Seasonal Influenza Vaccination Coverage in Canada, 2021–2022
Download the alternative format
(PDF format, 753 KB, 26 pages)
Organization: Public Health Agency of Canada
Published: January 2023
On this page
- About
- Key findings
- Introduction
- Methodology
- Results
- Discussion
- Strengths and limitations
- Conclusion
- References
About
This report summarizes the results from the 2021–2022 Seasonal Influenza Vaccination Coverage Survey. The survey is conducted every year to collect information on influenza vaccination uptake in the adult Canadian population. Respondents aged 18 years and older were questioned regarding their influenza vaccination uptake for the 2021–2022 season; reasons for vaccination and non-vaccination; knowledge, attitudes, and beliefs (KAB) regarding influenza vaccine, and vaccination in general; along with selected demographic information. With the current pandemic context, information related to COVID-19 vaccination was also collected. Data collection took place between January 4 and February 11, 2022.
Key findings
Influenza vaccine
- Overall, influenza vaccination coverage in the 2021–2022 season (39%) was similar to the 2020-2021 season (40%) and the 2019–2020 season (42%).
- Influenza vaccination coverage was higher in females (44%) than in males (33%).
- Among high-risk groups, coverage for seniors 65 years of age and older (71%) and adults aged 18–64 years with a chronic medical condition (CMC) (38%) remained below the national coverage goals of 80%.
- The majority had received their vaccine in October (36%) or November (40%).
- The main vaccination places were pharmacies (53%) or doctor's offices (22%).
- The most commonly reported reason for receiving the vaccine was to prevent infection or to avoid getting sick (40%), whereas the most common reason for non-vaccination was the perception of being healthy or never getting the flu (29%).
- Less than a third of Canadian adults (31%) stated that they had encountered difficulties in scheduling an appointment for getting the flu shot this year due to preventive measures in place to reduce the spread of COVID-19.
- Most adults (92%) reported that they believed flu shot is safe, and 71% of the population agreed that the opinion of their family doctor, general practitioner or nurse practitioner is an important part of their decision for getting the flu shot.
COVID-19 vaccines
- Most Canadian adults (94%) had either received a COVID-19 vaccine or booked an appointment for getting vaccinated at the time of the survey.
- A small proportion of adults (4%) did not plan to vaccinate against COVID-19, and 1% of the population were not sure if they would get vaccinated.
- Among people who did not receive a COVID-19 vaccine, the main reason for not getting vaccinated was concerns about the safety of the COVID-19 vaccines (22%).
- Overall, 47% of vaccinated individuals had received a COVID-19 booster dose.
- The proportion of those having received a COVID-19 booster was higher among seniors (78%) compared to younger adults without any CMC (35%).
- Among individuals who completed the primary series and did not receive a booster dose, 20% of them had already booked an appointment for getting a booster dose and 50% stated that they were very likely to get one in the future, whereas 10% were very unlikely to receive a booster dose.
- The proportion of people who reported being somewhat or very unlikely to receive a booster dose was lower among individuals who were vaccinated against flu this season (8%) compared to those who have not been vaccinated against flu (21%).
- The most commonly stated reason for receiving a booster dose was to put an end to the pandemic, whereas the most important reason for not receiving a booster dose was the perception of being well protected after receiving the primary series.
Introduction
Influenza, also known as the flu, is a respiratory illness caused primarily by the influenza A and B viruses. It is one of the leading causes of death in Canada, averaging 12,200 hospitalizations and 3,500 deaths each year.Footnote 1,Footnote 2 The flu viruses are constantly changing and can cause a wide spectrum of illness ranging from asymptomatic to severe, complicated illness.Footnote 1 Annual influenza vaccination is the most effective way to help prevent infection and to reduce the morbidity and mortality associated with influenza. Each year, based on the circulating virus strains expected to be dominant during the upcoming season, scientists and experts must choose which strains of virus to include in the vaccine in advance in order for vaccines to be produced and delivered on time.Footnote 2,Footnote 3 In Canada, the best time to get the influenza vaccine is between October and December, before the virus begins spreading in the community.Footnote 2,Footnote 4 The National Advisory Committee on Immunization (NACI) recommends that all individuals aged 6 months and older get the annual seasonal influenza vaccine, especially for populations at increased risk for influenza-related complications or hospitalization including:
- children between 6 months and under 5 years of age
- adults and children with certain CMCs, such as heart conditions, diabetes, cancer/immune disorder, anemia, renal diseases and morbid obesity
- seniors 65 years of age and older
- all pregnant peopleFootnote 5
Measuring vaccination coverage is necessary to track Canada's progress towards reaching its vaccination coverage goals by 2025, and to help identify under- and un-immunized populations. Identification of these populations can help inform and improve vaccination promotion efforts in order to increase vaccination uptake within targeted populations. The national vaccination coverage goals for the seasonal influenza vaccine (one dose per season) include:
- achieving 80% vaccination coverage among adults 65 years of age and older
- achieving 80% vaccination coverage among adults 18–64 years of age with chronic medical conditions (CMC)Footnote 6
Besides measuring adult vaccination coverage, this report also describes knowledge, attitudes and beliefs (KAB) regarding the influenza vaccine in particular, and vaccines in general, along with the reasons for non-vaccination. Understanding positive or negative perceptions regarding vaccination could help inform vaccination promotion efforts in order to better encourage vaccination uptake within the Canadian population.
Due to the ongoing COVID-19 pandemic, some additional questions were included in the survey to help measure the impact of the pandemic on influenza vaccination uptake and determine the potential difficulties encountered during vaccination. The respondents were also surveyed on their COVID-19 vaccination uptake and intention of getting a booster dose, with questions on factors behind non-vaccination, and reasons for hesitancy towards the COVID-19 vaccines. Identifying COVID-19 vaccine-related attitudes and intentions helps to inform successful vaccination campaigns given that vaccines are a critical part of the pandemic response.
Methodology
Survey sampling
The survey was conducted by Léger Marketing. A comprehensive description of the quantitative methodology can be found elsewhere.Footnote 7 Briefly, a stratified regional sampling approach was used, with survey respondents from each province and territory selected using random digit dialling of landlines and known cellphone-only household numbers.
Sample weights were calculated by Léger based on age, gender, region, language (mother tongue), education level, and whether the respondent lives in a cellphone-only household.
Data collection
Interviews were conducted between January 4, 2022 and February 11, 2022 in English and French, using a computer-assisted telephone interviewing (CATI) system. A total of 3,502 adults were surveyed regarding their influenza vaccination status, reasons for vaccination or non-vaccination, KAB regarding vaccination, COVID-19 vaccination status and intent, and select demographic information. Respondents who were unsure of their vaccination status for a specific vaccine were excluded from any subsequent analyses for the vaccine(s) they were unsure of.
Statistical analysis
Influenza vaccination coverage was estimated as the number of survey respondents who reported receiving the influenza vaccine in the 2021–2022 season, expressed as a weighted proportion of the survey respondents who provided a definitive response (i.e. responded yes or no to the influenza vaccination status question). Simple weighted proportions and 95% confidence intervals were calculated for categorical variables. Chi-squared tests with a p-value <0.05 were used to determine significant differences in vaccination coverage between genders within each age or risk group.
The precision of estimates was determined using the coefficient of variation. Estimates with a coefficient of variation from 16% to 33% indicated higher sampling error and are to be interpreted with caution. Estimates with a coefficient of variation greater than 33% or based on a count less than 10 were considered unreliable and therefore are not reported.
Results
The overall response rate calculated using the Marketing Research Intelligence Association's standard calculation method for the response rate of a telephone survey was 15%.Footnote 7
All the proportions (%) reported hereafter are weighted, whereas the sample sizes (n) are unweighted.
Seasonal influenza vaccination
Vaccination coverage
Overall, about 4 in 10 Canadian adults (39%) aged 18 years and older received the 2021–2022 influenza vaccine. Influenza vaccination uptake was significantly higher in females (44%) than in males (33%, p<0.001). The national influenza vaccination coverage goal for those at high risk of influenza-related complications or hospitalization (80%) has not been achieved; only 38% of the adults aged 18–64 years with CMC and 71% of seniors aged 65 years and older received the flu vaccine this year. The vaccination rate was lowest among adults 18–64 years of age without any CMC (27%). A significant difference in influenza vaccination uptake between females and males was observed among those 18–64 years of age without CMC and among seniors aged 65 years and older (Table 1.1).
| All | Male | Female | p | ||||
|---|---|---|---|---|---|---|---|
| Age group (years) | n | Vaccination coverage, % (95% CI) |
n | Vaccination coverage, % (95% CI) |
n | Vaccination coverage, % (95% CI) |
|
| All adults ≥18 | 3,487 | 38.7 (36.9–40.6) | 1,548 | 33.4 (30.8–36.0) | 1,914 | 43.9 (41.3–46.5) | <0.0001Footnote c |
| 18–64 | 2,389 | 30.1 (28.0–32.2) | 1,079 | 24.9 (22.1–27.8) | 1,286 | 35.0 (31.9–38.1) | <0.0001Footnote c |
| 18–64 with CMC | 713 | 37.6 (33.6–41.7) | 298 | 37.0 (31.0–43.1) | 407 | 38.3 (32.9–43.8) | 0.7544 |
| 18–64 without CMC | 1,658 | 26.8 (24.4–29.2) | 769 | 19.9 (16.9–23.0) | 873 | 33.7 (29.9–37.4) | <0.0001Footnote c |
| ≥65 | 1,098 | 71.0 (68.1–74.0) | 469 | 67.0 (62.2–71.8) | 628 | 74.6 (70.9–78.3) | 0.0126Footnote c |
Definitions: n: Number of respondents (unweighted). Footnotes:
|
|||||||
Overall, the influenza vaccination coverage rates for the 2021–2022 flu season are very close to the vaccination coverage estimates for previous seasons in Canada (Figure 1.1).Footnote 8, Footnote 9
Among high-risk groups, vaccination coverage rates for adults 18–64 years of age with a CMC and seniors 65 years of age and older remained steady over the past three seasons. Consistent with the previous cycles of the survey, the proportion of vaccinated respondents was highest among seniors aged 65 years and older (71%), lower among those 18–64 years of age with a CMC (38%), and lowest in those 18–64 years of age without a CMC (27%) (Figure 1.1).
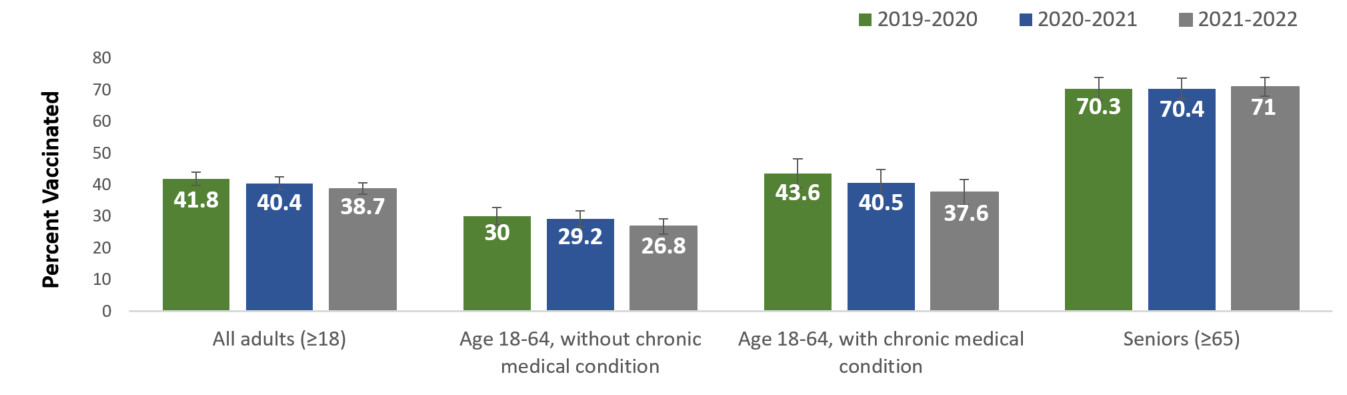
Figure 1.1: Text description
| Flu season | Percent vaccinated (%) |
|---|---|
| 2019–2020 | 41.8 |
| 2020–2021 | 40.4 |
| 2021–2022 | 38.7 |
| Flu season | Percent vaccinated (%) |
|---|---|
| 2019–2020 | 30.0 |
| 2020–2021 | 29.2 |
| 2021–2022 | 26.8 |
| Flu season | Percent vaccinated (%) |
|---|---|
| 2019–2020 | 43.6 |
| 2020–2021 | 40.5 |
| 2021–2022 | 37.6 |
| Flu season | Percent vaccinated (%) |
|---|---|
| 2019–2020 | 70.3 |
| 2020–2021 | 70.4 |
| 2021–2022 | 71.0 |
Month and place of vaccination
Among respondents who recalled the month they received their influenza vaccination (n=1,490), the majority received the vaccine in October (36%) or November (40%) 2021 (Table 2.1). In general, optimal antibody levels are achieved by two weeks following vaccination.Footnote 2 Therefore, it is best to be vaccinated early in the influenza season to allow time for the development of antibodies against the influenza virus before flu begins spreading in the community. September and October are generally good times to be vaccinated against flu.Footnote 2, Footnote 4 However, vaccination is still recommended until November or later, because flu most commonly peaks in February and significant activity can continue into May.Footnote 2
| Month | Proportion vaccinated in this month, % (95% CI) |
|---|---|
| September 2021 | 8.1 (6.5–9.7) |
| October 2021 | 35.8 (32.9–38.6) |
| November 2021 | 39.7 (36.8–42.7) |
| December 2021 | 15.0 (12.8–17.2) |
| January 2022 | 1.4 (0.6–2.2) |
Definition: CI: Confidence interval. Note: A total of 1,573 respondents were vaccinated and 1,490 respondents (94.7%) recalled the month of influenza vaccination. |
|
Consistent with previous seasons, the most commonly reported places of vaccination among adults were pharmacies (53%) and doctor's offices (22%) (Table 2.2). More and more people reported having received their flu vaccine in pharmacies, which may be due in part to the increasing number of jurisdictions allowing pharmacists to administer the influenza vaccine. Several provinces have implemented policies permitting pharmacists to administer influenza vaccines in community pharmacies to ease access to flu vaccination. A study has shown that influenza vaccination uptake has modestly increased in Canadian jurisdictions where pharmacists were allowed to administer influenza vaccines.Footnote 10
| Place of vaccination | Proportion vaccinated by place, % (95% CI) |
|---|---|
| Pharmacy | 53.4 (50.4–56.3) |
| Doctor's office | 22.2 (19.8–24.6) |
| Temporary vaccine clinic | 9.1 (7.4–10.7) |
| Workplace | 6.7 (5.0–8.4) |
| CLSC/Community health centre | 3.2 (2.1–4.3) |
| Hospital | 2.8 (1.8–3.7)Footnote a |
| Retirement residence | 1.7 (1.1–2.4)Footnote a |
| Other | 1.0 (0.4–1.5)Footnote a |
Definition: CI: Confidence interval. Note: A total of 1,573 respondents were vaccinated and 1,570 (99.8%) recalled their place of influenza vaccination. Footnotes: |
|
Reasons for vaccination
Among adults aged 18 years and older who provided a reason for receiving the vaccine (n=1,571), 40% were vaccinated because they wanted to prevent infection or to avoid getting sick. Among adults aged 18–64 years with CMC, being at higher risk because of their health condition was also a commonly reported reason for receiving the vaccine (19%); whereas for adults aged 18–64 years without CMC, avoid transmitting the disease to their family members, colleagues or friends (16%) was frequently reported as reason for vaccination (Table 3.1).
| Reason | % (95% CI) |
|---|---|
| All adults ≥18 (n=1,571) | |
| 1. To prevent infection/don't want to get sick | 39.9 (37.0–42.8) |
| 2. Receive it yearly (no specific reason) | 35.9 (33.1–38.6) |
| 3. To prevent transmitting the disease to family members, colleagues or friends | 10.9 (8.9–12.8) |
| 18–64 without CMC (n=485) | |
| 1. To prevent infection/don't want to get sick | 44.8 (39.5–50.0) |
| 2. Receive it yearly (no specific reason) | 27.5 (22.7–32.2) |
| 3. To prevent transmitting the disease to family members, colleagues or friends | 16.4 (12.3–20.5) |
| 18–64 with CMC (n=299) | |
| 1. To prevent infection/don't want to get sick | 36.0 (29.7–42.3) |
| 2. Receive it yearly (no specific reason) | 32.6 (26.6–38.7) |
| 3. At risk because of health condition | 19.0 (13.7–24.2) |
| ≥65 (n=779) | |
| 1. Receive it yearly (no specific reason) | 46.1 (42.3–50.0) |
| 2. To prevent infection/don't want to get sick | 37.2 (33.4–40.9) |
| 3. At risk because of age | 13.0 (10.4–15.6) |
Definition: n: Number of respondents (unweighted). Note: A total of 1,573 respondents were vaccinated and 1,571 respondents (99.9%) provided reasons for vaccination. Respondents could provide more than one reason. Footnotes:
|
|
Additionally, the non-specific reason of receiving it yearly (46%) and being at risk because of age (13%) were also commonly stated for having received the influenza vaccine among seniors aged 65 years and older. This suggested that these vaccinated respondents have adopted yearly influenza vaccination as a preventive health practice, potentially recognizing their increased risk for influenza-related complications.Footnote 11
Reasons for non-vaccination
Among unvaccinated respondents who provided their main reason for not getting the vaccine (n=1,897), the most common answer was the perception of being healthy or never getting the flu (23%). The most commonly provided reasons for non-vaccination did not vary much among different risk groups (Table 4.1).
| Reason | % (95% CI) |
|---|---|
| All adults ≥18 (n=1,897) | |
| 1. I am healthy/ never get the flu | 22.8 (20.7–25.0) |
| 2. No specific reason, just didn't get it | 17.7 (15.6–19.8) |
| 3. I did not get around to it | 13.0 (11.3–14.7) |
| 18–64 without CMC (n=1,164) | |
| 1. I am healthy/ never get the flu | 25.6 (22.8–28.4) |
| 2. No specific reason, just didn't get it | 17.1 (14.5–19.7) |
| 3. I did not get around to it | 13.3 (11.1–15.5) |
| 18–64 with CMC (n=411) | |
| 1. No specific reason, just didn't get it | 20.1 (15.5–24.7) |
| 2. I am healthy/ never get the flu | 15.2 (11.3–19.0) |
| 3. I did not get around to it | 13.6 (9.9–17.3) |
| ≥65 (n=312) | |
| 1. I am healthy/ never get the flu | 24.4 (19.3–29.5) |
| 2. No specific reason, just didn't get it | 16.8 (12.2–21.3) |
| 3. I did not get around to it | 10.3 (6.6–14.1)Footnote b |
Definition: n: Number of respondents (unweighted). Note: A total of 1,914 respondents were unvaccinated and 1,897 respondents (99.1%) provided reasons for non-vaccination. Footnotes:
|
|
Impact of the COVID-19 pandemic on influenza vaccination
In the context of the COVID-19 pandemic, the 2021–2022 influenza vaccination coverage survey also aimed to identify the potential impact of the pandemic on flu vaccination uptake. All of the respondents were asked if their likelihood of getting vaccinated against the flu had been affected due to the COVID-19 pandemic. Among those who provided a valid answer to the question (n=3,387), the majority (67%) stated that the COVID-19 pandemic did not affect their likelihood of getting the flu vaccine this year, while 20% were more likely to receive the flu vaccine and 13% were less likely to get the flu vaccine. A relatively lower proportion of individuals less likely to get the seasonal flu shot due to the pandemic was observed among seniors (7%) (Table 5.1).
| Response | % (95% CI) |
|---|---|
| All adults ≥18 (n=3,387) | |
| More likely to get the seasonal flu shot | 19.7 (18.2–21.3) |
| Less likely to get the seasonal flu shot | 13.2 (11.8–14.6) |
| Did not affect the likelihood of getting the seasonal flu shot | 67.1 (65.2–68.9) |
| 18-64 without CMC (n=1,613) | |
| More likely to get the seasonal flu shot | 17.9 (15.7–20.1) |
| Less likely to get the seasonal flu shot | 15.6 (13.5–17.7) |
| Did not affect the likelihood of getting the seasonal flu shot | 66.5 (63.8–69.2) |
| 18–64 with CMC (n=702) | |
| More likely to get the seasonal flu shot | 21.5 (18.0–24.9) |
| Less likely to get the seasonal flu shot | 12.1 (9.3–15.0) |
| Did not affect the likelihood of getting the seasonal flu shot | 66.4 (62.4–70.4) |
| ≥65 (n=1,054) | |
| More likely to get the seasonal flu shot | 22.8 (20.0–25.6) |
| Less likely to get the seasonal flu shot | 7.3 (5.5–9.1) |
| Did not affect the likelihood of getting the seasonal flu shot | 70.0 (66.9–73.0) |
Definition: CI: Confidence interval. Note: A total of 3,387 respondents provided a valid answer to this question. Footnotes:
|
|
Moreover, among individuals who had taken action to get vaccinated against flu this year (n=1,931), less than one third (31%) of them reported having encountered difficulties in scheduling an appointment for getting the flu shot due to the public health measures in place to reduce the spread of COVID-19. The proportion was lower comparing to previous year (47%).9 The most common difficulties encountered were limited appointment availability (11%); concerns about being exposed to COVID-19 (10%); and a lack of walk-in options (8%) (Table 5.2).
| Response | % (95% CI) |
|---|---|
| Limited appointment availability | 11.0 (9.3–12.7) |
| Concern about being exposed to COVID-19 | 10.3 (8.7–12.0) |
| Lack of walk-in options | 8.0 (6.5–9.5) |
| The vaccine was not offered at my usual/convenient location | 7.7 (6.2–9.1) |
| Other reasons | 7.1 (5.7–8.5) |
| I didn't encounter any difficulties in scheduling an appointment | 68.7 (66.2–71.2) |
Definition: CI: Confidence interval. Note: 1,289 of respondents have not taken any action to get vaccinated this year and 282 respondents did not provide a valid answer to the question, they are therefore excluded from the analysis. |
|
Knowledge, attitudes and beliefs regarding vaccination
Most Canadian adults (94%) strongly or somewhat agreed that vaccines are important for their health and thought that they know enough about vaccines to make a decision about getting vaccinated. A large majority (92%) believed that the flu vaccine is safe and a similar proportion (91%) understand why the flu vaccine is recommended annually (Table 6.1).
| Statements | n | Strongly or somewhat agree % (95% CI) |
|---|---|---|
| All vaccines in general | ||
| In general, I consider vaccines to be important for my health. | 3,477 | 93.7 (92.6–94.7) |
| I know enough about vaccines to make an informed decision about getting vaccinated. | 3,475 | 94.0 (93.0–95.0) |
| Influenza vaccine | ||
| The flu vaccine does not protect you against getting the flu. | 3,328 | 34.6 (32.7–36.5) |
| Sometimes, you can get the flu from the flu vaccine. | 3,229 | 37.6 (35.6–39.6) |
| It's a good thing for children to get natural immunity (protection) against flu by being exposed to the virus. | 3,174 | 60.3 (58.3–62.3) |
| It's a good thing for adults to get natural immunity (protection) against flu by being exposed to the virus. | 3,290 | 55.0 (53.0–57.0) |
| The opinion of my family doctor, general practitioner or nurse practitioner is an important part of my decision when it comes to getting the flu vaccine. | 3,308 | 70.7 (68.9–72.6) |
| The flu vaccine is safe. | 3,371 | 92.1 (91.0–93.3) |
| I understand why the flu vaccine is recommended annually. | 3,434 | 91.4 (90.2–92.5) |
| COVID-19 vaccines | ||
| The COVID-19 vaccination passport is a good tool to motivate myself for getting vaccinated against the disease. | 3,387 | 64.6 (62.7–66.5) |
| The COVID-19 vaccination passport is an effective tool to help protect myself/my family or friends/those most at-risk of more severe COVID-19 disease. | 3,427 | 75.0 (73.3–76.8) |
| It's a good thing for children to get natural immunity (protection) against COVID-19 by being exposed to coronavirus | 3,293 | 37.8 (35.9–39.8) |
| It's a good thing for adults to get natural immunity (protection) against COVID-19 by being exposed to coronavirus. | 3,362 | 35.7 (33.8–37.7) |
Definition: n: Number of respondents (unweighted). |
||
However, more than one third of respondents (35%) believed that the flu vaccine is ineffective to protect them against the virus. In addition, almost 4 in 10 adults (38%) believed that they can get the flu from the flu vaccine, which is not true. Flu vaccines cannot cause flu illness since flu vaccines are made with inactivated viruses that cannot cause disease.2 Besides, the majority of adults believed that it is a good thing for children (60%) or adults (55%) to get natural immunity (protection) against flu by being exposed to the virus. In fact, when an individual is exposed to viruses or bacteria naturally, the developed immune response and symptoms are typically greater. However, when scientists are designing vaccines, they determine the smallest amount of virus or bacteria needed to generate a protective immunologic response. In this situation, vaccines afford protection with better control of the exposure. Moreover, any flu infection can carry a risk of serious complications, hospitalization or death, even among otherwise healthy children and adults. Therefore, getting vaccinated is a safer choice than risking illness to obtain immune protection.Footnote 12
Overall, 71% of the population strongly or somewhat agreed that the opinion of their family doctor, general practitioner or nurse practitioner is an important part of their decision for getting the flu vaccine. This indicates that there is public trust in health care professionals and suggests that advice from a health care provider and the frequency of interaction with the health care system may play an important role in influenza vaccination uptake.
Regarding COVID-19 vaccines, the majority of the Canadian adults thought that the COVID-19 vaccination passport is a good tool to motivate themselves for getting vaccinated against the disease (65%) and to help protect others especially those most at-risk of more severe COVID-19 disease (75%). In addition, more than one third of the population (38%) strongly or somewhat agreed that it is a good thing for children to get natural immunity against COVID-19 by being exposed to coronavirus. Moreover, a similar proportion 36% believed that it is good for adults to get natural immunity against COVID-19 by being exposed to coronavirus. A previous COVID-19 infection or COVID-19 vaccination can both provide immunity and protection from serious outcomes. However, alike the flu vaccine, COVID-19 vaccination provides a higher, more robust, and more consistent level of immunity to protect people from COVID-19 than infection alone.Footnote 13
COVID-19 vaccination
With the current COVID-19 pandemic, in addition to the seasonal influenza vaccination, information related to COVID-19 vaccination and booster doses was also collected in the survey this year. At the time of the data collection, between January 4, 2022 and February 11, 2022, most Canadian adults (94%) had either received at least one dose of a COVID-19 vaccine or booked an appointment to get vaccinated. A small proportion of adults (4%) did not plan to vaccinate against COVID-19, and about 1% were not sure if they would get vaccinated (Table 7.1).
| Response | >% (95% CI) |
|---|---|
| Yes (vaccinated with at least one dose of a COVID-19 vaccine) | 93.9 (92.9–95.0) |
| No, but I already booked an appointment for getting vaccinated | 0.4 (0.2–0.7)Footnote a |
| No, not sure if I will get vaccinated | 1.2 (0.7–1.7)Footnote a |
| No, I am not getting vaccinated against COVID-19 | 4.4 (3.6–5.3) |
Definition: CI: Confidence interval. Note: A total of 3,479 respondents provided a valid answer to this question. Footnotes:
|
|
The main reasons for Canadian adults to not get vaccinated against COVID-19 were due to concerns about the safety (22%) or effectiveness (11%) of COVID-19 vaccines. Similarly, the most commonly reported reason for being hesitant about getting vaccinated against COVID-19 was also concerns about the safety and/or side effects of COVID-19 vaccines (35%).
Additional doses of COVID-19 vaccines received after completing the primary series are called booster doses. Booster doses are important because they can increase protection by activating immune response to restore protection that may have decreased over time.Footnote 14 Overall, less than half of the vaccinated individuals (47%) had received a COVID-19 booster dose. The proportion of those having received a COVID-19 booster was much higher among seniors (78%) compared to younger adults without any chronic medical conditions (35%) (Table 7.2).
| Age group (years) | n | COVID-19 booster dose coverage, % (95% CI) |
|---|---|---|
| All adults ≥18 | 3,314 | 46.5 (44.5–48.5) |
| 18–64 with CMC | 681 | 44.1 (39.9–48.4) |
| 18–64 without CMC | 1,545 | 34.8 (32.2–37.5) |
| ≥65 | 1,073 | 77.6 (74.8–80.4) |
Definition: n: Number of respondents (unweighted). Note: A total of 3,317 respondents were vaccinated against COVID-19 and 3,314 respondents (99.9%) provided a valid answer for this question. Footnotes:
|
||
Among individuals who completed the primary series and never received a booster dose, 20% of them stated that they already booked an appointment for getting a booster dose and 50% stated that they were very likely to get one in the future. However, 10% of people were very unlikely to receive a booster dose (Table 7.3).
| Response | % (95% CI) |
|---|---|
| Very unlikely | 9.8 (8.1–11.5) |
| Somewhat unlikely | 8.6 (6.8–10.4) |
| Somewhat likely | 11.8 (9.9–13.7) |
| Very likely | 49.7 (46.7–52.7) |
| I already booked an appointment for my booster dose | 20.1 (17.9–22.4) |
Definition: CI: Confidence interval. Note: A total of 1,511 respondents did not receive a COVID-19 booster dose of which 1,471 respondents (97.4%) provided a valid answer for this question. |
|
Overall, the most commonly stated reasons for receiving a booster dose among individuals who were somewhat or very likely to receive a booster dose was to put an end to the pandemic (29%), and to protect themselves (16%) or their family members (24%) from COVID-19 (Table 7.4).
| Reason | % (95% CI) |
|---|---|
| 1. To put an end to the pandemic | 29.1 (25.5–32.7) |
| 2. To protect my family members from COVID-19 | 24.2 (20.8–27.7) |
| 3. To protect myself personally from COVID-19 | 15.6 (12.8–18.4) |
Definition: CI: Confidence interval. Note: A total of 863 respondents were somewhat or very likely to receive a booster dose of which 858 respondents (99.4%) provided a valid answer to this question. |
|
In comparison, among adults who were somewhat or very unlikely to receive a COVID-19 booster dose, the most important reason for not getting a booster dose was the perception of being well-protected after receiving the primary series (Table 7.5).
| Reason | % (95% CI) |
|---|---|
1. I am well protected after receiving two doses/being fully vaccinated |
17.9 (12.4–23.3) |
2. I have concerns about the safety and/or side effects of having a booster dose of a COVID-19 vaccine |
16.8 (11.3–22.3)Footnote a |
3. I think COVID-19 vaccines are not effective in protecting me from the virus |
13.7 (9.1–18.3)Footnote a |
Definition: CI: Confidence interval. Note: A total of 254 respondents were somewhat or very unlikely to receive a booster dose of which 247 respondents (97.2%) provided a valid answer to this question. Footnotes:
|
|
Additionally, when comparing COVID-19 booster dose uptake between individuals who were vaccinated against flu with those who were unvaccinated against flu this year, the proportion of adults who reported receiving a COVID-19 booster dose was higher among those who received a flu vaccine (70%) comparing to those who did not get vaccinated against flu (30%) (Table 7.6). Another study showed that those individuals who had received the seasonal influenza vaccine demonstrated higher intention to receive a COVID-19 vaccine.Footnote 15
| COVID-19 booster dose uptake | Influenza vaccination | |
|---|---|---|
| Vaccinated against flu % (95% CI) |
Unvaccinated against flu % (95% CI) |
|
| Received at least one booster dose | 69.9 (67.0–72.7) | 30.0 (27.6–32.4) |
| Never received a booster dose | 30.1 (27.3–33.0) | 70.0 (67.6–72.4) |
Definition: CI: Confidence interval. Note: A total of 3,304 respondents who provided a valid answer for COVID-19 booster dose uptake and influenza vaccination uptake were included in the analysis. |
||
Furthermore, the proportion of people who completed their primary series and reported being somewhat or very unlikely to receive a COVID-19 booster dose was lower among individuals who were vaccinated against flu this season (8%) compared to those who have not been vaccinated against flu (21%) (Table 7.7).
| COVID-19 booster dose intent | Influenza vaccination | |
|---|---|---|
| Vaccinated against flu % (95% CI) |
Unvaccinated against flu % (95% CI) |
|
| Very unlikely | 3.2 (1.4–4.9)Footnote a | 11.8 (9.6–13.9) |
| Somewhat unlikely | 5.2 (2.3–8.1)Footnote a | 9.6 (7.5–11.8) |
| Somewhat likely | 10.4 (6.2–14.6)Footnote a | 12.2 (10.0–14.3) |
| Very likely | 50.7 (44.7–56.8) | 49.3 (45.9–52.8) |
| I already booked an appointment for my booster dose | 30.4 (25.0–35.8) | 17.1 (14.6–19.5) |
Definition: CI: Confidence interval. Note: A total of 1,467 respondents who provided a valid answer for COVID-19 booster dose intent and influenza vaccination uptake were included in the analysis. Footnotes:
|
||
Discussion
According to the 2021–2022 Seasonal Influenza Vaccination Coverage Survey results, 39% of Canadian adults aged 18 years and older had received an influenza vaccine in the 2021–2022 season, which was similar to the 2020–2021 season (40%) and the 2019–2020 season (42%). Comparing to the most recent estimates in the United States, the flu vaccination coverage was 50.2% among adults aged 18 years and older during the 2020–2021 season.Footnote 16 In Canada, the reported influenza vaccination coverage for target groups at higher risk of severe influenza-related complications, including adults aged 18 to 64 years with chronic diseases (38%) and seniors aged 65 years and older (71%), remained below the national vaccination coverage goal of 80%.Footnote 1 Despite a higher vaccination uptake among seniors, which was closer to the target coverage goal of 80%, very little improvement has been achieved in recent years. Individuals unaware that they are considered at high risk of influenza-related complications may contribute to low coverage.Footnote 17
While most Canadian adults thought that vaccines are important for their health, an important proportion of the population falsely believed that the flu vaccine does not protect them from flu (35%) and that they can get the flu from the flu vaccine (38%). Future influenza vaccination promotion campaigns should strive to dispel the myth that flu vaccines can cause the flu, and increase the Canadian population's awareness of the importance and usefulness of influenza vaccines.
In addition, the majority of adults believed that it is a good thing for children (60%) or adults (55%) to get natural immunity (protection) against flu by being exposed to the virus. These proportions are higher than those who thought that it is a good thing for children (38%) or adults (36%) to get natural immunity against COVID-19 by being exposed to coronavirus. This could be due to higher COVID-19 risk perception as the outbreak of COVID-19 has been a major interrupting event.
Regarding COVID-19 vaccines, the majority of the population already got vaccinated against COVID-19. The survey revealed favourable attitudes toward COVID-19 booster dose with 47% of Canadian adults who already received a booster dose, and 20% who stated having already booked an appointment for a booster dose. Among those who had not received a booster dose, 50% stated they were very likely to receive a booster dose. However, there was still about one fifth of the population that did not intend to get a COVID-19 booster dose. Understanding and addressing their concerns is crucial to promoting COVID-19 booster uptake since they help people maintain strong protection.Footnote 14
More than one third of the population believed that it is a good thing for children (38%) or adults (36%) to get natural immunity against COVID-19 by being exposed to coronavirus. Despite previous COVID-19 infection or COVID-19 vaccination can both provide immunity and protection from the infection, some research suggest that COVID-19 vaccines are more effective at preventing hospitalization than a previous infection.Footnote 16 Although severe disease from COVID-19 is less frequent in healthy young adults than in older adults or those with chronic disease, severe and lasting symptoms of COVID-19 do occur in younger adults.Footnote 18 It is therefore important for them to get vaccinated against COVID-19.
While almost one third of the Canadian adults surveyed stated that they had encountered difficulties in scheduling an appointment for getting the flu vaccine this year due to the public health measures in place to reduce the spread of COVID-19, it did not seem to have a significant impact on flu vaccination coverage.
Strengths and limitations
The major strength of this survey was the timely reporting of seasonal influenza vaccination coverage across Canada. The timeliness of this survey allows Canada to meet its international reporting obligations and help identify priorities for future vaccination program planning. Additionally, the Seasonal Influenza Vaccination Coverage Survey is flexible in allowing question modules to be added or removed on an annual basis in light of changing priorities.
Limitations of this survey included the relatively low response rate of 15%. This response rate can increase the potential for non-response bias, as survey respondents may differ from those who chose not to complete the survey.
Additionally, survey respondents were interviewed within 6 months of the beginning of the seasonal influenza vaccination campaign to further mitigate recall bias. However, recall bias is less likely to occur for the COVID-19 vaccination related questions due to high media coverage surrounding the COVID-19 vaccination campaign and the proof of vaccination credentials issued by many jurisdictions across Canada. Moreover, it appears in some studies that self-reported influenza vaccination status is a valid measure of vaccine exposure when medical records or registry data are not available.Footnote 19
Conclusion
Seasonal influenza vaccination coverage in the 2021–2022 season (39%) was similar to previous seasons. Coverage in those at increased risk of influenza-related complications, namely seniors over 65 years of age (71%) and adults 18–64 years of age with a CMC (38%) remained below the national goal of 80%.
The most commonly reported reasons for influenza vaccination were to prevent infection or to avoid getting sick (40%), whereas the most common reason for non-vaccination against influenza was the perception that the vaccine was not necessary (23%).
It is especially important for Canadians to get the flu vaccine to reduce the morbidity and mortality associated with influenza, and to reduce any further pressure on the health care system during the COVID-19 pandemic. Ongoing efforts to promote and educate the adult population on the benefits of recommended vaccines is required in order to increase uptake, particularly among the population who are considered at high risk of severe complications. Continued efforts on understanding and identifying the factors influencing vaccination uptake are essential to develop effective strategies and interventions in order to improve vaccination coverage.
References
- Footnote 1
-
Public Health Agency of Canada. Flu (influenza): For health professionals. 2021.
- Footnote 2
-
Centers for Disease Control and Prevention (CDC). Key Facts About Seasonal Flu Vaccine. 2021.
- Footnote 3
-
Petrova VN, Russell CA. The evolution of seasonal influenza viruses. Nature Reviews Microbiology 2017;16:47-60.
- Footnote 4
-
Public Health Agency of Canada. Flu (influenza): For health professionals. 2021.
- Footnote 5
-
An Advisory Committee Statement (ACS) National Advisory Committee on Immunization (NACI). Canadian Immunization Guide Chapter on Influenza and Statement on Seasonal Influenza Vaccine for 2021–2022. 2021.
- Footnote 6
-
Public Health Agency of Canada. Public Health Agency of Canada. Vaccination Coverage Goals and Vaccine Preventable Disease Reduction Targets by 2025. 2021.
- Footnote 7
-
Léger. Seasonal Influenza Vaccination Coverage Survey, 2021–2022. 2022.
- Footnote 8
-
Public Health Agency of Canada. Seasonal Influenza (Flu) Vaccination Coverage Survey Results, 2019-2020. 2020.
- Footnote 9
-
Public Health Agency of Canada. Vaccine uptake in Canadian Adults 2021. 2021.
- Footnote 10
-
Buchan SA, Rosella LC, Finkelstein M, Juurlink D, Isenor J, Marra F, et al. Impact of pharmacist administration of influenza vaccines on uptake in Canada. CMAJ 2017 Canadian Medical Association;189(4):E146-E152.
- Footnote 11
-
World Health Organization. Barriers of influenza vaccination intention and behavior—A systematic review of influenza vaccine hesitancy 2005–2016. 2016:10.
- Footnote 12
-
Centers for Disease Control and Prevention (CDC). Misconceptions about Seasonal Flu and Flu Vaccines. 2022
- Footnote 13
-
Bozio CH, Grannis SJ, Naleway AL, et al. Laboratory-Confirmed COVID-19 Among Adults Hospitalized with COVID-19–Like Illness with Infection-Induced or mRNA Vaccine-Induced SARS-CoV-2 Immunity — Nine States. 2021. MMWR Morb Mortal Wkly Rep 2021;70:1539–1544.
- Footnote 14
-
Public Health Agency of Canada. Vaccines for COVID-19:How to get vaccinated. Booster doses. 2022
- Footnote 15
-
Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 21, 804 (2021).
- Footnote 16
-
Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). Flu Vaccination Coverage, United States, 2020–21 Influenza Season. 2021
- Footnote 17
-
Schoefer Y, Schaberg T, Raspe H, Schaefer T. Determinants of influenza and pneumococcal vaccination in patients with chronic lung diseases. J Infect 2007;55(4):347-52.
- Footnote 18
-
Johns Hopskins Medicine. Coronavirus and COVID-19: Younger Adults Are at Risk, Too. 2020.
- Footnote 19
-
King JP, McLean HQ, Belongia EA. Validation of self-reported influenza vaccination in the current and prior season. Influenza Other Respi Viruses 2018 07/20; 2018/08;0(0).