Archived: Rapid risk assessment: Measles in Canada, public health implications in 2024
Download in PDF format
(732 KB, 28 pages)
Organization: Public Health Agency of Canada
Date published: 2024-03-27
Assessment completed: March 20, 2024 (with data as of March 15, 2024)
On this page
- Reason for the assessment
- Risk questions
- Risk statement
- Risk assessment summary
- Technical annex
- Event background
- Methods
- Definitions
- Key assumptions
- Detailed risk assessment summary
- Appendix A: Methods
- Appendix B: Estimation of the effective reproduction number (Re) for measles
- Appendix C: Mathematical models of expected outbreak sizes under different scenarios
- Appendix D: Acknowledgements
- Footnotes
- References
Reason for the assessment
Increased measles activity in Canada, reports of global increase of measles cases, and sub-optimal measles vaccine coverage in Canada.
Risk questions
What is the likelihood and impact of multiple outbreaks in specific communities/settings in the next 6 weeks?
What is the likelihood and impact of prolonged community transmission of measles in Canada in the next 3 months?
Risk statement
There is a high likelihood of infectious travellers with measles virus continuing to enter Canada and a high likelihood of multiple measles outbreaksFootnote a within the next 6 weeks in Canadian educationalFootnote b and healthcare settings as well as in un/under-vaccinated communities. The likelihood of outbreaks is very low in long-term care facilities.
The impact on infected individuals is expected to be minor for vaccinated individuals, moderate for unvaccinated individuals including children, and moderate to major for vulnerable individuals, including infants, immunocompromised individuals, and unvaccinated pregnant individuals. The population impact of these outbreaks is expected to range from minor to major, depending on the number and size of outbreaks, vaccine coverage, pre-existing immunity, effectiveness of control measures, and the number of people affected in groups at higher risk of severe outcomes. Specifically, moderate impacts are expected in educational settings including child-care and pre-school; while major impacts are expected in health care settings, especially in pediatric facilities, as well as in un/under-vaccinated communities, the latter due to expected issues in implementing effective interventions.
The likelihood and impact of prolonged community transmissionFootnote c in the general population in Canada in the next 3 months are both moderate. Recent declines in vaccination coverage in Canada suggest that measles susceptibility could be increasing, particularly among school-aged children. Although outbreaks outside of the specific settings outlined above could cause additional demand on public health resources and healthcare facilities, they are expected to be limited in size and in the number of generations of transmission given the high levels of vaccination and pre-existing immunity to measles in Canada overall.
Uncertainty in these estimates ranges from low (for likelihood of importation and outbreaks, as well as impact on individuals) to moderate (for impact of outbreaks and prolonged transmission). The sources of uncertainty for impact of outbreaks and prolonged transmission include limitations in available vaccination coverage and serological data, lack of detailed information on measles susceptibility in different parts of Canada, and the inherent unpredictability in the number, size and geographic distribution of outbreaks, including super-spreading events.
Risk assessment summary
| Estimate | Risk sub-question | |||
|---|---|---|---|---|
| Infectious travellers into Canada in the next 6 weeks | ||||
| Likelihood (Uncertainty) | High (Low) | |||
| Individual impact | ||||
| Impact (Uncertainty) | Vaccinated individuals: Minor (Low) |
Unvaccinated individuals (≥5 years): Moderate (Low) |
Unvaccinated children (1 to <5 years of age): Moderate (Low) |
Vulnerable individualsTable 1 Footnote a: Moderate to Major (Low) |
| Multiple outbreaks in specific settings/populations in the next 6 weeks | ||||
| Likelihood (Uncertainty) | Educational settingsTable 1 Footnote b: High (Low) |
Healthcare facilities: High (Moderate) |
Long-term care facilitiesTable 1 Footnote c: Very low (Low) |
Un/under-vaccinated communities: High (Low) |
| Impact (Uncertainty) | Educational settingsTable 1 Footnote b: Moderate (Moderate) |
Healthcare facilities: Major (Moderate) |
Long-term care facilitiesTable 1 Footnote c: Minor (Moderate) |
Un/under-vaccinated communities: Major (Moderate) |
| Prolonged transmission in broader Canadian population in the next 3 months | ||||
| Likelihood (Uncertainty) | Moderate (Low) | |||
| Impact (Uncertainty) | Moderate (Moderate) | |||
Notes: See Appendix A for definitions of likelihood and impact.
|
||||
Importation
There is a high likelihood of continued measles importation into Canada over the next 6 weeks, with low uncertainty given the ongoing increases in measles activity globally and the high volumes of travel expected during this time period.
Impact on individuals
The impact of measles infection on vaccinated individuals is expected to be minor, given the high efficacy of measles vaccine. The impact of measles infection on unvaccinated individuals, including unvaccinated children aged 1 to 5, is expected to be moderate, due to the higher risk of hospitalization, common complications such as otitis media and diarrhea and rare severe outcomes, including respiratory and neurological complications. The impact of measles infection on other vulnerable groups (unvaccinated pregnant individuals, immunocompromised individuals, and infants) is moderate to major, driven by the higher risk of severe illness, adverse birth outcomes, and death. There is low uncertainty in these estimates given the volume of evidence on clinical outcomes of measles.
Outbreaks in specific settings
There is a high likelihood of multiple measles outbreaksFootnote d within the next 6 weeks in three of the specific settings considered (educational and healthcare settings and un/under-vaccinated communities), and very low in others (long-term care facilities).
Initial modelling of outbreak sizes conducted by researchers at Simon Fraser University (SFU) (see Appendix C) suggests that in communities of ~1,000 individuals (e.g., secondary schools, or elementary schools and immediate contacts) with high vaccination coverage (≥90%), if measles outbreaks occur, they would be unlikely to exceed 50 cases with timely interventions, including prompt case finding, isolation and post-exposure prophylaxis. However, it is thought that vaccination coverage in many educational settings in Canada is lower than 90%. The lower the vaccination coverage, the more likely an introduced case would be to set off an outbreak, and the larger an outbreak would be (possibly > 100 cases in a setting with 1,000 individuals in which vaccination coverage is ≤ 80%). In larger communities of ~8,000 individuals, outbreaks could effectively be curtailed with timely interventions, as long as vaccination coverage or pre-existing immunity is above 75%. However, in communities of ~8,000 individuals in which vaccination coverage or pre-existing immunity is less than 75%, protracted outbreaks with hundreds of cases could occur even with timely interventions. It should be noted that public health interventions are challenging to incorporate into mathematical models and that results are highly dependent on individuals' acceptance of and capacity to adhere to control measures, such as isolation and post-exposure prophylaxis.
The impact in educational settings (including childcare settings) is assessed as moderate, due to extensive social mixing and high transmission potential in these settings, the higher frequency of severe outcomes, particularly in un/under-vaccinated children <5 years, and the potential impact of public health measures (e.g., exclusion of cases from educational settings) on children and caregivers.
In healthcare settings, the impact is expected to be major, due to the potential for exposure of vulnerable patients (e.g., immunocompromised individuals, unvaccinated pregnant individuals, infants) and the additional pressures imposed by outbreaks (including case isolation, contact tracing, diagnostics, infection prevention and control) on already limited healthcare resources.
The impact in long-term care facilities is expected to be minor, as measles susceptibility among older adults is expected to be very low due to pre-existing immunity. Uncertainty in this estimate is moderate; evidence indicates that immunity from natural infection is likely to be life-long, but there remains some uncertainty regarding the possibility of waning of immunity in post-elimination settings.
The impact of multiple outbreaks in un/under-vaccinated communities is expected to be major, driven by the higher incidence expected, the severity of measles in unvaccinated individuals, particularly young children and other vulnerable groups (e.g., immunocompromised individuals, unvaccinated pregnant individuals), the increased demand on public health and healthcare resources in potentially lower-resourced areas, and the expectation that intervention measures may not be as timely and/or accepted, lowering their effectiveness.
There is a moderate level of uncertainty in most impact estimates due to variations in outbreak sizes, which are dependent on context, the timeliness of interventions and public willingness and ability to adhere to interventions such as self-isolation and post-exposure prophylaxis, and the possibility of super-spreading events.
Prolonged transmission
The likelihood of prolonged community transmission in the general population in Canada in the next 3 months is moderate. A longer (i.e., 3 month) time period was chosen to assess this likelihood, as the timeframe for community transmission with several generations to occur is expected to be potentially longer than 6 weeks. Recent declines in vaccination coverage (from 87% in 2017 to 79% in 2021 for 2-dose measles-containing vaccine coverage by the age of 7 years) indicate that measles susceptibility is likely to be increasing, particularly among school-aged children. Higher volumes of travel, together with social gatherings during educational and religious holidays during March and April increase the likelihood of measles importation and subsequent transmission within Canada. The impact of prolonged community transmission in the general population is expected to be moderate; outbreaks outside of specific high-risk populations/settings would cause additional demand on public health and healthcare facilities in affected areas but are expected to be restricted in size and limited to a small number of generations of transmission due to the generally high levels of vaccination and pre-existing immunity to measles. There is moderate uncertainty in this estimate, due to limitations in the available vaccination coverage and serological data, the lack of detailed information on measles susceptibility in different parts of Canada, and the inherent unpredictability in the number, size and geographic distribution of outbreaks, including the possibility of super-spreading events resulting in large outbreaks.
Future risk in Canada
The incidence of measles globally, and the number of countries experiencing measles outbreaks, are expected to rise until vaccination gaps worldwide can be addressed. Increased numbers of measles importations into Canada are expected in the medium to long term, increasing opportunities for localized outbreaks. Extensive transmission in the general population is not anticipated due to generally high levels of vaccination and pre-existing immunity in Canada. However, outbreaks in specific higher risk settings such as educational settings, healthcare settings, or un/under-vaccinated communities are likely to occur. These outbreaks could be more complex and challenging to control especially in areas with lower population immunity to measles and higher demands on public health resources.
The worst-case scenario for future measles risk in Canada would be the occurrence of a chain of measles virus transmission in the general population that is sustained for 12 months or longer. This scenario could result in substantial health and socioeconomic burden and would result in the loss of Canada's measles elimination status. The occurrence of multiple outbreaks in different settings increases the risk for spillover into the wider population, particularly in areas with lower vaccination coverage. Such spillover events have been occasionally documented in settings with lower vaccination coverage; the largest outbreak in the past 20 years, in Québec in 2011, involved >650 cases and lasted 26 weeks, with transmission occurring in schools and daycare centres, healthcare facilities and the wider community. However, measles outbreaks in Canada have typically been contained with prompt control measures suggesting that the worst-case scenario is less likely.
The most plausible scenario over the next 12 months is multiple outbreaks in settings with low vaccine coverage. The global increase in measles incidence and suboptimal vaccination coverage, with resulting pockets of susceptibility within the Canadian population, increases the probability for outbreaks within Canada. Measles is highly transmissible with up to 100% secondary attack rates in susceptible populations. Given that individuals born prior to 1970 are likely to be immune from past infection with measles, outbreaks are likely to impact children and adults under the age of 55 years who have not received two doses of measles vaccine.
This scenario is driven by factors such as ongoing risk posed by case importations, vaccine hesitancy, as well as the ability to interrupt transmission to the wider community through prompt case identification, effective case and contact management, and increased vaccination coverage. However, the timeliness of case and contact management may be complicated by the potential for the virus to be transmitted prior to the appearance of the characteristic rash. In addition, measles outbreaks have been documented in settings with high vaccination coverage, involving cases among fully vaccinated individuals, who may present with atypical measles, and high levels of social contact, indicating that under some outbreak conditions, breakthrough infections may play a role in susceptibility and transmission.
The occurrence of measles outbreaks also has health equity implications, given that outbreaks could be more likely and have greater impact in communities experiencing both barriers to high vaccination coverage and delayed access to diagnosis and treatment due to social, economic and/or geographic factors. Continued efforts to reverse recent declines in vaccination coverage, increase public confidence in vaccines and reduce barriers to vaccination across Canada will be crucial to reducing future risk of measles as well as other vaccine-preventable diseases.
Proposed actions for public health authorities
Measles is a highly vaccine preventable disease; however, due to increases in measles activity internationally together with recent declines in overall vaccine coverage, it is important that the public health response be proportionate to the risk. A multipronged approach addressing public health intervention (e.g., targeted vaccination), enhanced surveillance, targeted educational and awareness campaigns for the affected settings and communities/population at risk, and standardized guidance for health professionals (e.g., early detection and management of measles cases and contacts) would be beneficial to prevent multiple outbreaks and community transmission.
Recommendations provided below are based on findings of this risk assessment. These are for consideration by jurisdictions according to their local epidemiology, policies, resources, and priorities. It is recommended to prepare for outbreaks and broader transmission into the general population, including among vulnerable individuals.
Public health interventions: prevention and response
Continue routine measles immunization while considering vaccination campaigns targeting at-risk settings and populations. In addition, explore mechanisms to reach un/under vaccinated communities at risk including vaccine hesitant communities.
Prepare to manage an increased volume of cases and contacts, e.g., ability to adequately isolate, laboratory testing capacity, supply and availability of vaccines and immunoglobulins. Consider updating and making available appropriate guidance pertaining to prevention and control of measles outbreaks, including guidance related to occupational health.
Collaboration and coordination
Continue to collaborate and coordinate with partners (including community and indigenous partners, and other levels of government) at all stages of preparedness, planning and response.
Surveillance and reporting
Continue to collect, collate, analyse and share measles data and summarise emerging evidence to inform the local, provincial/territorial and federal public health response.
Continue to monitor and assess local measles vaccination coverage to identify areas with higher susceptibility to measles outbreaks.
Risk communication
Consider facilitating the development of targeted educational and awareness messaging for populations at increased risk through the identification of approaches (e.g., using behavioural sciences, supporting community-led solutions etc.) while continuing with broad communication to Canadians on the current measles situation. When necessary, correct and counter mis- or disinformation.
Consider further awareness and education of health professionals on early detection and management of measles cases by sharing associated guidance including assessment, vaccination, infection prevention and control as well as post exposure prophylaxis. Additionally, continue to raise awareness among their patients, especially those intending to travel, about the importance of having their measles vaccination up to date.
Technical annex
Event background
Recent declines in measles vaccination coverage, augmented by disruptions to vaccination programs during the COVID-19 pandemic, as well as anti-vaccine sentiment driven by vaccine mis- and disinformation, have resulted in a global rise in measles. In 2023, 58,114 measles cases were reported from the World Health Organization (WHO) European Region compared with 904 in 2022, representing a 64-fold rise in incidenceFootnote 1Footnote 2. Globally, there was a 64% increase in measles incidence in 2023 compared to 2022, representing >280,000 cases from 169 Member StatesFootnote 3Footnote 4.
Canada has been considered free of endemic measles since 1998. Since 2015, fewer than 436 cases have been recorded, with half of these occurring in 2015. The majority of these cases are linked to measles importations from countries with measles activityFootnote 5; <5% are sporadic cases with an unknown source of exposure. Children aged 5-14 years account for a third of the cases, and 75% of all cases with known vaccination status occur in unvaccinated individuals. Historically, peak incidence occurs in the winter and spring months, with approximately 40% of cases occurring in March.
Figure 1. Exposure source of measles cases in Canada and global case counts, 2015-March 2024

Figure 1: Text description
| Year | Exposed outside of Canada (imported) |
Exposed in Canada linked to a case/chain |
Unknown source/exposure (sporadic) |
Global cases |
|---|---|---|---|---|
| 2015 | 9 (5%) | 185 (94%) | 2 (1%) | 214,808 |
| 2016 | 10 (91%) | 0 (0%) | 1 (9%) | 132,490 |
| 2017 | 9 (20%) | 35 (78%) | 1 (2%) | 173,457 |
| 2018 | 17 (59%) | 9 (31%) | 3 (10%) | 360,296 |
| 2019 | 42 (37%) | 63 (56%) | 8 (7%) | 873,022 |
| 2020 | 1 (100%) | 0 (0%) | 0 (0%) | 159,073 |
| 2021 | 0 (N/A) | 0 (N/A) | 0 (N/A) | 123,171 |
| 2022 | 3 (100%) | 0 (0%) | 0 (0%) | 205,181 |
| 2023 | 10 (83%) | 1 (8%) | 1 (8%) | 306,291 |
| 2024 | 10 (36%) | 11 (39%) | 7 (25%) | N/A |
As of March 15, 2024, a total of 29 cases have been reported in Canada, with 21 reported since February 28. Cases were reported in 4 jurisdictions. Of these 29 cases, 10 were likely exposed outside of Canada, while the remaining 19 were exposed in Canada to either another case, a common exposure, or an unknown source; 6 (21%) cases were aged <1 year. Vaccination status was known for 22 of these 29 cases, of which 72% were unvaccinated.
Canada's vaccination uptake is below the target of 95% coverage with two doses of measles-containing vaccine recommended for measles elimination. One-dose coverage has remained stable in recent years (based on data from 2021), with approximately 90% of children vaccinated by their second birthday, while 2-dose coverage by the age of 7 years declined from 87% in 2017 to 79% in 2021Footnote 6. Vaccination coverage varies greatly across Canada, with areas of robust coverage, and small communities with very low coverage that could be vulnerable if a case were to occur in these areas. Rising measles incidence internationally, particularly in countries with strong travel links to Canada, together with recent declines in vaccination coverage and pockets of susceptibility within the Canadian population, increases the risk of measles importations and the possibility for outbreaks within Canada.
Methods
This assessment was led by the Public Health Agency of Canada (PHAC) during March 1-18, 2024, in collaboration with subject matter experts in measles, mathematical modelling and risk assessment (see Appendix D for a list of contributors).
The rapid risk assessment (RRA) methodology has been adapted from the Joint Risk Assessment Operational Tool (JRA OT) to assess the risk posed by zoonotic disease hazardsFootnote 7 developed jointly by the World Health Organization (WHO), Food and Agriculture Organization of the United Nations (FAO), and the World Organization for Animal Health (WOAH). PHAC adapted the JRA OT by modifying the likelihood and impact scales and associated definitions to incorporate elements from other RRA frameworks that are relevant to the Canadian contextFootnote 8Footnote 9. A more detailed description of the methods is provided in Appendix A. Additionally, the results from a number of quantitative analyses have been incorporated into this assessment to support the impact estimates, including an estimation of the overall reproduction number for measles in Canada (Appendix B), and mathematical modelling simulations of expected outbreak sizes under different scenarios from two compartmental models, developed by the Public Health Risk Sciences Division at PHAC and the Department of Mathematics at Simon Fraser University (Appendix C).
Definitions
- Nationally, vaccination coverage is reported according to the number of doses of measles vaccine received by the age of 2 and 7 years:
- One-dose (MCV1) coverage refers to the percentage of children who have received at least one dose of measles-containing vaccine by their second birthday.
- Two-dose (MCV2) coverage refers to the percentage of children who have received at least two doses of measles-containing vaccine by their seventh birthday.
- Vaccinated refers to individuals who have received one or more doses of a measles-containing vaccine.
- Unvaccinated refers to individuals who have received zero doses of a measles-containing vaccine.
- Un/under-vaccinated communities: In the context of this RRA, un/under-vaccinated communities refer to communities historically known to have lower vaccination coverage than the general population. This may include remote or isolated communities, communities that experience barriers to vaccine access, and communities that do not accept vaccination for ideological or religious reasons.
- Vaccine failure: Primary vaccine failure refers to the absence of a measurable humoral immune response following vaccination. Secondary vaccine failure refers to a sub-optimal or non-protective response to vaccination or the loss of vaccine-induced immunity over timeFootnote 10Footnote 11.
- An outbreak of measles refers to two or more confirmed cases linked, either epidemiologically or virologically or bothFootnote 5.
- Prolonged community transmission: In the context of this RRA, prolonged community transmission refers to spread in the general population extending more than two generations of transmission. In low-incidence elimination settings such as Canada, measles importations occasionally result in some transmission among the general population (outside of specific high-risk settings such as educational institutions or un/under-vaccinated groups), but this is typically limited to a small number of cases due to generally high levels of naturally-acquired or vaccine-induced immunity in the population.
- Educational settings: In the context of this RRA, educational settings include child-care, pre-school, elementary, secondary, and post-secondary settings.
- Healthcare facilities: These include hospitals and ambulatory care settings.
- Long-term care facilities: Residential or congregate living facilities for elderly populations (including retirement homes and elder lodges).
- Vulnerable individuals: For the purposes of this RRA, vulnerable groups refer to individuals at particularly high risk of severe complications from measles infection, including infants, immunocompromised individuals, as well as unvaccinated pregnant individuals due to the risk of adverse birth outcomes.
Key assumptions
- Context assumptions:
- Global measles activity, and the number of countries reporting measles outbreaks, is expected to rise in the coming months.
- Individuals born in Canada before 1970 have immunity from natural infection in childhoodFootnote 12.
- Mitigating/control measures and standard practices are assumed to be in place for the purpose of estimating most likely spread scenarios and resulting impact:
- Canada has a robust system for measles surveillance, case detection and follow-up; in the past 10 years >95% of measles cases have been linked to a known exposure source.
- Pathway assumptions:
- Importation of measles into Canada and exposure to measles within Canada is already occurring and expected to continue over the timeframe of the assessment – these risk pathway steps are not specifically considered because the likelihood is considered to be high.
Detailed risk assessment results
Risk pathway
Figure 2. Risk pathway and sub-questions for measles in Canada
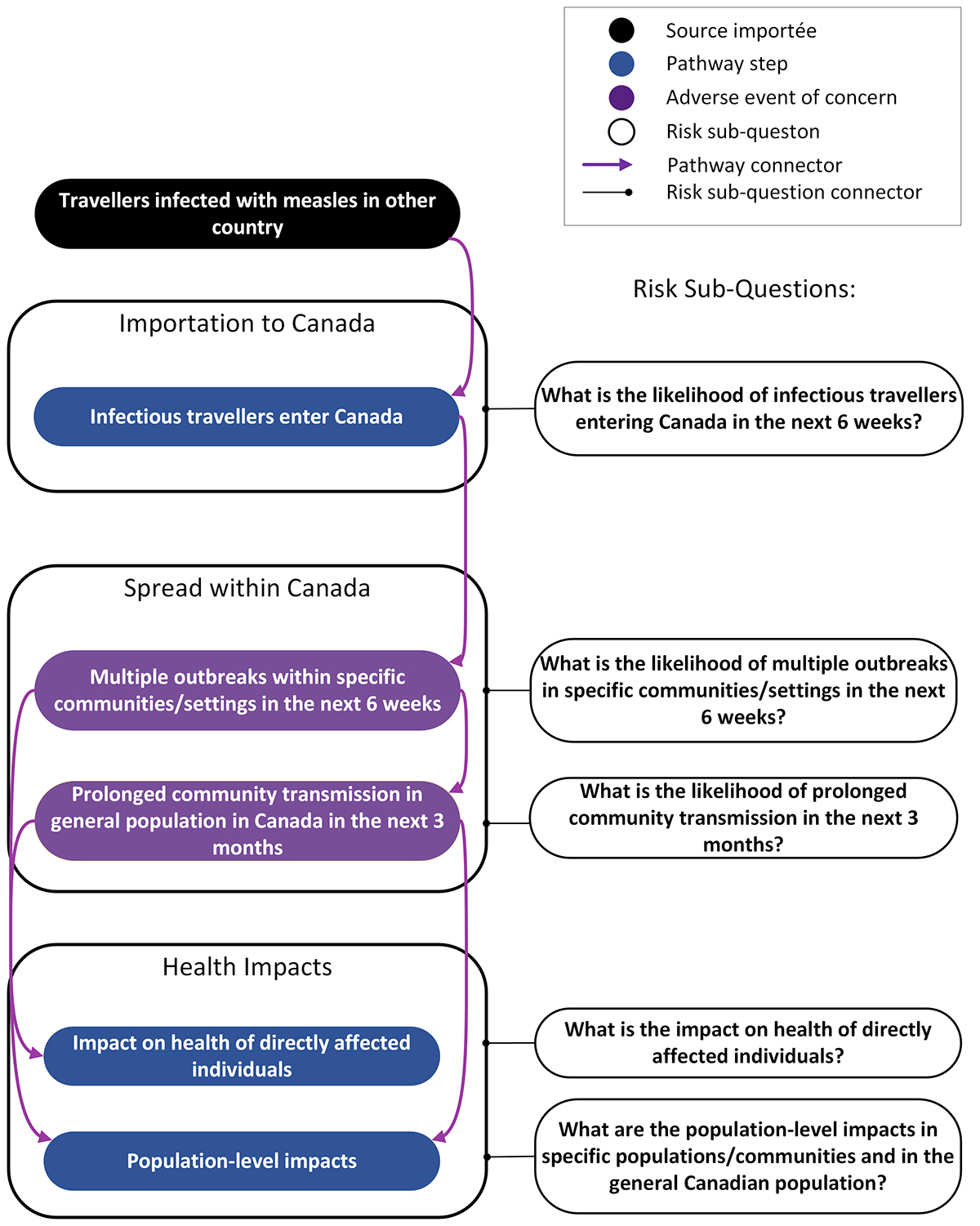
Figure 2: Text description
Importation to Canada
- Pathway connector from travellers infected with measles in other country leads to infectious travellers enter Canada
- Risk sub-question: What is the likelihood of infectious travellers entering Canada in the next 6 weeks?
Spread within Canada
- Pathway connector from infectious travellers enters Canada leads to adverse event of concern: Multiple outbreaks within specific communities/settings in the next 6 weeks
- Risk sub-question: What is the likelihood of multiple outbreaks in specific communities/settings in the next 6 weeks?
- Pathway connector from multiple outbreaks within specific communities/settings in the next 6 weeks leads to adverse event of concern: Prolonged community transmission in general population in Canada in the next 3 months
- Risk sub-question: What is the likelihood of prolonged community transmission in the next 3 months?
Health impacts
- Pathway connector from prolonged community transmission in general population in Canada in the next 3 months to Impact on health of directly affected individuals
- Risk sub-question: What is the impact on health of directly affected individuals?
- Pathway connector from prolonged community transmission in general population in Canada in the next 3 months to Population-level impacts
- Risk sub-question: What are the population-level impacts in the general Canadian population?
- Pathway connector from multiple outbreaks within specific communities/settings in the next 6 weeks to Population-level impacts
- Risk sub-question: What are the population-level impacts in specific populations/communities?
Note: Specific populations/communities include: Educational settings (child-care facilities, elementary, secondary, and post-secondary); Healthcare facilities (hospitals and ambulatory care settings); Long-term care facilities (residential or congregate living facilities for elderly populations, including retirement homes and elder lodges); and un/under-vaccinated communities (communities historically known to have lower vaccination coverage than the general population. This may include remote or isolated communities, communities that experience barriers to vaccine access, and communities that do not accept vaccination for ideological or religious reasons).
Risk question(s)
The following risk questions are derived from the risk pathway above:
- What is the likelihood and impact of multiple outbreaks in specific communities/settings in the next 6 weeks?
- What is the likelihood and impact of prolonged community transmission of measles in Canada in the next 3 months?
Likelihood and impact estimates
What is the likelihood of infectious travellers entering Canada within the next 6 weeks?
The likelihood of infectious travellers entering Canada within the next 6 weeks is expected to be high, with low uncertainty.
As of March 13, 2024, 10 of the 29 measles cases reported in 2024 in Canada were travel-related. Higher volumes of international travel during school holiday periods in March are expected to increase the likelihood of measles importation. Canada has strong travel links with several countries reporting high levels of measles activity; based on 2023 figures, during March to May >500,000 travellers could enter or return to Canada from the 10 countries reporting the highest incidence of measles in the past 6 months (between August 2023 and February 2024), including India, Pakistan and IndonesiaFootnote 13. Other popular sources of travel into Canada, including the United KingdomFootnote 14, EuropeFootnote 15, the United States of AmericaFootnote 16, and countries in the region of the AmericasFootnote 3 are experiencing increasing measles activity and travel volumes typically increase to these areas during spring break and are high over the coming months.
Uncertainty in this estimate is low given the well-documented increase in measles incidence internationally and the high volumes of travellers coming or returning to Canada in the next 6 weeks from countries reporting increased measles activity.
What would be the impact on an individual infected person (the magnitude of effects, including impact on mental health, disease morbidity/mortality, and/or welfare)?
The impact on vaccinated individuals is expected to be minor. The impact on unvaccinated individuals (>5 years) and unvaccinated children (1-5 years old) is expected to be moderate. The impact on vulnerable individuals (unvaccinated pregnant individuals, immunocompromised individuals, infants) is expected to be moderate to major. The uncertainty in these estimates is low.
The impact on an unvaccinated individual >1 year of age infected with measles is assessed as moderate, with low uncertainty.
Although the majority of measles cases are mild, measles infections can be severe and lead to long-term sequelae in unvaccinated and non-immune individuals, particularly young children. Approximately 20% of cases require hospitalizationFootnote 17Footnote 18. In Canada, between 2015-2023, 17% of cases were hospitalized (excluding ~3% of cases with unknown hospitalization status). Case fatality is 1-3 per 1000 cases and is highest in children <1 year of age, HIV-infected children, and adults over 20 years of ageFootnote 17. Diarrhea, otitis media and pneumonia due to secondary bacterial infections are common complicationsFootnote 17. Severe manifestations include respiratory failure and neurological complications such as post-infectious encephalitis (~1 in 1000 casesFootnote 17) and subacute sclerosing panencephalitis (SSPE), which is rare but can occur several years after measles infection. Measles infection has also been shown to diminish immunological memory, potentially increasing susceptibility to subsequent infection with other pathogensFootnote 19.
Among vulnerable individuals, the impact is expected to be moderate to major. The majority of infants under the age of one year are unvaccinated and at high risk of measles complications, hospitalization and deathFootnote 20 particularly between the time of loss of maternal antibodies and the time of first measles vaccination. Health and birth outcomes in pregnant individuals are likely to depend on prior immunity or vaccination status and timing of infection during pregnancy. However, measles in pregnancy carries a higher risk of hospitalization, pneumonia and deathFootnote 21. Measles infection in pregnancy also increases risk of pre-term birth and spontaneous abortionFootnote 21Footnote 22Footnote 23. Case fatality and respiratory and neurological complications are also more common among immunocompromised children and adults, and the exact impact on an individual is likely to vary depending on the type and extent of immunocompromiseFootnote 24.
Measles is expected to have minor health impacts in vaccinated individuals (that are not identified as vulnerable) and those with previous measles infection.
Uncertainty in this estimate is low; there is extensive evidence on the health impacts of measles.
What is the likelihood and impact of multiple outbreaks in educational settings in next 6 weeks?
The likelihood of multiple outbreaks in educational settings in the next 6 weeks is expected to be high, with low uncertainty. The impact of multiple outbreaks in educational settings is expected to be moderate, with moderate uncertainty.
School-aged children comprise the majority of measles cases in Canada and similar settingsFootnote 18. In Canada, 2-dose coverage among 7-year-olds declined from 87% in 2017 to 79% in 2021Footnote 6, suggesting that susceptibility among school-aged children could be increasing.
Outbreaks in educational settings (including child-care facilities, schools and post-secondary institutions) are known to occur in measles elimination settings and have been reported in CanadaFootnote 25Footnote 26Footnote 27Footnote 28. Educational settings with sub-optimal vaccination coverage are vulnerable to outbreaks because of the potential for accumulation of susceptible individuals in settings with high levels of social contact conducive to measles transmission. The majority of cases in these settings occur among unvaccinated or incompletely vaccinated individuals, indicative of measles introduction into a setting with sub-optimal immunity. However, measles outbreaks have been documented in secondary and post-secondary institutions with high vaccination coverage and involving cases among two-dose vaccine recipientsFootnote 29, indicating that under certain conditions waning immunity from vaccination and breakthrough infections may play a role in susceptibility and transmission in these settings.
Declines or delays in first-dose measles vaccination among 1 to 2-year-old children have also been reported in some jurisdictions because of the COVID-19 pandemicFootnote 30Footnote 31, indicating that susceptibility among pre-school children is likely to be higher for birth cohorts since 2019. Large outbreaks involving transmission in childcare and daycare settings have been reported in numerous settings including CanadaFootnote 25Footnote 32Footnote 33Footnote 34, notably in areas where vaccination coverage in the wider population was low. In a 2017 outbreak affecting primarily the Somali community in Minnesota, USA, and involving 12 childcare centres, transmission occurred in childcare centres for 43% of 75 cases and the attack rate was particularly high among children aged 1-4 years (69%); 91% of cases were unvaccinatedFootnote 32. In the 2011 outbreak in Québec, 83 children <5 years old were infected with measles, with daycare being the source of infection in about 20% of casesFootnote 25. Household exposure was also a prominent source of infection for children in these outbreaksFootnote 25Footnote 32Footnote 33, underlining the importance of maintaining high population vaccine coverage to reduce the risk of infection for partially vaccinated and unvaccinated children and infants.
Specific impacts are strongly dependent on context, the levels of immunity in the affected population and the capacity to implement control measures. Initial mathematical modelling suggests that in a population of 1,000 individuals (indicative of a secondary school, or an elementary school and immediate contacts such as teachers and household contacts), outbreaks involving 200-300 cases could occur if vaccination coverage is between 70% and 75% and no interventions are implemented (Table 2). Assuming a most likely scenario in educational settings of 80% vaccination coverage and stronger interventions, typical outbreaks with approximately 5 cases could be expected; outbreaks with >50 cases would be rare (for definitions of stronger and weaker interventions, see Appendix C). Outbreaks with 100-300 cases could occur if vaccine coverage <75% and weaker interventions are implemented (Table 2). These outbreaks could result in 20 to 60 hospitalizations and 10 to 30 cases with common measles complications (diarrhea, otitis media, pneumonia). It should be noted that public health interventions are challenging to incorporate into mathematical models and that results are highly dependent on individuals' acceptance of and capacity to adhere to control measures, such as isolation and post-exposure prophylaxis.
| Vaccination coverage | Probability of an outbreak | Median outbreak size (number of cases) |
|||
|---|---|---|---|---|---|
| Probability of an outbreak (≥2 cases; PHAC PHRSTable 2 Footnote a model, 5 initial cases) | Probability of outbreak size > 50 cases (PHAC PHRSTable 2 Footnote a model, 5 initial cases) | No intervention (PHAC PHRSTable 2 Footnote a model, 5 initial cases) | Weaker intervention (SFUTable 2 Footnote b model) | Stronger intervention (SFUTable 2 Footnote b model) | |
| 70% | 100% | 100% | 275 | 172 | 14 |
| 75% | 100% | 100% | 200 | 103 | 10 |
| 80% | 100% | 93% | 125 | 43 | 5 |
| 85% | 99% | 2% | 25 | 11 | 2 |
| 90% | 92% | 0 | 10 | 3 | 1 |
|
|||||
Outbreaks in pre-school and childcare settings are expected to be smaller in size due to the smaller number of children and staff in these settings, although health impacts are expected to be more severe in these younger age groups, particularly for unvaccinated children.
Educational settings allow for a large number of exposures which could require significant resources for contact tracing and follow-up vaccination with potential exposures. Public health measures to limit exposure to measles such as closure of childcare centres or exclusion of students from educational settings may have additional negative social and economic impacts on affected individuals and caregivers.
What is the likelihood and impact of multiple outbreaks in healthcare facilities in next 6 weeks?
The likelihood of multiple outbreaks in healthcare facilities in the next 6 weeks is expected to be high, with low uncertainty. The impact of multiple outbreaks in healthcare facilities is expected to be major, with moderate uncertainty.
Outbreaks involving nosocomial transmission are well recognized in the literature; transmission in healthcare facilities has been documented in outbreaks involving community transmissionFootnote 25Footnote 35Footnote 36. Measles virus can survive in evaporated droplets and on surfaces for up to two hours, facilitating transmission in emergency rooms, hospital waiting areas and outpatient settings even after an infectious individual has left the areaFootnote 5. During multiple outbreaks across CanadaFootnote 25, USAFootnote 37, and northern European countriesFootnote 25Footnote 38Footnote 39Footnote 40Footnote 41, index cases spread measles to between 2 and 17 other individuals (both patients and healthcare workers) during their initial visit to an emergency department or outpatient clinic.
Hospitals in Canada have strict guidelines for management of suspected measles casesFootnote 5. Healthcare workers should also have documented proof of measles immunity or immunization as appropriate. However, infectious individuals may visit healthcare facilities for other conditions before onset of measles symptoms; atypical clinical presentation of measles cases may also delay diagnosis and control measuresFootnote 42.
Timely implementation of control measures is expected for outbreaks in healthcare facilities to contain widespread transmission. However, certain healthcare facilities have high concentrations of vulnerable people (e.g., pregnant individuals, immunocompromised patients, infants) and more severe outcomes could occur if these groups are affected. Impacts could be greater in pediatric healthcare settings in which infants and unvaccinated young children could be exposed.
Outbreaks in healthcare facilities lead to additional demand for space (e.g., isolation rooms), resources (e.g., personal protective equipment), and on healthcare workers (e.g., enhanced infection, prevention and control measures; exclusion from work of exposed and potentially non-immune healthcare workers). Affected facilities also lead to disruption of services due to the need to divert resources for outbreak control, temporary reductions in staff if affected healthcare workers are excluded from work, or potential closure of critical services such as emergency rooms. Contact tracing and increased demand for diagnostics for suspected cases can also be significant. Given current strains on the healthcare system, particularly during the respiratory season, additional demands from measles outbreaks are expected to have major impacts on affected healthcare facilities.
Uncertainty in these estimates is moderate. There is recent and historical evidence of transmission of measles within healthcare facilities, but there is inherent unpredictability in the occurrence and extent of such outbreaks that are dependent on numerous factors including the type of healthcare facility and patient population served; levels of measles susceptibility in the population using health services; the number of contacts that could occur within a healthcare facility; the resources available for infection, prevention, and control (IPC); the alertness of healthcare workers for diagnosing individuals with measles; and the clinical presentation.
What is the likelihood and impact of multiple outbreaks in long-term care facilities in next 6 weeks?
The likelihood of multiple outbreaks in long-term care facilities in the next 6 weeks is expected to be very low, with low uncertainty. The impact of multiple outbreaks in long-term care facilities is expected to be minor, with moderate uncertainty.
In Canada, adults born before 1970 are presumed to have acquired natural immunity to measlesFootnote 12. Measles in individuals ≥60 years old is very rare: only 3 cases in this age group have been reported through measles surveillance since 1998Footnote 4Footnote 43Footnote 44. A meta-analysis of 8 different studies found that immunity does not wane significantly following natural infection, indicating that the likelihood of infection in older adults with previous infection is very lowFootnote 45.
Uncertainty in the likelihood estimate is low. Although data on immunity levels specifically among residents in long-term care facilities are not available, measles susceptibility in these settings is expected to be very low due to the high likelihood of naturally-acquired immunity in the age groups making up this population. There is some uncertainty regarding the extent to which diminished exposure to wildtype measles virus in the decades following measles vaccine introduction influences the maintenance of high levels of protective immunity among older adults, although currently available age-related serological data are consistent with high levels of immunity in this age groupFootnote 46Footnote 47.
The impact in these settings is expected to be minimal given the low likelihood of outbreaks. It should be noted, however, that these settings may experience additional impacts if there are staffing shortages due to illness.
What is the likelihood and impact of multiple outbreaks in un/under-vaccinated communities in next 6 weeks?
The likelihood of multiple outbreaks in un/under-vaccinated communities in the next 6 weeks is expected to be high, with low uncertainty. The impact of multiple outbreaks in un/under-vaccinated communities is expected to be major, with moderate uncertainty.
Measles outbreaks are known to occur in un/under-vaccinated, faith-based communities, that are resistant to or oppose vaccination, both in CanadaFootnote 48Footnote 49 and abroadFootnote 50Footnote 51. Unvaccinated children comprise the majority of cases in such outbreaks. Exposure risk in these communities can be amplified due to links with similar communities within Canada and abroadFootnote 48, and large outbreaks involving several hundred cases linked to schools in under-vaccinated communities have been documentedFootnote 49Footnote 50Footnote 51. Unvaccinated children also comprise the majority of cases in such outbreaks.
Within Canada, social inequalities in measles vaccination have also been recognizedFootnote 6. Results from the cNICS 2021 show that one-dose measles coverage among 2-year-olds is lower among children living in more remote areas compared to those living in easily accessible areas (65.3% vs 92.5%); children of parents with high school or lower education compared to children of parents with a bachelor degree or higher (80.2% vs 95.3%); and children from households with lower annual income (<$40,000: 80.2% vs ≥$160,000: 96.6%)Footnote 6. Delayed measles vaccination is also more likely among children in single-parent families and children born outside CanadaFootnote 52.
There are several specific considerations in relation to Indigenous and remote communities. Importation of measles into these communities is increased if community members become exposed due to travel, for example, by students who attend school outside their community and travel home during holidays. Exposures in school settings may result in risk of importations into Indigenous and remote communities with lower levels of immunization. Similarly, importations can result from temporary relocation of community members from remote and isolated communities to urban centres due to environmental hazards (e.g., spring flooding), or by healthcare staff providing services in remote communities, such as agency nurses who often travel through major air transport hubs, between multiple communities, and internationally. Some indigenous communities may be at higher risk for measles outbreaks due underlying challenges such as overcrowding and poor housing ventilation. In addition, some Indigenous and remote communities have proportionately higher populations of younger individuals and higher birth rates, increasing potential for measles transmission and risk of more severe outcomes among susceptible children.
Uncertainty in the likelihood estimate is low. Information on vaccine coverage and immunity in specific un/under-vaccinated populations is limited. However, there have been well-documented outbreaks linked to imported cases, particularly among under-vaccinated, faith-based communities. Low vaccination coverage in these populations could result in large outbreaks. Initial mathematical modelling suggests that in a community of 8,000 people, measles outbreaks could be controlled (i.e., the number of cases would be much smaller than the number of susceptible individuals) with stronger interventions even when vaccination coverage is 70%. However, if vaccination coverage falls to 60%, the model estimates that measles outbreaks with thousands of cases could occur, even with stronger interventions.
Large outbreaks in un/under-vaccinated populations would cause additional demand on healthcare services and public health resources, including resources for enhanced surveillance, contact tracing, and administration of vaccine and/or immunoglobulin, with potential impacts on local supply for these countermeasures. In lower resourced or more remote communities, outbreak impacts may be compounded by more limited capacity to implement timely control measures, and treatment of severe measles cases may be delayed if medical evacuation to a hospital is required. Finally, public health interventions are likely to be less effective in un/under-vaccinated communities, because of lower acceptance of post-exposure prophylaxis and/or vaccination in some communities, for example certain faith-based communities, or because of logistical and other challenges in remote and hard to reach communities.
What is the likelihood and impact of prolonged community transmission in the general population in Canada in the next 3 months?
The likelihood of prolonged community transmission in the general population in the next 3 months is expected to be moderate, with low uncertainty. The impact of prolonged community transmission in the general population is expected to be moderate, with moderate uncertainty.
Historically, measles outbreaks in Canada have primarily been contained within specific settings or communities with sub-optimal immunity. Outbreaks with spillover to the general population have occasionally been documented. The 2011 measles outbreak in Québec involved a large school outbreak that led to extended transmission in the wider population with multiple generations of transmission over 26 weeksFootnote 25.
Preliminary assessment, based on available age-stratified vaccination coverage and serological data, suggests that, if community transmission were to occur, the overall effective reproduction number, Re, for measles in Canada could be close to or exceed 1 (0.95 – 1.2 under different scenarios of population immunity and measles transmissibility), indicating that outbreaks with several generations of transmission in the wider population could occur in some areas, particularly if vaccine uptake is lower than the average coverage for Canada.
The incidence of measles globally is expected to continue rising in the coming months. Increasing numbers of importations due to travel during spring break increases the likelihood of seeding outbreaks domestically. Social gatherings, including those for religious holidays and celebrations (e.g., Easter, Eid Al-Fitr), could include individuals still within the infectious period of measles, such as those exposed to cases of measles acquired overseas, and post-secondary and secondary school students returning home. This could produce more opportunities for spillover into the wider population, particularly in areas with lower vaccination coverage.
Canada has generally high levels of measles vaccination coverage. Although large measles outbreaks involving community transmission are possible and have been observed, the severe health impacts of measles infection are expected to be primarily limited to unvaccinated and non-immune individuals. The largest measles outbreak in recent history occurred in Quebec in 2011 and involved 725 cases over 26 weeks; among the 86 hospitalizations, only 3% had received at least 2 doses of measles vaccineFootnote 25.
Areas with active outbreaks are expected to experience additional demand for healthcare facility space (e.g., for patient isolation) and resources for enhanced IPC measures. However, current healthcare capacity in many areas is already limited across Canada, and additional demands on health services during outbreaks could result in temporary but significant impact on healthcare services and disruption to services in affected areas. Additional demand on public health resources including enhanced surveillance, contact tracing, virological testing, and administration of vaccination and post-exposure prophylaxis would also be expected.
Uncertainty in these estimates is moderate. There is considerable variation in vaccination coverage across Canada and a more detailed quantitative assessment of this variation on population susceptibility to measles outbreaks is needed to assess the population level morbidity at a national scale. There are also variations in the acceptance of public health interventions among the population post-pandemic, and the capacity of the health system in these settings to respond, and the uncertainty regarding the possibility and potential impact of super-spreading events.
Gaps in knowledge
This assessment is based on facts known to PHAC at the time of publication and has several important limitations that affect the uncertainty in the estimates of likelihood and impact. Key scientific uncertainties and knowledge gaps identified during this assessment include:
| Domain | Knowledge/information gaps identified |
|---|---|
Introduction |
|
Exposure |
|
Susceptibility |
|
Spread |
|
Longer-term/indirect impacts |
|
Interventions |
|
Appendix A: Methods
Two committees supported the assessment: the Rapid Risk Assessment (RRA) Steering Committee and the RRA Technical Team. The Steering Committee (largely comprised of senior managers and decision makers) defined the hazard, agreed on the purpose and key objectives for the assessment, outlined the scope, drafted the risk question, and reviewed the recommendations. The Technical Team (largely comprised of those with expertise and/or information related to the assessment) characterized the risk by providing qualitative estimates of likelihood, impact and uncertainty in relation to the risk questions being assessed, based on the available evidence and expert opinion. The teams consisted of federal and provincial public health experts, as well as those in academia, representing a range of disciplines, including public health and epidemiology, virology, medicine, infection control, risk communication, behavioural science, mathematical modelling, travel health, and Indigenous health.
The risk questions being assessed were visualized using a risk pathway (Figure 1), a diagrammatic representation of the key components of the sequence of the hazard from its source to its infection of the adverse event of interest. Each step in the risk pathway is associated with a likelihood or impact sub-question to be addressed as part of the risk assessment.
Definitions of likelihood (Table A1), impact (Tables A2, A3), and uncertainty (Table A4) are provided below. Since the risk pathway describes the sequence of events leading up to the undesired outcome, the likelihood of each event is conditional on the likelihood of preceding steps in the risk pathway, as assessed in the estimation process for each risk pathway sub-question. The likelihood for the overall risk question is therefore determined by the lowest likelihood estimated along the risk pathway. The findings and conclusions represent the consensual, but not necessarily unanimous, opinions of experts contributing to this risk assessment, and should not be interpreted as representing the views of all participants and their respective organizations. Evidence was gathered by scientific experts using a rapid, non-systematic literature search and includes published articles and pre-print manuscripts, reports on the current outbreak including surveillance reports, and communication from subject matter experts. Where appropriate, some references have been included; where references are not included, this evidence was informed by input from the subject matter experts.
| Likelihood estimate | Criteria |
|---|---|
| High | The situation described in the risk assessment question is highly likely to occur (i.e., is expected to occur in most circumstances). |
| Moderate | The situation described in the risk assessment question is likely occur. |
| Low | The situation described in the risk assessment question is unlikely to occur. |
| Very low | The situation described in the risk assessment question is very unlikely to occur (i.e., is expected to occur only under exceptional circumstances). |
| Estimate | Criteria |
|---|---|
| Severe | Severe impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income). |
| Major | Major impact on mental health and/or disease morbidity/mortality and/or welfare (e.g. loss of income). |
| Moderate | Moderate impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income). |
| Minor | Minor impact on mental health and/or disease morbidity/mortality and/or welfare (e.g. loss of income). |
| Minimal | Minimal or no impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income). |
| Estimate | Impact criteria | Primary impact examples | Secondary impact examples |
|---|---|---|---|
Severe |
The situation described in the risk assessment question will have severe negative consequences on the population. |
Potential pandemic in the general population or large numbers of case reports, with significant impact on the well-being of the population. Severe impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income). |
|
Major |
The situation described in the risk assessment question will have major negative consequences on the population. |
Case reports with moderate to significant impact on the well-being of the population. Moderate to significant impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income) affecting a larger proportion of the population and/or several regions. |
|
Moderate |
The situation described in the risk assessment question will have moderate negative consequences on the population. |
Case reports with low to moderate impact on the well-being of the population. Low to moderate impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income) affecting a larger proportion of the population and/or several regions. |
|
Minor |
The situation described in the risk assessment question will have minor negative consequences on the population. |
Rare case reports, mainly in small at-risk groups, with moderate to significant impact on the well-being of the population Moderate to significant impact on mental health and/or disease morbidity/mortality and/or welfare (e.g., loss of income) on a small proportion of the population and/or small areas (regional level or below). |
|
Minimal |
The situation described in the risk assessment question will have minimal or no negative consequences on the population. |
No or very rare case reports with low to moderate impact on the well-being of the population. Negligible or no impact on mental health and/or disease morbidity/mortality, and/or welfare (e.g., loss of income). |
|
|
|||
| Uncertainty | Criteria |
|---|---|
| Very High | Lack of data or reliable information; results based on crude speculation only. |
| High | Limited data or reliable information available; results based on educated guess. |
| Moderate | Some gaps in availability or reliability of data and information, or conflicting data; results based on limited consensus. |
| Low | Reliable data and information available but may be limited in quantity or be variable; results based on expert consensus. |
| Very low | Reliable data and information are available in sufficient quantity; results strongly anchored in empiric data or concrete information. |
Appendix B: Estimation of the effective reproduction number (Re) for measles
The basic reproduction number, R0, represents the average number of persons that an infectious individual can infect in a totally susceptible population. In the presence of population immunity, either following naturally-acquired infection or vaccination, the average number of secondary infections arising from an infectious individual (the net or effective reproduction number, Re) depends on the proportion of the population that is susceptible to infection:
Re = sR0
The proportion of the population susceptible to infection, s, can be estimated using serological data, or data on vaccination coverage adjusted for the vaccine efficacy. Because social mixing patterns and vaccination coverage can vary by age, information on age-related contact patterns and immunity can be used to estimate the susceptible proportion in the population accounting for age-related social mixing, and Re can be derived for an assumed value of the basic reproduction number, R0. This approach can give an indication of the capacity for measles to be transmitted in the population given current levels of population immunity, if measles were to be successfully introduced. The method described by Funk et al.Footnote 53 was used to estimate the overall susceptible proportion for Canada in 2023, under different population immunity scenarios.
In Scenario 1, available data were used on 1- and 2-dose measles vaccination coverage for individual birth cohorts since 2007 from the Child National Immunization Coverage Survey (cNICS)Footnote 6. For earlier birth cohorts, serological data were used as reported by Osman et al.Footnote 46 based on samples collected between 2009 and 2013 through the Canadian Health Measures Survey, corrected for current age. For birth cohorts since 2007, we estimated the proportion immune by considering that one dose of measles-containing vaccine provides 95% protection and two doses provide 96% protectionFootnote 54, assuming that vaccination is distributed at random in the populationFootnote 46, based on samples collected between 2009 and 2013 through the Canadian Health Measures Survey, corrected for current age. For birth cohorts since 2007, we estimated the proportion immune by considering that one dose of measles-containing vaccine provides 95% protection and two doses provide 96% protectionFootnote 54, assuming that vaccination is distributed at random in the population. Infants were assumed to have 50% protection as a result of maternal antibody, and 80% of children aged 12 months were assumed to have received a first dose of measles vaccineFootnote 30Footnote 31. This scenario reflected average vaccine coverage levels for birth cohorts since 2007 of 90% for one dose by age 2 years, and 85% for two doses by age 7 years.
Scenario 2 assumed lower than average levels of vaccine coverage in birth cohorts since 2007, reflecting average vaccine coverage levels for birth cohorts since 2007 of 86% for one dose by age 2 years, and 78% for two doses by age 7 years. Immunity levels for earlier birth cohorts were as for Scenario 1.
To account for age-related contact patterns, we used a Canada-specific contact matrix developed by Prem et al.Footnote 55 Estimates of Re under each scenario were derived for different assumed values of R0 (12 or 15). Estimated immunity levels by age for the three scenarios are shown in Figure A1.
Figure A1. Percentage immune by age estimated from scenario 1 and scenario 2
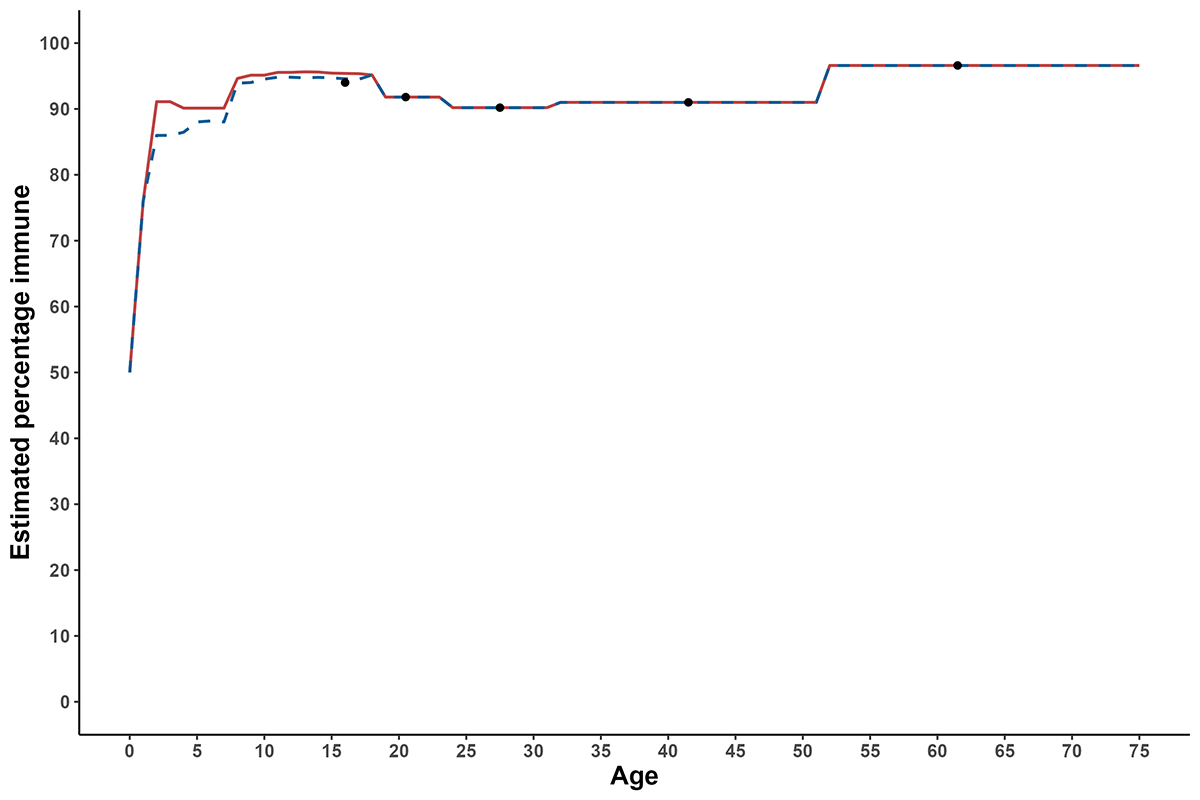
Figure A1: Text description
The line graph shows the percentage of the population immune to measles (y-axis) by age (x-axis) inferred from two different scenarios. In Scenario 1, the percentage immune rises from 50% among infants to 91% among 2-year old children, and to 95% for children aged 8-18 years. In Scenario 2, the percentage immune rises from 50% among infants to 86% among 2-year old children, and to slightly below 95% for children aged 8-18 years. In both scenarios, the percentage immune among adults is the same, and ranges from 90% among 24-year olds to 96% among individuals aged >50 years.
| Age (years) | Estimated percentage immune | ||
|---|---|---|---|
| Scenario 1 | Scenario 2 | Serological data | |
| 0 | 50.0 | 50.0 | - |
| 1 | 76.0 | 76.0 | - |
| 2 | 91.1 | 86.0 | - |
| 3 | 91.1 | 86.0 | - |
| 4 | 90.1 | 86.5 | - |
| 5 | 90.1 | 88.0 | - |
| 6 | 90.1 | 88.2 | - |
| 7 | 90.1 | 88.0 | - |
| 8 | 94.6 | 93.9 | - |
| 9 | 95.1 | 94.0 | - |
| 10 | 95.1 | 94.5 | - |
| 11 | 95.6 | 94.8 | - |
| 12 | 95.6 | 94.8 | - |
| 13 | 95.6 | 94.7 | - |
| 14 | 95.6 | 94.8 | - |
| 15 | 95.4 | 94.7 | - |
| 16 | 95.4 | 94.6 | 94.0 |
| 17 | 95.4 | 94.5 | - |
| 18 | 95.2 | 95.2 | - |
| 20 | 91.8 | 91.8 | 91.8 |
| 28 | 90.2 | 90.2 | 90.2 |
| 42 | 91.0 | 91.0 | 91.0 |
| 62 | 96.6 | 96.6 | 96.6 |
Estimates of R e for each scenario are presented below. Immunity levels based on available overall vaccine coverage estimates and serological data for Canada (Scenario 1) suggest a R e value of ~1, corresponding to the endemicity threshold.
| Population immunity scenario | R0 | Estimated % susceptible | Re |
|---|---|---|---|
| 1 | 12 | 7.9% | 0.95 |
| 1 | 15 | 7.9% | 1.18 |
| 2 | 12 | 8.2% | 0.98 |
| 2 | 15 | 8.2% | 1.22 |
Appendix C: Mathematical models of expected outbreak sizes under different scenarios
Two mathematical models of measles transmission were used to inform spread scenarios for measles under different settings and scenarios. The models were stochastic, compartmental Susceptible, Exposed, Infected, Recovered (SEIR) models developed by the PHAC Public Health Risk Sciences Division (PHRS) and the Department of Mathematics, Simon Fraser University (SFU).
The PHRS model considered a population of 1,000 individuals (indicative of a secondary or elementary school with immediate household contacts). The model simulated expected outbreak sizes following an initial introduction of varying numbers of infectious individuals (1, 5 and 10) and no interventions, exploring scenarios of varying population immunity (70%-90%).
The SFU model additionally considered a population of 8,000 individuals (indicative of a small community), as well as implementation of stronger and weaker interventions, defined as follows:
- Stronger interventions :
- Measles cases are notified and isolate within 1-2 days.
- Susceptible/exposed individuals are notified within 2 days of exposure; half are willing to self-isolate, with 35% effectiveness.
- Among those offered post-exposure prophylaxis, somewhat fewer accept it than isolateFootnote 56.
- Within 0.5-1 day of rash onset, most individuals isolate with high, but imperfect effectiveness.
- Weaker interventions:
- Measles cases are notified and isolate within 2-3 days.
- Susceptible/exposed individuals are notified within 3 days of exposure; half are willing to self-isolate, with 35% effectiveness.
- Post-exposure prophylaxis is offered to fewer individuals due to delayed detection.
- Within 1-2 days of rash onset, most individuals isolate with high, but imperfect effectiveness.
The model simulated expected outbreak sizes in these two populations under stronger and weaker interventions and different scenarios of vaccination coverage (55%-95%).
In both models, the basic reproduction number for measles, R0, was assumed to be 15. The models did not include social structure, such as age composition or age-specific contact rates.
Appendix D: Acknowledgements
Completed by the Public Health Agency of Canada's Centre for Surveillance, Integrated Insights and Risk Assessment within the Data, Surveillance and Foresight Branch.
Measles Rapid Risk Assessment Team
Public Health Agency of Canada: Rukshanda Ahmad, Disha Bhagat, Gabrielle Brankston, Melanie Cousins, Gwen Eagle, Kristyn Franklin, Sashini Kosgoda, Yi Qiao Liu, Kashmeera Meghnath, Akwasi Owusu-Kyem, Sandra Radons Arneson, Clarence Tam, Shelley Veilleux, Linda Vrbova
Mathematical modelling
Public Health Agency of Canada: Michael Li
Simon Fraser University: Caroline Colijn, Jennifer McNicol, Samara Chaudhury, Javad Valizadeh
The individuals listed below are acknowledged for their contributions to this report:
- Alberta Health: Amy Elefson, Joy Jaipaul
- Alberta Health Services: Francesco Rizzuti
- British Columbia Centre for Disease Control: Monika Naus, Keren Massey-Slipp
- Department of Health and Community Services, Government of
- Newfoundland and Labrador: Cheryl Foo
- Department of Health and Wellness, Government of Nova Scotia: Shelley Deeks, Jenni Cram
- Department of Health and Wellness, Prince Edward Island: Heather Morrison
- Department of Health, Government of Nunavut: Serge Kabore, Kethika Kulleperuma
- Health and Social Services, Government of Northwest Territories: Jenelle Hurley, Caroline Newberry
- Manitoba Health: Richard Baydack, Josee Hunter, Carol Kurbis, Santina Lee
- Ministère de la Santé et des Services sociaux du Québec: Danielle Auger, Monique Landry
- Ontario Ministry of Health: Michelle Murti
- Public Health Ontario: Christine Navarro, Sarah Wilson
- Saskatchewan Ministry of Health: Saqib Shahab, Lisa Haubrich
Other federal departments
Health Canada/Public Health Agency of Canada Communications: Gabriela Capurro Estremadoyro, Lidia Guarna, Chris Hinds, Sheila Manhire, Quenby Joanette
Immigration, Refugees and Citizenship Canada: Jessica Halverson, Catherine Rutledge-Taylor, Amy Styles, Janice Zhang
Indigenous Services Canada: Melanie Knight, Carrie Van Dusen, Tom Wong
Other individuals from various programs across PHAC
Oliver Baclic, Patricia Barcellos, Christopher Bell, Alain Boucard, Heather Deehan, Marwa Ebrahim, Aamir Fazil, Rhea Ferguson, Nicole Forbes, Nicolas Gilbert, Jeremy Gretton, Joanne Hiebert, Fanie Lalonde, Lisa Landry, Janice Merhej, Joshua Muncaster, Celine Nadon, Nicholas Ogden, Milan Patel, Mireille Plamondon, Nadine Sicard, Sheenu Singla, Ming Su, Nathalie Tremblay, Matthew Tunis, Ama Tweneboa Kodua.
Footnotes
- Footnote a
-
Here, an outbreak refers to two or more confirmed cases linked, either epidemiologically or virologically or both.
- Footnote b
-
Educational settings includes child-care facilities, elementary, secondary, and post-secondary.
- Footnote c
-
Here, prolonged community transmission refers to spread in the general population extending more than two generations of transmission.
- Footnote d
-
Here, an outbreak refers to two or more confirmed cases linked, either epidemiologically or virologically or both.
References
- Footnote 1
-
World Health Organization. EpiData 1/2023, https://www.who.int/andorra/publications/m/item/epidata-1-2023 (2023).
- Footnote 2
-
World Health Organization. EpiData 1/2024, https://www.who.int/andorra/publications/m/item/epidata-1-2024 (2024).
- Footnote 3
-
Pan American Health Organization / World Health Organization. Epidemiological Alert: Measles in the Region of the Americas. 29 January 2024. 2024. Washington, D.C.: PAHO/WHO, https://www.paho.org/en/documents/epidemiological-alert-measles-region-americas-29-january-2024.
- Footnote 4
-
Coulby C, Domingo FR, Hiebert J, et al. Measles surveillance in Canada, 2019. Canada Communicable Disease Report = Releve Des Maladies Transmissibles Au Canada 2021; 47: 149-160. DOI: 10.14745/ccdr.v47i03a05.
- Footnote 5
-
The Public Health Agency of Canada. Guidelines for measles outbreak in Canada. 2013, https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2013-39/guidelines-prevention-control-measles-outbreaks-canada.html.
- Footnote 6
-
The Public Health Agency of Canada. Highlights from the 2021 childhood National Immunization Coverage Survey (cNICS). 2023, https://www.canada.ca/en/public-health/services/immunization-vaccines/vaccination-coverage/2021-highlights-childhood-national-immunization-coverage-survey.html.
- Footnote 7
-
World Health Organization/The World Organization for Animal Health/Food and Agriculture Organization of the United Nations. Joint Risk Assessment Operational Tool (JRA OT): An Operational Tool of the Tripartite Zoonoses Guide – Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. 2020. Food and Agriculture Organization of the United Nations, https://www.who.int/initiatives/tripartite-zoonosis-guide/joint-risk-assessment-operational-tool.
- Footnote 8
-
World Health Organization. Rapid risk assessment of acute public health events. 2012. World Health Organization, https://www.who.int/publications/i/item/rapid-risk-assessment-of-acute-public-health-events.
- Footnote 9
-
European Centre for Disease Prevention and Control. Operational tool on rapid risk assessment methodology. 2019, https://www.ecdc.europa.eu/en/publications-data/operational-tool-rapid-risk-assessment-methodology-ecdc-2019.
- Footnote 10
-
Fappani C, Gori M, Canuti M, et al. Breakthrough Infections: A Challenge towards Measles Elimination? Microorganisms 2022; 10: 1567. DOI: 10.3390/microorganisms10081567.
- Footnote 11
-
McLean HQ, Fiebelkorn AP, Temte JL, et al. Prevention of Measles, Rubella, Congenital Rubella Syndrome, and Mumps, 2013: Summary Recommendations of the Advisory Committee on Immunization Practices (ACIP). 2013, https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6204a1.htm.
- Footnote 12
-
Public Health Agency of Canada. Measles vaccines: Canadian Immunization Guide. 2020, https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-12-measles-vaccine.html.
- Footnote 13
-
World Health Organization. Provisional monthly measles and rubella data, https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/surveillance/monitoring/provisional-monthly-measles-and-rubella-data (2024).
- Footnote 14
-
UK Health Security Agency. Latest measles statistics published, https://www.gov.uk/government/news/latest-measles-statistics-published (2024).
- Footnote 15
-
European Centre for Disease Prevention and Control. Notification rate of measles (per million), February 2023 - January 2024, https://www.ecdc.europa.eu/en/publications-data/notification-rate-measles-million-february-2023-january-2024 (2024, accessed 03-14 2024).
- Footnote 16
-
Centers for Disease Control and Prevention. Measles cases in 2024, https://www.cdc.gov/measles/cases-outbreaks.html (2024).
- Footnote 17
-
Perry RT and Halsey NA. The Clinical Significance of Measles: A Review The Journal of Infectious Diseases 2004; 189: S4-S16. DOI: 10.1086/377712.
- Footnote 18
-
Ramsay LC, Crowcroft NS, Thomas S, et al. Cost-effectiveness of measles control during elimination in Ontario, Canada, 2015. Euro Surveill 2019; 24: pii=1800370.
- Footnote 19
-
Mina M, Kula T, Leng Y, et al. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science 2019; 366: 599-606.
- Footnote 20
-
Centers for Disease Control and Prevention. Measles (Rubeola): For Healthcare Providers, https://www.cdc.gov/measles/hcp/index.html (2020).
- Footnote 21
-
Rasmussen S and Jamieson D. What Obstetric Health Care Providers Need to Know About Measles and Pregnancy. Obstet Gynecol 2015; 126: 163-170. DOI: 10.1097/AOG.0000000000000903.
- Footnote 22
-
Schönberger K, Ludwig M-S, Wildner M, et al. Epidemiology of Subacute Sclerosing Panencephalitis (SSPE) in Germany from 2003 to 2009: A Risk Estimation. PLOS ONE 2013; 8: e68909. DOI: 10.1371/journal.pone.0068909.
- Footnote 23
-
White S, Boldt K, Holditch S, et al. Measles, mumps, and rubella. Clin Obstet Gynecol 2012; 55: 550-559. DOI: 10.1097/GRF.0b013e31824df256.
- Footnote 24
-
Kimberlin DW, Barnett ED, Lynfield R et al. Measles. Red Book: 2021–2024 Report of the Committee on Infectious Diseases. American Academy of Pediatrics, 2021, https://publications.aap.org/redbook/book/347/Red-Book-2021-2024-Report-of-the-Committee-on.
- Footnote 25
-
De Serres G, Markowski F, Toth E, et al. Largest measles epidemic in North America in a decade--Quebec, Canada, 2011: contribution of susceptibility, serendipity, and superspreading events. The Journal of Infectious Diseases 2013; 207: 990-998. DOI: 10.1093/infdis/jis923.
- Footnote 26
-
Pielak K and Hilton A. University students immunized and not immunized for measles: a comparison of beliefs, attitudes, and perceived barriers and benefits. Can J Public Health 2003; 94: 193-196. DOI: 10.1007/bf03405065.
- Footnote 27
-
Sutcliffe P and Rea E. Outbreak of measles in a highly vaccinated secondary school population. CMAJ 1996; 155: 1407-1413.
- Footnote 28
-
Duclos P, Redd SC, Varughese P, et al. Measles in adults in Canada and the United States: implications for measles elimination and eradication. International Journal of Epidemiology 1999; 28: 141-146. DOI: 10.1093/ije/28.1.141.
- Footnote 29
-
Defay F, De Serres G, Skowronski DM, et al. Measles in Children Vaccinated With 2 Doses of MMR. Pediatrics 2013; 132: e1126-e1133. DOI: 10.1542/peds.2012-3975.
- Footnote 30
-
Kiely M, Mansour T, Brousseau N, et al. COVID-19 pandemic impact on childhood vaccination coverage in Quebec, Canada. Human Vaccines and Immunotherapeutics 2022; 18: 2007707. DOI: 10.1080/21645515.2021.2007707.
- Footnote 31
-
MacDonald SE, Paudel YR, Kiely M, et al. Impact of the COVID-19 pandemic on vaccine coverage for early childhood vaccines in Alberta, Canada: a population-based retrospective cohort study. BMJ Open 2022; 12: e055968. DOI: 10.1136/bmjopen-2021-055968.
- Footnote 32
-
Banerjee E, Griffith J, Kenyon C, et al. Containing a measles outbreak in Minnesota, 2017: methods and challenges. Perspectives in Public Health 2020; 140: 162-171. DOI: 10.1177/1757913919871072.
- Footnote 33
-
Stein-Zamir C, Shoob H, Abramson N, Zentner G. Who are the children at risk? Lessons learned from measles outbreaks. Epidemiology & Infection 2012; 140(9): 1578-88.
- Footnote 34
-
Breen K. Several children hospitalized in growing measles outbreak affecting 7 Ohio daycares. CBC News, 2022, https://www.cbsnews.com/news/children-hospitalized-measles-outbreak-ohio-daycares-columbus/.
- Footnote 35
-
Choi WS, Sniadack DH, Jee Y, et al. Outbreak of Measles in the Republic of Korea, 2007: Importance of Nosocomial Transmission. The Journal of Infectious Diseases 2011; 204: S483-S490. DOI: 10.1093/infdis/jir087.
- Footnote 36
-
Chen R, Goldbaum G, Wassilak S, et al. An explosive point - Source measles outbreak in a highly vaccinated population: Modes of transmission and risk factors for disease. American Journal of Epidemiology 1989; 129: 173-182. DOI: 10.1093/oxfordjournals.aje.a115106.
- Footnote 37
-
Centers for Disease Control and Prevention. Hospital-Associated Measles Outbreak — Pennsylvania, March–April 2009. Morbidity and Mortality Weekly Report (MMWR). 2012; 61(2): 30-2.
- Footnote 38
-
Hiller U, Mankertz A, Koneke N, et al. Hospital outbreak of measles – Evaluation and costs of 10 occupational cases among healthcare worker in Germany. Vaccine 2019; 37: 1905-1909. DOI: 10.1016/j.vaccine.2019.02.068.
- Footnote 39
-
Benno K, Schweintzger NA and Werner Z. Measles recognition during measles outbreak at a paediatric university hospital, Austria, January to February, 2017. Euro Surveill 2020; 25: pii=1900260. DOI: 10.2807/1560-7917.ES.2020.25.3.1900260.
- Footnote 40
-
Koenig C, Wojtynska O and Paradowska-Stankiewicz I. Measles outbreak in a public hospital, Szczecin, Poland, January 2019. European Journal of Public Health 2019; 29: ckz185.460. DOI: 10.1093/eurpub/ckz185.460.
- Footnote 41
-
Barrett P, Cotter S, Ryan F, et al. A national measles outbreak in Ireland linked to a single imported case, April to September, 2016. Euro Surveill 2017; 23: pii=1700655. DOI: 10.2807/1560-7917.ES.2018.23.31.1700655.
- Footnote 42
-
Maltezou H and Wicker S. Measles in health-care settings. American Journal of Infection Control 2013; 41: p661-663. DOI: 10.1016/j.ajic.2012.09.017.
- Footnote 43
-
The Public Health Agency of Canada. Notifiable Diseases Online, https://diseases.canada.ca/notifiable/ (2024).
- Footnote 44
-
Coulby C, Domingo FR, Hiebert J, et al. Measles surveillance in Canada: 2018. Canada Communicable Disease Report = Releve Des Maladies Transmissibles Au Canada 2020; 46: 77-83. DOI: 10.14745/ccdr.v46i04a04.
- Footnote 45
-
Bolotin S, Osman S, Hughes SL, et al. In Elimination Settings, Measles Antibodies Wane After Vaccination but Not After Infection: A Systematic Review and Meta-Analysis. The Journal of Infectious Diseases 2022; 226: 1127-1139. DOI: 10.1093/infdis/jiac039.
- Footnote 46
-
Osman S, Crowcroft NS, McLachlan E, et al. Population immunity to measles in Canada using Canadian Health Measures survey data – A Canadian Immunization Research Network (CIRN) study. Vaccine 2022; 40: 3228-3235. DOI: 10.1016/j.vaccine.2022.04.011.
- Footnote 47
-
Bolotin S, Severini A, Hatchette T, et al. Assessment of population immunity to measles in Ontario, Canada: a Canadian Immunization Research Network (CIRN) study. Human Vaccines and Immunotherapeutics 2019; 15: 2856-2864. DOI: 10.1080/21645515.2019.1619402.
- Footnote 48
-
Kershaw T, Suttorp V, Simmonds K, et al. Outbreak of measles in a non-immunizing population, Alberta 2013. Canada Communicable Disease Report 2014; 40: 243-250. DOI: 10.14745/ccdr.v40i12a04.
- Footnote 49
-
Naus M, Puddicombe D, Murti M, et al. Outbreak of measles in an unvaccinated population, British Columbia, 2014. Canada Communicable Disease Report = Releve Des Maladies Transmissibles Au Canada 2015; 41: 169-174. DOI: 10.14745/ccdr.v41i07a02.
- Footnote 50
-
Zucker JR, Rosen JB, Iwamoto M, et al. Consequences of Undervaccination — Measles Outbreak, New York City, 2018–2019. New England Journal of Medicine 2020; 382: 1009-1017. DOI: 10.1056/NEJMoa1912514.
- Footnote 51
-
Woudenberg T, van Binnendijk RS, Sanders EAM, et al. Large measles epidemic in the Netherlands, May 2013 to March 2014: changing epidemiology. Eurosurveillance 2017; 22: 30443. DOI: 10.2807/1560-7917.ES.2017.22.3.30443.
- Footnote 52
-
Périnet S, Kiely M, De Serres G, et al. Delayed measles vaccination of toddlers in Canada: Associated socio-demographic factors and parental knowledge, attitudes and beliefs. Human Vaccines and Immunotherapeutics 2018; 14: 868-874. DOI: 10.1080/21645515.2017.1412899.
- Footnote 53
-
Funk S, Knapp JK, Lebo E, et al. Combining serological and contact data to derive target immunity levels for achieving and maintaining measles elimination. BMC Medicine 2019; 17: 180. DOI: 10.1186/s12916-019-1413-7.
- Footnote 54
-
Pietrantonj CD, Rivetti A, Marchione P, et al. Vaccines for measles, mumps, rubella, and varicella in children. Cochrane Database of Systematic Reviews 2020. DOI: 10.1002/14651858.CD004407.pub4.
- Footnote 55
-
Prem K, Cook AR and Jit M. Projecting social contact matrices in 152 countries using contact surveys and demographic data. PLOS Computational Biology 2017; 13: e1005697. DOI: 10.1371/journal.pcbi.1005697.
- Footnote 56
-
Hall V, Banerjee E, Kenyon C, et al. Measles Outbreak — Minnesota April–May 2017. MMWR Morb Mortal Wkly Rep 2017; 66: 713-717. DOI: 10.15585/mmwr.mm6627a1.
