Infographic: Inequalities in mental illness hospitalization in Canada
Download the alternative format
(PDF format, 187 KB, 1 page)
Organization: Public Health Agency of Canada
- Cat.: HP35-113/10-2019E-PDF
- ISBN: 978-0-660-29696-8
- Pub.: 180788
Pan-Canadian Health Inequalities Reporting Initiative
Inequalities in Mental Illness Hospitalization in Canada
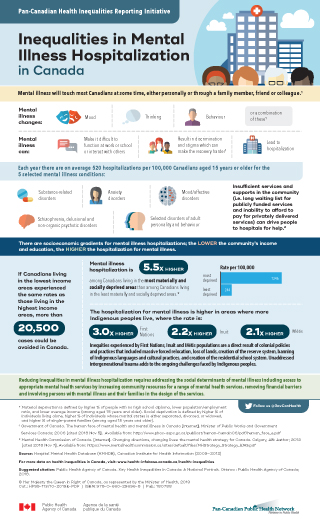
Mental illness will touch most Canadians at some time, either personally or through a family member, friend or colleague.Footnote 1
Mental illness changes:
- Mood
- Thinking
- Behaviour
- or a combination of theseFootnote 1
Mental illness can:
- Make it difficult to function at work or school or interact with others
- Result in discrimination and stigma which can make the recovery harderFootnote 1
- Lead to hospitalization
Each year there are on average 520 hospitalizations per 100 000 Canadians aged 15 years or older for the 5 selected mental illness conditions:
- substance-related disorders
- schizophrenia, delusional and non-organic psychotic disorders
- mood/affective disorders
- anxiety disorders
- selected disorders of adult personality and behaviour
Insufficient services and supports in the community (i.e. long waiting list for publicly funded services and inability to afford to pay for privately delivered services) can drive people to hospitals for help.Footnote 2
There are socioeconomic gradients for mental illness hospitalizations; the lower the community’s income and education, the higher the hospitalization for mental illness.
If Canadians living in the lowest income areas experienced the same rates as those living in the highest income areas, more than 20 500 cases could be avoided in Canada.
Mental illness hospitalization is 5.5 times higher among Canadians living in the most materially and socially deprived areas than among Canadians living in the least materially and socially deprived areas.Footnote *
Rate per 100,000
- Most deprived
- 1 346
- Least deprived
- 244
The hospitalization for mental illness is higher in areas where more Indigenous peoples live, where the rate is:
- First Nations
- 3.0 times higher
- Inuit
- 2.2 times higher
- Métis
- 2.1 times higher
Inequities experienced by First Nations, Inuit and Métis populations are a direct result of colonial policies and practices that included massive forced relocation, loss of lands, creation of the reserve system, banning of Indigenous languages and cultural practices, and creation of the residential school system. Unaddressed intergenerational trauma adds to the ongoing challenges faced by Indigenous peoples.
Reducing inequalities in mental illness hospitalization requires addressing the social determinants of mental illness including access to appropriate mental health services by increasing community resources for a range of mental health services, removing financial barriers and involving persons with mental illness and their families in the design of the services.
Follow us @GovCanHealth
Source: Hospital Mental Health Database (HMHDB), Canadian Institute for Health Information (2009–2012)
For more data on health inequalities in Canada, visit:
www.health-infobase.canada.ca/health-inequalities
Suggested citation: Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait. Ottawa: Public Health Agency of Canada; 2018.
© Her Majesty the Queen in Right of Canada, as represented by the Minister of Health, 2019 | Cat.: HP35-113/10-2019E-PDF | ISBN: 978-0-660-29696-8 | Pub.: 180788