Annex B - Physical Assessment Guide to Assess the Risk of COVID-19 in the Workplace
| Document Status: | Current |
|---|---|
| Document Type: | Guide |
| Approval: | D Safe G |
| SME: | D FHP SSO OEH |
| OPI: | D Safe G |
| Effective Date: | 15 Jun 2020 |
| Last Reviewed: | 15 Jun 2020 |
References
- DM/CDS JOINT DIRECTIVE – DND/CAF COVID-19 PUBLIC HEALTH MEASURES AND PERSONAL PROTECTION 1 May 2020
- Annex A Personnel Protective Recommendations, DFHP Advisory 6636-80, COVID-19: Force Health Protection Recommendations
- FRAGO 001 to CDS TASK ORD 002 – OP LASER 20-01 – FORCE EMPLOYMENT
- DFHP Advisory 6635-44, Guidance for Drinking Water in Low Occupancy and Closed Buildings
- Annex D Disinfection Guidelines, D FHP Advisory 6636-80, COVID-19: Force Health Protection Recommendations
- As the Defence Team (DT) returns to conducting business in DND/CAF facilities, each unit must plan for a safe return to the workplace. The goal during this period is to prevent transmission of the virus responsible for COVID-19 among DND employees and CAF members and to support workers in a safe and healthy return. A number of resources from the federal, provincial and territorial governments, as well as various international organizations, have been developed outlining guidance on this topic. This document attempts to summarize those materials and provide links to the publications.
- Public Health Measures - As individuals return to the workplace, the most important action currently available to prevent the spread of COVID-19 is strict adherence to public health measures (PHMs). Units must be prepared to actively promote these measures and support their personnel in following them. A number of the recommendations in the sections below will help units do this. The fundamental public health measures to follow include:
- Staying at home unless one is authorized to report for duty or work;
- Not reporting for duty if one has symptoms of COVID-19;
- Physical distancing—ensuring 2m separation from others, whenever possible, in work and common areas;
- Hand hygiene measures—frequent hand washing with soap and water for at least 20 seconds, or using an alcohol-based hand sanitizer if soap and water are not available;
- Avoiding touching one’s eyes, nose, and mouth; and
- Coughing/sneezing into one’s elbow.
- In addition, Ref A states that DT members shall wear a non-medical mask when at work and unable to maintain 2m separation from others.
- Workplace Risk Assessment - In advance of re-opening, each unit must ensure that they complete their own workplace risk assessment. The purpose of this effort is to identify policies and practices where there is an increased risk of COVID-19 transmission. The findings of this assessment then allow the unit to develop a tailored plan for each of its workplaces to mitigate those risks. The assessment involves each unit performing their own review and documentation of all their routinely performed activities, focusing on factors such as:
- Who performs the task?:
- Are there any workers who are considered at higher risk for contracting COVID-19 or of having a worse outcome if they do?;
- How is the task performed?:
- Is it performed alone or by more than one person?;
- Are workers within 2m of each other?;
- How long does the task take to be completed?; and
- Can the task be modified to allow workers to follow the PHMs?;
- Is the task performed indoors or outdoors?;
- What is the physical layout of the workplace and common areas?:
- Are there hand wash or hand sanitization stations at useful locations and easily accessible?;
- What is the ventilation in the workspace? Are there windows that can be opened?; and
- Does the workspace or common area have high touch surfaces (i.e., surfaces frequently touched by others)?; and
- Is the space open to other DT members or the public?:
- Are individuals other than unit personnel permitted to enter the workspace? If so, for how long?; and
- Is there a record of those who enter the workspace?.
- Who performs the task?:
- DFHP recommends using the risk assessment tool in Appendix 1, developed from resources produced by the Public Health Agency of Canada (PHAC). This appendix also provides more detailed recommendations for strategies to mitigate the identified risks in the workplace.
- Hierarchy of Controls - The occupational health and safety approach to reducing risk of workplace illness and injury is based on a concept known as the hierarchy of controls. This is a structured method of organizing control solutions for a given hazard in the workplace, such as COVID-19, in a way that moves from the most effective and protective to the least (Fig. 1).
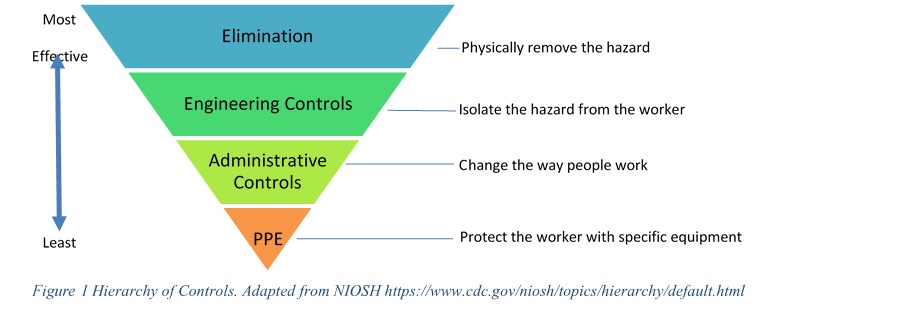
Figure 1 Hierarchy of Controls. Adapted from NIOSH https://www.cdc.gov/niosh/topics/hierarchy/default.html
- This hierarchy of controls can be used to organize and present various options for preventing worker exposure to COVID-19, primarily by facilitating physical distancing and hand hygiene. Examples of controls are presented in Table 1, below, but do not represent all possible options that may be employed in this context. Controls implemented in a workplace for COVID-19 must take into consideration previously identified hazards in that location and ensure that existing controls are not jeopardized, or that existing regulations (such as those from the fire marshal) are not violated. Furthermore, controls introduced for COVID-19 must not introduce new hazards for individuals in the workplace.
- Personal protective equipment (PPE) is the least effective control method of a workplace hazard and is used to protect the individual when that hazard cannot be otherwise eliminated or sufficiently reduced.
- PPE recommendations specific to COVID-19 for Health Care Providers can be found in Ref B. For DT members on Op LASER or Op LENTUS, PPE recommendations are contained in Ref C.
- At all times, PPE that is already recommended for a workplace (to address a known hazard) must continue to be used. Talk to your supporting Preventive Medicine Technician for guidance if uncertain as to what PPE to use or how existing controls may be impacted in a situation where there is combined COVID-19 and other pre-existing hazards.
- Non-medical masks (NMMs) are not considered a form of PPE. That is, they do not provide protection to the wearer, but they do help protect those around by containing the wearer’s respiratory droplets. Ref A states that all DT members will wear an NMM at work when unable to maintain 2m distance from others. The wearing of an NMM is not authorization to forego physical distancing measures.
- Table 1 provides examples of controls that could be implemented in various DND/CAF workplaces to help mitigate the risk of COVID-19 transmission.
| Hierarchy of control category | Examples of mitigation strategies |
|---|---|
| Engineering controls |
|
| Administrative controls |
|
| PPE and NMMs |
|
- Other prevention issues - A number of DND/CAF buildings will have been unoccupied or will have had low occupancy during the period of business shut down. It is important for building managers to ensure that their facilities are safe and ready for workers to return. One major consideration is the safety of building drinking water. See Ref D. for steps to follow to ensure appropriate water quality, if there are any questions consult with local Preventive Medicine resources.
- In addition, units must ensure that, at a minimum, routine cleaning practices shall be maintained as per Ref E. DFHP recommends that high touch areas such as door knobs, light switches, and horizontal work surfaces be cleaned and disinfected more often, as well as when visibly dirty.
- Illness in workplace - See Appendix 2 for recommendations if an individual who has returned to the workplace becomes ill.
- Inquiries - Inquiries related to this guidance are to be submitted to the OHS Secretariat by e-mail at: +OHS Secretariat-Secretariat de la SST@VCDS D Safe G@Ottawa-Hull (intranet/DWAN) or OHSSecretariatSST@forces.gc.ca (internet).
- Resources – You will find below various resources that were consulted in the creation of this guide:
- Public Health Agency of Canada. Appendix C: A framework for risk assessment and mitigation in community settings during the COVID-19 pandemic, retrieved from https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html#_Appendix_C:_A;
- Public Health Agency of Canada. Updated: Community-Based Measures to Mitigate the Spread of Coronavirus Disease (COVID-19) in Canada, retrieved from https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html;
- Canadian Centre for Occupational Health and Safety Pandemic (COVID-19) Tip Sheets, retrieved from https://www.ccohs.ca/products/publications/covid19/;
- Canadian Centre for Occupational Health and Safety. Workplace Tips for Both Employers and Workers. https://www.ccohs.ca/outbreaks/workplace; and
- American Industrial Hygienist Association. Get Back to Work Safely. https://www.backtoworksafely.org/.
Appendices
- Risk Mitigation Tool for Workplaces Operating During the COVID-19 Pandemic
- Addressing New COVID-19 Cases in the Workplace
Appendix 1 to Annex B
Risk Mitigation Tool for Workplaces
Operating During the COVID-19 Pandemic
- As DND/CAF prepares to re-open and resume fuller operations during the COVID-19 pandemic, units should consider the risks of COVID-19 transmission in their workplaces and identify risk mitigation strategies they can implement to facilitate a safer re-opening. It is possible that once the pandemic has ceased, some of the mitigation strategies implemented in workplaces might be removed.
- Public health measures taken by workplaces are part of Canada’s collective approach to mitigate the transmission of COVID-19. This tool is based on work by the Public Health Agency of Canada and public health assumptions that reflect the currently available scientific evidence and expert opinion, and is subject to change as new information on transmissibility, epidemiology, and effectiveness of public health measures and mitigation strategies becomes available. Use this tool along with relevant provincial/territorial health authority recommendations, where applicable. Refer to your provincial or territorial website for the list of essential services and updates on the restriction of non-essential services.
- This tool will assist DND/CAF workplaces in considering risks to DND employees, CAF members, contractors and visitors during the coronavirus disease (COVID-19) pandemic, and provide examples of strategies that may be implemented in the workplace to mitigate potential risks.
What are the COVID-19 Risks in my Workplace?
- The following facts about COVID-19 and associated questions can help you consider the risks of COVID-19 for individuals (Defence Team (DT) members and visitors) in your workplace.
- The risk level is affected by whether there is COVID-19 activity in the local community. If there is COVID-19 in your community, the likelihood that it could be introduced into the workplace is higher.
Person-to-Person Spread in the Workplace
| Facts |
|
|---|
Questions to consider for your workplace
- Are individuals required to work and interact within 2 metres of each other because of the workplace set up, the nature of the task being performed, or both?
- Do common spaces (e.g., eating areas) require individuals to be within 2 metres of each other?
- Do individuals have frequent close interactions with other individuals throughout their workday?
- Do individuals have prolonged close interactions with others?
- Is the workplace indoors or outdoors?
- If indoors, can windows be opened?
Spread From Surfaces to People in the Workplace
| Facts |
|
|---|
Questions to consider in your workplace
- Do individuals frequently have contact with high-touch surfaces (i.e., surfaces frequently touched by others)?
- Do individuals frequently have contact with equipment or tools that are also frequently handled by others?
- Does the set-up of your workplace enable individuals to wash their hands after contact with high-touch surfaces (e.g., access to hand hygiene stations/supplies)?
People at Greater Risk of Infection
| Facts |
|
|---|
Questions to consider for your workplace
- Do you know of any individuals in your workplace who are at higher risk of severe illness (e.g., older adults)? NOTE: Employers cannot assume they know the health status of individual employees and are not necessarily entitled to this information.
Core Personal Measures
| Facts |
|
|---|
Questions to consider for your workplace
- Are individuals in your workplace aware of and able to follow hygiene practices such as washing hands frequently, respiratory etiquette, and identifying when they are feeling ill and staying home?
Other Workplace Hazards and Controls
| Facts |
|
|---|
Questions to consider for your workplace
- Will measures considered for your workplace to combat COVID-19 adversely interfere with existing hazard controls?
- Will measures considered for your workplace to combat COVID-19 introduce new hazards or violate existing regulations, such as those from the fire marshal?
- Have other non-COVID-19 hazards been introduced to your workplace during the lockdown, including reduced potable water quality?
How Can My Workplace Mitigate COVID-19 Risks?
- To prevent and/or limit the spread of COVID-19 in your workplace, consider the following risk mitigation principles and strategies. The following list is not exhaustive – you are encouraged to find creative and adaptive ways to mitigate risk in your workplace setting. No one strategy listed here is considered mandatory.
Restrict people who are ill from entering the workplace
- Strengthen communication strategies for DT members and visitors
- Require that DT members stay at home if ill with symptoms of COVID-19 until criteria to discontinue isolationFootnote 1 have been met, in consultation with the local public health authority or healthcare provider
- Adjust absenteeism policies to enable DT members to stay home when ill, in quarantine (self-isolation) when directed to do so by medical personnel, or if they are taking care of children or someone who is ill
- Post accessible signage to discourage individuals who are ill from entering the workplace setting
- If feasible, consider asking visitors granted access if they are ill or have symptoms of COVID-19 before they enter the workplace setting or when making appointments, and ask visitors who are ill to not attend the workplace
Promote and facilitate personal public health practices
- Keep individuals informed about public health advice applicable to your workplace
- Promote the use of personal public health practices (e.g., frequent hand hygiene, avoid touching the face, respiratory etiquette, clean and disinfect frequently touched surfaces)
- Post signage that reminds individuals to practice these measures
- Provide increased access to hand hygiene facilities (e.g. by placing hand sanitizer dispensers in easy to see locations) and ensure accessibility for individuals with disabilities or other accommodation needs
- Promote increased environmental cleaning of DT members’ work environments (e.g., provide sanitizing wipes so individuals can clean their own workstations)
- Support and encourage individuals to take care of their mental health
Promote physical distancing
Note!
Physical distancing (keeping a distance of 2 metres from others) is one of the most effective ways to reduce the spread of illness.
- If possible, reduce all physical contact by enabling telework (e.g., work from home, use of email and teleconferencing)
- Adopt a contact-less business model (e.g., drive-through, delivery, curbside pickup)
- Establish 2 metre separation between individuals (e.g., desks, workstations, restaurant tables)
- Restrict occupant capacity of indoor spaces to reduce crowding
- Use visual cues to encourage 2 metre distance (e.g., accessible signage, floor markings)
- Reinforce general practices to maintain physical distancing, such as avoiding greetings like handshakes
- Identify a space where employees or clients can be isolated from others if they develop symptoms
Create physical barriers between employees/clients when physical distancing is not possible
- Install physical separations between employees/clients (e.g. physical barriers like a Plexiglass window or high walled cubicle)
Increase ventilation
- Open windows, if possible, and if weather permitsFootnote 2
- Move work outside when possible
Reduce risks from exposure to high-touch surfaces (i.e., surfaces frequently touched by others)
- Reduce the number of common surfaces that need to be touched (e.g., prop doors open, no-touch waste containers)
- Offer contactless payment methods (i.e., minimize use of cash), if possibleFootnote 3
- Restrict access to non-essential shared equipment
- Clean and disinfect essential shared equipment before and after use
- Increase frequency of environmental cleaning, especially of high touch surfaces or tools (e.g., shared photocopier, elevator buttons, cash register).
Mitigate risk for people at higher risk of severe illness
- Provide equitable workplace accommodations (e.g., role/task reassignment), if possible, for individuals who have risk factors for severe disease
Modify practices to reduce how many and how long individuals are in contact with each other
- Consider modifying service delivery (e.g., reducing the number of individuals using services at the same time, providing services outdoors)
- Close or restrict access to non-essential common areas
- Stagger work hours to reduce number of contacts
- Postpone non-essential meetings or travel
Should individuals wear masks?
- According to the DM/CDS Joint Directive – DND/CAF COVID-19 Public Health Measures and Personal Protection, all DT members will wear a non-medical mask (NMM) at work when unable to maintain 2m distance from others.
- Wearing of NMMs or homemade facial coverings is an additional public health practice that can be taken to prevent the infectious respiratory droplets of an unknowingly infected person from coming into contact with others or contaminating surfaces.
- NMMs are not considered personal protective equipment (PPE).
- When establishing policies regarding use of non-medical masks at your workplace, consider the job requirements of your DT members and the characteristics of the workplace and mitigate risks of physical or psychological injury that could inadvertently be caused by wearing a face covering (e.g., interfering with the ability to see clearly or becoming accidentally lodged in equipment the wearer is operating).
Should individuals wear personal protective equipment (PPE)?
- At all times, PPE that is already recommended for a workplace (to address a known hazard) must continue to be used. Talk to your supporting Preventive Medicine Technician for guidance if uncertain as to what PPE to use in a situation where there is combined COVID-19 and other pre-existing hazards.
- If PPEFootnote 4 is recommended, individuals must be trained on the appropriate use of PPE and the sequence for putting it on (donning) and taking it off (doffing). Individuals should also be trained about proper fit and provided with different sizes of PPE to account for anatomical differences, for example between women and men. Misuse of PPE can increase the risk of infection (e.g. through contact with potentially contaminated PPE).
Appendix 2 to Annex B
- DM/CDS joint directive - DND/CAF COVID-19 Public Health Measures and Personal Protection
- Treasury Board. Occupational Health and Safety Personal Information Bank, retrieved from https://www.canada.ca/en/treasury-board-secretariat/services/access-information-privacy/access-information/information-about-programs-information-holdings/standard-personal-information-banks.html#pse907
- Annex B COVID-19 Signage for Medical and Dental Clinics, D FHP Advisory 6636-80 COVID-19 COVID-19: Force Health Protection Recommendations
- Annex D Disinfection Guidelines, D FHP Advisory 6636-80 COVID-19 COVID-19: Force Health Protection Recommendations
- General Occupational Health Advisory: COVID-19 Public Service Occupational Health Program (PSOHP), Health Canada Updated: 15 March 2020
- As DND/CAF facilities re-open, units must have plans in place to deal with the possibility of a Defence Team (DT) member or other person granted access becoming symptomatic with COVID-19 while in the workplace or within 48 hours of having been there.
- As stated in Ref A, members of the DT will not report for duty if they have symptoms of COVID-19. DND employees and CAF members will follow applicable public health guidelines with respect to self-assessment by using the Government of Canada COVID Self-Assessment tool at https://ca.thrive.health/covid19/en. In addition, units should consider other measures to ensure screening individuals for symptoms of COVID-19 is completed prior to entering the workplace. Options include posting signs about symptoms of COVID-19 at entry points and reminding workers not to enter if they are ill. This information can also be provided in other formats such as websites, apps and texts. More active screening interventions could be considered and involve posting a designated screening person at entry points. At this time, thermal scanning cameras are not recommended as a means to detect fever in returning workers. Fever is not present in all infected individuals and the accuracy of such equipment is questionable for screening purposes. The following exhibits are sample tools that can be used in implementing a screening protocol:
- Exhibit A to this appendix provides a sample version of an active screening tool containing the most up-to-date (as of Jun 2020) COVID-19 symptom list from the Public Health Agency of Canada. Units may consider using this tool to screen non-DT members presenting to DND/CAF workplaces. Units may amend the screening tool to suit their needs, but may not alter the existing text within the table. If units choose to retain identifiable personal health information in this Occupational Health and Safety context, they must be certain to follow the Treasury Board guidance in Ref B and discuss with their unit Access to Information and Privacy Coordinator; and
- Exhibit B to this appendix provides a sample symptom screening sign that may be used at any general workplace entrance. Health care facilities should use the signage found in Ref C.
- As individuals return to the workplace, the cornerstone to prevent the spread of the virus responsible for COVID-19 is through strict adherence to public health measures. Units must be prepared to promote these measures and support their personnel in following them through modelling behaviours, communication, training and workplace modification, where required. The fundamental public health measures to follow include:
- Physical distancing—ensuring 2m separation from others, whenever possible, in all work and common areas;
- Hand hygiene measures—frequent hand washing with soap and water for at least 20 seconds, or using an alcohol-based hand sanitizer if soap and water are not available;
- Avoiding touching one’s eyes, nose, and mouth; and
- Coughing/sneezing into one’s elbow.
- In addition, units must ensure that, at a minimum, routine cleaning practices shall be maintained as per Ref D. DFHP recommends that high touch areas such as door knobs, light switches, and horizontal work surfaces be cleaned and disinfected more often, as well as when visibly dirty.
- Preparations for a COVID-19 positive DND employee or CAF member should include consideration of the following topics, with additional guidance for civilian employees found in Ref E. Some of these considerations may also be applicable to all persons granted access to the workplace.
- Symptomatic individual - Any DND employee or CAF member who develops symptoms consistent with COVID-19 while in the workplace should be directed to return home or to seek medical care (avoiding the use of public transportation), whichever is most appropriate for the situation.
- Until the symptomatic individual can leave the office, they should don a mask (a non-medical mask is sufficient) and be kept away from others in a separate room. If a separate room is not available, the sick individual should maintain as much of a spatial distance from others as is feasible (ideally at least 2 metres).
- Cleaning - In addition to routine cleaning of the workplace, procedures must be established to clean and disinfect the symptomatic individual’s workspace, as well as common areas used by that person. Ref D provides guidance on this and can be applied to any work setting.
- Communication - If an individual develops symptoms consistent with COVID-19 after returning to work, be prepared to support co-workers dealing with the situation. It may be necessary to respectfully communicate relevant information to co-workers to help allay fears and understand risk. Confidentiality of the affected individual is paramount, though, and supervisors should make all attempts to maintain that person’s personal privacy. Mental health information and resources for DT members and supervisors are available at https://www.canada.ca/en/department-national-defence/campaigns/covid-19/mental-health.html. An individual’s primary care provider, as well as the employee assistance program and member assistance program are available to support DND employees and CAF members during this time.
- Close contacts - Should an individual in your workplace become ill with COVID-19, contact tracing will be performed by CF H Svcs personnel and/or civilian public health authorities to identify, educate and monitor individuals who have had close contact with the infected person. These individuals are at a higher risk of becoming infected and sharing the virus with others. Contact tracing can help the individuals understand their risk and limit further spread of the virus.
- Contact tracing may result in recommendations from local CF H Svcs personnel or civilian public health authorities for either self-isolation at home of co-workers or self-monitoring for symptoms while continuing to be present in the workplace. Units must be prepared to support such recommendations.
- Return to work of individuals in self-isolation - The appropriate point at which isolation of cases and quarantine (i.e. self-isolation) of contacts can end may vary by federal, provincial or territorial guidance. DT members who have been in either isolation or self-isolation as a result of a COVID-19 diagnosis or close contact with an infected individual, respectively, should follow the medical direction of their public health authority and health care provider with respect to when they may safely return to the workplace.
- Inquiries - Inquiries related to this guidance are to be submitted to the OHS Secretariat by e-mail at: +OHS Secretariat-Secretariat de la SST@VCDS D Safe G@Ottawa-Hull (intranet/DWAN) or OHSSecretariatSST@forces.gc.ca (internet).
Exhibits
- COVID-19 Screening Tool
- Workplace COVID-19 Screening Sign
Exhibit A to Appendix 2 to Annex B
COVID-19 Screening Tool
Members of the Defence Team will not report for duty if they have symptoms of COVID-19.
| Do any of these apply to you? | |
|---|---|
|
|
|
|
IF YOU ANSWERED YES TO ANY OF THESE QUESTIONS, PLEASE DO NOT ENTER THIS WORKPLACE
INSTEAD, RETURN HOME AND CONTACT LOCAL PUBLIC HEALTH OR YOUR HEALTH CARE PROVIDER FOR GUIDANCE
Defence Team personnel, please notify your supervisor when able
Exhibit B to Appendix 2 to Annex B
Workplace COVID-19 Screening Sign
ATTENTION
- Are you experiencing any of these symptoms?
|
|
- In the last 14 days have you:
- Been in close contact with someone who is sick or has confirmed COVID-19?
- Returned from travel outside Canada?
IF YOU ANSWERED YES TO ANY OF THESE QUESTIONS, PLEASE DO NOT ENTER THIS WORKPLACE
INSTEAD, RETURN HOME AND CONTACT LOCAL PUBLIC HEALTH OR YOUR HEALTH CARE PROVIDER FOR GUIDANCE
Defence Team personnel, please notify your supervisor when able