Archived - Barriers of Hep C virus screening and testing

 Download this article as a PDF
Download this article as a PDF Published by: The Public Health Agency of Canada
Issue: Volume 44-7/8 : Can we eliminate hepatitis C?
Date published: July 5, 2018
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 44-7/8, July 5, 2018: Can we eliminate hepatitis C?
Scoping review
Barriers to and facilitators of hepatitis C virus screening and testing: A scoping review
N Shehata1, T Austin1, S Ha1, K Timmerman1
Affiliation
1 Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada, Ottawa, ON
Correspondence
Suggested citation
Shehata N, Austin T, Ha S, Timmerman K. Barriers to and facilitators of hepatitis C virus screening and testing: A scoping review. Can Commun Dis Rep 2018;44(7/8):166-72. https://doi.org/10.14745/ccdr.v44i78a03
Keywords: barriers, facilitators, screening, testing, hepatitis C
Abstract
Background: As part of the global effort to eliminate hepatitis C virus (HCV), it is important to understand the barriers to and facilitators of HCV screening and testing.
Objective: To examine the barriers and facilitators experienced by health care providers offering HCV screening and testing and patients seeking HCV testing.
Methods: A literature search was conducted using Embase, Medline and Scopus databases to collect studies published between January 2012 and July 2017. We extracted the following data: author, year of publication, study design, population, setting, country, method of data collection, and knowledge and awareness outcomes.
Results: A total of 16 articles were identified. Barriers to HCV screening and testing among patients included low self-perceived risk of acquiring HCV, perceived stigma and fear of a positive result. Facilitators of HCV screening and testing, as reported by patients, included increased knowledge of transmission and manifestations of HCV infection and having HCV testing included as part of routine care with or without HIV testing. Barriers to offering HCV screening and testing included time constraints, lack of specific knowledge about HCV and discomfort in asking about risk behaviours. Facilitators of offering HCV screening and testing included testing reminders and working in locations with a higher HCV caseload.
Conclusion: Lack of knowledge and fear of stigma and discrimination remain barriers to HCV testing at the patient level and lack of time, knowledge and discomfort in asking about risk behaviours remain barriers to offering HCV testing by health care providers. This identifies potential areas for future public health action.
Introduction
In 2016, the 69th World Health Assembly approved the Global Health Sector Strategy to eliminate hepatitis C virus (HCV) and hepatitis B virus as a public health threat by 2030Footnote 1. This goal has been made possible as a result of the availability of the new interferon-free direct acting antiviral (DAA) therapies, which are highly effective in stopping the progression of liver disease and eliminating the virusFootnote 2.
One of the challenges with diagnosing HCV infection is that it is often asymptomatic. Screening and testing for HCV infection is a fundamental step in identifying those who are unaware of their infection. Furthermore, the diagnosis of HCV infection can help reduce the burden of disease and limit transmission to those at increased risk of infection and those at risk of reinfectionFootnote 3. The more people with HCV infection are treated, the less transmission and the fewer new cases. Thus screening and testing is critical to achieving the World Health Assembly’s targets.
In 2011, it was estimated that 44% of people who were living with chronic HCV infection in Canada were unaware of their infectionFootnote 4. Current Canadian HCV screening guidelines recommend screening of individuals at increased risk of infectionFootnote 5. People at high risk include individuals with current or past history of injection drug use, HIV-positive gay/bisexual men who have sex with men, incarcerated populations, people experiencing homelessness, individuals exposed to previous health care procedures or personal services where there is a lack of infection prevention control, and individuals who were born, travelled, or resided in countries with high HCV prevalenceFootnote 6.
The objective of this scoping review is to examine the current barriers to and facilitators of HCV screening and testing from the perspectives of both patients and health care providers.
Methods
In this scoping review, we sought to examine the barriers to and facilitators of HCV testing among health care providers, patients and individuals other than injection drug users at risk of HCV infection. The rationale for this was that barriers to and facilitators of HCV screening and testing among people who inject drugs are well-documentedFootnote 7. In addition, people who inject drugs tend to have high testing ratesFootnote 5. Yet, few studies have examined the barriers to and facilitators of HCV screening and testing among other at-risk populations including where there may be a hidden burden.
We conducted a literature search for studies published between January 2012 and July 2017 to capture the most recent studies in the changing landscape of HCV screening and testing. We searched Embase, Medline and Scopus using the search terms “hepatitis C” or “HCV” and “screen” or “test” and “barriers” or “facilitators.” (Search strategy available upon request)
Studies were included if they were published between January 2012 and July 2017; published in English or French; focused on populations other than people who inject drugs; and conducted in well-resourced countries. Letters to the editors, narrative reviews and commentaries were excluded. Key populations were not determined a priori but rather emerged from the results of the search.
Once the articles were identified, title and abstracts were screened for relevance. We extracted data on the study population, location of study, study design, outcomes and results.
Results
Of the 126 articles identified in the search, 16 studies focused on the barriers to and facilitators of HCV screening and testing (Figure 1).
Figure 1: Search strategy flow diagram
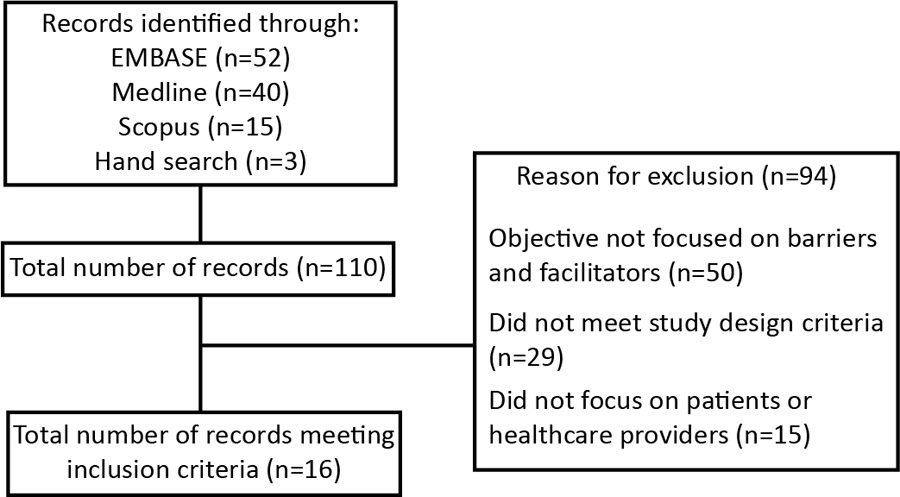
Text description: Figure 1
Figure 1: Search strategy flow diagram
Figure 1 depicts a flow diagram of the search strategy for articles focused on the barriers to and facilitators of hepatitis C virus screening and testing. The top left box indicates how articles were identified. The initial search included 52 articles from EMBASE, 40 articles from Medline, 15 articles from Scopus, and three identified from hand searching. This lead to a total of 110 records.
The box on the right identifies the reasons for exclusion of articles (n=94). Fifty articles were excluded due to the objective not being focused on barriers and facilitators. Twenty-nine articles did not meet the study design criteria. Fifteen articles did not focus on patients or healthcare providers.
The final box on the bottom left identifies the remaining records that met the inclusion criteria for this scoping review (n=16).
Most of the studies examined both health care provider and patient populations. Health care providers included general practitioners, clinical representatives from hospitals, newly qualified doctors, medical students, resident physicians and nursesFootnote 8Footnote 9Footnote 10Footnote 11Footnote 12Footnote 13Footnote 14. Patient groups included adults born between 1945 and 1965; patients attending sexually transmitted infections (STI) clinics, outpatient clinics or primary care facilities; youth and adults working in HIV/HCV prevention; immigrant and migrant populations; and sex workersFootnote 10Footnote 12Footnote 13Footnote 15Footnote 16Footnote 17Footnote 18Footnote 19Footnote 20Footnote 21Footnote 22Footnote 23.
Most of the studies were conducted in the United States (n=9), followed by Canada (n=2), United Kingdom (n=2), Australia (n=1), France (n=1) and Scotland (n=1). Study designs included observational studies, cross-sectional studies and qualitative interviews.
Barriers for health care providers
We identified three primary categories of barriers to health care providers’ offering HCV screening and testing: time constraints, lack of HCV specific knowledge and discomfort with discussing HCV. These barriers were reported across all specialities (i.e., by emergency department nurses, general practitioners, new medical residents) and settings (i.e., in emergency rooms, community health centres, primary care and STI clinics).
Time constraints
Time constraints—more specifically, limited consultation times, competing priorities and lengthy pre- and post-test counselling procedures—were commonly cited barriers to HCV screening and testingFootnote 8Footnote 10Footnote 11Footnote 12Footnote 13. As a result, health care providers—especially general practitioners—did not routinely ask patients about HCV risk factorsFootnote 8Footnote 21. HCV is also often accorded a low priority due to its slow progression compared with other health conditions that may need to be addressed during an appointmentFootnote 8Footnote 11Footnote 15.
Lengthy counselling procedures also emerged as a barrier to health care providers offering HCV testing. In a study conducted in an American teaching hospital, 75% of patients in a hospital setting were not screened because the medical resident circumvented the screening processFootnote 21.
Lack of specific knowledge
Health care providers demonstrated a general understanding of HCV risk factors but recognized the need for improving their knowledge of who to testFootnote 8Footnote 11. In a study conducted in Scotland, health care providers also reported limited knowledge about counselling, to whom and where to refer diagnosed patients and protocols for testingFootnote 11. Lack of knowledge of screening guidelines was also a barrierFootnote 12.
Lack of comfort
Most health care providers understand the importance of addressing risk factors and diagnosing HCV; however, many reported difficulties in raising the subject with their patientsFootnote 9. This was especially true if the patient did not have regular contact with the provider and patient–provider rapport was limited. Providers reported that they were more comfortable offering testing after they had built a rapport with their patient and had learned about patients’ history and risk factorsFootnote 8.
Location of practice was an important factor that contributed to health care providers’ comfort with HCV screening and testing. In regions with high prevalence of HCV infection, health care providers were more comfortable with offering testing. In contrast, health care providers who worked in regions with low HCV infection prevalence were less likely to encounter cases of HCV and were less likely to be comfortable with offering a testFootnote 8.
Patient barriers to testing
Common patient barriers to seeking HCV testing include lack of knowledge; low perceived risk of infection; fear, stigma and discrimination; and limited access to health care services.
Lack of knowledge
Lack of knowledge about HCV including risk factors, routes of transmission, manifestations and outcomes of untreated infection were frequently reported as barriers to patients seeking HCV testing. Knowledge gaps are evident among patients of all levels of risk. In addition, HIV/HCV stakeholders believed that health care providers’ reluctance to discuss HCV contributed to youth and adults’ reluctance to seek or discuss testingFootnote 18.
Low perceived risk of infection
Lack of knowledge about HCV leads to low self-perceived risk of infection, which in turn leads to under- and undiagnosed cases of HCV infection. Patients frequently reported not being at risk for HCV infection or not having any risk factorsFootnote 11Footnote 15Footnote 19. Moreover, patients who had had a previous HCV test were more likely to not seek testing againFootnote 19.
Fear, stigma and discrimination
In a Canadian qualitative study, youth and adult HIV/HCV-prevention stakeholders reported that stigmatizing perceptions and negative attitudes about HIV/HCV persist and are a significant barrier to patients seeking testingFootnote 18. Other studies have also reported patients—particularly immigrant and migrant populations—fearing a positive HCV diagnosis and the associated stigma and discrimination as barriers to HCV screeningFootnote 19Footnote 20Footnote 22.
Limited access to the health care system
Limited interactions with the health care system, lack of a primary care provider and an unstable socioeconomic status were all identified in the literature as barriers to HCV testing reported by patients. Adults born between 1945 and 1965 have reported cost of testing, lack of health insurance, limited access to hepatology clinics and long wait times for appointments as barriers to HCV screeningFootnote 13Footnote 19. Language barriers and lack of culturally sensitive health services limit migrant populations’ access to HCV testingFootnote 20Footnote 22Footnote 23.
Health care provider facilitators
Two key facilitators to health care providers offering HCV screening and testing are awareness and knowledge of HCV risk factors and reminders through electronic medical record (EMR) flags.
Awareness and knowledge of risk factors
Awareness and knowledge of HCV risk factors can help health care providers facilitate HCV screening and testing. In a study conducted by McLeod et al. (2017) in Scotland, general practitioners reported almost always offering an HCV test to patients with abnormal liver function test results when they are aware of the risk factorsFootnote 11.
Electronic medical record flags
A common facilitator of offering HCV screening and testing were reminders. Such reminders could decrease missed opportunities for testing. Health care providers mentioned computerized prompts built into EMRs, based on the patient’s health history and risk factors, as a method of being remindedFootnote 8Footnote 9. This could help ensure that patients who had not been previously offered a test or who had previously declined a test not miss other opportunities for testing. Although one study described “electronic medical record flag fatigue” (where health care providers receive too many reminders)Footnote 10 other studies noted health care providers’ forgetfulness as a barrier to screening and suggest EMR flags as a solutionFootnote 8.
Patient facilitators
A key facilitator of seeking HCV testing is awareness and knowledge of HCV.
Awareness and knowledge
Enhanced patient education emerged as an important facilitator of HCV testing. Education, either directly (i.e., health care providers informing patients about the risks of HCV infection) or through awareness campaigns (e.g., television advertisements, poster and public health campaigns), lets patients know the risk factors, routes of transmission and other general information on HCV, which could make them more likely to seek testingFootnote 8Footnote 19Footnote 20.
Table 1 summarizes the key barriers to and facilitators of HCV screening and testing. Details of the included studies are shown in Appendix 1.
| Population | Barriers | Facilitators |
|---|---|---|
Health care providers |
|
|
Patients |
|
|
| Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus | ||
Discussion
This scoping review presents a high-level snapshot of the barriers to and facilitators of health care providers offering HCV screening and testing and of patients seeking HCV testing. Barriers experienced by health care providers included time constraints, lack of specific knowledge about HCV and lack of comfort discussing HCV. Common barriers for patients were: lack of knowledge, low perceived risk of infection, fear of a positive diagnosis, stigma and discrimination, and limited access to the health care system. Facilitators for health care providers to screen were: electronic medical record flags and awareness and knowledge of HCV. Facilitators for patients to request screening were: awareness and knowledge of HCV. Given the estimated prevalence of undiagnosed cases of HCV infection, results of this scoping review are important for raising awareness of factors that facilitate and hinder HCV testing.
This review has two limitations. First, as a result of the variation in time and place of the studies, some refer to first-generation DAAs, while others refer to second generation DAAs. Although the review focused on barriers to and facilitators of HCV testing, it is important to note the treatment landscape when interpreting findings, particularly considering that some barriers (i.e., cost of treatment, fear of a positive result) may be linked to the availability of treatment.
Second, there are some limitations inherent to the methodological designs of the included studies. For example, seven of the studies were cross-sectional designs, which are only able to capture data at a specific point in time. Other limitations, such as sampling bias may also be applicable to some of the included studies.
The results from this review align with previous research and add to the literature on HCV screening and testing, particularly the barriers and facilitators. A strength of this review is the focus on populations other than injection drug users, including other at-risk populations (i.e., migrants, and sex workers), as well as the general public. Future research could include assessing the barriers to and facilitators of hepatitis C testing in special populations (e.g., Indigenous communities, remote/isolated regions) where the diagnostic and treatment environments of testing are unique.
Conclusion
Understanding the barriers to and facilitators of HCV screening and testing can inform public health actions to improve risk-based screening and reduce the number of individuals unaware of their HCV infection. Informed patients and health care providers who are given the means to address stigma and discomfort around HCV could help advance the goal of HCV eradication.
Authors’ statement
- NS – Writing (first draft – background and methods), data curation (extraction)
- TA – Data curation (verification), formal analysis, writing (final draft), review and editing
- SH – Conceptualization, methodology, writing (final draft), data curation, validation, formal analysis, reviewing and editing, supervision, project administration, visualization
- KT – Conceptualization, methodology, reviewing and editing, supervision, project administration, visualization
- NS and TA contributed equally to this article.
Conflict of interest
None.
Acknowledgements
We would like to thank Dr. Margaret Gale-Rowe, Dr. Jun Wu and Margaret Bodie for their contributions to the revision of this manuscript and Audréanne Garand for her support in the data curation and initial analysis.
Funding
This work was supported by the Public Health Agency of Canada.
Appendix 1
| Author(s), year of publication / Country | Study design / Setting / Population (n) | Barriers | Facilitators |
|---|---|---|---|
Allison et al. (2016)Footnote 15 |
Cross-sectional study |
|
|
Aparicio et al. (2012)Footnote 16 |
Observational study |
|
|
Datta et al. (2014)Footnote 8 |
Mixed-methods study |
|
|
Duerme et al. (2016)Footnote 9 |
Cross-sectional study |
|
|
Feldman et al. (2017)Footnote 17 US |
Cross-sectional study |
|
None reported |
Gahagan et al. (2015)Footnote 18 |
Scoping review and qualitative interviews |
None reported |
|
Goel et al. (2015)Footnote 10 |
Observational study (retrospective) |
|
|
Grannan (2017)Footnote 19 |
Cross-sectional study |
|
|
Guirgis et al. (2012)Footnote 20 |
Cross-sectional study |
|
|
McLeod et al. (2017)Footnote 11 |
Cross-sectional study (pre and post survey) |
|
|
Patil et al. (2016)Footnote 21 |
Observational study (retrospective) |
|
None reported |
Seedat et al. (2014)Footnote 22 |
Qualitative study |
|
None reported |
Socias et al. (2015)Footnote 23 |
Observational study |
|
None reported |
Szeto et al. (2014)Footnote 12 |
Observational study (retrospective) |
|
None reported |
Taylor et al. (2016)Footnote 13 |
Descriptive study |
|
None reported |
White et al. (2016)Footnote 14 |
Cross-sectional study |
|
None reported |
| Abbreviations: BC, British Columbia; EMR, electronic medical record; GP, general practitioner; HCV, hepatitis C virus; HIV, human immunodeficiency virus; STI, sexually transmitted infection; US, United States | |||