Community-based COVID-19 outbreak of the Alpha variant in Newfoundland

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 49-2/3, February/March 2023: Early Warning in Public Health
Date published: February/March 2023
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 49-2/3, February/March 2023: Early Warning in Public Health
Rapid Communication
Community-based COVID-19 outbreak of the B.1.1.7 (Alpha) variant of concern in Newfoundland, February to March 2021
Alexandra Nunn1, Andrea Morrissey2, Ashley Crocker2, Kaitlin Patterson3, Joanne Stares4, Kerri Smith2, Laura Gilbert5, Krista Wilkinson6
Affiliations
1 Centre for Emergency Preparedness, Public Health Agency of Canada, Ottawa, ON
2 Eastern Health, St. John's, NL
3 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
4 Centre for Emergency Preparedness, Public Health Agency of Canada, St. John's, NL
5 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, St. John's, NL
6 Vaccine Rollout Task Force, Public Health Agency of Canada, Ottawa, ON
Correspondence
Suggested citation
Nunn A, Morrissey A, Crocker A, Patterson K, Stares J, Smith KN, Gilbert L, Wilkinson K. Community-based COVID-19 outbreak of the B.1.1.7 (Alpha) variant of concern in Newfoundland, February to March 2021. Can Commun Dis Rep 2023;49(2/3):59–66. https://doi.org/10.14745/ccdr.v49i23a05
Keywords: COVID-19, Canada, variant of concern, outbreak, emerging infectious diseases, household transmission, school transmission, secondary attack rates, public health measures
Abstract
Background: From March 2020 to January 2021, Newfoundland and Labrador experienced 408 coronavirus disease 2019 (COVID-19) cases (incidence 78 per 100,000). In February and March 2021, a community outbreak of the B.1.1.7 (Alpha) variant occurred in the Eastern Regional Health Authority. This article describes the epidemiology of this variant of concern outbreak, identifies settings that likely contributed to spread and informs recommendations for public health measures (PHMs).
Methods: Provincial surveillance data were linked with case interview data and a school class roster. Descriptive epidemiological methods were used to characterize the outbreak. Secondary attack rates (SAR) were calculated for households and classrooms.
Results: This outbreak involved 577 laboratory-confirmed and 38 probable cases. Whole genome sequencing determined cases were B.1.1.7. The median age was 31 years and the highest proportion of cases were in the 15 to 19-year age group (29%); 293 (51%) were female and 140 (24%) were asymptomatic upon identification. Early cases were linked to a high school, sports activities, a restaurant and social gatherings. As the outbreak progressed, cases were associated with household transmission, a daycare, healthcare settings and a workplace. The unadjusted SAR estimate among laboratory-confirmed cases was 24.4% for households and 19.3% for classroom exposures. When adjusted for other potential exposures, SAR estimates were 19.9% for households and 11.3% for classrooms.
Conclusion: This outbreak demonstrated how B.1.1.7 spread rapidly through a community with previously low COVID-19 transmission and few preventative PHMs in place. Implementation and compliance with school and community-based PHMs is critical for preventing transmission during outbreaks.
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory disease caused by severe acute respiratory coronavirus 2 (SARS-CoV-2). Variant of concern (VOC) refers to a SARS-CoV-2 lineage characterized by significant genetic mutations that affect its spread, severity, detection, prevention or treatment Footnote 1. The B.1.1.7 (Alpha) VOC was first identified in England in September 2020. The first cases in Canada (Ontario) were identified in December 2020 Footnote 2. The B.1.1.7 variant was associated with significantly increased rates of transmission Footnote 3 Footnote 4 and increased disease severity Footnote 5 Footnote 6 compared to non-VOC SARS-CoV-2.
One of the first community outbreaks of B.1.1.7 in Canada occurred in February 2021 among residents of Newfoundland and Labrador (NL)'s largest health authority, Eastern Regional Health Authority (Eastern Health), when Canadian health authorities had little experience with the prevention and control of VOCs. Evidence was accumulating about the effectiveness of personal public health measures (PHMs) such as handwashing, mask wearing and physical distancing, and societal PHMs such as quarantine Footnote 7.
Newfoundland and Labrador had observed only 408 cases of COVID-19 across the province from March 2020 to January 2021 (incidence: 78 per 100,000) Footnote 1. The outbreak of 577 laboratory-confirmed cases in the Eastern Health region occurred primarily in a census metropolitan area of 206,000 population Footnote 8 and did not extend into other parts of the province.
The outbreak was identified when a restaurant worker, with no known exposures, became symptomatic on February 4, 2021, and tested positive the following day. On February 6, patrons were advised to seek testing if they had attended the restaurant during the index case's incubation period Footnote 9. Mass testing within surrounding communities identified cases and clusters linked to other potential transmission settings.
This outbreak investigation aimed to describe the epidemiology, identify settings that likely contributed to spread and inform recommendations for PHMs. Evaluating the effectiveness of PHMs in various settings was out of scope.
Methods
Eastern Health led data collection and case finding via case interviews and contact tracing. Data sources included case and contact data from the provincial COVID-19 surveillance system, detailed case interview information, a school class roster and documentation of PHMs (e.g. web pages, press releases, and internal government documents).
The provincial definition of a laboratory-confirmed case Footnote 9 was a person with confirmation of infection with SARS-CoV-2 documented by:
- Detection of at least one specific gene target by a validated laboratory-based nucleic acid amplification test-based assay (e.g. real-time polymerase chain reaction or nucleic acid sequencing) performed at a community, hospital or reference laboratory (National Microbiology Laboratory or a provincial public health laboratory)
OR
- The detection of at least one specific gene target by a validated point-of-care nucleic acid amplification test that has been deemed acceptable to provide a final result (i.e. does not require confirmatory testing)
OR
- Seroconversion or diagnostic rise (at least fourfold or greater from baseline) in viral-specific antibody titre in serum or plasma using a validated laboratory-based serological assay for SARS-CoV-2
Outbreak cases resided in the Eastern Health region, met the provincial definition of a laboratory-confirmed case Footnote 9, had an episode date of February 1, 2021, to March 31, 2021 (inclusive), did not have an out-of-province travel history in the 14 days prior to the episode date, were not linked to a travel-associated case, and whose viral lineage was B.1.1.7 or not typed. Lineage assignments were determined in a subset of cases with sufficient viral load using pangolin v.2.2.2 Footnote 10, following whole genome sequencing on the Oxford Nanopore Technology GridION platform using a 1,200-base pair tiled amplicon scheme Footnote 11.
Cases with a positive lab test were interviewed by a public health nurse using a standardized form to identify potential exposures and contacts. The episode date for each case was the date of symptom onset or of specimen collection (if asymptomatic). Contacts were identified through case interviews as individuals who had close interactions with cases during the communicability period, starting 72 hours before the episode date.
Social network diagrams were used to explore connections between cases and identify clusters, defined as four or more cases epidemiologically linked to a setting where there was reasonable evidence of transmission (i.e. likely exposure to a case during their period of communicability).
Secondary attack rates (SAR) were calculated for households and school classrooms. The first laboratory-confirmed case in each household or classroom was considered the primary case, and any subsequent case was secondary if their onset occurred one to 14 days after the episode date of the primary case (or the last classroom exposure). Co-primary cases whose onset dates were the same as other primary cases were not considered secondary cases and were excluded from the SAR analysis. Household contacts of cases were identified in the provincial surveillance system. Classroom contacts were identified by the class roster, assuming perfect attendance. The SARs were calculated as the number of secondary cases divided by the number of contacts and represent the proportion of contacts who became cases. The unadjusted classroom SAR was calculated for all secondary cases in a classroom, and adjusted classroom SARs excluded school-associated cases who were secondary within their household or linked to other clusters.
An acquisition setting was assigned for each case, based on a hierarchy. Secondary cases in households were assumed to have acquired COVID-19 in their home, due to high proximity and duration of household contact compared to other settings. All other cases were categorized by their linkage to a cluster and its setting. No attempt was made to further distinguish the acquisition setting of cases linked to multiple clusters.
Public health measures were immediately implemented for containment, with incremental school closures and subsequently a province-wide lockdown beginning on February 12, including closure of all nonessential businesses and facilities, restrictions on gathering in groups over five, and restricted visitation to long-term care homes and assisted living facilities Footnote 12 Footnote 13.
Analyses were completed in R/R Studio, using data accessed April 18, 2021 Footnote 14.
Results
There were 577 laboratory-confirmed and 38 probable cases in this outbreak. Of the confirmed cases, 183 (32%) were identified as B.1.1.7; the remainder were locally acquired and assumed B.1.1.7 as there had been no known community transmission prior to the outbreak. The median age was 31 years and the highest proportion of cases were in the 15 to 19-year age group (29%); 293 (51%) were female and 140 (24%) were asymptomatic upon identification (Table 1). The last episode date was March 28, 2021 (Figure 1).
| Population tested, age (years) | Percent positivity (%) |
|---|---|
| Younger than 10 | 1.1 |
| 10–14 | 2.1 |
| 15–19 | 4.1 |
| 20–29 | 0.6 |
| 30–39 | 0.7 |
| 40–49 | 1.6 |
| 50–59 | 1.0 |
| 60 and older | 0.7 |
| All | 1.2 |
|
|
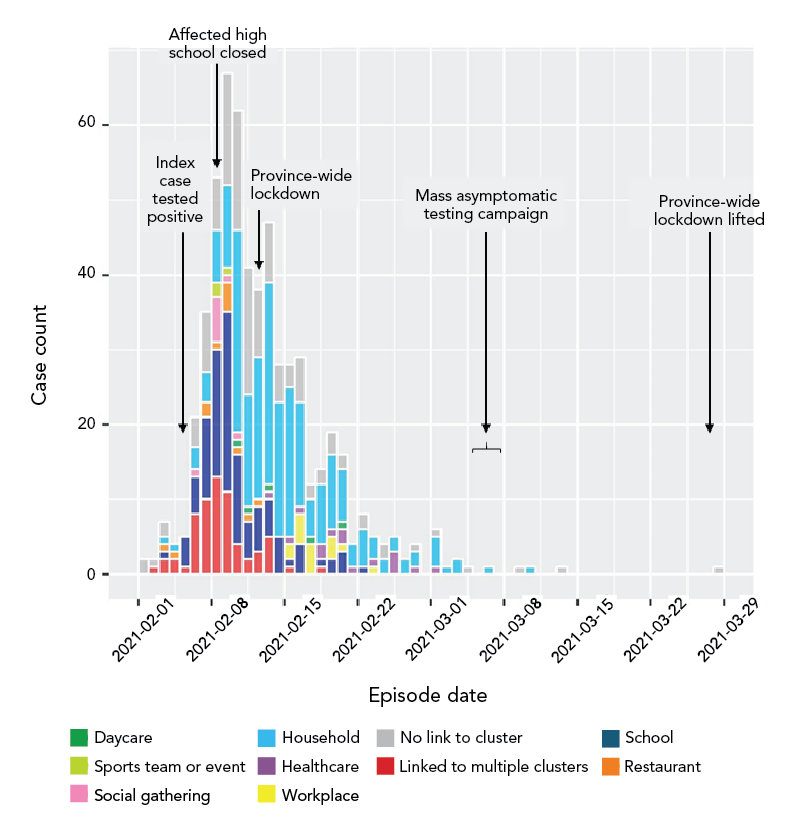
Figure 1 - Text description
This is a histogram showing the distribution of 557 confirmed cases in a COVID-19 outbreak that occurred in Newfoundland’s Eastern Health region from February 1, 2021 to March 31 2021. Cases are identified by episode date, meaning the date of symptom onset, or date of specimen collection for an asymptomatic case. The bars are colour coded by the acquisition setting of each case. The first and last cases respectively were February 1 and March 28, 2021. One peak occurred from February 8 to 10, 2021, with a maximum daily case count of 68. Labels show the dates when the index case tested positive (February 5), the affected high school was closed (February 8), the province-wide lockdown (February 12), and the mass asymptomatic testing campaign (March 5).
There were 15 hospitalizations, seven intensive care unit admissions and two deaths associated with this outbreak. Most hospitalized cases were females (67%); none were younger than 40 years (Table 2). The two deaths occurred in males who were 75 years or older. One breakthrough case was identified following two doses of a messenger ribonucleic acid (mRNA) vaccine.
| Case characteristic | Count | Percent (%) | |
|---|---|---|---|
| Age group (years) | Younger than 10 | 35 | 6 |
| 10–14 | 51 | 9 | |
| 15–19 | 166 | 29 | |
| 20–29 | 30 | 5 | |
| 30–39 | 51 | 9 | |
| 40–49 | 125 | 22 | |
| 50–59 | 63 | 11 | |
| 60 and older | 56 | 10 | |
| Sex | Female | 293 | 51 |
| Symptom status at time of identification | Asymptomatic | 63 | 11 |
| Presymptomatic | 77 | 13 | |
| Symptomatic | 437 | 76 | |
| Severe outcome(s) | Hospitalized | 15 | 3 |
| Admitted to intensive care unit | 7 | 1 | |
| Death linked to COVID-19 | 2 | Fewer than 1 | |
| Not reported | 561 | 97 | |
| Total | 577 | 100 | |
|
|||
Provincially, the cumulative number of COVID-19 tests increased by 55% from February 1 (n=142,398) to March 31 (n=221,205), as contacts and community members were encouraged to be tested following exposure, sometimes multiple times during the incubation period. The maximum daily percent positivity was 5.3%. Youth aged 15 to 19 years had the highest percent positivity (4.1%) during the outbreak period (Table 1).
The index case was likely not the primary case, given that they had no history of travel or contact with travellers. The suspected primary case was a rotational worker who returned on January 14, followed all applicable provincial guidance, and tested negative on day seven. The rotational worker isolated at home—but not from their household contacts (per public health direction), who were among the earliest outbreak cases according to episode dates and had multiple potential community exposures. The rotational worker was identified as a symptomatic case after their household contacts tested positive, with symptom onset more than 14 days after travelling.
The number of contacts per laboratory-confirmed outbreak case ranged from zero to 189. The median number of contacts was eight prior to implementation of the province-wide lockdown order on February 12; thereafter, cases had a median of three contacts. Among the eight cases who had more than 100 contacts, their ages ranged from five to 17 years.
Twenty-five clusters of four or more confirmed cases were associated with settings, events or locations where transmission may have occurred. Households were the most common acquisition setting (39%), followed by a senior high school (18%) (Table 3 and Figure 1). Approximately 21% of cases were not linked to a known cluster.
| Acquisition setting | Count | % |
|---|---|---|
| Household | 226 | 39 |
| No link to cluster | 122 | 21 |
| School | 106 | 18 |
| Linked to multiple clusters | 64 | 11 |
| Healthcare | 15 | 3 |
| Workplace | 15 | 3 |
| Restaurant | 12 | 2 |
| Social gathering | 9 | 2 |
| Daycare | 5 | 1 |
| Sports team or event | 3 | 1 |
| Total laboratory-confirmed cases | 577 | 100 |
|
||
Early cases in the outbreak were linked to school, sports activities/events, a restaurant and social gathering settings. As the outbreak progressed, cases were associated with household transmission, daycare, healthcare settings and a workplace (Figure 1).
A social network diagram (Figure 2) identified one large cluster and 25 smaller clusters of four or more cases. Figure 2 shows the connectivity of cases from contact tracing data and does not incorporate directionality or timing. Cases linked to multiple clusters (n=73) were centrally located among the largest clusters in the social network diagram; 68 (93%) were linked to the school, 44 (60%) to sports-related cluster(s), 36 (49%) to social gathering cluster(s) and 15 (21%) to the restaurant.
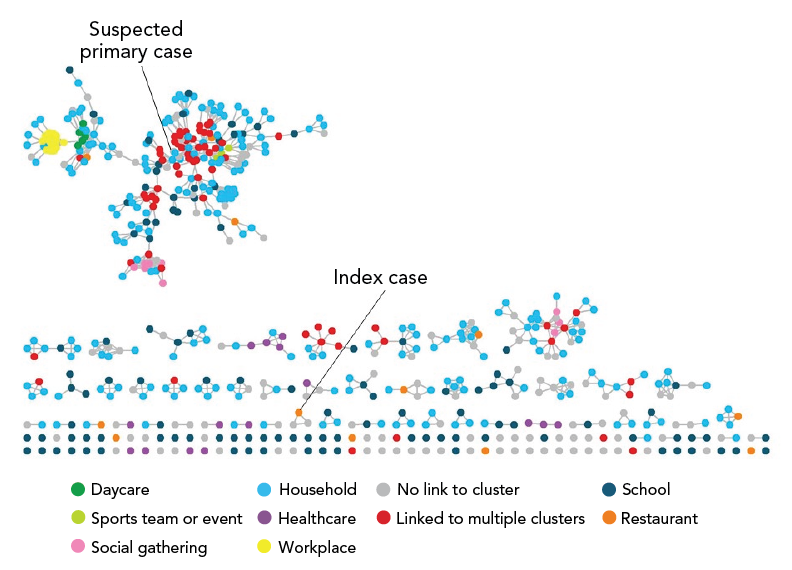
Figure 2 - Text description
This is a social network diagram showing all confirmed cases and linkages between cases who were identified as contacts during contact tracing. Cases are represented by dots, and lines connecting the dots depict connections, or contact, between cases. Dots are coloured according to their acquisition setting, including daycare, healthcare, household, linked to multiple clusters, no link to cluster, restaurant, school, social gathering, sports team or event, and workplace. There is one large cluster, and 25 smaller clusters of four or more cases.
The largest cluster of cases (n=183) was among individuals attending a senior high school, of which 167 (91%) were students and 16 (9%) were teachers or coaches. The number of COVID-19 cases per classroom ranged from zero to 19 (mean: 4.4).
Of all classroom groups in the school (n=298), 161 (54%) were exposed to a student or teacher case during their infectious period. Of the 945 students and teachers on the class list, 845 (89%) were exposed to an infectious student or teacher in their classroom, 17 (2%) were the primary cases in their classes and 163 (17%) became a confirmed case within 14 days following the last date of exposure in the classroom. Including all secondary classroom cases, the unadjusted classroom SAR was 19.3%. The adjusted classroom SAR was 17.8% when excluding those who were secondary cases within their household, and 11.6% when further excluding those linked to other clusters.
There were 308 households of two or more individuals that had at least one laboratory-confirmed outbreak case. Confirmed cases, probable cases and contacts were clustered by household in a social network diagram (Figure 3). The number of close household contacts per laboratory-confirmed outbreak case ranged from zero to 10 (median: 3). Transmission from a laboratory-confirmed primary household case to a laboratory-confirmed secondary household case appeared to have occurred in 119/308 (38.6%) households. The estimated household SAR was 24.4%. The adjusted household SAR was 28.5% when including probable cases and 19.9% when excluding secondary cases who were linked to other cluster types/settings.
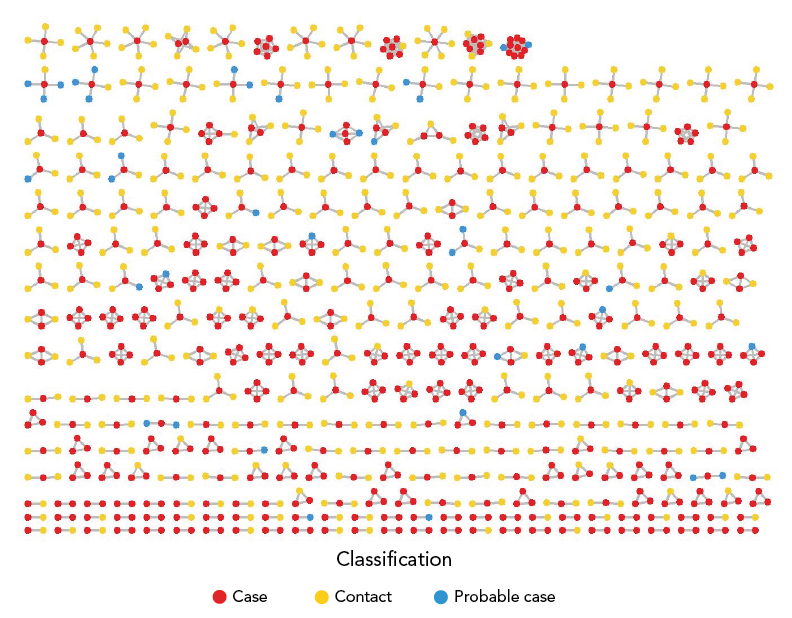
Figure 3 - Text description
This is a social network diagram showing 308 households of two or more individuals with one or more outbreak cases. Individuals are represented by dots, which are coloured by the individual’s classification as a case, probable case, or contact who did not become a case. Lines connecting the dots depict the identification of these individuals as household contacts during contact tracing. Clusters represent a household. Out of 308 households with at least one case, 119 (36.8%) households experienced secondary transmission within the household.
Discussion
Introduction of B.1.1.7 into Newfoundland (the island portion of one of Canada's least populous provinces) likely occurred through travel, given its relative geographic isolation, border quarantine measures and absence of prior evidence of community transmission. It is hypothesized that a rotational worker who returned from work and followed all applicable provincial guidance may have had a false-negative screening test on day seven, and/or may have had a longer incubation period (more than 14 days). Alternatively, it is possible that B.1.1.7 was circulating undetected within the community from an earlier introduction, and was identified upon reaching a susceptible population, resulting in rapid spread Footnote 15.
Major contributors to spread were identified as 1) the vulnerability of a highly connected, unvaccinated population including school-aged youth, 2) household transmission within the community and 3) asymptomatic or presymptomatic transmission.
At the time of B.1.1.7 introduction, most adults and all youth were unvaccinated. Less than 2% of the province's population had received one dose at the beginning of the outbreak period Footnote 16, while a phased approach to vaccine rollout was underway Footnote 17. Although PHMs were in place (e.g. mandatory masking and restrictions on occupancy of indoor settings) Footnote 18 Footnote 19, there were opportunities for community transmission in indoor settings such as restaurants, workplaces and private social gatherings.
Attendees of the senior high school had a high degree of connectedness due to in-person learning, no student or staff cohorting (i.e. students attended multiple classrooms with different teachers and students) and in-person extracurricular activities (e.g. sports tournaments). Non-medical masks (i.e. cloth masks or face coverings) were required in common areas but were not required in classrooms if students were distanced by at least one metre, and no requirements regarding ventilation and indoor air quality were in place for schools.
Evidence is conflicted regarding school-based transmission's contribution to community transmission Footnote 20 Footnote 21 Footnote 22 Footnote 23. Data and modelling show that without robust mitigation measures, school settings with an effective reproduction number above one can contribute to growth of an outbreak Footnote 24. The school setting was likely a driver of community transmission; however, the unadjusted classroom SAR of 19.3% decreased to 11.6% when excluding those linked to household exposure or other clusters, suggesting uncertainty about how directly school-associated cases can be linked with classroom transmission given other potential exposures.
The classroom SAR estimates are comparable to a May 2020 high school outbreak in Israel Footnote 25, but higher than in-school SAR estimates reported in meta or regional analyses Footnote 26 Footnote 27 Footnote 28, reflecting overdispersion in transmission Footnote 29. High school outbreaks of this size were unusual in Canada Footnote 30 Footnote 31; however, they have been documented elsewhere when PHMs were not in place or were not followed Footnote 25 Footnote 32. School sports have also been associated with secondary transmission in high and middle school settings in the United States Footnote 33.
Although mask-wearing (and other measures) is associated with reduced transmission in schools Footnote 34, the masking requirements in place at the school did not appear to curb transmission. Closing the affected school and implementing community-wide restrictions on indoor gatherings were key interventions in containing this outbreak. Improved ventilation could also have contributed to reducing the risk of transmission Footnote 35. Subsequent household transmission from school-associated cases in this outbreak is consistent with survey data from the United States that demonstrated increased odds of COVID-19-like illness within households with children in full-time in-person schooling Footnote 36.
Household settings accounted for the highest proportion of exposures among laboratory-confirmed cases (39%). Compared to other Canadian estimates for non-VOC COVID-19 household SARs (e.g. 20.2% in Ontario Footnote 37, and 14.7% in the Winnipeg Health Region Footnote 38), the estimated household SAR of 24.4% in this outbreak appears higher, which may reflect increased transmissibility of B.1.1.7. A similar SAR of 25.1% was observed among B.1.1.7 cases in Ontario Footnote 37.
In this outbreak, 24% of cases were asymptomatic or presymptomatic (i.e. developed symptoms after testing positive). The younger age groups (zero to nine and 10 to 19 years) had the highest proportion of asymptomatic or presymptomatic infection, which is consistent with evidence that children and adolescents are more commonly asymptomatic or have mild, non-specific symptoms Footnote 22 Footnote 39. Findings from this outbreak support asymptomatic testing as an important case finding intervention in outbreaks among children and youth.
Strengths and limitations
One strength of this investigation is the detailed analysis of potential transmission settings, possible because the outbreak was well contained in an area of low background transmission. There were several limitations to the study. First, the acquisition setting analysis was dependent on case interviews that may have been incomplete due to case volume, or subject to recall bias. Second, there may have been misclassification of COVID-19 lineage, since only 32% of cases were sequenced due to resource limitations. Similar to other jurisdictions Footnote 40, all locally acquired outbreak cases were managed thereafter as B.1.1.7. This potential misclassification means that when comparing attack rates in this outbreak to non-VOC outbreaks, the effect of B.1.1.7's increased transmissibility may be underestimated. Third, the analyses mostly excluded probable cases who tested negative, but clinical data suggests these symptomatic individuals who were contacts to laboratory-confirmed household cases were likely true cases Footnote 41. The SARs may have been underestimated due to the exclusion of probable cases. Fourth, although hypothesized, the primary case remains unknown.
Conclusion
This outbreak demonstrated how B.1.1.7 spread through an adolescent population and surrounding community with few preventative PHMs in place. Implementation and compliance with school- and community-based PHMs is critical to reduce the number of contacts and prevent transmission, particularly while vaccination coverage is low.
Authors' statement
AN, AM, AC, KP, JS, and KW contributed to conceptualization, analysis and interpretation of data. All authors contributed to drafting and revising the paper.
Competing interests
LG is a member of study teams that received funding from Roche Diagnostics and Seegene Inc. No other competing interests were declared.
Acknowledgements
We acknowledge the contributions of the Eastern Health Communicable Disease Control team, the Newfoundland and Labrador Centre for Health Information and the Department of Health and Community Services, and the Public Health Agency of Canada surge sites for diagnostic testing and whole genome sequencing support. The authors would like to thank R Needle and the Newfoundland and Labrador Provincial Public Health and Microbiology Laboratory for sharing data.
Funding
This work was supported by the Public Health Agency of Canada and Eastern Health.
References
- Footnote 1
-
Government of Canada. COVID-19: Outbreak update. Ottawa, ON: PHAC; 2022. [Accessed 2021 Aug 19]. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html
- Footnote 2
-
National Collaborating Centre for Infectious Diseases. Updates on COVID-19 Variants of Concern (VOC). Winnipeg, MB: NCCID; 2022. [Accessed 2021 May 31]. https://nccid.ca/covid-19-variants/
- Footnote 3
-
Campbell F, Archer B, Laurenson-Schafer H, Jinnai Y, Konings F, Batra N, Pavlin B, Vandemaele K, Van Kerkhove MD, Jombart T, Morgan O, le Polain de Waroux O. Increased transmissibility and global spread of SARS-CoV-2 variants of concern as at June 2021. Euro Surveill 2021;26(24):2100509. https://doi.org/10.2807/1560-7917.ES.2021.26.24.2100509
- Footnote 4
-
Davies NG, Abbott S, Barnard RC, Jarvis CI, Kucharski AJ, Munday JD, Pearson CA, Russell TW, Tully DC, Washburne AD, Wenseleers T, Gimma A, Waites W, Wong KL, van Zandvoort K, Silverman JD, Diaz-Ordaz K, Keogh R, Eggo RM, Funk S, Jit M, Atkins KE, Edmunds WJ; CMMID COVID-19 Working Group; COVID-19 Genomics UK (COG-UK) Consortium. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 2021;372(6538):eabg3055. https://doi.org/10.1126/science.abg3055
- Footnote 5
-
Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ 2021;372(579):n579. https://doi.org/10.1136/bmj.n579
- Footnote 6
-
Davies NG, Jarvis CI, Edmunds WJ, Jewell NP, Diaz-Ordaz K, Keogh RH; CMMID COVID-19 Working Group. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature 2021;593(7858):270–4. https://doi.org/10.1038/s41586-021-03426-1
- Footnote 7
-
Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, Li X, Xu W, Mesa-Eguiagaray I, Rostron J, Theodoratou E, Zhang X, Motee A, Liew D, Ilic D. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ 2021;375:e068302. https://doi.org/10.1136/bmj-2021-068302
- Footnote 8
-
Statistics Canada. Census Profile, 2016 Census. St. John's [Census metropolitan area], Newfoundland and Labrador and Newfoundland and Labrador [Province] (table). Ottawa, ON: StatCan; 2019. [Accessed 2021 Aug 19]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=CMACA&Code1=001&Geo2=PR&Code2=10&SearchText=St.%20John%27s&SearchType=Begins&
SearchPR=01&B1=All&GeoLevel=PR&GeoCode=001&TABID=1&type=0 - Footnote 9
-
Government of Newfoundland and Labrador. Department of Health and Community Services. Public Health Management of Cases and Contacts of COVID-19 in Newfoundland and Labrador. St. John's, NF: DHCS. [Updated 2021 March 2]. https://www.gov.nl.ca/covid-19/files/Public-Health-Management-of-Cases-and-Contacts-of-COVID-19-in-NL-Mar-2021.pdf
- Footnote 10
-
O'Toole Á, Scher E, Underwood A, Jackson B, Hill V, McCrone JT, Colquhoun R, Ruis C, Abu-Dahab K, Taylor B, Yeats C, du Plessis L, Maloney D, Medd N, Attwood SW, Aanensen DM, Holmes EC, Pybus OG, Rambaut A. Assignment of epidemiological lineages in an emerging pandemic using the pangolin tool. Virus Evol 2021;7(2):veab064. https://doi.org/10.1093/ve/veab064
- Footnote 11
-
Freed NE, Vlková M, Faisal MB, Silander OK. Rapid and inexpensive whole-genome sequencing of SARS-CoV-2 using 1200 bp tiled amplicons and Oxford Nanopore Rapid Barcoding. Biol Methods Protoc 2020;5(1):bpaa014. https://doi.org/10.1093/biomethods/bpaa014
- Footnote 12
-
Mullin M. Coronavirus variant puts N.L. back in lockdown; in-person voting in provincial election suspended. CBC News. 2021 Feb 12. https://www.cbc.ca/news/canada/newfoundland-labrador/newfoundland-labrador-election-lockdown-1.5913042
- Footnote 13
-
Government of Newfoundland and Labrador. Public Advisory: 50 New Cases of COVID-19 in Newfoundland and Labrador. St. John's, NL: Government of Newfoundland and Labrador; 2021. [Accessed 2021 Aug 19]. https://www.gov.nl.ca/releases/2021/health/0212n08/
- Footnote 14
-
R Foundation for Statistical Computing. R: A language and environment for statistical computing. Vienna (AT): R Core Team; 2021. https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006
- Footnote 15
-
Pekar J, Worobey M, Moshiri N, Scheffler K, Wertheim JO. Timing the SARS-CoV-2 index case in Hubei province. Science 2021;372(6540):412–7. https://doi.org/10.1126/science.abf8003
- Footnote 16
-
Government of Canada. COVID-19 vaccination in Canada. Ottawa, ON: Government of Canada; 2022. [Accessed 2022 Dec 18]. https://health-infobase.canada.ca/covid-19/vaccination-coverage/
- Footnote 17
-
Government of Newfoundland and Labrador. Newfoundland and Labrador Expecting More COVID-19 Vaccines to Arrive Over the Coming Weeks. St. John's, NL: Government of Newfoundland and Labrador; 2020. [Accessed 2022 Dec 18]. https://www.gov.nl.ca/releases/2020/exec/1223n06/
- Footnote 18
-
Government of Newfoundland and Labrador. Special Measures Order (General - Alert Level 2) (UPDATED). St. John's, NL: Government of Newfoundland and Labrador; 2020. [Accessed Dec 19, 2022]. https://www.gov.nl.ca/covid-19/files/SMO-General-Alert-Level-2-Updated-December-9-2020.pdf
- Footnote 19
-
Government of Newfoundland and Labrador. Special Measures Order (Masks). St. John's, NL: Government of Newfoundland and Labrador; 2020. [Accessed 2022 Dec 19]. https://www.gov.nl.ca/covid-19/files/Mandatory-Masking-045993-003.pdf
- Footnote 20
-
Lee B, Raszka WV Jr. COVID-19 Transmission and Children: The Child Is Not to Blame. Pediatrics 2020;146(2):e2020004879. https://doi.org/10.1542/peds.2020-004879
- Footnote 21
-
Ehrhardt J, Ekinci A, Krehl H, Meincke M, Finci I, Klein J, Geisel B, Wagner-Wiening C, Eichner M, Brockmann SO. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Württemberg, Germany. Euro Surveill 2020;25(36):2001587. https://doi.org/10.2807/1560-7917.ES.2020.25.36.2001587
- Footnote 22
-
US Centers for Disease Control and Prevention. CDC COVID-19 Science Briefs [Internet]. Science Brief: Transmission of SARS-CoV-2 in K-12 schools - Updated. Atlanta, GA: CDC; updated 2021. https://www.ncbi.nlm.nih.gov/books/NBK570438/
- Footnote 23
-
Amodio E, Battisti M, Kourtellos A, Maggio G, Maida CM. Schools opening and Covid-19 diffusion: evidence from geolocalized microdata. Eur Econ Rev 2022;143:104003. https://doi.org/10.1016/j.euroecorev.2021.104003
- Footnote 24
-
Gurdasani D, Alwan NA, Greenhalgh T, Hyde Z, Johnson L, McKee M, Michie S, Prather KA, Rasmussen SD, Reicher S, Roderick P, Ziauddeen H. School reopening without robust COVID-19 mitigation risks accelerating the pandemic. Lancet 2021;397(10280):1177–8. https://doi.org/10.1016/S0140-6736(21)00622-X
- Footnote 25
-
Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, Cayam R, Miskin I. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveill 2020;25(29):2001352. https://doi.org/10.2807/1560-7917.ES.2020.25.29.2001352
- Footnote 26
-
Aiano F, Mensah AA, McOwat K, Obi C, Vusirikala A, Powell AA, Flood J, Bosowski J, Letley L, Jones S, Amin-Chowdhury Z, Lacy J, Hayden I, Ismail SA, Ramsay ME, Ladhani SN, Saliba V. COVID-19 outbreaks following full reopening of primary and secondary schools in England: cross-sectional national surveillance, November 2020. Lancet Reg Health Eur 2021;6:100120. https://doi.org/10.1016/j.lanepe.2021.100120
- Footnote 27
-
Xu W, Li X, Dozier M, He Y, Kirolos A, Lang Z, Mathews C, Siegfried N, Theodoratou E; UNCOVER. What is the evidence for transmission of COVID-19 by children in schools? A living systematic review. J Glob Health 2020;10(2):021104. https://doi.org/10.7189/jogh.10.021104
- Footnote 28
-
Bark D, Dhillon N, St-Jean M, Kinniburgh B, McKee G, Choi A. SARS-CoV-2 transmission in kindergarten to grade 12 schools in the Vancouver Coastal Health region: a descriptive epidemiologic study. CMAJ Open 2021;9(3):E810–7. https://doi.org/10.9778/cmajo.20210106
- Footnote 29
-
Tupper P, Colijn C. COVID-19 in schools: mitigating classroom clusters in the context of variable transmission. PLOS Comput Biol 2021;17(7):e1009120. https://doi.org/10.1371/journal.pcbi.1009120
- Footnote 30
-
Public Health Ontario. Enhanced Epidemiologic Summary. COVID-19 in Ontario: Elementary and Secondary School Outbreaks and Related Cases, August 20, 2020 to April 24, 2021. Toronto, ON: PHO; 2021. https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/12/covid-19-school-outbreaks-cases-epi-summary.pdf?la=en
- Footnote 31
-
Covid Écoles Québec. https://www.covidecolesquebec.org/
- Footnote 32
-
Fontanet A, Tondeur L, Grant R, Temmam S, Madec Y, Bigot T, Grzelak L, Cailleau I, Besombes C, Ungeheuer MN, Renaudat C, Perlaza BL, Arowas L, Jolly N, Pellerin SF, Kuhmel L, Staropoli I, Huon C, Chen KY, Crescenzo-Chaigne B, Munier S, Charneau P, Demeret C, Bruel T, Eloit M, Schwartz O, Hoen B. SARS-CoV-2 infection in schools in a northern French city: a retrospective serological cohort study in an area of high transmission, France, January to April 2020. Euro Surveill 2021;26(15):2001695. https://doi.org/10.2807/1560-7917.ES.2021.26.15.2001695
- Footnote 33
-
Boutzoukas AE, Zimmerman KO, Benjamin DK, DeMuri GP, Kalu IC, Smith MJ, McGann KA, Koval S, Brookhart MA, Butteris SM. Secondary Transmission of COVID-19 in K-12 Schools: Findings From 2 States. Pediatrics 2022;149(12 Suppl 2):e2021054268K. https://doi.org/10.1542/peds.2021-054268K
- Footnote 34
-
Public Health Ontario. Mask-wearing in Children and COVID-19. What We Know So Far. Toronto, ON: PHO. [Accessed 2022 Dec19; revised 2022 Aug]. https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2021/08/wwksf-wearing-masks-children.pdf?sc_lang=en
- Footnote 35
-
Government of Canada. COVID-19: Guidance on indoor ventilation during the pandemic. Ottawa, ON: Government of Canada; 2022. [Accessed 2022 Dec 19]. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/guide-indoor-ventilation-covid-19-pandemic.html
- Footnote 36
-
Lessler J, Grabowski MK, Grantz KH, Badillo-Goicoechea E, Metcalf CJ, Lupton-Smith C, Azman AS, Stuart EA. Household COVID-19 risk and in-person schooling. Science 2021;372(6546):1092–7. https://doi.org/10.1126/science.abh2939
- Footnote 37
-
Brown KA, Tibebu S, Daneman N, Schwartz K, Whelan M, Buchan S. Comparative Household Secondary Attack Rates associated with B.1.1.7, B.1.351, and P.1 SARS-CoV-2 Variants. medRxiv 2021 Cold Spring Harbor Laboratory Press:2021.06.03.21258302.
- Footnote 38
-
Wilkinson K, Chen X, Shaw S. Secondary attack rate of COVID-19 in household contacts in the Winnipeg Health Region, Canada. Can J Public Health 2021;112(1):12–6. https://doi.org/10.17269/s41997-020-00451-x
- Footnote 39
-
Paquette D, Bell C, Roy M, Whitmore L, Currie A, Archibald C, MacDonald D, Pennock J. Laboratory-confirmed COVID-19 in children and youth in Canada, January 15-April 27, 2020. Can Commun Dis Rep 2020;46(5):121–4. https://doi.org/10.14745/ccdr.v46i05a04
- Footnote 40
-
Public Health Ontario. Enhanced Epidemiological Summary. COVID-19 Variants of Concern in Ontario: December 1, 2020 to May 9, 2021. Toronto, ON: PHO; 2021. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-variant-epi-summary.pdf?la=en
- Footnote 41
-
Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, Zambrano-Achig P, Del Campo R, Ciapponi A, Sued O, Martinez-García L, Rutjes AW, Low N, Bossuyt PM, Perez-Molina JA, Zamora J. False-negative results of initial RT-PCR assays for COVID-19: A systematic review. PLoS One 2020;15(12):e0242958. https://doi.org/10.1371/journal.pone.0242958
