Government of Canada's sexually transmitted and blood-borne infections (STBBI) action plan 2024-2030
Download in PDF format
(1.14 MB, 58 pages)
Organization: Public Health Agency of Canada
Date published: February 2024
Table of contents
- Land acknowledgement
- Ministerial foreword
- Acknowledgements
- Action plan in brief
- Section 1: Setting the stage
- Section 2: STBBI landscape in Canada
- Section 3: Government of Canada priorities and actions
- Section 4: Implementation
- Section 5: Conclusion
- Glossary of Terms
- Appendix A: Federal progress indicators
Land acknowledgement
We respectfully recognize and acknowledge that the lands on which we developed this Action Plan are the homelands of First Nations, Inuit, and Métis Peoples. We acknowledge our privilege to live and work on these lands and strive to foster equitable partnerships with Indigenous Peoples and work collaboratively to advance reconciliation in Canada.
This federal Action Plan was developed on lands across Canada, and we invite readers to reflect on the generations of First Nations, Inuit and Métis who have thrived and sustained themselves in the territories which you call home, and urge readers to recognize local Indigenous knowledge, and contribute to cultural revitalization and self-determination for Indigenous communities.
With this acknowledgment, we recommit ourselves to a future of healing, understanding, and reconciliation, honoring the invaluable contributions of Indigenous Peoples, the original habitants of this land now called Canada, to our collective history and future.
Ministerial foreword
The Government of Canada is committed to achieving global targets to reduce HIV/AIDS, hepatitis B and C, and sexually transmitted infections by 2030. These goals cannot be achieved by the federal government alone; we will continue to work with our dedicated partners and stakeholders to support those impacted by sexually transmitted and blood-borne infections (STBBI). The renewal of the Government of Canada STBBI Action Plan builds on our ongoing collective efforts and outlines a new path forward.
It is important that all people living in Canada have access to the sexual and reproductive health services they need, no matter where they live. Presently, rates of HIV, hepatitis B and C, syphilis, and other sexually transmitted infections remain high. Although progress has been made through the work of community-based partners and innovations such as HIV self-test kits and point-of-care tests (POCT) for HIV and syphilis, there is much more to be done. Efforts need to be strengthened and realigned in response to changes in STBBI incidence within key populations.
This is a critical point in time where Canada's response to STBBI can be informed by lessons learned from the COVID-19 pandemic. COVID-19 taught us the importance of clear and effective public health messaging, research, innovation, tailored interventions for key populations, and the need for collaborative and multisectoral action. This renewed Action Plan reflects these lessons, positioning us to learn from the past and build a better future together.
As we move forward, it is important to reflect on our progress and how far we have come. Over the past year, the Government of Canada funded Indigenous-led community interventions that weave together traditional medicines with Western healing practices. Canada also endorsed the global declaration on Undetectable = Untransmittable (U=U), building on Canada's leadership as the first country to formally endorse the U=U campaign in 2018. These are only a few examples; other contributions can be found in our latest progress report.
Finally, I would like to express my gratitude to all those who dedicated their time and knowledge to inform and shape this new Action Plan. This Action Plan outlines priority areas and is based on what we heard from people with lived and living experience, community-based organizations, and key populations. Together, we have developed an Action Plan that reflects the diverse perspectives and needs of those affected by STBBI. Your ongoing support will be crucial in implementing this Action Plan.
Once again, I express my thanks to all the stakeholders, community organizations, and individuals with lived and living experience of STBBI. Your contributions have made a lasting impact and will serve as a guiding force in our efforts to create a more inclusive, compassionate, and healthier future for all. I commend your resilience and look forward to working together.
Acknowledgements
The Government of Canada extends its gratitude to all those who actively participated in shaping this Action Plan. Your invaluable contributions have played a crucial role in crafting a comprehensive plan and have provided the federal government with a blueprint for addressing STBBI. Diverse community partners and stakeholders, especially people with lived and living experience have played an instrumental role in the development of the Action Plan. We thank you for generously sharing your knowledge, stories, and insights. We acknowledge the time, expertise and dedication you have brought to this process. Your perspectives and collaborative spirit have enriched the dialogue, ensuring that the Action Plan is not only informed by evidence but also reflective of the diverse needs and realities of the communities it aims to serve.
Our partnerships will continue to advance our federal STBBI priorities, demonstrating a collective commitment to fostering positive health outcomes and overall well-being for all people in Canada. As we implement the plan, we look forward to continued collaboration, and growing and learning together.
Action plan in brief
Sexually transmitted and blood borne infections (STBBI) continue to be a public health concern that requires a rights-based, collaborative and holistic approach. The renewal of the Government of Canada's STBBI Action Plan aims to accelerate prevention, diagnosis, and treatment to reduce the health impacts of STBBI in Canada by 2030 and meet global commitments. The priorities outlined in this plan are driven by evidence and reflect today's realities, including advances in science, intersecting social and structural determinants of health, the lasting impacts of COVID-19, and emerging infectious diseases.
The renewal of the Action Plan underscores the Government of Canada's commitment to reduce the impact of STBBI, improve public health outcomes, and advance overall health and well-being. Through the priorities and actions outlined in this plan, the federal government aims to drive positive change, reduce disparities, complement provincial and territorial efforts, and contribute to a healthier and more inclusive society.
Action plan priorities
Enabling Environment
- Support First Nations, Inuit and Métis priorities, leadership and self-determination
- Address STBBI-related stigma and discrimination
- Improve STBBI data monitoring and collection practices
- Strengthen and support research capacity
- Provide ongoing support, exchange, and convening opportunities
Prevention
- Promote comprehensive sexual health and wellbeing across the life course
- Enhance awareness of, and access to, biomedical STBBI prevention tools
- Advance development and uptake of vaccines and prevention innovations
- Support harm reduction programs and services
- Respond to emerging and reemerging infections
Testing
- Expand the availability of a range of testing modalities
- Improve access to STBBI testing for key populations and the general population
Initiation of Care and Treatment
- Facilitate access to wrap-around care and support
- Provide care for populations with health services or coverage from the federal government
Ongoing Care and Support
- Reinforce the importance of person-centered, trauma-informed, and linguistically and culturally relevant care
- Recognize and support peer-based approaches within the STBBI response
Section 1: Setting the stage
Overview of the action plan
In 2019, the Government of Canada released its Five-Year Action Plan on Sexually Transmitted and Blood-Borne Infections, which outlined the Government of Canada's role, priorities, actions and commitments for implementing the Pan-Canadian STBBI Framework for Action over five years (2019-2024).
The Government of Canada's renewed 2024-2030 STBBI Action Plan builds on our progress to date and reaffirms our commitment to achieve the World Health Organization (WHO) 2030 global STBBI targets. This renewed plan integrates advances in science and research, focuses on health equity and equity-deserving populations, acknowledges post-pandemic realities, and incorporates stakeholder and partner insights and expertise. Over several months in 2023, we consulted with stakeholders, rights holders and partners via an online survey, roundtable discussions, key informant interviews, and participation at STBBI meetings and events. We heard from over eight hundred people across Canada, including members of key populations, health care professionals, members and representatives from community-based organizations, researchers, advocates and activists. Their input and expertise helped shape the priorities and actions the Government of Canada will undertake as part of this renewed Action Plan.
WHO 2030 Global STBBI Targets:
HIV
- Zero new HIV infections
- Zero AIDS-related deaths
- Zero discrimination
Hepatitis
- 90% reduction in new cases of chronic viral hepatitis B and C infections
- 65% reduction in hepatitis B and C deaths
- 90% of viral hepatitis B and C infections are diagnosed
- 80% of eligible people receiving hepatitis B and C treatment
Sexually Transmitted Infections
- 90% reduction of syphilis incidence globally
- 90% reduction in gonorrhea incidence globally
- 50 or fewer cases of congenital syphilis per 100,000 live births in 80% of countries
- Sustain 90% national coverage and at least 80% in every district (or equivalent administrative unit) in countries with the human papillomavirus vaccine in their national immunization programme
Our objective is to accelerate prevention, diagnosis, and treatment to reduce the health impacts of STBBI in Canada by 2030 and to meet our global commitments. We also aim to address STBBI-related stigma and dispel misconceptions, promote understanding, and create more inclusive and supportive environments.
Guiding document: Pan-Canadian STBBI framework for action
Our Action Plan builds on an existing STBBI policy foundation, guided by the Pan-Canadian STBBI Framework for Action: Reducing the health impact of sexually transmitted and blood-borne infections in Canada by 2030, which was launched by federal, provincial and territorial Ministers of Health in 2018. The Framework provides a common vision and strategic goals to guide actions for all those involved in the STBBI response. In reviewing and implementing this federal STBBI Action Plan, it is important to recognize the interplay between provincial, territorial and federal health responsibilities in Canada. While each jurisdiction carries specific roles and mandates in addressing STBBI, there is a pressing need for collaboration and a cohesive, Canada-wide approach among all levels of government, stakeholders, partners, and affected populations to minimize the impact of STBBI in Canada.
Aligning with the Framework, this Action Plan focuses on key populations and four core pillars supported by the foundation of an enabling environment (Figure 1).
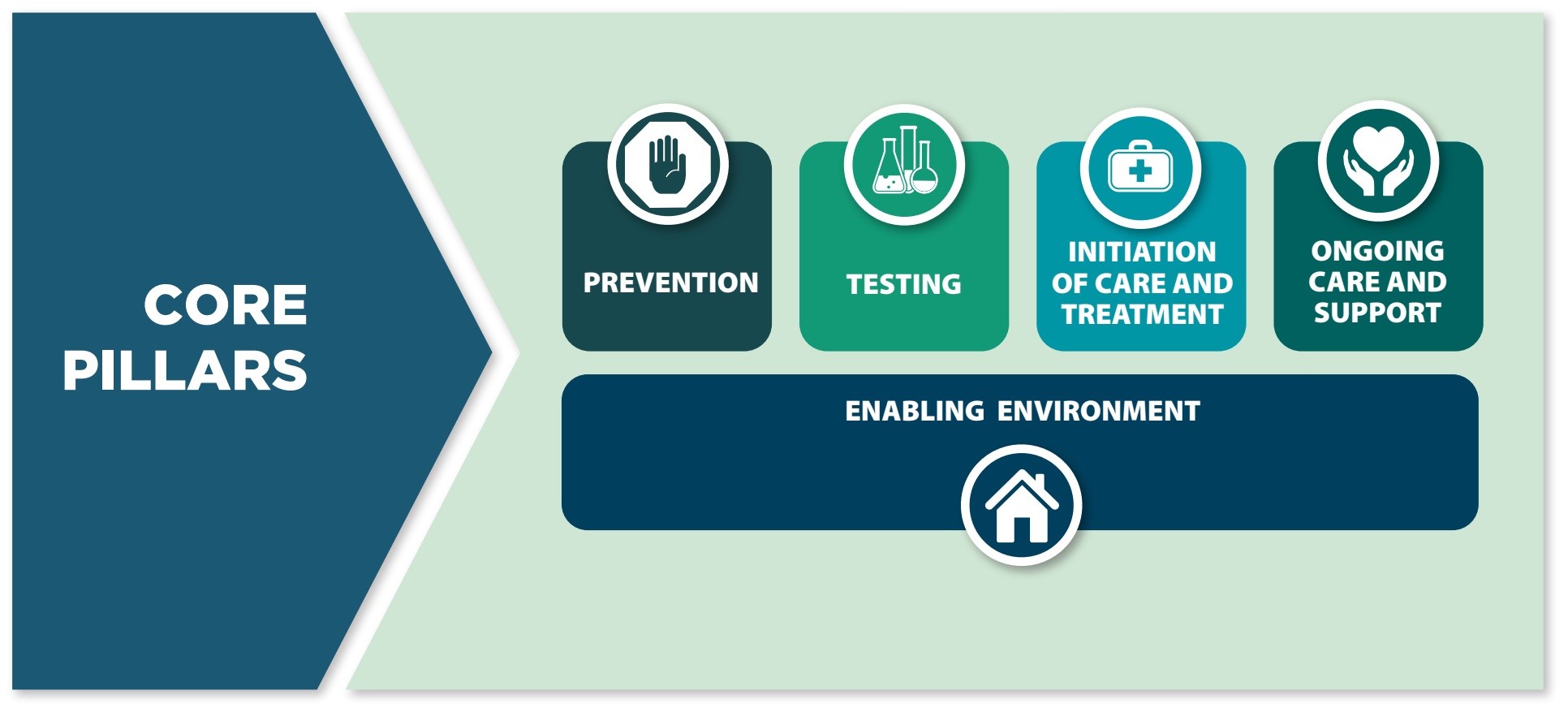
Figure 1 text equivalent description
The core pillars of the Pan-Canadian Sexually Transmitted and Blood-borne Infections Framework for Action are grouped into four areas which further identify the key opportunities for action that span the continuum of sexually transmitted and blood-borne infection care. The four core pillars include prevention, testing, initiation of care and treatment, and ongoing care and support.
Central to the four core pillars is an enabling environment. Opportunities for action within the enabling environment help to create the conditions to support successful sexually transmitted and blood-borne infection programs, policies, and actions that eliminate stigma and discrimination, and increase uptake, equitable coverage, and quality of health services.
This Action Plan will also be guided by the Guiding Principles from the Framework (Table 1).
Table 1. Action Plan Guiding Principles Footnote 1:
Meaningful engagement of people living with HIV and hepatitis B and C and key populations: People living with HIV and hepatitis B and C and key populations are meaningfully engaged in the development and implementation of policies and programs that affect them. This draws upon the principles of Greater Involvement of People Living with HIV/AIDS (GIPA) and the Meaningful Engagement of People Living with HIV/AIDS (MEPA). MEPA is a best practice approach that calls for the active and meaningful participation of people living with HIV in the establishment, development, implementation, monitoring and evaluation of HIV policies and programs.
Continued implementation of the Truth and Reconciliation Commission's Calls to Action: Policies and programs to address STBBI among Indigenous Peoples are developed by and with First Nations, Inuit and Métis communities through a relationship grounded in mutual respect and rooted in an understanding and recognition of and responsiveness to the ongoing impacts of colonization, health and social consequences of residential schools, structural inequities and systemic racism.
Integrated approach: Interventions and programs are designed to address the complexity and interrelated nature of risk factors and transmission routes for STBBI while recognizing that disease-specific approaches may be appropriate in some cases.
Cultural relevance: Policies and programs to address STBBI reflect and respect cultural realities and practices while ensuring the safety of individuals and communities.
Human rights: All people, regardless of their sexual orientation, race, culture, gender, abilities, or personal practices, are important and their human rights are recognized, respected and promoted.
Health equity: All people – regardless of sex, gender, race, income, sexual orientation, geographic location, status, age, or culture – have equitable access to opportunities and conditions that lead to better health for all.
Multi-sectoral approach: Multi-sectoral and multi-disciplinary approaches to prevention and care are embraced to improve collaboration and ensure interventions acknowledge the whole individual and their wellness needs.
Evidence-informed policy and programs: Interventions and programs are consistently developed with, and guided by, the most recent surveillance data, research and expertise from the community.
Section 2: STBBI landscape in Canada
Overview of STBBI trends globally and in Canada
There is a rise in STBBI globally, with more than 1 million STBBI being acquired every day Footnote 2. Infections that are transmitted through the exchange of genital fluids, through intimate skin-to-skin contact, or through contact with blood (e.g. via shared drug use equipment) are called STBBI. STBBI include chlamydia, gonorrhea, syphilis, human immunodeficiency virus (HIV), human papillomavirus virus (HPV), herpes simplex virus (HSV 1 and HSV 2), hepatitis B (HBV), and hepatitis C (HCV). In 2020, the World Health Organization (WHO) estimated 374 million new bacterial (chlamydia, gonorrhea and syphilis) sexually transmitted infections (STI) Footnote 3. Of global concern is the spread of antimicrobial resistant gonorrhea and Mycoplasma genitalium, outbreaks of syphilis and congenital syphilis, and the emergence of infections such as mpox (monkeypox) among sexual networks Footnote 4Footnote 5Footnote 6Footnote 7Footnote 8.
In Canada, there has been a lack of progress towards STBBI elimination. Similar to other countries, bacterial STI (chlamydia, gonorrhea, and syphilis) rates have been rising rapidly (see STBBI snapshot). Rates of hepatitis B and C, as well as HIV have not decreased in line with global targets. Since 2012, yearly cases and rates of HIV diagnoses in Canada have largely remained stable. Reported rates of acute HBV and cases of HCV have been relatively stable in recent years, despite an effective vaccine for preventing HBV and curative treatment for HCV Footnote 9Footnote 10. Other common STBBI, such as HSV 1, HSV 2 and HPV have limited incidence and prevalence data, yet continue to be of concern given their impact on health, stigma, quality of life, and their role in increasing the risk of acquiring or transmitting other STBBI, such as HIV.
Infectious syphilis rates increased by 109 % between 2018 and 2022, and the rate of congenital syphilis increased by 599% between 2018 and 2022 Footnote 11. Syphilis outbreaks have been declared in ten provinces and territories in 2018 and 2019Footnote 12. The number of cases among gay, bisexual, and other men who have sex with men have remained somewhat stable over time and the increased burden of disease (including increases in congenital syphilis) in recent years can be explained by the increase among heterosexual populations and females Footnote 13.
Research on the rising rates of syphilis, published in the Canadian Communicable Disease Report, indicates that social and structural determinants of health and health inequities undoubtedly play a crucial role in the inequitable occurrence of syphilis across different populations. These determinants include housing instability, experiences of violence, lack of access to culturally appropriate care, and experiences of stigma, discrimination and racism, particularly within the healthcare system Footnote 14.
STBBI data reported for the years 2020-2022 should be interpreted within the context of the COVID-19 pandemic (see STBBI snapshot). Reductions in STBBI rates and subsequent rebounds may be attributed to a decrease in demand for and ability to provide services related to STBBI during the pandemic, as reported in the Canadian COVID-19 STBBI impact surveysFootnote 15Footnote 16Footnote 17Footnote 18. information collected in the COVID-19 surveys provide context to better interpret STBBI trends during that time. They also indicate how populations disproportionately impacted by STBBI experienced deteriorating social determinants of health (employment or income loss, increased food insecurity, and feeling less safe in the home) and higher demand for mental health services coupled with barriers to access these services and increases in substance use. Taken together, these findings underscore the importance of prioritizing health equity.
Snapshot of STBBI in Canada
The latest nationally notifiable STBBI data are available on the Government of Canada's website: STBBI Canada.
Human Immunodeficiency Virus (HIV)
In 2020, an estimated 62,790 people in Canada were living with HIV Footnote 19. In 2022, 4.7 new diagnoses of HIV per 100,000 people were reported Footnote 20.
HIV disproportionately impacts key populations; gbMSM, people who inject drugs, Indigenous Peoples, and Black populations were estimated to represent 39.7%, 21.9%, 23.9%, and 15.4% of new HIV diagnoses in 2021, respectively Footnote 19Footnote 21. As race and/or ethnicity information was only available for 45.3% of individuals who were newly diagnosed in 2021, the proportions for Indigenous Peoples and Black populations must be interpreted with caution Footnote 21.
Infectious and Congenital Syphilis
Infectious syphilis increased by 109% between 2018 and 2022, and outbreaks were declared in 10 provinces and territories in 2018 and 2019 Footnote 11Footnote 12.
Cases reported among gbMSM represented 27% of all reported infectious syphilis cases in 2022, with increasing rates of infectious syphilis among the heterosexual population, and sharp increases among females. Cases of confirmed early congenital syphilis have increased markedly from 4 cases in 2016 to 117 confirmed cases in 2022 Footnote 11.
Hepatitis B (HBV)
In 2021, 3,524 cases of hepatitis B (acute, chronic, and unspecified cases combined) were reported for a rate of 9.2 cases per 100,000 people Footnote 22.
Nearly half of people with chronic HBV in Canada may be unaware of their status Footnote 23.
Certain communities and groups are more likely to have HBV, including migrants from countries with higher rates of HBV, gbMSM, people who inject drugs, Indigenous Peoples, people who experience unstable housing, people who have been incarcerated, and sex workers Footnote 24.
Chlamydia
In 2021, the national rate was 273.2 per 100,000 people Footnote 25. Reported rates of chlamydia increased by 22% between 2012 and 2019 in Canada Footnote 25.
During the first year of the COVID-19 pandemic (2020), the rate of nationally reported chlamydia cases dropped by 25% compared to 2019 Footnote 25.The rate remained stable in 2021 Footnote 25.
Chlamydia is most commonly reported among people younger than 30 years of age, increasing their susceptibility to HIV infection and other harmful effects, like infertility Footnote 12.
Hepatitis C (HCV)
In 2021, 7,535 cases of hepatitis C (acute, chronic and unspecified combined) were reported for a rate of 19.7 cases per 100,000 people Footnote 26. Rates varied significantly between jurisdictions Footnote 26.
Estimates indicate that in 2019, approximately 1 in 4 people who were ever exposed to the hepatitis C virus were undiagnosed Footnote 27.
Encouragingly, with the introduction of highly effective HCV treatment in Canada in 2014, it is estimated that more people were treated than there were new infections between 2017 and 2019 Footnote 27.
Gonorrhea
The national rate in 2021 was 84.2 per 100,000 Footnote 25.
Between 2012 and 2019 gonorrhea increased by 151% Footnote 12. In 2020, the rate of reported gonorrhea cases dropped by 14% compared to 2019, with a 4% rebound in 2021 Footnote 25.
The proportion of tested gonorrhea isolates identified as multi-drug resistant increased from 8.6% in 2015 to 12.4% in 2019 Footnote 28.
Notes on snapshot data:
- Canadian data on STBBI are collected through national public health surveillance. Most STBBI are nationally notifiable, meaning that provincial and territorial public health authorities share de-identified data on cases of STBBI diagnosed in their jurisdictions annually Footnote 29. The Public Health Agency of Canada conducts routine surveillance on the following nationally notifiable STBBI: Chlamydia, Gonorrhea, Syphilis, Hepatitis B, Hepatitis C, and HIV. Additional data among specific populations are available through enhanced and biobehavioural surveillanceFootnote 13Footnote 14Footnote 30Footnote 31.
- The term "surveillance" is often used to describe public health activities to understand trends in infectious diseases. We recognize that "surveillance" is also used by law enforcement, private security, and other parties for a different purpose. As a result, the term can raise discomfort or have negative meanings for some individuals and communities, especially racialized, 2SLGBTQI+, people who use drugs, people experiencing homelessness, and other marginalized populations. For public health STBBI surveillance, the minimum amount of data necessary is collected. Only provincial or territorial public health authorities have access to personal identifiable information (e.g., name or personal health card number) which are used for the purposes of providing health services and they remove this information before sending data to national systems. All data is stored securely and access to it is highly restricted. The reports created using national data are about trends, not people.
The social determinants of health and their impact on STBBI
Anti-Black racism is a system of inequities that discriminates against people from African, Caribbean and Black (ACB) communities. It is informed by the historical enslavement of ACB communities as well as by colonial practices, policies and frameworks, which become embedded in institutions (including public health systems) as systemic inequality Footnote 32.
Anti-Indigenous racism refers to race-based discrimination, negative stereotyping, prejudices and injustice experienced by Indigenous Peoples. It is fueled by colonial practices, policies, and frameworks that contribute to the establishment, maintenance, perpetuation of power imbalances and structural obstacles for Indigenous Peoples Footnote 32.
Within these national trends is great variability across populations and regions. STBBI do not affect all people equally. Contextual factors, like the social determinants of health, and legal, political and historical factors, influence vulnerability and resilience to STBBI. Experiences of stigma, discrimination and marginalization based on race/ethnicity, intergenerational trauma, disability, immigration status, social class, sexual orientation, gender identity, drug use, lived experience of incarceration, and involvement in sex work contribute to social and structural inequities. Inequities in education, employment, income, food security, mental health support, housing and health and social services influence risks for the acquisition of STBBI directly and indirectly Footnote 1. These experiences and social and structural inequities help explain why STBBI disproportionately impact certain key populations Footnote 19Footnote 27Footnote 33Footnote 34 (Table 2. Key Populations). Despite these potentially difficult circumstances, it is important to acknowledge individuals and communities' strength, uniqueness, and resilience.
Table 2. Key Populations affected by STBBI in Canada:
- First Nations, Inuit, and Métis communities;
- African, Caribbean, and Black communities and other racialized people;
- Gay, bisexual and other men who have sex with men (gbMSM);
- Two-spirit people;
- Transgender and non-binary persons;
- People who use drugs;
- People who experience incarceration;
- Sex workers and their clients;
- People living with HIV and people with lived and living experience of hepatitis;
- Newcomers, migrants and immigrants to Canada, particularly from regions with high HIV, hepatitis B or hepatitis C prevalence;
- Women among these populations, as appropriate
- Youth among these populations, as appropriate
NB: An intersectional lens is required as people may belong to multiple groups.
Addressing STBBI - challenges and advances
Although STBBI are preventable and, in many cases treatable or curable, many people experience negative impacts on their health and well-being, especially when treatment is delayed. A person with a STBBI can experience pain, certain cancers, immune deficiency, psychological distress, infertility, and adverse birth outcomes such as miscarriage, congenital defects and stillbirth Footnote 35Footnote 36Footnote 37. In addition to the burden on individual health Footnote 38, and quality of life, STBBI also lead to substantial healthcare utilization and related costs Footnote 39. Key populations also experience stigma and discrimination related to their infection, including in healthcare settings Footnote 19Footnote 33Footnote 40. For example, people who are involved in sex work and people who use drugs experience additional barriers to care due to stigma associated with substance use and sex work, respectively. This stigma prevents them from seeking care, elevating their STBBI-related risks.
Evidence suggests that criminalization of non-disclosure of HIV prior to otherwise consensual sexual activity can lead to the stigmatization of people living with HIV, which may discourage individuals from getting tested or seeking treatment. There has also been considerable progress in terms of HIV treatment, as reflected in the scientific evidence on rates of transmissibility. Together, these points suggest that it is prudent to periodically review criminal laws related to HIV non-disclosure Footnote 41.
Canada's unrelenting overdose and toxic drug crisis also poses additional challenges in addressing the elevated risk of STBBI among people who use drugs. From January 2016 to June 2023, there was a total of 40,642 apparent opioid toxicity deaths and a total of 39,435 opioid related and 16,863 stimulant related poisoning hospitalizations Footnote 42. The use of substances through intravenous injection or inhalation places individuals at a higher risk of contracting STBBI. In addition, the increasingly toxic drug supply also adds layers of complexity to healthcare interventions for both substance use related harms and STBBI and community organizations serving these key populations, which strains existing resources Footnote 42. Recognizing that harms related to opioids, stimulants, and other substances extend beyond overdoses/poisonings and deaths, we will continue to work with partners to support a whole of government approach to this public health crisis that addresses the broader health needs of people who use drugs.
Furthermore, challenges in the treatment of STBBI include the rise of antibiotic resistance. Antimicrobial resistance (AMR) is increasing globally due to the overuse and misuse of antimicrobials, the global movement of people, and socio-economic and health system inequities around the world. Specifically, multidrug resistance is rapidly increasing for gonorrhea, with resistance being reported against both first- and last-line antibiotics resulting in challenges to treatment including treatment failure Footnote 43Footnote 44. Antibiotic resistance increases the individual and health system burden of gonorrhea by prolonging infections and increasing the number of people with long-term complications of gonococcal infections (e.g., infertility, newborn eye infections and blindness) Footnote 43. Canada has also experienced a recent emergence in the occurrence of Shigella. This is of particular concern as the majority of these cases are also multidrug resistant. This mirrors the trend worldwide, with global reports of persistent transmission of shigellosis impacting the gbMSM community Footnote 45Footnote 46. Other factors that continue to impede the prevention and management of STBBI include social inequities, limited knowledge and awareness of STBBI testing and screening, under-resourced health Footnote 1.
Despite these challenges, there is reason for optimism and a renewed resolve as we have more prevention, diagnosis, and treatment tools than ever before. Our collective response to STBBI is anchored in 40 years of a robust, partnership-based HIV response across community, industry, policy and research. During the 2022 mpox outbreak these partnerships allowed for rapid mobilization, which enabled evidence-based information and vaccines to reach communities that needed it Footnote 7.
Further, the range of effective STBBI prevention strategies has expanded (e.g., HIV PrEP), and others are being actively studied at the time of writing (e.g., doxycycline for bacterial STI prophylaxis, vaccine for gonorrhea). New diagnostic modalities have also expanded access to testing (e.g., HIV self-tests, HCV, HIV/syphilis point-of-care tests, decentralized community-based testing, and dried blood spot-testing). Direct-acting antivirals for HCV means a cure is possible for the majority of people who acquire HCV and treatment for people with chronic HBV helps prevent long term consequences, including liver cirrhosis and cancer Footnote 47Footnote 48. Bacterial STI such as syphilis, gonorrhea, and chlamydia are curable with antibiotic treatments Footnote 49. While herpes and chronic HBV are long-term chronic infections, timely treatment reduces negative health impacts Footnote 49. In the case of herpes, treatment can help relieve symptoms and prevent transmission to newborns, especially when the primary infection occurs during pregnancy Footnote 49. Further, antiretroviral therapies enable people with HIV to live long, healthy lives and prevent onward transmission Footnote 49.
HIV Pre-exposure Prophylaxis (PrEP): An HIV prevention strategy in which a person who does not have HIV takes antiretroviral medications on an ongoing basis, starting before being potentially exposed to HIV.
HIV Post-exposure Prophylaxis (PEP): An HIV prevention strategy in which a person who does not have HIV takes antiretroviral medicines after being potentially exposed to HIV to reduce their risk of becoming infected.
Scientific studies show that HIV is not passed on through sex when a person living with HIV is on treatment and the amount of HIV in their blood remains very low (maintains a viral load of <200 copies/mL). This scientific advancement has been confirmed through a review of the evidence in 2023 Footnote 41. Raising awareness regarding HIV treatment as prevention through the Undetectable = Untransmittable (U=U) campaign can help alleviate HIV related stigma and improve quality of life Footnote 50Footnote 51. Knowledge of U=U increases uptake in HIV testing, treatment and achieving viral suppression, all of which supports progress toward the 95-95-95 HIV targets, and the global goal of ending HIV and AIDS as a public health concern by 2030. However, it is also important to note that, in campaigning around U=U, there are some people who cannot, for various reasons, achieve this level of viral suppression.
Undetectable = Untransmittable (U=U): A health promotion campaign used to communicate the scientific consensus that HIV is not passed through sex when a person living with HIV is on treatment and the amount of HIV in their blood remains very low (maintains a viral load of <200 copies/ml measured every 4-6 months) Footnote 52.
Section 3: Government of Canada priorities and actions
This Action Plan follows the format of the Pan-Canadian STBBI Framework with four core pillars - prevention, testing, initiation of care and treatment, and ongoing care and support - and the enabling environment as the foundation of those pillars. Within this Action Plan are 16 interrelated priorities that will guide federal actions over six years (2024-2030).
These priorities and actions were developed in consideration of input from stakeholders and partners. For each pillar and foundation, select quotes from stakeholder consultations illustrate the value these priority areas hold for our partners. Where appropriate, these priorities and actions are meant to apply across all key populations and all STBBI over six years (2024-2030). They serve as a guide to develop targeted interventions and programs that are evidence-based and tailored to the needs of specific populations. They emphasize a holistic approach, considering medical, social, and behavioural aspects of STBBI and acknowledge the importance of inclusive, comprehensive and coordinated efforts among diverse stakeholders and jurisdictions. Each action is attributed to lead federal departments and is accompanied by an indicator (Appendix A) to facilitate reporting on our progress. The mandates of each of the contributing federal departments are described in Table 3, as they relate to STBBI.
Table 3. Federal Departments contributing to the Action Plan
Canadian Institutes of Health Research (CIHR)
- CIHR is Canada's federal funding agency for health research. CIHR excels in the creation of new knowledge and its translation into improved health for Canadians, more effective health services and products, and a strengthened Canadian health care system.
Correctional Service Canada (CSC)
- CSC provides federally incarcerated individuals with efficient, effective health services that encourage individual responsibility, promote healthy reintegration, and contribute to safe communities.
Department of Justice (DOJ)
- DOJ acts as a policy department with broad responsibilities for overseeing all matters relating to the administration of justice that fall within the federal domain-in this capacity, it helps to ensure a fair, relevant and accessible justice system for all Canadians.
Department of National Defence (DND)
- DND provides a full spectrum of safe, high-quality health services through a well-governed health care system that meets or exceeds Canadian standards, both in garrison and during operations.
Health Canada (HC)
- HC works to increase access to high-quality health services, and to reduce health risks by educating the public on drugs and other substances, diseases and more; regulating drugs and health products to support public safety; and helping the public make informed decisions about health through science, research and testing.
Public Health Agency of Canada (PHAC)
- PHAC works to prevent and control infectious diseases; serves as a central point for sharing Canada's public health expertise with the rest of the world; and applies domestic and international research to Canada's public health programs.
Immigration, Refugees, and Citizenship Canada (IRCC)
- IRCC and specifically IRCC's Migration Health Branch, is the Government of Canada's centre of expertise for the management of health-related aspects of migration, including health screening, medical surveillance and notification, and the Interim Federal Health Program.
Indigenous Services Canada (ISC)
- ISC supports provinces and territories to improve access to high quality services for First Nations, Inuit, and Métis. ISC's vision is to support and empower Indigenous Peoples to deliver services and address socio-economic conditions.
Women and Gender Equality (WAGE)
- WAGE works to advance equality with respect to sex, sexual orientation, and gender identity or expression through the inclusion of people of all genders, including women, in Canada's economic, social, and political life.
Foundation: An enabling environment
"Without addressing the social determinants of health, we will be pushing the rock up the hill until the end of time." - Consultation Feedback
The enabling environment refers to the interrelated legal, social, cultural, physical and structural conditions that support successful STBBI programs, policies and actions. Creating an enabling environment for the prevention and management of STBBI is critical to foster equitable access to health services. By recognizing the importance of social determinants of health, supporting community-led responses, improving data practices, addressing stigma, and continuously sharing lessons learned, we can work towards creating environments that enable individuals and communities to make informed choices, protect their health and well-being, and seek testing and treatment without fear of stigma, discrimination, or criminalization.
To foster a strong enabling environment, the Government of Canada will take action on the following five priorities:
- Support First Nations, Inuit and Métis priorities, leadership and self-determination
- Address STBBI-related stigma and discrimination
- Improve STBBI data monitoring and collection practices
- Strengthen and support research capacity
- Provide ongoing support, exchange, and convening opportunities
| Actions | Lead Department |
|---|---|
| Priority: Support First Nations, Inuit and Métis priorities, leadership and self-determination | |
Support First Nations, Inuit and Métis led initiatives and priorities, in line with existing declarations that aim to eliminate anti-Indigenous racism in the health system. This includes the Truth and Reconciliation Commission's Calls to Action 18-24 |
All |
Foster a cadre of First Nations, Inuit and Métis researchers by providing funding for training, mentorship, and other supports that enable long and productive careers |
CIHR |
Build and sustain rapid testing capacity and reduce barriers to testing in underserved populations, particularly First Nations, Inuit and Métis communities, through the Northern, Remote and Isolated (NRI) Initiative |
PHAC, ISC |
Advocate for long-term funding to First Nations, Inuit and Métis led organizations (i.e., 10-years), wherever possible |
ISC |
| Priority: Address STBBI-related stigma and discrimination | |
Implement knowledge mobilization efforts to increase awareness of Undetectable=Untransmittable (U=U) message and HIV-related stigma among key populations, health professionals, and the general public |
PHAC |
Address STBBI related stigma and discrimination through comprehensive and ongoing knowledge mobilization activities and messaging that promotes STBBI prevention testing, treatment and care as integral components of a broader, holistic approach to health and well-being |
PHAC |
Develop research and community-based funding opportunities to understand, address and reduce the impact of stigma, racism, homophobia, transphobia, sexism and other forms of discrimination and systemically entrenched oppression |
CIHR |
Promote stigma reduction through public education efforts (e.g., national and targeted advertising), engaging people with lived experience, supporting organizations working to reduce stigma (e.g., via SUAP), and fostering partnerships that support the uptake of best practices for stigma reduction. These initiatives complement and support activities in the Canadian Drugs and Substances Strategy (CDSS) |
HC |
Synthesize and disseminate evidence on HIV transmission risk and the public health implications |
PHAC |
Establish culturally safe and accessible diagnostic services for urban isolated populations |
PHAC |
Continue to work toward reducing the over-criminalization of HIV non-disclosure in Canada |
DOJ |
| Priority: Improve STBBI data monitoring and collection practices | |
Improve monitoring of STBBI trends and progress for key populations, regions, ages, sexes, and race/ethnicity, and facilitate access to data on key STBBI (i.e., STBBI dashboard) |
PHAC |
Review and adapt national surveillance methods in collaboration with partners (including provinces and territories, First Nations, Inuit, Métis and other community-based partners) to improve reporting on STBBI epidemiology and monitor progress toward elimination goals |
PHAC, ISC |
Collaborate with communities affected by STBBI to support responsible and culturally appropriate practices in relation to data collection, stewardship, reporting standards, guidance and knowledge products, integrating diverse ways of understanding health and well-being, including Indigenous Ways of Knowing and Doing as appropriate |
PHAC |
Support data collection, analysis, research and knowledge on 2SLGBTQI+ communities to help inform the provision of healthcare services to 2SLGBTQI+ communities, including the importance of sexual health, experiences of stigma and discrimination and risk of STBBI |
WAGE |
| Priority: Strengthen and support research capacity | |
Develop and invest in knowledge mobilization which promotes community-centered and holistic approaches to research that advances the meaningful engagement of community members and people with lived experience throughout the research process |
CIHR |
Develop training initiatives that foster inter-and transdisciplinary approaches and support the current and next generation of HIV/AIDS and STBBI researchers in developing skills to integrate new technologies and methods in their research |
CIHR |
Support HIV/AIDS and STBBI researchers across their career journey by providing professional development supports (e.g., networking, mentorship) and strategic funding opportunities with a focus on researchers and trainees from underrepresented groups, those who are navigating early- and mid-career transitions and those leading research in the community setting |
CIHR |
| Priority: Provide ongoing support, exchange, and convening opportunities | |
Convene STBBI stakeholders and partners including HIV and Hepatitis C Community Action Fund (CAF) and Harm Reduction Fund (HRF) recipients, people with lived and living experience and national STBBI community to share wise practices, ongoing challenges, and lessons learned through various mechanisms (i.e. webinars, storytelling, meetings, working groups) |
PHAC |
Pillar 1: Prevention
"The narrative is all about doom and gloom. We need to normalize sex in these conversations." - Consultation Feedback
Policies and programs that aim to increase knowledge, change attitudes and behaviours, and support the uptake of existing and emerging prevention technologies are essential for decreasing new infections in Canada Footnote 1. Over the past several decades, STBBI prevention tools have significantly expanded as a result of scientific advances. Comprehensive sexual health education, and the consistent and correct use of condoms and sterile drug equipment remain critical to prevention Footnote 1. Provinces and territories play a central role in local STBBI prevention efforts and in tailoring strategies for regional needs and communities. Inclusive and culturally appropriate interventions that meaningfully involve people with lived and living experience
Comprehensive sexual health education gives people accurate, age-appropriate information and skill-building opportunities about sexuality, and their sexual and reproductive health. This is critical for overall health and well-being across the lifespan.
To enhance prevention efforts, the Government of Canada will take action on the following five priorities:
- Promote comprehensive sexual health and wellbeing across the life course
- Enhance awareness of, and access to, biomedical STBBI prevention tools
- Advance development and uptake of vaccines and prevention innovations
- Support harm reduction programs and services
- Respond to emerging and reemerging infections
| Actions | Lead Department |
|---|---|
| Priority: Promote comprehensive sexual health and wellbeing across the life course | |
Support initiatives and develop knowledge mobilization activities that promote sexual health as more than the absence of disease and work towards normalizing sexual health conversations (e.g., inclusive, strength-based, culturally appropriate, linguistically diverse, peer-to-peer based approaches) |
PHAC, HC |
Fund strength-based initiatives that are culturally safe and aimed at building capacity, adaptation, resilience, and empowerment by partnering within existing federal funding programs focused on health promotion (i.e., positive mental health, intersectoral factors, early childhood education) |
PHAC, ISC, HC |
Build on sexual and reproductive health research to enhance understanding of sex, gender, sexuality and systemic barriers in shaping experiences, risks and outcomes of STBBI |
CIHR |
Deliver comprehensive STBBI preventive services, including health education during basic training and deployment, HPV vaccination, and HIV PrEP/PEP, to all Canadian Armed Forces members according to clinical practice guidelines |
DND |
| Priority: Enhance awareness of, and access to, biomedical STBBI prevention tools | |
Provide policy and technical guidance based on evidence synthesis, cost effectiveness, efficacy, and best practice examples to inform the uptake of evidence based biomedical prevention tools (e.g., HIV PrEP and vaccination) and other potentially emerging biomedical prevention tools (e.g., STI PEP/PrEP, vaginal rings, injectables) |
PHAC |
| Priority: Advance development and uptake of vaccines and prevention innovations | |
Develop research funding opportunities to advance the design, development and implementation of next-generation interventions (i.e., vaccines, multipurpose prevention technologies, long-acting injectable antiretrovirals, and anti-bacterials) |
CIHR |
Provide public health guidance, based on scientific evidence and best practices, on existing and emerging vaccines through the National Advisory Committee on Immunization |
PHAC |
Establish a vaccination pilot project to offer vaccines on a voluntary basis, where accessible and available, against vaccine preventable diseases including Hepatitis B to IRCC clients at the time of the Immigration Medical Exam |
IRCC |
| Priority: Support harm reduction programs and services | |
Invest in community-based and community-led projects that incorporate harm reduction approaches to meet the needs of key populations, including substance related harms through the CAF, HRF and Substance Use and Addictions Program (SUAP) |
PHAC, ISC, HC |
Extend the Prison Needle Exchange Program and Overdose Prevention Service to strengthen efforts to prevent STBBI at federal correctional facilities across Canada |
CSC |
Support avenues that divert individuals found in possession of controlled substances away from the criminal justice system, including alternatives to prosecution, and where appropriate, refer them to the relevant health and social services |
DOJ |
Support the establishment of supervised consumption sites and temporary urgent public health need sites (known as overdose prevention sites) using streamlined regulatory approvals, in collaboration with provinces and territories as part of complementary and supporting activities through the Canadian Drugs and Substances Strategy (CDSS) |
HC |
Strengthen public policy and guidance to support harm reduction and health promotion efforts in the context of sexualized drug use |
PHAC |
| Priority: Respond to emerging and reemerging infections | |
Develop and invest in research funding opportunities that address and contribute to timely, culturally relevant and effective responses to emerging and re-emerging infections spread through sexual contact (e.g., infectious syphilis, congenital syphilis, mpox). |
CIHR, PHAC, ISC |
Strengthen public health capacity to respond to emerging and re-emerging STBBI public health threats by developing robust risk assessment processes and by embedding public health personnel in provinces and territories |
PHAC |
Adapt federal grants and contributions to respond to current priorities based on latest epidemiological data, including new and emerging infections |
PHAC |
Pillar 2: Testing
"We need to normalize testing. Baseline knowledge is very, very low, and how we communicate risk. There is so much shame around STBBI." - Consultation Feedback
Early detection of STBBI through testing enables timely diagnosis and treatment, improving health outcomes, preventing long-term harms and reducing the spread of STBBI. Testing, especially when integrated with counselling, education, and information about testing options, rights regarding privacy, and legal implications, can also support informed sexual health decision-making about safer sexual practices and consensual sexual activities. Given that testing and treatment services tend to be centralized in urban areas, this can present a barrier for rural, remote and isolated communities and those who cannot travel or access these services easily. By supporting the implementation of comprehensive testing strategies and new diagnostic tools, such as self-test kits and point-of-care testing, we can increase the availability of testing services and reduce barriers to testing. Access to a range of innovative testing practices including anonymous and non-nominal (i.e., using a code or initials) testing options is also important to implement. While testing primarily falls under provincial and territorial jurisdiction, there are actions the federal government can take.
To increase testing availability and access, the Government of Canada will take action on the following two priorities:
- Expand the availability of a range of testing modalities
- Improve access to STBBI testing for key populations and the general population
| Actions | Lead Department |
|---|---|
| Priority: Expand the availability of a range of testing modalities | |
Utilize regulatory and policy tools to facilitate access to STBBI tests on the Canadian market (i.e., pre-submission meetings with manufacturers to ensure regulatory requirements will be met, identification of tests for priority review, enabling access to unlicensed medical devices for health care professionals through the Special Access Program) |
HC |
Increase timely access to STBBI tests in Canada through international collaborations such as the joint US/Canada submission portals and the World Health Organization (WHO) joint assessment sessions for in-vitro diagnostic devices |
HC |
Invest in research for innovative technologies for testing and surveillance to better detect, characterize and monitor STBBI |
CIHR |
| Priority: Improve access to STBBI testing for key populations and the general population | |
Promote evidence informed STBBI testing strategies as part of overall sexual health and wellbeing for the general population, with targeted approaches among key populations including funding community-based approaches to reach the undiagnosed through the CAF |
PHAC |
Encourage testing and treatment in correctional facilities, supported by the direction of the National Infectious Diseases Medical Advisor |
CSC |
Develop and invest in funding opportunities focused on implementation science research to better understand, define and integrate the context, conditions and adjustments that will maximize uptake and adoption of new and existing testing modalities in different health, social and cultural settings |
CIHR |
Develop and deploy low barrier technologies that supports equitable access to high quality screening and confirmatory testing |
PHAC |
Pillar 3: Initiation of care and treatment
"Even if there is a huge testing initiative, then what? There is no support post-testing. You need to get people in treatment to get to U=U." - Consultation Feedback
Facilitating timely initiation of care and treatment for individuals diagnosed with an STBBI is crucial to improving health outcomes, reducing transmission rates, and enabling better quality of life. Advancements in STBBI research and treatment have had profound effects, notably in the treatment of HIV and HCV.
Despite available treatment options, inequities and challenges remain in terms of accessing STBBI treatment, ranging from geographic location to lack of coverage for STBBI treatments. Further, concerns about confidentiality, fear of stigma, anti-Black and anti-Indigenous racism, discrimination and violence, loss of personal relationships, and personal or cultural beliefs about sexual health and treatment options can also discourage or delay treatment.
While the delivery of health and social services, including the provision of treatment and care of STBBI, is the primary responsibility of provinces and territories the federal government and community organizations serve as partners in this collective effort. Local, regional, and provincial/territorial entities are on the front lines delivering prevention, treatment, and support services, while community organizations play a crucial role in providing targeted interventions, raising awareness, and facilitating access to care for key populations.
There are instances where the federal government provides treatment, or coverage for treatment, to federally served populations such as registered First Nations, and eligible Inuit, serving members of the Canadian Armed Forces, eligible veterans, people in federal penitentiaries, and refugees, refugee claimants, protected persons and victims of human trafficking through the Interim Federal Health Program. The federal government establishes national frameworks and guidelines that support the coordination and harmonization of efforts across provinces and territories, provides leadership and resources, and convenes provinces/territories, community organizations and other stakeholders to collaboratively address STBBI.
To facilitate timely initiation of care and treatment, the Government of Canada will take action on the following two priorities:
- Facilitate access to wrap-around care & support
- Provide care for populations with health services or coverage from the federal government
| Actions | Lead Department |
|---|---|
| Priority: Facilitate access to wrap-around care & support | |
Assess and report on ongoing gaps for STBBI treatment and care, through monitoring, surveillance, and storytelling to inform uptake initiatives among key populations |
PHAC |
Develop culturally appropriate and gender affirming and gender inclusive information, tools and resources to facilitate access to care |
PHAC |
| Priority: Provide care for populations with health services or coverage from the federal government | |
Provide ongoing voluntary STBBI testing, treatment and health services for eligible individuals, including serving members of the Canadian Armed Forces, certain immigrant populations, people living in federal correctional facilities, and registered First Nations and eligible Inuit |
ISC, CSC, DND, IRCC |
Pillar 4: Ongoing care and support
"We need to understand equity within the ever-present intersectionality. And for care providers, we need trauma informed, culturally safe care. Services need to be decolonized." - Consultation Feedback
Providing ongoing care and support for individuals living with chronic STBBI such as HIV, HBV or herpes is essential to promote overall well-being, manage the long-term impact of infections, and reduce stigma. Ongoing care is also important given the now long-term, chronic nature of HIV and the concurrent conditions faced by people living and aging with HIV. A compassionate support system that encompasses medical care, mental health support, peer networks, and community resources can help improve people's treatment adherence and quality of life. Holistic, culturally relevant, person-centred care focusing on the needs and priorities of individuals is essential as people living with or experiencing an STBBI often require care that extends beyond physical symptoms Footnote 1. Services must reflect the diversity of individuals living with STBBI and address a range of psychological, emotional, cultural, physical health, and practical needs Footnote 1. Initiatives that focus on increasing family-based and community wellness are also critical to our STBBI response.
Complex health system navigation, limited information about available services, stigmatizing health care encounters including anti-Indigenous and anti-Black racism and marginalized or criminalized status create barriers to care and support Footnote 1. These barriers also intersect, and compound given peoples' social position. For instance, for people involved in sex work, STBBI barriers are further exacerbated by occupational stigma and discrimination, leading to delayed, denied, or complete avoidance of STBBI care Footnote 53.
Healthcare providers with limited STBBI knowledge also face challenges in providing comprehensive care and support Footnote 1. Thus, it is imperative to equip health care providers with resources and tools and to build the capacity of a wide range of providers in various settings to improve the accessibility of STBBI care. Provincial and territorial health care systems and community organizations play integral roles in delivering targeted, localized services that cater to the unique needs of affected individuals and communities. The federal government supports ongoing care and support by sharing best practices, resources, and tools, providing funding and convening key partners and stakeholders. This partnership ensures that efforts to address STBBI are cohesive, comprehensive, and well-coordinated, ultimately working towards the wellbeing and equitable health outcomes of all people in Canada.
To facilitate ongoing care and support, the Government of Canada will take action on the following two priorities:
- Reinforce the importance of person-centered, trauma-informed and linguistically and culturally relevant care
- Recognize and support peer-based approaches within the STBBI response
| Actions | Lead Department |
|---|---|
| Priority: Reinforce the importance of person-centered, trauma-informed and linguistically and culturally relevant care | |
Equip healthcare professionals with readily accessible resources, and tools to support the delivery of comprehensive, holistic, trauma-informed, stigma and discrimination free, and culturally safe STBBI and sexual health care and support |
PHAC, HC |
Facilitate opportunities for research to develop, test and advance culturally safe and holistic models of care and evidence-based interventions to achieve more equitable health outcomes |
CIHR |
Collaborate with community stakeholders to co-design culturally appropriate and linguistically diverse tools, resources and campaigns to raise awareness of prevention, testing and treatment strategies (e.g., HIV PrEP, mpox, HPV and HBV vaccination) with all key populations |
PHAC |
| Priority: Recognize and support peer-based approaches within the STBBI response | |
Support peers and peer-based approaches (e.g., peer navigation programs, peer networks) that guide and empower individuals in accessing care and support |
PHAC |
Section 4: Implementation
Engagement, partnership and leadership
The success of Canada's STBBI response depends on the commitment of all partners and stakeholders working within their respective roles. Ongoing engagement and dialogue with stakeholders is critical to the successful implementation of this plan. To advance our collective priorities, we are committed to working with key populations and community partners. Working closely with Indigenous governments to ensure our collective efforts meet the diverse needs of First Nations, Inuit and Métis communities is deeply important. We also want to align our response with the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP).
UNDRIP is a comprehensive international human rights instrument on the rights of Indigenous Peoples around the world. It affirms and sets out a broad range of collective and individual rights that constitute the minimum standards to protect the rights of Indigenous Peoples and to contribute to their survival, dignity and well-being. Since endorsing UNDRIP in 2016 the United Nations Declaration on the Rights of Indigenous Peoples Act received Royal Assent in Cananda on June 21st, 2021, and immediately came into force. The Government of Canada released a draft of The United Nations Declaration on the Rights of Indigenous Peoples Act Action Plan in March 2023.The Action Plan is an evergreen roadmap, with opportunities to renew and further co-develop its contents as part of the UN Declaration implementation process.
The Government of Canada will strengthen existing collaborations through senior-level interdepartmental tables that foreground STBBI issues. The implementation of the Action Plan will be facilitated through existing mechanisms such as the Syphilis Response Steering Committee, the Pan-Canadian Public Health Network, and regularly scheduled meetings across Government of Canada departments.
We will provide ongoing support, exchange and convening opportunities for our stakeholders and partners using existing mechanisms, such as the Black Expert Working Group for National HIV Surveillance. We will also explore new mechanisms for engagement with key populations, people with lived and living experience of STBBI and the national STBBI community.
Priorities in this STBBI Action Plan aligns with other Government of Canada Action Plans and Strategies, such as the 2SLGBTQI+ Action Plan, the CIHR HIV/AIDS and STBBI Research Initiative - Strategic Plan, the Antimicrobial Resistance Action Plan, the National Immunization Strategy, and the Canadian Drugs and Substances Strategy.
Measuring and sharing our progress
We have much to build on as we implement this Action Plan. Progress on our federal response will be highlighted through key indicators for each Government of Canada Action, as presented in Appendix A. Efforts were made to identify indicators that were feasible, measurable, and specific to each action. Progress reports will detail federal achievements and deliverables in line with the key priorities and actions outlined within this Action Plan. Previous progress reports can be found for the year 2019-2020 and years 2020-2022. These progress reports will provide transparency on the Government of Canada's actions and activities accomplished each year and will allow partners across the country to learn from existing initiatives. Ongoing stakeholder engagement will also serve as another mechanism to determine and report on the success of our actions.
Section 5: Conclusion
This Action Plan reaffirms the Government of Canada's commitment to addressing STBBI by creating an enabling environment and improving access to prevention, testing, care and treatment. Canada's response to STBBI must be evidence-based, person-centred, culturally safe and focused on addressing stigma and discrimination. Implementing the actions outlined in this plan and moving towards our 2030 global targets will require collaboration with people with lived and living experience, in line with GIPA/MEPA principles, as well as our community partners, and provinces/territories. The Government of Canada is open to embracing new ideas, challenging current approaches, and both leading and learning as we implement this renewed Action Plan with our partners.
Glossary of terms
- ACB
- African, Caribbean, and Black People
- COVID-19
- Coronavirus disease 2019
- CAF
- HIV and Hepatitis C Community Action Fund
- gbMSM
- Gay, bisexual and men who have sex with men
- GIPA/MEPA
- Greater Involvement of People Living with HIV/AIDS/Meaningful Engagement of People Living with HIV/AIDS
- HRF
- Harm Reduction Fund
- HIV
- Human immunodeficiency virus
- HCV
- Hepatitis C virus
- HBV
- Hepatitis B virus
- HPV
- Human papillomavirus
- HSV
- Herpes simplex virus
- PrEP
- Pre-exposure prophylaxis
- PEP
- Post-exposure prophylaxis
- POCT
- Point-of-care testing
- SUAP
- Substance Use and Addictions Program
- STBBI
- Sexually transmitted and blood-borne infections
- U=U
- Undetectable = Untransmittable
- 2SLGBTQI+
- Two-Spirit; Lesbian; Gay; Bisexual; Transgender; Queer; Intersex, considers sex characteristics beyond sexual orientation, gender identity and gender expression; +: is inclusive of people who identify as part of sexual and gender diverse communities, who use additional terminologies
Appendix A: Federal progress indicators
| Actions | Lead Department |
Federal Progress Indicators |
|---|---|---|
| Priority: Support First Nations, Inuit and Métis priorities, leadership and self-determination | ||
Support First Nations, Inuit and Métis led initiatives and priorities, in line with existing declarations that aim to eliminate anti-Indigenous racism in the health system. This includes the Truth and Reconciliation Commissions Calls to Action 18-24 |
All |
Number of federally funded and/or supported initiatives that are led by First Nations, Inuit and Métis Peoples Number of Nation-to-Nation initiatives supporting Indigenous Communities rights of self-determination as it relates to STBBI programming Report on the application of incorporating Indigenous ways of Knowing and Doing by hearing feedback from First Nations, Inuit and Métis Peoples to determine progress on this action |
Foster a cadre of First Nations, Inuit and Métis researchers by providing funding for training, mentorship, and other supports that enable long and productive careers |
CIHR |
Amount of funding committed to opportunities for capacity building for First Nations, Inuit and/or Métis people, including training and mentoring |
Build and sustain rapid testing capacity and reduce barriers to testing in underserved populations, particularly First Nations, Inuit and Métis communities, through the Northern, Remote and Isolated (NRI) Initiative |
PHAC, ISC |
Number of tests (per infection type) deployed to support Community-led/Community-Based testing. Number of community engagement and training sessions. Number of communities participating and successfully completing Proficiency Testing for Community-Based Testing (CBT) |
Advocate for long-term funding to First Nations, Inuit and Métis led organizations (i.e., 10-years), wherever possible |
ISC |
Number of meetings with partners to advocate for long term funding Number of engagement sessions with partners to explore options of long-term funding |
| Priority: Address STBBI-related stigma and discrimination | ||
Implement knowledge mobilization efforts to increase awareness of Undetectable= Untransmittable (U=U) message and HIV-related stigma among key populations, health professionals, and the general public |
PHAC |
Number of knowledge mobilization activities completed related to HIV-related stigma, HIV treatment and U=U |
Develop research and community-based funding opportunities to understand, address and reduce the impact of stigma, racism, homophobia, transphobia, sexism and other forms of discrimination and systemically entrenched oppression |
CIHR |
Amount of funding committed to opportunities focused on stigma and discrimination. |
Promote stigma reduction through public education efforts (e.g., national and targeted advertising), engaging people with lived experience, supporting organizations working to reduce stigma (e.g., via SUAP), and fostering partnerships that support the uptake of best practices for stigma reduction. These initiatives complement and support activities in the Canadian Drugs and Substances Strategy (CDSS) |
HC |
Percentage of people living in Canada who have stigmatizing views |
Synthesize and disseminate evidence on HIV transmission risk and the public health implications |
PHAC |
Number of knowledge products that are produced and disseminated on HIV transmission risk |
Address STBBI related stigma and discrimination through comprehensive and ongoing knowledge mobilization activities and messaging that promotes STBBI prevention testing, treatment and care as integral components of a broader, holistic approach to health and well-being |
PHAC |
Number of knowledge mobilization activities completed to increase awareness of STBBI prevention, testing and treatment and stigma and discrimination |
Establish culturally safe and accessible diagnostic services for urban isolated populations |
PHAC |
Number of communities where support is provided, and capacity is being built |
Continue to work toward reducing the over-criminalization of HIV non-disclosure in Canada |
DOJ |
Number of activities that address over-criminalization of HIV non-disclosure in Canada |
| Priority: Improve STBBI data monitoring and collection practices | ||
Improve monitoring of STBBI trends and progress for key populations, regions, ages and sexes and facilitate access to data on key STBBI (e.g., STBBI dashboard) |
PHAC |
Description of improvements to monitoring and accessibility mechanisms |
Review and adapt national surveillance methods in collaboration with partners (including provinces and territories, First Nations, Inuit, Métis and other community-based partners) to improve reporting on STBBI epidemiology and monitor progress toward elimination goals |
PHAC, ISC |
Information needs are identified and agreed-upon with partners (for data disaggregation & monitoring progress) Strategies are implemented to improve data collection to address information needs |
Collaborate with communities affected by STBBI to inform responsible and culturally appropriate data collection, stewardship, reporting standards, guidance and knowledge products, integrating diverse ways of understanding health and well-being, including Indigenous Ways of Knowing and Doing as appropriate |
PHAC |
Number of advisory committees and working groups created and their associated meetings on data collection, stewardship and reporting |
Support data collection, analysis, research and knowledge on 2SLGBTQI+ communities to help inform the provision of healthcare services to 2SLGBTQI+ communities, including the importance of sexual health, experiences of stigma and discrimination and risk of STBBI |
WAGE |
Number of research projects supported by WAGE on healthcare services to 2SLGBTQI+ communities |
| Priority: Strengthen and support research capacity | ||
Develop and invest in knowledge mobilization which promotes community-centered and holistic approaches to research that advances the meaningful engagement of community members and people with lived experience throughout the research process |
CIHR |
Amount of funding committed to opportunities focused on knowledge mobilization which promotes community-centred research. |
Develop training initiatives that foster inter-and transdisciplinary approaches and support the current and next generation of HIV/AIDS and STBBI researchers in developing skills to integrate new technologies and methods in their research |
CIHR |
Amount of funding committed to training opportunities that are dedicated to inter- and transdisciplinary approaches that support current and next generation HIV/AIDS and STBBI researchers |
Support HIV/AIDS and STBBI researchers across their career journey by providing professional development supports (e.g., networking, mentorship) and strategic funding opportunities with a focus on researchers and trainees from underrepresented groups, those who are navigating early- and mid-career transitions and those leading research in the community setting |
CIHR |
Amount of funding committed to opportunities focused on HIV/AIDS and STBBI trainees and researchers' career development. |
| Priority: Provide ongoing support, exchange, and convening opportunities | ||
Convene STBBI stakeholders and partners including HIV and Hepatitis C Community Action Fund (CAF) and Harm Reduction Fund (HRF) recipients, people with lived and living experience and national STBBI community to share wise practices, ongoing challenges, and lessons learned through various mechanisms (i.e. webinars, storytelling, meetings, working groups) |
PHAC |
Number of meetings and stakeholders/partners convened across various activities |
| Actions | Lead Department |
Federal Progress Indicator |
|---|---|---|
| Priority: Promote comprehensive sexual health and wellbeing across the life course | ||
Support initiatives and develop knowledge mobilization activities that promote sexual health as more than the absence of disease and work towards normalizing sexual health conversations (e.g., strength-based, culturally appropriate, linguistically diverse, peer-to-peer based approaches) |
PHAC, HC |
Number of knowledge mobilization activities and CAF/HRF projects funded that apply a holistic sexual health lens |
Fund strength-based initiatives aimed at building capacity, adaptation, resilience, and empowerment by partnering within existing federal funding programs focused on health promotion (i.e., positive mental health, intersectoral factors, early childhood education) |
PHAC, ISC, HC |
Number of health promotion initiatives aimed at building capacity, adaptation, resilience and empowerment |
Build on sexual and reproductive health research to enhance understanding of sex, gender, sexuality and systemic barriers in shaping experiences, risks and outcomes of STBBI |
CIHR |
Amount of funding committed to opportunities for sexual and reproductive health research focused on sex, gender, sexuality, and/or systemic barriers with STBBI. |
Deliver comprehensive STBBI preventive services, including health education during basic training and deployment, HPV vaccination, and HIV PrEP/ PEP, to all Canadian Armed Forces members according to clinical practice guidelines |
DND |
Percentage of STBBI related services adopted by Department of National Defense based on guidelines |
| Priority: Enhance awareness of, and access to, biomedical STBBI prevention tools | ||
Provide policy and technical guidance based on evidence synthesis, cost effectiveness, efficacy, and best practice examples to inform the uptake of evidence based biomedical prevention tools (e.g., HIV PrEP and vaccination) and other potentially emerging biomedical prevention tools (e.g., STI PEP/PrEP, vaginal rings, injectables) |
PHAC |
Number of biomedical prevention tools assessed |
| Priority: Advance development and uptake of vaccines and prevention innovations | ||
Develop research funding opportunities to advance the design, development and implementation of next-generation interventions (i.e., vaccines, multipurpose prevention technologies, long-acting injectable antiretrovirals, and anti-bacterials) |
CIHR |
Amount of funding committed to opportunities for the development and/or implementation of next-generation interventions. |
Provide public health guidance, based on scientific evidence and best practices, on existing and emerging vaccines through the National Advisory Committee on Immunization |
PHAC |
Number of immunization guidance products released based on available evidence and best practices |
Establish a vaccination pilot project to offer vaccines on a voluntary basis, where accessible and available, against vaccine preventable diseases including Hepatitis B to IRCC clients at the time of the Immigration Medical Exam |
IRCC |
Number of hepatitis B vaccines offered to IRCC clients at the time of the Immigration Medical Exam Proportion of IRCC clients that consented to participate in the vaccine pilot at the time of the Immigration Medical Exam |
| Priority: Support harm reduction programs and services | ||
Invest in community-based projects that incorporate harm reduction approaches to meet the needs of key populations,including substance related harms through the CAF, HRF and Substance Use and Addictions Program (SUAP) |
PHAC, ISC, HC |
Number of funded CAF and HRF, projects that are targeted to reducing STBBI-related harms of substance use Percent change in the number of clients accessing services funded by SUAP that aim to reduce substance use harms |
Extend the Prison Needle Exchange Program and Overdose Prevention Service to strengthen efforts to prevent STBBI at federal correctional facilities across Canada |
CSC |
Number of new Prison Needle Exchange Programs and Overdose Prevention Services provided in federal correctional facilities |
Support avenues that divert individuals found in possession of controlled substances away from the criminal justice system, including alternatives to prosecution, and where appropriate, refer them to the relevant health and social services |
DOJ |
Number of legislative, policy, and programming opportunities that support the diversion of individuals found in possession of controlled substances |
Support the establishment of supervised consumption sites and temporary urgent public health need sites (known as overdose prevention sites) using streamlined regulatory approvals, in collaboration with provinces and territories as part of complementary and supporting activities through the Canadian Drugs and Substances Strategy (CDSS) |
HC |
Average number of visits to supervised consumption sites (SCS) per year |
Strengthen public policy and guidance to support harm reduction and health promotion efforts in the context of sexualized drug use |
PHAC |
Number of initiatives to support harm reduction and health promotion efforts in the context of sexualized drug use |
| Priority: Respond to emerging and reemerging infections | ||
Develop and invest in research funding opportunities that address and contribute to timely, culturally relevant and effective responses to emerging and re-emerging infections being spread through sexual contact (e.g., infectious syphilis, congenital syphilis, mpox). |
CIHR, PHAC, ISC |
Amount of funding committed to opportunities created to address emerging and/or reemerging infections |
Strengthen public health capacity to respond to emerging and re-emerging STBBI public health threats by developing robust risk assessment processes and by embedding public health personnel in provinces and territories |
PHAC |
Number of public health personnel embedded within provinces and territories Number of STBBI-related public health threats assessed by the risk assessment unit |
Adapt federal grants and contributions to respond to current priorities based on the latest epidemiological data, including new and emerging infections |
PHAC |
Number of times G&C programs were effectively adapted to address emerging or cluster infections |
| Actions | Lead Department |
Federal Progress Indicator |
|---|---|---|
| Priority: Expand the availability of a range of testing modalities | ||
Utilize regulatory and policy tools to facilitate access to STBBI tests on the Canadian market (i.e., pre-submission meetings with manufacturers to ensure regulatory requirements will be met, identification of tests for priority review, enabling access to unlicensed medical devices for health care professionals through the Special Access Program) |
HC |
Description of the additional supports provided to manufacturers to facilitate their progress through the regulatory approval process |
Increase timely access to STBBI tests in Canada through international collaborations such as the joint US/Canada submission portals and the World Health Organization (WHO) joint assessment sessions for in-vitro diagnostic devices |
HC |
Number of international collaborative engagements related to STBBIs |
Invest in research for innovative technologies for testing and surveillance to better detect, characterize and monitor STBBI |
CIHR |
Amount of funding committed to opportunities for research in innovative testing and/or surveillance technologies |
| Priority: Improve access to STBBI testing for key populations and the general population | ||
Promote evidence informed STBBI testing strategies as part of overall sexual health and wellbeing for the general population, with targeted approaches among key populations including funding community-based approaches to reach the undiagnosed through the CAF |
PHAC |
Number of community-based projects funded to promote STBBI testing strategies |
Encourage testing and treatment in correctional facilities, supported by the direction of the National Infectious Diseases Medical Advisor |
CSC |
Testing and treatment in correctional facilities is supported by the National Infectious Diseases Medical Advisor |
Develop and invest in funding opportunities focused on implementation science research to better understand, define and integrate the context, conditions and adjustments that will maximize uptake and adoption of new and existing testing modalities in different health, social and cultural settings |
CIHR |
Amount of funding committed to opportunities focused on implementation science to maximize uptake and adoption of new and/or existing testing modalities in different health, social and cultural settings |
Develop and deploy low barrier technologies that supports equitable access to high quality screening and confirmatory testing |
PHAC |
Number of novel point-of-care or near patient testing technologies to support diagnostic and patient management Number of pathogen specific quality management programs to support highly decentralized testing Number of culturally appropriate training resources to support highly decentralized testing |
| Actions | Lead Department |
Federal Progress Indicator |
|---|---|---|
| Priority: Facilitate access to wrap-around care & support | ||
Assess and report on ongoing gaps for STBBI treatment and care, through monitoring and surveillance to inform uptake initiatives among key populations |
PHAC |
Number of products focused on describing gaps qualitatively and quantitatively for STBBI treatment and care |
Develop culturally appropriate and gender affirming and gender inclusive information, tools and resources to facilitate access to care |
HC |
Number of products aimed at patients and healthcare professionals to facilitate early treatment |
| Priority: Provide care for populations with health services or coverage from the federal government | ||
Provide ongoing voluntary STBBI testing, treatment and health services for eligible individuals, including serving members of the Canadian Armed Forces, certain immigrant populations, people living in federal correctional facilities, and registered First Nations and eligible Inuit |
ISC, CSC, DND, IRCC |
Percentage of STBBI related services adopted by federal government departments based on guidelines |
| Actions | Lead Department |
Federal Progress Indicator |
|---|---|---|
| Priority: Reinforce importance of person-centered, trauma-informed and linguistically and culturally relevant care | ||
Equip healthcare professionals with readily accessible resources and tools to support the delivery of comprehensive, holistic, trauma-informed, stigma and discrimination free, and culturally safe STBBI and sexual health care and support. |
PHAC, HC |
Number of resources and tools released to healthcare professionals |
Facilitate opportunities for research to develop, test and advance culturally safe and holistic models of care and evidence-based interventions to achieve more equitable health outcomes |
CIHR |
Amount of funding committed to opportunities for culturally safe and/or holistic models of care and evidence-based interventions to achieve more equitable health outcomes. |
Collaborate with community stakeholders to co-design culturally appropriate and linguistically diverse tools, resources and campaigns to raise awareness of prevention, testing and treatment strategies (e.g., HIV PrEP, mpox, HPV and HBV vaccination) with all key populations. |
PHAC |
Number of funded initiatives |
| Priority: Recognize and support peer-based approaches within the STBBI response | ||
Support peers and peer-based approaches (e.g., peer navigation programs, peer networks) that guide and empower individuals in accessing testing care and support |
PHAC |
Number of peer-focused projects supported |
References
- Footnote 1
-
Public Health Agency of Canada. A pan-Canadian framework for action : reducing the health impact of sexually transmitted and blood-borne infections in Canada by 2030. 2018; Available at: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/reports-publications/sexually-transmitted-blood-borne-infections-action-framework.html
- Footnote 2
-
World Health Organization. WHO releases new guidance to improve testing and diagnosis of sexually transmitted infections. 2023; Available at: https://www.who.int/news/item/24-07-2023-who-releases-new-guidance-to-improve-testing-and-diagnosis-of-sexually-transmitted-infections/
- Footnote 3
-
World Health Organization. Sexually transmitted infections (STIs). 2023; Available at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
- Footnote 4
-
Gratrix J, Plitt S, Turnbull L, Smyczek P, Brandley J, Scarrott R, et al. Prevalence and antibiotic resistance of Mycoplasma genitalium among STI clinic attendees in Western Canada: a cross-sectional analysis. BMJ Open. 2017 Jul 10;7(7):e016300. doi: 10.1136/bmjopen-2017-016300
- Footnote 5
-
Gesink D, Racey CS, Seah C, Zittermann S, Mitterni L, Juzkiw J, et al. Mycoplasma genitalium in Toronto, Ont: Estimates of prevalence and macrolide resistance. Can Fam Physician. 2016 Feb;62(2):e96-101
- Footnote 6
-
Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Infectious and congenital syphilis in Canada, 2010–2015. CCDR. 2018 Feb 1;44(2):43-48. doi: 10.14745/ccdr.v44i02a02
- Footnote 7
-
Public Health Agency of Canada. Mpox (monkeypox). 2022; Available at: https://www.canada.ca/en/public-health/services/diseases/mpox.html
- Footnote 8
-
Public Health Agency of Canada. Enhanced Surveillance of Antimicrobial-Resistant Gonorrhea in Canada (infographic). 2022; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/enhanced-surveillance-antimicrobial-resistant-gonorrhea-canada-infographic.html
- Footnote 9
-
Public Health Agency of Canada. Hepatitis B in Canada: 2020 surveillance data update. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hepatitis-b-canada-2020-surveillance-data-update.html
- Footnote 10
-
Public Health Agency of Canada. Reported cases from 1924 to 2021 in Canada - Notifiable diseases on-line. 2023; Available at: https://diseases.canada.ca/notifiable/charts?c=pl
- Footnote 11
-
Public Health Agency of Canada. Infectious syphilis and congenital syphilis in Canada, 2022. CCDR. 2023 Oct;49(10)
- Footnote 12
-
Public Health Agency of Canada. Chlamydia, gonorrhea and infectious syphilis in Canada: 2020 (Infographic). 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/chlamydia-gonorrhea-infectious-syphilis-canada-2020-infographic.html
- Footnote 13
-
Public Health Agency of Canada. Infectious syphilis and congenital syphilis in Canada, 2021 (Infographic). CCDR. 2022;48(11)
- Footnote 14
-
Aho J, Lybeck C, Tetteh A, Issa C, Kouyoumdjian F, Wong J, et al. Rising syphilis rates in Canada, 2011–2020. CCDR. 2022 Feb 24;48(23):52-60
- Footnote 15
-
Public Health Agency of Canada. Findings from the Survey on the impact of COVID-19 on access to STBBI-related services, including harm reduction services, for people who use drugs or alcohol in Canada. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/survey-impact-covid-19-access-stbbi-services-harm-reduction-people-who-use-drugs-alcohol.html
- Footnote 16
-
Public Health Agency of Canada. Findings from the Survey on the impact of COVID-19 on access to STBBI-related services, including harm reduction services, for African, Caribbean and Black people in Canada. 2022 Sept; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/survey-impact-covid-19-access-stbbi-harm-reduction-services-african-caribbean-black-people.html
- Footnote 17
-
Public Health Agency of Canada. Findings from the Survey on the impact of COVID-19 on the delivery of STBBI prevention, testing and treatment, including harm reduction services, in Canada. 2022 Mar. Available at Survey on the impact of COVID-19 on the delivery of STBBI prevention, testing and treatment, including harm reduction services, in Canada - Canada.ca
- Footnote 18
-
Public Health Agency of Canada. Hepatitis C in Canada: 2020 surveillance data update. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hepatitis-c-canada-2020-surveillance-data-update.html
- Footnote 19
-
Public Health Agency of Canada. Estimates of HIV incidence, prevalence and Canada's progress on meeting the 90-90-90 HIV targets, 2020. Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/estimates-hiv-incidence-prevalence-canada-meeting-90-90-90-targets-2020.html
- Footnote 20
-
Public Health Agency of Canada. HIV in Canada: 2022 surveillance highlights. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-2022-surveillance-highlights.html
- Footnote 21
-
Public Health Agency of Canada. HIV in Canada Surveillance Report December 31 2021. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hiv-canada-surveillance-report-december-31-2021.html
- Footnote 22
-
Public Health Agency of Canada. Hepatitis B in Canada: 2021 surveillance data update. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hepatitis-b-canada-2021-surveillance-data-update.html
- Footnote 23
-
Rotermann M, Langlois K, Andonov A, Trubnikov M. Seroprevalence of hepatitis B and C virus infections: Results from the 2007 to 2009 and 2009 to 2011 Canadian Health Measures Survey. 2013 Nov;24(11):3-13
- Footnote 24
-
Public Health Agency of Canada. Report on Hepatitis B and C Surveillance in Canada: 2019. 2022; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/report-hepatitis-b-c-canada-2019.html
- Footnote 25
-
Chlamydia, gonorrhea and infectious syphilis in Canada: 2021 surveillance data update. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/chlamydia-gonorrhea-infectious-syphilis-2021-surveillance-data.html
- Footnote 26
-
Public Health Agency of Canada. Hepatitis C in Canada: 2021 surveillance data update. 2023; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/hepatitis-c-canada-2021-surveillance-data-update.html
- Footnote 27
-
Popovic N, Williams A, Périnet S, Campeau L, Yang Q, Zhang F, et al. National hepatitis C estimates: incidence, prevalence, undiagnosed proportion and treatment, Canada, 2019. CCDR. 2022 Dec;48(11/12)
- Footnote 28
-
Government of Canada. National surveillance of antimicrobial susceptibilities of Neisseria gonorrhoeae annual summary 2019. 2021; Available at: https://www.canada.ca/en/services/health/publications/drugs-health-products/national-surveillance-antimicrobial-susceptibilities-neisseria-gonorrhoeae-annual-summary-2019.html
- Footnote 29
-
Public Health Agency of Canada. Notifiable Diseases Online. 2023; Available at: https://diseases.canada.ca/notifiable/
- Footnote 30
-
Lydon-Hassen K, Jonah L, Mayotte L, Hrabowy A, Graham B, Missens B, et al. Summary findings from Tracks surveys implemented by First Nations in Saskatchewan and Alberta, Canada, 2018–2020. CCDR. 2022 Apr 6;48(4):146-156
- Footnote 31
-
Tarasuk J, Zhang J, Lemyre A, Cholette F, Bryson M, Paquette D. National findings from the Tracks survey of people who inject drugs in Canada, Phase 4, 2017–2019. CCDR. 2020 May 7;46(5):138-148
- Footnote 32
-
National Defence. Anti-racism lexicon. 2023; Available at: https://www.canada.ca/en/department-national-defence/services/systemic-racism-discrimination/anti-racism-toolkit/anti-racism-lexicon.html
- Footnote 33
-
The Canadian Network on Hepatitis C Blueprint Writing Committee and Working Group. Blueprint to inform hepatitis C elimination efforts in Canada. 2019 May; Available at: https://www.canhepc.ca/sites/default/files/media/documents/blueprint_hcv_2019_05.pdf
- Footnote 34
-
Public Health Agency of Canada. Syphilis in Canada: Technical report on epidemiological trends, determinants and interventions. 2020 Nov; Available at: https://www.canada.ca/en/services/health/publications/diseases-conditions/syphilis-epidemiological-report.html
- Footnote 35
-
Van Gerwen OT, Muzny CA, Marrazzo JM. Sexually transmitted infections and female reproductive health. Nat Microbiol. 2022 Aug 1;7(8):1116-1126. doi: 10.1038/s41564-022-01177-x
- Footnote 36
-
Public Health Agency of Canada. Sexually transmitted and blood-borne infections: Guides for health professionals. 2023; Available at: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines.html
- Footnote 37
-
Arnold SR, Ford-Jones EL. Congenital syphilis: A guide to diagnosis and management. Paediatr Child Health. 2000;5(8):463-469. doi: 10.1093/pch/5.8.463
- Footnote 38
-
Kwong JC, Crowcroft NS, Campitelli MA, Ratnasingham S, Daneman N, Deeks SL, et al. Ontario Burden of Infectious Disease Study Advisory Group; Ontario Burden of Infectious Disease Study (ONBOIDS): An OAHPP/ICES Report. 2010 Dec; Available at: https://www.ices.on.ca/publications/research-reports/ontario-burden-of-infectious-disease-study/
- Footnote 39
-
Diener A, Dugas J. Inequality-related economic burden of communicable diseases in Canada. CCDR. 2016 Feb 18,;42(S1):S1-13. doi: 10.14745/ccdr.v42is1a02
- Footnote 40
-
Public Health Agency of Canada. Addressing Stigma: Towards a More Inclusive Health System. 2021; Available at: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/addressing-stigma-toward-more-inclusive-health-system.html
- Footnote 41
-
Djiadeu P, Begum H, Sabourin S, Gadient S, Archibald C, LeBlanc M, et al. Risk of transmission of HIV viral load suppression. CCDR. 2023 Dec;49-11/12:457-64. doi: 10.14745/ccdr.v49i1112a01
- Footnote 42
-
Federal, provincial, and territorial Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and Stimulant-related Harms in Canada. 2023; Available at: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
- Footnote 43
-
World Health Organization. Multi-drug resistant gonorrhoea. 2023; Available at: https://www.who.int/news-room/fact-sheets/detail/multi-drug-resistant-gonorrhoea
- Footnote 44
-
Thorington R, Sawatzky P, Lefebvre B, Diggle M, Hoang L, Patel S, et al. Antimicrobial susceptibilities of Neisseria gonorrhoeae in Canada, 2020. CCDR. 2022;48(11/12):571-9. doi: 10.14745/ccdr.v48i1112a10
- Footnote 45
-
Bardsley M, Jenkins C, Mitchell HD, Mikhail AFW, Baker KS, Foster K, et al. Persistent Transmission of Shigellosis in England Is Associated with a Recently Emerged Multidrug-Resistant Strain of Shigella sonnei. J Clin Microbiol. 2020 Mar 25;58(4) :e01692-19. doi: 10.1128/JCM.01692-19
- Footnote 46
-
Gaudreau C, Bernaquez I, Pilon PA, Goyette A, Yared N, Bekal S. Clinical and Genomic Investigation of an International Ceftriaxone- and Azithromycin-Resistant Shigella sonnei Cluster among Men Who Have Sex with Men, Montréal, Canada 2017–2019. Microbiol Spectr. 2022 Jun 1;10(3):e0233721
- Footnote 47
-
Public Health Agency of Canada. Hepatitis C: For health professionals. 2023; Available at: https://www.canada.ca/en/public-health/services/diseases/hepatitis-c/health-professionals-hepatitis-c.html
- Footnote 48
-
Trépo C, Chan HLY, Lok A. Hepatitis B virus infection. Lancet. 2014 Dec 6;384(9959):2053-63. doi: 10.1016/S0140-6736(14)60220-8
- Footnote 49
-
Public Health Agency of Canada. Booklet: Sexually Transmitted Infections. 2020; Available at: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/booklet-sexually-transmitted-infections.html#_5.1
- Footnote 50
-
Prevention Access Campaign. Who are we and what we do. Available at: https://preventionaccess.com/
- Footnote 51
-
UNAIDS. Undetectable=Untransmittable Public Health and HIV Viral Load Suppression. 2018. Available at: https://www.unaids.org/en/resources/documents/2018/undetectable-untransmittable
- Footnote 52
-
Public Health Agency of Canada. HIV and AIDS: For health professionals. 2023; Available at: https://www.canada.ca/en/public-health/services/diseases/hiv-aids/health-professionals.html
- Footnote 53
-
Laprise C, Bolster-Foucault C. Understanding barriers and facilitators to HIV testing in Canada from 2009–2019: A systematic mixed studies review. CCDR. 2021 Mar 4;47(2):105-125. doi: 10.14745/ccdr.v47i02a03
