Supplemental Statement – Mammalian Cell Culture-Based Influenza Vaccines
Download the alternative format
(PDF format, 2.6 MB, 71 pages)
Organization: Public Health Agency of Canada
Published: 2020
Cat. : HP40-272-2020E-PDF
ISBN : 978-0-660-35644-0
Pub. : 200143
An Advisory Committee Statement (ACS)
National Advisory Committee on Immunization (NACI)
Table of contents
- Summary of information contained in this NACI statement
- I. Introduction
- II. Methods
- III. Vaccine
- IV. Discussion
- V. Recommendation
- Tables
- List of abbreviations
- Acknowledgments
- References
- Appendix A: PRISMA Flow Diagram
- Appendix B: Characteristics of Inlfuenza Vaccines Available For Use in Canada, 2020–2021
Preamble
The National Advisory Committee on Immunization (NACI) provides the Public Health Agency of Canada (PHAC) with ongoing and timely medical, scientific, and public health advice relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Over the coming years NACI will be refining methodological approaches to include these factors. Not all NACI Statements will require in-depth analyses of all programmatic factors. As NACI works towards full implementation of the expanded mandate, select Statements will include varying degrees of programmatic analyses for public health programs.
PHAC acknowledges that the advice and recommendations set out in this statement are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC’s Policy on Conflict of Interest, including yearly declaration of potential conflict of interest.
Summary of the information contained in this NACI supplemental statement
The following highlights key information for immunization providers. Please refer to the remainder of the Statement for details.
- What
Flucelvax® Quad is a mammalian cell culture-based, inactivated seasonal influenza vaccine that has recently been authorized for use in Canada in adults and children ≥9 years of age.
- Who
This supplemental statement addresses the annual influenza vaccination of adults and children who do not have contraindications for the influenza vaccine.
- How
Flucelvax® Quad may be considered among the quadrivalent influenza vaccines offered to adults and children ≥9 years of age for their annual influenza vaccination.
- Why
Flucelvax® Quad is considered effective, immunogenic, and safe in adults and children ≥9 years of age, and has a comparable immunogenicity and safety profile to egg-based influenza vaccines already licensed in Canada and Flucelvax®, which is a trivalent cell culture-based influenza vaccine that has been licensed in the United States, but for which licensure has never been sought in Canada. Flucelvax® Quad can provide broader protection against influenza B viruses when compared with trivalent influenza vaccines.
I. Introduction
Influenza is a viral infection that is estimated to cause approximately 12,200 hospitalizationsFootnote 1 and 3,500 deathsFootnote 2 in Canada annually. Influenza in humans is caused by two main types of influenza virus: A, which is classified into subtypes based on hemagglutinin (HA) and neuraminidase (NA) surface proteins, and B, which consists of two antigenically distinct lineages, B/Yamagata and B/Victoria. Seasonal influenza vaccines are either trivalent or quadrivalent formulations. Trivalent influenza vaccines contain two influenza A and one influenza B strain, and quadrivalent influenza vaccines contain the three strains included in trivalent vaccines and an additional influenza B strain from the other lineage of influenza B. Each year, the National Advisory Committee on Immunization (NACI) publishes a statement on seasonal influenza vaccines, which contains recommendations and guidance on the use of influenza vaccines for the upcoming influenza season.
Influenza vaccine production using mammalian cell culture-based technology is an innovative technique that may offer enhanced manufacturing scalability and sterility and, thus, a potentially valuable alternative to overcome some of the problems and vulnerabilities associated with egg-based productionFootnote 3,Footnote 4,Footnote 5,Footnote 6. Cell culture systems are more rapid, and robust, and produce yields with higher purity and a lower risk of production failure compared to standard egg-based manufacturing. The production timeline for the manufacturing of cell culture-based vaccines is more flexible compared to egg-based production because cells are frozen and banked, and virus amplification relies primarily on the capacity of bioreactorsFootnote 3,Footnote 4,Footnote 5. The use of cell-culture technology for the manufacturing of influenza vaccines offers the additional advantages of reduced microbial or chemical contamination due to a closed system of vaccine production. There is also potentially higher vaccine effectiveness relative to standard egg-based influenza vaccines due to insulation from egg-adaptive mutations changes, and there is potential for quicker large-scale production of vaccineFootnote 3,Footnote 4,Footnote 5,Footnote 6,Footnote 7. However, at the time of statement development, there is a lack of infrastructure and experience with the cell culture-based production platform for influenza vaccines and the resulting cost of these vaccines is typically greater compared to vaccines made using egg-based manufacturing.
Flucelvax® Quad (Seqirus, Inc.) is a mammalian cell culture-based quadrivalent inactivated, subunit influenza vaccine (IIV4-cc) that was authorized for use in Canada in adults and children 9 years of age and older on November 22, 2019Footnote 8. Flucelvax® Quad (also licensed as Flucelvax® Quadrivalent or Flucelvax® Tetra in other jurisdictions) is prepared from viruses propagated in mammalian cell lines [proprietary 33016-PF Madin-Darby Canine Kidney (MDCK) cell lines] adapted to grow freely in suspension in culture medium. The authorization of Flucelvax® Quad triggered the need for a supplemental NACI statement as it is the first and only available mammalian cell culture-based influenza vaccine in Canada, and NACI has not previously made a recommendation on cell culture-based influenza vaccines in any population.
Flucelvax® Quad builds on the clinical development of its trivalent predecessor, Flucelvax® (registered as Optaflu® in the European Union, Australia and Switzerland), a cell culture-grown, inactivated influenza vaccine developed by Novartis Vaccines and Diagnostics, Inc. (currently operating as Seqirus, Inc.). Flucelvax® was the first mammalian cell culture-derived inactivated influenza vaccine. It was approved for use in adults in Europe, under the trade name Optaflu®, from 2007 to 2017, and in the US under the trade name Flucelvax® since 2012. Originally, the same egg-derived candidate vaccine viruses (CVVs) used in egg-based manufacturing, but grown in cultured mammalian cells, were used in the production of Flucelvax®. On August 31, 2016, Seqirus, Inc. received approval from the US Food and Drug Administration (FDA) for the use of CVVs that had been isolated and propagated in MDCK cells for the manufacture of cell culture-based inactivated quadrivalent influenza vaccineFootnote 9. This approval enabled the production of completely cell-derived influenza vaccine viruses from the initial virus isolation through to the full manufacture of the vaccine. The Flucelvax® Quadrivalent vaccine (US product) for the 2017–2018 influenza season was the first vaccine to be manufactured from A(H3N2) CVVs produced exclusively using the cell-derived method, while the A(H1N1) and the B strain CVVs were egg-derived Footnote 4. For the 2018–2019 Flucelvax Quadrivalent vaccine, the A(H3N2) and B strain CVVs were derived from the mammalian cell line, while the A(H1N1) CVVs remained egg derived. The Flucelvax® quadrivalent formulation for the 2019–2020 influenza season was manufactured using CVVs for all four influenza viruses that were derived solely from mammalian cell lines. It has been hypothesized that propagation of CVVs in mammalian cells may improve vaccine effectiveness relative to licensed egg-based influenza vaccines by reducing the risk of antigenic drift and changes acquired in the HA of human influenza viruses during isolation, adaptation, and propagation in eggsFootnote 4,Footnote 6,Footnote 10.
Guidance Objective
The objective of this advisory committee supplemental statement is to review the evidence for efficacy, effectiveness, immunogenicity, and safety that is available for Flucelvax® Quad, and to provide guidance on its use in Canada in adults and children.
II. Methods
In brief, the broad stages in the preparation of a NACI Advisory Committee Statement are:
- Knowledge synthesis of the whole body of evidence on benefits and harms, considering the quality of the evidence and magnitude of effects observed.
- Translation of evidence into recommendations
Further information on NACI’s evidence-based methods is available in: Evidence-Based Recommendations for Immunization: Methods of the NACI, January 2009, CCDR.
A systematic literature review was conducted to accumulate evidence for NACI’s recommendations regarding the use of Flucelvax® Quad, which is licensed for adults and children ≥9 years of age in Canada. Mammalian cell culture-based influenza vaccines have been approved for use by the US FDA in adults and children 4 years or older since the 2013-2014 influenza season (6 years) and effectiveness, immunogenicity, and safety data is currently available for this age group. The systematic review methodology was developed with the NACI Influenza Working Group (IWG) and specified a priori in a written protocol that included review questions, search strategy, inclusion and exclusion criteria, and quality assessment.
Research question
What are the vaccine efficacy, effectiveness, immunogenicity, and safety of Flucelvax® Quad in persons 4 years of age and older?
- P (population):
- Children and adults (≥4 years of age)
- I (intervention):
- Mammalian cell culture-based influenza vaccine
- C (comparison):
- Egg-based, standard-dose quadrivalent inactivated influenza vaccine (IIV4-SD), trivalent, standard dose inactivated influenza vaccine (IIV3-SD), high-dose (IIV3-HD) or adjuvanted trivalent inactivated influenza vaccine (IIV3-Adj), mammalian cell culture-based trivalent inactivated, subunit influenza vaccine (IIV3-cc), placebo, or no comparator
- O (outcomes):
- Efficacy, effectiveness, immunogenicity, safety
The search strategy was developed based on the research question and PICO illustrated above, in conjunction with a librarian from the Health Library of Health Canada and PHAC (search strategy available upon request). The EMBASE, MEDLINE, Scopus, ProQuest Public Health, and ClinicalTrials.gov, electronic databases were searched for primary research articles and case reports from inception until February 12, 2019. Registered clinical trials and grey literature from international public health authorities and National Immunization Technical Advisory Groups were also considered. Searches were restricted to articles published in English and French due to the language proficiencies of the reviewers. Additionally, hand-searching of the reference lists of included articles was performed by one reviewer to identify additional relevant publications. Two reviewers independently screened the titles and abstracts of records retrieved from the database searches for potential eligibility. The full-texts of records deemed potentially eligible were obtained and further reviewed by both reviewers for potential inclusion in the review. Refer to Appendix A for the PRISMA Flow Diagram.
One reviewer extracted data from the studies included for review into an evidence table using a piloted data abstraction template designed to capture information on study design, population and outcomes of interest. A second reviewer independently validated the abstracted data with any disagreements or discrepancies resolved by discussion and consensus. The level of evidence (i.e. study design) and methodological quality of included studies was assessed independently by two reviewers using the design-specific criteria outlined by Harris et al.(2001)Footnote 11, which has been adopted by NACI for rating the internal validity of individual studies. Any disagreements or discrepancies in the data extraction and quality appraisal were resolved by discussion and consensus. The knowledge synthesis was performed by AS and JP, and was supervised by the Influenza Working Group (IWG).
Studies were included if they met the following criteria:
- The study population or subpopulation consisted of individuals ≥4 years of age; and
- Study assessed efficacy and effectiveness, immunogenicity, or safety of Flucelvax® Quad or safety of Flucelvax®
- Primary research studies from peer-reviewed scientific literature
- Case reports and case series
- Registered clinical trials and grey literature from international public health authorities
- Study is published in English or French
Studies were excluded if they met one or more of the following criteria:
- The study did not present data on any of: the efficacy, effectiveness, immunogenicity, or safety of Flucelvax® Quad, or the safety of Flucelvax®;
- The study is in a language other than English or French;
- The study is a non-human or in vitro study;
- The article is not a primary research study;
- The article is an editorial, opinion, commentary or news report;
- The article is an economic study, clinical practice guidelines, consensus conference, health technology assessment report; or
- The article was a doctoral dissertation, master’s thesis, or conference summary
Flucelvax® Quad has overlapping composition with Flucelvax® (the trivalent formulation) and is produced using the same MDCK manufacturing platformFootnote 12,Footnote 13. Therefore, studies that assessed the safety of Flucelvax® were also included in this literature review post hoc to supplement the evidence base for the safety outcome. Specialty trivalent vaccines (i.e., high-dose trivalent inactivated influenza vaccine (IIV3-HD) and adjuvanted trivalent inactivated influenza vaccine (IIV3-Adj) were also added as comparator vaccines post hoc, since these comparisons would originally have been excluded as there is currently no comparable quadrivalent formulation of these vaccines.
Development of Recommendations
Following critical appraisal of individual studies, summary tables with ratings of the quality of the evidence using NACI's methodological hierarchy (Table 4 and 5) were prepared, and proposed recommendations for vaccine use were developed. The evidence and proposed recommendations were discussed by the IWG in July 2019 and the NACI Vaccine Safety Working Group in August 2019. The IWG Chair and the Public Health Agency of Canada (PHAC) technical advisor (AS) presented the evidence and proposed recommendations to NACI on September 25, 2019. Following thorough review of the evidence, NACI approved the recommendation contained in this statement on December 16, 2019. The description of relevant considerations, rationale for specific decisions, and knowledge gaps are described in the following sections.
III. Vaccine
III.1 Mammalian Cell Culture-Based Influenza Vaccine Preparation Authorized for Use in Canada
Flucelvax® Quad is a subunit influenza vaccine prepared from CVVs isolated and propagated in a MDCK cell line. It is authorized for intramuscular (IM) injection and is available as a 0.5 mL single-dose, pre-filled syringe without a needle, and as a 5 mL multi-dose vial containing 10 doses (each dose is 0.5 mL). For more information on Flucelvax® Quad, refer to the product monographFootnote 8.
| Route of Administration | Dosage | Non-medicinal Ingredients |
|---|---|---|
| Intramuscular | Each 0.5 mL dose contains 15 μg of hemagglutinin (HA) of each of the four influenza virus strains contained in the vaccine. | Disodium phosphate dihydrate, magnesium chloride hexahydrate, potassium chloride, potassium dihydrogen phosphate, sodium chloride, thimerosal (multi-dose vial only) and water for injection. Each dose may also contain residual amounts of: |
III.2 Vaccine Efficacy and Effectiveness
No efficacy studies for Flucelvax® Quad were identified and studies evaluating the efficacy of Flucelvax® were beyond the scope of this review.
Four studies, two peer-reviewed and two not peer-reviewed were identified that assessed the effectiveness of Flucelvax® QuadFootnote 14,Footnote 15,Footnote 16,Footnote 17. Of these four studies, two were of good qualityFootnote 15,Footnote 16, while the quality of the other two studiesFootnote 14,Footnote 15,Footnote 16,Footnote 17 could not be assessed because they were published as conference abstracts or posters. Common concerns relating to the quality of evidence included potential residual or unmeasured confounding even after statistical adjustmentsFootnote 14,Footnote 15,Footnote 16,Footnote 17 and exposure and outcome misclassificationFootnote 14,Footnote 15,Footnote 16. The following section outlines the key effectiveness findings from all these studies; additional details regarding study characteristics and results are shown in Table 6.
III.2.1 Effectiveness against Influenza Infection
Two studies assessed the vaccine effectiveness (VE) of IIV4-cc compared to egg-based IIV against laboratory-confirmed influenza infection during the 2017–2018 influenza season in the USA. The first was a peer-reviewed study by DeMarcus et al. (2019), which used test-negative case-control design and was conducted by the US Department of Defense Global Respiratory Pathogen Surveillance ProgramFootnote 15. The DeMarcus et al. (2019) study included Department of Defense (DoD) healthcare beneficiaries (excluding service members) 6 months–94 years of age (median age: 13 years) who presented to a military treatment facility with symptoms of influenza-like illness (ILI) and had a respiratory specimen collected between October 1st 2017–April 28 2018. Individuals testing positive for influenza by reverse transcription polymerase chain reaction (RT-PCR) or viral culture, were classified as cases, while influenza-negative individuals were classified as controlsFootnote 15. The second study by Klein at al. (2018), which was not peer-reviewed, is a retrospective cohort analysis of VE against PCR-confirmed influenza A(H3N2) influenza virus infection among Kaiser Permanente Northern California members aged 4–64 years Footnote 17.
The results from the study by DeMarcus et al. (2019) indicated that the odds of having any laboratory-confirmed influenza infection were not statistically significantly different between individuals who had received IIV4-cc and those who received egg-based IIV (trivalent or quadrivalent formulation). The authors conducted sub-analyses by influenza subtype and by age group, and found that the odds of having influenza A(H1N1)pdm09 infection were higher overall for all DoD dependents (odds ratio [OR]: 2.0; 95% CI: 1.1–3.6 %) and for children (OR: 2.9; 95% CI: 1.3–6.3%) who received the IIV4-cc compared to those that received an egg-based IIV Footnote 15. The odds of having influenza A(H3N2) infection appeared to be lower overall and for adults who received the IIV4-cc compared to egg-based IIV, but the results did not reach statistical significanceFootnote 15. All other estimates showed no statistically significant difference between the two vaccine typesFootnote 15.
The results from the study by Klein et al. indicated that both IIV4-cc and egg-based IIV [trivalent (received by 86.2% of members) or quadrivalent formulation] had relatively low effectiveness with respect to the risk of laboratory-confirmed influenza during the 2017–2018 influenza season. The authors found no statistically significant difference in VE against laboratory-confirmed influenza A infection between individuals vaccinated with IIV4-cc versus egg-based IIV (adjusted rVE: 6.8%; 95% CI: -11.2–21.9%; P=0.43)Footnote 17. The adjusted absolute VE for subjects vaccinated with IIV4-cc was 30.2% (95% CI: 17.1–41.3%; P<0.0001) and 17.9% (95% CI: 12.1–23.3%; P<0.0001) for subjects vaccinated with either egg-based IIV4 or IIV3Footnote 17.
III.2.2 Effectiveness against Influenza-Related Health Care Interactions
One study by Izurieta et al. (2018) assessed the VE of IIV4-cc compared to 4 other egg-based influenza vaccines (egg-based, standard-dose quadrivalent IIV (IIV4-SD), egg-based IIV3, egg-based IIV3-Adj, and egg-based IIV3-HD) in preventing influenza-related health care interactions (i.e. office visits and hospital encounters). Influenza-related office visits were defined as community-based visits to physicians’ offices and hospital outpatient visits in which a rapid influenza test was performed by the healthcare provider and a therapeutic course of oseltamivir (75 mg twice daily for 5 days) was prescribed within 2 days following the testFootnote 16. Hospital encounters were defined as inpatient hospitalizations and emergency department visits in which International Classification of Diseases (ICD), Tenth revision, Clinical Modification, code for influenza was listed. This retrospective cohort study made use of electronic medical records (EMRs) providing data on enrolment in fee-for-service Medicare parts A and B in the 6 months before vaccination, inpatient and outpatient care, physician office visits, and prescription drugs for Medicare beneficiaries ≥65 years of age who received an influenza vaccine during the 2017–2018 influenza season(16). Estimates were adjusted using inverse probability of treatment weighting, and weights were derived from propensity scoresFootnote 16. Relative vaccine effectiveness (rVE) was defined as the difference in influenza-related hospital encounters between persons vaccinated with IIV4-cc versus egg-based vaccines.
In a 2-way comparison, IIV4-cc was statistically significantly more effective against office visits (rVE): 10.5%; 95% CI: 6.8%–14.0%) and hospital encounters (rVE: 10.0%; 95% CI: 7.0%–13.0%) than egg-based, IIV4-SDFootnote 16. In an analysis comparing this vaccine to four other egg-based formulations, IIV4-cc was statistically significantly (P≤0.05) more effective against office visits compared to egg-based IIV4-SD and IIV3-Adj, and against inpatient stays and hospital encounters, compared to egg-based IIV3-SD, IIV4-SD, and IIV3-AdjFootnote 16. In addition, IIV4-cc was statistically significantly more effective against office visits compared to egg-based IIV3-HD, but not against inpatient visits or hospital encountersFootnote 16.
III.2.3 Effectiveness against Influenza-Like Illness
One study that was recently accepted for publication assessed the effectiveness of Flucelvax® Quadrivalent for the prevention of ILIFootnote 14. Boikos et al. (2018) conducted a retrospective cohort study in the US during the 2017–2018 influenza season to determine the relative VE (rVE) of Flucelvax® Quadrivalent to standard-dose quadrivalent egg-based inactivated influenza vaccines against ILI [as defined by the Armed Forces Health Surveillance Centre (AFHSC) ICD Code Set B]Footnote 18 in individuals ≥4 years of ageFootnote 14. The rVE estimates were based on real-world primary care data from the EMRs of individual patients 4 years of age and older who were vaccinated with either Flucelvax® Quadrivalent (n= 92,192) or egg-based IIV4-SD (n=1,255,983). Results demonstrated that Flucelvax® Quadrivalent was statistically significantly more effective than egg-based IIV4-SD in preventing ILIFootnote 14. The estimate for rVE against ILI was 36.2% (95% CI: 26.1–44.9%; P<0.001) after adjusting for differences in age, sex, health status, and geographic region between the two exposure groupsFootnote 14. The result from a sensitivity analysis using propensity scores was consistent in terms of direction and statistical significance compared to the adjusted estimate (propensity-score matched rVE: 19.3%; 95% CI: 9.5–28.0%)Footnote 14. When stratified by age, however, Flucelvax® Quadrivalent was statistically significantly more effective than egg-based IIV4-SD in preventing ILI in adults aged 18–64 years (propensity-score matched rVE: 26.8%; 95% CI: 14.1–37.6%; P<0.001), but did not reach statistical significance in children 4-17 years of age (propensity-score matched rVE: 18.8 %; 95% CI: -53.9-57.2%) or adults 65 years of age or older (propensity-score matched rVE: -7.3 %; 95% CI: -51.6-24.0%)Footnote 14.
III.3 Immunogenicity
Regulators in Canada, the US, and Europe accept non-inferiority immunogenicity trials that compare the hemagglutination inhibition (HI) antibody response of the new vaccine to that of an existing licensed vaccine, or placebo-controlled immunogenicity trials that assess the HI antibody response to the new vaccine. Non-inferiority and placebo-controlled immunogenicity trials are often considered sufficient by regulatory authorities when there are bridging data to correlate immunogenicity outcomes to clinical protection, or when the new vaccines are considered by the regulators to be very similar to vaccines already authorized. Serological assessments based on the geometric mean titres (GMTs) of HI antibody that are used by regulators are: GMT ratio, seroprotection rate, and seroconversion rate. The FDA has published definitions for these serological assessments and criteria for immunogenicity data necessary for influenza vaccine licensureFootnote 19. These definitions and currently used criteria are shown in Table 2. Correlates of protection that are not based on HI antibody titres have not been well established.
Two studiesFootnote 20,Footnote 21 that assessed the immunogenicity of Flucelvax® Quad compared to different IIV3-cc (Flucelvax, Seqirus, Inc.) formulations were identified in this review; one study by Bart et al. (2016) was conducted with adult subjects 18 years of age and older, while the other study by Hartvickson et al. (2015) focused on pediatric subjects 4 to 17 years of age. Additional details on the immunogenicity findings from these studies are shown in Table 7. The adult randomized controlled trial (RCT) was of good quality overall. One methodological concern identified was that the study did not examine the subjects’ vaccination history from previous seasons. The pediatric study was of fair quality, as subjects’ HI titre was measured at different times, depending on whether the subject had been vaccinated previously or not.
Although no studies that assessed the immunogenicity of Flucelvax® Quad compared to egg-based IIV (trivalent or quadrivalent) were identified, non-inferiority of its trivalent predecessor, Flucelvax®, compared to egg-based IIV3 has been established in adult and pediatric subjectsFootnote 22,Footnote 23,Footnote 24,Footnote 25.
III.3.1 Immunogenicity in Adults
Bart et al. (2016) conducted a Phase III, double-blind, RCT study to assess the immunogenicity of Flucelvax Quad compared to two IIV3-cc (Flucelvax®; Seqirus), which contained either an influenza B/Victoria or B/Yamagata lineage strain, in healthy adults ≥18 years of ageFootnote 20. The study compared the GMT ratio, seroprotection rate, and seroconversion rate in the control and intervention groups 22 days after vaccinationFootnote 20. Flucelvax® Quad demonstrated non-inferiority to the two IIV3-cc in the HI antibody responses against influenza A(H1N1), A(H3N2), and the B lineage contained in the trivalent vaccines, based on GMT ratio and seroconversion rates. Flucelvax Quad demonstrated superiority for the influenza B lineage that was not included in the IIV3-ccFootnote 20. In a sub-analysis, Flucelvax® Quad also met the threshold for non-inferiority based on seroprotection rate for adults 18–64 years of age and ≥65 years of ageFootnote 20.
III.3.2 Immunogenicity in Children
Hartvickson et al. (2015) conducted a RCT study comparing the immunogenicity of Flucelvax® Quad to two formulations of IIV3-cc (Flucelvax®), containing either an influenza B/Victoria or B/Yamagata strain, in healthy children 4–17 years of ageFootnote 21. Children <9 years of age who were not previously vaccinated received two doses of influenza vaccine (n=694)Footnote 21. The study compared the GMT, seroprotection rate, and seroconversion rate in the control and intervention groups on day 22 post-vaccination for those who had been previously vaccinated and on day 50 for those that had not been previously vaccinatedFootnote 21. Flucelvax® Quad met non-inferiority criteria for all four influenza strains contained in the IIV3-cc vaccines in healthy children aged 4–17 yearsFootnote 21. Flucelvax® Quad also demonstrated superiority for both influenza B strains over the unmatched B lineage included in the comparator IIV3-ccFootnote 21. Flucelvax® Quad also met the threshold for seroprotection for all strainsFootnote 21.
The immunogenicity for Flucelvax® Quad is supported by evidence from the clinical development program for Flucelvax® (trivalent formulation), which has been licensed in the US and produced using the same MDCK manufacturing platform Footnote 36,Footnote 37,Footnote 38,Footnote 39. Flucelvax® has demonstrated non-inferiority to standard egg-based IIV3 comparators, including Agrippal® (Seqirus; marketed in Canada as Agriflu®) and Fluvirin® (GSK), for HI antibody responses overall to any strain in adults ≥18 years of age and for A(H1N1) and B strains specifically, but not A((H3N2), for persons 4 to 17 years of age, based on post-vaccination GMT ratios and seroconversion rates Footnote 22,Footnote 23,Footnote 24,Footnote 25.
III.4 Safety
This review identified two peer-reviewed studiesFootnote 20,Footnote 21 that assessed the safety of Flucelvax® Quad; both studies were RCTs with one focused on healthy adultsFootnote 20 and the other on healthy childrenFootnote 21. For both of these studies, the safety outcomes assessed included solicited local and systemic adverse events (AE) from day 1–7 post-vaccination, serious adverse events (SAE) through 6 months after the last vaccination, and unsolicited AEs from day 1–23 post-vaccination. No studies that assessed the safety of Flucelvax® Quad compared to egg-based IIV (trivalent or quadrivalent) were identified in this review.
Flucelvax® Quadrivalent has been licensed in the US for use in adults and children 4 years or older in since 2016. Since authorization, no safety signals have been identified through routine pharmacovigilance. AE that have been reported during post-licensure use of Flucelvax® Quadrivalent in the US include, allergic or acute hypersensitivity reactions, nervous system disorders (syncope, presyncope, paresthesia), generalized skin reactions (pruritus, urticaria or non-specific rash), and extensive swelling of injected limb. However, a reliable estimate of the frequency of these reactions is not available and no definitive causal link to vaccination with Flucelvax® Quadrivalent has been established.
In addition, six peer-reviewed clinical studiesFootnote 3, Footnote 26,Footnote 27,Footnote 28,Footnote 29,Footnote 30and one clinical review of casesFootnote 31 that assessed the safety of Flucelvax® were included in this review, four of which assessed safety in adults and two of which assessed safety in children. The safety evidence for Flucelvax® (trivalent) was considered relevant, as although licensure for Flucelvax® has never been sought in Canada, Flucelvax® and Flucelvax® Quad have overlapping compositions and are produced using the same MDCK manufacturing platform. In addition to these six published studies, it should be noted that Flucelvax® has an established record of safety in other jurisdictions, and no new safety signals have been identified through routine pharmacovigilance in the USA or Europe where the vaccine has been licensedFootnote 22,Footnote 23,Footnote 31.
Additional details on the safety evidence presented in this review are shown in Table 8. No published clinical data pertaining to safety of vaccination with IIV4-cc or IIV3-cc during pregnancy is currently available to inform vaccine-associated risks.
III.4.1 Adverse Events in Adults
Bart et al. (2015) assessed the safety of Flucelvax® Quadrivalent in healthy adults 18–64 years of age and older adults ≥65 years of age compared to two IIV3-cc produced using the same cell culture-based manufacturing processFootnote 20. Across the three vaccine groups, a similar proportion of adults reported at least one solicited AE. The reported solicited local and systemic AE were generally mild to moderate in intensity, self-limited, and did not precipitate sequelae. There were also no major differences in the percentages of all adults (≥18 years of age) who reported unsolicited AE [IIV4-cc: 16.1%; IIV3-cc (B/Yamagata): 14.7%; IIV3-cc (B/Victoria): 16.5%]. Subgroup analyses based on age, sex, and race or ethnicity did not reveal any major variations in the AE profiles of the three vaccine groups in this study.
Solicited adverse events
Injection site pain was the most common solicited AE and was reported by 33.6% of adults in the IIV4-cc group, 27.8% in the IIV3-cc (B/Yamagata) group, and 29.4% in the IIV3-cc (B/Victoria) groupFootnote 20. Although a slightly higher percentage of adults (0.2%) in the IIV4-cc group reported severe pain compared to the IIV3-cc groups (0.1%), the proportion of adults experiencing other solicited local AE was comparable between the different groups overallFootnote 20. Notably, one case of severe ecchymosis and one case of severe induration were identified after vaccination with IIV3-cc (B/Yamagata)Footnote 20. Fatigue and headache were the most common solicited systemic AE experienced by adults in this studyFootnote 20. Within the IIV4-cc group, 13.5% of subjects reported fatigue and 14.0% reported headaches. A similar proportion of adults in the IIV3-cc groups experienced fatigue (IIV3-cc (B/Yamagata): 16.3%; IIV3-cc (B/Victoria): 12.2%) and headaches (IIV3-cc (B/Yamagata): 13.4%; IIV3-cc (B/Victoria): 13.4%)Footnote 20. The incidence of severe systemic AEs was very low (<1%) overallFootnote 20. Only 15 subjects across the three vaccine groups reported experiencing fever following vaccination; however, the fever did not exceed 40°C in any of these casesFootnote 20. Across studies that assessed the safety of IIV3-cc compared to egg-based IIV3 Agrippal® (marketed in Canada as Agriflu®), pain and redness at the injection site were the most common local adverse reactions, while headache, myalgia, malaise, and fatigue were the most common systemic adverse reactions observed across the different age groupsFootnote 27,Footnote 28,Footnote 29. Overall, the local and systemic solicited reactions as well as unsolicited AE and SAE were comparable to those typically observed with other injectable influenza vaccinesFootnote 27,Footnote 28,Footnote 29. None of the deaths or SAEs reported over the course of these IIV3-cc studies were assessed as vaccine related Footnote 27,Footnote 28,Footnote 29.
Unsolicited adverse events and serious adverse events
The percentages of unsolicited AEs and medically attended AEs in the Bart el. al study were somewhat higher in adults ≥65 years of age compared to adults 18–64 years of age; however, these two age groups demonstrated a similar incidence of possibly vaccine-related AEs. New onset of chronic diseases (NOCD), specifically metabolic and nutritional disorders, cardiac disorders, and musculoskeletal and connective tissue disorders, were reported by 4.4% of study participants; however, there were no significant differences between vaccine groups or age groupsFootnote 20. No indication of new onset of neurologic disorders, increased frequency of specifically monitored SAEs, or other safety signals was identified among IIV4-cc recipientsFootnote 20. Over the course of this study, 12 deaths were reported (5 in the IIV4-cc group and 7 in the IIV3-cc groups) Footnote 20. The proportion of participants who died during the course of the study was similar across vaccine groups in both the 18–64 age group (IIV4-cc: 0%; IIV3-cc (B/Yamagata): 0%; IIV3-cc (B/Victoria): 0.3%) and the ≥65 age group (IIV4-cc: 0.8%; IIV3-cc (B/Yamagata): 1.5%; IIV3-cc (B/Victoria): 0.3%). None of the SAEs orAEs leading to premature withdrawal or deaths were considered to be vaccine-related by the sponsorFootnote 20. The proportion of adults who experience unsolicited AEs and SAEs were comparable to those typically observed with other injectable influenza vaccinesFootnote 20. This review also identified a case report of a 55-year-old woman with multiple comorbidities, who developed optic neuropathy and severe visual impairment in the right eye following vaccination with Flucelvax®Footnote 32. In this case, progressive unilateral optic neuritis occurred secondary to a systemic reaction involving a wide range of symptoms that began two days after influenza vaccinationFootnote 32. However, it should be noted that there was no definitive link established between this very rare serious adverse reaction and vaccination with IIV3-ccFootnote 32.
A clinical review of post-licensure surveillance data from the Vaccine Adverse Event Reporting System (VAERS), which closely monitors anaphylaxis events related to newly licensed vaccines prerecommended for use in the US, found that the crude reporting rate for hypersensitivity reactions among reports of AEs in adults aged ≥18 years who were vaccinated with Flucelvax® (IIV3-cc) during the first two influenza seasons of distribution (2013–2014 and 2014–2015) was similar to or less than what has been observed for other influenza vaccines (12.7 cases per million doses distributed)Footnote 31. Two reports of anaphylactic reactions were identified; one report met Brighton Collaboration criteria level 2, and the second report did not meet Brighton criteria but was diagnosed by the attending physician as an anaphylactic reaction. Notably, a causal association with IIV3-cc has not been established for these two anaphylaxis reports. The crude reporting rate for anaphylaxis over these 2 years was 0.4 per million doses distributed; however, estimates for crude reporting rates for hypersensitivity reactions and anaphylaxis should be interpreted with caution given the uncertainties regarding the completeness, quality, and consistency of the data reported to VAERS and the use of doses distributed as a denominatorFootnote 31.
III.4.2 Adverse Events in Children
Hartvickson et al. (2015) assessed the safety of Flucelvax® Quad in healthy children aged 4–18 years of age compared to two IIV3-cc (Flucelvax®): one containing an influenza B/Yamagata lineage and one containing a B/Victoria lineage. Most solicited adverse reactions among those receiving Flucelvax® Quad were mild in severity, and all resolved within a few days without sequelaeFootnote 21. The rates and types of unsolicited AEs in children who received IIV4-cc or a comparator IIV3-cc were comparable to those typically seen with routine childhood vaccinations Footnote 21.
Solicited adverse events
Across all vaccine groups in the Hartvickson et al. (2015) study, the most common solicited local AE was tenderness for children 4–5 years of age, and injection-site pain for children 6–8 and 9–17 years of ageFootnote 21. The proportion of children who experienced solicited local AEs were similar for the intervention and control groups across all agesFootnote 21. The largest difference in proportion between vaccine groups was for children 4–5 years of age reporting local AEs; 53% of children in the IIV4-cc group reported unsolicited local AEs compared to 44% and 36% in the IIV3-cc (B/Yamagata) and IIV3-cc (B/Victoria) groups respectivelyFootnote 21. For children <9 years of age who received a second dose, the proportions of solicited local AEs were also similar across study groupsFootnote 21. In general, of the children that received two doses, there was a higher proportion of local AEs after the first dose compared to the secondFootnote 21. The most common solicited systemic AEs were sleepiness for children 4–5 years of age, fatigue for children 6–8 years of age, and headache for children 9–17 years of age across all vaccine groupsFootnote 21. Among children 6–8 years of age, the proportion of children who reported solicited systemic AEs was generally higher after the first vaccination compared to the second vaccination. However, children 4–5 years of age demonstrated a 1–3% increase in the percentage of solicited systemic AEs after the second vaccine dose in each of the vaccine groupsFootnote 21.
Two studiesFootnote 26,Footnote 30 that assessed the safety of IIV3-cc compared to a standard egg-based IIV3 (Fluvirin®; licensed in the US but not available in Canada) in healthy children were identified in this review. Vesikari et al. (2012) found that the most common local AE among children 3–8 and 9–17 years of age was injection site pain, and the most common systemic AE were myalgia and headache Footnote 26. Nolan et al. (2016) assessed the safety of IIV3-cc in healthy children and adolescents 4-17 years of age stratified into two cohorts (4–8 year-olds and 9–17 year-olds)Footnote 30. Children 4-8 years of age who were not previously vaccinated received two doses of influenza vaccineFootnote 30. The proportion of children in the 4-8 year-old age group who were not previously vaccinated and experienced solicited local and systemic AEs was similar for the intervention and control groups after the second vaccinationFootnote 30. For previously vaccinated children 4-17 years of age who received a single dose, the proportions of solicited local AEs were similar to not previously vaccinated children 4-8 years of ageFootnote 30. Overall, no important differences in safety outcome were identified between children who had received the IIV3-cc and the egg-based IIV3 Footnote 26,Footnote 30.
Unsolicited adverse events and serious adverse events
The proportion of reported unsolicited AE was similar in the three vaccine groups in the Hartvickson et al. (2015) study, and ranged from 24–27%Footnote 21. Approximately 1% of children 4–17 years of age experienced any SAE in all study groupsFootnote 21. New onset of chronic diseases was reported in 2% of study participants in each of the vaccine groupsFootnote 21. No deaths were reported over the course of the study and none of the SAEs were considered to be related to the vaccineFootnote 21.
Vesikari et al. (2012) and Nolan et al. (2016) assessed the safety of IIV3-cc compared to egg-based IIV3 (Fluvirin). Unsolicited AEs occurred in 1-4% of subjects across age and vaccine groups in the Vesikari et al. (2012) study and 0 to <1% were considered at least possibly related to the study vaccines. There were no deaths reported over the course of Vesikari et al. (2012) study and none of the 28 SAEs (4 during the post-vaccination period, 24 during the 6-month safety follow-up period) documented in the study were assessed as vaccine related. No deaths or vaccine-related SAEs were reported in Nolan et al. (2016) study and one of the withdrawals from the study was due to a non-serious AE.
IV. Discussion
The present systematic review examined studies investigating the effectiveness, immunogenicity, and safety of Flucelvax® Quad, the first mammalian cell culture-based seasonal influenza vaccine to be approved for adult and pediatric use in Canada. The peer-reviewed published evidence on the effectiveness of Flucelvax® Quad manufactured from CVVs produced solely using the cell-derived method is sparse. Four observational VE studies, two peer-reviewed and two not peer-reviewed, were identified in this review. There was some data indicating that Flucelvax® Quad may potentially offer improved protection against influenza compared to egg-based IIV4 or IIV3, particularly against A(H3N2) virus infection. However, interpretation of the data from these observational studies is limited as all the analyses were conducted using data only from the 2017–2018 influenza season in the US, which was influenza A(H3N2)-dominant. Furthermore, two of the retrospective studiesFootnote 14,Footnote 16,Footnote 16 evaluating VE utilized real-world primary care data from the EMRs of individual patients. This approach for influenza VE estimation has not yet been validated and the potential sources of bias and confounding still need to be further investigated.
Two RCTs conducted in adults and children 4 years of age and olderFootnote 20,Footnote 21 that specifically assessed the immunogenicity and safety of Flucelvax® Quad were identified in this review. However, both studies used Flucelvax® IIV3-cc (produced by Seqirus using the same cell culture-based manufacturing process) as the comparator and were conducted during the 2013–2014 influenza season, which was prior to the FDA’s supplemental approval for the use of CVVs that had been isolated and propagated in MDCK cells for the manufacture of cell culture-based influenza vaccines. In both studies, Flucelvax® Quad demonstrated non-inferiority, based on GMT ratio and seroconversion rates, and met the threshold for seroprotection for all influenza strains contained in the IIV3-cc vaccines. The immunogenicity evidence for Flucelvax® Quad builds on the clinical development program of Flucelvax® IIV3-cc, noting that authorization for Flucelvax® (trivalent) has never been sought in Canada. Flucelvax® has demonstrated non-inferiority to licensed egg-based IIV3 comparators in for all strains in adults ≥18 years of age and A/H1N1 and B strains but not the A/H3N2 influenza strain for persons 4 to 17 years of age. Notably, Flucelvax® IIV3-cc was manufactured using egg-derived CVVs prior to the implementation of manufacturing methods using CVVs solely derived from MDCK cells.
This review also examined studiesFootnote 3, Footnote 26,Footnote 27,Footnote 28,Footnote 29,Footnote 30 that assessed the safety of Flucelvax®, which is a trivalent vaccine produced using the same cell culture-based manufacturing platform, to supplement the evidence base for safety. These studies found that IIV-cc are a safe, well-tolerated, and immunogenic alternative to conventional egg-based influenza vaccines for children and adults. There is a theoretical concern that inactivated influenza vaccines produced in canine kidney cells (MDCK 33016-PF) may cause adverse reactions in individuals with dog allergy. This issue has been investigated in two in vitro studies, which used biological assays to evaluate the potential allergenicity of MDCK cell-based vaccines Footnote 33,Footnote 34. The results of these studies suggest that influenza vaccines produced in MDCK cells do not have the potential to trigger hypersensitivity reactions in individuals with documented allergies associated with dogs. In addition, there has been no signal of an elevated risk of severe allergic reactions as compared to egg-based influenza vaccines identified through IIV-cc clinical trials or post-market safety surveillanceFootnote 33,Footnote 34.
Influenza vaccine production using mammalian cell culture-based technology may offer enhanced manufacturing scalability, sterility, timeliness, and flexibility compared to traditional egg-based manufacturing platforms. Implementation of cell culture-based influenza vaccine technologies and other alternatives to egg-based methods will also enable diversification of vaccine manufacturing platforms to overcome influenza vaccine supply vulnerabilities and improve vaccine-production capacity. Additionally, research has indicated that influenza A(H3N2) viruses can undergo changes that decrease antigenic relatedness to wild-type, circulating viruses when they are grown in eggs, and that certain egg-adaptive mutations may negatively affect the immunogenicity, efficacy, and effectiveness of standard egg-based influenza vaccines, especially during influenza A(H3N2)-dominant seasonsFootnote 4,Footnote 10,Footnote 35,Footnote 36,Footnote 37,Footnote 38,Footnote 39. Cell culture-based influenza vaccines solely derived from cell culture-based CVVs are insulated from such egg-adaptive changes and have the potential to provide enhanced protection in some seasons compared to standard egg-based influenza vaccinesFootnote 3,Footnote 6,Footnote 10. Nevertheless, adaptation in cell culture-based influenza vaccines needs to be further investigated given the potential for mutations in the genetic segments of HA and NA proteins resulting of serial passaging in MDCK cells Footnote 40,Footnote 41.Therefore, ongoing monitoring of vaccine effectiveness, immunogenicity, and safety will be important to compare prior and future seasons, across influenza subtypes, and overall VE for each vaccine type. A more robust, comprehensive and consistent body of evidence, including data on comorbidities, pregnant women, health status, and other potential confoundersFootnote 42, is also needed to evaluate the relative effectiveness and safety of Flucelvax® Quad compared to other injectable influenza vaccines.
V. Recommendation
The following section outlines the recommendation that NACI has made regarding the use of Flucelvax® Quad in adults and children. Additional information on the strength of NACI recommendations and the grading of evidence is available in Table 3.
The following recommendation for Flucelvax® Quad supplements NACI’s overarching recommendation for influenza vaccination, which is available in the NACI Seasonal Influenza Vaccine Statement. The overarching NACI recommendation for influenza vaccination is that an age appropriate influenza vaccine should be offered annually to anyone 6 months of age and older (Strong NACI Recommendation), noting product-specific contraindications.
- NACI recommends that Flucelvax® Quad may be considered among the IIV4 offered to adults and children ≥9 years of age (Discretionary NACI Recommendation)
- NACI concludes that there is fair evidence to recommend vaccination of adults and children ≥9 years of age with Flucelvax® Quad (Grade B Evidence).
Summary of Evidence and Rationale
- There is fair evidence that Flucelvax® Quad is effective, safe, and has non-inferior immunogenicity to comparable vaccines, based on direct evidence in adults and children ≥9 years of age.
- There is limited peer-reviewed evidence on the effectiveness, immunogenicity, and safety of Flucelvax® Quad manufactured using fully cell-derived viruses.
- There is some evidence that, overall, Flucelvax® Quad may be more effective than egg-based trivalent or quadrivalent influenza vaccines against non-laboratory confirmed influenza-related outcomes but there is insufficient evidence for laboratory-confirmed outcomes. The clinical significance and directness of the evidence provided by influenza-related outcomes, which are surrogate measures of influenza activity, and the validity of observational studies using EMRs for influenza vaccine effectiveness estimation remain uncertain and need to be further evaluated
- Although some data suggests that IIV4-cc may be more effective against laboratory-confirmed influenza A(H3N2) virus infection than egg-based IIV, there was no consistent and statistically significant difference in effectiveness identified for adults or children vaccinated with IIV4-cc compared to egg-based IIV. Therefore, no firm conclusions can be drawn at this time, and NACI will continue to monitor this issue.
- All studies that assessed effectiveness were conducted in the US during the same season (2017–2018), which was influenza A(H3N2)-dominant. As influenza seasons can vary widely from year to year, further evidence on effectiveness gathered during influenza seasons with different circulating viruses is needed before a conclusion on the relative effectiveness can be made.
- NACI will continue to monitor the evidence related to cell-culture based influenza vaccines and will update this supplemental statement as needed and as data on Flucelvax® Quad from several different influenza seasons accumulates.
An updated summary of the characteristics of influenza vaccines available in Canada for the 2020–2021 influenza season can be found in Appendix B. For complete prescribing information, readers should consult the product monograph available through Health Canada’s Drug Product Database.
Tables
| Serological assay | Definition | Threshold |
|---|---|---|
| GMT ratio | Ratio of GMT post-vaccination of licensed vaccine to GMT post-vaccination of new vaccine | Non-inferiority: The upper bound of the two-sided 95% CI on the ratio of the GMTs should not exceed 1.5. |
| Seroprotection | Proportion of subjects achieving an HI titre of ≥1:40 post-vaccination | Placebo-controlled: Lower limit of the two-sided 95% CI for the percent of subjects achieving seroprotection should meet or exceed 70% (for adults <65 and children) or 60% (for adults ≥65) |
| Seroconversion | Proportion of subjects achieving an increase from ≤1:10 HI titre pre-vaccination to ≥1:40 post-vaccination or achieving at least four-fold rise in HI titres | Non-inferiority: Upper limit of the two-sided 95% CI on the difference between the seroconversion rates (rate of licensed vaccine – rate of new vaccine) should not exceed 10 percentage points. Placebo-controlled: Lower limit of the two-sided 95% CI for the percent of subjects achieving seroprotection should meet or exceed 40% (for adults <65 and children) or 30% (for adults ≥65) |
Abbreviations: CI: confidence interval, GMT: geometric mean titre, HI: hemagglutination inhibition |
||
| Strength of NACI Recommendation | Grade of Evidence |
|---|---|
| Based on factors not isolated to strength of evidence (e.g. public health need) | Based on assessment of the body of evidence |
| Strong “should/should not be offered”
|
A - good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making | |
Discretionary
|
A - good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making |
| Level | Description |
|---|---|
| I | Evidence from randomized controlled trial(s). |
| II-1 | Evidence from controlled trial(s) without randomization. |
| II-2 | Evidence from cohort or case-control analytic studies, preferably from more than one centre or research group using clinical outcome measures of vaccine efficacy. |
| II-3 | Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence. |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees. |
| Quality Rating | Description |
|---|---|
| Good | A study (including meta-analyses or systematic reviews) that meets all design- specific criteriaFootnote * well. |
| Fair | A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criterionFootnote * but has no known "fatal flaw". |
| Poor | A study (including meta-analyses or systematic reviews) that has at least one design-specificFootnote * "fatal flaw", or an accumulation of lesser flaws to the extent that the results of the study are not deemed able to inform recommendations. |
Table 5 Footnotes
|
|
| Study Details | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings | Level of Evidence | Quality |
| DeMarcus L, Shoubaki L, Federinko S. Comparing influenza vaccine effectiveness between cell-derived and egg-derived vaccines, 2017–2018 influenza season. Vaccine. 2019 Jul 9;37(30):4015-4021. |
IIV4-cc (subunit) |
|
|
|
II-2 | Good |
| Izurieta HS, Chillarige Y, Kelman J, Wei Y, Lu Y, Xu W, Lu M, Pratt D, Chu S, Wernecke M, MaCurdy T,Forshee R. Relative effectiveness of cell-cultured and egg-based influenza vaccines among elderly persons in the United States, 2017-18, 2017-18. J Infect Dis. 2019 Sep 13; 220(8):1255-1264. | IIV4-cc (subunit) |
|
|
|
II-2 | Good |
| Boikos C, Sylvester G, Sampalis J, Mansi J.Effectiveness of the Cell Culture-and Egg-Derived, Seasonal Influenza Vaccine during the 2017-2018 Northern Hemisphere Influenza Season. Poster presented at: Canadian Immunization Conference (CIC) 2018; Dec 4-6, 2018 Ottawa, ON, Canada. | IIV4-cc (subunit) |
|
|
|
II-2 |
|
| Klein NP, Fireman B, Goddard K, Zerbo O, Asher J, Zhou J, King J, Lewis N. LB15. Vaccine Effectiveness of Flucelvax Relative to Inactivated Influenza Vaccine During the 2017–18 Influenza Season in Northern California. Open Forum Infect Dis. 2018;5(Suppl 1):S764. | IIV4-cc (subunit) |
|
|
|
II-2 | n/a (Study published as conference poster; unable to evaluate quality of evidence) |
Abbreviations: AFHSC; Armed Forces Health Surveillance Center; CI: confidence interval; HD: high-dose; IIV: inactivated influenza vaccine; IIV3-Adj: adjuvanted trivalent inactivated influenza vaccine; IIV4-cc: cell-culture based quadrivalent inactivated influenza vaccine IIV3-cc: cell-culture based trivalent inactivated influenza vaccine; IIV3-HD: high-dose trivalent inactivated influenza vaccine; IIV3-SD: standard-dose trivalent inactivated influenza vaccine; IIV4-SD: standard-dose quadrivalent inactivated influenza vaccine; ILI: influenza-like illness; IPTW: inverse probability of treatment weighting GMT: geometric mean titre; n/a: not applicable; OR: odds ratio; RCT: randomized controlled trial; rVE: relative vaccine effectiveness; US: United States. |
||||||
| Study Detials | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings | Level of Evidence | Quality |
Bart S., Cannon K., Herrington D., Mills R., Forleo-Neto E., Lindert K.,Abdul MA. Immunogenicity and safety of a cell culture-based quadrivalent influenza vaccine in adults: A phase III, double-blind, multicenter, randomized, non-inferiority study. Hum Vaccines Immunother. 2016;12(9):2278-88. ClinicalTrials.gov |
IIV4-cc (subunit) |
|
|
|
I | Good |
Hartvickson R., Cruz M., Ervin J., Brandon D., Forleo-Neto E., Dagnew A.F., Chandra R., Lindert K.,Mateen A.A. Non-inferiority of mammalian cell-derived quadrivalent subunit influenza virus vaccines compared to trivalent subunit influenza virus vaccines in healthy children: A phase III randomized, multicenter, double-blind clinical trial. Int J Infect Dis. 2015;41:65-72. ClinicalTrial.gov |
IIV4-cc (subunit) |
|
|
|
I | Fair |
Abbreviations: CI: confidence interval; GMT: geometric mean titre; n/a: not applicable; IIV: inactivated influenza vaccine; IIV3-cc: cell-culture based trivalent inactivated influenza vaccine; IIV4-cc: cell-culture based quadrivalent inactivated influenza vaccine; RCT: randomized controlled trial; US: United States |
||||||
| Study Detials | Summary | |||||
|---|---|---|---|---|---|---|
| Study | Vaccine | Study Design | Participants | Summary of Key Findings | Level of Evidence | Quality |
Bart S., Cannon K., Herrington D., Mills R., Forleo-Neto E., Lindert K.,Abdul MA. Immunogenicity and safety of a cell culture-based quadrivalent influenza vaccine in adults: A phase III, double-blind, multicenter, randomized, non-inferiority study. Hum Vaccines Immunother. 2016;12(9):2278-88. ClinicalTrials.gov |
IIV4-cc (subunit) |
|
|
Proportion (%) of the most commonly reported solicited local and systemic AEs in adults ≥18 years of age reporting between day 1 through day 7 after vaccination:
Proportion (%) of adults reporting any solicited AEs by age:
Proportion (%) reporting any solicited AEs by sex:
Proportion (%) of adults 18-64 reporting unsolicited AEs (collected from day 1 through day 22; SAEs, medically attended AEs, AEs leading to withdrawal from the study, and new onset of chronic diseases were collected from day 1 through day 181):
Proportion (%) of adults ≥65 reporting unsolicited AEs (collected from day 1 through day 22; SAEs, medically attended AEs, AEs leading to withdrawal from the study, and new onset of chronic diseases were collected from day 1 through day 181):
Proportion (%) of the most commonly reported unsolicited medically attended AEs by the MedDRA preferred Term:
Proportion (%) the most commonly reported unsolicited AEs by the MedDRA preferred Term deemed possibly or probably related:
Proportion (%) of the most commonly reported new onset of chronic disease by the MedDRA preferred Term:
Proportion (%) of study subjects reporting unsolicited AEs and medically attended AEs by sex:
|
I | Good |
| Ambrozaitis A, Groth N, Bugarini R, Sparacio V, Podda A, Lattanzi M. A novel mammalian cell-culture technique for consistent production of a well-tolerated and immunogenic trivalent subunit influenza vaccine. Vaccine. 2009;27(43):6022-9 |
IIV3-cc (subunit) |
|
|
Proportion (%) of local and systemic reactions in adults 18-60 years of age reporting between day 1 through day 7 after vaccination:
|
I | Good |
Szymczakiewicz-Multanowska A, Groth, N, Bugarini R, Lattanzi M, Casula D, Hilbert A, Tsai T, Podda A. Safety and Immunogenicity of a Novel Influenza Subunit Vaccine Produced in Mammalian Cell Culture. J Infect Dis. 2009;200(6): 841-8 ClinicalTrials.gov |
IIV3-cc (subunit) |
|
|
Proportion (%) of participants who received IIV3-cc or egg-based IIV3 reporting solicited local or systemic reactions by age group between day 1 through day 7 after vaccination:
Proportion (%) participants reporting local and systemic reactions between day 1 through day 7 after vaccination by vaccine group:
Proportion (%) of participants reporting injection pain site by age group between day 1 through day 7 after vaccination:
Proportion (%) adults 18-60 years of age reporting solicited local AEs in between day 1 through day 7 after vaccination:
Proportion (%) of adults 18-60 years of age reporting solicited systemic reactions in between day 1 through day 7 after vaccination:
Proportion (%) adults 18-60 years of age reporting solicited local AEs in between day 1 through day 7 after vaccination:
Proportion adults ≥61 years of age reporting solicited local AEs in between day 1 through day 7 after vaccination:
Proportion of adults ≥61 years of age reporting solicited systemic reactions in between day 1 through day 7 after vaccination:
Proportion (%) of adults ≥61 years of age reporting other solicited reactions in between day 1 through day 7 after vaccination:
Proportion (%) of subjects reporting AEs considered to be possibly or probably related to the vaccine:
|
I | Good |
| Nolan T, Chotpitayasunondh T, Rasrio Capeding M, Carson S, David Senders S, Jaehnig P, de Rooij R, Chandra R. Safety and tolerability of a cell culture derived trivalent subunit inactivated influenza vaccine administered to healthy children and adolescents: A Phase III, randomized, multicenter, observer-blind study. Vaccine. 2016; 34:230-236 | IIV3-cc (subunit) |
|
|
Proportion (%) of participants aged 4-8 years (NPV) reporting any solicited reactions within seven days after first dose:
Proportion (%) of participants aged 4-8 years reporting any solicited reactions within seven days after second dose:
Proportion (%) of participants aged 4-17 years reporting solicited reactions within seven days after single dose:
Proportion (%) of participants aged 4-8 years who reported any (severe* in brackets) solicited local reactions within 7 days of vaccination:
Proportion (%) of participants aged 9-17 years who reported any (severe* in brackets) solicited local reactions within 7 days of vaccination:
Proportion (%) of participants aged 4-8 years who reported any (severe* in brackets) solicited systemic reactions occurring within 7 days of vaccination:
Proportion (%) of participants aged 9-17 years who reported any (severe* in brackets) solicited systemic reactions occurring within 7 days of vaccination:
Proportion (%) of participants aged 4-8 years reporting unsolicited AEs after first dose:
Proportion (%) of participants aged 4-8 years reporting unsolicited AEs after second dose:
Proportion (%) of participants aged 9-17 years (PV) reporting unsolicited AEs after single dose:
Proportion (%) of participants aged 3-8 years (NPV/PV) with unsolicited AEs by preferred term
Proportion (%) of participants aged 9-17 (PV) with unsolicited AEs by preferred term:
|
I | Fair |
Vesikari T, Block SL, Guerra F, Lattanzi M, Holmes S, Izu A, Gaitatzis N, Katrin Hilbert A, Groth N. ClinicalTrials.gov |
IIV3-cc |
|
|
Proportion (%) of subjects 3-8 years of age reporting any local AEs between day 1 through day 7 after vaccination:
Proportion (%) of subjects 3-8 years of age reporting any systemic AEs between day 1 through day 7 after vaccination:
Proportion (%) of subjects 9-17 years of age reporting any AEs between day 1 through day 7 after vaccination:
Proportion (%) of subjects 3-8 years of age reporting mild and severe (brackets) solicited local AEs at injection site between day 1 through day 7 after first vaccination:
Proportion (%) of subjects 3-8 years of age reporting mild and severe (brackets) solicited local AEs between day 1 through day 7 after second vaccination:
Proportion (%) of subjects 3-8 years old reporting mild and severe (brackets) solicited systemic AEs between day 1 through day 7 after first vaccination:
Proportion of subjects 3-8 years old reporting mild and severe (brackets) solicited systemic AEs between day 1 through day 7 after second vaccination:
Proportion (%) of subjects 9-17 years of age reporting mild and severe (brackets) solicited local AEs between day 1 through day 7 after vaccination:
Proportion (%) of subjects 9-17 years old reporting mild and severe (brackets) solicited systemic AEs between day 1 through day 7 after vaccination
Proportion (%) of subjects 3-8 years of age reporting unsolicited AEs* collected for the 50-day study period:
|
I | Fair |
Frey S, Vesikari T, Szymczakiewicz-Multanowska A, Lattanzi M, Izu A, Groth N, Holmes S. ClinicalTrials.gov |
IIV3-cc (subunit) |
|
|
The overall proportion of participants reporting solicited local and systemic reactions between day 1 through day 7 after vaccination (not including SAEs) by the MedDRA Term was 51.11% for the IIV3-cc group, 46.42 % for the egg-based IIV3 group, and 35.62% for the placebo group. Proportion (%) of participants reporting solicited local reactions at injection site between day 1 through day 7 after vaccination (not including SAEs) by the MedDRA Term:
Proportion (%) of participants reporting solicited systemic reactions between day 1 through day 7 after vaccination (not including SAEs) by the MedDRA Term:
|
I | Fair |
Hartvickson R., Cruz M., Ervin J., Brandon D., Forleo-Neto E., Dagnew A.F., Chandra R., Lindert K.,Mateen A.A. ClinicalTrial.gov |
IIV4-cc (subunit) |
|
Healthy children aged 4-17 years
|
Proportion (%)* of children reporting solicited AEs (age-appropriate**) within 7 days after vaccination after the 1st dose:
Proportion (%) of children reporting solicited AEs (age-appropriate) within 7 days after vaccination after the 2nd dose:
Across all vaccine groups, the most common solicited local AE was tenderness for children 4-5 years of age and injection-site pain for children 6-8 and 9-17 years of age. The most common solicited systemic AEs across all vaccine groups for children 4-5 years of age, 6-8 years of age, and 9-17 years of age were sleepiness, fatigue and headache, and headache respectively. Proportion (%) of children reporting unsolicited AEs by group:
|
II-2 | Fair |
Loebermann M, Fritzsche C, Geerdes-Fenge H, Heijnen E, Kirby D, Reisinger EC. ClinicalTrial.gov |
IIV3-cc (subunit) |
|
|
Proportion (%) of subjects aged 18 to ≤60 years with solicited AEs after vaccination with IIV3-cc:
*Threshold for erythema, ecchymosis and induration: grade 0 (<10mm), any (≥10 mm) ** Includes subjects with body temperature ≥38̊C irrespective of route of measurement Proportion (%) of subjects aged ≥61 years with solicited AEs after vaccination with IIV3-cc:
*Threshold for erythema, ecchymosis and induration: grade 0 (<10mm), any (≥10 mm) ** Includes subjects with body temperature ≥38̊C irrespective of route of measurement Proportion (%) for all subjects with solicited AEs after vaccination with IIV3-cc:
*Threshold for erythema, ecchymosis and induration: grade 0 (<10mm), any (≥10 mm) ** Includes subjects with body temperature ≥38̊C irrespective of route of measurement Proportion (%) of subjects aged 18 to ≤60 years with unsolicited AEs after vaccination with IIV3-cc:
Proportion (%) of all subjects with unsolicited AEs after vaccination with IIV3-cc:
|
II-3 | Fair |
Moro PL, Winiecki S, Lewis P, Shimabukuro TT, Cano M. Surveillance of adverse events after the first trivalent inactivated influenza vaccine produced in mammalian cell culture (Flucelvax) reported to the Vaccine Adverse Event Reporting System (VAERS), United States, 2013-2015.Vaccine. 2015; 33(45):6684-6688. |
IIV3-cc (subunit) |
|
Persons vaccinated with IIV3-cc during July 1, 2013 through March 31, 2015 (reports received by April 30, 2015); excluding non-US reports
|
Proportion (%) of participants reporting local and systemic reactions:
*Each report was assigned a primary clinical category using MedDRA system organ classes (SOC) 19 (6.1%) of the 309 reports with an AE documented were serious. 313 reports of use in persons of inappropriate age (271 during the 2013–2014 initial season of IIV3-cc use); none of the 10 reports which described an AE were serious Among the serious reports, 1 death occurred in a 77-year-old female with a history of diabetes, chronic obstructive pulmonary disease, arthritis, and depression who received IIV-cc. Cause of death was reported as cardiovascular disease secondary to diabetes |
III | Good |
Abbreviations: AE: adverse event; CI: confidence interval; MedDRA: Medical Dictionary for Regulatory Activities; n/a: not applicable; IIV4-cc: cell-culture based quadrivalent inactivated influenza vaccine; RCT: randomized controlled trial; SAE: serious adverse event; IIV3-cc: cell-culture based trivalent inactivated influenza vaccine; US: United States; VAERS: Vaccine Adverse Event Reporting System, NPV: Not Previously Vaccinated, PV: Previously Vaccinated |
||||||
List of abbreviations
- Abbreviation
- Term
- AE
- Adverse event
- CI
- Confidence interval
- CVV
- Candidate vaccine virus
- EMR
- Electronic medical record
- DoD
- Department of Defense (US)
- FDA
- Food and Drug Administration (United States)
- GMT
- Geometric mean titre
- HA
- Hemagglutinin
- HI
- Hemagglutination inhibition
- IIV
- Inactivated influenza vaccine ki cc
- IIV3
- Trivalent inactivated influenza vaccine
- IIV3-Adj
- Adjuvanted trivalent inactivated influenza vaccine
- IIV3-cc
- Cell-culture based trivalent inactivated influenza vaccine
- IIV3-HD
- High-dose trivalent inactivated influenza vaccine
- IIV3-SD
- Standard-dose trivalent inactivated influenza vaccine
- IIV4
- Quadrivalent inactivated influenza vaccine
- IIV4-cc
- Cell-culture based quadrivalent inactivated influenza vaccine
- IIV4-SD
- Standard-dose quadrivalent inactivated influenza vaccine
- ILI
- Influenza-like illness
- IM
- Intramuscular
- IWG
- Influenza Working Group
- LAIV
- Live attenuated influenza vaccine
- LAIV3
- Trivalent live attenuated influenza vaccine
- LAIV4
- Quadrivalent live attenuated influenza vaccine
- MDCK
- Madin-Darby Canine Kidney
- MedDRA
- Medical Dictionary for Regulatory Activities
- Medical Dictionary for Regulatory Activities
- Not applicable
- NA
- Neuraminidase
- NACI
- National Advisory Committee on Immunization
- NOCD
- New onset of chronic diseases
- OR
- Odds ratio
- PHAC
- Public Health Agency of Canada
- RCT
- Randomized controlled trial
- rVE
- Relative vaccine effectiveness
- SAE
- Serious adverse event
- US
- United States
- VAERS
- Vaccine Adverse Event Reporting System (US)
- VE
- Vaccine effectiveness
Acknowledgments
This supplemental statement was prepared by: A Sinilaite, J Przepiorkowski, K Young, I Gemmill, R Harrison and approved by NACI.
NACI gratefully acknowledges the contribution of A House (Centre for Immunization and Respiratory Infectious Diseases [CIRID], PHAC), M Laplante (CIRID, PHAC), and K Merucci (Health Library, HC).
NACI Influenza Working Group
Members: I Gemmill (Chair), L Cochrane, N Dayneka, R Harrison, K Klein, D Kumar, J Langley, J McElhaney, A McGeer, D Moore, S Smith, B Warshawsky.
Liaison representative: L Grohskopf (Centers for Disease Control and Prevention [CDC], United States).
Ex-officio representatives: C Bancej (CIRID, PHAC), P Wolfe-Roberge (First Nations and Inuit Health Branch [FNIHB], Indigenous Services Canada [ISC]), and J Xiong (Biologics and Genetic Therapies Directorate [BGTD], Health Canada [HC]).
NACI
Members: C Quach (Chair), S Deeks (Vice-Chair), N Dayneka, P De Wals, V Dubey, R Harrison, K Hildebrand, K. Klein, J Papenburg, C Rotstein, B Sander and S Smith.
Former NACI members: M Salvadori and N Sicard.
Liaison Representatives: LM Bucci (Canadian Public Health Association), E Castillo (Society of Obstetricians and Gynaecologists of Canada), A Cohn (Centers for Disease Control and Prevention, United States), M Naus (Canadian Immunization Committee), J Emili (College of Family Physicians of Canada), D Moore (Canadian Paediatric Society), and A Pham-Huy (Association of Medical Microbiology and Infectious Disease Canada).
Ex-Officio Representatives: C. Rossi (National Defence and the Canadian Armed Forces), E Henry (CIRID, PHAC), J Gallivan (Marketed Health Products Directorate [MHPD], HC), M Lacroix (Public Health Ethics Consultative Group, PHAC), J Pennock (CIRID, PHAC), R Pless (Biologics and Genetic Therapies Directorate [BGTD], Health Canada [HC]), G Poliquin (National Microbiology Laboratory, PHAC), T Wong (First Nations and Inuit Health Branch [FNIHB], Indigenous Services Canada [ISC]).
Former ex-officio representatives: K Barnes (National Defence and the Canadian Armed Forces).
References
Footnotes
- Footnote 1
-
Schanzer DL, Allison M, Kathleen M. Statistical estimates of respiratory admissions attributable to seasonal and pandemic influenza for Canada. Influenza and Other Respiratory Viruses. 2013; 7(5):799-808.
- Footnote 2
-
Schanzer DL, Sevenhuysen C, Winchester B, Mersereau T. Estimating influenza deaths in Canada, 1992–2009. PLOS ONE. 2013; 8(11):e80481.
- Footnote 3
-
Frey S, Vesikari T, Szymczakiewicz-Multanowska A, Lattanzi M, Izu A, Groth N, Holmes S. Clinical Efficacy of Cell Culture—Derived and Egg-Derived Inactivated Subunit Influenza Vaccines in Healthy Adults. Clinical Infectious Diseases. 2010 Nov 1;51(9):997-1004.
- Footnote 4
-
The Centers for Disease Control and Prevention (CDC) (US). Seasonal Influenza (Flu): Cell-Based Flu Vaccines. [Internet]. 2016. [cited 2019 July 15]. Available from: https://www.cdc.gov/flu/prevent/cell-based.htm
- Footnote 5
-
Gregersen JP, Schmitt HJ, Trusheim H, Broker M. Safety of MDCK cell culture-based influenza vaccines. Future Microbiol 2011 Feb;6(2):143-152.
- Footnote 6
-
Barr IG, Donis RO, Katz JM, McCauley JW, Odagiri T, Trusheim H, Tsai TF, Wentworth DE. Cell culture-derived influenza vaccines in the severe 2017–2018 epidemic season: A step towards improved influenza vaccine effectiveness. NPJ Vaccines. 2018; 3(1):44.
- Footnote 7
-
Hampson A, Barr I, Cox N, Donis RO, Siddhivinayak H, Jernigan D, Katz J, McCauley J, Motta F, Odagiri T, Tam JS. Improving the selection and development of influenza vaccine viruses–Report of a WHO informal consultation on improving influenza vaccine virus selection, Hong Kong SAR, China, 18–20 November 2015. Vaccine. 2017; 35(8):1104-9.
- Footnote 8
-
Seqirus UK Limited. Product monograph: Flucelvax® QUAD: Influenza Vaccine (surface antigen, inactivated, prepared in cell cultures). [Internet]. 2019. Available from: https://pdf.hres.ca/dpd_pm/00054016.PDF.
- Footnote 9
-
US FDA, Department of Health and Human Services. Supplemental Approval BL 125408/174. [Internet]. 2016. [cited 2019 July 15]. Available from: https://www.fda.gov/media/100697/download
- Footnote 10
-
CDC (US). Advisory Committee on Immunization Practices Presentation Slides: June 2018 Meeting. [Internet]. 2018. [cited 2019 July 15]. Available from: https://www.cdc.gov/vaccines/acip/meetings/slides-2018-06.html
- Footnote 11
-
Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D. Current methods of the US Preventive Services Task Force: A review of the process. Am J Prev Med. 2001;20(3):21-35.
- Footnote 12
-
Seqirus. Flucelvax Doctor Discussion Guide. [Internet] Holly Springs, NC: Seqirus; 2017. [cited 2019 July 15]. Available from: https://labeling.cslbehring.com/PRODUCT-DOCUMENT/US/Flucelvax/EN/Flucelvax-Doctor-Discussion-Guide.pdf
- Footnote 13
-
Seqirus. US Product Monograph: Flucelvax Quadrivalent. [Internet]. Holly Springs, NC: Seqirus ;2016. [ cited 2019 July 15]. Available from: http://labeling.seqirus.com/PI/US/Flucelvax/EN/Flucelax-Prescribing-Information.pdf
- Footnote 14
-
Boikos C, Sylvester G, Sampalis J, Mansi J. Effectiveness of the Cell Culture-and Egg-Derived, Seasonal Influenza Vaccine during the 2017-2018 Northern Hemisphere Influenza Season. Canadian Immunization Conference 2018. 2018 Dec 04-06; Ottawa, ON, Canada [poster presentation].
- Footnote 15
-
DeMarcus L, Shoubaki L, Federinko S. Comparing influenza vaccine effectiveness between cell-derived and egg-derived vaccines, 2017–2018 influenza season. Vaccine. 2019 Jul 9;37(30):4015-4021.
- Footnote 16
-
Izurieta HS, Chillarige Y, Kelman J, Wei Y, Lu Y, Xu W, Lu M, Pratt D, Chu S, Wernecke M, MaCurdy T, Forshee R. Relative effectiveness of cell-cultured and egg-based influenza vaccines among elderly persons in the United States, 2017-18, 2017-18. J Infect Dis. 2019 Sep 13; 220(8):1255-1264.
- Footnote 17
-
Klein NP, Fireman B, Goddard K, Zerbo O, Asher J, Zhou J, King J, Lewis N. LB15. Vaccine Effectiveness of Flucelvax Relative to Inactivated Influenza Vaccine During the 2017–18 Influenza Season in Northern California. Open Forum Infect Dis. 2018; 5(Suppl 1):S764.t
- Footnote 18
-
US Armed Forces, Armed Forces Health Surveillance Center. Influenza-Like Illness (ILI). [Internet]. 2015. [cited 2019 July 15]. Available from: https://www.health.mil/Reference-Center/Publications/2015/10/01/Influenza-Like-Illness
- Footnote 19
-
US Food and Drug Administration. Guidance for industry: Clinical data needed to support the licensure of seasonal inactivated influenza vaccines. [Internet]. 2007. [cited 2019 July 15]. Available from: https://www.fda.gov/downloads/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/Guidances/Vaccines/ucm091990.pdf
- Footnote 20
-
Bart S., Cannon K., Herrington D., Mills R., Forleo-Neto E., Lindert K., Abdul MA. Immunogenicity and safety of a cell culture-based quadrivalent influenza vaccine in adults: A phase III, double-blind, multicenter, randomized, non-inferiority study. Hum Vaccines Immunother. 2016; 12(9):2278-88.
- Footnote 21
-
Hartvickson R., Cruz M., Ervin J., Brandon D., Forleo-Neto E., Dagnew A.F., Chandra R., Lindert K., Mateen A.A. Non-inferiority of mammalian cell-derived quadrivalent subunit influenza virus vaccines compared to trivalent subunit influenza virus vaccines in healthy children: A phase III randomized, multicenter, double-blind clinical trial. Int J Infect Dis. 2015; 41:65-72.
- Footnote 22
-
European Union European Medicines Agency. Assessment report for paediatric studies submitted according to Article 46 of the Regulation (EC) No 1901/2006. [Internet]. 2015. [cited 2019 July 15]. Available from: https://www.ema.europa.eu/en/documents/variation-report/optaflu-h-c-758-p46-0052-epar-assessment-report_en.pdf.
- Footnote 23
-
European Union European Medicines Agency. Optaflu European Public Assessment Report: Scientific Discussion. [Internet]. 2007. [cited 2019 July 15]. Available from: https://www.ema.europa.eu/en/documents/scientific-discussion/optaflu-epar-scientific-discussion_en.pdf.
- Footnote 24
-
US Food and Drug Administration. Flucelvax Quadrivalent. [Internet]. 2019. [cited 2019 July 15]. Available from: https://www.fda.gov/vaccines-blood-biologics/vaccines/flucelvax-quadrivalent
- Footnote 25
-
US Food and Drug Administration. FLUCELVAX - Seqirus, Inc. 1.14.1.3 US Package Insert. [Internet]. 2019. [cited 2019 July 15]. Available from: https://www.fda.gov/media/85322/download
- Footnote 26
-
Vesikari T, Block SL, Guerra F, Lattanzi M, Holmes S, Izu A, Gaitatzis N, Hilbert AK, Groth N. Immunogenicity, safety and reactogenicity of a mammalian cell-culture–derived influenza vaccine in healthy children and adolescents three to seventeen years of age. Pediatr Infect Dis J 2012 May; 31(5):494-500.
- Footnote 27
-
Ambrozaitis A, Groth N, Bugarini R, Sparacio V, Podda A, Lattanzi M. A novel mammalian cell-culture technique for consistent production of a well-tolerated and immunogenic trivalent subunit influenza vaccine. Vaccine. 2009; 27(43):6022-9.
- Footnote 28
-
Szymczakiewicz-Multanowska A, Groth, N, Bugarini R, Lattanzi M, Casula D, Hilbert A, Tsai T, Podda A. Safety and Immunogenicity of a Novel Influenza Subunit Vaccine Produced in Mammalian Cell Culture. J Infect Dis. 2009; 200(6): 841-8.
- Footnote 29
-
Loebermann M, Fritzsche C, Geerdes-Fenge H, Heijnen E, Kirby D, Reisinger EC. A phase III, open-label, single-arm, study to evaluate the safety and immunogenicity of a trivalent, surface antigen inactivated subunit influenza virus vaccine produced in mammalian cell culture (Optaflu®) in healthy adults. Infection. 2019; 47:105-109.
- Footnote 30
-
Nolan T, Chotpitayasunondh T, Rasrio Capeding M, Carson S, David Senders S, Jaehnig P, de Rooij R, Chandra R. Safety and tolerability of a cell culture derived trivalent subunit inactivated influenza vaccine administered to healthy children and adolescents: A Phase III, randomized, multicenter, observer-blind study. Vaccine. 2016; 34:230-236.
- Footnote 31
-
Moro PL, Winiecki S, Lewis P, Shimabukuro TT, Cano M. Surveillance of adverse events after the first trivalent inactivated influenza vaccine produced in mammalian cell culture (Flucelvax) reported to the Vaccine Adverse Event Reporting System (VAERS), United States, 2013-2015.Vaccine. 2015; 33(45):6684-6688.
- Footnote 32
-
Papke D., McNussen P.J., Rasheed M., Tsipursky M.S., Labriola L.T. A case of unilateral optic neuropathy following influenza vaccination. Semin Ophthalmol. 2017; 32(4):517-23.
- Footnote 33
-
Bencharitiwong R, Leonard S, Tsai T, Nowak-Wegrzyn A. In vitro assessment of the allergenicity of novel MF59-adjuvanted pandemic H1N1 influenza vaccine produced in dog kidney cells. Hum Vaccin Immunother. 2012 Jul;8(7):863-865.
- Footnote 3r
-
Wanich N, Bencharitiwong R, Tsai T, Nowak-Wegrzyn A. In vitro assessment of the allergenicity of a novel influenza vaccine produced in dog kidney cells in individuals with dog allergy. Ann Allergy Asthma Immunol. 2010 May;104(5):426-433.
- Footnote 35
-
Skowronski DM, Chambers C, De Serres G, Dickinson JA, Winter AL, Hickman R, Chan T, Jassem AN, Drews SJ, Charest H, Gubbay JB. Early season co-circulation of influenza A (H3N2) and B (Yamagata): interim estimates of 2017/18 vaccine effectiveness, Canada, January 2018. Eurosurveillance. 2018; 23(5).
- Footnote 36
-
Skowronski DM, Janjua NZ, De Serres G, Sabaiduc S, Eshaghi A, Dickinson JA, Fonseca K, Winter AL, Gubbay JB, Krajden M, Petric M. Low 2012–13 influenza vaccine effectiveness associated with mutation in the egg-adapted H3N2 vaccine strain not antigenic drift in circulating viruses. PloS one. 2014; 9(3):e92153.
- Footnote 37
-
Zost SJ, Parkhouse K, Gumina ME, Kim K, Perez SD, Wilson PC, Treanor JJ, Sant AJ, Cobey S, Hensley SE. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proceedings of the National Academy of Sciences. 2017; 114(47):12578-83.
- Footnote 38
-
Wu NC, Zost SJ, Thompson AJ, Oyen D, Nycholat CM, McBride R, Paulson JC, Hensley SE, Wilson IA. A structural explanation for the low effectiveness of the seasonal influenza H3N2 vaccine. PLoS pathogens. 2017; 13(10):e1006682.
- Footnote 39
-
The Francis Crick Institute. Worldwide Influenza Centre: Annual and Interim Reports – February 2018 interim report. [Internet]. 2018. [cited 2019 July 15]. Available from: https://www.crick.ac.uk/research/worldwide-influenza-centre/annual-and-interim-reports/
- Footnote 40
-
Harding AT, Heaton NS. Efforts to improve the seasonal influenza vaccine. Vaccines. 2018; 6(19):1–12.
- Footnote 41
-
Lin Y, Wharton SA, Whittaker L, Dai M, Ermetal B, Lo J, Pontoriero A, Baumeister E, Daniels RS, McCauley JW Influenza Other Respir Viruses. 2017 May; 11(3):263-274.
- Footnote 42
-
Remschmidt C, Wichmann O, Harder T. Frequency and impact of confounding by indication and health vaccinee bias in observational studies assessing influenza vaccine effectiveness: a systematic review. BMC Infect Dis 2015; 15 (429).
Appendix A: PRISMA Flow Diagram
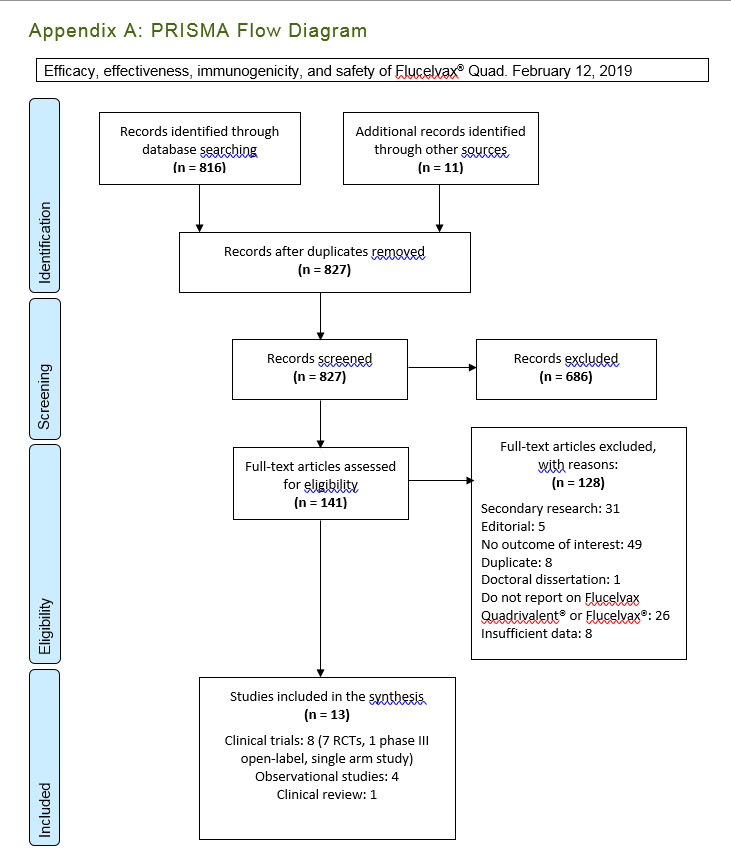
Figure 1 - Text description
Appendix A: PRISMA Flow Diagram
The PRISMA flow diagram describes the process by which articles were selected for the literature review. The process is broken down into four stages: Identification, Screening, Eligibility and Included.
Stage 1: Identification
- 816 records were identified through the February 12, 2019 database search and 11 records were identified through additional sources.
- 827 records remained after duplicates were removed.
Stage 2: Screening
- 827 records were then screened.
- Of these 827 records, 686 records were excluded.
Stage 3: Eligibility
- 141 full-text articles were assessed for eligibility.
- Of these 141 full-text articles, 128 were excluded. The exclusion breakdown is as follows: 31 were secondary research, 5 were editorials, 49 were no outcome of interest, 8 were duplicates; 1 was a doctoral dissertation, 26 did not report on Flucelvax Quadrivalent® or Flucelvax® and 8 had insufficient data.
Stage 4: Included
- 13 articles were included in the final synthesis: 8 clinical trials (7 RCT, 1 phase III open-label, single arm study), 4 observational studies and 1 clinical review.
Appendix B: Characteristics of Inlfuenza Vaccines Available For Use in Canada, 2020–2021Footnote *
| Product name (manufacturer) | Vaccine Characteristic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vaccine type | Route of administration | Authorized ages for use | Antigen content for each vaccine strain | Adjuvant | Formats available | Post-puncture shelf life for multi-dose vials | Thimerosal | Antibiotics (traces) | Production medium | |
| Quadrivalent | ||||||||||
| Flulaval® Tetra (GSK) | IIV4-SD (split virus) |
IM | 6 months and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial Single dose pre-filled syringe |
28 days | Yes (multi-dose vial only) |
None | Egg (Avian) |
| Fluzone® Quadrivalent (Sanofi Pasteur) | IIV4-SD (split virus) |
IM | 6 months and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial Single dose vial Single-dose pre-filled syringe without attached needle |
Up to expiry date indicated on vial label | Yes (multi-dose vial only) |
None | Egg (Avian) |
| Afluria® Tetra (Seqirus) | IIV4-SD (split virus) |
IM | 5 years and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial Single dose pre-filled syringe without attached needle |
Up to expiry date indicated on vial label | Yes (multi-dose vial only) |
Neomycin and polymyxin B | Egg (Avian) |
| Influvac® Tetra (BGP Pharma ULC, operating as Mylan) | IIV4-SD (subunit) |
IM or deep subcutaneous injection | 3 years and older | 15 µg HA /0.5 mL dose |
None | Single dose pre-filled syringe with or without a needle | Not applicable | No | Gentamicin or neomycin and polymyxin BFootnote § | Egg (Avian) |
| Flucelvax® Quad (Seqirus) | IIV4-cc (subunit) | IM | 9 years and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial Single dose pre-filled syringe without attached needle |
28 days | Yes (multi-dose vial only) |
No | Cell (Mammalian) |
| FluMist® Quadrivalent (AstraZeneca) | LAIV4 (live attenuated) |
Intranasal | 2–59 years | 106.5-7.5 FFU of live attenuated reassortants /0.2 mL dose (given as 0.1 mL in each nostril) |
None | Single use pre-filled glass sprayer | Not applicable | No | Gentamicin | Egg (Avian) |
| Trivalent | ||||||||||
| Agriflu® (Seqirus) | IIV3-SD (subunit) |
IM | 6 months and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial Single dose pre-filled syringe without attached needle |
28 days | Yes (multi-dose vial only) |
Kanamycin and neomycin | Egg (Avian) |
| Fluviral® (GSK) | IIV3-SD (split virus) |
IM | 6 months and older | 15 µg HA /0.5 mL dose |
None | 5 mL multi-dose vial | 28 days | Yes | None | Egg (Avian) |
| Fluzone® High-Dose (Sanofi Pasteur) | IIV3-HD (split virus) |
IM | 65 years and older | 60 µg HA /0.5 mL dose |
None | Single dose pre-filled syringe | Not applicable | No | None | Egg (Avian) |
| Fluad Pediatric® and Fluad® (Seqirus) | IIV3-Adj (subunit) |
IM | Pediatric: 6–23 months Adult: 65 years and older |
Pediatric: 7.5 µg HA /0.25 mL dose Adult: 15 µg HA /0.5 mL dose |
MF59 | Single dose pre-filled syringe without a needle | Not applicable | No | Kanamycin and neomycin | Egg (Avian) |
Abbreviations: FFU: fluorescent focus units; HA: hemagglutinin; IIV3-Adj: adjuvanted trivalent inactivated influenza vaccine; IIV3-HD: high-dose trivalent inactivated influenza vaccine; IIV3-SD: standard-dose trivalent inactivated influenza vaccine; IIV4-cc: cell-culture based quadrivalent inactivated influenza vaccine; IIV4-SD: standard-dose quadrivalent inactivated influenza vaccine; IM: intramuscular; LAIV4: quadrivalent live attenuated influenza vaccine; NA: neuraminidase. Footnotes
|
||||||||||