Archived FoodNet Canada Short Report 2015
Table of Contents
- Acknowledgements
- Introduction
- Human Case Summary
- Retail Component
- Agricultural Component
- Water Component
- Summary
Acknowledgments
The Public Health Agency of Canada acknowledges the significant investments made by our partners in all FoodNet Canada sentinel sites, our provincial and federal government agency colleagues, and academic and industry collaborators who help to make this program a continued success.
Introduction
The Public Health Agency of Canada's (PHAC) FoodNet Canada (FNC) integrated enteric pathogen surveillance system is based on a sentinel site surveillance model, which collects information on cases of infectious gastrointestinal illness and sources of exposure within defined communities. These data are analyzed to assist in determining what food and other sources are making Canadians ill and to accurately track disease with time. FNC's primary objectives are to (1) determine what food and other sources are making Canadians ill; (2) determine significant risk factors for enteric illness; (3) accurately track disease rates and risks over time; (4) provide practical prevention information to prioritize risks, compare interventions, direct actions, advance policy, and assess effectiveness of food safety activities and public health interventions and measure performance.
Download the alternative format
(PDF format, 927 Kb, 31 pages)
Organization: Public Health Agency of Canada
Type: Report
ISSN: 2292-8073
Published: January 2017
In 2015, the PHAC FNC surveillance system consisted of three sentinel sites; the Ontario (ON) site in the Middlesex-London Health Unit (MLHU) (FNC site period: Aug 2014-ongoing); the Alberta (AB) site in the Calgary and Central Zones of Alberta Health Services (AHS) (FNC site period: Jun 2014-ongoing); as well as the British Columbia (BC) site in the Fraser Health Authority (FHA) of lower mainland British Columbia (FNC site period: April 2010-ongoing). For the purpose of yearly comparisons in this Report, non-human data (2006-Mar 2014) from the ON pilot sentinel site (Region of Waterloo) have been included. In each sentinel site, enhanced human disease surveillance is performed in parallel with active surveillance of enteric pathogens in retail, animals and water sources.
This report presents the preliminary findings from the 2015 surveillance year across all sentinel sites. To be nationally representative, PHAC's FNC is designed to have five sites encompassing approximately 10% of the Canadian population. Note that FNC data need to be considered in the context of three active sentinel sites. This report will be followed by a comprehensive annual report, which will include more extensive analyses of temporal trends and subtyping information for an integrated perspective on enteric disease from exposure to illness.
For further information about FNC or FNC's sampling methodologies, please contact: phac-FoodNet.Canada-aspc@phac-aspc.gc.ca
Integration with PHAC's Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS)
PHAC's CIPARS monitors trends and the relationship between antimicrobial use and antimicrobial resistance in selected bacterial organisms from human, animal, and food sources across Canada to inform evidence-based policy decision making to contain the emergence and spread of resistant bacteria. Efforts have been ongoing towards better integrating PHAC's FNC and CIPARS. This includes the streamlining and sharing of sampling and sampling sites, retrospective and prospective testing of antimicrobial resistance in selected bacteria isolated from FNC samples, and improving data management mechanisms to maximize data linkages. For further information about CIPARS, please refer to the program's website.
Human Case Summary
The enhanced human disease surveillance component of PHAC's FNC is fully active in all three sentinel sites: BC, AB and ON. The FNC program was officially launched in the AB site in June 2014 and in the new ON site in August 2014. Since only partial year data are available for the ON and AB sites in 2014, comparisons were not made between the 2015 and 2014 rates for these sites.
PHAC's FoodNet Canada cases are classified into one of five groups - Endemic, Travel, Outbreak, Non-Endemic or Lost to Follow-Up (LTF):
Endemic cases: Reported cases of infection that are considered sporadic and domestically acquired (i.e., within Canada).
Travel-related cases: Reported sporadic cases that have travelled outside of Canada prior to onset of illness and the travel time overlapped with the expected disease incubation period (varies depending on the pathogen).
Outbreak-related cases: Reported cases found to be associated with a sudden increased occurrence of an infectious disease and whose illnesses are confirmed through a public health partner (AB, BC and ON sites) on the basis of laboratory and/or epidemiological evidence. This classification includes both domestically-associated outbreak cases and international travel-associated outbreak cases.
Non-endemic cases: Includes immigration-related cases where illness was acquired outside of Canada.
Lost to Follow-up (LTF): Reported cases that could not be followed-up with an interview by public health.
In 2015, campylobacteriosis, salmonellosis and giardiasis were the most commonly reported enteric diseases in FNC sentinel sites (Table 1).
Travel continues to be an important factor in the burden of enteric disease. In 2015, approximately 25% of all cases of enteric disease were associated with travel outside of Canada.
In 2015, a total of 47 outbreak-associated cases were reported in the sites: 33 Salmonella cases, 10 Verotoxigenic E. coli (VTEC) cases, two Campylobacter cases and one case each of Shigella and Cyclospora. Of the 47 outbreak-associated cases, two cases were associated with international travel.
| ON Site | AB Site | BC Site | National | ||||
|---|---|---|---|---|---|---|---|
| 2015 | 2015 | 2014 | 2015 | 2014 | |||
| Incidence Rate | Incidence Rate | Incidence Rate | Incidence Rate | Incidence Rate RatioFootnote a | Incidence Rate | ||
| AmoebiasisFootnote b | Total | 2.73 | 0.00 | 0.00 | . | -- | |
| Endemic | 1.26 | 0.00 | 0.00 | . | |||
| Travel | 0.63 | 0.00 | 0.00 | . | |||
| Outbreak | 0.00 | 0.00 | 0.00 | . | |||
| Non-Endemic | 0.00 | 0.00 | 0.00 | . | |||
| LTF | 0.84 | 0.00 | 0.00 | . | |||
| Campylobacteriosis | Total | 20.34 | 24.97 | 36.13 | 32.10 | 0.89 | 28.44 |
| Endemic | 10.07 | 15.85 | 24.59 | 21.90 | 0.89 | ||
| Travel | 5.24 | 5.25 | 8.34 | 6.38 | 0.76 | ||
| Outbreak | 0.42 | 0.00 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.21 | 0.00 | . | ||
| LTF | 4.61 | 3.86 | 2.99 | 3.83 | 1.28 | ||
| Cryptosporidiosis | Total | 3.57 | 3.86 | 1.92 | 1.70 | 0.88 | 2.50 |
| Endemic | 1.89 | 2.58 | 1.50 | 0.85 | 0.57 | ||
| Travel | 1.26 | 0.99 | 0.43 | 0.64 | 1.49 | ||
| Outbreak | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.42 | 0.30 | 0.00 | 0.21 | . | ||
| Cyclosporiasis | Total | 1.68 | 0.20 | 1.28 | 1.28 | 0.99 | 0.65 |
| Endemic | 0.21 | 0.00 | 0.21 | 0.00 | . | ||
| Travel | 1.26 | 0.20 | 0.86 | 1.28 | 1.49 | ||
| Outbreak | 0.21 | 0.00 | 0.21 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Giardiasis | Total | 10.91 | 10.70 | 9.83 | 10.21 | 1.04 | 10.26 |
| Endemic | 5.87 | 4.46 | 5.56 | 5.53 | 0.99 | ||
| Travel | 1.68 | 3.47 | 2.99 | 2.34 | 0.78 | ||
| Outbreak | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.42 | 2.08 | 0.00 | 0.85 | . | ||
| LTF | 2.94 | 0.69 | 1.28 | 1.49 | 1.16 | ||
| Listeriosis | Total | 0.00 | 0.10 | 0.64 | 0.00 | . | 0.41 |
| Endemic | 0.00 | 0.10 | 0.64 | 0.00 | . | ||
| Travel | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Outbreak | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| SalmonellosisFootnote c,Footnote d | Total | 16.78 | 27.65 | 33.57 | 28.49 | 0.85 | 21.45 |
| Endemic | 10.49 | 16.05 | 20.95 | 17.43 | 0.83 | ||
| Travel | 5.45 | 6.34 | 7.27 | 6.59 | 0.91 | ||
| Outbreak | 0.84 | 2.48 | 2.14 | 0.85 | 0.40 | ||
| Non-Endemic | 0.00 | 0.30 | 0.00 | 0.43 | . | ||
| LTF | 0.00 | 2.48 | 3.21 | 3.19 | 0.99 | ||
| Shigellosis | Total | 0.84 | 2.28 | 3.42 | 3.83 | 1.12 | 2.21 |
| Endemic | 0.00 | 0.40 | 1.07 | 1.28 | 1.19 | ||
| Travel | 0.42 | 1.68 | 1.92 | 1.49 | 0.77 | ||
| Outbreak | 0.00 | 0.00 | 0.21 | 0.21 | 0.99 | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.42 | 0.20 | 0.21 | 0.85 | 3.98 | ||
| Verotoxigenic E. coli (VTEC) | Total | 1.89 | 4.36 | 2.35 | 2.76 | 1.18 | 1.82 |
| Endemic | 1.26 | 2.58 | 2.14 | 2.34 | 1.09 | ||
| Travel | 0.21 | 0.69 | 0.21 | 0.43 | 1.99 | ||
| Outbreak | 0.42 | 0.79 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.00 | 0.30 | 0.00 | 0.00 | . | ||
| YersiniosisFootnote e | Total | 1.05 | 1.98 | 5.56 | 5.74 | 1.03 | -- |
| Endemic | 0.42 | 1.29 | 3.63 | 4.68 | 1.29 | ||
| Travel | 0.42 | 0.40 | 0.86 | 0.64 | 0.75 | ||
| Outbreak | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| Non-Endemic | 0.00 | 0.00 | 0.00 | 0.00 | . | ||
| LTF | 0.21 | 0.30 | 1.07 | 0.43 | 0.40 | ||
| Total Case Counts | Total | 285 | 768 | 443 | 405 | ||
| Endemic | 150 | 437 | 282 | 254 | |||
| Travel | 79 | 192 | 107 | 93 | |||
| Outbreak | 9 | 33 | 12 | 5 | |||
| Non-Endemic | 2 | 24 | 1 | 6 | |||
| LTF | 45 | 82 | 41 | 47 | |||
Note: Population estimates obtained from the Ontario Ministry of Health and Long-Term Care, Population Projections 2015, IntelliHEALTH Ontario for the ON site; the BC Ministry of Finance and Corporate Relations, BC Stats, Population Extrapolation for Organizational Planning with Less Error (P.E.O.P.L.E.), 2014-2015, for the BC site; and Alberta Health Services (2015 population data) for the AB site. National 2014 data from Canadian Notifiable Disease Surveillance System (CNDSS), Surveillance and Epidemiology Division, Centre for Communicable Diseases and Infection Control, PHAC (2014). Table 1 Footnotes
. Not applicable |
|||||||
It is also important to monitor longer-term disease trends over time when the historic data are available. The data were available for the BC site which includes all cases (endemic, travel, outbreak, non-endemic, and those lost to follow-up). The incidence rate of salmonellosis showed a statistically significant increase (43%) in 2015 compared with the 2006-2007 rate (Figure 1). The incidence rate of giardiasis showed a statistically significant decrease (48%) in 2015 compared with the 2006-2007 rate.
Figure 1: Estimated percent change (with 95% confidence interval) in annual incidence rates of reportable enteric disease casesFigure 1 Footnote a in the BC site in 2015, compared with the average annual incidence rate during 2006-2007, by pathogen
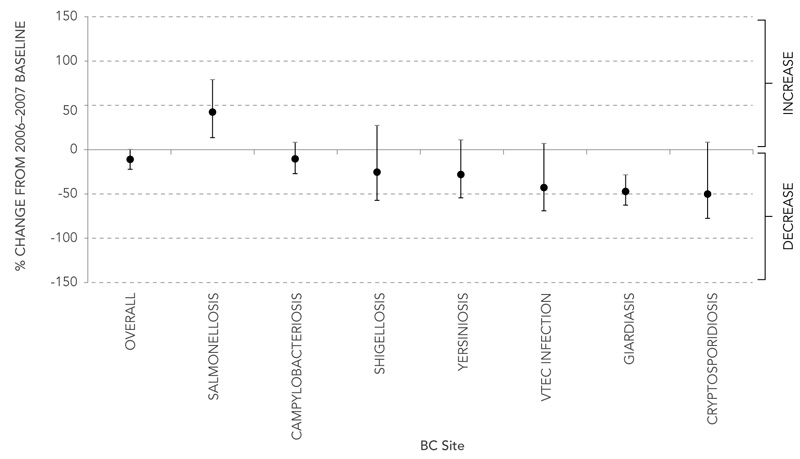
Note: Changes are not statistically significant if zero is within the estimate's 95% confidence interval; changes are statistically significant if zero is not within the confidence interval. Baseline 2006-2007 data from the BC site was provided by the FHA.
Figure 1 Footnotes
- Figure 1 Footnote a
-
Listeriosis was not included due to low case counts.
Figure 1 Text equivalent
| Disease | Estimated Percent Change | 95% Confidence Interval | |
|---|---|---|---|
| Lower Limit | Upper Limit | ||
| Overall | -11.27 | -21.22 | -0.06 |
| Salmonellosis | 42.97 | 14.00 | 79.30 |
| Campylobacteriosis | -11.02 | -26.78 | 8.10 |
| Shigellosis | -26.24 | -57.37 | 27.60 |
| Yersiniosis | -28.41 | -54.16 | 11.80 |
| VTEC Infection | -42.83 | -69.36 | 6.70 |
| Giardiasis | -47.86 | -62.19 | -28.12 |
| Cryptosporidiosis | -50.26 | -77.26 | 8.80 |
Figure 1 compares the incidence rates of all reported enteric cases (endemic, travel, outbreak, non-endemic and those lost to follow-up) in 2015 with the average incidence rates during 2006/2007 by disease. The difference between the incidence rates is shown as a percent change (left y-axis) and disease is shown on the x-axis. The lines extending from each point represent the 95% confidence interval.
Retail Component
Retail foods are recognized as an important source of human exposure to enteric pathogens. Core surveillance activities monitor the presence of major pathogens in retail chicken and beef on an annual basis. Targeted surveillance focuses on select items that are considered to be likely sources of human exposure, and may differ from year to year. In 2015, the targeted surveillance included chicken nuggets, fresh berries and fresh herbs.
Core Surveillance Activities
ON Site
In 2014, retail sampling concluded at the end of March in the pilot ON site (Region of Waterloo), while sampling in the new site (MLHU) began in July. In 2015 sampling took place in the new ON site all year. In 2015, Campylobacter was the most commonly found pathogen on chicken breasts (40%, 54/135), followed by Salmonella spp. (19%, 26/134) and Listeria monocytogenes (13%, 16/134)(Table 2). In ground beef, Listeria monocytogenes was the most commonly found pathogen (20%, 27/135) with both VTEC (2.2%, 3/135) and Salmonella (1.5%, 2/135) following at a relatively lower prevalence. There was no significant difference in the prevalence for any of the pathogens between 2014 and 2015 when both ON sites are combined. However, within the new ON site, there was a significant increase in Listeria monocytogenes prevalence in ground beef in 2015 (25%, 16/63) compared with 2014 (9.5%, 6/63) between July to December (P = 0.03).
| Pathogens Tested | Skinless Chicken Breast | Ground Beef | ||
|---|---|---|---|---|
| 2014Table 2 Footnote a† (n=96) |
2015 (n=135) |
2014Table 2 Footnote a† (n=96) |
2015 (n=135) |
|
| percent positive (number positive) | ||||
| Campylobacter | 49% (47) | 39% (54) | . | 0% (0) |
| Salmonella | 21% (20) | 19% (26) | . | 1.5% (2) |
| VTEC | . | . | 2.1% (2) | 2.2% (3) |
| Listeria monocytogenes | 17% (16) | 13% (17) | 13% (12) | 20% (27) |
Table 2 Footnotes
|
||||
Figure 2: Yearly distribution of pathogen contamination on retail meat in the ON sites, 2006 to 2015
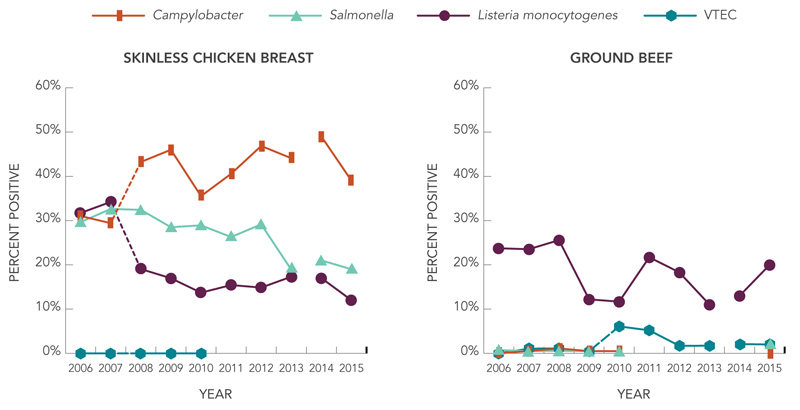
Note: Dashed lines indicate a laboratory or sampling method change. All data from 2006 to 2013 are from the pilot ON site and capture the whole year. In 2014 there was a site change in ON; the pilot ON site was sampled from January to March and the new ON site was sampled from July to December, representing only partial year data for each ON site.
Figure 2 text equivalent
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | 0.3103 | 0.2941 | 0.4324 | 0.46 | 0.3553 | 0.4057 | 0.4686 | 0.4409 | 0.49 | 0.39 |
| Salmonella | 0.2966 | 0.3262 | 0.3243 | 0.285 | 0.2893 | 0.2629 | 0.2914 | 0.189 | 0.21 | 0.19 |
| Listeria monocytogenes | 0.3172 | 0.3422 | 0.1905 | 0.1697 | 0.1371 | 0.1543 | 0.1486 | 0.1732 | 0.17 | 0.12 |
| VTEC | 0 | 0 | 0 | 0 | 0 |
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | 0 | 0.0053 | 0.0111 | 0.005 | 0.0051 | 0 | ||||
| Salmonella | 0.0072 | 0.0053 | 0.0056 | 0.005 | 0.0051 | 0.02 | ||||
| Listeria monocytogenes | 0.2374 | 0.2353 | 0.2558 | 0.122 | 0.1168 | 0.2171 | 0.1829 | 0.1102 | 0.13 | 0.2 |
| VTEC | 0 | 0.0107 | 0.0111 | 0.005 | 0.0609 | 0.052 | 0.017 | 0.0173 | 0.021 | 0.02 |
A line graph describing the trends in prevalence of pathogens tested on core meat products, skinless chicken breast and ground beef, in both Ontario sentinel sites between 2006 and 2015. The y-axis presents the percent positive value for each pathogen and the x-axis presents the individual years between 2006 and 2015. In 2014 there was a site change in ON; the pilot ON site was sampled from January to March and the new ON site was sampled from July to December, representing only partial year data for each ON site.
BC Site
Retail sampling was implemented in BC in January 2011 and has been ongoing ever since. In 2015, Campylobacter was the most commonly found pathogen on chicken breasts (43%, 58/135), followed by Salmonella spp. (33%, 45/135,) and Listeria monocytogenes (18%, 24/135) (Table 3). No significant differences in the prevalence of any of the pathogens on the chicken breasts were observed when comparing 2015 with 2014. In 2015, Listeria monocytogenes was the most prevalent pathogen found on ground beef (35%, 47/129), while no Campylobacter was detected. Salmonella and VTEC were identified on ground beef at relatively low prevalence. A significantly higher prevalence of Listeria monocytogenes in ground beef samples was observed in 2015 compared with 2014.
| Pathogens Tested | Skinless Chicken Breast | Ground Beef | ||
|---|---|---|---|---|
| 2014† | 2015 (n=135) |
2014† | 2015 (n=129) |
|
| percent positive (number positive/number tested) | ||||
| Campylobacter | 36% (44/121) | 43% (58) | . | 0% (0) |
| Salmonella | 26% (32/123) | 33% (45) | . | 1.5% (2) |
| VTEC | . | . | 2.5% (3/122) | 1.6% (2) |
| Listeria monocytogenes | 19% (23/123) | 18% (24) | 12% (15/123) | 35% (47)*** |
Table 3 Footnotes
|
||||
Prevalence of Listeria monocytogenes on retail chicken breasts significantly decreased in 2013 in comparison to 2012, remaining stable at this level over the last few years (Figure 3). In comparison, despite having a significant drop in prevalence between 2011 and 2012, the prevalence of Salmonella detected on chicken breasts has been slowly increasing since 2013. Among ground beef samples, VTEC prevalence has remained stable while a significant increase in Listeria monocytogenes was observed in 2015 compared to 2014.
Figure 3: Yearly distribution of pathogen contamination on retail meat samples collected in the BC site, 2011 to 2014
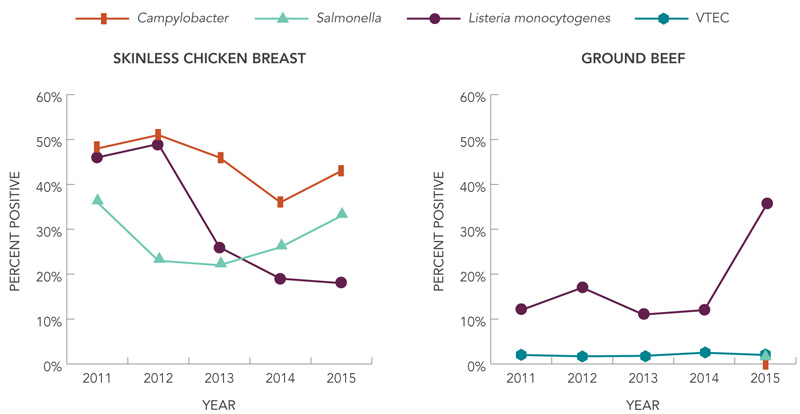
Figure 3 text equivalent
| Year | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|
| Campylobacter | 0.48 | 0.51 | 0.46 | 0.36 | 0.43 |
| Salmonella | 0.36 | 0.23 | 0.22 | 0.26 | 0.33 |
| Listeria monocytogenes | 0.46 | 0.49 | 0.26 | 0.19 | 0.18 |
| Year | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|
| Campylobacter | 0 | ||||
| Salmonella | 0.02 | ||||
| Listeria monocytogenes | 0.12 | 0.17 | 0.11 | 0.12 | 0.35 |
| VTEC | 0.02 | 0.017 | 0.018 | 0.025 | 0.02 |
A line graph describing the trends in prevalence of pathogens tested on core meat products, skinless chicken breast and ground beef, in the British Columbia sentinel site in the Fraser Health Authority between 2011 and 2015. The y-axis presents the percent positive value for each pathogen and the x-axis presents the individual years between 2011 and 2015.
AB Site
Retail sampling began in the AB site in May 2014 (Table 4) and continued throughout 2015. In 2015, Campylobacter was the most commonly found pathogen on chicken breasts (38%, 49/130), followed by Salmonella (17%, 22/130) and Listeria monocytogenes (12%, 15/130). In ground beef, Listeria monocytogenes was the most commonly isolated pathogen (31%, 41/132) with all other pathogens occurring with a relatively low prevalence. There was a significant increase in Listeria monocytogenes isolated in ground beef samples in 2015 compared with 2014.
| Pathogens Tested | Skinless Chicken Breast | Ground Beef | ||
|---|---|---|---|---|
| 2014† (n=79) |
2015 (n=130) |
2014† (n=78) |
2015 (n=132) |
|
| percent positive (number positive) | ||||
| Campylobacter | 47% (37) | 38% (49) | . | 0.8% (1) |
| Salmonella | 15% (12) | 17% (22) | . | 2% (3) |
| VTEC | . | . | 0% (0) | 3% (4) |
| Listeria monocytogenes | 11% (9) | 12% (15) | 9.0% (7) | 31% (41)*** |
Table 4 Footnotes
|
||||
Targeted Retail Surveillance
Retail Meat
In 2015, raw/uncooked frozen chicken nuggets continued to be sampled as part of the targeted retail meat surveillance in all sites. Frozen chicken nuggets sampled were labelled “Raw” or “Uncooked” and included chicken strips and nuggets (including breaded filets, processed meats or shaped meats, but excluding burgers).
ON Site
In 2015, Salmonella was the most commonly found pathogen on chicken nuggets (23%, 31/135). There were no significant differences found in the prevalence of either Salmonella or Listeria monocytogenes on chicken nuggets in 2015 compared with 2014 (Table 5).
| Pathogens Tested | Chicken Nuggets | |
|---|---|---|
| 2014Table 5 Footnote a† (n=96) |
2015 (n=135) |
|
| percent positive (number positive) | ||
| Salmonella | 28% (27) | 23% (31) |
| Listeria monocytogenes | 16% (15) | 12% (16) |
Table 5 Footnotes
|
||
BC Site
Salmonella was the most commonly found pathogen on chicken nuggets (34%, 46/135) and comparing 2014 and 2015 there were no significant differences in the prevalence of either Salmonella or Listeria monocytogenes on this product (Table 6).
| Pathogens Tested | Chicken Nuggets | |
|---|---|---|
| 2014† (n=123) |
2015 (n=135) |
|
| percent positive (number positive) | ||
Salmonella |
28% (34) | 34% (46) |
Listeria monocytogenes |
8.9% (11) | 24% (19) |
Table 6 Footnotes
|
||
AB Site
Targeted sampling of frozen chicken nuggets began in May 2014 and continued throughout 2015. Salmonella and Listeria monocytogenes were found on 27% (35/132) and 17% (22/132) of samples, respectively (Table 7). Comparing 2014 and 2015, there were no significant differences in the prevalence of either Salmonella or Listeria monocytogenes on this product (Table 7).
| Pathogens Tested | Chicken Nuggets | |
|---|---|---|
| 2014Table 7 Footnote a† (n=78) |
2015 (n=132) |
|
| percent positive (number positive) | ||
| Salmonella | 29% (23) | 27% (35) |
| Listeria monocytogenes | 23% (18) | 17% (22) |
Table 7 Footnotes
|
||
Produce
In 2015, a variety of fresh berries (e.g., raspberries, blueberries, blackberries etc.) and fresh herbs (e.g., parsley, dill, mint etc.) were collected from retail stores in all sentinel sites and tested for parasites, viruses, and bacteria (Table 8). In 2011, fresh berries were collected from the pilot ON site and BC, while in 2012 fresh herb samples were collected from these same two sites. In 2015, 100 berry samples (12 domestic, 84 imported, 4 unknown origin) and 110 herb samples (14 domestic, 68 imported, 28 unknown origin) were collected and tested in the ON site, 100 berry samples (6 domestic, 94 imported) and 110 herb samples (31 domestic, 74 imported, 5 unknown origin) in the BC site, and 100 berry samples (7 domestic, 90 imported, 3 unknown origin) and 112 herb samples (19 domestic, 74 imported, and 19 unknown origin) in the AB site. There were no positive samples among products labelled ‘domestic’.
A significant decrease in Giardia isolated from soft berries was seen in 2015 compared to 2011 (Table 8). A significant decrease in both Giardia and norovirus was also seen in fresh herbs in 2015 compared to 2012. Among the fresh berry samples, only one sample was found to be positive for Cryptosporidium (0.3%, 1/300). Cyclospora (0.3%, 1/332) and Hepatitis A (1.1%, 1/91) were the only organisms found among the herb samples collected. Since the parasites and viruses were all tested using PCR methodology, the viability of these detected pathogens and the subsequent potential risk to consumers, is unknown.
| Pathogens TestedTable 8 Footnote a | Berries | Herbs | ||
|---|---|---|---|---|
| 2011Table 8 Footnote b† (n=599) |
2015 (n=300) |
2012Table 8 Footnote b† (n=598) |
2015 (n=332) |
|
| percent positive (number positive/number tested) | ||||
| Cryptosporidium | 0.33% (2) | 0.34% (1) | 0% (0) | 0% (0) |
| Giardia | 9.0% (54) | 0 % (0)*** | 1.0% (6) | 0% (0)* |
| Cyclospora | 1.0% (6) | 0% (0) | 0% (0) | 0.3% (1) |
| Norovirus | 0.50% (3) | 0% (0) | 1.3% (8) | 0% (0)* |
| Rotavirus | 0.17% (1) | 0% (0) | 0% (0) | 0% (0) |
| Hepatitis A | . | 0% (0) | . | 1.1% (1) |
| Hepatitis E | . | 0% (0) | . | 0% (0) |
| Listeria monocytogenes | . | 0% (0) | . | 0% (0) |
Table 8 Footnotes
|
||||
Agriculture Component
Farms represent environmental and food-chain exposure sources of enteric pathogens. Farms are sampled by veterinarians throughout the year in conjunction with the CIPARS program with the aim of sampling approximately 30 farms within each site per commodity per year for FNC. In 2015, broiler chicken, swine, and turkey farms were sampled. For the broiler chicken and turkey farms, four fresh pooled manure samples were collected from each flock from different areas of the same barn. Both broiler chicken and turkey flocks were sampled within one week of transport for slaughter. Swine farms had a total of six fresh pooled samples from different pens collected per farm. Results are presented at the individual sample-level and at the farm-level to account for within-farm differences (some pathogens may be found at different prevalence rates within each farm and this may impact any comparisons based only on their sample-level results).
ON Site
In 2015 in ON, manure from broiler chickens and swine in the new site was collected and tested for Campylobacter (broiler chickens only) and Salmonella (broiler chickens and swine) (Table 9 and 10). Due to an avian influenza outbreak in ON in 2015, broiler chicken sampling was delayed until August. In 2014 in ON, broiler chicken sampling took place in the pilot site from January to March and in the new site from August to December. However, for comparison purposes, only the broiler chicken samples collected in 2014 from the new site are included here. Swine sampling took place all year in both 2014 and 2015 in ON. There was a significant increase in the prevalence of Campylobacter in broiler chicken manure at the sample-level in 2015 compared with 2014 and a significant decrease in the prevalence of Salmonella in swine manure at the sample-level in 2015 (Table 9). There were no significant differences at the farm- level in 2015 (Table 10). However, it is interesting to note that there appears to be more clustering at the farm-level in broilers than in swine.
| Pathogens Tested | Broiler ChickensTable 9 Footnote a | Swine | ||
|---|---|---|---|---|
| 2014† (n=52) |
2015 (n=88) |
2014† (n=156) |
2015 (n=150) |
|
| percent positive (number positive) | ||||
| Campylobacter | 7.7% (4) | 24% (21)** | . | . |
| Salmonella | 31% (16) | 45% (40) | 39% (61) | 29% (43)* |
Table 9 Footnotes
|
||||
| Pathogens Tested | Broiler ChickensTable 10 Footnote a | Swine | ||
|---|---|---|---|---|
| 2014† (n=13) |
2015 (n=22) |
2014† (n=26) |
2015 (n=25) |
|
| percent positive (number positive) | ||||
| Campylobacter | 7.7% (1) | 27% (6) | . | . |
| Salmonella | 38% (5) | 59% (13) | 62% (16) | 44% (11) |
Table 10 Footnotes
|
||||
It is difficult to interpret trends in 2015 due to the change of site in 2014 (Figure 4). However, the prevalence of some of the pathogens in 2015 appears similar to those seen in previous years. Dairy and beef were not sampled in ON in 2015 but are included here for reference.
Figure 4: Pathogen detection (sample-level) in manure from farms in the ON site, 2006 to 2015
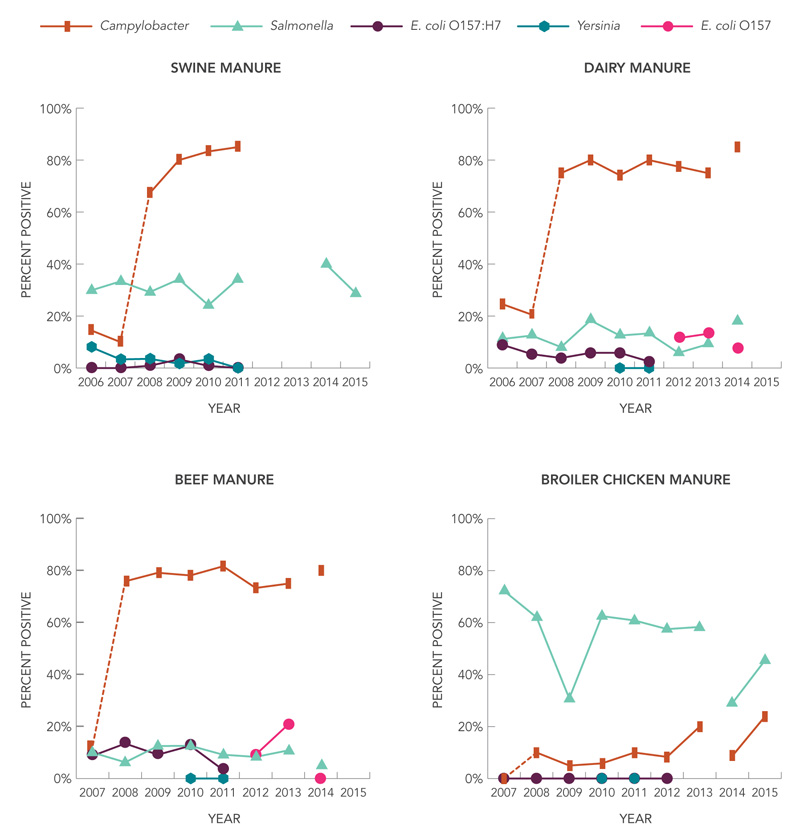
Note: Dashed lines indicate a laboratory or sampling method change. All data from 2006 to 2013 are from the pilot ON site. In 2014, there was a site change in ON; the pilot ON site was sampled from January to March for beef, broiler chickens, and dairy and the new ON site was sampled from August to December for broiler chickens and all year for swine. In 2015, the new ON site was sampled from August to December for broiler chickens and all year for swine. Beef and dairy were not sampled in ON in 2015.
Figure 4 Text Equivalent
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | 0.1452 | 0.1000 | 0.6726 | 0.8000 | 0.8333 | 0.8500 | Not tested | Not tested | Not tested | Not tested |
| Salmonella | 0.2984 | 0.3333 | 0.2920 | 0.3417 | 0.2417 | 0.3417 | Not tested | Not tested | 0.40 | 0.29 |
| E. coli O157:H7 | 0.0000 | 0.0000 | 0.0088 | 0.0333 | 0.0083 | 0.0000 | Not tested | Not tested | Not tested | Not tested |
| Yersinia | 0.0806 | 0.0333 | 0.0354 | 0.0167 | 0.0333 | 0.0000 | Not tested | Not tested | Not tested | Not tested |
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | 0.2458 | 0.2054 | 0.7500 | 0.8000 | 0.7417 | 0.8000 | 0.7750 | 0.7500 | 0.8500 | Not tested |
| Salmonella | 0.1117 | 0.1250 | 0.0804 | 0.1833 | 0.1250 | 0.1333 | 0.0583 | 0.0917 | 0.1800 | Not tested |
| E. coli O157:H7 | 0.0894 | 0.0536 | 0.0385 | 0.0583 | 0.0583 | 0.0250 | Not tested | Not tested | Not tested | Not tested |
| Yersinia | Not tested | Not tested | Not tested | Not tested | 0 | 0 | Not tested | Not tested | Not tested | Not tested |
| E. coli O157 | Not tested | Not tested | Not tested | Not tested | Not tested | Not tested | 0.1167 | 0.1333 | 0.075 | Not tested |
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | Not tested | 0.1250 | 0.7589 | 0.7917 | 0.7815 | 0.8167 | 0.7333 | 0.7500 | 0.8000 | Not tested |
| Salmonella | Not tested | 0.1000 | 0.0625 | 0.1250 | 0.1261 | 0.0917 | 0.0833 | 0.1083 | 0.0500 | Not tested |
| E. coli O157:H7 | Not tested | 0.0875 | 0.1346 | 0.0917 | 0.1261 | 0.0333 | Not tested | Not tested | Not tested | Not tested |
| Yersinia | Not tested | Not tested | Not tested | Not tested | 0 | 0 | Not tested | Not tested | Not tested | Not tested |
| E. coli O157 | Not tested | Not tested | Not tested | Not tested | Not tested | Not tested | 0.0917 | 0.2083 | 0 | Not tested |
| Year | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|
| Campylobacter | Not tested | 0.0000 | 0.1000 | 0.0500 | 0.0583 | 0.1000 | 0.0833 | 0.2000 | 0.0870 | 0.2386 |
| Salmonella | Not tested | 0.7222 | 0.6200 | 0.3083 | 0.6250 | 0.6083 | 0.5750 | 0.5833 | 0.2900 | 0.4545 |
| E. coli O157:H7 | Not tested | 0 | 0 | 0 | 0 | 0 | 0 | Not tested | Not tested | Not tested |
| Yersinia | Not tested | Not tested | Not tested | Not tested | 0 | 0 | Not tested | Not tested | Not tested | Not tested |
Four line graphs describing the trends in prevalence of pathogens tested in manure from four different production animal commodities, swine, dairy, beef, and broiler chickens, in both Ontario sentinel sites between 2006 and 2015. The y-axis presents the percent positive value for each pathogen and the x-axis presents the individual years between 2006 and 2015. In 2014 there was a site change in ON; the pilot ON site was sampled from January to March for beef, broiler chickens, and dairy and the new ON site was sampled from August to December for broiler chickens and all year for swine. In 2015, the new ON site was sampled from August to December for broiler chickens and all year for swine. Beef and dairy were not sampled in ON in 2015.
BC Site
In the BC site in 2015, manure from broiler chickens and turkey was collected and tested for Campylobacter and Salmonella, as in previous years (Table 11 and 12). However, due to an avian influenza outbreak in BC in 2015, both broiler chicken and turkey sampling was not initiated until September 2015. In 2014, broiler chicken and turkey samples were collected throughout the year. In turkey, there was a significant increase at the sample-level in the prevalence of both Campylobacter and Salmonella in 2015 compared with 2014 (Table 11). However, this increase may be due to a seasonal effect, particularly for Campylobacter, as in previous years FNC has often found Campylobacter prevalence in broiler chickens to be highest in the fall and this may be similar for turkey (2013 FNC Annual Report). When results from 2015 are compared with the same months in 2014 (September to December), the difference in prevalence is no longer significant for Campylobacter; however, the prevalence in 2014 remains similar for September to December (75%, 39/52) vs the entire year (73%, 85/116). Salmonella prevalence in turkey in 2014 for September to December is only 17% (9/52) (vs 23%, 27/116 all year) with a significant increase observed in 2015 relative to 2014 when the same months of 2014 are compared. At the farm-level, there was a significant increase in the prevalence of Salmonella in broiler chickens in 2015 compared with 2014, with almost all farms testing positive in 2015 (Table 12).
| Pathogens Tested | Broiler Chickens | Turkey | ||
|---|---|---|---|---|
| 2014† (n=116) |
2015Table 11 Footnote a (n=100) |
2014† (n=116) |
2015Table 11 Footnote a (n=120) |
|
| percent positive (number positive) | ||||
| Campylobacter | 22% (26) | 25% (25) | 73% (85) | 86% (103)** |
| Salmonella | 64% (74) | 72% (72) | 23% (27) | 39% (47)** |
Table 11 Footnotes
|
||||
| Pathogens Tested | Broiler Chickens | Turkey | ||
|---|---|---|---|---|
| 2014† (n=30) |
2015Table 12 Footnote a (n=25) |
2014† (n=29) |
2015Table 12 Footnote a (n=30) |
|
| percent positive (number positive) | ||||
| Campylobacter | 27% (8) | 28% (7) | 79% (23) | 90% (27) |
| Salmonella | 73% (22) | 92% (23)* | 38% (11) | 53% (16) |
Table 12 Footnotes
|
||||
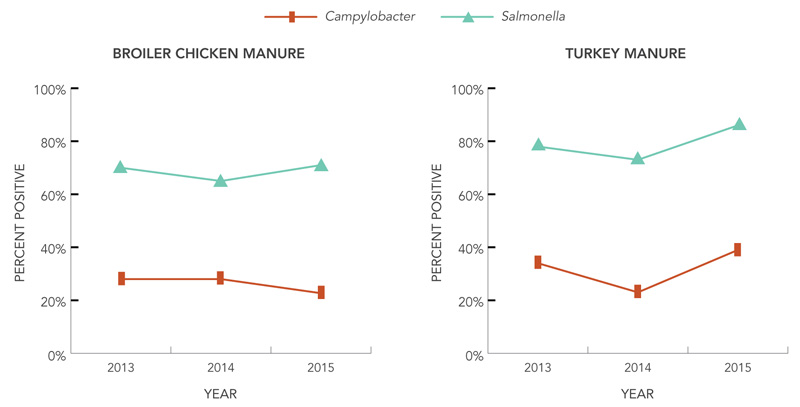
2015 is the first year where data from the BC site has been presented in a temporal figure (Figure 5). Over the last three years, the prevalence of Campylobacter and Salmonella in both broiler chickens and turkey has been relatively stable.
Figure 5: Pathogen detection (sample-level) in manure from farms in the BC site, 2013 to 2015
AB Site
In 2015 in the AB site, manure from broiler chickens and swine was collected and tested for Campylobacter (broiler chickens only) and Salmonella (broiler chickens and swine) (Table 13 and 14). Both of these commodities were sampled all year. At the sample-level, the prevalence of both Campylobacter and Salmonella was significantly higher in broiler chickens in 2015 compared to 2014 (Table 13). However, at the farm-level, this increase was only significant for Campylobacter (Table 14). There was no significant increase or decrease at either the sample- or farm-level in swine. However, one interesting finding is that the prevalence of Salmonella in swine appears to be lower in the AB site than in the ON site. This difference between the sites may be due to factors such as the distance between herds, age of the barns and other herd management factors.
| Pathogens Tested | Broiler Chickens | Swine | ||
|---|---|---|---|---|
| 2014† (n=120) |
2015 (n=120) |
2014† (n=108) |
2015 (n=108) |
|
| percent positive (number positive) | ||||
| Campylobacter | 9.2% (11) | 34% (41)*** | . | . |
| Salmonella | 37% (44) | 52% (62)** | 5.6% (6) | 2.8% (3) |
Table 13 Footnotes
|
||||
| Pathogens Tested | Broiler Chickens | Swine | ||
|---|---|---|---|---|
| 2014† (n=30) |
2015 (n=30) |
2014† (n=18) |
2015 (n=18) |
|
| percent positive (number positive) | ||||
| Campylobacter | 13% (4) | 37% (11)* | . | . |
| Salmonella | 57% (17) | 77% (23) | 5.6% (1) | 17% (3) |
Table 14 Footnotes
|
||||
Water Component
Surface and Irrigation Water
Water is another environmental source of enteric pathogens, through activities such as swimming or contamination of produce. In 2015, water samples were collected in all three sites. 2015 was the first year that water samples were collected in the new ON site. Surface water was collected approximately bi-weekly from six locations in the Ausable Bayfield Conservation Authority (a watershed adjacent to the new ON site) from July to November and tested for VTEC (Table 15).
| Pathogens Tested | Surface Water 2015 (n=59) |
|---|---|
| percent positive (number positive) | |
| VTEC | 39% (23) |
In BC in 2015, as in 2014, irrigation water was sampled from five locations in the Sumas and Matsqui watersheds approximately bi-weekly throughout the year and tested for Campylobacter, Salmonella, and VTEC (Table 16). In BC, with all locations combined, the prevalence of Campylobacter was significantly lower in 2015 compared with 2014 (Table 16).
| Pathogens Tested | Irrigation Canals/Creeks | |
|---|---|---|
| 2014† (n=101) |
2015 (n=75) |
|
| percent positive (number positive) | ||
| Campylobacter | 38% (38) | 21% (16)** |
| Salmonella | 9.9% (10) | 11% (8) |
| VTEC | 28% (28) | 24% (23) |
Table 16 Footnotes
|
||
In the AB site, irrigation water was collected approximately bi-weekly from 10 locations in the Western Irrigation District during the summer months (June to September in 2014 and June to August in 2015) and tested for Campylobacter, Salmonella, and VTEC (Table 17). In 2015, some of the samples were tested for Campylobacter using two different methods (in general, one method used 100mL of water while the other used 1L of water). Results from both of these methods combined are presented here. In the AB site, with all 10 locations combined, Salmonella was found to be significantly higher in 2015 compared with 2014 (Table 17).
| Pathogens Tested | Irrigation Canals/Creeks | |
|---|---|---|
| 2014† (n=48) |
2015 | |
| percent positive (number positive) | ||
| Campylobacter | 0% (0) | 4.9% (2/41) |
| Salmonella | 0% (0) | 9.8% (4/41)** |
| VTEC | 27% (13) | 42% (14/33) |
Table 17 Footnotes
|
||
Summary
2015 marks the 10th anniversary of PHAC's FoodNet Canada surveillance system. Over this time, PHAC's FNC has provided valuable information on enteric illness in Canada that has helped contribute in many different ways to food safety interventions and policy. With the expansion to three sites in 2014 and the continuation of this surveillance in 2015, PHAC is now able to provide even more information on some of the leading sources of food-borne illness in Canada.
According to FoodNet Canada data, in 2015, Campylobacter, Salmonella, and Giardia remained the most common causes of human enteric illness in the sentinel sites. Although travel was an important factor with many pathogens, the majority of campylobacteriosis and salmonellosis cases were endemic. For Campylobacter, Salmonella, and VTEC, the incidence for travel related cases were similar across the sites but the incidence for endemic cases was higher in the western sites.
When looking at longer term changes in rates, salmonellosis rates in 2015 were shown to be significantly higher than ten years ago in the BC site. According to PHAC's National Enteric Surveillance Program (NESP) data, S.Enteritidis (SE) is driving the higher rates of salmonellosis with 1955 cases of SE reported in 2009 in Canada compared to 3337 cases reported in 2014Footnote 1. This increase in rates will be described further in FoodNet Canada's comprehensive annual report.
In retail samples in 2015, Campylobacter continued to be the most commonly found pathogen on skinless chicken breasts in all three sites (38-43% positive), followed by Salmonella, which had a significantly higher prevalence in the BC site (33%) compared to the ON (19%) and AB (17%) sites. For chicken nuggets, Salmonella was the most common pathogen with a significantly higher prevalence in the BC site, with 34% of samples testing positive, compared to the ON site (23%). One particularly notable finding in 2015 was the significantly higher levels of Listeria monocytogenes found on ground beef in all three sites compared with 2014, with up to 35% of samples now testing positive.
In produce, very few samples of fresh berries and herbs were positive for the pathogens of interest, suggesting a more limited contribution of these sources to human enteric illness in Canada.
On farm, Salmonella was once again found to be the most common pathogen in the broiler chickens, with a significantly higher prevalence in the BC site, with 72% of manure samples testing positive, compared to the ON (45%) and AB (52%) sites. In turkey, Campylobacter remained the most prevalent pathogen. The prevalence of Salmonella in swine manure samples varied across the two sites with available information with 2.8% positive from the AB site and 29% positive from the ON site. The prevalence of all pathogens at the farm-level was higher than at the sample-level in all commodities, which is important to note when deciding on management practices for the control of these pathogens on the farm.
In water, VTEC was found to be the most common pathogen in the irrigation water samples from both BC and AB. The VTEC prevalence was also found to be similar in surface water from ON (where only VTEC was assessed). Campylobacter and Salmonella were also found in the irrigation water samples in 2015 in BC and AB. More research is needed to understand the impact on human health.
Continued surveillance of important enteric pathogens in PHAC's FNC three sentinel sites suggests that many of the sources tested remain important contributors to human illness. For example, poultry and poultry products appear to be important sources of both Campylobacter and Salmonella for humans. Environmental sources (e.g. surface water), could also have an impact on human enteric illness. Continued monitoring of potentially emerging issues, such as Listeria monocytogenes in ground beef, is also important. PHAC's FNC surveillance information continues to help protect Canadians and direct future food and water safety policies.
Special Update:
As Salmonella Enteritidis (SE) has been of increased concern in recent years, FNC implemented expedited subtyping of retail and on-farm samples in 2015 to provide more timely information. In 2015, the difference in rates of endemic salmonellosis across the sites was driven primarily by SE rates - 3, 9 and 9/100,000 respectively for ON, AB and BC sites. SE prevalence in chicken manure at the farm level differed as well – 0%, 8% and 27% respectively for ON, AB and BC sites. This was also reflected on chicken breasts at the retail level - 1%, 8% and 23% respectively for ON, AB and BC sites. There was little difference on chicken nuggets at the retail level - 9%, 12% and 14% respectively for ON, AB and BC sites. These data support national initiatives for pathogen reduction and identification of points of interventions which can vary across the sites.
- Footnote 1
-
Government of Canada. National Enteric Surveillance Program Annual Summary 2014: Public Health Agency of Canada, Guelph, 2016.