/a |
| Cases reported as being acquired in CanadaFootnote * | ||||||||||
| Confirmed | 56 | (70.9) | 56 | (65.1) | 96 | (60.0) | 133 | (59.9) | 341 | (62.3) |
| Probable | 23 | (29.1) | 30 | (34.9) | 64 | (40.0) | 89 | (40.1) | 206 | (37.7) |
| Total | 79 | n/a | 86 | n/a | 160 | n/a | 222 | n/a | 547 | n/a |
Travel-acquired Lyme disease cases
For the period 2009-2012, data on country of exposure was available for 80.5% of cases from provinces participating in the LDES. A total of 48 cases (22.1% of those for which information was available) were reported as having been acquired outside Canada in 2012. Since 2009, the annual number of cases acquired during travel outside Canada has remained similar (41, 38 and 41 respectively for 2009, 2010 and 2011). All cases from Alberta were acquired while travelling outside Canada. For the 54 cases for which the location of travel outside Canada was provided during the period 2009-2012, 70% were acquired in the USA and 30% were-acquired in Europe.
Lyme disease cases by age and gender
There were more men than women affected (56% vs 44%). Incidence of reported cases was highest for adults aged between 55 and 74, and amongst children incidence was highest for those aged between 5 and 14 (Figure 3).
Figure 3. The incidence of reported Lyme disease cases by sex and age category 2009-2012.
Figure 3 description
This is a bar chart with vertical bars showing the incidence (number per 100,000 population per year) of cases of Lyme disease reported during 2009-2012 categorised into 18 age groups from children aged 0-4 years on the left, to adults aged 85 years on the right. The graph shows that the incidence was highest in 55-74 year-old people, while amongst children incidence was highest amongst 5-14 year olds. The bar for each age group is divided into two, an upper dark grey bar and a lower light grey bar depicting, respectively, the incidence for males and females. Details of the incidence in the different age groups and sexes are presented in the following table:
| Age in category | Female | Male |
|---|---|---|
| 0-4 | 0.9 | 1.8 |
| 5-9 | 1.9 | 2.7 |
| 10-14 | 2.0 | 2.5 |
| 15-19 | 1.7 | 1.9 |
| 20-24 | 2.2 | 2.2 |
| 25-29 | 1.6 | 2.4 |
| 30-34 | 1.7 | 2.1 |
| 35-39 | 2.4 | 2.5 |
| 40-44 | 2.0 | 2.8 |
| 45-49 | 2.1 | 3.5 |
| 50-54 | 3.0 | 3.1 |
| 55-59 | 4.6 | 4.7 |
| 60-64 | 3.9 | 4.4 |
| 65-69 | 4.1 | 3.8 |
| 70-74 | 3.6 | 4.6 |
| 75-79 | 2.6 | 2.6 |
| 80-84 | 1.2 | 2.7 |
| >=85 | 0.0 | 0.5 |
Data were available from all cases from all provinces. The denominators for these age and sex categories were obtained from Statistics Canada.
Seasonal variation in Lyme disease risk
Data on date of onset or diagnosis of illness were reported from the provinces participating in the LDES. Most domestically-acquired cases (95%) were reported from April through November peaking in July when tick vectors are active and when Canadians are frequently involved in outdoor activities (Figure 4). Reporting of some Lyme disease cases in each month from December to March could suggest that there may be risk outside the usual season of tick activity and that ticks can become active during warm periods during the winter in some locations, although this observation could be due to delayed onset of clinical manifestations in some instances (Wormser et al. 2006).
Figure 4. The numbers of Lyme disease cases reported in the LDES, by month of illness onset and by year, 2009-2012.
Figure 4 description
This is a line graph showing the numbers of cases with an estimated onset date for each month of the year. One unbroken line shows the month of onset of all reported cases during 2009-2012, while the different patterned broken lines show the numbers of cases by month for each individual year. The graph shows that overall (and for most years) onset of illness occurred during the period May to September (peaking in July) although low numbers of cases had onset dates in winter early spring and autumn. Detailed figures are shown in the following table.
| Month | Years | ||||
|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | 2009-2012 | |
| January | 4 | 0 | 5 | 3 | 12 |
| February | 4 | 2 | 5 | 2 | 13 |
| March | 1 | 2 | 4 | 6 | 13 |
| April | 7 | 6 | 9 | 13 | 35 |
| May | 18 | 11 | 13 | 19 | 61 |
| June | 18 | 28 | 39 | 68 | 153 |
| July | 30 | 33 | 61 | 93 | 217 |
| August | 24 | 27 | 63 | 61 | 175 |
| September | 14 | 18 | 30 | 29 | 91 |
| October | 15 | 7 | 12 | 19 | 53 |
| November | 8 | 5 | 17 | 20 | 50 |
| December | 1 | 4 | 8 | 5 | 18 |
Where in Canada Lyme disease cases were acquired
For the 414 (46.5%) cases for which information on location of acquisition in Canada was available, nearly 90% were acquired in locations in the Maritimes, southern, eastern and north-western Ontario, and southern Manitoba where surveillance shows that the tick vectors of Lyme disease are known to occur (Ogden et al. 2014; Figure 5).
The identification of cases that are reported to have been acquired in areas where tick populations have not yet been identified will help inform future field surveillance for ticks.
Figure 5. The numbers of reported Lyme disease cases by municipality of acquisition, 2009-2012.
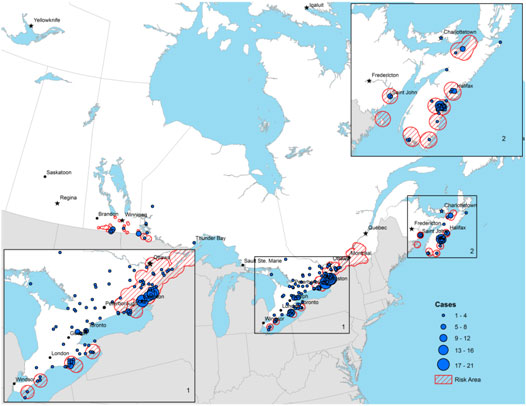
Figure 5 description
This figure is a map of Canada from Manitoba east with enlarged insets showing southern Ontario and the Maritimes. Lyme disease risk areas (i.e. areas where field surveillance has shown or suggests where tick vectors of Lyme disease have become established) are shown by red hatched areas, in the main map and insets as described in detail in the following. The locations of municipalities where Lyme disease cases were reported to have been acquired are shown as blue circles. The size of the circles represents categories of the numbers of cases reported for each municipality. The circles represent the following categories in order of increasing size: 1-4 cases, 5-8 cases, 9-12 cases, 13-16 cases and 17-21 cases. The locations of Lyme disease risk areas and of human Lyme disease cases are as follws:
- Lyme disease risk areas occur in southern Manitoba and western Ontario. These areas include six known endemic areas in Manitoba: an area of the west side of Lake of the Woods, the area of the Pembina escarpment including Pembina Valley Provincial Park, the region of St. Malo, the Vita/Arbakka region including the Roseau river, Beaudry Provincial Park and the Assiniboine River, locations adjacent to the Agassiz and Sandilands provincial forests. Risk areas where ticks have been found include southern Manitoba along the border with the US from south of Brandon to Lake of the Woods, around Winnipeg, and in western Ontario close to Lake of the Woods. southern Manitoba along the border with the US from south of Brandon to Lake of the Woods, around Winnipeg, and in western Ontario close to Lake of the Woods., in southern Manitoba/north west Ontario, southern Ontario along the north shores of Lake Erie and Ontario, along the St Lawrence valley in eastern Ontario and southern Quebec, and in locations in New Brunswick and Nova Scotia. In Manitoba, human cases were reported to have been acquired at locations around the Pembina Valley region adjacent to the US border, the St Malo region and around Lake of the Woods. In western Ontario, cases have reported location of acquisition near Lake of the Woods, Kenora and Thunder Bay.
- Lyme disease risk areas occur in southern and eastern Ontario and southern Quebec: There are seven known endemic areas that are at Pointe-Pelee National Park, Rondeau Provincial Park, Turkey Point Provincial Park, Long Point peninsula including Long Point Provincial Park and the National Wildlife area, Wainfleet bog near Welland on the Niagara peninsula, Prince Edward Point and parts of the Thousand Islands National Park. There are five known endemic areas in Montérégie, in the south of Québec. Lyme disease risk areas are locations around Kingston in the Saint Lawrence valley that extend north east towards Ottawa in Ontario extending to locations covering much of Montérégie, and parts of Estrie and Centre du Québec in the south of Québec. Some human cases in Ontario were reportedly acquired in each of the risk areas and endemic areas, with particularly high numbers reportedly acquired at or around Long Point and the Thousand Islands National Park. Small numbers of cases were reportedly acquired in each of a number of locations not currently known to be risk areas across southern Ontario including locations in the south west, central west, central east, Hamilton/Niagara, Toronto, south eastern and eastern regions, as well as in the North Bay region and Georgian Bay.
- Lyme disease risk areas occur in the Maritime Provinces. Two known endemic areas occur in New Brunswick (Millidgeville area of Saint John and North Head, Grand Manan Island) as well as six known endemic areas in Nova Scotia (areas of Halifax Regional Municipality and areas of the counties of Lunenburg, Shelburne, Yarmouth, Pictou and Queens) are shown. Possible risk areas shown are locations adjacent to known endemic areas in Pictou and Lunenburg counties in Nova Scotia. Human cases were reportedly acquired in and around all endemic areas, with the exception of the endemic area on Grand Manan Island. The highest numbers of cases were reportedly acquired at locations in Lunenburg county, Nova Scotia. Small numbers of cases were reportedly acquired around Charlottetown in Prince Edward Island and the north-eastern extent of mainland Nova Scotia.
The numbers of cases and municipalities for which location of acquisition was reported are detailed in the following table:
| Province | Number of cases | Number of municipalities |
|---|---|---|
| Data on location of acquisition are not available for cases acquired in British Columbia and Quebec so these are no cases shown for these provinces. | ||
| Manitoba | 25 | 6 |
| Ontario | 253 | 107 |
| New Brunswick | 10 | 2 |
| Nova Scotia | 126 | 47 |
| Prince-Eward Island | 1 | 1 |
| Total | 415 | 163 |
The symptoms of Lyme disease being reported in Canada
Over the period 2009-2012, a high proportion of cases (70%) were reported to have had symptoms of early Lyme disease (i.e. they showed erythema migrans [EM]). However, 55% of cases reported symptoms of disseminated Lyme disease: 28% of cases reported symptoms of early disseminated Lyme disease (i.e. neurological and cardiac symptoms) and 38% of cases reported symptoms of late Lyme disease (i.e. arthritis) (Figure 6). Of those cases acquired in known Canadian Lyme disease endemic or Lyme risk areas (defined in Ogden et al. 2014) 40% were reported as early Lyme disease, i.e. EM was the only reported symptom. For 37% of cases acquired in Canada for which EM was reported, clinical manifestations of later stages of Lyme disease were also reported.
Figure 6. The clinical manifestations of Lyme disease cases for which these data were reported, 2009-2012.
Figure 6 description
This is a bar chart with horizontal bars showing the proportion of Lyme disease cases that were reported as having shown clinical manifestations of (from top to bottom) cardiac symptoms (4.8%), Bell`s palsy (8.5%), other neurological symptoms (21%), arthritis (37.8%) and erythema migrans (70.5%).
Note that for many cases more than one clinical manifestation was reported for each case. Full details of the clinical manifestations of Lyme disease are not provided by all provinces.
Interpretation and conclusions
Endemic lyme disease occurs in British Columbia and in the eastern and central Canadian provinces of Nova Scotia, New Brunswick, Quebec, Ontario and Manitoba where it is continuing to emerge (Figure 1 and 2, Table 1). Lyme disease cases that were acquired while travelling in the USA or Europe continue to be reported in a number of provinces at a fairly constant rate since surveillance began (Table 2). Males, children aged between 5 and 14 years and adults between 50 and 74 years may be particularly at risk (Figure 3). Lyme disease cases are reported in all months but peak incidence occurs in the summer months (Figure 4). Most Lyme disease cases were reported as having been acquired in areas where Lyme disease risk associated with tick populations is known (Figure 5). Some cases reported acquisition in areas where established tick populations and Lyme disease risk has not been identified to date (Figure 5). These sporadic case reports may occur as a result of exposure to infected ticks dispersed by migratory birds (Ogden et al. 2008), or they may be the early indications of newly establishing tick populations in locations where field surveillance for ticks has yet to be conducted (Ogden et al. 2014). EM was reported in a high proportion of cases (Figure 6), but Lyme disease was diagnosed and/or reported at this early stage of infection (when EM is the only symptom) in a low proportion of cases (40%) compared to the proportion of cases reported as early Lyme disease in surveillance in the USA (> 60%: Bacon et al. 2008), where awareness of Lyme disease amongst the public and medical practitioners would be expected to be greater than in Canada. Therefore, affected members of the public in Canada are not presenting themselves for treatment in early Lyme disease, and/or front line medical practitioners are not reporting all early Lyme disease cases. This could be attributable to suboptimal awareness amongst health care workers and the public.
Early identification, diagnosis and treatment are key to successful health outcomes for Canadians suffering from Lyme disease. The above findings, combined with the growing proportion of cases acquired within Canada, support the need for a coordinated response to Lyme disease in Canada. As such, the Public Health Agency of Canada implemented an Action Plan on Lyme disease (Harymann et al. 2014), with the objective of increasing awareness among physicians and Canadians, enhancing surveillance and improving diagnosis.
Acknowledgments
The PHAC would like to thank all our partners at provincial and regional levels across Canada who contribute to the data collection and transfer and made this report possible.
References
- Bacon RM, Kugeler KJ, and Mead P (2008). Surveillance for Lyme Disease United States, 1992-2006. Morbidity and Mortality Weekly Report, 57.
- Harymann M, Ogden N, Lindsay R, Lawless V, Deilgat M, and Sternthal S (2014). Summary of the Public Health Agency of Canada's Action Plan on Lyme disease. Can Commun.Dis. Rep., 40, 88-90.
- Ogden NH, Koffi JK, Pelcat Y, and Lindsay LR (2014). Environmental risk from Lyme disease in central and eastern Canada: a summary of recent surveillance information. Can.Commun.Dis.Rep., 40, 74-82.
- Ogden NH, Lindsay LR, Hanincova K et al. (2008). Role of migratory birds in introduction and range expansion of Ixodes scapularis ticks, and Borrelia burgdorferi and Anaplasma phagocytophilum in Canada. Appl.Environ.Microbiol., 74, 1780-1790.
- Public Health Agency of Canada (2009). Cases definitions for diseases under national surveillance. Can.Commun.Dis.Rep., 35.
- Wormser GP, Dattwyler RJ, Shapiro ED et al. (2006). The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis., 43, 1089-1134.
Technical notes
- The data analyzed and presented in this report are provided by provincial public health authorities. The data represent cases reported to public health units and recorded in the different provincial notifiable diseases systems. Counts by province are subject to varying degrees of underreporting.
- Many provincial notifiable diseases systems are dynamic disease reporting systems that permit ongoing updates to the data if new information on cases comes to light. Therefore, data extracted from a provincial notifiable disease system represent a snap shot at the time of extraction and may differ from previous or subsequent reports.
- For this reason, data in this report may differ slightly from data displayed by provincial authorities.
- Data on possible area of exposure, travel and symptoms are provided by provinces that participate in the LDES.
Page details
- Date modified: