Canadian Antimicrobial Resistance Surveillance System 2017 Report
Download the entire report
(PDF format, 628 KB, 126 pages)
Organization: Public Health Agency of Canada
Published: 2017-11-06
Executive Summary
Message from the Chief Public Health Officer and the President of the Public Health Agency of Canada
Antimicrobial resistance (AMR) continues to be one of the most significant public health threats facing the world today. Drug resistant infections threaten healthcare as we know it, as it erodes our ability to prevent and treat infections. In Canada, although overall rates of AMR have remained stable in recent years, they are still well above levels we saw in the early 2000s. Collective and continued efforts to reduce the rates of AMR and preserve the effectiveness of existing antimicrobials are essential to ensuring our ability to fight infectious diseases.
September 2017 marked the release of Tackling Antimicrobial Resistance and Antimicrobial Use: A Pan-Canadian Framework for Action (Framework). The Framework resulted from collaborative efforts on the part of the federal government, provinces and territories and other key partners in the human and animal health sectors. It was designed to guide efforts across sectors to address AMR and antimicrobial use (AMU), with a focus on four key components: surveillance, stewardship, infection prevention and control, and research and innovation. The Canadian Antimicrobial Resistance Surveillance System (CARSS) provides a foundation of evidence upon which to build even greater integration.
Through the synthesis and analysis of information from PHAC's surveillance systems and laboratory reference services, CARSS provides an integrated picture of AMR and AMU in Canada. Making progress towards addressing the gaps identified in last year's report, the CARSS-2017 Report provides more surveillance data on AMR in priority organisms and on infections occurring in the community. It also presents new information on AMU among non-physician prescribers and expanded AMR surveillance in food-producing animals.
PHAC relies on relationships and the collective efforts of many partners to provide a more comprehensive view of AMR/AMU in Canada. We thank all contributors for their time and continued support and we look forward to new and continued collaborations to improve AMR and AMU surveillance in Canada.

Dr. Siddika Mithani
President, Public Health Agency of Canada
Dr. Theresa Tam
Chief Public Health Officer of Canada
Introduction
The Canadian Antimicrobial Resistance Surveillance System (CARSS) is Canada's national surveillance system for reporting on antimicrobial resistance (AMR) and antimicrobial use (AMU). CARSS integrates and synthesizes information from Public Health Agency of Canada (PHAC) surveillance systems and laboratory reference services, covering both human and food-producing animal populations. CARSS aims to provide evidence to support policy and programming to foster prudent AMU, and to prevent, limit, and control AMR in Canada. It is a core component of Tackling Antimicrobial Resistance and Antimicrobial Use: A Pan-Canadian Framework for ActionFootnote 1.
The CARSS-2017 Report provides a snapshot of 2015 and 2016 AMR and AMU data in Canada. In addition, it presents new information on antimicrobial resistant infections occurring in the community setting, antimicrobial prescribing practices among dentists, AMR and AMU on sentinel turkey farms, and AMU in companion animals.
In 2014, the Public Health Network's Communicable and Infectious Disease Steering Committee (CIDSC) and PHAC reviewed a proposed list of microorganisms that have shown resistance to antimicrobials. From this list, the CIDSC AMR Task Group identified the microorganisms of greatest importance to public health in Canada, and as such, of priority for national surveillanceFootnote 2. The technical information presented on the priority microorganisms in each CARSS publication is adapted as a result of data updating, data availability, and changing AMR information needs identified through ongoing consultation with stakeholders. In this way, CARSS endeavors to be flexible and responsive to issues related to AMR and AMU surveillance in Canada.
International comparisons between Canada and other countries with respect to AMR can only be made when data are presented at the national level, and are collected using comparable methodologies. While some Canadian data on antimicrobial resistant microorganisms are collected and reported in a way that allows for international comparison, most are not. Despite this challenge, the CARSS-2017 Report aims to provide an international perspective on AMR and AMU, where appropriate, to give greater context to the surveillance findings for Canada.
Although PHAC surveillance systems are producing useful, reliable data on AMR and AMU, there are areas for improvement. The CARSS-2017 Report describes the current limitations of Canada's AMR and AMU surveillance and provides an update on efforts planned or underway to address existing surveillance gaps.
The CARSS-2017 Report is divided into two parts. Part one is an executive summary that highlights AMR and AMU surveillance findings in Canada. Part two is a technical annex that provides a detailed look at AMR and AMU surveillance data. The technical annex has an AMR section that focuses on each priority microorganism and describes the surveillance methods used. The technical annex's AMU section provides information on antimicrobials intended for people. Data on human AMU focuses on the amount of antimicrobials dispensed through community pharmacies, prescriber specialization breakdowns, hospital purchasing of antimicrobials, and indications for antimicrobial use.
Executive Summary
Antimicrobial Resistance and Antimicrobial Use
From 2011 to 2016, Canada reported AMR rates that were similar to or lower than rates reported by many other developed countriesFootnote 3 Footnote 4 Footnote 5. While Canadian AMR infection rates relating to antimicrobial resistant organisms have fluctuated over recent years, upward trends were seen in the rate of methicillin-resistant Staphylococcus aureus (MRSA) blood stream infection (BSI) in pediatric hospitals, and the rate of vancomycin-resistant Enterococcus (VRE) BSI in adult hospitals. In addition, the rate of drug-resistant gonorrhea increased between the years 2014 and 2015. Conversely, rates of healthcare-associated Clostridium difficile infection (CDI) decreased over time.
Examining human antimicrobial use in the community in Canada, the rate of prescriptions dispensed was relatively stable between 2013 and 2016 and slightly lower than the rates observed between 2010 and 2012. Newfoundland and Labrador had the highest rate of prescriptions dispensed in the community in 2016; British Columbia had the lowest. In 2015, Canada was 13th lowest among 31 countries in consumption of antimicrobials, a slightly worse showing than in 2014 when Canada placed 12th among 31 countries in antimicrobial consumption. The antimicrobial prescribing rate among physicians and dentists is generally stable, following an increase seen in prescribing by dentists from 2010 to 2012. In terms of antimicrobial use in the hospital setting, the purchasing of antimicrobials remained stable between 2010 and 2016. In 2016, Manitoba, Prince Edward Island, and Newfoundland and Labrador had the highest antimicrobial purchasing rates per capita; Ontario and Alberta had the lowest rates. Of concern, hospitals in 2016 purchased more antimicrobials considered "last resort" (e.g., daptomycin) than in previous yearsFootnote 6.
The key findings on AMR and AMU surveillance are presented below.
Antimicrobial resistance
The promotion of standardized infection prevention and control techniques, in combination with antimicrobial stewardship, contribute to reducing the spread of infections, inappropriate prescribing, and in turn, help prevent the development of AMR in Canada. However, despite the relatively low rates of AMR observed in Canada, there are areas of concernFootnote 7.
Clostridium difficile (C. difficile), the bacteria responsible for C. difficile infection (CDI), may be a consequence of standard drug treatments routinely prescribed for unrelated infections, as C. difficile bacteria are naturally resistant to many antimicrobials and spread rapidly once competing microorganisms have been eliminated by these drugsFootnote 8. In 2016, rates of healthcare-associated CDI(HA-CDI) in Canada continued to decline. The overall rate of HA-CDI decreased from 6.64 cases per 10,000 patient-days in 2011 to 4.05 cases per 10,000 patient-days in 2016 (Figure 1). When types of hospitals were compared, the 2016 rate of HA-CDI continued to be higher in adult hospitals than in pediatric hospitals (4.50 and 3.25 cases per 10,000 patient-days, respectively). Surveillance of community-associated (CA)-CDI in sentinel hospitals began in 2015 and will continue for three years. First year surveillance data (2015) showed that 37% of all CDI reported among patients admitted to sentinel hospitals were community-associated. This proportion is similar to other proportions of CA-CDI that have been reported in the literatureFootnote 5.
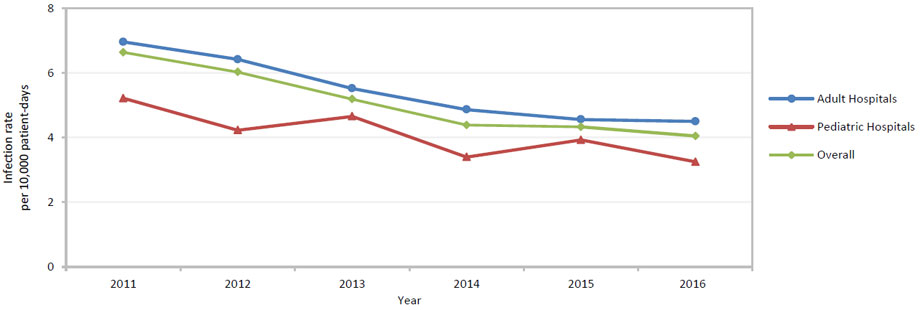
Figure 1 - Text Equivalent
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|
| Adult Hospitals | 6.96 | 6.42 | 5.52 | 4.87 | 4.56 | 4.50 |
| Pediatric Hospitals | 5.22 | 4.23 | 4.66 | 3.40 | 3.93 | 3.25 |
| Overall | 6.64 | 6.03 | 5.19 | 4.39 | 4.33 | 4.25 |
This line graph demonstrates the infection rate of clostridium difficile per 10,000 patient days by hospital type in Canada from 2011-2016. The horizontal axis represents the year and the vertical axis the infection rate.
A critical indicator for AMR in Enterobacteriaceae is resistance to the carbapenem class of antimicrobials. Infections caused by carbapenemase-producing Enterobacteriaceae (CPE) are generally multidrug-resistant, have limited treatment options, and are associated with poor health outcomes, making them a serious public health concern worldwideFootnote 9. Globally, infection rates of CPE and other carbapenemase-producing organisms have increased over timeFootnote 4 Footnote 5, while rates of CPE in sentinel Canadian hospitals have remained low and relatively stable. From 2011 to 2014, the overall rate of CPE in sentinel hospitals decreased from 0.13 cases to 0.07 cases per 10,000 patient-days. In 2015, this rate increased very slightly to 0.08 cases per 10,000 patient-days. In contrast, the number of CPE isolates voluntarily reported to provincial public health laboratories increased from 4 in 2009 to 779 in 2016. The greatest annual increase (1.8 fold) occurred between 2015 and 2016. This discrepancy between sentinel hospitals and laboratory surveillance findings may be due to increased cases of CPE infection in the community or among hospitals not represented in the group of hospitals under surveillance; increased awareness of and reporting of CPE; and/or other factors not yet identified.
First described in 1961, methicillin-resistant Staphylococcus aureus (MRSA) is a S. aureus that has acquired resistance to anti-staphylococcal β-lactam antibiotics (e.g., methicillin, oxacillin, and cefazolin). While MRSA has historically been associated with hospitals and other healthcare settings (healthcare-associated MRSA [HA-MRSA]), community-associated MRSA (CA-MRSA) is increasingly being observed as a cause of illness in Canada and elsewhereFootnote 3 Footnote 4 Footnote 5. The overall rate of MRSA infection in sentinel hospitals in Canada increased from 2.84 cases to 3.13 cases per 10,000 patient-days between 2011 and 2016. However, this rate remained below the 2009 rate of 3.78 cases per 10,000 patient-days. When hospitalized cases were compared by area of acquisition, the overall rate of HA-MRSA infection decreased between 2011 and 2016 (from 1.93 to 1.69 cases per 10,000 patient-days, respectively), while the overall rate of CA-MRSA infection increased during the same time period (from 0.56 to 0.96 cases per 1,000 admissions). From 2011 to 2016, the rate of CA-MRSA infection in pediatric hospitals was consistently higher than the rate in adult and mixed-patient hospitals (i.e., 1.56, 1.02, and 0.75 cases per 1,000 patient admissions in 2016, respectively). The rate of HA-MRSA blood stream infection (BSI) in adult hospitals was relatively stable from 2011 to 2016 (0.47 to 0.44 cases per 10,000 patient-days), whereas the rate of HA-MRSA BSI in pediatric hospitals increased more than fivefold (rising from 0.08 to 0.43 cases per 10,000 patient-days between 2011 and 2016) (Figure 2). This increase in pediatric BSI is concerning and requires closer monitoring.
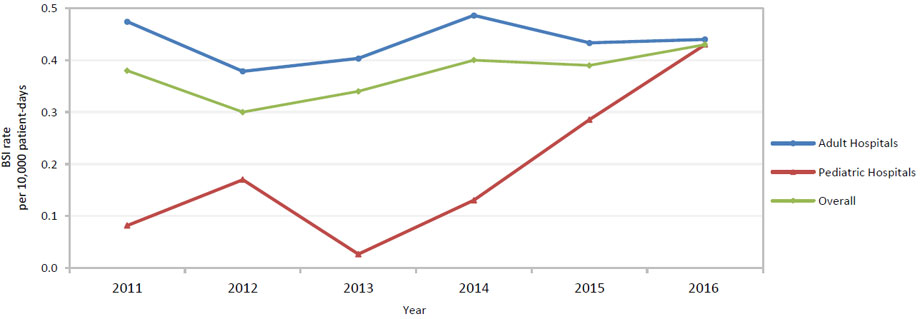
Figure 2 - Text Equivalent
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|
| Adult Hospitals | 0.47 | 0.38 | 0.40 | 0.49 | 0.43 | 0.44 |
| Pediatric Hospitals | 0.08 | 0.17 | 0.03 | 0.13 | 0.29 | 0.43 |
| Overall | 0.38 | 0.30 | 0.34 | 0.40 | 0.39 | 0.43 |
This line graph demonstrates the rate of healthcare-associated methicillin-resistant Staphylococcus aureus infections per 10,000 patient days by hospital type in Canada from 2011-2016. The horizontal axis represents the year and the vertical axis the infection rate.
Vancomycin-resistant enterococci (VRE) infections have limited treatment options, and are the focus of international surveillance effortsFootnote 3 Footnote 4 Footnote 5 Footnote 7. VRE in Canada has historically been associated with healthcare facilities, and the burden of VRE in the community is unknown. The overall rate of VRE infections in Canada increased sharply between 2007 (0.10 cases per 10,000 patient-days) and 2012 (0.61 cases per 10,000 patient-days), and then declined to 0.41 cases per 10,000 patient-days in 2015 (Figure 3). The rate increased slightly in 2016 to 0.44 cases per 10,000 patient-days. When compared by type of hospital and site of infection, the rate of VRE BSI in sentinel adult hospitals more than doubled between 2011 (0.12 cases per 10,000 patient-days) and 2016 (0.26 cases per 10,000 patient-days).This finding points to the need for ongoing monitoring of this microorganism in Canada.
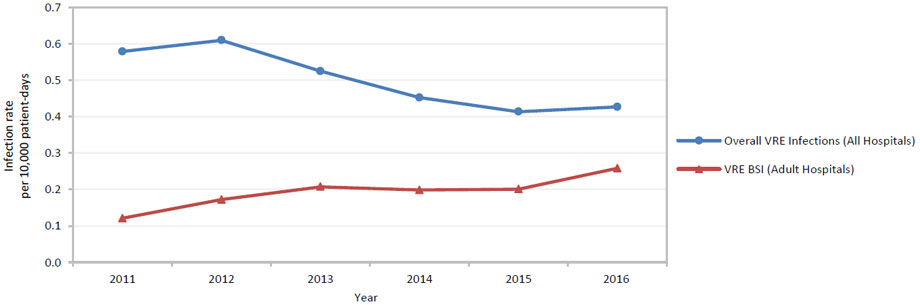
Figure 3 - Text Equivalent
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|
| Overall VRE Infections (All Hospitals) | 0.58 | 0.61 | 0.52 | 0.45 | 0.41 | 0.43 |
| VRE BSI (Adult Hospitals) | 0.12 | 0.17 | 0.21 | 0.20 | 0.20 | 0.26 |
A line graph showing the rate of overall vancomycin-resistant enterococci infections, and vancomycin-resistant enterococci bloodstream infections per 10,000 reported cases in Canada from 2011 to 2016. The horizontal axis represents the year and the vertical axis the infection rate per 100,000 reported cases.
Gonorrhea (caused by Neisseria gonorrhoeae) is one of the most commonly reported bacterial sexually transmitted infections (STI) in CanadaFootnote 10. The overall rate of gonorrhea more than doubled, from 21.8 cases per 100,000 population in 2001 to 55.4 cases per 100,000 population in 2015. The treatment and control of gonorrhea are major public health challenges worldwideFootnote 7 Footnote 11, due to the emergence and spread of AMR in N. gonorrhoeae. In Canada, the proportion of N. gonorrhoeae isolates resistant to many antimicrobials continued to rise in 2015 (Figure 4). Between 2014 and 2015, the proportion of cultured isolates resistant to at least one antimicrobial increased from 52% to 60%. Between 2010 and 2015, the proportion of azithromycin-resistant N. gonorrhoeae increased from 1.3% to 4.7%. When the proportion of antimicrobial-resistant N. gonorrhoeae strains obtained from isolates is at a level of 5% or more, or when an unexpected increase below 5% is observed in key populations with high rates of gonococcal infection, the World Health Organization recommends that countries review and modify their national guidelines for STI treatment and managementFootnote 12, a best practice that Canada implements. Isolates with decreased susceptibility to cefixime or ceftriaxone, two cephalosporin class antimicrobials used to treat gonorrhea, also increased between 2014 and 2015 (from 1.1.% to 1.9% and 2.7% to 3.5%, respectively). From 2012 to 2014, there was a very small proportion of isolates in Canada observed to be both resistant to azithromycin and to have decreased susceptibility to cephalosporins (cefixime or ceftriaxone), the currently recommended dual therapy treatment for gonorrhea (0.2% in 2012, 0.3% in 2013, and 0.03% in 2014, respectively). The United Kingdom reported the world's first dual therapy treatment failure in 2015Footnote 12. While Canada has had no reported treatment failures resulting from resistance to azithromycin and decreased susceptibility to cephalosporins, these findings highlight the need for ongoing monitoring of drug-resistant N. gonorrhoeae, and the appropriate use of antimicrobials to help maintain the effectiveness of current treatment regimens.
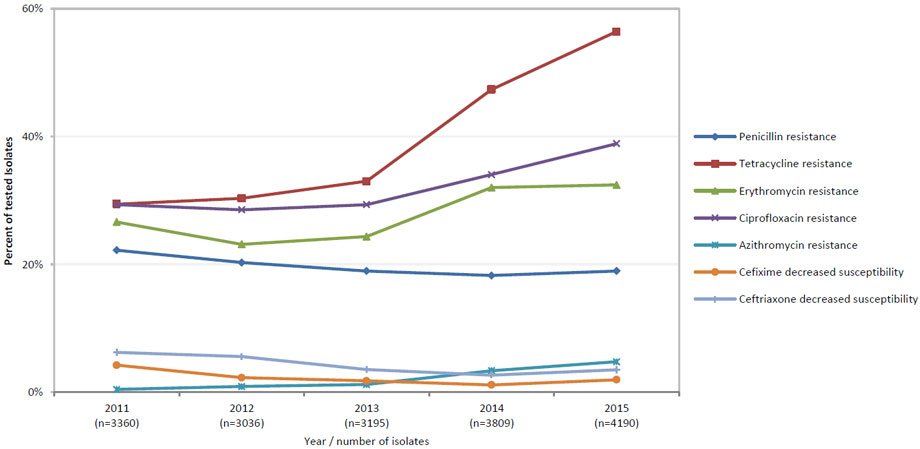
Figure 4 - Text Equivalent
| 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|
| Penicillin Resistance | 22.2 | 20.26 | 18.94 | 18.22 | 18.93 |
| Tetracycline Resistance | 29.4 | 30.3 | 32.99 | 47.34 | 56.42 |
| Erythromycin Resistance | 26.6 | 23.12 | 24.32 | 32 | 32.41 |
| Ciprofloxacin Resistance | 29.3 | 28.52 | 29.33 | 34.02 | 38.88 |
| Azithromycin Resistance | 0.39 | 0.86 | 1.16 | 3.33 | 4.73 |
| Cefixime Decreased Susceptibility | 4.2 | 2.24 | 1.75 | 1.1 | 1.91 |
| Ceftriaxone Decreased Susceptibility | 6.2 | 5.53 | 3.51 | 2.65 | 3.46 |
The line graph presents the percentage of gonorrhea isolates that are resistant to different antimicrobials (each represented by its own line) in Canada from 2011 to 2015. The horizontal axis represents the year and the vertical axis the percentage of isolates.
Antimicrobial use in humans
The use of antimicrobials is a major factor in the emergence and spread of resistant microorganisms. Prudent AMU is recognized as a core element in managing the risks of AMR to preserve the effectiveness of antimicrobials and slow the development of drug-resistant organisms. Programs and policies that highlight education, awareness-raising, as well as professional and regulatory oversight help foster rational prescribing, and use of antimicrobials in humans. AMR and AMU surveillance provide data for action to guide antimicrobial stewardship effortsFootnote 13.
Antimicrobial use in the community
In Canada, the majority of antimicrobials used by humans are available by prescription only. In 2016, an estimated 92% of doses of antimicrobials were dispensed in the community, while the remaining proportion (8%) was purchased for use in hospitals (Figure 5). The proportion of community dispensed antimicrobials did not change from previous yearsFootnote 14. In 2016, an estimated 22.6 million prescriptions were dispensed in Canada, with a total expenditure of nearly 700 million dollars. The rate of antimicrobial prescriptions dispensed in the community setting was relatively stable between 2013 and 2016 (approximately 625 prescriptions per 1,000 inhabitants) and slightly lower than the rates observed between 2010 and 2012 (660 to 683 prescriptions per 1,000 inhabitants). In 2016, amoxicillin was the most frequently prescribed antimicrobial (25% of prescriptions), followed by azithromycin (10% of prescriptions). In 2016, the rate of prescriptions dispensed in adults 60 years and older was 856 prescriptions per 1,000 inhabitants, nearly 1.5 times higher than rates in the 0 to 14 year and 15 to 59 year age groups (598 and 547 prescriptions per 1,000 inhabitants, respectively). Amoxicillin, ciprofloxacin, and cephalexin were the antimicrobials most commonly prescribed in the oldest age group.
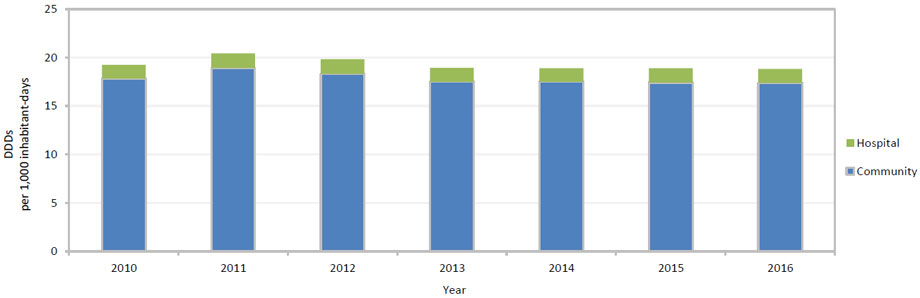
Figure 5 - Text Equivalent
| Community | Hospital | |
|---|---|---|
| 2010 | 17.8 | 1.4 |
| 2011 | 18.9 | 1.5 |
| 2012 | 18.3 | 1.5 |
| 2013 | 17.5 | 1.4 |
| 2014 | 17.5 | 1.4 |
| 2015 | 17.4 | 1.5 |
| 2016 | 17.4 | 1.4 |
This figure is a stacked bar graph with each bar depicting the defined daily doses (DDDs) per 1,000 inhabitant-days in Canada, from both hospital purchase and community prescription data from 2010-2016. The horizontal axis represents the year while the vertical axis is the defined daily doses per 1,000 inhabitant days.
In 2015, the European Surveillance of Antimicrobial Consumption Network (ESAC-Net) reported the overall consumption of antimicrobials for systemic use (J01) in both hospital and community settings for participating European countriesFootnote 5. ESAC-Net is a good candidate for human AMU comparisons to Canada, as ESAC-Net represents one of the largest, internationally standardized AMU data sources and uses methods comparable to Canada. Comparing 2015 outpatient consumption in Europe with 2015 Canadian community consumption (community pharmacist dispensing), Canada ranked 13th out of 31 countries (ranked from lowest to highest consumption), a slightly worse showing than in 2014 when Canada was 12th among 31 countries in community consumption of antimicrobials.
When data were compared by province in Canada, Newfoundland and Labrador had the highest prescription rate (955 prescriptions per 1,000 inhabitants) in 2016, a finding also observed in previous years. Prescription rates were lowest in British Columbia and among individuals covered by the Non-Insured Health Benefits (NIHB) program in the Territories (Figure 6). The reasons for these provincial differences are currently being explored. While use of most antimicrobials was higher in Newfoundland and Labrador than in other provinces, amoxicillin was prescribed at particularly high rates (data not shown).
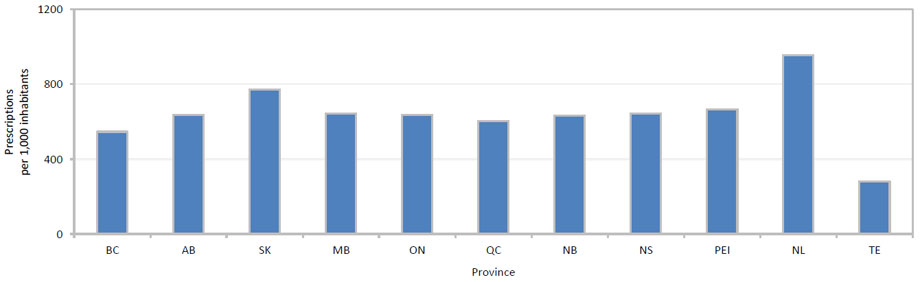
Figure 6 - Text Equivalent
| Province | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BC | AB | SK | MB | ON | QC | NB | NS | PEI | NL | TE | |
| Prescriptions (1,000 inhabitants) | 546.0 | 634.6 | 771.5 | 643.0 | 636.8 | 602.8 | 632.1 | 643.9 | 665.6 | 955.2 | 279.7 |
This bar graph shows the rate of antimicrobial prescriptions per 1,000 inhabitants in each of the provinces and territories in Canada in 2016. The horizontal axis contains the provinces and territories, and the vertical axis shows the rate of prescriptions per 1,000 inhabitants.
Notes: BC = British Columbia, AB = Alberta, SK = Saskatchewan, MB = Manitoba, ON = Ontario, QC = Québec, NB = New Brunswick, NS = Nova Scotia, PEI = Prince Edward Island, NL = Newfoundland and Labrador, TE = Territories (Yukon, Northwest Territories, and Nunavut)
In 2016, family physicians accounted for 65% of all prescriptions dispensed by community pharmacies in Canada. The most commonly prescribed antimicrobials by all physicians in private practice were amoxicillin, azithromycin, and cephalexin. As seen in previous years, antimicrobials were most often prescribed for respiratory infections, followed by genito-urinary system infections, and skin and soft tissue infections. In 2015, physicians in private practice wrote 446 antimicrobial prescriptions per 1,000 inhabitants, while the rate for dentists was 47 prescriptions per 1,000 inhabitants (Figure 7). Data in 2015 showed a downward trend in the antimicrobial prescribing rate of physicians and a generally stable rate for dentists, following an increase seen in prescribing by dentists from 2010 to 2012.
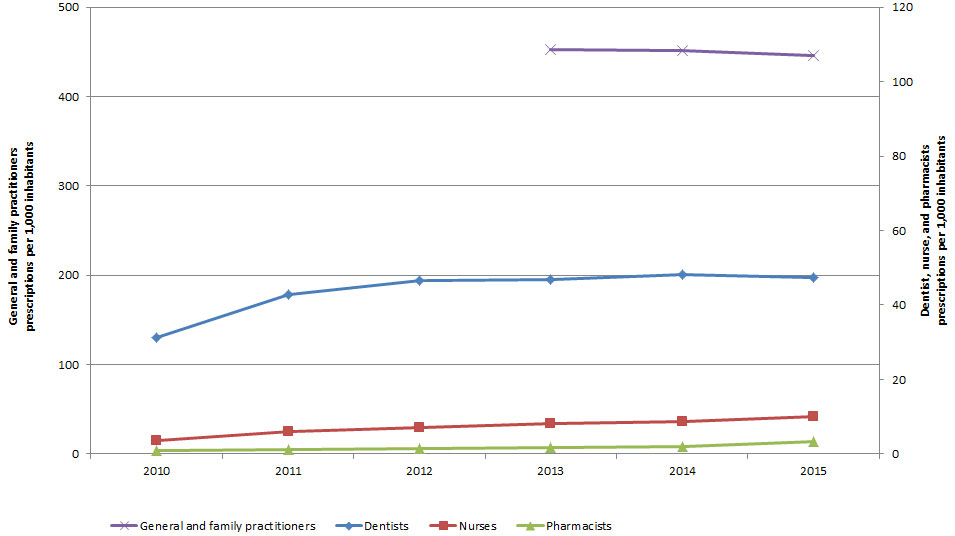
Figure 7 - Text Equivalent
| Dentists | Nurses | Pharmacists | General and family practitioners | |
|---|---|---|---|---|
| 2010 | 31.3 | 3.4 | 1.0 | N/A |
| 2011 | 42.7 | 6.0 | 1.3 | N/A |
| 2012 | 46.6 | 7.2 | 1.3 | N/A |
| 2013 | 46.9 | 8.1 | 1.6 | 452.2 |
| 2014 | 48.2 | 8.8 | 2.0 | 451.3 |
| 2015 | 47.4 | 10.0 | 3.3 | 445.7 |
The line graph in figure 7 show the rate of prescriptions dispensed in the community. The horizontal axis contains the years from 2010-2015. The figure employs two vertical axes, one with a range of 0-120 to cover the rate of prescriptions per 1,000 inhabitants dispensed by dentists, nurses, and pharmacists. The second vertical axis has a range of 0-500 and covers general and family practitioners prescriptions per 1,000 inhabitants.
Antimicrobial use in the hospital setting
In 2016, 8% of antimicrobial doses in Canada were purchased for use in the hospital setting (Figure 5); this proportion was unchanged from previous years. The rate of antimicrobial purchasing by hospitals varied throughout Canada during the surveillance period. In 2016, Manitoba, as well as Prince Edward Island and Newfoundland and Labrador combined, had the highest antimicrobial purchasing rates per capita (2.7 and 2.3 defined daily doses [DDDs] per 1,000 inhabitant-days, respectively). Ontario and Alberta had the lowest rates (1.0 and 1.3 DDDs per 1,000 inhabitant-days, respectively).
Cephalosporins were the most purchased antimicrobial drug class by hospitals in Canada in 2016, similar to previous years, followed by fluoroquinolones. While the rate of cephalosporin purchasing remained relatively stable from 2010 to 2016, the rate of purchasing of fluoroquinolones decreased by 43% during the same time period (0.25 to 0.17 DDDs per 1,000 inhabitant-days). Between 2010 and 2016, the purchasing rate for two drug classes, penicillin combinations (e.g., penicillins with an enzyme inhibitor) and β-lactamase sensitive penicillins (e.g., penicillin G), increased by 41% (0.09 to 0.15 DDDs per 1,000 inhabitant-days) and 34% (0.05 to 0.07 DDDs per 1,000 inhabitant-days), respectively. Of concern, hospital purchasing of daptomycin, one of the "last resort" antibiotics, increased in 2016. Daptomycin is generally reserved for use in the treatment of life-threatening S. aureus and Enterococcus infectionsFootnote 6. The reason for this increase is not known.
Antimicrobial use in food-producing and companion animals
Just as use of antimicrobials in humans can lead to the development and persistence of AMR, use of antimicrobials in food-producing and companion animals may also contribute to antimicrobial resistant bacteria. Such bacteria may then be transferred to humans through direct contact with animals, as well as foodborne or waterborne routes. Surveillance of antimicrobial use in animals, crops, and people provides important data to guide antimicrobial stewardship efforts and to contain AMR in Canada.
In 2016, approximately 1.0 million kilograms of medically important antimicrobials were distributed for sale for use in animals by the Canadian Animal Health Institute (CAHI) member companies. This volume was approximately 14% lower than 2007 and 17% lower than 2015. These reported quantities do not include antimicrobials imported for 'own use' or as active pharmaceutical ingredients intended for further compounding. Additionally, there were 0.6 million kg of ionophores and chemical coccidiostats distributed for use in animals (these antimicrobials are not considered medically important). In 2016, 99% of the antimicrobials distributed were intended for use in food-producing animals and 1% was intended for use in companion animals (based on kilograms of active ingredient).
The overall quantity of fluoroquinolones distributed for use in animals decreased by approximately 56% between 2015 and 2016. Fluoroquinolones are classified as "of very high importance to human medicine" by Health Canada's Veterinary Drugs Directorate. Fluoroquinolones are licensed for use in certain animal species in Canada and have warnings on their labels recommending against extra-label use due to AMR concerns and guidelines for use only after failure of an initial treatmentFootnote 15.
Between 2012 and 2016, there were provincial differences in the kilograms of active ingredient of antimicrobials distributed for sale by CAHI member companies, and year-to-year differences within provinces in the quantities distributed. The provinces with the greatest declines since 2015 (as relative percentages of their 2015 kilogram total) were New Brunswick, Manitoba, Nova Scotia, Newfoundland and Labrador, Saskatchewan, and Québec (decrease of >15% of total kg each). The only province with an increase in total kg active ingredient distributed for sale was Prince Edward Island (approximately 20% increase in kg).
The European Surveillance of Veterinary Antimicrobial Consumption (ESVAC) collects and reports information from member countries on antimicrobial agents intended for use in animals. ESVAC is a good candidate for animal AMU comparisons to Canada, as ESVAC is the only current multinational source of quantitative surveillance data on antimicrobial agents intended for use in animals. Canada uses reporting metrics similar to ESVAC, with the notable exception that Canada includes beef cows in the denominator. Using the latest ESVAC data (2015) and the latest Canadian data (2016), out of 31 countries, Canada was the fifth highest for consumption of antimicrobials measured as milligram of drug per kilogram of animal (equivalent to milligram per population corrected unit)Footnote 16. In 2016, Canada had higher consumption than the reported average for the participating European countries. Canada would report more antimicrobials per kg animal if the currently unknown quantities of antimicrobials imported for 'own use' or as active pharmaceutical ingredients for further compounding were included.
PHAC conducts farm level surveillance to describe trends in farm AMR and AMU and investigates associations between farm AMU and AMR to provide sound data for human health risk assessments. Farm-level surveillance indicated that a change in antimicrobial use policies on broiler chicken farms across Canada appeared to have achieved the desired goal of reducing the use of antimicrobial agents in classes considered of very high importance to human medicine, in particular the use of the antimicrobial ceftiofur (a 3rd generation cephalosporin).
Addressing surveillance data gaps
The CARSS-2017 Report provides a good overview of the current situation of AMR and AMU in Canada. There are strong data for specific AMR pathogens from large, tertiary hospitals. An added strength is the representation of AMR in foodborne bacteria from food-producing animals and food of animal origin. In addition, AMU information for both humans and animals has improved over time. For example, the reporting of AMU among Indigenous populations in Canada is now addressed in a more fulsome analysis, and PHAC has acquired farm-level data on how and why antimicrobials are used.
However, there are gaps that need to be addressed to increase the depth, breadth, and quality of AMR and AMU surveillance in Canada. For example, there are limited data on antimicrobial-resistant organisms in the community. There are also limited data on AMR in smaller, non-academic hospitals; Indigenous populations; AMR in long term-care facilities; and nor or limited data for northern healthcare settings. In addition, there are no or limited data on the appropriateness of antimicrobials that are prescribed.
AMR data along the food chain for animals and humans are restricted to specific bacterial organisms (e.g., Salmonella). The livestock species covered include the major meat-producing animals in Canada (e.g., cattle, pigs, broiler chickens, and turkeys) while no on-going surveillance is currently underway for other animal production areas (e.g., aquaculture, veal, and sheep). Farm-level AMU data are currently limited to sentinel farms in swine and poultry.
Since the release of the first CARSS report in 2015, PHAC has collaborated with a range of partners representing public health, health care, agriculture, and other sectors to address identified gaps and improve AMR and AMU surveillance in Canada. PHAC surveillance programs have many initiatives planned, under way, or recently completed to collect new data or to enhance the use of existing AMR or AMU data. Examples of such initiatives include:
- a point prevalence study on AMR and AMU in smaller community, rural, and Northern community-based hospitals, and long term-care facilities;
- an AMU 'Rapid Response' module in the Canadian Community Health Survey (CCHS) to provide answers to common questions on AMU and information on personal antibiotic stewardship practices;
- a three-year study of hospitalized cases of community-associated Clostridium difficile;
- turkey and nursery pig surveillance studies to examine AMU and AMR on farms; and
- a five-year study that will provide a greater understanding of how food production practices contribute to the development of AMR of human health concern.
Next steps/conclusions
The evolving epidemiology of AMR in Canada, and the growing threat of AMR globally, underscore the need for ongoing monitoring of this public health event. PHAC continues to address AMR and AMU surveillance gaps in partnership with other federal departments, the provinces and territories, non-governmental organizations, professional associations, and academia. To this end, PHAC is implementing a number of initiatives over the next several years to enhance surveillance information, with the goals of improving Canada's ability to respond to emerging AMR threats and supporting antimicrobial stewardship efforts by providing better evidence for decision-making.
Global problems require global solutions. Work is currently under way by PHAC to harmonize its surveillance methods in order to participate in international programs stemming from the Global Action Plan on Antimicrobial Resistance. These programs include the World Health Organization's Global Antimicrobial Resistance Surveillance System (GLASS) and the World Organization for Animal Health's global database on antimicrobial agents intended for use in animals. The first data contributions to GLASS by PHAC occurred in 2017, with the submission of 2015 human Salmonella data. Full participation is targeted for 2019. In addition to taking part in global programs, PHAC is committed to working with its international partners in other ways to identify common approaches and best practices to prevent, limit, and control the development and spread of AMR in Canada and worldwide.
References
- Footnote 1
-
Public Health Agency of Canada. Tackling Antimicrobial resistance and antimicrobial use: A pan-Canadian framework for action. Infectious Disease Prevention and Control Branch. Ottawa: Public Health Agency of Canada; 2017. [Internet] Available from: https://www.canada.ca/en/health-canada/services/publications/drugs-health-products/tackling-antimicrobial-resistance-use-pan-canadian-framework-action.html
- Footnote 2
-
Pan-Canadian Public Health Network. Antimicrobial resistance surveillance data requirements for priority organisms. The Communicable and Infectious Disease Steering Committee Antimicrobial Resistance Surveillance Task Group. Final Report to Public Health Network Council. Ottawa: April 2016. [Internet] Available from: http://www.phn-rsp.ca/pubs/arsdrpo-dsecrao/index-eng.php
- Footnote 3
-
Australian Commission on Safety and Quality in Health Care (ACSQHC). AURA 2016: First Australian report on antimicrobial use and resistance in human health. Sydney: Australian Commission on Safety and Quality in Health Care; 2016. [Internet] Available from: https://www.safetyandquality.gov.au/wp-content/uploads/2017/01/AURA-2016-First-Austarlian-Reprot-on-Antimicrobial-use-and-resistance-in-human-health.pdf
- Footnote 4
-
Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2013. [Internet] Available from: https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf#page-53
- Footnote 5
-
European Centre for Disease Prevention and Control (ECDC). Summary of the latest data on antimicrobial resistance in EU. Stockholm: European Centre for Disease Prevention and Control; 2016. [Internet] Available from: https://ecdc.europa.eu/sites/portal/files/documents/antibiotics-EARS-Net-summary-2016_0.pdf
- Footnote 6
-
World Health Organization. Critically important antimicrobials in human medicine, 5th edition. Geneva: World Health Organization. 2016. [Internet] Available from: http://www.who.int/foodsafety/publications/antimicrobials-fifth/en/
- Footnote 7
-
World Health Organization. Antimicrobial resistance: Global report on surveillance. Geneva: World Health Organization; 2014. [Internet] Available from: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf
- Footnote 8
-
Bloomfield LE, Riley TV. Epidemiology and risk factors for community associated Clostridium difficile infection: a narrative review. Infect Dis Ther 2016 Sep: 5(3): 231-251. doi: 10.1007/s40121-016-0117-y
- Footnote 9
-
van Duin D, Kaye KS, Neuner EA, Bonomo RA. Carbapenem-resistant Enterobacteriaceae: a review of treatment and outcomes. Diagn Microbiol Infect Dis. 2013 Feb;75(2):115-20 https://doi.org/10.1016/j.diagmicrobio.2012.11.009 [Internet] Available from: http://www.sciencedirect.com/science/article/pii/S0732889312004920
- Footnote 10
-
Public Health Agency of Canada. Canadian Guidelines on sexually transmitted infections, Gonococcal infections. Infectious Disease Prevention and Control, [Directorate]. Ottawa: Public Health Agency of Canada; Revised July 2013. [Internet] Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-34.html
- Footnote 11
-
World Health Organization. Global action plan to control the spread and impact of antimicrobial resistance in Neisseria gonorrheaae. Geneva: World Health Organization; 2012. [Internet] Available from: http://apps.who.int/iris/bitstream/10665/44863/1/9789241503501_eng.pdf
- Footnote 12
-
Fifer H, Natarajan U, Alexander S, Golparian D. Failure of dual antimicrobial therapy in treatment of Gonorrhea. N Engl J Med. 2016 Jun; 374:2504-2506. doi: 10.1056/NEJMc1512757
- Footnote 13
-
Khan F, Arthur J, Maidment L, Blue D. Advancing antimicrobial stewardship: Summary of the 2015 CIDSC Report. CCDR. 2016 Dec; 42-12: 238-241. Available from: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/ccdr-rmtc/16vol42/dr-rm42-11/assets/pdf/16vol42_11-eng.pdf
- Footnote 14
-
Finley R, Glass-Kaastra SK, Hutchinson J, Patrick DM, Weiss K, Conly J. Declines in outpatient antimicrobial use in Canada (1995-2010). PLoS ONE 8(10): e76398. https://doi.org/10.1371/journal.pone.00763989
- Footnote 15
-
Health Canada. Categorization of antimicrobial drugs based on importance in human medicine. [Branch], [Directorate]. Ottawa: Health Canada; (Version - April, 2009) [Internet] Available from: https://www.canada.ca/en/health-canada/services/drugs-health-products/veterinary-drugs/antimicrobial-resistance/categorization-antimicrobial-drugs-based-importance-human-medicine.html
- Footnote 16
-
European Medicines Agency, European Surveillance of Veterinary Antimicrobial Consumption, 2017.'Sales of veterinary antimicrobial agents in 30 European countries in 2015'. (EMA/184855/2017). [Internet] Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Report/2017/10/WC500236750.pdf. Accessed October 2017.