Module 2: Reporting processes to Health Canada
Download the alternative format
(PowerPoint format, 2.7 MB, 41 pages)
Organization: Health Canada
Published: 2019-12-13
Module 2 - Learning Outcomes
Completion of Module 2 will enable you to:
- Describe considerations for mandatory reporting
- Describe reporting options to Health Canada
- Differentiate among the following:
- Serious adverse drug reaction (serious ADR)
- Medical device incident (MDI)
- Medication incident
- Adverse reaction (AR)
- Medical device problem (MDP)
- Describe the information contained within the Guidance Document
- Describe voluntary reporting of ARs and MDPs to Health Canada
Module 2 - Outline
- Considerations for Mandatory Reporting
- Submitting Reports to Health Canada
- Case Examples
- Guidance Document
- Voluntary Reporting to Health Canada
- Key Points to Remember
- Abbreviations
- Resources
Conceptual Model of Serious ADR and MDI Reporting by Hospitals
Module 2 describes reporting processes to Health Canada.
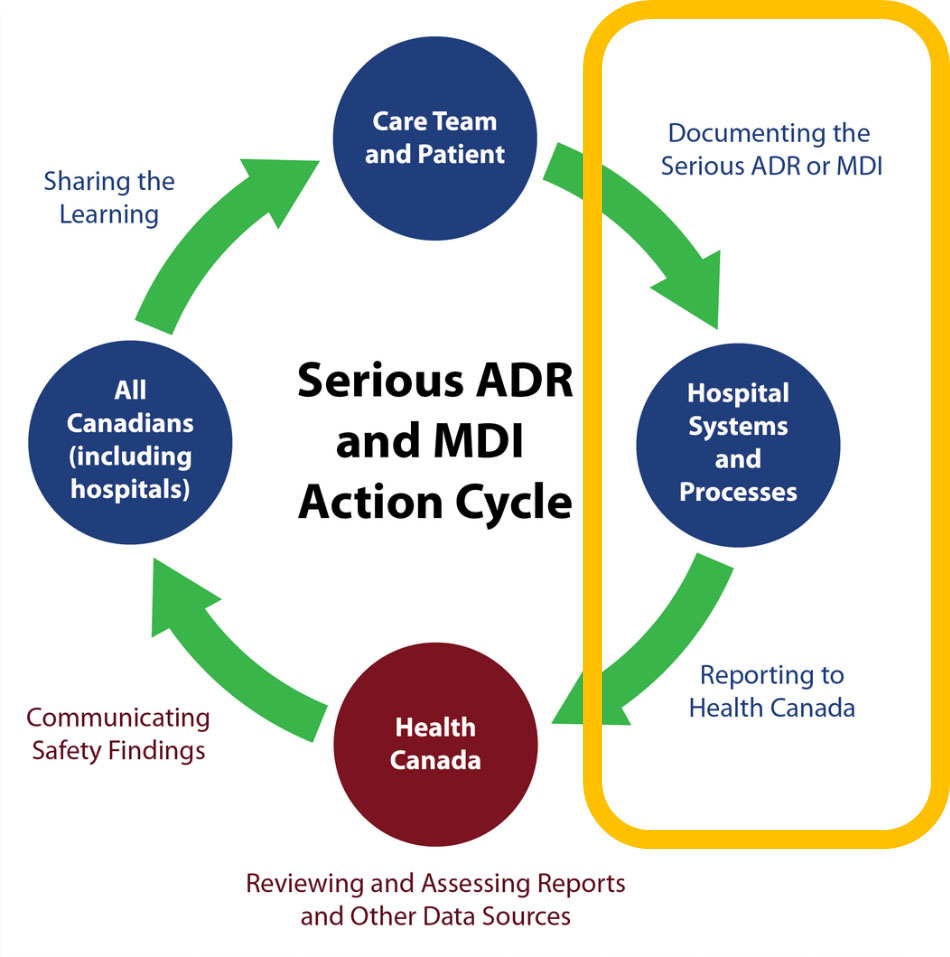
Source: Serious ADR and MDI Action Cycle. ISMP Canada, HSO, CPSI; 2019
Text description
A circle diagram depicts the action cycle for serious ADR and MDI reporting by hospitals. In summary, the figure illustrates that the care team and patients document the serious ADR or MDI. Reporting a serious ADR or MDI to Health Canada is supported by hospital systems and processes. Health Canada reviews and assesses reports and other data sources. Health Canada communicates safety findings to all Canadians, including hospitals, who are shown to share the learning. This concludes the action cycle.
The diagram superimposes a yellow rectangle shape around a specific part of the action cycle to bring focus to:
- documenting the serious ADR or MDIs
- reporting to Health Canada
Considerations for Mandatory Reporting
Hospital Considerations
- Hospital systems, processes, policies, procedures, and forms may need to be updated to reflect requirements for mandatory reporting of serious ADRs and MDIs to Health Canada.
- Hospitals are expected to:
- Develop and maintain internal policies and procedures in order
to comply with the requirements for mandatory reporting of
serious ADRs and MDIs to Health Canada - Determine and communicate internal roles and responsibilities
of staff in meeting the mandatory reporting requirements
- Develop and maintain internal policies and procedures in order
- The mandatory reporting requirements apply to the hospital and not to the individual health care providers working in the hospital. However, health care providers will have an important role in recognizing and documenting serious ADRs and MDIs.
Health Care Provider Considerations
- Health care providers have a role in identifying and documenting serious ADRs and MDIs, in accordance with hospital-defined processes.
- Health Canada is interested in reports about a serious ADR or MDI, even if:
- its association with the drug and/or medical device is only suspected;
- causality is not confirmed;
- all the details are not known; and/or
- it hasn’t caused serious harm but has the potential to cause serious harm if it was to reoccur (only in case of MDIs).
Tips for Recognizing a Serious ADR or MDI
- Serious harm from a drug or from a medical device can be mistaken for a symptom of a disease.
- A high level of suspicion, clinical awareness, and patient dialogue are key components in identifying a serious ADR or MDI. The following can help:
- Ask about the patient’s medical history
- Consider a serious ADR or MDI if there is:
- an unexpected change in the patient’s clinical condition
- a new health problem for the patient
- a need for urgent additional therapies, procedures or surgeries
- a sudden need for a rescue drug (e.g., naloxone, epinephrine, glucagon)
- a medical order for an acute change to therapy (e.g., abrupt discontinuation)
- A serious ADR or MDI can occur shortly after beginning treatment or much later
Considerations for Reporting to Industry/Vendors
- Mandatory reporting regulations do not require hospitals to report to industry/vendors; however, reporting to industry/vendors is strongly encouraged.
- Prompt voluntary reporting from hospitals to industry/vendors enables industry/vendors to conduct investigations to determine causes and corrective actions in a timely manner.
- MDIs: the hospital should inform industry/vendors of an MDI as soon as possible. The manufacturers/importers are required to determine causes and corrective actions.
- Hospitals should consider including a report to industry/vendors in internal reporting policies and procedures.
- Hospitals should consider sequestering the medical device involved in an MDI; it is important that industry/vendors have the device for further investigation and analysis.
- MDIs: the hospital should inform industry/vendors of an MDI as soon as possible. The manufacturers/importers are required to determine causes and corrective actions.
- Communication among all parties is an effective mechanism to ensure product improvement and patient safety.
Submitting Reports to Health Canada
Submitting Serious ADR and MDI Reports to Health Canada
- Health Canada remains flexible and is able to receive reports in various formats via multiple secure submission methods, recognizing that hospital systems vary.
- If interested in submitting reports electronically to Health Canada, please email the Canada Vigilance Program at hc.canada.vigilance.sc@canada.ca.
- Health Canada supports report submissions using a secure File Transfer Protocol (sFTP) and continues to explore system-to-system options.
- The reporting forms for serious ADRs and MDIs, together with instructions, are available on the Health Canada website:
Serious Adverse Drug Reaction (Serious ADR)
- A noxious and unintended response to a drug that occurs at any dose and that
- requires in-patient hospitalization or prolongation of existing hospitalization,
- causes congenital malformation,
- results in persistent or significant disability or incapacity,
- is life-threatening, or
- results in death.Footnote 1
Examples of Serious ADRs
- Kidney damage from a diuretic (water pill) that requires dialysis
- Lung damage from a chemotherapy drug that requires long-term oxygen therapy
- Allergic reaction to an antibiotic that is life-threatening
New Form for Mandatory Reporting of Serious ADRs
The new reporting form for serious ADRs, together with instructions, are available on the Health Canada website.
Medical Device Incident (MDI)
- An incident related to a failure of a medical device or a deterioration in its effectiveness, or any inadequacy in its labelling or in its directions for use that has led to the death or a serious deterioration in the state of health of a patient, user, or other person, or could do so were it to recur.Footnote 1
Examples of MDIs
- An infusion pump stopped due to a malfunction, but failed to give an alarm. The patient received an under-infusion of antibiotics; septic shock occurred and prolonged the patient’s stay in the hospital’s intensive care unit.
- An external defibrillator failed to deliver the programmed level of energy to a patient due to a malfunction. The patient was not revived.
Note: If the patient was revived, this would be considered a potential to cause serious harm (if it had not been for the timely intervention by a health care provider) and would also be reportable.
New Form for Mandatory Reporting of MDIs
The reporting form for MDPs was created for multiple reporting uses:
- Mandatory reporting for
- hospitals,
- Special Access Program (SAP),
- Investigational Testing Authorization (ITA)
- Voluntary reporting to Canadian Medical Devices Sentinel Network (CMDSNet) by participating institutions
The new reporting form for MDPs, together with instructions, are available on the Health Canada website.
Case Examples
Case Example 1: Is the Hospital Required to Report?
A patient had been taking warfarin, among other medications, and presented to the emergency department with a life-threatening gastrointestinal bleed. The patient required hospitalization in order to be stabilized.
Rationale:
- Life-threatening condition
- Resulted in in-patient hospitalization
- ADR meets the criteria of “serious”
Case Example 2: Is the Hospital Required to Report?
A patient diagnosed with Hodgkin's lymphoma was being treated with doxorubicin, bleomycin, vincristine, and dacarbazine. Following cycle 3, the patient was admitted as an in-patient with complaints of dry cough and shortness of breath on exertion. Bleomycin-induced pulmonary fibrosis was suspected.
Rationale:
- Life-threatening condition
- Resulted in in-patient hospitalization
- ADR meets the criteria of “serious”
Note: This ADR also meets the criteria of "serious" because bleomycin-induced pulmonary fibrosis may be considered a persistent and significant disability as it can impact the patient's quality of life, given that it can take a long time for an improvement in pulmonary function.
Case Example 3: Is the Hospital Required to Report?
A patient has been recently started on the oral anticoagulant warfarin and is having international normalized ratio (INR) monitored at an out-patient anticoagulation clinic at a hospital. The patient reported a nosebleed that occurred in the time between clinic appointments. Based on the patient's INR level, the patient's warfarin dose was adjusted. The patient will continue to have INR monitored at the hospital.
Rationale:
While the patient may be at increased risk for another bleed (with an elevated INR and recent nosebleed), the ADR does not meet the criteria for “serious”.
Case Example 4: Is the Hospital Required to Report?
A patient was being treated with doxorubicin and cyclophosphamide, and developed neutropenia. After assessing the severity of the neutropenia, a decision was made to continue with chemotherapy at a reduced dose with growth factor support.
Rationale:
While the patient may be at increased risk for potentially fatal infections, the ADR is not immediately life-threatening.
Note: This ADR would need to be reported if the patient developed febrile neutropenia and required in-patient hospitalization for treatment (e.g., antimicrobials to prevent infectious complications from febrile neutropenia).
Case Example 5: Is the Hospital Required to Report?
A patient experienced dizziness and sweating after a dose of insulin. The patient required glucose tablets to recover. It was discovered that a short-acting insulin had been provided instead of the patient’s usual long-acting insulin.
Rationale:
- A medication incident, also referred to as a medication error, is a mistake with medication or a problem that could cause a mistake with medication.
- Medication incidents are generally preventable and include errors such as receiving the wrong medication or dose, or using the wrong route of administration.
Note: Medication incident-related reporting and learning occurs through a separate and complementary program: the Canadian Medication Incident Reporting and Prevention System (CMIRPS).
Source: Health Canada's role in the Management and Prevention of Harmful Medication Incidents
Case Example 6: Is the Hospital Required to Report?
Patients undergoing endometrial ablation of the uterus suffered burns to adjacent organs; these burns were due to thin uterine walls and were an unanticipated side effect of ablation. The manufacturer failed to change the ablation device label to warn users of this side effect (which may be produced when the device is working within specification).
Rationale:
- Serious deterioration in the state of health of a patient
- Reportable MDI
Case Example 7: Is the Hospital Required to Report?
A health care professional reported that the sewing cuff was discovered to be defective during a heart valve implant. The defective valve was abandoned, a new valve was implanted, and pumping time during surgery was extended. This defect had the potential to cause serious harm.
Rationale:
- Potential for death or serious deterioration in the state of health of this patient due to extended surgical time and this possible defect being missed prior to surgical close on other patients leading to emergency failure
- Reportable MDI
Case Example 8: Is the Hospital Required to Report?
A batch of out-of-specification blood glucose test strips is released by a manufacturer. The patient uses strips according to instructions, but readings provide incorrect values leading to incorrect insulin dosage, resulting in hypoglycemic shock and hospitalization.
Rationale:
- Serious deterioration in the state of health of a patient
- Reportable MDI
Case Example 9: Is the Hospital Required to Report?
A user performed an inflation test prior to inserting the balloon catheter into the patient, as required in the instructions for use accompanying the device. A malfunction on inflation was detected and another balloon was used.
Rationale:
This device deficiency would always be found by the user prior to patient use and is an expected potential deficiency noted in the product’s instructions for use.
If the user performed the testing prior to use, as per the instructions, no harm would come to a patient.
Case Example 10: Is the Hospital Required to Report?
A patient died after dialysis treatment. The patient had end-stage renal disease and died of renal failure.
Rationale:
When the hospital has information that the cause of the incident was definitely due to a patient's condition, the incident does not need to be reported. The patient’s condition could be pre-existing or occurring during device use. An incident due to a patient’s condition does not meet the requirements of an MDI.
Mandatory Reporting of Serious ADRs and MDIs by Hospitals: Guidance Document
- Introduction
- The regulations and their purpose
- Purpose
- Serious ADR and MDI definitions
- Roles and responsibilities
- Role of hospitals / health care professionals
- Other types of facilities (e.g., private clinics, nursing homes, outpatient clinics)
- Hospital’s requirement to report in other situations (examples)
- Applicability of the regulations according to product type
- Applicable therapeutic products / medical devices
- Non-applicable therapeutic products / medical devices
- Determination of applicability for combination products
- Serious ADRs or MDIs to be reported by hospitals
- Serious ADR / MDI reportability considerations
- Serious ADR / MDI examples
- Outcomes associated with MDIs
- Causality assessment / hospital investigations
- Documentation examples
- Information requirements for serious ADR and MDI reports
- Serious ADR / MDI data elements
- When and how to submit serious ADR and MDI reports
- Reporting timeline
- Health Canada follow-up requests
- How to send reports (submission methods and formats)
- Links to ADR/MDI reporting forms
- Use of third-party reporters
- Feedback
- Privacy
- Privacy considerations when submitting reports
- Additional reporting considerations
- Submission of reports to manufacturers
- Submission of reports to CMDSNet
- Compliance and enforcement
- Health Canada compliance and enforcement actions for hospitals
Appendices
- Appendix 1: Acronyms, Definitions and Terminology
- Appendix 2: Third-party Reporting Authorization Form
- Appendix 3: Reporting requirements for therapeutic products not subject to the new regulations for hospitals
- Appendix 4: Quick Reference Guide
Voluntary Reporting to Health Canada
Voluntary Adverse Reaction (AR) and Medical Device Problem (MDP) Reporting
- Health Canada builds post-market safety knowledge integral to informing effective clinical use of health products. This safety knowledge is derived from several data sources, including serious ADR and MDI reports.
- Voluntary reporting of suspected ARs or MDPs by health professionals and consumers is another method to monitor the safety and effectiveness of marketed health products
Adverse Reaction (AR)
- A noxious and unintended effect to a health product.Footnote 2
Examples of ARs
- Reduced kidney function from a diuretic (water pill)
- Reduced lung capacity from a chemotherapy drug
- Allergic reaction to an antibiotic
Medical Device Problem (MDP)
- A medical device problem is related to:
- inadequate labelling or instructions for use
- a failure of the device or a deterioration in its effectiveness
- an actual or potential deficiency that may affect product performance or safetyFootnote 2
Note: Medical device problem reporting includes any type of medical device issue; it does not necessarily meet the definition of an MDI
Examples of MDPs
- Tubing leaked, causing a delay in treatment, but there was no serious harm to the patient
- Needle broke during a blood draw, but it was removed with minor injury to the patient
Canada Vigilance Program
The Canada Vigilance Program is a national post-market monitoring program that collects and assesses reports of suspected ARs and MDPs involving health products marketed in Canada.
AR Voluntary Reporting for Health Products
- Online form
- Telephone: 1-866-234-2345 (toll-free)
- Fax or Mail: Download, print and complete the Side Effect Reporting Form
(please read the instructions before completing the form)- Fax: 1-866-678-6789 (toll-free)
- Mail: Canada Vigilance Office (using the postage paid label)
MDP Voluntary Reporting
- The Canadian Medical Devices Sentinel Network (CMDSNet) is a pro-active surveillance program that encourages the reporting of MDP reports from all types of institutions.
- Only institutions participating in CMDSNet voluntarily report MDIs occurring within their organizations directly through the Canada Vigilance Program
- Other voluntary reporting from non-participating CMDSNet institutions, consumers, and health professionals are encouraged to report device-related incidents directly to Health Canada by completing a Health Product Complaint Form via the Regulatory Operations and Enforcement Branch.
Reporting ARs and MDPs to Health Canada
The Report an Adverse Reaction or Medical Device Problem web page provides access to more information and forms.
Key Points to Remember
- Hospital systems, processes, policies, procedures, and forms may need to be updated to reflect requirements for mandatory reporting of serious ADRs and MDIs to Health Canada.
- Health care professionals have an important role in serious ADR and MDI reporting.
- Health Canada is open to accepting different formats for reports of serious ADRs and MDIs, recognizing that hospital systems vary.
- It is important to understand the differences between serious ADRs, MDIs, medication incidents, ARs, and MDPs, and how to report them.
- The Guidance Document offers information to help hospitals comply with the regulatory requirements for serious ADR and MDI reporting to Health Canada.
- Health Canada values voluntary reporting and has programs to support it.
Abbreviations
- ADR:
- Adverse Drug Reaction
- AR:
- Adverse Reaction
- CMDSNet:
- Canadian Medical Devices Sentinel Network
- CMIRPS:
- Canadian Medication Incident Reporting and Prevention System
- ITA:
- Investigational Testing Authorization
- MDI:
- Medical Device Incident
- MDP:
- Medical Device Problem
- SAP:
- Special Access Program
- sFTP:
- Secure File Transfer Protocol
Resources
- Applications for Medical Device Investigational Testing Authorizations Guidance Document - Summary
- Canadian Medical Devices Sentinel Network
- Canadian Medication Incident Reporting and Prevention System
- Canada Vigilance Program
- MedEffect Canada
- Mandatory reporting of serious adverse drug reactions and medical device incidents by hospitals - Guidance document
- Health Canada's role in the Management and Prevention of Harmful Medication Incidents
- Health Product Complaint Form
- Medical Devices Regulations
- Medical Devices - Special Access Programme
- Side Effect Reporting Form
- Protecting Canadians from Unsafe Drugs Act (Vanessa’s Law) Amendments to the Food and Drugs Act (Bill C-17)
- Regulations Amending the Food and Drug Regulations (Serious Adverse Drug Reaction Reporting - Hospitals): SOR/2019-190
- Regulations Amending the Medical Devices Regulations (Medical Device Incident Reporting - Hospitals): SOR/2019-191
- Report An Adverse Reaction or Medical Device Problem
For additional information, please contact the Canada Vigilance Program at:
Email: hc.canada.vigilance.sc@canada.ca
Telephone: 1-866-234-2345
Acknowledgments
- All materials were developed by the collaborating parties: Health Canada, Institute for Safe Medication Practices Canada (ISMP Canada), Health Standards Organization (HSO), and the Canadian Patient Safety Institute (CPSI).
- Any stakeholder interested in using the materials should acknowledge Health Canada as the owner and source:
Educational Support for Mandatory Reporting. Health Canada; 2019.
- Footnote 1
-
Mandatory reporting of serious adverse drug reactions and medical device incidents by hospitals - Guidance document
- Footnote 2
-
Report an adverse reaction or medical device problem
Page details
- Date modified: