Updated Recommendations on the Use of Herpes Zoster Vaccines
Download the alternative format
(PDF format, 1.29 MB, 76 pages)
Organization: Public Health Agency of Canada
Date published: 2018-08-30
Related Topics
Related Links
An Advisory Committee Statement (ACS)
National Advisory Committee on Immunization (NACI)
Table of Contents
- Preamble
- Summary of information contained in this NACI Statement
- I. Introduction
- II. Methods
- III. Epidemiology
- IV. Vaccine
- V. Economics
- VI. Recommendations
- VII. Research Priorities
- VIII. Surveillance Issues
- Tables
- List of Abbreviations
- Acknowledgments
- Appendices
- References
Preamble
The National Advisory Committee on Immunization (NACI) provides the Public Health Agency of Canada (PHAC) with ongoing and timely medical, scientific, and public health advice relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the systematic consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be systematically considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Over the coming years NACI will be refining methodological approaches to include these factors. Not all NACI Statements will require in-depth analyses of all programmatic factors. As NACI works towards full implementation of the expanded mandate, select Statements will include varying degrees of programmatic analyses for public health programs.
PHAC acknowledges that the advice and recommendations set out in this statement are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC's Policy on Conflict of Interest, including yearly declaration of potential conflict of interest.
Summary of information contained in this NACI Statement
The following highlights key information for immunization providers. Please refer to the remainder of the Statement for details.
What
Herpes Zoster Disease
- Primary varicella zoster virus (VZV) infection causes varicella (chickenpox), and reactivated infection results in herpes zoster (shingles). Herpes zoster (HZ) is characterized by neuropathic pain and dermatomal vesicular rash.
- Reactivation of VZV occurs with reduced cellular immune response associated with aging or immune suppression. HZ occurs most frequently among older adults (with steep increases in incidence occurring over 50 years of age) and immunocompromised persons.
- Post-herpetic neuralgia (PHN), which can be debilitating, is the most frequent complication of HZ. Similar to incidence of HZ and hospitalization due to HZ, the risk of PHN among HZ cases increases significantly with age.
Herpes Zoster Vaccines
- Two HZ vaccines are currently authorized for use in Canada in immunocompetent individuals ≥50 years of age. A live attenuated vaccine, Zostavax®II (Live Zoster Vaccine, LZV), has been authorized since 2008. A recombinant subunit vaccine, Shingrix®, (Recombinant Zoster Vaccine, RZV) has been authorized in October 2017. Both vaccines have been shown to be safe, immunogenic, and reduce the incidence of HZ and PHN.
- Vaccine efficacy (VE) against HZ decreases with age and over time since vaccination with LZV whereas VE of RZV remains higher and appears to decline more slowly than VE of LZV across all age groups.
- RZV VE against incident HZ and PHN in the three years post-immunization appears to be double that observed for LZV overall.
- RZV VE against incident HZ in the four years post immunization remains consistent, with no significant decreases observed over time; in contrast, significant waning of protection has been observed one-year post immunization with LZV.
- Differences in RZV four-year VE against incident HZ are non-significant across different age groups; in contrast, LZV is significantly less effective in adults over 70 years of age compared to adults 50-59 years of age.
- Due to the adjuvant in RZV which induces a high cellular immune response to help address the natural age-related decline in immunity, this vaccine is more reactogenic than LZV.
- Both vaccines are cost effective in those 50 years of age and older compared to no vaccination, especially in those 65-79 years of age. RZV is more cost effective than LZV.
Who
NACI makes the following recommendations for public health program level and individual level decision-making. (While in this statement, the recommendations for both levels of decision-making are essentially the same, the rationale and context are somewhat different.)
For Public Health Program Level Decision-MakingFootnote *, NACI recommends that:
- RZV should be offered to populations ≥50 years of age without contraindications. (Strong NACI Recommendation, Grade A evidence)
- RZV should be offered to populations ≥ 50 years of age without contraindications who have previously been vaccinated with LZV. (Strong NACI Recommendation, Grade A Evidence)
- Re-immunization with 2 doses of RZV may be considered at least one year after LZV (Discretionary NACI Recommendation, Grade I evidence)
- RZV should be offered to populations ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation, Grade B Evidence)
- Immunization with 2 doses of RZV may be considered at least one year after the HZ episode (Discretionary NACI Recommendation, Grade I evidence)
- LZV may be considered for immunocompetent populations ≥50 years of age without contraindications when RZV vaccine is contraindicated, unavailable or inaccessible. (Discretionary NACI Recommendation, Grade A evidence).
- RZV (not LZV) may be considered for immunocompromised adults ≥50 years of age. (Discretionary NACI Recommendation, Grade I evidence). NACI will monitor results from ongoing trials in those who are immunocompromised and will reassess recommendations as evidence becomes available.
- Footnote *
-
For public health program level decision-making, NACI recognizes that there are differences in operational contexts across Canada and suggests that provinces and territories may wish to refer to the Management Options Table 10 to consider differences between age cohorts (e.g. with respect to epidemiology and cost-effectiveness) if prioritization of targeted immunization programs is required for implementation.
For Individual Level Decision-MakingFootnote **, NACI recommends that:
- RZV should be offered to individuals ≥50 years of age without contraindications. (Strong NACI Recommendation, Grade A evidence)
- RZV should be offered to individuals ≥ 50 years of age without contraindications who have previously been vaccinated with LZV. (Strong NACI Recommendation, Grade A Evidence)
- Re-immunization with 2 doses of RZV may be considered at least one year after LZV (Discretionary NACI Recommendation, Grade I evidence)
- RZV should be offered to individuals ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation, Grade B Evidence)
- Immunization with 2 doses of RZV may be considered at least one year after the HZ episode (Discretionary NACI Recommendation, Grade I evidence)
- LZV may be considered for immunocompetent individuals ≥50 years of age without contraindications when RZV vaccine is contraindicated, unavailable or inaccessible. (Discretionary NACI Recommendation, Grade A evidence).
- RZV (not LZV) may be considered for immunocompromised adults ≥50 years of age based on a case-by-case assessment of the benefits vs risks. (Discretionary NACI Recommendation, Grade I evidence). NACI will monitor results from ongoing trials in those who are immunocompromised and will reassess recommendations as evidence becomes available.
How
RZV
- RZV is administered intramuscularly as a two dose schedule, 2-6 months apart. To improve coverage of the 2nd dose (e.g. by simultaneous administration with another vaccine), a 0, 12-month schedule may be considered based on evidence of an acceptable safety profile and robust anti-gE immune response.
- RZV is contraindicated in those with a known hypersensitivity to any of the vaccine components. There is limited data in immunocompromised individuals, and no data in pregnancy and those who are breastfeeding, so RZV should be used with precaution in these populations at this time.
- In general, inactivated vaccines may be administered concomitantly with, or at any time before or after, other inactivated vaccines or live vaccines protecting against a different disease. For concomitant parenteral injections, different injection sites and separate needles and syringes should be used. RZV may be given at the same time as unadjuvanted seasonal influenza vaccine. Studies of co-administration with pneumococcal 23-valent polysaccharide vaccine (Pneu-P-23) and Boostrix®(Tetanus, low concentration diphtheria and acellular pertussis vaccine; Tdap), are ongoing. Studies of co-administration with adjuvanted seasonal influenza vaccine (Fluad®) have not been conducted.
LZV
- LZV is administered subcutaneously as a single dose.
- LZV is a live vaccine and is therefore contraindicated in pregnancy and immunocompromised individuals. It is also contraindicated in individuals with a known hypersensitivity to any vaccine component. Precaution should be used when deciding to administer it to those who are breastfeeding.
- In general, live vaccines given by the parenteral route may be administered concomitantly with other vaccines. For concomitant parenteral injections, different injection sites and separate needles and syringes should be used. If not administered concomitantly, a minimum interval of 4 weeks should be maintained between two live parenteral vaccines. LZV may be given at the same time as Pneu-P-23 based on evidence of no decrease in efficacy or increase in adverse events; no safety concerns or interference with immune response have arisen with co-administration with inactivated influenza vaccine.
Why
- HZ is painful and can have severe complications, including long lasting nerve pain.
- The incidence and severity of HZ and its complications increase with age.
- Nearly one in three Canadians develops HZ during their lifetime.
- HZ vaccines are safe, immunogenic, effective and cost-effective in preventing HZ and PHN.
Introduction
I.1 Objective of this statement
The need for this updated National Advisory Committee on Immunization (NACI) Advisory Committee Statement on the Use of Herpes Zoster (HZ) Vaccines was triggered by evidence on a newly authorized Recombinant subunit Zoster Vaccine (RZV) vaccine, Shingrix®, indicated for the prevention of HZ in individuals 50 years of age and older. The primary objective of this statement is to review current evidence and develop guidance on the use of Shingrix®, as well as to provide guidance on whether the previously authorized Live Zoster Vaccine (LZV), Zostavax®II, and/or the recently authorized RZV should be offered to Canadians ≥50 years of age and older:
- at a population-level, in publicly funded immunization programs
- at an individual-level, to individuals wishing to prevent HZ, or by clinicians wishing to advise individual patients about preventing HZ, with vaccines that may not currently be included in public health immunization programs.
Specific questions investigated to support the objective include:
- Is the RZV vaccine (vs placebo and vs LZV vaccine) immunogenic, efficacious, safe, cost-effective?
- In which age groups should HZ vaccines be offered?
- What are the relative merits of RZV vs LZV?
- Should RZV be offered to those who have previously been vaccinated with LZV? If offered, what should the interval between the doses be?
- Should RZV be offered to those who have had a previous episode of HZ? If offered, what should the interval between the HZ episode and vaccination be?
NACI will review the evidence on HZ vaccines in those who are immunocompromised in a separate advisory committee statement. Studies on RZV vaccine immunogenicity, safety and efficacy in various immunocompromised groups ≥18 years of age are ongoing at the time of NACI deliberations. While RZV is not contraindicated in those who are immunocompromised, there is no indication for the use of RZV in those <50 years of age in Canada, and evidence in immunocompromised populations is limited at this time. Preliminary, non-peer-reviewed evidence presented in conference abstracts of RZV in certain immunocompromised groups suggests no significant safety or immunogenicity concerns. NACI will continue to review the evidence as it evolves and reassess recommendations.
I.2 Overview of evidence-based recommendations on the use of HZ vaccines in this statement
Based on evidence reviewed and summarized in this advisory committee statement, NACI makes the following recommendations on the use of previously recommended LZV and newly authorized RZV vaccine in populations (Table 1) and individuals (Table 2). (While in this statement, the recommendations for both public health level and individual level decision-making are essentially the same, the rationale and context are somewhat different.)
(Please note:
- A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present.
- A discretionary recommendation may be considered for some populations/individuals in some circumstances. Alternative approaches may be reasonable.
Please see Table 11 for a more detailed explanation of strength of NACI recommendations and grade of the body of evidence.)
| NACI Recommendation (Strength of Recommendation) |
Grade of Evidence supporting recommendation |
|---|---|
| RZV | |
| 1. NACI recommends that RZV should be offered to populations ≥ 50 years of age without contraindications. (Strong NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence) |
| 2. NACI recommends that RZV should be offered to populations ≥ 50 years of age without contraindications who have previously been vaccinated with LZV. (Strong NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence). |
| 2a. NACI recommends that for adults ≥ 50 years of age who have previously been immunized with LZV, re-immunization with 2 doses of RZV may be considered at least one year after LZV. (Discretionary NACI Recommendation; based on expert opinion) |
NACI concludes that there is insufficient evidence to recommend an interval between LZV and RZV (Grade I Evidence). |
| 3. NACI recommends that RZV should be offered to populations ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation) |
NACI concludes that there is fair evidence to recommend immunization (Grade B Evidence). |
| 3a. NACI recommends that for adults ≥ 50 years of age who have had a previous episode of HZ, immunization with 2 doses of RZV may be considered at least one year after the HZ episode. (Discretionary NACI Recommendation; based on expert opinion) |
NACI concludes that there is insufficient evidence to recommend an interval between a previous episode of HZ and vaccination with RZV (Grade I Evidence). |
| LZV | |
| 4. NACI recommends that LZV may be considered for immunocompetent populations ≥ 50 years of age without contraindications when RZV is contraindicated or unavailable. (Discretionary NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence) |
| RZV vs LZV in Immunocompromised Populations | |
| 5. NACI recommends that RZV (not LZV) may be considered for immunocompromised adults ≥ 50 years of age. (Discretionary NACI Recommendation; based on expert opinion) NACI will review the evidence as it evolves and reassess recommendations. |
NACI concludes that there is insufficient evidence at this time to recommend immunization (Grade I evidence) |
|
|
| NACI Recommendation (Strength of Recommendation) |
Grade of Evidence supporting recommendation |
|---|---|
| RZV | |
| 1. NACI recommends that RZV should be offered to individuals ≥ 50 years of age without contraindications. (Strong NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence) |
| 2. NACI recommends that RZV should be offered to individuals ≥ 50 years of age without contraindications who have previously been vaccinated with LZV. (Strong NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence). |
| 2a. NACI recommends that for adults ≥ 50 years of age who have previously been immunized with LZV, re-immunization with 2 doses of RZV may be considered at least one year after LZV. (Discretionary NACI Recommendation; based on expert opinion) |
NACI concludes that there is insufficient evidence to recommend an interval between LZV and RZV (Grade I Evidence). |
| 3. NACI recommends that RZV should be offered to individuals ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation) |
NACI concludes that there is fair evidence to recommend immunization (Grade B Evidence). |
| 3a. NACI recommends that for adults ≥ 50 years of age who have had a previous episode of HZ, immunization with 2 doses of RZV may be considered at least one year after the HZ episode. (Discretionary NACI Recommendation; based on expert opinion) |
NACI concludes that there is insufficient evidence to recommend an interval between a previous episode of HZ and vaccination with RZV (Grade I Evidence). |
| LZV | |
| 4. NACI recommends that LZV may be considered for immunocompetent individuals ≥ 50 years of age without contraindications when RZV is contraindicated unavailable, or inaccessible. (Discretionary NACI Recommendation) |
NACI concludes that there is good evidence to recommend immunization (Grade A Evidence) |
| RZV vs LZV in Immunocompromised Individuals | |
| 5. NACI recommends that RZV (not LZV) may be considered for immunocompromised adults ≥ 50 years of age based on a case-by-case assessment of benefits vs risks. (Discretionary NACI Recommendation; based on expert opinion) NACI will review the evidence as it evolves and reassess recommendations. |
NACI concludes that there is insufficient evidence at this time to recommend immunization (Grade I evidence) |
|
|
No studies on RZV in individuals with a previous episode of Herpes Zoster Ophthalmicus (HZO) have been conducted.Footnote 1
I.3 Background of HZ vaccines, immunization programs, and recommendations in Canada
In Canada, a live-attenuated vaccine against HZ (LZV) was initially approved for use among persons 60 years and older by the Biologics and Genetic Therapies Directorate (BGTD) of Health Canada in August 2008, and in May 2011 it was approved for use in those age 50 years and older. In 2008, only a freezer stable product (Zostavax®) was available, however in 2011, a refrigerator-stable product (Zostavax®II) replaced it.
In 2010, the National Advisory Committee on Immunization (NACI) published an advisory committee statement recommending the only available vaccine at the time (LZV) for the prevention of herpes zoster and its complications in persons 60 years and older without contraindications (e.g. immunocompromise) based on what the committee considered to be good evidence. In 2014, NACI published an updated advisory committee statement recommending that the vaccine may be used in patients aged 50-59 years based on good evidence (this recommendation was unchanged from the previous statement, but the level of evidence was upgraded as the vaccine was subsequently shown to be both safe and efficacious in this age group. However, as the duration of protection from the vaccine was unknown beyond 5 years, it was uncertain whether vaccination at younger ages would provide ongoing protection at older ages when the incidence of HZ is highest.) In the 2014 recommendations, NACI also concluded that there was insufficient evidence to recommend for or against the administration of HZ vaccine in individuals with a history of HZO. Although causality was difficult to determine, cases of HZO had been reported after administration of HZ vaccine.
NACI's recommendations in the 2010 and 2014 Advisory Committee Statements on the Herpes Zoster vaccine authorized for use in Canada at the time (LZV) are summarized in Table 3.
| Population Scenarios | 2010 NACI Recommendations | 2014 NACI Recommendations |
|---|---|---|
| ≥60 year olds | Recommended (Grade A evidence) | Recommended (Grade A evidence) |
| 50-59 year olds | May be used (Grade B evidence) | May be used (Grade A evidence) |
| Previous episode of HZ | No recommendation (Grade I evidence) | May be administered (Grade B), at least one year after (expert opinion) - 2014 |
| Previous episode of HZO | No recommendation (Grade I evidence) | |
| Prior history of chickenpox or documented prior varicella infection | Recommended (Grade A evidence) | |
| Immunocompromised | ||
| - HIV, post-organ or Hematopoietic Stem Cell Transplantation (HSCT) or in those receiving high dose corticosteroids, chemotherapy or immune suppressing medications | No recommendation (Grade I evidence) | |
| - low dose immunosuppressives, anti-TNFs on a case-by-case basis | May be administered (Grade B evidence) | |
| Co-administration | ||
| - with Trivalent Influenza Vaccine (TIV) | At different site, Recommended (Grade A evidence) | |
| - with Pneu-P-23 | ≥4 weeks apart, Recommended (Grade B evidence) | Concomitantly at different site, Recommended (Grade A evidence) |
In May 2014, the Canadian Immunization Committee recommended routine offering of LZV to immunocompetent adults aged 60 to 65 years and older without contraindications on the basis of the epidemiology of varicella zoster virus, zoster vaccine characteristics, disease modeling and economic analysis, as well as on the feasibility and acceptability of zoster immunization programs.Footnote 2
The live attenuated HZ vaccine has been available for private purchase, however until recently, no publicly funded immunization program has been offered in Canada. In September 2016, Ontario was the first jurisdiction to provide HZ vaccine through a publicly funded program to individuals 65-70 years of age.
In October 2017, a recombinant subunit HZ vaccine (RZV) containing VZV glycoprotein E and the AS01B adjuvant system was authorized for use in Canada.
HZ is not a reportable disease in Canada, and there are no established national targets for disease reduction or vaccination coverage goals for this vaccine preventable disease at this time.
I.4 Background of HZ vaccines, immunization programs, and recommendations worldwide
LZV was authorized for use for prevention of HZ in the United States in 2006 and recommended by the Advisory Committee on Immunization Practices (ACIP) in 2008 for immunocompetent adults 60 years of age and olderFootnote 3 . In 2006, the European Medicines Agency (EMEA) issued a marketing authorization for LZV for routine vaccination in individuals aged 60 and overFootnote 4 , and expanded its recommendation to include individuals aged 50 and older in 2007.Footnote 5 Starting in 2013, the United Kingdom National Health Service (NHS)Footnote 6 began offering LZV to individuals between 70 and 79 years of age.
Currently, the new RZV vaccine is authorized for use in Canada, the United States, Europe and Japan. On October 25, 2017, the ACIP in the United States recommended the use of RZV vaccine preferentially over LZV vaccine in immunocompetent adults age 50 years and older, including those who previously received LZV vaccine. ACIP has not yet made a recommendation for the use of RZV vaccine specifically for immunocompromised populations. LZV remains a recommended vaccine for prevention of HZ in immunocompetent adults 60 years and older in the United States.Footnote 7
II. Methods
In brief, the broad stages in the preparation of a NACI advisory committee statement are:
- Knowledge synthesis (retrieve and summarize individual studies, rank the level [i.e. study design] and quality of the evidence which are summarized in the Summary of Evidence Tables in the Appendix)
- Synthesis of the body of evidence of benefits and harms, considering the quality of the evidence and magnitude of effects observed
- Translation of evidence into a recommendation.
Further information on NACI's standard evidence-based methododology is available.
For this advisory committee statement, NACI reviewed key questions for the evidence reviews as proposed by the Herpes Zoster Working Group (HZWG), including such considerations as the burden of illness and the target populations; safety, immunogenicity, efficacy, effectiveness of the HZ vaccines; vaccine schedules; economics, and other aspects of the overall immunization strategy. For the purposes of this Statement, separate strategies were used to compile evidence on the vaccine characteristics, burden of disease, and programmatic factors for HZ vaccines, which were then included in an overall knowledge synthesis by PHAC technical staff (SI, MT, OB, KE, MD, SDB) and contractor JH, supervised by the HZWG.
- In order to assess the burden of disease, key literature was synthesized by MD in the Epidemiology section and supplemented with figures from MB based on administrative data from several Canadian jurisdictions. There is currently no surveillance program in place in Canada to monitor HZ incidence, PHN, or HZ ophthalmicus.
- In order to assess vaccine efficacy, effectiveness, and safety, a collaboration was initiated between PHAC and the Canadian Institutes of Health Research (CIHR) Drug Safety and Effectiveness Network (DSEN). Within DSEN, the Methods and Applications Group for Indirect Comparisons (MAGIC) led a systematic review of published and unpublished studies on the safety, efficacy, and effectiveness of LZV and RZV vaccines.
- The HZ WG provided input and guidance on the study eligibility criteria as defined by the Population, Intervention, Comparator, Outcomes and Study design (PICOS) framework (P - adults 50 years and greater, I - HZ vaccines, C - sham (or placebo vaccine), no treatment, or another HZ vaccine, O - vaccine efficacy, effectiveness, safety and quality-of-life, S - RCTs and non-randomized studies) and the literature search strategy. The literature search strategy was developed by a librarian (EC) and peer-reviewed by another librarian (JM) using the Peer Review of Electronic Search Strategies (PRESS) checklist. MEDLINE, EMBASE, and the Cochrane Library were searched from inception to January 19, 2017 and supplemented with a grey literature search (i.e. difficult to locate and unpublished documents).
- Retrieved citations were independently screened for eligibility by pairs of MAGIC team members (WZ, RC, PK, VN, MG, RW, JPS) independently upon completion of a team calibration exercise to establish inter-rater agreement. Each relevant full text article was assessed for eligibility using a similar process. Once a list of studies that met the eligibility criteria (i.e. studies investigating efficacy, effectiveness or safety of either LZV or RZV vaccines in adults aged 50 years or older) was compiled by MAGIC, data were abstracted from each eligible article and appraised for risk of bias by two team members independently (WZ, RC, PK, VN, MG, RW, JPS) from the MAGIC team.
- Risk of bias was assessed using The Cochrane Collaboration Risk of Bias tool for randomized controlled trials, the Newcastle Ottawa Quality Assessment Scale for cohort studies and case-control studies, and the EPOC Risk of Bias tool for nonrandomized controlled trials. Studies were also appraised according to the standard NACI methodology for inclusion in evidence tables.
- In addition to the studies selected and appraised by MAGIC, the HZ WG included an additional 11 studies on safety and efficacy that were initially screened out by the MAGIC team as per the PICO criteria due to the lack of a comparator group. These additional studies were appraised for quality using the standard NACI methodology and downgraded where appropriate due to the lack of comparator groups. All included studies on efficacy and safety were extracted into evidence tables and synthesized into a narrative summary by technical staff at PHAC (SDB, OB, MT).
- In order to assess the immunogenicity of HZ vaccines, a literature review was contracted by PHAC, supervised by the NACI HZWG, including summary tables with ratings of the quality of the evidence using NACI's methodological hierarchy (Tables 12 and 13) as per standard NACI methodology. The search strategy was developed with a Health Canada librarian (LG), and a search was performed on June 5, 2017 and updated on October 10, 2017 based on the following research question: P - adults 50 years and greater, I - HZ vaccines, C - sham (or placebo vaccine), no treatment, another HZ vaccine, or no comparator, O - humoral immunity and/or cell-mediated immunity (CMI).
- In order to assess the cost effectiveness of different HZ vaccination strategies, an economic analysis was conducted by MD, ZZ, CS, PDW, VG, RA, EB, MB, under the supervision and guidance of the HZWG. The results of this model were presented to the HZ WG on January 12, 2018, and this evidence was synthesized in narrative summary by PHAC technical lead KE. Specific methods for the economic model can be found in the Economics section of this Statement.
Following a review of the synthesized body of evidence, proposed recommendations for vaccine use were developed. The Working Group chair and PHAC technical leads presented the evidence and proposed recommendations to NACI on February 7, 2018. Following thorough review of the evidence and consultation at the NACI meeting on February 7, 2018, the committee voted on specific recommendations. The description of relevant considerations, rationale for specific decisions, and knowledge gaps are described in the text.
For the analysis of vaccine safety, efficacy, effectiveness, and immunogenicity, results are presented for the "general population". However, it should be noted that the studies informing these sections may include both immunocompetent and immunocompromised subjects, but many of the studies did not stratify the data sufficiently to allow separate analyses.
Studies specifically investigating immunocompromised populations were not included in the narrative synthesis of the body of evidence. Although these studies were not excluded from the literature reviews and are presented in evidence tables, they were not explicitly discussed in this Statement because NACI determined that specific recommendations for immunocompromised populations will be developed at a later date when more evidence is available. Several clinical trials with the RZV vaccine are currently underway in a range of immunocompromised populations including individuals with solid tumors, solid organ transplant recipients, and hematopoetic stem cell transplant recipients. NACI will continue to monitor the evidence as it evolves and perform another knowledge synthesis for this population. NACI will issue recommendations based on forthcoming studies in addition to the specific studies identified in the present literature reviews.
III. Epidemiology
III.1 Disease Description
HZ, or shingles, is a painful vesicular eruption, typically affecting a single dermatome. HZ develops due to the reactivation in the dorsal root ganglia of latent varicella zoster virus (VZV) from previous primary varicella infection when VZV-specific immunity weakens (most commonly due to age or immunocompromise). Although less contagious than primary varicella, persons with acute HZ can transmit VZV to susceptible contacts, with transmission predominantly occurring via direct contact with vesicular lesions.Footnote 8 Footnote 9 Footnote 10
Up to 40% of persons with acute HZ report at least one complication from the illness.Footnote 11 Footnote 12 Footnote 13 Common complications are potentially severe, and include postherpetic neuralgia (PHN), a prolonged and often debilitating pain following HZ infection that occurs in approximately 20% of HZ casesFootnote 14 Footnote 15 Footnote 16 , and HZ ophthalmicus (HZO), where VZV reactivation occurs in the ophthalmic division of the trigeminal nerve in 10-15% of HZ casesFootnote 17 , and can cause severe chronic pain, facial scarring, and/or loss of vision. Less common but severe HZ complications include central nervous system infections, nerve palsies including Ramsay-Hunt Syndrome, neuromuscular diseases including Guillain-Barre Syndrome, pneumonia, hepatitis and secondary bacterial infections.Footnote 18 Footnote 19 Footnote 20 In general, HZ complications are more common and may be more severe among persons who are older and/or immunocompromisedFootnote 14 Footnote 17 Footnote 21 ; children without comorbidities are less likely to experience HZ complications.Footnote 22 Footnote 23
III.2 Disease Distribution
In the absence of HZ vaccination, nearly one in three Canadians developed HZ during their lifetimeFootnote 24 , and 130,000 HZ cases, 17,000 cases of PHN, and 20 deaths from HZ were estimated to occur in Canada annually.Footnote 11 Age is the major risk factor for development of HZ, with HZ incidence sharply increasing by age among persons 50 years of age and older.Footnote 17 Footnote 25 Footnote 26 Footnote 27 Footnote 28 Footnote 29 HZ incidence also varies by sex, with females having a roughly 1.3 times greater risk of HZ relative to males.Footnote 30
Age is also the predominant risk factor for development of PHN, with each 10-year increase in age associated with a mean 1.2 to 3.1 increase in the relative odds of developing PHN.Footnote 31 The risk of PHN is particularly high among persons 50 years of age and older, with PHN risks ranging from 4% to 15% among HZ cases 50 to 59 years of age, 7% to 26% among HZ cases 60 to 69 years of age, and 14% to 29% among HZ cases 70 years of age and older, in prospective cohort studies.Footnote 17 Evidence of a relationship between PHN risk and sex is conflicting, with a recent systematic review finding differing conclusions and considerable heterogeneity across studies.Footnote 31 Unlike PHN, the risk of HZO does not vary by age.Footnote 17 In general, risk factors relating to HZO incidence, complications, and severity are largely unknown, however, it has been hypothesized they may be related to infection virulence and/or host immune response.Footnote 32
Currently, HZ is not a reportable illness in Canada, and therefore, provincial estimates of HZ incidence have largely been inferred from administrative data. Administrative databases have inherent limitations in ascertaining HZ incidence, such as the inclusion of only medically-attended HZ cases and reliance upon administrative billing codes to identify HZ medical encounters. As a result, these studies have the potential to miss and/or misclassify HZ cases. Despite limitations, these studies remain useful particularly to identify and examine underlying trends in HZ disease, provided that administrative coding practices do not change over time.Footnote 33
To date, trends in HZ incidence and rates of medical utilization have been examined via administrative data from the provinces of Alberta, British Columbia, Manitoba, Ontario, and Québec.Footnote 24 Footnote 26 Footnote 27 Footnote 28 Footnote 29 Footnote 34 Footnote 35 Footnote 36 Generally, results were similar, with crude and adjusted population incidence rates of medically-attended HZ of 3 to 5 cases per 1,000 person-years.Footnote 24 Footnote 26 Footnote 27 Footnote 28 Footnote 29 Footnote 34 Footnote 35 HZ incidence was strongly associated with age, with minimum and maximum HZ incidence consistently observed among youngest and oldest age groups, respectivelyFootnote 24 Footnote 26 Footnote 27 Footnote 28 Footnote 29 Footnote 34 (Figure 1). Similar to global estimates of HZ incidenceFootnote 17 Footnote 25 , HZ incidence among Canadian populations steeply increased among persons 50 years of age and older, with HZ incidence ranging from 4 to 6 cases per 1,000 person-years among adults 50 years of age, 6 to 9 cases per 1,000 person-years among adults 60 years of age, 7 to 11 cases per 1,000 person-years among adults 70 years of age, and 8 to 13 cases per 1,000 person-years among adults 80 years of age and older (Figure 1). Females also had a greater risk of HZ across all age strata.Footnote 26 Footnote 27 Footnote 28 Footnote 29 Approximately 2% to 4% of Canadian HZ cases were hospitalized.Footnote 26 Footnote 27 Similar to incidence, hospitalization rates were strongly associated with age, with peak rates observed among persons 65 years of age and olderFootnote 24 Footnote 26 Footnote 29 Footnote 34 Footnote 36 (Figure 2). Likewise, international data from published studies of PHN risk per case of HZ reveal a strong association with age, particularly among those 65 years of age and older (Figure 3).
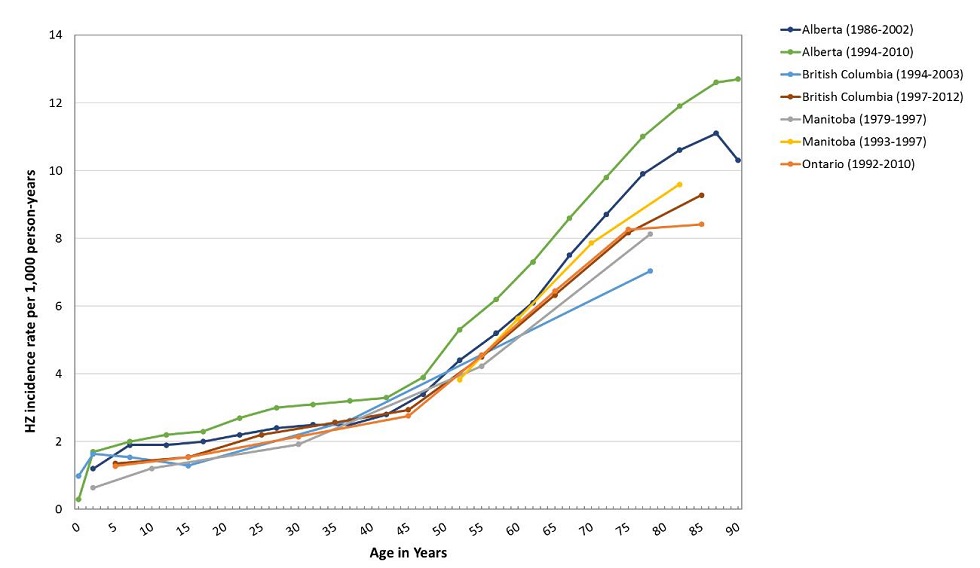
Figure 1 - Text description
Figure 1 shows HZ incidence rate per 1,000 person-years (vertical axis) with respect to population age in years (horizontal axis). Data points are based on published studies from Canadian provinces and territories. Among those studies where rates are reported for a range of ages, age is plotted based upon median age of the age category. For age categories that include a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages are presumed to be 0 and 90 years, respectively.
Study results are plotted in distinct individual colors, differentiating between province, territory and/or time interval from which the data was obtained. The provinces and time intervals from which published data was available were Alberta (1986-2002; dark blue), Alberta (1994-2010; green); British Columbia (1994-2003; light blue); British Columbia (1997-2012; maroon); Manitoba (1979-1997; grey); Manitoba (1999-1997; yellow) and Ontario (1992-2010; orange).
All provincial data plots are intertwined, following the same trend from ages ≤ 10 up to ages ≥ 75, when studies start showing more discrepancy, with one study from Alberta (1994-2010) exhibiting a trend towards higher incidence (approx. 1-3 PYs) than average. The overall trend is a slow increase in HZ incidence from zero to ~3 cases per 1,000 person-years from the ages of zero to 45 years old. At the age of 45, the slopes of all trend lines seem to increase, leading to HZ incidence between ~7 cases per 1,000 person-years (minimum - British Columbia 1994-2003) and ~13 cases per 1,000 person-years (maximum - Alberta 1994-2010) at age ≥ 75.
Please note: where rates were reported for a range of ages, age was plotted based upon median age of the age category. For age categories that included a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages were presumed to be 0 and 90 years, respectively.
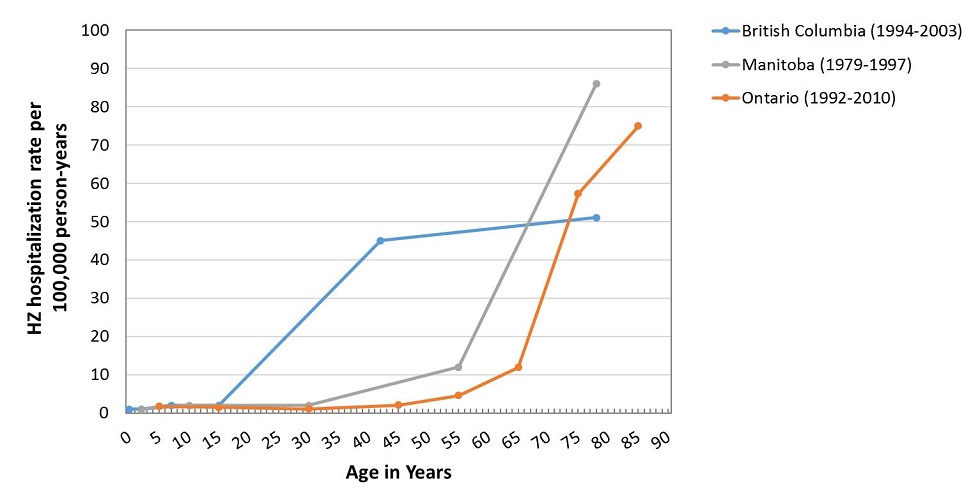
Figure 2 - Text description
Figure 2 shows HZ hospitalization rate per 100,000 person-years (vertical axis) with respect to population age in years (horizontal axis). Data points are based on published studies from Canadian provinces and territories. Among those studies where rates are reported for a range of ages, age is plotted based upon median age of the age category. For age categories that include a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages are presumed to be 0 and 90 years, respectively.
Study results are plotted in distinct individual colors, differentiating between province, territory and/or time interval from which the data was obtained. The provinces and time intervals from which published data was available were British Columbia (1994-2003; blue), Manitoba (1979-1997; grey) and Ontario (1992-2010; orange).
Both Manitoba and Ontario plots exhibit similar trends, i.e. a HZ hospitalization rate below 10 per 100,000 person-years for a population under the age of 45, along with a very significant slope increase starting at age 55 (Manitoba) and 65 (Ontario), increasing to maximums of ~87 HZ hospitalizations per 100,000 person-years at age 75 (Manitoba) and ~75 HZ hospitalizations per 100,000 person-years at age 85 (Ontario). The remaining plot (British Columbia) exhibits close-to-zero HZ hospitalizations per 100,000 person-years from among population aged ≤ 15, a steep increase to ~45 HZ hospitalizations per 100,000 person-years at age 45; and the lowest age ≥ 80 HZ hospitalization rate, being ~51 HZ hospitalizations per 100,000 person-years.
Please note: where rates were reported for a range of ages, age was plotted based upon median age of the age category. For age categories that included a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages were presumed to be 0 and 90 years, respectively.
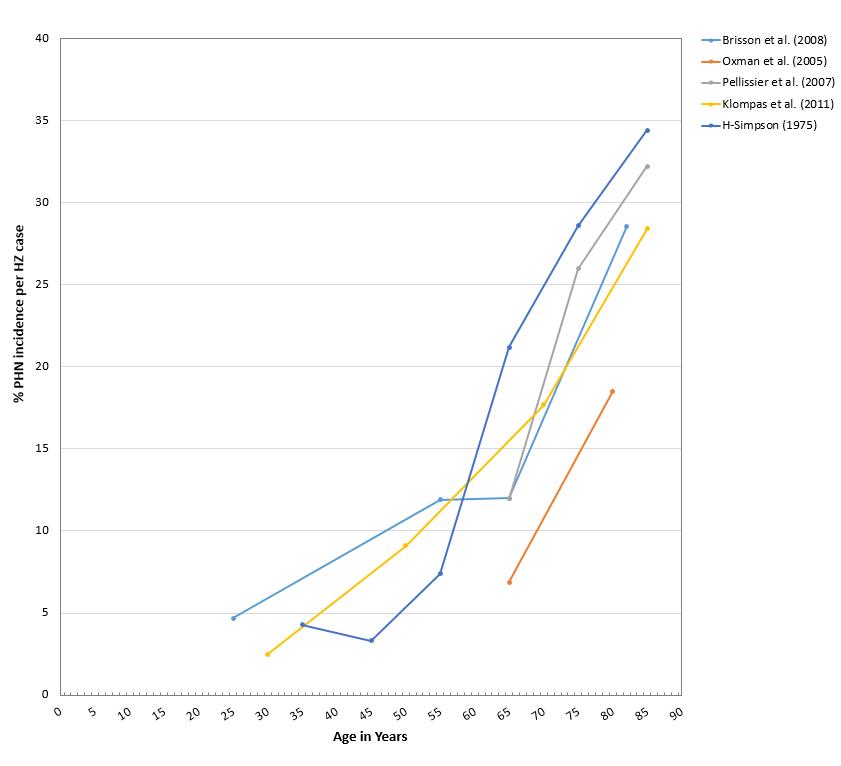
Figure 3 - Text description
Figure 3 shows the percentage of PHN incidence per HZ case (vertical axis) with respect to population age in years (horizontal axis) among published studies. In all studies, rates were reported for a range of ages, therefore age was plotted based upon median age of the age category. For age categories that included a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages were presumed to be 0 and 90 years, respectively.
Study results are plotted from data derived from published studies including a range of different study designs and methodologies. Study designs include: one RCT (Oxman et al, 2005 - orange), two analytic cohort models (Brisson et al, 2008 - light blue; Pellissier et al, 2007 - grey) and two retrospective cohort studies (H-Simpson, 1975 - dark blue; Klompas et al, 2011 - yellow).
All studies show a similar increasing trend of percentage of PHN incidence per HZ case along with age. The lowest values (below 5%) observed were among younger aged cohorts (25-45 years), and the lowest values observed among a more advanced aged cohort are shown by the plotted line from Oxman et al (2005), with a percentage of PHN incidence per HZ case of ~7% at age 65 and ~18% at age 80. The rest of the studies exhibit higher PHN incidence risk per case of HZ with advanced age, the second lowest % PHN risk per HZ case being ~12% and the highest being ~23% in the 60-65 age bracket, going all the way up to ~27% (lowest, Klompas et al 2011) to ~34% (highest, H-Simpson 1975) PHN incidence per HZ case in the ≥ 80 age bracket.
Please note: these data are derived from published studies including a range of different study designs and methodologies. Study designs include: one RCTFootnote 37 , two analytic cohort modelsFootnote 11 Footnote 38 , and two retrospective cohort studiesFootnote 13 Footnote 39 .
In all studies rates were reported for a range of ages, therefore age was plotted based upon median age of the age category. For age categories that included a non-discrete age range, (i.e. ages less than or greater than a designated age), the category minimum and maximum ages were presumed to be 0 and 90 years, respectively.
Several provincial studies have examined trends in HZ rates in relation to the adoption of childhood varicella vaccinationFootnote 26 Footnote 27 Footnote 29 Footnote 35 Footnote 36 , since it has been hypothesized that primary varicella vaccination may decrease natural boosting from circulating VZV, and result in a greater risk of VZV reactivationFootnote 40 Footnote 41 . While increases in HZ incidence or rates of clinical visits were observed over the study period in four out of five provincial studies, in two of these studiesFootnote 29 Footnote 35 , increasing HZ incidence was associated with the licensure of HZ vaccine, but not with the implementation of varicella vaccination. Based on these findings, authors hypothesized the increase in HZ incidence may be due to misclassification of visits pertaining to HZ vaccination as HZ disease. In the remaining two studies that reported an increase in HZ ratesFootnote 27 Footnote 36 , rates also increased during the pre-vaccine period making it difficult to ascertain the true relationship between HZ and primary varicella vaccination. In the remaining study, the risk of HZ during the post-publicly funded varicella vaccine program period was not statistically different from the non-publicly funded varicella vaccine period, after adjustment for potential confoundersFootnote 26. Varying trends in HZ incidence have been reported in studies of pre- and post-implementation primary varicella vaccination programs in the United States and elsewhereFootnote 17 Footnote 42 Footnote 43 . As a result, the relationship between primary varicella immunization programs and HZ incidence remains unclearFootnote 44 .
Since primary varicella vaccine-strains can reactivate to cause HZ, examination of HZ rates among vaccinated children is also of interest in the post-varicella vaccine era. Studies from Alberta, British Columbia, Ontario, and Québec found decreases in HZ rates in the post- relative to the pre-vaccination era among children under 10 years of age who were eligible for varicella vaccinationFootnote 26 Footnote 27 Footnote 29 Footnote 36 . These data are consistent with results from other studies that found a lower HZ risk among children vaccinated with varicella vaccine compared with unvaccinated childrenFootnote 45 Footnote 46 Footnote 47 Footnote 48 . The risk of HZ among children who received varicella vaccination is an area of continued interest, particularly as vaccinated children grow into those ages that are traditionally associated with greater HZ riskFootnote 8 Footnote 49 .
III.3 High Risk Groups
Individuals who are immunocompromised either due to underlying conditions or immunosuppressive agents have an increased risk of developing HZFootnote 26 Footnote 30 Footnote 50 , and may be more likely to experience atypical and/or more severe disease and complicationsFootnote 51 Footnote 52 Footnote 53 Footnote 54 Footnote 55 . A recent systematic review and meta-analysis examined the risk of HZ among persons living with autoimmune conditions, including rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease, and found a 1.4 to 2.1 times higher risk (varying by condition) among individuals living with these conditions relative to persons without comorbiditiesFootnote 17 Footnote 30 . Another systematic review and meta-analysis estimated a 1.2 to 2.2 times higher risk of HZ among persons taking an immunosuppressive drug, such as biologics that do not target tumor necrosis factor, nonbiological disease-modifying antirheumatic drugs, or corticosteroids (with risk varying by drug), relative to persons taking placebo or no drugsFootnote 50 . Persons who are immunocompromised may also be at greater risk of developing PHN, than the general population, with higher rates of PHN observed among people who are severely immunosuppressed, people living with diabetes mellitus, or people with systemic lupus erythematosusFootnote 31. Rates of PHN lasting more than 6 months were also higher among people living with conditions presumed to affect host CMI as compared with the general population, in an administrative database study from the United StatesFootnote 55 .
III.4 Summary of HZ immunization coverage in Canada
Currently, HZ vaccine coverage is not examined via national surveys in Canada. A recent study from Alberta, however, estimated that provincial HZ vaccine coverage was approximately 8% among persons 60 years of age or older in the absence of a public HZ vaccination program and during the 4 years following HZ vaccine authorizationFootnote 56 . Given its public HZ vaccination program, provincial HZ vaccine coverage is likely higher in Ontario; however, coverage data are currently not available (author correspondence).
IV. Vaccine
IV.1 Preparations authorized for use in Canada
Two HZ vaccines are currently authorized for use in Canada in immunocompetent individuals ≥50 years of age. A live attenuated unadjuvanted vaccine, Zostavax®, has been authorized since 2008, with the newer refrigerator stable product, Zostavax®II, replacing the original freezer stable product in 2011. A recombinant adjuvanted subunit vaccine (RZV), Shingrix®, has recently been authorized in October 2017.
LZV is based on the Oka/Merck attenuated varicella virus strain which is also used for varicella vaccine productionFootnote 57 . Although zoster vaccine contains the same components as the varicella vaccine Varivax®(Merck), it has 14-fold or higher virus concentration (≥19,400 plaque forming units per dose).
RZV combines an antigen (lyophilized recombinant varicella zoster virus surface glycoprotein E, VZV gE) and adjuvant system (AS01B). This adjuvant system is composed of liposomes containing two immunostimulants (3-O-desacyl-4'-monophosphoryl lipid A [MPL]) and Quillaja saponaria Molina, fraction 21 (QS-21)Footnote 58 and has been designed to enhance the humoral immune response as well as induce a high cellular immune response to help address the natural age-related decline in immunity (immunosenescence). Similar adjuvant systems (combinations of immunostimulatory molecules to enhance protection compared to aluminum salts), are present in two licensed vaccines in Canada (AS03 in pre/pandemic vaccine Arepanrix™ H5N1; and AS04 in human papillomavirus vaccine, Cervarix™)Footnote 59 , as well as vaccines currently in clinical trials. RZV is the first vaccine authorized in Canada that includes the AS01B adjuvant system, which is also being explored in candidate malaria vaccines.
Characteristics of the HZ vaccines currently authorized for use in Canada are summarized in Table 4.
| Product | Zostavax®IIFootnote a | Shingrix®Footnote b |
|---|---|---|
| Manufacturer | Merck Canada Inc | GlaxoSmithKline Inc |
| Date of authorization in Canada | 2008 (Zostavax®) - no longer available in Canada 2011 (Zostavax®II) |
October 2017 |
| Type of vaccine | Live attenuated | Recombinant subunit |
| Composition | Active ingredient: Oka/Merck strain of VZV developed through serial passages in tissue culture. Other ingredients: 31.16 mg of sucrose, 15.58 mg of hydrolyzed porcine gelatin, 3.99 mg of sodium chloride, 0.62 mg of monosodium L-glutamate, 0.57 mg of sodium phosphate dibasic, 0.10 mg of potassium phosphate monobasic, 0.10 mg of potassium chloride; residual components of MRC-5 cells including DNA and protein; and trace quantities of neomycin and bovine calf serum. |
VZV glycoprotein E recombinant (protein found on VZV) 50 mcg Powder (gE): dipotassium phosphate, Polysorbate 80, sodium dihydrogen phosphate dehydrate, sucrose. Adjuvant: AS01B (liposome-based) containing 50mcg plant extract Quillaja saponaria Molina fraction 21 (QS-21) + 50 mcg 3-O-desacyl-4'-monophosphoryl lipid A (MPL) from Salmonella minnesota combined with 1mg of dioleoyl phosphatidylcholine (DOPC) and 0.25mg cholesterol. Adjuvant suspension also contains: disodium phosphate anhydrous, potassium dihydrogen phosphate, sodium chloride, water. |
| Schedule | 1 dose | 2 doses, 2-6 months apart. (NACI suggests that a 0, 12 months schedule may be considered to improve coverage of the 2nd dose through simultaneous administration with another vaccine based on an acceptable safety profile of this schedule and robust anti-gE immune response, though it was not non-inferior to a 0, 2-month schedule) Footnote c |
| Route of Administration | Subcutaneous | Intramuscular |
| Indications | Prevention of HZ in individuals ≥ 50 years | Prevention of HZ in individuals ≥ 50 years |
| Contraindications | - History of hypersensitivity to any component of the vaccine, including gelatin and neomycin - Immunosuppression or immunodeficiency - Pregnancy |
-Known hypersensitivity to the active substance or to any component of the vaccine |
| Precautions | - Breastfeeding | - Pregnancy (no data in humans) - Breastfeeding (no data) - Immunocompromised individuals (limited data) |
| Storage Requirements | Zostavax®II: Refrigerator - stable (Zostavax®-- no longer available in Canada: Freezer- stable) |
Refrigerator - stable |
|
||
IV.2 Efficacy and Effectiveness
IV.2.1 Efficacy and effectiveness of LZV in the general population
There were 14 studies that assessed single-dose live zoster vaccine efficacy (VE) and effectiveness in the general population. Of these, 3 were good quality studies and 11 were rated as fair quality (Refer to Summary of Evidence Tables, Appendix A).
Efficacy of LZV in preventing HZ among adults 50-59 years of age was reported in a large RCT involving over 22,000 individualsFootnote 61 . Within 1.5 years of immunization, VE was estimated to be 69.8% (95% CI: 54.1%-80.6%). Lower vaccine effectiveness within one year of immunization (50.34% [95% CI: 36.01-51.55%]) in this age group was reported following an analysis of observational dataFootnote 62.
While comparable protective effects against incident HZ were reported in adults 60-69 years of age, a decline in vaccine effectiveness was generally observed with age. In the largest clinical trial that assessed vaccine protection in adults over 60 years of age, three-year efficacy was highest in adults less than 70 years of age (63.9% [95% CI: 55.5%-79.9%] vs. 37.6% [95% CI: 25%-48.1%] in adults 70 years of age and olderFootnote 37 Footnote 63 (overall trial VE 51.3% [95% CI: 44.2%-57.6%]). Although the sample population from the shingles prevention efficacy study (Department of Veterans Affairs Collaboration) might not provide a complete representation of the general population, the estimates were consistent with observational studies in which three-year effectiveness ranged from 48% (95% CI: 39%-56%) to 55% (95% CI: 52%- 58%)Footnote 62 Footnote 64 Footnote 65 Footnote 66 Footnote 67 Footnote 68 for adults over 60 years of age and from 33% (95% CI: 32%-35%) to 49.8% (95% CI: 46.6%-52.8%) for adults 70 years of age and older. In addition to the observed waning of protection with age, reviewed studies also reported continuous declines in effectiveness over time, with little or no protection observed beyond 6 years post-immunizationFootnote 61 Footnote 66 .
Immunization with LZV was also found to be protective against PHN and recurrent HZ. In clinical trials, three year effectiveness against PHN was reported to be 65.7% (95% CI: 20.4%-86.7%) in adults 60-69 years of age and 66.8% (95% CI: 43.3%-81.3%) in adults 70 years of age and olderFootnote 37 Footnote 63 . These estimates were similar to those reported in observational studiesFootnote 68 Footnote 70 . In individuals with previous HZ, protection within three years of immunization was only observed among adults less than 70 years of age (61% [95% CI: -3.45%-95%]), but not in those 70 years of age and older (-0.05% [95% CI: -1.09%-70%Footnote 69 ]).
IV.2.2 Efficacy and effectiveness of RZV in the general population
Estimates of RZV VE (two doses) were available from two pivotal clinical trials that recruited over 28,000 adults over 50 years of age. Both were rated as good quality studiesFootnote 71 Footnote 72 (See Summary of Evidence Tables). Among adults 50 to 59 years of age, three year efficacy was estimated to be 96.6% (95% CI: 89.6%-99.3%) for incident HZ and 100% (95% CI: 40.8%-100%) against PHN. In adults 60-69 years of age, efficacy against HZ was reported to be 97.4% (95% CI: 90.1%-99.7%). For adults 70 years of age and older, using pooled data from both studies, VE against incident HZ was estimated to be 91.3% (95% CI: 86.8%-94.5%). For adults 80 years of age and older, using pooled data from both studies, VE against incident HZ was estimated to be 91.4% (95% CI: 80.2%-97.0%). Although a decrease in efficacy in this age group was observed over a four-year post immunization period, differences between year one (97.6% [95% CI% 90.9%-99.8%]) and year four (84.7% [95% CI: 69%-93.4%]) were not found to be statistically significant. Overall VE against PHN was 91.2% (95% CI: 75.9-97.7) in adults 50 years of age and older, and 88.8% (95% CI: 68.7%-97.1%) in adults 70 years of age and older.
IV.3 Immunogenicity
Traditionally, studies of HZ vaccines have used anti-VZV antibodies to assess humoral immunity and a variety of cellular assays to assess CMI. More recently, to assess humoral immunity, pivotal trials of the RZV vaccine have specifically measured anti-gE antibodies in addition to anti-VZV antibodies. Some studies have reported only anti-gE antibodies. Equivalency between anti-VZV and anti-gE antibody responses following vaccination or infection has not been established in the literature, but manufacturer data on file report good correlation between anti-gE and anti-VZV antibodies.
There are currently no established humoral and/or cellular correlates of protection against herpes zoster or PHN among patients who have had primary VZV infection or prior vaccinationFootnote 73 Footnote 74 . Therefore, all studies evaluating the immunogenicity of zoster vaccination must be interpreted with caution. It does appear that CD4+ and CD8+ cells play a central role in preventing VZV reactivationFootnote 71 Footnote 75 ; and one studyFootnote 76 has suggested that CMI (as measured by IFN-gamma producing T-cells) at the time of zoster onset was associated with reduced disease severity and reduced likelihood of PHN, whereas humoral immunity (as measured by anti-VZV antibodies) was notFootnote 77 .
Many immunogenicity studies reviewed did not include control groups where patients did not receive any vaccination, and the overall quality of evidence for most studies was fair or poor (See Summary of Evidence Table, Appendix B).
IV.3.1 Immunogenicity of LZV in the general population
All reviewed studies used LZV (there were no other live vaccines in this population group). Studies generally all assessed humoral immunity through anti-VZV antibody levels, and many also assessed CMI through VZV-specific IFN-gamma spot-forming cells with ELISPOT or through responder cell frequency assays measuring counts per minute of H3-thymidine incorporation in peripheral blood mononuclear cells stimulated with VZV. LZV was found to be immunogenic (i.e. there were significant increases in antibody or T-cell levels) in all studies.
The duration of follow-up ranged from 4 weeks to up to 3 years (except for studies looking at those who were receiving a booster shot). In general, immunity as measured by antibody levels and T-cell counts peaked at 6 weeks and declined afterwards. One studyFootnote 76 , rated as good quality, suggested that CMI (as measured by IFN-gamma positive T-cells) at the time of zoster onset was associated with reduced disease severity and likelihood of PHN, whereas humoral immunity (as measured by anti-VZV antibodies) was not. Another study, rated as good quality, suggested that the rise in antibody titres up to 6 weeks post-vaccination was correlated with VE whereas antibodies levels after 6 weeks was notFootnote 77 .
Immune responses to LZV appeared to decline with age.One studyFootnote 78 , rated as good quality, suggested that the humoral response among those 50-59 years old was slightly higher than among those 60 years and older. Another fair quality study suggested that the CMI response was higher in those 60-69 years of age compared to those over 70 years of age.
In terms of the mechanism of administrationFootnote 79 , one fair quality study suggested that intradermal administration of LZV was associated with higher and more persistent increases in humoral immunity than traditional subcutaneous administration. Another fair-quality study did not find any differences in intramuscular versus subcutaneous administrationFootnote 80 . In terms of the number of doses required, two studiesFootnote 81 Footnote 82 suggested there were no differences in immunogenicity between 1 and 2-dose administrations of LZV. Regarding booster doses, one fair quality and one poor quality study assessed the effect of a booster dose among those older than 70 years of age compared to those who were being vaccinated for the first time. For those receiving boosters, there appeared to be a greater CMI response but no difference in humoral responseFootnote 83 Footnote 84 .
IV.3.2 Immunogenicity of RZV in the general population
Studies reviewed on immunogenicity of RZV generally all assessed humoral immunity through anti-gE antibody levels and many also assessed CMI, usually through CD4+ T-cells with at least two activation markers (including expression of IFN-gamma, IL-2, TNF-alpha, or CD40 ligand). RZV was found to be immunogenic in all studies.
With respect to duration of protection, one study available only as an abstract at the time of NACI deliberations found that measures of humoral and cell mediated immunity were still elevated from baseline at 9 years post-vaccination, with anti-gE and T-cell levels plateauing between years 4 and 9 post-vaccinationFootnote 85 . Another study, rated as poor quality, found that while humoral and CMI peak at month 3, anti-gE and CD4+ T-cells were elevated from baseline at 72 months post-vaccinationFootnote 86 .
Levels of immunity did not appear to vary by age. One study rated as poor quality, found that similar levels of CMI and humoral immunity were elicited across those aged 50-59, 60-69, and 70 years or overFootnote 105 . Among patients with prior zoster infection, the subunit vaccine was found to generate a robust humoral response that was similar for all age groups over 50Footnote 87 years in another study rated as poor quality. This study had limitations that precluded definitive evaluation of a prior episode of HZ.
One abstract (of a study which has since been published) suggested that prior vaccination with live vaccine at least 5 years prior did not appear to change the baseline measures of humoral or cell mediated immunity while vaccination with RZV led to a similar response in patients with and without a prior history of vaccination with live zoster vaccineFootnote 88 . Similarly, one study rated as poor quality demonstrated that among patients with a history of herpes zoster, RZV elicited a robust humoral immune response that was similar for all age groups over 50Footnote 87 years of age.
IV.3.3 Head-to-head comparisons of LZV versus RZV
Only one study by Weinberg et al. has compared immunogenicity between the live and subunit vaccines in a head-to-head fashion, and it is currently available only as an abstract that could not be rated for qualityFootnote 89 . This study suggests that there is a higher memory CD4+ and CD8+ response among those receiving RZV than those receiving the live vaccine. These results suggest that the RZV is more immunogenic than the live vaccine.
IV.4 Vaccine Administration and Schedule
IV.4.1 Vaccine administration and schedule for LZV
LZV is given as a subcutaneous injection, preferably in the deltoid region. It should be reconstituted immediately upon removal from the refrigerator. Please see the product monograph for details on reconstitution of the vaccine prior to administration.
Individuals should receive a single dose consisting of the entire content of the reconstituted vial (approximately 0.65 mL).
The need for a booster dose following primary vaccination has not been established.
IV.4.2 Vaccine administration and schedule for RZV
RZV is given as an intramuscular injection, preferably in the deltoid muscle. The vaccine is supplied as a vial of lyophilized recombinant varicella zoster virus surface glycoprotein E (VZV gE) which is reconstituted at the time of use with the accompanying vial of AS01B adjuvant suspension. Please see the product monograph for details on reconstitution of the vaccine prior to administration.
The primary vaccination schedule is a two dose series (0.5 mL/dose) with the second dose administered between 2 and 6 months after the first dose. Two doses of RZV administered 2 months apart have been shown to be immunogenic and efficacious against HZ. Immunogenicity studies that looked at alternative dosing schedules demonstrated that 0, 6months was non-inferior to 0, 2 months. However, non-inferiority of the 0, 12 months schedule was not demonstrated. The small study of 346 participants found that two doses of RZV elicited robust anti-gE immune responses in adults ≥50 years of age with 0-2, 6 and 12- month schedules with no safety concerns identified in any of the three schedules. Immune responses to RZV administered at months 0 and 6 were non-inferior to those elicited by a 0, 2-month schedule. Non-inferiority in terms of anti-gE humoral immune responses 1 month post-dose 2 was not demonstrated for the 0, 12-month schedule. This may have been due to a small number of participants with markedly lower anti-gE antibody levels post-vaccination, not observed in the other groups. No explanation for the low anti-gE antibody levels post-vaccination of these 9 participants in the 0, 12-month schedule could be identified by the investigators.
While the recommended interval between two doses of RZV is 2-6 months, a minimum interval between two doses of RZV (below which the second dose is considered invalid and should be repeated) of 1 month (4 weeks) should be maintained. Initial results from studies in immunocompromised populations using a one month interval between doses of RZV suggest no safety, immunogenicity, or efficacy concernsFootnote 61 . If an interval longer than 6 or 12 months after the first dose has elapsed, the vaccine series need not be restarted, however individuals may remain at risk of HZ during a longer than recommended interval between doses 1 and 2.
The need for a booster dose following the primary vaccination schedule has not been established.
IV.5 Serological Testing
Serologic testing is not recommended before or after HZ vaccination. There are no accepted correlates of protection following immunization against varicella and zoster using tests for humoral antibody or cell mediated immunity. HZ vaccination of healthy individuals who are VZV susceptible is not associated with any known safety risk. If, in the rare circumstance, an individual aged 50 years or older is known to be susceptible to VZV, two doses of univalent varicella vaccine should be administered rather than HZ vaccineFootnote 90. Immune protection against HZ cannot be readily tested therefore there is no role for post-immunization testing of antibody titres.
IV.6 Storage Requirements
IV.6.1 Storage requirements for LZV
During shipment, LZV must be maintained at a temperature between -50°C and +8°C to ensure that there is no loss of potency. LZV should be stored in a refrigerator at a temperature of +2°C to +8°C or colder until it is reconstituted for injection. The diluent should be stored separately at room temperature (+20 to +25°C) or in the refrigerator (+2 to +8°C). Before reconstitution, it should be protected from light. After reconstitution, the vaccine should not be frozen. If reconstituted vaccine is not used within 30 minutes, it should be discardedFootnote 57 .
IV.6.2 Storage requirements for RZV
The lyophilized gE vial and the adjuvant solution vial should both be stored in a refrigerator at a temperature of +2°C to +8°C in the original package (to protect from light). Neither vial should be frozen. After reconstitution, the vaccine should be used promptly. If this is not possible, it should be stored in a refrigerator at a temperature of +2°C to +8°C. If reconstituted vaccine is not used within 6 hours, it should be discardedFootnote 58 .
IV.7 Simultaneous Administration with Other Vaccines
Simultaneous administration of vaccines can be beneficial by decreasing the required number of patient visits and increasing compliance with recommended vaccines.
IV.7.1 Simultaneous administration of LZV with other vaccines
In general, live vaccines given by the parenteral route may be administered concomitantly with other vaccinesFootnote 91 . For concomitant parenteral injections, different injection sites and separateFootnote 91 needles and syringes should be used. If not administered concomitantly, a minimum interval of 4 weeks should be maintained between two live parenteral vaccines.
In 2014, NACI recommended that pneumococcal 23-valent polysaccharide vaccine (Pneu-P-23) may be administered concomitantly with LZV at a different body injection site, based on good evidence from a study that showed no increase in cases of HZ in those who received concomitant vs. sequential administration of vaccinesFootnote 69 .
Concomitant administration of LZV with quadrivalent influenza vaccine has been found to be non-inferior according to pre-specified criteria (GMT ratio 0.87) to non-concomitant administration and led to an anti-VZV antibody GMFR of 1.9Footnote 92 .
Among individuals who received LZV together with an inactivated influenza or Pneu-23 vaccine, co-administration did not results in an increase in AEs compared to separate vaccine administration.
IV.7.2 Simultaneous administration of RZV with other vaccines
In general, inactivated vaccines may be administered concomitantly with, or at any time before or after, other inactivated vaccines or live vaccines protecting against a different disease. For concomitant parenteral injections, different injection sites and separate needles and syringes should be usedFootnote 93 Footnote 94 .
A study of concomitant administration of RZV with quadrivalent influenza vaccine reveals no evidence of safety concerns or interference in immune responses for either vaccineFootnote 94 . Concomitant administration was found to be non-inferior (GMC ratio control to concomitant was 1.08) for both RZV and the influenza vaccine as measured by GMC ratios at 1 month post-vaccination.
Studies of simultaneous administration with Pneu-P-23 and Boostrix®(Tetanus, low concentration diphtheria and acellular pertussis vaccine) are ongoing. The safety and efficacy of administration of two adjuvanted vaccines (e.g., RZV and adjuvanted influenza vaccine Fluad®) either concomitantly or at other intervals, have not been evaluated.
IV.8 Adverse Events
IV.8.1 Adverse events with LZV in the general population
In total, 21 studies reported on short and long term vaccine safety following the administration of LZV of different potencies. Of these 11 were good quality studies, 8 were fair quality studies and 2 were poor quality studies (See Summary of Evidence Tables, Appendix C).
In adults less than 60 years of ageFootnote 61 Footnote 95 , injection site reactions were the most commonly reported AEs, the majority of which (>95%) were rated mild or moderate in intensity. In the pivotal clinical trial in which over 11,000 adults 50-59 years of age received LZV, injection site AE were reported by 63.9% of vaccine recipients (49.5% [95% CI: 48.4%-50%] risk difference compared to placebo). In the same trial, vaccine-related systemic AEs within one to 42 days following immunization were reported in 6.7% of individuals (2% [95% CI: 1.4%-2.6%] increased risk of systemic AEs compared to placebo). Among individuals less than 60 years of age, only one vaccine-related AE was reported in the reviewed studies.
Compared to adults less than 60 years of ageFootnote 63 Footnote 79 Footnote 80 Footnote 81 Footnote 82 Footnote 95 Footnote 96 Footnote 97 Footnote 98 Footnote 99 Footnote 100 , adults 60 years of age and older generally reported fewer injection site AEs. The majority (>95%) of these events were rated mild or moderate in intensity and were of less than 2 days duration. In observational studies, erythema, pain, tenderness, and swelling were the most common symptoms reported by one quarter to one third of individuals. In a pivotal clinical trial that assessed vaccine safety in over 3,300 adults over 60 years of age, injection site AEs were reported by 56.6% of study participants 60-69 years of age (37.7% [34.6%-40.6%] risk difference compared to placebo), and 39.2% of study participants 70 years of age and older (25.4% [22.5%-28.4%]) risk difference compared to placebo).
In adults 60 years of age and older, systemic vaccine-related AEs within 42 days following immunization were reported by less than 8% of individuals. In a pivotal clinical trial that assessed vaccine safety in over 3,300 adults, vaccine-related systemic events were reported by 6.3% of study participants (1.4% [95% CI: 0.3%-2.5%] risk difference compared to placebo). Vaccine-related SAEs in this age group were rarely reported, with only an increase in the rate of allergic reactions being observed among LZV recipients. There was no increase in vaccine-related SAEs (e.g. measured by an increase in hospitalization and emergency department admission rates) reported in the reviewed observational studiesFootnote 46 Footnote 69 Footnote 101 Footnote 102 . Studies that assessed the safety of LZV administration in individuals over 60 years of age with prior HZFootnote 83 Footnote 103 Footnote 104 reported similar rates of AEs as those reported in previously LZV unimmunized individuals.
IV.8.2 Adverse events with RZV vaccine in the general population
Vaccine safety of RZV vaccine was investigated in seven randomized studiesFootnote 71 Footnote 72 Footnote 86 Footnote 105 Footnote 106 Footnote 107 Footnote 108 . The largest studies were two pivotal trials in which over 14,000 adults over 50 years of age received two doses of RZV vaccine. Of studies identified through the literature search, 4 were good quality studies and 3 were rated as fair quality studies (See Summary of Evidence Tables, Appendix C).
Injection site AEs were commonly reported by participants, with approximately 80% reporting injection-site pain and approximately 30% reporting redness at the site of injection. In a pivotal trial that assessed vaccine safety in over 15,400 adults 50 years of age and older, Grade 3 injection site reactions (AEs that were severe enough to prevent normal activities) were reported by 9.5% (96% CI: 8.7%-10.4%) of vaccine recipients compared to 0.4% (95% CI: 0.2%-0.6%) of placebo recipients. Among adults 70 years of age and older, Grade 3 injection site AEs were reported by 8.5% (95% CI: 6.2%-11.3%) of vaccine and 0.2% (95% CI: 0-1.1%) of placebo recipients. Pain was generally more commonly reported by participants less than 70 years of age compared to those who were 70 years of age and older. The median duration of reported injection site AEs was 2 to 3 days.
The most frequently reported systemic AEs in clinical trials were fatigue and myalgia (reported by up to half of vaccine recipients) as well as headache (reported by up to 40% of vaccine recipients). In a pivotal trial that assessed vaccine safety in over 15,400 adults over 50 years of age, Grade 3 systemic reactions were reported by 11.4% (95% CI: 10.5%-12.4%) of vaccine recipients compared to 2.4% (95% CI: 2%-2.9%) of placebo recipients. In adults 70 years of age and older, Grade 3 systemic AEs were reported by 6% (95% CI: 4.1%-8.4%) of vaccine and 2% (95% CI: 1-3.6%) of placebo recipients. Systemic events that included Grade 3 reactions were more frequently reported after the receipt of the second RZV vaccine dose. The median duration of reported systemic AEs was 1 to 2 days.
Overall, the rates of SAEs in the reviewed studies were similar between the intervention and control groups, with none of the SAEs considered to be vaccine-related by the study investigators based on the plausibility and time since vaccination. The rates of reported vaccine-related SAEs and immune-mediated diseases were similar in the vaccine and the placebo group up to 9 years post immunization.
IV.9 Contraindications and Precautions
IV.9.1 Contraindications and precautions for LZV
LZV is contraindicated in individuals with a history of hypersensitivity to any component of the vaccine, including gelatin, or an anaphylactic/anaphylactoid reaction to neomycin (present in trace quantities in the vaccine).
As it is a live vaccine and may result in disseminated disease in individuals who are immunosuppressed or immunodeficient, LZV is contraindicated in individuals with primary and acquired immunodeficiency states. It is not contraindicated in those receiving topical or inhaled corticosteroids, low-dose systemic corticosteroids, or in those receiving corticosteroids as replacement therapy (e.g. for adrenal insufficiency). LZV is contraindicated in active untreated tuberculosis.
LZV is contraindicated in pregnancy, and pregnancy should be avoided for three months after vaccine administration. While no studies have been conducted in this population, naturally occurring VZV infection is known to cause fetal harm in some cases.
Caution should be taken when LZV is administered to those who are breastfeeding as it is not known whether VZV is secreted in breast milk. In the presence of fever >+38.5°C, deferral of vaccination should be consideredFootnote 57 .
IV.9.2 Contraindications and precautions for RZV
RZV is contraindicated in individuals with a known hypersensitivity to any component of the vaccine.
This vaccine should be used with precaution in those who are pregnant (as there are no data on its use in this population), or breastfeeding (as the effect on breast-fed infants of vaccination in those who are breastfeeding has not been studied). The safety and efficacy in individuals younger than 18 years of age has not been studied, and there are limited data on its use in immunocompromised individuals 50 years of age and olderFootnote 58 .
V. Economics
V.1 Economic model description
To estimate the cost-effectiveness of Herpes Zoster (HZ) vaccination, a Cost Utility Analysis (CUA) was adapted from Brisson et al 2008Footnote 11 to compare the clinical and economic outcomes of different vaccination options. In the aforementioned study the authors compared LZV to no vaccination in a cohort through different phases of HZ. In this study the model was extended to include vaccination with RZV. Therefore, this CUA 1) evaluated the cost-effectiveness of vaccination against HZ using one of the two vaccines (LZV and RZV) compared to the absence of vaccination and 2) compared the cost-effectiveness between LZV and RZV. In brief, the model follows a cohort of individuals through different phases of HZ. As depicted in Figure 4, different HZ disease phases are represented by the boxes and arrows indicate the transition along the disease. Individuals in the cohort start off without HZ and may develop HZ and progress to PHN. Death is also associated for each health state. Cases of HZ and PHN are characterized according to their pain severity: no pain, mild/moderate pain, and severe pain. The model compares the incidence of HZ and PHN, healthcare resource use, costs and Quality Adjusted Life Years (QALY) lost to HZ and PHN between cohorts of vaccinated and unvaccinated individuals.
The study perspective is that of the health care system, which includes all direct medical costs of treating the disease. The societal perspective which considers costs outside of the health care system, such as lost productivity, was not examined because these costs fall outside of vaccination programs and the health care system. The base case has vaccination of 65-year-olds. Additional analyses also examined vaccination between 50 and 85 years of age. The cohort is modelled over a lifetime with costs and benefits discounted at 3%.
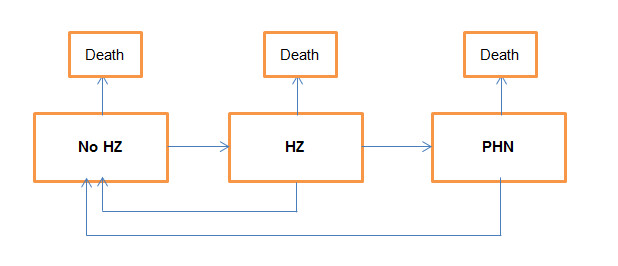
Figure 4 - Text description
Figure 4 shows different HZ disease phases. Each disease phase is depicted by a box. There are boxes to represent phases for No HZ, HZ, PHN and Death. Tryearsition from one disease phase to another is shown with arrows. At the phase of No HZ, the arrows show that disease can tryearsition to HZ or PHN or Death. At the phase of HZ, the arrows show that disease can tryearsition to PHN or Death or revert to No HZ. At the phase of PHN the arrows show that disease can tryearsition to Death or revert to No HZ. Reverting to No HZ occurs after treatment of the disease.
V.2 Model parameters: epidemiological, vaccine characteristics, and economic
The model parameters can be classified by the epidemiology, vaccine characteristics and economics (see Table 5). Vaccine characteristics on the efficacy for RZV and LZV were based on clinical trialsFootnote 61 Footnote 63 Footnote 71 Footnote 72 . Epidemiological data on age specific incidence of HZ and age specific incidence of hospitalization was obtained from administrative databases in QuebecFootnote 109 Footnote 110 and a literature review. Articles identified in the literature review are from OntarioFootnote 29 , BCFootnote 26 , and AlbertaFootnote 27 . The study considered the minimum and maximum values of these data sources and the base case is the mean of the minimum and maximum values identified. Other data on the length of stay, consultations per case, and PHN per case were derived from the literatureFootnote 11 Footnote 24 Footnote 63 Footnote 111 and MedEchoFootnote 110 and RAMQFootnote 109 . Economic data on the costs were inflated to 2015 Canadian dollars and obtained from the literature. Utility weights for each health state were used in the estimation of QALYs. These data were collected from the Monitoring and Assessing Shingles Through Education and Research (MASTER) studyFootnote 112 and from Brisson et alFootnote 11 .
| Parameters | Data Source |
|---|---|
| Epidemiology and health care resource use | |
| Incidence of HZ | RAMQ 2001-2015, Brisson et al 2008, Tanuseputro et al 2011, Marra et al 2016, Russell et al 2014. |
| Hospitalizations | MedEcho 2001-2015, Brisson et al 2008, Tanuseputro et al 2011, Brisson et al 2001. |
| Consultations (per case) | RAMQ 2001-2005, Brisson et al 2008, Najafzadeh et al 2009 |
| Length of Stay (days) | MedEcho 2001-2015, Brisson et al 2001, Najafzadeh et al 2009 |
| Case Fatality | Brisson et al 2008 |
| PHN (per case) | Oxman et al 2005, Brisson et al 2008 |
| Vaccine Characteristics | |
| Shingrix®(RZV) | |
| ZOE-50 | Lal et al 2015 |
| ZOE-70 | Cunningham et al 2016 |
| Zostavax®(LZV) | |
| SPS | Oxman et al 2005 |
| STPS | Schmader et al 2012 |
| Economic | |
| Unit costs (Canadian inflated to $2015) | |
| HZ GP consultation | Friesen et al 2017Footnote a, Najafzadeh et al 2009, Brisson et al 2008 |
| HZ Hospitalization | Friesen et al 2017Footnote a, Najafzadeh et al 2009, Brisson et al 2008 |
| Treatment per HZ episode | Friesen et al 2017Footnote a, Najafzadeh et al 2009, Brisson et al 2008 |
| Treatment per PHN episode | Friesen et al 2017Footnote a, Najafzadeh et al 2009, Brisson et al 2008 |
| Utility weights (QALY estimates) | Brisson et al 2008, Drolet et al 2010 |
|
|
V.2.1 Model parameters: vaccine characteristics
The vaccine characteristics were defined by the VE and waning rate. The VE reflects the proportion of individuals protected following immunization and the degree to which they are protected. The waning rate is the rate at which protection conferred by the vaccine diminishes over time. VE parameter values of the two vaccines were estimated by fitting the age-specific annual incidence of HZ predicted by the model with that observed in the vaccinated arm of the randomized clinical trials using 6 different functions of waning efficacy over time (Linear, 1-Exponential, Power, Exponential, Log, and 1-Power). This method, based on previous modeling studiesFootnote 11 Footnote 113 makes it possible to estimate both the short-term VE and waning efficacy from clinical trials, and explore the uncertainty surrounding the long-term efficacy of the two vaccines. Figure 5 shows the calibration results of the predicted VE to randomized clinical trials data (efficacy against HZ according to age, efficacy against HZ according to the years since vaccination, efficacy against PHN according to age).
Age specific VE parameter values were modelled. At each age RZV had higher VE compared to LZV. For LZV the VE against PHN was estimated to be higher than VE against HZ for individuals older than 70 y ears old (as seen in Brisson et al 2008). For RZV, trials did not show any significant difference in VE against HZ and PHN and the model assumed that both initial VE and waning efficacy were the same for HZ and PHN endpoints. The base case presumes full compliance for the RZV 2-dose series.
Figure 5: Fitted VE to vaccine clinical trial data
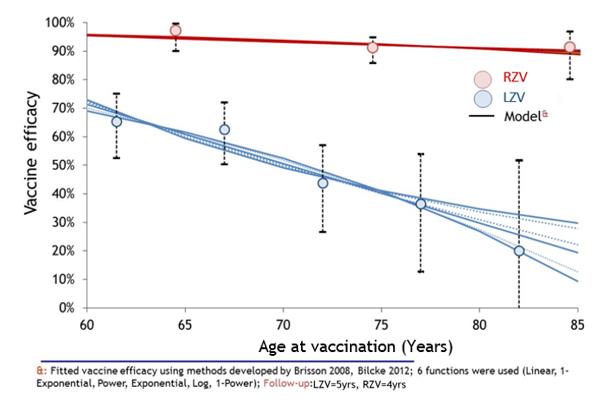
Figure 5A - Text description
Figure 5A shows line graphs depicting the estimated vaccine efficacy by age.
The horizontal axis contains the age at vaccination from age 60 to 85 years old at 5 year age increments. The vertical axis in the left has the vaccine efficacy in percentage from 0% to 100% at 10% intervals.
Red lines for RZV show the estimated vaccine efficacy whereas blue lines show LZV. RZV and LZV each has six lines based on six different estimations of vaccine efficacy.
Along the line graphs for RZV and LZV there are dots and confidence intervals representing the vaccine efficacy from clinical trials for all ages in order to demonstrate the accuracy of the estimated line graphs.
RZV vaccine efficacy for all six estimated lines is similar. At age 60 years the vaccine efficacy is over 95% and dCSlines to nearly 90% at age 85 years.
LZV vaccine efficacy for all six estimated lines is similar but the rate of dCSline is different after age 75 years. At age 60 years the vaccine is around 70% and dCSlines to around 10% to 30% at age 85 years.
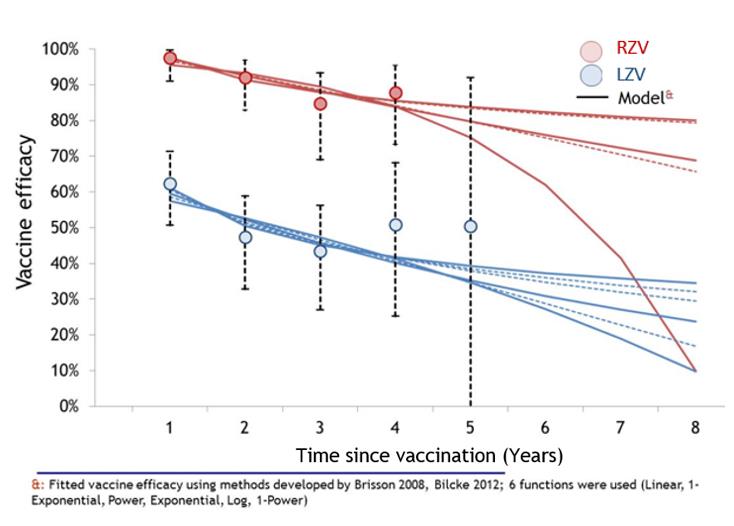
Figure 5B - Text description
Figure 5B shows line graphs depicting the estimated vaccine efficacy over time since vaccination.
The horizontal axis displays time since vaccination from years 1 to 8 in yearly increments. The vertical axis in the left has the vaccine efficacy in percentage from 0% to 100% at 10% intervals.
Red lines for RZV show the estimated vaccine efficacy whereas blue lines show LZV. RZV and LZV each has six lines based on six different estimations of vaccine efficacy.
Along the line graphs for RZV and LZV there are dots and confidence intervals representing the vaccine efficacy from clinical trials in years 1 to 4 in order to demonstrate the accuracy of the estimated line graphs. RZV vaccine efficacy for all 6 lines is similar from years 1-4, in which the vaccine efficacy remains around 90%. After the fourth year, five out of six estimated lines remain similar, showing vaccine efficacy between 70 to 85% after 8 years. Notably, the sixth estimated lines dCSlines all the way down to around 10% efficacy after 8 years post-vaccination.
LZV vaccine efficacy for all six estimated lines is similar but differentiate after the 5-year mark. The vaccine efficacy dCSreases from around 60% to 40% within the first 5 years, after which the lines reach a maximum of around 40% and a minimum of 10% at the 8-year mark, with the remaining lines in between those values.
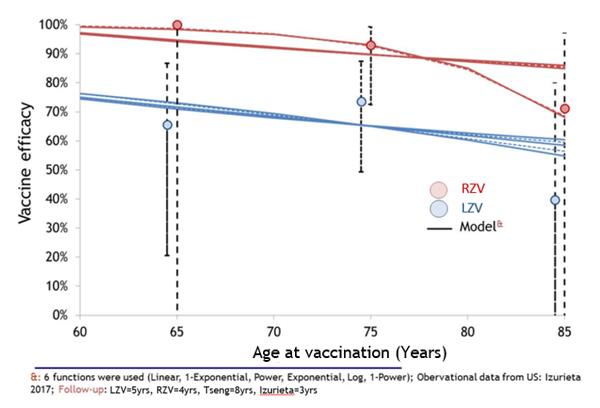
Figure 5C - Text description
Figure 5C shows line graphs depicting the estimated vaccine efficacy against PHN by age.
The horizontal axis contains the age at vaccination from age 60 to 85 years old at 5 year age increments. The vertical axis in the left has the vaccine efficacy in percentage from 0% to 100% at 10% intervals.
Red lines for RZV show the estimated vaccine efficacy whereas blue lines show LZV. RZV and LZV each has six lines based on different estimations of vaccine efficacy.
Along the line graphs for RZV and LZV there are dots and confidence intervals representing the vaccine efficacy from clinical trials for all ages in order to demonstrate the accuracy of the estimated line graphs.
RZV vaccine efficacy for all six estimated lines is similar from 90% to nearly 100% for ages 60-80. At age 80 years the vaccine efficacy around 90% remains constant for 4 out of 6 estimated lines, whereas two lines show a dCSrease in efficacy reaching near 75% at age 85 years. LZV vaccine efficacy for all six estimated lines are similar, exhibiting a slow but steady dCSrease from around 75% efficacy at age 60 years, down to around 65% at age 85.
V.2.2 Model parameters: epidemiological and health care resource use estimates
Parameters for epidemiology and health care resource use are presented in Table 6. For all parameters, the parameters from Brisson et al 2008 were examined and updated with literature reviews and specific analysis of available data sources. Parameters on the incidence, consultations, hospitalizations and deaths from HZ were updated through a systematic review and data extraction from Quebec administrative databases (Regie de l'Assurance Maladie du Quebec (RAMQ) and hospitalization database Med-Echo). The parameters in Table 6 represent the minimum and maximum values identified in the literature and from an unpublished Quebec administrative database analysis. The base case was assumed to be the mean of the minimum and maximum values. PHN was defined as a clinically significant pain persisting more than 90 days after rash onset. The proportion of HZ cases developing PHN used the minimum and maximum values from Brisson et al 2008, which were based on data from the Shingles Prevention StudyFootnote 63 and Edmunds et al 2001Footnote 114 . Case fatality values were based on studies from England and Wales given the lack of Canadian data of HZ related mortality.
| Age Range | Base | Min | Max | Reference |
|---|---|---|---|---|
| Herpes zoster incidence (per 1,000 person-year) | ||||
| 50-54 years | 3.8 | 3.5 | 4.2 | RAMQ 2001-2015 Brisson et al 2008 Tanuseputro et al 2011 Russell et al 2014 Marra et al 2016 |
| 55-64 years | 6.0 | 5.1 | 6.9 | |
| 65-74 years | 8.6 | 7.3 | 10.0 | |
| 75+ years | 9.9 | 8.0 | 11.8 | |
| Hospitalizations (per case) | ||||
| 50-54 years | 1.1% | 0.5% | 1.6% | MedEcho 2001-2015 Brisson et al 2008 Tanuseputro et al 2011 Brisson et al 2001 |
| 55-64 years | 1.6% | 0.7% | 2.5% | |
| 65-74 years | 3.3% | 1.5% | 5.1% | |
| 75+ years | 9.9% | 4.1% | 15.6% | |
| Consultations (per case) | ||||
| 50-54 years | 1.7 | 1.0 | 2.4 | RAMQ 2001-2015 Brisson et al 2008 Najafzadeh et al 2009 |
| 55-64 years | 2.0 | 1.0 | 2.9 | |
| 65-74 years | 2.3 | 1.0 | 3.5 | |
| 75+ years | 2.6 | 1.0 | 4.2 | |
| Length of Stay (days) | ||||
| 50-54 years | 9.3 | 5.9 | 12.7 | MedEcho 2001-2015 Brisson et al 2001 Najafzadeh et al 2009 |
| 55-64 years | 11.1 | 6.2 | 15.9 | |
| 65-74 years | 12.6 | 8.3 | 16.9 | |
| 75+ years | 18.0 | 12.4 | 23.6 | |
| Case-fatality | ||||
| 50-54 years | 0.000% | 0.000% | 0.002% | Brisson et al 2008 |
| 55-64 years | 0.000% | 0.000% | 0.002% | |
| 65-74 years | 0.012% | 0.012% | 0.083% | |
| 75+ years | 0.076% | 0.040% | 0.083% | |
| PHN risk (per case) | ||||
| 50-54 years | 9.4% | 6.9% | 11.9% | Oxman et al 2005 Brisson et al 2008 |
| 55-64 years | 9.4% | 6.9% | 11.9% | |
| 65-74 years | 26.0% | 18.5% | 33.4% | |
| 75+ years | 27.7% | 22.0% | 33.4% | |
V.2.3 Model parameters: economics
Parameter values for the economic inputs in the model were classified according to costing information and QALY estimates derived using utility weights (Tables 7 and 8). Costs represented expenditures on health care utilization to treat HZ using the mean costs from collected data sources and adjusted to 2015 according to the Consumer Price Index. This includes general practitioner (GP) consultation, hospitalization, prescription costs and costs of treating PHN based on data from the literature-see Table 7. Vaccine costs were both the price plus administrative costs. These costs considered the uncertainty of prices for RZV and LZV in publicly funded programs and also the variability of costs to administer a vaccine across provinces and territories. In Canada, the publicly available prices are the "list price", or retail price, which are both typically higher than negotiated prices with provincial and territorial vaccine programs through the bulk procurement program or individual contracts with jurisdictions. Given the uncertainty and confidentiality of negotiated prices and the variability in administrative costs, the base case instead investigated vaccine costs of $140 and $200 (price plus administration). Utility weights were used in the estimation of QALYs. These weights are anchored from 0 to 1 where 0 represents death and 1 is full health (or no disability). Weights valued between the anchors represent morbidity at a different health capacity. The QALYs lost per case (whether HZ or PHN) is the difference in the utility weights with and without disease over time. Utility weight data were obtained from the MASTER studyFootnote 112 and Brisson et al 2008Footnote 11 . The base case was assumed to be the mean of the minimum and maximum-see Table 8.
| Parameters | Costs (2015 $CAN) | Reference | ||
|---|---|---|---|---|
| Base Case Scenario | Min | Max | ||
| Hospitalizations | $876 | $473 | $1,419 | Friesen et al 2017Footnote a Najafzadeh et al 2009 Brisson et al 2008 |
| Consultations | $27 | $23 | $108 | Friesen et al 2017Footnote a Najafzadeh et al 2009 Brisson et al 2008 |
| Treatment per HZ episode | $129 | $52 | $244 | Friesen et al 2017Footnote a Najafzadeh et al 2009 Brisson et al 2008 |
| Treatment per PHN episode | $1,515 | $924 | $2,591 | Friesen et al 2017Footnote a Najafzadeh et al 2009 Brisson et al 2008 |
Min: Minimum values identified in literature; Max: Maximum values identified in literature; Base Case: Values from Friesen et al 2017
|
||||
| Age Range | QALYs lost (utility values) | Reference | ||
|---|---|---|---|---|
| Base Case Scenario | Min | Max | ||
| HZ | ||||
| 50 to 59 years old | 0.009 | 0.006 | 0.012 | Brisson et al 2008 Drolet et al 2010 |
| 60 to 69 years old | 0.010 | 0.006 | 0.013 | |
| 70+ years old | 0.010 | 0.007 | 0.014 | |
| PHN | ||||
| 50 to 59 years old | 0.041 | 0.032 | 0.052 | Brisson et al 2008 Drolet et al 2010 |
| 60 to 69 years old | 0.192 | 0.103 | 0.290 | |
| 70+ years old | 0.234 | 0.191 | 0.290 | |
Min: Minimum values identified in literature; Max: Maximum values identified in literature; Base Case: Values from Friesen et al 2017 |
||||
V.3 Results
All model estimates were based on 30,000 simulations and presented with the median and 90% Uncertainty Intervals (UI) which show the 5th and 95th percentile of the distribution of simulation results. To obtain these estimates, each parameter was assigned a triangular probability distribution and combinations of these parameter values were drawn using Latin hypercube sampling. The maximum and minimum values of the triangular distribution are the maximum and minimum values identified from the literature, and the median is the base case values found in Tables 6, 7, 8.
V.3.1 Results: Cost-effectiveness
The base case results examined 65 year olds (Figure 6). RZV has median ICERs ranging from cost savings to $6,356 per QALY at different vaccine costs ($100-$200). LZV has higher median ICERs ranging from $7,673 per QALY to $37,249 per QALY and less cost effective than RZV.
Figure 7 displays the results for all age groups at various vaccine costs (price plus administration). Compared to LZV, RZV has lower cost per QALYs for all age groups and vaccine costs and therefore more cost effective than LZV. At ages 65-79, RZV is the most cost-effective compared to other age groups because of higher burden of illness with age (increased risk of hospitalization and PHN per HZ case) and the likeliness that the vaccine will be effective during the years when burden of illness is high (unless VE wanes more quickly than anticipated).
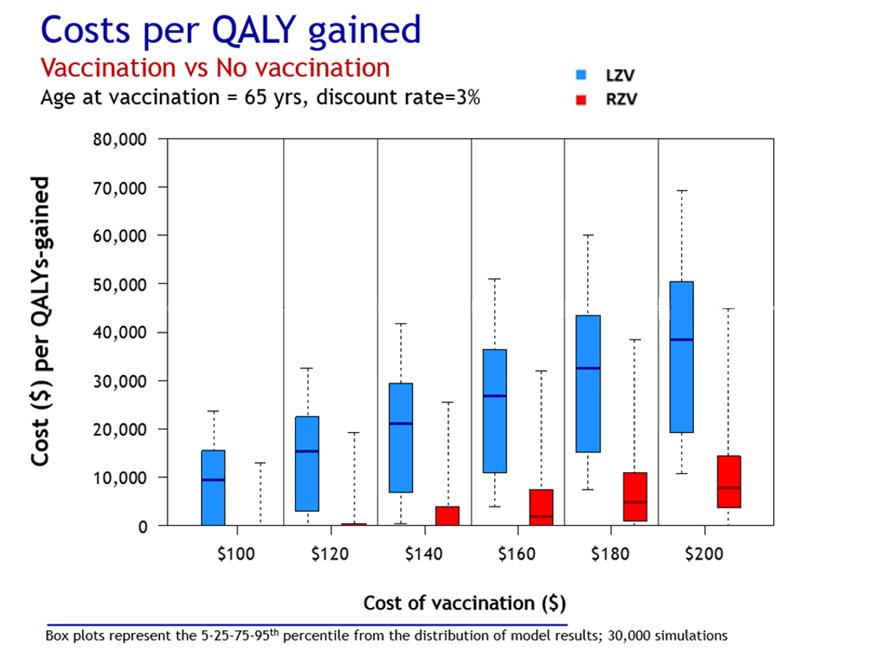
Figure 6 - Text description
| Age at vaccination/ Vaccine Cost | LZV Percentiles of model predictions |
RZV Percentiles of model predictions |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | 5th | 25th | Median | 75th | 95th | |
| 65 years | ||||||||||
| 100 $ | CS | CS | 7 673 | 14 224 | 22 710 | CS | CS | CS | CS | 11 778 |
| 120 $ | CS | 1 688 | 13 647 | 21 334 | 31 929 | CS | CS | CS | CS | 18 187 |
| 140 $ | CS | 5 828 | 19 576 | 28 434 | 41 349 | CS | CS | CS | 2 922 | 24 715 |
| 160 $ | 1 064 | 9 960 | 24 486 | 35 614 | 50 822 | CS | CS | 488 | 6 359 | 31 295 |
| 180 $ | 4 686 | 14 139 | 31 345 | 42 810 | 60 345 | CS | CS | 3 414 | 9 874 | 37 839 |
| 200 $ | 8 235 | 18 344 | 37 249 | 49 994 | 70 059 | CS | 1 507 | 6 356 | 13 433 | 44 382 |
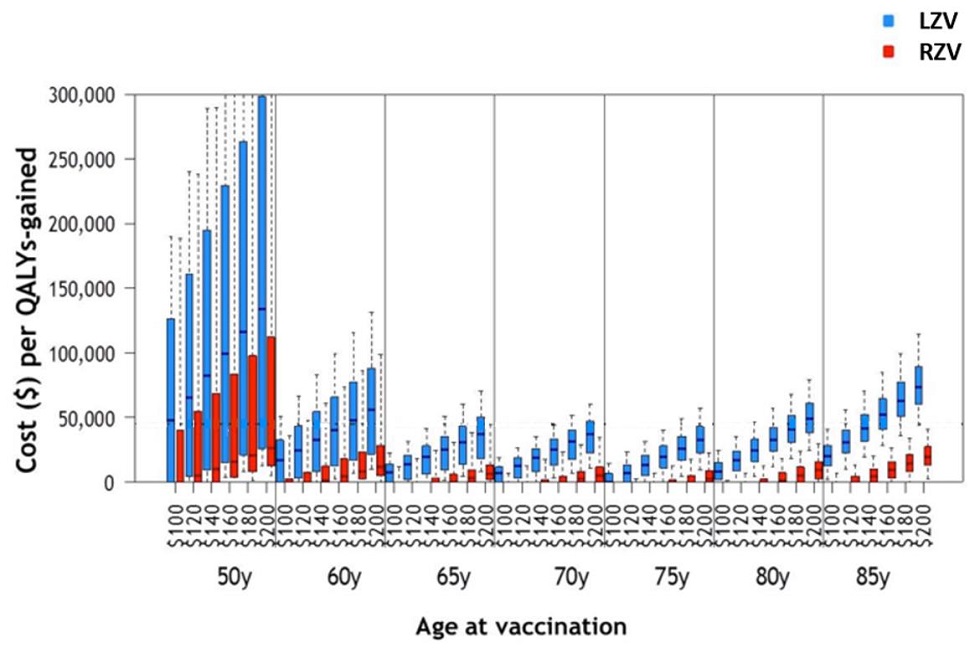
Figure 7 - Text description
| Age at vaccination/ Cost of vaccination | LZV Percentiles of model predictions |
RZV Percentiles of model predictions |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | 5th | 25th | Median | 75th | 95th | |
| 50 years | ||||||||||
| 100 $ | CS | CS | 48 218 | 126 144 | 190 174 | CS | CS | CS | 40 129 | 188168 |
| 120 $ | CS | 4 595 | 65 295 | 160 411 | 239 776 | CS | CS | 5 018 | 54 585 | 238517 |
| 140 $ | CS | 9 938 | 82 335 | 194 883 | 289 253 | CS | 288 | 10 391 | 68 986 | 289570 |
| 160 $ | 3 777 | 15 269 | 99 362 | 229 146 | 339 041 | CS | 4 266 | 15 704 | 83 534 | 339960 |
| 180 $ | 7 995 | 20 713 | 116 389 | 263 419 | 388 706 | 1 320 | 8 214 | 21 128 | 97 972 | 390442 |
| 200 $ | 12 200 | 26 172 | 133 416 | 297 892 | 438 704 | 5 067 | 12 164 | 26 651 | 112450 | 441319 |
| 60 years | ||||||||||
| 100 $ | CS | CS | 16 723 | 32 160 | 50 672 | CS | CS | CS | 2 673 | 35 736 |
| 120 $ | CS | 3 348 | 24 494 | 43 291 | 66 795 | CS | CS | CS | 7 667 | 48 432 |
| 140 $ | CS | 7 844 | 32 343 | 54 540 | 83 021 | CS | CS | 1 401 | 12 826 | 61 003 |
| 160 $ | 2 621 | 12 440 | 40 077 | 65 819 | 99 318 | CS | CS | 4 888 | 17 876 | 73 565 |
| 180 $ | 6 458 | 17 052 | 47 905 | 76 965 | 115 451 | CS | 2 353 | 8 431 | 22 972 | 86 128 |
| 200 $ | 10 151 | 21 691 | 55 856 | 88 191 | 131 697 | CS | 5 398 | 11 995 | 28 126 | 98 793 |
| 65 years | ||||||||||
| 100 $ | CS | CS | 7 673 | 14 224 | 22 710 | CS | CS | CS | CS | 11 788 |
| 120 $ | CS | 1 688 | 13 647 | 21 334 | 31 920 | CS | CS | CS | CS | 18 187 |
| 140 $ | CS | 5 828 | 19 576 | 28 434 | 41 349 | CS | CS | CS | 2 922 | 24 715 |
| 160 $ | 1 064 | 9 960 | 25 486 | 35 614 | 50 822 | CS | CS | 488 | 6 359 | 31 295 |
| 180 $ | 4 686 | 14 139 | 31 345 | 42 810 | 60 345 | CS | CS | 3 414 | 9 874 | 37 839 |
| 200 $ | 8 235 | 18 344 | 37 249 | 49 994 | 70 059 | CS | 1 507 | 6 356 | 13 433 | 44 382 |
| 70 years | ||||||||||
| 100 $ | CS | CS | 6 489 | 11 977 | 18 662 | CS | CS | CS | CS | 6 578 |
| 120 $ | CS | 3 517 | 12 759 | 19 026 | 26 835 | CS | CS | CS | CS | 12 122 |
| 140 $ | CS | 8 287 | 19 014 | 26 071 | 35 096 | CS | CS | CS | 1 531 | 17 638 |
| 160 $ | 2 884 | 12 982 | 25 241 | 33 217 | 43 540 | CS | CS | CS | 4 794 | 23 262 |
| 180 $ | 6 983 | 17 770 | 31 446 | 40 397 | 51 967 | CS | CS | 2 322 | 8 142 | 28 963 |
| 200 $ | 11 097 | 22 509 | 37 651 | 47 589 | 60 467 | CS | 498 | 5 345 | 11 513 | 34 667 |
| 75 years | ||||||||||
| 100 $ | CS | CS | 217 | 6 431 | 14 717 | CS | CS | CS | CS | CS |
| 120 $ | CS | CS | 6 649 | 13 531 | 22 971 | CS | CS | CS | CS | 2 327 |
| 140 $ | CS | 5 272 | 13 078 | 20 750 | 31 439 | CS | CS | CS | CS | 7 122 |
| 160 $ | CS | 11 006 | 19 604 | 28 101 | 40 086 | CS | CS | CS | 1 436 | 12 127 |
| 180 $ | 4 492 | 16 696 | 26 148 | 35 515 | 48 764 | CS | CS | CS | 5 109 | 17 214 |
| 200 $ | 9 457 | 22 290 | 32 659 | 42971 | 57 628 | CS | CS | 2 260 | 8 805 | 22 435 |
| 80 years | ||||||||||
| 100 $ | CS | 1 440 | 8 414 | 14 995 | 24 843 | CS | CS | CS | CS | 1 238 |
| 120 $ | CS | 8 904 | 16 492 | 24 060 | 35 479 | CS | CS | CS | CS | 6 616 |
| 140 $ | 4 739 | 16 314 | 24 594 | 33 231 | 46 389 | CS | CS | CS | 2 807 | 12 147 |
| 160 $ | 11 471 | 23 585 | 32 758 | 42 483 | 57 379 | CS | CS | 1 175 | 7 203 | 17 856 |
| 180 $ | 18 038 | 30 791 | 40 952 | 51 828 | 68 355 | CS | CS | 5 253 | 11 661 | 23 675 |
| 200 $ | 24 461 | 38 023 | 49 162 | 61 164 | 79 723 | CS | 2 717 | 9 281 | 16 146 | 29 630 |
| 85 years | ||||||||||
| 100 $ | 1 538 | 12 753 | 20 428 | 28 498 | 41 271 | CS | CS | CS | CS | 6 854 |
| 120 $ | 10 580 | 22 376 | 31 013 | 40 526 | 55 661 | CS | CS | CS | 4 826 | 13 360 |
| 140 $ | 19 343 | 31 855 | 41 575 | 52 584 | 70 095 | CS | CS | 4 392 | 10 394 | 20 133 |
| 160 $ | 27 814 | 41 316 | 52 256 | 64 758 | 84 823 | CS | 3 158 | 9 522 | 16 053 | 26 970 |
| 180 $ | 36 051 | 50 716 | 62 889 | 77 032 | 99 751 | CS | 8 061 | 14 643 | 21 784 | 34 035 |
| 200 $ | 44 151 | 60 056 | 73 533 | 89 362 | 114 693 | 2 694 | 12 894 | 19 800 | 27 617 | 41 170 |
V.3.2 Results: Epidemiology
The number needed to vaccinate (NNV) - the number of people that should be vaccinated to prevent a single case of HZ, PHN, ophthalmic HZ and hospitalization - was calculated as the number of people vaccinated divided by the number of events prevented. Fewer vaccinations were required for RZV compared to LZV across all ages. Figure 8 displays the NNV to reduce a case of HZ, PHN, ophthalmic HZ and hospitalization. At different ages, the NNV is relatively stable for RZV for all outcomes. LZV requires more people to be vaccinated to prevent a case of HZ, PHN and ophthalmic HZ at older ages (≥80 years old). For hospitalization, LZV requires relatively more people to be vaccinated for ages 50-65 and ≥80 years compared to 70-75 year olds.
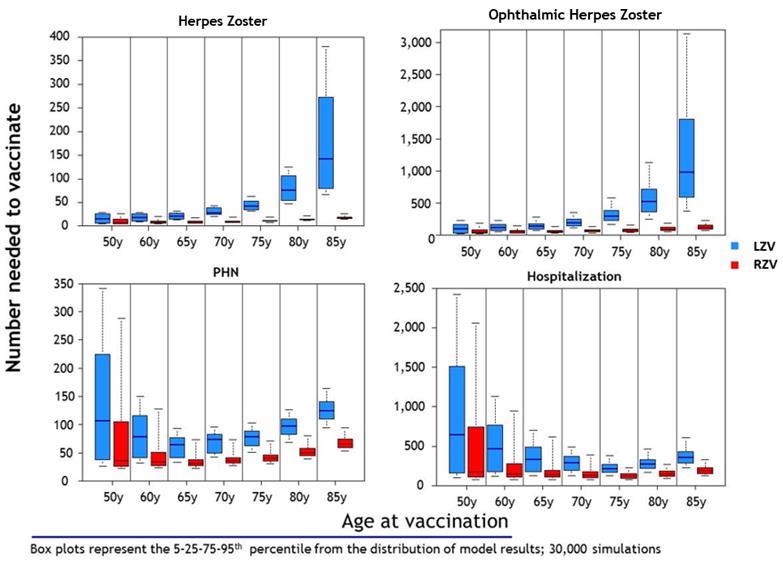
Figure 8 - Text description
| Age at vaccination | LZV Percentiles of model predictions |
RZV Percentiles of model predictions |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | 5th | 25th | Median | 75th | 95th | |
| 50 years | ||||||||||
| Herpes zoster | 6 | 6 | 15 | 26 | 28 | 5 | 5 | 7 | 14 | 26 |
| PHN | 26 | 37 | 106 | 225 | 341 | 22 | 26 | 36 | 105 | 288 |
| Hospitlization | 103 | 162 | 638 | 1511 | 2419 | 84 | 108 | 171 | 742 | 2061 |
| Herpes zoster Ophthalmic | 34 | 43 | 103 | 173 | 230 | 29 | 36 | 49 | 9626 | 193 |
| 60 years | ||||||||||
| Herpes zoster | 9 | 10 | 18 | 26 | 28 | 6 | 7 | 8 | 11 | 21 |
| PHN | 31 | 41 | 78 | 116 | 150 | 23 | 27 | 33 | 51 | 128 |
| Hospitlization | 119 | 178 | 463 | 771 | 1136 | 84 | 111 | 149 | 275 | 947 |
| Herpes zoster Ophthalmic | 56 | 74 | 122 | 168 | 229 | 34 | 43 | 54 | 76 | 150 |
| 65 years | ||||||||||
| Herpes zoster | 13 | 14 | 21 | 28 | 31 | 6 | 7 | 8 | 10 | 18 |
| PHN | 33 | 41 | 64 | 77 | 93 | 23 | 27 | 31 | 38 | 73 |
| Hospitlization | 124 | 179 | 335 | 491 | 700 | 82 | 107 | 137 | 191 | 613 |
| Herpes zoster Ophthalmic | 76 | 102 | 138 | 185 | 285 | 37 | 46 | 57 | 75 | 138 |
| 70 years | ||||||||||
| Herpes zoster | 21 | 24 | 28 | 39 | 43 | 7 | 9 | 9 | 11 | 19 |
| PHN | 42 | 50 | 73 | 83 | 96 | 27 | 31 | 35 | 40 | 73 |
| Hospitlization | 133 | 191 | 289 | 374 | 494 | 83 | 106 | 130 | 173 | 385 |
| Herpes zoster Ophthalmic | 123 | 157 | 196 | 251 | 362 | 43 | 54 | 65 | 85 | 139 |
| 75 years | ||||||||||
| Herpes zoster | 32 | 35 | 42 | 53 | 63 | 9 | 10 | 11 | 12 | 19 |
| PHN | 51 | 62 | 78 | 89 | 102 | 31 | 36 | 40 | 46 | 71 |
| Hospitlization | 126 | 172 | 215 | 267 | 378 | 75 | 95 | 116 | 152 | 226 |
| Herpes zoster Ophthalmic | 171 | 230 | 295 | 386 | 586 | 48 | 61 | 77 | 103 | 161 |
| 80 years | ||||||||||
| Herpes zoster | 47 | 54 | 75 | 106 | 125 | 11 | 13 | 14 | 15 | 22 |
| PHN | 68 | 82 | 97 | 109 | 126 | 40 | 45 | 50 | 57 | 80 |
| Hospitlization | 169 | 221 | 269 | 333 | 466 | 95 | 119 | 145 | 184 | 267 |
| Herpes zoster Ophthalmic | 257 | 365 | 523 | 721 | 1136 | 60 | 77 | 96 | 125 | 190 |
| 85 years | ||||||||||
| Herpes zoster | 67 | 80 | 142 | 273 | 380 | 15 | 17 | 18 | 20 | 25 |
| PHN | 94 | 110 | 124 | 140 | 164 | 52 | 59 | 66 | 74 | 94 |
| Hospitlization | 229 | 290 | 351 | 421 | 604 | 125 | 156 | 188 | 234 | 328 |
| Herpes zoster Ophthalmic | 377 | 590 | 983 | 1801 | 3133 | 79 | 101 | 124 | 159 | 237 |
V.3.3 Results: Sensitivity analysis
Univariate sensitivity analyses were performed for the key model parameters (e.g. percentage of HZ cases developing PHN, QALYs lost to PHN). To do so, the model fixed one key parameter value to its minimum or maximum value and varied all other parameters using triangular probability distribution. This procedure was repeated for all key parameters. This was performed at different vaccine costs (price plus administration) of $140 and $200 for both vaccines.
Epidemiological parameters
Key parameters varied in the univariate sensitivity analyses are: percentage of HZ cases developing PHN cases, PHN QALY lost, HZ incidence, hospitalization and percentage of all events among immunocompetent individuals (Figures 9, 10, 11 and 12). A low burden of illness from the minimum parameter values resulted in worse cost effectiveness (more cost per QALY), compared to the base case, because there are fewer cases to prevent. On the other hand, the maximum parameter values demonstrated a higher burden of illness translating to more prevented cases and therefore better cost effectiveness (lower cost per QALY). Nonetheless the magnitude of the ICERs, and conclusions, was not largely different than the base case ICER for both vaccines. However for LZV at $200 (price plus administration) which is more than the retail price and the negotiated price may be lower, the ICER was approximately $50,000 (base case approximately $37,000) when minimum values (lower burden) were used for key epidemiological parameters except hospitalisations.
Economic parameters
Key economic parameters varied were: cost of treatment per PHN episode, hospitalization, consultations, HZ treatment per episode and on the discount rate (Figures 13, 14, 15 and 16). The minimum and maximum values of each parameter resulted in stable median ICERs, and did not change conclusions, compared to the base case for LZV and RZV.
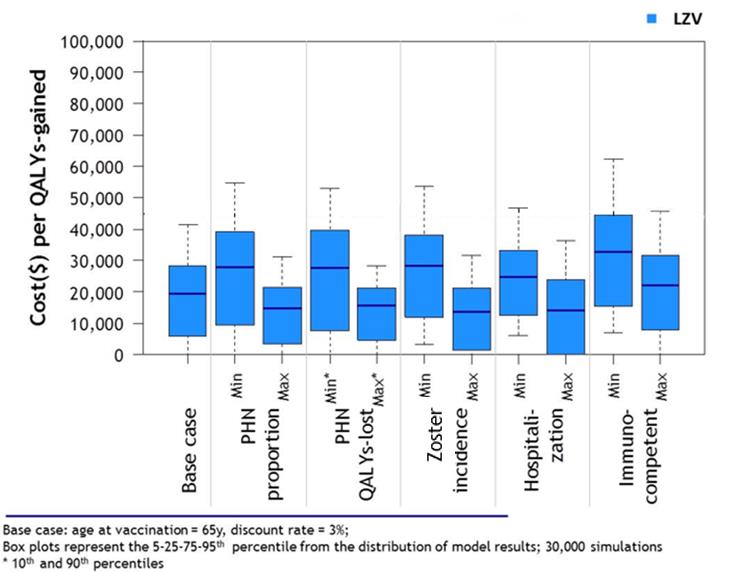
Figure 9 - Text description
| Parameters varied | LZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | CS | 5 828 | 19 576 | 28 434 | 41 349 |
| Proportion PHN min | CS | 9 486 | 27 840 | 39 188 | 54 900 |
| Proportion PHN max | CS | 3 509 | 14 760 | 21 436 | 31 088 |
| QALYs lost PHN min | CS | 7 591 | 27 518 | 39 594 | 52 996 |
| QALYs lost PHN max | CS | 4 625 | 15 656 | 21 406 | 28 413 |
| HZ incidence min | 3 218 | 11 871 | 28 217 | 38 193 | 53 451 |
| HZ incidence max | CS | 1 346 | 13 697 | 21 196 | 31 535 |
| Hospitalizations min | 6 207 | 12 380 | 24 725 | 33 084 | 46 842 |
| Hospitalizations max | CS | CS | 14 320 | 23 787 | 36 491 |
| Immunocompetent min | 6 873 | 15 610 | 32 836 | 44 548 | 62 448 |
| Immunocompetent max | CS | 7 827 | 22 135 | 31 635 | 45 684 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
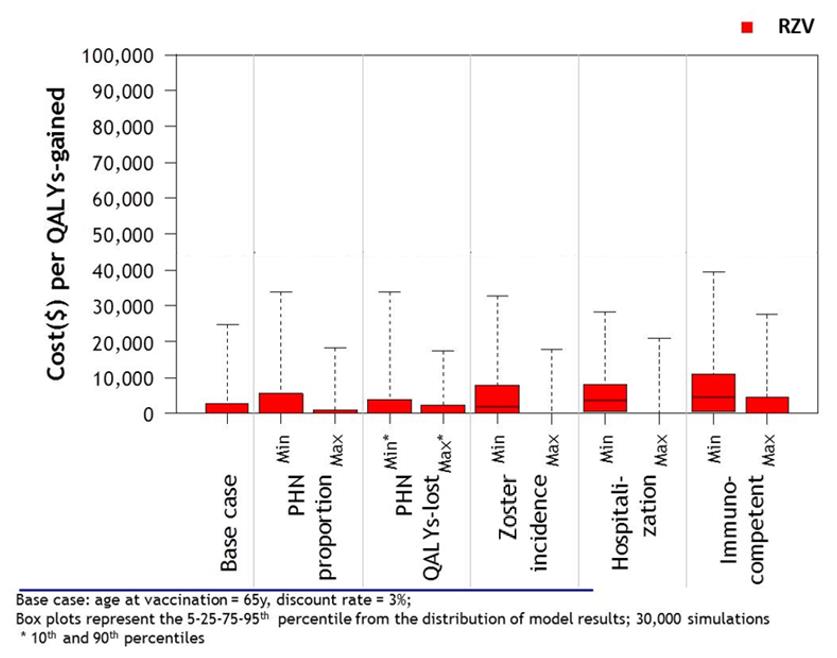
Figure 10 - Text description
| Parameters varied | RZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | CS | CS | CS | 2 922 | 24 715 |
| Treatment/PHN episode min | CS | CS | CS | 5 673 | 33 889 |
| Treatment/PHN episode max | CS | CS | CS | 1 166 | 18 191 |
| Hospitalizations min | CS | CS | CS | 3 933 | 33 849 |
| Hospitalizations max | CS | CS | CS | 2 359 | 17 604 |
| Consultations min | CS | CS | 1 835 | 7 831 | 32 990 |
| Consultations max | CS | CS | CS | CS | 17 994 |
| Treatment/HZ episode min | CS | 752 | 3 671 | 8 287 | 28 213 |
| Treatment/HS episode max | CS | CS | CS | CS | 21 080 |
| Discount rate 0% | CS | 564 | 4 716 | 11 010 | 39 464 |
| Discount rate 5% | CS | 7 827 | CS | 4 543 | 27 629 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
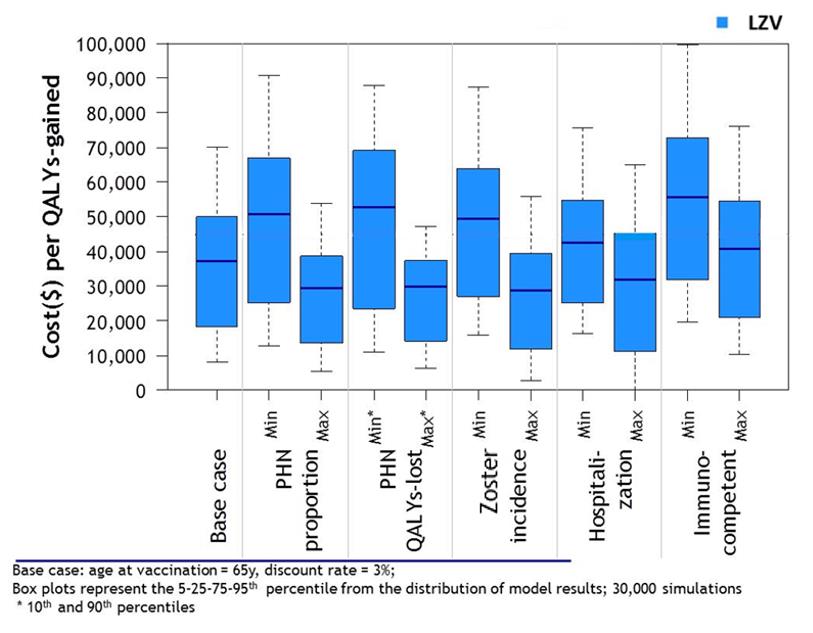
Figure 11 - Text description
| Parameters varied | LZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | 8235 | 18344 | 37249 | 49994 | 70059 |
| Proportion PHN min | 12597 | 25247 | 50803 | 66789 | 90787 |
| Proportion PHN max | 5364 | 13608 | 29242 | 38783 | 53821 |
| QALYs lost PHN min | 10892 | 23615 | 52727 | 69056 | 87860 |
| QALYs lost PHN max | 6527 | 14250 | 29869 | 37398 | 47227 |
| HZ Incidence min | 15987 | 27073 | 49431 | 63973 | 87371 |
| HZ Incidence max | 2915 | 11854 | 28962 | 39538 | 55750 |
| Hospitalizations min | 16308 | 25248 | 42407 | 54724 | 75753 |
| Hospitalizations max | 218 | 11174 | 31893 | 45208 | 64856 |
| Immunocompetent min | 19877 | 31785 | 55579 | 72709 | 99659 |
| Immunocompetent max | 10555 | 20949 | 40773 | 54485 | 75968 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||

Figure 12 - Text description
| Parameters varied | RZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | CS | 1507 | 6356 | 13433 | 44382 |
| Treatment/ PHN episode min | CS | 3909 | 9990 | 18902 | 59157 |
| Treatment/ PHN episode max | CS | CS | 3945 | 9643 | 34022 |
| Hospitalizations min | CS | 1985 | 8183 | 17458 | 60081 |
| Hospitalizations max | CS | 1187 | 5066 | 10460 | 31386 |
| Consultations min | 933 | 7384 | 12525 | 20625 | 56469 |
| Consultations max | CS | CS | 1786 | 7999 | 34829 |
| Treatment/ HZ episode min | 4535 | 8761 | 12631 | 19245 | 48011 |
| Treatment/ HZ episode max | CS | CS | CS | 7469 | 40679 |
| Discount rate 0% | 4473 | 10703 | 15969 | 24885 | 65366 |
| Discount rate 5% | CS | 3438 | 8350 | 15653 | 48629 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
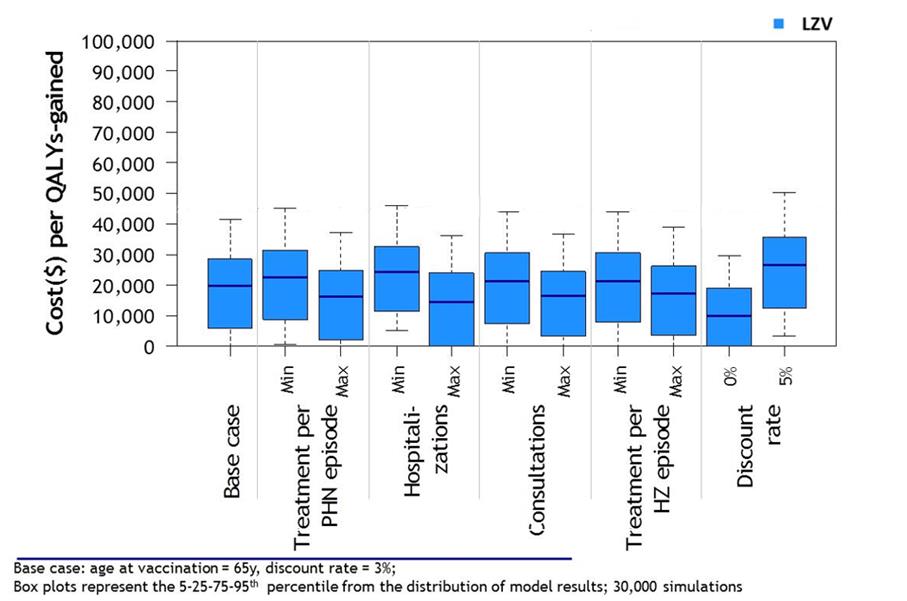
Figure 13 - Text description
| Parameters varied | LZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5e | 25e | Median | 75e | 95e | |
| Base Case Scenario | CS | 5828 | 19 576 | 28 434 | 41 349 |
| Treatment/PHN episode min | 450 | 8 695 | 22 420 | 31 447 | 45 143 |
| Treatment/PHN episode max | CS | 2 180 | 16 166 | 24 674 | 37 176 |
| Hospitalizations min | 5 135 | 11 257 | 24 081 | 32 450 | 45 865 |
| Hospitalizations max | CS | CS | 14 572 | 23 994 | 36 329 |
| Consultations min | CS | 7 228 | 21 417 | 30 385 | 44 082 |
| Consultations max | CS | 3 262 | 16 340 | 24 622 | 36 548 |
| Treatment/HZ episode min | CS | 7 744 | 21 383 | 30 461 | 43 845 |
| Treatment/HZ episode max | CS | 3 662 | 17 478 | 26 170 | 38 812 |
| Discount rate 0% | CS | CS | 9 830 | 19 036 | 29 650 |
| Discount rate 5% | 3 356 | 12 449 | 26 593 | 35 586 | 50 347 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
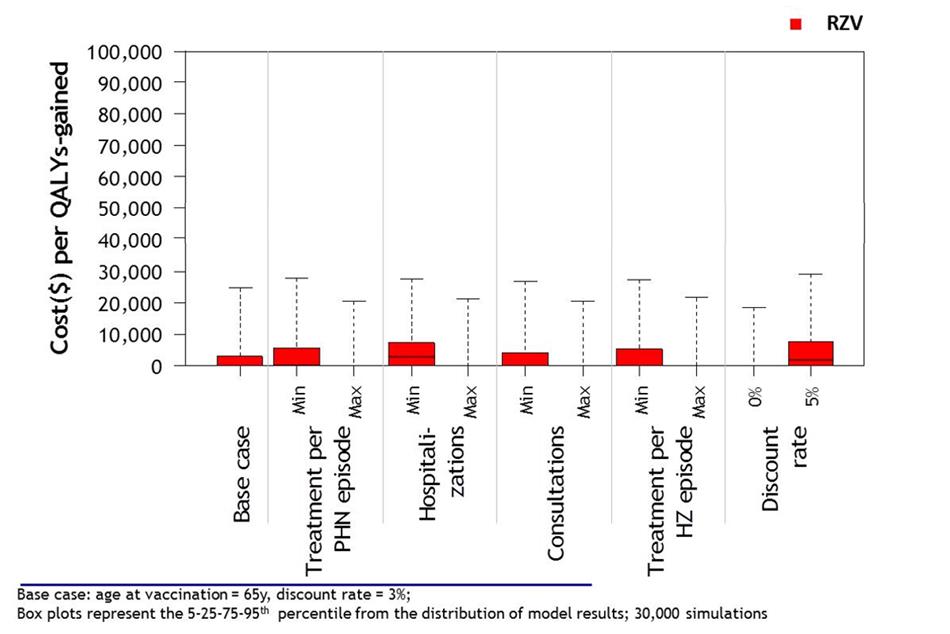
Figure 14 - Text description
| Parameters varied | RZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5e | 25e | Median | 75e | 95e | |
| Base Case Scenario | CS | CS | CS | 2 922 | 24 715 |
| Treatment/PHN episode min | CS | CS | 276 | 5 657 | 27 801 |
| Treatment/PHN episode max | CS | CS | CS | CS | 20 600 |
| Hospitalizations min | CS | CS | 2 656 | 7 348 | 27 565 |
| Hospitalizations max | CS | CS | CS | CS | 21 331 |
| Consultations min | CS | CS | CS | 4 289 | 26 717 |
| Consultations max | CS | CS | CS | 192 | 20 543 |
| Treatment/HZ episode min | CS | CS | CS | 5 322 | 27 488 |
| Treatment/HZ episode max | CS | CS | CS | 105 | 21 583 |
| Discount rate 0% | CS | CS | CS | CS | 18 384 |
| Discount rate 5% | CS | CS | 1 843 | 7 551 | 29 093 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
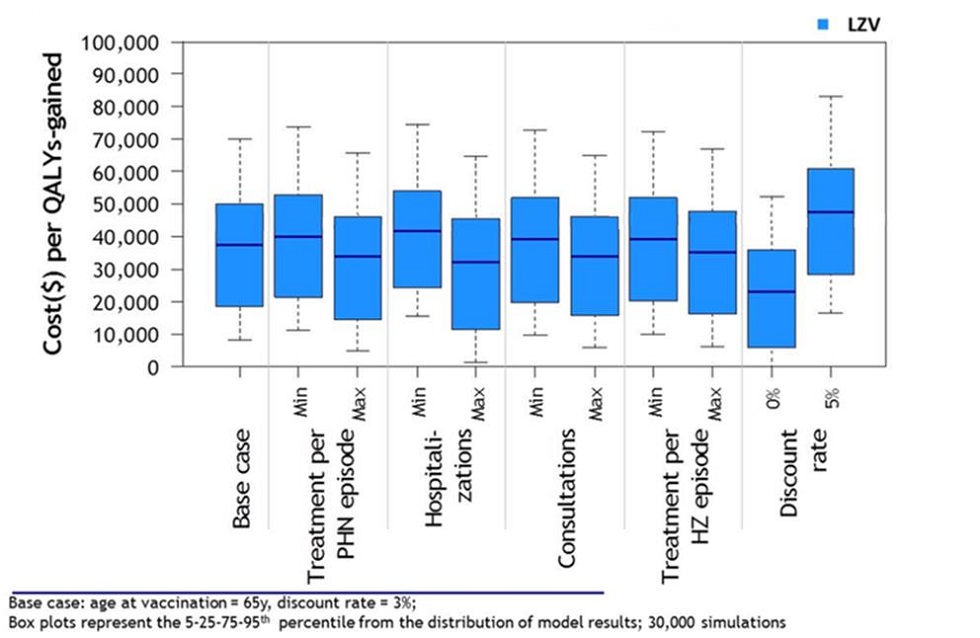
Figure 15 - Text description
| Parameters varied | LZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | 8235 | 18344 | 37249 | 49994 | 70059 |
| Treatment/PHN episode min | 11065 | 21263 | 40092 | 53000 | 73737 |
| Treatment/PHN episode max | 4850 | 14530 | 33893 | 46110 | 65627 |
| Hospitalizations min | 15269 | 24124 | 41754 | 54103 | 74649 |
| Hospitalizations max | 1182 | 11199 | 32165 | 45385 | 64497 |
| Consultations min | 9506 | 19601 | 39027 | 51930 | 72707 |
| Consultations max | 5882 | 15627 | 33903 | 46144 | 65000 |
| Treatment/HZ episode min | 9986 | 20303 | 39014 | 52045 | 72402 |
| Treatment/HZ episode max | 6210 | 16056 | 35141 | 47641 | 66898 |
| Discount rate 0% | CS | 5898 | 23111 | 35918 | 52175 |
| Discount rate 5% | 16370 | 28123 | 47368 | 60865 | 83201 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
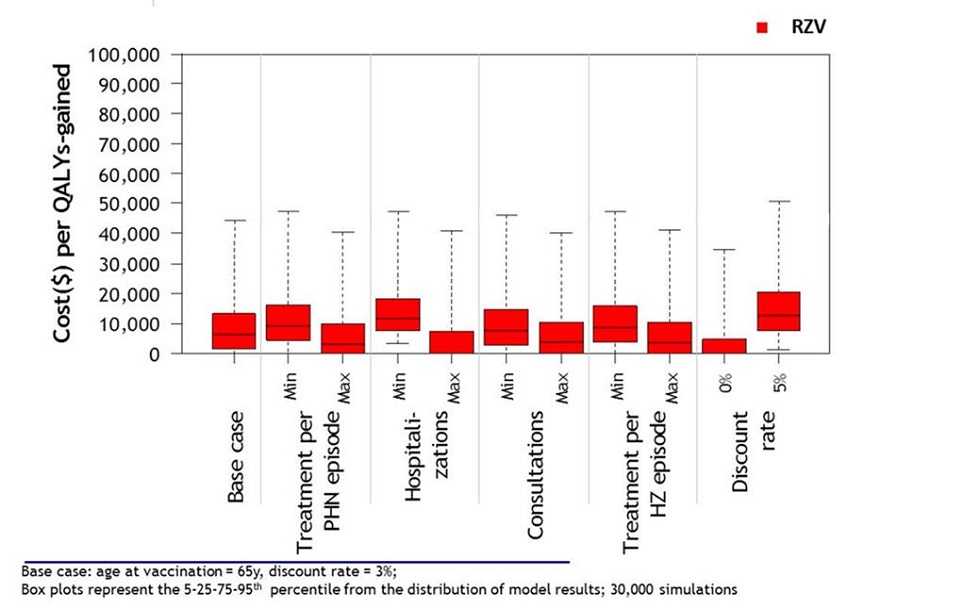
Figure 16 - Text description
| Parameters varied | RZV Percentiles of model predictions |
||||
|---|---|---|---|---|---|
| 5th | 25th | Median | 75th | 95th | |
| Base Case Scenario | CS | 1507 | 6356 | 13433 | 44382 |
| Treatment/PHN episode min | CS | 4324 | 9088 | 16285 | 47551 |
| Treatment/PHN episode max | CS | CS | 2887 | 9756 | 40539 |
| Hospitalizations min | 3401 | 7687 | 11653 | 18246 | 47322 |
| Hospitalizations max | CS | CS | CS | 7437 | 40807 |
| Consultations min | CS | 2822 | 7670 | 14870 | 46550 |
| Consultations max | CS | CS | 3773 | 10539 | 40173 |
| Treatment/HZ episode min | CS | 3930 | 8719 | 15900 | 47400 |
| Treatment/HZ episode max | CS | CS | 3553 | 10461 | 41206 |
| Discount rate 0% | CS | CS | CS | 4605 | 34648 |
| Discount rate 5% | 1289 | 7694 | 12754 | 20575 | 51280 |
CS : cost-saving; HZ : Herpes Zoster; PHN : Post-herpetic neuralgia |
|||||
V.4 Study Limitations
The model used data on health care costs of HZ and PHN that are incomplete for Canada. Although Canada has variability in healthcare costs thus leading to uncertainty in cost parameters, sensitivity analysis did not find that these costs have an impact on model conclusions. The baseline results presumed 100% compliance for 2 doses of RZV reflecting the clinical trials, however post-market realities are not likely to yield such a high compliance rate for both doses. The study did not take into account the potential impact of varicella vaccination on HZ incidence. It has been suggested that by reducing primary varicella incidence through varicella vaccination, universal varicella vaccination will lead to a short to medium term increase in zoster incidence among age groups that do not receive varicella vaccinationFootnote 11 Footnote 112 . If this occurs, the results in this study will be conservative and underestimate the cost effectiveness of a HZ vaccinationFootnote 11 .
VI. Recommendations
Following the review of available evidence summarized above and in the Management Options Table below (Table 9) comparing the HZ vaccines currently authorized for use in Canada, NACI makes the following recommendations for public health level and individual level decision-making. (While in this statement, the recommendations for both levels of decision-making are essentially the same, the rationale and context are somewhat different.)
Please note:
- A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present.
- A discretionary recommendation may be considered for some populations/individuals in some circumstances. Alternative approaches may be reasonable.
Please see Table 11 for a more detailed explanation of strength of NACI recommendations and grade of the body of evidence.
NACI will continue to monitor the scientific developments related to Herpes Zoster vaccines, including studies related to immunocompromised populations, and will update recommendations as evidence evolves.
VI.1 Recommendations for Public Health Program Level Decision-Making
(i.e. Provinces/Territories making decisions for publicly funded immunization programs)
In considering these recommendations and for the purposes of publicly funded program implementation, provinces and territories may take into account other local operational factors (e.g. current immunization programs, resources). Recognizing that there are differences in operational contexts across Canada, jurisdictions may wish to refer to Management Options Table 10 below for a summary of the relative merits of vaccinating different age cohorts (e.g. with respect to epidemiology and cost-effectiveness) if prioritization of targeted immunization programs is required for implementation.
RZV: Recommendations for Public Health Program Level Decision-Making
1. NACI recommends that Recombinant Zoster Vaccine should be offered to populations ≥ 50 years of age without contraindications. (Strong NACI Recommendation)
Summary of Evidence and Rationale:
- Age is the predominant risk factor for the development of HZ and PHN, and hospitalization among HZ cases. Steep increases in HZ incidence and PHN risk per HZ case occur over 50 years of age. Peak hospitalization rates for HZ and PHN risk per HZ case are observed among persons 65 years of age and older.
- Protection against HZ decreases with age at, and time since, vaccination with Live Zoster Vaccine (LZV) whereas VE of the newly authorized Recombinant Zoster Vaccine (RZV) remains higher and appears to decline more slowly than VE of LZV across all age groups.
- RZV VE against incident HZ and PHN in the three years post-immunization appears to be double that observed for LZV overall.
- RZV VE against incident HZ in the four years post immunization remains consistent, with no significant decreases observed over time; in contrast, significant waning of protection has been observed one-year post immunization with LZV.
- Four-year VE against incident HZ does not vary significantly across age groups for RZV; in contrast, LZV is significantly less effective in adults over 70 years of age compared to adults 50-59 years of age.
- Both vaccines are safe in immunocompetent individuals. Due to the adjuvant in RZV, which induces a high cellular immune response and helps address the natural, age-related decline in immunity, the RZV vaccine is more reactogenic than LZV. Grade 3 local and systemic reactions (i.e. severe enough to interfere with normal activities) have been more frequently reported following the receipt of RZV than LZV, but these reactions have been transient (lasting 2-3 days).
- Both LZV and RZV are immunogenic (though there are no established correlates of protection and study results must be interpreted with caution). For LZV, immune response appears more robust for those 50-59 years of age than for older age groups, but remains the same across all age groups over 50 years for RZV. Immunogenicity has been demonstrated up to 9 years post-vaccination with RZV compared to 3 years post-vaccination with LZV.
- Both LZV and RZV are cost effective compared to no vaccination (determined through a Cost Utility Analysis), and are most cost effective (lowest cost/QALY) in those 65-79 years of age. RZV was found to be more cost effective than LZV, even taking into account possible reactogenicity of RZV and non-compliance of a second dose of the vaccine.
- From a program implementation perspective, resources will be required to implement a 2-dose schedule (at 0, 2-6 months) for RZV (vs. a 1-dose schedule for LZV), and provide counseling on the reactogenicity of the RZV vaccine. Public health programs may consider a 0, 12-month schedule if it will improve coverage of the 2nd dose by simultaneous administration with other adult vaccines. Though in a small studyFootnote 60 this schedule did not meet non-inferiority criteria to a 0, 2-month schedule (as the 0, 6-month schedule did), it was found to have an acceptable safety profile and robust anti-gE immune response.
NACI considered various factors related to the HZ vaccines currently authorized for use in Canada (outlined in the Management Options Table 9). Both LZV and RZV are safe, immunogenic, and effective in preventing HZ and PHN. On balance, NACI felt that the higher efficacy of the RZV vaccine in adults 50 years of age and older, with minimal waning of protection, and factoring in cost-effectiveness of the immunization, all supported a public health program level recommendation to vaccinate populations ≥ 50 years of age. This population is at higher risk of HZ and PHN and will likely continue to be protected with RZV at older ages as the risk of HZ and PHN continues to increase. From a public health program level perspective, RZV has been shown to be more cost effective than LZV. Programs will require strategies (e.g. education, recalls/reminders) to ensure adherence to the two-dose schedule for RZV (as VE and duration of protection is unclear after only one dose), and provide counseling on short-term reactogenicity of the vaccine. If, due to operational constraints, prioritization of targeted immunization programs is required for implementation, jurisdictions may wish to refer to Management Options Table 10 below for a summary of the relative merits of vaccinating different age cohorts (e.g. with respect to epidemiology and cost-effectiveness).
2. NACI recommends that Recombinant Zoster Vaccine should be offered to populations ≥ 50 years of age without contraindications who have previously been vaccinated with Live Zoster Vaccine. (Strong NACI Recommendation)
2a. NACI recommends that for adults ≥ 50 years of age who have previously been immunized with LZV, re-immunization with 2 doses of RZV may be considered at least one year after LZV. (Discretionary Recommendation)
Summary of Evidence and Rationale:
- For the reasons outlined above, including good evidence on higher VE of RZV across all age groups (especially among older age groups) and minimal waning of protection after vaccination with RZV compared to LZV (which is particularly important given the increased incidence of HZ and PHN with age), NACI concludes that prior recipients of LZV will benefit from increased protection with RZV.
- VE of LZV wanes after the first year post-immunization.
- At this time, there is limited evidence on minimal and recommended intervals between LZV and RZV. A recently published study of adults ≥65 years of age vaccinated with RZV revealed comparable immunogenicity and reactogenicity in those who were vaccinated with LZV at least 5 years previously vs those who had never received LZV. No safety concerns were evident within 1 month of the completed 2-dose RZV schedule. Shorter intervals between the 2 vaccines have not been studied.
- In general, inactivated vaccines may be administered concomitantly with, or at any time before or after, other live vaccines protecting against a different disease. There are no guidelines for intervals between an inactivated and live vaccine protecting against the same diseaseFootnote 91 .
- The minimum interval shown to be safe and effective between doses of RZV is 2 months; similar data do not exist regarding minimum intervals between LZV and RZV.
Prior recipients of LZV vaccine will derive additional protection from completion of the 2-dose series of RZV given higher and more durable VE across age groups. Comparable safety, reactogenicity and immunogenicity have been demonstrated between those who have previously been vaccinated with LZV and those who have not. For those who have previously been vaccinated with LZV, consideration of the interval between LZV and RZV vaccination will depend on age of vaccination with LZV (since VE decreases with age), as well as time since LZV vaccination (since efficacy wanes after the first year). Based on limited evidence summarized above, NACI suggests re-immunization with 2 doses of RZV after one year post LZV administration due to rapidly declining LZV effectiveness after the first year post-vaccination. While the only published study to date investigating immunization with RZV following LZV used an interval of at least 5 years, there is no reason to believe that a shorter interval would be harmful.
3. NACI recommends that Recombinant Zoster Vaccine should be offered to populations ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation)
3a.NACI recommends that for adults ≥ 50 years of age who have had a previous episode of HZ, immunization with 2 doses of RZV may be considered at least one year after the HZ episode. (Discretionary Recommendation)
Summary of Evidence and Rationale:
- In its 2014 Advisory Committee Statement, NACI recommended that LZV may be administered to individuals with a previous episode of HZ (based on Grade B evidence), at least one year after the HZ episode (based on expert opinion). Please see the 2014 NACI statement for a summary of this evidence.
- As summarized in the 2014 NACI statement on HZ, recurrent episodes of HZ have been confirmed in immunocompetent individuals and some studies suggest that the risk of HZ in those with a prior history is comparable to the risk in those without a history of HZ. Therefore this population is still at risk for HZ and is likely to benefit from the protection afforded by vaccinationFootnote 60.
- A reported history of a previous occurrence of HZ may be incorrect as no laboratory evaluations to confirm a diagnosis exist.
- Currently there is only one study (rated as poor quality) that investigated immunogenicity and safety of RZV among patients with prior HZ infection. In this study, immune responses to, and the safety profile of RZV in adults ≥ 50 years with a physician-documented history of HZ were consistent with those observed in those ≥50 years without a documented history of HZ. No formal comparisons by time since prior HZ episode were made in this study.
- In its 2014 recommendations, NACI concluded that there was insufficient evidence to recommend for or against the administration of HZ vaccine in individuals with a history of HZO. Although causality was difficult to determine, cases of HZO had been reported after administration of LZV.
Similar to its 2014 recommendation for LZV, NACI recommends immunization with RZV in individuals with a prior episode of HZ. Individuals with a prior episode of HZ are still at risk of HZ, and a history of HZ is unreliable, therefore vaccination with RZV in those who report a prior history of HZ may be beneficial. Furthermore, one study has shown no differences in safety or immunogenicity of RZV in individuals with a prior episode of HZ. In the absence of evidence on an appropriate interval, NACI maintains its previous suggestion of waiting at least one year post HZ episode prior to the administration of herpes zoster vaccine. No studies on RZV in individuals with a previous episode of Herpes Zoster Ophthalmicus (HZO) have been conducted.
LZV: Recommendations for Public Health Program Level Decision-Making
4. NACI recommends that Live Zoster Vaccine may be considered for immunocompetent populations ≥ 50 years of age without contraindications, when Recombinant Zoster Vaccine is contraindicated or unavailable. (Discretionary NACI Recommendation)
Summary of Evidence and Rationale:
- NACI concludes (as it has in previous Herpes Zoster advisory committee statements) that there is good evidence to recommend immunization with LZV in adults aged ≥60 years (Grade A Evidence). However, the recommendation on the use of this vaccine in immunocompetent populations ≥ 60 years of age is now "Discretionary" due to the comparative evidence on higher efficacy, longer duration of protection, and relative cost effectiveness of the newly authorized RZV vaccine (summarized above and in the Management Options Table 9).
- Although LZV is safe and efficacious in 50-59 year olds and was previously recommended by NACI on a discretionary basis for this age group, waning protection of the vaccine means that it may not provide optimal ongoing protection at older ages where the risk of HZ and PHN are greatest. With the newly authorized RZV vaccine and its higher efficacy and longer duration of protection in this age group, NACI now strongly recommends that RZV be used in 50-59 year olds in addition to adults ≥60 years without contraindications.
- LZV vaccine may still be considered in individuals in whom RZV vaccine is contraindicated (i.e. known hypersensitivity to any component of the vaccine), or if RZV is not available. LZV has been authorized in Canada since 2008 and has been shown to be safe, immunogenic, and effective.
Other recommendations regarding the use of LZV vaccine in the 2014 NACI Statement on the Use of Herpes Zoster Vaccine (recommendations #3-5 and #9 regarding administration of LZV in those with a previous episode of HZ or HZO, booster dose, and co-administration with Pneu-P-23) are still relevant, and may be found on the Statement on the Use of Herpes Zoster Vaccine.
RZV vs LZV in Immunocompromised Populations: Recommendations for Public Health Program Level Decision-Making
5. NACI recommends that Recombinant Zoster Vaccine (not Live Zoster Vaccine) may be considered for immunocompromised adults ≥ 50 years of age. (Discretionary NACI Recommendation)
Summary of Evidence and Rationale:
- Individuals who are immunocompromised, either due to underlying conditions or immunosuppressive agents, have an increased risk of developing HZ and may be more likely to experience atypical and/or more severe disease and complications.
- Although, in general, immunocompromised individuals should not receive live vaccines because of the risk of disease caused by the vaccine strains, NACI has previously recommended the use of LZV in individuals on low dose immunosuppressive therapy and anti-TNF biologics on a case-by-case basis. The recommendation was made in the absence of an inactivated vaccine and on the assumption that individuals have existing immunity to varicella-zoster virus.
- In immunocompromised individuals, because antigens in the vaccine cannot replicate, NACI generally recommends the use of inactivated vaccines over live vaccines.
- The magnitude and duration of vaccine-induced immunity are often reduced in immunocompromised individuals.
- In general, experts in immunodeficiency recommend vaccines like RZV to patients with immunodeficiency even when the efficacy in this population is uncertain. This is based on the assumption that the vaccine will not do any harm and may do some good, and that immunocompromised individuals are not homogeneous and often will have some responsiveness.
- Immunocompromise is a contraindication for LZV. While there are currently limited peer-reviewed, published data specifically supporting the use of RZV in immunocompromised populations, immunocompromise is not a contraindication for the use of RZV.
Unlike with LZV, immune compromise is not a contraindication for RZV. Based on the burden of illness of HZ in immunocompromised individuals and general guidance on the use of inactivated vaccines versus live vaccines in those who are immunocompromised (summarized above), NACI feels that the benefits of considering vaccination with RZV (instead of LZV) in those who are immunocompromised outweighs the risks at this time.
NACI will monitor the evidence as it evolves and will reassess individual level and public health program level recommendations in immunocompromised individuals and populations as soon as the evidence from ongoing trials (in different immunocompromised populations ≥18 years of age with differing 2- and 3-dose schedules) becomes available.
VI.2 Recommendations for Individual Level Decision-Making
(i.e. Individuals wishing to prevent HZ, or clinicians wishing to advise individual patients about preventing HZ with vaccines that may not currently be included in public health immunization programs.)
RZV: Recommendations for Individual Level Decision-Making
1. NACI recommends that Recombinant Zoster Vaccine should be offered to individuals ≥ 50 years of age without contraindications. (Strong NACI Recommendation)
Summary of Evidence and Rationale:
(See points above in Recommendation #1 for Public Health Program Level Decision-Making)
On balance, NACI felt that the higher efficacy of the RZV vaccine in adults 50 years of age and older, and minimal waning of protection supports an individual-level recommendation to vaccinate individuals ≥ 50 years of age who are at higher risk of HZ and PHN and will likely continue to be protected with RZV at older ages as the risk of HZ and PHN continues to increase. From an individual level perspective, individuals wishing to prevent HZ or clinicians wishing to advise patients should consider the decision points outlined in the Management Options Table 9 when making a decision as well as the individual cost of RZV vs LZV vaccines. Individuals should be prepared to adhere to a 2 dose schedule for the RZV vaccine (as VE and duration of protection is unknown after only one dose), and understand that they may experience more short term reactogenicity from the RZV vaccine. Management Options Table 10 outlines the relative merits of vaccinating with RZV at different ages, primarily from a health care system perspective.
2. NACI recommends that Recombinant Zoster Vaccine should be offered to individuals ≥ 50 years of age without contraindications who have previously been vaccinated with Live Zoster Vaccine. (Strong NACI Recommendation)
2a. NACI recommends that for adults ≥ 50 years of age who have previously been immunized with LZV, re-immunization with 2 doses of RZV may be considered at least one year after LZV. (Discretionary Recommendation)
Summary of Evidence and Rationale:
(See points above in Recommendation #2 and 2a for Public Health Program Level Decision-Making)
Prior recipients of LZV vaccine will derive additional protection from the completion of a 2-dose series of RZV given higher and more durable VE across age groups. Comparable safety, reactogenicity and immunogenicity have been demonstrated between those who have previously been vaccinated with LZV and those who have not. For those who have previously been vaccinated with LZV, consideration of the interval between LZV and RZV vaccination will depend on age of vaccination with LZV (since VE decreases with age), as well as time since LZV vaccination (since efficacy wanes after the first year). Based on limited evidence summarized above, NACI suggests re-immunization with 2 doses of RZV at least one year year post LZV administration due to rapidly declining LZV effectiveness after the first year post-vaccination. While the only published study to date investigating immunization with RZV following LZV used an interval of at least 5 years, there is no reason to believe that a shorter interval would be harmful.
3. NACI recommends that Recombinant Zoster Vaccine should be offered to individuals ≥ 50 years of age without contraindications who have had a previous episode of HZ. (Strong NACI Recommendation)
3a. NACI recommends that for adults ≥ 50 years of age who have had a previous episode of HZ, immunization with 2 doses of RZV may be considered at least one year after the HZ episode. (Discretionary Recommendation)
Summary of Evidence and Rationale:
(See points above in Recommendation #3 and 3a for Public Health Program Level Decision-Making)
HZ vaccination is still beneficial in individuals who report a prior history of HZ since individuals with a prior episode of HZ are still at risk of HZ. Furthermore, one study has shown no differences in safety or immunogenicity of RZV in individuals with a prior episode of HZ. In the absence of evidence on an appropriate interval, NACI maintains its previous suggestion of waiting at least one year post HZ episode prior to the administration of herpes zoster vaccine.
LZV: Recommendations for Individual Level Decision-Making
4. NACI recommends that Live Zoster Vaccine may be considered for immunocompetent individuals ≥ 50 years of age without contraindications, when Recombinant Zoster Vaccine is contraindicated, unavailable or inaccessible. (Discretionary NACI Recommendation)
Summary of Evidence and Rationale:
(See points above in Recommendation #4 for Public Health Program Level Decision-Making)
LZV vaccine may be considered in individuals in whom RZV vaccine is contraindicated, unavailable, or in individuals who prefer this vaccine over RZV vaccine after reviewing the decision points as outlined in the Management Options Table 9 (e.g. individuals who will not complete the 2-dose schedule for RZV vaccine, or for whom RZV is too expensive). LZV has been authorized in Canada since 2008 and has been shown to be safe, immunogenic, and effective. However, based on comparative evidence on higher efficacy and longer duration of protection against HZ with the newly authorized RZV vaccine, especially in older age groups as the risk of HZ and PHN increase, NACI's recommendation for LZV is "discretionary" (see Table 11 for a description of the strength of NACI recommendations).
Other recommendations regarding the use of LZV vaccine in the 2014 NACI Statement on the Use of Herpes Zoster Vaccine (recommendations #3-5 and #9 regarding administration of LZV in those with a previous episode of HZ or HZO, booster dose, and co-administration with Pneu-P-23) are still relevant, and may be found here.
RZV vs LZV in Immunocompromised Individuals: Recommendations for Individual Level Decision-Making
5. NACI recommends that Recombinant Zoster Vaccine (not Live Zoster Vaccine) may be considered for immunocompromised adults ≥ 50 years of age based on a case-by-case assessment of benefits vs risks. (Discretionary NACI Recommendation)
(See points above in Recommendation #5 for Public Health Program Level Decision-Making)
Immune compromise is a contraindication for the use of LZV, but not for the use of RZV. Based on the burden of illness of HZ in immunocompromised individuals and general guidance on the use of inactivated vaccines versus live vaccines in those who are immunocompromised (summarized above), NACI feels that the benefits of considering vaccination with RZV (vs LZV) in immunocompromised individuals on a case-by-case basis outweighs the risks at this time.
NACI will monitor the evidence as it evolves and will reassess individual level and public health program level recommendations in immunocompromised individuals and populations as soon as the evidence from ongoing trials (in different immunocompromised populations ≥18 years of age with differing 2- and 3-dose schedules) becomes available.
VI.3 Management Options
There are two vaccines authorized for use in Canada for the prevention of HZ in those 50 years of age and older. The decision on which vaccine option is preferable depends on the key considerations for each vaccine, and a comparison of the relative merits of both, as summarized in Table 9 below.
| Options LZV vs RZV |
Factors for Consideration | Decision Points |
|---|---|---|
| 1. LZV | Efficacy against HZ (VE [95%CI]) Based on clinical trial data:
Efficacy against PHN (VE [95% CI]
- VE against HZ 51% in ≥60 year olds; decreases with age at receipt of vaccine Duration of protection against HZ Effectiveness against HZ [95% CI] Immunogenicity Safety Economics Feasibility/Acceptability |
- LZV has been authorized for use in Canada and elsewhere (e.g. U.S. Europe, UK) for over a decade and NACI recommendations for the use LZV have been in place since 2010. RZV has recently been authorized for use in Canada and the U.S. in October 2017. Epidemiology Duration of Protection Unknowns: Immunogenicity Unknowns: Safety Unknowns: Economics - The additional dose required for the RZV immunization schedule will require additional administrative costs Feasibility/Acceptability Unknowns: |
| 2. RZV | Efficacy against HZ (VE [95%CI]) (Based on 2 large Phase 3 RCT)
Efficacy against PHN (VE [95%CI])
Duration of protection against HZ Immunogenicity Safety (The following based on 2 large Phase 3 RCT and smaller studies)Footnote fFootnote g
Cost-Effectiveness Feasibility/Acceptability Issues |
|
|
||
Management Options Table 10 summarizes the relative merits of vaccinating different age cohorts if prioritization of targeted immunization programs is required for implementation.
| Options Age Cohorts |
Factors for Consideration | Decision Points |
|---|---|---|
| 50-64 year olds | Efficacy against HZ (VE [95%CI])
Efficacy against PHN (VE [95%CI])
Epidemiology (The following numbers related to HZ incidence, hospitalization and PHN risk are baseline parameter values used in the economic analysis, derived from the literature) HZ Incidence (per 1,000 person-yrs [min, max]) Footnote c Footnote d Footnote e Footnote f Footnote g Footnote h
HZ Hospitalizations (per case [min, max]) Footnote c Footnote f Footnote i
PHN Risk (per case [min,max]) Footnote c Footnote j
Economics Higher Incremental Cost Effectiveness Ratio (ICER) implies lower cost effectiveness. i.e. pay more per unit of QALY Median ICER (cost per QALY) for RZV
|
50-64 year olds
|
| 65-79 year olds | 65-79 year olds
|
|
| ≥80 year olds | ≥80 year olds
|
|
|
||
VII. Research priorities
Research to address the following outstanding questions is encouraged:
New and emerging research priorities
- What is the vaccine effectiveness and duration of protection after one dose of RZV vaccine?
- What is the duration of protection after two doses of RZV vaccine (beyond 4 years)?
- What is the vaccine immunogenicity, efficacy, effectiveness, and safety of RZV vaccine in immunocompromised populations <50 years of age and >50 years of age?
- How will vaccination with RZV affect individuals with a prior history of HZO?
- How do LZV and RZV vaccines compare in head to head trials?
- What will HZ vaccine effectiveness, efficacy, immunogenicity and safety be in cohorts vaccinated with varicella vaccine in childhood (and not exposed to wild type VZV)?
- What is the immunological correlate of protection against herpes zoster disease and PHN?
- What is the immunogenicity of a 0, 12-month schedule of RZV? (Additional studies with larger study populations would be helpful.)
- What is the safety, immunogenicity, and efficacy of an interval shorter than 5 years between a dose of RZV and LZV in those who have been previously vaccinated with LZV?
- Are there safety, efficacy or immunogenicity concerns with co-administration of RZV and other vaccines such as Pneu-P-23, Tdap, adjuvanted influenza?
Standing research priorities
From the 2014 NACI Statement on LZV:
- Persistence of VE in persons >50 years of age.
- The need for booster doses of HZ vaccine in the long-term.
- Efficacy of immunization on persons with prior history of HZ.
- Assessing safety of HZ vaccine in individuals with a prior history of HZO and the association of HZ vaccine with the recurrence of HZO.
- What are the vaccine efficacy, effectiveness, and safety of HZ vaccines in immunocompromised populations?
- Further study on co-administration of HZ vaccine and Pneu-P-23.
VIII. Surveillance issues
Ongoing and systematic data collection, analysis, interpretation and timely dissemination is fundamental to planning, implementation, evaluation, and evidence-based decision-making. To support such efforts, NACI encourages surveillance improvements in the following areas:
- Epidemiology
- Examination of the Canadian burden and epidemiology of herpes zoster and its complications over time in the general population, and among cohorts vaccinated with varicella vaccine in childhood
- Evaluation of the impact of HZ vaccination in provinces and territories on HZ burden, complications, and epidemiology
- Vaccine (coverage, adverse events)
- HZ vaccination coverage among adults 50 years and older in provinces and territories
- Compliance rate of 2nd dose of RZV vaccine
- Long term safety of RZV vaccine
- Attitudes and behaviours
- Impact of reactogenicity of RZV on attitudes and behaviours of patients and providers
Tables
Summary of Evidence Tables for primary studies can be found in the Appendices.
| STRENGTH OF NACI RECOMMENDATION Based on factors not isolated to strength of evidence (e.g. public health need) |
GRADE OF EVIDENCE Based on assessment of the body of evidence |
|---|---|
Strong
OR Known/Anticipated disadvantages outweigh known/anticipated advantages ("should not")
|
A - good evidence to recommend |
| B - fair evidence to recommend | |
| C - conflicting evidence, however other factors may influence decision-making | |
| D - fair evidence to recommend against | |
| E - good evidence to recommend against | |
| I - insufficient evidence (in quality or quantity), however other factors may influence decision-making | |
Discretionary
|
A - good evidence to recommend |
| B - fair evidence to recommend | |
| C - conflicting evidence, however other factors may influence decision-making | |
| D - fair evidence to recommend against | |
| E - good evidence to recommend against | |
| I - insufficient evidence (in quality or quantity), however other factors may influence decision-making |
| Level | Description |
|---|---|
| I | Evidence from randomized controlled trial(s). |
| II-1 | Evidence from controlled trial(s) without randomization. |
| II-2 | Evidence from cohort or case-control analytic studies, preferably from more than one centre or research group using clinical outcome measures of VE. |
| II-3 | Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence. |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees. |
| Quality Rating | Description |
|---|---|
| Good | A study (including meta-analyses or systematic reviews) that meets all design-specific criteriaFootnote * well. |
| Fair | A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criterionFootnote * but has no known "fatal flaw". |
| Poor | A study (including meta-analyses or systematic reviews) that has at least one design-specificFootnote * "fatal flaw", or an accumulation of lesser flaws to the extent that the results of the study are not deemed able to inform recommendations. |
|
|
List of abbreviations
- AE
- Adverse Effect
- AS
- Adjuvant System
- BGTD
- Biologics and Genetic Therapies Directorate
- BOI
- Burden of Illness
- CUA
- Cost Utility Analysis
- CIHR
- Canadian Institutes of Health Research
- CMI
- Cell-Mediated Immunity
- CI
- Confidence Interval
- CKD
- Chronic Kidney Disease
- DSEN
- Drug Safety and Effectiveness Network
- GM
- Geometric Mean
- GMR
- Geometric Mean Ratio
- GMRI
- Geometric Mean Ratio Increase
- GP
- General Practitioner
- HR
- Hazard Ratio
- HSCT
- Hematopoietic Stem Cell Transplantation
- HZ
- Herpes Zoster
- HZWG
- Herpes Zoster Working Group
- HZO
- Herpes Zoster Ophthalmicus
- ICER
- Incremental Cost-Effectivness Ratio
- IM
- Intramuscular Administration
- IR
- Incidence Rate
- LZV
- Live Zoster Vaccine
- MAGIC
- Methods and Applications Group for Indirect Comparisons
- NACI
- National Advisory Committee on Immunization
- NNV
- Number Needed to Vaccinate
- PHN
- Post-Herpetic Neuralgia
- PICOS
- Population, Intervention, Comparator, Outcomes and Study design
- Pneu-P-23
- Pneumococcal polysaccharide 23-valent vaccine
- PY
- Person Years
- QALY
- Quality Adjusted Life Years
- RAMQ
- Regie de l'Assurance Maladie du Quebec
- RCF
- Responder Cell Frequency
- RR
- Relative Risk
- RZV
- Recombinant Zoster Vaccine
- SAE
- Serious Adverse Effect
- SAAE
- Serous Autoimmune Adverse Event
- SC
- Subcutaneous Administration
- SFC
- Spot Forming Cells
- SPS
- Shingles Prevention Study
- STPS
- Short-Term Persistence Substudy
- TIV
- Trivalent Influenza Vaccine
- UI
- Uncertainty Intervals
- VE
- Vaccine Efficacy
- VZV
- Varicella Zoster Virus
Acknowledgments
This statement was prepared by: Dr. S. Ismail, Dr. M. Tunis, Dr. O. Baclic, Dr. M. K. Doll, Dr. J. Hu, Dr. R. Warrington, Mr. K. Eng, Mr. S. Duchesne-Belanger, and approved by NACI.
Herpes Zoster Working Group Members: Dr. R. Warrington (Chair), Dr. S. Deeks, Dr. P. De Wals, Dr. K Dooling, K. Eng, Dr. J. Gallivan, Dr. S. Ismail, M. Landry, Dr. C. Rotstein, Dr. C Sauvageau, Dr. S. E Straus, Dr. M. Tunis.
NACI Members: Dr. C. Quach (Chair), Dr. W. Vaudry (Vice-Chair), Dr. N. Dayneka, Dr. P. De Wals, Dr. S. Deeks, Dr. V. Dubey, Dr. R. Harrison, Dr. M. Lavoie, Dr C. Rotstein, Dr. M. Salvadori, Dr. B. Sander, Dr. N. Sicard, Dr. R. Warrington.
Liaison Representatives: Dr. J. Brophy (Canadian Association for Immunization Research and Evaluation [CAIRE]), Dr. E. Castillo (Society of Obstetricians and Gynaecologists of Canada), Dr. A. Cohn (Centers for Disease Control and Prevention, United States), Ms. T. Cole (Canadian Immunization Committee), Dr. J. Emili (College of Family Physicians of Canada), Dr. K. Klein (Council of Chief Medical Officers of Health), Dr. C. Mah (Canadian Public Health Association), Dr. D. Moore (Canadian Paediatric Society), Dr. A. Pham-Huy (Association of Medical Microbiology and Infectious Disease [AMMI] Canada).
Ex-Officio Representatives:, Dr. (LCdr) K. Barnes (National Defence and the Canadian Armed Forces), Ms. G. Charos (Centre for Immunization and Respiratory Infectious Diseases [CIRID], Public Health Agency of Canada [PHAC]), Dr. G. Coleman (Biologics and Genetic Therapies Directorate [BGTD], Health Canada [HC]), Dr. J. Gallivan (Marketed Health Products Directorate [MHPD], HC), Ms. J. Pennock (CIRID, PHAC), Mr. G. Poliquin (National Microbiology Laboratory), Dr. T. Wong (First Nations and Inuit Health Branch [FNIHB], HC).
NACI gratefully acknowledges the contribution of: The team from University of Laval, Centre de recherché du CHU de Quebec, and INSPQ for contributions to the economic analysis including Dr. M. Brisson, Dr. Z. Zhou, Dr. M. Drolet, Dr. C. Sauvageau, Dr. P. De Wals, Dr. V. Gilca, Dr. JF. Laprise, and Dr. R. Amini. This team, however, are not the authors of the economic section in the Statement.
Ms. J. Chor, Ms. A. Fleurant, and Ms. C. Mauviel (CIRID, PHAC), Ms. L. Gamble (Health Library, HC) for supporting the immunogenicity search strategy, and the MAGIC team for their contribution to the safety, effectiveness, and efficacy analysis including Dr. A. C. Tricco, Dr. S. E. Straus, Ms. W. Zarin, Dr. R. Cardoso, Dr. A.A. Veroniki, Dr. P. A. Khan, Dr. V. Nincic, Mr. M. Ghassemi, Ms. R. Warren, Ms. J. Sharpe and Dr. A. Page. The safety, effectiveness, efficacy literature search strategy was developed and peer-reviewed by librarians Dr. E. Cogo and Dr. J. McGowan.
Appendices: Summary of Evidence Tables
(See Tables 12 and 13 of the NACI Advisory Committee Statement on Updated Recommendations on the Use of Herpes Zoster for details on the ranking of level of evidence and quality of individual studies as summarized in the Summary of Evidence Tables, below.)
Appendix A: Summary of Evidence Related to Efficacy and Effectiveness of Herpes Zoster Vaccines
- LZV (Zostavax®)
- Immunocompetent individuals
- Immunocompromised individuals
- RZV (Shingrix®)
- Immunocompetent Individuals
Appendix B: Summary of Evidence Related to Immunogenicity of Herpes Zoster Vaccines
- LZV (Zostavax®)
- General population
- Immunocompromised
- RZV (Shingrix®)
- Head to Head Comparison of LZV and RZV
- Concomitant Administration with Other Vaccines
Appendix C: Summary of Evidence Related to Safety of Herpes Zoster Vaccines
- LZV (Zostavax®)
- Immunocompetent individuals
- RZV (Shingrix®)
- Immunocompetent individuals
Appendix A: Summary of Evidence Related to Efficacy and Effectiveness of Herpes Zoster Vaccines
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
| Langan et al, 2013 | Zostavax® | Age Number (immunocompetent): Antiviral definition group: General definition group: |
Analyses were adjusted for age, gender, race, low income, immunosuppression, and important comorbidities associated with zoster, and then stratified by immunosuppression status. Cohort was followed for a total of 1,233,333 Person Years (PY). Results: Zoster vaccine effectiveness against incident HZ: Antiviral definition:
Vaccinated:
General definition:
Vaccinated:
Zoster vaccine effectiveness against incident PHN after 30 days (adjusted for age, gender, race, immunosuppression status, low income, COPD, IBD, kidney disease, diabetes mellitus, rheumatoid arthritis, and SLE): Antiviral definition: Unvaccinated:
Vaccinated:
General definition: Unvaccinated:
Vaccinated:
Zoster vaccine effectiveness against incident PHN after 90 days (adjusted for age, gender, race, immunosuppression status, low income, COPD, IBD, kidney disease, diabetes mellitus, rheumatoid arthritis, and SLE): Antiviral definition: Unvaccinated:
Vaccinated:
General definition: Unvaccinated:
Vaccinated:
|
II-2 | Fair | |
| Langan et al, 2016 | Zostavax® | Cohort study (5% random sample of adults enrolled in US Medicare from 2007 to 2009) | Age Number: Comorbidities: |
Analysis conducted on total of 1,320,100 PYs of follow-up. CKD was present in 24% of individuals (183,762). Zoster vaccine effectiveness against incident HZ, adjusted for age, gender, race, low income, immunosuppression, immune-mediated disorders and COPD: Overall: Unvaccinated:
Vaccinated:
With Chronic Kidney Disease: Unvaccinated:
Vaccinated:
With Diabetes Mellitus: Unvaccinated:
Vaccinated:
With CKD and Diabetes Mellitus: Unvaccinated:
Vaccinated:
|
II-2 | Fair |
| Marin et al, 2015 | Zostavax® | Matched case-control study | Age Number Pre-Exposure History: Vaccinated and not vaccinated |
Vaccination was associated with 54% (95% CI:32%-69%) reduction in HZ incidence, 58% (95% CI:31%-75%) reduction in HZ HZ vaccine was statistically significant effective at preventing postherpetic neuralgia (PHN) measured at 30 days after rash onset, 61% (95% CI: 22%-80%). Among persons who developed HZ, no differences were found by vaccination status in severity or duration of HZ pain after rash onset. Vaccine effectiveness against Herpes Zoster (HZ) overall and by age at vaccination and against other HZ-related outcomes: Case-patient vs Controls; Vaccine Efficacy (VE) (95% CI)
|
II-2 | Fair |
| Oxman et al, 2005 | Vaccine: live attenuated Oka/Merck Placebo: not stated |
Randomized, placebo-controlled, double-blind clinical trial (SPS study) | Age Number Pre-Exposure History: |
During the mean duration of HZ surveillance of 3.13 years, reduction in the Burden of Illness (BOI) due to HZ was estimated to be 61.1% (51.1-69.1), PHN 66.5% (47.5-79.2), and HZ incidence 51.3% (44.2-57.6). Results: The Effect of Zoster Vaccine on the BOI in HZ in the Modified Intention-to-Treat Population: Vaccine Group: All subjects:
60-69 yr:
70 yr:
Male:
Female:
Placebo Group: All subjects:
60-69 yr:
70 yr:
Male:
Female:
The Effect of Zoster Vaccine on PHN in the Modified Intention-to-Treat Population: Vaccine Group: All subjects (n=19,254):
60-69 yr (n=10,370):
70 yr (n=8,884):
Male (n= 11,390):
Female (n=7,864):
30-day Persistence of PHN among all subjects:
60-day Persistence of PHN among all subjects:
90-day Persistence of PHN among all subjects:
120-day Persistence of PHN among all subjects:
182-day Persistence of PHN among all subjects:
Placebo Group: All subjects (n=19,247):
60-69 yr (n=10,356):
70 yr (n=8,891):
Male (n= 11,337):
Female (n=7,910):
30-day Persistence of PHN among all subjects:
60-day Persistence of PHN among all subjects:
90-day Persistence of PHN among all subjects:
120-day Persistence of PHN among all subjects:
182-day Persistence of PHN among all subjects:
|
I | Good |
| Oxman et al, 2008 | Vaccine: live attenuated Oka/Merck Placebo: not stated |
Randomized, placebo-controlled, double-blind clinical trial (SPS study) | Age: Number: Pre-Exposure History: |
During the mean duration of HZ surveillance of 3.13 years, HZ vaccine reduced the HZ BOI by 61.1% (95% [CI], 51.1%-69.1%; P <.001) and reduced the incidence of PHN by 66.5% (95% CI, 47.5%-79.2%; P <.001). The incidence of HZ was also reduced by 51.3% (95% CI, 44.2%-57.6%; P <.001). Results: HZ VE for the HZ BOI: All subjects (95% CI):
60-69 yr:
70 yr or more:
HZ VE for the incidence of HZ: All subjects (95% CI):
60-69 yr:
70 yr or more:
HZ VE for the Incidence of PHN: All subjects (95% CI):
60-69 yr:
70 yr or more:
|
I | Good |
| Schmader et al, 2012 | Vaccine: Zostavax® Placebo: all Zostavax®vaccine constituents except VZV or virus components |
Randomized, double-blind, placebo-controlled study | Age Number Pre-Exposure History: |
The ZV reduced the incidence of HZ (30 cases in vaccine group, 1.99/1000 PYs vs. 99 cases in placebo group, 6.57/1000 PYs). VE against incident HZ over an average of 1.3 years follow-up was 69.8% (95% CI, 54.1-80.6). Results: ITT entire study duration (n=11,211):
ITT 0.0-0.5 years (n= 11,186):
ITT >0.5-1.0 years (n=10,954):
ITT >1.0-1.5 years (n= 10,747):
ITT >1.5 years (n= 3,743):
MITT (n=11,165):
Placebo Group (n= 11,228) ITT entire study duration (n=11,228):
ITT 0.0-0.5 years (n= 11,210):
ITT >0.5-1.0 years (n=10,953):
ITT >1.0-1.5 years (n= 10,712):
ITT >1.5 years (n= 3,728):
MITT (n=11,189):
|
I | Good |
| Schmader et al, 2012 | Vaccine: live attenuated Oka/Merck Placebo: not stated |
Follow-up to SPS double-blind randomized controlled trial (STPS study) | Age Number Pre-Exposure History: |
In the STPS analysis of 16,500 PYs follow-up involving over 14,000 adults, as compared to the SPS, VE for HZ BOI decreased from 61.1% to 50.1%, VE for the incidence of PHN decreased from 66.5% to 60.1%, and VE for the incidence of HZ decreased from 51.3% to 39.6%, although the differences were not statistically significant. Analysis of VE in each year after vaccination for all 3 outcomes showed a decrease in VE after year 1, with a further decline thereafter. VE was statistically significant for the incidence of HZ and the HZ BOI through year 5. Summary of Study Outcomes, by Year After Vaccination, in the Shingles Prevention Study (SPS) Population, the Short-Term Persistence Substudy (STPS) Population, and the Combined SPS and STPS Populations: Zoster Vaccine Group (n= 19,270): One year since randomization (n= 19,254):
Two years since randomization (n= 19,024):
Three years since randomization (n= 18,692):
Four years since randomization (n= 11,689):
Five years since randomization (n= 7,197):
Six years since randomization (n= 7,086):
Seven years since randomization (n= 4,054):
SPS Years 0-4.9 (n= 19,254):
Short-Term Persistence Study Years (STPS) 3.3-7.8 (n= 7,320):
SPS + STPS Years 0-7.8 (n= 19,254):
Placebo Group (n= 19,276): One year since randomization (n= 19,247):
Two years since randomization (n= 18,948):
Three years since randomization (n= 18,494):
Four years since randomization (n= 11,474):
Five years since randomization (n= 6,887):
Six years since randomization (n= 6,055):
Seven years since randomization (n= 2,237):
SPS Years 0-4.9 (n= 19,247):
Short-Term Persistence Study Years (STPS) 3.3-7.8 (n= 6,950):
SPS + STPS Years 0-7.8 (n= 19,247):
|
II-3 | Fair |
| Morrison et al, 2015 | Vaccine: live attenuated Oka/Merck Placebo: not stated |
Follow-up to SPS double-blind randomized controlled trial |
Age Number |
Seven years since randomization (nPYs= 6,865):
Eight years since randomization (nPYs= 6,564):
Nine years since randomization (nPYs= 6,280):
Ten years since randomization (nPYs= 5,005):
Eleven years since randomization (nPYs= 1,470):
|
II-3 | Fair |
| Tseng et al, 2011 | Zostavax® | Retrospective cohort study | Age Number Immune status: Pre-Exposure History: |
Analysis conducted for a total of 486,074 PYs. Comparison of HZ Incidence in Study Cohorts by Vaccination Status (adjusted for age, sex, race, health care utilization, and chronic disease in the model): Vaccinated Cohort (n= 75,761): Age 60-64 years (n= 23,195):
Age 65-69 years (n= 20,166):
Age 70-74 years (n=15,426):
Age 75-79 years (n= 10,978):
Age 80 or more years (n= 5,996):
Overall (n= 75,761):
Unvaccinated Cohort (n= 227,283): Age 60-64 years (n= 69,585):
Age 65-69 years (n= 60,498):
Age 70-74 years (n=46,278):
Age 75-79 years (n=32,934):
Age 80 or more years (n= 17,988):
Overall (n= 227,283):
|
II-2 | Fair |
| Tseng et al, 2012 | Zostavax® | Retrospective cohort study | Age Number: Vaccinated cohort: immunized between January 2007 and December 2010 and with Unvaccinated cohort: |
The average period from the initial HZ episode to the end of follow-up was 3.3 years. Adjusted HRs comparing incidence of recurrent HZ between the vaccinated and the unvaccinated cohort (confirmed case): Vaccinated Cohort (n= 1,036) Age <70 years (n= 533):
Age 70 or more (n= 503):
Total (n= 1,036):
Confirmed, probable and possible case: Age < 70 years (n= 533):
Age 70 or more (n= 503):
Total (n= 1,036):
Diagnosis code (electronic record): Age < 70 years (n= 533):
Age 70 or more (n= 503):
Total (n= 1,036):
Unvaccinated Cohort (n= 5,180) Age < 70 years (n= 2,665):
Age 70 or more (n= 2,515):
Total (n= 5,180):
Confirmed, probable and possible case: Age < 70 years (n= 2,665):
Age 70 or more (n= 2,515):
Total (n= 5,180):
Diagnosis code (electronic record): Age < 70 years (n= 2,665):
Age 70 or more (n= 2,515):
Total (n= 5,180):
|
II-2 | Fair |
| Tseng et al, 2015 | Zostavax® | Retrospective cohort study | Age Number |
Overall, PHN risk was 40% lower in vaccinated adults (adjusted RR, 0.59; 95% CI,.41-.85).Thirty vaccinated women (4.2%) experienced PHN, compared with 75 unvaccinated women (10.4%), with an adjusted relative risk of 0.41 (95% CI,.26-.64). PHN occurred in 26 vaccinated men (6.0%) versus 25 unvaccinated men (5.8%), with an adjusted relative risk of 1.06 (.58-1.94). These associations did not differ significantly by age. Results: Male patients aged 60-69 years (n= 162):
Male patients aged 70 or more (n= 270):
Total male patients (n= 432):
Female patients aged 60-69 years (n= 293):
Female patients aged 70 or more (n= 430):
Total female patients (n= 723):
All patients aged 60-69 years (n= 455):
All patients aged 70 or more (n= 700):
Total patients (n= 1 155):
Unvaccinated Group (n= 1 155): Male patients aged 60-69 years (n= 173):
Male patients aged 70 or more (n= 259):
Total male patients (n= 432):
Female patients aged 60-69 years (n= 316):
Female patients aged 70 or more (n= 407):
Total female patients (n= 723):
All patients aged 60-69 years (n= 489):
All patients aged 70 or more (n= 666):
Total patients (n= 1 155):
|
II-2 | Fair |
| Tseng et al, 2016 | Zostavax® | Retrospective cohort study | Age Number: Pre-exposure history: |
The effectiveness of HZ vaccine decreased from 68.7% (95% CI, 66.3%-70.9%) in the first year to 4.2% (95% CI, −24.0% to 25.9%) in the eighth year. Results: Effectiveness and 95% CI of ZV, by Year After Vaccination: 60-69 years old:
70 years and older:
Total:
Comparison of HZ incidence in study cohorts by HZ vaccination status: Vaccinated (n= 176,078) Age 60-64 (n= 72,553):
Age 65-69 (n= 41,276):
Age 70-74 (n= 25,278):
Age 75-79 (n= 18,915):
Age 80 or more (n= 18,056):
Unvaccinated (n= 528,234) Age 60-64 (n= 219,165):
Age 65-69 (n= 122,248):
Age 70-74 (n= 75,614):
Age 75-79 (n=56,809):
Age 80 or more (n= 54,398):
|
II-2 | Fair |
| Tseng et al, 2016 | Zostavax® | Retrospective cohort study | Age Number Comorbidities: |
The number of HZ cases was 16 in 1373 PYs (11.7 per 1000 PYs; 95% CI, 7.1-19.0) among the vaccinated and 126 in 5644 PYs (22.3 per 1000 PYs; 95% CI, 18.7-26.6) among the unvaccinated. The 36-month cumulative risk of incident HZ was 4.1% and 6.6%, respectively. HZ vaccination was associated with a reduced risk of HZ (adjusted HR = 0.49; 95% CI,.29-.85). The reduced risk seems more prominent if the vaccine is given within two years of dialysis initiation. Comparison of HZ incidence in ESRD patients by HZ vaccination status: Vaccinated Group (n= 582): Aged < 70 years (n= 331):
Aged 70 or more years (n= 251):
Hemodialysis (n= 496):
Peritoneal dialysis (n= 86):
< 2 years on dialysis before index date (n= 256):
2 or more years on dialysis before index date (n= 326):
Total (n= 582):
Unvaccinated Group (n= 582): Aged < 70 years (n= 1 655):
Aged 70 or more years (n= 1255):
Hemodialysis (n= 2,574):
Peritoneal dialysis (n= 336):
< 2 years on dialysis before index date (n= 1320):
2 or more years on dialysis before index date (n= 1590):
Total (n= 2910):
|
II-2 | Fair |
| McDonald et al, 2017 | Zostavax® | Retrospective cohort Study | Age 50 years of age and older Number 1,094,236 (1,005,869 immunocompetent; 636,581 50-59 years of age) |
Among 1,094,236 individuals identified in the Alberta Health Care Insurance Plan Registry (AHCIP) cohort (2009-2015), 85,439 (7.80%) received Zostavax®. HZ IR was 9.03 [95% CI: 8.95, 9.11] cases per 1,000 PY (49,243 cases). Vaccine Effectiveness from Years 1-5 since vaccination (95% CI):
|
II-2 | Fair |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
| Cunningham et al. 2016 | Vaccine: Shingrix® Placebo: 0.9% saline |
Randomized, placebo-controlled, phase 3 trials (ZOE-50 and ZOE-70) | Age Number: |
Participants received two doses of RZV or RZV Group: Placebo Group: Results: HZ
RZV Group
Placebo Group:
Postherpetic Neuralgia (PHN)
RZV Group
Placebo Group:
Vaccine effectiveness against PHN among 3,491 individuals 50-59 years of age was also reported: 100% (40.8%-100%) |
I | Good |
| Lal et al, 2015 | Vaccine: Shingrix® Placebo:0.9% saline solution |
Randomized, placebo-controlled, phase 3 study (ZOE-50) | Age Number |
Modified vaccinated cohort (n=14,759): Participants received 2 doses of vaccine 2 months apart Total vaccinated cohort (n=15,411): Participants received at least 1 vaccine. During a mean follow-up of 3.2 years, HZ was confirmed in 6 participants in the vaccine group and in 210 participants in the placebo group (IR, 0.3 vs. 9.1 per 1000PYs). Modified vaccinated cohort:
RZV Group:
Placebo Group:
Total vaccinated cohort:
RZV Group:
Placebo Group:
|
I | Good |
Appendix B: Summary of Evidence Related to Immunogenicity of Herpes Zoster Vaccines
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Gilbert et al, 2014 |
Zostavax®among 50-59 year olds |
Randomized controlled trial (subset of ZEST trial) to assess correlates of protection |
n=2491 n=1218 (vaccine group) n=1273 (placebo group) |
Anti-VZV antibodies using gpELISA measured at baseline and 6 weeks GMT in vaccine group increased from 284 (95% CI 267,303) to 662 (95% CI 627, 698); GMFR was 2.31 (95% CI 2.20, 2.43) GMT and GMFR were unchanged in placebo group |
Level I |
Good |
Levin et al, 2013 |
Zostavax®among 50-59 year olds |
Randomized, double-blind, placebo-controlled multicentre study |
n=2269 (subset of ZV efficacy trial n=22,439) n=1136 (vaccine group) n=1133 (placebo group) |
Anti-VZV antibodies through gpELISA at baseline and week 6 GMT increase from 293.1 to 660.0 from baseline to week 6 in vaccine group, a GMFR of 2.31 while antibodies were unchanged in placebo group |
Level I |
Good |
Levin et al, 2008 |
Zostavax®among 60 years and older |
Randomized, double-blind, placebo-controlled trial Denver and San Diego |
n=1395 (subset of SPS n=38,546) n=691 (vaccine group) n=704 (control group) |
CMI: Responder cell frequency (RCF) assay and spot forming cells (SFCs) (IFN-gamma) via ELISPOT at baseline, week 6, and years 1, 2, and 3 Humoral immunity: Anti-VZV antibodies with gpELISA at baseline, week 6, and years 1, 2, and 3 CMI (both measures) and humoral immunity were higher among those who received vaccine, an effect that persisted up to 3 years. RCF & SCF GMTs and Anti-VZV antibodies peaked at 6 weeks and decreased afterwards |
Level I |
Good |
Vermeulen et al, 2011 |
Zostavax®among 60 years and older |
Randomized, placebo-controlled, double-blind, trial |
n=210 (all ≥60 years) n=104 (2 doses of Zostavax®6 weeks apart) n=105 (placebo) |
CMI: IFN-gamma SFCs through ELISPOT at baseline, 2 and 6 weeks after each dose), and 6 months post-vaccination GMCs were higher among the vaccine group and peaked at 2 weeks post-vaccination 1; by 6 months post-vaccination 2, GMCs were higher than baseline but lower than peak levels Humoral immunity: Anti-VZV antibodies through gpELISA at baseline and 2 and 6 weeks after immunization Anti-VZV antibodies were higher among the vaccine group and peaked at 2 weeks post-vaccination 1 In general, a second dose of Zostavax®did not boost VZV-specific immunity |
Level I |
Good |
Weinberg et al, 2009 |
Zostavax® |
Randomized, double-blind, placebo-controlled, trial |
n=2,343 (from SPS trial) n=981 (developed zoster) n=1,362 (no zoster) |
CMI (IFN-gamma through ELISPOT) corresponded with zoster morbidity whereas humoral immunity (Anti-VZV antibodies through gpELISA) did not correspond as strongly with morbidity |
Level I |
Good |
Beals et al, 2016 |
Zostavax®(in various doses intradermally and subcutaneously) |
Randomised, partially-blinded parallel group study (there were concomitant placebo given) 3 clinics in Colorado and Florida |
n=223 6 groups (full dose & 1/3 dose subcutaneous; full dose, 1/3 dose, 1/10 dose, and 1/27 dose intradermal) ≥ 50 with a history of varicella or residing in a varicella endemic country for 30 years or more |
Anti-VZV antibodies (GMT through gpELISA, GMC through ELISPOT) pre-vaccination and at 6 weeks and 18 months Full dose subcutaneous (SC) resulted in GMFR of 1.74 (90% CI 1.48, 2.04) post 6-weeks compared to 3.25 (90% CI 2.68, 3.94) for intradermal. GMFR persisted for intradermal but not SC administration at 18 months. |
Level I |
Fair (no control group that did not receive vaccine, imbalance in gender distribution for some of the groups) |
Diez-Domingo et al, 2015 |
Zostavax®(administered subcutaneous-ly and intramuscular IM) |
Open-label non-inferiority trial |
n=354 n=177 (IM group) n=177 (SC group) |
CMI: ELISPOT assay measured for a subset of participants using at baseline and 4 weeks post-vaccination CMI was comparable between IM and SC groups Humoral immunity: VZV antibody titres measured for all participants at baseline and 4 weeks post-vaccination Humoral immunity was comparable between IM and SC groups. |
Level I |
Fair (No control group that did not receive vaccine, CMI was measured only for a subset of study population) |
Gilderman et al, 2008 |
Zostavax®(refrigerator-stable versus frozen formulation) |
Double-blind, randomized controlled trial |
n=368 initial enrollment n=182 (refrigerated vaccine) n=185 (frozen vaccine) |
Anti-VZV antibodies using gpELISA measured at baseline and 28 days GMT and GMFR for refrigerator and frozen formulations were similar |
Level I |
Fair (on control group without vaccine) |
Sutradhar et al, 2009 |
Zostavax® |
Randomized, double-blind, clinical trial |
n=1122 (from two separate multicentre trials) n=389 (50-59y years) n=733 (≥60 years) |
Anti-VZV antibodies through gpELISA at baseline and 4 weeks GMTS and GMFRs were higher among both groups following vaccination, but slightly higher among 50-59 age group - adjusting for pre-vaccination titers, GMFR ratio for 50-59 versus ≥60 was |
Level I |
Fair (no control group that did not receive vaccine) |
Vesikari et al, 2013 |
Zostavax®(1 dose and 2 doses at 0 and 1 months or 0 and 3 months) |
Phase 3, open-label, randomized trial |
n=759 (all ≥70 years) n=243 (1 dose) n=203 (2 doses 1 month apart) n=198 (2 doses 3 months apart) |
Anti-VZV antibodies through gpELISA at baseline and 4-weeks post-dose 1 and 2 and 12 months post last dose GMCs were similar between the 1 and 2-dose schedules at all time points |
Level I |
Fair (no control group that did not receive vaccine) |
Levin et al, 2016 |
Zostavax®(second dose administered 10 years after first dose) |
Non-randomized controlled study |
n=600 n=201 (prior Zostavax®, ≥70 years) n=199 (no prior Zostavax®, ≥70 years) n=100 (no prior Zostavax®, 60-70 years) n=100 (no prior Zostavax®, 50-60 years) |
CMI: SFCs (IFN-gamma & IL-2) via ELISPOT at baseline and weeks 1, 6, and 52 SFCs were significantly higher at baseline and up to 52 weeks after re-vaccination for those previously vaccinated compared to other groups, suggesting a residual effect of CMI that is enhanced by booster Humoral immunity: Anti-VZV antibodies with gpELISA at baseline and weeks 1, 6, and 52 All groups developed an increase in GMT at week 1 which peaked at week 6 while by week 52 GMTs were not significantly higher than baseline In general, baseline levels of CMI and humoral immunity were higher among younger people |
Level II-1 |
Fair (no randomization, not all outcome measures were compared) |
Arnou et al, 2011 |
Zostavax®(one dose) |
Phase IV Open-label non-randomized study of Zostavax®within 6 months of expiration 6 centres in France |
n=96 n=50 between 50-59 years; n=46 ≥ 60 years |
Anti-VZV antibodies through gpELISA pre-vaccination and 28-35 days after vaccination GMFR for the 50-59 age group was 3.9 (95% CI 3.0, 5.1) compared to 2.6 (95% CI 2.0, 3.4). |
Level II-2 |
Poor (no control group, patient characteristics not reported, no description of withdra-wals) |
Choi et al, 2016 |
Zostavax®(one dose) in Korean Adults |
Open-label, single-arm Phase 4 study |
n=180 |
VZV antibody GMT and GMFR at baseline and 4 weeks GMT increased from baseline of 66.9 (95% CI 59.2, 75.5) to 185.4 (95% CI 167.0, 205.9), representing GMFR of 2.8 (95% CI 2.3-3.1) GMFR for ≥60 was 2.6 while for 50-59 was 2.9 |
Level II-2 |
Poor (no control group, protocol deviation in 14 or 7.8% of subjects) |
Laing et al, 2015 |
Zostavax® |
Cohort |
n=12 |
Magnitude and breadth of CD4+ T-cell response at baseline and 2, 4, and 26 weeks post-vaccination Essentially, vaccination increased the magnitude (2.3 times) and breadth (4.2 times) of CD4+ cells at one-month, although levels declined by 6 months |
Level II-2 |
Poor (non-randomized, small sample size) |
Macaladad et al, 2006 |
Zostavax®among seronegative and low-seropositive adults |
Cohort study (initially conceived of as RCT, but enrollment too low) |
n=21 (adults ≥ 30 years) n=18 (vaccine group) n=3 (placebo group) |
Anti-VZV antibodies through gpELISA at baseline and week 6 Antibody response was higher in vaccine group compared to placebo, but higher among low-seropositive (GMT=25.7 units/mL) than among seronegative (GMT=12.0 units/mL) |
Level II-2 |
Poor (small sample size, very small control group) |
Patterson-Bartlett et al, 2007 |
Zostavax® |
Cohort study for phenotypic and functional characterization of T-cells |
n=25 (20 of whom are ≥ 60 years) n=10 (vaccine group) n=10 (placebo group) n=5 (young adult controls) |
Vaccine significantly increased VZV-specific Th1, memory, early effector, and cutaneous homing receptor-bearing T-cells |
Level II-2 |
Poor |
Qi et al, 2016 |
Zostavax® |
Cohort study to assess defective T-memory cell differentiation |
n=39 |
IFN-gamma ELISPOT at baseline, and day 8, 14, and 28 post-vaccination and Anti-VZV antibodies through ELISA at baseline and 28-days post-vaccination IFN-gamma T-cells increased peaked at 10 times baseline between 8 and 14 days and declined to 3 times baseline by day 28; correlation between increases in Anti-VZV antibodies and T-cell frequencies did not reach significance, suggesting these responses are independent |
Level II-2 |
Poor |
Sei et al, 2015 |
Zostavax® |
Cohort study to assess breadth, magnitude, and quality of ex vivo CD4+ & CD8+ response |
n=21 |
The response of multiple antigens to multiple types of T-cells was assessed. Authors postulate that an increase in poly-functional CD4+ and ORF9-specific CD8+ cells contribute to efficacy |
Level II-2 |
Poor |
Weinberg et al, 2017 |
Zostavax® |
Cohort study to assess differences in immune response between younger and older adults |
n=58 n=25 (25-40 years old) n=33 (60-80 years old) |
Older adults appear to have higher proportion of senescent and exhausted VZV-specific T-cells, leading to overall poor effector response to a VZV challenge. |
Level II-2 |
Poor |
Yao et al, 2015 |
Zostavax®among Taiwanese adults |
Cohort study |
n=150 |
Anti-VZV antibodies through gpELISA were higher 4 weeks post-vaccination, with a GMFR of 3.05 (95% CI 2.6, 3.6) |
Level II-2 |
Poor |
Sullivan et al, 2013 |
Zostavax® |
Cohort study comparing B and T-cell proliferation among young and old |
n=39 n=16 (25-40 years old) n=23 (60-79 years old) |
There was a transient increase in B-cell proliferation in both groups, but a significant reduction in the elderly group. There were no differences in proliferation of CD4+ or CD8+ T-cells between young and old |
Level II-2 |
N/A pending full methods |
Weinberg et al, 2015 [abstract] |
Zostavax® |
Cohort study |
n=400 (all ≥70 years) n=201 (Zostavax®≥10 years prior) n=199 (no prior Zostavax®) |
Anti-VZV antibodies increased following vaccination and GMCs were similar across both groups IFN-gamma cell counts were higher in previously vaccinated group at week 6 (peak response) and year 1 |
Level II-2 |
N/A pending full methods |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Mullane et al, 2013 |
ZVHT administered four times 30 days apart in populations with solid tumor malignancy, hematologic malignancy, HIV with CD4 <200, autologous HSCT, and allogenic HSCT |
Randomized, double-blind, placebo-controlled multicentre study |
n=262 (vaccine group) n=79 (placebo group) |
Anti-VZV antibodies through gpELISA and IFN-gamma ELISPOT counts pre-vaccination and 28 days after 4 doses GMFR for anti-VZV antibodies ranged from 0.9 to 2.4 depending on type of immunosuppression; For allogenic and autologous HSCT patients there were no changes in GMFR for anti-VZV antibodies. GMFR for IFN-gamma ELISPOT ranged from 0.2 to 9.0 depending on type of immunosuppression; For allogenic HSCT patients there was a significant decline in GMFR for IFN-gamma. |
Level I |
Good |
Russell et al, 2015 |
Zostavax®in patients on chronic / maintenance corticosteroids |
Randomized, double-blind, placebo-controlled, multicentre study |
n=314 (initial enrollment, (adults ≥60 years) n=206 (VZV group) n=101 (placebo group) |
Anti-VZV antibodies through gpELISA at baseline and 6 weeks GMFR among vaccine group was 2.3 (95% CI 2.0, 2.7), higher than that of placebo group with a GMFR of 1.1 (95% CI 1.0, 1.2) |
Level I |
Good |
Winthrop et al, 2017 |
Zostavax®among rheumatoid arthritis patients on methotrexate with and without Tofacitinb |
Randomized controlled trial |
n=112 n=55 (Tofacitinib group started 2- weeks post-vaccination) n=57 (no Tofactinib group) |
Both CMI and humoral immunity were similar among those receiving Tofacitinb and placebo at 6 weeks post vaccination: The GMFR for Anti-VZV antibodies was 2.11 in the Tofacitinib group versus 1.74 in the placebo group while the GMFR for IFN-gamma SFCs was 1.50 in the Tofacitinib group versus 1.29 in the placebo group. The magnitude of the humoral response was comparable to those seen in patients without rheumatoid arthritis while the CMI response was slightly less than in patient without rheumatoid arthritis. |
Level I |
Fair (no control group that did not receive vaccine, small sample size) |
Camacho et al, 2010 |
ZVHT administered four times 30 days apart in adults with hematologic malignancy |
Phase I randomized, double-blind, placebo-controlled study |
n=80 n=61 received ZVHT n=19 received placebo |
Anti-VZV antibodies through gpELISA and IFN-gamma ELISPOT counts pre-vaccination and 28 days after 4 doses GMFR for anti-VZV antibodies was 1.3 (90% CI 1.1, 1.5) and 2.2 (90% CI 1.4, 3.5) for IFN-gamma ELISPOT. |
Level I |
N/A |
McAdam et al, 2013 [abstract] |
Inactivated Varicella Zoster Virus vaccine - ZVin (4 doses, 30 days apart) among patients with autoimmune disease on and not on biologics |
Randomized, double-blind, placebo-controlled trial |
n~340 n~180 (ZVin at lower Ag level) n~100 (ZVin at higher Ag level) n~60 (placebo) |
Anti-VZV antibodies through gpELISA and IFN-gamma through ELISPOT at baseline, postdose 2 (half of patients), postdose 3 (other half of patients), and 4 weeks after last dose At 28 days, there were statistically significant increases for both gpELISA (GMFR 1.57) and ELISPOT (GMFR 2.01) assays |
Level I |
N/A pending full methods |
Winston et al, 2011 [abstract] |
Heat-treated zoster vaccine (ZVHT) among patients with allogenic or autologous HSCT |
Randomized, double-blind, placebo-controlled trial |
n=100 n=40 (vaccine group allogenic HSCT) n=10 (no vaccine allogenic HSCT) n=40 (vaccine group autologous HSCT) n=10 (no vaccine autologus HSCT) |
Humoral immunity as measured through VZV-specific antibodies declined among patients with allogenic and autologous HSCT. CMI as measured through IFN-gamma response were elicited among autologous HSCT patients (GMFR 7.6 at post-dose 4) but not among allogenic HASCT patients (GMR 0.2 at post-dose 4) |
Level I |
N/A pending full methods |
Wasan et al, 2016 |
Zostavax®among IBD patients on low-dose immunomo-dulators or 5-ASA or no therapy |
Cohort study of patients immunosuppressed and not |
n=39 n=14 (immunosuppressed - i.e. low-dose immunomodulators) n=25 (not immunosuppressed - i.e. 5-ASA or no therapy) |
Immunosuppressed patients had a weaker immune response (both CMI & humoral) compared those not immunosuppressed, but their response was still significant at 2 and 6 weeks post-vaccination. |
Level II-2 |
Fair (control group present, but small sample size and no randomization) |
Hata et al, 2013 |
Zostavax®among diabetes mellitus patients |
Cohort study |
n=20 n=10 (healthy volunteers) n=10 (diabetic patients) |
CMI: IFN-gamma through ELISPOT at baseline and months 3 and 6 Humoral immunity: Antibodies through immunoadherence hemagglutination (IAHA) test at baseline and months 3 and 6 No significant difference in antibody titres at 6 months between the two groups |
Level II-2 |
Poor (non-randomized trial, small sample size) |
Irwin et al, 2013 |
Zostavax®among patients with major depressive disorder (MDD) |
Cohort study |
n=92 (subset of the SPS study population) n=40 (MDD stratified by those on and not on antidepressant medications) n=52 (never mentally ill) |
CMI: VZV-RCF and IFN-gamma ELISPOT at baseline and 6, 52, and 104 weeks Among those with MDD who were treated, VZV-RCF levels at 6 weeks were similar to non-depressed controls; Among those with MDD who were not treated, VZV-RCF at 6 weeks was unchanged from baseline; no significant differences in IFN-gamma levels across time and age groups Humoral immunity: Anti-VZV antibodies using gpELISA at baseline and 6, 52, and 104 weeks No significant differences in VZV-antibody levels across time and age groups |
Level II-2 |
Poor (non-randomized, outcome reporting unclear, 12 of 52 initially selected in MDD group refused to participate) |
Parrino et al, 2017 |
Inactivated zoster vaccine (ZVin 4 dose regimen) among patients with hematologic malignancies with anti-CD20 monoclonal antibody treatment |
Open-label, single-arm Phase 1 study |
n=80 (adults ≥ 18 years) |
VZV IFN-gamma ELISPOT assay at baseline and 28-35 days postdose 4 GMFR 28-35 days postdose 4 was 4.34 (90% CI 3.0, 6.2) |
Level II-2 |
Poor (no control group) |
Kho et al, 2016 [abstract] |
Zostavax®among patients with end-stage renal disease awaiting transplant |
Cohort study |
n=53 n=26 (ESRD patients) n=27 (gender and age-matched kidney donors) |
VZV-specific IgG titres measured at baseline and 1, 3, and 12 months post-vaccination IgG titers among ESRD patients and controls were comparable and higher at all time points after baseline |
Level II-2 |
N/A pending full methods |
Wasan et al, 2012 |
Zostavax®among IBD patients on methrotrexate or thiopurines |
Cohort study of patients ≥50 years |
n=17 n=8 (low dose immunosuppres-sive therapy) n=9 (no immunosuppresive therapy) |
Immunocompetent patients with IBD were able to mount a significant humoral and CMI response while immunosuppressed patients did not mount a significant humoral response but did mount a significant but reduced CMI response. |
Level II-2 |
N/A pending full methods |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Chlibek et al, 2013 |
RZV (Two 50 ug doses 2 months apart with different amounts and types of adjuvant) |
Phase 2 randomized controlled trial Czech Republic, Spain, United States |
n=410 initial enrolment n=150 (RZV + AS01B) n=38 (saline alone) |
CMI: CD4+ T-cells with at least two activation markers) at baseline, 1, and 3 months Response highest in those with AS01B, then AS01E, then saline Humoral immunity: Serum anti-gE and Anti-VZV antibodies at baseline, 1, and 3 months Response highest in those with AS01B, then AS01E, then saline Similar immunogenicity was noted across 50-59, 60-69, and ≥70 age groups for those given AS01B |
Level I |
Good |
Leroux-Roels et al, 2012 |
RZV (two doses 2 months apart), Varilrix (two doses 2 months apart), or both |
Phase 1/2 open-label, randomized, parallel-group study Belgium |
n=155 n=135 (age 50-70) - 45 each in the RZV, Varilrix, and RZV + Varilrix groups n=20 (age 18-30) - 10 each in RZV and RZV + Varilrix groups |
CMI: CD4+ T-cells with at least 2 immune markers at baseline and months 1, 2, 3, and 12 for all patients; older adults who received RZV alone and met certain criteria were also sampled at months 30 and 42 Up to 12 months, CD4+ T-cells were higher with RZV than with Varilrix and not different between RZV and RZV + Varilrix groups By 42 months, CD4+ T-cells were lower than at 12 months but higher than baseline Humoral immunity: Anti-VZV and anti-gE titres at baseline and months 1, 2, 3, and 12 for all patients; older adults who received RZV alone and met certain criteria were also sampled at months 30 and 42 Up to 12 months, anti-VZV GMCs were higher with RZV than with Varilrix and not different between RZV and RZV + Varilrix groups; the anti-gE humoral response rate was higher than for anti-VZV By 42 months, antibody levels were lower than at 12 months but higher than baseline |
Level I |
Fair (no control group that did not receive vaccine) |
Lal et al, 2017 |
RZV (2 50 ug doses at 0/2, 0/6, and 0/12 months to assess for non-inferiority of different schedules) |
Phase 3 randomized, open-label non-inferiority trial |
n=354 initial enrollment n=117 (0/2 month group) n=116 (0/6 month group) n=113 (0/12 month group) |
Humoral immunity: Anti-gE antibodies at 1 month post-dose 2 for all groups. GMC ratios were 1.16 (97.5% CI 0.98, 1.39) and 1.19 (97.5% CI 0.93, 1.53) for the 0/2 month group to the 0/6 and 0/12 month groups respectively Authors state that non-inferiority was demonstrated for the 0/6 month administration but not the 0/12 month administration |
Level I |
Fair (open-label, no control group without vaccine) |
Vink et al, 2017 |
RZV (2 doses two months part IM and SC administration) among Japanese adults |
Phase3, open-label, randomized trial |
n=60 n=30 (subcutaneous) n=30 (IM) |
Anti-gE antibodies through ELISA at baseline and 1 and 12 months post-dose 2 There was a decline in anti-gE antibodies between 1 and 12 months post-dose 2, but an increase in levels above baseline; there was no difference between SC versus IM injection |
Level I |
Fair (small sample size) |
Diez-Domingo et al, 2016 [abstract] |
RZV (two doses 2 months apart) among European adults |
Randomized clinical trial |
n=23,289 ≥50 years (from ZOE-50 and ZOE-70 studies) |
Humoral response: anti-gE GMC at baseline and 1-month post-second dose 38.0 times increase in anti-gE above baseline CMI: CD4+ T-cell frequencies with two activation markersat baseline and 1-month post-second dose 21.2 times increase in CD42+ frequency above baseline |
Level I |
N/A pending full methods |
Grupping et al, 2017 (ID week poster) |
RZV in patients previously vaccinated (5 years ago or more) with live vaccine |
Phase 3, matched, open-label, prospective trial |
n=430 n=215 (previously vaccinated) n=215 (not previously vaccinated) |
CMI: CD4+ T-cells with at least two activation markers at baseline, 1 month post-dose 1, and 1 month post-dose 2 Humoral immunity: anti-gE antibody concentrations baseline, 1 month post-dose 1, and 1 month post-dose 2 Measure of CMI and humoral immunity were similar at baseline for the two groups; by 1 month post-dose 2, they had increased significantly. |
Level I |
N/A pending full methods |
Chlibek et al, 2016 |
RZV (Two 50 ug doses 2 months apart) |
Phase 2 open-label, single-group trial Czech Republic, Germany, Sweden, Netherlands |
n=166 initial enrollment n=129 at month 48 n=119 at month 72 |
CMI: CD4+ T-cells with at least two activation markers) at 48, 60, 72 months CD4 counts peaked at month 3 and then declined, but higher than pre-vaccination levels - Pre-vaccination:119.4 (Q1-3, 67.8, 286.9); at 36 months 640.0 (Q1-3 403.0-1,405.4); at 72 months 477.3 (Q1-3 231.4, 1,037.0) Humoral immunity: Anti-gE antibody concentrations at 48, 60, 72 months Anti-gE antibodies peaked at month 3 and then declined, but higher than pre-vaccination levels - Pre-vaccination: 1,121.3 mIU/mL (Q1-3 624.2, 2,309.0); at 72 months 8,159.0 (Q1-3 5,451.2, 12,212.4) |
Level II-2 |
Poor (no control group - at least for the 72 month arm - initial study at control groups but only measured to 36 months) |
Godeaux et al, 2017 |
RZV (two doses 2 months apart) among adults with a prior history of herpes zoster |
Phase III, non-randomized trial |
n=96 initial enrollment divided equally across 50-59, 60-69, and ≥70 |
Anti-gE GMCs and mean geometric increase at baseline and 28 days post-second dose GMC across all participants increased from 2398 (95% CI 1,779 3,233) to 47,759 (95% CI 42,259, 53, 794); mean geometric increase was 19.9 |
Level II-2 |
Poor (no |
Lal et al, 2013 |
RZV (two doses 2 months apart) |
Phase 1, open-label study Conducted in Australia but all patients were ethnically Japanese |
n=39 n=20 (age 18-30) n=19 (age 50-69) |
Anti-gE antibodies and Anti-VZV antibodies Among the older patients, anti-gE GMC increased from 2,123 to 65,589 (31-fold increase) while anti-VZV GMC increased from 1,284 to 12,883 (11-fold increase); response was higher among those aged 18 to 30 |
Level II-2 |
Poor (no control group, small sample size) |
Pauksens et al, 2017 (ID week poster) |
RZV |
Phase 3b, open-label, long-term extension cohort study with 9 years follow-up |
n=70 |
CMI (CD4+ cells with at least two activation markers) and humoral immunity (anti-gE antibody levels) peaked at month 3 but at 9 years was still higher than baseline (3.4 times for CMI and 7.4 times for humoral). Levels plateaued between years 4 and 9 |
Level II-2 |
N/A pending full methods |
| Subunit vaccine studies in immunocompromised populations (n=5) | ||||||
Berkowitz et al, 2015 |
RZV (three doses at 0, 2, 6 months) in HIV+ patients |
Phase ½, randomized, placebo controlled study |
3 cohorts of HIV positive patients n=112 completed 18 month follow-up (67 in RZV group, 45 in control group) Mean age 46, range 23-74 |
CMI: CD4+ T-cells expressing at least 2 activation markers at baseline ad months 1, 2, 3, 6, 7, and 18 Among the ART, high CD4 and ART-naive high CD4 patients, Geometric mean ratio was higher for RZV than placebo: 21.95 (70% CI 12.97, 38.02); increases persisted to month 18 Humoral immunity: Anti-gE antibody concentrations pre-vaccination and at months 1, 2, 3, 6, 7, and 18 Among the ART, high CD4 and ART-naive high CD4 patients, Geometric mean ratio at 7 months was higher for RZV than placebo: 46.22 (70% CI 33.63, 63.53); increases persisted to month 18 No benefit to third dose |
Level I |
Good |
Stadtmauer et al, 2014 |
RZV (2 and 3-dose regimes) in autologous HSCT transplant patients |
Phase 1/2a randomized, observer-blind placebo-controlled trial |
n=121 (initial enrollment) - n=99 remained by month 15 n=30 (3 doses AS01B) n= 29 (3 doses AS01E) n=31 (2 doses AS01B) n=30 (3 doses saline) |
CMI: CD4+ & CD8+ cells with at least 2 activation markers at baseline, month 4, and month 15 CMI was higher among all vaccine groups compared to saline, a response that persisted to the end of the study Humoral immunity: anti-gE antibody concentrations at baseline, month 4, and month 15 GMCs were higher among all vaccine groups compared to saline, a response that persisted for at least one year after last vaccination; GMCs decreased between 29-46% from month 4 to 15 Combined CMI & humoral response was superior in 3-dose AS01B compared to AS01E (p<0.25) and compared to 2-dose AS01B (p<0.15) |
Level I |
Fair (fairly high dropout rate by end of study, not all outcome comparison done) |
Oostovegels, 2017 (ID Week poster) |
RZV in patients with hematologic malignancy |
Phase 3 observer-blind, placebo-controlled trial |
n=562 n=415 in humoral immunogenicity group (vaccine =217, placebo=198) n=132 in cell-mediated immunogenicity group (vaccine =69, placebo=16) |
CMI: CD4+ T-cells expressing at least two activation markers at baseline, 1-2 months post-dose 1, and 1 month post-dose 2 (n=132) CMI VRR was ~80% compared to <10% in vaccine vs. placebo 1 month post-dose 2 Humoral immunity: anti-GE antibody levels at baseline, 1-2 months post-dose 1, and 1 month post-dose 2 (n=415) Humoral VRR was 80% compared to around 0% in vaccine vs. placebo 1 month post-dose 2 |
Level I |
N/A pending full methods - study is ongoing |
Vink 2017 (ID Week Poster) |
RZV in patients with solid tumors before & after immunosuppressive therapy |
Phase 2/3 observer-blind, placebo-controlled trial |
n=232 n=117 (vaccine group, 90 pre-chemo, 27 on chemo) n=115 (placebo group, 91 pre-chemo, 24 on chemo) |
CMI: CD4+ T-cells expressing at least two activation markers at baseline and months 1, 2, 6, and 12 post-vaccination in patients yet to start chemotherapy Adjusted GM frequency ratio was 9.9 (95% CI 3.6-27.2) at month 2 between vaccine & placebo group; 17.6% (month 12) and 50.0% (month 2) of the pre-chemo group met criteria for CMI vaccine response Humoral immunity: Anti-GE antibody levels at baseline and months 1, 2, 6, and 12 post-vaccination in all patients Adjusted GMC ratio was 23.2 (95% CI 17.9-30.0) at month 2 between vaccine & placebo group; While GMC declined with time in vaccine group, it was higher for vaccine group than placebo group at all points of follow-up |
Level I |
N/A pending full methods |
Vink (2), 2017 (ID Week Poster) |
RZV in renal transplant patients on chronic immunosuppression |
Phase 2/3 observer-blind, placebo-controlled trial |
n=264 n=132 (vaccine group) n=132 (placebo group) |
CMI was assessed in 72 patients (36 in each group): CD4+ T-cells expressing at least two activation markers at baseline, 1-2 months post-dose 1, and 1 month post-dose 2 Adjusted GM frequency ratio was 17 (95% CI 5.9, 20.4) at 1 month post-dose 2 Humoral immunity was assessed in 240 patients (121 vaccine, 119 placebo): anti-GE antibody levels at baseline, 1-2 months post-dose 1, and 1 month post-dose 2 Adjusted GMC ratio was 14.0 (95% CI 10.9, 18.0) at 1 month post-dose 2 |
Level I |
N/A pending full methods |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Weinberg et al, 2017 (abstract) |
Zostavax vs. RZV |
Unclear |
Unknown - patients were either 50-70 with no vaccine or 70+ who had received Zostavax®at least 5 years ago; at entry they received Zostavax®or RZV |
CMI & humoral immunity measured at days 0, 30, 90, and 365. Higher memory CD4+ & CD8+ response detected in RZV group |
Unknown |
N/A |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
MacIntyre et al, 2010 |
Zostavax®with concomitant administration of Pneumovax 23 vaccine |
Randomized, double-blind, placebo-controlled trial |
n=473 (initial enrollment) n=237 (concomitant vaccination) n=236 (Pneumovax Day 0, Zostavax®Day 28) |
Anti-VZV antibodies through gpELISA at baseline and week 8 GMT ratio (concomitant to non-concomitant) was 0.70 (95% CI 0.61, 0.80), suggesting lower response for concomitant administration; however, the estimated GMFR for concomitant administration did meet acceptable antibody response in absolute terms |
Level I |
Good |
Levin et al, 2017 |
Zostavax®with concomitant administration of influenza vaccine |
Randomized, double-blinded, placebo-controlled trial |
n=882 (all ≥50 years) n=441 received Zostavax®and influenza vaccine concurrently n=441 received Zostavax®4 weeks after influenza |
Anti-VZV antibodies through gpELISA, measured at baseline and 4 weeks post-vaccination Post-vaccination, GMT were non-inferior according to authors in concomitant administration group versus non-concomitant group: GMT ratio 0.87 (95% CI 0.80, 0.95); GMFR in concomitant group was 1.9 (95% CI 1.76, 2.05) |
Level I |
Good |
Schwarz et al, 2017 |
RZV with concomitant administration of influenza vaccine |
Phase 3, randomized, open-label, multicentre clinical trial |
n=828 (all ≥50 years) n=413 (Coadministrat-ion - received RZV at day 0 and month 2; flu vaccine at day 0) n=415 (Control - received RZV su at month 2 & 4; flu vaccine at day 0) |
Anti-gE antibodies measured at baseline, day 21, and months 2, 3, and 5 The GMC ratio of control to concomitant administration groups was 1.08 (95% CI 0.97, 1.20) demonstrating non-inferiority of RZV. Non-inferiority was also demonstrated for all four influenza vaccine strains. |
Level I |
Fair (non-blinded) |
Appendix C: Summary of Evidence Related to Safety of Herpes Zoster Vaccines
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Arnou et. al, 2011 |
Zostavax®, refrigerator-stable |
Open-label, single-arm study |
Age: Number (N=): |
Adverse events (AEs) reported within 28-days post-immunization Results n (%): Any injection-site reactions or systemic AEs related to the vaccine: 52 (54.2%); at least one systemic AE reported by 22.9% of study participants Injection-site reactions (day 0-28): 50 (52.1)
Systemic AEs related to the
vaccine (day 0-28): 8 (8.3) |
II-2 | Poor |
Baxter et al, 2012 |
Zostavax® |
Cohort study (insurance claims data) Rate of diagnosis codes for days 1-42 following LZV administration compared to codes days 91-180 post vaccination (vaccinees used as their own "controls") |
Age: Number (N=): |
AEs observed during a 42-day port-immunization period. No increased RR observed in 382 comparisons performed for the main analysis 4 comparisons which had an increased RR with a nominal (unadjusted) p-value ≤0.05 were further investigated and after record reviews found to be no longer statistically significant. Allergic reactions in the 1-7 days window in the outpatient and ED settings was the only significantly increased risk identified in the study. |
II-2 | Fair |
Beals et al, 2016 |
Zostavax® |
Randomized, partly blinded trial (dosing study) Intradermal injection provided using NanoPass MicronJet600 device (microneedles, 0·60 mm in length) |
Age: Number (N=): |
AEs observed during a 42-day port-immunization period. Results: Full dose (N = 52) :
1/3 dose (N = 34) :
Intradermal administration: Full dose (N= 34):
1/3 dose (N= 35):
1/10 dose (N= 34):
1/27 dose (N = 34):
Placebo (N = 39):
No SAEs or temperatures greater than 38°C were reported in the study |
I | Fair |
Choi et al, 2016 |
Zostavax® |
Open label, single arm |
Age Number |
Results n (%, 95% CI) One or more AEs: 113 (62.8; 55.3-69.9)
AEs related to the vaccine: 97 (53.9; 46.3-61.3)
One or more SAEs: 3 (1.7;
0.4-4.8) The injection-site AEs were more frequently reported by adults 50 to 59 years of age (58.4%) than those 60 years of age and older (48.4%). The majority of AEs in the study were of less than 2 days duration |
II-2 | Fair |
Diez-Domingo et al, 2014 |
Zostavax® |
Open-label, randomised, comparative, study (IM vs. SC administration) |
Age Number |
Results n (%):
|
I | Fair |
Gilderman et al 2008 |
Vaccine 1: Zostavax®(refrigerator stable formulation) Vaccine 2: Zostavax®(frozen formulation) |
Randomized, controlled, double-blind |
Age Number: |
Mean age: 63 years Results during a 28-day follow-up period: n (%) Group 1 (n = 180):
Group 2 (n=183):
All AE were generally mild. |
I | Good |
Hata et al 2016 |
Vaccine: Placebo: purified distilled water for injection All study participants received PPSV23 concomitantly with LZV or placebo |
Double-blind randomized placebo-controlled study |
Age Number Immune status: |
PPSV23 was provided simultaneously. Results n (%): Zoster vaccine group (n = 27)
Placebo group (n = 27)
|
I | Fair |
Kerzner et al, 2007 |
Vaccines: Placebo: |
Randomized, double-blinded clinical trial Concomitant group received ZVL and IIV on Day 1 and placebo at Week 4. Nonconcomi-tant group received IIV and placebo on Day 1 and ZVL at Week 4. |
Age Number concomitantly vaccinated (n=382) Sequentially vaccinated (n=380) . |
Results Days 1-28 Post vaccination: Concomitant Group (n=382) All vaccinated subjects with follow-up (n=378):
Subjects aged ≥ 50 with follow-up (n=125)
Subjects aged ≥ 60 with follow-up (n=253)
Nonconcomitant Group (n=380) All vaccinated subjects with follow-up (n=376):
Subjects aged ≥ 50 (n=127)
Subjects aged ≥ 60 (n=249)
|
I | Good |
Lai et al, 2015 |
Zostavax® |
Case-control study Cases and controls identified from 18,534 events in VAERS reported after LZV |
Age Number |
No increased risk of SAAEs identified except for alopecia and arthritis (OR: 2.2 [95% CI:1.2-4.3] and 2.7 (1.7-4.3], respectively) In total 40 cases of alopecia and 61 cases of arthritis reported in VAERS during the study period with a median of 4 days between vaccination and symptom onset. |
II-2 | Poor |
Levin et al, 2016 |
Zostavax® |
Non-randomized controlled study |
Age Number Pre-Exposure History: |
The vaccine was generally well tolerated in all groups (Table 2). As many as 57% of subjects in groups 1 and 2 and 75% of subjects in groups 3 and 4 reported ≥1 adverse experience through week 52. Most of the AEs were injection site reactions (pain and erythema) occurring 1-5 days after ZV receipt. Only 6 subjects reported injection-site adverse experiences from day 6 to week 6 after ZV receipt. The higher rate of AEs in groups 3 and 4 was primarily related to a higher rate of injection site reactions. Vaccine-related non-injection site reactions occurred in 3%-8% of subjects ≤6 weeks after ZVL receipt. Group 1 (n = 200): Group 2 (n= 200): Group 3 (n=100): Group 4 (n= 100): Results: Group 1 (n=200), Participants, No. (%):
Group 2 (n=200), Participants, No. (%):
Group 3 (n=100), Participants, No. (%):
Group 4 (n=100), Participants, No. (%):
|
II-1 |
Fair |
MacIntyre et al, 2010 |
Vaccines: Zostavax® and PPV23 Placebo: not specified |
Randomized, double-blind, placebo-controlled study At Day 1, all adults received open-label PPV23 while administration of ZVL or placebo at Day 1 and Week 4 was blinded Concomitant group received ZVL and PPV23 on Day 1 and placebo at Week 4. Nonconcomitant group received PPV23 and placebo on Day 1 and ZVL at Week 4. |
Age Number |
Postvaccination of ZVL, clinical AEs were numerically but not significantly higher in nonconcomitant group. The incidence of injection-site AEs was similar in both groups. All 6 reported SAEs were deemed not related to study vaccine. Results: no. cases (estimated risk %): Concomitant group (n=235): AEs Summary
Injection-site AEs Injection site for ZOSTAVAX®:
Injection site for Placebo:
Non-concomitant group (n= 236) : AEs Summary
Injection-site AEs Injection site for ZOSTAVAX®:
Injection site for Placebo:
|
I | Good |
Mills et al, 2010 |
Vaccine: LZV ~89,000 PFUs Placebo: not stated |
Randomized Controlled Trial |
Age Number Pre-Exposure History: |
In HZ history-positive adults ≥50 years of age, zoster vaccine was well tolerated. Randomized Group1 (n=51): Randomized Group2 (n=50): Results n (%): Zostavax® Overall per-protocol summary:
Subjects with 5-9 years since prior HZ episodes:
Subjects with ≥10 years since prior HZ episodes:
Subjects 50-59 years of age:
Subjects ≥60 years of age:
Placebo: Overall per-protocol summary:
Subjects with 5-9 years since prior HZ episodes:
Subjects with ≥10 years since prior HZ episodes:
Subjects 50-59 years of age:
Subjects ≥60 years of age:
|
I | Good |
Morrison et al, 2013 |
Vaccine: Zostavax® |
Case-control |
Age Among SPS placebo recipients who received LZV, there were 420 with documented HZ during the SPS and 13,261 individuals without prior HZ (comparator group) |
LZV provided at mean 3.6 years following a prior HZ episode A total of 4 SAEs were reported among 4/ 420 adults with prior HZ, and 111 SAEs among 88/13,261 adults with no history of HZ. No differences in SAEs were found in the proportion of vaccine recipients with and without prior HZ, and no unexpected injection site AEs were reported by the study participants in the 28 days post vaccine administration. |
II-2 | Good |
Murray et al, 2010 |
Vaccine: Zostavax® Placebo: Zostavax®vaccine stabilizer without VZV or virus components |
Randomized, placebo-controlled trial |
Age Number |
No statistically significant differences found in SAEs among vaccine and placebo recipients in the 42-day or 182-day observation period Zoster Vaccine Group (n= 5,983): Primary Safety Follow-up Period (Day 1 to Day 42 Postvaccination):
Secondary Safety Follow-Up Period (Day 1 To Day 182 Postvaccination)
Placebo Group (n= 5,997): Primary Safety Follow-up Period (Day 1 to Day 42 Postvaccination):
Secondary Safety Follow-Up Period (Day 1 To Day 182 Postvaccination)
|
I | Good |
Oxman et al, 2005 |
Vaccine: live attenuated Oka/Merck VZV vaccine 18,700 to 60,000 PFUs per dose (>90% received <32,300 PFUs) Placebo: not stated |
Randomized, placebo-controlled, double-blind clinical trial (SPS study) |
Age Number |
Vaccine Group From day of vaccination to end of study:
From day of vaccination to day 42:
Subjects in the AE substudy (n= 3345): From day of vaccination to end of study:
From day of vaccination to day 42:
Placebo Group: All Subjects (n= 19,276): From day of vaccination to end of study:
From day of vaccination to day 42:
Subjects in the AE substudy (n= 3271): From day of vaccination to end of study:
From day of vaccination to day 42:
|
I | Good |
Schmader et al, 2012 |
Vaccine: Zostavax® Placebo: all Zostavax®vaccine constituents except VZV or virus components |
Randomized, double-blind, placebo-controlled study |
Age Number |
AEs were reported by 72.8% of subjects in the ZV group and 41.5% in the placebo group, with the difference primarily due to higher rates of injection-site AEs and headache. The proportion of subjects reporting SAEs occurring within 42 days postvaccination (ZV, 0.6%; placebo, 0.5%) and 182 days postvaccination (ZV, 2.1%; placebo, 1.9%) was similar between groups. Results no. (%):
Placebo Group (n=11,116):
|
I | Good |
Simberkoff et al, 2010 |
Vaccine: live attenuated Oka/Merck |
Randomized, placebo-controlled, double-blind clinical trial (SPS study) |
Age Number |
After inoculation, 255 (1.4%) vaccine recipients and 254 (1.4%) placebo recipients reported EIG. Local inoculation-site side effects were reported by 1,604 (48%) vaccine recipients and 539 (16%) placebo recipients in the substudy. A total of 977 (56.6%) of the vaccine recipients reporting local side effects were aged 60 to 69 years, and 627 (39.2%) were older than 70 years. After inoculation, HZ occurred in 7 vaccine recipients versus 24 placebo recipients. Long-term follow-up (mean, 3.39 years) showed that rates of hospitali-zation or death did not differ between vaccine and placebo recipients. Aged 60-69 Years: HZ Group no. (risk%) (n=1,726):
Placebo Group (n= 1,709)
Aged 70 Years or more: HZ Group no. risk% (n=1,600):
Placebo Group (n= 1540)
|
I | Good |
Tseng et al, 2012 |
Zostavax® |
Observational study using a cohort analysis by case-centered and self-controlled case series designs |
Age Number |
Risk of SAEs in the 42 days following vaccination was not statistically different compared to the historical comparison period. Allergic reactions in the 1-7 days window in the outpatient and emergency department settings were higher compared to the historical comparison period (RR = 2.13, 95% CI: 1.87-2.40 by case-centred method and RR = 2.32, 95% CI: 1.85-2.91 by SCCS) |
II-2 | Fair |
Tyring et al, 2007 |
Vaccine 1: LZV~207,000 Vaccine 2: LZV~58,000 |
Randomized clinical trial |
Age Number |
No serious vaccine-related AEs were reported. Similar AE rates were observed in the higher and lower potency groups (overall systemic AEs: 37.5 and 39.3%, vaccine-related systemic AEs: 10.9 and 13.2%, injection-site AEs: 63.0 and 59.8%). Rates for a combined endpoint of moderate or severe injection-site pain/tenderness/soreness and swelling were 17.2% (95% CI 13.9, 21.0) and 9.0% (95% CI 5.6, 13.4), respectively. Most combined endpoint events were reported as moderate in intensity. Higher Potency Group (n=459) Aged 50-59 years (n= 123):
Aged 60 years or more (n= 336):
Total (n= 459):
Lower Potency Group (n=234) Aged 50-59 years (n= 62):
Aged 60 years or more (n= 172):
Total (n= 234):
|
I | Fair |
Vermeulen et al, 2012 |
Vaccine: LZV ~23,000 PFUs Placebo: Not stated |
Randomized controlled trial Vaccine administration provided on days 0 and 42 |
Age Number |
No serious vaccine-related AEs occurred in 42-day period following immunization. Results no. cases (%): Postvaccination 1 (n=104):
Postvaccination 2 (n=98):
Placebo Group: Postvaccination 1 (n=105):
Postvaccination 2 (n=101):
|
I | Good |
Vesikari et al, 2013 |
Zostavax® |
Randomized Controlled Trial Single dose of LZV provided
on - day 0 (visit 1) only; or |
Age Number |
HZ vaccine was generally well tolerated, with no evidence of increased AE incidence after the second dose with either schedule. Results no. cases (%):
Post-dose 2, 1-month schedule (n= 232):
Post-dose 2, 3-month schedule (n= 221):
|
I | Good |
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings Using Text or Data | Level of Evidence | Quality |
Chlibek et al. 2013 |
Vaccine: Shingrix® Placebo: saline |
Randomized control trial |
Age Number (N=): |
Results: gE/AS01b (n=150)
Placebo (n=38)
|
I | Good |
Chlibek et al. 2014 |
Shingrix® |
Randomized control trial |
Age Number= Subjects randomized to receive two doses of different HZsu formulations; only AEs for currently licenced product presented |
Results: percentage % [95% CI] Shingrix®(50 µg gE/AS01B) (N=166): Local Symptoms: Overall cohort
60-69 years
≥70 years
General Symptoms: Overall Cohort
Grade 3a: Defined as preventing normal everyday activities Grade 3b: Defined as a diameter of > 100mm Any (c): Defined as an oral/axillary temperature of ≥37.5°C. Grade 3d: Defined as an oral/axillary temperature of > 39°C. |
I | Fair |
Chlibek et al. 2016 |
Shingrix® |
Follow-up to, randomized controlled trial |
Age Number= |
All SAEs developed by study participants were considered unrelated to vaccination by the study investigators |
II-2 | Good |
Cunningham et al. 2016 |
Vaccine: Shingrix® Placebo: 0.9% saline solution |
Randomized, placebo-controlled trial (ZOE-70) Participants received two doses of RZV or placebo administered intramuscularly 2 months apart. |
Age Adults 70 years or older Number: 1,010 |
Results: n/ntot, % [95% CI] RZV Group
Throughout the study period in the total vaccinated cohort (ntot = 6950)
Placebo Group
Throughout the study period in the total vaccinated cohort (ntot = 6950)
|
I | Good |
Lal et al, 2015 |
Vaccine: Shingrix®, Placebo: 0.9% saline solution |
Randomized, placebo-controlled trial (ZOE-50) |
Age Number: 15,411; reactogenicity subgroup: 8,926 |
SAE recorded in all participants for up to 12 months after the second dose Results: n/ntot, % (95% CI): RZV Group Reactogenicity Group (n=4460) Within 30 days after vaccination:
Within 7 days after vaccination:
Total vaccinated cohort
(n=7,698):
Within 30 days after vaccination:
Placebo Group Reactogenicity Group (n=4,466) Within 30 days after vaccination:
Within 7 days after vaccination:
Total vaccinated cohort
(n=7713):
Within 30 days after vaccination:
|
I | Good |
Leroux-Roels et al, 2012 |
Vaccines: Shingrix®and LZV |
Randomized, parallel-group trial HZsu or LZV or HZsu+LZV provided at months 0 and 2 |
Age Number |
Few grade 3 events and no SAE were reported. Fatigue, myalgia, headache, and injection site pain were the most common solicited reactions for RZV and occurred more frequently than with LZV Results no. (%) 95% CI: Percentage of Subjects Adults aged 50-70 years (n = 135) LZV only group (n=45): General reactions:
Local reactions:
RZV only group (n=45): General reactions:
Local reactions:
RZV + LZV group (n=45): General reactions:
Local reactions:
Adults aged 18-30 years (n = 20) RZV only group (n=10): General reactions:
Local reactions:
RZV + LZV group (n=10): General reactions:
Local reactions:
|
I | Fair |
Vink et al, 2017 |
Shingrix® |
Randomized open-label controlled trial Vaccine administered SC or IM |
Age Number |
Intervention details: Results 7-day post-vaccination, (%): SC Group (n= 30):
IM Group (n= 28):
These SAEs were not considered to be causally related to the study vaccine by the investigator. No HZ cases or potential immune medicated diseases were reported during the study period. |
I | Fair |