Full report: The Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2023
Download in PDF format
(3,342 KB, 112 pages)
Organization: Public Health Agency of Canada
Date published: 2023-10-24
Cat.: HP2-10E-PDF
ISBN: 1924-7087
Pub.: 230270
On this page
- Message from the Chief Public Health Officer of Canada
- About this report
- Introduction
- Section 1: Emergencies and population health
- Section 2: Emergency management systems in Canada
- Section 3: A health promotion approach to emergency management
- Section 4: Applying health promotion actions to the emergency management continuum
- Way forward
- Appendix A: Key health promotion tools for emergency management procedures
- Appendix B: An update on COVID-19 in Canada
- Appendix C: Methodology
- Acknowledgements
- References
Message from the Chief Public Health Officer of Canada
In recent years, our communities have faced monumental challenges, from the scale and scope of the COVID-19 pandemic to more frequent extreme weather events driven by climate change.
Emergencies are increasingly becoming a part of our daily lives, both here in Canada and around the world. In the past year alone, we have witnessed record heat waves, devastating floods, and an unprecedented wildfire season that has affected the air we breathe and forced the evacuation of thousands of people in communities across the country.
These events can have profound impacts on our physical and mental health, as well as on the well-being of our communities. In some cases, recovery from one emergency may not even be possible before another one hits. Emergency response is becoming more complex and more challenging.
In this report, I explore how public health can work with communities and partners across sectors to build healthier and more resilient communities. When communities are more resilient, we are better equipped to prevent, withstand, and recover from emergencies. Just as strengthening our physical infrastructure is important for emergency preparedness, such as reinforcing power grids, we must also invest in our social infrastructure to ensure strong community supports are in place for times of crisis.
Some communities are disproportionately affected by emergencies
The impacts of emergencies are not the same for everyone. Some populations are at greater risk of exposure and poor health outcomes because of pre-existing social, economic, environmental, or health inequities, including those related to racism, discrimination, and colonization. For example, people experiencing homelessness, populations that are racialized, and people living with mental health conditions or substance use disorders experienced more negative health impacts from the COVID-19 pandemic, with worse outcomes for those facing multiple and overlapping barriers to good health.
Likewise, First Nations, Inuit, and Métis communities have been disproportionately affected by climate-related emergencies, such as wildfires and floods. These events do not just damage property, they destroy homes, livelihoods, and shared community spaces and culture that are an integral part of community resilience and are key determinants of health.
I am calling for us to reflect on and reset how we think about emergencies. We need to look beyond the immediate response and work on the foundational conditions that keep our communities healthy and strong.
Health promotion can strengthen emergency management
A growing focus on community resilience is already part of emergency management efforts. Public health has an important role to play and can bring existing tools to support this work.
Health promotion, an essential public health function, provides ways to work with communities and partners to advance health equity, strengthen social supports, and build trusted relationships that can foster social cohesion. These are all essential for an effective response to emergencies as well as other public health crises, such as the current toxic drug crisis. Health promotion can also support partnerships with First Nations, Inuit, and Métis leadership and Indigenous-led approaches, while honouring our commitments to broader reconciliation efforts.
The COVID-19 pandemic showed us that we have to do better. We saw the inequitable impacts. We listened and learned about the barriers faced by communities and how we can effectively address them. We achieved more when we worked across sectors to bring our collective expertise and tools to the table and supported trusted community organizations to reach diverse populations.
Now is the time to apply these lessons to emergency management. We can do this by integrating health promotion into emergency management plans and ensuring that communities are prioritized in all aspects of the planning cycle, from prevention to recovery. We must also put equity at the core of emergency management science, evidence, and technology.
If we take these steps, Canada can be at the forefront of international health promotion efforts. Fifty years ago, the Lalonde Report helped to spur a paradigm shift in how we think about health in Canada, beyond just health care and treatments, to include the social and economic conditions in which we live, work, and play. We have to move forward with this legacy if we want to succeed in building a stronger and more equitable society that prioritizes safety and well-being before, during, and after emergencies.
Dr. Theresa Tam
Canada's Chief Public Health Officer
About this report
Each year, the Chief Public Health Officer of Canada (CPHO) writes a report on the state of public health in Canada. These reports are intended to highlight important public health issues, spark discussion, and support action to improve population health and the conditions of health. This year's annual report explores the inequitable health impacts of emergencies. It highlights opportunities for public health to contribute to emergency management through the essential public health functions, particularly health promotion approaches that can support equity and resilience.
A key objective of this report is to ensure better health security by including critical health promotion capabilities and capacities in emergency management plans and activities. If systematically integrated, health promotion can help communities to be more resilient, increase social connections and cohesion, and foster trust amongst communities, response partners, and decision makers.
The report builds on previous CPHO reports that detailed the inequitable risks and impacts of climate change and infectious disease emergencies. It also continues the conversation from the 2021 CPHO report on public health transformation, with the goal of optimizing existing public health skills and capacities to best support the health and well-being of all people living in Canada.
Orientation of the report
Section 1 explores the rise in emergency frequency and intensity, the different types of hazards that can lead to emergencies in Canada, and the inequitable population impacts of emergencies. By describing the growing risk of emergencies, as well as their widespread and differential consequences, this section details why emergencies are a public health priority.
Section 2 summarizes how we address emergencies in Canada, including governance structures, key documents guiding emergency management, and emergency management with First Nations, Inuit, and Métis communities. This section outlines emergency management as an essential public health function.
Section 3 describes how health promotion, which is another essential public health function, can contribute to emergency management. This includes the key action areas of building healthy public policy, creating supportive environments, and strengthening community action. This section also explores considerations for the use of health promotion approaches with First Nations, Inuit, and Métis communities.
Section 4 details specific opportunities to apply health promotion approaches to emergency management, spanning the different components of prevention and mitigation, preparedness, response, and recovery. This includes summaries of available research evidence, examples of relevant tools, and applied case studies from across Canada.
The Way forward outlines tangible actions to bring health promotion into emergency management policies and practice.
Appendix A provides select examples of key health promotion tools and approaches that may be applicable for emergency management procedures.
Appendix B gives a brief update on the COVID-19 pandemic in Canada between August 2022 and August 2023. This includes epidemiological trends, the continuing impact on people and healthcare systems, and the ongoing long-term management of COVID-19.
In addition to research evidence, including rapid reviews completed by the National Collaborating Centre for Methods and Tools as well as the COVID-19 Evidence Network to Support Decision-making (COVID-END), this report includes quotes from discussions with public health experts and community organizations. Further details on the methods and limitations are provided in Appendix C.
A key mechanism to action the report's recommendations is through the generation of new knowledge. Generating Knowledge for a Health Promotion Approach to Emergencies is a companion resource that outlines priority knowledge gaps and research needs. The objectives are to bridge the science-to-policy divide, catalyze collective scientific activity, and provide the evidence base needed to support the application of a health promotion approach to emergencies in Canada. These priorities are geared toward a broad audience, including individual researchers, organizations, funding agencies, and others wishing to mobilize research and knowledge on this important topic.
Health of people in Canada dashboard
Previous CPHO reports have included key indicators on the health of people living in Canada. These data are now included in an interactive online dashboard. The CPHO message that accompanies the dashboard provides a high-level overview of current population trends. All dashboard information will be periodically updated.
Land acknowledgement
We respectfully acknowledge that the lands on which we developed this report are the homelands of First Nations, Inuit, and Métis Peoples. Specifically, this report was developed in the following cities:
- In Ottawa, also known as Adawe, on the traditional and unceded territory of the Algonquin People, members of the Anishinabek Nation Self-Government Agreement.
- In Halifax, also known as K'jipuktuk, a part of Mi'kma'ki, the ancestral and unceded territory of the Mi'kmaq People. This territory is covered by the "Treaties of Peace and Friendship" which Mi'kmaq and Wolastoqiyik (Maliseet), and Passamaquoddy Peoples signed between 1725 and 1779. The treaties did not deal with surrender of lands and resources but in fact recognized Mi'kmaq, Wolastoqiyik (Maliseet), and Passamaquoddy title and established the rules for what was to be an ongoing relationship of peace and friendship between nations.
- In Montreal, also known as Tiohti:áke, the traditional and unceded territory of the Kanien'kehá:ka. A place which has long served as a site of meeting and exchange amongst many First Nations, including the Kanien'kehá:ka of the Haudenosaunee Confederacy, Huron/Wendat, Abenaki, and Anishinaabeg.
- In Toronto, also known as Tkaronto, the traditional territory of many nations, including the Mississaugas of the Credit, the Anishnaabeg, the Chippewa, the Haudenosaunee, and the Wendat peoples and is now home to many diverse urban First Nations, Inuit, and Métis Peoples. Toronto is within the lands protected by the Dish with One Spoon Wampum Belt Covenant, an agreement between the Haudenosaunee and Anishinaabe and allied nations to peaceably share and care for the resources around the Great Lakes.
- Lastly, in Central Saanich, on Vancouver Island, the traditional territory of the SȾÁUTW̱ and W̱JOȽEȽP First Nations, 2 of the 5 communities that constitute the W̱SÁNEĆ Nation.
We recognize that there is much more work ahead to address the harmful impacts of colonialism and racism that continue to generate inequities between Indigenous and non-Indigenous communities. We remain strongly committed to working collaboratively to address health inequities across the country, create a culturally humble public health system, and support the self-determination of Indigenous communities.
Introduction
Emergencies have significant health, social, environmental, and economic impacts. The frequency and severity of emergencies in Canada are growing and it has become increasingly difficult for individuals, communities, and emergency management systems to respond to them.Footnote 1 This has necessitated a renewed focus on preventing emergencies and reducing their impacts, as well as growing attention to community resilience.
A resilient community, whether defined by geography, interest, experience, or identity, is one that has the resources to help prevent, withstand, and recover from emergencies. Resilient communities are able to adapt despite disturbances caused by emergencies and return to acceptable levels of functioning.Footnote 2 Further, the community attributes and systems that support emergency resilience could also contribute to broader social, economic, health, and environmental benefits before, during, and after emergencies.Footnote 1Footnote 3Footnote 4Footnote 5Footnote 6
However, some communities have less access to key conditions that enable resilience. This is due to the inequitable distribution of power and resources in society. During an emergency, some communities are more likely to be exposed to hazards and risk. These same communities may also have less access to the resources needed to respond to and recover from emergencies.Footnote 4Footnote 5Footnote 7 This can create compounding and inequitable negative health, social, and economic effects on individuals and their communities.
These inequitable impacts were evident throughout the COVID-19 pandemic. Many groups were disproportionately impacted by the pandemic, including essential workers, older adults, Indigenous Peoples, people experiencing homelessness, populations that are racialized, people with disabilities, and people with mental or substance use disorders.Footnote 8Footnote 9 Emphasizing a focus on equity within resilience efforts can help ensure that key resources, such as social and economic protections, safe and secure housing, and access to culturally safe health care, are fairly distributed across communities.
The emergency management sector has increasingly been shifting attention to emergency preparedness, as well as the prevention of emergencies and mitigation of impacts.Footnote 2Footnote 10 Public health systems are already implicated in this work through the essential public health function of emergency preparedness and response.
However, all essential public health functions could be used to further support emergency management. Insights and approaches from the field of health promotion are particularly relevant to preparedness, prevention, and resilience. Public health systems can support the application of health promotion by modeling its use within emergency management actions led by public health, as well as by bringing key aspects of health promotion, such as equity and community, whenever public health is involved in decision making across sectors.
Health promotion involves policy and program activities that support people and communities to improve health and its determinants.Footnote 11Footnote 12Footnote 13Footnote 14 Critically, it moves beyond a focus on individual behaviour towards a wide range of social, economic, and environmental interventions that support individual and collective health and well-being.Footnote 11Footnote 12Footnote 13Footnote 14
Emergencies often bring different communities and sectors together to meet a common goal, and a health promotion approach can help encourage ongoing collaboration. Health promotion prioritizes intersectoral approaches to strengthen population-level resilience by targeting the determinants that drive the inequitable impacts of emergencies.Footnote 11Footnote 15Footnote 16Footnote 17 With most emergencies happening at the local level, health promotion can also help strengthen resilience through a focus on community engagement and community-level action on the living conditions that shape health and well-being.Footnote 18
The relevance of health promotion for emergency management has been underlined by several key lessons from the COVID-19 pandemic and recent extreme weather events. Some of these lessons include:
- The increase in emergency frequency and intensity has made it difficult to effectively respond. Recognizing that not all emergencies are within our control, nevertheless, greater attention is needed on preventing emergencies, mitigating their impacts, and preparing for them. Doing so will require whole-of-society commitments, intersectoral collaboration, and a focus on resilience.Footnote 1Footnote 6Footnote 19
- Equity, justice, and human rights are essential considerations in emergency management.Footnote 8Footnote 20 Everyone has the right to be safe in the context of an emergency. This includes ensuring that all people have the opportunity and resources to follow guidance to protect themselves, and that they have access to culturally safe health and emergency services. As noted by the World Health Organization (WHO), a rights-based approach calls for the prioritization of the needs of those who are most disproportionately impacted.Footnote 21 There are a number of existing human rights instruments of relevance, including the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) which summarizes the rights of Indigenous Peoples.Footnote 22
- Communities are best positioned to understand their vulnerabilities in times of emergency and the specific needs of their members. Community engagement and leadership are therefore crucial for emergency preparedness, and to strengthen community resilience before, during, and after emergencies. Emergency management activities need to reflect and adapt to diverse community contexts, guided by community knowledge and leadership.Footnote 1Footnote 19Footnote 23
Ongoing COVID-19 recovery and reflection creates an opportunity to explore how all public health functions can be applied to support emergency management. In particular, it prompts consideration as to how health promotion and emergency management can be brought together more systematically to promote and protect health and well-being with communities, while optimizing existing public health resources and capacities. This report will show how public health systems can bring this integrated perspective as part of their contribution to emergency management initiatives more broadly.
Section 1: Emergencies and population health
Emergencies in Canada
Emergencies are growing in frequency and severity in Canada for multiple reasons.Footnote 1Footnote 2 Most notably, climate change is driving ecological changes and more frequent and extreme weather events, which cause injuries and death, damage homes and infrastructure, threaten the availability and safety of water and food, and enable the emergence and spread of infectious diseases.Footnote 7 The way we live has increased the potential for serious consequences during and after emergencies. A growing reliance on technology can create vulnerabilities, with widespread impacts when power grids are disrupted or electronic devices are disabled, including essential medical services.Footnote 24Footnote 25 As a result of increased urbanization, population growth and density, and globalization, there is also the potential for more people to be affected when an emergency happens.Footnote 26
All of the above lead to an increase in hazards and an increased likelihood of co-occurring emergencies (see Figure 1 for the difference between a hazard and an emergency). This can hinder capacity to respond and recover, and results in compounded and more severe impacts.Footnote 1Footnote 27Footnote 28 Hazards have the potential to impact health, safety, property, or the environment. An emergency or disaster occurs when a hazard results in serious and adverse consequences that exceed a community's ability to cope (e.g., flood). This can occur because of a vulnerability (e.g., housing built in low-lying areas). Actions across the emergency management continuum can reduce the occurrence or impact of emergencies by reducing the likelihood of a hazard or by preventing severe consequences.
"The environment has changed, we have hurricanes now. What used to be a simple 3 or 4 hour power outage now may be 3 or 4 days. The whole landscape is definitely changing, and we need to change with it."

Figure 1 - Text description
Figure 1: Text description
The figure describes distinctions between a hazard, emergency, and disaster. The figure also provides an example which demonstrates how a hazard could lead to an emergency, and eventually a disaster.
Hazard
- A hazard is a physical event, phenomenon, or human activity that has potential to cause damage, disruption, or loss. Hazards are often local in nature and may not require immediate attention.
- A hazard can lead to an emergency when it poses an immediate threat to health, safety, property, and/or the environment.
Emergency
- An emergency is a serious event requiring immediate action to protect the health and safety of people, and limit damage to property and the environment.
- The impacts of an emergency can be managed using available resources and response systems of the affected area (e.g., individual and community skills, materials, equipment, and services).
Disaster
- A disaster is a critical event that threatens or causes widespread and significant disruption to everyday life and essential functions, including injuries, displacement, damage, and human, economic, and environmental loss.
- The impacts of a disaster exceed the capacity of an affected area to withstand, respond, or recover with its existing resources, requiring external assistance.
- Disasters may be triggered by a naturally occurring phenomenon, or malicious or unintentional human action.
Note that the distinction between emergencies and disasters is subjective as the severity may vary.
The example describes heavy rainfall as a hazard, and the circumstances in which heavy rainfall could escalate to an emergency and eventually, a disaster.
Hazard: A prolonged period of heavy rainfall occurs in a region, causing water bodies to rise. This creates a hazard of potential flooding, posing a threat to low-lying areas and properties near water bodies.
Emergency: Heavy rains continue, and water levels rise rapidly, exceeding their banks and inundating nearby areas, property, and infrastructure. Local authorities in the affected area declare a state of emergency and activate emergency systems to respond to the impacts, protect residents, and mitigate further damage.
Disaster: Floodwaters continue to rise, leading to widespread and severe floods. Numerous communities are affected. Floodwater inundates homes, damages critical infrastructure, disrupts business operations, and causes loss of life, injuries, and significant displacement of residents. External assistance is required to support the immediate response and long-term recovery efforts.
Note, the term "emergency" will be used broadly throughout the report to refer to both emergencies and disasters.
More than 90% of emergencies in Canada are handled locally or at the provincial/territorial level.Footnote 31 Some emergencies, like the COVID-19 pandemic, require national or international emergency responses. In Canada, emergencies are generally categorized into 5 main types, each potentially caused by a wide range of hazards. Canada has experienced emergencies across these types, with select examples included in Figure 2.

Figure 2 - Text description
The figure describes 5 categories of hazards and provides examples from Canada for each. This includes:
Meteorological and hydrological hazards, such as avalanche, cold event, drought, flood, heat event, hurricane, storm surge, tornado, and wildfire. Examples of meteorological and hydrological emergencies in Canada include:
- A flood in Saguenay River Valley, QC (1996);
- An ice storm in Ontario, Quebec, and New Brunswick (1998);
- A wildfire in Fort McMurray, AB (2016);
- The heat dome in British Columbia and Alberta (2021); and,
- Hurricane Fiona in Quebec, New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador (2022).
Biological hazards, such as infectious and communicable diseases, food-borne illnesses, vector-borne diseases, water-borne illnesses, and zoonotic diseases. Examples of biological emergencies in Canada include:
- Flu pandemic, global (starting in 1918);
- A contaminated water supply in Walkerton, ON (2000);
- The SARS pandemic, global (2003);
- The H1N1 pandemic, global (2009); and,
- The COVID-19 pandemic, global (starting in 2020).
Geological hazards, such as earthquake, landslide, tsunami, and volcano. Examples of geological emergencies in Canada include:
- A landslide in Frank, AB (1903);
- A tsunami in the Burin Peninsula, NL (1929);
- An earthquake in Haida Gwaii, BC (1949);
- A landslide in Saint-Jean-Vianney, QC (1971); and,
- An earthquake in Val-des-Bois and Gracefield, QC (2010).
Conflict hazards, such as arson, civil incident, hijacking, and terrorist and cyber attacks. Examples of conflict emergencies in Canada include:
- A mass shooting at École Polytechnique in Montreal, QC (1989);
- A mass shooting at the Islamic Cultural Centre in Quebec City, QC (2017);
- A vehicle-ramming attack in Toronto, ON (2019);
- A mass shooting across multiple locations in Nova Scotia (2020); and,
- A mass stabbing in James Smith Cree Nation and Weldon, SK (2022).
Technological hazards, such as fire, explosion, hazardous chemicals, transportation accident, infrastructure failure, and space event. Examples of technological emergencies in Canada include:
- The Halifax Harbour explosion in Halifax, NS (1917);
- The Second Narrows Bridge collapse in Vancouver, BC (1958);
- The Northeast blackout affecting Ontario (2003);
- The train derailment in Lac-Mégantic, QC (2013); and,
- An oil spill in Gale Pass, BC (2016).
Infectious disease emergencies may have unique characteristics compared to other types of emergencies. They often occur on a different time scale (e.g., epidemics may have a slower onset but last longer than other events) and are not always tied to a specific physical location.Footnote 33 Since everyone may be simultaneously impacted across a large area during these emergencies, resources for response can become limited.Footnote 34Footnote 35 Additionally, stigma can be associated with infectious diseases. This can create barriers to, or hesitation about, accessing health care and contribute to difficulties implementing measures to reduce disease spread.Footnote 36Footnote 37Footnote 38 Despite these characteristics, there is sufficient overlap between infectious diseases and other types of hazards to take similar approaches to emergency management.Footnote 33
Other public health issues may be described using the language of emergencies, epidemics, or crises, such as opioid toxicity, mental health, suicide, homelessness, gender-based violence and intimate partner violence, or racism.Footnote 39Footnote 40Footnote 41Footnote 42Footnote 43Footnote 44 Crisis or emergency declarations related to these issues are intended to emphasize the urgency and severity of the issue. Such crises may be deemed social emergencies.Footnote 45Footnote 46 For example, to help define social emergencies, First Nations communities in Ontario, led by the Mushkegowuk Council, created a social emergency protocol.Footnote 45 As defined by the Nishnawbe Aski Nation, a social emergency is an event or situation which carries risk to human life or health, mental wellness, or to the social fabric and well-being of communities.Footnote 45 Like other emergencies, it exceeds the capacities and resources of a community, requiring immediate response and support from governments, external agencies, and service providers.Footnote 45
Unlike other emergencies, the declaration of a social emergency is not necessarily linked to additional resources to address the crisis.Footnote 45 Some have called for the elimination of the distinction between social emergencies and other types of emergency hazards, or for dedicated funding for social emergencies.Footnote 45 In some instances, such as the toxic drug crisis, additional resources have been allocated, and existing emergency strategies and structures have been adapted to help address the crisis.Footnote 39Footnote 47Footnote 48 While social emergencies are important public health priorities, they may not meet legislative definitions of an emergency and therefore are often not planned for as part of the formal emergency management structures that are discussed in this report.
Impacts of emergencies on population health
While emergencies can be caused by a variety of hazards, they often present similar challenges to health and well-being. Emergencies have direct and indirect impacts on health and the determinants and conditions that influence health, with the potential for both short- and long-term consequences (see Figure 3). The often widespread and severe health impacts of emergencies, and their inequitable distribution, underline why emergency management is a priority for public health.

Figure 3 - Text description
The figure lists a selection of emergencies that have occurred in Canada, and provides examples of the direct and indirect impacts on health associated with these emergencies. The examples provided do not cover the full range of impacts of each emergency.
COVID-19:
- As of August 2023, there have been more than 53,000 COVID-19 related deaths in Canada.
- From April 2021 to March 2022, the estimated total cost of hospital stays due to COVID-19 in Canada was about $2.9 billion.
- From March 2020 to September 2022, about 937,000 fewer surgeries were performed in Canada compared with before the pandemic.
Heat dome:
- The 2021 heat dome led to 619 heat-related deaths in British Columbia, many of which were among older adults who lived alone and whose health was compromised by multiple chronic conditions.
- Nearly 12,000 calls were made to 911 in one day in British Columbia, a new record and about double normal daily call volumes.
- There were 530 excess hospitalizations across British Columbia during the week of the heat dome.
Wildfire:
- Six months after the 2016 Fort McMurray, AB wildfire, 20% of residents surveyed met the criteria for generalized anxiety disorder.
- Approximately 579,767 hectares of land was burned causing the evacuation of over 90,000 people and destroying 8% of all private dwellings in the area.
- The wildfire was one of the most expensive emergencies in Canadian history with total costs reaching $4 billion in losses.
Train derailment:
- The 2013 train derailment and explosion in Lac-Mégantic, QC resulted in 47 deaths and the evacuation of one third of the local population.
- After the event, 67% of local survey participants reported moderate to severe symptoms of post-traumatic stress.
- The disaster was responsible for spilling 6 million litres of crude oil into the environment, contaminating surrounding waterways and soil.
Floods:
- Flooding in 2010-2011 caused the highest water levels and flows in modern history across parts of Manitoba and Saskatchewan. Governments at all levels spent nearly $1 billion on flood fighting and victim compensation.
- In Manitoba, the floods displaced 7,100 residents, primarily from First Nations communities. At the end of 2011, 2,700 evacuees were still displaced because homes were uninhabitable.
- During the flood, more than 650 roads and nearly 600 bridges were damaged, disrupting transportation networks across Manitoba.
Ice storm:
- In 1998, freezing rain fell across parts of Ontario, Quebec, and New Brunswick resulting in at least 35 deaths, over 900 injuries, power outages for approximately 3.5 million people, and over 600,000 evacuees.
- Approximately 19% of workers in Canada were impeded or prevented from travelling to work during the storm and its immediate aftermath.
- Over 15,000 Canadian Armed Forces personnel were deployed to provide shelter, medical care, and assistance with restoring the power grid.
Direct impacts of emergencies, including deaths, can be caused by acute injuries or infections, lack of access to health care, or disruptions to essential goods, like food and water.Footnote 7Footnote 67 Impacts on the availability and safety of water, food, and housing can be ongoing, posing long-term challenges.Footnote 15Footnote 67 Damage to physical infrastructure may cause other direct health impacts, like water-borne diseases from flooding or acute respiratory and gastrointestinal symptoms from crude oil spills.Footnote 68Footnote 69Footnote 70
Emergencies can also cause significant indirect and longer-term impacts on physical and mental health.Footnote 7Footnote 15Footnote 28Footnote 67 These types of impacts are often similar across different kinds of hazards.Footnote 71Footnote 72 For example, smoke from wildfires is associated with an increased incidence of cancer as well as negative respiratory and cardiovascular outcomes.Footnote 73Footnote 74Footnote 75 Biological emergencies, like disease outbreaks, can also cause chronic conditions, such as post-COVID-19 condition (see Appendix B).Footnote 67Footnote 76
The mental health effects of emergencies can be serious and long-lasting. This is because psychosocial effects can persist after an emergency, are linked to the development of chronic physical conditions, and possibly affect people who were not directly exposed to the hazard.Footnote 77Footnote 78Footnote 79 For instance, after the 2013 train derailment in Lac-Mégantic, 67% of local survey participants reported moderate to severe symptoms of post-traumatic stress.Footnote 80 In another example, the Final Report of the Mass Casualty Commission described the need for mental health supports for a wide range of people affected by the 2020 mass shooting in Nova Scotia.Footnote 81 This included the individuals present during the attack, family and loved ones, first responders and witnesses, as well as the local communities and wider population.Footnote 81
Measures to protect health during an emergency, such as community evacuations, can also create challenges. These include family separation, disruption of important social and cultural practices, and deterioration of relationships with the environment.Footnote 67Footnote 82 According to a report from the Auditor General of Canada, in the past 13 years, First Nations communities have faced more than 1,300 emergencies, resulting in over 580 evacuations and impacting the lives of more than 130,000 individuals.Footnote 83 Evacuations and long-term displacement can have negative consequences on mental health and well-being, as well as spiritual impacts.Footnote 7Footnote 77 Research also suggests that each additional exposure to an emergency increases the probability of experiencing negative mental and physical health outcomes.Footnote 5Footnote 7Footnote 28Footnote 67Footnote 84Footnote 85
Emergencies may further impact the conditions that influence health and well-being, such as education, income, housing, food security, and access to health care. For example, flooding or wildfires can destroy housing, and evacuation can disrupt employment.Footnote 5 Public health measures could necessitate virtual rather than in-person education and reduce access to health services.Footnote 86 Emergencies can also drive changes to other factors that influence health, which was seen during the COVID-19 pandemic related to healthy behaviours (e.g., the decrease in physical activity in children and youth; the increase in substance-related hospital care), discrimination (e.g., the increase in hate crimes), and family and gender-based violence (e.g., the rise in calls to police, which is part of an ongoing trend).Footnote 87Footnote 88Footnote 89Footnote 90Footnote 91
Structural drivers cause inequities in emergency risk, resources, and outcomes
"When we think in terms of emergency preparedness and response, again COVID was a great example of how emergency situations can exacerbate existing inequities. We must recognize from the outset, that we're not all at the same starting block, we're not all experiencing the same barriers or opportunities."
The impacts of emergencies are determined not only by the nature and severity of hazards, but also how these hazards interact with broader physical, social, ecological, political, and economic contexts.Footnote 1Footnote 7Footnote 92 These contexts include systems of oppression, such as colonialism, and other overlapping forms of systemic discrimination such as racism, heterosexism, classism, and ageism. Whether, and to what degree, an emergency impacts individuals and communities is influenced by how likely they are to be exposed to a hazard, the intersecting inequities or vulnerabilities they experience, and their access to resources to respond and recover (see Figure 4).
Some groups can more easily access the power and resources needed to protect themselves during an emergency.Footnote 93 This is due to social, structural, and ecological drivers that shape the living conditions and ecosystems in which people are born, grow, live, work, and age (for an illustration of these pathways, see Figure 4).Footnote 94Footnote 95 Together, these make up the determinants of health. Intersections across these determinants can create layered and compounded risks for some populations or communities.Footnote 96Footnote 97Footnote 98 During the COVID-19 pandemic, these intersecting risks exacerbated existing inequities related to determinants of health, such as sex, gender, racialization, income, housing, employment, and other socioeconomic factors.Footnote 5Footnote 96Footnote 97

Figure 4 - Text description
This figure depicts pathways to inequitable outcomes from emergencies. From left to right, the figure depicts the determinants of health, impacts, and outcomes. From left to right the figure describes the following components:
Social, structural, and ecological drivers:
- Cultural and societal norms and values;
- Political, social, and economic structures and policies;
- Natural environment, the land, and climate change; and,
- History and legacy, ongoing colonialism, structural discrimination (e.g., racism, gender identity stigma, ableism)
Living conditions and ecosystems:
- Physical and built environment (e.g., housing, land use, transportation);
- Social environment (e.g., social connectedness, social cohesion, experience of discrimination, violence);
- Economic and work environment (e.g., employment, income, occupational hazards);
- Service environment (e.g., education, social services and family/childcare supports, health care, emergency services, community level resources); and,
- Digital environment (e.g., digital services, digital connectivity, digital media, algorithm technology)
The impacts of these drivers and determinants of health are:
- Differential exposure: More likely to experience a hazard;
- Differential vulnerability: More likely to be negatively impacted by an emergency; and,
- Differential capacity: Less likely to have the resources and community organizations to respond to and recover from emergencies
These differential impacts mean some populations and communities experience compounded effects of increased exposure and vulnerability and reduced capacity.
The outcome of this pathway is disproportionate negative health impacts from emergencies.
Source: Figure adapted from Blumenshine et al., Pandemic Influenza Planning in the United States from a Health Disparities Perspective (2008); Pan American Health Organization, Just Societies: Health Equity and Dignified Lives. Report of the Commission of the Pan American Health Organization on Equity and Health Inequalities in the Americas (2019); Public Health Agency of Canada, Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2022: Mobilizing Public Health Action on Climate Change in Canada (2022).
These determinants of health, and their interactions, drive inequities in exposure, vulnerability, and capacity to respond to and recover from emergencies.Footnote 4Footnote 5Footnote 7
Differential exposure occurs when some populations or communities are more likely to experience a hazard than others. Exposure can be influenced by geography, such as for those who live in areas prone to earthquakes or flooding. It can also be influenced by social or economic policies that reflect, drive, and sustain systemic discrimination in society.Footnote 5 This was evident during the COVID-19 pandemic, when factors at work (e.g., employment in essential services, lack of paid sick leave), and at home (e.g., long-term care facilities, overcrowded housing), increased the likelihood of viral exposure.Footnote 5Footnote 99 Research has demonstrated that exposure risk was higher among certain populations, such as those who are racialized, because of social and economic inequities, contributing to their overrepresentation in COVID-19 infections.Footnote 5 Differential exposure also applies to natural hazards, such as flooding.Footnote 100 For example, exposure to flood risk is more significant in neighbourhoods in Canada with higher proportions of persons living alone, Indigenous Peoples, people of South Asian descent, older adults, other visible minorities, and economically insecure residents.Footnote 1Footnote 100Footnote 101Footnote 102
Differential vulnerability refers to how susceptible a population or community is to being impacted by a hazard (see text box "What is vulnerability?").Footnote 30 Vulnerability can be influenced by a number of factors, including demographic characteristics, health status, and occupation. For example, children and adolescents, first responders, and individuals with pre-existing mental health conditions may be more likely to experience adverse mental health impacts after emergencies.Footnote 103 Research has demonstrated that people living with chronic health conditions and older adults have been more negatively impacted by emergencies such as COVID-19, wildfire smoke, or heat waves.Footnote 1Footnote 5Footnote 104Footnote 105
Some differential vulnerability is caused by social, economic, environmental, and political drivers (e.g., colonization, stigma and discrimination, income and wealth inequality, gendered distribution of labour). These lead to inequitable access to the resources and conditions necessary to achieve and maintain good health (e.g., income, education, housing), leading to health inequities.Footnote 106 In other instances, drivers such as stigma and discrimination increase susceptibility to indirect impacts of emergencies. For example, in August 2020, Chinese, Korean, Southeast Asian, and Black survey respondents in Canada were twice as likely as white participants to report experiencing discrimination during the COVID-19 pandemic.Footnote 107Footnote 108 In another example, some research has suggested there were disproportionate impacts of the COVID-19 pandemic among some 2SLGBTQIA+ populations in Canada, including potentially widening mental health and substance use inequities, increased safety concerns, or increased challenges accessing gender-affirming medical care.Footnote 109Footnote 110Footnote 111Footnote 112Footnote 113
What is vulnerability?
The term "vulnerability" has been critiqued as stigmatizing, deficit-oriented, and paternalistic, since it may imply risks are inherent to an individual or community.Footnote 114Footnote 115Footnote 116 Instead, public health researchers and practitioners advocate for language and analysis that focus on the societal systems that inequitably distribute risk and negative outcomes across populations and communities.Footnote 114Footnote 115Footnote 116
The field of emergency management uses "vulnerability" differently, to reflect how susceptible individuals, groups, or communities are to the impact of hazards.Footnote 117 In emergency management, vulnerability is influenced by physical, social, economic, and environmental factors.Footnote 117 For example, a remote community that is close to wildland and far from emergency services may be more vulnerable to the consequences of wildfire. However, use of the term "vulnerable" can be harmful when applied to populations facing structural barriers as there is increased risk of reinforcing damaging socially constructed stereotypes. The terms "vulnerable" and "vulnerability" will only be used in this report when referencing specific concepts related to public health emergencies or emergency management.
Differential capacity to respond to and recover from emergencies refers to unequal access to the power and resources needed to effectively react during an emergency and reconstruct lives and livelihoods afterwards. For example, some communities face challenges in accessing, affording, and understanding property insurance, which limits their ability to rebuild after a flood or wildfire.Footnote 118Footnote 129 Certain groups, like people with disabilities, may face accessibility barriers to evacuation or other response efforts.Footnote 120Footnote 121 Those living in rural and remote areas with limited access to transportation infrastructure can experience barriers to accessing health care and other services needed for response and recovery.Footnote 1
"Not everybody has internet, not everyone can afford data. And if you don't know where the shelter is in the community beforehand, how are you going to get there?"
Populations and communities can face one or a combination of differential exposure, vulnerability, and capacity. This may vary over time and across hazards (see text box "First Nations, Inuit, and Métis communities are disproportionately impacted by emergencies"). Political, social, and economic conditions can create intersecting, systemic disadvantages causing the same communities to repeatedly experience differential exposure, vulnerability, and capacity across different hazards.
First Nations, Inuit, and Métis communities are disproportionately impacted by emergencies
First Nations, Inuit, and Métis communities hold distinct knowledges and science which have created unique economies and cultures of sustainability and resiliency. The legacy and continuation of colonial practices and perspectives has led to direct losses and damages to Indigenous cultures, health, and overall well-being. The historic and enduring legacy of colonialism perpetuates health, social, and economic inequities facing First Nations, Inuit, and Métis communities. This results in differential exposure, vulnerability, and capacity to respond to and recover from emergencies, further driving inequitable health outcomes.Footnote 122
Differential exposure can be influenced by geographic location and the state of local infrastructure, particularly for remote communities. Some First Nations, Inuit, and Métis communities are more susceptible to emergencies.Footnote 123 For example, First Nations communities living on reserve were estimated to account for 1.1% of the Canadian population, but 2.9% of the population living in the wildland-urban interface, making them more exposed to wildland fires than other communities.Footnote 124 In Nunavut, where 85% of the population is Inuit, frequent states of emergencies are declared related to clean water safety because of poor infrastructure quality.Footnote 125Footnote 126 During the COVID-19 pandemic, some Indigenous communities faced increased risks of exposure to the virus because inadequate housing has led to overcrowding.Footnote 127
Differential vulnerability is influenced by the ongoing health impacts of colonization, racism, intergenerational trauma, and barriers to self-governance. All of these factors are associated with chronic diseases that increase vulnerability to negative health impacts.Footnote 67 Similarly, more extensive consequences of long-term evacuations tend to fall on First Nations, Inuit, and Métis communities due to the cultural dislocation and trauma associated with geographic displacement.Footnote 128Footnote 129 This is particularly true for the many communities who have been evacuated multiple times.Footnote 1 These factors also affect the state of local infrastructure, further increasing vulnerability. For example, as a result of severe infrastructure deficits, 26% of Inuit, 20% of First Nations, and 10% of Métis Peoples in Canada lived in housing that needed major repairs in 2021, compared to 5.7% among the non-Indigenous population.Footnote 130 Housing in need of major repairs could be less likely to withstand a hazard.
Differential capacity to respond and recover is often due to lack of adequately resourced, accessible, and relevant services, including emergency services.Footnote 122 Some of the key factors driving this are lack of culturally safe and trauma-informed services that prioritize Indigenous Knowledges, difficulties in providing emergency services to remote or isolated communities, and mistrust resulting from colonialism and racism that can impact access to and use of healthcare services.Footnote 122 Further, research in Canada has noted that some evacuees have experienced racism and discrimination in host communities, making them feel unwelcome or unsafe.Footnote 131Footnote 132Footnote 133Footnote 134
Despite these structural inequities, Indigenous cultural identity can also act as a protective factor and asset. Traditional cultural values and practices, from community gatherings to traditional land use and ceremonies, have been shown to promote coping and healing from trauma for Indigenous Peoples.Footnote 123Footnote 135Footnote 136Footnote 137Footnote 138Footnote 139Footnote 140
Section 2: Emergency management systems in Canada
By their multi-faceted and complex nature, emergencies often demand attention and resources across sectors and levels of government, from next-door neighbours to the federal government, and from local businesses to the Canadian Armed Forces. In addition to the important assistance that people living in Canada provide to each other during times of crisis, there are formal and structured emergency systems dedicated to preventing, preparing for, responding to, and recovering from emergencies. Public health is one of many sectors within these systems.
Emergency management governance
As a discipline and field of practice, emergency management originated in civil defence in the 1950s and then expanded from its initial focus on wartime threats to provide rescue and immediate aid in the context of extreme weather events or human-made disasters.Footnote 2Footnote 141
In Canada, responsibility for emergency management is shared among federal, provincial, territorial, municipal, and Indigenous governments, as well as other partners. These partners include communities, National Indigenous Organizations, the private sector, and academia. Non-governmental organizations also play a key role in emergency management. For example, the Canadian Red Cross publishes and promotes household guides to emergency preparedness and was also instrumental in boosting surge capacity at vaccination clinics, hospitals, and voluntary self-isolation sites during the COVID-19 pandemic.Footnote 142Footnote 143 All the above groups have shared and complementary roles, often determined by jurisdiction or hazard type. This work is guided by frameworks at national, provincial/territorial, and local levels.
The main federal legislation for emergency management is the Emergency Management Act. This law sets out the powers and responsibilities for preparing for emergencies, developing emergency plans, and for coordinating across departments and levels of government. Much of the actual coordination work takes place through the policy document An Emergency Management Framework for Canada and its associated strategies and action plans.Footnote 117 Provincial and territorial governments are responsible for emergency management within their respective jurisdictions. Each province and territory has a central emergency management statute. These function like the Emergency Management Act by delegating roles and responsibilities and setting out the processes for declaring an emergency and using emergency powers.Footnote 144
The Government of Canada leads in responding to emergencies of international and national concern, developing national policies, providing financial support, and assisting provinces and territories when requested (e.g., supplies, equipment). This includes financing through the Disaster Financial Assistance Arrangement and the Disaster Mitigation and Adaptation Fund.Footnote 145Footnote 146 This work is led by Public Safety Canada, who is also responsible for Canada's domestic implementation of the United Nations Sendai Framework for Disaster Risk Reduction.Footnote 147 Public Safety Canada works closely with other federal departments and agencies, such as Environment and Climate Change Canada, the Department of National Defence, Indigenous Services Canada, and the Public Health Agency of Canada. Under the Emergency Management Act, every minister must also identify risks within their area of responsibility and prepare, test, maintain, and implement emergency plans.Footnote 144 Given the inherently intersectoral nature of emergency management, there are several targeted guidance documents and response plans across the Government of Canada (see text box "Key emergency management documents in Canada").
Key emergency management documents in Canada
Legislation
- Emergencies ActFootnote 148, 1988: This is a federal law that sets out specific requirements for declaring a national emergency and granting temporary, additional, and necessary powers to the federal government in the event of an emergency.
- Emergency Management ActFootnote 149, 2007: This is a federal law that establishes an emergency management program, which includes roles and responsibilities, developing emergency plans, and coordination across departments and levels of government.
Public Safety Canada policy
- An Emergency Management Framework for CanadaFootnote 117, 2017: This is a federal framework that establishes a common approach for federal, provincial, and territorial collaborative emergency management initiatives.
- Emergency Management Strategy for Canada: Toward a Resilient 2030Footnote 2, 2019: This strategy builds on "An Emergency Management Framework for Canada" by identifying federal, provincial, and territorial priorities aimed at strengthening resilience.
- 2021-22 Federal, Provincial, and Territorial Emergency Management Strategy Interim Action PlanFootnote 150, 2022: This is the first in a series of action plans that identify defined outcomes within the "Emergency Management Strategy for Canada: Toward a Resilient 2030" and demonstrate concrete steps that federal, provincial, and territorial governments, and other emergency management partners intend to take to advance resilience.
Sector-specific guidance
- Federal/Provincial/Territorial Public Health Response Plan for Biological EventsFootnote 151, 2017: This plan outlines formal coordination of federal, provincial, and territorial response to public health events that are biological in nature to ensure a common emergency management approach across jurisdictions.
- Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health SectorFootnote 152, 2018: This is a guidance document that outlines how federal, provincial, and territorial jurisdictions will work together to ensure a coordinated and consistent health-sector approach to pandemic preparedness and response. Lessons learned from COVID-19 and stakeholder consultations will inform the future direction of this document.
- Canada's National Adaptation Strategy: Building Resilient Communities and a Strong EconomyFootnote 153, 2023: This strategy lays out a framework to reduce the risk of climate-related disasters, improve health outcomes, protect nature and biodiversity, build and maintain resilient infrastructure, and support a strong economy and workers.
At the provincial and territorial level, emergency management is also typically the responsibility of a public safety lead that collaborates across departments. However, the emergency management structure looks different across provinces and territories. For example, in some jurisdictions there are separate laws and policies for natural or human-caused emergencies, and public health emergencies like infectious disease outbreaks.
Since most emergencies occur at a local level, the first response is almost always by local or provincial and territorial authorities. Provinces and territories delegate responsibilities and powers to regional governments to manage local emergencies. However, provinces and territories usually retain significant oversight and control. For example, some provinces and territories can cancel a local declaration of emergency at any time, order changes to local emergency plans, or decline requests for support. Each regional and/or local authority is usually required to lead local emergency management and coordinate across other sectors within their purview. This means developing and implementing emergency management programs and plans and conducting community hazard and vulnerability assessments.
Priorities can vary across Canada due to local context, including different risks or vulnerabilities. If an emergency escalates beyond capacity to cope, provincial and territorial governments may request assistance from the federal government.
First Nations, Inuit, and Métis communities
First Nations, Inuit, and Métis communities are also the first line of response during emergencies. The configuration of broader emergency management governance for these communities varies greatly depending on agreements with federal and provincial/territorial governments. First Nations, Inuit, and Métis authorities are in different stages of developing agreements with provincial/territorial and federal governments.Footnote 122 Emergency responses may also look different depending on local context.Footnote 144 This could include alternative evacuation measures that avoid replicating conditions associated with residential schools, stronger travel or border controls, or providing safe and culturally relevant activities and supports.Footnote 154
At the federal level, in addition to funding and providing health services, Indigenous Services Canada, in accordance with Public Safety Canada, provides emergency management funding and support to First Nations communities on reserve. The Emergency Management Assistance Program can be applied to a range of activities, including emergency planning, training and exercises, emergency operation centres, and emergency response equipment and supplies.Footnote 51 Métis and Inuit communities generally fall under the jurisdiction of the provincial/territorial and local government services.
National, regional, and local Indigenous organizations may also address emergency management in their mandates. For example, the Assembly of First Nations is working continuously to secure new funding for emergency management, enhance programs and services, reform policies, and foster respectful working relationships between First Nations Peoples and all levels of government.Footnote 155 The Métis National Council is developing emergency management strategies and action plans, aligned with national approaches, to integrate Indigenous Knowledges and practices in emergency management, and support Métis settlements and communities.Footnote 156
Indigenous emergency management research and funding is often focused on First Nations Peoples living on reserve and more work is needed to understand and address the experiences and needs of First Nations, Inuit, and Métis Peoples living in other communities and urban centres.Footnote 32Footnote 150
Emergency management as an essential public health function
Along with health promotion and 4 other functions, emergency management is an essential public health function in Canada (see the 2021 CPHO report for a description of all essential public health functions).Footnote 34Footnote 157Footnote 158Footnote 159 It is typically a part of health emergency management, which also includes ensuring the integrity of healthcare infrastructure and its capacity to provide medical care for physical and mental health during emergencies. Health emergency management feeds into broader emergency efforts. These broader efforts occur across governments but are often led by the public safety sector.Footnote 2
Modern emergency management uses an all-hazards approach (see Figure 5). This approach can increase efficiency by identifying and integrating emergency management elements common across all potential risks and impacts.Footnote 117 Specific components are added, as necessary, to address the unique needs of each hazard type.Footnote 117 While emergency management is presented as a continuum, these activities are not sequential. Actions across the continuum, from prevention and mitigation to preparedness, response, and recovery, occur concurrently to best support communities before, during, and after emergencies.
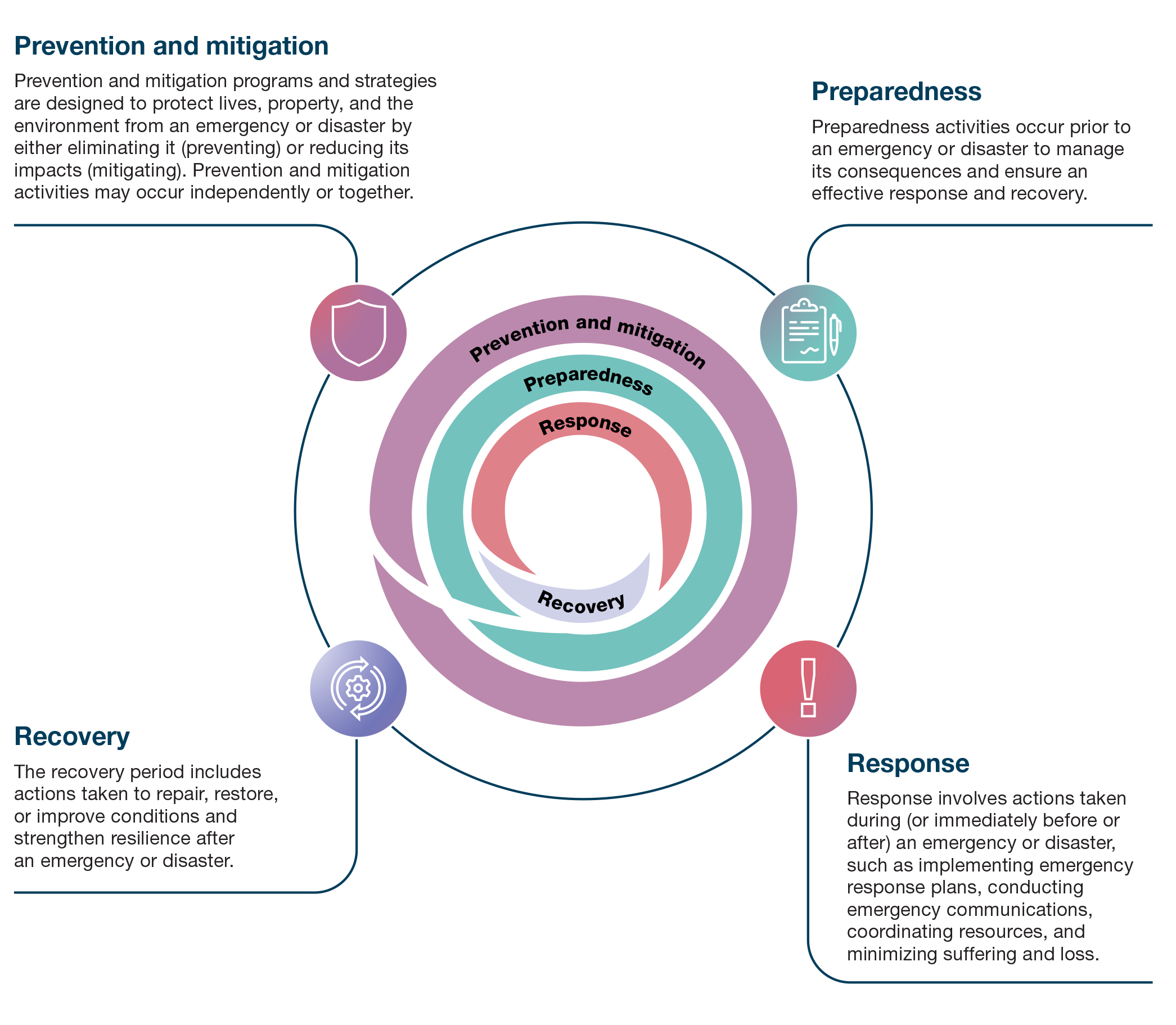
Figure 5 - Text description
The 4 components of the emergency management continuum are illustrated in a diagram of concentric circles, with prevention and mitigation in the outside circle, then preparedness, and finally an inner circle that encompasses response and recovery. From the outside circle working in, the components are as follows:
Prevention and mitigation: Prevention and mitigation programs and strategies are designed to protect lives, property, and the environment from an emergency or disaster by either eliminating it (preventing) or reducing its impacts (mitigating). Prevention and mitigation activities may occur independently or together.
Preparedness: Preparedness activities occur prior to an emergency or disaster to manage its consequences and ensure an effective response and recovery.
Response: Response involves actions taken during (or immediately before or after) an emergency or disaster, such as implementing emergency response plans, conducting emergency communications, coordinating resources, and minimizing suffering and loss.
Recovery: The recovery period includes actions taken to repair, restore, or improve conditions and strengthen resilience after an emergency or disaster. The recovery phase blends back into the continuum, demonstrating its influence on prevention and mitigation and preparedness activities.
Public health systems play leadership and supporting roles in the different components of emergency management, depending on the nature of the hazard.Footnote 117Footnote 161 For example, public health authorities and professionals have lead roles in responding to infectious disease emergencies, which rank as the deadliest disasters in human history.Footnote 162 They also contribute to planning and response efforts for extreme weather events or human-made disasters, to minimize serious illness and death as well as societal disruption. However, the intersectoral nature of emergency management can make it difficult to generalize public health roles and responsibilities, which may vary across and within provinces/territories. As such, this report encompasses the emergency management processes and activities that reflect the critical collaboration among public health, health emergency management experts, and public safety departments.
Section 3: A health promotion approach to emergency management
The increasing frequency and severity of emergencies in Canada has prompted further consideration across sectors on how best to prevent, prepare for, respond to, and recover from emergencies. A similar reflection is occurring within public health, sparked in part by the COVID-19 pandemic and other recent emergencies.
Research and reports on the COVID-19 response, as well as those exploring climate adaptation and disaster resilience, have emphasized the importance of addressing inequities and creating the social, economic, environmental, and political conditions for good health and well-being.Footnote 1Footnote 6Footnote 8Footnote 19Footnote 20Footnote 163Footnote 164 Public health can contribute to a growing focus on prevention, mitigation, and preparedness by supporting intersectoral attention to the determinants of health and strengthening collective action at the community level. This work can be guided by the insights and approaches of health promotion.
"With health promotion, there's a lot of opportunities. I think it would be a bit of a paradigm shift to get people to think in these terms. To get upstream and address what is really the underlying causes of emergencies. We should also be doing the community engagement work and community building. It'll create supportive networks so that when there is an emergency you have a community that has greater resiliency."
Health promotion can support emergency management
All public health functions have a role to play in addressing emergencies. For example, health protection efforts can address threats to safe drinking water after a flood, whereas health surveillance or population health assessment can reveal adverse health effects that develop after exposure to wildfire smoke.
However, recent shifts within emergency management, to focus on resilience and communities, emphasize the relevance of health promotion.Footnote 2Footnote 5Footnote 92Footnote 153Footnote 165 Specifically, health promotion can offer approaches to improve health and well-being focused on collaborating with communities (see text box "What is a community?") and targeting the determinants of health.Footnote 166Footnote 167Footnote 168 This occurs through equity-oriented interventions that rely on healthy public policy, community action, and building supportive environments.Footnote 169 With a greater focus on the unique impacts of colonization, and guided by Indigenous leaders, health promotion also has the potential to complement Indigenous Knowledges focused on the interconnectedness of physical, emotional, mental, environmental, and spiritual well-being.Footnote 170Footnote 171Footnote 172Footnote 173
What is a community?
Communities exist in various forms, including location-based communities where people share an attachment to a place and social connection communities based on relationships between people. In public health, the concept of "community" can encompass groups of individuals who share common geographic locations, interests, experiences, concerns, and/or identities.Footnote 174 It also includes groups or networks with shared experiences, identities, or professional backgrounds (see examples in Figure 6). Community members may include residents, individuals with experiential knowledge, community organizations and services, and leaders. However, the composition of communities is diverse and will vary depending on the context and the specific focus of each. Communities with shared identities or interests can be local, regional, national, or international in scale.Footnote 174Footnote 175 Individuals can also be members of multiple communities.Footnote 176

Figure 6 - Text description
This figure provides examples of different types of communities. From left to right, the figure describes:
Communities based on location, such as neighbourhoods; urban, rural, and remote Indigenous communities; rural communities, and regions (e.g., towns, cities).
Communities based on social connection, such as family, friends, and peer groups; co-workers; hobby, lifestyle, and interest-based groups; and social media and online groups.
Communities based on shared experiences, such as people with lived experience of emergencies; and support groups (e.g., physical and mental health conditions, substance use recovery, parents and caregivers, bereavement).
Communities based on a shared identity, such as Indigenous Peoples; 2SLGBTQIA+ populations; cultural and ethnic groups; religious, spiritual, and faith-based groups; and language-based communities.
Communities based on professional background, such as occupational groups (e.g., frontline workers); and professional associations.
Health promotion as rooted in the Ottawa Charter
Health promotion has its origins in the earliest beginnings of public health in the 19th century.Footnote 177Footnote 178 The modern discipline of health promotion was introduced in the report A New Perspective on the Health of Canadians (known as the Lalonde Report).Footnote 179 Health promotion was formalized in The Ottawa Charter for Health Promotion, adopted at the first International Conference on Health Promotion in 1986, a World Health Organization (WHO) initiative.Footnote 11 The Ottawa Charter is widely considered by the public health sector to be a landmark document for public health practice.Footnote 180
Health promotion was defined in the Ottawa Charter as the process of enabling people to increase control over, and to improve, their health. Importantly, health is situated as a product of the conditions in which people live, play, learn, work, and age, not just because of their behaviours or access to health care.Footnote 178Footnote 180 Improving these conditions requires a range of social, economic, and ecological interventions, as well as community action and leadership. The work of health promotion draws from many disciplines within and alongside public health, including epidemiology, sociology, behavioural science, anthropology, psychology, political science, geography, ethics, and economics.
The Ottawa Charter details action areas central to a health promotion approach: building healthy public policy, creating supportive environments, developing personal skills, strengthening community action, and re-orienting health services.Footnote 11 The areas of healthy public policy, supportive environments, and community action are particularly relevant for the role of public health in emergency management (see Figure 7). They offer important concepts, applied tools, and evidence-informed interventions that can support efforts across the emergency management continuum to improve the conditions for community resilience (see text box "Health promotion areas of action for emergency management from the Ottawa Charter").
Health promotion areas of action for emergency management from the Ottawa Charter

Figure 7 - Text description
This figure illustrates health promotion areas of action to support the conditions for community resilience.
In the centre of the figure is the emergency management continuum. This diagram of concentric circles illustrates the 4 components of the emergency management continuum (from the outside, moving in): prevention and mitigation, preparedness, response, and recovery.
Surrounding the emergency management continuum diagram are 3 'wings' which represent the health promotion areas of action: build healthy public policy, strengthen community action, and create supportive environments.
Build healthy public policy
Health is influenced by policies from many sectors. A focus on healthy public policy, policies that support health and well-being, must therefore extend beyond the health sector. Healthy public policy combines legislative, fiscal, or policy initiatives to promote equity and target the broader determinants of health.Footnote 11 This could include social policies that tackle the root causes of discrimination, such as racism and ableism; education policies that support inclusive and high-quality schools; or economic policies focused on addressing income and wealth inequities. It might comprise policies that help prevent emergencies (e.g., energy policies that reduce greenhouse gas emissions to mitigate environmental health effects) or reduce their impact (e.g., municipal policies that require new residential buildings to include air conditioning to protect residents during extreme heat events).
A key tool to encourage healthy public policy is Health in All Policies. This is an approach to policy-making that encourages decision-makers across sectors to systematically consider how their proposed policies may influence health and the determinants of health, with the goal of maximizing co-benefits and minimizing harm.Footnote 181
Create supportive environments
Supportive environments foster good health and well-being by improving the conditions of daily life. A supportive environment, strengthened through healthy public policy, could include quality housing, decent work, connected and socially cohesive communities, social protections, food security, access to health and social services, childcare and education, and clean water and air.Footnote 11Footnote 182Footnote 183 Supportive environments may reduce the impacts of a hazard (e.g., adapting housing to be more resilient to damage from earthquakes, floods, or wildfires) or enable adherence to public safety recommendations during an emergency (e.g., accessible and culturally safe vaccination programs during a pandemic).
As technology has advanced, the digital and commercial determinants of health emerged as key areas of focus for building supportive environments.Footnote 184 While advances in technology can offer many benefits, they also facilitate the development and sharing of mis- and disinformation. As such, the parameters of a supportive environment have expanded to include actions that prevent and address mis- and disinformation, as well as accessible resources for digital literacy.Footnote 185
Supportive environments also help encourage behaviour change to promote and protect health and well-being during an emergency. For example, adding more buses to busy routes, or changing the built environment to support more walking or biking and avoid public transit, could help people physically distance during a pandemic.Footnote 186Footnote 187 Providing transportation assistance could help support evacuation from wildfires or floods for people who do not have private transportation.Footnote 188Footnote 189
Strengthen community action
Effective health promotion requires governments to connect local context, community knowledge, and community priorities with formal decision making and initiatives.Footnote 11Footnote 190 Meaningful collective action relies on community leadership, and sustained resources for community engagement, community organizations, and participating community members.Footnote 191Footnote 192 A health promotion approach prioritizes collective action at the community level and on the social, economic, political, and environmental determinants that shape health. By focusing on community knowledge and leadership, community action can help inform emergency management activities that reflect local context, meet local needs, build trust, and strengthen community resilience.
Healthy public policy, supportive environments, and community action may support the reorientation of health systems towards a stronger lens on prevention and health promotion. A strengthened public health system, centred on equity, can work with other sectors to build healthy and resilient populations and protect against current and future public health emergencies. Such a reorientation would reduce demand on the healthcare system. Further details of a strengthened public health system can be found in the 2021 CPHO report, A Vision to Transform Canada's Public Health System.
The Ottawa Charter remains a global health touchstone for health promotion, but its application has evolved to reflect and respond to rapid social, political, economic, environmental, and technological changes. This has led to updates to the fundamental principles of health promotion.Footnote 184 For example, the most recent WHO charter titled The Geneva Charter for Well-being (2021) reflects a broad health promotion narrative that positions health as influenced by a larger environmental, social, economic, and political ecosystem. This includes an expanded list of the determinants of health, such as ecological, digital, and commercial determinants. The Geneva Charter also identified the role that health promotion can play in achieving sustainable "well-being societies", societies in which the different aspects of well-being are prioritized.Footnote 193Footnote 194
While a health promotion approach to emergency management is relevant across all communities, it is particularly important for communities that have and continue to experience historic and systemic exclusion and discrimination. With these communities, including Indigenous communities, racialized communities, communities facing stigma (e.g., 2SLGBTQIA+ communities), and communities living with low-income, it is especially important that health promotion initiatives engage in deeper and more sustained collaboration to honour local leadership, build trust, develop shared accountability, support two-way knowledge sharing, and prioritize co-development of all activities in a culturally safe and strength-based manner. This requires ongoing resourcing for communities to support equitable participation.Footnote 192Footnote 195Footnote 196 For First Nations, Inuit, and Métis communities, this would be connected to broader frameworks of self-governance and self-determination.
Indigenous leadership and decolonization have been increasingly prioritized in international health promotion.Footnote 172 The Tiohtià:ke statement from the 2022 International Union for Health Promotion and Education conference called for global action to centre planetary health, well-being, and equity in all policy action. It highlighted the importance of recognizing the ongoing leadership of Indigenous health promotion and enhancing Indigenous voices and Knowledges.Footnote 172
Health promotion with First Nations, Inuit, and Métis communities
Long before European settler governments arrived, Indigenous Peoples had laws and practices for dealing with hazards, such as wildfires.Footnote 197 Although the intergenerational transfer of Indigenous Knowledges was, and continues to be, severely disrupted by residential schools or other ongoing colonial practices, First Nations, Inuit, and Métis communities continue to use their experience with emergencies to address present-day situations, such as climate change and the COVID-19 pandemic, in culturally responsive ways.Footnote 123Footnote 196Footnote 197Footnote 198Footnote 199
As a result of Canada's colonial history and its current impacts, it is important to reflect on the relevance and value of Western conceptualizations of emergency management and health promotion with First Nations, Inuit, and Métis communities. Although health promotion may generally be useful in emergency management processes with First Nations, Inuit, and Métis communities, it is insufficient on its own and should not subsume Indigenous-led approaches. Among First Nations, Inuit, and Métis communities, such approaches may be rooted in the following:
- Interconnectedness of physical, emotional, mental, environmental, and spiritual well-being;Footnote 200
- Importance of asset- and strength-based approaches;Footnote 196Footnote 201Footnote 202
- Decolonization of systems and practices and addressing historical and ongoing impacts of colonization and systemic discrimination;Footnote 196Footnote 203
- Meaningfully engaging with multiple viewpoints and building bridges between sectors;Footnote 172 and,
- Recognition of First Nations, Inuit, and Métis Knowledges, culture, and expertise.Footnote 128Footnote 196
The United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) can provide a road map for emergency management professionals when working with First Nations, Inuit, and Métis communities.Footnote 22Footnote 204 UNDRIP sits alongside other rights-based tools intended to protect the inherent rights and dignity of all humans (e.g., Inherent and Treaty Rights, United Nations Human Rights, Committee on the Elimination of Racial Discrimination).Footnote 205Footnote 206Footnote 207 The following 4 UNDRIP themes represent the minimum standards necessary for the prosperity, dignity, and well-being of Indigenous Peoples.
- The right to self-determination
Autonomy in decision making and self-governance can help mitigate the negative impacts of health emergencies, like the COVID-19 pandemic.Footnote 196 UNDRIP reaffirms that Indigenous Peoples have the right to decide what is best for them and their communities, the right to control their own government structures, and the right to determine their own political, cultural, social, and economic development.Footnote 22Footnote 204 This may include First Nations, Inuit, and Métis communities taking control of, co-leading, or engaging with emergency management systems. While action on self-governance related to emergency management is being implemented across Canada (see text box "Examples of First Nations, Inuit, and Métis self-determination relating to emergencies"), resource gaps and jurisdictional challenges remain that can prevent Indigenous communities from achieving full self-governance.Footnote 45Footnote 154Footnote 208Footnote 209
These jurisdictional challenges can impact First Nations, Inuit, and Métis communities in different ways. Due to the parameters of the Indian Act, Inuit and Métis communities do not have the same types of joint emergency management governance processes as First Nations communities.Footnote 210 Métis self-government agreements are negotiated under the Canada-Métis Nation Accord of 2017, but emergency management planning is not resourced.Footnote 154 The 5 Inuit-Crown modern treaties set out various governance agreements and Inuit rights in relation to the land and resources, however emergency management is not specified.Footnote 211 Instead, Inuit and Métis communities rely on provincial, territorial, and municipal emergency and public health services. In some communities with First Nations and/or Inuit and Métis populations, First Nations can be self-governing, but Inuit and Métis populations are included in municipal responses. Similarly, urban Indigenous populations fall under provincial, territorial, and municipal jurisdictions for emergency services, with urban Indigenous organizations, like the Friendship Centres, filling service and jurisdictional gaps without dedicated emergency management resources. Since 44% of Indigenous Peoples in Canada live in large urban centres, there is an ongoing need to support culturally relevant emergency management policies and practices with these populations.Footnote 212Footnote 213Footnote 214
Examples of First Nations, Inuit, and Métis self-determination relating to emergencies
First Nations
The Assembly of First Nations has been advocating for First Nations communities to assume control of their own emergency management and gain access to funding that is comparable to municipal services.Footnote 215 Recent advocacy efforts in this area include the promotion of the development of First Nations-led emergency management and ensuring all Indigenous Services Canada emergency management policies, processes, and procedures are inclusive of regional First Nations representation and contribution. At the time of writing this report, work on a strategic plan is underway. The goal is for First Nations communities to become fully autonomous in controlling and developing their own emergency management programs in full partnership with the federal, provincial, and territorial governments, as well as regional emergency management organizations.
Examples from the provincial level include the British Columbia First Nations Leadership Council, the Government of British Columbia, and the Government of Canada signing a memorandum of understanding in 2019 that recognizes First Nations leaders and communities "as full partners in the governance and operations of emergency management".Footnote 216 Also in British Columbia, the Nisga'a Nation is an example of a First Nation community that is responsible for its own emergency management. This includes an emergency management plan, as well as dedicated plans for each of its 4 villages.Footnote 154Footnote 217Footnote 218
Inuit
As part of the National Inuit Climate Change Strategy, Inuit Tapiriit Kanatami developed a companion framework: Working Better Together: Collaborating with Inuit on Climate Actions in Inuit Nunangat – A Framework for Governmental and Non-governmental Bodies to Take Action on Climate Change.Footnote 219 The framework serves as a guide for partners to foster meaningful partnerships that advance Inuit-driven climate action.Footnote 219 It advocates for the valuing of high-level Inuit climate policy contributions and self-determined decision making, recognizing Inuit as rights-holders and knowledge-holders, and the shared understanding of Inuit governance and foundational principles for meaningful engagement.
Métis
The Métis National Council (MNC) has highlighted gaps in emergency management for Métis communities and is advocating for adequate, appropriate, and sustainable resources to support Métis-dedicated services and Métis-led intersectoral action without fiscal and administrative barriers.Footnote 154 The MNC has also called for the following: a shift in perspective beyond the territory-specific lens due to the geographical dispersal and governance of Métis communities; adequate funding for nation-to-nation engagement; and Métis-dedicated emergency management funding, services, and research based on self-determination and co-development principles.Footnote 154 In June 2023, at the annual Crown-Métis Nation Summit, the President of the MNC and the Prime Minister of Canada identified emergency management as an official priority for government-to-government collaboration.Footnote 220
- The right to cultural identity
Connection to cultural identity acts as a protective factor for Indigenous Peoples, and traditional cultural practices can promote coping and healing.Footnote 123Footnote 137Footnote 139Footnote 140 UNDRIP states that Indigenous Peoples are equal to all other peoples and have the right to their practices, culture, traditions, and traditional knowledges.Footnote 22 Indigenous Knowledges have been recognized for their essential contributions to environmental protection, climate action, and addressing the risks of specific hazards (e.g., forest management practices that reduce the risk of wildfires).Footnote 197Footnote 221Footnote 222Footnote 223 The Sendai Framework, to which Canada is a signatory, recognizes the importance of this approach, emphasizing the value of integrating traditional, Indigenous, and local knowledges and practices in disaster risk assessment and the development and implementation of tailored action.Footnote 10 Despite this, the incorporation of Indigenous Knowledges in emergency management has been slow.Footnote 139Footnote 222Footnote 224
While there are many diverse Nations across Canada, and each is best positioned to inform and lead culturally responsive and safe emergency management initiatives for their own communities, there are several areas for emergency management professionals to consider:Footnote 128Footnote 209Footnote 225Footnote 226Footnote 227Footnote 228
- Implement trauma-informed cultural safety training, including training on the impacts of colonization and intergenerational trauma, for volunteers, responders, and government representatives;
- Seek Indigenous leadership to integrate cultural considerations into planning and response activities, and to evaluate emergency management practices;
- Place value on cultural and historic sites when prioritizing emergency response resources;
- Recognize cultural diversity among communities;
- Prioritize cultural continuity during recovery from emergencies; and,
- Integrate traditional healing practices with traditional healers and knowledge holders.
The Indigenous Emergency Management Capabilities Inventory is an example of a culturally responsive, inclusive, and sustainable approach to emergency management (see text box "The Indigenous Emergency Management Capabilities Inventory Project").
The Indigenous Emergency Management Capabilities Inventory ProjectFootnote 229Footnote 230
The Assembly of First Nations and Public Safety Canada have co-led the Indigenous Emergency Management Capabilities Inventory Project since 2017, with support and input from other Indigenous representatives, as well as provinces, territories, and emergency management partners. The inventory maps emergency management risks, capabilities, priorities, needs, and gaps in First Nations, Inuit, and Métis communities across Canada. This initiative recognizes the value of Indigenous Knowledges and is an opportunity for Indigenous communities to inform a culturally responsive approach to emergency management.
- The right to free, prior, and informed consent
UNDRIP reaffirms that Indigenous Peoples have the right to be consulted and involved in the decision-making process on all issues that impact them.Footnote 22 First Nations, Inuit, and Métis are self-determining and have unique local and land-based understandings for how to address emergencies and protect their lands and territories. This includes valuable insights into environmental conditions and traditional and cultural practices that can complement and inform emergency responses.Footnote 123Footnote 197Footnote 221Footnote 222Footnote 231 Incorporating Indigenous Knowledges into emergency management requires collaboration and respectful engagement, as well as the application of a distinction-based approach that reflects the nationhood of First Nations, Inuit, and Métis communities and their distinct cultures, contexts, knowledge systems, and emergency management priorities. Of relevance to emergency management, Indigenous Peoples have the right to not be removed or relocated by force from their lands without their free, prior, and informed consent. This includes the right to make decisions on emergency evacuations without pressure and to be compensated for their relocation, with the option to return to their land, if possible.Footnote 22 According to a 2022 Auditor General report, key issues concerning evacuation have not been addressed, including access to essential health and mental health services, and the needs and priorities of elders, women, and youth.Footnote 83
- Protection from discrimination
As stated in UNDRIP, Indigenous Peoples have the right to be safe and free from discrimination.Footnote 22 This includes freedom from discriminatory policies or actions during emergency management efforts, and sufficient funding, services, and resources. It requires culturally safe emergency management efforts and ensuring cultural continuity during recovery from an emergency (see text box "First Nations Health Authority and Emergency Management BC Declaration of Commitment to Cultural Safety and Humility").
There have been calls for governments to build cultural safety training and awareness of racism and discrimination throughout the emergency management continuum.Footnote 231Footnote 232Footnote 233 Furthermore, non-Indigenous governments that lead emergency management with First Nations, Inuit, and Métis communities can work toward the decolonization of decision-making structures. This requires true partnerships between governments and First Nations, Inuit, and Métis communities that are based on trust, respect, and mutual understanding, and prioritizing the needs and perspectives of Indigenous Peoples.Footnote 22
First Nations Health Authority and Emergency Management BC Declaration of Commitment to Cultural Safety and Humility
In May 2019, the First Nation Health Authority and Emergency Management and Climate Readiness (formally Emergency Management BC) in British Columbia signed the Declaration of Commitment to Cultural Safety and Humility in Emergency Management Services for First Nations People in British Columbia. Cultural humility is a life-long process of self-reflection to understand personal and systemic biases and to develop and maintain mutually respectful relationships with Indigenous Peoples.Footnote 234 Cultural safety is an outcome based on respectful engagement that recognizes and strives to address power imbalances.Footnote 234
The declaration is based on the following guiding principles: cultural humility builds relationships founded in mutual trust and respect, and enables cultural safety; cultural safety and humility must be understood, embraced, and practiced at all levels of the emergency services system, including governance, organizational, and within individual practice; and we have achieved cultural safety when First Nations and Indigenous People tell us we have. Applying these principles involves open and honest conversations, identifying and removing barriers, and developing and implementing cultural safety and humility strategies and workplans at multiple levels to evaluate progress.Footnote 234 The declaration outlines a plan to integrate cultural safety and humility into Emergency Management and Climate Readiness' training, policies, and practices.Footnote 234
Section 4: Applying health promotion actions to the emergency management continuum
"A lot of health promotion efforts are not yet truly institutionalized. If you want something there in an emergency, you have to support it in a non-emergency. We actually need to make health promotion a legitimate and resourced and professionalized part of what we do."
In the following sections, health promotion actions are applied to the 4 components of the emergency management continuum. These actions are building healthy public policy, creating supportive environments, and strengthening community action, alongside overarching principles of equity and justice (see Figure 8). A toolkit of potential health promotion tools that can be applied across emergency management processes can be found in Appendix A.
Health promotion approaches employed in any of the overlapping emergency management components may facilitate action throughout the continuum. For example, investing in community level social infrastructure for prevention and mitigation can help ensure community organizations have the resources to collaborate on preparedness plans that consider local context. These actions then assist with building relationships and trust between formal emergency systems and communities, which can be used to ensure rapid and effective response during an emergency.

Figure 8 - Text description
In the centre of the figure is the emergency management continuum. This diagram of concentric circles illustrates the 4 components of the emergency management continuum (from the outside, moving in): prevention and mitigation, preparedness, response, and recovery.
Surrounding the emergency management continuum diagram are examples of health promotion actions for each component of the emergency management continuum. These examples of health promotion actions are:
Prevention and mitigation:
- Take action on the drivers of emergencies and determinants of health
- Redefine community resilience to address equity and power
- Strengthen social infrastructure and support community leadership
Preparedness:
- Prepare for healthy public policy during emergencies
- Establish inclusive community partnerships
- Plan for equity
Response:
- Create supportive environments to promote health and enable behaviour change
- Engage communities to strengthen trust and social cohesion
- Integrate equity into response processes
Recovery:
- Build resilience into recovery
- Foster an ongoing role for communities
- Improve future preparedness and response efforts
Prevention and mitigation
Preventing and mitigating emergencies requires action to reduce the likelihood of hazards, the extent of their impact, and the inequitable distribution of resources needed to prevent, respond to, and recover from them. Health promotion can contribute through attention on the determinants of health and by supporting community-centred resilience through a focus on social infrastructure and community leadership (see Figure 9).

Figure 9 - Text description
This figure depicts pathways to improving the determinants of health and strengthening social infrastructure to build resilience and reduce inequitable health impacts from emergencies. From left to right, the figure depicts the determinants of health, impacts, and outcomes. From left to right the figure describes the following components:
Social, structural, and ecological drivers:
- Cultural and societal norms and values;
- Political, social, and economic structures and policies;
- Natural environment, the land, and climate change; and,
- History and legacy, ongoing colonialism, structural discrimination (e.g., racism gender identity stigma, ableism)
Living conditions and ecosystems:
- Physical and built environment (e.g., housing, land use, transportation);
- Social environment (e.g., social connectedness, social cohesion, experience of discrimination, violence);
- Economic and work environment (e.g., employment, income, occupational hazards);
- Service environment (e.g., education, social services and family/childcare supports, health care, emergency services, community level resources); and,
- Digital environment (e.g., digital services, digital connectivity, digital media, algorithm technology)
Arrows above and below the determinants of health illustrate the role of taking action on the drivers of emergencies and determinants of health and by strengthening social infrastructure and supporting community leadership.
The impacts of these actions include:
- Exposure: Less likely to experience a hazard;
- Vulnerability: Less likely to be negatively impacted by an emergency; and,
- Capacity: More likely to have the resources and community organizations to respond to and recover from emergencies
This means communities and populations are more resilient, able to withstand and recover from emergencies. The outcomes of these actions are fewer health inequities from emergencies.
Source: Figure adapted from Blumenshine et al., Pandemic Influenza Planning in the United States from a Health Disparities Perspective (2008); Pan American Health Organization, Just Societies: Health Equity and Dignified Lives. Report of the Commission of the Pan American Health Organization on Equity and Health Inequalities in the Americas (2019); Public Health Agency of Canada, Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2022: Mobilizing Public Health Action on Climate Change in Canada (2022).
As a field, emergency management is already moving to increase its focus on prevention and mitigation.Footnote 165Footnote 235 This shift is emphasized in the Emergency Management Strategy for Canada: Toward a Resilient 2030, which calls for greater investment in mitigation to prevent emergencies or reduce their impact, such as the construction of floodways or changing building codes to include cooling requirements.Footnote 2 Prevention and mitigation are also components of Canada's climate action plans, including A Healthy Environment and a Healthy Economy, the Emissions Reduction Plan 2030, and the National Adaptation Strategy.Footnote 236Footnote 237 They are similarly prioritized within public health's role in emergency management, particularly in recent COVID-19 reviews that call for action to prevent and mitigate the impact of future pandemics.Footnote 8Footnote 238
Take action on the drivers of emergencies and determinants of health
"Emergency preparedness for extreme heat or wildfire smoke needs to include policies for clean air, for housing. It's a natural fit to bring these pillars into our emergency planning explicitly. It becomes more of an upstream exercise, not solely response."
Environmental drivers that increase exposure and vulnerability to hazards include climate change, land use change, and biodiversity loss.Footnote 4 The Intergovernmental Panel on Climate Change identified several key mitigation activities to reduce greenhouse gas emissions, including substantial reductions in the use of fossil fuels, greater energy efficiency and conservation, using electric vehicles powered by low-emissions electricity, prioritizing sustainable energy and materials, and increasing carbon uptake and storage.Footnote 7Footnote 239
Addressing the impacts of these drivers could be supported by using a One Health approach.Footnote 240 One Health is a collaborative, intersectoral, and transdisciplinary approach to achieving optimal health outcomes that recognizes the interconnection between people, animals, plants, and their shared environment.Footnote 241 For emergency management, One Health is particularly relevant to the prevention and mitigation of emerging zoonotic diseases that could lead to pandemics.Footnote 240Footnote 242
"Health promotion can be most effective when it's at the level of the population and its policies. Some of the work that needs to be done to prepare for pandemics is really population level interventions. Climate change is a good example, like the smoke is here again today. You can try to help people, or you can try to prevent the smoke from happening. We need to do both … but the actual prevention work needs to be transformative."
A health promotion approach supports the above actions on environmental determinants, as well as actions to support the prerequisites for good health: peace, shelter, education, food, income, a stable eco-system, sustainable resources, social justice, and equity.Footnote 169 There is overlap between these requirements and those that support resilience (For example, see text box "Housing as an important point of intervention").Footnote 243Footnote 244Footnote 245
Housing as an important point of intervention
Housing can offer essential protection during an emergency. Inadequate housing can also pose risks during an emergency, particularly for those who are unhoused or living in shelters.Footnote 246Footnote 247Footnote 248 Additional challenges may be experienced by individuals living in long-term care facilities, overcrowded housing, and in correctional facilities.Footnote 249Footnote 250Footnote 251Footnote 252Footnote 253 Action that promotes resilience in housing needs to be multi-pronged and rooted in healthy public policy, supportive environments, and community action.Footnote 104Footnote 254Footnote 255
Healthy public policy: An example of housing-focused healthy public policy that might contribute to emergency resilience is Housing First policies.Footnote 254Footnote 256 These policies prioritize access to permanent housing without conditions or barriers (e.g., mental health or substance use treatment), alongside the provision of additional supports as needed. This could help to reduce exposure to hazards like extreme weather or pandemics.
Supportive environments: Neighbourhoods are an important component of good quality housing. Increasing green space or walkability of neighbourhoods are examples of how interventions related to supportive environments can reduce risks and exposure to hazards.Footnote 7 These aspects of the built environment can offer co-benefits, including climate change mitigation and reductions in exposure to extreme temperatures.
Community action: Community development and advocacy initiatives led by resident or tenant associations are examples of community action related to housing. This could include action within large apartment buildings to build community trust and social cohesion that could help residents collaborate to meet urgent needs during an emergency (e.g., checking in on people who live alone).Footnote 257
Since the determinants of health have a broad impact on individual and community health, interventions targeting these determinants offer potential co-benefits across hazards and beyond emergencies.Footnote 7Footnote 34
A focus on co-benefits supports efficiencies and economic benefits, but also helps build resilience to concurrent hazards. For example, the dual impacts of COVID-19 and heat waves challenged typical public health responses, since use of cooling centres may have been limited by concerns about COVID-19 transmission, and physical distancing requirements may have precluded families or neighbours checking in with people facing higher heat risks.Footnote 105 A health promotion lens could help identify opportunities to promote health and well-being across these crises. For example, advocating for changes to the built environment to increase access to shaded green space could help reduce urban heat effects and support physical distancing among those looking for respite from the sun.Footnote 105
Sharing knowledge about how to take action on the conditions for good health is an important potential role for health promotion experts working within emergency management. A qualitative study of emergency managers and social service directors in Canada noted that there is recognition of the importance of addressing social determinants of health to improve emergency management and a desire to move toward prevention, but uncertainty about how best to do so.Footnote 166
Redefine community resilience to address equity and power
Communities are central to emergency management, since exposures and impacts of hazards occur at the local level, and emergency first responders are generally local actors.Footnote 17Footnote 258 Communities can also be the centre of resilience building efforts. While resilience is already a focus within emergency management, health promotion can bring additional insights and ways of defining and supporting community-centred resilience.
At a community level, emergency resilience generally focuses on capacity to adapt to a hazard's disturbances and maintain functioning by persevering, recuperating, or changing.Footnote 2Footnote 258 Many indicator frameworks have been developed to measure elements of community resilience.Footnote 243Footnote 244Footnote 259Footnote 260Footnote 261 Different measures meet different needs. Some measures are focused on assessing the baseline and improvement related to community resilience, whereas others are intended more to support emergency planning based on community characteristics.Footnote 243Footnote 244Footnote 259Footnote 260Footnote 261 For example, indicators that capture the age of community members can be used to help identify specific needs within a community but are not used to assess change in community resilience after an intervention.Footnote 259
Indicators that rely on quantitative data from existing datasets (e.g., income) may be applicable to measure differences between communities and over time. Locally developed indicators can provide more context-specific data to understand and support community experiences (e.g., trust).Footnote 243 Composite measures that use quantitative and mapped geographic data are also popular, but have been criticized for being reductive, and for suggesting resilience is static.Footnote 262 Some measures are aggregates of individuals characteristics within a community (e.g., the percentage of individuals living in multi-unit housing), while other measures reflect the community as a whole (e.g., presence and nature of local infrastructure).
A systematic review examining community resilience related to disasters identified possible core elements, including local knowledge, community networks and relationships, communication, health, governance and leadership, resources, economic investment, preparedness, and mental outlook (see Table 1. "Possible core elements of community resilience related to disasters").Footnote 263 More work is needed to determine the relevance and applicability of these elements for different contexts.
| Element of community disaster resilience | Details and/or sub-elements |
|---|---|
| Local knowledge | Factual knowledge base of the community, including knowledge of local vulnerabilities to disaster, elements of preparedness Training and education, including capacity building related to emergency response Collective efficacy and empowerment, including a shared belief in a community's ability to overcome effects of disaster |
| Community networks and relationships | Connections and social relationships across community Cohesion, including trust and shared values |
| Communication | Effective communication, including strong communication infrastructure Effective risk communication, including understanding of community norms and social context Crisis communication systems that can provide up-to-date information to community during emergencies |
| Health | Pre-existing physical and mental health of community members Capacity to maintain the delivery and quality of health services during and after emergency |
| Governance/leadership | Infrastructure and services, including ability to respond effectively, efficiently, and quickly during and after emergency Public involvement and support, including local engagement in emergency planning, response, and recovery |
| Resources | Adequate and accessible natural, physical, human, financial, and social resources |
| Economic investment | Distribution of financial resources after disaster Investments to rebuild local economy |
| Preparedness | Completion of preparedness plans, risk assessments, and practice exercises |
| Mental outlook | Attitudes and feelings when facing uncertainty, with key concepts such as hope and adaptability |
Scholars in Canada have offered critiques and re-conceptualizations of resilience relevant for health promotion. They have noted that resilience definitions may focus on self-reliance and the status quo, rather than engaging with issues of power, justice, and equity.Footnote 192Footnote 264Footnote 265 Indigenous scholars have identified the "unjust necessity" of resilience among Indigenous Peoples, drawing attention to the devastations of colonization and associated social, economic, environmental, and political injustices.Footnote 266 Further, they have emphasized how a focus on resilience can redirect responsibility from government to individuals and have called for new conceptualizations of resilience centred on the strengths of Indigenous communities and cultural knowledge.Footnote 201 These critiques have been echoed in relation to other communities facing differential risk.Footnote 267Footnote 268Footnote 269Footnote 270
Researchers have recently introduced the concept of community-centred resilience.Footnote 191Footnote 245Footnote 271 Whereas community resilience is often used to reflect capacity to cope with emergencies, community-centred resilience offers a more proactive and all-hazards approach, focused on sustainably and equitably resourcing and partnering with communities to broadly improve community health and well-being.Footnote 191Footnote 245Footnote 271 The components of community resilience may be seen as the resources that communities need to be able to help implement key emergency preparedness and response activities. In contrast, community-centred resilience identifies an approach to sharing power with community. This involves equitably providing resources so communities can identify and implement actions on their own priorities that strengthen community well-being. A community-centred resilience perspective would help strengthen components of community resilience, but such an approach also goes beyond those components of resilience to address the inequitable allocation of risks and resources across communities.Footnote 191Footnote 245Footnote 271
Strengthen social infrastructure and support community leadership
"We have a lot of control within our organization, but that's not where a lot of disasters and responses are. They're out in the communities. We need to work with emergency social services, with municipality. So how do we build these relationships? How do we work closer with them? And also how do we support them in their health promotion pieces?"
Within emergency management, proactive prevention and mitigation measures often focus on infrastructure, particularly "hard" infrastructure related to structural (e.g., storm sewers, electrical grids) or non-structural (e.g., building codes) activities.Footnote 2Footnote 245 A health promotion lens supports and encourages a lens that also incorporates "social" infrastructure. Social infrastructure is a broad term that contains the organizations (e.g., grassroots organizations, social services organizations), spaces (e.g., parks), and services (e.g., childcare) within a community. It includes how these resources build and sustain communities through service delivery, social connections, and community engagement.Footnote 245Footnote 272Footnote 273
A community's social infrastructure is made of a wide range of organizations, each with a potential role during an emergency and in community-centred resilience.Footnote 191Footnote 245 This includes organizations centred on social services, recreation and arts, grassroots mutual aid, and/or community development (see Figure 10).Footnote 245 Community organizations serve a wide variety of critical functions. For example, organizations that serve newcomers provide settlement supports in areas such as language training, education, employment, housing, health care, and building community connections.Footnote 274Footnote 275 These services are particularly important in the current context, since 23% of the population was, or had ever been, a landed immigrant or permanent resident in Canada in 2021.Footnote 276 This is the highest proportion among the G7, and the largest since Confederation.Footnote 276

Figure 10 - Text description
The figure is a table, with columns for types of community organizations, examples of this type, the governance structure, and the role in community-centred resilience of each.
Type of community organization: Community services
- Examples: Public libraries, recreation centres, public health departments, and schools.
- Governance structure: Organizations with multiple branches and centralized governance and decision making, so may not be able to facilitate local community-driven initiatives.
- Role in community-centred resilience: Can be a conduit between formal systems and communities; often have large local facilities that can be used for preparedness and response activities.
Type of community organization: Social service organizations
- Examples: Foodbanks, employment centres, immigration services, legal aid, counselling centres.
- Governance structure: Generally local or centralized governance; focus is on meeting urgent individual needs.
- Role in community-centred resilience: Play essential role in supporting individuals and families with chronic or acute needs, focus is generally individual-level rather than facilitating collective action.
Type of community organization: Interest focused organizations
- Examples: Arts organizations, recreational sports leagues, after-school programs.
- Governance structure: Generally local or centralized governance; focus is on supporting shared interests.
- Role in community-centred resilience: Can play important roles in response, but generally not focused on broader community action.
Type of community organization: Grassroots organizations
- Examples: Mutual aid networks, peer-to-peer support groups, faith-based organizations, residents' and neighbourhood associations, Indigenous urban organizations.
- Governance structure: Deeply rooted at local level; governance could be formal or informal; could focus on urgent needs, community organizing or advocacy.
- Role in community-centred resilience: Critical for community-centred resilience, deep connections to local knowledge and community leaders.
Type of community organization: Community development organizations
- Examples: Neighbourhood resource centres.
- Governance structure: Governance and decision making based in community with focus on grassroots and resident participation, processes, and local capacity for community-led solutions to local issues.
- Role in community-centred resilience: Critical for meaningful community-centred resilience since activities are based on local context, lived experience, and local knowledge.
Type of community organization: Community backbone organizations
- Examples: Local integrators or intermediaries (e.g., East Scarborough Storefront, Notre-Dame-de-Grâce Community Council).
- Governance structure: Similar to community development organizations but primary focus is facilitating connections, strategy and action across community leaders and organizations.
- Role in community-centred resilience: Well-suited to bridge across local and formal organizations and facilitate collective efforts on prevention, preparedness, response, and recovery.
Source: Figure adapted from Poland, B, et al., A Connected Community Approach: Citizens and Formal Institutions Working Together to Build Community-Centred Resilience (2021).
As with investments in physical infrastructure, strengthening social infrastructure may help reduce the likelihood that a hazard will result in an emergency.Footnote 16Footnote 245 Resources for social infrastructure can support prevention and mitigation by increasing resilience through community-led action to meet urgent needs, build social cohesion, and engage with government to improve the determinants of health.Footnote 277Footnote 278Footnote 279Footnote 280Footnote 281Footnote 282 During preparedness and response, a strong social infrastructure can assist with meeting community needs through direct service provision and by facilitating community engagement with formal emergency management systems.Footnote 191Footnote 245Footnote 271
These important roles do not mean that responsibility for resilience should be downloaded to community members and organizations. Support for social infrastructure must occur alongside broader structural- and community-level action.Footnote 191Footnote 245Footnote 258 Further, to ensure action is informed by local knowledge to meet local needs, resources for social infrastructure can focus on community priorities and leadership.Footnote 283
A focus on social infrastructure may shift attention from community vulnerability to community assets and strengths. Community assets can be used to protect and promote health, and include social, physical, financial, environmental, or human resources.Footnote 284 An asset- or strengths-based orientation prompts attention to existing community resources as well as to how these resources can be further supported.Footnote 166Footnote 284 This involves identifying and mapping community assets.Footnote 285Footnote 286 This approach is a cornerstone of health promotion in public health and has more recently been explored for its potential contribution to emergency preparedness and risk reduction.Footnote 18Footnote 80Footnote 287Footnote 288Footnote 289 Bolstering community assets can contribute to healthier communities before an emergency occurs, as well as help mobilize these assets during emergency.Footnote 18 It is important to invest in this process early. Identifying and strengthening assets, including specific assets needed during an emergency, requires time and resources.Footnote 18
These efforts to strengthen social infrastructure can be supported specifically through long-term resources for community organizations.Footnote 191Footnote 283Footnote 290 Much of the funding available to community organizations is project-based. Such funding, requiring significant administrative resources to apply for and manage, leaves organizations vulnerable to financial instability, leads to inequities in funding across organizations, and does not cover all costs associated with program development, implementation, and evaluation.Footnote 291 Project-based funding often targets pre-defined outcomes rather than addressing community-based priorities or supporting community leadership.Footnote 245
"With project-level funding, the outcomes are created by people who aren't at the community level working. Someone or a committee decides these are the outcomes that we expect for 5 years under this project. In the middle of that 5 years, if an [emergency] happens, we as community no longer can respond immediately because we are tied into these squares of outcomes that have been decided by others. It fundamentally changes our business continuity plan and all of our work within community around emergency preparation and response."
In contrast, unrestricted or core operating funding may offer security and flexibility while supporting the sustainability of community organizations, their connections and networks, and their responsiveness and innovation to new challenges, such as emergencies.Footnote 290Footnote 291 Several foundations and corporate funders in Canada increased funding flexibility to community organizations during the pandemic, assisting organizations to be adaptive and resilient during crisis.Footnote 292 Like other pandemic initiatives, it is important to explore where and how these types of resourcing innovations might be appropriate for ongoing consideration. It is also important to ensure that funding is equitably distributed across communities so that everyone has access to the resources and benefits that are fostered by robust social infrastructure.Footnote 245Footnote 293Footnote 294
"A lot of community agencies are under-funded, under-resourced and if we are coming to them, they want to know exactly what we're reaching out with… that we're coming to them with potential solutions and asking for their input on it."
Providing sustainable resources for community and grassroots organizations helps ensure that these community connections are quickly available, to community members and formal emergency management systems, as an emergency occurs.Footnote 191 Crises are often times of uncertainty and fear, making it difficult to build connections and cooperation.Footnote 295 Sustained investment before, during, and after emergencies can create infrastructure and relationships to be activated in crisis.Footnote 295Footnote 296 Adequate resources for community members and organizations are also essential to provide compensation for their work and expertise.Footnote 191Footnote 295
"If I had a sustainable number of dollars in terms of preparedness work, not only would we know that we could continue doing that, but it also allows us the opportunity to be able to do other innovative things that we haven't even thought about at this particular point in time. And it allows us the opportunity to be able to provide a service to vulnerable families in our communities that no one else is doing."
The Importance of having an existing community infrastructure was demonstrated during the 2022 to 2023 mpox (monkeypox) outbreak in Canada. Community networks and organizations that served communities at higher risk of infection, mainly cis or trans, gay, bisexual or queer (GBTQ+) men and other men who have sex with men (MSM), were a cornerstone of community-based public health efforts (see text box "Community mobilization as a key element of the mpox response").
Community mobilization as a key element of the mpox response
"It was a lot about partner mobilization. Most of the work was done on the ground with the organizations and specialized health clinics. We really mobilized the same approaches that we use for STBBIs [sexually transmitted and blood-borne infections], and already strong relationships with these partners, so that they became the messengers for the vaccine, safe practices, etc. It was a great success!"
In May 2022, Montreal experienced the first major mpox outbreak in North America. The successful control of this outbreak was achieved through early and continuous engagement with the affected communities, along with the rapid availability of a vaccine for populations who were most at risk of exposure and being disproportionately impacted.Footnote 297 Established and strong relationships among community partners, including those supporting GBTQ+ and MSM, and local public health entities were critical to efficiently disseminate and promote prevention information. The Direction régionale de santé publique de Montréal worked with trusted community organizations to develop tailored mpox prevention and awareness to communicate risks, inform the communities about the outbreak, promote vaccine mobilization, and minimize stigmatization. Vaccinations were made available at mass vaccination sites located near affected communities in addition to sexual health clinics and a mobile clinic. Strategies employed to raise awareness of vaccinations included distributing posters and flyers to local businesses, conducting outreach in busy areas, and disseminating information through social media and a dating app.Footnote 297Footnote 298 As a result of these concerted efforts, over 30,000 individuals in Quebec received at least 1 dose of the vaccine, contributing to the control and containment of the outbreak.Footnote 299
Preparedness
Emergency preparedness is the foundation of response and recovery, and therefore inclusive processes and comprehensive plans are required for effective action.Footnote 300 There is considerable evidence that emphasizes the inequitable impacts of emergencies, as well as the essential role for communities in emergency response.Footnote 4Footnote 7Footnote 8Footnote 34Footnote 296 Health promotion principles and approaches can facilitate the use of this evidence to support robust, community-informed emergency preparedness plans and activities. For an example of how a public health authority is working with government and community organizations to apply these health promotion approaches, see text box "Working with communities and building healthy public policy to improve heat preparedness and response in Vancouver".
Health promotion may also inform the development of emergency preparedness plans so that they account for the full scope of emergency impacts, including unintended impacts from emergency response efforts. This also includes anticipating the potential need for action on healthy public policy during emergencies. Health promotion approaches to community action can facilitate the development of preparedness efforts that are co-designed by communities, anticipate and provide guidance to address emerging equity and ethical issues, and are developed in a way that builds relationships and trust across partners.
Working with communities and building healthy public policy to improve heat preparedness and response in Vancouver
Following the unprecedented heat dome in 2021, Vancouver Coastal Health (VCH) has been working closely with non-governmental organizations to better prepare for future extreme heat events.Footnote 53 Wellness checks by community organizations were identified as a powerful tool to reduce risk during these events. However, VCH heard from community partners that they need more formal advice, resources, and guidance if they are to be true partners in these efforts.
In response, VCH developed the Heat Check-in Supports Project. The objectives of the project are to increase community checks on people most at risk during heat events, and support organizations to prepare for heat events by providing evidence-based resources and training to non-healthcare staff, volunteers, and the public to conduct heat check-ins.
To develop these resources, VCH engaged with local governments and community organizations, interviewing their staff and volunteers, to learn what they and their communities needed. The team also met with community members who might be receiving wellness checks, to determine how these interactions can be empowering and positive, rather than intrusive or paternalistic.Footnote 301 VCH are continuing to foster these community relationships to inform other programs to increase community resiliency.Footnote 302
As part of larger efforts to encourage action on improving living conditions, VCH also reviewed policy tools and regulatory options that could support thermally safe residential spaces. In collaboration with Fraser Health, VCH provided guidance on safe and cool housing for owners and managers of rental and strata housing.
There have also been important larger public policy changes to improve living conditions in extreme heat. The Government of British Columbia is providing $10 million for publicly funded portable air conditioners. BC Hydro expects to install 8,000 air-conditioning units over the next 3 years for people who live with low income and are medically vulnerable to heat.Footnote 303 The City of Vancouver changed city building by-laws to require all new multi-unit residential buildings to have mechanical cooling capable of maintaining an indoor temperature of 26°C or less by 2025.Footnote 304Footnote 305
Prepare for healthy public policy during emergencies
It is important that preparedness efforts reflect the complex context in which emergencies take place.Footnote 300 Preparedness plans can do so by anticipating the need for action on healthy public policy during an emergency. While this may be particularly relevant for protracted emergencies, such as pandemics, research in Canada has underlined the wide-ranging social and economic impacts of a variety of hazards, including flooding and wildfires.Footnote 103Footnote 306Footnote 307 Action on healthy public policy can help reduce the extent of an emergency's direct and indirect impacts on health and the determinants of health, boost resilience, and enable health-promoting behaviours.
The COVID-19 pandemic demonstrated the importance of addressing the broader social and economic impacts of an emergency, including those unintentionally caused by necessary public health interventions. Pandemic reviews specifically emphasized the need to be prepared to protect groups experiencing greater risk and vulnerability.Footnote 163Footnote 308Footnote 309 These reviews identified a number of health promotion interventions that were implemented to address the indirect impacts of the pandemic, including healthy public policies and programs related to food security, income assistance, social protection, employment, family and gender-based violence, and mental health.Footnote 8Footnote 9Footnote 163 Many of these required policy action from other sectors to reduce exposure risk and address key social determinants of health.
The complexity of the pandemic and the need for rapid response created challenges in the design and implementation of some of the policies intended to ameliorate the social and economic impacts.Footnote 310Footnote 311Footnote 312Footnote 313Footnote 314 Anticipating required policy responses for various emergency types as part of preparedness could improve the use of healthy public policy during response (e.g., preparedness planning with transit sectors, to be ready to respond to emergencies that require evacuation or physical distancing). This may also include implementing policies in advance that promote health and well-being before, during, and after emergencies (e.g., paid sick leave).
"An example of this would be paid sick leave. A lot of provinces did respond and said, even in the midst of this emergency, we need to actually make policy changes, healthy public policy... and this was positive to see. Sometimes, unfortunately, there is failure for these things to stick. I think that a health promotion lens could be a good support for making more permanent some of these interventions."
During the pandemic, researchers created a framework to identify potential inequitable effects of public health measures.Footnote 315 This framework was used to evaluate policy actions for possible physical, psychological, and social harms, as well as opportunity costs, across the PROGRESS-Plus equity domains.Footnote 315 These domains are: place of residence, race/ethnicity, occupation, gender/sex, religion, education, socioeconomic status, social capital, among others.Footnote 315 The framework has potential relevance across emergency types, to help identify and mitigate possible inequitable adverse effects of policy and practice actions during emergency response and recovery.Footnote 315
The COVID-19 pandemic also underlined the need to bring a human rights perspective to understanding and addressing the inequitable impacts of emergencies.Footnote 308 For example, a 2023 report by the British Columbia Human Rights Commissioner noted that preparedness efforts should anticipate, and work to prevent and mitigate, a rise in hate speech and hate-fueled violence during a crisis.Footnote 308 This requires attention during preparedness planning, including designing crisis communication strategies that promote inclusion and cohesion and denounce hate.Footnote 308
Establish inclusive community partnerships
"We need to do a better job at listening to what communities are experiencing and what they are looking for, as opposed to assuming we know."
"Including community-based organizations at the table as a voice for folks that have traditionally been left out of the conversations...when all these big policies are being developed around community safety...those folks need safety too."
Partnering with diverse communities to support preparedness has been widely recommended in the wake of the COVID-19 pandemic, as well as in climate disaster preparedness and climate adaptation reports.Footnote 1Footnote 6Footnote 153Footnote 163Footnote 316Footnote 317Footnote 318 This includes involving community as partners to design, plan, implement, and evaluate preparedness activities.Footnote 295Footnote 296Footnote 319 Community engagement can help integrate community knowledge, build trust, support connections between formal and community systems, and structure community roles during crisis. Emergency response often requires rapid action. Engaging with communities in advance of crises can help build trusted relationships and connections with community knowledge, such that they can be quickly leveraged in emergency response.
An inclusive and transparent planning process promotes trust and relationships with community leaders and community organizations.Footnote 8Footnote 300 Trust built before an emergency can facilitate rapid action when a crisis occurs.Footnote 8Footnote 23Footnote 296Footnote 300 Early and ongoing relationship building can help bring the strengths of formal systems and communities together, and support integration between emergency services and existing community networks and structures.Footnote 245Footnote 283Footnote 296 Trust may also be fostered through accountability structures for regular and routine engagement before and throughout an emergency, to guide and evaluate public health responses.Footnote 320
"It's absolutely key that who is at the table is directly connected and working with the population that is harder to reach or new to the community. Who here is working with families that might not have transportation, that might not have food?"
Community organizations played essential roles in the emergency response during COVID-19, but these efforts may have been ad-hoc and related to gaps or challenges in the formal public health response.Footnote 191Footnote 271Footnote 321Footnote 322Footnote 323 Greater structure and clarity about the roles that communities and community organizations can play during preparedness and response could help build more systematic connections between communities and emergency management (for an example, see text box "Newfoundland and Labrador Vulnerable Populations Task Group for the COVID-19 response: An ongoing community and public health collaboration").
"If we really value preparedness over response and recovery, then we might want to invest some resources in supporting those emergency management organizations, for example, to reach out to those community [partners] to have that conversation and build that governance model so that they're not doing it at the last minute as an emergency is unfolding."
Newfoundland and Labrador Vulnerable Populations Task Group for the COVID-19 response: An ongoing community and public health collaboration
The Newfoundland and Labrador Vulnerable Populations Task Group (VPTG) was established in March 2020, with diverse membership representing government and communities (about 60 individuals), to help respond during COVID-19. The group was built on previous relationships between the Department of Health and Community Services and community organizations. Thirteen sub-working groups were formed around topics such as housing and homelessness; food security; rural, remote and Indigenous health; gender-based needs; and persons with disabilities.
Community sector leaders provided public health officials with insights on disproportionate impacts on populations, and public health contributed epidemiological information and were able to adapt public health measures to reflect the needs of these populations. The structure removed silos and hierarchies.
Successful actions taken to meet the needs raised at these tables included the establishment of a provincial food security helpline, a low barrier shelter, a provincial opioid dependence treatment line, a domestic violence helpline, and peer support texting for the deaf community. This approach also resulted in stronger partnerships and collaboration between community organizations to offer a more comprehensive support network for vulnerable populations.
Two evaluations were conducted. Results reflected a desire to maintain the structure to address other public health emergencies and systemic issues present before the pandemic (e.g., affordable housing, food security, poverty, mental health, and gender-based violence).
The VPTG model is well-positioned to become a more formal component of the provincial emergency preparedness and response structure. It represents a successful example of intersectoral community and public health collaboration that can be scoped and scaled to address other public health priorities.
Thank you to contributing Authors:
Niki Legge, MSW, RSW, Director of Mental Health and Addictions, Department of Health and Community Services, Government of Newfoundland and Labrador.
Dr. Janice Fitzgerald, Provincial Chief Medical Officer of Health, Department of Health and Community Services, Government of Newfoundland and Labrador.
"As a reflection [from the] pandemic, I think the biggest elements that really came to the forefront is the need for a very early community engagement and partnership with communities. Communities know their needs. They're going to identify barriers that we might not see coming, from being within."
Partnering with communities allows for a more comprehensive understanding of community needs and assets, which helps ensure planning accounts for local context.Footnote 17Footnote 245Footnote 296Footnote 300Footnote 317 For example, collaborating with communities during preparedness planning assists with identifying key community resources, such as communication assets (e.g., community-oriented social media channels), trusted community leaders who can guide local response and liaise with government (e.g., faith leaders), trusted community organizations (e.g., culturally safe organizations), or physical assets in the community (e.g., vaccination sites that are accessible and acceptable for those facing barriers).Footnote 284Footnote 324 Local and Indigenous Knowledges can support understanding of local ecology and environments as well as culture and traditions.Footnote 123Footnote 139Footnote 231Footnote 233Footnote 325 Partnering with communities is also key to resilience-building efforts focused on identifying local risks and the actions necessary to address them (see text box "Enhanced Vulnerability and Capacity Assessment").Footnote 326
"What assets do communities already have that we can rely on, that they can rely on, during emergency? Some of those assets are leadership assets, some of those assets are communication network assets, some of them are infrastructure assets, which I think is often where the emergency responders' community tends to go… but those communication assets, those leadership assets are actually critically important to emergency response."
Enhanced Vulnerability and Capacity Assessment
The International Federation of the Red Cross and Red Crescent Societies has developed the Enhanced Vulnerability and Capacity Assessment (EVCA).Footnote 326 The EVCA is a tool for communities, with support as necessary from national Red Cross Red Crescent societies, to assess local risks, where risks come from, who is most exposed, and what actions could be undertaken to reduce risk.Footnote 326 The Canadian Red Cross is adapting the EVCA tool and approach for use with diverse communities across Canada. This is part of "Roots for Resilience", a broader initiative between the Canadian Red Cross and the Resilience Institute. This project will support community engagement activities and initiatives related to disaster risk reduction and climate adaptation programming.
Power dynamics and power relationships are also an important consideration, particularly between government, community members, and community-based organizations.Footnote 93Footnote 245Footnote 258Footnote 327 Centring communities as experts and partners and focusing on fostering community power can help move past short-lived mobilization to more systematic and long-term community-centred resilience building efforts. Attention to power and equity is necessary to ensure that an emergency response reduces, rather than reinforces, existing inequities.Footnote 245
"People are not experiencing emergencies in isolation. They're experiencing multiple emergencies often, sometimes concurrently and sometimes one right after the other. We need to think about trauma-informed practice approaches."
Understanding and collaborating with communities is also key to a trauma-informed approach to response and recovery, which is receiving growing attention in emergency management.Footnote 328Footnote 329Footnote 330Footnote 331 Trauma occurs in response to events or circumstances that are physically or emotionally harmful or life threatening, with the potential for long-term negative effects on mental, physical, social, emotional, or spiritual health and well-being.Footnote 329 A trauma-informed approach to recovery does not require a focus on treating trauma specifically, rather it is an overall orientation to policy, programs, and practice that emphasizes minimizing harm and re-traumatization.Footnote 329 It has potential application across sectors. The 2019 CPHO report identified the relevance of trauma-informed approaches to address stigma, and the 2020 CPHO report explored potential applications of a trauma-informed approach to COVID-19 recovery in mental health, health, social service, and educational contexts.Footnote 5Footnote 36
A trauma-informed lens can be applied to preparedness planning so it can be activated within response and recovery (see Table 2. "Trauma-informed recovery planning"). Trauma-informed approaches prioritize community knowledge, building trust, and collaborative community action to support healing and connectedness.Footnote 330 Local knowledge is particularly important to understand how historic traumas in the community may be compounded by recent emergencies.Footnote 330 A focus and response at the community-level is important because trauma can be community-wide and community context can influence individual trauma.Footnote 331
| Trauma-informed approach principle | Application to trauma-informed recovery planning |
|---|---|
| Cultural, historical, and gender issues | Work with local partners to understand community context, strengths, and historic trauma. Prioritize equitable access for all groups |
| Safety | Consider and support physical and psychological safety at all times |
| Transparency and trustworthiness | Strengthen trust with communities through ongoing and transparent communication, be reliable and accountable in follow-up and actions |
| Peer support | Promote local resources and support peer-to-peer collaboration |
| Empowerment and choice | Prioritize community knowledge and prioritize community decision making |
| Collaboration and mutuality | Promote community voices and action and provide options for participation and decision making |
| Source: Table adapted from Rosenberg, Errett, and Eisenman, Working with Disaster-Affected Communities to Envision Healthier Futures: A Trauma-Informed Approach to Post-Disaster Recovery Planning (2022). | |
Plan for equity
Inequities in the direct and indirect impacts of emergencies have led to calls for equity analyses in preparedness plans. This includes the need for plans that promote equity across gender identities, racialized status, 2SLGBTQIA+ identities, and for individuals with disabilities.Footnote 308Footnote 332Footnote 333Footnote 334Footnote 335Footnote 336 Targeting equity within emergencies is a public health priority, recently emphasized by the International Association of National Public Health Institutes and the WHO.Footnote 337 In the "zero draft" of the new pandemic accord, the WHO prioritized equity as a principle, an indicator, and an outcome of pandemic prevention, preparedness, and response.Footnote 338
There are a number of overlapping opportunities to prioritize equity during preparedness planning. This includes applying existing tools (see text box "Tools for health equity analysis"), collecting data that can be disaggregated, learning from community, focusing on equity within existing frameworks (e.g., ethical frameworks or public health system indicators), and addressing the potential for bias in key models and tools (e.g., artificial intelligence).
Tools for health equity analysis
There are a range of tools to help decision-makers understand, integrate, and analyze equity when designing or evaluating programs, policies, and services.Footnote 339 Two prominent tools for health equity analysis are Sex- and Gender-Based Analysis Plus (SGBA Plus) and Health Equity Impact Assessment.
(Sex- and) Gender-Based Analysis Plus
SGBA Plus is an analytic process used by the Government of Canada's Health Portfolio to assess how determinants of health, such as sex, gender, age, race, ethnicity, socioeconomic status, disability, sexual orientation, cultural background, migration status, and geographic location, interact and intersect with each other and broader systems and structures, to shape individual and population health outcomes.Footnote 340 This can support the development of evidence-informed initiatives that promote greater health equity, diversity, and inclusion. Originally, SGBA Plus focused on sex and gender. It has since evolved into an intersectional approach used to assess how broader systems and structures shape individual and population health, including group membership, social context, and systems of oppression (see Figure 11).

Figure 11 - Text description
This figure illustrates some of the factors which can be considered while applying Sex and Gender-Based Analysis Plus. A figure depicting intersectionality is centered within a concentric circle with 4 layers. From the centre of the circle, and moving outwards the figure describes intersectionality considerations related to individual-level factors, group membership, social context, and systems of oppressions.
The centre of the circle depicts the concept of intersectionality, and some of the individual-level factors which can intersect with sex and gender. Six oblong shapes of differing colors overlap and fan out. "Intersectionality" is written in the middle where all the shapes intersect. Each oblong has 2 identity factors written on it. The middle oblong has the word "sex" written on the left and "gender" written on the right. From the word "sex", in a clockwise order, other identity factors are written: geography, culture, income, sexual orientation, education, language, race/ethnicity, religion, age, and (dis)ability.
The second layer of the circle represents group membership considerations such as family, peer groups, and social networks.
The third layer of the circle represents social context considerations such as institutions, privilege, attitudes, norms, and beliefs.
The fourth and final layer on the outside of the circle describes systems of oppression, such as systemic/structural inequalities, colonialism, racism, sexism, ableism, ageism, classism, cisgenderism, heterosexism, religious oppression, and distribution of resources and power.
The term Gender-Based Analysis Plus (GBA Plus) is used throughout the Government of Canada, while the term SGBA Plus is used when applied to health to highlight the role of biological sex in the health context.Footnote 343Footnote 344Footnote 345 Both terms refer to the same analysis. The Government of Canada has been committed to using GBA Plus in the development of policies, programs, and legislation since 1995.Footnote 1Footnote 346
SGBA Plus is a 5-step process that is cyclical in nature (see Figure 12). At each stage in the process the tool guides users through key questions and encourages gathering both quantitative and qualitative data to inform analyses.

Figure 12 - Text description
The figure describes 5 steps of the Sex and Gender-Based Analysis Plus (SGBA Plus) process, and provides examples of questions to ask at each step of the process.
The SGBA Plus process is circular. The 5 steps are spread clockwise around a circle, encompassing central text which describes the key goals of SGBA Plus: make evidence-based decisions, and challenge assumptions and biases. Starting at the top and moving clockwise, the SGBA Plus process includes the following steps:
- Identify the issue
- Identify people and their needs
- Identify inequalities and inequities
- Develop options
- Implement, monitor, and evaluate
Gathering data to inform analysis is required throughout each step of the SGBA Plus process. Examples of questions at each step of the SGBA Plus process to support evidence gathering include:
Step 1: Identify the issue
- Who has identified this problem?
- Are there other ways of understanding the problem?
Step 2: Identify people and their needs
- How do different factors shape who is impacted and change the nature and extent of their impacts?
- How have the needs of individuals and diverse groups been shaped by their histories, their experiences with institutions, and/or by discourses?
Step 3: Identify inequalities and inequities
- What inequalities and inequities exist and who experiences them? Why might they exist?
- Is there any evidence of explicit or implicit discrimination against groups of people in any legislation, program, service, or policy related to the issue?
Step 4: Develop options
- What are the expressed needs and priorities of those impacted by this issue?
- Do the options identified perpetuate existing inequalities? Do they create new ones? Do they address inequities?
Step 5: Implement, monitor, and evaluate
- How will the performance of the proposed initiative be measured throughout implementation?
- Will outcomes or impacts be explored across multiple identities or positions while also considering how they intersect?
Culturally relevant SGBA Plus considers the historic and current issues faced by Indigenous Peoples and the distinct lived experiences not only between but within First Nations, Inuit, and Métis communities. Therefore, different Indigenous organizations each have a unique perspective on how GBA Plus is framed in their communities and are at various stages of developing GBA Plus resources that are specific to their respective contexts.Footnote 348Footnote 349Footnote 350 For example, the Native Women's Association of Canada is working with Canadian Red Cross to apply a distinction-based, culturally relevant, and trauma-based intersectional lens when reviewing disaster preparedness research, project activities, materials, and approaches.Footnote 351
Health Equity Impact Assessments
Health Equity Impact Assessments (HEIA) arose from Health Impact Assessments (HIA). HIA gained significant international traction in the 2000s to provide decision-makers with information about how proposed policies are likely to affect the determinants of health. Although HIA frequently discuss health inequities, there was a need for methodology more focused on equity.Footnote 352Footnote 353 As a result, HEIAs were developed to address this gap by public health authorities in multiple jurisdictions, many of which consider intersecting identities.Footnote 353Footnote 354Footnote 355Footnote 356
Although they are tailored to the local context, HEIA typically guide users through screening, scoping, data collection, impact appraisal, recommendations, and monitoring/evaluation.Footnote 357
Some examples of guiding questions include:Footnote 353
- Does the program or policy acknowledge that different individuals or groups occupy different positions of social advantage in society?
- Does the program or policy acknowledge that unfair differences (inequities) exist in the opportunities or outcomes that are presented to different individuals or groups? Are these differences at the individual, community, or systemic levels?
- Are the root causes of the inequities recognized and are attempts made to address them?
- Has the program or policy been accepted by the target organizations? Have any proposals concerning health equity been accepted?
- Where would be a good forum to disseminate the results of the HEIA?
These are just 2 examples of many tools that can support health equity analysis of interventions (see Appendix A for a list of equity tools for emergency management procedures). Each tool has its strengths and may focus on different aspects of equity assessment. The selection of a particular tool depends on the context, purpose, and needs of the user.Footnote 358
There are also broader tools for equity analysis without a focus on health. One example is the Racial Equity Impact Assessment Toolkit that guides users through examining how different racial and ethnic groups will be affected by a proposed decision.Footnote 359
"When you're doing Hazard Identification Risk Assessments, there is a huge opportunity that you put in equity lens on that risk assessment… maybe integrating a Health Equity Impact Assessment to see what are the disproportionate impacts that are going to hit in certain groups… so that you're going to do your preparedness to make sure that groups who face inequitable risks are going to have greater attention."
Planning for how to integrate community knowledge is particularly important. Community knowledge can help emergency management professionals understand and support the experiences of people whose multiple intersecting identities require additional consideration in emergency contexts. This includes communities connected by identity rather than geography. For example, during the COVID-19 pandemic, 2SLGBTQIA+ youth in Canada faced additional challenges when public health measures to stay at home were implemented, including the potential for abuse and victimization at home due to their sexual and gender identities.Footnote 112Footnote 360Footnote 361Footnote 362Footnote 363Footnote 364 As a result, 2SLGBTQIA+ youth may need additional and tailored resources to address housing, mental health, social support, and substance use challenges during and after emergencies.
Planning for equity can also occur within existing public health frameworks and indicators. This includes the broader ethical frameworks used to guide public health decision making during fast-moving emergencies.Footnote 365Footnote 366Footnote 367 The COVID-19 pandemic demonstrated the importance of ethical principles in public health decision making, including key discussions on trust, justice, human rights, maximizing benefits, and minimizing harms.Footnote 368Footnote 369Footnote 370 Building on these experiences can facilitate adequate attention to both the development and intended application of equity-oriented and ethical decision-making frameworks during preparedness planning. A focus on equity can be further integrated into existing measures of public health system performance (see text box "Applying 'equity prompts' to a public health system readiness framework for emergencies").
"But it's the performance measures, like there has to be some sort of performance system being tied to whether this kind of health promotion activity's occurring. That's part of the obligation to be ready."
Applying "equity prompts" to a public health system readiness framework for emergencies
The National Collaborating Centres for Infectious Diseases (NCCID) and Determinants of Health (NCCDH) expanded public health emergency preparedness indicators developed by Public Health Ontario to measure public health system performance in addressing inequities and integrating equitable approaches across preparedness, response, and recovery.Footnote 300Footnote 371
These equity prompts are intended to support public health authorities to identify which populations are already facing barriers and which could experience disadvantage (or further disadvantage) due to the actions or inactions of public health. They also address equity in community engagement. In a small qualitative study documenting their pilot of this tool with a regional public health organization, NCCDH and NCCID found that the indicator prompts provided a useful structure for conversations on how to explicitly identify, assess, and improve how health equity considerations are included in their organization.Footnote 372
| Original indicator | Prompt to encourage health equity |
|---|---|
| The public health agency's policies align with requirements for reporting to the provincial/territorial and/or federal public health authority on community health risks in the context of an emergency. For example, radio-nuclear, chemical, or biosecurity events. | Risk assessments and reports are explicit about disadvantaged populations and why there are additional risks for certain population groups, including by sex, gender, sexual orientation, age, place of residence (e.g., rural), race, ethnicity, place, and terms of employment. |
| The public health agency's emergency management plans and/or protocols relate to all phases of a disaster (i.e., prevention/ mitigation, preparedness, response, and recovery). | Actions to mitigate inequities and contribute to community resilience are integrated in the agency's emergency management plans/protocols for all stages of a disaster. |
| The public health agency uses locally relevant data to inform risk assessment. Examples of data sources may include: communicable diseases, vector-borne diseases, food and water testing, population health determinants, and noncommunicable diseases, such as injuries. | Data used for risk assessment are collected, available, reported, and presented disaggregated by sociodemographic and socioeconomic factors, including but not limited to, sex, gender, sexual orientation, age, co-morbidities and co-occurring conditions, geographic location (rural, remote, urban), First Nations, Métis, and Inuit, and race. Data are analyzed and used in ways that reduce potential negative associations and stigma for disadvantaged populations. |
| The public health agency provides and/or endorses education programs directed at the public to raise awareness about preparedness for relevant community risks. | Education programs are tailored for a variety of audiences (e.g., format, delivery), taking into consideration languages spoken, literacy levels, cultural safety, availability of on-line technology, and other population-level specifics like age. Education includes community actions that strengthen and draw from community resilience. |
| The public health agency dedicates time for the continuous development of relationships with community organizations relevant to preparedness for local risks and the agency context. For example, building relationships with members of the public and/or advocacy groups that represent the public. | Relationships include representation from persons with previous/lived experience and consideration of social services in housing, income assistance, economic development, and corrections, for example. |
| The public health agency has or participates in an established structure to facilitate inclusion of community considerations in relevant aspects of public health emergency management. For example, a community advisory committee to inform emergency mitigation, planning and/or recovery including members of the public and/or advocacy groups that represent the public. | The "established structure" includes representation by disadvantaged populations and uses structures and mechanisms that facilitate community voice, input, and influence at all levels. Public health agency is able to identify "who is missing?" and why. |
| The public health agency and/or its network partners engage with Indigenous communities regarding emergencies and related risks. Engagement may include community-specific risk assessments, plans and/or protocols, and inclusion of Indigenous knowledge where possible and appropriate. | Explicit inclusion of representation and leadership from First Nations, Métis, and Inuit communities, including urban dwellers, integrated throughout plans and protocols for preparedness, response, mitigation, and recovery. |
| Source: Table adapted from Haworth-Brockman and Betker, Measuring What Counts in the Midst of the COVID-19 Pandemic: Equity Indicators for Public Health (2020). | |
An equity focus requires attention on potential bias within technological tools used in emergency management. These tools, including artificial intelligence and in particular machine learning, have or can be used in areas such as hazard monitoring, disaster risk modelling, vaccine development, vulnerable infrastructure identification, and disaster impact estimates.Footnote 373Footnote 374Footnote 375Footnote 376Footnote 377Footnote 378
As with other applications of artificial intelligence, there are concerns. This includes the potential for bias in the training data sets, in selecting outcomes, or in a focus on aggregate rather than disaggregated data.Footnote 373Footnote 378Footnote 379 In one potential example, bias against communities with lower economic status could occur if risk calculations to determine where to allocate resources rely on data such as property values.Footnote 373 This kind of analysis may determine that communities with higher economic status are more cost-effective to protect against an incoming hazard.Footnote 373 In another example, a machine learning model used to develop community evacuation plans may be biased if the underlying data are not further disaggregated, such as by age and disability.Footnote 373 Such a model would neglect to consider unique evacuation needs, which could result in inadequate or misallocated resources.Footnote 373
Response
Emergency response will always be a crucial component of emergency management. Even with a growing emphasis on prevention, mitigation, and preparedness, people living across Canada will continue to experience significant emergencies. A health promotion lens can bolster a necessary focus on equity and communities during response. This includes building supportive environments that are designed to increase the accessibility and effectiveness of emergency response interventions and guidance. A health promotion lens may also help centre equity-based decision making throughout the response, to monitor and address differential impacts of emergency on populations facing greater risks.
Create supportive environments to promote health and enable behaviour change
Public health emergencies often require individuals to change their behaviour to support their health and safety. This can include changes necessary to adhere to emergency response recommendations focused on health protection. It may further comprise reducing other health risks or accessing health services during emergency. However, the option to change behaviour during an emergency is not equally available to everyone.
Behaviour is influenced by many individual, community, and population factors, such as trust in government, societal inequities, cultural and historic context, health literacy, values, and the built environment.Footnote 324 Initiatives focused on behaviour change therefore require support from fiscal, environmental, legislative, regulatory, communication, or service initiatives.Footnote 324 Emergency response interventions that target only individual behaviour change without exploring the broader social and structural context may not be as effective and could lead to blame and stigma.Footnote 8Footnote 235Footnote 324 An overreliance on behaviour-focused interventions has been a criticism of both public health and emergency management, particularly when it results in "lifestyle drift".Footnote 166Footnote 168Footnote 380 Lifestyle drift occurs when there is recognition that structural determinants of health are causing inequities, but interventions to address these inequities target behaviour change (i.e., promoting healthy lifestyles) rather than tackle those structural determinants.Footnote 381
Health promotion facilitates a deeper understanding of how behavioural choices are supported or constrained by broader environments. It further strengthens the adaptations necessary to provide equitable and accessible opportunities for populations to access relevant interventions (e.g., transportation and housing for those who need to evacuate).Footnote 324 The COVID-19 pandemic demonstrated that behaviour change can be enabled through supportive environments and that additional interventions may be necessary for those who experience barriers to adhere to emergency response recommendations.Footnote 8 For example, interventions to reduce workplace transmission for essential workers could include paid sick leave, on-site rapid testing, and improved protocols for workplace health and safety.Footnote 382Footnote 383
The National Collaborating Centre for Methods and Tools identified in a commissioned review a number of relevant examples of health promotion approaches during COVID-19 that targeted supportive environments.Footnote 9 These included increasing options for physical distancing in congregate living environments, virtual health care, mobile testing sites, culturally appropriate food boxes for households experiencing food insecurity, safe voluntary isolation sites, changes to the built environment, and eviction moratoria.Footnote 9 Another example is the rapid implementation of community-led and culturally safe testing networks during COVID-19 (see text box "Point-of-care community-based testing for northern, remote, and isolated communities"). Interventions such as these can help enable health promoting and protecting behaviours.
Point-of-care community-based testing for northern, remote, and isolated communities
Northern, remote, and isolated (NRI) communities, which have significantly greater proportions of First Nations, Métis, and Inuit Peoples than communities in southern Canada, have historically experienced obstacles to equitable access to healthcare services like diagnostic testing.Footnote 384 This is due to several factors, including lack of access to a healthcare provider, the need to travel to centralized testing locations, long wait times for results, and concerns about confidentiality and stigma. As a result, there can be delays in diagnoses and treatment, and challenges with implementing effective public health measures to stop transmission of infectious diseases.Footnote 384
During the COVID-19 pandemic, many NRI communities undertook the development of community-based rapid point-of-care testing for COVID-19 with support from the National Microbiology Laboratory (NML) and Indigenous Services Canada. NRI communities worked directly with the NML to acquire diagnostic testing devices and access supportive training, as well as building capacity to design and perform their own COVID-19 testing prior to the widespread availability of rapid-antigen tests.Footnote 34 Many years of pre-pandemic relationship building between NRI communities and the NML enabled health authorities to identify the communities most in need.Footnote 385 Over the course of 32 months, this initiative provided over 3 million tests at more than 400 sites.Footnote 386
The success of this project is also an example of how community-led initiatives built upon trust, and respect for community rights of self-determination, can ultimately lead to ongoing interventions that increase resilience. Partners have identified ways to expand the community-based testing network beyond COVID-19 to cover community goals for other types of testing, including for sexually transmitted and blood-borne infections, such as HIV, hepatitis C, and syphilis. One of the priorities of community leadership was that First Nations, Métis, and Inuit communities be able to direct the expansion of testing in their communities and take ownership over their own health care.Footnote 386
A rapid evidence profile completed by COVID-END identified a number of policies and programs that were implemented with the goal of enabling health promoting behaviour.Footnote 387 Many of these were focused on building a supportive information environment. This includes educational or informational initiatives reinforced by adaptations to physical infrastructure (e.g., floor markers or one-way routes to support physical distancing), as well as partnering with community to deliver educational or outreach programs (e.g., building trust in public health messages through community-led initiatives). See text box "Building a supportive information environment to encourage health promoting behaviour" for more examples.Footnote 387
Building a supportive information environment to encourage health promoting behaviour
In addition to the social, economic, and built environment, the information environment can also drive behaviour. Supportive information environments are particularly important to help counter mis- and disinformation. Mis- and disinformation lead to increased polarization, decreased public trust, lower adherence to public health advice, and illness and death from preventable diseases.Footnote 388 A study estimated that mis- and disinformation contributed to vaccine hesitancy for an estimated 2.35 million people in Canada between March and November 2021.Footnote 388 By November 2021, without these refusals or delayed vaccinations, there could have been an estimated 198,000 fewer COVID-19 cases, 2,800 fewer deaths, and $299 million saved in hospital costs.Footnote 388
The role of community action to build supportive information environments is especially necessary to reach populations who experience stigma and discrimination and mistrust government and/or public health as a result.Footnote 324Footnote 389 The National Collaborating Centre for Indigenous Health (NCCIH) used strength-based communication to address the spread of mis- and disinformation and increase vaccine and public health measures acceptance for Indigenous Peoples. The NCCIH mobilized Indigenous-informed evidence through collaborations and partnerships, first conducting a survey to identify information needs and priorities for First Nations, Inuit, and Métis communities. They used various communication media that were grounded in the strengths and wisdom of First Nations, Inuit, and Métis teachings. These media included a COVID-19 quick links webpage, a series of webinars with Indigenous organizations and experts, podcasts with Indigenous experts, and animated videos and resources to address COVID-19 stigma, vaccine hesitancy, and vaccine confidence.Footnote 390
A health promotion approach can also use the lens of supportive environments to help adapt existing health programming during an emergency. Public health emergencies may limit healthcare service delivery if resources are shifted to address urgent crises. For example, the COVID-19 pandemic presented challenges to sexual health care, and sexually transmitted and blood-borne infection service providers developed new delivery models to overcome these barriers. This included remote services, mobile outreach for testing services, needle equipment distribution programing, and providing curbside self-serve harm reduction supplies.Footnote 86
Engage communities to strengthen trust and social cohesion
Building trust through community engagement is essential to create an environment that supports health promoting behaviour. The role of trust during the COVID-19 pandemic has been emphasized in international research, including associations at the population level between higher governmental or institutional trust and lower COVID-19 cases or mortality.Footnote 391Footnote 392 At the individual level, trust and social cohesion were associated with higher levels of face mask wearing, physical distancing, and vaccination.Footnote 8
"Governments are not the first trusted source of information. It's going to be their Elders or key people in the community who they trust, or non-governmental organizations that have that interface with them. We wait and build that trust, but they may not recognize that the government is a trusted source of information. If they do connect with you in a partnership, it is because they have started to trust you and your leadership"
The infodemic during the COVID-19 pandemic, including widespread mis- and disinformation, contributed to distrust.Footnote 393 Research from during the COVID-19 pandemic suggests that trust requires community engagement, as well as communication approaches that reflect community context, are timely, transparent, evidence-based, and action-oriented.Footnote 238Footnote 393Footnote 394Footnote 395 One example of community outreach and engagement is detailed in the text box "'Bonjour! Comment ça va?' - From response to recovery: The Laval Awareness Brigade, Quebec".
"Bonjour! Comment ça va?" - From response to recovery: The Laval Awareness Brigade, Quebec
"Bonjour! Comment ça va? (Hello! How are you?)" It is with this simple question that the Laval Awareness Brigade approaches citizens in Laval, Quebec.Footnote 396 Instigated in May 2021 by the Direction de santé publique de Laval of the Centre intégré de santé et de services sociaux (CISSS) de Laval, the "Brigade COVID-19" was set up to share information on testing and public health measures and raise awareness about the importance of the COVID-19 vaccine.
The multilingual (7 languages in total) and multigenerational brigade did 2,559 outreach engagements and met more than 90,000 citizens via door-to-door visits, at bus stops, libraries, shopping centres, or during local activities. The outreach workers used a personal approach to refer citizens to relevant resources and community organizations.Footnote 397
In 2022, the Brigade was repurposed as the Laval Awareness Brigade (Brigade sensibilisation Laval) with a focus on supporting recovery and psychosocial well-being.Footnote 398 In partnership with the non-profit organization Coopérative de soutien à domicile de Laval, the Brigade mobilized 20 to 24 non-healthcare outreach workers trained by the Canadian Red Cross, community organizations and CISSS Laval.Footnote 397 An important part of the brigade's new mandate is to listen to the needs of the community and inform the adaptation of interventions. During recent emergencies, such as the April 2023 ice storm, in collaboration with the City of Laval, the outreach workers visited vulnerability zones known to the brigade and informed citizens about the risk of carbon monoxide poisoning caused by generators or other gas-powered devices. During the May 2023 floods, the brigade was preventively deployed in flood prone areas, considering the trauma experienced by some citizens during the 2017 and 2019 floods.Footnote 397
A community advisory committee and a liaison committee facilitated relationship building between local partners and optimal collaboration with the community tables.Footnote 397 The Brigade is being evaluated as part of a research study that explores how outreach community practices can support health and social services.
Integrate equity into response processes
Equity needs to be considered in real-time and embedded as part of emergency response activities. Doing so requires understanding of the emergency's potential inequitable impacts, applying equity analysis tools as emergencies unfold, and integrating an equity focus within formal emergency response operations.
Prioritizing equity during emergencies requires public health and emergency management practitioners to be able to understand how different groups are affected. This can be supported by community knowledge, disaggregated surveillance data, and academic research on the inequitable direct and indirect impacts of emergencies on health and the determinants of health.Footnote 23Footnote 316Footnote 371Footnote 399Footnote 400 This includes ensuring access to data in a culturally safe manner, respecting the rights of Indigenous communities to own, share, and control their own data, and addressing significant data gaps for First Nations living off reserve and Inuit and Métis Peoples living outside of community and in urban settings, such as being able to provide distinction-based analyses.Footnote 34Footnote 401Footnote 402Footnote 403
Access to data on inequities can guide critical decision making during response, including equitable resource allocation and the distribution of scarce resources.Footnote 338Footnote 371Footnote 404 Decision making can also be supported by applying the equity tools discussed during preparedness planning (see text box "Tools for health equity analysis"). In the midst of emergencies, when decisions must sometimes be made very quickly, an accelerated tool may be necessary, such as the Public Policy Analysis Tool for Rapid Decision Making in Public Health developed by the National Collaborating Centre for Healthy Public Policy. This tool guides users through 17 questions covering a broad spectrum of issues, including equity and unintended effects on health and its determinants.Footnote 405
It is also important to consider opportunities to embed equity expertise directly into decision-making structures. This can be accomplished by integrating an equity expert within emergency operations. Emergency response often uses an Incident Management System or Incident Command System. Both are standardized approaches to emergency management that encompasses personnel, facilities, equipment, procedures, and communications within a clear decision-making hierarchy and regulated procedures. It is scalable and gives communities and organizations a recognizable framework and command structure to communicate, coordinate, and collaborate in complex situations. An Incident Command System is site-specific and often used in field-level operations while an Incident Management System is typically used in emergency operations centres, for non-site-specific responses, or for complex long-term health emergencies.Footnote 160Footnote 406
During the COVID-19 pandemic, several jurisdictions in the United States recognized the need to explicitly address health equity within formal response structures. As a result, some operations centres advocated for and designated a Health Equity Officer or health equity team as part of the core member of the command structure.Footnote 407Footnote 408Footnote 409Footnote 410 The responsibilities of this Officer included strengthening disaggregated data collection and monitoring, interfacing with community-based organizations, ensuring the use of culturally appropriate communications channels, and bringing an equity lens into executive decision making.Footnote 408Footnote 410 One local government reported that embedding an Equity Officer into their COVID-19 emergency operations centre led to better identification of and action on urgent community needs, especially for groups who were disproportionately impacted.Footnote 408
Recovery
Public health has many potential roles in emergency recovery, including ongoing surveillance and communication, identifying the needs of diverse groups, and working with the rest of the health system on the provision of health services.Footnote 411 A health promotion lens offers additional priorities, including building resilience for the future, engaging with communities, and evaluating for learning and improvement. These efforts can support forward-looking approaches to reduce vulnerability.
Build resilience into recovery
Recovery is seen as a time to return to, or improve upon, the way things were before an emergency. During recovery, it is particularly important to consider opportunities to address inequities that emerged or were exacerbated by the emergency. This could include addressing areas such as infrastructure restoration and ecosystem recovery (e.g., impact to the land, animals, and traditional foods) with First Nations, Inuit, and Métis communities.Footnote 231 A health promotion lens may provide a useful frame to support recovery efforts that go beyond short-term pressures to promote long-term social and economic resilience.Footnote 316Footnote 412
Based on research related to the COVID-19 pandemic, resilience-oriented recovery can include long-term and intersectoral policies in areas such as early child development, quality education, good jobs, adequate living income, vibrant and healthy communities, a high-quality care sector (including long-term care), affordable and sustainable housing, and addressing racism and discrimination.Footnote 20Footnote 163Footnote 254Footnote 316Footnote 413Footnote 414 These policies echo those highlighted to support prevention and mitigation, because a health promotion lens prioritizes a consistent focus on conditions necessary for good health across the emergency management continuum.
Emergencies are opportunities to collaborate across sectors, and the recovery period can be used to expand on these collaborations to achieve progress on policy goals and build towards resilience.Footnote 163Footnote 316 As a component of COVID-19 recovery, the United Nations has called for further research on how to effectively work with non-health sectors to prioritise health promoting policies.Footnote 316 Similarly, the Pan American Health Organization asked for health transformation to focus on intersectoral interventions on the social determinants of health.Footnote 163
When considering how to build resilience through emergency recovery, it is important to consider different experiences during an emergency. For example, some chronic health issues caused by emergencies can persist for months or years.Footnote 15 This includes direct (e.g., smoke inhalation during wildfires, post-COVID-19 condition) or indirect (e.g., mental health challenges associated with evacuation or property destruction) impacts of emergencies, as well as lasting effects from disruptions to essential services, like health care (e.g., delayed surgeries or diagnostic care).Footnote 73Footnote 74Footnote 77Footnote 415Footnote 416Footnote 417 Tracking long-term outcomes associated with emergencies is important, especially to understand inequitable impacts.Footnote 1Footnote 67Footnote 80
Inequitable impacts during an emergency also mean that recovery does not start at the same time, from the same stage, or with the same resources, for everyone. For example, during the COVID-19 pandemic, women in Canada were disproportionately burdened by social and economic impacts resulting from caregiving responsibilities, job losses, and experiences of violence.Footnote 418Footnote 419 This was particularly the case for women who are racialized, Indigenous, or living with a disability.Footnote 418Footnote 419
Foster an ongoing role for communities
In addition to intersectoral collaboration to build resilience, a health promotion approach to recovery emphasizes the importance of partnering with and supporting communities. This requires an ongoing focus on prioritizing community knowledge, rebuilding social infrastructure, and supporting social cohesion following an emergency. Engaging communities has been identified as key to recovery, to ensure local and Indigenous voices and Knowledges are centred within research, program and policy design, collective action, and decision making.Footnote 316Footnote 411
"We have the opportunity, obviously in government broadly, but in public health and institutional public health, to facilitate more community participation in recovery stages and from building back. I think that it will be more successful if we have long term partnerships with community organizations."
Traditional emergency management approaches may engage outside experts to provide short-term support. Partnering with local community organizations for recovery can increase the relevance of recovery efforts and contribute to ongoing community-centred resilience.Footnote 191Footnote 328Footnote 420Footnote 421 With adequate resources, local community organizations can offer longer-term and community-driven assistance across the emergency management continuum.Footnote 420Footnote 422 Evidence from emergencies, such as 2018 flooding in Grand Forks, British Columbia, the 2012 wildfire evacuation by Dene Tha' First Nation, and the COVID-19 pandemic, demonstrate that community leadership is key for effective response, recovery, and short- and long-term resilience.Footnote 245Footnote 423Footnote 424
Recognizing and facilitating a central role for communities is reflected in trauma-informed approaches to recovery. For example, community members may avoid participating in recovery initiatives that remind them of the trauma of the emergency, which can impede the relevance and success of recovery efforts.Footnote 330 Tangible ways to support inclusion in community meetings could include reviewing location exits and safety resources at in-person meetings, acknowledging trauma and offering mental health resources, compensating community organizations and partners for their role in engagement, and ensuring ample time for community members to share stories and collaboratively make decisions.Footnote 330 It is also necessary to understand the inequitable impacts of trauma and work to ensure inclusive and trauma-informed recovery across and within communities.Footnote 330Footnote 331
A health promotion approach to recovery can facilitate a focus on social cohesion, which is critical for designing and implementing recovery initiatives.Footnote 316 Leveraging social connections for action is valuable, but it also may be necessary to help rebuild them after an emergency. This was seen during COVID-19, when physical distancing, including school closures, working from home, and cancelling in-person social and cultural events, disrupted social connections.Footnote 316 Bringing community together for recovery can rebuild trust and social cohesion, while supporting equitable and effective recovery activities (see text box "A community-based approach to recovery: The Lac-Mégantic train derailment").Footnote 316
A community-based approach to recovery: The Lac-Mégantic train derailment
On July 6, 2013, a train carrying 72 cars of crude oil derailed in Lac-Mégantic (Quebec, Canada), causing a major fire and a series of explosions. This technological disaster resulted in 47 deaths and the evacuation of one third of the local population, and generated significant health, social, economic, and environmental impacts.Footnote 57
The Direction de santé publique for the Estrie region used a community-based approach in their response to this event.Footnote 425 This included ongoing population-level data collection, which incorporated asset measures (e.g., resilience, positive mental health), community reflection and asset mapping, as well as co-development of a recovery plan that prioritized psychosocial support and community connections and involvement.Footnote 80Footnote 287Footnote 288Footnote 289 For example, a permanent outreach team was established and organized a variety of community initiatives, such as a walking club, a photovoice project to map community assets, and entertainment events in a new outdoor gathering space.Footnote 289Footnote 421
This work was inspired by the EnRiCH community resilience framework for high-risk populations, which focused on addressing disaster risk in a manner aligned with health promotion. Three elements were identified as critical to the success of this work: a focus on community strengths and engagement, political commitments to prevention, and public health resources to support the project.Footnote 80Footnote 287Footnote 288Footnote 289
These efforts were future-oriented, intended to promote resilience, but also included prevention and mitigation work related to future emergencies. During the COVID-19 pandemic, for example, the outreach team was able to quickly adapt its interventions to offer support and activities to the community.Footnote 425
Improve future preparedness and response efforts
Recovery is a time to review what worked and what did not work during emergency preparedness and response, and how these lessons can be used to improve efforts across the emergency management continuum. It is also a time to build on, expand, and embed initiatives implemented during crises that have the potential to improve equity and resilience across hazards into the future.Footnote 300 For example, the COVID-19 pandemic changed how people engage with their built and natural environments. Local efforts to support health promoting activities during the pandemic (e.g., access to green space) could be maintained and formalized given the ongoing health and environmental co-benefits.Footnote 316
When determining what worked during an emergency and how to embed it into future decision making, health promotion principles can help prioritize community engagement, equity, intersectionality, and human rights in research and evaluation.Footnote 316 The United Nations Research Roadmap for the COVID-19 Recovery emphasized the importance of meaningful participation with affected communities in evaluating solutions based on their priorities and preferred outcomes.Footnote 316 Such an approach can help change power dynamics and advance more collaborative research and evaluation approaches.Footnote 316
"In terms of recovery, one of the things we don't always do well, if you look at it from a purely emergency management standpoint, is the evaluation. We do these after-action reviews, but that's very internally focused. It doesn't actually ask the question in the communities, which is a health promotion approach, to say How did this look on the ground for you? What can we do better next time?"
There is potential to bring this lens to existing emergency management learning instruments, such as the After-Action Review (see text box "Example of equity in emergency exercises and after-action reviews"). After-Action Reviews occur at the end of an emergency response, with the aim of bringing stakeholders together to identify what worked, what did not work, and how lessons can be applied to future responses.Footnote 426
Example of equity in emergency exercises and after-action reviews
In February 2023, the Federal Government Operations Centre coordinated the National Priority Exercise, Coastal Response 2023 (CR23), which simulated a magnitude 6.8 in-slab catastrophic earthquake in the lower mainland of British Columbia. The CR23 included approximately 200 whole-of-society partners from across the Emergency Management community. The Government Operations Centre used a GBA Plus lens to design the exercise. Participants were required to consider urban, suburban, vulnerable, and Indigenous and First Nations communities (including those that are remote), in various terrains such as coastal and mountainous regions. These communities were also represented in all exercise planning meetings. The after-action reporting was developed in consultation with these partners to identify best practices and areas for improvement for integration into the capstone exercise design. Following the exercise, the Government Operations Centre conducted after-action activities and the results of which will be summarized and circulated to federal partners for their integration and application for future events in 2023 to 2024.Footnote 427
Thank you to contributing Author:
Continuous Improvement Program, Government Operations Centre, Public Safety Canada
For emergencies that occur over a longer-term, such as the COVID-19 pandemic, it is also important to include In-Action Reviews, to ensure ongoing learning throughout the emergency response. The WHO incorporated equity-oriented pillars within their guidance on In-Action Reviews for COVID-19, such as how populations whose conditions make them vulnerable were considered in the response.Footnote 428 However, there is need for further progress. A 2022 global analysis of In-Action Reviews showed that there is inadequate attention to these populations in existing reviews.Footnote 428
Way forward
Emergencies are becoming more frequent and intense in Canada, as we have recently witnessed with the COVID-19 pandemic and extreme climate-related events. These emergencies can cause significant impacts to the physical and mental health of people in Canada and exacerbate existing health inequities. New ways of understanding and addressing emergencies are urgently needed.
Response will always be core to emergency management, but the growing impacts of emergencies also require greater attention to prevention, mitigation, recovery, and resilience against all types of hazards. It necessitates action on the environmental drivers of emergencies (e.g., climate change), as well as on the structural and social determinants of health. This includes working to achieve equitable and community-centred resilience. As a whole-of-society project, all sectors have a role to play in addressing the determinants of health and strengthening communities.
Public health's role can be informed by a health promotion approach that focuses on equity and the social, economic, and environmental conditions that keep people healthy and well. At the heart of this approach is cultivating trusted partnerships with communities to target structural change, advance community-led priorities, and build supportive environments that enable health-promoting behaviours. Working in collaboration with communities this way assists public health and emergency management practitioners to adapt interventions to local contexts and needs, which is essential in the face of emergencies.
This work is tightly connected to broader public health system transformation, which calls for a greater focus on prevention, community leadership, and collaboration across sectors. In order to achieve this, additional resources are needed for public health systems and communities, especially local level organizations, to sustain their work in supporting community well-being before, during, and after emergencies.
Recognizing the historic and ongoing stewardship of Indigenous Peoples, and First Nations, Inuit, and Métis Knowledges and practices, can inform prevention and mitigation initiatives. In keeping with Canada's action plan to achieve the objectives of the United Nations Declaration on the Rights of Indigenous Peoples, we need to support the inherent right to self-determined decision-making for First Nations, Inuit, and Métis communities as it relates to emergency management. This includes strengthening dedicated and sustainable resources to support Indigenous-led community-based emergency management and Indigenous leadership on the areas of action below.
While 2024 marks the 50th anniversary of the Lalonde Report and the beginnings of modern health promotion, the concept of health promotion has never been timelier. Canada has an opportunity to build on this historic precedent and the subsequent Ottawa Charter for Health Promotion by bringing this approach to the urgent and growing discipline of emergency management. In doing so, Canada can reinvigorate its leadership role in international health promotion efforts and champion community resilience as foundational for health security.
Priorities for bringing a health promotion approach to emergency management
The following highlighted priorities focus on areas that public health and emergency management practitioners can intervene on together, at the systems level. For a more fulsome list of tangible actions to advance these and other systems-level priorities identified in the report, see "Actions to apply health promotion to emergency management".
Prioritize community across the emergency management continuum
This means partnering with communities to integrate local knowledge, strengthen social infrastructure, and build trusted relationships and social cohesion. Emergency planning requires community leadership to ensure equitable processes and outcomes, and continuous engagement with communities to understand the differential impacts of policies and programs and identify leading practices. Ongoing resources are required to enable the full participation of communities in emergency efforts, including simplifying and streamlining funding mechanisms across sectors. Public health and emergency management workforce development is also needed to support practitioners to better engage communities and build long-term, culturally safe relationships.
Systematically integrate health promotion into emergency management policies, plans, and procedures at national, regional, and community levels
This requires health promotion expertise at emergency management decision and operational tables (e.g., health equity liaison officers), as well as the application of equity- and community-oriented tools (e.g., equity checklists and indicators, "rosters" of existing community networks/organizations). It also means embedding community engagement as a key component of emergency management plans and procedures. Cross-training opportunities will be needed for public health and emergency management teams to effectively exercise, apply, and evaluate this new approach to pandemic and other emergency plans and procedures.
Embed equity in emergency management science, evidence, and technology
As with other complex public health problems, integrated and timely surveillance systems are needed that can provide disaggregated data to identify differential risks, vulnerabilities, and inequitable outcomes related to emergencies. These systems must also be able to support the collection of longitudinal data to monitor long-term outcomes from emergencies on the health of populations and communities, and the underlying conditions that influence health. Research is needed as well; broad research on how to build effective health promotion approaches and tools into emergency management, and more targeted research to understand how to enable health-promoting behaviour during emergencies. Identifying and addressing issues of bias in key emergency management technologies and modelling can help further embed a focus on equity.
Actions to apply health promotion to emergency management
Facilitate collective action on the determinants of health
- Promote intersectoral action across the emergency management continuum, to target the environmental, economic, and social factors that influence health and leave some populations more vulnerable to emergencies and with fewer resources to respond.
- Create funding opportunities to support intersectoral action on the structural and social determinants of health, such as local intersectoral tables that work to improve community well-being before, during, and after emergencies.
- Support research to better understand what concrete actions can be taken to build supportive environments to enable health-promoting behaviour and adherence to protective measures during emergencies.
Provide communities with resources to strengthen social infrastructure
- Increase opportunities for sustainable core funding to community organizations, with a focus on equitable distribution of funds across communities.
- Coordinate community funding across government departments to reduce administrative burden for local organizations.
- Develop and implement innovative and participatory funding approaches that support community priorities and community-led interventions for emergency management.
- Support dedicated and sustainable funding for Indigenous-led community-based emergency management.
Partner with communities to integrate local knowledge and prioritize community-centred planning across the emergency management continuum
- Bring a health promotion lens to existing risk and vulnerability assessment tools, to strengthen focus on community knowledge, community assets, and community priorities.
- Work with community partners to develop community-level indicators of resilience that target and support essential community processes and assets.
- Leverage expertise and relationships from existing public health programs and networks (e.g., organizations addressing chronic diseases, or those that serve older adults, children, and families).
- Explore how First Nations, Inuit, and Métis Knowledges and practices can inform prevention and mitigation initiatives, recognizing the ongoing stewardship of Indigenous Peoples.
Centre equity in emergency management science, evidence, and technology
- Explore how to identify and address issues of bias in key emergency management technologies (e.g., disaster risk modelling, vulnerable infrastructure mapping).
- Build integrated and timely surveillance systems and research endeavours that can collect and disaggregate data to identify differential risks, vulnerabilities, and outcomes related to emergencies, ensuring Indigenous data sovereignty is respected, and community engagement is prioritized.
- Collect longitudinal data to monitor long-term outcomes from emergencies on health and the underlying conditions that influence the health of populations and communities.
- Engage with communities to understand the differential impacts of emergency-related policies and programs, identify leading practices, and guide action to ensure equitable processes and outcomes.
Foster workforce development and planning to better reflect and engage with community
- Create training and skill building opportunities for public health and emergency management professionals on partnering with communities and building culturally safe relationships.
- Prioritize long-term relationship building with community as a key public health emergency management function within workforce planning, with dedicated and ongoing resources.
- Undertake research to understand current workforce composition and how to build a diverse emergency management workforce that reflects the communities it serves.
Support cross-training to optimize use of existing public health and emergency management expertise
- Include health promotors in the implementation and evaluation of emergency training exercises, to support a focus on equity and community.
- Incorporate health promotion approaches and concepts in training for emergency management professionals (e.g., equity, trauma-informed practices, cultural safety, supportive environments, intersectoral healthy public policy to support the determinants of health).
- Create opportunities to train health promoters in emergency management procedures, so they can be quickly deployed to strengthen supportive environments that enable adherence to emergency measures.
Integrate health promotion considerations and approaches into emergency management policies, plans, and procedures
- Advocate for the inclusion of health promotion professionals at public health emergency management decision-making tables (e.g., health equity liaison officers).
- Apply equity- and community-oriented tools, such as equity checklists and indicator prompts, to public health system readiness frameworks, preparedness plans, risk assessments, and other procedural and guidance documents.
- Develop and implement accountability structures to engage community as ongoing partners across the emergency management continuum.
- Support research on how to bring health promotion approaches and tools into emergency management.
Appendix A: Key health promotion tools for emergency management procedures
The following table lists some of the key health promotion tools or approaches that are featured in the report. Each tool has its strengths and may be tailored for different scenarios (e.g., type of emergency, level of government, targeted sub-population, urgency of intervention). This table is provided for general information. It is the user's responsibility to select the tool or tools that best fit their context, purpose, and needs. Note that this list is a selection of examples and is not exhaustive or validated.
These tools may be applicable for the following emergency management procedures:
- Planning
- Emergency activation
- Intra- and after-action review
- Training
- Emergency exercises
| Tool | Description |
|---|---|
Gender-based analysis Sex- and Gender-Based Analysis Plus (SGBA Plus)Footnote 345 Culturally relevant SGBA Plus (Native Women's Association of Canada, Women of the Métis Nation, Pauktuutit Inuit Women of Canada)Footnote 348Footnote 349Footnote 350 |
SGBA Plus is an analytic process used by the Government of Canada's Health Portfolio. It began as a sex and gender analysis but has since evolved into an intersectional approach, to assess how determinants of health interact and intersect with each other and broader systems and structures to shape individual and population health outcomes. The tool operationalizes intersectionality, allowing for the formulation of responsive and inclusive public health initiatives that promote equitable health outcomes. Culturally relevant SGBA Plus considers the historic and current challenges faced by Indigenous Peoples and the distinct lived experiences not only between but within First Nations, Inuit, and Métis communities. |
Equity impact assessments Racial equity impact assessment toolkitFootnote 359 Health equity impact assessment toolFootnote 353 |
Equity impact assessments are decision support tools that walk users through the steps of identifying how a program, policy, or services will impact population groups in different ways. Many jurisdictions have developed their own frameworks and templates. Some are specific to health while others may focus on broader outcomes. |
Tools to support rapid decision making, including equity analysis Public policy analysis tool for rapid decision making in public healthFootnote 405 |
The National Collaborating Centre for Healthy Public Policy collaborated with the Institut national de santé publique du Québec to develop a public policy analysis tool adapted to rapid decision-making contexts. This tool is particularly relevant in the context of a health emergency, where decisions must be made at an accelerated pace. It includes 2 guiding questions for users to consider equity implications specifically. |
Equity indicators for public health systems for pandemic preparedness, response, and recovery Public health emergency preparedness framework and indicatorsFootnote 429 Equity indicators for public healthFootnote 371 |
Public Health Ontario developed a framework for public health emergency preparedness and defining corresponding indicators for guiding performance measurement and improvement in Canada. The National Collaborating Centres for Infectious Diseases and Determinants of Health expanded on these original indicators to measure public health system performance in addressing inequities and integrating equitable approaches. These indicators support the integration of health equity considerations in all decision making for emergency preparedness, response, and recovery. Note that 4 of these indicators specifically deal with community engagement. |
Ethical frameworks Framework for ethical deliberation and decision-making in public healthFootnote 365 Public health ethics framework: A guide for use in response to the COVID-19 pandemic in CanadaFootnote 368 COVID-19 ethical decision-making frameworkFootnote 369 List of other ethics frameworksFootnote 367 |
Public health ethics frameworks are broad tools to help public health practitioners and decision-makers analyze ethical challenges or dilemmas. Especially during a health emergency, difficult choices about allocating scarce resources and protecting communities must often be made with unknown or unpredictable variables. Recognizing the ethical nature of these choices, these tools can support users in clarifying, identifying, and deciding possible courses of action. |
Trauma-informed approaches Trauma-informed practices for children and families during the COVID-19 pandemicFootnote 329 Trauma and violence-informed approaches to policy and practiceFootnote 430 |
Trauma-informed policies, programs, and services emphasize minimizing harm and re-traumatization. This is done by prioritizing community knowledge, building trust, and collaborative community action to support healing and connectedness. |
Risk and capacity assessments Enhanced vulnerability and capacity assessment (EVCA)Footnote 431 |
The EVCA is a participatory process developed by the International Federation of the Red Cross and Red Crescent Societies that communities can use to assess local risks, where risks come from, who is most exposed, and what actions could be undertaken to reduce risk. It includes climate change and gender and diversity considerations as well as guidance on how to conduct these assessments in urban contexts. |
Appendix B: An update on COVID-19 in Canada
Preamble
COVID-19 had, and will continue to have, significant impacts on the health of populations around the world. As of August 2023, globally there have been over 769 million reported cases of COVID-19 and almost 7 million deaths.Footnote 162 However, 2023 marked a pivotal time in the evolution of the pandemic, with the World Health Organization declaring on May 5th that COVID-19 was no longer a public health emergency of international concern. This came as a result of more than a year of decreasing cases and mortality, increasing population immunity from vaccination and infection, and easing pressures on health systems.Footnote 432Footnote 433
This appendix to the 2023 CPHO Annual Report serves as a brief update on key COVID-19 events in Canada between August 2022 and August 2023. It describes public health surveillance data, the continuing impact of COVID-19 and other respiratory diseases on people and the health system, and the efforts to implement long-term, sustainable approaches to the management of COVID-19.
Transitioning to a new epidemiological pattern
In 2020 and 2021, the pandemic was characterized by repeated waves of infection with high peaks and low troughs.Footnote 52 However, the arrival of the highly transmissible Omicron variant changed the trajectory of the pandemic. Following the Omicron-driven maximum peak in January 2022, COVID-19 activity declined and the previous pattern of distinct waves of infection began to subside. COVID-19-related hospitalizations and intensive care unit admissions gradually decreased as a result of high levels of population immunity from both vaccination and infection (see Figure 13). Despite the repeated emergence of new and highly transmissible Omicron sub-lineages, indicators of severe outcomes remained lower than during early Omicron waves through the summer of 2023.Footnote 52Footnote 434
However, COVID-19 continued to have serious acute and lingering impacts, particularly for older and immunocompromised populations as well as those with underlying health conditions.Footnote 434Footnote 435 Hospitalization rates remained highest among people aged 80 years and older.Footnote 52
As overall COVID-19 activity decreased and at-home rapid antigen tests became widely available, public health surveillance moved away from reporting confirmed cases to tracking indicators of severe illness (e.g., hospitalizations) and broader trends in virus activity. Wastewater monitoring in major cities in Canada became an increasingly important source of information on the transmission of COVID-19. By July 2023, detection of COVID-19 in wastewater reached the lowest levels since wastewater surveillance began in 2021.Footnote 436 Although indicators of COVID-19 activity remained lower than earlier in the pandemic, in August 2023 there were some early signs of increasing activity.Footnote 437
The establishment of smaller scale community-led wastewater testing in northern, remote, and isolated communities in 2022 was also noteworthy. These communities, which have much greater proportions of First Nations, Inuit, and Métis Peoples than communities in southern Canada, often face significant barriers to timely access to health care. Wastewater testing allows these communities to get early warning and take preventative action quickly.Footnote 438
Given that SARS-CoV-2 is still a new virus and continues to rapidly evolve, whether it will converge to predictable patterns or seasonality, like other respiratory viruses, remains to be seen. Regardless, it is important to be prepared for resurgences, especially given the co-circulation of other respiratory diseases in the fall and winter months.

Figure 13 - Text description
The figure is a graph which displays an overview of Canada's COVID-19 pandemic from March 2020 to August 2023. The vertical axes display the number of COVID-19 cases hospitalized and the number admitted to intensive care units as 7-day moving averages by each case's onset date (or best approximation). The horizontal axis displays the date in months. The dominant periods of the COVID-19 variants are superimposed on the figure, from left to right: multiple variants of concern dominant from April 2021 to May 2021, Delta variant dominant from July 2021 to December 2021, and Omicron variant dominant from January 2022 onwards. A period where data are accumulating is also noted for the final 30 days in the figure where it is anticipated data may be added over time and is subject to change.
| Date (selected time points) | Number of hospitalizations (7-day moving average) | Number of intensive care unit admissions (7-day moving average) |
|---|---|---|
| 2020-02-29 | 1.3 | 0.6 |
| 2020-03-31 | 134.9 | 38.3 |
| 2020-04-30 | 161 | 22.3 |
| 2020-05-31 | 56.6 | 12.7 |
| 2020-06-30 | 17 | 3 |
| 2020-07-31 | 18.3 | 5 |
| 2020-08-31 | 15.9 | 3 |
| 2020-09-30 | 78.7 | 17.3 |
| 2020-10-31 | 138.3 | 21.6 |
| 2020-11-30 | 239.6 | 41.9 |
| 2020-12-31 | 319.1 | 51.9 |
| 2021-01-31 | 165.6 | 27 |
| 2021-02-28 | 120.6 | 22 |
| 2021-03-31 | 223.9 | 55.6 |
| 2021-04-30 | 273.1 | 56.7 |
| 2021-05-31 | 92 | 20.7 |
| 2021-06-30 | 34.9 | 7.6 |
| 2021-07-31 | 28.6 | 8.4 |
| 2021-08-31 | 133.9 | 30.3 |
| 2021-09-30 | 154.7 | 29.6 |
| 2021-10-31 | 79.7 | 16.9 |
| 2021-11-30 | 82 | 20.3 |
| 2021-12-31 | 462.1 | 73.1 |
| 2022-01-31 | 526.7 | 67.6 |
| 2022-02-28 | 207.6 | 26.9 |
| 2022-03-31 | 312.9 | 31.1 |
| 2022-04-30 | 367.4 | 31.1 |
| 2022-05-31 | 135.3 | 11.9 |
| 2022-06-30 | 183.3 | 12.6 |
| 2022-07-31 | 266 | 22 |
| 2022-08-31 | 189.9 | 15.4 |
| 2022-09-30 | 239.6 | 13.7 |
| 2022-10-31 | 260.6 | 15 |
| 2022-11-30 | 228.6 | 14 |
| 2022-12-31 | 251.9 | 17 |
| 2023-01-31 | 132 | 10.1 |
| 2023-02-28 | 157.6 | 12 |
| 2023-03-31 | 123.3 | 9.7 |
| 2023-04-30 | 102.9 | 7 |
| 2023-05-31 | 62 | 5.4 |
| 2023-06-30 | 30.4 | 1.4 |
| 2023-07-31 | 31.4 | 2.4 |
| 2023-08-25 | 56.7 | 2.4 |
| Note the dominant periods of the COVID-19 variants are as follows: multiple variants of concern dominant from April 2021 to May 2021, Delta variant dominant from July 2021 to December 2021, and Omicron variant dominant from January 2022 onwards. | ||
Data as of August 25, 2023, extracted on September 7, 2023.
Source: Detailed case data submitted to the Public Health Agency of Canada by the provinces and territories.
Trend lines reflect 7-day moving averages. Hospitalizations include data from 9 provinces and territories (representing 84% of the population) and Intensive Care Unit admissions include data from 8 provinces and territories (representing 80% of the population). Hospitalized cases include those admitted to the Intensive Care Unit.
"Tripledemic" of COVID-19, respiratory syncytial virus, and influenza overwhelmed pediatric hospitals
Since the first year of the pandemic, the use of public health measures intended to help reduce the transmission of COVID-19 also helped curb the spread of other respiratory viruses. As jurisdictions across Canada eased many public health measures, transmission of these other viruses increased. This, in combination with lower population-level immunity, led to higher rates of infection.Footnote 439
Beginning in the spring of 2022, Canada experienced a brief, atypical late-onset influenza epidemic. A second influenza surge for 2022 began in October, marking the first respiratory virus season since 2020 without widespread population-level public health measures. This occurred at the same time as unusually high respiratory syncytial virus (RSV) activity and ongoing COVID-19 infections. Coined a "tripledemic", the percentage of positive tests for influenza and RSV in the fall of 2022 were 3 times higher than pre-pandemic averages.Footnote 440 Hospitalization rates surged, particularly among the pediatric population, putting increased strain on already stressed healthcare systems.Footnote 441 Media reported on canceled surgeries and significant wait times as pediatric hospital staff were redeployed to overcrowded emergency departments and intensive care units.Footnote 442Footnote 443Footnote 444Footnote 445Footnote 446Footnote 447 Peak disease activity of the "tripledemic" lasted a few weeks, with indicators returning to expected levels by the end of December 2022.Footnote 440
Immunity from vaccination and infection remained high for adults
As of June 2023, 80.5% of people living in Canada had completed their primary series of a COVID-19 vaccine. Vaccine coverage was highest among adults aged 60 years and older (94.9% having received at least 1 dose) and lowest among young children (50% of 5- to 11-year-olds and 9.3% of 0- to 4-year-olds having received at least 1 dose).Footnote 448 In addition, research conducted by the COVID-19 Immunity Task Force using data gathered from blood donations estimated that 80% of people living in Canada had been previously infected with SARS-CoV-2 by the end of June 2023. Consistent with other studies, they also found that racialized donors continued to experience higher rates of infection compared to white donors.Footnote 449
As of July 2023, the National Advisory Committee on Immunization continues to recommend COVID-19 vaccination for those who have not been immunized. For the fall of 2023, the committee is recommending a dose of the new formulation of the vaccine for those previously vaccinated against COVID-19. This includes people in the authorized age group if it had been at least 6 months from the previous COVID-19 vaccine dose or known SARS-CoV-2 infection (whichever is later).Footnote 450 Immunization is particularly important for those at increased risk of infection or severe disease, such as adults 65 years of age or older or individuals with underlying medical conditions. Ensuring that all who are eligible have access to culturally safe vaccination programs requires ongoing support for community-led initiatives.
Post-COVID-19 condition continues to be a public health challenge
Evidence has emerged over the past 2 years that the health impacts of COVID-19 can extend beyond the initial infection. In some individuals, COVID-19 increases the risk of developing certain chronic conditions, such as diabetes and cardiovascular disease.Footnote 435Footnote 451Footnote 452Footnote 453 Additionally, the cluster of mid- and long-term symptoms that some people experience after the acute disease is referred to as post-COVID-19 condition, also known as "long COVID". These symptoms include respiratory, cardiovascular, neurological, and cognitive impairments that can be debilitating.Footnote 76Footnote 435Footnote 454Footnote 455 As of August 2022, Statistics Canada estimated that 16% of adults experienced symptoms more than 3 months after their initial SARS-CoV-2 infection.Footnote 456 Preliminary results showed that being female, having certain chronic conditions, a more severe initial infection, living with obesity, identifying as a person with a disability, and being infected earlier in the COVID-19 pandemic were all associated with an increased risk of reporting longer-term symptoms. However, being vaccinated prior to infection was associated with a reduced risk of longer-term symptoms.Footnote 454
Post-COVID-19 condition has broad socioeconomic impacts on individuals and communities. People living with it describe facing stigma, inequitable access to and inadequate support from healthcare systems, long wait times for tests and diagnoses, and the loss of personal and professional identity.Footnote 435 Additional barriers influenced by the social determinants of health, such as an inability to take time off work for appointments, language barriers, and lack of access to primary care may further exacerbate pre-existing health inequities.Footnote 435Footnote 455Footnote 457
To address these challenges, it will be important to consider the health impacts and equity considerations of SARS-CoV-2 infection in the short- and long-term. Some examples of federal initiatives in 2022 and 2023 to improve the management and mitigation of COVID-19's longer-term effects include the Public Health Agency of Canada's work to support clinical practice guidelines and the Canadian Institutes of Health Research's funding to establish a pan-Canadian post-COVID-19 condition research network.Footnote 434Footnote 458
Canada continues to monitor international trends
The improved epidemiological situation in Canada allowed for the de-escalation of COVID-19 border measures. By October 2022, the Government of Canada had removed all COVID-19 entry restrictions, as well as testing, quarantine, and isolation requirements for anyone entering Canada.Footnote 459 The elimination of border measures was facilitated by several factors, including surveillance and modelling that indicated Canada had largely passed a peak of infections, high vaccination coverage, lower hospitalization and death rates, as well as the availability and use of additional vaccine doses, rapid tests, and treatments for COVID-19.Footnote 459
However, as part of continued vigilance, the Government of Canada re-introduced temporary, country-specific border measures when warranted. On January 5th, 2023, Canada re-implemented pre-departure testing requirements for travellers arriving from the People's Republic of China, Hong Kong, or Macao, in response to reports of a major increase of local COVID-19 cases and the limited epidemiological data available.Footnote 460 The measures were lifted on March 17th, 2023, when the COVID-19 epidemiological situation in China showed signs of improvement.Footnote 461 The Government of Canada continues to work with domestic jurisdictions, international partners, and other stakeholders (e.g., cruise ship operators) to closely monitor the global evolution of SARS-CoV-2 and the emergence of potential new variants of concern.Footnote 462
Moving forward
While there has been a decline in COVID-19 activity globally, the SARS-CoV-2 virus will continue to circulate and evolve worldwide for the foreseeable future. At the time of writing this report, hospitalizations, test positivity, and wastewater surveillance levels were increasing, an early sign of rising COVID-19 activity.Footnote 437 Canada's response, which includes vaccination programs and the adoption of personal protective layers, will need to continue to adapt. As with other health emergencies, the unpredictable nature of infectious disease pandemics necessitates prevention and preparedness efforts that promote and protect the health and well-being of communities across Canada.
Appendix C: Methodology
Process
The 2023 Chief Public Health Officer of Canada (CPHO) Annual Report was drafted based on a review of the best available evidence, including academic research, guidance from expert advisors, and engagement with emergency management, public health, First Nations, Inuit, and Métis, and community experts. Where possible, Canadian research and representative data were prioritized.
The evidence was identified through the approaches summarized below.
Research reviews
- A rapid scoping review commissioned by the Office of the CPHO (OCPHO) and led by the National Collaborating Centre for Methods and Tools (NCCMT) at McMaster University to answer the question: "What is known about the application of upstream and midstream health promotion approaches in the context of H1N1, COVID-19, and mpox pandemic preparedness and response?".Footnote 9 The process for this rapid scoping review included a review of literature published in English or French, completed on January 25, 2023, found through:
- A search of 7 electronic databases: MEDLINE, Embase, Emcare, Global Health Database, Political Science Database, PAIS Index, and Trip Medical Database. The search dates varied by topic area, with 2009 to 2023 for H1N1, 2020 to 2023 for COVID-19, and 2022 to 2023 for mpox; and,
- The NCCMT issuing a call to senior decision makers across Canada to share relevant published or unpublished reports, research, or policy publications.
- A rapid evidence profile commissioned by the OCPHO and led by COVID-END (COVID-19 Evidence Network to support Decision-making), to answer the question: "How were downstream health promotion approaches that focus on individual behaviour change conceived of and used, and with what effectiveness, as part of COVID-19 pandemic preparedness and response?".Footnote 387 The process for this rapid evidence profile included a review of literature, in English or French, completed in January 2023, found through:
- A search of 7 electronic databases: ACCESSSS, Health Evidence, Health Systems Evidence, Social Systems Evidence, the COVID-END inventory of best evidence syntheses, COVID-END website, and PubMed; and,
- Hand-searching of the following sources: a COVID-19 behavioural research tracker maintained by The Policy Lab at Brown University; government and stakeholder websites for reports relevant to the question; Nexus Uni for news articles; and legislation and reports that detailed community action and engagement efforts.
- A rapid synthesis completed by COVID-END to answer the question: "Which strategies did downstream health promotion approaches use or recommend to support capability, opportunity, and motivation for adoption and maintenance of individual behaviour change as part of COVID-19 pandemic preparedness and response?".Footnote 463 This rapid synthesis applied a behavioural lens to evidence on health promotion approaches identified in the COVID-END rapid evidence profile described above.
- Ongoing and frequent literature searches by OCPHO, completed by report sub-topics relating to health promotion and/or emergency management in English and French, using online databases, such as Medline and Scopus.
Public health reports and other grey literature
- Ongoing and frequent literature searches completed by OCPHO to find grey literature and public health reports on health promotion and/or emergency management from trusted sources, such as public health organizations (e.g., World Health Organization, Pan American Health Organization) and government publications (e.g., federal, provincial/territorial, municipal, and Indigenous governments).
- Collaboration with the National Collaborating Centre for Determinants of Health, which provided expert support on key topics relating to health promotion in the report.
- Identification of applied public health examples and case studies through engagement with external public health and emergency management experts.
- Policy, grey literature, and applied examples scan conducted by a Public Health Agency of Canada (PHAC) internal reference group consisting of emergency management coordinators and analysts with health promotion expertise from regional offices.
Engagements and key informant interviews
- A targeted engagement process, completed by OCPHO, focused on:
- Local examples of bringing a health promotion or equity approach to emergency management;
- Challenges to implementing a health promotion lens in emergency management;
- First Nations, Inuit, and Métis experiences and perspectives on emergency management that relate to health promotion principles and approaches; and,
- Community organizations' needs and perspectives on how to facilitate action on equity, community mobilization, and emergency management.
- The engagement process included interviews with 16 local medical officers of health in June 2023. Potential interviewees were identified through reviewing scientific and grey literature and engaging with internal and external experts and partners. The OCPHO also sent requests for volunteers to the Urban Public Health Network and the Northern, Remote and Rural Public Health Network. Targeted interview requests were made to ensure representation from a diversity of settings across Canada.
- Ongoing and targeted engagements and collaboration with the Assembly of First Nations, the First Nations Health Authority, Inuit Tapiriit Kanatami, the Métis National Council, the Native Women's Association of Canada, and the Ontario Federation of Indigenous Friendship Centres.
- Access to complementary data from 7 interviews with PHAC-funded community organizations collected by the PHAC Atlantic Regional Office on bringing an equity perspective to emergency management.
COVID-19 update for Appendix B
- Information published or shared by PHAC, Statistics Canada, and other federal, provincial, territorial, or municipal government sources.
- Grey literature and policy reviews of trusted sources, such as health organizations (e.g., World Health Organization, Canadian Institute for Health Information) and government publications (e.g., Public Health Ontario).
- Press briefings by health authorities and media statements, where necessary.
Limitations
Scope and literature search
The 2023 CPHO Annual Report explores the health impacts of emergencies in Canada, as well as the potential to bring a health promotion approach into emergency management. Health promotion and emergency management are both large fields, with research and practice that cross a number of academic and professional disciplines. Since the purpose of the report is to provide an overview of presented topics and concepts, there are necessary restrictions on the level of detail provided in each section. Accordingly, the report does not represent an exhaustive evidence review, but rather a summary of select key literature. Only literature published in English and French was reviewed. A detailed assessment of study quality and risk of bias was not conducted in this review.
Language
To the extent possible, the report writers attempted to use standardized, inclusive, and culturally appropriate language when drawing on evidence related to different communities and their experiences of health. However, in some instances they relied on the terminology included in the source documents (e.g., vulnerable populations), if this language had particular meaning or relevance in those materials.
Acknowledgements
Many people and organizations contributed to the development of this report.
I would like to express my gratitude to my annual report advisors who provided invaluable advice, strategic guidance, and expertise:
- Dr. Marcia Anderson, Vice-dean Indigenous health, social justice, and anti-racism, University of Manitoba
- Dr. Suzanne Jackson, Associate Professor Emerita, Co-Director WHO Collaborating Centre in Health Promotion, Dalla Lana School of Public Health, University of Toronto
- Dr. Ilona Kickbusch, Professor, Global Health Centre, Graduate Institute of International and Development Studies, Geneva
- John Lavery, Chief Provincial Health Emergency Management Officer, Health Emergency Management British Columbia (HEMBC), Provincial Health Services Authority
- Dr. Cory Neudorf, Professor, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan
My deep appreciation to experts from across Canada, including medical officers of health, public health and emergency management practitioners, researchers, non-governmental organizations, and community partners who participated in conversations and interviews on how public health systems can apply health promotion to emergency management. I also would like to extend my thanks to the Urban Public Health Network and the Northern, Rural and Remote Public Health Network for facilitating recruitment for the interviews with medical officers of health.
I would like to thank the analysts and emergency management experts from Indigenous organizations who provided input and advice on the report content: Assembly of First Nations, First Nations Health Authority, Inuit Tapiriit Kanatami, Métis National Council, Native Women's Association of Canada, and Ontario Federation of Indigenous Friendship Centres.
Thank you to the many colleagues at the Public Health Agency of Canada, Health Canada, Indigenous Services Canada, and Public Safety who provided insights and guidance throughout the development of the report, and for their critical review of report drafts.
Finally, I am grateful for the work of my office members who came together to support the development and mobilization of this report. Special thanks to the Reports and Science Policy teams for their commitment and dedication in seeing this report from conception to publication: Fabienne Boursiquot, Dr. Marie Chia, Dr. Charlene Cook, Elyse Fortier, Rhonda Fraser, Dr. Kim Girling, Dr. Kimberly Gray, Dr. David Grote, Jessica Lepage, Danielle Noble, Shauna Sanvido, Dr. Sarah Schwarz, Kelsey Seal, and Inès Zombré.
References:
- Footnote 1
-
Public Safety Canada. National Risk Profile: A National Emergency Preparedness and Awareness Tool. Government of Canada; 2023.
- Footnote 2
-
Public Safety Canada. Emergency Management Strategy for Canada: Toward a Resilient 2030. Government of Canada; 2019.
- Footnote 3
-
Tanner, T, Surminski, S, Wilkinson, E, Reid, R, Rentschler, J, Rajput, S. The Triple Dividend of Resilience: Realising Development Goals through the Multiple Benefits of Disaster Risk Management. Overseas Development Institute, The World Bank; 2015.
- Footnote 4
-
Schnitter, R, Moores, E, Berry, P, Verret, M, Buse, C, Macdonald, C, et al. Chapter 9: Climate Change and Health Equity. In: Berry P, Schnitter R, editors. Health of Canadians in a Changing Climate: Advancing Our Knowledge for Action. Ottawa, ON: Government of Canada; 2022.
- Footnote 5
-
Public Health Agency of Canada. Chief Public Health Officer's Report on the State of Public Health in Canada 2020: From Risk to Resilience – an Equity Approach to COVID-19. Ottawa, ON: Public Health Agency of Canada; 2020.
- Footnote 6
-
Expert Panel on Disaster Resilience in a Changing Climate. Building a Resilient Canada. Ottawa, ON: Council of Canadian Academies; 2022.
- Footnote 7
-
Public Health Agency of Canada. Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2022: Mobilizing Public Health Action on Climate Change in Canada. Ottawa, ON: Public Health Agency of Canada; 2022.
- Footnote 8
-
Sachs, JD, Karim, SSA, Aknin, L, Allen, J, Brosbøl, K, Colombo, F, et al. The Lancet Commission on Lessons for the Future from the COVID-19 Pandemic. The Lancet. 2022; 400(10359):1224-80.
- Footnote 9
-
National Collaborating Centre for Methods and Tools. Rapid Scoping Review: What Is Known About the Application of Upstream and Midstream Health Promotion Approaches in the Context of H1N1, COVID-19, and Mpox Pandemic Preparedness and Response? : National Collaborating Centre for Methods and Tools; 2023.
- Footnote 10
-
United Nations Office for Disaster Risk Reduction. What Is the Sendai Framework for Disaster Risk Reduction? : United Nations Office for Disaster Risk Reduction; 2015.
- Footnote 11
-
Ottawa Charter for Health Promotion: An International Conference on Health Promotion. Ottawa, ON: Government of Canada; 1986.
- Footnote 12
-
World Health Organization. Health Promotion. World Health Organization.
- Footnote 13
-
Public Health Ontario. Health Promotion. Public Health Ontario; 2023.
- Footnote 14
-
Pan American Health Organization. Health Promotion. Pan American Health Organization.
- Footnote 15
-
Nomura, S, Parsons, AJQ, Hirabayashi, M, Kinoshita, R, Liao, Y, Hodgson, S. Social Determinants of Mid- to Long-Term Disaster Impacts on Health: A Systematic Review. International Journal of Disaster Risk Reduction. 2016; 16:53-67.
- Footnote 16
-
Keim, ME. Preventing Disasters: Public Health Vulnerability Reduction as a Sustainable Adaptation to Climate Change. Disaster Medicine and Public Health Preparedness. 2011; 5(2):140-8.
- Footnote 17
-
World Health Organization. Health Emergency and Disaster Risk Management Framework. World Health Organization; 2019.
- Footnote 18
-
O'Sullivan, TL, Kuziemsky, CE, Corneil, W, Lemyre, L, Franco, Z. The EnRiCH Community Resilience Framework for High-Risk Populations. PLoS Currents. 2014; 6(1).
- Footnote 19
-
Haldane, V, Jung, A-S, Neill, R, Singh, S, Wu, S, Jamieson, M, et al. From Response to Transformation: How Countries Can Strengthen National Pandemic Preparedness and Response Systems. BMJ. 2021; 375:e067507.
- Footnote 20
-
Marmot, M, Allen, J, Goldblatt, P, Herd, E, Morrison, J. Build Back Fairer: The COVID-19 Marmot Review. The Health Foundation; 2020.
- Footnote 21
-
World Health Organization. Human Rights. World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/human-rights-and-health
- Footnote 22
-
United Nations General Assembly. United Nations Declaration on the Rights of Indigenous Peoples. United Nations General Assembly; 2007.
- Footnote 23
-
Mishra, S, Walker, JD, Wilhelm, L, Larivière, V, Bubela, T, Straus, SE. Use and Misuse of Research: Canada's Response to COVID-19 and Its Health Inequalities. BMJ. 2023; 382:e075666.
- Footnote 24
-
Lokmic-Tomkins, Z, Bhandari, D, Bain, C, Borda, A, Kariotis, TC, Reser, D. Lessons Learned from Natural Disasters around Digital Health Technologies and Delivering Quality Healthcare. International Journal of Environmental Research and Public Health. 2023; 20(5).
- Footnote 25
-
Casey, JA, Fukurai, M, Hernández, D, Balsari, S, Kiang, MV. Power Outages and Community Health: A Narrative Review. Current Environmental Health Reports. 2020; 7(4):371-83.
- Footnote 26
-
Gu, D. Exposure and Vulnerability to Natural Disasters for World's Cities. United Nations; 2019.
- Footnote 27
-
Lawrence, J, Blackett, P, Cradock-Henry, NA. Cascading Climate Change Impacts and Implications. Climate Risk Management. 2020; 29:100234.
- Footnote 28
-
Leppold, C, Gibbs, L, Block, K, Reifels, L, Quinn, P. Public Health Implications of Multiple Disaster Exposures. The Lancet Public Health. 2022; 7(3):E274-E86.
- Footnote 29
-
Public Safety Canada. An Emergency Management Framework for Canada. 2nd ed: Government of Canada; 2011.
- Footnote 30
-
Sendai Framework Terminology on Disaster Risk Reduction. United Nations Office for Disaster Risk Reduction; Available from: https://www.undrr.org/terminology.
- Footnote 31
-
Public Safety Canada. National Emergency Response System. Government of Canada; 2022.
- Footnote 32
-
Public Safety Canada. Canadian Disaster Database Reference - Reference Table for Symbols and Definitions. Government of Canada; 2015.
- Footnote 33
-
Penta, S, Marlowe, VG, Gill, K, Kendra, J. Of Earthquakes and Epidemics: Examining the Applicability of the All-Hazards Approach in Public Health Emergencies. Risk, Hazards & Crisis in Public Policy. 2017; 8(1):48-67.
- Footnote 34
-
Public Health Agency of Canada. Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2021: A Vision to Transform Canada's Public Health System. Ottawa, ON: Public Health Agency of Canada; 2021.
- Footnote 35
-
Canadian Institute for Health Information. Impact of COVID-19 on Canada's Health Care Systems. Canadian Institute for Health Information; 2022.
- Footnote 36
-
Public Health Agency of Canada. Chief Public Health Officer's Report on the State of Public Health in Canada 2019: Addressing Stigma: Towards a More Inclusive Health System. Ottawa, ON: Public Health Agency of Canada; 2019.
- Footnote 37
-
Saeed, F, Mihan, R, Mousavi, SZ, Reniers, RLEP, Bateni, FS, Alikhani, R, et al. A Narrative Review of Stigma Related to Infectious Disease Outbreaks: What Can Be Learned in the Face of the COVID-19 Pandemic? Frontiers in Psychiatry. 2020; 11.
- Footnote 38
-
Fischer, LS, Mansergh, G, Lynch, J, Santibanez, S. Addressing Disease-Related Stigma During Infectious Disease Outbreaks. Disaster Medicine and Public Health Preparedness. 2019; 13(5-6):989-94.
- Footnote 39
-
Ministry of Mental Health and Addictions. Escalating BC's Response to the Overdose Emergency. Government of British Columbia; 2018.
- Footnote 40
-
Board of Health. Hl17.9 - Addressing Anti-Black Racism as a Public Health Crisis in the City of Toronto. City of Toronto; 2020.
- Footnote 41
-
Tuccaro, B-J. A State of Emergency Declared. Fort Chipewyan, Alberta: Mikisew Cree First Nation; 2023.
- Footnote 42
-
Eggertson, L. Nunavut Suicides a "Public Health Emergency". Canadian Medical Association Journal. 2015; 187(16):E462.
- Footnote 43
-
City of Toronto. Toronto City Council Approves Changes to Warming Centre Operations, Urges Provincial and Federal Governments to Respond to Homelessness Emergency. City of Toronto; 2023.
- Footnote 44
-
City Council. Cc8.2 - Declaring Gender-Based Violence and Intimate Partner Violence an Epidemic in the City of Toronto. City of Toronto; 2023.
- Footnote 45
-
Nishnawbe Aski Nation. Final Report: Emergency Management for First Nations in Ontario. Nishnawbe Aski Nation; 2021.
- Footnote 46
-
Canadian Red Cross. Supporting Communities Facing Social Emergencies. Canadian Red Cross; 2019.
- Footnote 47
-
Tam, T. Fifteen Years Post-SARS: Key Milestones in Canada's Public Health Emergency Response. Canada Communicable Disease Report. 2018; 44(5):98-101.
- Footnote 48
-
Department of Finance Canada. Budget 2023 - a Made-in-Canada Plan: Strong Middle Class, Affordable Economy, Healthy Future. Government of Canada; 2023.
- Footnote 49
-
Agyapong, VIO, Hrabok, M, Juhas, M, Omeje, J, Edward, D, Nwaka, B, et al. Prevalence Rates and Predictors of Generalized Anxiety Disorder Symptoms in Residents of Fort McMurray Six Months after a Wildfire. Frontiers in Psychology. 2018; 9.
- Footnote 50
-
Canadian Institute for Health Information. COVID-19 Hospitalization and Emergency Department Statistics. Canadian Institute for Health Information; 2023.
- Footnote 51
-
Canadian Institute for Health Information. Surgeries Impacted by COVID-19: An Update on Volumes and Wait Times. Canadian Institute for Health Information; 2023.
- Footnote 52
-
Government of Canada. COVID-19 Epidemiology Update: Current Situation. 2023.
- Footnote 53
-
British Columbia Coroners Service Death Review Panel. Extreme Heat and Human Mortality: A Review of Heat-Related Deaths in B.C. In Summer 2021. Government of British Columbia; 2022.
- Footnote 54
-
Statistics Canada. Infographic: Fort McMurray 2016 Wildfire – Economic Impact. Statistics Canada; 2017.
- Footnote 55
-
Public Safety Canada. Canadian Disaster Database. Government of Canada; 2020.
- Footnote 56
-
Généreux, M, Maltais, D, Petit, G, Roy, M. Monitoring Adverse Psychosocial Outcomes One and Two Years after the Lac-Mégantic Train Derailment Tragedy (Eastern Townships, Quebec, Canada). Prehospital and Disaster Medicine. 2019; 34(3):251-9.
- Footnote 57
-
Généreux, M, Petit, G, Maltais, D, Roy, M, Simard, R, Boivin, S, et al. The Public Health Response during and after the Lac-Mégantic Train Derailment Tragedy: A Case Study. Disaster Health. 2014; 2(3-4):113-20.
- Footnote 58
-
Environment and Climate Change Canada. Top Ten Weather Stories for 2011: Story One. Environment and Climate Change Canada; 2017.
- Footnote 59
-
Health Canada. Emergency Management: Taking a Health Perspective. Government of Canada; 2009.
- Footnote 60
-
Government of Canada. Surviving the Heat: The Impacts of the 2021 Western Heat Dome in Canada. Government of Canada; 2022.
- Footnote 61
-
Beugin, D, Clark, D, Miller, S, Ness, R, Pelai, R, Wale, J. The Case for Adapting to Extreme Heat: Costs of the 2021 B.C. Heat Wave. Ottawa, ON: Canadian Climate Institute; 2023.
- Footnote 62
-
Canadian Meteorological and Oceanographic Society. Canada's Top Ten Weather Stories for 2016. Canadian Meteorological and Oceanographic Society; 2019.
- Footnote 63
-
Manitoba 2011 Flood Review Task Force Report. Government of Manitoba; 2013. Available from: https://www.gov.mb.ca/asset_library/en/2011flood/flood_review_task_force_report.pdf.
- Footnote 64
-
Blais, E-L, Greshuk, J, Stadnyk, T. The 2011 Flood Event in the Assiniboine River Basin: Causes, Assessment and Damages. Canadian Water Resources Journal / Revue canadienne des ressources hydriques. 2016; 41(1-2):74-84.
- Footnote 65
-
Lecomte, EL, Pang, AW, Russell, JW. Ice Storm '98. Institute for Catastrophic Loss Reduction; 1998.
- Footnote 66
-
Bonikowsky, L, Block, N. Ice Storm of 1998. The Canadian Encyclopedia; 2016.
- Footnote 67
-
Health of Canadians in a Changing Climate: Advancing Our Knowledge for Action. Berry P, Schnitter R, editors. Ottawa, ON: Government of Canada; 2022.
- Footnote 68
-
Giorgadze, T, Maisuradze, I, Japaridze, A, Utiashvili, Z, Abesadze, G. Disasters and Their Consequences for Public Health. Georgian Medical News. 2011; 194:59-63.
- Footnote 69
-
Du, W, FitzGerald, G, Clark, M, Hou, X. Health Impacts of Floods. Prehospital and Disaster Medicine. 2010; 25(3):265-72.
- Footnote 70
-
Eykelbosh, A. Health Effects of Oil Spills and Implications for Public Health Planning and Research. National Collaborating Centre for Environmental Health; 2014
- Footnote 71
-
World Health Organization. Key Approaches to Strengthening Emergency Preparedness and Response. World Health Organization.
- Footnote 72
-
Bayntun, C. A Health System Approach to All-Hazards Disaster Management: A Systematic Review. PLOS Current; 2012.
- Footnote 73
-
Chen, H, Samet, JM, Bromberg, PA, Tong, H. Cardiovascular Health Impacts of Wildfire Smoke Exposure. Particle and Fibre Toxicology. 2021; 18(1):2.
- Footnote 74
-
Korsiak, J, Pinault, L, Christidis, T, Burnett, RT, Abrahamowicz, M, Weichenthal, S. Long-Term Exposure to Wildfires and Cancer Incidence in Canada: A Population-Based Observational Cohort Study. The Lancet Planetary Health. 2022; 6(5):e400-e9.
- Footnote 75
-
Yao, J, Brauer, M, Wei, J, McGrail Kimberlyn, M, Johnston Fay, H, Henderson Sarah, B. Sub-Daily Exposure to Fine Particulate Matter and Ambulance Dispatches during Wildfire Seasons: A Case-Crossover Study in British Columbia, Canada. Environmental Health Perspectives. 128(6):067006.
- Footnote 76
-
Government of Canada. Post COVID-19 Condition (Long COVID). Government of Canada; 2023.
- Footnote 77
-
National Collaborating Centre for Environmental Health. Psychosocial Impacts of Disasters: Resources for Mitigation, Response and Recovery. National Collaborating Centre for Environmental Health; 2023.
- Footnote 78
-
Scott, KM, Lim, C, Al-Hamzawi, A, Alonso, J, Bruffaerts, R, Caldas-de-Almeida, JM, et al. Association of Mental Disorders with Subsequent Chronic Physical Conditions: World Mental Health Surveys from 17 Countries. JAMA Pyschiatry. 2016; 73(2):150-8.
- Footnote 79
-
Hetherington, E, McDonald, S, Wu, M, Tough, S. Risk and Protective Factors for Mental Health and Community Cohesion after the 2013 Calgary Flood. Disaster Medicine and Public Health Preparedness. 2018; 12(4):470-7.
- Footnote 80
-
Généreux, M, Maltais, D, Petit, G, Roy, M. Monitoring Adverse Pyschosocial Outcomes One and Two Years after The Lac-Mégantic Train Derailment Tragedy (Eastern Townships, Quebec, Canada). Prehospital and Disaster Medicine. 2019; 34(3):251-9.
- Footnote 81
-
Mass Casualty Commission. Turning the Tide Together: Final Report of the Mass Casualty Commission Volume 4: Community. Mass Casualty Commission; 2023.
- Footnote 82
-
Hayes, K, Blashki, G, Wiseman, J, Burke, S, Reifels, L. Climate Change and Mental Health: Risks, Impacts and Priority Actions. International Journal of Mental Health Systems. 2018; 12(28).
- Footnote 83
-
Auditor General of Canada. Report 8 - Emergency Management in First Nations Communities - Indigenous Services Canada. Office of the Auditor General of Canada; 2022.
- Footnote 84
-
Hahn, MB, Van Wyck, R, Lessard, L, Fried, R. Compounding Effects of Social Vulnerability and Recurring Natural Disasters on Mental and Physical Health. Disaster Medicine and Public Health Preparedness. 2022; 16(3):1013-21.
- Footnote 85
-
Agyapong, B, Shalaby, R, Eboreime, E, Obuobi-Donkor, G, Owusu, E, Adu, MK, et al. Cumulative Trauma from Multiple Natural Disasters Increases Mental Health Burden on Residents of Fort McMurray. European Journal of Psychotraumatology. 2022; 13(1):2059999.
- Footnote 86
-
Public Health Agency of Canada. Impact of COVID-19 on the Delivery of STBBI-Related Services in Canada, Including Harm Reduction Services. Government of Canada; 2020.
- Footnote 87
-
Illingworth, H, Ferrara, N. COVID-19 and the Increase in Domestic Violence against Women: Living in Fear… between Two Pandemics. Office of the United Nations High Commissioner for Human Rights; 2020. Available from: https://www.ohchr.org/sites/default/files/Documents/Issues/Women/SR/VAWJournalists/Government/canada.pdf.
- Footnote 88
-
Colley, RC, Watt, J. The Unequal Impact of the COVID-19 Pandemic on the Physical Activity Habits of Canadians. Statistics Canada; 2022.
- Footnote 89
-
Statistics Canada. Police-Reported Hate Crime, 2021. The Daily; 2023.
- Footnote 90
-
Canadian Institute for Health Information. Unintended Consequences of COVID-19: Impact on Harms Caused by Substance Use. Ottawa, ON: Canadian Institute for Health Information; 2021.
- Footnote 91
-
Statistics Canada. Victims of Police-Reported Family and Intimate Partner Violence in Canada, 2021. The Daily; 2022.
- Footnote 92
-
Aitsi-Selmi, A, Egawa, S, Sasaki, H, Wannous, C, Murray, V. The Sendai Framework for Disaster Risk Reduction: Renewing the Global Commitment to People's Resilience, Health, and Well-Being. International Journal of Disaster Risk Science. 2015; 6(2):164-76.
- Footnote 93
-
National Collaborating Centre for Determinants of Health. Let's Talk: Redistributing Power to Advance Health Equity. Antigonish, NS: National Collaborating Centre for Determinants of Health, St. Francis Xavier University; 2023.
- Footnote 94
-
Solar, O, Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). Geneva, Switzerland: World Health Organization; 2007.
- Footnote 95
-
Marmot, M. Achieving Health Equity: From Root Causes to Fair Outcomes. The Lancet Global Health. 2007; 370(9593):1153-63.
- Footnote 96
-
Public Health Agency of Canada. How to Integrate Intersectionality Theory in Quantitative Health Equity Analysis? A Rapid Review and Checklist of Promising Practices. Public Health Agency of Canada; 2022.
- Footnote 97
-
Crenshaw, K. Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. 1991; 43(6):1241-99.
- Footnote 98
-
National Collaborating Centre for Determinants of Health. Let's Talk: Intersectionality. Antigonish, NS: National Collaborating Centre for Determinants of Health, St. Francis Xavier University; 2022.
- Footnote 99
-
Public Health Agency of Canada. Social Inequalities in COVID-19 Mortality by Area- and Individual-Level Characteristics in Canada – January 2020 to December 2020/March 2021. Government of Canada; 2022.
- Footnote 100
-
Chakraborty, L, Thistlethwaite, J, Henstra, D. Flood Vulnerability and Climate Change. Canadian Climate Institute; 2021.
- Footnote 101
-
Chakraborty, L, Thistlethwaite, J, Scott, D, Henstra, D, Minano, A, Rus, H. Assessing Social Vulnerability and Identifying Spatial Hotspots of Flood Risk to Inform Socially Just Flood Management Policy. Risk Analysis. 2023; 43(5):1058-78.
- Footnote 102
-
Chakraborty, L, Rus, H, Henstra, D, Thistlethwaite, J, Minano, A, Scott, D. Exploring Spatial Heterogeneity and Environmental Injustices in Exposure to Flood Hazards Using Geographically Weighted Regression. Environmental Research. 2022; 210:112982.
- Footnote 103
-
Public Safety Canada. National Risk Profile: Strengthening Canada's All-Hazards Approach to Emergency Management. Government of Canada; 2022.
- Footnote 104
-
Henderson, SB, McLean, KE, Lee, MJ, Kosatsky, T. Analysis of Community Deaths during the Catastrophic 2021 Heat Dome: Early Evidence to Inform the Public Health Response during Subsequent Events in Greater Vancouver, Canada. Environmental Epidemiology. 2022; 6(1).
- Footnote 105
-
Health Canada. Extreme Heat and COVID-19: Considerations for Heat Health Programming in the Context of COVID-19 - Advice for Public Health Officials. Government of Canada; 2021.
- Footnote 106
-
Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait - Executive Summary. Government of Canada; 2018.
- Footnote 107
-
Statistics Canada. Experiences of Discrimination during the COVID-19 Pandemic. The Daily; 2020.
- Footnote 108
-
Miconi, D, Li, ZY, Frounfelker, RL, Venkatesh, V, Rousseau, C. Socio-Cultural Correlates of Self-Reported Experiences of Discrimination Related to COVID-19 in a Culturally Diverse Sample of Canadian Adults. International Journal of Intercultural Relations. 2021; 81:176-92.
- Footnote 109
-
Slemon, A, Richardson, C, Goodyear, T, Salway, T, Gadermann, A, Oliffe, JL, et al. Widening Mental Health and Substance Use Inequities among Sexual and Gender Minority Populations: Findings from a Repeated Cross-Sectional Monitoring Survey during the COVID-19 Pandemic in Canada. Psychiatry Research. 2022; 307:114327.
- Footnote 110
-
Kia, H, Rutherford, L, Jackson, R, Grigorovich, A, Ricote, CL, Scheim, AI, et al. Impacts of COVID-19 on Trans and Non-Binary People in Canada: A Qualitative Analysis of Responses to a National Survey. BMC Public Health. 2022; 22(1):1284.
- Footnote 111
-
Somé, NH, Shokoohi, M, Shield, KD, Wells, S, Hamilton, HA, Elton-Marshall, T, et al. Alcohol and Cannabis Use during the COVID-19 Pandemic among Transgender, Gender-Diverse, and Cisgender Adults in Canada. BMC Public Health. 2022; 22(1):452.
- Footnote 112
-
Hawke, LD, Hayes, E, Darnay, K, Henderson, J. Mental Health among Transgender and Gender Diverse Youth: An Exploration of Effects during the COVID-19 Pandemic. Psychology of Sexual Orientation and Gender Diversity. 2021; 8(2):180-7.
- Footnote 113
-
Trans PULSE Canada COVID Cohort Working Group. Impact of COVID-19 on Health Care Access for Transgender and Non-Binary People in Canada. Trans PULSE Canada; 2020.
- Footnote 114
-
McLaren, L, Masuda, J, Smylie, J, Zarowsky, C. Unpacking Vulnerability: Towards Language That Advances Understanding and Resolution of Social Inequities in Public Health. Canadian Journal of Public Health. 2020; 111(1):1-3.
- Footnote 115
-
Katz, AS, Hardy, B-J, Firestone, M, Lofters, A, Morton-Ninomiya, ME. Vagueness, Power and Public Health: Use of 'Vulnerable' in Public Health Literature. Critical Public Health. 2020; 30(5):601-11.
- Footnote 116
-
Clark, B, Preto, N. Exploring the Concept of Vulnerability in Health Care. Canadian Medical Association Journal. 2018; 190(11):E308.
- Footnote 117
-
Public Safety Canada. An Emergency Management Framework for Canada - Third Edition. Government of Canada; 2017.
- Footnote 118
-
Canada's Task Force on Flood Insurance and Relocation. Chapter 4: Equity and Social Vulnerability Analysis. In: Adapting to Rising Flood Risk: An Analysis of Insurance Solutions for Canada. Government of Canada; 2022.
- Footnote 119
-
Organisation for Economic Co-operation and Development. Enhancing Financial Protection against Catastrophe Risks: The Role of Catastrophe Risk Insurance Programmes. Organisation for Economic Co-operation and Development; 2021.
- Footnote 120
-
Pyke, C, Wilton, R. Planning for Inclusion? An Assessment of Ontario's Emergency Preparedness Guide for People with Disabilities. International Journal of Disaster Risk Reduction. 2020; 51:101888.
- Footnote 121
-
United Nations Office for Disaster Risk Reduction. Disability Inclusion in Disaster Risk Reduction. United Nations Office for Disaster Risk Reduction.
- Footnote 122
-
National Collaborating Centre for Environmental Health. Indigenous Disaster Response. National Collaborating Centre for Environmental Health; 2019.
- Footnote 123
-
Atkinson, D, Stout, R, Halseth, R, Greenwood, M. Chapter 2: Climate Change and Indigenous Peoples' Health in Canada. In: Berry P, Schnitter R, editors. Health of Canadians in a Changing Climate: Advancing Our Knowledge for Action. Ottawa, ON: Government of Canada; 2022.
- Footnote 124
-
Erni, S, Johnston, L, Boulanger, Y, Manka, F, Bernier, P, Eddy, B, et al. Exposure of the Canadian Wildland–Human Interface and Population to Wildland Fire, under Current and Future Climate Conditions. Canadian Journal of Forest Research. 2021; 51(9):1357-67.
- Footnote 125
-
Statistics Canada. Focus on Geography Series, 2016 Census - Nunavut. Government of Canada; 2019.
- Footnote 126
-
Nunavut Tunngavik. Nunavut's Infrastructure Gap. Iqaluit, NU: Nunavut Tunngavik Incorporated; 2020.
- Footnote 127
-
Statistics Canada. First Nations People, Métis and Inuit and COVID-19: Health and Social Characteristics. Statistics Canada; 2020.
- Footnote 128
-
National Collaborating Centres for Public Health. Health and Social Impacts of Long-Term Evacuation Due to Natural Disasters in First Nations Communities: A Summary of Lessons for Public Health. National Collaborating Centres for Public Health; 2021.
- Footnote 129
-
Stares, J. Evidence Review: Use of Evacuation to Protect Public Health during Wildfire Smoke Events. BC Centre for Disease Control; 2014.
- Footnote 130
-
Statistics Canada. Housing Conditions among First Nations People, Métis and Inuit in Canada from the 2021 Census. Statistics Canada; 2022.
- Footnote 131
-
McGee, TK. Evacuating First Nations during Wildfires in Canada. Fire Safety Journal. 2021; 120:103120.
- Footnote 132
-
Khalafzai, M-AK, McGee, TK, Parlee, B. Spring Flooding and Recurring Evacuations of Kashechewan First Nation, Northern Ontario, Canada. International Journal of Disaster Risk Reduction. 2021; 63:102443.
- Footnote 133
-
Asfaw, HW, Sandy Lake First Nation, McGee, TK, Christianson, AC. A Qualitative Study Exploring Barriers and Facilitators of Effective Service Delivery for Indigenous Wildfire Hazard Evacuees during Their Stay in Host Communities. International Journal of Disaster Risk Reduction. 2019; 41:101300.
- Footnote 134
-
Ballard, M, Coughlin, J, Martin, D. Reconciling with Minoaywin: First Nations Elders' Advice to Promote Healing from Forced Displacement. Canadian Journal on Aging / La Revue canadienne du vieillissement. 2020; 39(2):169-77.
- Footnote 135
-
McIvor, O, Napoleon, A, Dickie, KM. Language and Culture as Protective Factors for at-Risk Communities. Journal of Aboriginal Health. 2009; 5:6-25.
- Footnote 136
-
Walters, KL, Simoni, JM. Reconceptualizing Native Women's Health: An "Indigenist" Stress-Coping Model. American Journal of Public Health. 2002; 92(4):520-4.
- Footnote 137
-
MacDonald, JP, Willox, AC, Ford, JD, Shiwak, I, Wood, M, IMHACC Team, et al. Protective Factors for Mental Health and Well-Being in a Changing Climate: Perspectives from Inuit Youth in Nunatsiavut, Labrador. Social Science & Medicine. 2015; 141:133-41.
- Footnote 138
-
Fleming, J, Ledogar, RJ. Resilience, an Evolving Concept: A Review of Literature Relevant to Aboriginal Research. Pimatisiwin. 2008; 6(2):7-23.
- Footnote 139
-
Montesanti, S, Thurston, W, Turner, D, Traveler, R. A First Nations Framework for Emergency Planning: A Community-Based Response to the Health and Social Effects from a Flood. International Journal of Indigenous Health. 2019; 14(1):85-106.
- Footnote 140
-
Auger, MD. Cultural Continuity as a Determinant of Indigenous Peoples' Health: A Metasynthesis of Qualitative Research in Canada and the United States. International Indigenous Policy Journal. 2016; 7(4).
- Footnote 141
-
Public Safety Canada. Archive - Canadian Emergency Management College History. Government of Canada; 2015.
- Footnote 142
-
Canadian Red Cross. Be Ready: Emergency Preparedness and Recovery. Canadian Red Cross; 2023. Available from: https://www.redcross.ca/how-we-help/emergencies-and-disasters-in-canada/be-ready-emergency-preparedness-and-recovery.
- Footnote 143
-
Canadian Red Cross. How Red Cross Is Helping in Canada. Canadian Red Cross; 2023.
- Footnote 144
-
Stacey, J. Governing Emergencies in an Interjurisdictional Context. Public Order Emergency Commission; 2022.
- Footnote 145
-
Public Safety Canada. Disaster Financial Assistance Arrangements. Government of Canada; 2023.
- Footnote 146
-
Infrastructure Canada. Disaster Mitigation and Adaptation Fund: Overview. Government of Canada; 2023.
- Footnote 147
-
Public Safety Canada. Canada's Midterm Review of the Implementation of the Sendai Framework for Disaster Risk Reduction 2015-2030. Government of Canada; 2022.
- Footnote 148
-
Emergencies Act. Revised Statutes of Canada (1985, c. 22 (4th Supp.)); Available from: https://laws-lois.justice.gc.ca/eng/acts/e-4.5/page-1.html.
- Footnote 149
-
Emergency Management Act. Revised Statutes of Canada (2007, c. 15); Available from: https://laws-lois.justice.gc.ca/eng/acts/e-4.56/.
- Footnote 150
-
Public Safety Canada. Federal, Provincial, and Territorial Emergency Management Strategy Interim Action Plan 2021-22. Government of Canada; 2022.
- Footnote 151
-
Government of Canada. Federal/Provincial/Territorial Public Health Response Plan for Biological Events. Government of Canada2017.
- Footnote 152
-
Public Health Agency of Canada. Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector. Government of Canada; 2022.
- Footnote 153
-
Environment and Natural Resources Canada. Canada's National Adaptation Strategy: Building Resilient Communities and a Strong Economy. Government of Canada; 2023.
- Footnote 154
-
Métis National Council. Métis National Council Emergency Management Review. Métis Nations; 2022.
- Footnote 155
-
Assembly of First Nations. Emergency Services. Assembly of First Nations; Available from: https://www.afn.ca/policy-sectors/housing-infrastructure-water-emergency-services/emergency-services/.
- Footnote 156
-
Métis National Council. Emergency Management. Métis National Council; Available from: https://www.metisnation.ca/what-we-do/environment/emergency-management.
- Footnote 157
-
World Health Organization. Technical Brief: Essential Public Health Functions. World Health Organization; 2022.
- Footnote 158
-
Naylor, D, Basrur, S, Bergeron, MG, Brunham, RC, Butler-Jones, D, Dafoe, G, et al. Learning from SARS: Renewal of Public Health in Canada. Ottawa, ON: National Advisory Committee on SARS and Public Health; 2003.
- Footnote 159
-
Canadian Public Health Association. Public Health in the Context of Health System Renewal in Canada: Position Statement. Canadian Public Health Association; 2019.
- Footnote 160
-
Health Canada, Public Health Agency of Canada. Internal Training – Emergency Management and Public Health (FG408). Government of Canada; 2023.
- Footnote 161
-
Government of Canada. Federal Emergency Management. Government of Canada; 2021.
- Footnote 162
-
World Health Organization. WHO Coronavirus (COVID-19) Dashboard. World Health Organization; 2023.
- Footnote 163
-
Pan American Health Organization. Strategy for Building Resilient Health Systems and Post-COVID-19 Pandemic Recovery to Sustain and Protect Public Health Gains. Washington, D. C.: Pan American Health Organization; 2022.
- Footnote 164
-
Lazarus, JV, Romero, D, Kopka, CJ, Karim, SA, Abu-Raddad, LJ, Almeida, G, et al. A Multinational Delphi Consensus to End the COVID-19 Public Health Threat. Nature. 2022; 611(7935):332-45.
- Footnote 165
-
United Nations Office for Disaster Risk Reduction. Sendai Framework for Disaster Risk Reduction 2015-2030. United Nations; 2015.
- Footnote 166
-
Bournival, V, Oostlander, SA, O'Sullivan, TL. 'Lifestyle Drift' in Disaster Risk Reduction Practices Magnifies Inequities for High-Risk Populations. SSM - Qualitative Research in Health. 2022; 2:100190.
- Footnote 167
-
Stephen, C. Rethinking Pandemic Preparedness in the Anthropocene. Healthcare Management Forum. 2019; 33(4):153-7.
- Footnote 168
-
Baum, F. How Can Health Promotion Contribute to Pulling Humans Back from the Brink of Disaster? Global Health Promotion. 2021; 28(4):64-72.
- Footnote 169
-
The 1st International Conference on Health Promotion, Ottawa, 1986. World Health Organization; Available from: https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference.
- Footnote 170
-
Tu'itahi, S, Watson, H, Egan, R, Parkes, MW, Hancock, T. Waiora: The Importance of Indigenous Worldviews and Spirituality to Inspire and Inform Planetary Health Promotion in the Anthropocene. Global Health Promotion. 2021; 28(4):73-82.
- Footnote 171
-
Sanchez-Pimienta, CE, Masuda, J, M'Wikwedong Indigenous Friendship, C. From Controlling to Connecting: M'wikwedong as a Place of Urban Indigenous Health Promotion in Canada. Health Promotion International. 2021; 36(3):703-13.
- Footnote 172
-
Tiohtià:Ke Statement: Catalysing Policies for Health, Well-Being and Equity. Global Health Promotion. 2022; 29(4):3-7.
- Footnote 173
-
Loppie, C. Chapter 10: Promising Practices in Indigenous Community Health Promotion. In: Rootman I, Pederson A, Frohlich K, Dupéré S, editors. Health Promotion in Canada: New Perspectives on Theory, Practice, Policy, and Research, Fourth Edition. Toronto, ON: Canadian Scholars Press; 2017.
- Footnote 174
-
World Health Organization. Track 1: Community Empowerment. World Health Organization.
- Footnote 175
-
Räsänen, A, Lein, H, Bird, D, Setten, G. Conceptualizing Community in Disaster Risk Management. International Journal of Disaster Risk Reduction. 2020; 45:101485.
- Footnote 176
-
Government of Ontario. Appendix B: Emergency Management Glossary. In: Provincial Emergency Response Plan. Government of Ontario; 2022.
- Footnote 177
-
Madsen, W. Early 20th Century Conceptualization of Health Promotion. Health Promotion International. 2017; 32(6):1041-7.
- Footnote 178
-
Rutty, C, Sullivan, SC. This Is Public Health: A Canadian History. Ottawa, ON: Canadian Public Health Association; 2010.
- Footnote 179
-
Public Health Agency of Canada. A New Perspective on the Health of Canadians. Government of Canada; 2001.
- Footnote 180
-
Potvin, L, Jones, CM. Twenty-Five Years after the Ottawa Charter: The Critical Role of Health Promotion for Public Health. Canadian Journal of Public Health. 2011; 102(4):244-8.
- Footnote 181
-
Marcello, T, Kwok-Cho, T, Pierre-Gerlier, F. Canada Needs a "Health in All Policies" Action Plan Now. Canadian Medical Association Journal. 2020; 192(3):E61.
- Footnote 182
-
BC Centre for Disease Control. Healthy Social Environments Framework. BC Healthy Communities; 2020. Available from: http://bchealthycommunities.ca/wp-content/uploads/2020/11/SE-Framework-Summary-V1-Dec2020.pdf.
- Footnote 183
-
Health Canada. Social Determinants of Health and Health Inequalities. Government of Canada; 2022.
- Footnote 184
-
Kickbusch, I. Visioning the Future of Health Promotion. Glob Health Promot. 2021; 28(4):56-63.
- Footnote 185
-
Borges do Nascimento, IJ, Pizarro, AB, Almeida, JM, Azzopardi-Muscat, N, Gonçalves, MA, Björklund, M, et al. Infodemics and Health Misinformation: A Systematic Review of Reviews. Bulletin of the World Health Organization. 2022; 100(9):544-61.
- Footnote 186
-
Li, X, Farrukh, M, Lee, C, Khreis, H, Sarda, S, Sohrabi, S, et al. COVID-19 Impacts on Mobility, Environment, and Health of Active Transportation Users. Cities. 2022; 131:103886.
- Footnote 187
-
Chen, T. Transitioning from COVID-19 Restrictions to New Norms: Innovating Strategies to Restore Trust and Transit Ridership. National Collaborating Centre for Environmental Health; 2021.
- Footnote 188
-
Renne, JL, Mayorga, E. What Has America Learned since Hurricane Katrina? Evaluating Evacuation Plans for Carless and Vulnerable Populations in 50 Large Cities across the United States. International Journal of Disaster Risk Reduction. 2022; 80:103226.
- Footnote 189
-
Renne, JL. Emergency Evacuation Planning Policy for Carless and Vulnerable Populations in the United States and United Kingdom. International Journal of Disaster Risk Reduction. 2018; 31:1254-61.
- Footnote 190
-
Canadian Public Health Association. Action Statement for Health Promotion in Canada. Canadian Public Health Association; 1996.
- Footnote 191
-
Jackson, SF, Morgan, GT, Gloger, A, Luca, S, Cerda, E, Poland, B. Relationships Are Everything: The Underpinnings of Grassroots Community Action in the COVID-19 Pandemic in Toronto. Cities. 2023; 134:104163.
- Footnote 192
-
Mulligan, K. Strengthening Community Connections: The Future of Public Health Is at the Neighbourhood Scale. Toronto, ON: University of Toronto, Dalla Lana School of Public Health; 2022.
- Footnote 193
-
World Health Organization. Achieving Well-Being - a Draft Global Framework for Integrating Well-Being into Public Health Utilizing a Health Promotion Approach. World Health Organization; 2022.
- Footnote 194
-
World Health Organization. Geneva Charter for Well-Being. World Health Organization; 2022.
- Footnote 195
-
Dhamanaskar, R, Abelson, J, Boothe, K, Massie, J, You, J, Just, D, et al. Trends in Public Engagement in Canadian Health Policy from 2000-2021: Results from a Comparative Descriptive Analysis McMaster University; 2022.
- Footnote 196
-
National Collaborating Centre for Indigenous Health. Visioning the Future: First Nations, Inuit, & Métis Population and Public Health. Prince George, BC: National Collaborating Centre for Indigenous Health; 2021.
- Footnote 197
-
Hoffman, KM, Christianson, AC, Dickson-Hoyle, S, Copes-Gerbitz, K, Nikolakis, W, Diabo, DA, et al. The Right to Burn: Barriers and Opportunities for Indigenous-Led Fire Stewardship in Canada. FACETS. 2022; 7:464-81.
- Footnote 198
-
Tsilhqot'in National Government. Tsilhqot'in in the Time of COVID: Strengthening Tsilhqot'in Ways to Protect Our People. Tsilhqot'in National Government; 2021.
- Footnote 199
-
Anderson, M, MacKinnon, M. We Can Learn from the COVID-19 Pandemic Management Strategy of First Nations Communities in Canada. British Medical Journal. 2023; 382:p1675.
- Footnote 200
-
Health Canada. First Nations Mental Wellness Continuum Framework. Ottawa, ON: Health Canada; 2015.
- Footnote 201
-
Thomas, D, Mitchell, T, Arseneau, C. Re-Evaluating Resilience: From Individual Vulnerabilities to the Strength of Cultures and Collectivities among Indigenous Communities. Resilience. 2016; 4(2):116-29.
- Footnote 202
-
First Nations Health Authority, Office of the Provincial Health Officer. First Nations Population Health and Wellness Agenda. First Nations Health Authority, Office of the Provincial Health Officer; 2021.
- Footnote 203
-
The Truth and Reconciliation Commission of Canada. Honouring the Truth, Reconciling for the Future: Summary of the Final Report of the Truth and Reconciliation Commission of Canada. The Truth and Reconciliation Commission of Canada; 2015.
- Footnote 204
-
Blackstock, C. United Nations Declaration on the Rights of Indigenous Peoples for Indigenous Adolescents. New York, NY: UNICEF; 2013.
- Footnote 205
-
Crown-Indigenous Relations and Northern Affairs Canada. The Government of Canada's Approach to Implementation of the Inherent Right and the Negotiation of Aboriginal Self-Government. Government of Canada; 2023.
- Footnote 206
-
United Nations. Universal Declaration of Human Rights. United Nations.
- Footnote 207
-
United Nations Human Rights Treaty Bodies. Committee on the Elimination of Racial Discrimination. United Nations; 2023.
- Footnote 208
-
Indigenous Services Canada. Grants and Contributions to Support Urban Programming for Indigenous Peoples. Government of Canada; 2022.
- Footnote 209
-
Standing Committee on Indigenous and Northern Affairs. Arctic Security and Sovereignty, and the Emergency Preparedness of Indigenous Communities. Parliament of Canada; 2023.
- Footnote 210
-
Indian Act. Revised Statutes of Canada (1985, c. I-5); Available from: https://laws-lois.justice.gc.ca/eng/acts/I-5/section-81.html.
- Footnote 211
-
Crown-Indigenous Relations and Northern Affairs Canada. Inuit Nunangat Policy. Government of Canada; 2022.
- Footnote 212
-
Indigenous Services Canada. Urban Programming for Indigenous Peoples. Government of Canada; 2022.
- Footnote 213
-
National Association of Friendship Centres. Lack of Emergency Support for Friendship Centres Ties Hands and Delays Response. GlobeNewswire; 2023.
- Footnote 214
-
Statistics Canada. Indigenous Population Continues to Grow and Is Much Younger Than the Non-Indigenous Population, Although the Pace of Growth Has Slowed. The Daily; 2022.
- Footnote 215
-
Assembly of First Nations. Sector Update - Governance: Emergency Services Unit. Assembly of First Nations; 2021.
- Footnote 216
-
British Columbia Assembly of First Nations. Emergency Management MOU. 2019.
- Footnote 217
-
Nisga'a Lisims Government. Emergency Management Overview. Nisga'a Lisims Government; 2012.
- Footnote 218
-
Nisga'a Lisims Government. About - Accomplishments and Benefits of Nisga'a Treaty. Nisga'a Lisims Government.
- Footnote 219
-
Inuit Tapiriit Kanatami. National Inuit Climate Change Strategy. Inuit Tapiriit Kanatami; 2019.
- Footnote 220
-
Prime Minister of Canada. Working in Partnership to Make Life Better for Métis. Government of Canada; 2023.
- Footnote 221
-
United Nations Climate Change. How Indigenous Peoples Enrich Climate Action. United Nations Climate Change; 2022.
- Footnote 222
-
United Nations Office for Disaster Risk Reduction. Using Traditional Knowledges for Disaster Risk Reduction: Words into Action. United Nations Office for Disaster Risk Reduction; 2022.
- Footnote 223
-
Intergovernmental Panel on Climate Change. Summary for Policymakers. In: Core Writing Team, Lee H, Romero J, editors. Climate Change 2023: Synthesis Report. Geneva, Switzerland: Intergovernmental Panel on Climate Change; 2023. p. 1-34.
- Footnote 224
-
Lambert, SJ, Scott, JC. International Disaster Risk Reduction Strategies and Indigenous Peoples. International Indigenous Policy Journal. 2019; 10(2).
- Footnote 225
-
First Nations Health Authority. #Itstartswithme FNHA's Policy Statement on Cultural Safety and Humility. West Vancouver, BC: First Nations Health Authority.
- Footnote 226
-
Canada School of Public Service. Call to Action 57: A Duty of Reconciliation with Indigenous Peoples for All Public Servants (Ira1-V40). Government of Canada; 2022.
- Footnote 227
-
Office of the Auditor General of Canada. Emergency Management in First Nations Communities. Government of Canada; 2022.
- Footnote 228
-
Eykelbosh, A, Slett, CM, Wilson, P, Pillsworth, L, Luttrell, G, Reid, D. Supporting Indigenous Communities during Environmental Public Health Emergencies. Environmental Health Review. 2018; 61(1):9-11.
- Footnote 229
-
Assembly of First Nations. Advocating to Ensure Access and Support for Emergency Management in First Nations Communities. Assembly of First Nations; 2023.
- Footnote 230
-
Public Safety Canada. Emergency Management in Indigenous Communities. Government of Canada; 2019.
- Footnote 231
-
Tzembelicos, A, Erhardt, A, de Faye, B, Guy, B, Kent, C, Bedwell, C, et al. Addressing the New Normal: 21st Century Disaster Management in British Columbia. British Columbia Government; 2018.
- Footnote 232
-
Waakebiness-Bryce Institute for Indigenous Health. What We Heard: Indigenous Peoples and COVID-19: Public Health Agency of Canada's Companion Report. Public Health Agency of Canada; 2021.
- Footnote 233
-
The Standing Committee on Indigenous and Northern Affairs. From the Ashes: Reimagining Fire Safety and Emergency Management in Indigenous Communities. House of Commons Canada; 2018.
- Footnote 234
-
First Nations Health Authority. New Declaration Commits to Cultural Safety in Emergency Management Services in BC. First Nations Health Authority; 2019.
- Footnote 235
-
Phibbs, S, Kenney, C, Severinsen, C, Mitchell, J, Hughes, R. Synergising Public Health Concepts with the Sendai Framework for Disaster Risk Reduction: A Conceptual Glossary. International Journal of Environmental Research and Public Health. 2016; 13(12).
- Footnote 236
-
Environment and Climate Change Canada. Government of Canada Adaptation Action Plan. Gatineau, QC: Environment and Climate Change Canada; 2023.
- Footnote 237
-
Environment and Natural Resources Canada. Canada's Climate Plans and Targets. Government of Canada; 2022.
- Footnote 238
-
The Independent Panel for Pandemic Preparedness and Response. COVID-19: Make It the Last Pandemic. The Independent Panel for Pandemic Preparedness and Response; 2021.
- Footnote 239
-
Skea, J, Shukla, PR, Reisinger, A, Slade, R, Fradera, R, Pathak, M, et al. Climate Change 2022 Mitigation of Climate Change: Summary for Policy Makers. Intergovernmental Panel on Climate Change; 2022.
- Footnote 240
-
World Health Organization. A Health Perspective on the Role of the Environment in One Health. World Health Organization; 2022.
- Footnote 241
-
One Health High-Level Expert Panel. One Health High-Level Expert Panel Annual Report 2021. World Health Organization; 2021.
- Footnote 242
-
Mubareka, S, Amuasi, J, Carabin, H, Jack, JC, Jardine, C, Keefe, G, et al. Strengthening a One Health Approach to Emerging Zoonoses. Royal Society of Canada; 2022.
- Footnote 243
-
Tariq, H, Pathirage, C, Fernando, T. Measuring Community Disaster Resilience at Local Levels: An Adaptable Resilience Framework. International Journal of Disaster Risk Reduction. 2021; 62:102358.
- Footnote 244
-
Abrash Walton, A, Marr, J, Cahillane, MJ, Bush, K. Building Community Resilience to Disasters: A Review of Interventions to Improve and Measure Public Health Outcomes in the Northeastern United States. Sustainability. 2021; 13(21).
- Footnote 245
-
Poland, B, Gloger, A, Morgan, GT, Lach, N, Jackson, SF, Urban, R, et al. A Connected Community Approach: Citizens and Formal Institutions Working Together to Build Community-Centred Resilience. International Journal of Environmental Research and Public Health. 2021; 18(19).
- Footnote 246
-
Kidd, SA, Greco, S, McKenzie, K. Global Climate Implications for Homelessness: A Scoping Review. Journal of Urban Health. 2021; 98(3):385-93.
- Footnote 247
-
Morris, SC. Disaster Planning for Homeless Populations: Analysis and Recommendations for Communities. Prehospital and Disaster Medicine. 2020; 35(3):322-5.
- Footnote 248
-
Sundareswaran, M, Ghazzawi, A, O'Sullivan, TL. Upstream Disaster Management to Support People Experiencing Homelessness. PLoS Curr. 2015; 7.
- Footnote 249
-
Pierce, JR, Morley, SK, West, TA, Pentecost, P, Upton, LA, Banks, L. Improving Long-Term Care Facility Disaster Preparedness and Response: A Literature Review. Disaster Medicine and Public Health Preparedness. 2017; 11(1):140-9.
- Footnote 250
-
Ricciardelli, R, Bucerius, S, Tetrault, J, Crewe, B, Pyrooz, D. Correctional Services during and Beyond COVID-19. FACETS. 2021; 6:490-516.
- Footnote 251
-
Labesse, ME, St-Louis, A, Ades, J, Robitaille, É, Bergeron, P. Housing and Social Inequalities in Health in Times of COVID-19: Strategies for Promoting Affordable Quality Housing. Institut national de santé publique du Québec; 2022.
- Footnote 252
-
Office of the Chief Science Advisor of Canada. Long-Term Care and COVID-19: Report of a Special Task Force Prepared for the Chief Science Advisor of Canada. Government of Canada; 2020.
- Footnote 253
-
Yang, F-J, Aitken, N. People Living in Apartments and Larger Households Were at Higher Risk of Dying from COVID-19 during the First Wave of the Pandemic. Statistics Canada; 2021.
- Footnote 254
-
Persaud, N, Woods, H, Workentin, A, Adekoya, I, Dunn, JR, Hwang, SW, et al. Recommendations for Equitable COVID-19 Pandemic Recovery in Canada. Canadian Medical Association Journal. 2021; 193(49):E1878.
- Footnote 255
-
Swope, C, Hernández, D, Yoon, L. The Four Pillars of Housing Influencing Health Equity. National Collaborating Centre for Environmental Health; 2023.
- Footnote 256
-
Baxter, AJ, Tweed, EJ, Katikireddi, SV, Thomson, H. Effects of Housing First Approaches on Health and Well-Being of Adults Who Are Homeless or at Risk of Homelessness: Systematic Review and Meta-Analysis of Randomised Controlled Trials. Journal of Epidemiology and Community Health. 2019; 73(5):379.
- Footnote 257
-
Hey Neighbour Collective. Building Resilience and Emergency Preparedness through Social Connections: Video. Hey Neighbour Collective; 2023.
- Footnote 258
-
Graveline, M-H, Germain, D. Disaster Risk Resilience: Conceptual Evolution, Key Issues, and Opportunities. International Journal of Disaster Risk Science. 2022; 13(3):330-41.
- Footnote 259
-
Federal Emergency Management Agency. Community Resilience Indicator Analysis: Commonly Used Indicators from Peer-Reviewed Research: Updated for Research Published 2003-2021 Federal Emergency Management Agency; 2022.
- Footnote 260
-
Asadzadeh, A, Kötter, T, Salehi, P, Birkmann, J. Operationalizing a Concept: The Systematic Review of Composite Indicator Building for Measuring Community Disaster Resilience. International Journal of Disaster Risk Reduction. 2017; 25:147-62.
- Footnote 261
-
Cariolet, J-M, Vuillet, M, Diab, Y. Mapping Urban Resilience to Disasters – a Review. Sustainable Cities and Society. 2019; 51:101746.
- Footnote 262
-
Carvalhaes, TM, Chester, MV, Reddy, AT, Allenby, BR. An Overview & Synthesis of Disaster Resilience Indices from a Complexity Perspective. International Journal of Disaster Risk Reduction. 2021; 57:102165.
- Footnote 263
-
Patel, SS, Rogers, MB, Amlôt, R, Rubin, GJ. What Do We Mean by 'Community Resilience'? A Systematic Literature Review of How It Is Defined in the Literature. PLoS Currents. 2017; 9.
- Footnote 264
-
Fitzgibbons, J, Mitchell, CL. Inclusive Resilience: Examining a Case Study of Equity-Centred Strategic Planning in Toronto, Canada. Cities. 2021; 108:102997.
- Footnote 265
-
Meerow, S, Pajouhesh, P, Miller, TR. Social Equity in Urban Resilience Planning. Local Environment. 2019; 24(9):793-808.
- Footnote 266
-
Isbister-Bear, O, Hatala, A, Sjoblom, E. Strengthening Âhkamêyimo among Indigenous Youth: The Social Determinants of Health, Justice, and Resilience in Canada's North. Journal of Indigenous Well-being. 2017; 2(3):76-89.
- Footnote 267
-
Preston, V, Shields, J, Akbar, M. Migration and Resilience in Urban Canada: Why Social Resilience, Why Now? Journal of International Migration and Integration. 2022; 23(3):1421-41.
- Footnote 268
-
Gyan, C, Chireh, B, Chuks-Eboka, N, Yeboah, AS. Reconsidering the Conceptualization of Resilience: The Experiences of Refugee and Immigrant Youth in Montreal. Applied Research in Quality of Life. 2023.
- Footnote 269
-
Goddard-Durant, SK, Doucet, A, Tizaa, H, Sieunarine, JA. A Decolonizing, Intersectional, Black Feminist Approach to Young Black Caribbean-Canadian Mothers' Resilience. Journal of Family Studies. 2022:1-21.
- Footnote 270
-
Hutcheon, E, Lashewicz, B. Theorizing Resilience: Critiquing and Unbounding a Marginalizing Concept. Disability & Society. 2014; 29(9):1383-97.
- Footnote 271
-
Morgan, GT, Poland, B, Jackson, SF, Gloger, A, Luca, S, Lach, N, et al. A Connected Community Response to COVID-19 in Toronto. Global Health Promotion. 2021; 29(1):101-4.
- Footnote 272
-
Latham, A, Layton, J. Social Infrastructure and the Public Life of Cities: Studying Urban Sociality and Public Spaces. Geography Compass. 2019; 13(7):e12444.
- Footnote 273
-
Davern, M, Gunn, L, Whitzman, C, Higgs, C, Giles-Corti, B, Simons, K, et al. Using Spatial Measures to Test a Conceptual Model of Social Infrastructure That Supports Health and Wellbeing. Cities & Health. 2017; 1(2):194-209.
- Footnote 274
-
Lauer, S, Yan, MC. Social Infrastructure and Social Capacity Development among Newcomers to Canada: The Role of Neighborhood Houses in Vancouver. Journal of International Migration and Integration. 2022; 23(2):911-29.
- Footnote 275
-
Praznik, J, Shields, J. An Anatomy of Settlement Services in Canada: A Guide. Social Sciences and Humanities Research Council of Canada; 2018.
- Footnote 276
-
Statistics Canada. Immigrants Make up the Largest Share of the Population in over 150 Years and Continue to Shape Who We Are as Canadians. The Daily; 2022.
- Footnote 277
-
O'Sullivan, TL, Kuziemsky, CE, Toal-Sullivan, D, Corneil, W. Unraveling the Complexities of Disaster Management: A Framework for Critical Social Infrastructure to Promote Population Health and Resilience. Social Science & Medicine. 2013; 93:238-46.
- Footnote 278
-
Murray, S, Poland, B. Neighbourhood Climate Resilience: Lessons from the Lighthouse Project. Canadian Journal of Public Health. 2020; 111(6):890-6.
- Footnote 279
-
Jewett, RL, Mah, SM, Howell, N, Larsen, MM. Social Cohesion and Community Resilience During COVID-19 and Pandemics: A Rapid Scoping Review to Inform the United Nations Research Roadmap for COVID-19 Recovery. International Journal of Health Services. 2021; 51(3):325-36.
- Footnote 280
-
Dalmer, NK, McKenzie, P, Rothbauer, P, Martin-Yeboah, E, Oswald, K. Palaces for the People: Mapping Public Libraries' Capacity for Social Connection and Inclusion. FIMS Publications; 2022.
- Footnote 281
-
Bhardwaj, M, Mamatis, D, Sanford, S. Promoting Health and Well-Being through Social Inclusion in Toronto: Local Scan of Interventions to Promote Social Inclusion. Toronto Public Health, Wellesley Institute; 2019.
- Footnote 282
-
Poulin, V, Provencher, V, Nicole, M, Shea, V, Aubin, G, Beaulieu, M, et al. Challenges and Strategies to Adapt the Provision of Support Services to Older Adults and Caregivers During the COVID-19 Pandemic: The Perspective of Community Organizations. Canadian Journal on Aging / La Revue canadienne du vieillissement. 2021; 40(4):591-603.
- Footnote 283
-
Ramsbottom, A, O'Brien, E, Ciotti, L, Takacs, J. Enablers and Barriers to Community Engagement in Public Health Emergency Preparedness: A Literature Review. Journal of Community Health. 2018; 43(2):412-20.
- Footnote 284
-
Piltch-Loeb, R, Bernard, D, Quiñones Vallejo, B, Harriman, N, Savoia, E. Engaging Community Leaders in Sharing Local Knowledge for Emergency Preparedness to Leverage Communication and Trusted Assets for Vulnerable Populations. Disaster Medicine and Public Health Preparedness. 2022; 16(4):1452-8.
- Footnote 285
-
Cassetti, V, Powell, K, Barnes, A, Sanders, T. A Systematic Scoping Review of Asset-Based Approaches to Promote Health in Communities: Development of a Framework. Global Health Promotion. 2019; 27(3):15-23.
- Footnote 286
-
Martin-Kerry, J, McLean, J, Hopkins, T, Morgan, A, Dunn, L, Walton, R, et al. Characterizing Asset-Based Studies in Public Health: Development of a Framework. Health Promotion International. 2023; 38(2).
- Footnote 287
-
Généreux, M, Petit, G, Roy, M, Maltais, D, O'Sullivan, T. The "Lac-Mégantic Tragedy" Seen through the Lens of the EnRiCH Community Resilience Framework for High-Risk Populations. Canadian Journal of Public Health. 2018; 109(2):261-7.
- Footnote 288
-
Généreux, M, Roy, M, O'Sullivan, T, Maltais, D. Salutogenesis as a Framework for Social Recovery after Disaster. In: Mittelmark MB, Bauer GF, Vaandrager L, Pelikan JM, Sagy S, Eriksson M, et al., editors. The Handbook of Salutogenesis. Cham: Springer International Publishing; 2022. p. 533-42.
- Footnote 289
-
Généreux, M, Maltais, D. Social Reconstruction of the Lac-Mégantic Community Following the Tragedy: Assessment of the First Six Years. Centre Intégré universitaire de santé et de services sociaux de l'Estrie; 2019.
- Footnote 290
-
Canadian Women's Foundation, Ontario Nonprofit Network, Canadian Centre for Policy Alternatives, Lahey, K. Resetting Normal: Funding a Thriving Women's Sector. Canadian Women's Foundation; 2020.
- Footnote 291
-
Edwards, C, Jensen, E, Muermann, S. Core Funding: Supporting Nonprofit Missions, Resilience and Impact. Imagine Canada; 2022.
- Footnote 292
-
Ayer, S, Anderson, P. Trust & Impact: Funders' Perspectives on Unrestricted Funding. Imagine Canada; 2022.
- Footnote 293
-
City of Vancouver. Spaces to Thrive: Vancouver Social Infrastructure Strategy - Policy Framework. City of Vancouver; 2021.
- Footnote 294
-
Holden, M, Firth, C, Fassihi, F. South Vancouver and Marpole Neighbourhood Equity Report. Simon Fraser University; 2021.
- Footnote 295
-
Abdalla, SM, Koya, SF, Jamieson, M, Verma, M, Haldane, V, Jung, A-S, et al. Investing in Trust and Community Resilience: Lessons from the Early Months of the First Digital Pandemic. BMJ. 2021; 375:e067487.
- Footnote 296
-
The Independent Panel for Pandemic Preparedness and Response. Centering Communities in Pandemic Preparedness and Response - Background Paper 10. The Independent Panel for Pandemic Preparedness and Response; 2021.
- Footnote 297
-
Bergeron, G, Cadieux, G, Sachdeva, H, Shahin, R. Mpox Outbreaks in Montreal & Toronto: Successes, Challenges & Lessons Learned. The Ontario Public Health Convention; 2023.
- Footnote 298
-
Harrison, LB, Bergeron, G, Cadieux, G, Charest, H, Fafard, J, Levade, I, et al. Monkeypox in Montréal: Epidemiology, Phylogenomics, and Public Health Response to a Large North American Outbreak. Annals of Internal Medicine. 2022; 176(1):67-76.
- Footnote 299
-
Institut national de santé publique du Québec. L'INSPQ et Ses Partenaires Évaluent L'efficacité Vaccinale Contre la Variole Simienne. Institut national de santé publique du Québec; 2023.
- Footnote 300
-
Khan, Y, O'Sullivan, T, Brown, A, Tracey, S, Gibson, J, Généreux, M, et al. Public Health Emergency Preparedness: A Framework to Promote Resilience. BMC Public Health. 2018; 18(1):1344.
- Footnote 301
-
Vancouver Coastal Health. Policy Tools to Create and Support Cooler, Safer Indoor Living Spaces. Vancouver Coastal Health; 2023.
- Footnote 302
-
Vancouver Coastal Health, Fraser Health. Heat Check-in Support Framework for Non-Governmental Organizations. Vancouver Coastal Health,; 2023.
- Footnote 303
-
BC Gov News. Province Launches New Initiative to Protect People during Extreme Heat Emergencies. Government of British Columbia; 2023.
- Footnote 304
-
City of Vancouver. Council Meeting Minutes - May 17, 2022. City of Vancouver; 2022.
- Footnote 305
-
City of Vancouver. Climate Emergency – Bylaw and Policy Updates Applicable to New Buildings City of Vancouver; 2022.
- Footnote 306
-
Eisenman, DP, Galway, LP. The Mental Health and Well-Being Effects of Wildfire Smoke: A Scoping Review. BMC Public Health. 2022; 22(1):2274.
- Footnote 307
-
Glenn, N, Myre, M. Post-Flooding Community-Level Psychosocial Impacts and Priorities in Canada: A Preliminary Report. Vancouver, BC: National Collaborating Centre for Environmental Health; 2022.
- Footnote 308
-
British Columbia's Office of the Human Rights Commissioner. From Hate to Hope: Report of the Inquiry into Hate in the COVID-19 Pandemic. Vancouver, BC: British Columbia's Office of the Human Rights Commissioner; 2023.
- Footnote 309
-
Lee, JM, Jansen, R, Sanderson, KE, Guerra, F, Keller-Olaman, S, Murti, M, et al. Public Health Emergency Preparedness for Infectious Disease Emergencies: A Scoping Review of Recent Evidence. BMC Public Health. 2023; 23(1):420.
- Footnote 310
-
Perri, M, Dosani, N, Hwang, SW. COVID-19 and People Experiencing Homelessness: Challenges and Mitigation Strategies. Canadian Medical Association Journal. 2020; 192(26):E716.
- Footnote 311
-
Oudshoorn, A, Benjamin, T, Smith-Carrier, TA, Benbow, S, Marshall, CA, Kennedy, R, et al. A Rapid Review of Practices to Support People Experiencing Homelessness during COVID-19. Housing, Care and Support. 2021; 24(3/4):105-22.
- Footnote 312
-
Mantler, T, Veenendaal, J, Wathen, CN. Exploring the Use of Hotels as Alternative Housing by Domestic Violence Shelters During COVID-19. International Journal on Homelessness. 2021; 1(1):32-49.
- Footnote 313
-
Xuereb, S, Jones, C. Estimating No-Fault Evictions in Canada: Understanding BC's Disproportionate Eviction Rate in the 2021 Canadian Housing Survey. Balanced Supply of Housing Research Partnership; 2023.
- Footnote 314
-
Edmonds, J, Flahault, A. Refugees in Canada during the First Wave of the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(3).
- Footnote 315
-
Glover, RE, van Schalkwyk, MCI, Akl, EA, Kristjannson, E, Lotfi, T, Petkovic, J, et al. A Framework for Identifying and Mitigating the Equity Harms of COVID-19 Policy Interventions. Journal of Clinical Epidemiology. 2020; 128:35-48.
- Footnote 316
-
United Nations. UN Research Roadmap for the COVID-19 Recovery: Leveraging the Power of Science for a More Equitable, Resilient and Sustainable Future. United Nations; 2020.
- Footnote 317
-
World Health Organization. Community Engagement: A Health Promotion Guide for Universal Health Coverage in the Hands of the People. Geneva: World Health Organization; 2020.
- Footnote 318
-
Brown, C, Jackson, E, Harford, D, Bristow, D. Chapter 2: Cities and Towns. In: Warren FJ, Lulham N, editors. Canada in a Changing Climate: National Issues Report. Ottawa, ON: Government of Canada; 2021.
- Footnote 319
-
Public Health Physicians of Canada. Public Health Lessons Learned from the COVID-19 Pandemic. Public Health Physicians of Canada; 2022.
- Footnote 320
-
Haldane, V, Jung, A-S, De Foo, C, Bonk, M, Jamieson, M, Wu, S, et al. Strengthening the Basics: Public Health Responses to Prevent the Next Pandemic. British Medical Journal. 2021; 375:e067510.
- Footnote 321
-
Gautier, L, Di Ruggiero, E, Jackson, C, Bentayeb, N, Blain, M-J, Chowdhury, F, et al. Learning from Intersectoral Initiatives to Respond to the Needs of Refugees, Asylum Seekers, and Migrants without Status in the Context of COVID-19 in Quebec and Ontario: A Qualitative Multiple Case Study Protocol. Health Research Policy and Systems. 2023; 21(1):59.
- Footnote 322
-
Mantler, T, Wathen, CN, Burd, C, MacGregor, JCD, McLean, I, Veenendaal, J. Navigating Multiple Pandemics: A Critical Analysis of the Impact of COVID-19 Policy Responses on Gender-Based Violence Services. Critical Social Policy. 2022; 43(1):29-50.
- Footnote 323
-
Social Policy and Projects Research and Data Team. Vancouver's Non-Profit Sector: Current State Analysis. 2020.
- Footnote 324
-
Lee, J-K, Bullen, C, Ben Amor, Y, Bush, SR, Colombo, F, Gaviria, A, et al. Institutional and Behaviour-Change Interventions to Support COVID-19 Public Health Measures: A Review by the Lancet Commission Task Force on Public Health Measures to Suppress the Pandemic. International Health. 2021; 13(5):399-409.
- Footnote 325
-
National Collaborating Centres for Public Health. Out of the Ashes: Ashcroft Indian Band and the Elephant Hill Wildfire - Insights for a Public Health Response to Long-Term Evacuation (Case Study #1). National Collaborating Centres for Public Health; 2021.
- Footnote 326
-
International Federation of the Red Cross and Red Crescent Societies. What Is the EVCA? : International Federation of the Red Cross and Red Crescent Societies; 2018.
- Footnote 327
-
Heller, JC, Little, OM, Faust, V, Tran, P, Givens, ML, Ayers, J, et al. Theory in Action: Public Health and Community Power Building for Health Equity. Journal of Public Health Management and Practice. 2023; 29(1).
- Footnote 328
-
Myre, M, Glenn, N. A Guide to Post-Flooding Community-Level Psychosocial Response and Recovery in Canada. National Collaborating Centre for Environmental Health; 2023.
- Footnote 329
-
Public Health Ontario. Trauma-Informed Practices for Children and Families during the COVID-19 Pandemic. Public Health Ontario; 2020.
- Footnote 330
-
Rosenberg, H, Errett, NA, Eisenman, DP. Working with Disaster-Affected Communities to Envision Healthier Futures: A Trauma-Informed Approach to Post-Disaster Recovery Planning. International Journal of Environmental Research and Public Health. 2022; 19(3).
- Footnote 331
-
Heris, CL, Kennedy, M, Graham, S, Bennetts, SK, Atkinson, C, Mohamed, J, et al. Key Features of a Trauma-Informed Public Health Emergency Approach: A Rapid Review. Frontiers in Public Health. 2022; 10.
- Footnote 332
-
World Health Organization. Mainstreaming Gender within the WHO Health Emergencies Programme: 2022–2026 Strategy. Geneva: World Health Organization; 2022.
- Footnote 333
-
Pan American Health Organization. Key Considerations for Integrating Gender Equality into Health Emergency and Disaster Response: COVID-19. Pan American Health Organization; 2020.
- Footnote 334
-
Jesus, TS, Kamalakannan, S, Bhattacharjya, S, Bogdanova, Y, Arango-Lasprilla, JC, Bentley, J, et al. Preparedness, Response and Systemic Transformation (Pre-Re-Syst): A Model for Disability-Inclusive Pandemic Responses and Systemic Disparities Reduction Derived from a Scoping Review and Thematic Analysis. International Journal for Equity in Health. 2021; 20(1):204.
- Footnote 335
-
Finucane, ML, Warren May, L, Chang, J. A Scoping Literature Review on Indicators and Metrics for Assessing Racial Equity in Disaster Preparation, Response, and Recovery. Santa Monica, CA: RAND Corporation; 2021.
- Footnote 336
-
Phillips II, G, Felt, D, Ruprecht, MM, Wang, X, Xu, J, Pérez-Bill, E, et al. Addressing the Disproportionate Impacts of the COVID-19 Pandemic on Sexual and Gender Minority Populations in the United States: Actions toward Equity. LGBT Health. 2020; 7(6):279-82.
- Footnote 337
-
International Association of National Public Health Institutes. Stockholm Statement: The Role of National Public Health Institutes in Supporting Preparedness and Response to Emergencies Affecting Population Health. International Association of National Public Health Institutes; 2022.
- Footnote 338
-
World Health Organization. Zero Draft of the WHO CA+ for the Consideration of the Intergovernmental Negotiating Body at Its Fourth Meeting - WHO Convention, Agreement or Other International Instrument on Pandemic Prevention, Preparedness and Response ("WHO CA+"). World Health Organization; 2023.
- Footnote 339
-
Pauly, B, MacDonald, M, Hancock, T, O'Briain, W, Martin, W, Allan, D, et al. Health Equity Tools 2.0. Victoria. B.C.: University of Victoria; 2016.
- Footnote 340
-
Health Canada. Health Portfolio Sex- and Gender-Based Analysis Plus Policy: Advancing Equity, Diversity and Inclusion Government of Canada; 2023.
- Footnote 341
-
Women and Gender Equality Canada. Introduction to GBA Plus. Government of Canada; 2022.
- Footnote 342
-
Public Health Agency of Canada. Toward Health Equity: A Guide to SGBA Plus in PHAC Programs and Policies 2021-22 Update. GCpedia; 2022.
- Footnote 343
-
Greaves, L, Ritz, SA. Sex, Gender and Health: Mapping the Landscape of Research and Policy. International Journal of Environmental Research and Public Health. 2022; 19(5).
- Footnote 344
-
Women and Gender Equality Canada. What Is Gender-Based Analysis Plus? In: Module 3 – What Is Gender-Based Analysis Plus (GBA Plus)? Government of Canada; 2022.
- Footnote 345
-
Women and Gender Equality Canada. What Is Gender-Based Analysis Plus. Government of Canada; 2022.
- Footnote 346
-
Women and Gender Equality Canada. Government of Canada's Approach on Gender-Based Analysis Plus. Government of Canada; 2022.
- Footnote 347
-
Women and Gender Equality Canada. Gender Based Analysis Plus (GBA Plus): Step-by-Step Guide GCpedia; 2021.
- Footnote 348
-
Native Women's Association of Canada. A Culturally Relevant Gender-Based Analysis (CRGBA) Starter Kit: Introduction, Incorporation, and Illustrations of Use. Native Women's Association of Canada; 2020.
- Footnote 349
-
Pauktuutit Inuit Women of Canada. Inuit-Specific GBA+ Framework. Pauktuutit Inuit Women of Canada; 2023.
- Footnote 350
-
Women of the Métis Nation. Métis-Specific Gender Based Analysis Plus (GBA+) Tool. Women of the Métis Nation; 2021.
- Footnote 351
-
Native Women's Association of Canada. Environment : COP27 to Water Carriers to Disaster Preparedness: Fall 2022 a Busy Time for Environment Unit. Native Women's Association of Canada; 2022.
- Footnote 352
-
Heller, J, Givens, ML, Yuen, TK, Gould, S, Jandu, MB, Bourcier, E, et al. Advancing Efforts to Achieve Health Equity: Equity Metrics for Health Impact Assessment Practice. International Journal of Environmental Research and Public Health. 2014; 11(11):11054-64.
- Footnote 353
-
Government of Ontario. Health Equity Impact Assessment (HEIA) Workbook. Government of Ontario; 2012.
- Footnote 354
-
Harris-Roxas, BF, Harris, PJ, Harris, E, Kemp, LA. A Rapid Equity Focused Health Impact Assessment of a Policy Implementation Plan: An Australian Case Study and Impact Evaluation. International Journal for Equity in Health. 2011; 10(1):6.
- Footnote 355
-
Signal, L, Martin, J, Cram, F, Robson, B. The Health Equity Assessment Tool: A User's Guide. Wellington, NZ: Ministry of Health 2008.
- Footnote 356
-
Gouvernement du Québec. Évaluation D'impact sur la Santé Lors de L'élaboration des Projets de Loi et Règlement au Québec. Gouvernement du Québec; 2006.
- Footnote 357
-
Povall, SL, Haigh, FA, Abrahams, D, Scott-Samuel, A. Health Equity Impact Assessment. Health Promotion International. 2014; 29(4):621-33.
- Footnote 358
-
National Collaborating Centre for Determinants of Health. Health Equity Frameworks as a Tool to Support Public Health Action: A Rapid Review of the Literature. Antigonish, NS: National Collaborating Centre for Determinants of Health; 2023.
- Footnote 359
-
Race Forward. Racial Equity Impact Assessment Toolkit. Race Forward; 2009.
- Footnote 360
-
Chaiton, M, Musani, I, Pullman, M, Logie, CH, Abramovich, A, Grace, D, et al. Access to Mental Health and Substance Use Resources for 2SLGBTQ+ Youth during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(21).
- Footnote 361
-
Abramovich, A, Pang, N, Moss, A. Experiences of Family Violence among 2SLGBTQ+ Youth at Risk of, and Experiencing, Homelessness before and during the COVID-19 Pandemic. Journal of Gay & Lesbian Mental Health. 2022; 26(3):265-88.
- Footnote 362
-
Turner, BJ, Robillard, CL, Ames, ME, Craig, SG. Prevalence and Correlates of Suicidal Ideation and Deliberate Self-Harm in Canadian Adolescents During the Coronavirus Disease 2019 Pandemic. The Canadian Journal of Psychiatry. 2021; 67(5):403-6.
- Footnote 363
-
Craig, SG, Ames, ME, Bondi, BC, Pepler, DJ. Canadian Adolescents' Mental Health and Substance Use during the COVID-19 Pandemic: Associations with COVID-19 Stressors. Canadian Journal of Behavioural Science / Revue canadienne des sciences du comportement. 2023; 55(1):46-55.
- Footnote 364
-
Iacono, G, Craig, SL, Pascoe, R. Critical Reflections and Reflexivity on Responding to the Needs of LGBTQ+ Youth in a Global Pandemic. Qualitative Social Work. 2021; 20(1-2):479-86.
- Footnote 365
-
Public Health Agency of Canada. Framework for Ethical Deliberation and Decision-Making in Public Health: A Tool for Public Health Practitioners, Policy Makers and Decision-Makers. Ottawa, ON: Public Health Agency of Canada; 2017.
- Footnote 366
-
MacDonald, M. Introduction to Public Health Ethics 3: Frameworks for Public Health Ethics. Montréal, Québec: National Collaborating Centre for Healthy Public Policy; 2015.
- Footnote 367
-
National Collaborating Centre for Healthy Public Policy. Repertoire – Ethics Frameworks for Public Health. National Collaborating Centre for Healthy Public Policy; 2021.
- Footnote 368
-
Public Health Agency of Canada. Public Health Ethics Framework: A Guide for Use in Response to the COVID-19 Pandemic in Canada. Government of Canada; 2022.
- Footnote 369
-
BC Centre for Disease Control. COVID-19 Ethical Decision-Making Framework. Government of British Columbia; 2020.
- Footnote 370
-
Filiatrault, F, Désy, M, Leclerc, B. Référentiel de Valeurs pour Soutenir L'analyse Éthique des Actions en Santé Publique. Gouvernement du Québec; 2015.
- Footnote 371
-
Haworth-Brockman, M, Betker, C. Measuring What Counts in the Midst of the COVID-19 Pandemic: Equity Indicators for Public Health. National Collaborating Centre for Infectious Diseases, National Collaborating Centre for Determinants of Health; 2020.
- Footnote 372
-
Haworth-Brockman, M, Betker, C, Keynan, Y. Saying It out Loud: Explicit Equity Prompts for Public Health Organization Resilience. Frontiers in Public Health. 2023; 11.
- Footnote 373
-
Global Facility for Disaster Reduction and Recovery, World Bank, Deltares. Responsible AI for Disaster Risk Management: Working Group Summary. Global Facility for Disaster Reduction and Recovery; 2021.
- Footnote 374
-
Rosenblum, AJ, Wend, CM, Akhtar, Z, Rosman, L, Freeman, JD, Barnett, DJ. Use of Big Data in Disaster Recovery: An Integrative Literature Review. Disaster Medicine and Public Health Preparedness. 2023; 17:e68.
- Footnote 375
-
Algiriyage, N, Prasanna, R, Stock, K, Doyle, EEH, Johnston, D. Multi-Source Multimodal Data and Deep Learning for Disaster Response: A Systematic Review. SN Computer Science. 2021; 3(1):92.
- Footnote 376
-
Sun, W, Bocchini, P, Davison, BD. Applications of Artificial Intelligence for Disaster Management. Natural Hazards. 2020; 103(3):2631-89.
- Footnote 377
-
Niyazi, M, Behnamian, J. Application of Emerging Digital Technologies in Disaster Relief Operations: A Systematic Review. Archives of Computational Methods in Engineering. 2023; 30(3):1579-99.
- Footnote 378
-
World Health Organization. Ethics and Governance of Artificial Intelligence for Health: WHO Guidance. World Health Organization; 2021.
- Footnote 379
-
Gevaert, CM, Carman, M, Rosman, B, Georgiadou, Y, Soden, R. Fairness and Accountability of AI in Disaster Risk Management: Opportunities and Challenges. Patterns. 2021; 2(11):100363.
- Footnote 380
-
National Collaborating Centre for Determinants of Health. Let's Talk: Moving Upstream. Antigonish, NS: National Collaborating Centre for Determinants of Health, St. Francis Xavier University; 2014.
- Footnote 381
-
Morrison, V. Policy Approaches to Reducing Health Inequalities: Social Determinants of Health and Social Determinants of Health Inequalities. Montréal, Québec: National Collaborating Centre for Healthy Public Policy; 2017.
- Footnote 382
-
Wang, L, Calzavara, A, Baral, S, Smylie, J, Chan, AK, Sander, B, et al. Differential Patterns by Area-Level Social Determinants of Health in Coronavirus Disease 2019 (COVID-19)–Related Mortality and Non–COVID-19 Mortality: A Population-Based Study of 11.8 Million People in Ontario, Canada. Clinical Infectious Diseases. 2023; 76(6):1110-20.
- Footnote 383
-
Rao, A, Ma, H, Moloney, G, Kwong, JC, Jüni, P, Sander, B, et al. A Disproportionate Epidemic: COVID-19 Cases and Deaths among Essential Workers in Toronto, Canada. Annals of Epidemiology. 2021; 63:63-7.
- Footnote 384
-
Respiratory Virus Infections Working Group. Canadian Public Health Laboratory Network Supporting Northern Remote Communities in Canada. Canada Communicable Disease Report. 2020; 46(10):322-3.
- Footnote 385
-
Government of Canada. Point-of-Care Testing Brings Rapid COVID-19 Testing to Underserved Communities. Government of Canada; 2021.
- Footnote 386
-
Myers, A, Sandstrom, P. The Northern, Remote and Isolated Indigenous Communities Initiative: Community-Based Testing from COVID-19 to HIV and STBBI. CATIE Blog; 2023.
- Footnote 387
-
Rapid Evidence Profile #46. McMaster Forum; 2023.
- Footnote 388
-
Expert Panel on the Socioeconomic Impacts of Science and Health Misinformation. Fault Lines. Ottawa, ON: Council of Canadian Academies; 2023.
- Footnote 389
-
National Collaborating Centre for Methods and Tools. Rapid Review: What Is Known About Reasons for Vaccine Confidence and Uptake in Populations Experiencing Inequities? : National Collaborating Centre for Methods and Tools; 2021.
- Footnote 390
-
Greenwood, M, Atkinson, D, Sutherland, J. Supporting Health Equity for First Nations, Inuit and Métis Peoples. Canada Communicable Disease Report. 2022; 48(4):119-23.
- Footnote 391
-
Oksanen, A, Kaakinen, M, Latikka, R, Savolainen, I, Savela, N, Koivula, A. Regulation and Trust: 3-Month Follow-up Study on COVID-19 Mortality in 25 European Countries. JMIR Public Health Surveill. 2020; 6(2):e19218.
- Footnote 392
-
Chang, D, Chang, X, He, Y, Tan, KJK. The Determinants of COVID-19 Morbidity and Mortality across Countries. Scientific Reports. 2022; 12(1):5888.
- Footnote 393
-
National Collaborating Centre for Methods and Tools. Rapid Review: What Were the Public's Experiences Accessing and Interacting with Public Health Information during the COVID-19 Pandemic? : National Collaborating Centre for Methods and Tools; 2023.
- Footnote 394
-
National Collaborating Centre for Methods and Tools. Rapid Review Update 2: What Are Best Practices for Risk Communication and Strategies to Mitigate Risk Behaviours? : National Collaborating Centre for Methods and Tools; 2023.
- Footnote 395
-
Public Health Ontario. Evidence Brief: Risk Communication and Trust in Public Health during the COVID-19 Pandemic. Toronto, ON: Public Health Ontario; 2023.
- Footnote 396
-
Centre intégré de santé et de services sociaux de Laval. La Brigade Sensibilisation Laval. 2022. Available from: https://www.youtube.com/watch?v=2SRetQhSVRM.
- Footnote 397
-
Centre intégré de santé et de services sociaux de Laval. Réseaux des Éclaireurs en Santé Psychologique : Présentation de la Brigade Sensibilisation Laval. Gouvernement du Québec; 2023.
- Footnote 398
-
Centre intégré de santé et de services sociaux de Laval. La Brigade Sensibilisation Laval Continuera de Sillonner la Région de Laval Afin D'améliorer la Santé Psychologique et le Bien-Être de la Population Gouvernement du Québec; 2022.
- Footnote 399
-
Government of Manitoba. COVID-19 Infections in Manitoba: Race, Ethnicity, and Indigeneity. Government of Manitoba; 2021.
- Footnote 400
-
World Health Organization. WHO Guidance on Research Methods for Health Emergency and Disaster Risk Management. Geneva: World Health Organization; 2021.
- Footnote 401
-
First Nations Information Governance Centre. The First Nations Principles of OCAP®. First Nations Information Governance Centre; 2021. Available from: https://fnigc.ca/ocap-training/.
- Footnote 402
-
Rotondi, MA, O'Campo, P, O'Brien, K, Firestone, M, Wolfe, SH, Bourgeois, C, et al. Our Health Counts Toronto: Using Respondent-Driven Sampling to Unmask Census Undercounts of an Urban Indigenous Population in Toronto, Canada. BMJ Open. 2017; 7(12):e018936.
- Footnote 403
-
Canadian Institute for Health Information. Race-Based and Indigenous Identity Data Collection and Health Reporting in Canada: Supplementary Report. Ottawa, ON: Canadian Institute for Health Information; 2022.
- Footnote 404
-
Guay, M, Maquiling, A, Chen, R, Lavergne, V, Baysac, D-J, Kokaua, J, et al. Sociodemographic Disparities in COVID-19 Vaccine Uptake and Vaccination Intent in Canada. Statistics Canada; 2022.
- Footnote 405
-
National Collaborating Centre for Healthy Public Policy. Public Policy Analysis Tool for Rapid Decision Making in Public Health. National Collaborating Centre for Healthy Public Policy; 2022.
- Footnote 406
-
Government of Ontario. Section 1: Introduction — the Who, What, When, Where, Why and How of IMS. In: Incident Management System (IMS) Guidance: Version 2. Government of Ontario; 2022.
- Footnote 407
-
Goralnick, E, Serino, R, Clark, CR. Equity and Disasters: Reframing Incident Command Systems. American Journal of Public Health. 2021; 111(5):844-8.
- Footnote 408
-
Myint, P, Hawes, E, Ellis, G, Boman-Davis, M, Montgomery, G. Embedding Equity in a Local Government's Response to COVID-19. Journal of Public Health Management and Practice. 2022; 28(Supplement 1).
- Footnote 409
-
Public Health Alliance of Southern California, Bay Area Regional Health Inequities Initiative. Embedding Equity into Emergency Operations: Strategies for Local Health Departments During COVID-19 & Beyond. Public Health Alliance of Southern California; 2020.
- Footnote 410
-
Public Health Seattle & King County. ESF 8 Plan Response Annex: Equity Response Annex. Public Health Alliance of Southern California; 2019.
- Footnote 411
-
Belita, E, Neil-Sztramko, SE, Miller, A, Anderson, LN, Apatu, E, Bellefleur, O, et al. A Scoping Review of Strategies to Support Public Health Recovery in the Transition to a "New Normal" in the Age of COVID-19. BMC Public Health. 2022; 22(1):1244.
- Footnote 412
-
Finucane, ML, Acosta, J, Wicker, A, Whipkey, K. Short-Term Solutions to a Long-Term Challenge: Rethinking Disaster Recovery Planning to Reduce Vulnerabilities and Inequities. International Journal of Environmental Research and Public Health. 2020; 17(2).
- Footnote 413
-
Canadian Women's Foundation, Canadian Centre for Policy Alternatives, Ontario Nonprofit Network, Fay Faraday. Resetting Normal: Women, Decent Work and Canada's Fractured Care Economy. Canadian Women's Foundation; 2020.
- Footnote 414
-
Estabrooks, CA, Straus, S, Flood, CM, Keefe, J, Armstrong, P, Donner, G, et al. Restoring Trust: COVID-19 and The Future of Long-Term Care. Royal Society of Canada; 2020.
- Footnote 415
-
Fernandez, A, Black, J, Jones, M, Wilson, L, Salvador-Carulla, L, Astell-Burt, T, et al. Flooding and Mental Health: A Systematic Mapping Review. PLOS ONE. 2015; 10(4):e0119929.
- Footnote 416
-
Malagón, T, Yong, JHE, Tope, P, Miller Jr, WH, Franco, EL, McGill Task Force on the Impact of COVID-19 on Cancer Control Care. Predicted Long-Term Impact of COVID-19 Pandemic-Related Care Delays on Cancer Mortality in Canada. International Journal of Cancer. 2022; 150(8):1244-54.
- Footnote 417
-
Eskander, A, Li, Q, Hallet, J, Coburn, N, Hanna, TP, Irish, J, et al. Access to Cancer Surgery in a Universal Health Care System During the COVID-19 Pandemic. JAMA Network Open. 2021; 4(3):e211104-e.
- Footnote 418
-
Robson, J, Tedds, L, Akin, L, Baiden, D, Brayton, B, Brooks, K, et al. Impacts of the COVID-19 Pandemic on Women in Canada. Royal Society of Canada; 2022.
- Footnote 419
-
The Standing Committee on the Status of Women. Impacts of the COVID-19 Pandemic on Women. House of Commons Canada; 2021.
- Footnote 420
-
Hayes, K, Poland, B, Cole, DC, Agic, B. Psychosocial Adaptation to Climate Change in High River, Alberta: Implications for Policy and Practice. Canadian Journal of Public Health. 2020; 111(6):880-9.
- Footnote 421
-
Généreux, M, Roy, M, O'Sullivan, T, Maltais, D. A Salutogenic Approach to Disaster Recovery: The Case of the Lac-Mégantic Rail Disaster. International Journal of Environmental Research and Public Health. 2020; 17(5).
- Footnote 422
-
Imperiale, AJ, Vanclay, F. Conceptualizing Community Resilience and the Social Dimensions of Risk to Overcome Barriers to Disaster Risk Reduction and Sustainable Development. Sustainable Development. 2021; 29(5):891-905.
- Footnote 423
-
Hoogeveen, D, Klein, K. Social Impacts of the 2018 Grand Forks Flood: A Gender Based Plus Analysis of Climate Risk. Government of British Columbia; 2021.
- Footnote 424
-
Mottershead, KD, McGee, TK, Christianson, A. Evacuating a First Nation Due to Wildfire Smoke: The Case of Dene Tha' First Nation. International Journal of Disaster Risk Science. 2020; 11(3):274-86.
- Footnote 425
-
Généreux, M. Des Initiatives Prometteuses Pour Mobiliser La Communauté Locale En Contexte De Rétablissement. Centre intégré universitaire de santé et de services sociaux de l'Estrie – Centre hospitalier universitaire de Sherbrooke; 2021.
- Footnote 426
-
Public Health Ontario. Rapid Review: Best Practices for Conducting in- and after Action Reviews as Part of Public Health Emergency Management. Public Health Ontario; 2022.
- Footnote 427
-
Public Safety Canada. Gender-Based Analysis Plus. Government of Canada; 2023.
- Footnote 428
-
World Health Organization. A Global Analysis of COVID-19 Intra-Action Reviews: Reflecting on, Adjusting and Improving Country Emergency Preparedness and Response during a Pandemic. World Health Organization; 2022.
- Footnote 429
-
Public Health Ontario. Public Health Emergency Preparedness Framework and Indicators: A Workbook to Support Public Health Practice Public Health Ontario; 2020.
- Footnote 430
-
Public Health Agency of Canada. Trauma and Violence-Informed Approaches to Policy and Practice. Government of Canada; 2018.
- Footnote 431
-
International Federation of the Red Cross and Red Crescent Societies. Enhanced Vulnerability and Capacity Assessment (EVCA). International Federation of the Red Cross and Red Crescent Societies; 2018.
- Footnote 432
-
Ghebreyesus, TA. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. World Health Organization; 2020.
- Footnote 433
-
Ghebreyesus, TA. WHO Director-General's Opening Remarks at the Media Briefing – 5 May 2023. World Health Organization; 2023.
- Footnote 434
-
Tam, T. Remarks from the Chief Public Health Officer, March 10, 2023. Public Health Agency of Canada; 2023.
- Footnote 435
-
Office of the Chief Science Advisor of Canada. Post-COVID-19 Condition in Canada: What We Know, What We Don't Know, and a Framework for Action. Government of Canada; 2022.
- Footnote 436
-
Government of Canada. COVID-19 Wastewater Surveillance Dashboard. Government of Canada; 2023.
- Footnote 437
-
Government of Canada. COVID-19 Epidemiology Update: Summary. Government of Canada; 2023.
- Footnote 438
-
Government of Canada. Community-Led Wastewater Testing in Northern, Remote and Isolated Communities. Government of Canada; 2023.
- Footnote 439
-
Ogden, NH, Turgeon, P, Fazil, A, Clark, J, Gabriele-Rivet, V, Tam, T, et al. Counterfactuals of Effects of Vaccination and Public Health Measures on COVID-19 Cases in Canada: What Could Have Happened? Canada Communicable Disease Report. 2022; 48(7/8):292–302.
- Footnote 440
-
Public Health Agency of Canada. Respiratory Virus Report, Week 31 - Ending August 5, 2023. Government of Canada; 2023.
- Footnote 441
-
Tam, T. Remarks from the Chief Public Health Officer, December 14, 2022. Public Health Agency of Canada; 2022.
- Footnote 442
-
Hamilton Health Sciences. Update: Pressures Continue at MCH. Hamilton Health Sciences; 2022.
- Footnote 443
-
DeLaire, M. 'We Are So Overwhelmed': Children's Hospitals across Canada Stretched as RSV Cases, Flu-Like Illnesses Spike. CTV News; 2022.
- Footnote 444
-
Public Health Agency of Canada. Respiratory Virus Report, Week 43 - Ending October 29, 2022. Government of Canada; 2022.
- Footnote 445
-
CBC News. B.C. Children's Hospital Activates Emergency Overflow Amid Respiratory Illness Surge. CBC News; 2022.
- Footnote 446
-
Lee, J. Staff Redeployment Possible as Alberta Children's Hospital Struggles with Wave of Sick Kids. CBC News; 2022.
- Footnote 447
-
Patil, A. Iwk Chief Paints Concerning Picture of Children in Intensive Care Units. CBC News; 2022.
- Footnote 448
-
Government of Canada. About COVID-19 Vaccination and Approved Vaccines. In: COVID-19 Vaccination: Vaccination Coverage. Government of Canada; 2023.
- Footnote 449
-
Canadian Blood Services. COVID-19 Seroprevalence Report - Report #35: June 2023 Survey. Canadian Blood Services; 2023. Available from: https://www.covid19immunitytaskforce.ca/wp-content/uploads/2023/08/covid-19-full-report-june-2023.pdf.
- Footnote 450
-
Public Health Agency of Canada. Guidance on the Use of COVID-19 Vaccines in the Fall of 2023. Public Health Agency of Canada; 2023.
- Footnote 451
-
Kwan, AC, Ebinger, JE, Botting, P, Navarrette, J, Claggett, B, Cheng, S. Association of COVID-19 Vaccination with Risk for Incident Diabetes after COVID-19 Infection. JAMA Network Open. 2023; 6(2):e2255965-e.
- Footnote 452
-
Barrett, CE, Koyama, AK, Alvarez, P, Chow, W, Lundeen, EA, Perrine, CG, et al. Risk for Newly Diagnosed Diabetes >30 Days after SARS-CoV-2 Infection among Persons Aged <18 Years — United States, March 1, 2020–June 28, 2021. Morbidity and Mortality Weekly Report. 2022; 71(2):59-65.
- Footnote 453
-
Xie, Y, Xu, E, Bowe, B, Al-Aly, Z. Long-Term Cardiovascular Outcomes of COVID-19. Nature Medicine. 2022; 28(3):583-90.
- Footnote 454
-
Government of Canada. COVID-19: Longer-Term Symptoms among Canadian Adults - Second Report. Government of Canada; 2023.
- Footnote 455
-
Quinn, KL, Katz, GM, Bobos, P, Sander, B, McNaughton, CD, Cheung, AM, et al. Understanding the Post COVID-19 Condition (Long COVID) in Adults and the Expected Burden for Ontario. Ontario COVID-19 Science Advisory Table; 2022.
- Footnote 456
-
Statistics Canada. Table 13-10-0867-01 Long Term COVID-19 Symptoms among Canadian Adults Who Self-Reported a Prior Positive Test or Suspected SARS-CoV-2 Infection, by Sex and Age Group. Statistics Canada; 2023. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310086701.
- Footnote 457
-
Sanford, S, Roche, B. The Healthcare Experiences of People with Long COVID in the GTA. Wellesley Institute; 2023.
- Footnote 458
-
Public Health Agency of Canada. Government of Canada Welcomes Task Force Report on Post COVID-19 Condition. Government of Canada; 2022.
- Footnote 459
-
Public Health Agency of Canada. Government of Canada to Remove COVID-19 Border and Travel Measures Effective October 1. Government of Canada; 2022.
- Footnote 460
-
Duclos, J-Y. Statement from the Minister of Health on Update to COVID-19 Border Measures for Travellers Arriving from the People's Republic of China, Hong Kong or Macao. Public Health Agency of Canada; 2023.
- Footnote 461
-
Public Health Agency of Canada. Government of Canada Will Remove COVID-19 Testing Requirement for Air Travellers Arriving from the People's Republic of China, Hong Kong or Macao. Government of Canada; 2023.
- Footnote 462
-
Public Health Agency of Canada. Guidance for Marine Operators: Reporting Illness on Board. Government of Canada; 2023.
- Footnote 463
-
McMillan, G, Presseau, J. Health Promotion Approaches to the COVID-19 Pandemic Preparedness and Response: A Behavioural Science Lens. McMaster Forum; 2023.