Expert Advisory Group Report 1: Charting a Path toward Ambition
Download the alternative format
(PDF format, 660 KB, 14 pages)
Organization: Public Health Agency of Canada
Published: 2021-06-17
Table of contents
- Preface
- Terminology used in this report
- Ambition
- Current state of health data
- Vision for the Canadian health data ecosystem
- Charting a new course: Strengthening Canada's Data Foundation
- Conclusion: A Path Forward
- Contact
Quote from Martin Wilk report "Health Information for Canadians" (1991), describing the state of the health data ecosystem with many of its bold recommendations unfulfilled.
"I was aware from the outset that Canadian health information was not in good shape. My current assessment is that it is in a deplorable state. My image of health information is somewhat like an unmapped forest with undefined boundaries. Multitudinous health constituencies have important information needs associated with their responsibilities (they need a map pertinent to their position in "the forest"). Typically, those information needs - for policy, management, research, health care provision, evaluation, outcomes monitoring, personnel planning and training, budgeting, resource allocation - are unmet or inadequately met, with important exceptions. And this situation is co-existent with a vast array of data collected and accumulated by many constituencies, public agencies and care-givers."
Preface
In summer 2020, I was honoured to be asked to assume the role of "Health Data Champion for the pan-Canadian Health Data Strategy". The purpose of the role is to help address the systemic problems that have prevented the timely and trusted collection, sharing, and use of data for the benefit of Canadians.
As demonstrated during the first wave of COVID-19, and subsequent waves, significant gaps remain in Canada's health data ecosystem, from timely reporting of basic data on individual cases and outbreaks, to genomic surveillance for new variants, or assessment of vaccine coverage, safety, and effectiveness in real-time. There is no doubt that our response to the pandemic has been severely limited as a result. Numerous high-profile reports and recommendations over many decades have repeatedly outlined what needs to be done. We need to tackle the root causes of the problems that have plagued our ability to make progress toward a common aim for all Canadians. Put simply, our systems, processes and policies are geared towards an analog world, while we live in a digital age.
To that end, an Expert Advisory Group, leveraging a cross section of experts from across the country, has been formed. This group has reviewed hundreds of reports and articles, some dating back to the 1960s, and deliberated on practical approaches to make progress.
This first report from the Expert Advisory Group articulates key findings from those deliberations including: establishing an ambition for Canada's health data ecosystem, understanding the root causes that have prevented progress, highlighting opportunities from a revitalised approach, and developing a practical set of areas of focus and principles. These will be elaborated in future reports to guide the development of a pan-Canadian Health Data Strategy.
There is no "smoking gun" - the challenges to implementation are the result of a complex set of interactions between multiple levels of government, health professionals and organizations, and the public and private sector with the common goal of access to data while preserving privacy and confidentiality. Accordingly, there are no simple solutions or easy fixes.
In parallel with the Expert Advisory Group developing our advice for the Strategy, there will be an engagement in the coming months with stakeholders across the country to inform the final recommendations that will elaborate how to achieve an ideal future state. This report provides a foundation for further analysis and discussion.
By working together now, we can benefit from past efforts and create a common path forward so that timely and accurate health data can improve the lives of all persons in Canada.
Dr. Vivek Goel
Chair, pan-Canadian Health Data Strategy Expert Advisory Group
Terminology used in this report
There is no consistent language for talking about health data in Canada. This is a list of terminology used in this document.
- Access is the act of providing access to the data for authorized individuals. Access can be achieved by data visiting (where data remain in place) or physical data sharing (where data are copied)
- Health data refers to publicly and privately held data related to health care, public health, population health, and health research, inclusive of relevant socio-demographic factors (e.g. race, ethnicity, gender, age) and data from other sectors
- Health data ecosystem is the set of governance, policies, processes, designs, and data flows for an interoperable network designed and developed to ensure the best possible health services and outcomes for Canadians based on excellent research, population and public health services and policies, and delivery, organization and management of health care.
- The public includes individuals and their families and caregivers and encompasses all persons living in Canada including those who have contact with health services as a result of disease or injury as well as maintaining and promoting health for all
Quote from 2003 National Advisory Committee on SARS and Public Health, identifying challenges in Canada's health data ecosystem. Many of these same issues persist today.
"A great many systemic deficiencies in the response to SARS were identified as the Committee went about its task. Among these were:... difficulties with timely access to laboratory testing and results; absence of protocols for data or information sharing among levels of government; uncertainties about data ownership; inadequate capacity for epidemiologic investigation of the outbreak; lack of coordinated business processes across institutions and jurisdictions for outbreak management and emergency response; … and weak links between public health and the personal health services system, including primary care, institutions, and home care."
Ambition
All persons in Canada deserve to achieve the best health outcomes with appropriate protection for their data. Those who hold health data hold it in trust. Holding something in trust means to protect it and to optimize its value. Canadians expect their health data to be used to improve their own care while protecting their privacy. This same data may be used for better decision making to aid in the health and safety of others, support public health, and improve health systems. These are compatible goals and inseparable components of trust.
Over the last 60 years, many reports have been written and efforts undertaken with an eye toward the better use and protection of data for improved individual, population, and public health outcomes. Despite clear political drivers (e.g. SARS), funding for action (e.g. Panorama - see sidebar on page 3), and technical blueprints, Canada's progress lags other countriesFootnote 1. As has been demonstrated during COVID-19, significant gaps remain.
A Champion for health data was appointed in summer 2020 to help guide a long-term strategic approach to address those gaps. This evolved into the pan-Canadian Health Data Strategy (pCHDS). Governance for the strategy was agreed in fall 2020 and an Expert Advisory Group (EAG) for the pCHDSFootnote 2 was appointed shortly thereafter.
This is the first report of the EAG. The objective of this report is to set the stage for the urgent need to improve the use and protection of health data in Canada by addressing the root causes that have been preventing progress on a pan-Canadian scale.
This report lays out a bold common vision for health data for Canadians. It looks at the current state and the root causes that have prevented progress. Finally, it lays the basis for developing a practical approach to strengthen Canada's health data foundation and principles for its implementation.
The advice in this report will support the co-development of a long-term pCHDS by federal, provincial, and territorial governments that aligns and complements data strategies of First Nations, Inuit, and Métis peoples across geographies, which are being developed by the appropriate distinctions-based entities. Further advice from the EAG will be published through fall 2021 including practical approaches to strengthen the foundation for Canada's health data. This advice will be used by governments to create a co-developed vision, principles, implementation plan, and roadmap which will be shared with the Conference of Deputy Ministers of Health in winter 2021/22.
Current state of health data
The current Canadian health data ecosystem impedes the best possible health outcomes, results in poor patient and provider experience, and incurs higher costs.
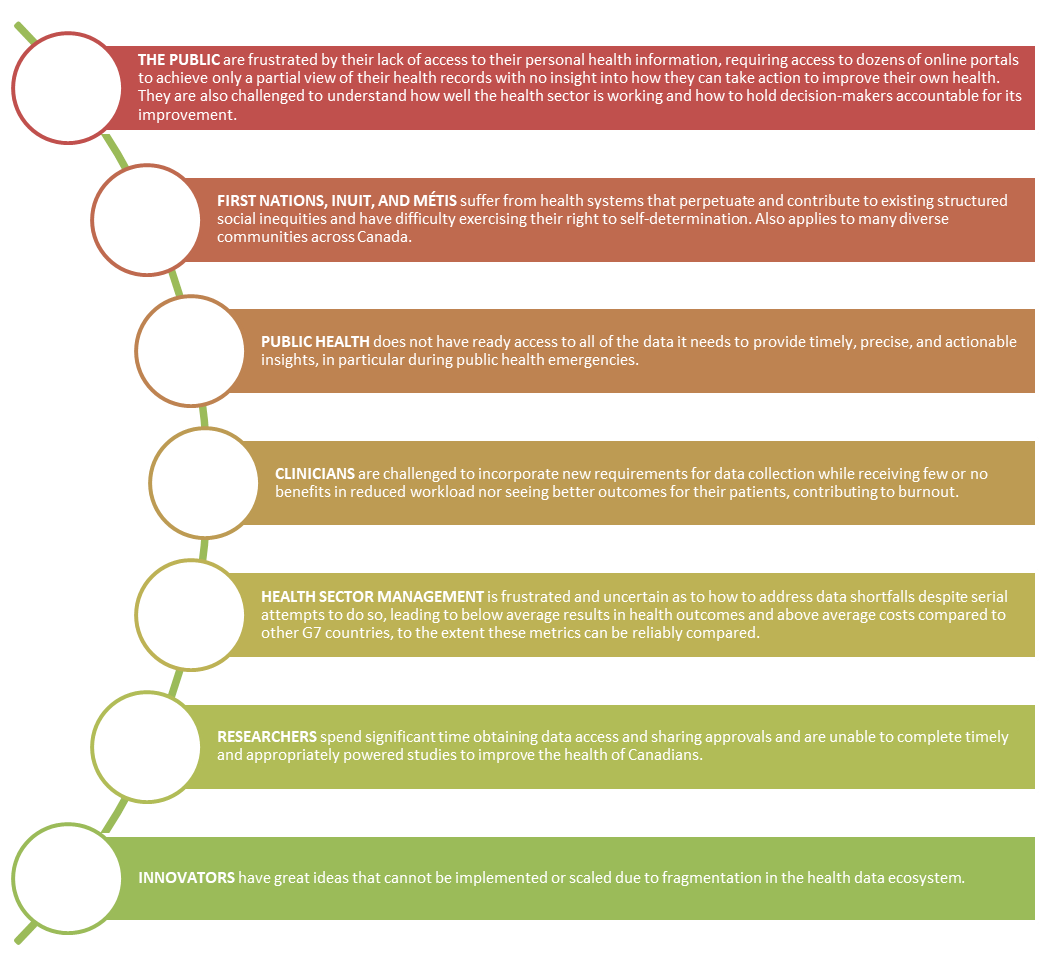
Figure 1 - Text description
The current state of health data impacts groups in different ways.
The public are frustrated by their lack of access to their personal health information, requiring access to dozens of online portals to achieve only a partial view of their health records with no insight into how they can take action to improve their own health. They are also challenged to understand how well the health sector is working and how to hold decision-makers accountable for its improvement.
First Nations, Inuit, and Métis suffer from health systems that perpetuate and contribute to existing structured social inequities and have difficulty exercising their right to self-determination. Also applies to many diverse communities across Canada.
Public health does not have ready access to all of the data it needs to provide timely, precise, and actionable insights, in particular during public health emergencies.
Clinicians are challenged to incorporate new requirements for data collection while receiving few or no benefits in reduced workload nor seeing better outcomes for their patients, contributing to burnout.
Health sector management is frustrated and uncertain as to how to address data shortfalls despite serial attempts to do so, leading to below average results in health outcomes and above average costs compared to other G7 countries, to the extent these metrics can be reliably compared.
Researchers spend significant time obtaining data access and sharing approvals and are unable to complete timely and appropriately powered studies to improve the health of Canadians.
Innovators have great ideas that cannot be implemented or scaled due to fragmentation in the health data ecosystem.
A core reason for this situation is a weak foundation for data collection, sharing, and use, resulting in a highly fragmented health data ecosystem. These issues have been underscored through Canada's response to COVID-19 - challenges in timely collection and use of testing, case, and vaccination data; assessing impacts of the pandemic in specific populations; sharing genomic data for management of variants; and the persistent challenges of long-term care.
Root causes must be addressed for a strategy to be successful
Several historical factors have hindered progress toward a cohesive health data ecosystem.
Panorama: Canada attempted to rollout a comprehensive public health data platform, which included a consistent approach to tracking vaccinations in anticipation of future pandemics.
This started in 2004 and the platform was called Panorama. After 8 years and more than $130MM of federal money (and significant additional funds from provincial and territorial jurisdictions), Canada had a series of unconnected solutions in eight jurisdictions with no ability to integrate or scale. Since then, some improvements have been made; however, the original objectives of Panorama have not been achieved.
There are many reasons for the failure of Panorama, much of which rests on a lack of appreciation (and prioritization) for the value of long-term consistency, unclear accountability, and a lack of trust among partners. Strong, consistent, and reliable leadership is required to remind and champion decisions aligned with long-term goals.
The short-term won out, much to the loss of Canada during COVID-19.
- Lack of trust and clear accountability for data and analysis within and between jurisdictions, governmental organizations and data custodians (e.g. health providers).
- A culture of risk aversion among senior leadership, data custodians and privacy officers who have incentives to prevent privacy breaches rather than both ensuring public benefits from the use of their data holdings and the protection of personal health data. This is exacerbated by insufficient understanding of applicable personal health information legislation and inconsistencies between these statutes across jurisdictions.
- A culture of avoidance amongst health providers and leaders of potentially embarrassing results of comparative analysis.
- Misaligned incentives and lack of a common vision resulting from different policy goals, priorities, risk tolerances, and cultures that do not encourage collaboration across silos.
- A reluctance to include conditional requirements for fiscal transfersFootnote 3 in the interest of maintaining cooperation resulting in a failure to create a cohesive health data ecosystem.
- Antiquated data policy environment designed for paper records and analog transmission that does not consider approaches that would achieve better health outcomes while also protecting data in the digital age.
- Limited public insight and involvement in conversations around data use, which misses the opportunity to increase data literacy and minimizes public influence on those decisions.
- Inconsistent and insufficient investment in data capacity and capability that undervalues efforts to sustain and generate long-term value from data through a comprehensive person based approach that generates timely insights.
- Fiscal pressures to contain growing costs of health services leads to focus on "front-line" health expenditures, crowding out investments in data capacity, capability, and infrastructure.
- An uncoordinated approach to procuring and implementing data and technology solutions without requirements for data access, interoperability, and cohesion for care, population health, and public health.
- Lack of consensus and follow-up on pan-Canadian interoperability compounded by short-term incentives to implement vendor-centric or narrowly focused solutions that limit leveraging, strengthening, and learning from a common data foundation.
- A failure to spread and scale excellence in the collection, sharing, and / or use of data across the country.
- Significant data debt resulting from fragmented and dysfunctional legacy IT systems - within and across jurisdictions - and data assets that cause an expensive patchwork of ad hoc solutions to integrate data that are difficult to untangle.
Vision for the Canadian health data ecosystem
By 2030, all persons living in Canada will benefit from a fully integrated and continuously optimized health data ecosystem that honours data ownership and collective quality care through the cooperative use of individual and aggregate health data.
Breaking apart this vision:
- All persons living in Canada encompasses all Canadians including those who have contact with health services due to disease or injury as well as maintaining and promoting health for all.
- Fully integrated includes within and across jurisdictions in all care settings.
- Continuously optimized incorporates a learning health system and evidence-informed public and population health policy to achieve outcomes aligned with the needs of the public.
- Health data refers to publicly and privately held data related to health care, public health, population health, and health research, inclusive of socio-demographic factors (e.g. race, ethnicity, gender, age) and data from other sectors.
- Health data ecosystem is the set of governance, policies, processes, designs, and data flows for an interoperable network designed and developed to ensure the best possible health services and outcomes for Canadians based on excellent research, population and public health services and policies, and delivery, organization and management of health care.
- Data ownership incorporates meaningful individual access to their own health records and the ability to govern its use in the context of communities and the health data ecosystem recognizing the need for population and public health uses that require comprehensive data.
- Collective quality careFootnote 4 incorporates several dimensions of care including safety, health outcomes, effectiveness, efficiency, equity, person-centred care, and timeliness.
- Cooperative includes cooperation from all levels in public sector governments, health delivery organizations, the private sector, and other critical stakeholders.
To be successful, a vision would be pan-Canadian and adopted by provincial, territorial, and federal governments. Adoption would recognize autonomy in jurisdictional delivery of care while maintaining pan-Canadian consistency and cohesiveness in the areas that matter most to achieving the vision.
The vision is not to create a single centralized technology solution as modern tools allow for significant levels of interoperability across distributed systems. The vision is to foster a robust health data ecosystem that enables timely access and interoperability of data to achieve individual, regional, provincial / territorial, and pan-Canadian outcomes.
How the Vision would benefit all health system stakeholders
At its core, the vision would ensure the right data are available with the right details to the right people with the right protections at the right time to inform evidence, insight, and action. When implemented Canada will be a global leader in health outcomes, cost per capita for care, health research, and patient experience.
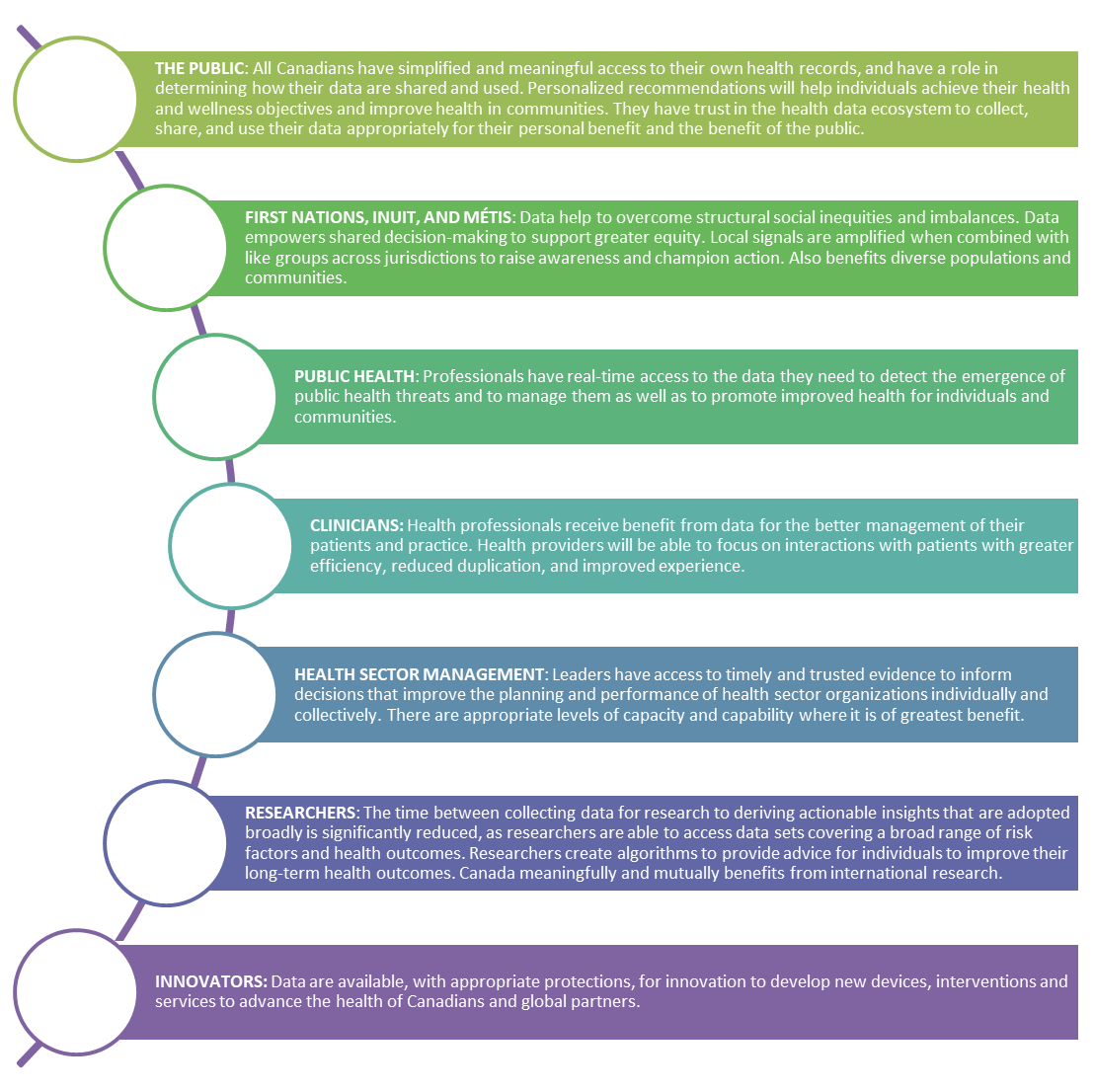
Figure 2 - Text description
A future state for health data after implementation of the Vision for the Canadian health data ecosystem could benefit different groups in the following ways.
For the public, all Canadians have simplified and meaningful access to their own health records, and have a role in determining how their data are shared and used. Personalized recommendations will help individuals achieve their health and wellness objectives and improve health in communities. They have trust in the health data ecosystem to collect, share, and use their data appropriately for their personal benefit and the benefit of the public.
For First Nations, Inuit, and Métis peoples, data help to overcome structural social inequities and imbalances. Data empowers shared decision-making to support greater equity. Local signals are amplified when combined with like groups across jurisdictions to raise awareness and champion action. Also benefits diverse populations and communities.
Public health professionals have real-time access to the data they need to detect the emergence of public health threats and to manage them as well as to promote improved health for individuals and communities.
Clinicians and health professionals receive benefit from data for the better management of their patients and practice. Health providers will be able to focus on interactions with patients with greater efficiency, reduced duplication, and improved experience.
Health sector management leaders have access to timely and trusted evidence to inform decisions that improve the planning and performance of health sector organizations individually and collectively. There are appropriate levels of capacity and capability where it is of greatest benefit.
For researchers, the time between collecting data for research to deriving actionable insights that are adopted broadly is significantly reduced, as researchers are able to access data sets covering a broad range of risk factors and health outcomes. Researchers create algorithms to provide advice for individuals to improve their long-term health outcomes. Canada meaningfully and mutually benefits from international research.
Charting a new course: Strengthening Canada's Data Foundation
Addressing the complexity in the health data ecosystem requires a combination of boldness, political will, funding, expert advice, clear accountability, practicality, and public input and support.
The first step is to focus on the common elements that matter most by strengthening Canada's health data foundation. A strong foundation is key for long-term sustainability, stability, and value creation. Canada's health data foundation needs to be deliberately designed and orchestrated in partnership across all jurisdictions and stakeholders.
This health data foundation would be made of five components:
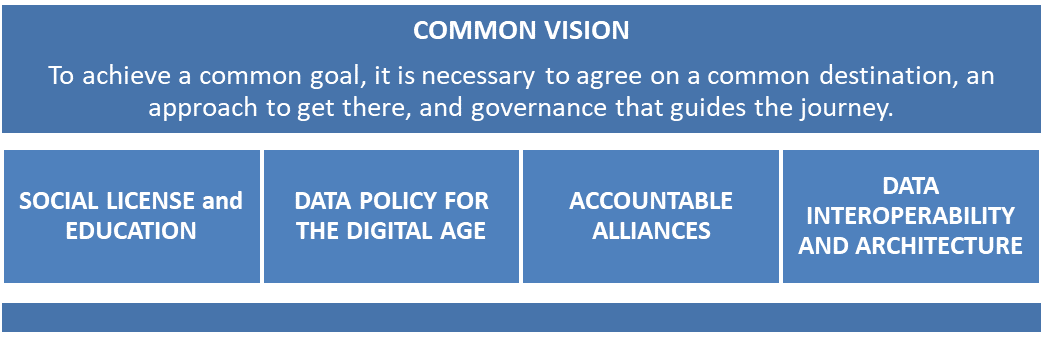
Figure 3 - Text description
Canada's health data foundation would have five components. The first component is a common vision that underpins the four others. To achieve a common goal, it is necessary to agree on a common destination, an approach to get there, and governance that guides the journey. The other four components are:
- Social license and education
- Data policy for the digital age
- Accountable alliances
- Data interoperability and architecture
- Social license and education: The public and health workforce must be educated, active, and involved partners in the journey to improve data capability and capacity. In addition to education, there must be channels for diverse public voices to be expressed and embedded in the development of solutions. Establishing transparency as a key practice will be crucial to build and sustain trust.
- Data policy for the digital age: The data policy environment (including access, privacy, ethics, and security) must be re-invented for the digital age, reimagining traditional consent and custodianship models to be effective, efficient and equitable in a networked health data ecosystem.
- Accountable alliances: Commitment from all levels of government is necessary to take action, with clear accountability for leadership, governance, and incentives to establish and sustain alliances and political will.
- Data interoperability and architecture: With advances in technology, adopting approaches that foster integrated real-time data access are essential to optimize quality health care, public health, policy, and research.
Common principles will guide the path to develop and implement the strategy
Several principles should guide development of the strategy:
- Respect First Nations, Inuit, and Métis data sovereignty and uncover and address structured health inequities experienced by First Nations, Inuit, and Métis peoples across geographies.
- Be co-developed by provincial, territorial, and federal jurisdictions.
- Respect and encompass diversity, equity and human rights.
- Be transparent, inclusive, and written in plain language.
The implementation of the strategy will:
- Put the public at the centre of governance, policy, and architecture.
- Build on strengths of jurisdictional developments, similarities, and differences; focus on consistency where it has significant impact and matters most.
- Prioritize sustainable mutual value, delivering early wins while focusing on long-term stretch goals.
- Challenge the status quo and address systemic data obstacles.
- Adopt leading international, domestic, and regional data principles, best practices, and standards.
- Actively adapt to emerging trends and be prepared for future change.
- Drive a disciplined approach that finishes what is started.
- Enable data-driven, collaborative, and cooperative culture with capacity to deliver.
- Promote equity, diversity, and inclusion, particularly for First Nations, Inuit, and Métis peoples across geographies, racialized minorities and marginalized populations.
- Be continuously optimized and evergreen - preferring timely good solutions that can be improved.
Conclusion: A Path Forward
Canada is losing ground when compared with peer countries in health. Better use of health data assets will deliver quality timely care, world-leading research, and strengthen health promotion and prevention.
This report is intended to raise awareness and visibility of the imperative for a cohesive pan-Canadian approach to health data for the benefit of Canadians. The report has described the opportunities in a revitalized approach and the costs of the status-quo.
Over the next several months, the EAG will deliberate on specific advice for the pCHDS. This will include gaining a more detailed understanding of the current state of the health data ecosystem and elaborating a future state by learning from leading approaches in other countries and across Canada. A second report from the EAG is planned for late fall 2021.
In parallel, the Public Health Agency of Canada is acting as the secretariat for this initiative with the broad scope as described above. The overall objective is to co-develop and recommend a practical implementation plan and roadmap with federal, provincial, and territorial governments by winter 2022.
The implementation plan and roadmap would be informed by EAG advice and broad stakeholder engagements which will be held over the summer and fall 2021. Engagements will focus on elaborating the health data foundation and approaches to overcome systemic obstacles to advancing the protected use of health data for individual and public good.
Related information
Contact
To contact the secretariat directly:
Email: pchds-spcds@phac-aspc.gc.ca
Footnotes
- Footnote 1
-
https://www.commonwealthfund.org/publications/surveys/2019/dec/2019-commonwealth-fund-international-health-policy-survey-primary
- Footnote 2
-
https://www.canada.ca/en/public-health/corporate/mandate/about-agency/external-advisory-bodies/list/pan-canadian-health-data-strategy-overview.html
- Footnote 3
-
Can include transfers from federal government to provinces and territories; and from jurisdictional governments to regions, health organizations and providers, and with vendors of systems.
- Footnote 4
-
Institutes of Medicine, https://www.ahrq.gov/patient-safety/quality-resources