Recombinant influenza vaccines: A supplemental statement of the Canadian Immunization Guide chapter on influenza and statement on seasonal influenza vaccine for 2022–2023
Download in PDF format
(944 KB, 59 pages)
Organization: Public Health Agency of Canada
Published: 2022-09-12
Table of contents
- Summary of the information contained in this NACI supplemental statement
- I. Introduction
- II. Methods
- III. Vaccine
- IV. Discussion
- V. Recommendations
- VI. Tables
- VII. List of abbreviations
- VIII. Acknowledgements
- IX. Appendix A: Prisma flow diagram
- X. Appendix B: Characteristics of influenza vaccines available for use in Canada, 2022–2023
- XI. References
Preamble
The National Advisory Committee on Immunization (NACI) provides the Public Health Agency of Canada (hereafter referred to as PHAC) with ongoing and timely medical, scientific, and public health advice relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Over the coming years NACI will be refining methodological approaches to include these factors. Not all NACI Statements will require in-depth analyses of all programmatic factors. As NACI works towards full implementation of the expanded mandate, select Statements will include varying degrees of programmatic analyses for public health programs.
PHAC acknowledges that the advice and recommendations set out in this statement are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC's Policy on Conflict of Interest, including yearly declaration of potential conflicts of interest.
Summary of the information contained in this NACI supplemental statement
The following highlights key information for immunization providers. Please refer to the remainder of this supplemental statement for details.
1. What
Supemtek™ is a quadrivalent recombinant seasonal influenza vaccine (RIV4) that has recently been authorized for use in Canada in adults 18 years of age and older. Supemtek is the first and, to date, the only seasonal influenza vaccine made with recombinant technology available in Canada. Other influenza vaccines are made in eggs or mammalian cell cultures.
2. Who
This supplemental statement addresses the annual influenza vaccination of adults who do not have contraindications to Supemtek.
3. How
Supemtek may be considered among the quadrivalent influenza vaccines offered to adults 18 years of age and older for their annual influenza vaccination.
4. Why
Supemtek is considered effective, immunogenic, and safe in adults 18 years of age and older and has a comparable immunogenicity and safety profile to egg- and cell culture-based, inactivated, live attenuated, adjuvanted, and high-dose seasonal influenza vaccines already licensed in Canada. Supemtek can provide a broader protection against influenza when compared to trivalent vaccines as its formulation contains both influenza B lineages. In addition, it contains identical hemagglutinin proteins to target influenza strains.
I. Introduction
Influenza is a viral infection that has been estimated to cause approximately 12,200Footnote 1 hospitalizations and 3,500 deathsFootnote 2 in Canada annually. In the five seasons prior to the COVID-19 pandemic (2014–2015 to 2018-2019 seasons), an average of 47,000 laboratory-confirmed cases of influenza were reported to FluWatch, Canada's national surveillance system, each yearFootnote 3Footnote 4Footnote 5. The burden of influenza illness varies from year to year. Influenza activity has been at a historical low during the COVID-19 pandemic, which has been associated with various reasons including the implementation of non-pharmaceutical public health measures (e.g., masking, social distancing) against COVID-19. Only 69 confirmed cases of influenza were identified in Canada during the 2020-2021 season and no community circulation of influenza occurredFootnote 5. A return of persistent sporadic influenza activity was observed in the 2021-2022 season. It is expected that seasonal influenza will continue to re-circulate following the relaxation of COVID-19 pandemic-related public health measures. Low exposure to influenza during the COVID-19 pandemic may lead to higher infection rates when influenza begins circulating as levels of immunity to influenza may have decreased during the pandemicFootnote 6. An increased number of influenza infections and larger outbreaks compared to those observed during the COVID-19 pandemic when infections were reported to be at historic lowsFootnote 6Footnote 7 may occur. Additionally, the resurgence of seasonal influenza may not follow usual seasonal patternsFootnote 5Footnote 8. Vaccination against seasonal influenza remains the best method of preventing and limiting the spread and impact of seasonal influenza circulation.
Influenza in humans is caused by two main types of influenza virus: A, which is classified into subtypes based on hemagglutinin (HA) and neuraminidase (NA) surface proteins, and B, which consists of two antigenically distinct lineages, B/Yamagata and B/Victoria. Seasonal influenza vaccines are either trivalent or quadrivalent formulations. Trivalent influenza vaccines contain two influenza A and one influenza B strain, and quadrivalent influenza vaccines contain the three strains included in trivalent vaccines and an additional influenza B strain from the other lineage of influenza B. Each year, the National Advisory Committee on Immunization (NACI) publishes a statement on seasonal influenza vaccines, which contains recommendations and guidance on the use of influenza vaccines for the upcoming influenza season.
Supemtek (Sanofi Pasteur, Ltd.) is a quadrivalent recombinant seasonal influenza vaccine (RIV4) that was authorized for use in Canada in adults 18 years of age and older on January 14, 2021Footnote 9. Supemtek is created using an insect cell-baculovirus expression vector system and influenza virus proteins (i.e., HA antigens)Footnote 9. The vaccine manufacturing process involves inserting the gene for the production of the HA antigen into a baculovirus to produce a recombinant baculovirus. Insect cells [proprietary expresSF+ insect cells] are then infected with the recombinant baculovirus. The baculovirus facilitates the transportation of the genetic instructions for producing the HA antigen to the host insect cells. A single HA antigen is cloned in these host cells. The individual HA antigens are then extracted from the host cells and further purified to be formulated into the final vaccine product.
Recombinant technology is a novel platform for influenza vaccine manufacturing that aims to overcome challenges associated with egg-based vaccine production and to improve the development process and quality of seasonal influenza vaccinesFootnote 10Footnote 11Footnote 12. Although Supemtek is the only seasonal influenza vaccine made with recombinant technology authorized for use in Canada, the recombinant protein technology is a an established technique that has been utilized to produce vaccines for other vaccine-preventable diseases, including hepatitis B, human papillomavirus, meningococcal group B, herpes zoster, cholera, traveller's diarrhea and COVID-19Footnote 13. Additionally, RIV has been licensed in the United States (US) for 9 years.
The recombinant manufacturing platform offers several advantages over egg-based or cell-based vaccine production including faster production times, high vaccine purity, and reduced risk of mismatch between the vaccine and circulating viral strainsFootnote 12Footnote 14. The recombinant production is not dependent on egg supply nor the availability of an avian or canine kidney cell substrate, as it does not require expansion of live egg-grown nor cell-grown viruses for development of a candidate vaccine virus. It therefore allows for a faster manufacturing process that can be valuable during a pandemic response or in cases of vaccine supply shortageFootnote 11Footnote 14. Recombinant vaccines are made from stable genetic sequences from original wild-type human isolates, so large quantities of highly purified HA can be produced in a relatively short period of time without preservativesFootnote 11Footnote 14.
Additionally, recombinant vaccine technology ensures an exact match of HA protein included in the vaccine to the influenza strains recommended seasonally by the World Health Organization (WHO). It is not subject to the risk of mutations related to egg-adaptive changes and therefore may potentially have higher vaccine effectiveness relative to standard egg-based influenza vaccinesFootnote 12. At the time of this Statement's development, the infrastructure required for manufacturing recombinant vaccines is limited compared to the vast infrastructure for producing egg-based influenza vaccinesFootnote 15Footnote 16. Thus, the cost of recombinant influenza vaccines (RIV) is typically greater compared to egg-based vaccinesFootnote 15Footnote 16.
The authorization of Supemtek triggered the need for a supplemental NACI statement, as it is the first, and currently the only, RIV available in Canada, and NACI has not previously made a recommendation on RIV in any population. Supemtek (licensed in the US under the tradename Flublok® Quadrivalent) builds on the clinical development of its trivalent predecessor, Flublok (RIV3), a RIV developed by Protein Sciences, Inc. (currently operating as Sanofi Pasteur, Ltd.). Flublok and its quadrivalent formulation, Flublok Quadrivalent, have been licensed for use among adults in the US since 2013 and 2016, respectively. Supemtek has also been licensed for use in the European Union (EU) since 2020. The trivalent and quadrivalent RIV formulations have the same manufacturing process. Additionally, both formulations have a high purity of HA and similar compositions, with the differentiation being that the quadrivalent formulation has a higher content of recombinant HA (180 instead of 135 µg/dose) due to the inclusion of one additional HA antigenFootnote 9. The Supemtek formulation comprises antigens from two influenza A subtype viruses (H1N1 and H3N2) and two influenza type B virus lineages (B/Yamagata lineage and B/Victoria lineage). Supemtek contains three times higher HA content per strain compared with cell- and egg-based standard-dose quadrivalent influenza vaccines. Despite the higher HA content, administration of the vaccine does not appear to be associated significant increase in adverse events (AEs)Footnote 17Footnote 18.
Guidance objective:
The objective of this advisory committee supplemental statement is to review the available evidence on the efficacy, effectiveness, immunogenicity, and safety of Supemtek, and to provide guidance on its use among adults in Canada.
II. Methods
In brief, the broad stages in the preparation of this NACI statement included:
- Knowledge synthesis;
- Synthesis of the body of evidence of benefits and harms, considering the quality of the synthesized evidence and certainty of effects observed across studies;
- Translation of evidence into recommendations.
Details of NACI's evidence-based process for recommendation development can be found elsewhereFootnote 19Footnote 20.
To develop comprehensive, appropriate immunization program recommendations, NACI considers a number of factors. In addition to critically appraising the evidence on burden of disease and vaccine characteristics such as safety, efficacy, immunogenicity and effectiveness, NACI uses a published, peer-reviewed framework and evidence-informed tools to ensure that issues related to ethics, equity, feasibility, and acceptability (EEFA) are systematically assessed and integrated into its guidanceFootnote 21. The NACI Secretariat applied this framework with accompanying evidence-informed tools (Ethics Integrated Filters, Equity Matrix, Feasibility Matrix, and Acceptability Matrix) to consider these programmatic factors systematically for the development of clear, comprehensive, appropriate recommendations for timely, transparent decision-making. For details on the development and application of NACI's EEFA Framework and evidence-informed tools, please see A framework for the systematic consideration of ethics, equity, feasibility, and acceptability in vaccine program recommendations.
For this advisory committee statement, NACI used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework to organize the information and to develop recommendations. Further information on this framework can be found in the GRADE handbook .
A systematic review, including scientific and grey literature, and a meta-analysis were undertaken to develop recommendations for the use of Supemtek seasonal influenza vaccine in adults 18 years of age and older in Canada. The literature review and knowledge synthesis were performed by PHAC staff and supervised by the NACI Influenza Working Group (IWG). Following critical appraisal of individual studies, proposed recommendations for vaccine use were developed. The evidence and proposed recommendations were presented to NACI for deliberation on October 27, 2021 and approved following a thorough review of the evidence. Relevant considerations, rationale for specific decisions, and knowledge gaps are described in the following sections.
II.1 NACI literature review
The policy and research questions addressed in this statement are:
Policy question: Should Supemtek be considered alongside the influenza vaccines already recommended for use by NACI?
Research question: What are the vaccine efficacy, effectiveness, immunogenicity, and safety of Supemtek in persons 18 years of age and older?
The literature search and data extraction were conducted according to the following PICOT framework (Population, Intervention, Comparators, Outcomes and Time):
- P (Population):
- Adults (18 years of age and older)
- I (Intervention):
- Quadrivalent recombinant influenza vaccine (RIV4)
- C (Comparator):
- Egg-based, standard-dose quadrivalent inactivated influenza vaccine (IIV4-SD), trivalent, standard-dose inactivated influenza vaccine (IIV3-SD), high-dose (IIV3- HD) or adjuvanted trivalent inactivated influenza vaccine (IIV3-Adj), mammalian cell culture-based trivalent inactivated influenza vaccine (IIV3-cc) or quadrivalent inactivated influenza vaccine (IIV4-cc), placebo, or no comparator
- O (Outcome):
- Efficacy, effectiveness, immunogenicity, safety
- T (Time):
- Studies published January 2000 or later
The search strategy was developed based on the research question and PICOT illustrated above, in conjunction with a librarian from the Health Library of Health Canada and PHAC (search strategy available upon request). The EMBASE, MEDLINE, Cochrane Central, Scopus, ProQuest Public Health, and ClinicalTrials.gov, electronic databases were searched for primary research articles and case reports. Registered clinical trials and grey literature from international public health authorities and National Immunization Technical Advisory Groups were also considered. Searches were restricted to articles published in English or French due to the language proficiencies of the reviewers. Additionally, hand-searching of the reference lists of included articles was performed by one reviewer to identify additional relevant publications. All searches were performed on January 12, 2021, with an update to August 8, 2021.
Two reviewers independently screened the titles and abstracts of records retrieved from the database searches for potential eligibility. DistillerSR® (Evidence Partners Inc., Ottawa, Canada) was used to operationalize screening and data management. The full texts of records deemed potentially eligible were obtained and independently reviewed by both reviewers for potential inclusion in the review. Refer to Appendix A for the PRISMA Flow Diagram of study selection.
Studies were included if they met the following criteria:
- The study population or subpopulation consisted of adults 18 years of age and older;
- Study assessed efficacy and effectiveness, immunogenicity, or safety of RIV4;
- Primary research studies from peer-reviewed scientific literature;
- Case reports and case series;
- Registered clinical trials and grey literature from international public health authorities (Australian Technical Advisory Group on Immunisation [ATAGI]; Centers for Disease Control and Prevention [CDC]; clinicaltrials.gov; European Centre for Disease Prevention and Control [ECDC]; European Medicines Agency [EMA]; Department of Health Services Research & Policy [HSRP]; International Clinical Trials Registry Platform [ICTRP]; World Health Organization [WHO]);
- Study is published in English or French; and
- Published in 2000 or later.
Studies were excluded if they met one or more of the following criteria:
- The study did not present data on any of: the efficacy, effectiveness, immunogenicity, or safety of RIV4;
- The study is in a language other than English or French;
- The study is a non-human or in vitro study;
- The article is not a primary research study;
- The article is an editorial, opinion, commentary or news report;
- The article is an economic study, clinical practice guideline, consensus conference, health technology assessment (HTA) report;
- The article was a doctoral dissertation, master's thesis, or conference summary; or
- The article is a duplicate.
One reviewer extracted data from the studies included for review into an evidence table using a piloted data abstraction template designed to capture information on study design, population and outcomes of interest. A second reviewer independently validated the abstracted data. Two reviewers independently assessed the risk of bias within each included study using the Cochrane tools (RoB 2.0Footnote 22 for randomized trials and ROBINS-IFootnote 23 for non-randomized studies of interventions). The Joanna Briggs Institute (JBI) checklist was used to examine potential risks of bias in case reports or case seriesFootnote 24. The strength and certainty of evidence included in syntheses were assessed by two independent reviewers using the GRADE systemFootnote 25Footnote 26. In the current review, GRADE assessment was reserved for outcomes deemed to be critical or important to decision making by the IWG based on the results of a prioritization exercise. The following critical outcomes and definitions were identified:
- Serious Adverse Event (SAE): Any untoward medical occurrence that at any dose results in death, requires inpatient hospitalization or prolongation of existing hospitalization, results in persistent or significant disability or incapacity, or is life-threatening.
- Laboratory Confirmed Influenza (LCI)-related mortality: A death during an influenza season resulting from a clinically compatible illness that was confirmed to be influenza by an appropriate laboratory test (e.g., reverse transcription polymerase chain reaction (RT-PCR), virus culture or antigen detection); all influenza (A and B).
- Laboratory Confirmed Influenza (LCI): Symptoms of influenza with a positive laboratory diagnosis by reverse transcription polymerase chain reaction (RT-PCR), virus culture or antigen detection; all influenza (A and B).
- Solicited systemic AE: Intentionally solicited systemic reactions including but not limited to fever, malaise, muscle pain, headache or loss of appetite.
- Seroprotection: Proportion of subjects achieving a hemagglutination inhibition (HI) titre of ≥1:40 post-vaccinationFootnote 27.
- Seroconversion: Proportion of subjects achieving an increase from ≤1:10 HI titre pre-vaccination to ≥1:40 post-vaccination or achieving at least four-fold rise in HI titresFootnote 27.
- Geometric Mean Titre Ratio (GMTR): Ratio of Geometric Mean Titre (GMT) post-vaccination of previously licensed vaccine to GMT post-vaccination of new vaccineFootnote 27.
For each outcome definition identified, the GRADE framework was used to assess the strength and certainty of the evidence. GRADE guidance was followed for determining the extent of the risk of bias for the body of evidence. Any disagreements or discrepancies during the data extraction and quality appraisal processes were resolved by discussion and consensus. The knowledge synthesis was performed by AG, AS, MX, and PD, and was supervised by the IWG.
Data were compiled by outcome to evaluate: the availability of quantitative evidence; heterogeneity with respect to comparisons, outcome definitions, and time point of measurement; and feasibility and appropriateness of meta-analysis. Meta-analyses were performed to pool study estimates for seroconversion rates and proportion of study participants who experienced an AE following immunization with Supemtek compared to other seasonal influenza vaccine recipients. Only estimates from studies deemed to be clinically and methodologically similar were pooled. A random effects model was used for all meta-analyses. Subgroup analyses were conducted by age group (18 to 49 years old, 50 to 64 years old, 65 years and older), vaccine strains, and influenza vaccine type. Potential heterogeneity between studies was assessed using the I2 statistic, with a threshold of 50% or higher suggesting potentially important heterogeneity. Forest plots have been provided to present meta-analyses. Potential publication bias was assessed using funnel plots.
All analyses were conducted using the RevMan 5.0 meta-analysis softwareFootnote 28.
III. Vaccine
III.1 Recombinant influenza vaccine preparation authorized for use in Canada
Supemtek is an unadjuvanted RIV4 made from recombinant HA expressed in proprietary expresSF+ insect cells (derived from Spodoptera frugiperda cells) using baculovirus as a vector for protein expression. It is authorized for intramuscular (IM) injection and is available as a 0.5 mL single-dose, pre-filled syringe without a needle. Supemtek does not contain egg proteins, antibiotics, or preservatives. There is no gelatin added in Supemtek as a stabilizer. The single-dose, prefilled syringes also do not contain any natural rubber latex. For more information on Supemtek, refer to the product monographFootnote 9.
| Route of administration | Dosage | Non-medicinal ingredients |
|---|---|---|
| Intramuscular | Each 0.5 mL dose contains 45 μg of HA of each of the four influenza virus strains contained in the vaccine |
Sodium chloride, monobasic sodium phosphate, dibasic sodium phosphate, and polysorbate 20. Each dose may also contain residual amounts of: Baculovirus and Spodoptera frugiperda cell proteins, baculovirus and cellular DNA, and Triton X-100. |
III.2 Vaccine efficacy and effectiveness
Two vaccine efficacy and effectiveness outcomes were ranked as critical during the outcome prioritization process: efficacy or effectiveness against laboratory-confirmed influenza (LCI)-related mortality and efficacy or effectiveness against LCI.
One peer-reviewed study that assessed the efficacy of Supemtek against LCI was identified and included in the reviewFootnote 17 and is summarized below.
Although one effectiveness study reporting on influenza hospital encounters was identified as part of this review, the study by Izurieta et al. (2020)Footnote 29 was not included in the evidence synthesis because it did not provide data on LCI outcomes that were pre-specified as critical for decision making in this analysis. Therefore, the certainty of evidence from this study was not assessed and the study will not be presented further.
Peer-reviewed, published clinical data pertaining to the efficacy or effectiveness of vaccination with RIV4 during pregnancy or including breastfeeding were not available at the time of this review.
Efficacy against laboratory-confirmed influenza-related mortality
No studies reported on the efficacy of Supemtek against LCI-related mortality and studies evaluating the efficacy of Flublok against LCI-related mortality were beyond the scope of this review.
Efficacy against laboratory-confirmed influenza infection
The study by Dunkle et al. (2017a)Footnote 17 assessed the relative vaccine efficacy (rVE) of Supemtek compared to egg-based IIV4-SD against LCI infection during the 2014-2015 influenza season in the US. Specifically, Dunkle et al. (2017a) conducted a participant, care provider, investigator, and outcomes assessor-blind parallel Phase 3-4 randomized clinical trial to determine the rVE of Supemtek compared to egg-based IIV4-SD against reverse transcription polymerase chain reaction (RT-PCR) confirmed influenza infection and culture-positive influenza infectionFootnote 17. The clinical trial was conducted in medically stable, ambulatory adults 50 years of age and older (mean age: 63; age range: 50-96) at 40 outpatient centres across the USFootnote 17. Individuals testing positive for influenza by RT-PCR or viral culture between 14 and 224 days after vaccination were classified as casesFootnote 17.
The results from the study by Dunkle et al. (2017a) indicated that study participants who received Supemtek had statistically significantly lower risk of having any RT-PCR LCI infection compared to study participants who received IIV4-SD (rVE: 30%; 95% confidence interval (CI): 10 to 47%; hazard ratio [HR]: 0.69; 95% CI: 0.53 to 0.90; p=0.006)Footnote 17. In separate sub-group analyses, the rVE for adults 50 years of age and older who were vaccinated with Supemtek versus IIV4-SD was statistically significant for influenza A (rVE: 36%; 95% CI: 14 to 53%) and was not statistically significant against RT-PCR LCIB (rVE: 4%; 95% CI: -72 to 46%)Footnote 17. This trial was performed during the 2014-15 influenza season which was characterized by widespread circulation of antigenically mismatched influenza A(H3N2)Footnote 17. The pre-specified non-inferiority criterion required a lower bound of the 95% CI for rVE greater than −20% and the pre-specified superiority criterion required a lower bound of the 95% CI for rVE greater than 9%Footnote 17. A pre-specified exploratory analysis for superiority was also assessed if the primary endpoint had a lower bound 95%CI of > 9%. Since the lower bound here was 10% for the primary endpoint, this pre-specified endpoint for superiority was met. However, subgroup analyses by influenza type demonstrated that adults 50 years of age and older who were vaccinated with Supemtek had statistically significantly lower risk of having any RT-PCR LCIA (rVE: 36%; 95% CI: 14 to 53%; HR: 0.64; 95% CI: 0.48 to 0.86; p=0.003)Footnote 17. rVE against RT-PCR LCI for adults 50 to 64 years of age who were vaccinated with Supemtek compared to egg-based IIV4-SD was 42% (95% CI: 15 to 61%) and 17% (95% CI: -20 to 43%) for adults > 64 years of ageFootnote 17. rVE estimates were similar between RT-PCR LCI infections and viral culture-positive influenza infections for all subgroup analyses conductedFootnote 17. This study was conducted in adults aged 50 years and over and, therefore, the findings may not be directly applicable to younger adult populations. Moreover, the study presented wide CIs around the outcome measures important to this analysis. Due to the limitations of the available vaccine efficacy data, the overall quality of the body of evidence for this outcome was rated as low. Additional details regarding study characteristics and results are shown in Table 4.
III.3 Immunogenicity
Regulators in Canada, the US, and Europe accept non-inferiority immunogenicity trials that compare the HI antibody response of the new vaccine to that of an existing licensed vaccine, or placebo-controlled immunogenicity trials that assess the HI antibody response to the new vaccine. Non-inferiority and placebo-controlled immunogenicity trials are often considered sufficient by regulatory authorities when there are bridging data to correlate immunogenicity outcomes to clinical protection, or when the new vaccines are considered by the regulators to be very similar to vaccines already authorized. Serological assessments based on the GMTs of HI antibody that are used by regulators are: GMTR, seroprotection rate, and seroconversion rate. The US Food and Drug Administration (FDA) has published definitions for these serological assessments and criteria for immunogenicity data necessary for influenza vaccine licensureFootnote 27, which are also used in Canada. These definitions and currently used criteria are shown in Table 3. Correlates of protection that are not based on HI antibody titres have not been well established.
Three vaccine immunogenicity outcomes were ranked as critical during the outcome prioritization process of this review: seroprotection rate, seroconversion rate, and GMTR. Although GMT was not identified as a critical outcome, evidence reporting on GMT will be presented to supplement the evidence base for immunogenicity.
Eight RCTs that assessed the immunogenicity of Supemtek compared to different influenza vaccines, including IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), IIV3-Adj (Fluad®, Seqirus, Inc.), IIV4-SD (FluQuadri™, Sanofi Pasteur; Fluarix Quadrivalent, GlaxoSmithKline; Fluzone Quadrivalent, Sanofi Pasteur), and IIV4-cc (Flucelvax® Quadrivalent, Seqirus), were identified in this review. One study was conducted among adult military beneficiaries 18 years of age and olderFootnote 30, one study was conducted among adult participants 50 years of age and olderFootnote 17, three studies were conducted among adult participants 65 years of age and olderFootnote 31Footnote 32Footnote 33, two studies focused on adult participants 18 to 49 years of ageFootnote 34Footnote 35, and one study was conducted among healthcare personnel 18 to 64 years of ageFootnote 36. Of these studies, two were conducted during the 2014-2015 influenza seasonFootnote 17Footnote 34, three were conducted over the 2017-2018 influenza seasonFootnote 31Footnote 32Footnote 35, and three were conducted over the 2018-2019 influenza seasonFootnote 30Footnote 33Footnote 36. Additional details on the immunogenicity findings from these studies are shown in Table 5. Overall, there was fair evidence (of moderate certainty) that the immunogenicity for Supemtek is non-inferior to traditional egg-based comparators, based on data in adults aged 18 years and older. Three RCTs were identified to have an unclear risk of selection bias as these studies did not specify the method of random sequence generationFootnote 30Footnote 32Footnote 35. Two RCTs were identified to have a moderate risk of recruitment bias as these studies were conducted at a single-centre that may not be representative of the population of interestFootnote 31Footnote 35. One RCT was identified to have an unclear risk of recruitment bias as it did not specify the site used for recruitmentFootnote 32.
Seroprotection rate
Four RCTs were identified that assessed the seroprotection rate of HI titres against HA of Supemtek at approximately three to five weeks post-vaccinationFootnote 17Footnote 31Footnote 33Footnote 36. Of these studies, one was conducted during the 2014-2015 influenza seasonFootnote 17, one was conducted over the 2017-2018 influenza seasonFootnote 31, and two were conducted over the 2018-2019 influenza seasonFootnote 33Footnote 36. The comparator vaccines for these four studies included IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline), IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), and IIV3-Adj (Fluad, Seqirus, Inc.). Three RCTs were conducted among adult participants 50 years of age and olderFootnote 17Footnote 31Footnote 33 and one RCT was conducted among adult healthcare personnel 18 to 64 years of ageFootnote 36. Only one RCT out of the four studies also assessed the seroprotection rate of HA of Supemtek at 56 days and 182 days post-vaccinationFootnote 33. The comparator vaccines for this study included IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 33.
At approximately one month post-vaccination, the seroprotection rate in Supemtek recipients was similar to or higher than seroprotection rates for recipients of the comparator vaccines (IIV4-SD, IIV4-cc, IIV3-HD, IIV3-Adj) in adults 18 years of age and olderFootnote 17Footnote 31Footnote 33Footnote 36. In two of the four studies, RIV4 met the non-inferiority criteria specified by the US FDA for all tested influenza strains including A(H1N1), A(H3N2), B/Yamagata lineage, and B/Victoria lineageFootnote 33Footnote 36. Across the four RCTs, RIV4 met non-inferiority criteria against five of seven tested strains of A(H3N2)Footnote 17Footnote 31Footnote 33Footnote 36. In Belongia et al. (2020), RIV4 demonstrated lower rates of seroprotection for older adults 65 to 74 years of age against two of four tested strains of A(H3N2)Footnote 31. However, one limitation was the small sample size of the studyFootnote 31. In the study by Dunkle et al. (2017a), RIV4 met the non-inferiority threshold for seroprotection against influenza A(H1N1), A(H3N2), and B/Yamagata lineage, but not against influenza B/Victoria lineage in adults aged 50 and olderFootnote 17 Please link to reference at end of document. The FDA non-inferiority criterion required a lower bound of the 95% CI for the percentage of participants achieving seroprotection greater than or equal to 70% for adults under 65 years of age and greater than or equal to 60% for adults 65 years of age or olderFootnote 27.
At 56 and 182 days post-vaccination, seroprotection rate against A/Michigan/45/2015 (H1N1) and B/Colorado/06/2017 (Victoria lineage) were slightly lower in Supemtek recipients compared to IIV3-HD recipientsFootnote 33. However, no test of significance was conducted. At 56 and 182 days post-vaccination, seroprotection rates in Supemtek recipients against other tested influenza strains were comparable to or greater than seroprotection rates for recipients of the comparator vaccine (IIV3-HD) in adults 65 years of age and olderFootnote 33. Additional details on the immunogenicity findings in adults can be found in Table 5.
Seroconversion rate
Eight RCTs were identified that assessed the seroconversion rate of HA of Supemtek at approximately three to five weeks post-vaccinationFootnote 17Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36. Of these studies, two were conducted during the 2014-2015 influenza seasonFootnote 17Footnote 32, three were conducted over the 2017-2018 influenza seasonFootnote 31Footnote 32Footnote 35, and three were conducted over the 2018-2019 influenza seasonFootnote 30Footnote 33Footnote 36. The comparator vaccines for these eight studies included IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus, Inc.), IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline; FluQuadri, Sanofi Pasteur; Fluzone Quadrivalent, Sanofi Pasteur), and IIV4-cc (Flucelvax Quadrivalent, Seqirus). One RCT assessed the seroconversion rate of HA of Supemtek at 56 days and 182 days post-vaccinationFootnote 33. The comparator vaccines for this study included IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 33. Of the eight studies, one study was conducted among adult military beneficiaries 18 years of age and olderFootnote 30, one study was conducted among adult participants 50 years of age and olderFootnote 17, three studies were conducted among adult participants 65 years of age and olderFootnote 31Footnote 32Footnote 33, two studies focused on adult participants 18 to 49 years of ageFootnote 34Footnote 35, and one study was conducted among healthcare personnel 18 to 64 years of ageFootnote 36.
In four of the eight studies, at approximately three to five weeks post-vaccination, Supemtek demonstrated non-inferiority to IIV3-HD, IIV3-Adj, IIV4-SD, and IIV4-cc in the HI antibody responses against influenza A(H1N1), A(H3N2), B/Yamagata and B/Victoria lineage contained in the comparator vaccines, based on seroconversion ratesFootnote 31Footnote 32Footnote 33Footnote 36. The FDA non-inferiority criterion required that the difference between the upper bound of the 95% CI of the seroconversion between the licensed vaccine and the new vaccine (i.e., seroconversion of licensed vaccine – seroconversion of new vaccine) did not exceed 10 percentage pointsFootnote 27.
There were different results in the remaining studies. The two studies by Dunkle et al. (2017) demonstrated that, compared to IIV4-SD, RIV4 met the non-inferiority threshold in HI antibody responses for 3 of the 4 virus strains. Non-inferiority, however, was not met against the B/Victoria lineage in adults 18 to 64 years of ageFootnote 17Footnote 34. Additionally, rates of seroconversion following RIV4 did not meet the non-inferiority threshold compared to IIV4-SD against influenza A(H1N1) in adults 64 and olderFootnote 17. Non-inferiority could not be assessed for the remaining two RCTs as these studies did not state CIs for seroconversion estimatesFootnote 30Footnote 35. Due to the heterogeneity in the influenza strain, vaccine type, follow-up period, and population in the seroconversion rates measured, only three of the eight studies identified could be pooled through meta-analysis. When data from three RCTs in adult participants 50 years of age and older were combined and weighted using a random effects model, there was little difference in seroconversion rates between Supemtek and other seasonal influenza vaccine comparators (odds ratio [OR]: 1.36; 95% CI: 1.00 to 1.86; Figure 1)Footnote 17Footnote 32Footnote 33.
At 56 and 182 days post-vaccination, Supemtek demonstrated comparable HI antibody responses against A(H1N1), A(H3N2), B/Victoria lineage, and B/Yamagata lineage to IIV3-HD (Fluzone High-Dose, Sanofi Pasteur) in adults 65 years of age and older, based on seroconversion ratesFootnote 33.
Geometric Mean Titre and Geometric Mean Titre Ratio
Eight RCTs assessed the GMT and/or GMTR of Supemtek compared to various different influenza vaccines including IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus, Inc.), IIV4-SD (FluQuadri, Sanofi Pasteur; Fluarix Quadrivalent, GlaxoSmithKline; Fluzone Quadrivalent, Sanofi Pasteur), IIV4-cc (Flucelvax Quadrivalent, Seqirus) at approximately three to twenty-six weeks (i.e., six months) following influenza vaccination were identified in this reviewFootnote 17Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36Footnote 37. Of these studies, two were conducted during the 2014-2015 influenza seasonFootnote 17Footnote 34Footnote 37, three were conducted over the 2017-2018 influenza seasonFootnote 31Footnote 32Footnote 35 and three were conducted over the 2018-2019 influenza seasonFootnote 30Footnote 33Footnote 36.
Three studies assessed the GMTR of Supemtek compared to IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline; Fluzone Quadrivalent, Sanofi Pasteur) at approximately one month following vaccination in adults 18 years of age or olderFootnote 17Footnote 34Footnote 36Footnote 37. In one study, RIV4 met the non-inferiority criteria specified by the US FDA for all tested influenza strains including A(H1N1), A(H3N2), B/Yamagata lineage, and B/Victoria lineageFootnote 36. In two of the three studies, seroresponses to A(H1N1), A(H3N2), and B/Yamagata lineage in RIV4 recipients aged 18 to 64 years were comparable to seroresponses in IIV4-SD recipients based on the GMTRFootnote 17Footnote 34Footnote 37. However, the GMTR against B/Victoria lineage for IIV4-SD recipients compared to RIV4 recipients did not meet the non-inferiority criteria set by the US FDAFootnote 17Footnote 34Footnote 37. The FDA non-inferiority criterion required an upper bound 95% CI on the GMTR to be less than or equal to 1.5Footnote 27. Geometric mean titre estimates could not be pooled during meta-analysis due to the heterogeneity between study populations (i.e., studies were conducted among different age groups).
Five RCTs assessed the GMT of Supemtek compared to various different influenza vaccines including IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus, Inc.), IIV4-SD (FluQuadri, Sanofi Pasteur; Fluarix Quadrivalent, GlaxoSmithKline; Fluzone Quadrivalent, Sanofi Pasteur), IIV4-cc (Flucelvax Quadrivalent, Seqirus) at three to eight weeks following vaccinationFootnote 30Footnote 31Footnote 32Footnote 33Footnote 35. GMTs in Supemtek recipients were similar to or higher than GMTs for recipients of the comparator vaccinesFootnote 30Footnote 31Footnote 32Footnote 33Footnote 35.
Additional details on the immunogenicity findings in adults can be found in Table 5.
III.4 Safety
Two vaccine safety outcomes were ranked as critical during the outcome prioritization process for this review: SAEs and solicited systemic AEs.
This review identified six peer-reviewed studies that assessed the safety of Supemtek in adults, including five RCTs and one review of post-marketing surveillance data in adultsFootnote 17Footnote 32Footnote 33Footnote 34Footnote 38Footnote 39. Of these studies, two were conducted during the 2014-2015 influenza seasonFootnote 17Footnote 34, two were conducted during the 2017-2018 influenza seasonFootnote 32Footnote 38, one was conducted during the 2018-2019 influenza seasonFootnote 33, and one study reported data from the Vaccine Adverse Event Reporting System (VAERS) from July 1, 2017, through June 30, 2020Footnote 39. Among the five RCTs, one study was conducted among adult participants 18 to 49 years of ageFootnote 34, one study was conducted among adult participants 50 years of age and olderFootnote 17, and three studies focused on adult participants 65 years of age and olderFootnote 32Footnote 38Footnote 39. Notably, no published clinical data pertaining to the safety of vaccination with RIV4 during pregnancy were available at the time of this review to inform vaccine-associated risks. Vaccine comparators used in the five RCTs included IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus, Inc.), IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline; FluQuadri, Sanofi Pasteur)Footnote 17Footnote 32Footnote 38Footnote 39. There was moderate certainty of evidence for the safety outcomes overall. A common concern across the studies reporting on the safety of Supemtek in adults was the imprecision of the estimates due to the lack of CIs reported in four of the five RCTsFootnote 17Footnote 32Footnote 34Footnote 38 and the uncertainties regarding the completeness, quality, and consistency of the data reported to VAERSFootnote 39.
Additional details on the safety evidence presented in this review are shown in Table 6.
Serious adverse events
Five studies were identified that evaluated the occurrence of SAEs in recipients of Supemtek, including four RCTsFootnote 17Footnote 32Footnote 33Footnote 34 and one review of post-marketing surveillance data in adultsFootnote 39 SAEs reported across clinical trials were not considered by the investigators to be related to the trial vaccinesFootnote 17Footnote 32Footnote 33Footnote 34Footnote 39 and SAE rates were not significantly different between the study vaccine and the comparator vaccine(s).
One RCT examined the occurrence of SAEs in adult participants 18 to 49 years of age six months following Supemtek or IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline) administrationFootnote 34. In this study, 1% of individuals who received Supemtek experienced at least one SAEs within six months following vaccinationFootnote 34. The occurrence of SAEs was similar between the vaccine groups, and the study did not find any deaths or SAEs to be related to the study vaccinesFootnote 34.
Three RCTs examined the occurrence of SAEs in adult participants 50 years of age or olderFootnote 17Footnote 32Footnote 33. Cowling et al. (2020a) found that 6.6% of Supemtek recipients experienced hospitalization within 30 days following vaccinationFootnote 32. This proportion was comparable to or less than the proportion of participants who experienced hospitalization within 30 days of receiving a comparator vaccine, and all SAEs were deemed unrelated to the study vaccinesFootnote 32. One RCT found that 3.4% and 3.0% of adult participants 50 years of age or older experienced at least one SAE within six months of receiving Supemtek and IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline), respectivelyFootnote 17. Common SAEs among this group of participants included cardiac disorders, musculoskeletal and connective tissue disorders, and infections and infestationsFootnote 17. Death occurred in 8 Supemtek recipients and in 12 IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline) recipientsFootnote 17. The occurrence of SAEs was similar between the vaccine groups, and the study did not find any deaths or SAEs to be related to the study vaccinesFootnote 17. The third RCT examined the occurrence of SAEs in adult participants 65 years of age or older within six months after receiving Supemtek or IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 33. This RCT found that 2% and 3.9% of adult participants 65 years of age or older experienced a SAE within six months after receiving Supemtek and IIV3-HD (Fluzone High-Dose, Sanofi Pasteur), respectivelyFootnote 33. Common SAEs found in this study included infections and infestations, metabolism and nutrition disorders, and injury, poisoning, and procedural complicationsFootnote 33. No SAEs were considered to be related to the study vaccinesFootnote 33. When data from two RCTs in adult participants 50 years of age and older were combined and weighted using a random effects model, there was no difference in the odds of experiencing a serious adverse event following administration of Supemtek and other seasonal influenza vaccine comparators (OR: 1.01; 95% CI: 062 to 1.66; Figure 2)Footnote 17Footnote 33.
A clinical review of post-licensure surveillance data from the VAERS, which is a passive surveillance system useful for detecting safety issues related to newly licensed vaccines for use in the US, identified 849 AE reports following Supemtek administration from July 1, 2017, through June 30, 2020Footnote 39. Of these 849 AE reports, 39 were SAEFootnote 39. Notably, ten reports of Guillain-Barré syndrome were identified; two reports met Brighton Collaboration criteria level 1, five reports met Brighton Collaboration criteria level 2, and three reports met Brighton Collaboration criteria level 3Footnote 39. Three serious reports of anaphylaxis were identified, including two reports that met Brighton Collaboration criteria level 2, and one report that did not meet Brighton Collaboration criteria, but was diagnosed by the attending physician as an anaphylactic reactionFootnote 39.
Solicited systemic adverse events
Four studies were identified that evaluated the occurrence of solicited systemic AEs in recipients of Supemtek, including three RCTsFootnote 33Footnote 34Footnote 38 and one review of post-marketing surveillance data in adultsFootnote 39. Most systemic reactions reported by the clinical trials were mild to moderate in severity and were transient in natureFootnote 33Footnote 34Footnote 38.
One RCT examined the proportion of adult participants 18 to 49 years of age who experienced solicited systemic AEs of any severity within 6-7 days following vaccination with Supemtek or IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline)Footnote 34. The proportion of participants who experienced at least one solicited systemic AE of any severity, at least one Grade 3 (i.e., severe) solicited systemic AE, and at least one Grade 4 (i.e., life-threatening) solicited systemic AE following Supemtek or the comparator vaccine IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline), were similarFootnote 34. Of the participants who received Supemtek, 34.1% experienced at least one solicited systemic AE of any severity, 2.3% experienced a Grade 3 (i.e., severe) solicited systemic AE, and 0% experienced a Grade 4 (i.e., life-threatening) solicited systemic AE within 6-7 days following vaccinationFootnote 34. Common solicited systemic AEs included headache, fatigue, and muscle painFootnote 34.
One RCT examined the proportion of adult participants 65 years of age or older who experienced at least one mild, moderate, or severe solicited systemic AE at one, three to four, seven to nine, and 14 to 16 days following vaccination with Supemtek, IIV4-SD (FluQuadri, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus), and IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 38. The proportion of participants who experienced at least one solicited systemic AE of each severity was similar between Supemtek and the comparator vaccines, including IIV4-SD (FluQuadri, Sanofi Pasteur), IIV3-Adj (Fluad, Seqirus), and IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 38. At one day following vaccination, 0.4%-5.0%, 0% and 0.4% of Supemtek recipients reported mild, moderate and severe solicited systemic AEs, respectivelyFootnote 38. At three to four days following vaccination, 1.5%-5.5%, 0.7%-1.1% and 0% of Supemtek recipients reported mild, moderate and severe solicited systemic AEs, respectivelyFootnote 38. At seven to nine days following vaccination, 0.3%-5.9%, 0.3%-0.7% and 0.3% of Supemtek recipients reported mild, moderate and severe solicited systemic AEs, respectivelyFootnote 38. At 14 to 16 days following vaccination, 0%-5.2%, 0%-1.6%, 0.7% of Supemtek recipients reported mild, moderate and severe solicited systemic AEs, respectivelyFootnote 38. Common solicited systemic AEs at all three time points included mild fatigue, mild muscle pain, mild feverishness, and other mild systemic AEsFootnote 38.
One RCT examined the proportion of adult participants 65 years of age or older who experienced at least one solicited systemic AE within six days of receiving Supemtek or IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 33. The proportion of participants who experienced at least one solicited systemic AE of any severity and at least one severe solicited systemic AE was similar between Supemtek and the comparator vaccine IIV3-HD (Fluzone High-Dose, Sanofi Pasteur)Footnote 33. Within six days following vaccination, 25.8% (95% CI: 19.1, 33.6) of 151 Supemtek recipients experienced at least one solicited systemic AE of any severity and 2.6% (95% CI: 0.7to 6.6%) of the Supemtek recipients experienced at least one severe adverse eventFootnote 33. Common solicited systemic AEs included muscle pain, fatigue, and headacheFootnote 33.
A clinical review of post-licensure surveillance data from the VAERS, identified 849 adverse event reports following Supemtek administration from July 1, 2017, through June 30, 2020Footnote 39. Of these reports, the most common solicited systemic AEs reported included pyrexia, headache, and rash.
IV. Discussion
This systematic review examined studies of the efficacy, immunogenicity, and safety of Supemtek, a recombinant seasonal influenza vaccine approved for adult use in Canada. The peer-reviewed published evidence on the efficacy of Supemtek against LCI illness was sparse. One RCT that evaluated the rVE of Supemtek was identified in this reviewFootnote 17. The efficacy study by Dunkle et al. (2017) demonstrated that Supemtek was statistically significantly more efficacious than egg-based IIV4-SD in preventing LCI-A infection in adults 50 years of age or older. Compared to IIV4-SD, RIV4 met the non-inferiority threshold in HI antibody responses for 3 of the 4 virus strains. Non-inferiority, however, was not met against the B/Victoria lineage in adults 50 years of age and olderFootnote 17. The data from this clinical trial have limitations. The results may not be applicable to all influenza seasons as the study was conducted in the 2014-2015 influenza season in the US, which was A(H3N2)-dominant. Additionally, since the efficacy estimates were derived from one clinical trial conducted among adults 50 years of age or older, these efficacy estimates may not be generalizable to younger adults (e.g., adults 18 to 49 years of age). Furthermore, the CIs surrounding the efficacy estimates were wide, suggesting a risk of imprecision. A previous study by Treanor et al. (2011) found that the efficacy of Flublok, the previously FDA-approved trivalent formulation of Supemtek, was superior to a saline placebo against culture-positive influenza A, but not culture-positive influenza B in adults 18 to 49 years of age during the 2007-2008 influenza season in the USFootnote 40. The NACI IWG had prespecified vaccine efficacy against laboratory confirmed influenza-related mortality to be a critically important outcome to be considered, but no data were available for this outcome.
Eight RCTs conducted in adults that specifically assessed the immunogenicity of Supemtek were identified in this reviewFootnote 17Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36. Overall, across the eight studies, Supemtek demonstrated non-inferiority compared to egg-based influenza vaccines against influenza A(H1N1), most strains of A(H3N2), and B/Yamagata lineageFootnote 17Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36. Findings differed across studies regarding the non-inferiority of RIV4 compared to egg-based influenza vaccines against influenza B/Victoria lineage based on seroconversion rates, seroprotection rates, GMTs, and GMTRFootnote 17Footnote 34. The immunogenicity evidence for Supemtek builds on the clinical development program of Flublok (RIV3) in the US.
This review also examined six studies that assessed the safety of Supemtek, including five RCTsFootnote 17Footnote 32Footnote 33Footnote 34Footnote 38 and one post-marketing surveillance studyFootnote 39. The five RCTs found that Supemtek is a safe, well-tolerated, and immunogenic alternative to conventional egg-based influenza vaccines for adults (noting that no published clinical data pertaining to the safety of vaccination with RIV4 during pregnancy were available at the time of this review to inform vaccine-associated risks)Footnote 17Footnote 32Footnote 33Footnote 34Footnote 38. Post-marketing surveillance data revealed that the lack of egg proteins in Supemtek does not eliminate the risk of allergic reactions following vaccine administration, as allergic reactions can occur following exposure to any drug or vaccineFootnote 41. The five RCTs did not identify an elevated risk of severe allergic reactions compared to traditional egg-based influenza vaccinesFootnote 17Footnote 32Footnote 33Footnote 34Footnote 38.
Recombinant technology is a method of influenza vaccine production that is significantly different from existing egg-based and mammalian cell-culture-based technology. Recombinant technology is the quickest method of influenza vaccine production as it does not depend on the growth of candidate vaccine viruses. Unlike egg- or cell-based vaccines, recombinant technologies do not result in vaccine viruses that are adapted from growth in eggs or in cells; instead, recombinant technology ensures an exact match to the key component of the influenza strains recommended annually by the WHO. Furthermore, RIV are insulated from egg-adaptive changes and pose negligible mutation riskFootnote 12. As such, they have the potential to provide enhanced protection in some seasons compared to standard egg-based influenza vaccinesFootnote 12. Similar to mammalian cell culture-based vaccines, recombinant vaccines may offer enhanced manufacturing scalability, sterility, timeliness, and flexibilityFootnote 10Footnote 11Footnote 12. The flexible and quick manufacturing process of recombinant vaccines may be helpful in a prompt response to rapid and emerging circulating seasonal influenza strains in a post-COVID-19 pandemic setting. The diversification of vaccine platforms can help to overcome influenza supply vulnerabilities and to improve vaccine-production capacity, which may be particularly helpful in an influenza pandemic setting, in cases of vaccine shortage, and in cases of egg supply shortageFootnote 10.
The NACI Secretariat applied the Committee's EEFA Framework to assess the implications of ethics, equity, feasibility and acceptability of its recommendation for the use of Supemtek for the prevention of influenza in adults aged 18 years and older in Canada. There were no potential inequities or ethical considerations identified that could arise with the recommendation of Supemtek. However, acceptability of a newly approved vaccine such as Supemtek by the general public, providers and policymakers could be affected by the vaccine's real or perceived potential risks and unknowns. Potential feasibility issues identified are the limited manufacturing infrastructure and the comparatively higher cost of RIV compared to egg-based vaccines. No cost analyses or economic evaluations were conducted prior to the development of this statement and the true cost of RIV, particularly following the optimization of manufacturing infrastructure, is unknownFootnote 16.
Given the novelty of RIV, ongoing monitoring of new and emerging evidence on RIV4 efficacy, effectiveness, immunogenicity, and safety will be important. As additional research data on RIV4 become available, further analyses could explore comparisons of these outcomes between seasons and against different influenza subtypes, with comparisons to existing egg-based and mammalian cell culture-based influenza vaccines.
Notably, very limited peer-reviewed, published data on the use of RIV in pregnant individuals and in other vulnerable populations are available to inform vaccine-associated risks. For example, a new study has been published on the safety of Supemtek compared to IIV4-SD in adults self-identified as ethnically Chinese and aged 18-64 years, including pregnant individuals, during the 2018-2019 influenza season in the USFootnote 42. The study found that RIV4 has a comparable safety profile to IIV4-SD and demonstrated safety findings consistent with the studies included in this review.
In addition, safety data on the use of RIV3 in pregnant adults are available and may be considered to supplement the safety evidence base given that the trivalent and quadrivalent RIV formulations are produced using the same manufacturing platform and have overlapping compositions. For example, a supplemental safety analysis stratified on pregnancy status that was conducted as part of a retrospective cohort study evaluating the safety of RIV3 compared to IIV3 in adults aged 18 years and older during a single influenza season (2015-2016) did not detect any safety concernsFootnote 43. A more robust, comprehensive, and consistent body of evidence, including further data on comorbidities, pregnant individuals, health status, and other potential confoundersFootnote 44, is needed to evaluate the relative effectiveness and safety of Supemtek compared to other injectable influenza vaccines.
V. Recommendations
Following the thorough review of available evidence summarized above, as well as the assessment of ethics, equity, feasibility and acceptability considerations with the EEFA Framework, the following section outlines the evidence-informed recommendation made by NACI regarding the use of Supemtek in adults 18 years of age and older. NACI will continue to carefully monitor the scientific developments related to influenza vaccines, as well as ongoing vaccine pharmacovigilance, and will update its recommendations as required. Additional information on the strength of NACI recommendations and the grading of evidence is available in Table 3.
The following recommendation for Supemtek supplements NACI's overarching recommendation for influenza vaccination, which is available in the NACI Seasonal Influenza Vaccine Statement. The overarching NACI recommendation for influenza vaccination is that an age-appropriate influenza vaccine should be offered annually to anyone 6 months of age and older (Strong NACI Recommendation), noting product-specific contraindications.
1. NACI recommends that Supemtek may be considered among the seasonal influenza vaccines offered to adults 18 years of age and older. (Discretionary NACI Recommendation)
NACI concludes that there is fair evidence to recommend vaccination of adults 18 years of age and older with Supemtek. (Grade B Evidence)
Summary of evidence and rationale
- There is fair evidence that Supemtek is effective, safe, and has non-inferior immunogenicity to comparable vaccines, based on direct evidence in adults 18 years of age and older.
- There is some evidence that Supemtek may potentially offer improved protection against laboratory-confirmed influenza A infection compared to standard egg-based influenza vaccines. However, all the relative vaccine efficacy analyses were conducted using data only from the 2014-2015 influenza season in the US, which was influenza A(H3N2)-dominant, and in adults aged 50 years and older. Therefore, no firm conclusions can be drawn at this time, and NACI will continue to monitor this issue.
- A more robust, comprehensive and consistent body of evidence, including data on comorbidities, health status, and other potential confounders, is needed to evaluate the relative effectiveness of Supemtek compared to other injectable influenza vaccines.
- There is very limited peer-reviewed, published data on the use of Supemtek in pregnant individuals.
- NACI will continue to monitor the evidence related to RIV and will update this supplemental statement as needed and as data on Supemtek from several different influenza seasons accumulates.
An updated summary of the characteristics of influenza vaccines available in Canada for the 2022–2023 influenza season can be found in Appendix B. For complete prescribing information, readers should consult the product monograph available through Health Canada's Drug Product Database.
VI. Tables
| Serological assay | Definition | Threshold |
|---|---|---|
| GMTR | Ratio of GMT post-vaccination of licensed vaccine to GMT post-vaccination of new vaccine | Non-inferiority: The upper bound of the two-sided 95% CI on the ratio of the GMTs should not exceed 1.5. |
| Seroprotection | Proportion of subjects achieving an HI titre of ≥1:40 post-vaccination | Placebo-controlled: Lower limit of the two-sided 95% CI for the percent of subjects achieving seroprotection should meet or exceed 70% (for adults < 65 and children) or 60% (for adults ≥65) |
| Seroconversion | Proportion of subjects achieving an increase from ≤1:10 HI titre pre-vaccination to ≥1:40 post-vaccination or achieving at least four-fold rise in HI titres |
Non-inferiority: Upper limit of the two-sided 95% CI on the difference between the seroconversion rates (rate of licensed vaccine – rate of new vaccine) should not exceed 10 percentage points. Placebo-controlled: Lower limit of the two-sided 95% CI for the percent of subjects achieving seroprotection should meet or exceed 40% (for adults < 65 and children) or 30% (for adults ≥65) |
|
Abbreviations: CI: confidence interval, GMT: geometric mean titre, GMTR: geometric mean titre ratio, HI: hemagglutination inhibition |
||
| Strength of NACI recommendation | Grade of evidence |
|---|---|
| Based on factors not isolated to strength of evidence (e.g., public health need) | Based on assessment of the body of evidence |
|
Strong "should/should not be offered" Ø Known/Anticipated advantages outweigh known/anticipated disadvantages ("should"), OR Known/Anticipated disadvantages outweigh known/anticipated advantages ("should not") Ø Implication: A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present |
A - good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making | |
|
Discretionary "may be considered" Ø Known/Anticipated advantages closely balanced with known/anticipated disadvantages, OR uncertainty in the evidence of advantages and disadvantages exists Ø Implication: A discretionary recommendation may be considered for some populations/individuals in some circumstances. Alternative approaches may be reasonable |
A - good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making |
| Study details | ||||
|---|---|---|---|---|
| Study | Vaccine | Study design | Participants | Summary of key findings |
|
Dunkle L, Izikson R, Patriarca P, Goldenthal K, Muse D, Callahan J, Cox M, PSC12 Study Team. Efficacy of Recombinant Influenza Vaccine in Adults 50 Years of Age or Older. New England Journal of Medicine. 2017; 376(25):2427-2436. ClinicalTrials.gov NCT02285998 |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase III-IV
US
2014-2015 Funded by Protein Sciences Corporation |
Adults 50 years of age or older living independently without clinically significant acute illness, not receiving ongoing immunosuppressive therapy, and with no contraindications to trial vaccines 58.5% female Mean age: 63 RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur): n= 4,303 IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline): n= 4,301 |
The efficacy of RIV4 relative to IIV4-SD was calculated as 100×(1−RR), where RR is the relative risk of influenza attack rates in the two groups (RIV4 attack rate/IIV4-SD attack rate). rVE (95% CI) for RT-PCR–positive, protocol-defined influenza-like illness.
rVE (95% CI) for culture-positive, protocol-defined influenza-like illness.
|
|
Abbreviations: CI: confidence interval; IIV4-SD: standard-dose quadrivalent inactivated influenza vaccine; ILI: Influenza-like illness RCT: randomized controlled trial; RIV4: quadrivalent recombinant influenza vaccine; RR: risk ratio; RT-PCR: reverse transcription polymerase chain reaction; rVE: relative vaccine efficacy; SD: standard-dose; US: United States. |
||||
| Study details | ||||
|---|---|---|---|---|
| Study | Vaccine | Study design | Participants | Summary of key findings |
|
Dawood FS, Naleway AL, Flannery B, Levine MZ, Murthy K, Sambhara S, Gangappa S, Edwards L, Ball S, Grant L, Belongia E. Comparison of the Immunogenicity of Cell Culture-Based and Recombinant Quadrivalent Influenza Vaccines to Conventional Egg-Based Quadrivalent Influenza Vaccines Among Healthcare Personnel Aged 18–64 Years: A Randomized Open-Label Trial . Clinical Infectious Diseases. 2021. ClinicalTrials.gov Immunogenicity Trial of Egg- Versus Non-Egg-Based Influenza Vaccines Among HCP. |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase IV
US
2018-2019
Funded by the US Centres |
Adult healthcare personnel aged 18 to 64 years 82.4% female
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
IIV4-cc
IIV4 (Fluarix, GSK Biologics)
IIV4 (Fluzone Quadrivalent, Sanofi Pasteur) |
Ratio of geometric mean titers (95% CI) [IIV4-SD/RIV4]) at 1 month post-vaccination among RIV4 recipients compared to egg-based IIV4 recipients.
Proportion that achieved seroconversion (95% CI) 1 month post-vaccination in 18-64 year old age group (intention-to-treat population). RIV4:
IIV4 (Fluzone):
IIV4 (Fluarix):
IIV4-CC:
Proportion that achieved seroprotection (95% CI) 1 month post-vaccination in 18-64 year old age group. RIV4:
IIV4 (combined):
IIV4-CC:
|
|
Dunkle L, Izikson R, Patriarca P, Goldenthal K, Muse D, Callahan J, Cox M, PSC12 Study Team. Efficacy of Recombinant Influenza Vaccine in Adults 50 Years of Age or Older. New England Journal of Medicine. 2017; 376(25):2427-2436.
ClinicalTrials.gov NCT02285998 |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase III-IV
US
2014-2015 Funded by Protein Sciences Corporation |
Adults 50 years of age or older living independently without clinically significant acute illness, not receiving ongoing immunosuppressive therapy, and with no contraindications to trial vaccines 58.5% female Mean age: 63
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
50-64 age group:
> 65 age group:
IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline):
50-64 age group:
> 65 age group: Adults 50 years of age or older living independently without clinically significant acute illness, not receiving ongoing immunosuppressive therapy, and with no contraindications to trial vaccines 58.5% female Mean age: 63
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
50-64 age group: > 65 age group:
IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline):
50-64 age group:
> 65 age group: |
GMT ratio (95% CI) 28 days post-vaccination (IIV4/RIV4) in 50 year and older age group.
Proportion that achieved seroconversion (95% CI) 28 days post-vaccination:
50-64 age group:
> 65 age group:
Proportion that achieved seroprotection (95% CI) 28 days post-vaccination in 50 year and older age group. RIV4:
IIV4-SD:
|
|
Belongia E, Levine M, Olaiya O, Gross F, King J, Flannery B, McLean H. Clinical trial to assess immunogenicity of high-dose, adjuvanted, and recombinant influenza vaccines against cell-grown A(H3N2) viruses in adults 65 to 74 years, 2017–2018. Vaccine. 2020; 38(15):3121-3128.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Open label RCT
US
2017-2018 Funding by Centers for Disease Control and Prevention to the Marshfield Clinic Research Institute |
Adults 65 to 74 Years of Age 56% female Mean age: 70
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
IIV3-HD (Fluzone High-Dose, Sanofi Pasteur):
IIV3-Adj (Fluad, Seqirus): |
GMT (95% CI) 28±5 days post-vaccination in 65-74 year old age group. RIV4:
IIV3-HD:
IIV3-Adj:
Proportion that achieved seroconversion (95% CI) 28±5 days post-vaccination in 65-74 year old age group. RIV4:
IIV3-HD:
IIV3-Adj:
Proportion that achieved seroprotection (95% CI) 28±5 days post-vaccination in 65-74 year old age group. RIV4:
IIV3-HD:
IIV3-Adj:
|
|
Shinde V, Cai R, Plested J, Cho I, Fiske J, Pham X, Zhu M, Cloney-Clark S, Wang N, Zhou H, Zhou B, Patel N, Massare M, Fix A, Spindler M, Thomas D, Smith G, Fries L, Glenn G. Induction of Cross-Reactive Hemagglutination Inhibiting Antibody and Polyfunctional CD4+ T-Cell Responses by a Recombinant Matrix-M–Adjuvanted Hemagglutinin Nanoparticle Influenza Vaccine. Clinical Infectious Diseases. 2020.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase II, observer blind RCT
US
2018-2019 Funded by Novavax Inc. |
Clinically stable adults aged ≥65 years
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur): Mean age: 72.9 57.6% female
IIV3-HD (Fluzone High-Dose, Sanofi Pasteur); Mean age: 72.5 64.7% female |
GMT (95% CI) 28 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
GMT (95% CI) 56 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
GMT (95% CI) 182 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroconversion (95% CI) 28 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroconversion (95% CI) 56 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroconversion (95% CI) 182 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroprotection (95% CI) 28 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroprotection (95% CI) 56 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
Proportion that achieved seroprotection (95% CI) 182 days post-vaccination in 65 year and older age group. RIV4:
IIV3-HD:
1A/Switzerland/9715293/2013 (Drift Strain) 2A/Wisconsin/19/2017 (Drift Strain) |
|
Dunkle L, Izikson R, Patriarca P, Goldenthal K, Muse D, Cox M. Randomized Comparison of Immunogenicity and Safety of Quadrivalent Recombinant Versus Inactivated Influenza Vaccine in Healthy Adults 18–49 Years of Age. The Journal of Infectious Diseases. 2017;216(10):1219-1226.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase III
US 2014-2015 influenza season Funded by Protein Sciences Corporation |
Ambulatory, medically stable adults aged 18 to 49 years with no contraindications to either study vaccine. 64.7% female
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur): Mean age: 33.3
IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline): Mean age: 34.0 |
GMT (95% CI) ratio 28 days post-vaccination (IIV4/RIV4) in 18-49 year old age group:
Proportion that achieved seroconversion (95% CI) 28 days post-vaccination in 18-49 year old age group. RIV4:
IIV4-SD:
|
|
Wang W, Alvarado-Facundo E, Vassell R, Collins L, Colombo R, Ganesan A, Geaney C, Hrncir D, Lalani T, Markelz A, Maves R, McCle nathan B, Mende K, Richard S, Schofield C, Seshadri S, Spooner C, Utz G, Warkentien T, Levine M, Coles C, Burgess T, Eichelberger M, Weiss D. Comparison of A(H3N2) Neutralizing Antibody Responses Elicited by 2018–2019 Season Quadrivalent Influenza Vaccines Derived from Eggs, Cells, and Recombinant Hemagglutinin. Clinical Infectious Diseases. 2020.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Open label, phase IV
US 2018-2019 influenza season Funded by US Food and Drug Administration, Department of Defense, and Centers for Disease Control and Prevention |
Adult military healthcare beneficiaries aged 18 to 83 years 47.4 female
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) Mean age: 48.3
IIV4-SD (Fluarix), GlaxoSmithKline Biologicals): Mean age: 48.1
IIV4-cc (Flucelvax Quadrivalent, Seqirus, Inc.): Mean age: 45.7 |
GMT (%) 21-35 days post vaccination in 18-83 year old age group. RIV4:
IIV4-SD:
IIV4-cc:
Proportion (%) that achieved seroconversion 21-35 days post vaccination in 18-83 year old age group. RIV4:
IIV4-SD:
IIV4-cc:
|
|
Cowling B, Perera R, Valkenburg S, Leung N, Iuliano A, Tam, Wong J, Fang V, Li A, So H, Ip D, Azziz-Baumgartner E, Fry A, Levine M, Gangappa S, Sambhara S, Barr G, Skowronski D, Peiris J, Thompson M. Comparative Immunogenicity of Several Enhanced Influenza Vaccine Options for Older Adults: A Randomized, Controlled Trial. Clinical Infectious Diseases. 2020;71(7):1704-1714. ClinicalTrials.gov Immunogenicity of Alternative Annual Influenza Vaccination Strategies in Older Adults in Hong Kong (PIVOT) |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase IV Hong Kong 2017-2018 influenza season
Funded by the Centres for Disease |
Community-dwelling older adults who were 65–82 years of age, residing in Hong Kong, and had not already received northern hemisphere 2017–2018 formulation of influenza vaccination. 60.6% female Mean age: n/a
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
IIV4-SD (FluQadri, Sanofi Pasteur):
IIV3-Adj (Fluad, Sequiris):
IIV3-HD (Fluzone High-Dose, Sanofi Pasteur): |
GMT (95% CI) 30 days post-vaccination in 65-82 year old age group. RIV4:
IIV4-SD:
IIV3-Adj:
IIV3-HD:
Proportion that achieved seroconversion (95% CI) 30 days post vaccination in 65-82 year old age group. RIV4:
IIV4-SD:
IIV3-Adj:
IIV3-HD:
|
|
Gouma S, Zost S, Parkhouse K, Branche A, Topham D, Cobey S, Hensley S. Comparison of Human H3N2 Antibody Responses Elicited by Egg-Based, Cell-Based, and Recombinant Protein–Based Influenza Vaccines During the 2017–2018 Season. Clinical Infectious Diseases. 2020;71(6):1447-1453.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase IV
US Funded by National Institute of Allergy and Infectious Diseases at the National Institutes of Health |
Healthy adults aged 18 to 49 years 57.6% female Mean age: n/a
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur)
IIV3-HD (Fluzone High-Dose; Sanofi Pasteur):
IIV4-cc (Flucelvax Quadrivalent, Seqirus, Inc.):
IIV3- HD (Fluzone High-Dose; Sanofi Pasteur): |
GMT (95% CI) 28 days post vaccination in 18-49 year old age group. RIV4:
IIV4-cc:
IIV4-SD:
IIV3-HD:
Proportion (%) that achieved seroconversion 28 days post vaccination in 18-49 year old age group. RIV4:
IIV3-HD:
1A/Hong Kong/4801/2014 2A/Pennsylvania/49/2018 3A/Hong Kong/4801/2014 egg-adapted 4A/Singapore/GP2050/2015 cell/adapted |
|
Abbreviations: CI: confidence interval; GMT: geometric mean titre; IIV3-Adj: adjuvanted trivalent inactivated influenza vaccine; IIV3-HD: high-dose trivalent inactivated influenza vaccine; IIV4-cc: cell-culture based quadrivalent inactivated influenza vaccine; IIV4-SD: standard-dose quadrivalent inactivated influenza vaccine; N/A: not applicable; RCT: randomized controlled trial; RIV4: quadrivalent recombinant influenza vaccine; US: United States. |
||||
| Study details | ||||
|---|---|---|---|---|
| Study | Vaccine | Study design | Participants | Summary of key findings |
|
Dunkle L, Izikson R, Patriarca P, Goldenthal K, Muse D, Callahan J, Cox M, PSC12 Study Team. Efficacy of Recombinant Influenza Vaccine in Adults 50 Years of Age or Older. New England Journal of Medicine. 2017; 376(25):2427-2436.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase III-IV
US 2014-2015 influenza season Funded by Protein Sciences Corporation |
Adults 50 years of age or older living independently without clinically significant acute illness, not receiving ongoing immunosuppressive therapy, and with no contraindications to trial vaccines 58.5% female Mean age: 63
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline): |
Proportion (%) of reported serious adverse events according to System Organ Class1 in adults 50 years of age and older reporting within 182 days (6 months) post-vaccination: Any serious AE2
Infections and infestations
Cardiac disorders
Musculoskeletal and connective tissue disorders
Nervous system disorders
Gastrointestinal disorders
Neoplasms benign, malignant and unspecified (including cysts and polyps)
General disorders and administration site conditions
Respiratory, thoracic and mediastinal disorders
Injury, poisoning and procedural complications
Metabolism and nutrition disorders
Vascular disorders
Surgical and medical procedure
Renal and urinary disorders
Hepatobiliary disorders
Reproductive system and breast disorders
Blood and lymphatic system disorders
Investigations
Psychiatric disorders
Ear and labyrinth disorders
Skin and subcutaneous tissue disorders
1Events coded according to MedDRA, Version 17 2Subjects may have reported more than one serious AE term |
|
Dunkle L, Izikson R, Patriarca P, Goldenthal K, Muse D, Cox M. Randomized Comparison of Immunogenicity and Safety of Quadrivalent Recombinant Versus Inactivated Influenza Vaccine in Healthy Adults 18–49 Years of Age. The Journal of Infectious Diseases. 2017;216(10):1219-1226.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase III
US 2014-2015 influenza season Funded by Protein Sciences Corporation |
2Ambulatory, medically stable adults aged 18-49 years with no contraindications to either study vaccine. 64.7% female
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
Systemic AEs population, Mean age: 33.3
IIV4-SD (Fluarix Quadrivalent, GlaxoSmithKline): Mean age: 34.0 |
Proportion (%) of serious AEs in adults 18-49 years of age, within 182 days (6 months) post-vaccination: Any serious AE
Myocardial infarction
Gastrointestinal haemorrhage
Pancreatitis
Small intestinal obstruction
Cholecystitis
Appendicitis
Periumbilical abscess
Road traffic accident
Neck pain
Metabolic encephalopathy
Abortion spontaneous
Ovarian cyst
Arm amputation
Proportion (%) of reported systemic AEs in adults 18-49 years of age, within 7 days post-vaccination. Any systemic reaction1:
Fatigue:
Shivering/chills:
Joint pain:
Muscle pain:
Headache:
Nausea:
Fever2, 3:
1 The grading system systemic adverse events was as follows: Grade 1, mild; Grade 2, moderate; Grade 3: severe; Grade 4: life threatening. 2 For fever, the denominator were 990 and 327 for the RIV4 and IIV4-SD groups, respectively. 3 The grading system for fever was as follows: Grade 1, 38–38.4°C (100.4–101.1°F); Grade 2, > 38.4–38.9°C (101.2–102.0°F); Grade 3, > 38.9–40°C (102.1–104°F); Grade 4, > 40°C (> 104°F). |
|
Cowling B, Perera R, Valkenburg S, Leung N, Iuliano A, Tam, Wong J, Fang V, Li A, So H, Ip D, Azziz-Baumgartner E, Fry A, Levine M, Gangappa S, Sambhara S, Barr I, Skowronski D, Peiris J, Thompson M. Comparative Immunogenicity of Several Enhanced Influenza Vaccine Options for Older Adults: A Randomized, Controlled Trial. Clinical Infectious Diseases. 2020;71(7):1704-1714.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase IV Hong Kong 2017-2018 influenza season
Funded by the Centers for Disease |
Community-dwelling older adults who were 65-82 years of age, residing in Hong Kong, and had not already received northern hemisphere 2017–2018 formulation of influenza vaccination. 60.8% female Mean age: n/a
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
IIV4-SD (FluQadri, Sanofi Pasteur):
IIV3-Adj (Fluad, Sequiris):
IIV3-HD (Fluzone High-Dose, Sanofi Pasteur): |
Proportion (%) of reported hospitalizations in adults 65-82 years of age reporting throughout the study. No other serious adverse event was identified by the authors and hospitalizations were deemed unrelated to the study vaccines. Overall hospitalizations:
Time since vaccination, < 1 month:
Time since vaccination, 1-3 months:
Time since vaccination, 4-6 months:
Time since vaccination, > 6 months:
|
|
Cowling B, Thompson M, Ng T, Fang V, Perera R, Leung N, Chen Y, So H, Ip D, Iuliano A. Comparative Reactogenicity of Enhanced Influenza Vaccines in Older Adults. The Journal of Infectious Diseases. 2020;222(8):1383-1391.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Hong Kong 2017-2018 influenza season
Funded by the Centres for Disease |
65–82 years of age, residing in Hong Kong, and had not already received northern hemisphere 2017–2018 formulation of influenza vaccination. 60.8% female Mean age: n/a
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur):
3-4 days population,
7-9 days population,
14-16 days population, IIV4-SD (FluQuadri, Sanofi Pasteur):
1 day population, IIV3-Adj (Fluad, Sequiris):
1 day population, IIV3-HD (Fluzone High-Dose, Sanofi Pasteur):
1 day population, |
Proportion (%) of reported systemic AEs1, 2 in adults 65-82 years of age, within 1 day post-vaccination: Fatigue (mild)
Feverishness (mild)
Muscle pain (mild)
Nausea (mild)
Others (mild)
Fatigue (moderate)
Feverishness (moderate)
Muscle pain (moderate)
Nausea (moderate)
Others (moderate)
Fatigue (severe)
Feverishness (severe)
Muscle pain (severe)
Nausea (severe)
Others (severe)
Proportion (%) of reported systemic AEs1, 2 in adults 65-82 years of age, within 3-4 days post-vaccination: Fatigue (mild)
Feverishness (mild)
Muscle pain (mild)
Nausea (mild)
Others (mild)
Fatigue (moderate)
Feverishness (moderate)
Muscle pain (moderate)
Nausea (moderate)
Others (moderate)
Fatigue (severe)
Feverishness (severe)
Muscle pain (severe)
Nausea (severe)
Others (severe)
Proportion (%) of systemic AEs1, 2 in adults 65-82 years of age, 7-9 days post-vaccination: Fatigue (mild)
Feverishness (mild)
Muscle pain (mild)
Nausea (mild)
Others (mild)
Fatigue (moderate)
Feverishness (moderate)
Muscle pain (moderate)
Nausea (moderate)
Others (moderate)
Fatigue (severe)
Feverishness (severe)
Muscle pain (severe)
Nausea (severe)
Others (severe)
Proportion (%) of systemic AEs1, 2 in adults 65-82 years of age, 14-16 days post-vaccination: Fatigue (mild)
Feverishness (mild)
Muscle pain (mild)
Nausea (mild)
Others (mild)
Fatigue (moderate)
Feverishness (moderate)
Muscle pain (moderate)
Nausea (moderate)
Others (moderate)
Fatigue (severe)
Feverishness (severe)
Muscle pain (severe)
Nausea (severe)
Others (severe)
1Mild: symptom is easily tolerated and does not interfere with any usual activities; moderate: symptom interferes with usual activities; severe: participant cannot carry out usual activities. 2Other symptoms included sore throat, headache, runny nose, cough, dry eyes and upset stomach |
|
Shinde V, Cai R, Plested J, Cho I, Fiske J, Pham X, Zhu M, Cloney-Clark S, Wang N, Zhou H, Zhou B, Patel N, Massare M, Fix A, Spindler M, Thomas D, Smith G, Fries L, Glenn G. Induction of Cross-Reactive Hemagglutination Inhibiting Antibody and Polyfunctional CD4+ T-Cell Responses by a Recombinant Matrix-M–Adjuvanted Hemagglutinin Nanoparticle Influenza Vaccine. Clinical Infectious Diseases. 2020.
ClinicalTrials.gov |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur) |
Phase II, observer blind RCT
US 2018-2019 influenza season Funded by Novavax Inc. |
Clinically stable adults aged ≥65 years
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur): Mean age: 72.9 57.6% female
IIV3-HD (Fluzone High-Dose, Sanofi Pasteur); Mean age: 72.5 64.7% female |
Proportion of serious1 AEs (95% CI) in adults 65 years of age and over, 181 days post-vaccination: Subjects with at least one serious adverse event
Infections and infestations
Nervous system disorders
Cardiac disorders
Gastrointestinal disorders
Injury, poisoning, and procedural complications
Metabolism and nutrition disorders
Neoplasms benign, malignant and unspecified (including cysts and polyps)
Respiratory, thoracic, and mediastinal disorders
General disorders and administration site conditions
Musculoskeletal and connective tissue disorders
Blood and lymphatic system disorders
Hepatobiliary disorders
Reproductive system and breast disorders
Skin and subcutaneous tissue disorders
Vascular disorders
1MedDRA System Organ Class and Preferred Term Proportion of systemic AEs (95 % CI):in adults 65 years of age and over, 6 days post-vaccination: All systemic AEs
Chills
Fatigue
Headache
Joint pain
Muscle pain
Oral temperature
Diarrhea
Nausea
Vomiting
Chest tightness
Cough
Difficulty breathing
Difficulty swallowing
Eye redness
Eyelid swelling
Facial swelling
Hoarseness
Sore throat
Wheezing
|
| Woo E, Moro P. Postmarketing safety surveillance of quadrivalent recombinant influenza vaccine: Reports to the vaccine adverse event reporting system. Vaccine. 2021;39(13):1812-1817. |
RIV4 (Supemtek/ Flublok Quadrivalent, Sanofi Pasteur)
US 2017-2018, 2018-2019, 2019-2020 influenza seasons |
Post-marketing safety surveillance of cases identified through VAERS |
Persons vaccinated with RIV4 during July 1, 2017 through June 30, 2020 Mean age: 43.7 69.7% female
Reports on serious adverse events: |
Proportion (%) of serious AEs reported after RIV4 vaccination: Neurological
Guillain-Barré syndrome
Seizure
Exacerbation of pre-existing multiple sclerosis
Optic papillitis
Sensorineural hearing loss
Immunological
Anaphylaxis / allergic reaction
Serum sickness-type reaction, allergic reaction to influenza vaccine
Stevens Johnson syndrome after lisinopril and atorvastatin
Local reaction
Injection site reaction or local cellulitis
Respiratory
Exacerbation or complications of pre-existing pulmonary conditions (chronic obstructive pulmonary disease asthma, or lung transplantation)
Cardiac or cardiovascular
Bradycardia
Takotsubo cardiomyopathy, cardiogenic shock, and pulseless electrical activity
Cardiomegaly (544 g) and hypertension
Viral-type symptoms
Flu-like symptoms, fatigue, chills, or myalgia
Other
Mesenteric panniculitis
Proportion (%) of systemic adverse events identified from non-serious reports after RIV4 vaccination: Pyrexia
Headache
Rash
Dizziness
Fatigue
Chills
Nausea
|
|
Abbreviations: AE: Adverse Event; CI: confidence interval; IIV3-Adj: adjuvanted trivalent inactivated influenza vaccine; IIV3-HD: high-dose trivalent inactivated influenza vaccine; IIV4-SD: standard-dose quadrivalent inactivated influenza vaccine; MedDRA: Medical Dictionary for Regulatory Activities; n/a: not applicable; RCT: randomized controlled trial; RIV: recombinant influenza vaccine; RIV4: quadrivalent recombinant influenza vaccine; SAE: Serious Adverse Event; SD: standard-dose; US: United States; VAERS: Vaccine Adverse Event Reporting System. |
||||
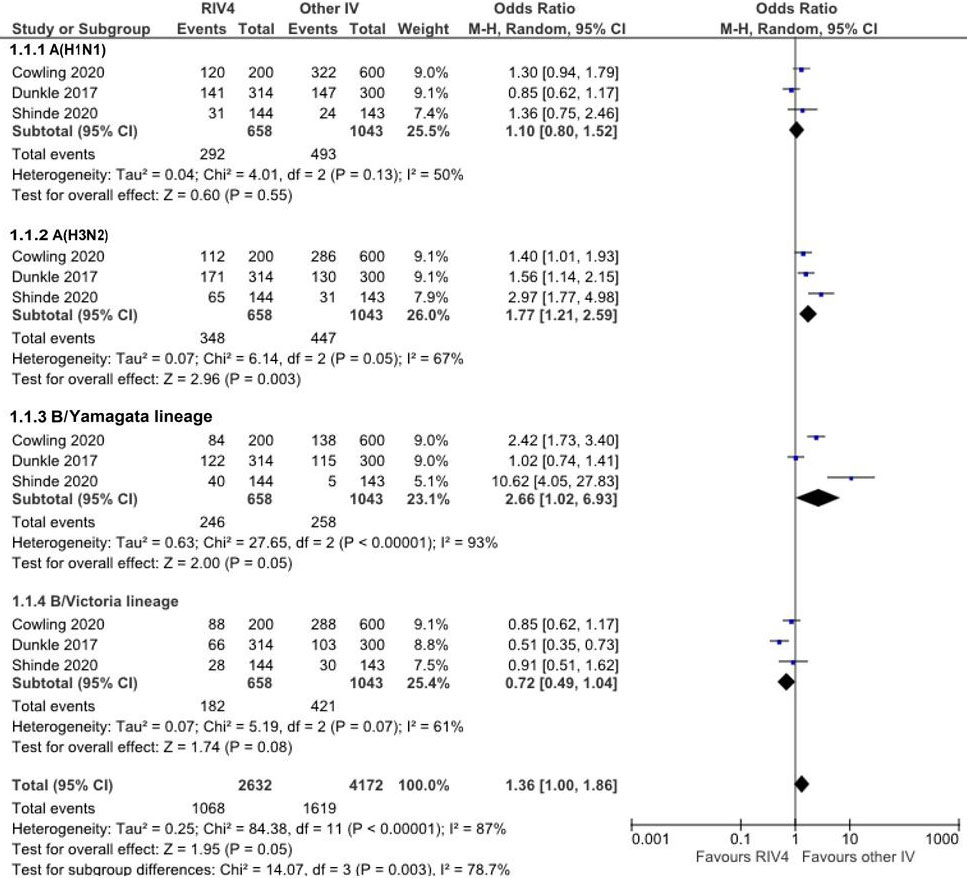
Figure 1 - Text description
Figure 1 depicts a forest plot showing the results of a random-effects meta-analysis reporting the odds of seroconversion rate following immunization of quadrivalent recombinant influenza vaccine (RIV4) compared to other seasonal influenza vaccine (IV) in recipients aged 50 years and older. The leftmost column shows the identities of the three included studies by influenza strain. The included studies are represented by the last name of the first author and the year of publication. Next, to the right, data regarding the number of patients having the outcome of interest (events), the sample size of the intervention (RIV4) and comparison group (other IV) are presented. The x-axis representing OR estimates and 95% confidence interval (CI) ranges from 0.001 to 1000. The vertical line of "no effect" appears at the value of 1 and separates outcomes that favor RIV4 (on the left) and other IV (on the right). Each horizontal line on the forest plot represents an individual study with the result plotted as a box and the 95% CI of the result displayed as the line. The size of the box surrounding each estimate represents the relative weight of that study in producing the pooled result. The black diamonds show the pooled results when the individual studies are combined together and averaged. The horizontal points of the diamonds are the limits of the 95% CI of each combined point estimate.
The following information is depicted in this figure:
Effect estimates from the single studies:
| Author | Influenza Strain | RIV4 Events | RIV4 Sample Size | Other IV Events | Other IV Sample Size | Weight | OR [95% CI] |
|---|---|---|---|---|---|---|---|
| A/H1N1 | |||||||
| Cowling 2020 | A/H1N1 | 120 | 200 | 322 | 600 | 9.0% | 1.30 [0.94, 1.79] |
| Dunkle 2017 | A/H1N1 | 141 | 314 | 147 | 300 | 9.1% | 0.85 [0.62, 1.17] |
| Shinde 2020 | A/H1N1 | 31 | 144 | 24 | 143 | 7.4% | 1.36 [0.75, 2.46] |
| A/H3N2 | |||||||
| Cowling 2020 | A/H3N2 | 112 | 200 | 286 | 600 | 9.1% | 1.40 [1.01, 1.93] |
| Dunkle 2017 | A/H3N2 | 171 | 314 | 130 | 300 | 9.1% | 1.56 [1.14, 2.15] |
| Shinde 2020 | A/H3N2 | 65 | 144 | 31 | 143 | 7.9% | 2.97 [1.77, 4.98] |
| B/Yamagata lineage | |||||||
| Cowling 2020 | B/Yamagata lineage | 84 | 200 | 138 | 600 | 9.0% | 2.42 [1.73, 3.40] |
| Dunkle 2017 | B/Yamagata lineage | 122 | 314 | 115 | 300 | 9.0% | 1.02 [0.74, 1.41] |
| Shinde 2020 | B/Yamagata lineage | 40 | 144 | 5 | 143 | 5.1% | 10.62 [4.05, 27.83] |
| B/Victoria lineage | |||||||
| Cowling 2020 | B/Victoria lineage | 88 | 200 | 288 | 600 | 9.1% | 0.85 [0.62, 1.17] |
| Dunkle 2017 | B/Victoria lineage | 66 | 314 | 103 | 300 | 8.8% | 0.51 [0.35, 0.73] |
| Shinde 2020 | B/Victoria lineage | 28 | 144 | 30 | 143 | 7.5% | 0.91 [0.51, 1.62] |
Pooled results:
| Statistical model | Influenza Strain | RIV4 total events | RIV4 Sample Size | Other IV total Events | Other IV Sample Size | Weight | Pooled OR [95% CI] |
Heterogeneity: (p value), IFootnote 2 |
Test for overall effect: Z (p value) |
Test for subgroup differences Chi Footnote 2, df (p value), IFootnote 2 |
|---|---|---|---|---|---|---|---|---|---|---|
| Random effect model | A/H1N1 | 292 | 658 | 493 | 1043 | 25.5% | 1.10 [0.80, 1.52] | 0.04; 4.01, 2 (p= 0.13); 50% | 0.60 (p= 0.55) | - |
| Random effect model | A/H3N2 | 348 | 658 | 447 | 1043 | 26.0% | 1.77 [1.21, 2.59] | 0.07; 6.14; 2 (p= 0.05); 67% | 2.96 (0.003) | - |
| Random effect model | B/Yamagata lineage | 246 | 658 | 258 | 1043 | 23.1% | 2.66 [1.02, 6.93] | 0.63; 27.65; 2 (p < 0.00001); 93% | 2.00 (p= 0.05) | - |
| Random effect model | B/Victoria lineage | 182 | 658 | 421 | 1043 | 25.4% | 0.72 [0.49, 1.04] | 0.07; 5.19; 2 (p=0.07); 61% | 1.74 (p= 0.08) | - |
| Random effect model | All studies | 1068 | 2632 | 1619 | 4172 | 100.0% | 1.36 [1.00, 1.86] | 0.25; 84.38; 11 (p < 0.00001, 87%) | 1.95 (p = 0.05) | 14.07; 3 (P = 0.003); 78.7% |
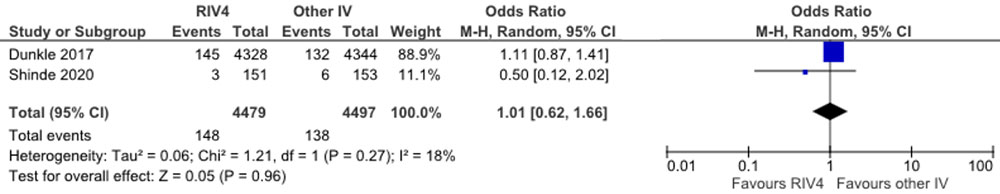
Figure 2 - Text description
Figure 2 depicts a forest plot showing the results of a random-effects meta-analysis reporting the odds of experiencing a serious adverse event within 180 days of vaccination following immunization of quadrivalent recombinant influenza vaccine (RIV4) compared to other seasonal influenza vaccine (IV) in recipients aged 50 years and older. The leftmost column shows the identities of the two included studies. The included studies are represented by the last name of the first author and the year of publication. Next, to the right, data regarding the number of patients having the outcome of interest (events) and the sample size of the intervention (RIV4) and comparison group (other IV) are presented. The next two columns include the same information in numerical format that is contained in the diagram. The penultimate column to the right contains the year of the study publication. The diagram located in the rightmost column visually displaying the results. The x-axis representing OR estimates and 95% confidence interval (CI) ranges from 0.01 to 100. The vertical line of "no effect" appears at the value of 1 and separates outcomes that favor RIV4 (on the left) and other IV (on the right). Each horizontal line on the forest plot represents an individual study with the result plotted as a box and the 95% CI of the result displayed as the line. The size of the box surrounding each estimate represents the relative weight of that study in producing the pooled result. The black diamonds show the pooled results when the individual studies are combined together and averaged. The horizontal points of the diamonds are the limits of the 95% CI of each combined point estimate.
The following information is depicted in this figure:
Effect estimates from the single studies:
| Author | RIV4 Events | RIV4 Sample Size | Other IV Events | Other IV Sample Size | Weight | OR [95% CI] |
|---|---|---|---|---|---|---|
| Dunkle 2017 | 145 | 4328 | 132 | 4344 | 88.9% | 1.11 [0.87, 1.41] |
| Shinde 2020 | 3 | 151 | 6 | 153 | 11.1% | 0.50 [0.12, 2.02] |
Pooled results:
| Statistical model | RIV4 total events | RIV4 Sample Size | Other IV total Events | Other IV Sample Size | Weight | Pooled OR [95% CI] |
Heterogeneity: (p value), IFootnote 2 |
Test for overall effect: Z (p value) |
|---|---|---|---|---|---|---|---|---|
| Random effect model | 148 | 4479 | 138 | 4497 | 100% | 1.01 [0.62, 1.66] | 0.06; 1.21; 1 (P = 0.27); 18% | 0.05 (p= 0.96) |
VII. List of abbreviations
Abbreviation Term
- AE
- Adverse event
- CI
- Confidence interval
- EEFA
- Ethics, equity, feasibility, and acceptability
- FDA
- Food and Drug Administration (United States)
- GMT
- Geometric mean titre
- GMTR
- Geometric mean titre ratio
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluation
- HA
- Hemagglutinin
- HI
- Hemagglutination inhibition
- IIV
- Inactivated influenza vaccine
- IIV3
- Trivalent inactivated influenza vaccine
- IIV3-Adj
- Adjuvanted trivalent inactivated influenza vaccine
- IIV3-cc
- Cell-culture based trivalent inactivated influenza vaccine
- IIV3-HD
- High-dose trivalent inactivated influenza vaccine
- IIV3-SD
- Standard-dose trivalent inactivated influenza vaccine
- IIV4
- Quadrivalent inactivated influenza vaccine
- IIV4-cc
- Cell-culture based quadrivalent inactivated influenza vaccine
- IIV4-SD
- Standard-dose quadrivalent inactivated influenza vaccine
- ILI
- Influenza-like illness
- IM
- Intramuscular
- IWG
- Influenza Working Group
- LCI
- Laboratory-confirmed influenza
- NA
- Neuraminidase
- NACI
- National Advisory Committee on Immunization
- OR
- Odds ratio
- PHAC
- Public Health Agency of Canada
- RCT
- Randomized controlled trial
- RIV
- Recombinant influenza vaccine
- RIV3
- Trivalent recombinant influenza vaccine
- RIV4
- Quadrivalent recombinant influenza vaccine
- RR
- Risk ratio
- RT-PCR
- Reverse transcription polymerase chain reaction
- rVE
- Relative vaccine efficacy
- SAE
- Serious Adverse Event
- US
- United States
- VAERS
- Vaccine Adverse Event Reporting System (US)
VIII. Acknowledgements
This supplemental statement was prepared by: A Gil, A Sinilaite, M Xi, R Harrison and J Papenburg on behalf of NACI.
NACI gratefully acknowledges the contribution of: P Doyon-Plourde, R Stirling, C Tremblay, M Tunis and K Young.
Influenza Working Group
Members: J Papenburg (Chair), P De Wals, D Fell, I Gemmill, R Harrison, J Langley, A McGeer and D Moore.
Former members: N Dayneka, K Klein, D Kumar, J McElhaney and S Smith.
Liaison representatives: L Grohskopf (Centers for Disease Control and Prevention [CDC],
United States).
Ex-officio representatives: C Bancej (Centre for Immunization and Respiratory Infectious
Diseases [CIRID], PHAC), J Reiter (First Nations and Inuit Health Branch [FNIHB], Indigenous Services Canada [ISC]), B Warshawsky (Vice President's Office, Infectious Disease Prevention and Control Branch [IDPCB]), and J Xiong (Biologics and Genetic Therapies Directorate [BGTD], Health Canada [HC]).
NACI
Members: S Deeks (Chair), R Harrison (Vice-Chair), M Andrew, J Bettinger, N Brousseau, H Decaluwe, P De Wals, E Dubé, V Dubey, K Hildebrand, K Klein, J Papenburg, A Pham-Huy, B Sander, S Smith, and S Wilson.
Former NACI members: N Dayneka, C Rotstein, C Quach-Thanh.
Liaison representatives: L Bill / M Nowgesic (Canadian Indigenous Nurses Association), LM Bucci (Canadian Public Health Association), E Castillo (Society of Obstetricians and Gynaecologists of Canada), A Cohn (Centers for Disease Control and Prevention, United States), L Dupuis (Canadian Nurses Association), D Fell (Canadian Association for Immunization Research and Evaluation), S Funnell (Indigenous Physicians Association of Canada), J Hu / N Ivers (College of Family Physicians of Canada), M Lavoie (Council of Chief Medical Officers of Health), D Moore (Canadian Paediatric Society), M Naus (Canadian Immunization Committee), A Ung (Canadian Pharmacists Association).
Ex-officio representatives: V Beswick-Escanlar (National Defence and the Canadian Armed Forces), E Henry (Centre for Immunization and Respiratory Infectious Diseases (CIRID), PHAC), M Lacroix (Public Health Ethics Consultative Group, PHAC), C Lourenco / S Hardy (Biologic and Radiopharmaceutical Drugs Directorate, Health Canada), D MacDonald (COVID-19 Epidemiology and Surveillance, PHAC), S Ogunnaike-Cooke (CIRID, PHAC), K Robinson / D Danoff (Marketed Health Products Directorate, HC), G Poliquin (National Microbiology Laboratory, PHAC), and T Wong (First Nations and Inuit Health Branch, Indigenous Services Canada).
IX. Appendix A: Prisma flow diagram
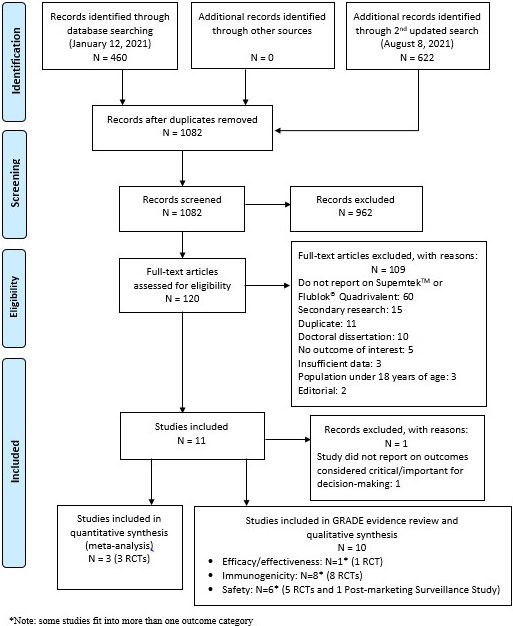
Prisma flow diagram - Text description
Appendix A: PRISMA Flow Diagram
The PRISMA flow diagram describes the process by which articles were selected for the literature review. The process is broken down into four stages: Identification, Screening, Eligibility and Included.
Stage 1: Identification
- 460 records were identified through the January 12, 2021 database search, 0 records were identified through additional sources and 622 additional records were identified through the August 8, 2021 database search.
- 1082 records remained after duplicates were removed.
Stage 2: Screening
- 1082 records were then screened.
- Of these 1082 records, 962 records were excluded.
Stage 3: Eligibility
- 120 full-text articles were assessed for eligibility.
- Of these 120 full-text articles, 109 were excluded. The exclusion breakdown is as follows: 60 did not report on SupemtekTM or Flublok®Quadrivalent, 15 were secondary research, 11 were duplicates, 10 were doctoral dissertations, 5 did not report on outcomes of interest, 3 had insufficient data, 3 had a study population under 18 years of age and 2 were editorials.
Stage 4: Included
- 11 articles were included.
- Of these 11 articles, 1 was excluded as the study did not report on outcomes considered critical or important for decision making.
- Of these 11 articles, 3 RCTs were included in the quantitative synthesis (meta-analysis).
- Of these 11 articles, 10 were included in the GRADE evidence review and qualitative synthesis under the following outcome categories: 1 RCT reported on efficacy/effectiveness, 8 RCTs reported on immunogenicity and 6 studies (5 RCTs and 1 post-market surveillance study) reported on safety. Some studies fit into more than out outcome category.
X. Appendix B: Characteristics of influenza vaccines available for use in Canada, 2022–2023Footnote a
| Product name (manufacturer) | Vaccine characteristic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vaccine type | Route of administration | Authorized ages for use | Antigen content for each vaccine strain | Adjuvant | Formats available | Post-puncture shelf life for multi-dose vials | Thimerosal | Antibiotics (traces) | Production medium | |
| Quadrivalent | ||||||||||
|
Flulaval® Tetra |
IIV4-SD (split virus) |
IM | 6 months and older |
15 µg HA |
None | 5 mL multi-dose vial | 28 days |
Yes |
None | Egg (Avian) |
|
Fluzone® Quadrivalent |
IIV4-SD |
IM | 6 months and older |
15 µg HA |
None |
5 mL multi-dose vial Single-dose pre-filled syringe without attached needle |
Up to expiry date indicated on vial label |
Yes |
None | Egg (Avian) |
|
Afluria® Tetra |
IIV4-SD |
IM | 5 years and older |
15 µg HA |
None |
5 mL multi-dose vial Single dose pre-filled syringe without attached needle |
Up to expiry date indicated on vial label |
Yes |
Neomycin and polymyxin B | Egg (Avian) |
|
Influvac® Tetra |
IIV4-SD |
IM or deep subcutaneous injection | 6 months and older |
15 µg HA |
None | Single dose pre-filled syringe with or without attached needle | Not applicable | No | Gentamicin or neomycin and polymyxin BFootnote b | Egg (Avian) |
| Flucelvax® Quad (Seqirus) |
IIV4-cc |
IM | 6 months and older |
15 µg HA |
None |
5 mL multi-dose vial Single dose pre-filled syringe without attached needle |
28 days |
Yes |
None | Cell culture (Mammalian) |
|
Fluzone® High-Dose Quadrivalent |
IIV4-HD |
IM | 65 years and older |
60 µg HA |
None | Single dose pre-filled syringe without attached needle | Not applicable | No | None | Egg (Avian) |
|
Supemtek™ |
RIV4 |
IM | 18 years and older |
45 µg HA |
None | Single dose pre-filled syringe without attached needle | Not applicable | No | None | Recombinant protein (Baculovirus Expression Vector System) |
|
FluMist® |
LAIV4 |
Intranasal | 2–59 years |
106.5-7.5 FFU of live attenuated reassortants |
None | Single use pre-filled glass sprayer | Not applicable | No | Gentamicin | Egg (Avian) |
| Trivalent | ||||||||||
|
Fluad Pediatric® |
IIV3-Adj |
IM |
Pediatric: Adult: |
Pediatric: Adult: |
MF59 | Single dose pre-filled syringe without a needle | Not applicable | No | Kanamycin and neomycin | Egg (Avian) |
|
Abbreviations: FFU: fluorescent focus units; HA: hemagglutinin; IIV3-Adj: adjuvanted egg-based trivalent inactivated influenza vaccine; IIV4-cc: standard-dose cell culture-based quadrivalent inactivated influenza vaccine; IIV4-SD: standard-dose egg-based quadrivalent inactivated influenza vaccine; IM: intramuscular; LAIV4: quadrivalent live attenuated influenza vaccine; NA: neuraminidase; RIV4: quadrivalent recombinant influenza vaccine.
|
||||||||||
XI. References
- Footnote 1
-
Schanzer DL, McGeer A, Morris K. Statistical estimates of respiratory admissions attributable to seasonal and pandemic influenza for Canada. Influenza Other Respir Viruses. 2013 Sep;7(5):799–808.
- Footnote 2
-
Schanzer DL, Sevenhuysen C, Winchester B, Mersereau T. Estimating Influenza Deaths in Canada, 1992–2009. Nishiura H, editor. PLoS ONE. 2013 Nov 27;8(11):e80481.
- Footnote 3
-
Government of Canada [Internet]. FluWatch annual report: 2018-19 influenza season. 2020. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/fluwatch/2018-2019/annual-report.html
- Footnote 4
-
Government of Canada [Internet]. FluWatch annual report: 2019-2020 influenza season. 2021. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/fluwatch/2019-2020/annual-report.html
- Footnote 5
-
Nwosu A, Lee L, Schmidt K, Buckrell S, Sevenhuysen C, Bancej C. National Influenza Annual Report, Canada, 2020–2021, in the global context. Can Commun Dis Rep. 2021 Oct 14;47(10):405–13.
- Footnote 6
-
Groves HE, Papenburg J, Mehta K, Bettinger JA, Sadarangani M, Halperin SA, et al. The effect of the COVID-19 pandemic on influenza-related hospitalization, intensive care admission and mortality in children in Canada: A population-based study. Lancet Reg Health - Am. 2022 Mar;7:100132.
- Footnote 7
-
He D, Lui R, Wang L, Tse CK, Yang L, Stone L. Global Spatio-temporal Patterns of Influenza in the Post-pandemic Era. Sci Rep. 2015 Sep;5(1):11013.
- Footnote 8
-
Tang JW, Bialasiewicz S, Dwyer DE, Dilcher M, Tellier R, Taylor J, et al. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID‐19 pandemic. J Med Virol. 2021 Jul;93(7):4099–101.
- Footnote 9
-
Sanofi Pasteur Limited [Internet]. Product monograph: Supemtek: Quadrivalent Recombinant Influenza Vaccine. 2021. Available from: https://pdf.hres.ca/dpd_pm/00059645.PDF
- Footnote 10
-
Sell TK, Gastfriend D, Watson M, Watson C, Richardson L, Cicero A, et al. Building the global vaccine manufacturing capacity needed to respond to pandemics. Vaccine. 2021 Mar;39(12):1667–9.
- Footnote 11
-
The Centers for Disease Control and Prevention (CDC) (US) [Internet]. Seasonal Influenza (Flu): Recombinant Flu Vaccines. Available from: https://www.cdc.gov/flu/prevent/qa_flublok-vaccine.htm
- Footnote 12
-
Barr IG, Donis RO, Katz JM, McCauley JW, Odagiri T, Trusheim H, et al. Cell culture-derived influenza vaccines in the severe 2017–2018 epidemic season: a step towards improved influenza vaccine effectiveness. Npj Vaccines. 2018 Dec;3(1):44.
- Footnote 13
-
Government of Canada [Internet]. Canadian Immunization Guide: Part 4 - Active Vaccines. 2021. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines.html
- Footnote 14
-
Arunachalam AB, Post P, Rudin D. Unique features of a recombinant haemagglutinin influenza vaccine that influence vaccine performance. Npj Vaccines. 2021 Dec;6(1):144.
- Footnote 15
-
Centers for Disease Control and Prevention [Internet]. Archived CDC Vaccine Price List as of February 2, 2017. Available from: https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/2017/2017-02-02.html
- Footnote 16
-
Harding AT, Heaton NS. Efforts to Improve the Seasonal Influenza Vaccine. Vaccines. 2018 Mar 30;6(2):E19.
- Footnote 17
-
Dunkle LM, Izikson R, Patriarca P, Goldenthal KL, Muse D, Callahan J, et al. Efficacy of Recombinant Influenza Vaccine in Adults 50 Years of Age or Older. N Engl J Med. 2017 Jun 22;376(25):2427–36.
- Footnote 18
-
Cox MMJ, Hollister JR. FluBlok, a next generation influenza vaccine manufactured in insect cells. Biologicals. 2009 Jun;37(3):182–9.
- Footnote 19
-
Ismail SJ, Langley JM, Harris TM, Warshawsky BF, Desai S, FarhangMehr M. Canada's National Advisory Committee on Immunization (NACI): Evidence-based decision-making on vaccines and immunization. Vaccine. 2010 Apr;28:A58–63.
- Footnote 20
-
Government of Canada [Internet]. Evidence-Based Recommendations for Immunization: Methods of the NACI, January 2009, CCDR. 2009. Available from: http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/09vol35/acs-1/index-eng.php
- Footnote 21
-
Ismail SJ, Hardy K, Tunis MC, Young K, Sicard N, Quach C. A framework for the systematic consideration of ethics, equity, feasibility, and acceptability in vaccine program recommendations. Vaccine. 2020 Aug;38(36):5861–76.
- Footnote 22
-
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;l4898.
- Footnote 23
-
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016 Oct 12;i4919.
- Footnote 24
-
The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews [Internet]. Checklist for Case Series. Available from: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Case_Series2017_0.pdf
- Footnote 25
-
Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working Group [Internet]. GRADE Handbook. 2013. Available from: https://gdt.gradepro.org/app/handbook/handbook.html
- Footnote 26
-
Hill RR. How to GRADE the quality of the evidence. Cochrane Consumers and Communication Group [Internet]. Available from: https://colorectal.cochrane.org/sites/colorectal.cochrane.org/files/public/uploads/how_to_grade.pdf
- Footnote 27
-
US Food and Drug Administration [Internet]. Guidance for industry: Clinical data needed to support the licensure of seasonal inactivated influenza vaccines. 2007. Available from: https://www.fda.gov/media/73706/download
- Footnote 28
-
Review Manager (RevMan). The Cochrane Collaboration; 2014.
- Footnote 29
-
Izurieta HS, Chillarige Y, Kelman J, Wei Y, Lu Y, Xu W, et al. Relative Effectiveness of Influenza Vaccines Among the United States Elderly, 2018–2019. J Infect Dis. 2020 Jun 29;222(2):278–87.
- Footnote 30
-
Wang W, Alvarado-Facundo E, Vassell R, Collins L, Colombo RE, Ganesan A, et al. Comparison of A(H3N2) Neutralizing Antibody Responses Elicited by 2018–2019 Season Quadrivalent Influenza Vaccines Derived from Eggs, Cells, and Recombinant Hemagglutinin. Clin Infect Dis. 2021 Dec 6;73(11):e4312–20.
- Footnote 31
-
Belongia EA, Levine MZ, Olaiya O, Gross FL, King JP, Flannery B, et al. Clinical trial to assess immunogenicity of high-dose, adjuvanted, and recombinant influenza vaccines against cell-grown A(H3N2) viruses in adults 65 to 74 years, 2017–2018. Vaccine. 2020 Mar;38(15):3121–8.
- Footnote 32
-
Cowling BJ, Perera RAPM, Valkenburg SA, Leung NHL, Iuliano AD, Tam YH, et al. Comparative Immunogenicity of Several Enhanced Influenza Vaccine Options for Older Adults: A Randomized, Controlled Trial. Clin Infect Dis. 2020 Oct 23;71(7):1704–14.
- Footnote 33
-
Shinde V, Cai R, Plested J, Cho I, Fiske J, Pham X, et al. Induction of Cross-Reactive Hemagglutination Inhibiting Antibody and Polyfunctional CD4+ T-Cell Responses by a Recombinant Matrix-M–Adjuvanted Hemagglutinin Nanoparticle Influenza Vaccine. Clin Infect Dis. 2021 Dec 6;73(11):e4278–87.
- Footnote 34
-
Dunkle LM, Izikson R, Patriarca PA, Goldenthal KL, Muse D, Cox MMJ. Randomized Comparison of Immunogenicity and Safety of Quadrivalent Recombinant Versus Inactivated Influenza Vaccine in Healthy Adults 18–49 Years of Age. J Infect Dis. 2017 Dec 5;216(10):1219–26.
- Footnote 35
-
Gouma S, Zost SJ, Parkhouse K, Branche A, Topham DJ, Cobey S, et al. Comparison of Human H3N2 Antibody Responses Elicited by Egg-Based, Cell-Based, and Recombinant Protein–Based Influenza Vaccines During the 2017–2018 Season. Clin Infect Dis. 2020 Sep 12;71(6):1447–53.
- Footnote 36
-
Dawood FS, Naleway AL, Flannery B, Levine MZ, Murthy K, Sambhara S, et al. Comparison of the Immunogenicity of Cell Culture-Based and Recombinant Quadrivalent Influenza Vaccines to Conventional Egg-Based Quadrivalent Influenza Vaccines Among Healthcare Personnel Aged 18–64 Years: A Randomized Open-Label Trial. Clin Infect Dis. 2021 Dec 6;73(11):1973–81.
- Footnote 37
-
European Medicines Agency (EMA) [Internet]. Assessment Report: Supemtek. 2021. Available from: https://www.ema.europa.eu/en/documents/assessment-report/supemtek-epar-public-assessment-report_en.pdf
- Footnote 38
-
Cowling BJ, Thompson MG, Ng TWY, Fang VJ, Perera RAPM, Leung NHL, et al. Comparative Reactogenicity of Enhanced Influenza Vaccines in Older Adults. J Infect Dis. 2020 Sep 14;222(8):1383–91.
- Footnote 39
-
Woo EJ, Moro PL. Postmarketing safety surveillance of quadrivalent recombinant influenza vaccine: Reports to the vaccine adverse event reporting system. Vaccine. 2021 Mar;39(13):1812–7.
- Footnote 40
-
Treanor JJ, Sahly HE, King J, Graham I, Izikson R, Kohberger R, et al. Protective efficacy of a trivalent recombinant hemagglutinin protein vaccine (FluBlok®) against influenza in healthy adults: A randomized, placebo-controlled trial. Vaccine. 2011 Oct;29(44):7733–9.
- Footnote 41
-
Grohskopf LA, Alyanak E, Broder KR, Blanton LH, Fry AM, Jernigan DB, et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2020–21 Influenza Season. MMWR Recomm Rep. 2020 Aug 21;69(8):1–24.
- Footnote 42
-
Hsiao A, Hansen J, Nunley KV, Lewis N, Selmani A, Inamdar A, et al. Safety of recombinant quadrivalent influenza vaccine compared to inactivated influenza vaccine in Chinese adults: An observational study. Vaccine. 2022 Jan;S0264410X21016418.
- Footnote 43
-
Hansen J, Goddard K, Timbol J, Zhang L, Lewis N, Dunkle L, et al. Safety of Recombinant Influenza Vaccine Compared to Inactivated Influenza Vaccine in Adults: An Observational Study. Open Forum Infect Dis. 2020 Jun 1;7(6):ofaa179.
- Footnote 44
-
Remschmidt C, Wichmann O, Harder T. Frequency and impact of confounding by indication and healthy vaccinee bias in observational studies assessing influenza vaccine effectiveness: a systematic review. BMC Infect Dis. 2015 Dec;15(1):429.