Lyme disease surveillance report: Preliminary annual report 2018
On this page
- Surveillance highlights 2018
- Introduction
- Methods
- Epidemiology
- Discussion
- Public health conclusions
- Acknowledgements
- References
Surveillance highlights 2018
- A total of 1,487 human cases of Lyme disease were reported to the Public Health Agency of Canada, of which, 1,053 (71%) were confirmed cases and 434 (29%) probable cases.
- Incidence was highest in adults aged 60−74 years (28% of cases) and children aged 5−14 years (11% of cases) with predominance in males.
- 31% of cases reported an illness onset in July.
- 97% of cases were reported in Manitoba, Ontario, Quebec and Nova Scotia.
- 8% of the reported cases were likely infected during travel outside of Canada.
Introduction
Zoonotic diseases are infectious diseases caused by bacteria, viruses and parasites that spread between animals and humans. Lyme disease is a multisystemic infection which can lead to health issues such as erythema migrans rash, cardiac, neurologic or arthritic manifestations. It is caused by the bacterium Borrelia burgdorferi, which is transmitted by the bite of an infected tick; the blacklegged tick, Ixodes scapularis, in Manitoba, central and eastern Canada and the western blacklegged tick, Ixodes pacificus in British Columbia. The ticks become infected after feeding on infected small mammals or birds.
Over the past decade, the northward geographic range expansion of the blacklegged tick populations in southeastern and south central Canada, in part due to climate warming, has resulted in an increase of the number of locally acquired Lyme disease cases. Surveillance for ticks and human Lyme disease cases are conducted using a One Health approach to minimize the burden of what has become the most reported vector−borne disease in Canada. This report focuses on the human component of Lyme disease surveillance, providing surveillance overview of data on cases reported in 2018.
Methods
Since becoming nationally notifiable in 2009, human cases of Lyme disease in Canada have been reported voluntarily to the Public Health Agency of Canada (PHAC) by provincial/territorial health ministries/agencies through the Canadian Notifiable Disease Surveillance System (CNDSS). These case reports are accompanied by some basic demographic information. In 2011, PHAC developed and implemented the Lyme Disease Enhanced Surveillance System whereby participating jurisdictions (eight provinces in 2018) report information additional to that collected by the CNDSS, including information on geographic location of infection acquisition, clinical features and laboratory results (for further information see Surveillance of Lyme disease on the Canada.ca website). Cases reported to PHAC are classified using the national Lyme disease 2016 case definition. Further information about the Lyme disease case definition can be found on the Canada.ca website.
Data obtained from provincial notifiable disease systems represent a snapshot at the time of data extraction and may differ from previous/subsequent reports, data displayed by provincial health authorities and from CNDSS.
Epidemiology
Changes in incidence amongst years
In 2018, 1,487 human cases of Lyme disease were reported in Canada. Of those, 1,053 (70.8%) were confirmed and 434 (29.2%) were probable cases. From 2009 through 2017, the total reported Lyme disease cases increased from 144 to 2,025 (an incidence of 0.4 and 5.5 per 100,000 population, respectively) and then decreased by 26.6% to 1,487 in 2018 (an incidence of 4.0 per 100,000 population) (Figure 1).
Noteworthy, although the surveillance system does not collect information about the outcome of the cases, Manitoba recorded one death attributed to Lyme carditis in 2018 Reference 1.
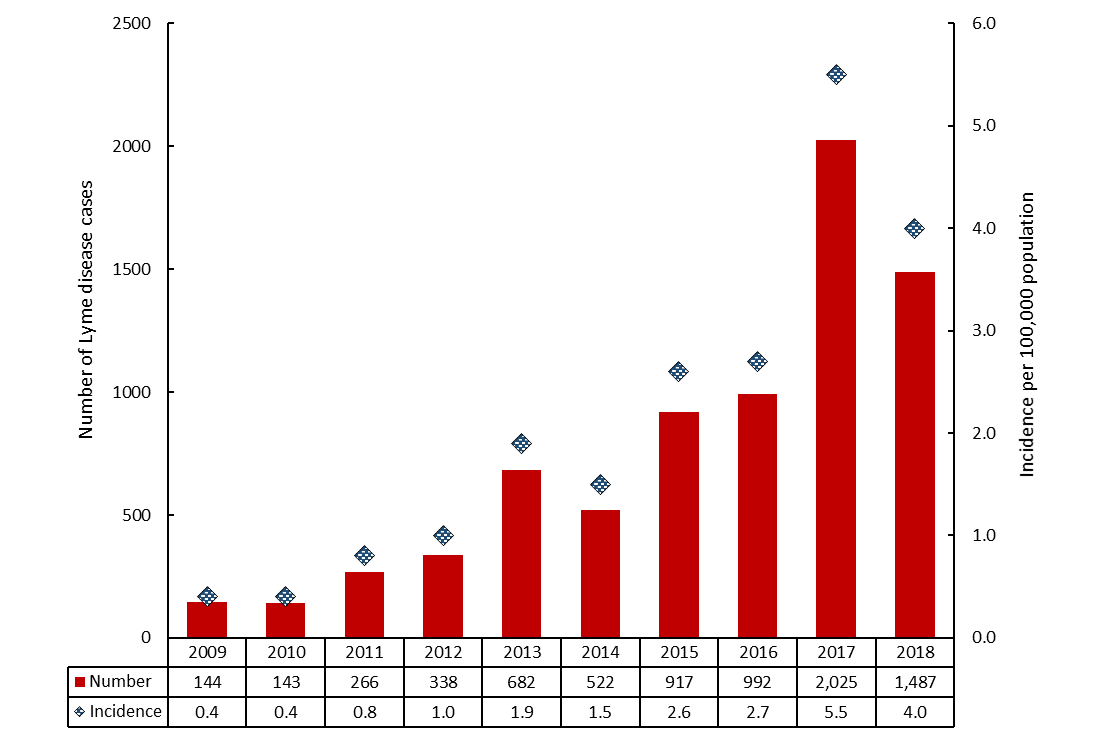
Figure 1 - Text description
This is a bar chart with vertical bars showing the numbers of cases reported in each year, from left to right, from 2009 to 2018. The red filled bars shows the total numbers of cases reported each year from 2009 to 2018. Above the filled bars is blue marker that displays the incidence per 100,000 population over each year from 2009 to 2018. The number of cases and incidence per year are detailed in the following table:
| Year | Number of cases | Incidence per 100,000 population |
|---|---|---|
| 2009 | 144 | 0.4 |
| 2010 | 143 | 0.4 |
| 2011 | 266 | 0.8 |
| 2012 | 338 | 1.0 |
| 2013 | 682 | 1.9 |
| 2014 | 522 | 1.5 |
| 2015 | 917 | 2.6 |
| 2016 | 992 | 2.7 |
| 2017 | 2,025 | 5.5 |
| 2018 | 1,487 | 4.0 |
Geographic distribution
Both locally and travel-acquired cases are reported to PHAC. The majority of all cases (96.7%) were reported from Ontario (n = 628), Nova Scotia (n = 451), Quebec (n = 305) and Manitoba (n = 54) (Figure 2). Nova Scotia was the province with the highest incidence (47.0 per 100,000 pop.) (Figure 2) which is 11.7 folds greater than the national incidence (of 4.0 per 100,000 pop.). The greatest decline in the reported cases from 2017 to 2018 was seen in Ontario where the number fell from 1,005 in 2017 (incidence of 7.1 per 100,000 pop.) to 628 in 2018 (incidence of 4.4 per 100,000 pop.); a decrease of 37%.
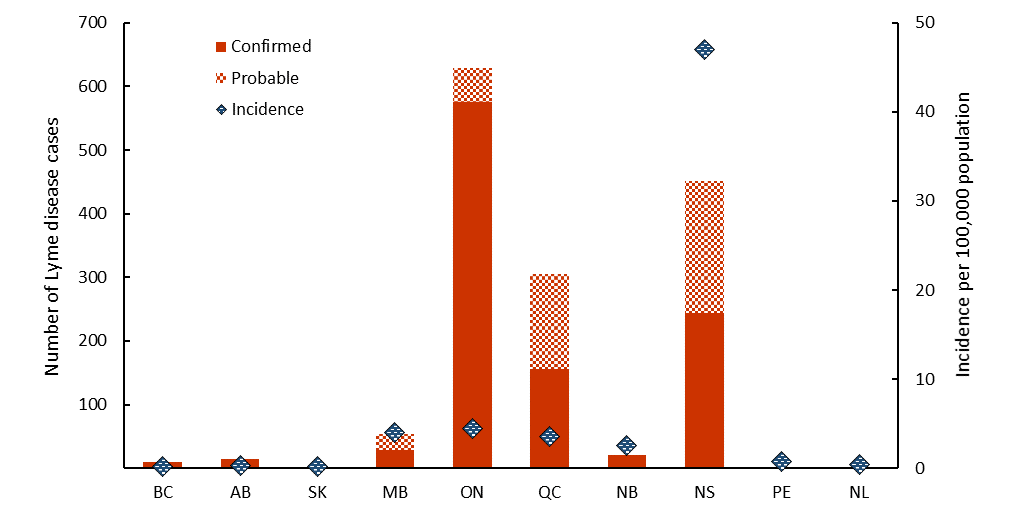
Figure 2 - Text description
This figure is a stacked bar graph with red filled bars showing the numbers of confirmed cases and probable (upper red pattern filled bars) Lyme disease cases reported by each province (from left to right, British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia, Prince Edward Island and Newfoundland & Labrador). The blue diamonds show the incidence of the disease in each province. The numbers of cases and incidence per province are detailed in the following table:
| Case classification | Total | Incidence per 100,000 population | ||
|---|---|---|---|---|
| Confirmed | Probable | |||
| British Columbia | 9 | 0 | 9 | 0.2 |
| Alberta | 15 | 0 | 15 | 0.3 |
| Saskatchewan | 2 | 0 | 2 | 0.2 |
| Manitoba | 29 | 25 | 54 | 4.0 |
| Ontario | 576 | 52 | 628 | 4.4 |
| Quebec | 156 | 149 | 305 | 3.6 |
| New Brunswick | 20 | 0 | 20 | 2.6 |
| Nova Scotia | 244 | 207 | 451 | 47.0 |
| Prince Edward Island | 0 | 1 | 1 | 0.7 |
| Newfoundland & Labrador | 2 | 0 | 2 | 0.4 |
Abbreviations: BC, British Columbia; AB, Alberta; SK, Saskatchewan; MB, Manitoba; ON, Ontario; QC, Quebec; NB, New Brunswick; NS, Nova Scotia; PE, Prince Edward Island; NL, Newfoundland & Labrador.
Locally acquired cases
In Canada, Lyme disease cases were acquired in six provinces in 2018; British Columbia, Manitoba, Ontario, Quebec, New Brunswick and Nova Scotia (Figure 3).
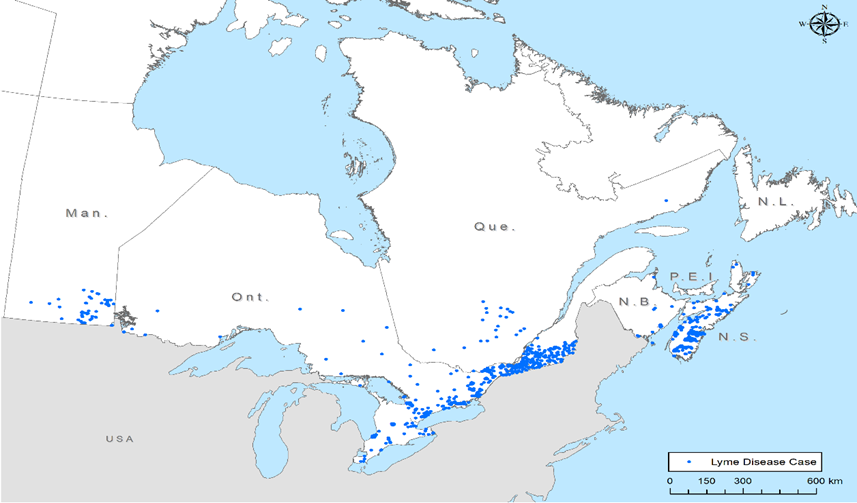
Figure 3 - Text description
The number of Lyme disease cases by probable province of acquisition are detailled in the following table:
| Province | Number of cases | Number of census subdivisions | Number of health regions |
|---|---|---|---|
| Manitoba | 48 | 22 | na |
| Ontario | 365 | 100 | na |
| Quebec | 218 | na | 8 |
| New Brunswick | 19 | 8 | na |
| Nova Scotia | 334 | 41 | na |
| Total | 984 | 171 | 8 |
Legend: Each dot on the map represents the probable location of infection acquisition, randomly distributed at the health region level for Quebec and at the census subdivision level for the other provinces. The majority of locally reported cases are concentrated in locations in southern Manitoba, southern and southeastern Ontario, southern Quebec and in Nova Scotia. Data on location of acquisition was available for 69% of the locally acquired cases. The data on location of acquisition at a sub-provincial level were not available for British Columbia. Furthermore, cases reported by Alberta, Saskatchewan, Prince Edward Island and Newfoundland & Labrador were travel−related only.
Travel−related cases
Lyme disease is mostly acquired in parts of Canada where blacklegged tick populations are established (i.e., at− risk areas) or during travel in countries where the disease is endemic. In 2018, the information of travel−history was available for 1,217 Lyme disease cases. Of these, 100 cases (8.2%) were likely infected during travel outside of Canada, and were probably acquired either in the USA (51 cases), or in Europe (49 cases).
Demographic characteristics
In 2018, information on age and sex was available for 1,115 cases (75.2%). The average age of reported Lyme disease cases was 47 years old. The highest incidence of reported Lyme disease was in adults aged 60−74 and in children aged 5−14 (Figure 4), representing 27.7% and 11.4% of all cases, respectively. Except for the 75−79 age group, incidence in males was higher than in females, and overall 58.1% of reported cases were males.
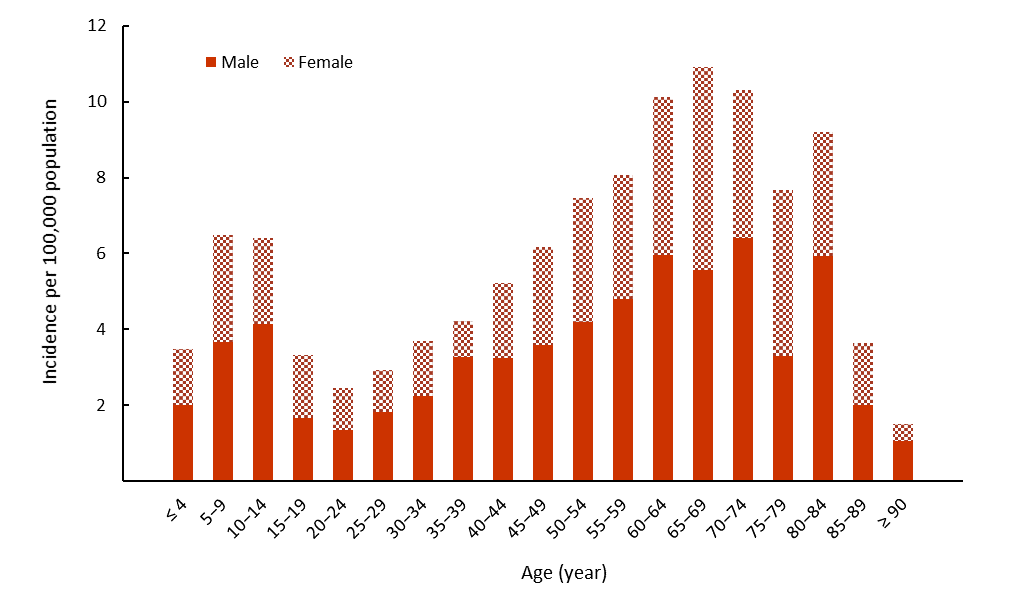
Figure 4 - Text description
This figure is a stacked bar graph with red filled bars showing the incidence per 100,000 population of male and female (upper red pattern filled bars) Lyme disease cases reported by age group (intervals of five years). The incidences by age group are detailed in the following table:
| Age (year) | Incidence per 100,000 | |
|---|---|---|
| Male | Female | |
| ≤ 4 | 2.0 | 1.5 |
| 5−9 | 3.7 | 2.8 |
| 10−14 | 4.1 | 2.3 |
| 15−19 | 1.7 | 1.7 |
| 20−24 | 1.3 | 1.1 |
| 25−29 | 1.8 | 1.1 |
| 30−34 | 2.3 | 1.4 |
| 35−39 | 3.3 | 0.9 |
| 40−44 | 3.2 | 2.0 |
| 45−49 | 3.6 | 2.6 |
| 50−54 | 4.2 | 3.2 |
| 55−59 | 4.8 | 3.3 |
| 60−64 | 6.0 | 4.2 |
| 65−69 | 5.6 | 5.3 |
| 70−74 | 6.4 | 3.9 |
| 75−79 | 3.3 | 4.4 |
| 80−84 | 5.9 | 3.3 |
| 85−89 | 2.0 | 1.6 |
| ≥ 90 | 1.0 | 0.5 |
Seasonality
In 2018, Lyme disease cases were reported in every month; however, 95.3% of the cases occurred from May through November. More than 69% of the cases had symptom onset during the summer months of June (22.8%), July (30.8%) and August (16.2%) (Figure 5).
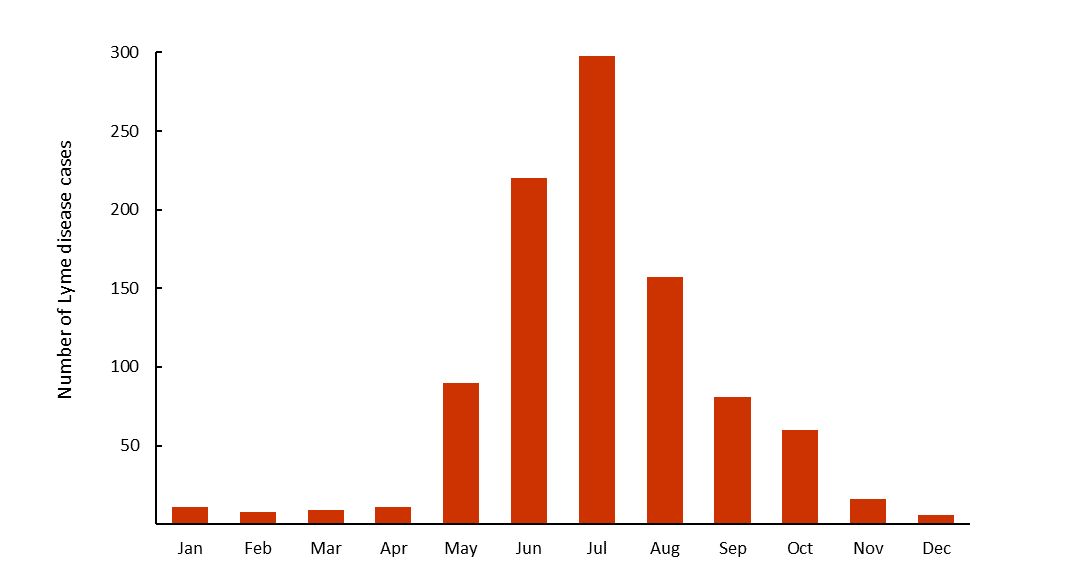
Figure 5 - Text description
This is a bar chart with vertical red bars showing the months of illness onset of Lyme disease cases acquired locally, from left to right, from January to December. The months of illness onset of Lyme disease cases are detailed in the following table:
| Month | 2018 |
|---|---|
| Jan | 11 |
| Feb | 8 |
| Mar | 9 |
| Apr | 11 |
| May | 90 |
| Jun | 220 |
| Jul | 298 |
| Aug | 157 |
| Sep | 81 |
| Oct | 60 |
| Nov | 16 |
| Dec | 6 |
Discussion
In 2018, ten provinces reported 1,487 cases to PHAC representing a decrease of 26.6% compared to the previous year. Impacts of human activities, climate and landscape changes can influence the human infection risk on the long term. However, change in the frequency of human exposure, infection, detection and reporting of cases may vary amongst years. Environmental and human behavioural factors may have caused a reduction in the risk of acquiring infection in 2018, as was seen in 2014. Similar interannual variations have been seen in surveillance data in the US Reference 2, and these may be due to interannual variations in weather that affect tick activity and survival Reference 3, or time spent doing outdoor pursuits by the public Reference 4. To some extent, this may also reflect efforts by the different Canadian public health authorities at the federal, provincial/territorial and local levels, to enhance prevention of Lyme disease, including promotion of measures to prevent tick bites, and increase the availability of post−tick bite antimicrobial prophylaxis in some jurisdictions Reference 5 Reference 6. Despite the 2018 decrease in the number of reported cases, long−term risk of human infection is increasing Reference 7 Reference 8 in part because of the warming climate that drives the northward range expansion of the blacklegged ticks in eastern Canada. In addition, as for any surveillance system, it is likely that there is some underreporting Reference 9 because some cases may be undetected or not reported.
In 2018, children aged 5−14 years and adults aged 60−74 years are the age groups with apparently higher risk of acquiring Lyme disease, while for nearly all age groups incidence was higher in males. Age and sex− based variation in risk may be related to behavioural or occupational/recreational risk factors, which lead to higher likelihood of tick bites and Lyme disease transmission Reference 2 Reference 10 Reference 11. It would be worthwhile for public health programs to target these at−risk groups to increase their vigilance and adoption of preventive measures in order to reduce the risk for Lyme disease in areas where the vector ticks are present (learn about Prevention of Lyme disease on the Canada.ca website).
Lyme disease cases were observed in every month in 2018; however, most had symptom onset from May to November and there were distinct peaks in cases during the summer months when nymphal ticks are most active Reference 12 Reference 13 and people are most likely to be engaged in outdoor activities. However, illness onset occurred throughout the year, which would be consistent with the onset of manifestations of disseminated Lyme disease some months post−infection Reference 14 (learn about Lyme disease, its causes, symptoms, risks, treatment and prevention on the Canada.ca website). Health care providers should be aware that Lyme disease cases can occasionally be observed outside the peak activity period for ticks and as a result should not exclude Lyme disease diagnosis when there is evidence of compatible clinical manifestations.
The majority of reported cases acquired infection in locations in southern Manitoba, southern and southeastern Ontario, southern Quebec and in Nova Scotia, where the main vector of Lyme disease, the blacklegged tick is established Reference 15 (for more details, see where is the risk in Canada? on the Canada.ca website). However, some cases appear to have been acquired outside of known risk areas, which may indicate that, albeit at a low level, there is a real risk of acquiring Lyme disease from adventitious blacklegged ticks dispersed by migratory birds. In western provinces, only British Columbia reported a few locally-acquired cases. In this province, the risk from infected western blacklegged tick (the other main vector of Lyme disease) remains stable compared with the provinces where blacklegged tick is established Reference 16.
In 2018, where information on travel−history was available, the 100 travel−related cases acquired infection in the USA or Europe. Canadians travelling to endemic areas in the USA and Europe should be aware of outdoor activities that put them at increased risk and ensure the use of personal protection measures to prevent tick bites and Lyme disease (see Lyme disease prevention toolkit on the Canada. ca website).
Public health conclusions
Lyme disease is the most frequently reported vector−borne disease in Canada. Although the number of cases dipped in 2018, it is anticipated that the number of reported Lyme disease cases will continue to increase in the future. This trend will be driven in part by local abundance of infected nymphal tick populations and by continued range expansion of tick populations in Canada.
The key findings of this report highlight the need for further development and implementation of targeted awareness campaigns designed to minimize the burden of Lyme disease in Canada.
Acknowledgements
The Public Health Agency of Canada acknowledges the provincial and territorial partners for their participation to the Canadian Notifiable Disease Surveillance System and Lyme Disease Enhanced Surveillance System.
References
- Reference 1
-
Milena S, Richard R, Terence W. Fatal Lyme carditis presenting as fluctuating high-grade atrioventricular block. Can Med Assoc J. 2020;192(21).
- Reference 2
-
Schwartz AM, Hinckley AF, Mead PS, Hook SA, Kugeler KJ. Surveillance for Lyme Disease–United States, 2008–2015. Morb Mortal Wkly Rep. 2017;66(22):1.
- Reference 3
-
Berger KA, Ginsberg HS, Dugas KD, Hamel LH, Mather TN. Adverse moisture events predict seasonal abundance of Lyme disease vector ticks (Ixodes scapularis). Parasites & vectors. 2014;7(1):181.
- Reference 4
-
Bouchard C, Dibernardo A, Koffi JK, Wood H, Leighton PA, Lindsay LR. Increased risk of tick-borne diseases with climate change. Can Commun Dis Rep. 2019;45:4.
- Reference 5
-
Institut national de santé publique du Québec. Recommandation de prophylaxie postexposition de la maladie de Lyme [Internet]. 2017 [cited 21 Jan 2020]. Available from: https://www.inspq.qc.ca/publications/2301.
- Reference 6
-
Leeds Grenville & Lanark District Health Unit. Lyme disease prophylaxis algorithm for the Leeds, Grenville & Lanark area [Internet]. 2015 [cited 21 Jan 2020]. Available from: http://healthunit.org/wp-content/uploads/ Attached_Tick_Prophylaxis_for_Lyme_Disease_Algorithm.pdf.
- Reference 7
-
Gasmi S, Ogden NH, Ripoche M, Leighton PA, Lindsay LR, Nelder MP, et al. Detection of municipalities at–risk of Lyme disease using passive surveillance of Ixodes scapularis as an early signal: A province–specific indicator in Canada. PLoS One. 2019;14(2):e0212637.
- Reference 8
-
Leighton PA, Koffi JK, Pelcat Y, Lindsay LR, Ogden NH. Predicting the speed of tick invasion: an empirical model of range expansion for the Lyme disease vector Ixodes scapularis in Canada. J Appl Ecol. 2012;49(2):457-64.
- Reference 9
-
Ogden NH, Bouchard C, Badcock J, Drebot MA, Elias SP, Hatchette TF, et al. What is the real number of Lyme disease cases in Canada? BMC public health. 2019;19(1):849.
- Reference 10
-
Gasmi S, Ogden NH, Lindsay LR, Burns S, Fleming S, Badcock J, et al. Surveillance for Lyme disease in Canada: 2009–2015. Can Commun Dis Rep. 2017;43(10):194-9.
- Reference 11
-
Ogden NH, Koffi JK, Leonard E, Fleming S, Monbourquette DC, Sanford C, et al. Surveillance for Lyme disease in Canada, 2009–2012. Can Commun Dis Rep. 2015;41(6):132-45.
- Reference 12
-
Gasmi S, Ogden NH, Leighton PA, Lindsay LR, Thivierge K. Analysis of the human population bitten by Ixodes scapularis ticks in Quebec, Canada: Increasing risk of Lyme disease. Ticks Tick Borne Dis. 2016;7(6):1075-81.
- Reference 13
-
Kurtenbach K, Hanincová K, Tsao JI, Margos G, Fish D, Ogden NH. Fundamental processes in the evolutionary ecology of Lyme borreliosis. Nat Rev Microbiol. 2006;4(9):660-9.
- Reference 14
-
Hatchette TF, Davis I, Johnston BL. Lyme disease: clinical diagnosis and treatment. Can Commun Dis Rep. 2014;40(11):194.
- Reference 15
-
Ogden NH, Koffi JK, Pelcat Y, Lindsay LR. Environmental risk from Lyme disease in central and eastern Canada: a summary of recent surveillance information. Can Commun Dis Rep. 2014;40(5):74-82.
- Reference 16
-
Ogden NH, Lindsay LR, Morshed M, Sockett PN, Artsob H. The emergence of Lyme disease in Canada. Can Med Assoc J. 2009;180(12):1221-4.
Contact us
Related links
Footnotes
- Footnote 1
-
The denominators used to calculate the incidences were obtained from Statistics Canada, population estimates on July 1st.
- Footnote 2
-
Month of illness onset is the month when symptoms first occurred.
