Opioid-related harms and mental disorders in Canada: A descriptive analysis of hospitalization data
Canada is currently experiencing an opioid overdose crisis. The Public Health Agency of Canada (PHAC), in collaboration with the provincial and territorial (PT) offices of Chief Coroners and Chief Medical Examiners, PT public health and health partners, and Emergency Medical Services data providers, releases quarterly reports on apparent opioid-related deaths and Emergency Medical Services responses for suspected opioid-related overdoses. PHAC also collaborates with Health Canada to report on hospitalizations for opioid-related poisonings (overdoses) using hospital administrative data from the Canadian Institute for Health Information (CIHI).
There is evidence to suggest that many people experiencing opioid-related harms also experience other mental disorders Footnote 1, Footnote 2, Footnote 3, Footnote 4, Footnote 5, Footnote 6, Footnote 7. Gaining a better understanding of the mental health profile of individuals who experience opioid-related harms has been identified as a priority to inform evidence-based policies and interventions Footnote 8, yet there are limited national data on this topic.
The objective of this analysis is to describe the pattern of co-diagnosed mental disorders among opioid-related harm hospitalizations in Canada (excluding Quebec). Data are presented for the time period from April 1, 2018 to March 31, 2019 (the most recent data available at the time of analysis), and examine how patterns differ by sex and age.
Definitions included in this report
Opioid-related poisonings: opioid poisoning harms (overdose) resulting from incorrect use of opioids in an intentional, accidental or unknown manner. Opioid poisonings may involve non-pharmaceutical opioids, pharmaceutical opioids, or both. Pharmaceutical opioids refer to opioids that were manufactured by a pharmaceutical company and approved for medical purposes in humans. Pharmaceutical opioids can be obtained by a personal prescription or by other means.
Adverse drug reactions from prescribed opioids: occurs when an opioid is taken as prescribed and results in harm, for example, delirium, confusion, or respiratory depression.
Opioid use disorders: includes mental and behavioural disorders that are related to the use of opioids, for example the harmful use of opioids or dependence on opioids. This may include a strong desire or difficulty in controlling use, persistent use despite harmful consequences, or physical withdrawal states. Opioid use disorders are a category within mental disorders, as described below.
Mental disorders: includes mental and behavioural disorders as captured by the International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA). Mental disorders examined in this report include:
- substance-related and addictive disorders
- schizophrenia and psychotic disorders
- mood disorders
- anxiety disorders, and
- selected disorders of personality and behaviour.
Opioid use disorders, listed under opioid-related harms above, are a category of mental disorders. When reporting mental disorder co-diagnoses for opioid use disorder hospitalizations, mental disorders due to the use of opioids are excluded.
In a hospital setting, recording diagnoses of mental disorders is mandatory if the mental disorder(s):
- significantly affects the treatment received
- requires treatment beyond maintenance of the pre-existing condition, or
- increases the length of stay in hospital by at least 24 hours.
Therefore, the data presented in this report does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms, but rather mental disorders that were deemed relevant to the patient’s hospital stay. More detailed information can be found in Appendix B.
Key findings
Opioid-related hospitalizations with a co-diagnosis of a mental disorder
Between April 2018 and March 2019, for Canada (excluding Quebec), there were a total of 20,484 opioid-related hospitalizations:
- 5,068 for opioid-related poisonings
- 6,185 for adverse drug reactions from prescribed opioids, and
- 10,082 for opioid use disordersFootnote 1.
Overall, 43% of opioid-related hospitalizations also had a co-diagnosis of another mental disorder. However, this percentage varied based on the category of opioid-related hospitalization.
Co-diagnoses of other mental disorders were the most common among those hospitalized for opioid use disorders compared to other opioid-related hospitalizations (Figure 1). More than half of hospitalizations (56%) for opioid use disorders included a co-diagnosis of another mental disorder during the hospital stay. Co-diagnosed mental disorders were also common among opioid-related poisoning hospitalizations (43%). Hospitalizations for adverse drug reactions from prescribed opioids had the lowest percent of co-diagnoses for mental disorders (15%).
In terms of the specific types of mental disorders, other substance-related and addictive disorders were the most common co-diagnosis for all categories of opioid-related hospitalizations. 46% of hospitalizations for opioid use disorders indicated the patient had a diagnosis for another substance-related or addictive disorder, including disorders due to the use of alcohol, cannabinoids, cocaine, other stimulants, sedatives or hallucinogens. Substance-related and addictive disorders were also common among opioid-related poisoning hospitalizations, with 28% of hospitalizations also including a diagnosis for these mental disorders. Substance-related and addictive disorder co-diagnoses were lowest among hospitalizations for adverse drug reactions from prescribed opioids, with less than 1 out of 10 hospitalizations (9%) having this type of mental disorder recorded.
The percentage of hospitalizations with co-diagnoses of other mental disorders varied by opioid-related hospitalization (Figure 1). Among hospitalizations for opioid-related poisonings, mood disorders were the second most prevalent co-diagnosis at 12% of hospitalizations. This may reflect the association between mood disorders and intentional self-harm by opioid-related poisoning. Additional analyses will be required to examine mental disorder co-diagnoses among intentional and unintentional opioid-related poisoning hospitalizations.
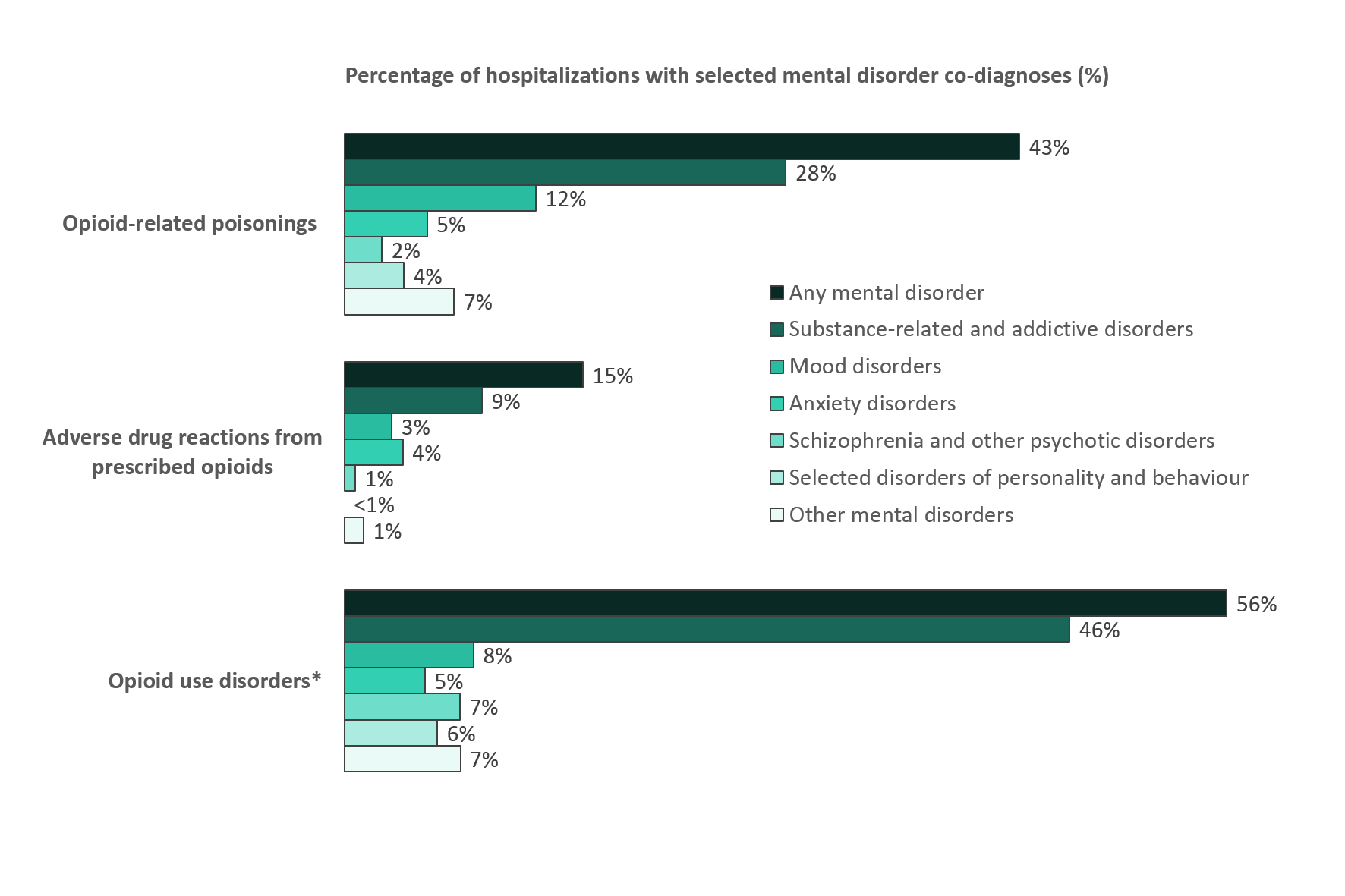
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 1)
| Opioid-related Hospitalization | Total hospitalizations for opioid harm category, N | Any mental disorder co-diagnosis, N (%) |
Substance-related and addictive disorder co-diagnosis, N (%) |
Mood disorder co-diagnosis, N (%) |
Anxiety disorder co-diagnosis, N (%) |
Schizophrenia and other psychotic disorder co-diagnosis, N (%) |
Selected disorders of personality and behaviour co-diagnosis, N (%) | Other mental disorder co-diagnosis, N (%) |
|---|---|---|---|---|---|---|---|---|
| Opioid-related poisonings | 5068 | 2159 (43%) | 1412 (28%) | 612 (12%) | 264 (5%) | 120 (2%) | 190 (4%) | 341 (7%) |
| Adverse drug reactions from prescribed opioids | 6185 | 936 (15%) | 537 (9%) | 185 (3%) | 228 (4%) | 42 (1%) | 13 (less than 1%) | 74 (1%) |
| Opioid use disorders | 10082 | 5615 (56%)Footnote * | 4615 (46%)Footnote * | 822 (8%) | 512 (5%) | 734 (7%) | 591 (6%) | 737 (7%) |
|
||||||||
Opioid-related hospitalizations with a co-diagnosis of a mental disorder by sex
Between April 2018 and March 2019, the percentage of opioid-related hospitalizations with a mental disorder co-diagnosis were relatively similar for males and females. However, patterns by sex differed when examining the mental disorder categories. Overall, the percentage of hospitalizations with a co-diagnosis of substance-related and addictive disorders was higher among males than females. Mood and anxiety disorder co-diagnoses were more common among females than males for all opioid-related hospitalizations, most notably for opioid-related poisoning hospitalizations (Figures 2-4).
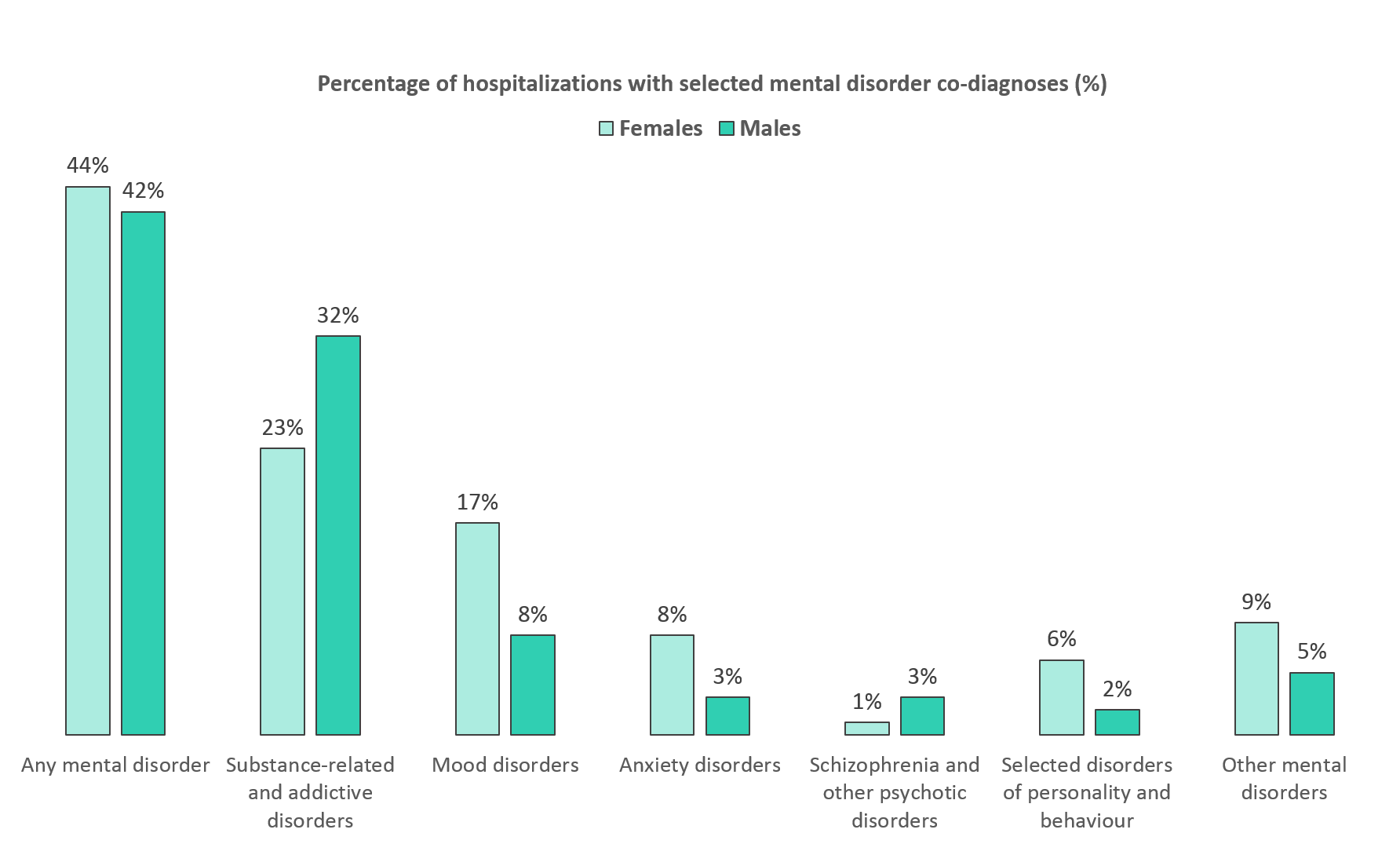
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 2)
| Opioid-related poisoning hospitalizations | Any mental disorder co-diagnosis, N (%) |
Substance-related and addictive disorder co-diagnosis, N (%) |
Mood disorder co-diagnosis, N (%) |
Anxiety disorder co-diagnosis, N (%) |
Schizophrenia and other psychotic disorder co-diagnosis, N (%) |
Selected disorders of personality and behaviour co-diagnosis, N (%) | Other mental disorder co-diagnosis, N (%) |
|---|---|---|---|---|---|---|---|
| Female | 975 (44%) | 514 (23%) | 381 (17%) | 169 (8%) | 32 (1%) | 129 (6%) | 203 (9%) |
| Male | 1179 (42%) | 897 (32%) | 231 (8%) | 95 (3%) | 88 (3%) | 61 (2%) | 138 (5%) |
Co-diagnoses of mental disorders in this report represent diagnoses which were significant to the patient’s stay in hospital. It does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms. Multiple co-diagnoses are possible for any given hospital stay. |
|||||||
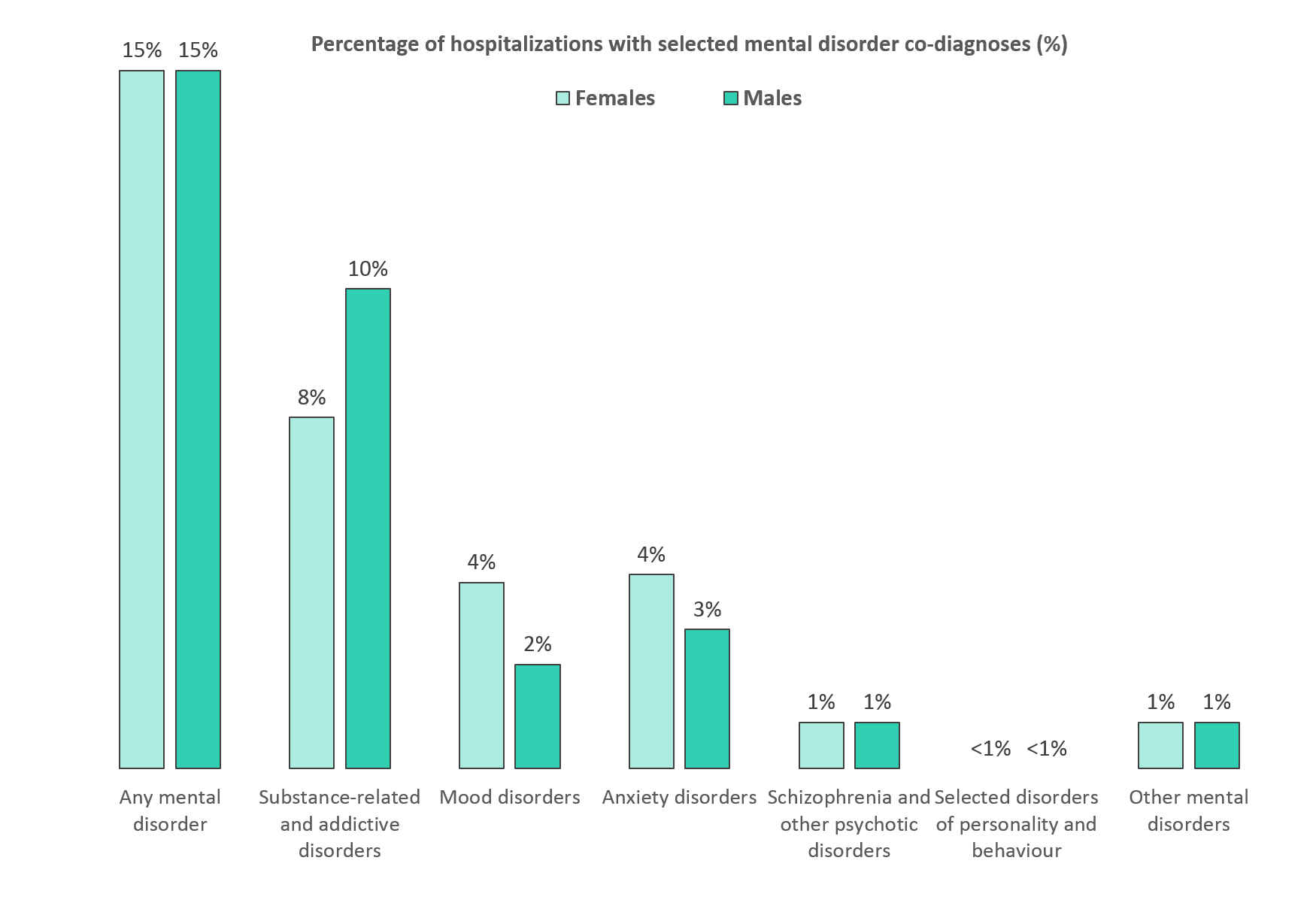
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 3)
| Adverse drug reactions from prescribed opioids hospitalizations | Any mental disorder co-diagnosis, N (%) |
Substance-related and addictive disorder co-diagnosis, N (%) |
Mood disorder co-diagnosis, N (%) |
Anxiety disorder co-diagnosis, N (%) |
Schizophrenia and other psychotic disorder co-diagnosis, N (%) |
Selected disorders of personality and behaviour co-diagnosis, N (%) | Other mental disorder co-diagnosis, N (%) |
|---|---|---|---|---|---|---|---|
| Female | 542 (15%) | 275 (8%) | 128 (4%) | 152 (4%) | 25 (1%) | 7 (less than 1%) | 54 (1%) |
| Male | 389 (15%) | 262 (10%) | 57 (2%) | 76 (3%) | 17 (1%) | 6 (less than 1%) | 20 (1%) |
Co-diagnoses of mental disorders in this report represent diagnoses which were significant to the patient’s stay in hospital. It does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms. Multiple co-diagnoses are possible for any given hospital stay. |
|||||||
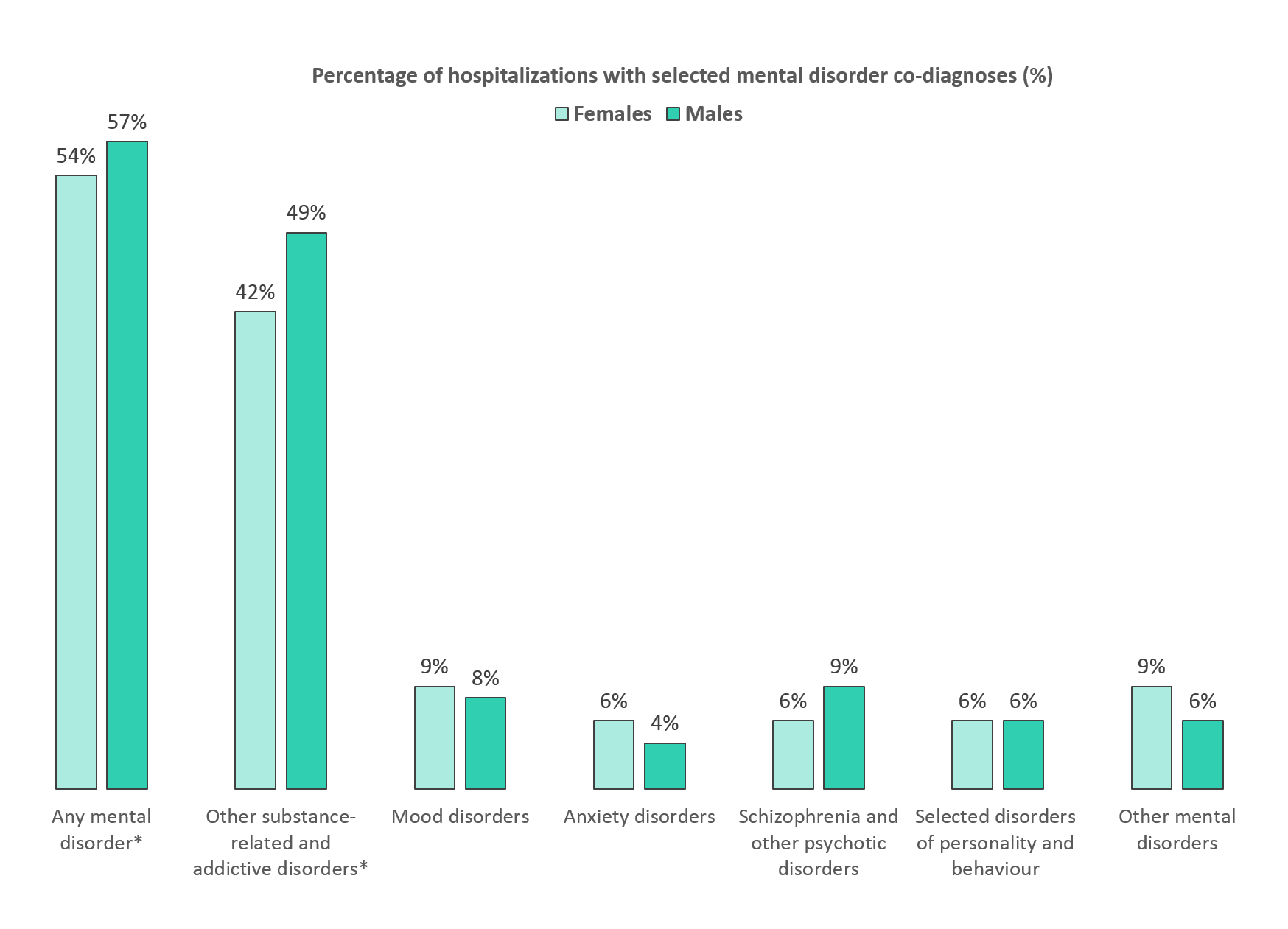
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 4)
| Opioid use disorder hospitalizations | Any mental disorder co-diagnosis, N (%) |
Substance-related and addictive disorder co-diagnosis, N (%) |
Mood disorder co-diagnosis, N (%) |
Anxiety disorder co-diagnosis, N (%) |
Schizophrenia and other psychotic disorder co-diagnosis, N (%) |
Selected disorders of personality and behaviour co-diagnosis, N (%) | Other mental disorder co-diagnosis, N (%) |
|---|---|---|---|---|---|---|---|
| Female | 2476 (54%)Footnote * | 1893 (42%)Footnote * | 407 (9%) | 288 (6%) | 257 (6%) | 282 (6%) | 428 (9%) |
| Male | 3126 (57%)Footnote * | 2716 (49%)Footnote * | 415 (8%) | 224 (4%) | 476 (9%) | 306 (6%) | 307 (6%) |
|
|||||||
Opioid-related hospitalizations with a co-diagnosis of a mental disorder by sex and age
Females aged 0 to 19 years and 30 to 39 years had the highest percentage of co-diagnoses for mental disorders among opioid-related poisoning hospitalizations. For all other age categories, the percentages with co-diagnoses were more similar for males and females (Figure 5). Among hospitalizations for adverse reactions from prescribed opioids, males aged 20 to 29 and 30 to 39 had the highest percentage with a co-diagnosed mental disorder, at 27% for each age group (Figure 6). Among opioid use disorder hospitalizations, younger males had the highest percentage of mental disorders, with 80% of males aged 0 to 19 years having a co-diagnosis (Figure 7).
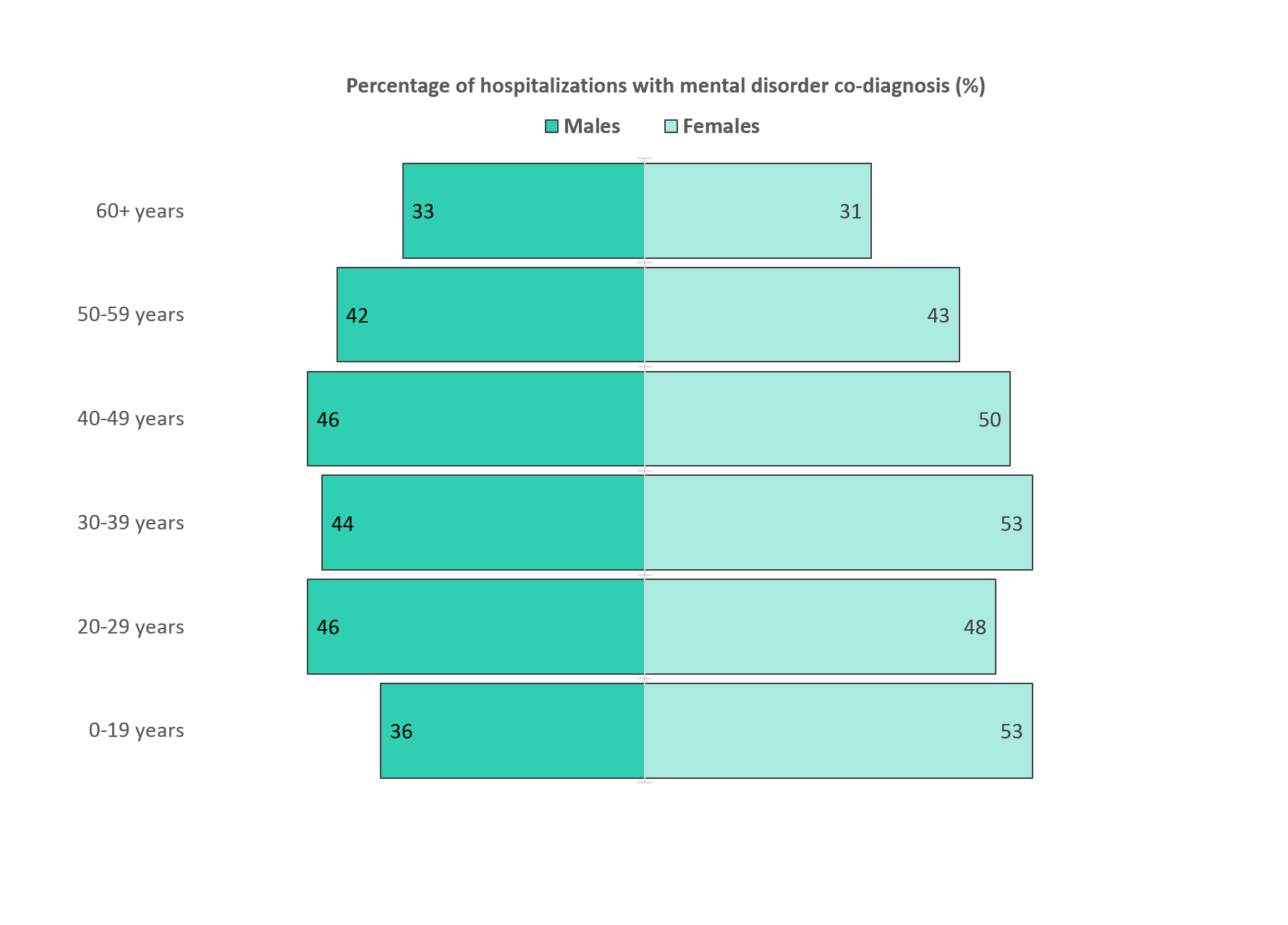
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 5)
| Opioid-related poisoning hospitalizations | 0 to 19 years, N (%) | 20 to 29 years, N (%) |
30 to 39 years, N (%) |
40 to 49 years, N (%) |
50 to 59 years, N (%) |
60 years and over, N (%) |
|---|---|---|---|---|---|---|
| Female | 102 (53%) | 159 (48%) | 167 (53%) | 172 (50%) | 183 (43%) | 192 (31%) |
| Male | 49 (36%) | 260 (46%) | 293 (44%) | 200 (46%) | 191 (42%) | 186 (33%) |
Co-diagnoses of mental disorders in this report represent diagnoses which were significant to the patient’s stay in hospital. It does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms. Multiple co-diagnoses are possible for any given hospital stay. |
||||||
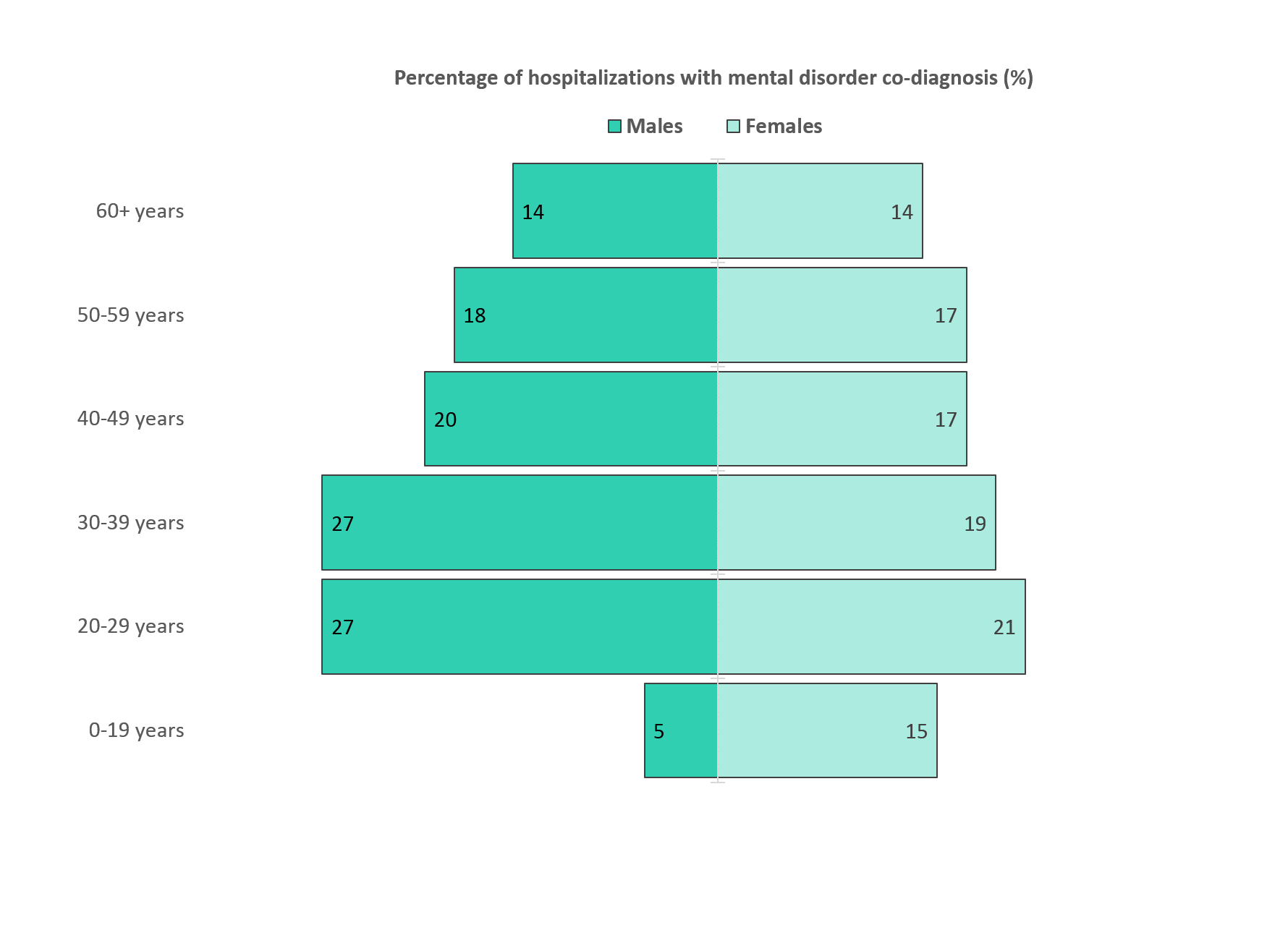
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 6)
| Adverse drug reactions from prescribed opioids hospitalizations | 0 to 19 years, N (%) | 20 to 29 years, N (%) |
30 to 39 years, N (%) |
40 to 49 years, N (%) |
50 to 59 years, N (%) |
60 years and over, N (%) |
|---|---|---|---|---|---|---|
| Female | 16 (15%) | 19 (21%) | 31 (19%) | 37 (17%) | 72 (17%) | 367 (14%) |
| Male | 5 (5%) | 15 (27%) | 17 (27%) | 25 (20%) | 58 (18%) | 269 (14%) |
Co-diagnoses of mental disorders in this report represent diagnoses which were significant to the patient’s stay in hospital. It does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms. Multiple co-diagnoses are possible for any given hospital stay. |
||||||
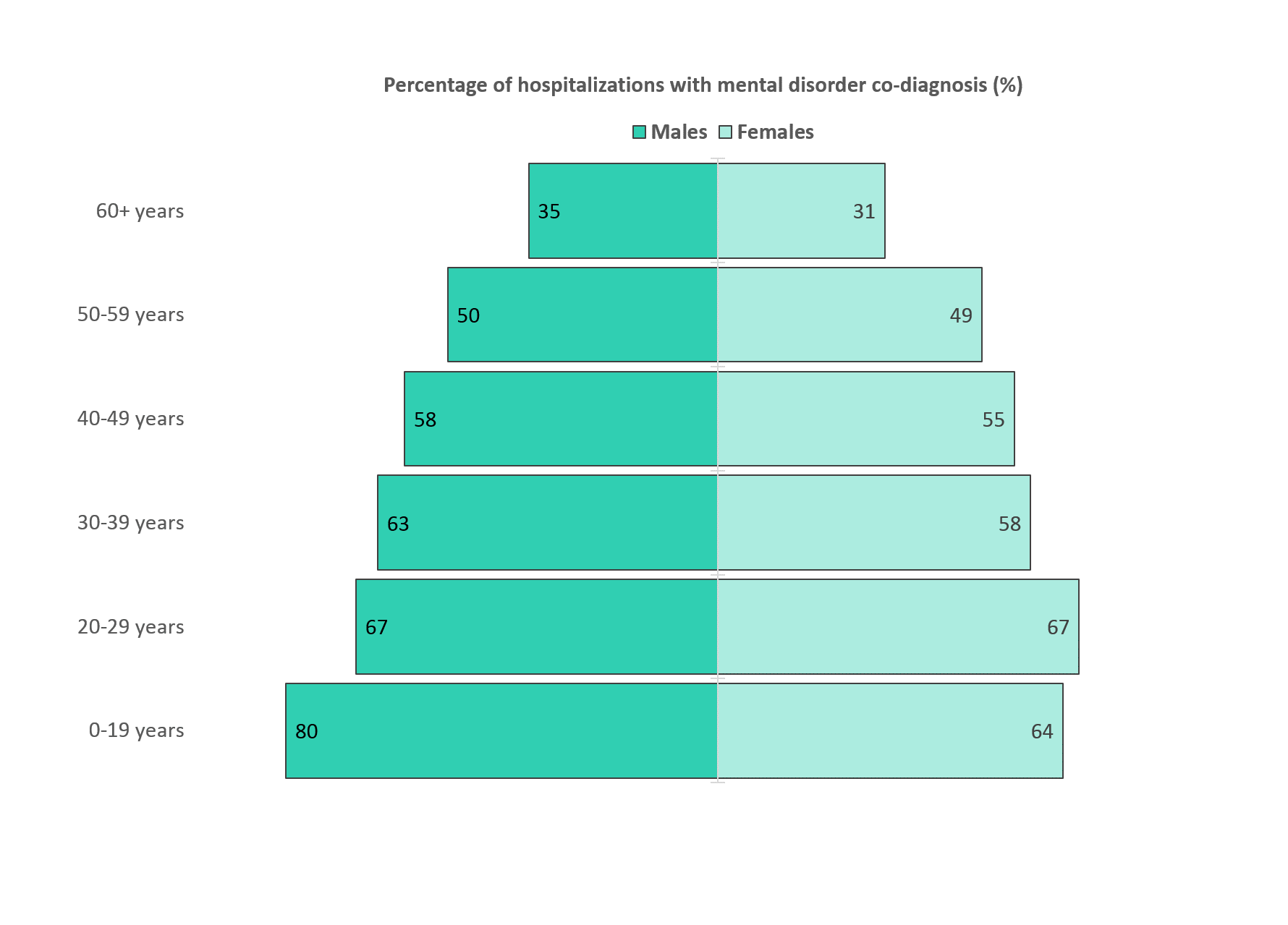
Source: Discharge Abstract Database (2018/19 fiscal year), Canadian Institute for Health Information
Text equivalent (Figure 7)
| Opioid use disorder hospitalizationsFootnote * | 0 to 19 years, N (%) | 20 to 29 years, N (%) |
30 to 39 years, N (%) |
40 to 49 years, N (%) |
50 to 59 years, N (%) |
60 years and over, N (%) |
|---|---|---|---|---|---|---|
| Female | 106 (64%) | 731 (67%) | 707 (58%) | 428 (55%) | 278 (49%) | 226 (31%) |
| Male | 82 (80%) | 748 (67%) | 892 (63%) | 623 (58%) | 479 (50%) | 302 (35%) |
|
||||||
In summary
People are experiencing a variety of harms from opioid use across Canada, including but not limited to:
- opioid-related poisonings
- opioid use disorders
- adverse reactions from prescribed opioids.
Understanding the relationship between these opioid-related harms and mental disorders can help inform comprehensive clinical and public health actions to address the crisis. These data demonstrate that co-diagnoses of mental disorders are common among people hospitalized for opioid-related harms, most notably for opioid-related poisonings and opioid use disorders. For people hospitalized for these opioid-related harms, other substance-related and addictive disorders (including disorders due to the use of opioidsFootnote 2, alcohol, cannabinoids, cocaine, other stimulants, sedatives and hallucinogens) were the most common co-diagnosed mental disorders. These findings highlight the importance for interventions to incorporate a poly-substance use lens that accounts for varying harms by substance type and context of use.
The observed sex and age differences in the pattern of opioid-related harm hospitalizations with mental disorder co-diagnoses is also informative. Overall, a higher percentage of opioid-related hospitalizations among males also had a co-diagnosed substance-related or addictive disorder. Hospitalizations among females had higher percentages of mood and anxiety disorder co-diagnoses. These findings highlight the importance for research and interventions to consider how harms and co-diagnosis may vary within different populations.
It is important to note that this report does not reflect the overall prevalence of co-occurring mental disorders among people hospitalized from opioid-related harms in Canada, but rather co-diagnoses of mental disorders which were considered significant to the patient’s hospital stay. Therefore, the mental disorder data included in this report can be reflective of minimal estimates, and future research is warranted to determine overall co-occurring prevalence. It is also important to note that this report does not explore the causal relationship between mental disorders and opioid-related harms. Further research is needed to better understand the reciprocal relationship between substance use and mental disorders. The Government of Canada will continue to improve data and analysis to inform strategies and interventions to reduce opioid-related harms across the country.
Acknowledgements
We would like to acknowledge the Canadian Institute for Health Information (CIHI) for collecting and providing the data used for reporting opioid-related hospitalizations.
Disclaimer
Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the authors, and not necessarily those of the Canadian Institute for Health Information (CIHI).
Technical notes
Methodology
Data from CIHI's Discharge Abstract Database (DAD) for the fiscal year April 1, 2018 to March 31, 2019 was analyzed for this report. This analysis was limited to acute inpatient hospitalizations, which are nationally representative across Canada, with the exception of Quebec. This analysis presents the number of acute inpatient hospitalizations for opioid-related harms, it does not reflect the number of patients who were hospitalized in the analysis year. It is possible some patients may have been hospitalized more than once for an opioid-related harm.
The International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) is used in the DAD to capture diagnoses from the patient's hospitalization. It is the national standard for reporting morbidity statistics. More information on the DAD and ICD-10-CA coding can be found on CIHI's website.
Identifying opioid-related hospitalizations
A complete listing of all ICD-10-CA diagnosis codes used to identify opioid-related harms presented in this report can be found in Appendix A. For opioid-related poisoning and opioid use disorders, analyses were restricted to the following significant diagnosis types:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnosis ("W", "X", and "Y")
These significant diagnosis types capture hospitalizations in which the opioid-related harm was considered influential to the time spent in hospital and treatment received by the patient while there. Adverse drug reactions from prescribed opioids are considered external cause of injury codes. In line with CIHI coding standards, a diagnosis type of "9" was used for identifying these records. A diagnosis prefix of "Q", indicating unconfirmed diagnoses or query diagnoses recorded by the physician, were excluded from these analyses. Records indicating the patient was admitted to the facility as a cadaveric donor and stillbirths were also excluded.
Identifying co-diagnoses of mental disorders
The methodology for identifying mental disorders was adapted from CIHI’s indicator for Repeat Hospital Stays for Mental Illness in their Your Health System tool. The following ICD-10-CA codes were used to identify mental disorders:
- substance-related and addictive disorders: F10-F19, F55, F63.0
- schizophrenia and other psychotic disorders: F20, F21, F22, F23, F24, F25, F28, F29
- mood disorders: F30, F31, F32, F33, F34, F38, F39, F53.0, F53.1
- anxiety disorders: F40, F41, F93.0, F93.1, F93.2, F94.0
- selected disorders of personality and behaviour: F60, F61, F62, F68 (excluding F68.1), F69
- other mental disorders: F42, F43, F44, F45, F48.0, F48.1, F48.8, F48.9, F50, F51, F52, F53.8, F53.9, F54, F59, F63 (excluding F63.0), F68.1, F90, F91, F92, F93.3, F93.8, F93.9, F94.1, F94.2, F94.8, F94.9, F95, F98.0, F98.1, F98.2, F98.3, F98.4, F98.5, F98.8, F98.9, F99, O99.3
- specific to this report, at least one occurrence of any of the above ICD-10-CA codes were grouped into a broad category for “Any mental disorder”
Specific examples of diagnoses that are included in each mental disorder category can be found in Appendix B. When examining recorded co-diagnoses of mental disorders during the patient’s opioid-related hospital stay, all diagnosis types and prefixes were included as the scope of this analysis was concerned with capturing secondary and suspected diagnoses for mental disorders. When reporting mental disorder co-diagnoses for opioid use disorder hospitalizations, mental disorders due to the use of opioids were excluded.
Limitations
General notes
- Co-diagnoses of mental disorders in this report represent diagnoses which were significant to the patient’s stay in hospital. It does not reflect the overall prevalence of mental disorders among those hospitalized for opioid-related harms.
- The terminology used in this report aligns with the terms used in the International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA).
- Hospitalizations for opioid use disorders are underrepresented in this report as the data source used (Discharge Abstract Database) does not include full coverage for hospitalizations due to mental and substance use disorders. Additional opioid use disorder hospitalizations may be captured in the Ontario Mental Health Reporting System (OMHRS) and therefore these results should be interpreted with caution.
- The DAD captures patients discharged from hospital. Patients who were still hospitalized during the analysis year are not captured in this report.
- Data released by provinces and territories may differ from the data provided in this report due to the availability of updated data, differences in the type of data reported, the use of alternate age groupings, differences in time periods presented and/or population estimates used for calculations, etc.
Data on sex
- In the DAD, data on sex is typically recorded based on biological determination or legal documentation. Although 'other' sex group is available, the counts were too low to include in this report. Therefore, 'other' sex group was retained in overall analyses, but were excluded from all analyses by sex to avoid disclosure.
Data suppression
Values representing less than five hospitalizations are suppressed according to CIHI's privacy guidelines.
Appendix A
| Type of Opioid-Related Harm | ICD-10-CA Code | Description |
|---|---|---|
| Opioid-related poisonings | T40.0 | Poisoning by opium |
| T40.1 | Poisoning by heroin | |
| T40.2 | Poisoning by other opioids | |
| T40.20 | Poisoning by codeine and derivatives | |
| T40.21 | Poisoning by morphine | |
| T40.22 | Poisoning by hydromorphone | |
| T40.23 | Poisoning by oxycodone | |
| T40.28 | Poisoning by other opioids not elsewhere classified | |
| T40.3 | Poisoning by methadone | |
| T40.4 | Poisoning by other synthetic narcotics | |
| T40.40 | Poisoning by fentanyl and derivatives | |
| T40.41 | Poisoning by tramadol | |
| T40.48 | Poisoning by other synthetic narcotics not elsewhere classified | |
| T40.6 | Poisoning by other and unspecified narcotics | |
| Adverse drug reactions from prescribed opioids | Y45.0 | Opioids and related analgesics |
| Y45.01 | Codeine and derivatives | |
| Y45.02 | Morphine | |
| Y45.03 | Hydromorphone | |
| Y45.04 | Oxycodone | |
| Y45.05 | Fentanyl and derivatives | |
| Y45.06 | Tramadol | |
| Y45.09 | Other and unspecified opioids and related analgesics | |
| Opioid use disorders | F11.0 | Mental and behavioural disorders due to use of opioids, acute intoxication |
| F11.1 | Mental and behavioural disorders due to use of opioids, harmful use | |
| F11.2 | Mental and behavioural disorders due to use of opioids, dependence syndrome | |
| F11.3 | Mental and behavioural disorders due to use of opioids, withdrawal state | |
| F11.4 | Mental and behavioural disorders due to use of opioids, withdrawal state with delirium | |
| F11.5 | Mental and behavioural disorders due to use of opioids, psychotic disorder | |
| F11.6 | Mental and behavioural disorders due to use of opioids, amnesic syndrome | |
| F11.7 | Mental and behavioural disorders due to use of opioids, residual and late- onset psychotic disorder | |
| F11.8 | Mental and behavioural disorders due to use of opioids, other mental and behavioural disorders | |
| F11.9 | Mental and behavioural disorders due to use of opioids, unspecified mental and behavioural disorder |
Appendix B
| Mental disorder category | Examples of specific mental disorder diagnoses (not an exhaustive list) |
|---|---|
| Substance-related and addictive disorders | Mental and behavioural disorders due to use of alcohol, cannabinoids, cocaine, other stimulants, sedatives or hallucinogens. Pathological gambling.Footnote * |
| Schizophrenia and other psychotic disorders | Schizophrenia, schizotypal disorders, psychotic disorders, induced delusional disorders, and schizoaffective disorders |
| Mood disorders | Manic episodes, bipolar affective disorders, and depressive disorders |
| Anxiety disorders | Phobic anxiety disorders, panic disorders, generalized anxiety disorders, and separation anxiety disorders |
| Selected disorders of personality and behaviour | Paranoid personality disorders, schizoid personality disorders, dissocial personality disorders, and emotionally unstable personality disorders |
| Other mental disorders | Somatoform disorders including hypochondria disorders, eating disorders, nonorganic sleep disorders, conduct disorders, and post-traumatic stress disorders |
|
|
More detailed information regarding the diagnosis codes included in this report can be found in CIHI’s version 2018 ICD-10-CA manual. More general information on ICD-10 can be found in the World Health Organizations ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines. The World Health Organization also provides a list of key terms and definitions in mental health as a reference.
References
- Footnote 1
-
Rose C, Shahanaghi A, Romero-Gonzalez M, Yarzebski J, Andre M, DiGirolamo GJ, Brown AP, Gonzalez G. Mortality associated with opioid overdose: a review of clinical characteristics and health services received in the year prior to death. Psychiatric services. 2019 Feb 1;70(2):90-6. DOI: 10.1176/appi.ps.201800122
- Footnote 2
-
Peterson C, Liu Y, Xu L, Nataraj N, Zhang K, Mikosz CA. US national 90-day readmissions after opioid overdose discharge. American journal of preventive medicine. 2019 Jun 1;56(6):875-81. DOI: 10.1016/j.amepre.2018.12.003
- Footnote 3
-
Barocas JA, Wang J, Marshall BD, LaRochelle MR, Bettano A, Bernson D, Beckwith CG, Linas BP, Walley AY. Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug and alcohol dependence. 2019 Jul 1;200:59-63. DOI: 10.1016/j.drugalcdep.2019.03.014
- Footnote 4
-
Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. Jama. 2011 Apr 6;305(13):1315-21. DOI: 10.1001/jama.2011.370
- Footnote 5
-
Dilokthornsakul P, Moore G, Campbell JD, Lodge R, Traugott C, Zerzan J, Allen R, Page II RL. Risk factors of prescription opioid overdose among Colorado Medicaid beneficiaries. The Journal of Pain. 2016 Apr 1;17(4):436-43. DOI: 10.1016/j.jpain.2015.12.006
- Footnote 6
-
Feng J, Iser JP, Yang W. Medical encounters for opioid-related intoxications in Southern Nevada: sociodemographic and clinical correlates. BMC health services research. 2016 Dec;16(1):1-0. DOI: 10.1186/s12913-016-1692-z
- Footnote 7
-
Krawczyk N, Eisenberg M, Schneider KE, Richards TM, Lyons BC, Jackson K, Ferris L, Weiner JP, Saloner B. Predictors of overdose death among high-risk emergency department patients with substance-related encounters: a data linkage cohort study. Annals of emergency medicine. 2020 Jan 1;75(1):1-2. DOI: 10.1016/j.annemergmed.2019.07.014
- Footnote 8
-
Public Health Agency of Canada. Statement from the Co-Chairs of the Special Advisory Committee on the Epidemic of Opioid Overdoses on Updated Data Related to the Opioid Crisis [Internet]. 2019 [cited August 20, 2020]. Available from: https://www.canada.ca/en/public-health/news/2019/06/statement-from-the-co-chairs-of-the-special-advisory-committee-on-the-epidemic-of-opioid-overdoses-on-updated-data-related-to-the-opioid-crisis.html
Footnotes
- Footnote 1
-
It is possible for a person to be hospitalized for an opioid-related poisoning and an opioid use disorder at the same time. This means that total hospitalizations for opioid-related harms may be less than the sum of hospitalizations for the individual harms.
- Footnote 2
-
When reporting mental disorder co-diagnoses for opioid use disorder hospitalizations, mental disorders due to the use of opioids are excluded.