Characteristics of patients with repeat hospitalizations for substance-related harms in Canada
Table of contents
- Background
- Definitions included in this report
- Key findings
- In summary
- Acknowledgements
- Disclaimer
- Suggested citation
- Technical notes
- Appendix A
- Appendix B
- Appendix C
- References
Background
Canada is currently experiencing an overdose crisis. In addition to ongoing surveillance, the Public Health Agency of Canada (PHAC) releases targeted analytical reports on specific topics in substance-related harms to help fill gaps identified by stakeholders.
Hospitalizations for substance-related harms, including substance use disorders (SUDs) and substance-related poisonings (overdoses), frequently occur in Canada. For Canadians aged 10 and older, hospitalizations for substance-related harms increased from 477 stays per 100,000 Canadians in 2017 to 555 stays per 100,000 Canadians in 2021Footnote 1.
Overall, SUDs were the fifth most common reason for hospitalization in Canada from 2021 to 2022Footnote 2. Alcohol alone contributes to more than half of hospitalizations related to substance useFootnote 1. In addition to alcohol, other substances that are commonly involved in hospitalizations include:
- cannabis
- opioids
- stimulantsFootnote 3
People who have been hospitalized with an SUD have high rates of repeat (multiple) hospitalizationsFootnote 4 Footnote 5. Repeat hospitalizations for substance-related harms may differ by the reason for hospitalization. For example, the rate of repeat hospitalizations for individuals with an opioid use disorder (OUD) is higher than that for opioid poisoningsFootnote 6.
Rates of repeat hospitalizations for reasons related to mental health and substance use have been increasing in Canada, from 11.6% in 2013 to 13.5% in 2021Footnote 7. As such, it is important to describe the distribution and characteristics of repeat hospitalizations for substance-related harms.
The objectives of this analysis are to describe:
- the distribution of repeat hospitalizations in Canada for substance-related poisonings and substance-related disorders (SRDs)
- how repeat hospitalizations differ by patient demographics of sex and age
- how they differ by hospitalization characteristics:
- length of stay
- discharge disposition
- poisoning intention
Findings can be used to inform prevention strategies, treatment and recovery services and systems, and harm reduction interventions to improve the health of people who are hospitalized for substance-related poisonings and SRDs.
Definitions included in this report
Substance-related poisonings
A substance poisoning harm (overdose) resulting from the use of one or multiple substances in an accidental, intentional, or unknown manner.
Substance-related disorders (SRDs)
A mental or behavioural disorder related to the use of substances (such as a substance use disorder), or a medical condition related to the use of substances (such as alcoholic liver disease).
Repeat hospitalizations
A hospitalization for a substance-related harm (that is, substance-related poisoning or SRD) that is following at least one other hospitalization for the same reason as their first identified hospitalization (that is, another substance-related poisoning or SRD) in the previous five years.
For more information, please see Technical notes.
Key findings
In Canada (excluding Quebec) in 2021, there were more patients with repeat hospitalizations in the past five years for SRDs (n = 46,441) than for substance-related poisonings (n = 1,690) (Figure 1).
There was a similar proportion of patients with single hospitalizations (51%) as repeat hospitalizations (49%) for SRDs. In comparison, there was a greater proportion of patients with single hospitalizations (86%) compared to repeat hospitalizations (14%) for substance-related poisonings.
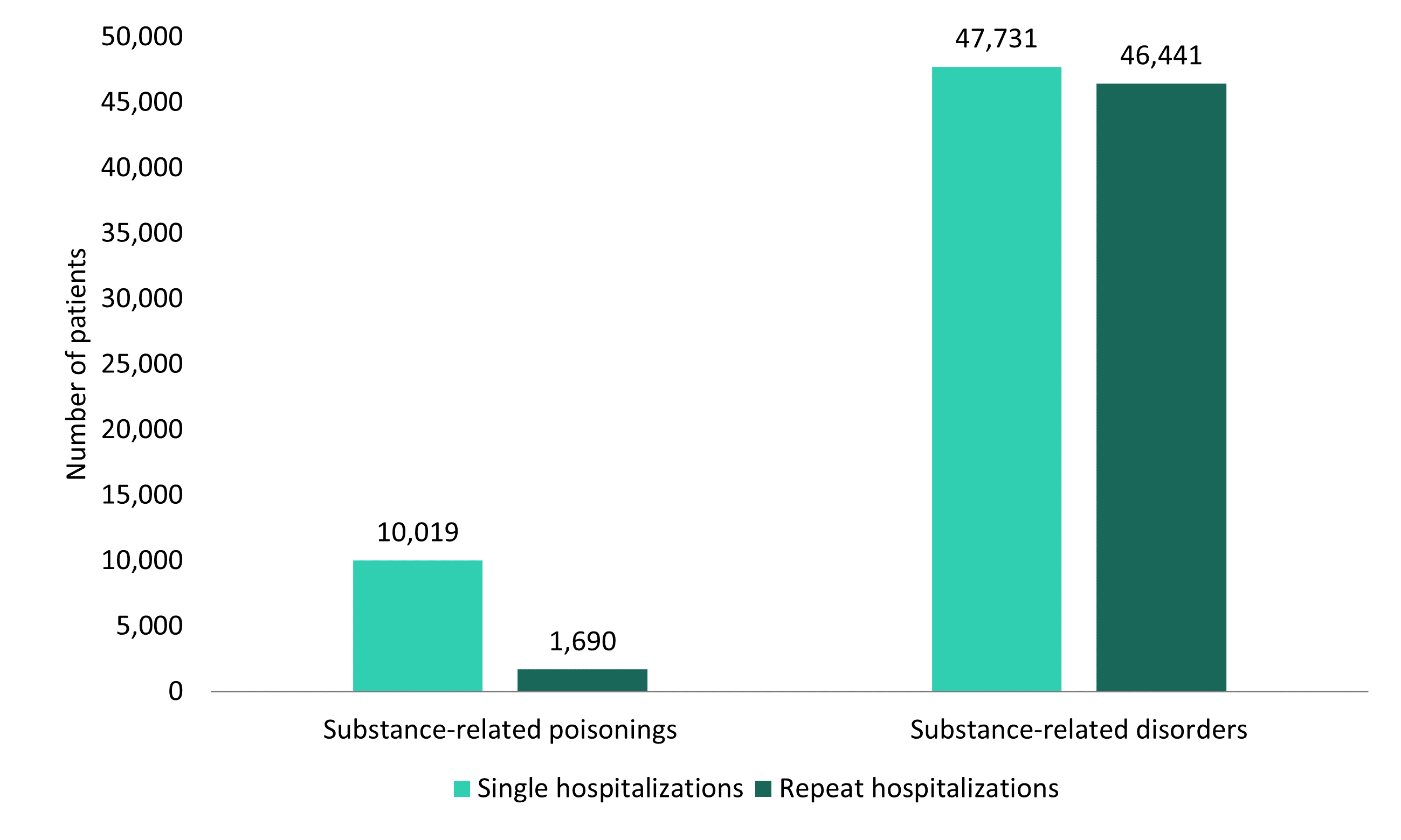
Figure 1 - Text description
| Substance-related poisonings | Substance-related disorders | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| Single hospitalizations | 10,019 | 86 | 47,731 | 51 |
| Repeat hospitalizations | 1,690 | 14 | 46,441 | 49 |
| Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). | ||||
Sex
In the past five years, the number of patients in Canada (excluding Quebec) in 2021 with single or repeat hospitalizations for SRDs was greater among males than females (Figure 2a), whereas numbers were somewhat similar for substance-related poisonings (Figure 2b). For substance-related poisonings, the number of patients with repeat hospitalizations were 864 for males and 826 for females. In contrast, the number of patients with repeat hospitalizations for SRDs was almost twice as high for males (n = 30,019) than for females (n = 16,410). Proportions of patients with single and repeat hospitalizations for substance-related harms were similar between males and females.
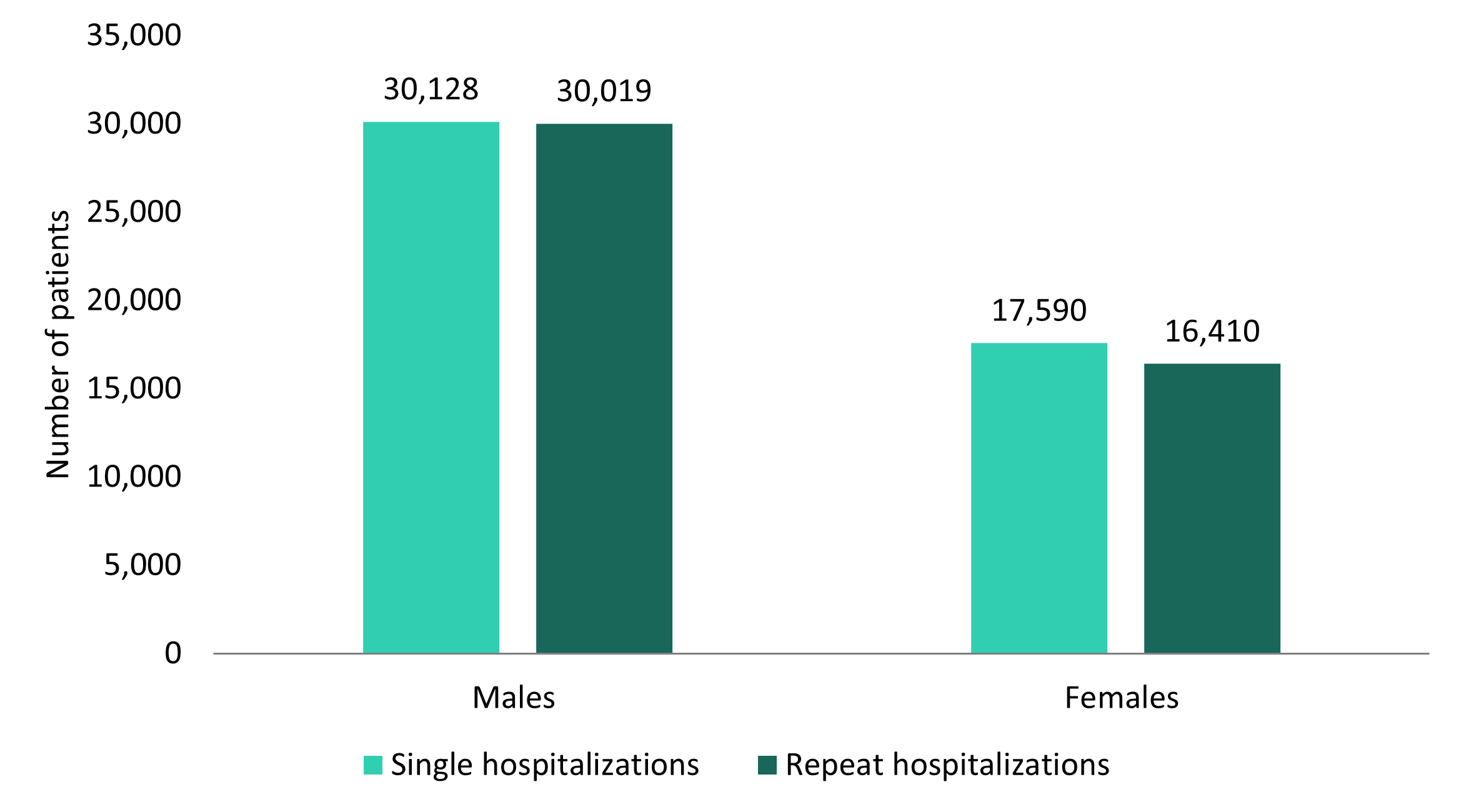
Figure 2a - Text description
| Males | Females | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| Single hospitalizations | 30,128 | 50 | 17,590 | 52 |
| Repeat hospitalizations | 30,019 | 50 | 16,410 | 48 |
Notes: Counts within sex may not align with total counts due to missing values for some variables (for example, individuals whose sex was "other" or unknown were excluded due to low numbers). Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
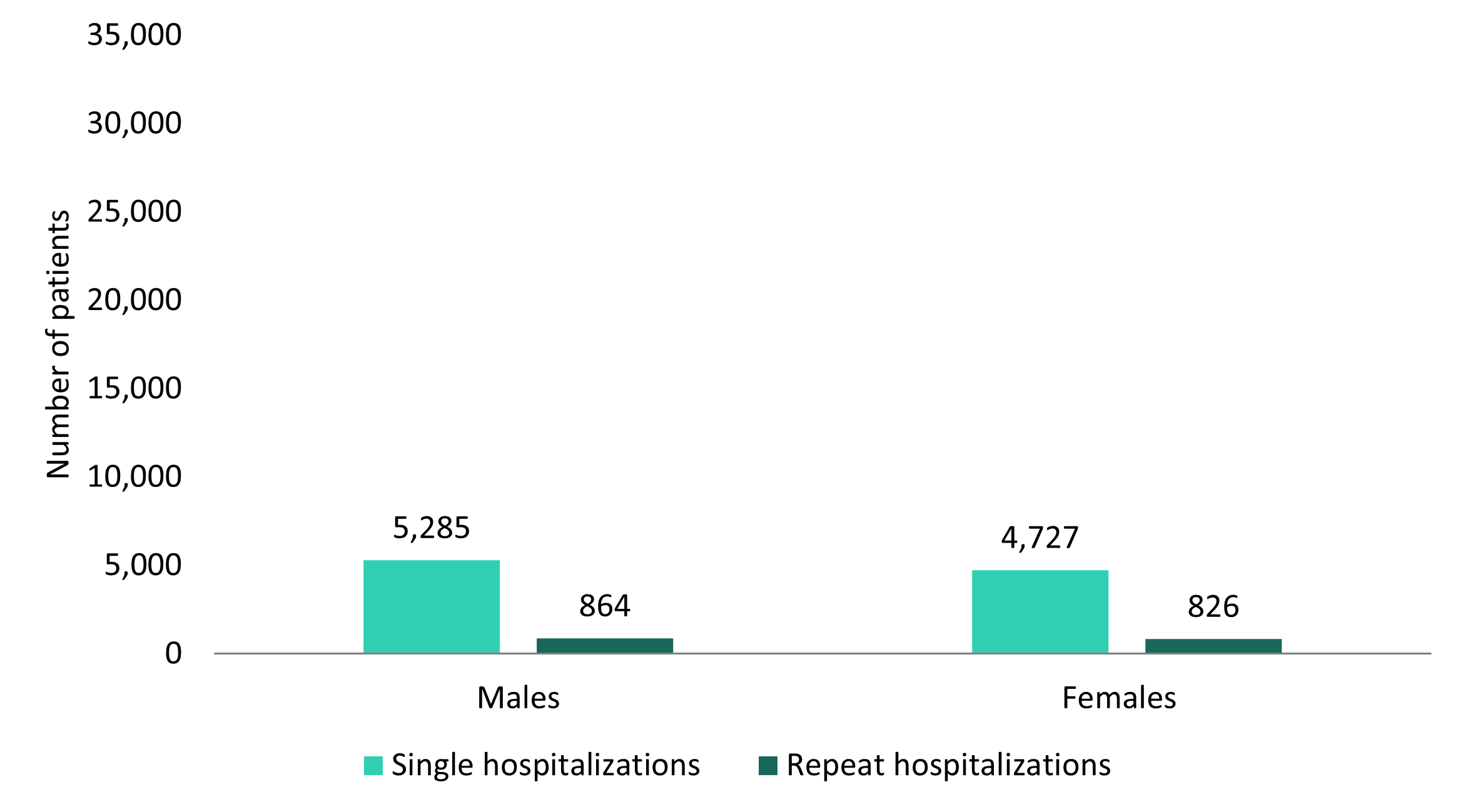
Figure 2b - Text description
| Males | Females | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| Single hospitalizations | 5,285 | 86 | 4,727 | 85 |
| Repeat hospitalizations | 864 | 14 | 826 | 15 |
Notes: Counts within sex may not align with total counts due to missing values for some variables (e.g., individuals whose sex was "other" or unknown were excluded due to low numbers). Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
Age
Repeat hospitalizations in the past five years for SRDs and substance-related poisonings were greatest among those aged 30 to 39, where there were 11,195 patients with repeat hospitalizations for SRDs and 377 patients with repeat hospitalizations for substance-related poisonings (Table 1a and Table 1b). However, the numbers of patients with single hospitalizations for SRDs (n = 11,442) and for substance-related poisonings (n = 2,015) were greatest among those aged 60 years and older.
| Single hospitalizations | Repeat hospitalizations | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| 0 to 19 years | 3,235 | 70 | 1,408 | 30 |
| 20 to 29 years | 9,116 | 51 | 8,727 | 49 |
| 30 to 39 years | 9,519 | 46 | 11,195 | 54 |
| 40 to 49 years | 7,154 | 46 | 8,282 | 54 |
| 50 to 59 years | 7,263 | 47 | 8,082 | 53 |
| 60 years and older | 11,442 | 57 | 8,747 | 43 |
Notes: Counts within age may not align with total counts due to missing values for some variables. Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
| Single hospitalizations | Repeat hospitalizations | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| 0 to 19 years | 1,313 | 93 | 106 | 7 |
| 20 to 29 years | 1,756 | 84 | 325 | 16 |
| 30 to 39 years | 1,908 | 84 | 377 | 17 |
| 40 to 49 years | 1,564 | 84 | 309 | 17 |
| 50 to 59 years | 1,462 | 84 | 270 | 16 |
| 60 years and older | 2,015 | 87 | 303 | 13 |
Notes: Counts within age may not align with total counts due to missing values for some variables. Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
Length of stay
In 2021, patients in Canada (excluding Quebec) with both single and repeat hospitalizations in the past five years for SRDs had longer lengths of stay in hospital, on average, than patients hospitalized for substance-related poisonings (Figure 3). For substance-related poisonings, the length of stay is longer for patients with repeat hospitalizations than for patients with single hospitalizations. Conversely, for SRDs, those with single hospitalizations had a slightly longer length of stay.
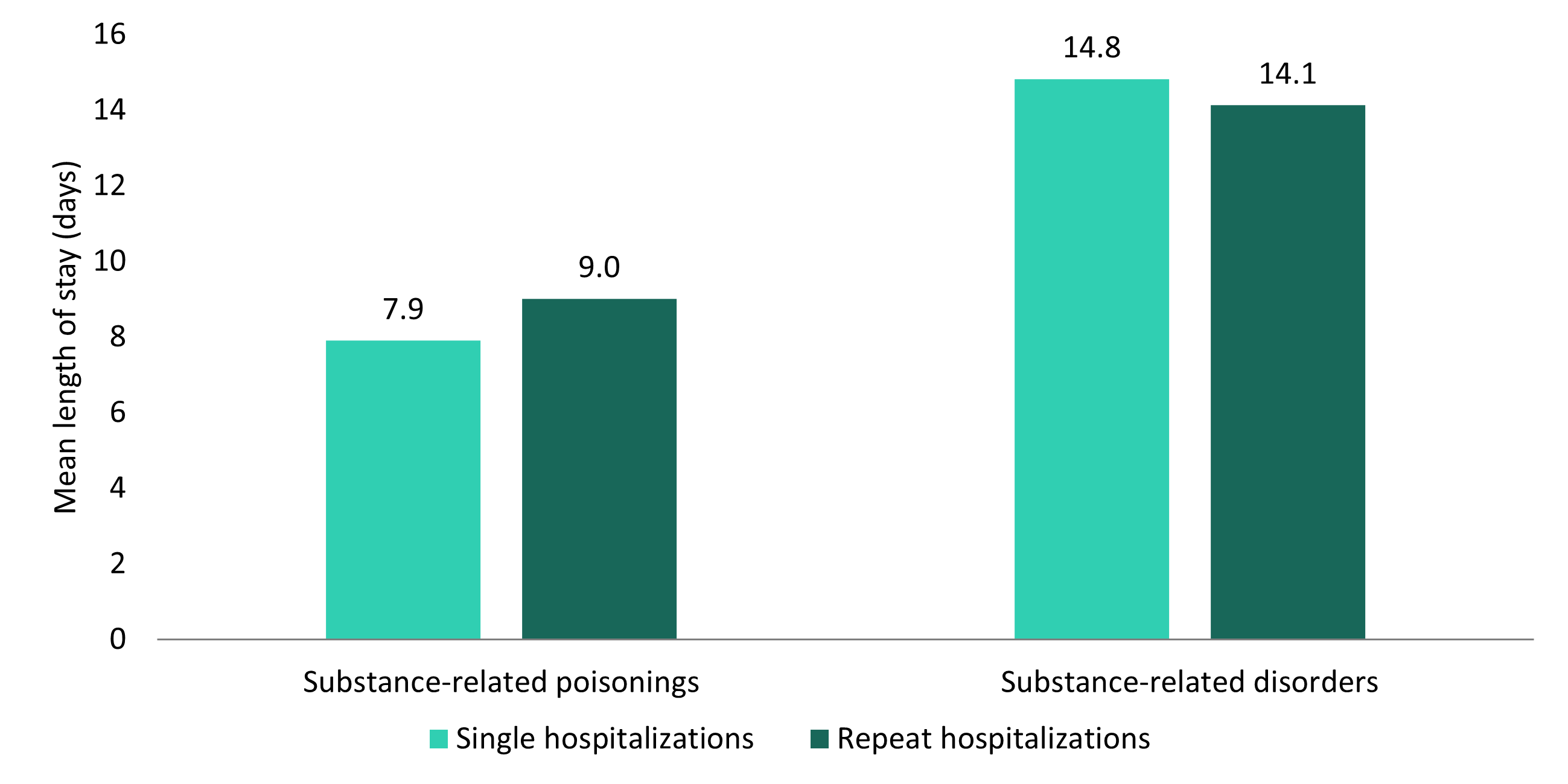
Figure 3 - Text description
| Substance-related poisonings | Substance-related disorders | |
|---|---|---|
| Mean length of stay (days) | ||
| Single hospitalizations | 7.9 | 14.8 |
| Repeat hospitalizations | 9.0 | 14.1 |
| Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). | ||
Discharge disposition
In 2021, a majority of patients with hospitalizations for both substance-related poisonings and SRDs in Canada (excluding Quebec) were discharged home without support (Figure 4a and Figure 4b). Compared to patients with single hospitalizations, a greater proportion of patients with repeat hospitalizations for substance-related poisonings or SRDs either left against medical advice or were transferred.
A larger proportion of patients with repeat hospitalizations for SRDs were discharged home without support (59%), compared to patients with repeat hospitalizations for substance-related poisonings (52%). In contrast, a larger proportion of patients with repeat hospitalizations for substance-related poisonings left against medical advice (17%), compared to patients with repeat hospitalizations for SRDs (11%). A similar pattern was seen for patients with single hospitalizations.
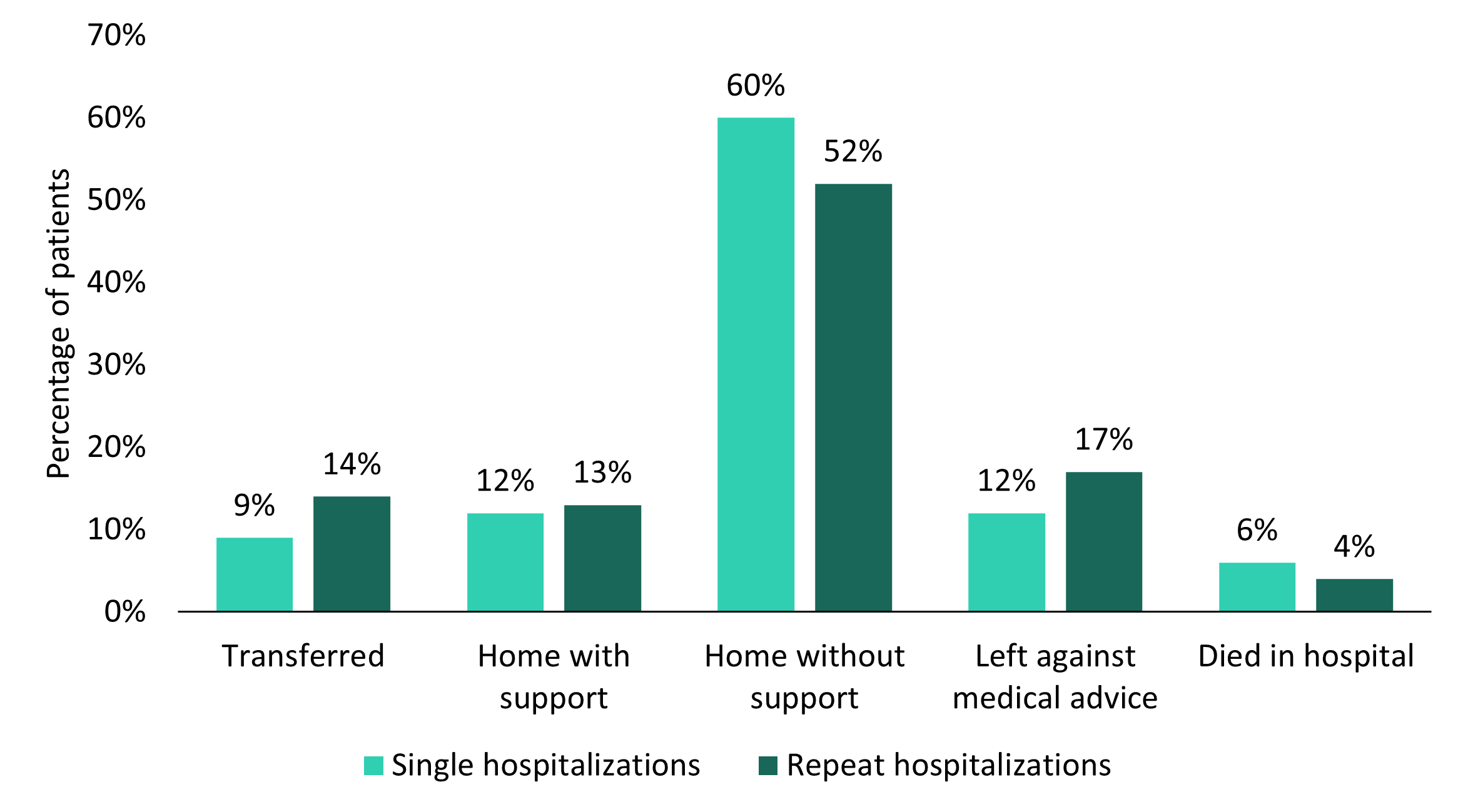
Figure 4a - Text description
| Single hospitalizations | Repeat hospitalizations | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| Transferred | 935 | 9 | 236 | 14 |
| Home with support | 1,216 | 12 | 220 | 13 |
| Home without support | 6,048 | 60 | 879 | 52 |
| Left against medical advice | 1,227 | 12 | 281 | 17 |
| Died in hospital | 593 | 6 | 74 | 4 |
Notes: Counts within discharge disposition may not align with total counts due to missing values for some variables. Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
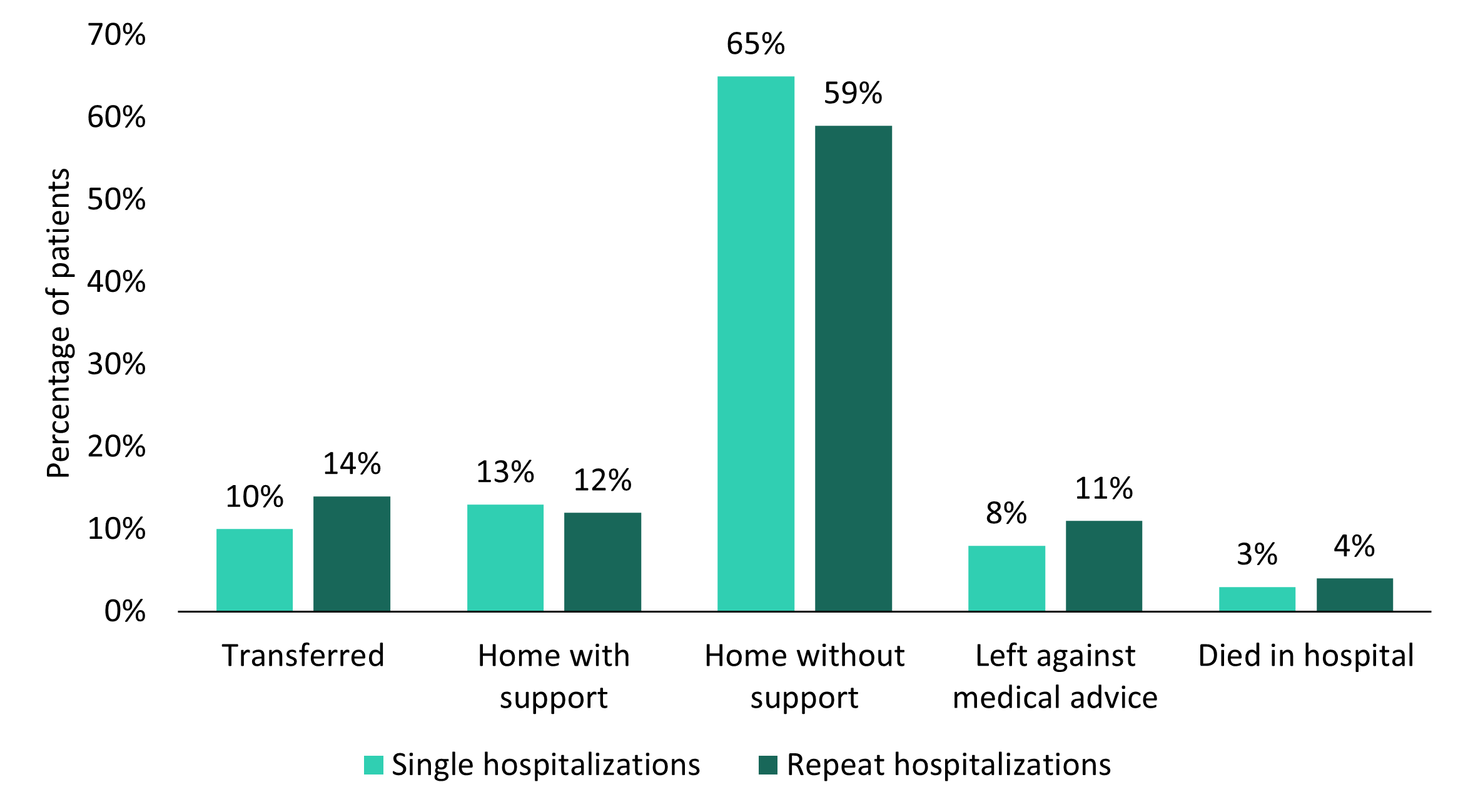
Figure 4b - Text description
| Single hospitalizations | Repeat hospitalizations | |||
|---|---|---|---|---|
| Number of patients | Percentage of patients (%) | Number of patients | Percentage of patients (%) | |
| Transferred | 5,003 | 10 | 6,621 | 14 |
| Home with support | 6,202 | 13 | 5,667 | 12 |
| Home without support | 31,013 | 65 | 27,183 | 59 |
| Left against medical advice | 3,945 | 8 | 5,218 | 11 |
| Died in hospital | 1,568 | 3 | 1,752 | 4 |
Notes: Counts within discharge disposition may not align with total counts due to missing values for some variables. Sources: Discharge Abstract Database (DAD) and Ontario Mental Health Reporting System (OMHRS) 2016-2021, Canadian Institute for Health Information (CIHI). |
||||
Intention of substance-related poisoning
In Canada (excluding Quebec) in 2021, intention of substance-related poisoning hospitalizations did not vary regardless of single or repeat hospitalization status in the past five years. Most patients (55%) with single and repeat hospitalizations for substance-related poisonings in the past five years had poisonings that were reported as accidental. Substance-related poisonings classified as intentional accounted for 35% of poisonings among both patients with single and repeat hospitalizations. Substance-related poisoning hospitalizations of undetermined intention accounted for the lowest proportion among both patients with single and repeat hospitalizations, at approximately 10%.
In summary
Canada continues to experience an overdose crisis, and understanding healthcare utilization can help to inform opportunities for prevention, treatment and recovery services and systems, and harm reduction interventions. In particular, understanding the distribution and characteristics of repeat hospitalizations for substance-related harms can help target interventions and strategies based on sex, age groups, the nature and intent of the harms, and discharge disposition.
The findings from this report highlight that repeat hospitalizations largely occur among those experiencing SRDs, rather than substance-related poisonings. Overall, while patients with single and repeat hospitalizations for substance-related harms had some similar characteristics (such as poisoning intention and length of stay), key differences emerged.
With regards to patient characteristics, a greater number of patients with repeat hospitalizations for substance-related poisonings or SRDs were aged 30 to 39 years, whereas a greater number of patients with single hospitalizations for substance-related poisonings or SRDs were aged 60 and older. While males had more overall substance-related harm hospitalizations than females, particularly for SRDs, the proportions of repeat hospitalizations were similar. This suggests that younger people (such as those aged 30 to 39 years) and males may be at a higher risk for repeat hospitalizations, particularly for SRDs.
When considering hospitalization characteristics, the greatest proportion of patients with repeat hospitalizations for substance-related poisonings or SRDs were discharged home without support and a smaller proportion were transferred or left against medical advice. These patients may not be accessing the care that they need, which may contribute to an increased risk for repeat hospitalizations. Repeat interactions with the healthcare system offer opportunities to support individuals experiencing substance-related harms. For example, an Ontario study found that approximately half of people who died of an opioid-related toxicity between March 17, 2020 and December 31, 2020 had past-month contact with the healthcare systemFootnote 8. Given that 35% of substance-related poisonings were classified as intentional, it is important to develop interventions to reduce intentional poisonings, both among those with single and those with repeat hospitalizations.
Future research could explore how repeat hospitalizations for substance-related harms differ between substances involved such as alcohol, opioids, or stimulants, to better understand populations who are at higher risk of repeat hospitalizations for substance-related harms. Further analyses could explore the distribution and characteristics of other indicators of substance-related harms, such as repeat emergency department visits. The Government of Canada will continue to improve data and analysis to inform strategies and interventions to help reduce substance-related harms across Canada.
Acknowledgements
We would like to acknowledge the Canadian Institute for Health Information (CIHI) for collecting and providing the data and analyses used in this report.
Disclaimer
Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of CIHI.
Suggested citation
Characteristics of patients with repeat hospitalizations for substance-related harms in Canada. Ottawa: Public Health Agency of Canada; September 2023.
Technical notes
Methodology
Data from the Canadian Institute for Health Information's (CIHI) Discharge Abstract Database (DAD) and the Ontario Mental Health Reporting System (OMHRS) between January 1, 2016 and December 31, 2021 were used for this descriptive report. This analysis included hospital stays for inpatient care and day surgery, which are nationally representative across Canada, except for Quebec.
To identify substance-related poisonings and substance-related disorders (SRDs), International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) codes were used in the DAD. To identify SRDs, ICD-10-CA codes and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used in the OMHRS.
Repeat hospitalizations
While many analyses of hospitalization data are event-based (meaning counts refer to individual hospitalizations), this analysis is person-based (meaning counts refer to individual patients). Patients with repeat hospitalizations were identified from their most recent hospitalization discharge for a substance-related poisoning or SRD in 2021. If that patient had at least one other hospitalization for the same reason as their first identified hospitalization (meaning another substance-related poisoning or SRD) in the previous five years, they were identified as having a repeat hospitalization.
For example, if the patient was hospitalized on March 1, 2021, the look back period would extend to March 1, 2016. If they did not have another hospitalization for the same reason in the previous five years, they were identified as having a single hospitalization. If a patient received a diagnosis for a substance-related poisoning and a SRD within a single hospitalization, they were counted in both substance-related harm categories.
Substance-related poisonings
A complete list of all ICD-10-CA codes used to identify substance-related poisonings is available in Appendix AFootnote 9. Poisonings may include the following substances:
- Alcohol
- Cannabis
- Central nervous system (CNS) stimulants
- Hallucinogens
- Opioids
- Other CNS depressants
- Unknown substances
- Multiple substances
Information on these substance-related poisonings was extracted from patient charts by trained coders, which may be based on toxicological analysis or patient self-report.
For substance-related poisoning diagnoses in the DAD, analyses included the following diagnosis types:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnoses ("W", "X", and "Y")
- Unconfirmed or query ("Q")
Records indicating the patient was admitted to the facility as a cadaveric donor and stillbirths were excluded ("R" or "S"), as were secondary diagnoses ("3"). For 2018 to 2019 data onward, medical assistance in dying (MAID; "73") was also excluded.
Intention
For all poisonings, coders assign an external cause ICD-10-CA code from physician documentation where available to indicate the intention (reason) for the poisoningFootnote 10. Three groups are outlined by the ICD-10-CA.
Accidental
A substance-related poisoning hospitalization that is considered to be non-intentional in nature and is identified by an associated external cause ICD-10-CA code of X41, X42, or X45.
Intentional
A substance-related poisoning hospitalization that occurred as a result of purposely self-inflicted harm and is identified by an associated external cause ICD-10-CA code of X61, X62, or X65.
Undetermined
A substance-related poisoning hospitalization which has been documented to be of undetermined or unknown intention and is identified by an associated external cause ICD-10-CA code of Y11, Y12, or Y15.
Substance-related disorders
A complete list of all ICD-10-CA codes and DSM-5 codes used to identify SRDs is available in Appendix B and Appendix C, respectivelyFootnote 9. SRDs may include the following substances:
- Alcohol
- Opioids
- Cannabis
- Other central nervous system (CNS) depressants
- Cocaine
- Other CNS stimulants
- Other substances
- Unknown substances
- Multiple substances
For SRD diagnoses in the DAD, analyses included the following diagnosis types:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnoses ("W", "X", and "Y")
- Unconfirmed or query ("Q")
For SRD diagnoses for alcohol in the OMHRS, analyses included the following diagnosis types:
- DSM-5 codes 100% attributable to alcohol coded as a principal or secondary diagnosis for inpatient records
- Category diagnosis of a substance-related or addictive disorder coded as a principal or secondary diagnosis with an emergency department visit (NACRS) than is 100% attributable to alcohol within seven days prior to admission to an OHMRS bed
For SRD diagnoses for other substances in the OMHRS, analyses included the following diagnosis types:
- DSM-5 codes for harm caused by substance use
- Category diagnosis of a substance-related or addictive disorder coded as a principal or secondary diagnosis
Records indicating the patient was admitted to the facility as a cadaveric donor and stillbirths were excluded ("R" or "S"). For data from 2018 to 2019 and onward, medical assistance in dying (MAID; "73") was also excluded.
Sex and age
Assigned sex at birth (for example, recorded on the original birth certificate) and age group were identified from the patient's most recent hospitalization discharge. Assigned sex at birth can be self-reported or clinician-recorded where it is clinically relevant. Age is recorded at discharge, not at admission.
Length of stay
Length of stay is calculated as the difference in days between the admission date and the discharge date, for the patient's most recent hospitalization. If the admission date is the same as the discharge date, the length of stay is calculated as one day.
Discharge disposition
Discharge disposition refers to the location where the patient was discharged to or the status of the patient on discharge. Discharge disposition was identified from the patient's most recent hospitalization. A total of five categories of discharge were investigated.
- Transfer: Identified by a field value of 10, 20, 30, 40, or 90
- Home without support: Identified by a field value of 05
- Home with support: Identified by a field value of 04
- Left against medical advice: Identified by a field value of 61, 62, 65, 66, or 67
- Died in hospital: Identified by a field value of 72, 73, or 74
Limitations
- This descriptive report presents differences between single and repeat hospitalizations by patient demographics and hospitalization characteristics but does not evaluate why these differences occur. Statistical significance between groups was also not evaluated.
- Patient demographics and hospitalization characteristics are based on the patient's most recent hospitalization in 2021, and do not represent previous hospitalizations.
- Some of the hospitalization data in this report was recorded during the COVID-19 pandemic in Canada. This could have led to changes in hospitalization practices and differences in the frequency of single and repeat hospitalizations.
- Patients with unknown or invalid health card numbers were excluded from this analysis, as they could not be linked to their past hospitalizations.
- Substance-related poisonings are classified as accidental unless there is clear documentation of intentional self-harm or undetermined intentionFootnote 11. This may reflect an overrepresentation of accidental poisonings.
- Determining intention can rely on self-reported information which patients may not be willing to disclose due to various reasons, or unable to due to disability or death.
- This analysis reports on assigned sex at birth and does not report on gender identity. It also does not include any individuals who are not recorded as male or female (such as "other" sex or unknown), due to low numbers.
- This report does not include data from the province of Quebec.
- Data released by provinces and territories may differ from the data provided in this report due to the availability of updated data, differences in the type of data reported, the use of alternate case definitions, differences in time periods presented or population estimates used for calculations, or other factors.
Appendix A
| Category | Poisoning ICD-10-CA codes and descriptions |
|---|---|
| Alcohol |
|
| Cannabis |
|
| Central nervous system stimulants |
|
| Hallucinogens |
|
| Opioids |
|
| Other central nervous system depressants |
|
| Unknown and multiple substances |
|
Appendix B
| Category | Mental and behavioural disorders ICD-10-CA codes and descriptions | Medical condition ICD-10-CA codes and descriptions |
|---|---|---|
| Abuse of non-dependence producing substances | F55 Abuse of non-dependence producing substances |
|
| Alcohol | F10 Mental and behavioural disorders due to use of alcohol |
|
| Cannabis | F12 Mental and behavioural disorders due to use of cannabinoids |
|
| Central nervous system stimulants | F14 Mental and behavioural disorders due to use of cocaine F15 Mental and behavioural disorders due to use of other stimulants, including caffeine |
|
| Hallucinogens | F16 Mental and behavioural disorders due to use of hallucinogens |
|
| Opioids | F11 Mental and behavioural disorders due to use of opioids |
|
| Other central nervous system depressants | F13 Mental and behavioural disorders due to use of sedatives or hypnotics |
|
| Solvents | F18 Mental and behavioural disorders due to use of volatile solvents |
|
| Unknown and multiple substances | F19 Mental and behavioural disorders due to use of multiple drug use and use of other psychoactive substances |
|
|
||
Appendix C
| Category | DSM-5 (ICD-9-CM) codes and descriptions | DSM-5 (ICD-10-CA) codes and descriptions |
|---|---|---|
| Alcohol |
|
|
| Cannabis |
|
|
| Central nervous system stimulants |
|
|
| Opioids |
|
|
| Other CNS depressants |
|
|
| Hallucinogens |
|
|
| Solvents |
|
|
| Unknown and multiple substances |
|
|
| Contributes towards a specific substance if relevant ICD-10-CA codes are found in NACRS or towards the unknown and multiple substances category if no relevant code is found |
|
|
|
||
References
- Footnote 1
-
Canadian Institute for Health Information. Your Health System: Hospital Stays for Harm Caused by Substance Use. [Internet]. [cited 2023Jul18]. Available from: https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en&_ga=2.146367223.274130803.1553524706-1669226068.1536351146#!/indicators/080/hospital-stays-for-harm-caused-by-substance-use/;mapC1;mapLevel2;sex(A);trend(C1);/
- Footnote 2
-
Canadian Institute for Health Information. Hospital Stays in Canada [release summary]. 2023 [cited 2023Jul18]. Available from: https://www.cihi.ca/en/hospital-stays-in-canada
- Footnote 3
-
Canadian Institute for Health Information. Hospital Stays for Harm Caused by Substance Use, 2020–2021 and 2021–2022: Substance, Age and Region Level Results — Data Tables. Ottawa, ON: CIHI; 2022 [cited 2023Jul18]. Available from: https://yourhealthsystem.cihi.ca/hsp/inbrief?lang=en&_ga=2.146367223.274130803.1553524706-1669226068.1536351146#!/indicators/080/hospital-stays-for-harm-caused-by-substance-use/;mapC1;mapLevel2;overview;sex(A);trend(C1);/
- Footnote 4
-
Rush B, Furlong A. Rapid Access Models for Substance Use Services: A Rapid Review. Ottawa, ON: Canadian Centre on Substance Use and Addiction; 2020. Available from: https://www.ccsa.ca/sites/default/files/2020-10/CCSA-Rapid-Access-Models-Substance-Use-Services-Rapid-Review-Report-2020-en.pdf
- Footnote 5
-
Nordeck CD, Welsh C, Schwartz RP, Mitchell SG, Cohen A, O'Grady KE, Gryczynski J. Rehospitalization and substance use disorder (SUD) treatment entry among patients seen by a hospital SUD consultation-liaison service. Drug and Alcohol Dependence. 2018 Mar;186:23-28. https://doi.org/10.1016/j.drugalcdep.2017.12.043
- Footnote 6
-
Alsabbagh MW, Chang F, Cooke M, Elliott SJ, Chen M. National trends in population rates of opioid-related mortality, hospitalization and emergency department visits in Canada between 2000 and 2017. A population-based study. Addiction. 2021 Jun;116(12):3482-3493. https://doi.org/10.1111/add.15571
- Footnote 7
-
Canadian Institute for Health Information. Repeat Hospital Stays for Mental Health and Substance Use [indicator]. 2023 [cited 2023Jul18]. Available from: https://www.cihi.ca/en/indicators/repeat-hospital-stays-for-mental-health-and-substance-use
- Footnote 8
-
Gomes T, Murray R, Kolla G, Leece P, Kitchen S, Campbell T, Besharah J, Cahill T, Garg R, Iacono A, Munro C, Nunez E, Robertson L, Shearer D, Singh S, Toner L, Watford J. on behalf of the Ontario Drug Policy Research Network, Office of the Chief Coroner for Ontario and Ontario Agency for Health Protection and Promotion (Public Health Ontario). Patterns of medication and healthcare use among people who died of an opioid-related toxicity during the COVID-19 pandemic in Ontario. Toronto, ON: Ontario Drug Policy Research Network; 2022. Available from: https://odprn.ca/wp-content/uploads/2022/01/Opioid-Related-Toxicity-Deaths-and-Healthcare-Use-Report.pdf
- Footnote 9
-
Canadian Institute for Health Information. Hospital Stays for Harm Caused by Substance Use — Appendices to Indicator Library, December 2022. Ottawa, ON: CIHI; 2022. Available from : https://www.cihi.ca/sites/default/files/document/appendix-hospital-stays-for-harm-caused-by-substance-use-en-web.pdf
- Footnote 10
-
Canadian Institute for Health Information. Types of Opioid Harms in Canadian Hospitals: Comparing Canada and Australia. Ottawa, ON: CIHI; 2018. Available from: https://www.cihi.ca/sites/default/files/document/types-opioids-harm-report-can-aus-nov2018-en-web.pdf
- Footnote 11
-
Canadian Institute for Health Information. Canadian Coding Standards for Version 2022 ICD-10-CA and CCI. Ottawa, ON: CIHI; 2022. Available from: https://secure.cihi.ca/free_products/canadian-coding-standards-2022-en.pdf