Rheumatoid arthritis in Canada
Download the alternative format
(PDF format, 2 MB, 6 pages)
Organization: Public Health Agency of Canada
Date published: September 2020
Highlights from the Canadian Chronic Disease Surveillance System
Rheumatoid arthritis is the most common chronic inflammatory joint disease and is a leading cause of disability worldwide.Footnote 1 People with rheumatoid arthritis are at a higher risk of mortality than the general population due to the associated comorbidities that present with this disease.Footnote 2Footnote 3 There is no cure for rheumatoid arthritis, however, early diagnosis and treatment can reduce associated joint pain and symptoms, helping individuals to live active lives.
The Public Health Agency of Canada (PHAC), in collaboration with all Canadian provinces and territories, conducts national surveillance of rheumatoid arthritis to support public health action. This fact sheet presents an overview of diagnosed rheumatoid arthritis data from the Canadian Chronic Disease Surveillance System (CCDSS). For further information, refer to What's in the Data?
What is rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease resulting from the body's immune system mistakenly attacking the lining of the joints and other tissues.Footnote 2 Inflammation in the joints causes swelling, pain, and stiffness, which left untreated, can lead to joint damage. Rheumatoid arthritis can affect multiple joints in the body and most commonly the joints of the hands, wrists, and feet. The inflammation may also affect other organs, such as the eyes, skin, lungs, or heart.
How many Canadians live with rheumatoid arthritis (prevalence) and how many are newly diagnosed each year (incidence)?
Approximately 374,000 (1.2%) Canadians aged 16 years and older live with diagnosed rheumatoid arthritis and 23,000 (0.8 per 1,000 persons per year) were newly diagnosed in 2016–2017. The prevalence and incidence of diagnosed rheumatoid arthritis generally increase with age and are higher among females (1.7% and 1.0 per 1,000 persons per year, respectively) compared to males (0.8% and 0.5 per 1,000 persons per year, respectively) (Figures 1 and 2).
Figure 1: Prevalence (%) of diagnosed rheumatoid arthritis by sex and age group, Canada,Footnote a 2016–2017
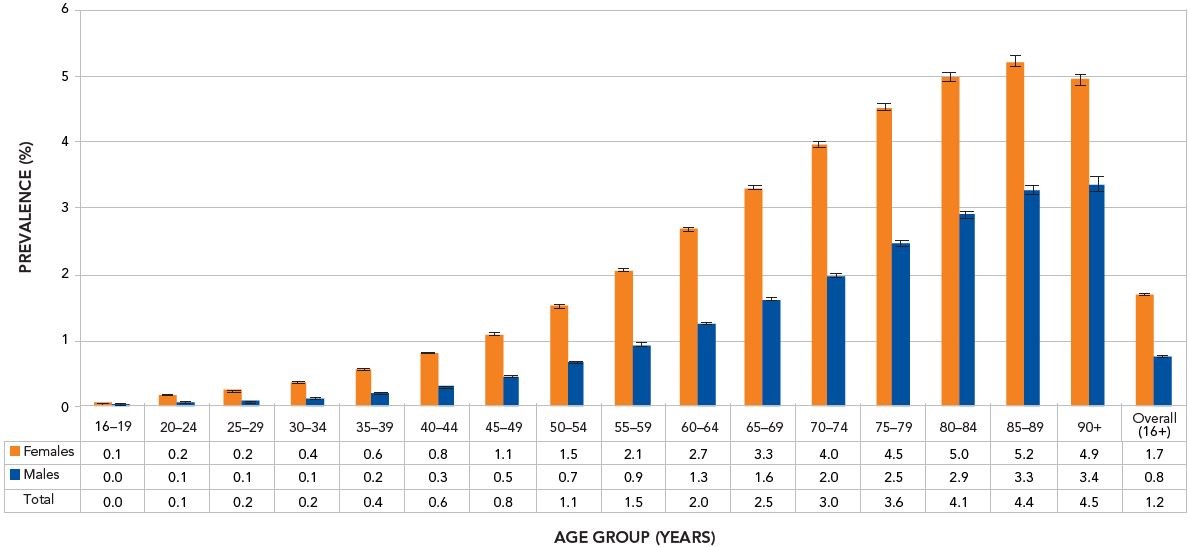
- Footnote a
-
Data from SK were not available for fiscal year 2016–2017. Data from NL were excluded.
Notes: The 95% confidence interval shows an estimated range of values which is likely to include the true prevalence 19 times out of 20.
Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, August 2019.
Text description
| Age Group (years) | Prevalence among females for fiscal year 2016-2017 | Prevalence among males for fiscal year 2016-2017 | Total prevalence for fiscal year 2016-2017 |
|---|---|---|---|
| 16-19 | 0.1 | 0.0 | 0.0 |
| 20-24 | 0.2 | 0.1 | 0.1 |
| 25-29 | 0.2 | 0.1 | 0.2 |
| 30-34 | 0.4 | 0.1 | 0.2 |
| 35-39 | 0.6 | 0.2 | 0.4 |
| 40-44 | 0.8 | 0.3 | 0.6 |
| 45-49 | 1.1 | 0.5 | 0.8 |
| 50-54 | 1.5 | 0.7 | 1.1 |
| 55-59 | 2.1 | 0.9 | 1.5 |
| 60-64 | 2.7 | 1.3 | 2.0 |
| 65-69 | 3.3 | 1.6 | 2.5 |
| 70-74 | 4.0 | 2.0 | 3.0 |
| 75-79 | 4.5 | 2.5 | 3.6 |
| 80-84 | 5.0 | 2.9 | 4.1 |
| 85-89 | 5.2 | 3.3 | 4.4 |
| 90+ | 4.9 | 3.4 | 4.5 |
| Overall (16+) | 1.7 | 0.8 | 1.2 |
Figure 2: Incidence of diagnosed rheumatoid arthritis (per 1,000 persons per year), by sex and age group, Canada,Footnote b 2016–2017
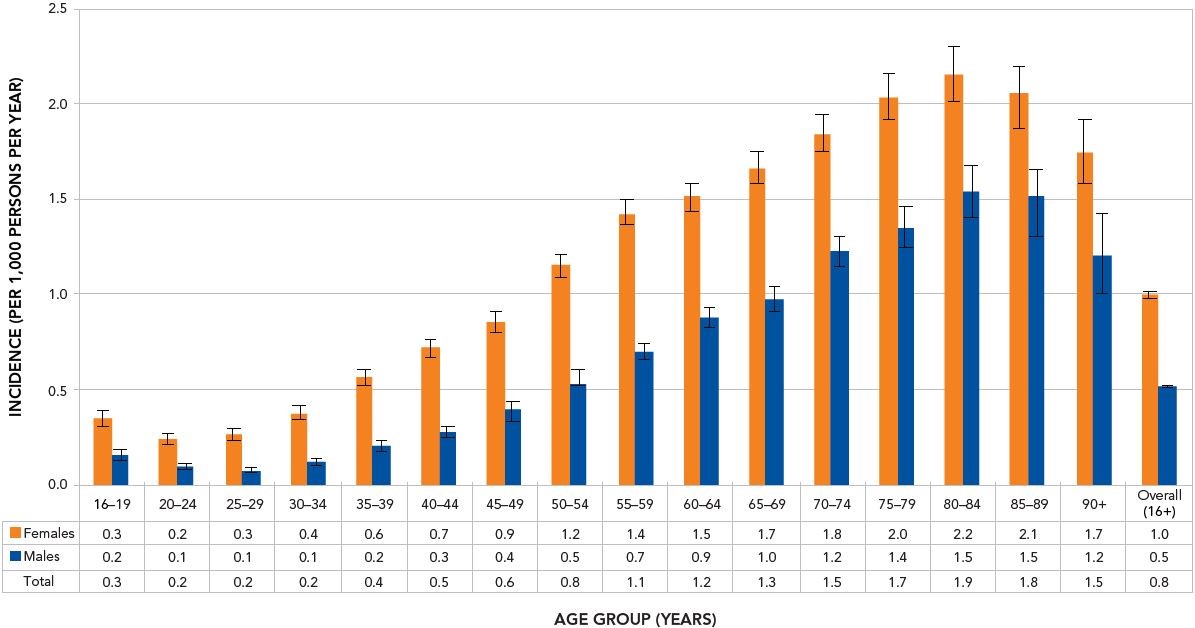
- Footnote b
-
Data from SK were not available for fiscal year 2016–2017. Data from NL were excluded.
Notes: The 95% confidence interval shows an estimated range of values which is likely to include the true incidence 19 times out of 20.
Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, August 2019.
Text description
| Age Group (years) | Incidence among females for fiscal year 2016-2017 | Incidence among males for fiscal year 2016-2017 | Total incidence for fiscal year 2016-2017 |
|---|---|---|---|
| 16-19 | 0.3 | 0.2 | 0.3 |
| 20-24 | 0.2 | 0.1 | 0.2 |
| 25-29 | 0.3 | 0.1 | 0.2 |
| 30-34 | 0.4 | 0.1 | 0.2 |
| 35-39 | 0.6 | 0.2 | 0.4 |
| 40-44 | 0.7 | 0.3 | 0.5 |
| 45-49 | 0.9 | 0.4 | 0.6 |
| 50-54 | 1.2 | 0.5 | 0.8 |
| 55-59 | 1.4 | 0.7 | 1.1 |
| 60-64 | 1.5 | 0.9 | 1.2 |
| 65-69 | 1.7 | 1.0 | 1.3 |
| 70-74 | 1.8 | 1.2 | 1.5 |
| 75-79 | 2.0 | 1.4 | 1.7 |
| 80-84 | 2.2 | 1.5 | 1.9 |
| 85-89 | 2.1 | 1.5 | 1.8 |
| 90+ | 1.7 | 1.2 | 1.5 |
| Overall (16+) | 1.0 | 0.5 | 0.8 |
What are the trends over time?
Between 2007–2008 and 2016–2017, the age-standardized prevalence of diagnosed rheumatoid arthritis increased among females (from 1.3% to 1.5%) and remained around 0.7% among males (Figure 3).
During the same time period, the age-standardized incidence of diagnosed rheumatoid arthritis decreased from 1.2 to 0.9 per 1,000 persons per year in females and from 0.6 to 0.5 per 1,000 persons per year in males.
Figure 3: Age-standardizedFootnote c prevalence (%) and incidence (per 1,000 persons per year) of diagnosed rheumatoid arthritis among Canadians aged 16 years and older, by sex, Canada,Footnote d from 2007–2008 to 2016–2017
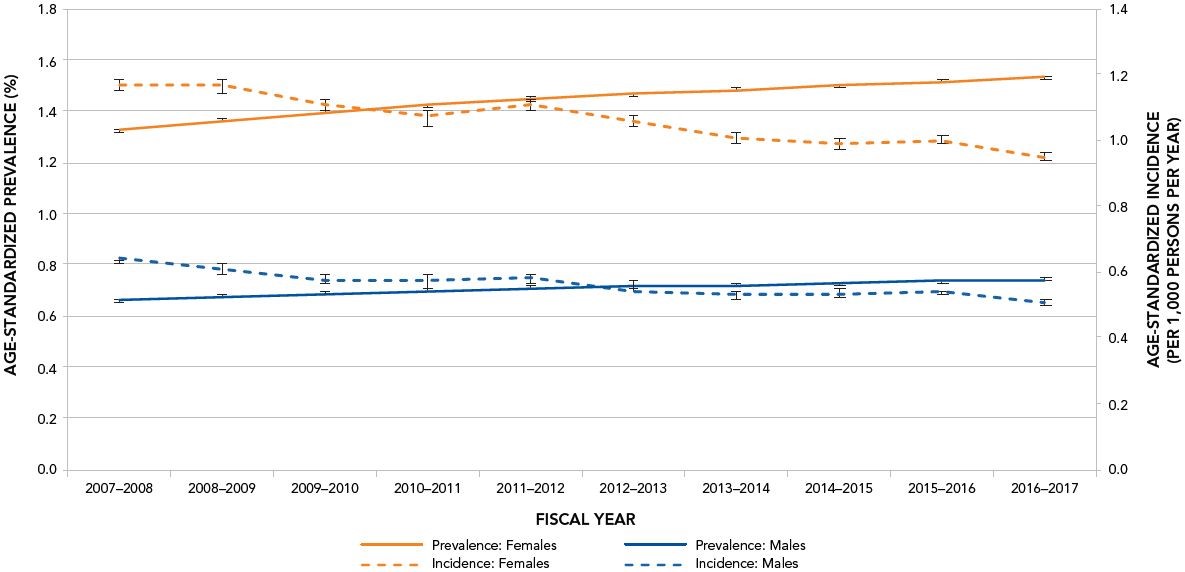
- Footnote c
-
Rates were age-standardized to the 2011 final postcensal Canada population released in 2013.
- Footnote d
-
Data from SK were not available for fiscal year 2016–2017. Data from YT were excluded before fiscal year 2010–2011. Data from NL were excluded.
Notes: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20.
Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, August 2019.
Text description
| Fiscal Year | Age-standardized prevalence among females aged 16 years and older | Age-standardized prevalence among males aged 16 years and older | Age-standardized incidence among females aged 16 years and older | Age-standardized incidence among males aged 16 years and older |
|---|---|---|---|---|
| 2007-2008 | 1.3 | 0.7 | 1.2 | 0.6 |
| 2008-2009 | 1.4 | 0.7 | 1.2 | 0.6 |
| 2009-2010 | 1.4 | 0.7 | 1.1 | 0.6 |
| 2010-2011 | 1.4 | 0.7 | 1.1 | 0.6 |
| 2011-2012 | 1.4 | 0.7 | 1.1 | 0.6 |
| 2012-2013 | 1.5 | 0.7 | 1.1 | 0.6 |
| 2013-2014 | 1.5 | 0.7 | 1.0 | 0.5 |
| 2014-2015 | 1.5 | 0.7 | 1.0 | 0.5 |
| 2015-2016 | 1.5 | 0.7 | 1.0 | 0.5 |
| 2016-2017 | 1.5 | 0.7 | 0.9 | 0.5 |
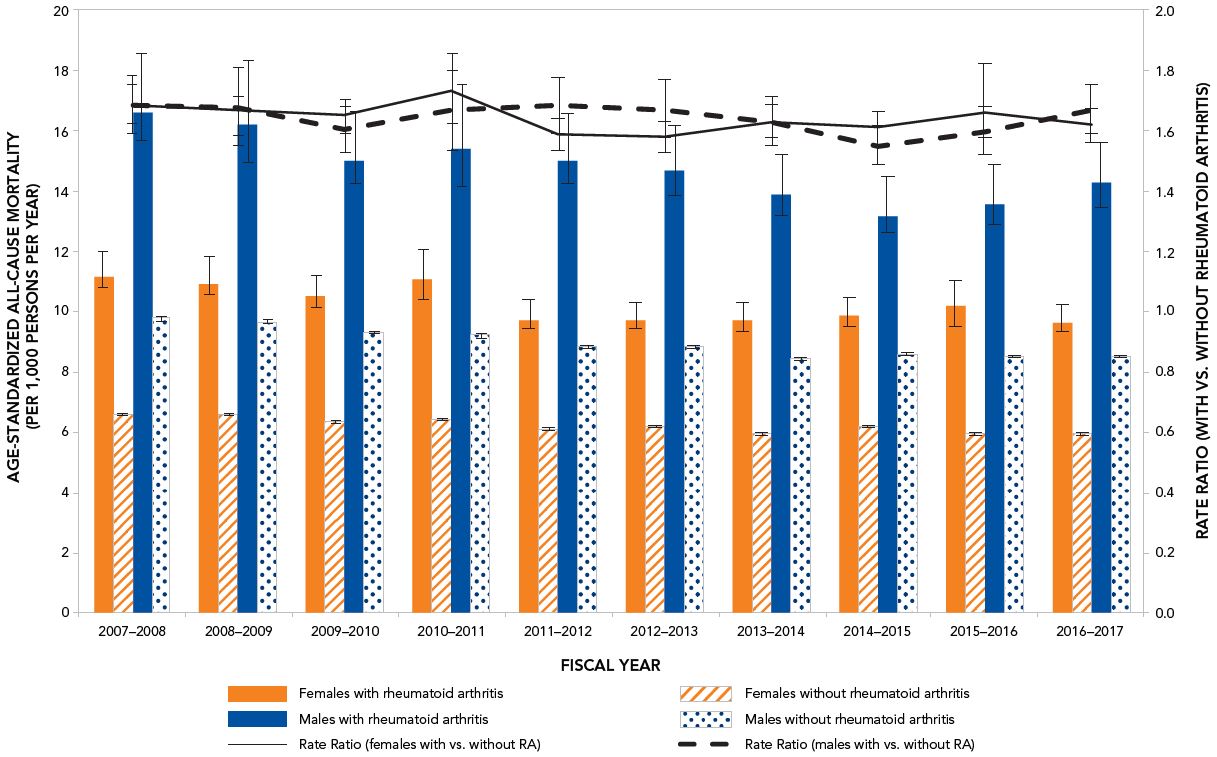
What are the mortality rates (due to any cause of death) among Canadians with or without rheumatoid arthritis?
Between 2007–2008 and 2016–2017, age-standardized all-cause mortality rates (i.e. mortality due to any cause) decreased among females with diagnosed rheumatoid arthritis (11.2 per 1,000 persons per year to 9.7 per 1,000 persons per year) and among males with diagnosed rheumatoid arthritis (16.6 per 1,000 persons per year to 14.2 per 1,000 persons per year) (Figure 4). Mortality rates were consistently higher among males compared to females.
Over the surveillance period, the age-standardized all-cause mortality rate ratios (i.e., comparing individuals with, versus without, diagnosed rheumatoid arthritis) were relatively stable ranging from 1.7 to 1.6 in females and from 1.5 to 1.7 in males. While rate ratios were similar among females and males, they showed an increase in mortality risk among those with diagnosed rheumatoid arthritis.
Figure 4: Age-standardizedFootnote e all-cause mortality rates (per 1,000 persons per year) and rate ratios among Canadians aged 16 years and older with and without diagnosed rheumatoid arthritis (RA), Canada,Footnote f from 2007–2008 to 2016–2017
- Footnote e
-
Rates were age-standardized to the 2011 final postcensal Canada population released in 2013.
- Footnote f
-
Data from SK were not available for fiscal year 2016–2017. Data from YT were excluded before fiscal year 2010–2011. Data from NL were excluded.
Notes: The 95% confidence interval shows an estimated range of values that is likely to include the true value 19 times out of 20.
Data source: Public Health Agency of Canada, using CCDSS data files contributed by provinces and territories, August 2019.
Text description
| Fiscal Year | Age-standardized all-cause mortality among females aged 16 years and older with diagnosed rheumatoid arthritis | Age-standardized all-cause mortality among females aged 16 years and older without diagnosed rheumatoid arthritis | Age-standardized all-cause mortality among males aged 16 years and older with diagnosed diagnosed rheumatoid arthritis | Age-standardized all-cause mortality among males aged 16 years and older without diagnosed diagnosed rheumatoid arthritis | Rate ratio among females aged 16 years and older (females with versus without diagnosed diagnosed rheumatoid arthritis) | Rate ratio among males aged 16 years and older (males with versus without diagnosed diagnosed rheumatoid arthritis) |
|---|---|---|---|---|---|---|
| 2007-2008 | 11.2 | 6.6 | 16.5 | 9.8 | 1.7 | 1.7 |
| 2008-2009 | 10.8 | 6.6 | 16.2 | 9.7 | 1.7 | 1.7 |
| 2009-2010 | 10.5 | 6.4 | 14.9 | 9.3 | 1.6 | 1.6 |
| 2010-2011 | 11.1 | 6.4 | 15.3 | 9.2 | 1.7 | 1.7 |
| 2011-2012 | 9.7 | 6.1 | 14.9 | 8.8 | 1.6 | 1.7 |
| 2012-2013 | 9.7 | 6.2 | 14.3 | 8.8 | 1.6 | 1.7 |
| 2013-2014 | 9.7 | 6.0 | 13.8 | 8.4 | 1.6 | 1.6 |
| 2014-2015 | 9.9 | 6.2 | 13.3 | 8.6 | 1.6 | 1.5 |
| 2015-2016 | 9.8 | 5.9 | 13.6 | 8.5 | 1.7 | 1.6 |
| 2016-2017 | 9.6 | 6.0 | 14.2 | 8.5 | 1.6 | 1.7 |
How can rheumatoid arthritis be managed?
The specific causes of rheumatoid arthritis are unknown, but there are a number of factors associated with an increased risk of developing the disease including family history, smoking, increased age and occupational exposures.Footnote 4Footnote 5 While there is no cure for rheumatoid arthritis, there are treatment options which aim to alleviate joint symptoms and improve function. Individuals often work with a rheumatologist to develop a treatment plan to prevent further joint damage. Medication is often prescribed as a first line of therapy and is key to controlling disease and preventing damage. Other ways to manage include physical therapy, occupational therapy and education.Footnote 6 Individuals with rheumatoid arthritis who are diagnosed and treated early are less likely to experience long-term joint damage and functional impairments.
What do the national data on rheumatoid arthritis tell us?
- The prevalence and incidence of diagnosed rheumatoid arthritis are more common among females compared to males and increase with age.
Acknowledgements
This work was made possible through collaboration between PHAC and all Canadian provincial and territorial governments and expert contribution from the CCDSS Arthritis Working Group. Results and interpretations reported in this fact sheet are those of the authors. No endorsement by the provinces and territories is intended or should be inferred.
How to learn more
Visit: Canada.ca search "arthritis" or "rheumatoid arthritis"
Get data: Canadian Chronic Disease Surveillance System Data Tool
Follow us: @GovCanHealth
Like us: @HealthyCdns
More: visit the Arthritis Society
What's in the data?
The data used in this publication are from the Canadian Chronic Disease Surveillance System (CCDSS), a collaborative network of provincial and territorial chronic disease surveillance systems, supported by the Public Health Agency of Canada (PHAC).
The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries.
While CCDSS data reflect the health status of the Canadian population, they may also reflect changes in data collection methods, coding and classification systems, or clinical and billing practices. These factors must also be taken into consideration when interpreting time trends.
Definition of diagnosed rheumatoid arthritis in the CCDSS
Canadians aged 16 years and older are identified as having diagnosed rheumatoid arthritis if they have: at least one hospitalization record or two physician visits greater than or equal to eight weeks apart within two years (with exclusion criterion) with an International Classification of Diseases (ICD-9 or ICD-10) code for rheumatoid arthritis.
References
- Footnote 1
-
Widdifield J, Bernatsky S, Bombardier C, Paterson M. Rheumatoid arthritis surveillance in Ontario: monitoring the burden, quality of care and patient outcomes through linkage of administrative health data. Healthc Q. 2015 Oct;18(3):7–10.
- Footnote 2
-
Public Health Agency of Canada (PHAC). Life with arthritis in Canada: a personal and public health challenge. Ottawa (ON): PHAC; 2010 [cited 2019 Mar 20]. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/arthritis/life-arthritis-canada-a-personal-public-health-challenge.html
- Footnote 3
-
Van den Hoek J, Boshuizen HC, Roorda LD, Tijhuis GJ, Nurmohamed MT, van den Bos GA, Dekker J. Mortality in patients with rheumatoid arthritis: a 15-year prospective cohort study. Rheumatol Int. 2017 Apr;37(4):487–93.
- Footnote 4
-
Di Giuseppe D, Discacciati A, Orsini N, Wolk A. Cigarette smoking and risk of rheumatoid arthritis: a dose-response meta-analysis. Arthritis Res Ther. 2014 Apr;16(2):R61.
- Footnote 5
-
Turk SA, van Beers-Tas MH, van Schaardenburg D. Prediction of future rheumatoid arthritis. Rheum Dis Clin North Am. 2014 Nov;40(4):753–70.
- Footnote 6
-
Hurd K, Barnabe C. Systematic review of rheumatic disease phenotypes and outcomes in the Indigenous populations of Canada, the USA, Australia and New Zealand. Rheumatol Int. 2017 Apr;37(4):503–21.