Health Portfolio Emergency Response Plan
On this page
- Record of amendments
- Executive summary
- Plan maintenance
- Authority
- 1) Introduction
- 2) Concept of operations
- 3) Seven-phase response process
- 3.1) Phase 1 – Initial assessment and alerting
- 3.2) Phase 2 – Public health risk and capability assessment
- 3.3) Phase 3 – Initial event assessment and response activation
- 3.4) Phase 4 – Response strategy review and approval
- 3.5) Phase 5 – Response implementation and action planning
- 3.6) Phase 6 – De-escalation and demobilization
- 3.7) Phase 7 – After action review
- Appendix A: Generic health portfolio IMS
- Appendix B: Acronyms
- Appendix C – Health portfolio situational assessment team (health portfolio SAT) standing agenda/decision brief template
- Appendix D: Sample de-escalation bidirectional indicators
- Appendix E: Annex 2: of the IHR decision instrument
- Endnotes
Record of amendments
| Amendment | Approved By | ||
|---|---|---|---|
| Number | Date of Issue | Name | Date Inserted |
| 1.0 | December 2013 | ERP Review and Revision Task Group on behalf of Health Portfolio Emergency Preparedness Committee (Health Portfolio EPC) | December 2013 |
| 2.0 | Aug 2022 (***Phases 1-3 only) |
Extended (PHAC + HC) Director General Emergency Management Executive Committee (DG EMEC) | September 2022 |
| 3.0 | August 2023 | PHAC President, Health Canada Deputy Minister, Extended VP and DG EMECs | September 2023 |
Executive summary
The Emergency Response Plan (ERP) is issued under the authority of the Minister of Health to meet legislative requirements as outlined in the Emergency Management Act. It adheres to the Federal Policy for Emergency Management, is subordinate to the Health Portfolio Strategic Emergency Management Plan (HP SEMP) and is fully interoperable with the Federal Emergency Response Plan (FERP).
The ERP outlines an operational planning framework enabling the Health Portfolio to coordinate the delivery of support capabilities to provincial, territorial, other federal departments and international partners during an emergency. The ERP is a foundational key element in the Health Portfolio's overall emergency preparedness and response program.
The ERP is an "all hazards" plan that defines the framework within which the Public Health Agency of Canada (PHAC) and Health Canada (HC) will operate to ensure an appropriate response to any emergency; it is augmented by annexes addressing specific threats and hazards.
At the heart of the ERP is a seven-phase response process designed to optimize the delivery of a coordinated Health Portfolio emergency response. The response process is presented in a linear fashion and recognizes that during an emergency, modifications may be necessary depending on the nature, speed, severity or duration of the threats or hazards faced.
The ERP is not intended to be prescriptive, but rather applied as a "handrail" to provide guidance for Health Portfolio emergency response. The ERP's Concept of Operations describes the initial assessment that takes place upon notification of a potential event/emergencyFootnote 1 by the Health Portfolio.
While specific response functions – i.e., Health Portfolio Operations Centre (HPOC) activities such as implementation of an Incident Management System (IMS) are operational responsibilities and thus outside the scope of the plan, the ERP defines the roles and responsibilities of key response entities. It also defines Health Portfolio Activation Levels and the related authorities to activate, along with Level indicators and sample scenarios and objectives.
Context of 2023 updates
The 2023 version of the ERP seeks to address initial lessons learned from the COVID-19 pandemic, as well as other recent activations and exercises. Analysis of COVID lessons learned and incorporation of updated best practices will be ongoing for some time, however, both nationally and globally.
Additionally, there are significant changes in motion within the Health Portfolio, e.g., defining the roles and responsibilities of new programs such as PHAC's Centre for Integrated Risk Assessment, or the evolving role of the Centre for Emergency Response.
The broader federal emergency management landscape is also changing, with Public Safety Canada and other implicated federal entities endeavouring to re-vision Canada's emergency management policy framework, including updates to the Federal Emergency Response Plan and its supporting Emergency Support Functions (ESF).
As such, the ERP will continue to incorporate additional refinements through a robust cyclical planning process as these initiatives progress.
To better understand the HP ERP context and intent, it is recommended that users also have prior understanding and familiarity with:
- Emergency management in the Canadian context as outlined in An Emergency Management Framework for Canada;
- the Federal Emergency Response Plan and whole-of-government federal emergency response coordination;
- The HP roles and responsibilities and mandate for federal emergency response as defined in the Health Portfolio Strategic Emergency Management Plan.
Plan maintenance
The ERP will be reviewed and updated annually by the Director identified below to reflect changes in legislation, policy or priorities and to address any gaps identified during its implementation.
Maintenance, review and revision of the ERP will be coordinated by PHAC, as the Health Portfolio entity responsible for emergency management direction and priority setting, information-sharing, consultation, decision-making and tracking/reporting of related initiatives.
PHAC will also liaise with subject matter expert representatives from across the Health Portfolio to support this work, including endorsement from the technical working level and management bodies comprised of PHAC and Health Canada representatives, which is required before plan revisions can receive final approval.
The Director General responsible may authorize administrative amendments as necessary to the plan and associated appendices under their purview, with such amendments shared as appropriate.
More substantive revisions will be reviewed by a Vice President/Assistant Deputy Minister-level governance body comprised of appropriate PHAC/Health Canada representatives, who will also assess the need for subsequent President/Deputy Minister-level approval.
Suggested amendments, comments or inquiries related to this plan should be forwarded to the attention of:
Director
Emergency Management Plans, Exercises, and Continuous Improvement
Centre for Emergency Preparedness
Regulatory, Operations and Emergency Management Branch
Public Health Agency of Canada
100 Colonnade Road
Ottawa, ON K1A 0K9
hpoc-cops@phac-aspc.gc.ca
Authority
This plan has been developed under the authority of the Minister of Health to meet legislative requirements under the Emergency Management Act.
It is effective upon approval by the PHAC President and the Deputy Minister of Health Canada.
The ERP (2023) replaces the ERP (2013).
President
Public Health Agency of Canada
Date: September 14, 2023
Deputy Minister
Health Canada
Date: September 14, 2023
1. Introduction
1.1 Purpose
The ERP provides guidance to the Health Portfolio to deliver on its federally mandated responsibility to effectively coordinate the delivery of support functions and capabilities to partners, including but not limited to the provinces/territories (P/Ts), other government departments (OGDs), non-governmental organizations (NGOs), international counterparts and the people of Canada, as applicable during events of public health significance.
It aims to guide decision-making on how the Health Portfolio transitions from normal business to response operations through to de-escalation when a return to normal operations can take place. Simply put, the purpose of this plan is to coordinate and integrate Health Portfolio activities for any risk-based event requiring escalated response beyond normal day-to-day operations.
The ERP is not intended to be followed as a step-by-step manual but is designed to provide staff and decision-makers with an overview of key concepts that should be considered for any response (e.g., assessing a situation, analyzing risks, defining objectives, etc.). All Health Portfolio employees – not just those with emergency management roles and responsibilities – should be familiar with its contents.
While the ERP is the overarching foundational response plan for the Health Portfolio, it is further supported by annexes addressing the unique requirements of particular threats or hazards. All ERP annexes model the same seven-phase response as the ERP and use a modified response structure to ensure interoperability with the parent plan. Current hazard-specific annexes include the following:
- Annex A. Health Portfolio Chemical, Biological, Radiological, Nuclear Intentional Events Annex
- Annex B. Health Portfolio Chemical Emergency Response Annex
- Annex C. Health Portfolio Nuclear Emergency Response Annex
- Annex D. Health Portfolio Foodborne Illness Emergency Response Plan
- Annex E. Health Emergency Risk Communications Protocol
- Annex F. Regional Emergency Response Plans
1.2 Strategic objectives
The ERP's key objectives are to:
- Provide a standardize public health event response framework for the Health Portfolio;
- Formalize the response process to ensure that event situational awareness, risks, capabilities, goals, objectives and resource commitments are clearly defined, horizontally coordinated and effectively communicated to guide decision-makers;
- Define a scalable response process, with clearly defined activation levels and authorities, to coordinate the Health Portfolio's all-hazard event response posture from initial escalation to de-escalation;
- Optimize the engagement of key partners and resources from across the Health Portfolio to support event response; and
- Establish a cyclical planning approach whereby event response activities are assessed to identify successes, challenges, gaps, opportunities and other lessons learned, with resultant recommendations shared and used to guide future planning, exercises and response activities.
1.3 Health equity
Health equity is achieved when all people can reach their full health potential without being disadvantaged by social, economic, or environmental conditions. When those determinants of health are unequal or unfairly distributed, affected populations can face worse health outcomes – these are health inequities.
During an emergency, any existing health inequities are often exacerbated, increasing negative health, social and economic impacts from the event. Conversely, a population with fewer such disparities should see more positive outcomes for having an inherently higher resilience – a pillar of the United Nations' Sendai Framework on Disaster Risk Reduction.
It is a Health Portfolio and Government of Canada priority to enhance health outcomes for Canadians by maximizing equity and minimizing disparities. It is also a key goal of emergency management to reduce such conditions of vulnerability before, during and after emergencies – noting that health inequities are modifiable and avoidable. These considerations jointly reinforce the importance of applying a health equity lens to emergency planning at PHAC.
This plan seeks to provide a framework for applying considerations before, during and after event response. These include the need to operationalize health equity considerations by:
- enhancing health equity competencies for operational staff through training;
- considering population inequities in risk assessment and operational planning;
- advocating for event partners to assess and mitigate health equity impacts;
- integrating health equity considerations and principles as part of decision-making;
- embedding health equity perspectives in response processes; and
- incorporating health equity assessment in after action reports and recommendations.
Through this lens, the Health Portfolio will create more equitable outcomes and better support Canadians to sustain their wellness during the spectrum of public health emergencies in years ahead, from infectious diseases to climate-related events.
1.4 Scope
The ERP is the Health Portfolio's scalable all-hazard emergency response plan. It is intended for use by Health Portfolio staff and decision-makers to guide the transition from normal day-to-day operations to response operations, and back again. It also offers guidance as to when the scope and/or intensity of an event exceeds program operational capacities and thus necessitates a coordinated Health Portfolio response supported by the HPOC.
A coordinated Health Portfolio response will likely be required when a hazard/threat impacts a Health Portfolio area of responsibility (e.g., infectious diseases, nuclear emergencies, bioterrorism, natural disasters, cyclicalFootnote 2 events), and
- A provincial/territorial authority requests significant federal support to assess and manage human health consequences resulting from an event;
- An event may have direct implications for Health Portfolio regulatory and/or program mandates;
- There is a high potential for cross-jurisdictional impacts, multiple requests for assistance and/or a need to coordinate mutual aid agreements to affected provinces/territories;
- There are significant impacts to Indigenous-led health operations and/or support required by federal Indigenous authorities (i.e., First Nations and Inuit Health Branch/Indigenous Services Canada);
- The event impacts a priority within Health Portfolio mandate and/or there is significant public interest requiring enhanced internal/external coordination and communication; or
- The event may constitute a Public Health Emergency of International Concern as defined by the International Health Regulations (IHR).
Out of scope:
Business Continuity Planning (BCP): these internal Health Portfolio processes are separate from the response, intended to restore critical functions and promote the continuation or resumption of operations for any event impacting Health Portfolio staff or operations (e.g., a natural disaster, pandemic, cyber-attack).
Operational guidelines and tactical instructions for HPOC or program response functions, e.g., considerations found in the Centre for Emergency Response's Concept of Operations, HPOC Standard Operating Procedures or Business Cycle templates, etc.
1.5 Alignment and relationship to other plans
The Health Portfolio Strategic Emergency Management Plan (SEMP) provides the policy and governance framework to guide strategic emergency management activities across the Health Portfolio, with a focus on all four phases of the emergency management continuum: prevention/mitigation, preparedness, response and recovery. The ERP is subordinate to the SEMP.
The ERP is aligned with the Federal Emergency Response Plan (FERP), the Government of Canada's all hazard plan, to ensure that the Health Portfolio can contribute, when requested, to an integrated Government of Canada response. The FERP is the core plan for coordinating a response to emergencies where support is required from multiple federal institutions, while the ERP and its annexes provide direction for managing events within the Health Portfolio areas of responsibility.
When this plan is used within the context of the FERP being implemented, Health Portfolio authorities and responsibilities will be respected, but the ERP will integrate with the coordinating structures/governance, processes and protocols prescribed in the FERP.
The ERP, as with all Health Portfolio plans, is required to integrate and be interoperable with other federal, provincial and territorial (FPT) health sector national plans such as the FPT Public Health Response Plan for Biological Events, as well as with other Government of Canada emergency management plans such as the Federal Nuclear Emergency Plan (FNEP).
Hierarchy of Health Portfolio Emergency Management Plans
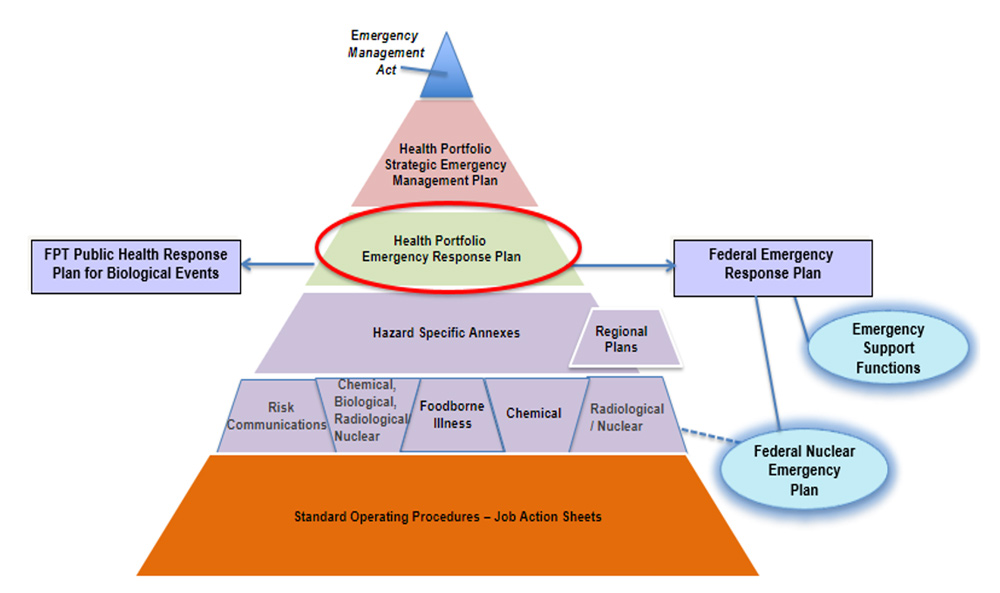
Text description
Pyramid divided into six levels. Level1: the top of the pyramid shows the Emergency Management Act. Level 2: depicts the Strategic Emergency Management Plan. Level 3: depicts the Health Portfolio Emergency Response Plan with a circle around it. On the left side there is an arrow pointing to a box with FPT Public Health Response Plan for Biological Events. On the left side there is an arrow pointing to a box with Federal Emergency Response Plan. Underneath the Federal Emergency Response Plan box there are two ovals connected to the box, one is Emergency Support Functions and one is Federal Nuclear Emergency Plan. Level 4: depicts Hazard Specific Annexes and a box for Regional Plans. Level 5: depicts multiple boxes depicting the individual Hazard Specific Annexes. There is a dotted line from the Radiological/Nuclear Annex to the oval of the Federal Nuclear Emergency Plan. Level 6: The bottom level depicts Standard Operating Procedures and Job Action Sheets.
2. Concept of operations
The ERP Concept of Operations describes how various parts of the organization will work together to ensure a coherent response. It covers key roles and responsibilities, Health Portfolio activation levels, notification and a description of the IMS.
2.1 Key roles and responsibilities
- Regulatory, Operational and Emergency Management Branch (ROEMB):
- ROEMB is the Health Portfolio's centre of expertise for emergency management functions, providing response coordination for unplanned or intentional emergency events, as well as planned mass gatherings or High-Visibility Events.Footnote 3
- Centre for Emergency Preparedness (CEP):
- The CEP leads emergency preparedness activities, including: developing, updating and testing all-hazard plans; facilitating continuous improvement through lessons learned; leading exercises for EM capacity building and training for Health Portfolio staff; providing a first line of responders for P/T surge requests for epidemiological assistance through the Canadian Field Epidemiology and Public Health Officers Programs; developing applied public health readiness competencies through training and fieldwork; disseminating and analyzing classified and unclassified intelligence products to support decision-making, in liaison with the national security community; and contributing to domestic and international emergency management policy and governance initiatives. The CEP also serves as the policy arm of Canada's IHR National Focal Point Office, providing expert advice to program areas on IHR assessment, reporting, notifications and communications, as well as supporting IHR implementation activities.
- Centre for Emergency Response (CER):
- During events, the CER provides a sustainable and scalable centre of public health emergency response expertise, which is the primary lead for responses to and recovery from events and emergencies impacting the Health Portfolio. The CER assumes a lead role in delivering on a renewed vision for emergency management at PHAC, helping to build an emergency management community of practice with federal, provincial and territorial partners.
- Health Portfolio Operations Centre (HPOC):
- The HPOC is part of the Centre for Emergency Response. It functions as a 24/7 all-hazard single window which triages and informs decision-makers of relevant public health events that require immediate attention, and delivers regular and just-in-time reporting to inform event-related situational awareness and decision-making. It also provides a facility where responsible personnel can gather to coordinate operational information and resources for strategic and/or tactical management of public health events and emergencies. The HPOC Watch Office serves as the operational arm of Canada's IHR National Focal Point Office by supporting 24/7 communications between Canada, the World Health Organization (WHO) and States Parties, as well as disseminating information to/and from stakeholders.
- Centre for Integrated Risk Assessment (CIRA):
- The CIRA is located within the Corporate Data and Surveillance Branch and coordinates and oversees integrated risk assessment in PHAC (including external stakeholders when necessary) to anticipate, detect and assess public health risks to Canadians in the immediate (signal detection), short, medium and longer terms (foresight). The CIRA also ensures clarity on accountability for action stemming from risk assessments and ensures documentation across the full life cycle of a potential risk. Risk assessment is a general term that refers to any assessment activities whether they are for the immediate (e.g., signal assessment, threat assessment), short (e.g., rapid risk assessment), medium (e.g., full-scale risk assessment) or longer term (e.g., foresight risk analysis).
- Event Lead ("the Lead"):
- The Health Portfolio program/Region(s) with primary mandate responsibilities and impacts related to an event. The Lead Vice President/Assistant Deputy Minister(s)during a response will be engaged by CER on activation approvals, also coordinating program/regional supports, accountability and subject matter expertise.
- Event Manager (EM):
- An EM is designated for any level of activation, and is responsible for event response leadership, management, coordination and oversight, including providing information and advice to and executing direction from the Health Portfolio Executive Group. The Event Manager may be the Executive Director (ED) or DG of the CER, or may be appointed from across the Health Portfolio with previous experience and/or specialized training.
- Chief Public Health Officer (CPHO):
- The CPHO is appointed as an "officer" of the Agency, accountable to the Minister and President for provision of science-based public health advice. The CPHO has delegated responsibilities for the public health provisions of the Public Health Agency of Canada Act, the Quarantine Act, the Human Pathogens and Toxins Act, the Department of Health Act and the Emergency Management Act. The CPHO holds the authority to be a spokesperson for the Health Portfolio on public health issues during an event. As the lead health professional for the Government of Canada, the CPHO may communicate with the public, voluntary organizations, the private sector, governments, public health authorities or organizations in the public health field (within Canada or internationally) for the purpose of providing information or seeking input on public health issues.
- Chief Science Officer (CSO):
- The CSO is the PHAC research lead during an activation. The research lead function involves providing science and research leadership and scalable support for evidence-informed decision-making during event response. This includes collaboration and liaison with the Chief Science Advisor and other VPs/ADMs (within PHAC and interdepartmentally) on horizontal science/research matters. It also involves coordination of horizontal science priorities and science advice requiring engagement and convening of internal and external subject matter experts and engagement with research funding organizations about research priorities and investments.
- Communications:
- The Communications and Public Affairs Branch (CPAB) is responsible for event-related communications, in alignment with the Protocols for Health Emergency Risk Communication Annex to the ERP. Their event responsibilities include: integrating risk communications activities within the overall risk management to ensure appropriate preparedness; developing and implementing strategic and operational communications planning including social marketing and advertising, social media, and web strategies; promoting clear, common messaging across relevant spokespersons; responding to media inquiries; leading crisis communications response; evaluating communications plans and responses; and developing staff risk and crisis communications capacity through training and exercises.
- Data and Surveillance Systems:
- Data is a key component supporting and guiding an effective response. The Chief Data Officer (CDO) supports access to the data needed to mount an effective and precise response. Surveillance systems, programs as well as data from external sources (including OGDs and P/Ts) provides the Health Portfolio with the ability to detect, understand and act on public health threats.
- Incident Action Team meeting (IAT):
- The IAT is an initial meeting staged at the onset of a fast-moving unplanned event, convening CER/HPOC and Lead representatives along with other supporting functions as required. The IAT meeting will assess preliminary situational information, assess relevant event risks and capabilities, establish initial Health Portfolio goals and objectives and identify relevant resources and processes needed to support the response.
- Incident Management System (IMS):
- A standardized approach to emergency management used by Health Portfolio Operations Centres encompassing personnel, facilities, equipment, procedures, and communications operating within a common organizational structure. The IMS is predicated on the understanding that in any and every incident there are certain management functions that must be carried out regardless of the number of persons who are available or involved in the emergency response.
- Emergency Response Cell (ERC):
- The ERC refers to the collective HPOC and core stakeholder team of response positions tasked to manage an event and support the Lead, from the start of the event until and if there is a governance decision to activate a full IMS.
- Health Portfolio Coordination Committee (HPCC):
- The primary forum for coordinating key response activities on a regular basis during an event. With membership comprising key Lead and event subject expert representatives and chaired by the Event Manager or delegate, its role is to facilitate ongoing situational awareness, update event plans and objectives and assign/update related Health Portfolio taskings.
- Health Portfolio Situational Assessment Team meeting (Health Portfolio SAT):
- The Health Portfolio SAT meeting is more formal and at a higher level than the IAT meeting; it is drawn from a broader set of internal stakeholders but is generally staged to execute similar functions with a more strategic focus and/or events of larger scope and/or longer duration.
- Health Portfolio Executive Group (HPEG):
- The HPEG is an executive-level forum; it meets as needed to provide strategic event decision-making and oversight through the Event Manager during responses. An HPEG could usually be struck if joint PHAC and HC involvement is required, when there are complex issues around financial authorities and/or a need for physical/human resources to be deployed from across the Health Portfolio or externally. The HPEG is supported by the HPOC in developing advice to roll out through Deputy Heads for advising Ministers, the Privy Council Office, Prime Minister's Office and/or Other Government Departments.
2.2 Key terms
- Activation Level refers to the Health Portfolio's response posture, not the response of the HPOC or Incident Management System. The Health Portfolio changes its response posture by escalating or de-escalating Activation Levels.
- The IMS is a response tool that may be mobilized to support an event and then demobilized following the response. It is initiated and supported by the HPOC but should not be referred to as an HPOC IMS.
2.3 Notification
Upon notification of an event, a rapid determination is made by CER based on initial situational assessment. When applicable and feasible, CER may seek advice from CIRA and other decision-makers from key areas from the Health Portfolio.
While initial event information and intelligence may come from various sources, the most important consideration is that this information reaches the relevant Technical Program Area(s) so an early public health risk assessment can be performed, and information distributed appropriately to ensure timely and accurate briefing of appropriate decision-makers.
During an event, implicated program area(s) will proactively make contact with appropriate partners, maintain lines of communication, monitor the situation, execute mandated activities, and prepare to support external requests for assistance.
| Internal to the HP | External Partners | Other Networks | Leadership |
|---|---|---|---|
|
|
|
|
2.4 Health Portfolio activation levels and authorities
The Health Portfolio has three levels of activation, summarized in the table below. The initial decision as to the appropriate activation level begins with an assessment of the level of risk associated with an event and considers a variety of factors. These include the complexity, severity, speed, duration and extent of the resources needed to respond to the event as well as the processes needed to support them – both for Health Portfolio support requirements and to address requests for assistance from external partners. These levels are generally sequential, though some events may require an immediate Level 2/3 response.
Authorities for Health Portfolio activation
In general, decision-making on Activation Levels is led by PHAC's Emergency Management Branch, Centre for Emergency Response, in coordination with the Lead.
- Level 1: Escalation to or from Level 1 is executed on the authority of the ED CER, in concurrence with the parallel authority of the Lead.
- Level 2: Activation to or from Level 2 is executed on the authority of the VP ROEMB, in concurrence with the parallel authority of the Lead.
- Level 3: Escalation to or from Level 3 is executed on Deputy Head authority, by recommendation of the VP ROEMB and Lead VP/ADM.
If an HPEG is active, it must concur with any increase or decrease of Levels. The CPHO may provide advice guiding activation at any level.
| Level | Authority (for escalation/de-escalation) |
Indicators (triggers for escalation/de-escalation) |
|---|---|---|
| 0: Routine operations (Green) |
N/A | Day-to-day operational cycle All-hazard monitoring, assessment and reporting |
| 1: Enhanced reporting and planning (Yellow) |
CER + Lead DG(s) (or delegates) | Unplanned incident OR planned event requires dedicated planning, coordination and/or minor commitment of Lead resources AND/OR Moderate exposure (e.g., public interest, local or regional media) |
| 2: Mobilized response (Red) |
VP ROEMB+ Lead VP/ADM(s) (or delegates) | Response exceeds capacity of Lead AND/OR Requires significant Health Portfolio resources to manage response or support partners AND/OR Significant exposure (e.g., public interest, national media) |
| 3: Full-scale activation (Purple) |
PHAC President/ Health Canada Deputy Minister By recommendation of VP ROEMB, Lead VP/ADM(s) (or delegates) |
Coordinated Health Portfolio response required, involving multiple program areas Prolonged and extensive commitment of Health Portfolio resources to manage response or support partners AND/OR Intense exposure (e.g., public interest, international media) |
2.5 Incident Management System (IMS)
An IMS is a standardized emergency management approach used to enable effective coordination and collaboration of event response activities. It is designed to be flexible, scalable and quickly adapted to meet the changing needs of a response and available capabilities/resources.
An IMS is built on the premise that similar core incident management functions and processes are required, regardless of the nature of the emergency, with resources being added or removed to tailor response efforts and specific functions depending on event scope and cadence.
IMS provides a unified command and control function for impacted Health Portfolio teams by establishing a formalized event coordination hierarchy, unifying reporting and management for all response functions and optimizing information flow by defining consistent and standardize terminology, roles, responsibilities and processes.
IMS positions will normally be filled by a combination of CER and program technical experts initially, and further resourced through Health Portfolio callouts for extended mobilizations.
Regional and National Microbiological Laboratory Branch (NMLB) Levels
HP Coordination/Operations Centres generally use a form of IMS based on the HP ERP generic IMS structure (Appendix A).
Regional Emergency Coordination Centres (RECCs) have three activation levels. A RECC may activate concurrently with the Health Portfolio in the event of an emergency impacting the HP both nationally and regionally, or independently to coordinate a region-specific response. RECC activation levels do not need to mirror the HP activation level but are based on the level of effort and resources required to support the RECC. RECCs activate under the authority of regional HP executives, according to the respective HP Regional Emergency Response Plans.
The NMLB Operations Centre has four levels, which also do not mirror the Health Portfolio IMS structure given its uniqueness in domestic and international requests for diagnostic surge capacity. For example, deployment of a mobile laboratory and an NMLB team may require an increased NMLB activation level, but not warrant HPOC activation. NMLB activates under its own Branch authorities and the NMLB Emergency Response Plan. NMLB works closely with HPOC to keep them abreast of NMLB Operational Centre activations and, where appropriate, the NMLB Operations Centre falls within the IMS structure.
3. Seven-phase response process
Upon notification of an event of potential public health significance, the Health Portfolio will follow a seven-phase response process. This incorporates a comprehensive situational analysis and public health risk assessment, implicated partners, governance processes, formalized and documented decision-making, escalation, de-escalation and after-action reporting.
The response process illustrates the spectrum between normal and emergency response operations. This generic process may be modified in hazard-specific annexes to address unique associated variables. Annex response processes do not mirror the parent ERP but are aligned and use similar concepts and terminology.
The descriptions below include a specific start and end point for each phase; however, these examples are for illustrative purposes only. There are no prescriptive criteria for the start and end of a phase, and depending on the event, some phases may overlap and merge.
Seven Phase Response Process
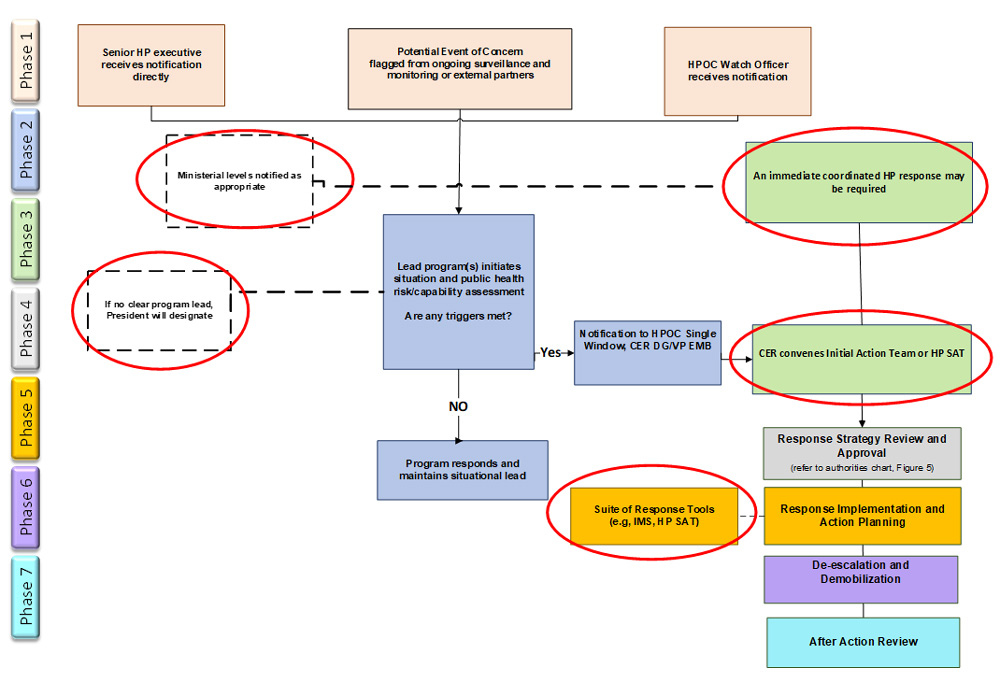
Text description
An organizational chart depicting seven phases of the response process. Level 1 depicts Phase 1: initial assessment and alerting. Level 2 depicts Phase 2: public health risk and capability assessment process. Level 3 depicts Phase 3: initial event assessment and response activation. Level 4 depicts Phase 4: response strategy review and approval. Level 5 depicts Phase 5: response implementation and action planning. Level 6 depicts Phase 6: de-escalation and demobilization. Level 7 depicts Phase 7: after action review. Dotted lines denote informational considerations. Red circles denote key revisions since the 2013 version of the plan
Note: Colours denote different Phases of the response. Dotted lines/boxes denote informational considerations. Red circles denote key revisions since 2013 version.
3.1 Phase 1 – Initial assessment and alerting
Summary: Notification about a potential event of public health significance reaches the Health Portfolio and is triaged to the Lead for initial assessment. For significant events where an immediate response is required, Phase 3 is initiated instead.
Starts with: The Health Portfolio is notified of a potential event of public health significance.
Ends with: The Lead is identified and conducts an initial public health risk assessment.
| Theme | Actions |
|---|---|
| Notification | While intel of an actual/potential event of public health significance (a signal) may come into the Health Portfolio in several ways and from a variety of sources, the recipients most likely to receive the initial notification of the event are:
|
| Alerting | Regardless of how the Health Portfolio becomes aware of an event, the most important consideration is to ensure that notification reaches the Lead with the technical expertise to evaluate and/or action it. HPOC Watch Office: The Watch Officer determines the Lead by referring to internal HPOC processes and Standard Operating Procedures for the threat/hazard. The Watch Officer disseminates the notification to the Lead and others as needed, using corresponding distribution lists. A similar process takes place if notification is received by the HPOC Duty Officer after hours. Senior Leadership/Executives: If notification is received by Senior Leadership/Executives, they will identify the appropriate Lead, notify their VP/ADM and share the information/intelligence received. The HPOC single window (PHAC-ASPC.HPOC-COPS@phac-aspc.gc.ca) and the ED CER and VP ROEMB should be included for situational awareness. |
| Atypical Leads | The Health Portfolio Chemical, Biological, Radiological/Nuclear Intentional Events Annex and other hazard specific Annexes and plans (i.e., FNEP) would be used for an intentional event. In the case of natural disasters with the potential to impact public health and requiring national coordination, the Lead will be the CER, supported by the impacted Region(s). If no national coordination is required, the impacted Region(s) will be the Lead. When no clear Lead exists, CIRA may help to identify a Lead in collaboration with senior management and, if required, by the President. |
| Partner Notification | Alerts may also be shared through official International Health Regulations (IHR) channels, provincial/territorial networks and laboratory networks. Notification to the Minister's Office (MINO), Privy Council Office (PCO), Chief Medical Officers of Health (CMOH)/Public Health Network (PHN) and others may also occur through regular channels and/or as directed by senior leadership. |
| Initial Risk Assessment | Signals indicating a potential public health concern can originate from a variety of sources including the HPOC single window, GPHIN, PHN, etc. The Lead performs routine assessments using hazard-specific guidance as part of normal operations to verify, validate and investigate. During this process, the Lead may choose to provide awareness to senior executives via the PHAC Daily Committee, Briefing Note, Flash Report, etc. If a validated signal is found to be of concern, it is considered a threat and is brought forward for coordinated threat assessment by the Scientific Committee for Coordinated Threat Assessment (SCCTA). Threats may also be escalated if hazard-specific triggers are met. |
3.2 Phase 2 – Public health risk and capability assessment
Summary: The Lead will further assess related risk, potentially with the support of CIRA for PHAC-led events, or through hazard-specific annexes/plans for HC-led events. When the risk reaches a threshold of potentially significant concern, assessment of available capabilities and requirements to respond begins. Up to that stage, the Lead is responsible for ongoing surveillance and monitoring. Data and scientific information will be key considerations in supporting assessment and guiding response efforts.
If initial response efforts exceed the capabilities of the Lead, its DG or VP/ADM will contact the Executive Director of CER, ED CER or VP ROEMB to seek support from the HPOC.
Starts with: The Lead continues risk assessment activities, which can be supported by the CIRA or by hazard-specific annexes.
Ends with: The Lead contacts the CER to discuss HPOC support.
| Theme | Actions |
|---|---|
| Risk Assessment | If further assessment activities are warranted based on hazard-specific plans (e.g., radiological/nuclear/chemical), the Lead will convene early risk assessment teams and assess hazard-specific triggers to determine the need for escalation, HPOC notification and/or engagement of additional Program/Region(s) or external partners. If further assessment activities are warranted for public health hazards without such formal plans, the CIRA convenes a team of subject matter and public health risk assessment experts from within PHAC and, if necessary, external public health partners (e.g., the CFIA, Environment and Climate Change Canada, Health Canada, P/Ts). The CIRA provides leadership in methodology, documentation and communication of the assessment, which is used to support science-driven decision-making for PHAC's response and thus serves to inform this or any other phase of the ERP. In other words, risk assessment can help continued understanding and guidance of the situation throughout the emergency response. |
| Capability Assessment | The ROEMB's Risk and Capability Assessment Unit (RCAU) is responsible for initiating the assessment of available capabilities, resources and requirements to respond to an identified threat. This would be triggered by the Lead via recommended actions in the Threat Report, public health risk assessments, etc. The Health Portfolio Capability Catalogue outlines Health Portfolio capabilities and the methodology for this assessment. Under some hazard-specific plans (e.g., CBRN intentional events, chemical and radiological/nuclear annexes), this process will be heavily guided by program expertise, with the RCAU providing a supporting role through insight on Health Portfolio resources outside the program's technical area or mandate (i.e., National Emergency Strategic Stockpile Emergency Social Services resources, etc.). For other events (i.e., where the CER is the Lead) RCAU will play a central role. Depending on the event, the RCAU may also share pre-assessed capability assessments and/or materials from exercises or other existing preparedness/planning materials. The purpose of the Capability Assessment is to determine what activities and/or resources are available and to help inform a decision on Health Portfolio Activation. |
| Significant Events | The Lead, CIRA and RCAU can use the following considerations to determine whether an event is significant and potentially requires support from the HPOC: Geographic reach and impact:
Public health impact:
Visibility of the hazard:
Legislative or mandated requirements:
Requirement for Health Portfolio coordination, surge capacity or centralized response planning:
|
| Contacting CER | If response efforts are likely to exceed the Lead's capacity, their DG must advise the ED CER, VP ROEMB and HPOC single window for situational awareness. Depending on severity and/or urgency, the Lead may also notify Health Portfolio DGs, VP/ADMs, Deputy Heads, CPHO and/or HPEG as appropriate or based on requirements in hazard-specific annexes. |
3.3 Phase 3 – Initial event assessment and response activation
Summary: The CER initiates event support by convening an Initial Action Team meeting (for fast-moving events) or a Health Portfolio SAT meeting (for larger-scale, slower-moving events). Either way, this meeting will:
- Provide an updated situational assessment;
- Review risks and capabilities;
- Establish an initial response strategy with goals, objectives and required resources; and
- Begin notifying the implicated Lead, Programs/Regions, Health Portfolio decision-makers and external partners of the meeting outcomes immediately following the meeting.
Optional outputs include:
- Designation of Health Portfolio Activation Level (0-3), per authorities;
- Identification of escalation triggers; and
- Designation of response tools required to effectively manage the event (e.g., IMS, HPCC, HPEG, Health Portfolio SAT, etc.).
This forum may also be used to discuss:
- concurrent plan activation (e.g., FNEP, Chemical Annex) if applicable;
- initial internal CER situational assessments;
- outreach to stakeholders; and
- considerations for briefing upward to support decision-making.
If immediate mobilization of an IMS is warranted to respond to significant/severe events (e.g., confirmed release of radiological/nuclear material in Canada, severe earthquake, etc.), CER will resource an IMS in the initial stages of a response (following approval by the appropriate executive level) until broader Health Portfolio resources can be mobilized. Phase 5 of the ERP will be immediately initiated, with available information shared amongst partners to support coordination efforts.
Starts with: The HPOC/CER convenes an IAT or Health Portfolio SAT meeting to assess and implement appropriate event response measures.
Ends with: Notifications issued to establish horizontal Health Portfolio situational awareness, Phase 4 approval sought to confirm response activities, goals and objectives and guide subsequent incident action planning and response activities.
| Theme | Actions |
|---|---|
| IAT meeting |
|
| Health Portfolio SAT | Purpose A Health Portfolio SAT meeting may occur multiple times during an event, either replacing or following an IAT meeting, to provide additional strategic outcomes, including assessment of:
Health Portfolio SAT Participants The CER provides the Health Portfolio SAT Secretariat function; it is responsible for maintaining the core membership list and engaging the Lead to identify additional participants as warranted. The ED CER or their designate chairs the meeting. Other participants will provide critical input from their program areas. The list below is flexible and should be adapted to reflect the nature, complexity, scope and speed of the event, while also ensuring that no response elements or capabilities are overlooked. DGs may delegate participation to technical subject matter experts. ROEMB
Lead
Corporate Data and Surveillance Branch
Health Security and Regional Operations Branch
Corporate Services Branch
Other
Standing Agenda The meeting should be rapid, flexible and non-prescriptive. See Annex C for a sample agenda. Outcomes should be documented and shared with participants by adapting the agenda as a Decision Brief, or through a standard Record of Decision as warranted. |
3.4 Phase 4 – Response strategy review and approval
Summary: Phase 3 outcomes are provided by the CER to the appropriate executive level for approval.
If an HPEG has been established, Health Portfolio Activation escalation/de-escalation and/or IMS mobilization/demobilization requires HPEG approval.
Starts with: Decision-makers with the appropriate level of authority receive an overview of the situation, a risk and capability assessment and recommended Health Portfolio goals, objectives and response activities.
Ends with: Decision-makers review and approve the initial event response strategy, incorporating any desired changes.
| Level | Authority (for escalation/de-escalation) |
|---|---|
| 0: Routine ops (Green) |
N/A |
| 1: Enhanced reporting and planning (Yellow) |
DG Centre for Emergency Response + Lead counterpart (or delegates) |
| 2: Mobilized response (Red) |
VP Emergency Management Branch + Lead counterpart (or delegates) |
| 3: Full-scale activation (Purple) |
PHAC President / Health Canada Deputy Minister By recommendation of VP ROEMB, Lead counterpart (or delegates) |
3.5 Phase 5 – Response Implementation and Action Planning
Summary: Following executive approval, the VP ROEMB/ED CER will designate an Event Manager to implement response action planning in alignment with established event risks, capabilities, goals, objectives and activities.
Starts with: Identification of the Event Manager, implementation of incident action planning and management by objectives.
Ends with: When it is determined that Health Portfolio response goals and objectives have been met, the EM instructs the Planning Chief to initiate Phase 6 (De-escalation and demobilization).
| Theme | Actions |
|---|---|
| Event Manager Selection | The Event Manager is identified by the VP ROEMB/ED CER and may be appointed from a roster of qualified EMs from across the Health Portfolio with previous experience and/or specialized training. Selection is approved by the ED CER, VP ROEMB, HPEG (if established) and/or the PHAC President. |
| Management by Objectives | Response action planning will be driven by established response goals and objectives and will define the strategies to achieve them through specific actions. |
| Action Planning Cycle | Due to the unpredictable nature of events, objectives will change as the situation evolves, with Health Portfolio response requirements adjusted accordingly. This fluidity is best managed using an iterative planning process that is based on regular, cyclical re-evaluation of response requirements and objectives known as the action planning cycle. This cycle includes:
The first iteration of the planning cycle will be heavily informed by the situational assessment and initial ERP Response Phases that preceded it, e.g., the outcomes of the IAT and HP SAT meetings or HPCC as applicable. |
| Incident Action Plan | The IAP describes the specific objectives for a set operational period to achieve larger event management goals. During the early stages of the response, it is likely that the initial plan will be developed quickly with incomplete situational information. As the response effort evolves over time, IMS staff and better information will become available and shared, and connectivity will enable more detailed planning. IAPs are a key tool in the early identification of the need to adjust a response posture and should include bidirectional indicators/criteria to guide escalation or de-escalation based on response objective status. See Appendix D for an example of the de-escalation bidirectional indicators used for COVID-19. |
| IMS | If and when an IMS is mobilized by the appropriate executive level authority, CER will establish an IMS structure, identify the required functions and program areas required for the IMS, initiate the mobilization of personnel and send a notification via the HPOC single window to inform implicated staff and partners of activation activities. The maintenance of rosters and the identification and resourcing of personnel are led by HPOC, with processes differing in the Regions and NMLB. Health Portfolio programs may also maintain their own rosters to support generic IMS or specialized technical functions. ***Mobilization also refers to the temporary assignment of Health Portfolio employees outside of their normal work function and/or location to support efforts related to event response; this may include external domestic and international mobilizations. |
3.6 Phase 6 – De-escalation and demobilization
De-escalation of Health Portfolio Activation Levels and response posture follows the inverse process and same authorities as escalation.
Demobilization of an IMS is recommended by the Planning Group to the EM, who may in turn consult with ED CER VP ROEMB or Lead VP/ADM.
For responses where an HPEG has been established as the senior strategic-level decision-making body, de-escalation or demobilization requires their approval.
The need for de-escalation or demobilization should be continually reassessed during a response to ensure that the event remains appropriately framed and adequately resourced.
Following approval to de-escalate or demobilize, the HPOC single window releases a broad notification to all internal and external stakeholders. Health Portfolio programs and the HPOC return to normal operations.
Summary: The need for de-escalation or demobilization is continually reassessed throughout the action planning cycle described in Phase 5.
Starts with: De-escalation triggers or demobilization plan criteria are met.
Ends with: Health Portfolio programs and the HPOC return to normal operations and initiate Phase 7 After Action Review.
| Theme | Actions |
|---|---|
| IMS Demobilization | Process: Demobilization planning is led by the IMS Planning Chief with input from the other IMS sections and Health Portfolio programs. Significant, protracted national public health emergencies (e.g., COVID-19) could implicate the HPEG or provinces/territories in de-escalation discussions. See: FPT Public Health Response Plan for Biological Events. The demobilization process will be informed by technical situational/risk assessments, with surveillance information and possibly modelling forming the basis for these assessments. Ongoing operational coordination requirements to maintain the response and support program areas (e.g., frequency of senior briefings, reporting and communications demands) will also factor into demobilization recommendations. Plan: The EM is responsible for tasking the IMS Planning Chief with the development of a formal demobilization plan. Not all levels of responses will require the same level of effort and detail for demobilization. The template for a demobilization plan and guidance to develop one are maintained by the CER. Criteria: Demobilization criteria should be specific to the event but may include the following:
HR Demobilization: The most important Health Portfolio resource used during event response is our staff. In addition to developing surge planning strategies and approaches for specific events to efficiently add event response capacity, the CER should engage appropriate internal resources (e.g., HR, Corporate Services, Psychosocial teams, etc.) to ensure that staff who support response efforts are in turn effectively supported in demobilizing to their regular work. This should include debriefings for continual improvement, access to any required well-being supports and appropriate recognition for their efforts. Bidirectional criteria: used for events for which Health Portfolio impacts and resource requirements repeatedly increase and decrease, along with the accompanying transfer of functions between the IMS and Lead. See Appendix D for the criteria used to manage COVID-19. |
| Recovery | The process of returning to "normal operations" (vs. normal conditions) is different from recovery. Recovery consists of activities aimed at restoring normal conditions after an emergency. Public health recovery from an emergency may range from hours to years depending on many factors such as persistence of the hazard, the magnitude of the event, the size and vulnerability of the affected populations and the coping capabilities of the jurisdictions concerned. While recovery activities are outside the scope of the ERP, it is recognized that activities such as scientific and analytical advice, public health risk assessment and guidance to physicians are examples of support that may require ongoing support from Health Portfolio programs following an event to help address the long-term health effects. |
3.7 Phase 7 – After action review
Summary: Following an event, an After-Action Review (AAR) process may be conducted to create an AAR Report documenting best practices and opportunities for improvement, while also identifying recommendations for specific, actionable improvements and corrective actions.
Starts with: The Event Manager, Planning Chief and Emergency Management Continuous Improvement Team (EMCI) agree to the AAR process best suited to the response.
Ends with: The AAR report is shared through Health Portfolio emergency management governance bodies for review and comments and is ultimately approved by the VP ROEMB.
| Theme | Actions |
|---|---|
| After Action Reviews | These are part of the Health Portfolio's routine emergency response cycle and provide an opportunity to capture the lived experience of personnel, reflect best practices and opportunities for improvement and identify actionable recommendations that will enhance the Health Portfolio's resiliency for future events. While there is a focus in capturing observations after the event, it is equally important to ensure that a continuous improvement lens is applied to the event response. This encourages a robust real-time review that supports course corrections. Additionally, it is recommended that a real-time capture of observations be integrated into HPOC structures to ensure that gaps are identified, and best practices are codified. |
| Roles, Responsibilities and Accountabilities | The AAR will be tasked by the HPOC EM and led by EMCI in collaboration with key partners. AAR planning will usually take place only for Level 2 or 3 events and is normally triggered once de-escalation and/or demobilization are underway. In the event of prolonged responses, CER may ask EMCI to conduct a review during a specific period or phase of the response to inform course corrections and/or review a specific time period or response activity. CER will engage EMCI to initiate the review planning process, following which EMCI will aim to initiate review activities within 60 days of return to normal operations. The Event Manager and EMCI will jointly establish the AAR objectives and scope, which will inform further preparations such as the format for collecting observations and identifying participants. |
| AAR Process | Collecting and Reviewing Relevant Background Information To support the AAR process, the HPOC will provide EMCI with adequate background information to understand the response actions implemented. This may include plans, event-specific products, chronology and operational functions. Capturing Observations To analyze actions taken in response to an event and to identify challenges and best practices, the EMCI team may use a mixed-method approach to collect observations. This may include facilitator-led discussions (hotwashes), targeted interviews, surveys and other types of written input. The mixed methodology will seek to identify observations along the pre-approved themes, which may include:
While observations are primarily collected following an event, efforts should also be made to capture them throughout the response. |
| Drafting the Final AAR Report | At the close of the AAR, EMCI will prepare an AAR Report that summarizes best practices and opportunities for improvement and provides actionable recommendations to enhance the Health Portfolio's operational readiness for future events. The Report may be shared with the Centre for Emergency Response and Lead for review, and will be shared through existing governance structures for review and endorsement. A final version will be approved at the Vice President level, and may be shared with Lead executives, Health Portfolio governance structures or otherwise for awareness and follow-up. |
| Implementing Recommendations | Upon final approval of the AAR, Offices of Primary Interest (OPI) will be identified for all recommendations. The AAR report will be presented to Health Portfolio emergency management governance bodies, which may request an Action Plan to track the execution of recommendations and/or designation of a lead to oversee implementation through a process such as a Management Response Action Plan. |
| AAR Activities by Other Partners | In large scale or prolonged activations requiring national coordination, concurrent AARs may be developed by other Health Portfolio groups (e.g., Programs, Office of Audit and Evaluation) and/or OGDs. If a Lead identifies AAR requirements for internal purposes and/or lower-level activations, EMCI can provide advisory support and products to help enable this process. Further, as a shared service, the Office of Audit and Evaluation (OAE) plays an important oversight and advisory role by conducting reviews that support improvements to the Health Portfolio's EM functions. The OAE may lead on evaluating specific elements of a Health Portfolio response and may leverage support from third-party external evaluators. Further, the Health Portfolio may also contribute to AARs led by P/Ts through the F/P/T Public Health Network Council. |
Appendix A: Generic health portfolio IMS
Health Portfolio Incident Management System/ Multiple Hazard Emergencies
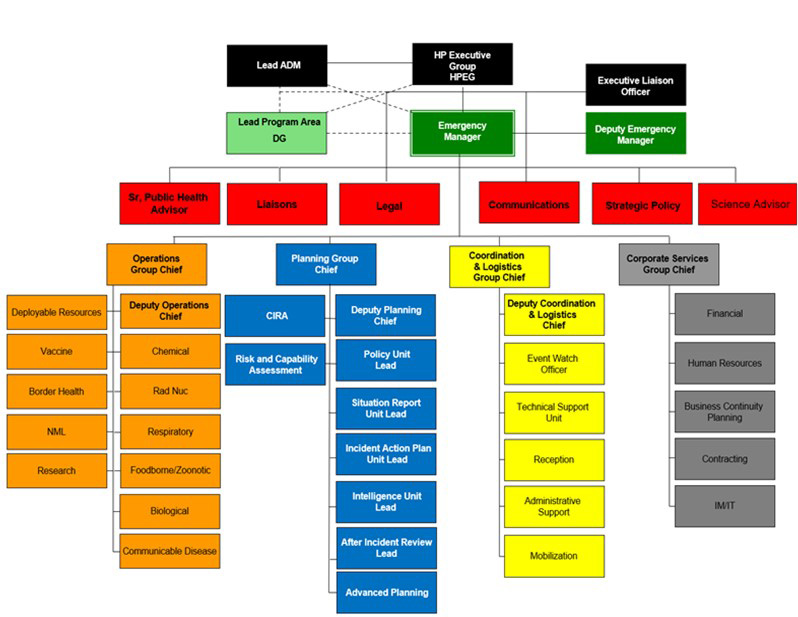
Text description
The depiction of an Incident Management System for multiple hazard emergencies. The structure appears as an organizational chart with multiple levels. The first level at the top is the leadership level, comprised of:
- Health Portfolio Executive Group
- Lead ADM
- Lead Program Area DG
- Emergency Manager
- Executive Liaison Officer
- Deputy Emergency Manager
The next level down are the boxes for Command Staff and advisors. These include:
- Senior Public Health Advisor
- Liaisons
- Legal
- Communications
- Strategic Policy
- Science Advisor
Underneath this level are four different streams led by a Group Chief:
- Operations Group Chief
- Planning Group Chief
- Coordination and Logistics Group Chief
- Corporate Services Group Chief
On the left side of the structure is the Operations Group Chief under which there are various functions that include:
- Deployable resources
- Vaccine
- Border Health
- NML
- Research
- Deputy Operations Chief
- Chemical
- Radiological/Nuclear
- Respiratory
- Foodborne/Zoonotic
- Biological
- Communicable Disease
On the left side of the Operations Group Chief is the Planning Group Chief under which there are various functions that include:
- CIRA
- Risk and Capability Assessment
- Deputy Planning Chief
- Policy Unit Lead
- Situation Report Unit Lead
- Incident Action Plan Unit Lead
- Intelligence Unit Lead
- After Incident Review Lead
- Advance Planning
On the left side of the Planning Group Chief is the Coordination and Logistics Group Chief under which there are various functions that include:
- Deputy Coordination & Logistics Chief
- Event Watch Officer
- Technical Support Unit
- Reception
- Administrative Support
- Mobilization
On the left side of the Coordination and Logistics Group Chief is the Corporate Services Group Chief under which there are various functions that include:
- Financial
- Human Resources
- Business Continuity Planning
- Contracting
- IM/IT
Note: The emergency response structure is scalable, and all the functional areas depicted are unlikely to be mobilised at the same time. The exact make up of the response structure will vary depending on the nature of the event. Two or more events/ emergencies occurring simultaneously that are different in nature (i.e., Infectious Disease and Chemical) will require hazard specific Operations leaders who will report to an all-hazards Operations Chief. This is the distinction between the standard HP Emergency Response Structure for one event.
Appendix B: Acronyms
- AAR
- After Action Report
- ADM
- Assistant Deputy Minister
- AP
- Action Plan
- BCP
- Business Continuity Plan
- CBRN
- Chemical, Biological, Radiological/Nuclear
- CEP
- Centre for Emergency Preparedness
- CEPRU
- Chemical Emergency Preparedness and Response Unit
- CER
- Centre for Emergency Response
- CFEZID
- Centre For Food-Borne, Environmental and Zoonotic Infectious Diseases
- CFIA
- Canadian Food Inspection Agency
- CIRA
- Centre for Integrated Risk Assessment
- CIRID
- Centre for Immunization and Respiratory Infectious Diseases
- CLG
- Coordination and Logistics Group
- CONOPS
- Concept of Operations
- CPAB
- Communications and Public Affairs Branch
- CPHLN
- Canadian Public Health Laboratory Network
- CPHO
- Chief Public Health Officer
- CSB
- Corporate Services Branch
- DG
- Director General
- DM
- Deputy Minister
- ED
- Executive Director
- EM
- Event Manager
- ROEMB
- Regulatory, Operational and Emergency Management Branch
- EMCI
- Emergency Management Continuous Improvement
- EMCT
- Emergency Management Coordination Team
- EMPECI
- Emergency Management Plans, Exercises and Continuous Improvement
- EOCs
- Emergency Operations Centres
- ERC
- Emergency Response Cell
- ERP
- Emergency Response Plan
- ESF
- Emergency Support Function
- FERP
- Federal Emergency Response Plan
- FNEP
- Federal Nuclear Emergency Plan
- GPHIN
- Global Public Health Intelligence Network
- HC
- Health Canada
- HP
- Health Portfolio
- HPCC
- Health Portfolio Coordination Committee
- HPEG
- Health Portfolio Executive Group
- HPOC
- Health Portfolio Operations Centre
- HP SAT
- Health Portfolio Situational Assessment Team
- HP SEMP
- Health Portfolio Strategic Emergency Management Plan
- HVE
- High Visibility Events
- IAEA
- International Atomic Energy Agency
- IAP
- Incident Action Plan
- IAT
- Incident Action Team meeting
- IHR
- International Health Regulations
- IMS
- Incident Management System
- JAS
- Job Action Sheets
- MCMs
- Medical Counter Measures
- MINO
- Minister's Office
- MRAP
- Management Response Action Plan
- NESS
- National Emergency Strategic Stockpile
- NGO
- Non-Governmental Organization
- NMLB
- National Microbiology Laboratory Branch
- NMLB OC
- National Microbiology Laboratory Operations Centre
- OAE
- Office of Audit and Evaluation
- OGD
- Other Government Department(s)
- OIA
- Office of International Affairs
- OPI
- Office of Primary Interest
- PAHO
- Pan American Health Organization
- PCO
- Privy Council Office
- PHAC
- Public Health Agency of Canada
- PHEIC
- Public Health Emergency of International Concern
- PHN
- Public Health Network
- PMO
- Prime Minister's Office
- PTs
- Provinces/Territories
- RCAU
- Risk and Capability Assessment Unit
- RECC
- Regional Emergency Coordination Centre
- RFA
- Request for Assistance
- SME
- Subject Matter Expert
- SOP
- Standard Operating Procedures
- VP
- Vice President
- WHO
- World Health Organization
Appendix C – Health Portfolio situational assessment team (Health Portfolio SAT) standing agenda/decision brief template
Event Name:
Date and Time of Meeting:
Meeting Location:
Dial-in Information:
Local:
Long Distance:
Conference Id:
Chair: DG, Centre for Emergency Response (or designate)
Co-Chair: DG, HP Lead Program Area
Recommended Participants: Health Portfolio Operations Centre, HP Lead Program Area, Impacted Region(s), Public Health Medical Advisor, Centre for Integrated Risk Assessment, National Microbiology Laboratory, National Emergency Strategic Stockpile, Communications, Strategic Policy, Office of International Affairs, Office of Border and Travel Health, Legal Services, Health Equity, Risk and Capability Assessment, Public Health Security and Intelligence, CEP Emergency Management Planning, CEP Continuous Improvement, Other (as required)
Attendance:
Secretariat: Health Portfolio Operations Centre (HPOC)
Purpose: The purpose of the Health Portfolio SAT meeting is to address the following issues:
- What are the potential implications of relevance to the Health Portfolio mandate?
- What capabilities might the Health Portfolio need to bring to bear?
- Is there a requirement for an HPOC IMS to lead/support coordination? If so, what will be the purpose/goal of that IMS, what are the immediate/near-term priorities? What are the functions that need to be established?
Instructions: After the outputs are captured from the Health Portfolio SAT, this document may be submitted to the relevant level of Senior Management as a Decision Brief.
| Time | Item | Outputs |
|---|---|---|
| 00:00 – 00:10 |
Orientation and Situation Synopsis Lead: ED CER Once the Health Portfolio SAT meeting is convened, the DG of CER will provide an overview of the purpose of the Health Portfolio SAT. They will review the agenda, outline the meeting objectives and what is hoped to be achieved by the end of the meeting. The Chair will identify and document the Lead for the event/response. They will brief the team on the situation and confirm the ERP triggers/considerations that warranted a coordinated Health Portfolio response. If other plan triggers have been met based on the current state of the event, they should also be presented and discussed (i.e., hazard-specific annexes, FTP Bio, etc.) – see below. The ED CER should lead participants through the risk assessment review, identification of response goals and objectives, initial mitigation measures and capability assessment and consideration of concurrent plan activation. |
n/a |
| 00:10 – 00:25 |
Risk Assessment Lead: Program Area DG and CIRA Identify and document the Lead for this input. Has a risk assessment been completed? Does one need to be developed? What do we know about the current risk of the event? Have we assessed the risk of the event for equity-deserving populations? Potential areas to consider with respect to risk:
|
n/a |
| 00:25 – 00:35 |
Response Goals and Objectives Lead: ED CER
|
n/a |
| 00:35 – 00:45 |
Initial Mitigation Measures and Capability Assessment Lead: Program Area DG and Risk and Capability Assessment Unit, ROEMB Identify and document the lead program area/s for this input. Guided by the Health Portfolio Capability Catalogue. Discussion on initial mitigation measures implemented, and capabilities at hand and required. What capabilities does the Health Portfolio currently have in place? What are the capabilities we are mandated to have in place? Have these capabilities been recently assessed against this event? What are the gaps in capabilities? Example of capabilities for discussion:
|
n/a |
| 00:45 – 00:50 |
Concurrent Plan Activation Lead: ED CER Consider future potential hazard-specific triggers or concurrent activation of other key plans. This should be prepared in consultation with PHAC's Emergency Management Branch Planning Unit SMEs. |
n/a |
| 00:50 – 1:00 |
Decision on potential Health Portfolio IMS Activation Lead: Program Area DG and ED CER At this point, the meeting is returned to the ED CER to summarize key points and formalize the group's recommendations. Note on High Visibility Events (HVE): Generally speaking, the risk and capability assessments will inform the necessity of mobilizing an IMS. In some cases, however, there may be an emerging issue that is receiving, or is likely to receive (in Canada or abroad), a high degree of media public and/or political attention. These types of events may not represent an actual public health risk; however, risk perception may necessitate activation of the IMS to support enhanced Health Portfolio coordination (e.g., communications and briefing) |
n/a |
Summary:
| Activation Level | Authority Requirement for Approval |
|---|---|
| Level 1 | n/a |
| Level 2 | n/a |
| Level 3 | n/a |
| Other: | n/a |
Immediate Courses of Action:
Courses of Action are the required actions for accomplishing each of the objectives identified above. These are typically developed by answering the following questions: What is the action? Who is responsible? When does it take place? What are the resources needed to perform the action?
- Example: The HPOC (who) will refer to existing rosters (what) in order to mobilize the appropriate personnel (resources) for the required IMS structure, by date (when).
Key Messages (delete if already captured above):
Approved by:
(Name) DG, CER, or alternate
(Name) DG, Program Area (if applicable)
Date:
Month/Day/Year
Appendix D: Sample de-escalation bidirectional indicators
Indicators Used to Inform De-escalation of the Incident Management System for COVID-19 – COVID-19 Readiness Dashboard
COVID-19 IMS De-escalation / Escalation Readiness Assessment
- The readiness assessment tool, using ten bi-directional criteria, is applied to validate programs' capacity to manage their COVID-19 demands, responsibilities and assess the programs' operational needs/support required by the COVID-19 IMS.
- The culmination of this information results in a recommendation for the COVID-19 IMS activation level to be lowered, escalated or remain at status quo.
| Category | Criteria | Current State | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | 2022 | 2023 | |||||||||
| Nov | June 6 | Jul 19 | Aug 3 | Sep 26 | Oct 28 | Nov 28 | Dec 31 | Jan 26 | Feb 22 | ||
| Level 3 | Level 2 | ||||||||||
| 1. Domestic Situation | 1.1 Extent of IMS supporting programs with epidemiological analyses / surveillance. | H | L | L | L | L | NIL | NIL | NIL | NIL | NIL |
| 1.2 Extent of IMS supporting programs / PTs with Requests for Assistance (RFAs) for PHAC-related surge support. | H | L | L | L | L | L | L | L | NIL | NIL | |
| 1.3 Extent of IMS supporting other government departments and P/Ts and their role in COVID surveillance, response, border and travel and public health measures. | H | M | L | L | L | L | L | L | L | L | |
| 1.4 Extent of IMS supporting the Regional Emergency Coordination Centers (RECCs). | H | L | L | L | L | NIL | NIL | NIL | NIL | NIL | |
| 2. International Situation | 2.1.Extent of IMS supporting programs in international epidemiological analyses / surveillance. | H | L | L | L | L | L | NIL | NIL | NIL | NIL |
| 2.2 Extent of IMS supporting engagement with international partners / federal departments (e.g., GAC). | H | M | L | L | L | L | L | L | L | L | |
| 3. Coordination / Briefing | 3.1 Change in frequency of meetings and scope of issues required for taskings including briefings, briefing products, committee hearings, and other coordination efforts. | H | L | L | L | L | L | L | M | L | L |
| 3.2 Change in IMS operational and standby requirements and incurred overtime. | H | L | L | L | L | L | L | L | L | L | |
| 3.3 Change in frequency of incoming reports and requirement for outgoing IMS reporting products including Situation Report, Incident Action Plan, Placemats and Surge Report. | H | M | M | M | M | M | L | M | M | L | |
| 3.4 Change in frequency of PHAC COVID communications (news releases, press statements, QPs, Parliamentary documents, web pages, guidance documents) that require review and input from the IMS. | H | M | M | M | L | L | L | L | L | L | |
Recommendation: In the Agency, programs have evolved to meet the challenge of COVID response. The pandemic is not over, but the Agency is at a stage where programs can fully assume response operations from the COVID-19 IMS. It is recommended that the COVID-19 IMS de-escalates, effective March 1, 2023. This is the final readiness assessment dashboard by the COVID-19 IMS |
|||||||||||
Appendix E: Annex 2: of the IHR decision instrument
Under the International Health Regulations (2005), each state party must assess events (a manifestation of disease or an occurrence that creates a potential for disease) occurring within its territory by using the following decision instrument. The decision instrument contains a series of questions which, if the answer to any two of them is yes, require the States Party to notify the WHO, within 24 hours of making the assessment, of all events that may constitute a public health emergency of international concern (PHEIC).
If immediate global action is needed to provide a public health response to prevent or control the international spread of disease, the IHR (2005) give the Director General of WHO the authority to determine that the event constitutes a PHEIC. On such occasions, an IHR Emergency Committee will provide its views to the Director General on temporary recommendations on the most appropriate and necessary public health measures to respond to the emergency. Annex 2 Decision Instrument for the Assessment and Notification of Events That May Constitute A Public Health Emergency of International Concern can be found on pages 52 – 53 of the following:
International Health Regulations (2005) Third Edition
Endnotes
- Footnote 1
-
A comprehensive HP glossary of emergency management terminology will be developed to compliment this plan. In the interim, the Emergency Management Vocabulary developed by the Translation Bureau and Public Safety Canada provides relevant French and English emergency management terminology. PDF: https://publications.gc.ca/collections/collection_2012/tpsgc-pwgsc/S52-2-281-2012.pdf
- Footnote 2
-
Cyclical events are natural disasters that are expected to occur on a regular basis in Canada, and with increasing frequency owing to climate change e.g., wildfires, flooding, extreme temperatures.
- Footnote 3
-
Mass events are significant social, political, cultural or sporting events. Significant public confidence or portfolio risks justify categorizing these as a High Visibility Event.
- Footnote 4
-
A higher authority can always direct escalation/de-escalation (e.g., Minister, PHAC President, etc.). If the Health Portfolio Executive Group is active, they must approve escalation/de-escalation.