At-a-glance – Traumatic brain injury management in Canada: changing patterns of care
Health Promotion and Chronic Disease Prevention in Canada
Deepa P. Rao, PhD; Steven McFaull, MSc; Wendy Thompson, MSc; Gayatri C. Jayaraman, PhD
https://doi.org/10.24095/hpcdp.38.3.05
Author reference:
Public Health Agency of Canada, Ottawa, Ontario, Canada
Correspondence: Deepa P. Rao, Public Health Agency of Canada, 785 Carling Avenue, Office 707B1, Ottawa, ON K1A 0K9; Tel: 613-867-8303; Fax: 613-941-2057; Email: deepa.rao@canada.ca
Abstract
Introduction: With growing awareness about traumatic brain injuries (TBI), there is limited information about population level patterns of TBI care in Canada.
Methods: We examined data from the Canadian Community Health Survey (years 2005, 2009, and 2014) among all respondents ages 12 years and older. TBI management characteristics examined included access to care within 48 hours of injury, point of care, hospital admission, and follow-up.
Results: We observed that many Canadians sought care within 48 hours of their injury, with no changes over time. We found a significant decline in the proportion of Canadians opting to visit an emergency department (p = 0.03, all ages), and a significant increase in youth opting to visit a doctor’s office (p < 0.01).
Conclusion: TBIs are an important and growing health concern in Canada. Care for such injuries appears to have shifted towards the use of health care professionals outside the hospital environment, including primary care doctors.
Keywords: traumatic brain injury, concussion, surveillance
Highlights
- Approximately 80% of Canadians reporting a traumatic brain injury (TBI) sought care within 48 hours of their injury.
- Examining trends over 10 years, there is a significant decline in the proportion of youth reporting a TBI who went to an emergency department for their care.
- Current data demonstrates that approximately 1 in 10 (interpret with caution) Canadians who report a TBI said they went to a doctor’s office for treatment following injury.
Introduction
Ms. Rowan Stringer was a high school rugby player who died following brain injury due to a concussion. Subsequent to her death, a strong initiative to raise awareness and improve treatments for concussions ultimately lead to the Royal Assent of the Rowan’s Law Advisory Committee Act in 2016.Footnote 1 At present, an ever-growing number of professionals across Canada are investing resources in preventing and addressing concussion and other traumatic brain injuries (TBI). A recent study reports that the incidence of TBIs is increasing in Canada: the annual percent change (APC) in TBI among those who reported any type of serious injury in the past 12 months was found to be 9.6% (95% CI: 8.2–11.0).Footnote 2
This so-called ‘invisible epidemic’ of TBIs is challenged by difficulties in accurate and timely diagnosis.Footnote 3 Whether or not a diagnosis is made, some of those with a TBI are at risk of persistent post-concussion syndrome (PPCS; symptoms that persist over a period of weeks or monthsFootnote 4,Footnote 5).With young athletes there is a risk (albeit small) of second impact syndrome (a subsequent concussion before a previous one has resolved).Footnote 6 Early identification of a TBI event can be important given that the consequence of misdiagnosis or faulty management is the possibility of disability or even death.Footnote 7,Footnote 8 With regard to where people seek care, the latest international sport-related concussion guidelines, as well as the Canadian guidelines, describe that when an individual is suspected to have a TBI they should be removed from play and assessed by a physician or licensed healthcare provider.Footnote 9,Footnote 10 Where individuals choose to seek care appears to be changing: a recent study reported a shift in pediatric TBI care from emergency departments (ED) towards primary and speciality providers.Footnote 11,Footnote 12
The objective of the present descriptive analysis is to provide population level estimates related to TBI care: whether individuals reporting receiving care within 48 hours after their injury, where they went for treatment, whether they were admitted to hospital, and whether they were receiving ongoing care. Given the dearth in national-level information regarding TBIs in Canada, a secondary objective of this study is to use questions available from existing national surveys to examine trends in TBI management over time.
Methods
Data sources
The Canadian Community Health SurveyFootnote 13 (CCHS) is a cross-sectional health survey of Canadians aged 12 years and older but not those living in nursing homes or long-term care facilities or on reserves, full-time members of the Canadian Armed Forces, or civilian residents of military bases. The survey was designed to derive estimates at the national and provincial levels and for 110 health regions in Canada. Self-reported data from the CCHS (years 2005, 2009 and 2014) were used to examine characteristics associated with TBI among the Canadian population aged 12 years (youth: ages 12 to 17 years, adults: ages 18 years and older).
Key variables
Cases of TBI were identified from those who reported an injury (all types of injury or ATI) “that occurred in the past 12 months and [that was] serious enough to limit [their] normal activities the day after the injury occurred,” and who identified this primary ATI as a TBI. The TBI care characteristics examined in the present analysis, which were only analyzed among those individuals who self-reported a TBI, are: (i) access to care within 48 hours of injury, (ii) point of care, (iii) admission to the hospital overnight, and (iv) ongoing follow-up care. These were selected from the limited survey questions available regarding care received, and do not reflect any recommendations regarding TBI management.
The ‘access to care within 48 hours of injury’ characteristic was selected based on a corresponding survey question meant to collect information on the time taken to access care; “Did [you] receive any medical attention for the injury from a health professional in the 48 hours following the injury?” Individuals who responded yes were then asked where they went for their care, which was used to examine ‘points of care’ such as the ED or other settings (an outpatient clinic, chiropractor’s office, community health center, hospital outpatient clinic, doctor’s office, or where the TBI occurred). Among those who indicated treatment within 48 hours, ‘hospitalization following injury’, was examined through the survey question, “Were you admitted to a hospital overnight?” Finally, information regarding ‘ongoing follow-up care, was captured at the time of data collection from a response to, “At the present time, are you getting follow-up care from a health professional because of this injury?”
Statistical analyses
We completed descriptive analyses using SAS Enterprise Guide version 5.1 (Cary, NC). Incidence and proportion estimates were weighted to reflect the Canadian household population and 95% confidence intervals were calculated using bootstrap re-sampling methods. Generalized logistic models were used to estimate annual percent change (APC) and significance was determined at p < 0.05.
Results
Roughly 4 in 5 individuals reporting a TBI sought medical care within 48 hours of their injury in 2014 (Table 1). While the majority of these individuals went to an ED, an analysis of the trend over time suggests this choice of point of care is significantly decreasing among youth (Table 1) (youth APC: −3.1%, 95% CI: −3.8 to −2.4, p < 0.001; adults APC: −2.6%, 95% CI: −5.4 to 0.3, p = 0.08; all ages APC: −2.7%, 95% CI: −5.1 to −0.2, p = 0.03). Although estimates from 2005 and 2009 were too rare to report, those from 2014 show that approximately 1 in 10 people with a TBI injury now seek care at a doctor’s office (11.5%, 95% CI: 5.2–17.8, interpret with caution). Examining trends over time, there is a significantly increasing trend of people reporting that they visited a doctor’s office among youth (youth APC: 0.3%, 95% CI: 0.2–0.3, p < 0.001; adults APC: 0.06%, 95% CI: −0.07 to 0.2, p = 0.34; all ages APC: 0.1%, 95% CI: 0.02–0.2, p = 0.02).
| 2005 | 2009 | 2014 | Annual Percent Change | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population | Incidence (%) | 95% CI | Population | Incidence (%) | 95% CI | Population | Incidence (%) | 95% CI | % | 95% CI | ||||||
| Received care within 48 hours of injury | All | 38 214 | 72.3 | 65.5-79.1 | 68 525 | 83.8 | 75.3-92.3 | 123 478 | 81.0 | 73.5-88.5 | 1.9% | -1.9 to 5.7 | ||||
| Youth | 11 596 | 68.7 | 56.1-81.4 | 13 127 | 70.6 | 51.3-89.9 | 27 447 | 75.2 | 63.3-87.1 | 2.2% | -1.8 to 6.2 | |||||
| Adults | 26 618 | 74.0 | 65.8-82.1 | 55 398 | 87.7 | 79.7-95.7 | 96 031 | 82.8 | 73.7-91.9 | 2.0% | -1.9 to 6.0 | |||||
| Treatment at ED |
All | 30 879 | 80.8 | 73.2-88.4 | 45 452 | 66.3 | 52.0-80.7 | 79 037 | 64.0 | 53.1-74.9 | -2.7% | -5.1 to -0.2 | ||||
| Youth | 9 396 | 81.0 | 68.3-93.7 | 9 158 | 69.8 | 49.9-89.6 | 16 878 | 61.5 | 45.4-77.6 | -3.1% | -3.8 to -2.4 | |||||
| Adults | 21 483 | 80.7 | 71.0-90.4 | 36 295 | 65.5 | 48.5-82.5 | 62 159 | 64.7 | 51.1-78.3 | -2.6% | -5.4 to 0.3 | |||||
Source: CCHS, 2005, 2009 and 2014. Abbreviations: CCHS, Canadian Community Health Survey; CI, confidence interval; ED, emergency department. Notes: The youth category reflects ages 12 to 17 years, and the adults category reflects ages 18 years and above. |
||||||||||||||||
Data from 2005 shows that 21.9% (95% CI: 12.7–31.2, interpret with caution) of Canadians reporting a TBI were admitted overnight, compared with 13.4% (95% CI: 5.5–21.3, interpret with caution) in 2014. A higher proportion of people who were hospitalized, than not hospitalized, reported that they were being followed-up by a health professional at the time of data collection (Figure 1). Independent of hospitalization history, the most recent data shows that the majority of individuals who reported a TBI in the past year were not receiving follow-up care from a health professional at the time they participated in the survey (youth: 86.8%, 95% CI: 77.8–95.9; adults: 69.3%, 95% CI: 57.6–80.9; all ages: 73.5%, 95% CI: 64.2–82.7).
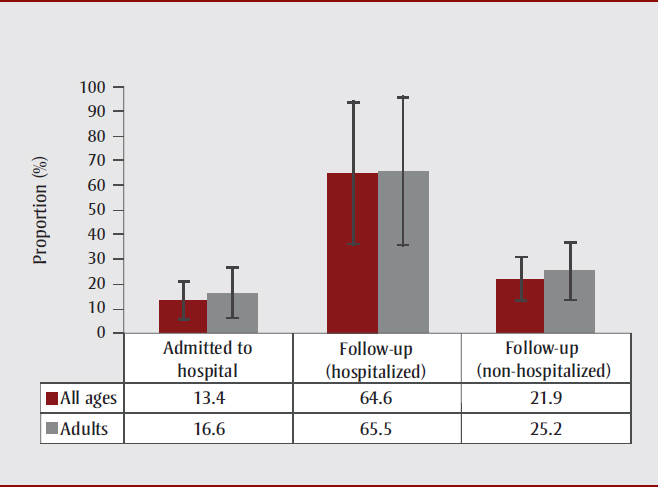
Source: CCHS, 2014.
Abbreviation: CCHS, Canadian Community Health Survey.
Notes: Estimates for youth were too unstable to report. Estimates for adults reflect individuals ages 18 years and above.
Estimates for traumatic brain injury are reported among all Canadians who reported any type of injury.
Estimates of self-reported follow-up care (hospitalized) refer to respondents who reported they were currently receiving follow-up care and who said they received treatment within 48 hours and were hospitalized.
Estimates of self-reported follow-up care (non-hospitalized) refers to respondents who reported they were currently receiving follow-up care and who said they received treatment within 48 hours and who reported that they were not hospitalized.
Figure 1 - Text Description
In this figure, we see that a higher proportion of people who were hospitalized (64.6% for all ages, 65.5% for adults), than not hospitalized (21.9% for all ages, 25.2% for adults), reported that they were being followed-up by a health professional at the time of data collection.
Discussion
Increasing rates of TBI have been reported both in CanadaFootnote 2 and in the U.S.Footnote 14 This prompts the question: where are Canadians going for their TBI care and what follow-up are they receiving? Examining these questions, we observed significant changes in where many Canadians were opting to receive care, namely that a doctor’s office was an important and emerging point of care and that there were declines in the proportion of youth opting to visit an ED. Our findings are similar to those observed in a recent study examining TBI care in a pediatric population in the U.S.Footnote 12,Footnote 15 Although changes in locations of care do not likely bear the same insurance concerns here in Canada as they may in the U.S.,Footnote 15 the ease and accessibility to primary care may nevertheless play a role. We did not observe any changes with regard to whether people sought health care advice within 24 hours of their TBI. The recent increasing trend in TBI has been attributed to factors such as improved data capture of mild TBI cases.Footnote 16,Footnote 17 A recent assessment of sport concussion and return-to-play guidelines,Footnote 18 however, suggests that, while research in this area is still preliminary, there is no evidence of an effect of these guidelines on TBI prognosis.Footnote 19 Future studies to examine factors associated with the increasing trend in TBIs, and to evaluate prognosis after TBI, should help to better inform evidence-based guidelines for TBI care.Footnote 19
Strengths and limitations
National surveys rely on self-reported information and do not capture fatal cases. The former provides for the potential of respondent bias and for diminished validity due to retrospective self-reported injury recall.Footnote 20 The lack of fatal cases limited the generalizability of our findings to only non-fatal cases. In the examination of follow-up care, the phrasing of the question limited the ability to detect cases where an individual had received such care but which had been completed by the time of the survey, or where the individual had yet to begin follow-up care. This question did, however, permit detection of differences between key groups; i.e., between those who were hospitalized versus those who were not. While limitations to the internal and external validity may exist, the better data capture of cases outside of those diagnosed within an ED is a strength of the present study. Furthermore, since most TBIs are not fatal (only about 3% of TBI cases areFootnote 14), our findings apply to the vast majority of TBIs in Canada.
Conclusion
There has been a significant increase in the incidence of reported TBIs over the past decade.Footnote 2 While these may have been influenced by a variety of factors, these trends call attention to how individuals manage their TBIs. Our observation of changes in where individuals reporting a TBI sought care is important, and the decreasing use of EDs among youth appears to be one such notable change in recent years. Building capacity among relevant professionals to identify TBIs would thus be beneficial given this changing landscape.
Conflicts of interest
All authors declare no conflicts of interest.
Author contributions and statement
All authors have read and approved of the content of this article. DPR was involved in data analysis, interpretation, and manuscript preparation. SM was involved in data interpretation as well as manuscript preparation and GJ and WT were involved in manuscript preparation.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.