The Chief Public Health Officer's Report on the State of Public Health in Canada 2013 – Sexually transmitted infections – A continued public health concern
Sexually Transmitted Infections–A Continued Public Health Concern
Highlights
- Sexually transmitted infections are a significant and increasing public health concern in Canada and worldwide.
- In Canada, reported rates of chlamydia, gonorrhea and syphilis have been steadily rising since the late 1990s.
- Young Canadians have the highest reported rates of sexually transmitted infections; however, increasing numbers of cases are being reported among middle-aged and older adults.
- Untreated sexually transmitted infections can have long-term health outcomes.
- Preventing and reducing the spread and impact of infection involves individual and broader commitments.
Sexually transmitted infections are preventable but continue to be a significant public health issue in Canada.Footnote 1 Reported rates of chlamydia, gonorrhea and infectious syphilis have been rising since the late 1990s, and this trend is expected to continue.Footnote 1 While the majority of reported chlamydia and gonorrhea cases continue to be among younger Canadians, reported rates of infections have increased significantly among middle-aged and older adults.Footnote 1 If left untreated some STIs can have long-term health outcomes.Footnote 2, Footnote 3 Since STIs are preventable, public health opportunities to reduce and manage the transmission of infection do exist.
STIs in Canada–an ongoing presence
Sexually transmitted infections (STIs) are spread primarily through direct person-to-person sexual contact; however, some infections such as HIV and syphilis can be transmitted with other forms of contact such as from mother to child during pregnancy and birth.Footnote 4 Bloodborne infections are spread by contact with blood or other body fluids contaminated with blood from an infected person.Footnote 5
Rates of STIs reported to the Canadian Notifiable Disease Surveillance System (CNDSS) have increased since 1997.Footnote 1 It is unclear whether these increasing rates are a result of actual increase in the number of people with STIs or because of changes in diagnosing and reporting procedures (see the textbox "Monitoring infections in Canada").Footnote 6 Regardless, STIs remain a public health concern. In 2008, 70% of the 161,592 cases of notifiable diseases reported by the CNDSS were sexually transmitted and bloodborne infections.Footnote 6 In particular, chlamydia accounted for 51% of all cases of notifiable infectious diseases reported.Footnote 6 These trends are comparable to those observed in other similarly developed countries such as the United States, Australia and the United Kingdom.Footnote 1
Monitoring infections in Canada
Surveillance is the ongoing and timely systematic collection, analysis and interpretation of data essential to public health practice. The occurrences of infectious diseases that are deemed important (by the Advisory Committee on Epidemiology) need to be reported to public health officials.Footnote 7 The reporting of notifiable diseases is mandated by provinces and territories and is voluntarily reported to the CNDSS. The list of reported notifiable diseases is agreed upon by consensus among provincial, territorial and federal health officials against specified criteria.Footnote 1, Footnote 7
Canada monitors a range of STIs through the CNDSS. Some STIs have been tracked for many years while others are more recent additions. For example, gonorrhea and infectious syphilis have been nationally notifiable infectious diseases since 1924 while chlamydia has only been a notifiable disease since 1990.Footnote 1 Other STIs, such as herpes and human papillomavirus (HPV) are not nationally reported.Footnote 1
The number of STI cases reported to the CNDSS, and the population rates calculated as a result, do not account for all infections in the population.Footnote 8 For example, an infected individual may not show symptoms and thus may not be tested and recorded.Footnote 8 In addition, since women tend to interact more frequently with the healthcare system, they are more likely than men to be screened or to seek treatment for STIs.Footnote 9 This may partly explain why more infections are diagnosed and reported among women than among men. Changes in rates over time must also be interpreted cautiously because they are subject to changes in both screening practices and laboratory technology and diagnostic capabilities. In addition, when the number of cases is very small the rates are more prone to fluctuations over time.Footnote 1
Chlamydia
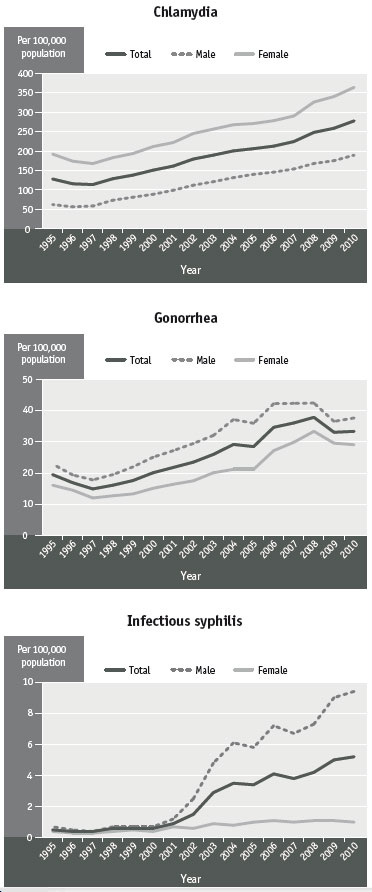
Figure 1 Reported rates of chlamydia, gonorrhea and infectious syphilis by sex, Canada, 1995 to 2010Footnote 1
Text Equivalent - Figure 1
| Year | Chlamydia | Gonorrhea | Infectious syphilis | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | Total | Male | Female | |
| 1995 | 128.2 | 62.6 | 192.2 | 19.5 | 22.9 | 16.1 | 0.5 | 0.7 | 0.4 |
| 1996 | 115.9 | 56.6 | 174.0 | 16.9 | 19.4 | 14.5 | 0.4 | 0.5 | 0.3 |
| 1997 | 113.9 | 58.7 | 167.8 | 14.9 | 17.8 | 12.0 | 0.4 | 0.4 | 0.3 |
| 1998 | 129.0 | 73.7 | 183.1 | 16.1 | 19.5 | 12.7 | 0.6 | 0.7 | 0.4 |
| 1999 | 138.2 | 81.4 | 193.6 | 17.6 | 22.0 | 13.3 | 0.6 | 0.7 | 0.5 |
| 2000 | 150.9 | 88.9 | 211.6 | 20.1 | 25.1 | 15.1 | 0.6 | 0.7 | 0.4 |
| 2001 | 161.4 | 99.2 | 221.9 | 21.8 | 27.2 | 16.4 | 0.9 | 1.2 | 0.7 |
| 2002 | 179.5 | 112.3 | 245.1 | 23.5 | 29.5 | 17.5 | 1.5 | 2.5 | 0.6 |
| 2003 | 189.6 | 121.3 | 256.5 | 26.0 | 32.1 | 20.1 | 2.9 | 4.8 | 0.9 |
| 2004 | 200.5 | 131.8 | 267.7 | 29.2 | 37.2 | 21.2 | 3.5 | 6.1 | 0.8 |
| 2005 | 206.2 | 140.2 | 270.8 | 28.5 | 36.0 | 21.2 | 3.4 | 5.8 | 1.0 |
| 2006 | 212.7 | 145.8 | 278.1 | 34.7 | 42.3 | 27.2 | 4.1 | 7.2 | 1.1 |
| 2007 | 224.4 | 154.0 | 290.1 | 36.1 | 42.4 | 29.9 | 3.8 | 6.7 | 1.0 |
| 2008 | 248.0 | 168.1 | 326.0 | 37.9 | 42.5 | 33.4 | 4.2 | 7.3 | 1.1 |
| 2009 | 258.6 | 175.3 | 340.1 | 33.1 | 36.6 | 29.6 | 5.0 | 9.0 | 1.1 |
| 2010 | 277.6 | 189.5 | 363.8 | 33.4 | 37.7 | 29.1 | 5.2 | 9.4 | 1.0 |
Chlamydia, an infection caused by the bacterium Chlamydia trachomatis, is the most commonly reported bacterial STI in Canada.Footnote 1 Infection with chlamydia is frequently asymptomatic. In the absence of screening, a lack of symptoms can increase the risk of unknowingly spreading the disease as well the risk of longer-term health implications for infected individuals. Nationally reported chlamydia rates have increased each year since 1997, resulting in a relative increase of 72% between 2001 (161.4 per 100,000) and 2010 (277.6 per 100,000) (see Figure 1).Footnote 1 In 2010, 94,690 cases of chlamydia infection were reported in Canada.Footnote 1
Common in both men and women, infections that are detected and reported (usually by screening people with no symptoms) disproportionately affect younger people, particularly women.Footnote 1 Between 2001 and 2010, reported rates of chlamydia infection increased for both men (91% from 99.2 to 189.5 per 100,000) and women (64% from 221.9 to 363.8 per 100,000).Footnote 1 In 2010, young women between 20 and 24 years old had the highest reported rate of chlamydia infections (2,005.5 cases per 100,000 population), more than seven times the overall national rate (277.6 cases per 100,000) and more than five times the overall rate for females (363.8 cases per 100,000 population).Footnote 1
Most strains of chlamydia are laboratory diagnosed and are treatable with antibiotics. Longer-term complications of untreated chlamydia for women include pelvic inflammatory disease, which can lead to chronic pelvic pain, ectopic pregnancy and infertility.Footnote 1, Footnote 3, Footnote 10 If left untreated, pregnant women can transmit chlamydia to their infants during childbirth which may result in neonatal conjunctivitis (infection of eyelid), pneumonia and reinfection.Footnote 1, Footnote 3, Footnote 10, Footnote 11 Although complications of chlamydia are less common in men, they can experience health outcomes such as epididymoorchitis (a penile or testicular disorder) as a result.Footnote 1, Footnote 3
Gonorrhea
Gonorrhea, an infection caused by the bacterium Neisseria gonorrhoeae, is the second most commonly reported bacterial STI in Canada.Footnote 1 In 2010, the highest rates of reported gonococcal infections (147.0 cases per 100,000 population) were among young women between 15 and 19 years old.Footnote 1 Reported rates among this young female population were more than four times the overall national average (33.4 cases per 100,000 population).Footnote 1 Reported rates of gonorrhea have also steadily increased over time–with an overall increase of 53.4% from 2001 to 2010 (see Figure 1).Footnote 1 However, during this same period of time, increases and advancements in diagnostic and screening practices have also influenced the effectiveness of reporting this disease.Footnote 1
Untreated gonorrhea infections can lead to complications for both men and women. Health outcomes for women include pelvic inflammatory disease, infertility and ectopic pregnancy.Footnote 1, Footnote 3, Footnote 10 Although uncommon, gonorrhea can also infect the blood stream and joints. Footnote 1, Footnote 2 While gonorrhea is usually curable with antibiotics, resistance to treatment is on the rise (see "Antimicrobial Resistance–A Shared Responsibility").Footnote 12-Footnote 15 Over the last 30 years, strains of gonorrhea have become less susceptible to certain treatments such as penicillin, erythromycin and tetracycline.Footnote 1, Footnote 2 Resistance to cephalosporins has recently been observed and which is of concern to public health practitioners.Footnote 1, Footnote 2
Infectious syphilis
Syphilis is an infection caused by the bacterium Treponema pallidum.Footnote 1 If left untreated, syphilis will progress through stages of infection referred to as primary, secondary and early latent stages. If syphilis remains untreated, it will progress to the late latent phase, which while not infectious, may lead to serious complications including damage to the central nervous system, cardiovascular system, eyes, skin and other internal organs.Footnote 1, Footnote 2 Only infectious syphilis is nationally reported.Footnote 1
From 1993 to 2000, reported rates of infectious syphilis were relatively stable but in 2001, the rates began to sharply increase (see Figure 1).Footnote 1 For the next 10 years, reported syphilis rates increased 456.7% (from 0.9 to 5.2 per 100,000).Footnote 1 In 2010, 1,757 cases of infectious syphilis were reported with an overall population rate of 5.2 per 100,000. In the same year, reported rates were higher in males than in females in all age groups.Footnote 1 In particular, young men between 30 and 39 years had the highest reported rate with 16.2 cases per 100,000 population, more than three times the overall national average.Footnote 1 Dramatic increase in syphilis incidence has been most notable among men who have sex with men (MSM).Footnote 1, Footnote 16 Co-infection of syphilis among those who are HIV positive is increasing.Footnote 1, Footnote 16 Syphilis infection can increase vulnerability to HIV and with associated neurological outcomes.Footnote 1, Footnote 17, Footnote 18 Reported rates of congenital syphilis, where the bacterium is transmitted from an infected mother to her fetus, is very infrequent in Canada.Footnote 1, Footnote 19 The impact on the fetus can be significant, and sometimes even fatal.Footnote 19
Human immunodeficiency virus
Human immunodeficiency virus (HIV) attacks the immune system and can develop into a chronic progressive illness that can make an individual vulnerable to other infections and to chronic diseases.Footnote 20 HIV is transmitted from one person to another through blood or body fluids during unprotected sexual intercourse or by sharing or using unsterilized needles. An HIV-infected mother can also transmit the virus to her infant during pregnancy, delivery or breastfeeding if she is not taking antiretroviral medication.Footnote 20, Footnote 21
In 2011, there were an estimated 3,175 new HIV infections reported in Canada.Footnote 22 This number has remained relatively stable since 2008 (being slightly less than the 2008 estimate).Footnote 22 Some sub-populations, such as MSM (46.6% of new infections) and intravenous drug users (13.7%), disproportionately account for these estimated new HIV infections.Footnote 22 The rate among people originating from HIV-endemic countries is about nine times higher than that in the Canadian-born population.Footnote 22
The Public Health Agency of Canada estimates that 71,300 Canadians were living with HIV infection (including AIDS) in 2011, an 11.4% increase from the 2008 estimate of 64,000.Footnote 22 The number of Canadians living with HIV is increasing, in part because new infections continue to occur and in part because fewer people are dying prematurely as a result of the disease due to the availability of effective antiretroviral treatments.Footnote 22 It is estimated, however, that 25% of Canadians infected with HIV, or 17,980 people, are unaware of their infection and thus not seeking treatment; they may also be unknowingly infecting others.Footnote 22 Having an STI such as chlamydia or syphilis can increase the risk of HIV transmission and infection.Footnote 1, Footnote 16, Footnote 17
Data limitations and sub-populations
Data on other STIs, such as herpes and HPV, are not collected through national surveillance. HPV is estimated to be one of the most common STIs and more than 70% of sexually active Canadians (both men and women) are estimated to have a sexually transmitted HPV infection at some time over their lifecourse.Footnote 2 Most people have no symptoms and the infections disappear without treatment.Footnote 23 In cases where HPV infections persist the infections can lead to genital warts or cervical, penile and other types of cancer.Footnote 1, Footnote 23 In fact, HPV is the cause of almost all cervical and most anal cancers.Footnote 24 Young adults are most at risk for contracting HPV, and the prevalence among this population is expected to increase over time.Footnote 1 Women younger than 25 years old are more likely to test positively for oncogenic (potentially cancer-causing) HPV than are women over this age.Footnote 25, Footnote 26
STI data for sub-populations tend to be limited and underreported, making it difficult to address health issues associated with these STIs. Laboratory-confirmed cases of STIs inconsistently report on demographic factors such as ethnicity. For example, First Nations, Inuit and Métis may be only broadly identified as Aboriginal.Footnote 27, Footnote 28 Sub-population data may be older data than those available for the overall population and therefore not comparable. As well, testing methods have changed over time, making results non-comparable across time (particularly with regard to infections such as HPV). Regardless of these data limitations, some sub-populations are thought to be at increased risk of certain STIs:
- STI prevalence among Aboriginal persons is estimated to be higher than that of the overall population.Footnote 28, Footnote 29 In particular, chlamydia is estimated to be almost seven times higher among First Nation adults than the rate of the overall population.Footnote 28 Rates of HIV and AIDS are also disproportionately higher among Aboriginal persons, and new HIV infections are occurring at a rate that is estimated to be 3.5 times higher than that of the non-Aboriginal population.Footnote 22
- Recent immigrant populations underuse the healthcare system, and therefore, there are fewer opportunities for routine screening and treatment.Footnote 2 Citizenship and Immigration Canada tests individuals 15 years of age and older for syphilis and HIV upon entry into Canada.Footnote 2, Footnote 30
- A proportion of Canada's incarcerated populations may be from vulnerable populations where risk behaviours (e.g. intravenous drug use and unprotected sex) are present. As a result, disproportionately high rates of sexually transmitted and bloodborne infections, including HIV and hepatitis B (HBV) and hepatitis C (HCV), prevail.Footnote 2
- Among sexual minorities, particularly MSM, the prevalence of STIs has fluctuated over time. Within the last decade, outbreaks of syphilis have been reported among MSM, with a large proportion also co-infected with HIV and lymphogranuloma venerum (infection caused by certain strains of Chlamydia trachomatis).Footnote 2, Footnote 16, Footnote 31-Footnote 35 Co-infection is an ongoing public health concern as syphilis and other STIs can increase the likelihood of transmitting and acquiring HIV as well as other infectious and chronic illnesses.Footnote 1, Footnote 16, Footnote 17
STIs such as HIV, syphilis and HPV have some long-term outcomes or can develop into chronic conditions.Footnote 2 Being vigilant about infectious disease is not just about primary prevention; disease also needs to be monitored and managed over the lifecourse to improve overall health, well-being and life expectancy. Increases in STI cases as well as increases in the numbers of people living with these infectious diseases chronically points to the need for programs that adapt to this reality.
Changing outcomes
Preventing STIs is the first step to reducing them. Preventing and managing STIs is both an individual and community responsibility. Prevention typically focuses on individuals; however, broader structural interventions include a combination of education and awareness, biomedical interventions (e.g. immunization, medical research and screening programs) and population-based interventions such as those that invest in the determinants of health and related factors, for example, education, income, housing, mental health and anti-stigma programs.Footnote 36 Efforts are being made in these areas at all levels and jurisdictions (see the textbox "Prevention and control strategies").
Prevention and control strategies
The World Health Organization (WHO) suggests that efforts to control the spread of STIs have waned despite increasing global rates. Preventing and managing STIs and related health outcomes are linked and need to be part of broader, more comprehensive sexual and reproductive health services. The WHO's Global strategy for the prevention and control of sexually transmitted infections: 2006-2015 was designed with technical and advocacy components in mind. The technical portion of the strategy focuses on practice of promoting healthy sexual behaviour and providing effective and accessible care for STI patients, and the upgrading of monitoring and evaluation of STI control.Footnote 36 Canada is a signatory on the WHO global strategy.Footnote 2
The Canadian Guidelines on Sexually Transmitted Infections is a collaborative effort involving expert input from medicine, nursing, laboratories and public health to create evidence-based recommendations for preventing, diagnosing, treating and managing STIs in Canada.Footnote 2 The guidelines emphasize the need for collaboration efforts to have greatest impact on those at greatest risk of STIs. In addition, many recommendations focus on the role of healthcare providers and the need to provide a continuum of services including patient-centred STI screening, diagnosis and treatment options that also address longer-term chronic conditions.Footnote 2
Individual responsibility
Many factors can influence individual risk behaviours. Risk reduction strategies range from abstinence; limiting sexual relations to long-term and monogamous partners; condom use; and sharing information on sexual history with partners. Seeking testing and treatment (where necessary) for sexually transmitted and bloodborne infections is also key to reducing risk of infection.Footnote 2, Footnote 4
Increasing awareness and education interventions
A variety of sexual health education interventions target youth and young adults. Comprehensive in-school educational programs can be effective in changing youth behaviours when programs combine learning about sexual risk and protection with non-sexual factors such as building healthy relationships.Footnote 37, Footnote 38 Programs that address diversity (e.g. location, age, sex and gender, sexual orientation and culture) and provide access to health services can be more effective.Footnote 37 For example, in-school educational programs often focus on needs of girls. However, those programs that engage boys and encourage open discussions about sexual health are effective at building more respectful relationships among youth.Footnote 39, Footnote 40
Despite increases in STIs among older adults, broad awareness campaigns tend to target youth and have not been widely used with older populations.Footnote 1, Footnote 41-Footnote 44 All members of the community, regardless of age, benefit from sexual education combined with programs such as clinical services, counselling and social services. However, negative perceptions about older adults' sexuality persist, and stigma, embarrassment and discrimination can create barriers for older adults to discuss sexual health with their healthcare providers.Footnote 41, Footnote 42, Footnote 45 General practitioners also report being reluctant to discuss sex and STIs with older (particularly female) patients.Footnote 42, Footnote 45, Footnote 46
Biomedical and management interventions
Primary care is necessary for the diagnosis and clinical management of infection. The Canadian Guidelines on Sexually Transmitted Infections highlight how important it is for public health practitioners to recognize individual STI risks and how these risks differ among individuals and across the lifecourse.Footnote 2 Healthcare providers can incorporate STI prevention into routine patient care by assessing and discussing their individual STI risks and how to minimize risks and recognize symptoms (if any). They should also offer patient-centred counselling about STI treatment and management as well as counselling on partner notification.Footnote 2 STI screening is important; however, use of tests is often based on patient history and known risk factors as well as symptoms. Patients are frequently reluctant to undergo screening, believing that STI screening is unnecessary because of previous negative results or being under the impression that routine physicals and blood tests include STI screening.Footnote 2
Immunization can be used to prevent and control spread of infection including STIs (e.g. HPV, hepatitis and emerging vaccines for HIV and herpes simplex virus).Footnote 47 For example, the quadrivalent HPV vaccine protects against four types of HPV infections that can have known and significant health issues.Footnote 25 Generally, HPV is administered in three doses prior to sexual debut to maximize protective benefit; however, it is also being administered to women later in life.Footnote 25, Footnote 48 While there are a number of HPV strains, two vaccines have been developed to protect against the highest risk types of HPV that are associated with cancers.Footnote 1 Vaccine-preventable strains of HPV were found in 70.2% of these cervical cancer test cases.Footnote 49 By 2008, all provinces and territories had introduced HPV vaccinations for girls as part of their routine immunization.Footnote 25 In 2012, the National Advisory Committee on Immunization extended the recommended use of the HPV vaccine to include older females (up to 45 years old) and young males (9 to 26 years).Footnote 25 Future evaluations will need to measure how the vaccine affects men, women and various at-risk sub-populations as well as the long-term effectiveness in reducing incidence of related cancers.
Advancements in treatment have helped increase life expectancy for people living with HIV and may play a role in decreasing onward transmission of the virus. Antiretroviral therapies (ART) started to be used in the 1990s and continue to significantly change the way HIV affects the short- and long-term health of infected individuals. ARTs reduce the replication of HIV, allowing an individual's immune system to rebuild so as to fight disease.Footnote 20, Footnote 21 The near-elimination of mother-to-child HIV transmission and investment in a safe blood supply have been important advances in the HIV response.Footnote 20, Footnote 21
Under-diagnosis due to asymptomatic characteristics and limited testing influence available data on incidence and prevalence of STIs in Canada.Footnote 1, Footnote 8 Provinces and territories collect physician data, where available, and report these nationally.Footnote 1 However, there are differences between federal and provincial/territorial reporting structures, data elements and reportable infections.Footnote 1, Footnote 7, Footnote 8 National data and trends inform public health guidelines and policies; as numbers increase, so does the need for broad interventions and policies that address serious public health problems. Regardless, some STIs, such as HPV and herpes simplex, are not subject to the same systematic surveillance.Footnote 1 As a result, less is known about the burden of these infections.Footnote 1
Addressing the broader determinants of health
Making upstream investments in the health and social conditions that influence overall health outcomes can significantly reduce rates of STIs, their long-term health impacts and risk of comorbidities. Having an income, a place to live and social support can make a difference to health. For example, street-involved youth have higher rates of STIs and greater susceptibility to HBV and HCV infections than youth in the overall population.Footnote 50-Footnote 53 At some point in their lives, many street involved youth have reported experiencing abuse and neglect; being involved in child welfare; a mental illness; inadequate income or housing; or lack of employment, parental support or income.Footnote 53, Footnote 54 Addressing determinants of health could have long term impacts for those vulnerable youth. Research indicates that there is a relationship between risky sexual behaviour and residential stability, and HIV risk behaviours decrease with residential stability.Footnote 54 Programs such as the Housing First approach and Canada's At Home/Chez Soi provide housing as the building block to reducing risks to health.Footnote 55
Living with infections such as HIV can increase the risk of comorbidity over time. In general, individuals who can access health and social services have better health outcomes and as a result are less likely to develop additional illness (or comorbidities). There is a growing recognition among healthcare professionals of the importance of integrating services among the chronic infectious diseases such as HIV, HBV and HCV and channelling efforts where there are common risk factors.Footnote 21 In recognition of the common transmission routes, risk behaviours and socio-economic risk factors that affect transmission of these infections, those involved in the response are increasingly taking an integrated, holistic approach to prevention, care, treatment and support.Footnote 56
Stigma for any reason–a health issue, culture, gender, sexual orientation–can negatively affect an individual's ability to develop holistically, socialize, go to school, work and volunteer, and seek care and treatment.Footnote 21, Footnote 57, Footnote 58 Stigma associated with sexually transmitted and bloodborne infections can lead people to avoid testing, treatment and talking about their health status with sexual partners. In addition, some people living with HIV or AIDS experience "stigma layering" because the stigma associated with HIV as well as other co-infections (e.g. HCV) is added to the stigma of having HIV or belonging to certain population groups (e.g. racial, ethnic or sexual minorities or people who inject drugs).Footnote 59 Having support networks and access to services can contribute to positive health outcomes.Footnote 21, Footnote 60
Actions for success
Despite broad efforts to prevent, diagnose and treat STIs, reported rates continue be a health concern in Canada. Not only are increasing rates a concern but so too are the longer-term impacts. If STIs are left untreated, serious health effects may ensue. Making a difference to reduce incidence and impacts will involve changing perspectives, being vigilant and looking at disease beyond the point of infection. All Canadians can make individual and collective efforts to protect, prevent and manage the impact of STIs.
- Preventing and managing STIs is both an individual and community responsibility.
- Canadians must be vigilant about STIs before and after the point of infection.
- Healthcare professionals can provide patient-centred services, counselling and treatment.
- Canada can continue to improve STI screening and surveillance and can increase reporting on specific populations.
- Canada can continue to contribute to global reduction of STIs through research and development.
Page details
- Date modified: