Archived - Influenza vaccine safety in Ontario

 Download this article as a PDF (175 KB - 6 pages)
Download this article as a PDF (175 KB - 6 pages)Published by: The Public Health Agency of Canada
Issue: Volume 42-9: Scientific writing
Date published: September 1, 2016
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 42-9, September 1, 2016: Scientific writing
Surveillance
Assessing vaccine safety within Ontario’s Universal Influenza Immunization Program, 2012–2013 to 2014–2015
Harris T1*, Wong K1, Nair J1, Fediurek J1, Deeks SL1,2
Affiliations
1 Public Health Ontario, Toronto, ON
2 Dalla Lana School of Public Health, University of Toronto, Toronto, ON
Correspondence
Suggested citation
Harris T, Wong K, Nair J, Fediurek J, Deeks SL. Assessing vaccine safety within Ontario’s Universal Influenza Immunization Program, 2012-2013 to 2014-2015. Can Comm Dis Rep 2016;42:181-6. https://doi.org/10.14745/ccdr.v42i09a04
Abstract
Background: Influenza vaccine is recommended to prevent influenza-related morbidity and mortality. Post-marketing surveillance of adverse events following influenza vaccine is essential to monitor vaccine safety, inform immunization program planning and evaluation, and build confidence in immunization.
Objective: To summarize adverse events following immunization (AEFIs) reported after receipt of influenza vaccines administered within the Universal Influenza Immunization Program in Ontario.
Methods: AEFIs following administration of influenza vaccines between September 1, 2012 and August 31, 2015 were extracted from the Integrated Public Health Information System (iPHIS) on September 1, 2015. Events were grouped by provincial surveillance definitions. Reporting rates were calculated using provincial population estimates or net doses distributed as the denominator. The standard World Health Organization definition of serious AEFIs was used.
Results: There were 12.1 million doses of influenza vaccine distributed in Ontario and 528 AEFIs reported following influenza vaccines administered over three seasons. The annualized reporting rate was 4.4 per 100,000 doses distributed with a significant decreasing trend over time (p<0.05). The median age was 39.6 years (range six months-96 years); children under four years of age had the highest reporting rate (3.5 per 100,000 population). Disproportionate reporting among females was observed (76.5 percent), most notably in those 18 years and older. The most frequently reported events were injection site reactions (36.2 percent of reports). Others included allergic skin reactions (21.1 percent) and rashes (17.3 percent). Serious AEFIs were rare with a reporting rate of 1.6 per million doses distributed.
Conclusion: This assessment found a low rate of reported adverse events following influenza vaccines administered in Ontario. Most reported events were mild and resolved completely. The findings were consistent with the very good safety profile of influenza vaccines.
Introduction
Influenza is a respiratory infection which causes approximately 12,200 hospitalizations and 3,500 deaths in Canada each yearFootnote 1. Annual seasonal influenza vaccination is the most effective way to prevent influenza and its complications. There are multiple influenza vaccines authorized in Canada for use in individuals six months of age and older. Specific products include inactivated trivalent and quadrivalent vaccines (including adjuvanted and high-dose formulations) and live attenuated trivalent and quadrivalent vaccines with varying indications based on age and immune statusFootnote 1Footnote 2. The National Advisory Committee on Immunization (NACI) recommends influenza vaccine to all individuals six months of age and older without contraindications, with particular focus on people at high risk of influenza-related complications or hospitalization and people capable of transmitting influenza to those at high riskFootnote 1. Ontario has had a publicly-funded Universal Influenza Immunization Program since 2000Footnote 3. All Ontarians six months of age and older, who live, work or go to school in the Province are eligible for yearly publicly-funded influenza vaccine. Most influenza vaccines in the Province are administered within the Universal Influenza Immunization Program, however influenza vaccine products which are authorized for use but not included in the public program may be purchased privately.
Influenza vaccines are generally safe and well tolerated. For influenza vaccines administered by intramuscular injection, the most common side effect is pain at the injection site, which affects between 40 to 60 percent of healthy adults, but is generally mild and resolves within a few daysFootnote 4Footnote 5. Higher frequencies of injection site reactions are observed for adjuvanted and high-dose formulations. The occurrence of serious adverse events is rare and includes anaphylaxis and Guillain-Barré syndrome (GBS)Footnote 1. Post-marketing surveillance of influenza vaccines is essential to continue to demonstrate vaccine safety over time, to inform evaluation and build confidence in influenza immunization programs. Information from public health surveillance of adverse events following immunization (AEFIs) provides relevant and timely information to address concerns about vaccine safety, which have been shown to be a key barrier influencing vaccine acceptance among the general populationFootnote 6Footnote 7Footnote 8 and health care workersFootnote 9Footnote 10Footnote 11.
Our objective is to summarize influenza AEFIs reported in Ontario during three recent influenza seasons to support a comprehensive evaluation of the Universal Influenza Immunization Program in Ontario.
Methods
Definitions
A confirmed AEFI is defined as "Any reported event in a vaccine recipient which follows immunization that cannot be clearly attributed to other causes. A causal relationship with the administration of the vaccine does not need to be proven"Footnote 12. Adverse events are defined according to event-specific provincial surveillance criteriaFootnote 12. AEFIs are further defined as serious if they meet the World Health Organization standard definition which specifies that a serious AEFI is one that results in death, is life-threatening, requires in-patient hospitalization or prolongation of existing hospitalization, results in persistent or significant disability/incapacity, or is a congenital anomaly/birth defectFootnote 13Footnote 14. Other important medical events include: anaphylaxis, encephalitis, acute disseminated encephalomyelitis, myelitis, meningitis, GBS, acute cerebellar ataxia and thrombocytopenia. These events do not meet the above definition of serious and were measured and presented separately. Reports of events managed as anaphylaxis were further assessed using the Brighton Collaboration case definition and diagnostic levels of certaintyFootnote 15.
In Ontario, reporting of AEFIs by specific health professionals (e.g., physicians, nurses and pharmacists) is mandated by provincial public health legislation Footnote 16; however, voluntary reporting from vaccine recipients or their caregivers also occurs. Reports of AEFIs are received by local public health units (PHUs) who investigate and enter information according to provincial surveillance guidelines into the Integrated Public Health Information System (iPHIS), the electronic reporting system for reportable diseases and AEFIs in Ontario.
The review included all AEFIs reported following administration of influenza vaccines administered within the Universal Influenza Immunization Program between September 1, 2012 and August 31, 2015. Data was extracted from iPHIS on September 1, 2015. Vaccine products utilized within the Universal Influenza Immunization Program between 2012-2013 and 2014-15 were trivalent inactivated vaccines including: Fluviral®, Agriflu®, Vaxigrip®, Fluzone® (2014-2015 only) and Fluad® (for 65 years and older who reside in long-term care facilities). Reports following administration of live attenuated influenza vaccine only were excluded, as they represented a very small number of reports (n=4) and were not part of the Universal Influenza Immunization Program during the reporting period.
Proportions were based on reports with completed data in iPHIS, therefore the denominator varies by variable. Temporal trends were assessed by influenza season, defined as September 1 to August 31 for the purposes of provincial influenza AEFI surveillance. AEFI reporting rates were calculated using both doses distributed and population-based denominators. Reporting rates were calculated over time and by event-type using net doses distributed within the publicly-funded program as the denominator. This was calculated based on estimates of net vaccine distribution data provided by the Ontario Government Pharmaceutical and Medical Supply Service which is adjusted for wasted or returned reusable vaccine. Reporting rates were calculated by demographic groups (e.g., age, sex and geography) using population-based denominators in the absence of information about dose distribution within these groups. Population denominators were based on 2012 and 2013 estimates for the 2012-2013 and 2013-2014 influenza seasons, respectively and 2014 projections for the 2014-2015 seasonFootnote 17Footnote 18. A statistical analysis was performed using SAS version 9.3 and Microsoft Excel 2010. Trends in incidence rate over the entire study period were assessed using Poisson regression and p-values less than 0.05 were considered statistically significant. This project was approved by the Public Health Ontario Ethics Review Board.
Results
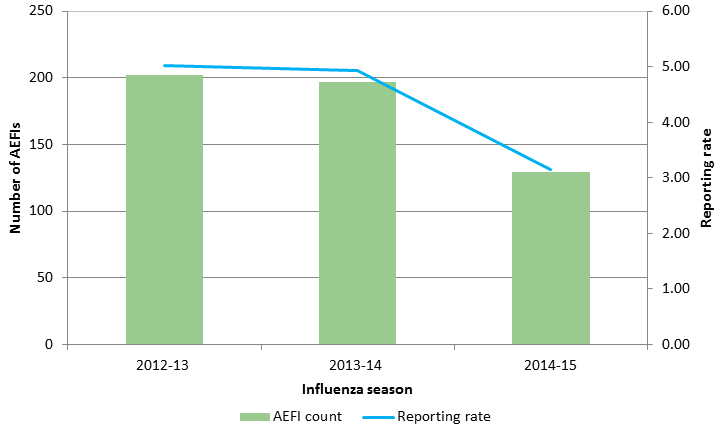
There were 528 AEFIs reported following influenza vaccines administered within the Universal Influenza Immunization Program in Ontario between September 1, 2012 and August 31, 2015. During this time period, over 12.1 million net doses of Universal Influenza Immunization Program vaccine were distributed, for an annualized reporting rate of 4.4 per 100,000 doses distributed. A significant decreasing trend in the reporting rate by season was observed, with a marked drop in the reporting rate in 2014-2015, compared to 2012-2013 and 2013-2014 (p<0.05) (Figure 1).
Figure 1: Number of influenza AEFIs and reporting rate (per 100,000 doses distributed) in Ontario, 2012-2013 to 2014-2015
Text description: Figure 1
Figure 1: Number of influenza AEFIs and reporting rate (per 100,000 doses distributed) in Ontario, 2012-2013 to 2014-2015
| Flumist only | |||
|---|---|---|---|
| Season | |||
| 2012/2013 | 2013/2014 | 2014/2015 | |
| Count Flumist AEFIs | 1 | 2 | 1 |
| Doses distributed (all Flumist from manufacturer) | 7,580 | 10,240 | 13,380 |
| Rate | 13.19 | 19.53 | 7.47 |
| All publicly funded (excluding PCCHU Flumist pilot) | |||
|---|---|---|---|
| Season | |||
| 2012/2013 | 2013/2014 | 2014/2015 | |
| AEFI count | 202 | 197 | 129 |
| Doses distributed | 4,020,830 | 3,999,990 | 4,108,661 |
| Reporting rate | 5.02 | 4.93 | 3.14 |
| All combined (All publicly funded + Flumist doses from AstraZeneca) | |||
|---|---|---|---|
| Season | |||
| 2012/2013 | 2013/2014 | 2014/2015 | |
| Count all flu AEFIs (including Flumist) | 203 | 199 | 130 |
| Doses distributed | 4,028,410 | 4,010,230 | 4,122,041 |
| Reporting rate | 5.04 | 4.96 | 3.15 |
| All OGP (publicly funded plus PCCHU Flumist pilot) | |||
|---|---|---|---|
| Season | |||
| 2012-13 | 2013-14 | 2014-15 | |
| Count Flu AEFIs (all combined) | 203 | 199 | 130 |
| Doses distributed (OGP all) | 4,020,830 | 4,000,270 | 4,108,661 |
| Rate | 5.05 | 4.97 | 3.16 |
OVERALL REPORTING RATE (including all doses and vaccines): 4.374755
OVERALL REPORTING RATE (publicly funded, excluding Flumist)
Individuals with AEFIs ranged in age from six months to 96 years (median 39.6 years). Over half of all reports (58.2 percent) were in adults 18-64 years of age; however, the highest age-specific reporting rates were in children less than four years and five to nine years of age (3.5 and 2.8 per 100,000 population, respectively) (Table 1). Reporting rates within age group decreased over the three seasons with significant decreases in children less than four and adults 50 to 64 years of age. Disproportionate reporting among females was observed (76.5 percent overall), particularly in adult age groups (93.3 and 86.5 percent in 18-49 and 50-64 year olds, respectively). The highest female-to-male reporting rate ratios were in adults 18-49 and 50-64 years of age (13.8 and 6.2, respectively). Geographically, reporting rates by PHU varied widely from zero to 9.9 per 100,000 population with no noted pattern.
| Age Category (years)Footnote1 | CountFootnote 2 | Percent of AEFIsFootnote 2 | Percent of populationFootnote3 | Reporting rate (per 100,000 population)Footnote4 |
|---|---|---|---|---|
| ≤4 | 75 | 14.3 | 5.3 | 3.49 |
| 5-9 | 61 | 11.6 | 5.4 | 2.78 |
| 10-17 | 22 | 4.2 | 9.0 | 0.59 |
| 18-49 | 180 | 34.2 | 43.8 | 1.00 |
| 50-64 | 126 | 24.0 | 20.9 | 1.50 |
| 65-79 | 50 | 9.5 | 11.5 | 1.11 |
| 80+ | 12 | 2.3 | 4.2 | 0.72 |
| Total | 526 | 100.0 | 100.0 | 1.29 |
Most adverse events were reported following administration of influenza vaccine only (93.6 percent; n=494); 34 reports involved co-administration with other vaccines, most commonly, pneumococcal polysaccharide 23-valent (Pneu-P-23) vaccine (n=15) and tetanus, diphtheria, acellular pertussis (Tdap) vaccine (n=7). The most frequently reported events were injection site reactions which were documented in 36.2 percent of all reports. Other frequently reported types of events included allergic skin reactions (21.1 percent) and rashes (17.3 percent) (Table 2). The highest event-specific reporting rates were similar to reporting volume with the highest rates for pain, redness and swelling at the injection site, allergic skin reactions and rash (1.3, 0.9 and 0.8 per 100,000 doses distributed, respectively). Medically important events (n=27) included anaphylaxis (n=22), thrombocytopenia (n=1) and acute rhabdomyolosis (n=1) as well as three serious events described below. Reports of events managed as anaphylaxis ranged in age from four to 84 years, were predominantly (81.8 percent; n=18) female and none were classified as serious. Eight (36.4 percent) met the Brighton Collaboration anaphylaxis case definition (one level I, six level II, one level III) and the remaining 14 reports (63.6 percent) did not contain sufficient evidence to meet the definition. Based on events that met the Brighton definition, the reporting rate of anaphylaxis was 0.7 per one million doses distributed.
| Adverse event typeTable 2 Footnote 1 | Adverse eventTable 2 Footnote 2 | Number of AEFI reportsTable 2 Footnote 3 | Reporting rateTable 2 Footnote 4 | Percent of all AEFI reportsTable 2 Footnote 3 | Number of serious reports |
|---|---|---|---|---|---|
| Injection site reactions | Total | 190 | 1.6 | 36.2 | 8 |
| Cellulitis | 30 | 0.2 | 5.7 | 6 | |
| Infected Abscess | 2 | < 0.1 | 0.4 | 1 | |
| Nodule | 4 | < 0.1 | 0.8 | 0 | |
| Pain/redness/swelling at the injection siteTable 2 Footnote 1 | 162 | 1.3 | 30.9 | 3 | |
| Pain/redness/swelling extending beyond nearest joint | 40 | 0.3 | 7.6 | 1 | |
| Pain/redness/swelling <4 daysTable 2 Footnote 5 | 7 | 0.1 | 1.3 | 0 | |
| Pain/redness/swelling ≥4 days | 129 | 1.1 | 24.6 | 2 | |
| Sterile abscess | 2 | < 0.1 | 0.4 | 0 | |
| Systemic reactions | Total | 156 | 1.3 | 29.7 | 7 |
| Adenopathy/lymphadenopathy | 10 | 0.1 | 1.9 | 0 | |
| Arthritis/arthralgia | 16 | 0.1 | 3 | 1 | |
| Fever ≥ 38 °C in conjunction with another reportable event | 42 | 0.3 | 8 | 6 | |
| Hypotonic-hypo-responsive episode (HHE) | 1 | < 0.1 | 0.2 | 0 | |
| Parotitis | 1 | < 0.1 | 0.2 | 0 | |
| Persistent crying/screaming | 1 | < 0.1 | 0.2 | 0 | |
| Rash | 91 | 0.8 | 17.3 | 1 | |
| Severe vomiting/diarrheaTable 2 Footnote 6 | 14 | 0.1 | 2.7 | 1 | |
| Syncope with injuryTable 2 Footnote 6 | 1 | < 0.1 | 0.2 | 0 | |
| Thrombocytopenia | 1 | < 0.1 | 0.2 | 0 | |
| Allergic events | Total | 145 | 1.2 | 27.6 | 1 |
| Allergic reaction - skin | 111 | 0.9 | 21.1 | 1 | |
| Allergic reaction - otherTable 2 Footnote 5 | 6 | < 0.1 | 1.1 | 0 | |
| Event managed as anaphylaxisTable 2 Footnote 6 | 22 | 0.2 | 4.2 | 0 | |
| Oculorespiratory syndrome (ORS) | 11 | 0.1 | 2.1 | 0 | |
| Neurologic events | Total | 32 | 0.3 | 6.1 | 8 |
| Anaesthesia/paraesthesiaTable 2 Footnote 6 | 10 | 0.1 | 1.9 | 2 | |
| Bell's palsy | 4 | < 0.1 | 0.8 | 0 | |
| Convulsions/seizures | 9 | 0.1 | 1.7 | 3 | |
| Encephalopathy/encephalitis | 2 | < 0.1 | 0.4 | 1 | |
| Guillian-Barré syndrome (GBS) | 3 | < 0.1 | 0.6 | 2 | |
| Paralysis other than Bell's palsy | 4 | < 0.1 | 0.8 | 0 | |
| Other severe/unusual events | Total | 105 | 0.9 | 20.0 | 8 |
There were 20 serious AEFI reports across all seasons, representing 3.8 percent of all AEFIs and a reporting rate of 1.6 per million doses distributed. The proportion of reports that were classified as serious by season steadily decreased (5.0, 3.6 and 2.3 percent for 2012-2013 to 2014-2015, respectively) as did the serious reporting rate (from 2.5 per million doses distributed in 2012-2013 to 1.8 and 0.7 per million doses distributed in 2013-2014 and 2014-2015, respectively). The age range of serious reports was one to 81 years with the greatest number of reports in older adults 50-64 and 65-79 years, as well as children one to four years of age (four reports each). Females accounted for 60 percent of serious reports. The most frequent type of event among serious AEFIs was cellulitis (requiring hospital admission for treatment with IV antibiotics) (n=6). Other serious events included seizures (n=2; one febrile in a child, one afebrile in an adult), anaesthesia/paraesthesia (n=2), GBS (n=3), bilateral panuveitis (n=2; one also diagnosed with GBS), encephalitis (n=1), chronic inflammatory demyelinating process (n=1), polymyalgia rheumatic (n=1), febrile rash illness (n=1), infective abscess (n=1) and one report of sudden onset of mobility limitation with spontaneous resolution. No deaths were reported.
Out of all AEFIs, the majority were reported by health care professionals (63.8 percent: 25.3 percent from physicians and 38.5 percent from other health professionals), followed by self-reports and reports by family members (12.1 percent, 8.2 percent, respectively). For those reports with health care utilization information completed, 68.2 percent (n=353) sought outpatient medical consultation, 23.1 percent (n=121) were seen in the emergency department and 3.9 percent (n=20) were hospitalized. In most cases, the individual was recovered at the time of reporting (70.0 percent, n=336), 26.0 percent were not yet recovered (but full recovery was expected) and 4.0 percent (n=19) were documented as having residual effects. Among all reports, two were noted as being pregnant; both were mild, non-serious events which resolved completely. There were six AEFI reports where an immunization error was noted. All involved incorrect injection technique (e.g., intramuscular injection administered too high, needle length too short) resulting in prolonged pain at the injection site and one serious report of cellulitis.
Discussion
This assessment of adverse events following influenza immunization reported in Ontario during three recent influenza seasons is consistent with the well-established safety profile of influenza vaccines. Ontario's influenza AEFI reporting rate of 4.4 per 100,000 doses distributed between the 2012-2013 and 2014-2015 seasons represents one of the lowest vaccine-specific reporting rates of all publicly-funded vaccines in the Province Footnote 19. This rate was also lower than the most recently reported national influenza AEFI reporting rate (8.9 per 100,000 doses distributed; 2012-2013 to 2014-2015) Footnote 20 suggesting under-reporting in Ontario compared to other Canadian jurisdictions.
The decrease in reporting rate observed in 2014-2015 compared to previous years was unexpected and not fully understood. It was however, consistent with a decrease observed nationally during the same season. Some of the decrease could have been due to changes in provincial AEFI case definitions, which occurred during the first season in 2013 (e.g., limiting reporting of events involving pain, redness or swelling at the injection site to those that persist for four days or longer). Delayed reporting may play a role although in Ontario the proportion of late reports (e.g., reported after August 31) for 2012-2013 and 2013-2014 was minimal (3.5 and 1.5 percent, respectively) and a similar proportion of delayed reports for the 2014-2015 season would still result in a lower AEFI rate.
Age group-specific population-based reporting rates of influenza AEFIs were generally as expected with higher rates and proportions of AEFIs (compared to population distribution) in the youngest age groups. The observed female predominance in AEFI reporting has been previously noted in Ontario Footnote 21Footnote 22 and in other passive AEFI surveillance systems Footnote 23Footnote 24Footnote 25 although it appears particularly striking in this current assessment (93.3 and 86.5 percent in 18-49 and 50-64 year olds, respectively). The reasons for this phenomenon are likely multi-factorial. Differences in vaccine uptake between males and females may play a role, especially as health care workers (a target group for influenza vaccine) are more likely to be female. However, provincial estimates from the Canada Community Health Survey (12 years of age and older; influenza immunization, less than one year ago) suggest only a slight female predominance among those immunized (54.1 percent were female) Footnote 26. Other potential factors include: differences between males and females in health care seeking behavior Footnote 27Footnote 28Footnote 29 once an AEFI occurs and different biologic response to vaccines Footnote 30Footnote 31. The difference in AEFI reporting by sex was less pronounced for serious AEFIs among which 60 percent were female.
Injection site reactions were the most frequently reported type of event in this assessment which is consistent with clinical trials and post-marketing surveillance of influenza vaccine products administered by intramuscular injectionFootnote 4Footnote 5Footnote 23Footnote 32. Unlike the relatively high volume of injection site reactions among all AEFIs, the rate of reporting was quite low (1.6 per 100,000 doses distributed). While this rate likely underestimates the actual occurrence of localized reactions, some degree of under-reporting is expected for these events which are typically mild and resolve on their own. Allergic events were also frequently reported, most of which were allergic skin reactions which is consistent with previous AEFI assessmentsFootnote 19Footnote 20Footnote 23. A small number of allergic events were classified as an event managed as anaphylaxis. Based on reports that met the Brighton definition, the reporting rate of anaphylaxis was comparable, albeit slightly lower than the expected rate of anaphylaxis following influenza vaccines which has been estimated at about one per million doses of vaccineFootnote 33Footnote 34.
As expected, serious events following influenza vaccine during this time period were rare and most often related to events known to be rarely reported following receipt of influenza vaccines. For example, GBS is a rare event which is consistently reported in post-marketing surveillance of influenza vaccines, including in Ontario where there were three reports of GBS following influenza vaccine over three years. While the evidence considering influenza vaccination and GBS is inadequate to accept or reject a causal associationFootnote 35, the absolute risk of approximately one excess case per one million vaccinesFootnote 36Footnote 37Footnote 38 is much lower than that associated with influenza diseaseFootnote 39Footnote 40. Of note, there were two reports of bilateral panuveitis during this time period which have been described in more detail by Manusow and colleaguesFootnote 41. Panuveitis is a rare condition most often associated with infectious or inflammatory causesFootnote 42 although there is no known causal association with vaccinesFootnote 43.
Limitations of this analysis include those which are inherent to many passive AEFI surveillance systems such as data quality, completeness and reporting biasFootnote 23Footnote 24. Under-reporting of AEFIs has been previously demonstrated to be more prominent in Ontario compared to other jurisdictionsFootnote 19 and is again suggested here. Reporting rates were calculated using the total population or doses distributed as the denominator, both of which are proxies for doses administered in the absence of a provincial population-based immunization registry. Although doses distributed are widely used in analyses of passive AEFI surveillance systemsFootnote 23Footnote 24, it can underestimate AEFI reporting rates if vaccine wastage is not well captured or understood. Trend analysis includes only three seasons therefore interpretation may be limited. Analyses of additional seasons over a longer time period will further inform ongoing assessment of trends in AEFI reporting.
Conclusion
This assessment found that influenza vaccines administered within the Universal Influenza Immunization Program in Ontario resulted in a low rate of reported adverse events. Most reported events were mild and resolved completely. No unexpected safety issues were identified. These findings are consistent with the very good safety profile of influenza vaccines used in Canada and internationally. Continued surveillance is important to monitor for safety signals and reporting trends over time, particularly with the introduction of new influenza vaccines and to maintain professional and public confidence in influenza vaccine safety. Further analysis is needed to understand the decreasing rate over time and under-reporting within the surveillance system to optimize AEFI surveillance data in Ontario.
Acknowledgements
Sincere thanks is extended to public health unit staff across the province for their efforts in investigation and reporting of AEFIs which are essential to the evaluation of the Universal Influenza Immunization Program and influenza vaccine safety in Ontario.
Conflict of interest
None.
Funding
Funding for this project was provided by Public Health Ontario.