Who’s at risk and what can be done about it? A review of the literature on the social isolation of different groups of seniors
On this page
- Executive summary
- Introduction
- Methodology
- Prevalence and impact
- General risk factors
- Risk factors among different groups of seniors
- Research gaps
- Policy considerations
- Conclusion
- Reference list
Request other formats online or call 1 800 O-Canada (1-800-622-6232). If you use a teletypewriter (TTY), call 1-800-926-9105. Large print, braille, audio cassette, audio CD, e-text diskette, e-text CD and DAISY are available on demand.
Executive summary
Canada’s population is aging rapidly as a growing proportion of baby boomers transition into their senior years. In this context, the issue of social isolation – which has profound impacts on the health and wellbeing of seniors from all walks of life – has come to occupy an increasingly important place in discussions on seniors and aging in Canada. It is estimated that up to 16% of seniors experience social isolation (Statistics Canada, 2010). Who’s at Risk and What Can Be Done About It builds on earlier work undertaken by the National Seniors Council (NSC) on the issue of the social isolation of seniors. Specifically, the current review looks at what the literature says about how different groups of vulnerable seniors are affected by social isolation and identifies promising interventions to tackle social isolation and reconnect seniors to their communities.
Nine groups of seniors are examined: Aboriginal seniors,Footnote 1 seniors who are caregivers, immigrant seniors, LGBT seniors, seniors living alone, seniors living in remote or rural areas, low-income seniors and those living in poverty, seniors with mental health issues (including Alzheimer's and other dementias), and seniors with health challenges or disabilities. The review begins with an examination of the literature on each group before exploring the literature on promising interventions, most of which focuses on seniors as a whole. It concludes with four main findings.
First, the different groups of seniors examined are indeed at risk of social isolation. At the same time, the literature on each group is uneven, both in terms of the quantity and quality of studies. Greater efforts are required to further develop the research on the barriers that specific groups of seniors encounter, and to tailor initiatives that address social isolation to their needs. Second, a two-pronged approach to addressing social isolation seems warranted, one that combines coordinated policy interventions that can facilitate social inclusion across the general population of seniors with targeted interventions for specific at-risk groups. The concept of age-friendly communities has the potential to underpin a range of interventions that fall within the scope of both approaches. Third, research on social isolation would benefit from greater segmentation, increased reliance on mixed methods (qualitative and quantitative), conceptual clarity and consistency, and exploration of social isolation across the life course. Finally, there is a need for more high quality program evaluation studies of different programs and approaches, and practitioners should be encouraged to build an outcome measurement component into all of their programs (though funding limitations can often make this difficult). In general, however, there is sufficient evidence to identify several common characteristics of successful interventions as well as different types of interventions.
The findings of the review are meant to be of interest to stakeholders working with seniors who are looking to increase their understanding of this complex, multifaceted issue. They are meant to inform the actions of the federal government, as well as other stakeholders such as researchers and frontline service providers. As such they complement suggestions for federal action on social isolation that were made in the National Seniors Council's Report on the Social Isolation of Seniors.Footnote 2 Given its complex societal nature, social isolation requires a multi-stakeholder approach; this review contributes to knowledge-mobilization efforts to support such an approach.
Introduction
Canada's population is aging rapidly as a growing proportion of baby boomers transition into their senior years. In 2015, for the first time, the number of persons aged 65 years and older exceeded the number of children aged 0 to 14 years. At the same time, the growth rate of the population aged 65 years and older was 3.5% – approximately four times the growth rate of the total population.Footnote 3 This process brings with it new challenges to ensure that the needs of seniors are being adequately addressed by policymakers, service providers, communities and other stakeholders. In this context, the issue of social isolation – which has profound impacts on the health and wellbeing of seniors from all walks of life – has come to occupy an increasingly important place in discussions on seniors and aging in Canada. While most seniors are engaged in mutually-supporting social networks and are involved in their communities, there are significant numbers who experience episodic or long term social isolation. It is estimated that up to 16% of seniors experience social isolation (Statistics Canada, 2010).Footnote 4 The causes of social isolation are complex, and include individual-level factors such as the loss of a loved one to broader societal factors such as the norms and values we attach to the wellbeing of others and our shared sense of community. Footnote 5
In November 2013, the National Seniors Council (NSC) launched a series of consultations with stakeholders from multiple sectors to assess how social isolation affects seniors and to explore ways to prevent and reduce it. In total, 305 stakeholders participated in the consultation process. Among other things, the consultations revealed that certain groups of seniors seemed to be at greater risk of social isolation than the general population of seniors. Furthermore, the NSC’s Report on the Social Isolation of Seniors indicated that "stakeholders identified the need to undertake further research to validate the impact, quality and value of innovative and promising practices as well as increase the knowledge base with respect to social isolation and the health of seniors" (National Seniors Council, 2014a).
This literature review extends the NSC’s earlier work on social isolation by looking at how different groups of vulnerable seniors are affected by social isolation, and by identifying promising interventions to tackle social isolation and reconnect seniors to their communities. Far from being a homogeneous group, Canadian seniors have multiple identities and experience different life circumstances that make broad generalizations problematic. This must be taken into consideration in analyzing social isolation and in maximizing the impact of different policy interventions. The review therefore surveys what is known about the occurrence of social isolation in different groups of seniors, the interaction and cumulative impact of different risk factors, and the potential for different programmatic interventions. While the Council has endeavoured to identify the most relevant (English and French-language) studies on these topics, the review is by no means exhaustive given the growing literature in this area and the multiple sub-themes that could be further explored. That said, gaps in the state of knowledge on social isolation among specific groups of seniors have been identified for future research.
The findings of the review are meant to be of interest to stakeholders working with seniors who are looking to increase their understanding of this complex, multifaceted issue. They are meant to inform the actions of the federal government, as well as other stakeholders such as researchers and frontline service providers. Given its complex societal nature, social isolation requires a multi-stakeholder approach; this review contributes to knowledge-mobilization efforts to support such an approach.
Overall, the review finds that the different groups of seniors that are examined are at risk of social isolation. At the same time, the state of knowledge on each group is uneven, both in terms of the quantity and quality of studies. Moreover, given the diversity of methods used in studies on social isolation and different groups of seniors, it is not possible to rank or order these different groups according to risk level. Social isolation is a complex phenomenon that seems to affect different groups of seniors distinctively even as there are general risk factors that cut across groups without discrimination.
This suggests the need for a two-pronged approach to addressing social isolation. Since many risk factors are general in nature, coordinated policy interventions that can facilitate social inclusion across the population of seniors, such as improved housing, access to transportation, and the reduction of ageism and discrimination are required; for those factors that are more specific to a particular group, targeted interventions, such as providing support to senior caregivers to prevent isolation, are also recommended. This means that social isolation should become a key consideration for a range of policy areas linked to seniors in addition to being a policy focus in its own right. The review ends with some specific examples of general and targeted interventions based on findings from the literature.
Methodology
Definitions
The concept of social isolation is multi-faceted and overlaps with other related concepts such as loneliness, social vulnerability, social inclusion and exclusion, social connectedness, and social capital. Social isolation is commonly defined as a low quantity and quality of contact with others, and includes "number of contacts, feeling of belonging, fulfilling relationships, engagement with others, and quality of network members" (Nicholson, 2009). Socially isolated persons lack social contacts, social roles and mutually rewarding relationships (Keefe et al., 2006; North Sky Consulting Group Ltd, 2013). The severity of isolation can vary from person to person depending upon whether it is voluntary or involuntary, permanent or chronic, episodic or temporary.Footnote 6 While researchers define social isolation differently, most agree that it has a more objective dimension to it than loneliness, which depends upon an individual's subjective reactions to their environment and relationships rather than the more general condition of having few social contacts. Still, in the literature on social isolation, the terms are often used interchangeably. While this review focuses on social isolation, findings on loneliness and other related concepts are sometimes referred to where they help provide a more complete picture of the situation of specific groups of seniors.
Research scope and methods
To guide the literature review, two key research questions were identified:
- What is known about the different groups of seniors who may be vulnerable to social isolation? (Note that the groups themselves were already identified through NSC consultations).
- What does the literature say about the riskFootnote 7correlates of social isolation – and how these factors interact – among these groups of seniors?
A thorough review of the scholarly and program/policy literature was undertaken, with approximately 150 articles, reports, books and book-chapters identified and reviewed. An exhaustive list of search terms was developed and used to identify the literature. While a majority of articles and reports were in English and came from Canada or the United States, a significant sample of French-language articles was also included in the report (with a focus on the Canadian literature and particularly influential reports from Europe). One hundred and twenty pieces of literature were reviewed in English and 30 in French.
Measuring the overall prevalence and impact of social isolation brings with it a series of methodological challenges. First, a major stumbling block for both researchers and practitioners is how to find the isolated, who – by definition – are not connected and are difficult to find (Newall, 2015). Frontline workers also report that linguistic and cultural barriers – along with stigma surrounding isolation – can make it even more difficult to reach certain groups of seniors (North Sky Consulting Group Ltd, 2013; see also section below on Immigrant Seniors). The overall incidence of isolation may therefore be under-reported. A distinct but related problem is obtaining accurate data on the size of population groups affected by social isolation. In this review, for instance, data on certain population groups, such as LGBT seniors, seniors who are caregivers, seniors with mental health issues and seniors with health challenges – are primarily based upon self-reporting in surveys. Self-reporting can lead to under-estimations, particularly for LGBT seniors, who are reluctant to be open about their sexual orientation or gender identity (Tang, 2015).
Second, social isolation is a complex phenomenon associated with multiple factors. While some researchers deploy multivariate analyses to isolate causal factors, this is not always possible (or desirable, depending upon the purpose of the research).Footnote 8 Thus, some studies may identify factors associated with social isolation without being able to determine whether they are causal factors per se, or the extent to which they are generalizable, or how exactly they interact. Third, even when large-scale studies are conducted, the relationship between social isolation and other factors can be reciprocal or bidirectional in nature, further compounding the challenge of determining causality. For example, the literature on social isolation clearly demonstrates that social isolation can have an impact on various measures of health, but it is equally well established that health challenges can further exacerbate social isolation. Fourth, there may be cumulative or synergetic effects across risk factors that combine to influence social isolation and related experiences within and between vulnerable groups of seniors.
This review takes into consideration these various challenges and seeks to contextualize research findings as much as possible. It takes a general approach to understanding the dynamics of social isolation by looking at the interaction of multiple risk factors that can create a cascading of riskFootnote 9 that render an individual – or a group of seniors – particularly vulnerable. Taken as a whole, the accumulation of risk factors can place seniors at multiple jeopardy of experiencing loneliness and social isolation.
Prevalence and impact
Given the diversity of methodologies used in studying isolation and the challenges in reaching the isolated, estimates on the prevalence of isolation are wide ranging. However, data from the Canadian Community Health Survey, a large-scale study with a range of social isolation indicators, provide an overall sense of the magnitude of the problem (Statistics Canada, 2010). Accordingly:
- 16% of seniors felt isolated from others often or some of the time
- 6% of seniors reported spending little or no time with someone with whom they could complete enjoyable activities
- 5% indicated having someone to listen to them none or little of the time
- More than 8% reported having someone to receive advice about a crisis none or little of the time
- 3.9% of seniors reported having someone who shows love and affection to them none or little of the time
- 6% reported having someone to do something enjoyable with none or little of the time
- 6% reported never or not often participating in activities with family and friends
- 17.3% reported feeling excluded often or some of the time
These findings suggest that a significant portion of seniors experience social isolation in a variety of different ways. Preliminary results from the Canadian Longitudinal Study on Aging (CLSA) support these findings.Footnote 10
The impact of social isolation is no less significant. A substantial body of literature has demonstrated that loneliness and social isolation are recognised as risk factors for poor health and reduced wellbeing – and that social isolation is significantly and independently related to health status and various quality-of-life indicators (Hawton et al., 2011). Conversely, Canadians with more family and friend supports are usually more likely to be in very good physical and mental health (Sinha, 2014), and individuals with strong social relationships are more likely to live longer than individuals with poor social relations (Holt Lunstad et al., 2015).
In one systematic review of the literature, researchers found that nearly all studies found a detrimental effect of isolation or loneliness on health. Health risks associated with isolation and loneliness have been compared to the well-established detrimental effects of smoking and obesity (Courtin and Knapp, 2014). Indeed, one researcher has suggested that social isolation can be equivalent to smoking 15 cigarettes a day in terms of health consequences (Wilson, 2015). The most commonly studied health outcome association with isolation was depression, followed by cardiovascular health and wellbeing/quality of life (Courtin and Knapp, 2014). Loneliness is associated with higher levels of cortisol, changes with immune response, disrupted sleep, increased risk of heart attacks (Bolton, 2012; Courtin and Knapp, 2014), and stroke (Bohic, 2012). Loneliness and isolation are also associated with poorer cognitive function among older adults (Shankar et al., 2013), and can increase the likelihood of falls (Do et al., 2015). In a review of the literature on suicide prevention among seniors, Saïas et al. (2013) found that isolation is a major risk factor associated with suicide among seniors, who already have a higher suicide rate than younger age groups.Footnote 11 In addition to the health impacts, there are also recognized economic and social implications of isolation.Footnote 12
General risk factors
Numerous risk factors have been identified in the literature on social isolation. These risk factors are embedded within several overarching social contexts, including ageism, discrimination, limited access to resources and services, and marginalization. Below, these factors are grouped together in 9 general categories. Here, the purpose is not to provide a new typology of factors, but rather to provide additional context for the reader before examining how they interact within specific groups of seniors.Footnote 13 While none of these factors may be sufficient in themselves to cause isolation, each may increase the chance of isolation and may combine with other factors to produce a cascading of risk. It should also be noted that, in some cases, the opposite of a risk factor is a protective factor. For example, not having access to affordable housing is a risk factor; having access to affordable housing can protect against the risk of social isolation.
Age and gender: being 80 or older; being a woman (since women, on average, live longer).
Ethnicity: being an immigrant (specifically, having a different cultural and linguistic background from the general Canadian population or community in which you live); being from an official language minority community.Footnote 14
Geography: living in a rural or remote area where service provision and distance between individuals and families is less proximate; living in a deprived neighbourhood; living in a community where there has been a loss of community or neighbourhood values; living in a low-density neighbourhood.
Health and disability: having health issues (mental and/or physical) including having multiple chronic health problems (e.g., vision, hearing, incontinence, speech/cognitive impairment); lifelong health problems or late-onset or age-related condition such as incontinence; mental illness (e.g., dementia, depression); stigma associated with mental illness, poor health or a disability; low access to health care; minimal walking time; poor perception of one’s own health.
Knowledge and awareness: challenges relating to technology (costs, literacy, comfort); lack of information on services; lack of awareness or access to community services and programs
Life transitions: loss of a spouse; loss of sense of community; disruption of social networks; lack of family and friend supports; loss or restriction of drivers’ license; entry into care; care-giving and associated factors (intensity of care-giving, low levels of care satisfaction, inability to leave the care recipient alone); divorce; living in a nursing home.
Poverty and lack of access to resources: lack of affordable housing and care options; living with low income; lacking access to transportation (no license or public bus system); financial dependence; living in a deprived neighbourhood (also considered a geography factor).
Sexual and gender identity: being lesbian, gay, bisexual or transgendered (LGBT); history of discrimination; having a weak primary social network; lack of social recognition; discrimination in the health-care system; fear of coming out in older age.
Social relationships: low quality of relationships; having no children or contact with family; living alone (greater likelihood among women, gay men and lesbians); not being married or common-lawed; loss of friends and social network; experiencing ageism.
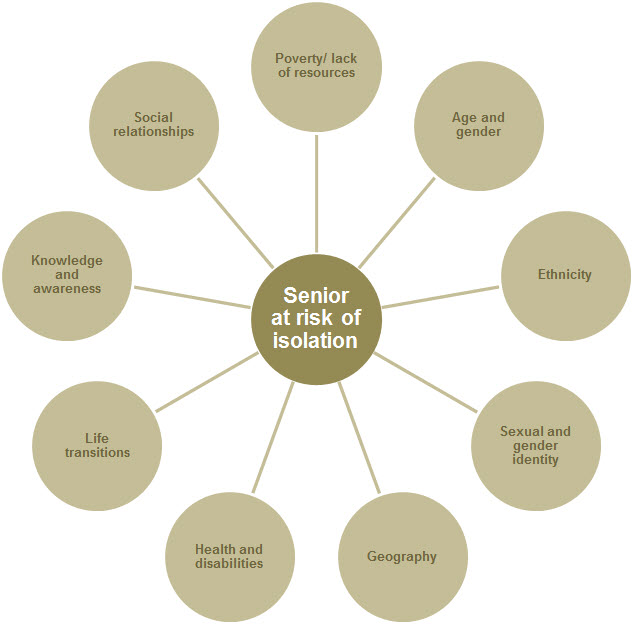
Image description of the Figure 1: General Risk Factors Identified in the Literature for Seniors at Risk of Isolation
- Poverty/lack of resources
- Age and gender
- Ethnicity
- Sexual and gender identity
- Geography
- Health and disabilities
- Life transitions
- Knowledge and awareness
- Social relationships
Risk factors among different groups of seniors
With these general risk factors in mind, the review of the literature turns to the specific factors associated with different groups of seniors. Nine groups are reviewed:
- Aboriginal seniors
- Seniors who are caregivers
- Immigrant seniors
- LGBT seniors
- Seniors living alone
- Seniors living in rural or remote areas
- Low-income seniors and those living in poverty
- Seniors with mental health issues (including Alzheimer's and other dementias), and
- Seniors with health challenges or disabilities
Although an individual senior may belong to more than one group, this review treats each group distinctly for the purpose of analytical clarity. In some cases, there is also overlap between a specific risk factor and a particular group of seniors (for instance, health challenges are a category of risk factors but seniors with health challenges can also be seen as a specific group of seniors). Elsewhere, certain categories of risk factors may cut across multiple groups (such as lack of access to resources like transportation, or the experience of widowhood). In effect, there are two different, yet overlapping, ways of looking at social isolation: one from the vantage point of risk factors, the other from the perspective of particular groups of seniors. The latter approach is important since it humanizes the experience of social isolation and tells the story from the perspective of real groups of people.
The groups that are examined below were identified as potentially being at high risk during the NSC consultations undertaken in 2013-2014, as well as through the NSC Scoping Review of the Literature: Social Isolation of Seniors conducted in the same year. The list of groups is not meant to be exhaustive, however, and others may also be deserving of attention. For example, a report published by the Office of the Commissioner of Official Languages (2013) called attention to observations made by the Special Senate Committee on Aging that seniors from official language minority communities (OLMCs) may be at greater risk of social isolation, especially when moving to an assisted-living or long-term care facility. "Aging in place" for such groups may actually mean being detached from their language and culture when they transition to care facilities. Thus far, the research on social isolation among seniors from OLMCs is virtually non-existent and the topic merits further consideration.
Aboriginal seniors
Based on the National Household Survey (NHS), the Aboriginal population of Canada was estimated at 1,400,685 people in 2011, representing 4.3% of the total Canadian population (Statistics Canada, 2013a).Footnote 15 Although only 6% of the Aboriginal population is aged 65 and over, (compared to 16% in the Canadian population), the proportion of Aboriginal seniors is increasing over time due to declines in mortality (more survivors to older ages) and lower fertility (smaller younger cohorts).Footnote 16 Aboriginal seniors are a highly diverse group with about half living in cities, and the other half in rural and remote areas, mostly on reserve (Wister and McPherson, 2014).Footnote 17 Recommendations to tackle social isolation need to recognize the unique characteristics of these groups.
Aboriginal seniors have faced numerous challenges over the course of their lives that may follow them into older age. These include higher levels of unemployment and poverty, substandard housing, higher rates of crime and abuse, separation from families during the residential school period, higher mortality and morbidity rates, and fewer health care, residential and community services (Wilson et al., 2011; Wister and McPherson, 2014). In addition, as a result of the colonial experience, they have experienced marginalization, especially those living on reserve in more rural and remote areas (Richmond, 2007). This makes them a highly vulnerable group and one prone to risks associated with social isolation. Yet, research into social isolation among Aboriginal seniors is scarce, with most literature focusing on access to health and community care or social inclusion among Aboriginal people in general (Health Canada, 2009).
Approaches to addressing aging-related needs among Aboriginal communities from the vantage point of social inclusion have identified complex barriers and challenges (Habjan et al., 2012; Haskell and Randall, 2009; Wilson et al., 2011). Haskell and Randall (2009), for instance, note how social connectedness at the interpersonal level has often been fragmented due to traumatic experiences (e.g., family violence, suicide, substance abuse, poverty, dislocation, etc.). Treloar et al. (2014) identify three situational barriers that can undermine the experience of social inclusion of Aboriginal people in cancer treatments: low socio-economic security, lack of trust in health care provision, and lack of knowledge about the system of cancer treatment (health literacy). To overcome these challenges, health-care providers must acknowledge them and create practical and symbolic responses in partnership with Aboriginal people, communities and health organisations.
Similarly, Habjan et al. (2012) identified multiple barriers regarding health and social support, including lack of a family caregiver, limited access to professional and health care services and providers, educational and training needs, barriers linked to community and government relationships, and relevant and safe care. Beatty and Berdahl (2011) have also identified multiple factors that lead to health challenges among Aboriginal seniors, including poverty, lack of housing, lack of nursing homes, and education and literacy barriers, as well as limited policymaker and caregiver knowledge of the needs of Aboriginal seniors. To address these complex barriers, multi-level changes are required.
Numerous studies have shown that Aboriginal communities can harness community-based resources especially through participatory and action-oriented approaches that empower seniors, their families, and their communities (Wister and McPherson, 2014). At the same time, a paradox exists with respect to social support and health among Aboriginal people – while they experience higher rates of social support within Aboriginal communities, this important social determinant of health has not resulted in better health status for Aboriginal seniors (Richmond, 2009). Fewer personal (especially economic) and interpersonal resources likely contribute to this paradox. Additionally, Richmond (2009) has shown that there can be stress associated with the supportive roles community members are expected to fill. Due to the small size of many Aboriginal communities and their relative isolation, community members who are also nurses or social workers may have difficulties escaping their professional roles. This can have negative consequences for those providing support as well as those receiving it.
The level of social isolation experienced by older Aboriginal people is not known, and it is likely that there is a tremendous degree of diversity depending on the community, and type of senior (e.g., middle-class urban dweller, senior living in an isolated reserve community, etc.). However, cultural and structural factors, coupled with high rates of significant traumatic events over the life course, and trust and understanding of the health and community care systems, may increase the risk of loneliness and social isolation. Low education and health literacy, low income or poverty, geographic location and isolation, poor health status, cultural separation, a higher likelihood of experiencing traumatic events, and fragmented informal and formal support systems create a cascading of risk for social isolation among Aboriginal seniors. Approaches to reducing the risk of social isolation need to address a number of risk factors that appear to be integrally connected to historic, cultural and social marginalization and rooted in economic disadvantage.
Seniors who are caregivers
Caregivers are the backbone of the continuing care system in Canada. In 2012, 8 million Canadians, or 28% of the population aged 15 and over, provided care to family members or friends with a long-term health condition, a disability or problems associated with aging (Turcotte, 2013). Among these caregivers, the majority provided care to a senior.
Although literature shows positive effects of caregiving, there is a substantial body of research that has established negative effects on the caregiver, especially when the intensity of care and related stressors increases, such as when the care recipient experiences serious physical and/or cognitive impairment (Pinquart and Sörensen, 2003; Robinson et al., 2009). Negative effects on the caregiver include burden, depression, stress, financial problems, poor health, loneliness and social isolation (Chappell and Funk, 2011).
While there is a vast literature on caregivers, not much of it has explored the issue of social isolation. Those studies that have been conducted suggest that caregiving in general does not lead to feelings of loneliness and social isolation per se. However, caregivers who experience lower levels of caregiving satisfaction experience more loneliness and social isolation. When caregiving is particularly demanding – when it entails heavy or live-in 24-hour care, for instance, or caring for someone with moderate or severe dementia or a serious physical disability, or when the care competence of the caregiver is low or challenged – it can result in feeling alone or being disconnected from the wider community of family, friends and neighbours (Lecovich, 2015; Robinson et al., 2009). Spousal caregivers may also be at greater risk of experiencing decreased social support and loneliness (Centre for Addiction and Mental Health, 2010). A qualitative study on caregiving in Elliot Lake, a retirement community in northern Ontario, found that caregivers' opportunity to participate in social activities is significantly reduced by the inability to leave the care recipient alone, and that caregivers can feel a great sense of isolation in the post-caregiving stage as they need to find new identities, social roles and activities (Sherman and Lacarte, 2012). Caregivers who are looking after spouses with dementia face the additional challenge of, in the words of one expert, "waking up every day with someone who has nothing to say."Footnote 18
Caregivers in remote areas may face particular challenges to isolation and loneliness. Qualitative research undertaken by Chappell et al. (2008) found that caregivers in remote areas faced a number of challenges, such as small isolated populations, severe winters, non-existent community programs, lack of community facilities in which to meet with others, and costly travel for services.
There are also a number of ameliorating factors that can protect against the negative impact of caregiving on health and well-being, including loneliness and social isolation. For instance, Robinson et al. (2009) found that lack of formal care services and financial difficulty were by far the strongest predictors of negative consequences of caregiving. Similarly, accessibility barriers can reduce social participation opportunities for both care recipients and caregivers, and lack of information on available services can increase caregiver burden and affect social participation (Sherman and Lacarte, 2012).
Thus, the provision of helping and financial support through informal assistance, respite services, home care or related services, and income and tax relief programs can have an enormous impact on the reduction of loneliness and social isolation of caregivers in these extreme situations (Sims-Gould and Martin-Matthews, 2007; Sussman and Regehr, 2009).Footnote 19
Immigrant seniors
Canada possesses a significant population of immigrants from a diversity of countries and regions. In 2011, approximately 22% of the Canadian population was born outside of Canada, including 4.5 million seniors.Footnote 20 Generally, immigrant seniors in Canada have been here for a long time since people tend to migrate when they are relatively young. Indeed, seniors aged 65 and older represented a relatively smaller proportion of new arrivals between 2006 and 2011 (only 3.3%). According to the Canada Mortgage and Housing Corporation (2012), the more recent the period of immigration, the lower the probability that a senior immigrant lives alone. This finding may be partly explained by the fact that many recent immigrant seniors live with members of their family who sponsored them when they came to Canada. Furthermore, among certain immigrant groups, it is traditional for elderly people to live with their children or other relatives.
De Jong Gierveld et al.’s (2015b) study found that, on average, older immigrants are significantly lonelier than older adults who are Canadian-born. Among the immigrant population of seniors, however, there is considerable diversity. Those who originate from countries with different languages and cultures than Canada are significantly lonelier than their Canadian-born counterparts while those who share English or French as a first language are not.Footnote 21 Interventions targeting the senior immigrant population must therefore take into account language and ethnicity.
This finding is reinforced by the experience of frontline workers. Among older socially-isolated immigrants in Vancouver, for instance, program administrators of the SUCCESS Seniors Quality of Life Outreach Project identified lack of proficiency in English as a major risk factor. Consequently, the program organizes activities and events in the languages of its clientele (primarily Cantonese and Mandarin) (Li, 2010).Footnote 22
Other factors were also shown to be significant in de Jong Gierveld et al. (2015a), particularly sense of belonging to the local community and frequency of social contacts (though not frequency of contact with relatives). Perhaps surprisingly, loneliness was also significantly associated with having a network of people who speak one’s native language. The authors speculate that this could be because such networks reinforce a feeling of cultural loss, or may be too small (and insular) to help the person connect to a broader network of people across a broader geographic space. In France, immigrant seniors seem to be at greater risk of experiencing several difficulties, including poverty and isolation (Alisaid-Guérain, 2015).
As a segment of the immigrant population, qualitative research undertaken by Vatz Laaroussi (2013) on older refugee women in Montreal suggests that migrational trajectories may have an impact on the experience of social isolation. Vatz Laaroussi found that first-generation exiles who came to Quebec in the 1960s and 70s with higher levels of education and autonomy were unlikely to experience isolation compared to women who migrated from refugee camps in the 1980s and 90s who tended to be more culturally distant from their children and grandchildren.Footnote 23
Some immigrant senior groups may also possess traits that provide a measure of protection against social isolation. Ng and Northcott (2015) found that familial living arrangements of South Asian immigrants, who typically live in extended families, were an important factor protecting against isolation in Edmonton. What mattered most, however, was not the living arrangement per se, but the amount of waking time spent alone at home and the quality of family relationships.Footnote 24
Limited research has also been undertaken on factors related to successful aging among immigrant groups with implications for the issue of social isolation. Noubicier and Charpentier (2013), for instance, studied the perceptions of senior immigrant women from Sub-Saharan Africa in Montreal towards aging, and found that social engagement, intergenerational relationships, financial autonomy, and faith were all key elements of successful aging.Footnote 25
In some cases, identifying seniors from immigrant groups who experience social isolation may be challenging. As part of its Age Friendly Initiative, the City of Nanaimo (British Columbia) sought to identify and remove barriers to social isolation for seniors in the community (North Sky Consulting Group Ltd, 2013). While only a small number of socially-isolated senior immigrants were identified, the authors speculate that referral agencies and others may have been hesitant to identify isolated immigrant seniors out of the fear that this could somehow jeopardize their immigration status.
Other factors may also interact with social isolation among senior immigrant groups. In the broader social isolation literature, for instance, there is a convincing body of knowledge suggesting that younger immigrant women are at high risk of social isolation. From the limited published work, however, gender differences among immigrant seniors could not be identified as a compounding factor.Footnote 26 Little is also known about the comparative prevalence of isolation among specific groups of immigrant seniors. Although more research is required on immigrant seniors and social isolation, it is clear that strategies to address this issue should consider culture, language, and the broader familial environment.
LGBT seniors
The LGBT community is a heterogeneous group comprised of lesbian, gay, bisexual and transgender individuals. According to census estimates, there are approximately 335,000 LGBT seniors in Canada, though this figure is understood to be an underestimate. Self-reporting is limited because many LGBT seniors are reluctant to be open about their sexual orientation or gender identity (Tang, 2015).
While many social and legislative changes in Canada have led to a considerable increase in the recognition of the rights of LGBT Canadians (Brotman et al., 2010), the history of the LGBT community is tainted in Canada and around the world by homophobic discrimination, stigmatization and exclusion by society (Brotman et al., 2010; Cassidy, 2007; Groupe SOS, SOS homophobie and AIDES, 2013). Yet LGBT seniors, many of whom were once required to keep their identity or sexual orientation secret, are still afflicted by the consequences of their traumatic experiences; and many forms of discrimination are still ongoing.
Discrimination towards older LGBT adults can be related to numerous factors; for example, as a result of having a sexual orientation that is different from the majority, aging, being a woman, having HIV/AIDS, or identifying with a sub-culture. Such discrimination can have a multiplier rather than a cumulative effect (Hébert et al., 2012; Orel, 2014). For certain LGBT seniors, living with multiple forms of discrimination poses additional challenges when they need support from their friends and families, or when they are looking for a suitable place to live (Orel, 2014). This complicates their access to services, such as health care, and has a direct impact on their overall health (Porter and Krinsky, 2014).
Indeed, there is considerable literature demonstrating that LGBT people experience discrimination in accessing health services. Several studies carried out in the 1990s and early 2000s revealed that older LGBT adults stated that they experienced discrimination in their interactions with health care professionals (Brotman et al., 2010), a situation that appears to be unchanged (Orel, 2014; Stein et al., 2010).
A study in the United States showed that discrimination can prevent LGBT seniors from seeking out resources (Orel, 2014), which may have serious consequences on their well-being (Brotman et al., 2010). Trans seniors who have not completed their physical transformation have even been forced to revert to behaviours associated with their original gender (clothing, etc.) (Latham, 2016). These experiences can lead to social isolation.
Additionally, LGBT seniors may have weak primary networks on which they can count on in situations of lost autonomy (Groupe SOS, SOS homophobie and AIDES, 2013; Stein et al., 2010). This may be due to the fact that they did not have children or that their network does not accept their LGBT identity (Orel, 2014). LGBT individuals who reveal their identity once they are older risk living separated from their friends and family (Groupe SOS, SOS homophobie and AIDES, 2013), which leads to a fear of coming out or a tendency to keep a certain distance in order to avoid rejection (Orel, 2014). Moreover, LGBT seniors who are out and maintain good relations with their friends and family indicate that these ties seem to break down as they get older for no apparent reason (Orel, 2014). The social network of LGBT seniors is therefore most often comprised of other LGBT persons (Orel, 2014). For some of them, in particular lesbians, friends come to be considered as family members (Gabrielson et al., 2014).
Furthermore, the spread of HIV in the 1980s directly affected the primary network of several LGBT people as a result of the death of their significant others, which contributed to the breakdown of their social network and their increased isolation (Groupe SOS, SOS homophobie and AIDES, 2013; Larkin, 2008; Orel, 2014). The weak social network, combined with difficult social recognition leads some LGBT people to dread the moment when they will lose their autonomy (Orel, 2014). Some consider suicide in order to avoid finding themselves in this type of situation (Witten, 2014, quoted by Zelle and Arms, 2015).
Other factors are also important. Isolation is apparently easier to overcome in an urban setting, where the LGBT community is larger and more visible (Erdley et al., 2014). This poses major challenges in a country like Canada, where urban settings are limited. Social isolation seems to have a more direct effect on homosexuals and bisexuals who hide their identity or don’t fully accept it than on those who assume their identity more openly (Camenzind, 2012). Additionally, the more that LGBT seniors live anonymously, the harder it is for services to reach them (Camenzind, 2012). This difficulty is also experienced by trans seniors depending on when their identity change took place (Hébert et al., 2012). Those who begin it later in life have much more difficulty with psychological and physiological adaptation, as well as with social acceptance (Cook-Daniels, 2001, quoted by Hébert et al., 2012).
As they age, older homosexual adults, and in particular men, also report feeling excluded from their community, which has a strong sub-culture that values youth and sexuality (Cassidy, 2007). Some seniors therefore have their need to socialize met in open religious communities, where they can become involved and have social relationships that are not focused on sexuality (Cassidy, 2007).
The literature therefore suggests that LGBT seniors are particularly vulnerable when it comes to social isolation, though precise numbers are often lacking. Given the multilayered challenges they encounter related to complex and ongoing histories of discrimination, LGBT seniors face many challenges that contribute to isolation and loneliness.
Seniors living alone
Among the Canadian population, living alone becomes increasingly more common as people age, especially for older women. According to the 2011 census, 31.5% of women aged 65 and over lived alone compared to 16% of senior men. Among those aged 85 and over, 36.6% of women lived alone compared to 21.7% of men (Statistics Canada, 2012). This is due to the higher life expectancy of women, men marrying younger women, lower rates of remarriage among women, and increasing preferences for independent living over time (Wister and McPherson, 2014). Older women are also more likely to live in institutions: among those aged 85 and over, 35.2% of women compared to 22.6% of men lived in institutions (Statistics Canada, 2012).
The association between living alone, social isolation and loneliness is complex. Living or not living with others does not necessarily result in a lack of social contact (Victor et al., 2000), yet it may be a sufficient cause. Living alone has been associated with fewer social contacts and lower social support, partly because people who live alone are not married or partnered, thereby lowering the amount of proximal support available (Sinha, 2014). Widowed, divorced and never married seniors have been shown to experience higher rates of loneliness and social isolation than married seniors (de Jong Gierveld et al., 2015a; Keefe et al., 2006; National Seniors Council, 2014a and 2014b). Recent findings from the English Longitudinal Study on Aging (ESLA)Footnote 27 revealed that household size is inversely related with prevalence of loneliness: seniors who live in larger households are less likely to be lonely (Iparraguirre, 2015).
Seniors living alone are also much more likely to be living in low income, which may increase the risk of being isolated (see below). Similarly, while living in a deprived neighbourhood increases the risk of all seniors of living in isolation, the effect is even greater among seniors who live alone. Transportation issues may also arise for single or widowed seniors who have never learned to drive (British Columbia Ministry of Health, 2004).
Data from the Canadian Community Health Survey – Healthy Aging, revealed that people living alone are particularly likely to need help with transportation, and that inadequate access to transportation or difficulty getting around may be a barrier to social participation (Turcotte, 2012).
While living alone and social isolation and loneliness share many of the same correlates (e.g., age, gender, widowhood, childlessness, entry into care, and mortality), they differ in terms of various resource-based risk factors, especially those linked to social class, physical and mental health status (Victor et al., 2000; Holt-Lunstad et al., 2015). Thus, it may not be living alone that contributes to social isolation and loneliness, but rather, other risk factors associated with both (Perissinotto and Covinsky, 2014). For instance, Ng and Northcott (2015) found that, among a sample of South Asian seniors living in Edmonton (who tend to live in extended families – see above), loneliness was associated with the quality of relationships and walking time, rather than living arrangement per se. Also, in a recent systematic review, Holt-Lunstad et al. (2015) found that mortality risk was increased by 29%, 26%, and 32% respectively for persons experiencing social isolation, loneliness and living alone, controlling for other correlates. This underscores the importance of examining the cumulative effects of risk and protective factors underlying social isolation and loneliness.
There is a need for research that can disentangle the common and distinct causes and consequences of living alone, loneliness and social isolation, before living alone can be used as a proxy or correlate of the latter.
Seniors living in remote or rural areas
Approximately 23% of all seniors in Canada live in rural areas, a pattern that is similar to the overall population since four out of five Canadians lived in urban areas in 2011 (Canada Mortgage and Housing Corporation, 2012). Large-scale studies on the overall prevalence of social isolation in rural areas in Canada are virtually non-existent, and few studies have compared differences between urban and rural areas. Kobayashi et al. (2009) found that as many as 17% of older adults, living primarily in small-town and small-city environments in British Columbia, were socially isolated.Footnote 28
Gender differences were also identified, with rural older men having smaller support networks and lower utilization rates of health and social services compared to rural women, who used more services and received more support from family and friends. The authors conclude that geographic and gender differences require targeted programs to help individuals sustain or enhance social integration.
For seniors living in rural areas with advanced cancer, lack of community support and access to services can lead to isolation and loneliness (Duggleby et al., 2011). Inadequate resources, loss in community and devaluing of rurality have also been linked to loneliness and a negative view of one’s self among rural senior women in Ontario. Ethnicity and gender were additional negative factors, with Aboriginal women pointing to a long history of discrimination and exclusion (Panazzola and Leipert 2013). In focus groups conducted by Hall et al. (2003), the inadequacy or non-existence of transportation services in rural areas was brought up as a source of isolation and loneliness. Keating et al. (2013) also found that loneliness among long-time residents in rural areas of newly affluent communities may have been linked to the fact that they were no longer able to take part in activities and organizations due to financial challenges (see also section on seniors with low income). The link between lack of transportation and isolation in rural areas has been noted elsewhere in the literature (Keefe et al., 2006). (See above for findings on isolation and living in remote areas among caregivers).
The way in which social isolation interacts with mental health may also vary by living environment. While seniors in rural, urban, and small-town environments exhibit similar levels of depressive symptoms (about 11.5% of the senior population), the factors associated with depression vary significantly across different environmental settings.
For seniors in rural areas, living alone, perceiving one's income as inadequate, and having a functional impairment were associated with depressive symptoms (St. John et al., 2006) in contrast to a different set of factors for urban and small-town seniors.Footnote 29
Despite the limited research on rurality and social isolation among seniors, the literature suggests that social isolation has an impact on the wellbeing of rural seniors that cannot be assimilated to the more general experience. More comparative research is required in this area.
Low-income seniors and those living in poverty
Approximately 4.7 million people – or 13.8% of the population – lived with low income in 2012 (Statistics Canada, 2014).Footnote 30 After 20 years of reductions, Canada’s elderly poverty rate rose between the mid-1990s and late 2000s, particularly among older women (The Conference Board of Canada, 2013). Drawing on data from Statistics Canada, Shillington (2016) reports that, low income among Canadian seniors has been steadily rising, from a low of 4% in 1995 to 11% – or one in nine seniors – in 2013. For seniors living alone, the poverty rate is particularly high.
Over the same period, the rate rose from 9% to 28% —almost one in three persons—for single women seniors, and from 6% to 24% for single male seniors. Many other groups of seniors are also more likely to experience poverty, including seniors with less education, seniors with intermittent work histories and low wages, older immigrants, Aboriginal seniors, seniors with chronic health problems, and seniors with disabilities (National Seniors Council, 2009).
Poverty and low income have been associated with experiences of loneliness and social isolation among the general population (Stewart et al., 2007). However, there have been few studies that focus specifically on older adults. Yet, older adults are more likely to live with low income than most other age groups, and low income has been associated with poorer health outcomes and lower quality of life indicators among seniors (Wister and McPherson, 2014). Thus, seniors living with fewer financial resources are faced with a number of potential negative outcomes which have been linked to loneliness and social isolation (Keefe et al., 2006; National Seniors Council, 2014a and 2014b).
After controlling for a large number of other risk factors, de Jong Gierveld et al. (2015a) found that income exhibited a weak but statistically significant inverse association with loneliness among seniors. A review of the literature on the social participation of seniors carried out by Raymond et al. (2008) also revealed that income is negatively associated with isolation, and a representative study in Belgium revealed that social isolation among seniors with low income was 29 percentage points higher than those with higher income (Vandenbroucke et al., 2012). Low income or poverty may often work in combination with other related risk factors to place people at ‘multiple jeopardy.’ One recent study has established a connection between low income, social isolation and nutritional risk among older adults, and these associations were especially strong among senior men who were members of a racial minority group (Locher et al., 2005). Research has also shown that low income is often associated with low self-esteem, which can inhibit the search for new social contacts (Pinquart and Sörensen, 2000).
In addition, MacCourt et al., (2011) found that poverty limits the ability of seniors to have adequate housing, while Gilmour (2012) found that retired seniors living in low income housing were more likely to be lonely. A report on housing for marginalized people in France found that aging and poverty put seniors at risk of isolation. While inadequate housing not adapted to the needs of seniors can be a major contributing factor to social isolation, adequate housing can be a major preventative factor (Haut comité pour le logement des personnes défavorisées, 2012).Footnote 31
One researcher also found that seniors in public long-term care (LTC) facilities were more likely than those in private facilities, where residents have greater economic and familial resources, to experience isolation (Trépied, 2012). Living in a deprived neighbourhood can also promote loneliness, especially among seniors who are living alone (British Columbia Ministry of Health, 2004). Seniors living on a low income in deprived neighbourhoods may have safety concerns related to leaving their dwelling (Abbott and Sapsford, 2005). This can be particularly challenging since many seniors look to their neighbourhoods to meet both practical and emotional needs (Freiler, 2004). Gentrification may also have an impact on increasing loneliness. Research in rural Canada, for example, found evidence of loneliness among long-time residents of newly affluent communities who were no longer able to take part in activities and organizations and for whom financial challenges limited social connections (Keating et al., 2013).Footnote 32
Older people who live alone are more likely to be near or below the poverty line than other older people. These seniors, in turn, face greater barriers to social participation, particularly if they live in rural or small-town environments, where there are often fewer social and leisure activities available (Kobayashi et al., 2009). One study of low-income senior women living alone in British Columbia found that, while their support networks were comparable to other groups, they relied more heavily on family support; greater efforts were required to diversify both their informal and formal sources of support since small family networks can be quickly overwhelmed (Ryser and Halseth, 2011).
Conversely, high income has been shown to be associated with less loneliness, possibly because those with higher income have commercial networks that can be used for social opportunities and because they are also in a better position to return support from others (Pinquart and Sörensen, 2000). Early evidence from the English Longitudinal Study on Aging has also shown that isolation decreases as wealth increases (Shankar, 2015). In the General Social Survey, Statistics Canada found that, although household income does not have a large influence on the number of close relatives and friends, Canadians in the highest income bracket ($150,000 or more) have larger networks of "other" friends (double the size of those with a household income of $20,000 or less) (Sinha, 2014).
In recognition of the complex interaction between poverty, isolation and other risk factors, some policymakers have adopted a comprehensive approach toward addressing social isolation among seniors with a strong economic dimension. France, for example, recently adopted a law related to societal adaptation to aging that focuses on reducing social inequality and isolation (Assemblée nationale, 2014). The law builds on previous efforts to address social isolation, including the national mobilization against the isolation of seniors,Footnote 33 a program which was embedded in the national plan to fight against poverty and for social inclusion (Serres, 2013). (Prior to the adoption of the law, a study on the social benefit for seniors found that the majority of recipients were socially isolated, and that the benefit was not sufficient to lift them out of poverty (Chaput et al., 2007)). In a related vein, Greenfield et al. (2015) argue that age-friendly community initiatives have the potential to address multiple issues related to older adults’ health and wellbeing, including economic insecurity and social isolation (the concept of age-friendly communities is discussed in Section 7.1.).
Seniors with mental health issues (including Alzheimer’s and other dementias)
Mental health has been defined as the capacity of each of us to feel, think and act in ways that enhance an individual’s ability to enjoy life and deal with life challenges. Mental illnesses, in contrast, are seen as alterations in thinking, mood or behaviour associated with some significant distress and impaired functioning (Standing Committee on Social Affairs, Science and Technology, 2004). The literature also includes cognitive and age-related mental health issues as part of the mental health spectrum. For example, the Mental Health Commission of Canada, as outlined in Guidelines for Comprehensive Mental Health Services for Older Adults in Canada, promotes a holistic approach considering mental illnesses as including Alzheimer’s disease and age-related dementias, serious and persistent mental illnesses complicated by aging issues, and mental illnesses that occur for the first time in old age.
Approximately 20% of seniors living in the community and up to 90% of those living in institutions are estimated to have a mental health problem or illness (Public Health Agency of Canada, 2010). The most common conditions include: depression, dementia, anxiety, delirium, and delusional disorders. Persons diagnosed with mental health issues tend to have fewer social resources, poor social competencies and symptoms that can pose barriers to maintaining connections to family, friends or community (Smith and Hirdes, 2009).
The stigma attached to an individual experiencing a mental illness can be a powerful agent in separating them from social contacts and social support systems (MacCourt et al., 2011; National Seniors Council, 2014a and 2014b). Several studies have shown that there are higher rates of reported loneliness amongst seniors with a mental illness, particularly dementia (e.g., British Columbia Ministry of Health, 2004; Victor et al., 2015). In one recent survey of people with dementia in the UK – the majority of whom were aged 65 and over – nearly two-thirds of those living alone reported feeling lonely, and a third said they had lost friends (Kane and Cook, 2013).
Mental health and mental illness among seniors can be connected to aspects of the aging process as well as situational factors that are associated with end of life experiences. Often, mental illness can be incurred or magnified due to stressors associated with advanced age, such as declines in resilience, physical health, low perceived control over health, death of a partner, moving to a new environment, financial difficulties, social isolation or loneliness (Newall et al., 2013 and 2014; Wister and McPherson, 2014). In this sense, the relationships between social isolation and mental health problems are often related to other aging-related challenges for many individuals.
At the same time, mental health issues of any kind may follow individuals throughout their life in a continual or episodic manner. An earlier onset of mental illness may lead to greater barriers in developing strong social contacts and maintaining social engagement with time, which can be carried forward into old age (Smith and Hirdes, 2009). The association between social isolation and mental health, therefore, needs to be examined from a life-course perspective as well as a dynamic one.
Seniors who become socially isolated, in turn, are at greater risk of mental illness given that social support is a protective factor for mental health problems (Chappell and Funk, 2011). For instance, Iliffe et al. (2007) found that social isolation was a predictor of depressed mood and perceived health among seniors who were not living in institutional settings. Similarly, in a review of the literature on suicide prevention among seniors, Saïas et al. (2013) found that isolation is a major risk factor associated with suicide among seniors. Social contact also attenuates two factors that are closely associated with suicide – depression and sleep disorders (and thus acts as a protective factor). There is also a connection between social isolation and addiction. Graziani (2010), for example, has shown that alcohol abuse among seniors can be a response to solitude, isolation or the loss of social support. The association between social isolation and mental health is therefore complex and bidirectional.
While mental health outcomes appear to be more associated with feelings of loneliness than social isolation per se (Coyle and Dugan, 2012), there is need for more research into the potentially cumulative and reciprocal effects of social isolation and mental health over the later life courses of individuals. Kobayashi et al. (2009) have found, for instance, that socially isolated adults are significantly different from their non-socially isolated counterparts in terms of several factors related to psychological well-being, including having higher levels of distress, lower coping abilities, and more negative feelings.
Seniors with health challenges or disabilities
As people age, they may experience physical symptoms associated with illness, frailty or the aging process. For others, disabilities may be a life-long or long-term experience. Although physical health issues and disabilities are distinct factors, both may be associated with physical vulnerability to social isolation. In Canada, most persons aged 65 and over have at least one chronic illness, and a majority have more than one chronic illness (Public Health Agency of Canada, 2010). Additionally, approximately 45% of seniors report a mild, moderate or severe disability, with this rising to 75% among those aged 85 and over (Statistics Canada, 2007).
While a majority of older adults rate their perceived health, well-being and daily functional ability as high even in the face of chronic illness or aging-related disability, many seniors nonetheless face challenges to daily functioning and maintaining connections with their family, friends and community. These impairments include pain, limited mobility due to sight, strength, and balance problems, loss of breath, general weakness, or fatigue, and other indicators of frailty and mobility impairment (Wister and McPherson, 2014). In the Canadian Community Health Survey – Healthy Aging (CCHS), health reasons were the most common reason given by seniors 75 years and over who were unable to participate in activities as much as they would have liked (Turcotte, 2012).
In a study on social isolation among seniors in British Columbia, Kobayashi et al. (2009) found that individuals who report being in fair or poor health have considerably higher odds of being socially isolated than those who report being in excellent, very good, or good health. Data from the CCHS revealed that the odds of being lonely were significantly higher for seniors who reported urinary incontinence than for those who did not, even when age, sex, education and living arrangements were taken into account (Ramage-Morin and Gilmour, 2013).Footnote 34 Keefe et al. (2006) also found that higher number of chronic illness was associated with higher levels of vulnerability to isolation even when controlling for other factors. Earlier research from the 1990s showed that chronic illness was one of the main factors linked to social isolation (see Hall et al., 2003).
Although physical health has been associated with social isolation and loneliness, the directionality of the relationship remains ambiguous. Most research have examined the effects of social isolation on a variety of health outcomes, including perceived health, functional health (disability), chronic illness, and accessing health care (Cornwell and Waite, 2009; de Jong Gierveld et al., 2015a; Kobayashi et al., 2009; Newall et al., 2015).Footnote 35
By definition, social isolation can restrict connectedness with social networks, which can result in fewer resources, lower social support, poorer health behaviours and lower access to health and community care system, all of which result in poorer health outcomes and lower levels of healthy aging (Keefe et al., 2006; National Seniors Council, 2014a and 2014b). Social isolation can also act as an aggravating factor in the diagnosis of disabilities among seniors – with fewer family members and friends, socially isolated individuals who develop sensorial problems as they age are likely to go untreated (Covelet, 2007).
Physical vulnerabilities can also limit mobility, which can compound transportation difficulties, particularly in areas where there is inadequate transportation provision. In the CCHS, when controlling for all other factors, seniors who travelled mostly by driving their car were more likely to participate than those who used any other form of transportation. Seniors who were mainly passengers and did not have a licence and those who used accessible transit or taxis had the lowest participation rates (Turcotte, 2012). In qualitative research undertaken by Hall et al. (2003), seniors indicated that the cessation of driving due to health problems was a problem of particular significance, especially in rural areas (see also North Sky Consulting Group Ltd, 2013). Some also mentioned the stigma of being dependent upon others as a barrier to asking for assistance. According to the World Health Organization, transportation is in turn a determinant of health because of the role it plays in seniors’ independence and ability to access resources (Keefe et al., 2006).
| Senior population | Identified risk factors | State of the research |
|---|---|---|
| Aboriginal seniors | Poverty; lack of resources; traumatic experiences; low access to health services; geographic location and isolation. | Little research (mostly focused on health). Need to validate risk factors and relative weight of each through quantitative research. Qualitative research on the experience of social isolation also required. |
| Seniors who are caregivers | Low levels of caregiving satisfaction; caregiving that is particularly demanding; caring for a spouse; inability to leave care recipient alone; accessibility barriers; lack of caregiving services (or information on services); financial difficulties; transition from post-care. | Some research, both quantitative and qualitative. Further studies could shed additional light. |
| Immigrant seniors | First language other than English or French; culture that is significantly different than Canada's; low sense of belonging to local community; low frequency of social contacts; network of people who speak one's native language; migration patterns of groups. | Some research, both quantitative and qualitative. Need for quantitative research on relationship between isolation and migration patterns (timing, reasons for migration, refugee status, etc.), gender, and incidence among specific groups, and qualitative research looking at the experience of specific groups. |
| LGBT seniors | Sexual orientation and gender identity; weak primary networks; rural setting; hiding one's identity; identity change that occurred later in life (for trans seniors); exclusion from community of sub-culture (for gay older men). | Some research, mostly qualitative and focused on the US experience. More quantitative research required to validate factors linked to isolation (particularly in Canada), and qualitative research to explore how isolation is experienced in different settings (e.g., rural-urban). |
| Seniors living alone | Lower levels of proximal support; low income; living in a deteriorated neighbourhood; not having learned to drive. | Little research, mostly quantitative. More qualitative research required on the experience of isolation, as well as additional quantitative research on underlying causes. |
| Seniors living in remote and rural areas | Gender (older men more at risk); lack of community support and services; loss of community; devaluing of rurality; ethnicity; lack of transportation. | Little research. Need for quantitative research to validate risk factors and to explore the relationship between rurality, ethnicity, Aboriginal status and isolation, and qualitative research on how isolation is experienced in different rural settings. |
| Low-income seniors and those living in poverty | Factors linked to poverty also linked to isolation (unattached older women; low education; intermittent work history; immigrants; Aboriginal people; chronic health conditions; low physical activity); low-income housing; living alone; rurality; low wealth. | Some research, mostly quantitative. Need for more quantitative research on how poverty and other risk factors interact to increase the risk of isolation, and qualitative research on poverty and the experience of isolation. |
| Seniors with mental health issues | Low social resources; low social competence; early onset of illness; stigma; general risk factors related to health; higher levels of distress; low coping abilities; negative feelings. | Some research, mostly quantitative. More quantitative research required on the cumulative and reciprocal effects of social isolation and mental health, and qualitative research on how seniors with different mental health issues experience isolation. |
| Seniors with health challenges or disabilities | Poor health; chronic illness; restricted social networks; low resources; low social support; low access to health and community care system; low physical activity; loss of driver's license; lack of transportation; accessibility barriers; mobility issues. | Some research, mostly quantitative. More quantitative research required on the relationship between physical dimensions of health and isolation, and qualitative research on how seniors with different health issues experience isolation. |
* The extent to which each factor has been linked to social isolation among particular groups is discussed in the previous sections. As noted throughout, some factors are more generalizable depending upon the methodologies of specific studies.
Research gaps
Overall, the review finds that the different groups of seniors that are examined are at risk of social isolation. At the same time, the literature on each group is uneven, both in terms of the quantity and quality of studies devoted to each one. Moreover, given the diversity of methods used in studies on social isolation and different groups of seniors, it is not possible to rank or order these different groups according to risk level (even if this was desirable). Social isolation is a complex phenomenon that seems to affect different groups of seniors distinctively even as there are general risk factors that cut across groups without discrimination.
Despite the growing body of literature on seniors and social isolation, there are many areas that require additional research and investigation. While the central task of this review was not to explore the literature as a whole, it ends with both some general comments on gaps in the state of knowledge on social isolation among seniors, particularly the groups examined above, before raising some considerations for policymakers.
From a general perspective, the research on social isolation would benefit from greater reliance on mixed or multi-method approaches. While quantitative approaches help to isolate primary risk factors, they reveal less about the actual experience of social isolation. Likewise, qualitative approaches tell us more about how seniors make sense of their own experiences with isolation and the meaning they attach to it than they do about which factors tend to be most important across population groups. A combination of both approaches promises to yield more conceptually rich discussions and a wider set of considerations to inform policy development.
There is also, at times, a need for greater conceptual clarity. While several studies use similar definitions and measures of social isolation, comparing findings can be challenging given the inconsistency of approaches and the overlap of concepts such as social isolation, loneliness, social inclusion, social participation, social engagement, and social capital (to name only a few). Since all of these concepts merit exploration in their own right, there is little to be done except to encourage, where possible, researchers to use consistent definitions and measures of social isolation to ensure comparability across the findings of studies and to avoid conceptual confusion. That being said, this is not always possible and specific conceptual definitions may be contentious.
Another missing element in the general research on social isolation is the lack of exploration on the changing nature of social isolation over the life-course. Some seniors may begin by experiencing episodic isolation before moving onto more long-term and chronic forms. What are the distinct pathways and bi-directional patterns associated with each form? How does episodic isolation become more chronic and acute? What are the early-warning signs and risk factors and how do these become compounded with time? It should be noted that the Canadian Longitudinal Study on Aging offers an unprecedented opportunity for researchers to develop a research agenda on social isolation based on a long-range, time horizon that may help answer some of these questions.
Looking at specific groups of the seniors, none of the groups reviewed here have been comprehensively examined, though there is enough evidence to suggest that each of them is at risk of social isolation. Greater segmentation as well as analysis of how different social identities overlap and intersect with social isolation would add considerably to the literature. Figure 2 summarizes the state of the literature on each group and suggests key areas that require further investigation. Again, a combination of qualitative and quantitative methods are required to explore the interaction of factors across groups in more depth, and to better understand the actual experience of isolation in specific groups (some of the studies on immigrant seniors can serve as a model in this regard). In examining the literature on specific groups, a dearth of studies on the specific protective factors within vulnerable groups are noted; however there is a need to know what protects individuals as much as what places them at risk. Indeed, the literature on the effectiveness of different strategies to reduce or eliminate social isolation among seniors is still at an early stage (as discussed below), and will require much further development.
Policy considerations
In reviewing the literature on specific groups of seniors and social isolation, it is apparent that there are many universal factors that cut across groups. At the same time, certain groups experience their own unique set of circumstances that render them particularly vulnerable. This suggests the need for a two-pronged approach to addressing social isolation. Since many risk factors are general in nature, coordinated policy interventions that can facilitate social inclusion across the population of seniors, such as improved housing and access to transportation, are required. For those factors that are more specific to a particular group, targeted interventions, such as providing support to senior caregivers to prevent isolation, and those attempting to reduce ageism and discrimination of specific vulnerable groups, are also recommended. This means that social isolation should become a key consideration for a range of policy areas linked to seniors in addition to being a policy focus in its own right. It also underscores the importance of multi-sectoral approaches bringing together multiple actors, as emphasized by Hanlon and Halseth (2005).
This collaborative approach of bringing together multiple actors to address seniors’ social isolation is currently being implemented by the Government of Canada, through the New Horizons for Seniors Program (NHSP).Footnote 36 Applicants of the NHSP’s 2015-2016 pan-Canadian call for proposals were required to submit collective impact plans coordinating the work of a variety of community partners to measurably reduce the rate of social isolation among seniors in a target population. This resulted in funding being made available for over 40 projects targeting groups of seniors, including caregivers, new immigrants, and persons with disabilities, in nine regions across Canada.
Age-friendly communities
In the Council’s previous report on social isolation (National Seniors Council, 2014a), the notion of age-friendly communities was raised as providing an important conceptual and practical approach to tackling many seniors’ issues, including social isolation. This approach is again noted here as it has the potential to mitigate many of the general risk factors that seniors from different walks of life experience. Developed by the World Health Organization (WHO), the concept of age-friendly communities (AFCs) addresses eight key domains of community living that enable seniors with varying needs and capacities to live in security, good health and to participate fully in society.Footnote 37
These include:
- Transportation
- Housing
- Social participation
- Respect and social inclusion
- Civic participation and employment
- Communication and information
- Community support and health services, and
- Outdoor spaces and buildings
AFCs provide opportunities to improve the quality of life not just for seniors, but for the whole community. As the Chief Public Health Officer of Canada (CPHO) (Public Health Agency of Canada, 2010) has noted, however, AFCs require not just increased service delivery, but also community awareness of services for seniors. "Developing outreach strategies for programs and services for seniors," the CPHO notes, "will require identifying which populations are underutilizing services and targeting attention to those seniors (and their networks) in program marketing plans." Changing the lived environment so that there are more meeting spaces for seniors and places to rest (including outdoor benches) are modest albeit important steps (Caradec, 2006). Underlying the success of AFCs is their ability to secure funding and resources over time (Greenfield et al., 2015). While age-friendly policies have the potential to combat ageism, a barrier to their implementation can also be discriminatory attitudes towards older people (Edwards, 2015).Footnote 38
Many provinces in Canada have undertaken age-friendly community initiatives. Garon et al. (2014) examined two case studies in Quebec and identified several factors that can determine success or failure. Among other things, they found that a pluralistic, participatory, and collaborative approach among stakeholders was essential (as opposed to a traditional top-down approach). Key to the success, according to one of the cases they looked at, was the identification of common goals and the development of a simple model on which there was consensus among stakeholders.
The Age-Friendly Communities in Canada: Community Implementation Guide – Toolbox (Nova Scotia Centre on Aging, 2012) presents useful and practical tips on how such communities can become a reality. The Public Health Agency of Canada (PHAC) promotes the uptake of AFC in Canada and provides a variety of tools and resources related to age-friendly communities. In 2015, PHAC has also prepared the Age-Friendly Communities Evaluation Guide to provide communities with practical information on how to use indicators to measure progress and evaluate their age-friendly initiatives.
Promising interventions for senior in general
With these high-level policy considerations in mind, the review ends with a brief overview of some of the promising interventions that have been identified in the literature that was consulted to tackle social isolation and reconnect seniors to their communities. While most of this literature focuses on seniors in general, findings on specific groups of seniors are referenced, where such findings are available. For information on various federal and provincial programs that address social isolation, the NSC’s Report on the Social Isolation of Seniors (2014) cites several relevant examples.Footnote 39
A brief note on the limitations of this literature is in order. Although interventions targeting social isolation have increased in number over the last decade, the number of high quality evaluation studies of programs remains relatively low, limiting the evidence to fully assess their impact. Writing in 2003, Findlay noted that “research evidence to support the belief that intervention can counteract social isolation and its adverse effects on older people is almost non-existent.” Responding to the dearth in evidence, Sabir et al. (2009) offered practice-based suggestions for a social isolation research agenda, including efficacy studies of multicomponent interventions.Footnote 40 While the state of knowledge has gradually increased, there are still important limitations to be noted. As Jopling (2015) has recently suggested, evidence on the impact of interventions to address social isolation exists in a spectrum, though “even where the evidence is of a lower quality it can be an important step in the development of a firmer understanding of what works." International networks of researchers and practitioners have also begun to coalesce around the topic of social isolation, including the UK Campaign to End Loneliness.Footnote 41 The Campaign has launched a Research Hub to increase and develop the evidence base on the issue of loneliness in older age.
Available evaluation studies indicate that there is a high degree of diversity in terms of the types of interventions that are assessed, the methodology used, and the quality of the evaluation (Dickens et al., 2011). Research designs range from randomized control and quasi-experimental studies to a variety of qualitative-evaluation approaches.Footnote 42
Further compounding the challenges, socially isolated individuals can be hard to reach to take part in evaluations (with the most isolated being the most invisible), diversity across seniors means that program impacts can be variable and funds for large-scale evaluations are often lacking. The result is that evaluations often have small and sometimes biased samples. Finally, researchers use different conceptual frameworks for classifying different types of interventions, which makes the task of comparing programs more difficult. Qualitative research has helped fill the void, but many studies are small-scale and it is not always clear whether findings can be generalized. Lurking in the background of many of these studies is the question as to whether or not program success is scalable – that is, can positive results be replicated at a larger level.
Still, important lessons can be gleaned from the literature. Systematic reviews of randomized control and quasi-experimental studies suggest that there is moderate evidence demonstrating the success of programs targeting social isolation in seniors.Footnote 43 Common characteristics of successful programs and types of programs are listed in the table below.
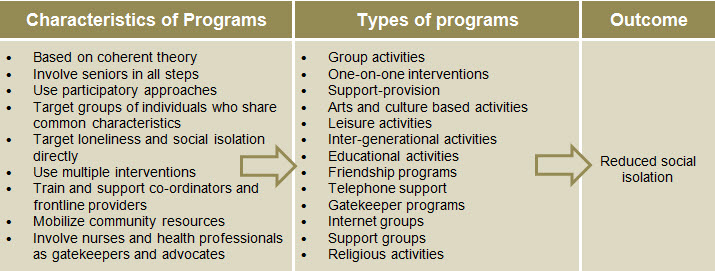
Image description of the Figure 3 : Successful Ways of Combatting Social Isolation
Characteristics of programs:
- Based on coherent theory
- Involve seniors in all steps
- Use participatory approaches
- Target groups of individuals who share common characteristics
- Target loneliness and social isolation directly
- Use multiple interventions
- Train and support co-ordinators and frontline providers
- Mobilize community resources
- Involve nurses and health professionals as gatekeepers and advocates
Types of programs:
- Group activities
- One-on-one interventions
- Support-provision
- Arts and culture based activities
- Leisure activities
- Inter-generational activities
- Educational activities
- Friendship programs
- Telephone support
- Gatekeeper programs
- Internet groups
- Support groups
- Religious activities
Outcome:
- Reduced social isolation
In terms of characteristics, programs that are based on a coherent theoretical basis of how to address social isolation have a greater chance of being successful, as are those that involve seniors in all programming steps, from planning to implementation, and evaluation. Participatory approaches that involve seniors in decision making and group activities are also important. Programs that target groups of individuals who share common characteristics – such as the various groups of seniors discussed in this review – can be fruitful, as well as those that target loneliness and social isolation directly (as opposed to targeting these indirectly while focusing on another issue). Programs that offer more than one method of intervention – such as group activities or individual support – have greater potential. Providing co-ordinators and frontline providers with good training and support is also important, as are mobilizing community assets to promote innovative approaches that pool resources, and involving nurses or allied health professionals as gatekeepers and advocates.
Jopling’s (2015) study on social isolation programs in the United Kingdom, conducted under the auspices of the UK Campaign to End Loneliness, further identifies the “structural enablers” that help facilitate success. These include designing programs at the neighbourhood level, using asset-based community development approaches – which focuses on identifying and mobilizing individual and community assets – creating opportunities for seniors to volunteer, and promoting age-positive approaches among key organizations and institutions within a local area. Joplin provides several useful descriptions of programs that have adopted these approaches.
In terms of the types of programs that are successful, the literature suggests that many different kinds of interventions can have a positive impact, including group activities, one on-one interventions and support provision (though group activities may have a greater impact according to the World Health Organization, 2015), arts and culture based activities, leisure activities, inter-generational activities, educational activities, friendship programs, telephone support, gatekeeper programs, internet groups, support groups, and religious activities. Thus, a range of different kinds of interventions can yield success – including those that use technology to create new communities – though in-person group activities are frequently mentioned as being particularly impactful.
In one systematic review, the Ministry of Health and Long-Term Care Ontario (2008) examined two different kinds of interventions – in-person group support activities and technology assisted interventions – and found that both showed positive results. Similarly, McDaid et al. (2015) looked at empirical studies testing the effectiveness of multiple programs and found that there was a small evidence base demonstrating that all of them had positive effects. These included arts and culture-based activities, friendship programs, intergenerational activities, and what they referred to as “Third Age” education. Toepoel (2013) examined data from a representative survey in the Netherlands and found that, among adults 65 years of age and older, cultural activities, reading books, and hobbies contribute to decreasing loneliness.
Individual program evaluations demonstrate positive results though they are usually based on small samples. An evaluation of Contact the Elderly (2008), for instance, indicated that a majority of participants felt less lonely as a result of the program. The program, which boasts 320 groups across the United Kingdom, organizes monthly Sunday afternoon teas between volunteers and seniors. Likewise, an evaluation of the Seniors Centre without Walls program, which provides free social and educational programming for older adults via telephone in Manitoba, revealed that the vast majority of participants felt more connected and less isolated (Newall and Menec, 2015). TeleVisit, a California-based non-profit, adopts a similar approach by facilitating group activities among seniors via teleconference and easy to use tablets.
In addition to these studies and evaluations, there is an emerging descriptive literature providing information on programs that tackle social isolation. For example, the World Health Organization (2015) describes several programs in Europe that have adopted innovative approaches, such as the Telephone Rings at 5 in Portugal, Multigenerational Centres in Germany, Cité Seniors in Switzerland, and Men’s Sheds in Australia and Ireland. Beach and Bamford (2015) also provide a useful summary of multiple projects in England including Walking Football, the Culture Club, and the Seafarers Project. The Belgium-based, Fondation Roi Baudouin, which provides funding to community initiatives to address social isolation, describes 20 separate projects that have been undertaken, their successes and challenges. Projects range from collective suppers, groups for cultural outings, and cross-cultural discussion groups to collective pampering sessions, inter-generational groups to promote knowledge exchange, and pen-pal groups between seniors and children (Teller and Dorsselaer, 2007). In France, social cafés have been established in several places where seniors can get together, converse, and participate in different activities, including intergenerational ones (Saci, 2012).
The organization, Pour Que l’Esprit Vive, hosts monthly musical concerts for seniors in care facilities in rural France as a way to encourage socialization and combat isolation. Both contemporary and older forms of music are played (Desjobert, 2012). Social actions centres (clubs du Centre d’Action Sociale), where physical activities are organized for seniors, and open houses (Maison Ouverte), where seniors can drop in to participate in activities, also exist in France (Hallier-Nader, 2011).
The annual reports of organizations tackling social isolation can also be extremely instructive. Les Petits Frères (2016), an organization that is active in 15 regions of Quebec, provides annual updates on its many activities, including inter-generational pairing of older people with young volunteers for social activities (jumelage), holiday celebrations, regional trips, and other ongoing outings and activities.
Finally, there are multiple toolkits that provide useful suggestions on how to start programs to address social isolation, including the Nelson Allan Project Toolkit, which provides practical information for grassroots groups and community organizations (Nelson Allan Project, 2015). Innoweave (2015) also provides practical information on how projects addressing social isolation among seniors can be scaled up and make use of social innovation techniques. Within the context of the UK Campaign to End Loneliness, the Hidden Citizens project provides practical steps to service providers on identifying those who experience loneliness (Goodman et al., 2015). The Campaign has also developed a guide to assist practitioners with evaluation.
Promising interventions for specific groups of seniors
In terms of the evaluation literature on programs addressing social isolation among specific groups of seniors, the literature is mostly suggestive. The following illustrates some potential promising interventions, however as previously stated, the evidence-base for some of these is still very much in its early stages, and this is not meant to be an exhaustive list:
- For Aboriginal seniors, activities that incorporate traditional activities and foods, including going out on the land, may be an effective way of addressing isolation and improving health outcomes. Some organizations that provide services to Aboriginal seniors, including Saanich First Nations Adult Care Society and Peter Ballantyne Cree Nation, connect seniors with youth, emphasizing the important role of First Nations Elders and storytelling (Health Council of Canada, 2013).
- For seniors who are caregivers, telephone-support groups may be an effective way of reducing social isolation (Stewart et al. 2006).Footnote 44 A study on caregiving in Elliot Lake recommended that, to enhance social participation among caregivers, the needs of care recipients must be met. Other recommendations included organizing social activities with both the caregiver and recipient involved, as well as activities that involve only the caregiver.
- For spousal caregivers caring for partners with dementia, adult day programs are an effective way of providing respite (Sussman and Regehr, 2009).
- For immigrant seniors, group activities provided in their main language can help break down linguistic barriers. As previously noted, the SUCCESS Seniors Quality of Life Outreach Project in Vancouver offers both recreational and educational activities in Mandarin and Cantonese to socially isolated seniors. In Belgium, immigrant and non-immigrant seniors are grouped together through the Mémoire Vivante program for cross-cultural learning as a way to overcome isolation (Teller and Dorsselaer, 2007). Similarly, in France, cafés for seniors adopt a mixed cultural and social approach to promote activities between ethnic groups and across generations and social classes (Saci, 2012).
- For older women living alone, educational activities via telephone have demonstrated some success based on participant self-reporting in the context of the Seniors Centre without Walls program in Manitoba (Newall and Menec, 2015). Widowhood bereavement support groups are also effective (Stewart et al., 2001).
- For seniors with dementia and their caregivers, memory cafés that provide naturally forming support groups can be effective (McFadden and Koll, 2014). Intergenerational programs such as the intergenerational choir for college students and persons with dementia and their family caregiver also show signs of success (Harris and Caporella, 2014).
- For LGBT seniors, countering discrimination is imperative. Training of health care staff involving LGBT cultural competency has demonstrated good results and has improved reception of and openness towards older LGBT adults, as well as consideration for their reality and specific needs (Porter and Krinsky, 2014). Training centres that address the experiences of LGBT individuals and their needs should be encouraged (Porter and Krinsky, 2014), including for social workers, who are particularly well placed to provide services to LGBT seniors and advocate on their behalf (Erdley et al., 2014).
- Inter-generational programs for LGBT seniors can also help build solidary and counter isolation. To counter ageism and social isolation in the LGBT community, a New York organization, Services and Advocacy for Gay, Lesbian, Bisexual and Transgender Seniors (SAGE), pairs LGBT seniors with LGBT volunteers with similar life experiences (age, orientation / sexual identity) (Larkin, 2008.)
Although programs and initiatives addressing social isolation seem to be multiplying with the growing awareness of this important issue, programs targeting specific groups of seniors, with some exceptions, are rare. While general programs are necessary, targeted ones could provide further impetus to efforts by stakeholders to combat social isolation. In both cases, evaluation efforts are essential to further develop the collective knowledge of the effectiveness of different types of interventions.
Conclusion
As the Canadian population continues to age, social isolation is a key challenge that affects the wellbeing of many seniors and increases their exposure to multiple health risks. This document built on the previous work of the NSC on social isolation, and aimed to contribute to knowledge-mobilization efforts in support of a multi-stakeholder approach to address this important issue. The NSC Report on the Social Isolation of Seniors (2014) proposed suggested measures for federal action. Specifically, the NSC recommended that efforts be made to 1) raise public awareness of the social isolation of seniors; 2) promote improved access to information, services and programs for seniors; 3) build the collective capacity of organizations to address isolation of seniors through social innovation; and 4) support research to better understand the issue of social isolation. Practitioners were also reminded of the funding that is available for projects addressing social isolation through the New Horizons for Seniors Program.
In conclusion, based on this review, the following general summary of findings is intended to inform the actions of the federal government, as well as other stakeholders such as researchers and frontline service providers. First, the review generally finds that the different groups of seniors that were examined are at risk of social isolation. At the same time, the literature on each group is uneven, both in terms of the quantity and quality of studies devoted to each one. This suggests that greater efforts are required to further develop the research on the barriers that specific groups of seniors encounter, and to tailor initiatives that address social isolation to their needs.
Second, given that social isolation is related to both general factors that cut across different groups of seniors and specific factors that are linked to issues faced by particular groups, a two-pronged approach to addressing social isolation seems warranted. On the one hand, coordinated policy interventions that can facilitate social inclusion across the population of seniors, such as improved housing and access to transportation, are required; on the other hand, targeted interventions, such as providing support to senior caregivers to prevent isolation, are also recommended. The concept of age-friendly communities has the potential to underpin a range of interventions that fall within the scope of both approaches.
Third, research on social isolation would benefit from greater segmentation, analysis of how different social identities overlap and intersect with social isolation, increased reliance on mixed methods (qualitative and quantitative), conceptual clarity and consistency, and exploration of social isolation across the life course. Additional research on protective factors would also be useful. Research on social isolation is growing, but there is still a limited amount of studies on how social isolation is experienced by specific groups of seniors.
Finally, the literature on effective interventions indicates that there is a high degree of diversity in terms of the types of interventions that are assessed, the methodology used, and the quality of the evaluation. There is a need for more high quality program evaluation studies of different programs and approaches, and programmers should be encouraged to build an evaluation component into all of their programs (recognizing that funding limitations can often make this difficult). In general, there is sufficient evidence to identify several common characteristics of successful interventions – such as involving seniors in the planning, implementation and evaluation stages – as well as different types of interventions, from group activities to educational phone chats. Training programs for frontline workers delivering programs is essential, as well as adequate resources. More generally, socially-isolated seniors could benefit from increased efforts to raise awareness of the underlying causes of isolation and to fight ageism. These are not easy issues to resolve, and addressing social isolation will require not only the coordinated and concerted action of multiple stakeholders, but also increased understanding of the importance of this issue among the Canadian public. This report provides a stepping stone to meet these goals so that social isolation among seniors can be prevented and/or reduced in the face of a rapidly aging Canadian population.
Reference list
Abbott, P. and R. Sapsford. (2005). “Living on the Margins: Older People, Place and Social Exclusion.” Policy Studies 26.1: 29-46.
Alisaid-Guérain, C. (2015). “Les populations immigrées face à la perte d’autonomie.” La Gazette Santé-Social 116: 36.
Assemblée nationale. (2014). “Projet de loi, adopté par l’Assemblée Nationale, relatif à l'adaptation de la société au vieillissement.” Session extraordinaire de 2013-2014. No. 804.
Bartsch, D. et al. (2013). “Outcomes of Seniors Reach Gatekeeper Referrals: Comparison of Spokane Gatekeeper Program, Colorado Senior Reach, and Mid-Kansas Senior Outreach.” Case Management Journals 14.1: 11-20.
Beach, B. and S.-M. Bamford. (2015). “Isolation: The Emerging Crisis for Older Men – A Report Exploring Experiences of Social Isolation and Loneliness Among Older Men in England.” Independent Age.
Beatty, B. and L. Berdahl. (2011). “Health Care and Aboriginal Seniors in Urban Canada: Helping a Neglected Class.” The International Indigenous Policy Journal 2.1.
Bohic, N. (2012). “Prévention des accidents cérébraux et vieillissement. Impact des inégalités sociales et territoriales de santé.” Gérontologie et société 5.1: 217-227.
Bolton, M. (2012). “Loneliness – The State We’re In.” A Report of Evidence Compiled for the Campaign to End Loneliness. Age UK Oxfordshire.
British Columbia Ministry of Health. (2004). “Social Isolation Among Seniors: An Emerging Issue.” An Investigation by the Children’s, Women’s and Seniors Health Branch, British Columbia Ministry of Health.
Brotman, S. et al. (2010). “Comprendre et soutenir les aînés gais et lesbiennes.” Vieillir au pluriel. Perspectives sociales. Presses de l’Université du Québec. 93-107
Camenzind, M. (2012). “Les personnes âgées homosexuelles : J’ai besoin d’un toit pour mon âme.” Soins infirmiers 105.4: 42-45.
Canada Mortgage and Housing Corporation. (2012). “Housing for Olders Canadians – The Definitive Guide to the Over 55 Market.” Volume 1. Understanding the Market.
Caradec, V. (2006). “Contribution: Isolement et vie relationnelle des personnes âgées.” Gérontologie 140: 30-31.
Cassidy, D.F. (2007). “L’intimité chez les hommes et les femmes homosexuels âgés.” Gérontologie et société 122: 233-245.
Cattan, M. et al. (2005). “Preventing Social Isolation and Loneliness Among Older People: A Systematic Review of Health Promotion Interventions.” Ageing and Society 25: 41-67.
Centre de Recherche et d’Information Nutritionnelles. (2010). “Personnes âgées à l’épreuve: vieillir sans trop s’appauvrir.” Alimentation, Santé et Petit budget 51: 2-4.
Centre for Addiction and Mental Health. (2010). “Best Practice Guidelines for Mental Health Promotion Programs: Older Adults 55+.” Centre for Addiction and Mental Health, Dalla Lana School of Public Health (University of Toronto) and Toronto Public Health.
Chappell, N.L. et al. (2008). “Respite for Rural and Remote Caregivers.” Rural Ageing.
Chappell, N.L. and L.M. Funk. (2011). “Social Support, Caregiving and Aging.” Canadian Journal on Aging 30.3: 355-370.
Chaput, H. et al. (2007). “L’aide à la vieillesse pauvre: la construction du minimum vieillesse.” Revue française des affaires sociales 1.1: 57-83.
Contact the Elderly. (2008). “Reaching Isolated Older People: Results of a Project to Evaluate Alternative Methods of Service Delivery and Support to Isolated and Lonely Older People.”
Cornwell, E.Y. and L.J. Waite. (2009). “Social Disconnectedness, Perceived Isolation, and Health Among Older Adults.” Journal of Health and Social Behaviour 50: 31-48.
Courtin, E. and M. Knapp. (2014). “Health and Wellbeing Consequences of Social Isolation in Old Age.” National Institute for Health Research.
Covelet, R. (2007). “Prendre enfin conscience des enjeux des déficits sensoriels des personnes âgées.” Gérontologie et société123.
Coyle, C.E. and E. Dugan. (2012). “Social Isolation, Loneliness and Health Among Older Adults.” Journal of Aging and Health 24.8: 1346-1363.
De Jong, J. et al. (2006). “Loneliness and Social Isolation.” In D. Perlman and A. Vangelisti (eds.), The Cambridge Handbook of Personal Relationships. Cambridge: Cambridge University Press.
De Jong Gierveld, J. et al. (2015a). “Determinants of Loneliness Among Older Adults in Canada.” Canadian Journal on Aging 34.2: 125-136.
De Jong Gierveld et al. (2015b). “Loneliness of Older Immigrant Groups in Canada: Effects of Ethnic-Cultural Background.” Journal of Cross-Cultural Gerontology 30.3: 251–268.
Desjobert, A. (2012). “Lutter contre l’isolement par l’art et la culture.” Gérontologie sans frontières 163: 43-50.
Dickens, A. et al. (2011). “Interventions Targeting Social Isolation in Older People: A Systematic Review.” BMC Public Health 11: 647.
Do, M.T. et al. (2015). “Fall-related Injuries Among Canadian Seniors, 2005–2013: An Analysis of the Canadian Community Health Survey.” Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice 35.7.
Duggleby, W.D. et al. (2011). “'I Am Part of the Community but...' The Changing Context of Rural Living for Persons with Advanced Cancer and their Families.” Rural and Remote Health 11.3: 1733.
Edwards, P. (2015). « Moving from Ageist to Age-Friendly Policies and Practices in Manitoba. » Centre on Aging, Winnipeg, Manitoba.
Erdley, S.D. et al. (2014). “Breaking Barriers and Building Bridges: Understanding the Pervasive Needs of Older LGBT Adults and the Value of Social Work in Health Care.” Journal of Gerontological Social Work 57.2-4: 362–385.
Findlay, R. (2003). “Interventions to Reduce Social Isolation Among the Elderly: Where is the Evidence?” Ageing and Society 23.5: 647-658.
Freiler, C. (2004). “Why Strong Neighbourhoods Matter: Implications for Policy and Practice.” Prepared for the Strong Neighbourhoods Task Force Toronto.
Gabrielson, M.L. et al. (2014). “Are they Family or Friends? Social Support Instrument Reliability in Studying Older Lesbians.” Journal of Homosexuality 61.11: 1589-1604.
Garon, S. et al. (2014). "Collaborative Partnership in Age-Friendly Cities: Two Case Studies from Quebec, Canada.” Journal of Aging & Social Policy 26.1-2: 73-87.
Gilles, L. and A. Loones. (2011). “Précarité, isolement et conditions de logement: La profonde fragilité des personnes âgées.” CRÉDOC, Consommation et modes de vie 245: 1-4.
Gilmour, H. (2012). “Social Participation and the Health and Well-Being of Canadian Seniors.” Health Reports: Statistics Canada 23.4, Cat. no. 82-003-X.
Goodman A. et al. (2015). “Hidden Citizens – How Can we Identify the Most Lonely Older Adults?” Campaign to End Loneliness.
Graziani, P. (2010). “La consommation excessive d’alcool chez la personne âgée.” Drogues, santé et société 9.2: 49-74.
Greenfield, E.A. et al. (2015). “Age-Friendly Community Initiatives: Conceptual Issues and Key Questions.” The Gerontologist 55.2: 191-198.
Groupe SOS, SOS homophobie and AIDES. (2013) “Rapport sur le vieillissement des personnes lesbiennes, gays, bisexuelles et transsexuelles (LGBT) et des personnes vivant avec le VIH (PVVIH).”
Habjan, S. et al. (2012). “Caregiving for Elders in First Nations Communities: Social System Perspective on Barriers and Challenges.” Canadian Journal on Aging 31.2: 209-222.
Hall, M. et al. (2003). “The Experience of Social Isolation and Loneliness Among Older Men in Manitoba.” Report Prepared for Veterans Affairs Canada. Aging in Manitoba.
Hallier-Nader, B. (2011). “Les territoires de vie des 75 ans et plus à Paris: quel environnement urbain pour une qualité de vie durable?” Université Paris-Est.
Hanlon, N. and G. Halseth. (2005). “The Greying of Resource Communities in Northern British Columbia: Implications for Health Care Delivery in Already-underserviced Communities.” The Canadian Geographer 49.1: 1-24.
Harris, P. and C. Caporella. (2014). “An Intergenerational Choir Formed to Lessen Alzheimer’s Disease Stigma in College Students and Decrease the Social Isolation of People with Alzheimer’s Disease and their Family Members: A Pilot Study.” American Journal of Alzheimer’s Disease & Other Dementias 29.3: 270-281.
Haskell, L. and M. Randall. (2009). “Disrupted Attachments: A Social Context Complex Trauma Framework and the Lives of Aboriginal Peoples in Canada.” Journal of Aboriginal Health 5.3: 48-99.
Haut comité pour le logement des personnes défavorisées. (2012). “Habitat et vieillissement: Vivre chez soi, mais vivre parmi les autres!” 17e rapport du Haut comité pour le logement des personnes défavorisées.
Hawton, A. et al. (2011). “The Impact of Social Isolation on the Health Status and Health-Related Quality of Life of Older People. Quality of Life Research 20.1: 57-67.
Health Canada. (2009). “Summative Evaluation of the First Nations and Inuit Home and Community Care.” First Nations and Inuit Health, Health Canada.
Hébert, B. et al. (2012). “Les aîné-es trans : une population émergente ayant des besoins spécifiques en soins de santé, en services sociaux et en soins liés au vieillissement.” Frontières 25.1: 57-81
Holt-Lunstad, J. et al. (2015). “Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-analytic Review.” Perspectives on Psychological Science 10.2: 227–237.
Iliffe, S. et al. (2007). “Health Risk Appraisal in Older People 2: The Implications for Clinicians and Commissioners of Social Isolation Risk in Older People.” British Journal of General Practice 57: 277-282.
Innoweave. (2015). “Seniors SI. Reducing Social Isolation for Seniors.” National Webinar.
Iparraguirre, J. (2015). “Socioeconomic Determinants of Risk of Harmful Alcohol Drinking Among People Aged 50 or Over in England.” BMJ Open 5.7.
Jopling, K. (2015). “Promising Approaches to Reducing Loneliness and Isolation in Later Life.” AgeUK – Campaign to End Loneliness.
Kane, M. and L. Cook. (2013). “Dementia 2013: The Hidden Voice of Loneliness.” Alzheimer Society.
Keating, N. et al. (2013). “Age-Friendly Rural Communities: Conceptualizing 'Best-Fit’.” Canadian Journal on Aging 32.4: 319-332.
Keefe, J. et al. (2006). “A Profile of Social Isolation in Canada.” Submitted to the Chair of the F/P/T Working Group on Social Isolation. Province of British Columbia and Mount Saint Vincent University.
Kirkland, S.A. et al. (2015). “Mining a Unique Canadian Resource: The Canadian Longitudinal Study on Aging.” Canadian Journal on Aging 34.3: 366-377.
Kobayashi, K.M. et al. (2009). “Making Meaningful Connections: A Profile of Social Isolation and Health Among Older Adults in Small Town and Small City, British Columbia.” Journal of Aging and Health 21.2: 374-397.
Larkin, M. (2008). “Social Networks Promote Engagement, Reduce Isolation, Boost Health.” The Journal on Active Aging 7.5: 32-40.
Latham, J.R. (2016). “Transgender People’s Experiences of Elder Abuse in Australia.” Presentation at the 4th National Elder Abuse Conference, Australia.
Lecovich, E. (2015). “Do Caregiving Burden and Satisfaction Predict Loneliness in Older Care Recipients?” Aging and Mental Health 20.4: 441-449.
Li, D. (2010). “SUCCESS Provides an Antidote to Social Isolation of Immigrant Seniors.” Immigrants and Refugees Issue of Visions Journal 6.3: 22.
Libres propos. (2011). “Prendre soin et accompagner les femmes migrantes âgées.” Le café social Ayyem Zamen. Entretien avec Moncef Labidi. Gérontologie et société 4.139: 87-97.
Locher, J.L. et al. (2005). “Social Isolation, Support, and Capital and Nutritional Risk in an Older Sample: Ethnic and Gender Differences.” Social Science & Medicine 60.4: 747–761.
McFadden, S. and A. Koll. (2014). “Popular Memory Cafes in Wisconsin’s Fox Valley Battle Social Isolation.” Generations 38.1: 68-72.
MacCourt, P. et al. (2011). “Guidelines for Comprehensive Mental Health Services for Older Adults in Canada.” Mental Health Commission of Canada.
MacVinnie, M. and C. Talbot. (2011). “A Research Review of Seniors, Isolation, and Best Practises in Service Provision.” The Nelson Allan Project Toolkit.
McDaid, D. et al. (2015). “Promoting Mental Wellbeing, Tackling Loneliness: A Review of the Effectiveness of Actions Delivered Outside of the Health Sector.” Presentation. The Finnish Association for Mental Health, National Institute for Health and Welfare and LSE-PSSRU.
Ministry of Health and Long-Term Care Ontario. (2008). “Aging in the Community.” Ontario Health Technology Assessment Series 8.1-6.
National Seniors Council. (2009). “Report of the National Seniors Council on Low Income Among Seniors.”
National Seniors Council. (2014a). “Report on the Social Isolation of Seniors.”
National Seniors Council. (2014b). “Scoping Review of the Literature: Social Isolation of Seniors.”
Nelson Allan Project. (2015). “Toolkit – The Nelson Allan Project: Connecting Seniors from Isolation to Activation.”
Newall, N. (2015). “Who’s at my Door Project – How Organizations Find and Assist Socially Isolated Older Adults.” Centre on Aging. University of Manitoba.
Newall, N.E. and V.H. Menec. (2015). “Targeting Socially Isolated Older Adults: A Process Evaluation of the Senior Centre Without Walls Social and Educational Program.” Journal of Applied Gerontology 34.8: 958-976.
Newall, N.E. et al. (2013). “Consequences of Loneliness on Physical Activity and Mortality in Older Adults and the Power of Positive Emotions.” Health Psychology 32.8: 921–924.
Newall, N.E.G. et al. (2014). “Predicting Stability and Change in Loneliness in Later Life.” Journal of Social and Personal Relationships 31.3: 335-351.
Newall, N. et al. (2015). “A Longitudinal Examination of Social Participation, Loneliness, and Use of Physician and Hospital Services.” Journal of Aging and Health 27.3: 500-518.
Ng, C.F. and H.C. Northcott. (2015). “Living Arrangements and Loneliness of South Asian Immigrant Seniors in Edmonton, Canada.” Ageing and Society 35.2: 552-575.
Nicholson, N.E. Jr. (2009). “Social Isolation in Older Adults: An Evolutionary Concept Analysis.” Journal of Advanced Nursing 65.6: 1342-1352.
North Sky Consulting Group Ltd. (2013). “Removing Barriers to Social Isolation.” City of Nanaimo, The Harbour City.
Noubicier, A.F. and M. Charpentier. (2013). “Vieillissement réussi : perception des femmes aînées immigrantes de l’Afrique noire à Montréal.” Santé mentale au Québec 38.2: 277-295.
Nova Scotia Centre for Aging. (2012). “Age-Friendly Communities in Canada: Community Implementation Guide – Toolbox.” Submitted to the Public Health Agency of Canada.
Office of the Commissioner of Official Languages. (2013). “Enjoying your Senior Years in your Own Language, Culture, and Community: Federal Support from Key Institutions and a Portrait of English-Speaking Seniors in Quebec.”
Orel, N.A. (2014). “Investigating the Needs and Concerns of Lesbian, Gay, Bisexual, and Transgender Older Adults: The Use of Qualitative and Quantitative Methodology.” Journal of Homosexuality 61.1: 53-78.
Panazzola, P. and B. Leipert. (2013). “Exploring Mental Health Issues of Rural Senior Women Residing in Southwestern Ontario, Canada: A Secondary Analysis Photovoice Study.” Rural and Remote Health 13.2: 2320.
Perissinotto, C.M. and K.E. Covinsky. (2014). “Living Alone, Socially Isolated or Lonely – What Are We Measuring?” Journal of General Internal Medicine 29.11: 1429-1431.
Petits Frères. (2016). “Une famille pour la vie.” Rapport annuel 2015-2016.
Pinquart, M. and S. Sörensen. (2000). “Influences of Socioeconomic Status, Social Network, and Competence on Subjective Well-Being in Later Life: A Meta-Analysis.” Psychology and Aging 15. 2: 187-224.
Pinquart, M. and S. Sörensen. (2003). “Differences Between Caregivers and Noncaregivers in Psychological Health and Physical Health: A Meta-Analysis.” Psychology and Aging 18.2: 250-267.
Porter, K.E. and L. Krinsky. (2014). “Do LGBT Aging Trainings Effectuate Positive Change in Mainstream Elder Service Providers?” Journal of Homosexuality 61.1: 197-216.
Public Health Agency of Canada. (2010). “The Chief Public Health Officer's Report on the State of Public Health in Canada 2010: Growing Older – Adding Life to Years.”
Public Health Agency of Canada. (2015). “Age-Friendly Communities Evaluation Guide: Using Indicators to Measure Progress.”
Ramage-Morin, P.L. and H. Gilmour. (2013). “Urinary Incontinence and Loneliness in Canadian Seniors.” Health Reports: Component of Statistics Canada 24.10, Cat. No. 82-003-X.
Raymond, E. et al. (2008). “La participation sociale des aînés dans une perspective de vieillissement en santé : réflexion critique appuyée sur une analyse documentaire.” Direction de santé publique de l’Agence de la santé et des services sociaux de la Capitale-Nationale, Institut national de santé publique du Québec, Centre d’excellence sur le vieillissement de Québec et Institut sur le vieillissement et la participation sociale des aînés de l’Université Laval.
Raymond, E. et al. (2013). “On the Track of Evaluated Programmes Targeting the Social Participation of Seniors: A Typology Proposal.” Ageing and Society 33.2: 267-296.
Richmond, C.A. (2007). “Narratives of Social Support and Health in Aboriginal Communities.” Canadian Journal of Public Heath 98.4: 347-351.
Richmond, C.A.M. (2009). “Explaining the Paradox of Health and Social Support Among Aboriginal Canadians.” Canadian Issues 1.1: 65-71.
Robinson, J. et al. (2009). “A Broader View of Family Caregiving: Effects of Caregiving and Caregiver Conditions on Depressive Symptoms, Health, Work and Social Isolation.” The Journals of Gerontology – Series B (Psychological Sciences and Social Sciences) 64.6:788-798
Ryser, L. and G. Halseth. (2011). “Informal Support Networks of Low-Income Senior Women Living Alone: Evidence from Fort St. John, BC.” Journal of Women and Aging 23.3: 185-202.
Sabir, M. et al. (2009). “A Community-based Participatory Critique of Social Isolation Intervention Research for Community-dwelling Older Adults.” Journal of Applied Gerontology 28.2: 218-234.
Saci, K. (2012). “ADEL, un café social pour rompre avec l’isolement des vieux immigrés. Témoignage.” Habiter et vieillir. Une société pour tous les âges? Quelles articulations entre les chercheurs, experts et acteurs sociaux dans le champ des politiques de la vieillesse? Les Cahiers des Ateliers de dialogue Recherche – Action – Expertise 4: 57-59.
Saïas, T. et al. (2013). “Prévention du suicide de la personne âgée : la place des interventions communautaires.” Pratique psychologiques 19.2: 103-117.
Serres, J.F. (2013). “Rapport MONALISA : Préconisations pour une MObilisation NAtionale contre l'ISolement social des Âgés.” Ministère des affaires sociales et de la santé.
Shankar, A. et al. (2013). “Social Isolation and Loneliness: Relationships with Cognitive Function During 4 Years of Follow-Up in the English Longitudinal Study of Ageing.” Psychosomatic Medicine 75.2: 161–170.
Shankar, A. (2015). “Social Connections in Older Adults: Associations with Health and Well-Being.” Presentation. Department of Epidemiology and Public Health, UCL.
Sherman, J.E. and S. Lacarte. (2012). “Social Inclusion of Seniors and Informal Caregivers in Elliot Lake. Phase II: Experiences of Informal Caregivers.” Prepared for Human Resources and Skills Development Canada.
Shillington, R. (2016). “An Analysis of the Economic Circumstances of Canadian Seniors.” Broadbent Institute.
Sims-Gould, J. and A. Martin-Matthews. (2007). “Family Caregiving or Caregiving Alone: Who Helps the Helper?” Canadian Journal on Aging 26.suppl 1: 27-46.
Sinha, M. (2014). “Canadians' Connections with Family and Friends.” Analytical Paper. Spotlight on Canadians: Results from the General Social Survey. Cat. no. 89‑652‑X — No. 006.
Smith, T.F. and J.P. Hirdes. (2009). “Predicting Social Isolation Among Geriatric Psychiatry Patients.” International Psychogeriatrics 21.1: 50-59.
St. John, P.D. et al. (2006). “Depressive Symptoms Among Older Adults in Urban and Rural Areas.” International Journal of Geriatric Psychiatry 21.1): 1175-1180.
Standing Committee on Social Affairs, Science and Technology. (2004). “Mental Health, Mental Illness and Addiction: An Overview of Policies and Programs in Canada.”
Statistics Canada. (2007). “Participation and Activity Limitation Survey 2006.” Tables. Cat. No. 89-628-XIE.
Statistics Canada. (2010). Cycle 4.2 of Canadian Community Health Survey – Healthy Aging. Cross tabulations undertaken by the NSC.
Statistics Canada. (2011). “National Household Survey 2011.”
Statistics Canada. (2012). “Living Arrangements of Seniors.” Census in Brief. Cat. no. 98-312-X2011003.
Statistics Canada. (2013a). “Aboriginal Peoples in Canada: First Nations People, Métis and Inuit.” Analytical Paper. Cat. no. 89-519-XIE.
Statistics Canada. (2013b). “The General Social Survey: An Overview.” Pub. no. 89F0115X.
Statistics Canada. (2014). “Canadian Income Survey, 2012”. The Daily.
Statistics Canada. (2015). “Canada's Population Estimates: Age and Sex, July 1, 2015”. The Daily.
Stein, G.L. et al. (2010). “Lesbian and Gay Elders and Long-Term Care: Identifying the Unique Psychological Perspectives and Challenges.” Journal of Gerontological Social Work 53.5: 421-435.
Stewart, M. et al. (2001). “Promoting Positive Affect and Diminishing Loneliness of Widowed Seniors Through a Support Intervention.” Public Health Nursing 18.1: 54-63.
Stewart, M. et al. (2006). “Accessible Support for Family Caregivers of Seniors with Chronic Conditions: From Isolation to Inclusion.” Canadian Journal on Aging 25.2: 179-192.
Stewart, M. et al. (2007). ““Left Out”: Perspectives on Social Exclusion and Social Isolation in Low-Income Populations.” Canadian Journal of Nursing Research 39.3: 209-212.
Sussman, T. and C. Regehr. (2009). “The Influence of Community-Based Services on the Burden of Spouses Caring for their Partners with Dementia.” Health and Social Work 34.1: 29-39.
Tam, S. and S. Neysmith. (2006). “Disrespect and Isolation: Elder Abuse in Chinese Communities.” Canadian Journal on Aging 25.2: 141-151.
Tang, K. (2015). “LGBTQ Seniors: Health, Housing and Social Support: An Annotated Bibliography.” Prepared for Pride Seniors Project: Into the Closet – A Needs Assessment.
Teller, M. and I. Van Dorsselaer. (2007). “Seniors admis, seniors amis: 20 projets pour lutter contre l’isolement des plus âgés.” Fondation Roi Baudouin.
The Conference Board of Canada (2013). “Elderly Poverty.” How Canada Performs.
Toepoel, V. (2013). “Ageing, Leisure, and Social Connectedness: How Could Leisure Help Reduce Social Isolation of Older People?” Social Indicators Research 113: 355-372.
Treloar, C. et al. (2014). ““I Can’t Do This, It’s Too Much”: Building Social Inclusion in Cancer Diagnosis and Treatment Experiences of Aboriginal People, Their Carers and Health Workers.” International Journal of Public Health 59.2: 373-379.
Trépied, V. (2012). “Les personnes âgées vivant en EHPAD, isolement ou solitude?” Documents Cleirppa 8.47: 24-28.
Turcotte, M. (2012). “Profile of Seniors’ Transportation Habits.” Canadian Social Trends. Component of Statistics Canada Cat. no. 11-008-X.
Turcotte, M. (2013). “Family Caregiving: What are the Consequences?” Insights on Canadian Society. Statistics Canada Cat. no. 75-006-X.
Umberson, D. and J. Karas Montez. (2010). “Social Relationships and Health: A Flashpoint for Health Policy.” Journal of Health and Social Behavior 51(Suppl): S54–S66.
Vandenbroucke, S. et al. (2012). “Vieillir, mais pas tout seul. Une enquête sur la solitude et l’isolement social des personnes âgées en Belgique.” Fondation Roi Baudouin.
Vatz Laaroussi, M. (2013). “L’impact des séparations et du veuvage dans la transmission auprès de trois générations de femmes réfugiées.” Conseil de recherches en sciences humaines du Canada (CRSH), Alliance recherche communautés-universités (ARUC).
Victor, C. et al. (2000). “Being Alone in Later Life: Loneliness, Social Isolation and Living Alone.” Reviews in Clinical Gerontology 10.4: 407-417.
Victor, C. et al. (2015). “Is Loneliness a Cause or Consequence of Dementia?” The Gerontologist 55 (Supplement 2): 593.
Wilson, D. et al. (2010). “Upstream Thinking and Health Promotion Planning for Older Adults at Risk of Social Isolation.” International Journal of Older People Nursing 6.4: 282-288.
Wilson, K. et al. (2011). “Aboriginal Peoples, Health and Healing Approaches: The Effects of Age and Place on Health.” Social Science and Medicine 72.3: 355-364.
Wilson, K. (2015). “The Impact of Isolation on Older Americans.” Presentation. AARP Foundation.
Wister, A. and B. McPherson (2014). “Aging as a Social Process.” Canadian Perspectives, Sixth Edition.
World Health Organization. (2015). “World Report on Ageing and Health.”
Zelle, A. and T. Arms. (2015). “Psychosocial Effects of Health Disparities of Lesbian, Gay, Bisexual, and Transgender Older Adults.” Journal of Psychosocial Nursing and Mental Health Services 53.7: 25–30
Page details
- Date modified:
