Federal Framework on Posttraumatic Stress Disorder: Recognition, collaboration and support
Download the alternative format
(PDF format, 2.1 MB, 94 pages)
Organization: Public Health Agency of Canada
Published: 2019-01-22
Related Topics
Table of Contents
- Acknowledgements
- Minister's message
- Executive summary
- Part I: Context and background
- Organizational roles and responsibilities
- Informing the Framework
- Part II: The Federal Framework on PTSD
- The Framework at a glance
- Scope and purpose of the Framework
- Vision
- Guiding principles
- Priority areas
- Priority Area 1: Improved tracking of the rate of PTSD and its associated economic and social costs
- Priority Area 2: Promotion of guidelines and sharing of best practices related to the diagnosis, treatment and management of PTSD
- Priority Area 3: Creation and distribution of educational materials related to PTSD to increase national awareness and enhance diagnosis, treatment and management
- Priority Area 4: Strengthened collaboration and linkages among partners and stakeholders
- Part III: Moving forward
- Conclusion
- Part IV: Appendices
- Appendix A – Federal Framework on PTSD Act and observations from the Senate Committee
- Appendix B – Other populations affected by PTSD
- Appendix C – Current PTSD initiatives in Canada
Abbreviations
- CAF
- Canadian Armed Forces
- CCG
- Canadian Coast Guard
- CFNU
- Canadian Federation of Nurses Union
- CIHR
- Canadian Institutes of Health Research
- CIMVHR
- Canadian Institute for Military and Veteran Health Research
- CIPSRT
- Canadian Institute for Public Safety Research and Treatment
- CISM
- Critical Incident Stress Management
- CSIS
- Canadian Security Intelligence Service
- DFO
- Department of Fisheries and Oceans
- DND
- Department of National Defence
- EAP
- Employee assistance programs
- EAS
- Employee Assistance Services
- LGBTQ2
- Lesbian, Gay, Bisexual, Transgender, Queer, Two-Spirit
- MHCC
- Mental Health Commission of Canada
- MHFA
- Mental Health First Aid
- OSI
- Operational stress injury
- OSISS
- Operational Stress Injury Social Support
- OTSSC
- Operational Trauma and Stress Support Centres
- PHAC
- Public Health Agency of Canada
- PSC
- Public Safety Canada
- PTSD
- Posttraumatic Stress Disorder
- PTSI
- Posttraumatic Stress Injuries
- RCMP
- Royal Canadian Mounted Police
- VAC
- Veterans Affairs Canada
Acknowledgements
The Federal Framework on Posttraumatic Stress Disorder (PTSD)Footnote a was developed in recognition of those who live with PTSD, their families and support networks and those who are at risk of developing PTSD.
We are deeply grateful for the impassioned involvement of the many partners and stakeholders who informed the development of the Framework through: the National Conference on PTSD in April 2019; our official governance structure; and, the many conversations that have taken place since the Federal Framework on PTSD Act received Royal Assent in June of 2018. These partners and stakeholders include federal government departments, non-governmental organizations, provincial and territorial groups and governments, Indigenous organizations and other experts reflecting the diversity of Canada's geographical and social communities.
Many who contributed to the Framework have experienced PTSD firsthand. We acknowledge their lived and professional expertise and are grateful for their candour in sharing their insights.
Finally, we acknowledge that symptoms of PTSD are not always recognized by individuals, family members, co-workers, support networks, health care providers, or employers. Stigma and other barriers to timely diagnosis, care and treatment remain. The Framework, which would not have been possible without our partners and stakeholders, will help us work together to address these challenges.
If you or someone you know needs mental health support, you are not alone. Please visit the Government of Canada Mental Health Support web page for more information.
Minister's message
I am privileged to share Canada's first Federal Framework on Posttraumatic Stress Disorder (PTSD). Many Canadians may develop PTSD during their lifetimes in the wake of exposure to trauma. The Framework recognizes that a great number face increased risks because of the unique nature and demands of their occupation.
The release of the Framework marks an important milestone in our efforts to better recognize, collaborate with and support those impacted by PTSD. The content was informed by a national conference on PTSD held in April 2019, and further developed with the direct involvement of a diverse group of stakeholders and partners, including those with lived experience. We heard many inspiring stories of courage and healing. At the same time, we heard about significant gaps and lack of access to PTSD supports across Canada. We are hopeful that many of the relationships we have built during the development of the Framework will continue to grow as we move forward to address these gaps.
While important advances have been made in a relatively short period, our work must continue. The call to action from our partners and stakeholders was evident: we must end the stigma, improve our understanding of PTSD, promote evidence-based practices for its treatment and management, increase awareness and learn from each other by working collaboratively.
As we move forward, the Framework can guide our collective efforts. It encourages us to work together to advance our knowledge of PTSD, while building on many important initiatives and investments that are already in place.
Through the actions outlined in the Framework, we hope to make a meaningful difference in the lives of those affected by PTSD. I sincerely thank all those who contributed to the Framework's development and have helped us get to this point. I am confident that with the help of our partners and stakeholders, we can achieve the vision set out in this document, "A Canada where people living with PTSD, those close to them, and those at risk of developing PTSD, are recognized and supported along their path toward healing, resilience, and thriving."

The Honourable Patty Hajdu, P.C., M.P.
Minister of Health
Quotes
"The Government of Canada is providing national leadership to help address the mental health needs of Canadians who are impacted by PTSD and post-traumatic stress injuries (PTSI). Public safety personnel put their lives on the line every day, which can put them at risk of developing PTSI. That is why last April we released a national action plan on PTSI for all public safety personnel across Canada. I am pleased to see the Federal Framework on PTSD building on this work and the work of others."
The Honourable Bill Blair
Minister of Public Safety and Emergency Preparedness
"While we have come a long way in our understanding of the invisible wounds that Canada's Veterans may be struggling with, we know more must be done. With this Framework, our government pledges to support effective programs and treatment for all these brave Canadians. I congratulate everyone who contributed to the creation of this Federal Framework, and I thank all the brave Canadians it will serve for their sacrifices."
The Honourable Lawrence MacAulay
Minister of Veterans Affairs
"Posttraumatic Stress Disorder (PTSD) can have a profound impact on those faced with it and on their families, friends and colleagues. The Department of National Defence proudly supports the Federal Framework on PTSD. Through education, early intervention and world-class treatment we will make sure the women and men of the Canadian Armed Forces receive the highest standard of health care and support."
The Honourable Harjit Sajjan
Minister of National Defence
Executive summary
The Federal Framework on Post-Traumatic Stress Disorder Act became law on June 21, 2018, after receiving all-party support in Parliament. The Act underscores the diversity of occupational groups at higher risk of developing PTSD and the need for a coordinated approach to support those affected. As such, the Act called for the development of a comprehensive federal framework, informed by a national conference. The Public Health Agency of Canada (PHAC) was mandated to lead this work.
The National Conference on PTSD was held on April 9-10th, 2019, in Ottawa. Over 200 conference participants representing a wide-range of partners and stakeholders, including individuals with lived-experience, provided meaningful and productive dialogue on issues pertaining to:
- improved tracking of the rate of PTSD and its associated economic and social costs;
- the promotion of guidelines and sharing of best practices related to the diagnosis, treatment and management of PTSD; and,
- the creation and distribution of educational materials related to PTSD to increase national awareness and enhance diagnosis, treatment and management.
While the National Conference was the main consultation mechanism, engagement with partners and stakeholders continued throughout the development of the Framework. The entirety of engagement activities, as well as the requirements stated in the legislation, provided the foundation for the Framework.
Part I provides background and context, defining PTSD and providing information on occupations and populations at higher risk of developing PTSD. It describes key organizational roles and responsibilities for PTSD in Canada and summarizes the engagement that took place to inform this Framework, including highlights from the National Conference.
Part II, the heart of the Framework, sets out the scope, purpose, vision and guiding principles, including the importance of complementing existing initiatives and leveraging partnerships in addressing PTSD. This section also provides information on the drivers and considerations for each of the priority areas set out in the legislation, as well as federal actions setting the path to progress in each of them. Finally, an additional priority area highlighting the importance of collaboration among partners and stakeholders, which was not specifically articulated in the Act, is included in this section.
Part III outlines next steps in implementation, including the role of the PTSD Secretariat at PHAC. It reiterates the need for collaboration with all partners and stakeholders in advancing the priority areas, and encourages all parties to build on the vision and guiding principles of the Framework in advancing their own initiatives in the area of PTSD. It concludes by stating that the Framework is intended to encourage continuous open dialogue and that as we learn more about PTSD, the actions under this Framework will undoubtedly continue to evolve.
Additional information is provided in the Appendices. This section includes an overview of a number of non-occupation related populations at increased risk of developing PTSD, a high level synopsis of current PTSD initiatives in Canada, and a Glossary outlining definitions related to PTSD and trauma developed by the Canadian Institute for Public Safety Research and Treatment (CIPSRT) in collaboration with a number of experts.
As mandated by the Act, PHAC will complete a review of the effectiveness of the Framework within five years from the date of this Framework's publication.
Part I: Context and background
Introduction
Posttraumatic Stress Disorder (PTSD) has an enormous impact on individuals, families, caregivers, and workplaces. All Canadians can be at risk for PTSD following exposure to trauma, but some populations are at greater risk because of the type of job they do. That is why in June 2018, the Government of Canada enacted the Federal Framework on Post-Traumatic Stress Disorder Act (the Act), which called for the development of a Federal Framework on PTSD (the Framework). The Act, as well as the Observations provided by the Senate Standing Committee on National Security and Defence at the time of enactment, are included as Appendix A.
The Act specified three priority areas for the Framework:
- Improved tracking of the incidence rate and associated economic and social costs of PTSD;
- The establishment of guidelines regarding:
- the diagnosis, treatment and management of PTSD, and
- the sharing throughout Canada of best practices related to the treatment and management of PTSD; and
- The creation and distribution of standardized educational materials related to PTSD for use by Canadian public health care providers that are designed to increase national awareness about the disorder and enhance its diagnosis, treatment and management.
This Framework addresses occupation-related PTSD and builds on existing federal initiatives, such as Supporting Canada's Public Safety Personnel: An Action Plan on Post-Traumatic Stress Injuries, which focuses on supporting the mental health of public safety personnel, and the recently created Centre of Excellence on PTSD and Related Mental Health Conditions, funded by Veterans Affairs Canada.
The Framework acknowledges that people can be affected by PTSD outside of the occupational setting and broad applicability will be considered in the implementation of federal actions.
What is PTSD?
PTSD is a mental disorder that may occur after a traumatic event where there is exposure to actual or threatened death, serious injury, or sexual violence.Endnote 1 Potentially traumatic events include war/combat, major accidents, natural- or human-caused disasters, and interpersonal violence. PTSD can affect any person regardless of age, culture, occupation, sex, or gender.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a diagnosis of PTSD requires that the trauma be experienced throughEndnote 1:
- Direct personal exposure.
- Witnessing of trauma to others.
- Indirect exposure: learning that the traumatic event occurred to a family member or close associate.
- Firsthand repeated or extreme exposure to aversive details of a traumatic event(s).
Most people recover in a relatively short period following a traumatic event; however some people experience symptoms that worsen and persist over months or years. In some cases, the onset of symptoms may not appear until months or years after the experience. At present, we do not fully understand the biological, psychological, social, and environmental reasons for why individuals can react very differently to the same traumatic event.
A diagnosis of PTSD requires that symptoms be present for more than one month and cause significant distress or impairment in function. Symptoms of PTSD includeEndnote 1:
- Recurring, involuntary, intrusive, and distressing memories, nightmares, and/or flashbacks.
- Avoidance or attempts to avoid distressing memories, thoughts, feelings, or reminders of the event.
- Persistent negative changes in thoughts or mood (e.g., negative emotions, diminished interest in activities, inability to experience positive emotions, feelings of detachment).
- Changes in arousal or reactivity (e.g., irritable behaviour, angry outbursts, reckless or self-destructive behaviour, hyper-vigilance, exaggerated startle response, trouble concentrating, or disturbed sleep).
PTSD often occurs with other mental health conditions such as depression and substance use disorders; chronic diseases and conditions such as diabetes, high blood pressure, and chronic pain;Endnote 2,Endnote 3 and, suicidal thoughts and behaviours.Endnote 4,Endnote 5
The terms posttraumatic stress injury (PTSI) and operational stress injury (OSI) are increasingly used to describe mental health conditions related to traumatic events. On occasion, PTSI and OSI have been used interchangeably. By definition, a PTSI does not necessarily involve an injury following exposure to a traumatic event while serving in a professional capacity, whereas an OSI implies the injury was sustained as a result of operational duty. These non-clinical terms capture the full range of mental injuries that can occur following a traumatic event and include PTSD, depressive disorders, anxiety disorders, or substance use disorders. PTSI and OSI are used in an intentional effort to reduce stigma associated with other language (e.g., mental disorder or mental health problems).Endnote 6
Although the Framework focuses on PTSD as a clinically diagnosed mental health condition, the Government of Canada acknowledges that many different mental health conditions can result from exposure to traumatic events.
Can PTSD be prevented?
Currently, the only way we know of to prevent PTSD is to avoid exposure to traumatic events. Although mental health education and resiliency training can be beneficial, there is no evidence that these programs prevent the development of PTSD. The same is true of pre- or post- trauma debriefings.Endnote 7,Endnote 8
We do know that mental health education to increase knowledge and coping skills can alert people to early signs and symptoms of conditions such as PTSD, and may lead to early treatment-seeking behaviours. Timely evidence-based treatment of PTSD will help decrease the risk of long-term negative outcomes. This is especially important in cases where trauma exposures are more frequent due to the nature of an occupation.Endnote 9
Following exposure to a potentially traumatic event, many people experience distressing symptoms such as poor sleep, nightmares, and increased anxiety. However, the majority will recover from these symptoms spontaneously. Time, self-care and social support help, but some will go on to develop PTSD. Some evidence suggests that the severity of a traumatic event, lack of social support, or a history of adverse childhood experiences or previous mental health conditions can add to the risk of developing PTSD.Endnote 10,Endnote 11,Endnote 12
Who is affected by PTSD?
About three quarters of Canadians are exposed to one or more events within their lifetime that could cause psychological trauma.Endnote 13
A study using nationally representative data collected in 2002, based on self-reported symptoms, indicated that lifetime prevalence of PTSD in Canada was 9.2% and current (past month) prevalence was 2.4%.Endnote 13
The Canadian Community Health Survey – Mental Health, a nationally-representative survey in which participants were asked if they had a current diagnosis of PTSD, indicated prevalence rates of 1.0% in 2002 and 1.7% in 2012. An increase over time was observed among females — 1.2% in 2002 and 2.4% in 2012. The rates for males remained stable over time.Endnote 14
PHAC conducted a systematic review on the prevalence of PTSD in Canadian studies and found that data on PTSD is limited and updated statistics are needed. Reported rates of PTSD can vary across surveys because questions about PTSD are asked in different ways. The timeframe of questions can be shorter (e.g., past month) or longer (e.g., lifetime), with longer timeframes leading to higher rates. Some questionnaires collect data based on PTSD symptoms while others ask if an individual has been diagnosed with PTSD.Endnote 15
Many individuals with PTSD will not seek treatment because of stigma, lack of awareness, or other barriers. Also, individuals may be reluctant to share detailed mental health information. As a result, questions about a PTSD diagnosis may lead to different estimates than those based on symptom assessments, and both methods likely underestimate the true prevalence.
Sex, gender, and other factors can influence risk and vulnerability, access to health services, and socioeconomic consequences at different points in the life cycle. These factors intersect and can result in unique challenges that further complicate PTSD assessments and require additional research.
PTSD in men and women
- PTSD appears to be twice as common in women as in men.Endnote 16
- Men and women present symptoms of PTSD differentlyEndnote 17,Endnote 18:
- Women are more likely to report symptoms of numbing and avoidance, as well as concurrent mood and/or anxiety disorders.
- Men are more likely to report symptoms of irritability and impulsiveness, as well as concurrent substance use disorders.
- The uneven distribution of men and women in certain professions leads to research challenges. For example, over 90% of Canadian nurses are womenEndnote 19,Endnote 20 and over 95% of Canadian firefighters are men.Endnote 21
*Information about other gender identity and expressions is provided in Appendix B.
Below are some available data, evidence, and considerations for specific populations in Canada that are at increased risk for developing PTSD. This information is not intended to exclude any occupational group or population. Research and evidence about PTSD continues to evolve and it is possible that there are additional groups or occupations at higher risk.
Canadian Armed Forces Serving Members and Veterans
Canadian Armed Forces Serving Members
There are two broad categories of Canadian Armed Forces (CAF) membership: 1) Regular CAF members, who make a full-time commitment and often have dedicated their career to military service; and 2) Reserve Forces who generally work part-time in addition to pursuing their regular career or education. Both types of members can be enrolled in the Navy, Army, or Air Force.
Military-related PTSD can result from exposure to traumatic events experienced during training, deployment-related combat, peacekeeping and humanitarian operations, or as a result of non-deployment trauma (e.g., military police).Endnote 22 PTSD rates among serving military personnel and Veterans increase proportionately to their exposure to traumatic and disturbing events such as participating in combat roles, and events that transgress deeply held moral and ethical standards. (See text box on the concept of moral injury).Endnote 23 Among serving military personnel and Veterans, exposure to non-military related potentially traumatic factors, such as adverse childhood experiences, are also thought to play a role in susceptibility to PTSD in later life.Endnote 24
The Canadian Armed Forces (CAF) has reliable estimates of mental disorders in serving CAF members based on collaborative work with Statistics Canada and other related studies. According to a 2014 report, the number of active CAF Regular Forces members who reported symptoms of PTSD nearly doubled from 2002 to 2013 (from 2.8% to 5.3%).Endnote 25 In 2013, 16.5% of active CAF members had evidence of one or more of six mental disorders such as Major Depressive Disorder, PTSD, and Generalized Anxiety Disorder (GAD). Traumatic events experienced during deployment may be associated with a higher risk for mental disorders and suicide.Endnote 26
What is Moral Injury?
Moral Injury is an evolving concept that continues to be discussed among experts. It usually refers to a type of psychological trauma characterized by intense guilt, shame, and spiritual crisis. It can result from experiencing a significant violation of deeply held moral beliefs, ethical standards, or spiritual beliefs, experiencing a significant betrayal, or witnessing trusted individuals committing atrocities. Moral Injury has also been described as an injury to identity, core being, spirit, and sense of self that results in fractured relationships.Endnote 6
Canadian Armed Forces Veterans (Former CAF Members)
Veterans Affairs Canada (VAC) has reliable estimates of the prevalence of self-reported PTSD diagnoses in Veterans based on collaborative work with Statistics Canada. The prevalence of PTSD in Regular Force Veterans released from service during 1998-2012 and surveyed in 2013 was 13.1%. The rate was significantly higher than the general population, even after accounting for age and sex.Endnote 27 The prevalence of self-reported PTSD in Reserve Force Veterans deployed on operational duties with the Regular Force was 7.5%, which was also higher than the general population. Similar results were seen in Regular Force Veterans released during 1998-2015 and surveyed in 2016, where 16.4% reported PTSD.Endnote 28 In international studies, PTSD is usually higher in Veterans than among active serving members.Endnote 23 This may reflect in part the stresses that Veterans face when they leave the military and transition to civilian life or by differences in survey methods.Endnote 27
Public safety personnel
Public safety personnel include frontline personnel who ensure the safety and security of Canadians across all jurisdictions such as police, firefighters (career and volunteer), paramedics, correctional employees, border services personnel, operational and intelligence personnel, search and rescue personnel, Indigenous emergency managers, and public safety communications personnel (e.g., 911 operators, dispatchers). Given the broad range of occupations within the public safety community, it is important to recognize their distinct contexts and considerations related to experiences of trauma.
Public safety personnel may be at increased risk of PTSD because their jobs routinely expose them to a range of traumatic events.Endnote 29 They respond to crimes, accidents, and disasters and may witness or experience serious injuries, threats to life or death, as well as long-term exposure to disturbing material or communications. Feelings of guilt and shame may also contribute to the development of PTSD symptoms, particularly in situations where they were unable to help, identified with the victim or were overwhelmed by the event.Endnote 30
In a study conducted in 2016 and 2017, 44.5% of participating public safety personnel reported clinically significant symptoms consistent with one or more mental disorders. An estimated 23.2% showed symptoms of PTSD.Endnote 31
Health care providers
Nurses, physicians, psychologists, social workers, and other health care providers witness trauma, pain, suffering, and/or death on a regular basis in their work to care for the health of individuals, families, and communities.Endnote 32 Research about PTSD in health care providers in Canada is limited; however, available studies indicate that PTSD rates among health care providers are higher than in the general population.Endnote 33 For example, a report released in 2015 by the Manitoba Nurses Union indicated that one in four participating nurses reported PTSD symptoms. The same document indicated that 43% of new nurses experience high levels of psychological distress because of their work.Endnote 19,Endnote 20
Health care providers may also be called to care for individuals who remind them of loved ones, which can result in feeling guilt and shame if they are unable to help.Note de fin de document 19,Endnote 34 They may experience higher rates of compassion fatigue and/or burnout when caring for, empathizing with, and emotionally investing in, people who are suffering.Endnote 35 In addition, violence toward health care providers, such as nurses, is a serious concern and likely functions as a contributing factor to the development of PTSD.Endnote 19,Endnote 20,Endnote 36
Other occupations
There are other occupational roles or professions that also face an increased risk for developing PTSD. For example:
- Jurors may experience vicarious trauma as a result of exposure to traumatic content in the context of legal trials related to violent crimes.Endnote 37
- Journalists are exposed to potentially traumatic events when they arrive early on the scene and/or report about the circumstances of the event. Journalists (especially war correspondents) may also face an increased risk of personal physical harm.Endnote 38
Indigenous People who work in high-stress occupations and additional considerationsFootnote b
First Nations, Inuit and Métis individuals working in high-stress occupations (such as public safety personnel and health care providers) face unique challenges.
These frontline workersFootnote c are an integral part of Indigenous communities. Consequently, communities often have high expectations towards these workers. As a result, it may be difficult for frontline workers to set and maintain personal and work-life boundaries. In some cases, they may be the only one providing a specialized service in their community, and may have to intervene in a professional capacity during traumas and critical incidents involving family members or friends. They may also take on multiple roles in their community (e.g., as both a frontline worker and as a decision maker or leader determining how to respond organizationally or politically to a family or community crisis).Endnote 39 As a result, they may experience many different impacts from a singular trauma, which can lead to feelings of helplessness, numbness, avoidance and a reduction in empathy.Endnote 32
In addition, First Nation, Inuit and Métis frontline workers often serve communities that experience higher rates of poverty, mental health conditions, crime, or victimization.Endnote 40 Other challenges they may face include lack of resources and unsupportive human and organizational infrastructures. These challenges may worsen their own histories of trauma and put them at greater risk of experiencing mental health conditions, including PTSD.Endnote 41 The lack of resources and infrastructure also means there is often limited support to help frontline workers deal with the cumulative impact of stress and trauma, leading to potential long-term negative effects on their mental health and wellbeing.Endnote 42 All of these factors are magnified for workers in remote communities, who may also be confronted with isolation and extreme environmental conditions.Endnote 41
First Nations, Inuit, and Métis Peoples working in high-stress occupations outside Indigenous communities (e.g., in an urban center like Toronto or while serving in the Canadian Armed Forces) may also have their own personal history of trauma, which can increase their risk of developing mental health conditions, including PTSD.Endnote 43
Finally, non-Indigenous frontline workers serving Indigenous communities may also experience challenges. For example, many Indigenous communities employ or receive nursing services by non-Indigenous nurses. These nurses may find themselves ill-equipped to manage the layers of trauma with the scarcity of human and practical resources available to them which can affect their wellbeing and mental health.Endnote 44
Unique factors that impact PTSD in Indigenous Peoples
Historical and current trauma among First Nations, Inuit and Métis is significant and well documented by initiatives such as the Truth and Reconciliation Commission and the Inquiry into Missing and Murdered Indigenous Women and Girls.Endnote 45,Endnote 46 Past colonization policies have resulted in intergenerational, social and community trauma, which continue to impact the health and wellness of Indigenous Peoples and communities.Endnote 47
First Nations, Inuit and Métis have distinct histories, contexts, world views and knowledge systems that need to be considered to understand and treat PTSD within those populations, whether in an occupational setting or not.
Other populations
Many people are at increased risk for PTSD as a result of experiences outside of an occupational setting such as survivors of sexual or interpersonal violence, refugees, LGBTQ2 populations, Indigenous Peoples, people experiencing homelessness, as well as survivors of major accidents or disasters. Each of these populations face a unique set of circumstances, complexities, and challenges that impact the diagnosis, treatment, and management of PTSD. Appendix B provides a high-level overview of PTSD from experiences outside of occupational settings.
Organizational roles and responsibilities
To address PTSD in Canada, we require the knowledge, expertise, and involvement of organizations from multiple sectors and disciplines. These include federal, provincial/territorial, regional and local governments, the research and academic community, pan-Canadian health organizations, non-government organizations, employers, and community organizations.
In addition to these organizations, health care providers are central to the diagnosis, treatment, and management of PTSD. The experiences and expertise of people with lived experience – the individuals living with PTSD and their families and peers – inform our efforts and compel us to action.
This section outlines some of the current roles and responsibilities of governments, employers, and other stakeholders.
Government of Canada
The Government of Canada fosters connections, provides information, supports research and innovation, and undertakes activities to promote and protect the physical and mental health of Canadians. The Government of Canada is a leader, partner, funder, and convenor on issues of importance to Canadians, including PTSD.
The Government of Canada provides or funds some direct health care services (including mental health services) to groups under federal jurisdiction. These groups include serving members of the CAF, First Nations living on reserve and Inuit living in the North, and federal inmates.
The federal government also funds and administers supplementary and occupational health care benefits (including coverage for mental health services) for members of the Royal Canadian Mounted Police (RCMP), Veterans, First Nations and Inuit populations, as well as refugees, asylum claimants and other specific, vulnerable foreign nationals. Many people within these populations are at higher risk of developing PTSD.
The federal government is Canada's largest employer and has prioritized workplace mental health by adopting procedures and measures, as well as championing initiatives that promote positive mental health in the workplace.
Provincial and territorial governments
Provincial and territorial governments provide leadership, policy direction, and programs that support the health of their residents, and the delivery of services under their jurisdiction. This includes health care and other social services, including mental health supports, such as hospital services, crisis intervention, treatment, and follow-up. Provinces and Territories also have workers compensation boards, which have responsibilities related to health and labour issues.
All provinces and territories have mental health strategies, which focus on upstream approaches (i.e., promote positive mental health, resiliency, and wellness across the lifespan), mental health services, stigma reduction, and treatment. These strategies recognize the impacts of trauma (including intergenerational and historical trauma) on mental health and as a risk factor for substance-related harms and suicide.
Most provinces and territories have recognized the impact that certain occupations can have on an individual's mental health and have implemented corresponding presumptive legislation for workers' compensation claims. (See text box.) The intention is to allow for early intervention, which should help to mitigate aggravation or recurrence of mental health challenges such as PTSD.
Presumptive Legislation
Presumptive Legislation Presumptive legislation facilitates workers' compensation coverage by presuming, in the absence of evidence to the contrary, that the injury or illness is work related. Presumptive legislation may be limited to PTSD and a narrow group of occupations (e.g., police, firefighter, paramedic) and/or may be more broadly applicable to mental illnesses beyond PTSD and to a broader scope of occupations, or all occupations.
Employers
All employers including federal, provincial/territorial, and municipal governments, as well as non-governmental organizations and private sector companies have a responsibility to ensure the health and safety of their employees. Employers must think ahead and act proactively to minimize or protect against psychological injuries and promote psychological wellbeing. Wherever possible, these efforts should be based on peer-reviewed research and the best available practices as indicated by scientist-practitioners with appropriate mental health expertise and experience.
In occupations where there is a higher risk of employees developing PTSD, some employers have implemented specific mental health initiatives. The CAF developed the Road to Mental Readiness (R2MR) training program to promote early awareness of distress, encourage care-seeking, normalize mental health challenges, and provide evidence-based skills to manage the demands of service and daily life. The CAF recently adapted the most recent version of the R2MR program to create an edition appropriate for delivery to public safety personnel and this training is being made available across Canada through the collaborative efforts of Public Safety Canada, the CAF, and the Canadian Institute of Public Safety Research and Treatment (CIPSRT).
Many workplaces (including the federal government) have established employee assistance programs (EAP) to assist employees with personal problems and/or work-related issues that may impact their job performance as well as their physical/mental health, and emotional wellbeing. EAPs usually offer free and confidential assessments, short-term counselling, referrals, and follow-up services for employees and their families.
Stakeholder and community groups
Across Canada, multiple stakeholders and communities are mobilizing to address the challenges of PTSD and related mental health conditions. These stakeholder organizations (often led by individuals with lived experience) operate at both the national and regional level. They can provide services and peer support, as well as leadership and expertise to strengthen research, innovation, knowledge exchange and awareness, and to develop tools and resources for Canadians, employers, and health care providers. Many stakeholder organizations work closely and collaboratively with governments to inform policy, and advocate on behalf of people experiencing PTSD.
Informing the Framework
The implementation of the Federal Framework on Post-Traumatic Stress Disorder Act and the resulting Federal Framework on PTSD was coordinated by PHAC in collaboration with multiple partners and stakeholders.
PHAC engaged with more than fifteen federal government departments to foster connections and share initiatives related to PTSD and other occupation-related mental health conditions. PHAC also consulted with stakeholder groups who fell within the scope of the Act and other experts in the field of PTSD and mental health.
In October 2018, an early stakeholder consultation was held on the margins of the Canadian Institute for Military and Veteran Health Research (CIMVHR) Forum. This consultation was attended by members of the CIPSRT Public Safety Steering Committee, members of the CIMVHR Technical Advisory Committee, and key federal departments.
As specified in the Act, in April 2019, a National Conference on PTSD took place in Ottawa, Ontario. This conference was the main engagement mechanism to obtain a variety of perspectives for the development of the Framework. The conference brought together 200 diverse participants and encouraged collaboration and knowledge sharing across sectors and disciplines. Participants included: representatives of occupational groups at higher risk for PTSD, people living with PTSD and their support networks, researchers/academics, health care providers, representatives of populations at higher risk for PTSD, Indigenous groups, federal and provincial government representatives, workers' compensation board representatives, and Pan-Canadian health organizations.
To ensure the Indigenous context and considerations were well reflected in the Framework, PHAC continued to engage with Indigenous organizations through a First Nations Reference Group on PTSD, the Métis Nation Health Committee, and the National Inuit Committee on Health.
Key themes from the National Conference on PTSD
- Health care benefits and access to care and resources vary across the country and across different occupational groups – Some occupational groups have access to a variety of educational tools and services, but others struggle to receive basic supports. These disparities were particularly salient for individuals in rural and remote communities, as well as those in volunteer positions, and in certain medical professions, such as nurses. For example: a nurse living in a remote location may experience a very different path to treatment than a nurse located in an urban centre; volunteer firefighters may not be eligible for the same health benefits as their paid counterparts; and, services and benefits offered to municipal police services may not be analogous to those offered federally to the RCMP.
- There is a need to achieve parity between physical and mental health – There is general knowledge of PTSD, but stigma remains an ongoing barrier to care and treatment. Participants shared that some individuals fear that seeking help will hinder their careers. Others shared that while workplace policies may be in place to support individuals with PTSD, longstanding occupational cultures and organizational leadership continue to reinforce the perception that mental health conditions such as PTSD are a sign of weakness. Participants also noted the importance of continued research, including in the field of identifying biological markers for PTSD.
- A number of resources exist, but there is a need for comprehensive ways to share evidence-based best practices – Participants reported that the amount of information on PTSD can be overwhelming and there may be opportunities to use or build on successful initiatives; however, knowing what is truly of value to help persons living with PTSD in their recovery can be extremely difficult. Participants expressed the need for standardized evidence-based resources that can be adapted (e.g., based on the community, culture, sex or gender). Indigenous participants expressed the need for studies that involve individuals of Indigenous ancestry and that use culturally appropriate methodologies. Participants also noted the need for consistent language and terminology around PTSD.
- PTSD has impacts beyond the individual. There is a need to consider how families, children and the diagnosed individual's support networks are affected – On several occasions participants shared that spouses, children, family members and other support networks of those who experience PTSD are significantly affected by a loved one's PTSD. Individuals in the immediate social circle of a person with PTSD can be important assets in recovery; however, the same individuals will also require effective supports to best assist the person living with PTSD, as well as to maintain their own mental health and wellbeing.
- There is a need for quality and timely data, as well as qualitative input and insight from individuals with lived experience to inform policies and programs – Participants and experts agreed that the current available data on PTSD has significant gaps and is, at times, outdated. They commented on the power of sharing personal stories in helping those who are struggling, and in informing policies and programs. Participants also emphasized the importance of sharing personal stories in a safe and sensitive way.
- There is a need to improve organizational capacity to respond to and support employees at higher risk of developing PTSD– More proactive and early intervention initiatives are required to help employees recognize PTSD symptoms, seek treatment when needed, and strengthen their support networks and resilience (e.g., including peer support, return-to-work strategies, and training that promotes healthy coping). Finally, participants emphasized the importance of trauma-informed approaches as a means of reducing stigma, supporting employees, and shifting organizational culture so that all staff are aware and able to integrate knowledge of trauma into practice.
Part II: The Federal Framework on PTSD
Federal Framework on PTSD – at a glance
Scope
The focus of the Framework is on occupation-related PTSD. The Framework also acknowledges people affected by non-occupation-related PTSD and broad applicability will be considered in the implementation of federal actions.
Purpose
Strengthen knowledge creation, knowledge exchange and collaboration across the federal government, and with partners and stakeholders, to inform practical, evidence-based public health actions, programs and policies, to reduce stigma and improve recognition of the symptoms and impacts of PTSD.
Vision
A Canada where people living with PTSD, those close to them, and those at risk of developing PTSD, are recognized and supported along their path toward healing, resilience, and thriving.
Guiding principles
- Complement current initiatives and leverage partnerships.
- Advance compassionate, non-judgemental and strengths-based approaches.
- Base initiatives on evidence of what works or shows promise of working.
- Understand and respond to equity, diversity and inclusion.
- Apply a public health approach.
Priority areas
Data and tracking
- Explore strategies to support national surveillance activities and examine the feasibility of using health administrative data and enhanced data linkages to capture and report on PTSD.
- Continue supporting data collection on PTSD.
Guidelines and best practices
- Work with partners and engage experts to compile existing guidance on PTSD and identify where gaps may exist.
- Continue to support research to bridge PTSD-related information gaps, inform effective guidance for health care providers, and advance evidence-based decision making.
Educational materials
- Work with partners and engage health care providers to identify current PTSD educational materials, understand the educational gaps, and seek advice on best practices for the dissemination, adaptation, and uptake of educational materials.
Strengthened collaboration
- Work with partners and stakeholders to identify the best mechanism(s) to increase collaboration among key departments, partners and stakeholders, as well as for ongoing sharing of information, including uptake of common and culturally appropriate terminology, definitions, and safe language about PTSD and trauma.
Scope and purpose of the Framework
The Federal Framework on PTSD establishes the Government of Canada's vision, guiding principles, and actions to address occupation-related PTSD, as they relate to the three legislated areas of priority.
The purpose of the Framework is to strengthen knowledge creation, knowledge exchange and collaboration across the federal government, and with partners and stakeholders, to inform practical, evidence-based public health actions, programs and policies, to reduce stigma and improve recognition of the symptoms and impacts of PTSD.
Appendix C lists PTSD initiatives currently underway in Canada, including federal initiatives to support high-risk populations. The following graphic illustrates how the various ongoing initiatives can connect to the Framework to help those impacted by PTSD.
Figure 1. Linking other existing initiatives to the Federal Framework on PSTD
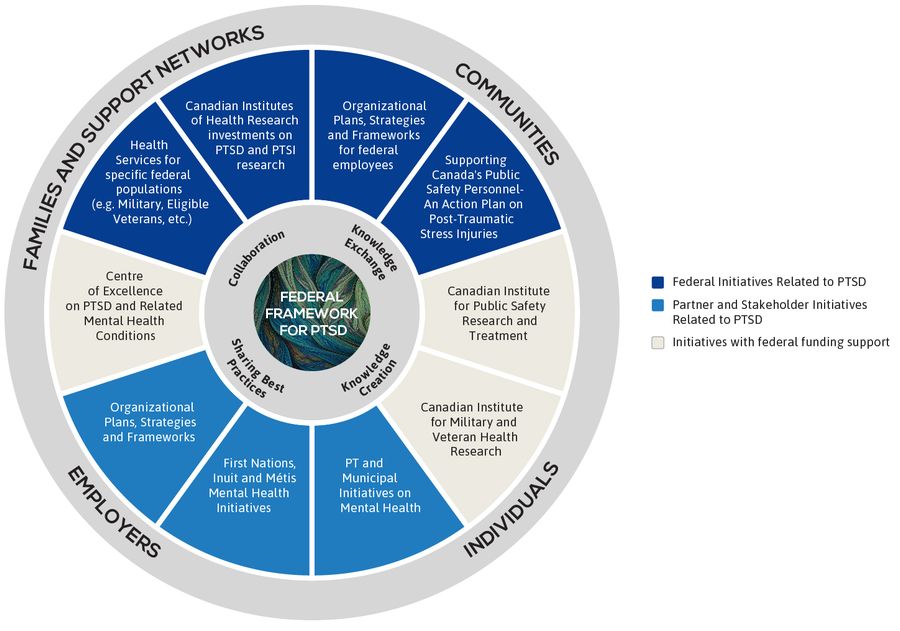
Figure 1 - Text Description
The image is a circle with inner and outer rings, showing the Federal Framework on PTSD at the centre, surrounded following four key words describing its purpose: collaboration, knowledge creation, knowledge exchange, and sharing best practices.
The middle ring shows how various, ongoing initiatives can connect to the Federal Framework to help those impacted by PTSD. There are three types of initiatives described with examples provided under each type of initiative.
The first set shows federal initiatives related to PTSD (appearing in dark blue) including:
- Health services for specific populations (e.g. military, eligible Veterans, etc.);
- Canadian Institutes of Health Research investments in PTSD and PTSI research;
- Organizational plans, strategies and frameworks for federal employees; and
- An Action Plan on Post-Traumatic Stress Injuries in support of Canada's Public Safety personnel.
The next set shows initiatives that have received federal funding (appearing in beige) including:
- The Centre of Excellence on PTSD and Related Mental Health Conditions;
- The Canadian Institute for Public Safety Research and Treatment; and
- The Canadian Institute for Military and Veteran Health Research.
Finally, the last set shows partner and stakeholder initiatives related to PTSD (appearing in light blue) including:
- Organizational plans, strategies and frameworks;
- First Nations, Inuit and Métis mental health initiatives; and
- Provincial, territorial and municipal initiatives on mental health.
The outermost ring shows the types of groups who are impacted by PTSD and could benefit from these initiatives including: families and support networks, communities, employers, and individuals.
Vision
A Canada where people living with PTSD, those close to them, and those at risk of developing PTSD, are recognized and supported along their path toward healing, resilience, and thriving.
Guiding principles
The following principles are intended to guide the actions outlined in the Framework, as well as other efforts by the Government of Canada to address PTSD.
- Complement current initiatives and leverage partnerships. Improve coordination, collaboration, and linkages across government and among non-governmental organizations, Indigenous organizations and communities, the private sector, provinces and territories, research organizations, communities, practitioners, and those with lived experience.
- Advance compassionate, non-judgemental, strengths-based and trauma-informed approaches. Engage with people who have lived experience of PTSD. Be aware of how stigma, discrimination and racism increase risks and create barriers to treatment. Apply trauma-informed approaches: understand the impact of trauma; create emotionally, culturally, and physically safe environments; foster opportunities for choice, control and collaboration; provide a strengths-based approach to support coping and resilience.
- Base initiatives on evidence of what works or shows promise of working. Recognize the importance of research in generating evidence and knowledge about PTSD. Ensure high-quality information is available, and apply research results to new and existing interventions, treatment, policies, programs, and training across Canada.
- Understand and respond to equity, diversity and inclusion. Ensure that approaches to education, treatment, and reintegration into society and the workplace are adaptable and individualized to occupational settings and realities. Consider culture, including Indigenous cultures, community, sex, gender, and other identity factors, such as race and ethnicity. Apply culturally safe approaches that ensure people can draw strength from their identity, culture, spirituality, and community in an environment that is free from racism and discrimination.
- Apply a public health approach. PTSD is a public health issue. Focus on the population or community and emphasize protective factors such as mental wellness, social cohesion, culturally appropriate and safe programs and services (particularly at the community level) to build safe and healthy environments, resilience, and coping skills.
Priority areas
The Federal Framework on PTSD Act outlines three priority areas to be addressed in the Framework. These areas formed the basis of consultations with partners and stakeholders and were discussed in depth during the National Conference on PTSD.
Based on consultations, an additional priority area was added to focus on strengthening collaboration and linkages among partners and stakeholders.
This section provides an overview of these priority areas and their drivers, considerations, and the federal actions needed to advance them.
Priority Area 1: Improved tracking of the rate of PTSD and its associated economic and social costs
Data on PTSD in Canada is limited. To better inform policies and programs and to improve our understanding of PTSD and its risk factors, there is a need for high-quality, ongoing, and timely data collection, surveillance, and research, as well as insights from individuals with lived experience. Nationally representative data can identify how many Canadians are living with PTSD and the associated risk factors. Routine collection of data can also measure trends over time, and inform policy and program interventions. A variety of PTSD data collection tools are available but the approaches differ and this process is further hampered because the diagnosis of PTSD is complex, and health care providers may not always recognize or properly assess symptoms. In addition, many individuals do not realize they may have PTSD or seek care.
The Act calls for improved tracking of the incidence (the number of new cases of PTSD over a period of time); however, stakeholders, researchers, and policy-makers have recommended that first and foremost, we need an understanding of the prevalence of PTSD (the number of new and existing cases).
Research and data collection on certain sub-populations is taking place, but further effort should focus on Canadian population-level data. Population-level data establishes a prevalence estimate for the general population that serves as a point of comparison for estimates in sub-populations, including those at increased risk of PTSD.
The Act also calls for improved tracking of the associated economic and social costs of PTSD so we can fully understand impacts on individuals living with PTSD, their families, and their communities. These costs can include those related to lost wages, treatment, lost productivity, substance-related harms and/or mental health conditions, homelessness, etc. In order to generate accurate estimates of economic and social costs, we first need a clearer picture of PTSD prevalence in Canada.
Advancements in data collection, insights into existing data-related initiatives, and a deeper understanding of the social and economic costs of PTSD will provide a more complete picture of PTSD in Canada and therein better inform the development of policies, tools, and interventions.
Data on PTSD in Canada is limited and requires updating.
Recognizing the importance of data in understanding PTSD and its impacts, and in informing policies and programs, the Government of Canada will:
- Explore strategies to support national surveillance activities to measure the rate of PTSD and its associated costs and examine the feasibility of using health administrative data and enhanced data linkages to capture and report on PTSD. This work will be led by PHAC in collaboration with other partners and stakeholders.
- Continue supporting data collection to better understand PTSD and related mental health conditions, through ongoing investments and initiatives.
Priority Area 2: Promotion of guidelines and sharing of best practices related to the diagnosis, treatment and management of PTSD
Diagnosing, treating, and managing PTSD is complex. What leads to PTSD in one person may be completely different for another person. People who experience PTSD symptoms may experience other concurrent mental health conditions (e.g., anxiety disorders or substance use disorders), which can hamper recognition, diagnosis, and treatment. Other factors such as individual differences, personal preferences, health provider expertise, resource availability, and the ability to access resources and services may also affect recognition, diagnosis, and treatment.
There is no one-size-fits-all approach to treat and manage PTSD. Treatment plans need to be individualized based on a person's clinical presentation and personal experience, and should recognize cultural, occupational, sexual and/or gender-based differences. Relevant social determinants of health, trauma-informed care, and reintegration practices must also be at the centre of any treatment plan to ensure physical, cultural and emotional safety.
A number of clinical practice guidelines provide practical, evidence-based recommendations for the diagnosis, treatment, and management of PTSD. (See text box.) Guidelines require regular updating as research evolves, which require time and specific expertise. The development, review, and updating of clinical practice guidelines is the responsibility of guideline groups, health authorities or health care providers, along with their associations, accreditors, and regulators.
Examples of Clinical Practice Guidelines on PTSD
- International Society for Traumatic Stress Studies (ISTSS): PTSD Prevention and Treatment Guidelines: Methodology and Recommendations (March, 2019; US)
- National Institute for Health and Care Excellence (NICE): Post-traumatic stress disorder – NICE guideline (December, 2018; UK)
- US Department of Veterans Affairs and Department of Defense (VA/DoD): Clinical Practice Guideline for the Management of PTSD and Acute Stress Disorder (2017; US)
- American Psychological Association (APA): Clinical Practice Guideline for the Treatment of PTSD (February, 2017; US)
- Anxiety Disorders Association of Canada: Canadian Clinical Practice Guidelines for the Management of Anxiety, Posttraumatic Stress and Obsessive-Compulsive Disorders (2014; Canada)"
Guidance and best practices also exist to guide service delivery and models of care for specific populations, but gaps remain, and awareness of these tools is sometimes lacking.
There are also emerging and innovative interventions, such as peer support programs, meditation, internet-based therapies, couples-based trauma treatment, and land-based activities, which provide options that may help in the healing process based on individual needs and pace of recovery. Current dialogue on emerging treatments also includes the possible use of cannabis to manage symptoms of PTSD. For Indigenous Peoples, traditional ceremonial practices enacted in cultural settings can promote healing and wellness. Emerging and innovative interventions may not be included in clinical practice guidelines and are currently considered as adjuncts to first-line evidence-based treatments. Additional and systematic research into emerging and innovative interventions is required to build the evidence base and to ensure their safety, efficacy, and effectiveness.
With more research, we can better determine which policies, programs, and treatments will make the most difference for the mental wellness and resilience of a greater number of Canadians impacted by PTSD.
Knowledge transfer and the sharing of best practices around innovative interventions should be undertaken in a timely way to benefit those living with PTSD and their support networks.
Evidence-based guidelines and best practices are essential to ensure the best care and support of those affected by PTSD.
Recognizing that many resources already exist, but awareness of these tools is sometimes lacking, and recognizing that research is essential in the advancement of guidance development, the Government of Canada will:
- Through PHAC, work with partners and engage experts to compile existing guidance on PTSD, and identify where guidance gaps may exist.
- Support research, including applied research, through existing investments, to bridge PTSD-related information gaps, inform effective guidance for health care providers and advance evidence-based decision making for policy and program makers across all levels of government and key partners and stakeholder organizations.
Priority Area 3: Creation and distribution of educational materials related to PTSD to increase national awareness and enhance diagnosis, treatment and management
Canadian health care providers are often the first line of contact for people experiencing symptoms of PTSD. Health care providers play an important and influential role in helping those affected find appropriate treatments and supports. To be effective, health care providers need to be well informed and knowledgeable about PTSD and how it impacts different populations. Educational tools and resources exist, but there is limited understanding of the quality and availability of tools and resources for health care providers.
The Act specifically identified the need for educational materials for "public health care providers"; however, partners and stakeholders also stressed the need for tools and resources for individuals experiencing symptoms of PTSD, their support networks, and for employers and workplaces.
Individuals experiencing symptoms of PTSD need tools and resources that are accessible, clear, concise, and that encourage them to seek help. There is no single mechanism to share these materials–instead, a breadth of educational tools and resources are available across Canada in a variety of formats. For example, general information on the signs, symptoms, causes, risk factors, diagnosis, and treatment of PTSD can be found on non-governmental organization (NGO) websites, including the Canadian Mental Health Association, the Centre for Addictions and Mental Health, and the Canadian Psychological Association.
The PTSD Coach Canada mobile app provided by VAC is available to people who may be seeking additional information and resources on PTSD. It features information and self-help tools based on research. The app, which is available to all Canadians, can be used as an education and symptom management tool, prior to, or as part of in-person care provided by a health care provider.
Family members and support networks of people experiencing PTSD, especially spouses, are often the first to recognize early warning signs and encourage their loved one to seek support. Families and support networks need specialized tools and resources that can help them recognize symptoms and cope with the impact of PTSD on their own lives.
This is especially true for children of people living with PTSD, who may be affected in multiple ways and may not understand what is happening to their parent or family member. Symptoms of PTSD, and the stress of coping with them, can impact a parent's ability to meet their child(ren)'s basic physical, psychological, emotional and spiritual needs, and their need for social and intellectual development. Educational materials for families and support networks need to emphasize coping strategies and point to available resources for support.
VAC publications on PTSD and the Family and the "Post-Traumatic Stress Disorder (PTSD) and the Family for Parents with Young Children" PDF publication are good examples.
Employers and workplaces have a crucial role in raising awareness about PTSD, preventing psychological injury, promoting psychological wellbeing and providing support to employees with PTSD. Workplace educational tools exist, such as the Road to Mental Readiness and The Working Mind programs. This content has already been adapted for some workplaces, but given diverse cultures and contexts, may need to be further adapted for applicability to specific audiences.
Trauma-informed policies in the workplace also promote resilience, encourage employees to seek early intervention, and reduce stigma toward mental health issues in the workplace.
Providing high quality, compassionate, action-oriented information on PTSD can empower people with PTSD, their family and support networks, and employers/workplaces to recognize the symptoms and impacts of PTSD, and encourage them to seek support and treatment.
Recognizing the importance of education in raising awareness, reducing stigma, and enhancing PTSD diagnosis, treatment, and management, the Government of Canada will:
- Through PHAC, work with partners and engage with health care providers to identify current PTSD educational materials, understand information and educational gaps, and seek advice on best practices for their dissemination, adaptation, and uptake.
Priority Area 4: Strengthened collaboration and linkages among partners and stakeholders
A number of PTSD-related initiatives are currently underway in Canada, including federal initiatives to support high-risk populations, such as Supporting Canada's Public Safety Personnel: An Action Plan on Post-Traumatic Stress Injuries, and the recently created Centre of Excellence on PTSD and Related Mental Health Conditions, funded by VAC.
A concerted and coordinated effort is needed to ensure awareness of new and existing PTSD initiatives and to engage partners and stakeholders, including people with lived experience. Working collectively allows for meaningful linkages and informed action across the Government of Canada, as well as with provinces and territories, Indigenous governments and organizations and communities, non-governmental organizations, researchers, practitioners, occupational communities and individuals. Connecting our efforts helps prevent duplication and ensures that we build on new approaches or resources as they are developed.
Strengthening connections and working collaboratively also involves an exploration of terminology. Language is important, not only in establishing a common understanding, but also in reducing stigma. There are many terms that are used interchangeably to capture the range of symptoms and health concerns associated with exposure to trauma and a common language can help build consistency among stakeholders and partners.
The Canadian Institute for Public Safety Research and Treatment (CIPSRT), in collaboration with a number of experts, has developed a Glossary outlining definitions related to PTSD and trauma. A version of the Glossary was disseminated at the National Conference on PTSD to ensure a common understanding among participants as they provided their insights and perspectives. Recognizing that language changes over time, the Glossary is intended to be a living document that will be updated regularly to reflect contemporary consensus on language. The most current version of the Glossary is included in Appendix D.
Collaboration is essential to minimize duplication and maximize the impact of our efforts to address PTSD.
In recognition of the complexity of PTSD, the diversity of those affected, the many partners and stakeholders involved in managing PTSD and the wide range of initiatives underway, the Government of Canada will:
- Work via PHAC with partners and stakeholders to identify the best mechanism(s) for increased collaboration among key federal departments, partners, and stakeholders, as well as for ongoing sharing of information, including uptake of common and culturally appropriate terminology, definitions, and safe language related to PTSD and trauma.
Part III: Moving forward
PTSD Secretariat
The PTSD Secretariat was established within PHAC to lead the implementation of the Federal Framework on PTSD Act. Since that time, the Secretariat has worked with partners and stakeholders together to inform the development of the Framework in a variety of ways, including the National Conference on PTSD in April 2019.
Given the numerous players, initiatives, and far-reaching impacts of PTSD in Canada, as well as the need for coordination of actions outlined in this Framework, the PTSD Secretariat will continue to exist at PHAC. The PTSD Secretariat will provide leadership and bring partners and stakeholders together to continue to foster connections, as well as to identify existing and possible collaborations to further support the progressing and evolving efforts to address PTSD.
The PTSD Secretariat will work with partners and stakeholders to leverage existing mechanisms, resources, and efforts to avoid duplication.
Reporting to Parliament
As mandated by the Federal Framework on Post-Traumatic Stress Disorder Act, PHAC will complete a review of the effectiveness of the Framework five years after the publication of the Framework. This review, which must be laid before each house of Parliament, will include a progress update on the priority areas and actions outlined in the Framework, and highlight any new initiatives and their results.
Conclusion
PTSD has a long history of being under-recognized, misunderstood and misdiagnosed. PTSD affects a significant number of Canadians; nevertheless, getting on a path to recovery can be extremely complex for these reasons. People living with PTSD are certainly impacted by the disorder, but so are their loved ones, colleagues, and support networks, all of whom also need to be supported as part of managing the disorder.
Achieving the vision set out in the Framework will require collaboration from multiple partners and stakeholders, including people with lived experience, their families and support networks, employers, researchers, health care providers, community organizations, and all levels of government. We encourage all partners and stakeholders to build on the vision and guiding principles of the Framework to advance initiatives in the area of PTSD.
The Framework is intended to encourage continuous open dialogue. The actions identified herein will undoubtedly continue to evolve as we learn more about PTSD through ongoing efforts across the Government of Canada and by the many partners and stakeholders.
Part IV: Appendices
Appendix A – Federal Framework on PTSD Act and Observations from the Senate Committee
Federal Framework on Post-Traumatic Stress Disorder Act
S.C. 2018, c. 13
Assented to 2018-06-21
An Act respecting a federal framework on post-traumatic stress disorder
Preamble
Whereas post-traumatic stress disorder (PTSD) is a condition that is characterized by persistent emotional distress occurring as a result of physical injury or severe psychological shock and typically involves disturbance of sleep and constant vivid recall of the traumatic experience, with dulled responses to others and to the outside world;
Whereas there is a clear need for persons who have served as first responders, firefighters, military personnel, corrections officers and members of the RCMP to receive direct and timely access to PTSD support;
Whereas, while not-for-profit organizations and governmental resources to address mental health issues, including PTSD, exist at the federal and provincial levels, there is no coordinated national strategy that would expand the scope of support to ensure long-term solutions;
And whereas many Canadians, in particular persons who have served as first responders, firefighters, military personnel, corrections officers and members of the RCMP, suffer from PTSD and would greatly benefit from the development and implementation of a federal framework on PTSD that provides for best practices, research, education, awareness and treatment;
Now, therefore, Her Majesty, by and with the advice and consent of the Senate and House of Commons of Canada, enacts as follows:
Short Title
1 This Act may be cited as the Federal Framework on Post-Traumatic Stress Disorder Act.
Interpretation
Definitions
2 The following definitions apply in this Act.
Agency means the Public Health Agency of Canada. (Agence)
federal framework means a framework to address the challenges of recognizing the symptoms and providing timely diagnosis and treatment of post-traumatic stress disorder. (cadre fédéral)
Minister means the Minister of Health. (ministre)
Federal Framework on Post-Traumatic Stress Disorder
Conference
3 The Minister must, no later than 12 months after the day on which this Act comes into force, convene a conference with the Minister of National Defence, the Minister of Veterans Affairs, the Minister of Public Safety and Emergency Preparedness, provincial and territorial government representatives responsible for health and stakeholders, including representatives of the medical community and patients' groups, for the purpose of developing a comprehensive federal framework in relation to
- improved tracking of the incidence rate and associated economic and social costs of post-traumatic stress disorder;
- the establishment of guidelines regarding
- the diagnosis, treatment and management of post-traumatic stress disorder, and
- the sharing throughout Canada of best practices related to the treatment and management of post-traumatic stress disorder; and
- the creation and distribution of standardized educational materials related to post-traumatic stress disorder, for use by Canadian public health care providers, that are designed to increase national awareness about the disorder and enhance its diagnosis, treatment and management.
Preparation and tabling of report
- 4 (1) The Minister must prepare a report setting out the federal framework and cause a copy of the report to be laid before each House of Parliament within 18 months after the day on which this Act comes into force.
Publication of report
(2) The Minister must publish the report on the Agency's website within 30 days after the day on which it is laid before a House of Parliament.
Review and Report
Review
5 The Agency must
- complete a review of the effectiveness of the federal framework no later than five years after the day on which the report referred to in section 4 is published; and
- cause a report on its findings to be laid before each House of Parliament within the next 10 sitting days after the review is completed.
Monday, June 11, 2018
The Standing Senate Committee on National Security and Defence has the honour to present its
Eighteenth Report
Your committee, to which was referred Bill C-211, An Act respecting a federal framework on post-traumatic stress disorder, has, in obedience to the order of reference of Thursday, May 3, 2018, examined the said bill and now reports the same without amendment but with certain observations, which are appended to this report.
Respectfully submitted,
GWEN BONIFACE
Chair
Observations
to the Eighteenth Report Report of the Standing Senate Committee on National Security and Defence (Bill C-211)
- The bill's sponsor, Todd Doherty, MP (Cariboo—Prince George), told your committee that the exclusion of various occupations from the preamble to the bill was an accidental oversight and that he had intended to be as inclusive as possible. Your committee shares Mr. Doherty's view that the conference and federal framework should be as inclusive as possible.
- Your committee would like to ensure that health care providers and individuals in other high-stress occupations be asked to participate in developing the federal framework on post-traumatic stress disorder that is proposed in the bill. Your committee wishes to emphasize that the words "in particular" in the fourth paragraph of the bill's preamble indicate that the conference and the federal framework on post-traumatic stress disorder should include not only first responders, firefighters, military personnel, corrections officers and members of the Royal Canadian Mounted Police, but also a wide range of occupations whose members are affected by post-traumatic stress and related problems, including nurses, psychologists and other health care providers and first responders.
- Your committee shares the concern expressed by officials from the Canadian Psychological Association regarding clause 3(b)(i) that addresses the development of guidelines. This clause states that the conference aiming to establish a federal framework on post-traumatic stress disorder focus, among other topics, on "the establishment of guidelines regarding the diagnosis, treatment and management of post-traumatic stress disorder." Representatives of the Canadian Psychological Association stated that developing guidelines in this regard is the responsibility of health professionals and their associations, accreditors and regulators, not the government. Your committee therefore suggests that the conference on the federal framework on post-traumatic stress disorder promote the establishment and dissemination of guidelines, rather than developing them as such, as recommended by the Canadian Psychological Association.
- Your committee would like to ensure that the full range of mental health conditions obtained from high-stress occupations are considered in the development of the federal framework on post-traumatic stress disorder that is proposed in the bill. Your committee therefore advises that the conference on the federal framework on post-traumatic stress disorder consider the use of the term "operational stress injury." This term includes post-traumatic stress disorder, but also includes conditions like occupation-linked depression, anxiety disorders, adjustment disorder and the full range of substance disorders that people may face as a result of being in a high-stress work environment.
- Your committee is concerned that the current wording of Bill C-211 could imply that the national framework on post-traumatic stress disorder should only focus on cases that manifest as a direct consequence of the demands of their occupation. However, many cases of work-related cases of post-traumatic stress disorder are directly linked to cases of sexual misconduct and harassment. Your committee therefore suggests that the conference on the federal framework on post-traumatic stress disorder include these cases in its development of the national framework.
Appendix B – Other populations affected by PTSD
Survivors of physical, sexual and/or psychological violence
Survivors of physical, sexual and/or psychological violence may experience PTSD. Victimization rates are higher for certain groups such as women, Indigenous people, persons experiencing homelessness, and those who are LGBTQ2. Children and youth are especially vulnerable to violence and have a higher risk of mental health conditions in adulthood. For example, a study of sexually abused children who were followed over 40 years showed that women who were sexually abused during childhood were over seven times more likely to be diagnosed with PTSD.Endnote 48
Survivors of disasters
Disasters can occur at any time, often with limited or no warning at all. Disasters can be natural, such as wildfires, earthquakes, tornadoes, floods; or human made, such as acts of terrorism, motor vehicle crashes, and house fires. Disaster survivors may experience a tremendous sense of loss especially if they have been injured or have lost loved ones, shelter, and/or employment. Individuals who experience disasters may be at increased risk of developing PTSD.Endnote 49 In the first year post-disaster, the prevalence of PTSD among disaster survivors ranges between 30% and 40%.Endnote 50
Indigenous PopulationsFootnote d
There is very little research available on the prevalence of PTSD in First Nations, Inuit and Métis communities.
To understand trauma in Indigenous communities we must consider the effects of colonization, including the residential school experience, and the resulting intergenerational trauma experienced by multiple generations across Canada. For example, a study conducted in 2003 investigating the mental health status of 127 former residential school students in British Columbia found that 64% met the diagnostic criteria for PTSD.Endnote 51
Historical, intergenerational, and ongoing forms of trauma increase risk factors that can impact the mental health of Indigenous Peoples, and increase risks of developing PTSD.Endnote 45,Endnote 46 For example, compared to non-Indigenous Canadians, First Nations, Inuit and Métis Peoples experience significantly higher rates of social health challenges such as lower educational attainment and employment levels and living in poverty. There is also more intimate partner violence reported by Indigenous Peoples compared to non-Indigenous people and the incidence of childhood sexual and physical abuses is much higher than other cultural groups. Indigenous Peoples are also more likely to experience stressful experiences in adulthood compared to the population at large, including violence, homicide, assault, and witnessing traumatic events.Endnote 51
Additionally, Indigenous Peoples often encounter systemic racism and discrimination in many different systems where they access services (e.g., health care, education system). The current systems are created from a non-Indigenous worldview and are often experienced as alienating and unwelcoming. Feelings of mistrust in service providers and systems of care are commonly reported and are by-products of culturally unsafe care. Culturally unsafe systems of care may trigger historical memories, affect health-seeking behaviours, and prolong intergenerational trauma at an individual and collective level.Endnote 52
LGBTQ2
LGBTQ2 youth and adults experience higher rates of victimization, trauma, and PTSD compared to heterosexual/cisgender youth and adults.Endnote 53 Additionally, gender nonconformity (gender expression that does not conform with the traits or conventional norms typically associated with their sex assigned at birth) increases the risk of abuse and PTSD symptoms due to stigma and discrimination.Endnote 54 Studies have found evidence of an association between discrimination linked with one's gender identity and/or expression and symptoms of PTSD, even when adjusting for other known sources of trauma.Endnote 55,Endnote 56,Endnote 57,Endnote 58
Refugees and other newcomers
The rates of mental health conditions in adult newcomers are significantly lower compared to other Canadians; however, rates may increase over time due to stress and uncertainty during the settlement process.Endnote 59
Some refugees arrive in Canada bearing psychological trauma from their experiences witnessing and/or surviving acute violence and/or war.Endnote 59 Exposure to violence and trauma can also increase the risk of mental disorders, including PTSD, which may manifest over a period of time following their arrival. A meta-analysis of 20 studies that included 6,743 adult refugees who resettled in developed countries, the current prevalence rate of PTSD in refugees was 9%.Endnote 60 PTSD is also thought to be the most common mental health condition among children and youth exposed to war and violence.Endnote 61,Endnote 62,Endnote 63 Refugee children and youth have been shown to have ten times higher rates of PTSD than non-refugee children in the general population.Endnote 64
The mental health of refugee children has also been associated with the severity of PTSD experienced by their caregivers, which adds complexity to treatment and recovery.Endnote 65 Newcomers also face challenges accessing mental health supports and services due to lack of awareness, language, and cultural barriers.
People experiencing homelessness
The causal pathways to PTSD in people experiencing homelessness are especially complex. PTSD can be a precursor to or the result of homelessness. This interactive relationship may be due to the higher likelihood of exposure to trauma while experiencing homelessness, such as robbery or assault. Losing a stable shelter, experiencing food insecurity and living in ongoing stressful conditions can also be perceived as traumatic. People experiencing homelessness are also at an elevated risk of substance-related harms. In a British Columbia study of 489 participants who were living in a shelter or on the street, 100 individuals (20.5%) met the criteria for PTSD and, 92% of whom had a concurrent substance use disorder.Endnote 66
Appendix C – Current PTSD initiatives in Canada
There is a wide range of initiatives offered by government, non-government organizations, and non-profit organizations that provide services and support to people affected by trauma and PTSD. Some are longstanding and others more recent. The variety and diversity of these initiatives is an indication of the collective commitment and understanding in Canada that resources and efforts must be dedicated at many levels to support all those affected by PTSD.
The wide range of current initiatives is an indication of the value of comprehensive approaches adaptable to various communities and cultures, including First Nations, Inuit and Métis cultures, as well as the need for initiatives and interventions that are offered across a continuum from raising awareness and building resiliency, to effective and timely access to evidence-based treatments.
| Interventions designed to promote positive mental health, wellness, and resilience | Interventions designed to provide support following a traumatic event | Clinical, evidence-based interventions to treat PTSD |
|---|---|---|
| When: Ongoing | When: May be immediate, or in the weeks and months, following exposure to a traumatic event | When: As soon as possible following diagnosis |
| Who: All individuals | Who: All individuals exposed to a traumatic event, as well as the people who support them, who may or may not be experiencing symptoms of stress | Who: Specific individuals who have received a PTSD diagnosis |
Activity type
|
Activity type
|
Activity type
|
| Supported by research, frameworks, policies, legislation, etc. | ||
The following overview of PTSD initiatives provided by government and key stakeholders and partner organizations is not exhaustive, but is intended to showcase the breadth and depth of existing initiatives.
Federal government
The Government of Canada works to improve the mental health and wellbeing of all Canadians. The federal government is also the country's single largest employer and offers multiple initiatives to support the mental health of its workforce, which is spread across the country and around the world and includes a range of occupations.
There are federal initiatives that specifically support those living with PTSD, people at risk of developing PTSD and their family and support networks. They include research, data gathering, knowledge development, awareness, proactive protection and resiliency training, sharing best practices, support for employees, and in some case, the direct delivery of care for populations under federal jurisdiction.
Canadian Armed Forces Members and Veterans
The mental health programs for Canadian Armed Forces (CAF) members, Veterans, their loved ones and communities, include a range of services to build positive mental health, as well as help for those affected by operational stress injuries (OSI), including, but not limited to, PTSD. For example, in the CAF-VAC Joint Suicide Prevention Strategy there are over 160 actionsFootnote e underway or under development in the areas of education and health promotion, national peer support, clinical care and psychosocial services. Research programs are also in place to better understand the mental health burden in CAF members, Veterans, and their loved ones, and what type of programming best addresses their well-being.
Programs and services provided by the CAF include:
- Specialized mental health services for ill and injured members of the CAF at 31 medical clinics across Canada, including seven Operational Trauma and Stress Support Centres (OTSSCs).
- CAF and VAC jointly sponsor the Operational Stress Injury Social Support (OSISS) service, a national peer support network serving CAF members and Veterans and their families affected by an OSI.
- The Member Assistance Program (MAP) for CAF members offers confidential, short-term counselling for any issue. (In partnership with Health Canada).
- The Road to Mental Readiness (R2MR) training, which is intended to increase early awareness of distress, encourage care-seeking, normalize mental health challenges, and provide evidence-based skills to manage the demands of service and daily life.
- Operation HONOUR is the CAF's mission to eliminate sexual misconduct in the Canadian military by supporting people affected by sexual misconduct, developing procedures, programs and policies for affected individuals and the chain of command and preventing sexual misconduct from occurring through increased understanding of the issue, training and education programs.
Programs and services sponsored by VAC:
- A national network of Operational Stress Injury Clinics, specialized in providing mental health care to CAF Veterans, RCMP members, and CAF serving members impacted by an OSI.
- Free online and mobile applications such as PTSD Coach Canada and OSI Connect.
- VAC Assistance Service for Veterans, former RCMP members, their families, and caregivers, which offers confidential counselling for any issue. Pastoral support is available for those who would like to receive support from a member of the clergy. (In partnership with Health Canada).
- Support for the Canadian Institute for Military and Veteran Health Research (CIMVHR).
- Support for a Centre of Excellence on PTSD and Related Mental Health Conditions. The mission of the Centre is to increase Canadian expertise about Veteran and military OSIs (including but not limited to PTSD) and to make the expertise accessible to health care providers, people with lived experience, family members and support networks, researchers and the Canadian public.
- Support for a new Centre of Excellence on Chronic Pain in Veterans. Chronic physical health conditions and chronic pain frequently co-occur with mental health conditions in Veterans. The mission of this Centre of Excellence is to increase Canadian expertise about chronic pain.
In 2018, Statistics Canada conducted a Mental Health Follow-up Survey in collaboration with the CAF, VAC and the University of Manitoba. The purpose of the survey was to re-assess the mental health of respondents who participated in a similar survey conducted in 2002. Results of the 2018 Canadian Armed Forces Members and Veteran Mental Health Follow-up Survey are now available.
Public safety personnel
With support from the Canadian Institutes of Health Research (CIHR) and Public Safety Canada, an online survey of Canadian public safety personnel was conducted from September 2016 to January 2017 to provide estimates of mental disorder symptom frequencies and severities in this population. The survey assessed current symptoms, and participation was solicited from national public safety personnel agencies and advocacy groups. In total, 5,813 participants took part in the survey (32.5% women) and were grouped into six categories (i.e., call centre operators/dispatchers, correctional workers, firefighters, municipal/provincial police, paramedics, and RCMP). The results were released in 2018.Endnote 21
Supporting Canada's Public Safety Personnel: An Action Plan on Post-Traumatic Stress Injuries (PTSI), released on April 8, 2019 recognizes that, while public safety personnel work in multiple jurisdictions, each with their own responsibilities for providing mental health supports, there is a clear and urgent need for country-wide leadership on the challenges they all face. The Action Plan aims to strengthen the collective understanding of PTSI through research (including applied research and treatment trials); to support mental health resilience through evidence-based research to inform public awareness, training, and other initiatives that emphasize prevention, early intervention and stigma reduction; and to identify ways public safety personnel organizations can better monitor and manage the mental health of public safety personnel through support for care and treatment.
The Action Plan includes 16 key actions to complement recent initiatives and actions by the Government of Canada to support research, training, and treatment and advance the ability to make evidence-based decisions, including:
- A new national research consortium between CIHR and the CIPSRT to address PTSI among public safety personnel. The research is focusing on understanding, identifying, mitigating and/or preventing PTSI and adverse mental health outcomes for public safety personnel. CIPSRT will act as the national research consortium's knowledge exchange hub, bringing together relevant stakeholders to mobilize the knowledge created into active use.
- The development of an Internet-based Cognitive Behavioural Therapy Pilot to provide greater access to care and treatment of public safety personnel, particularly those in rural and remote areas.
- The RCMP Longitudinal Study on PTSD is an innovative and unique multi-year research project to investigate the effects of policing on the mental health of RCMP members and assess the benefits of a specialized, skills-based mental health training program. The ultimate goal of the study is to develop a skills-based training system for mental health that reduces risk, increases resilience, and enhances treatment efforts. RCMP cadets who participate will provide important data about their physical and mental health, beginning in their earliest days of training, and then throughout their first five years as RCMP officers. The findings of this study will help develop appropriate mental wellness and remedial strategies for the RCMP, and also inform the approaches of other emergency response organizations. RCMP cadet participation in the study began in April 2019.
- Building on successes from the CAF, R2MR training is being adapted to public safety personnel groups across government, including border services personnel, federal corrections officers, RCMP, and operational and intelligence personnel.
In partnership with Public Safety Canada, Defence Research and Development Canada's (DRDC) Centre for Security Science (CSS) works to strengthen Canada's ability to anticipate, prevent/mitigate, prepare for, respond to, and recover from acts of terrorism, crime, natural disasters, and serious accidents through the convergence of Science and Technology with policy, operations, and intelligence. As part of this work, DRDC funds projects that work to inform the current and future needs of Canadian public safety personnel through the development of specific health and wellness standards and through research into health and wellness models of care.
The Canadian Security Intelligence Service (CSIS), Canadian Border Services Agency and the RCMP also provide training, protocols, and support programs for employees in positions at high risk of exposure to offensive and abhorrent material.
Canadian Coast Guard employees
The Canadian Coast Guard (CCG) has developed a Trauma Resilience Training Program to acknowledge and address the needs of CCG and Department of Fisheries and Oceans (DFO) operational employees who are suffering from, or may suffer from OSI, trauma and PTSD. The risk of being impacted by traumatic events among Coast Guard employees is considered to be high and this training module is used as a means of building resilience through pre-incident awareness and tools to help employees cope when incidents occur. The intention of trauma resilience training is to create a more trauma-informed organization, de-stigmatize trauma reactions, and prevent traumatization.
All federal employees
Employee Assistance Services (EAS), Health Canada, has developed and trained a Psychosocial Emergency Response Team. This team of trauma professionals from across Canada is available, upon request, to assist federal departments and agencies to manage the psychological and social response and recovery activities when a major traumatic event occurs in the workplace. This team has been deployed to events such as the Lac Mégantic rail disaster and the Toronto Young Street van attack.
The EAS also provides Pre-Event training, which focuses on understanding and categorizing stress types and common reactions to excessive stress emphasizing the range of tools required to manage stress and create resiliency.
Federal departments with employees at higher risk of exposure to traumatic events have additional tools such as Critical Incident Stress Management (CISM) Programs, which provide psychosocial support before, during and after a disaster event or critical incident. For example, Correctional Service Canada provides the CISM program to all employees, the Department of Fisheries and Oceans offers CISM to Coast Guard, Protection and Conservation Officers, and Health Canada has a CISM program that provides prevention and response-oriented services for nurses (federal and band-transferred) working in remote First Nations communities.
The federal government also has a suite of tools and resources to support employees with mental health issues. These include: employee assistance programs that provide access to mental health care providers (including support for traumatic events); disability management; return to work; duty to accommodate programs; and workers' compensation benefits for occupational injuries and illnesses.
In 2016, the federal government adopted the Federal Public Service Workplace Mental Health Strategy, which requires federal departments to develop comprehensive action plans on mental health. As a result, many have adopted a holistic approach to health and wellness, focused on physical and psychological wellbeing of employees through prevention, promotion and intervention and de-stigmatization of mental health issues in the workplace. This includes the adoption of the National Standard for Psychological Health and Safety in the Workplace.
Indigenous Populations
The Indian Residential Schools Resolution Health Support Program, and Missing and Murdered Indigenous Women and Girls (MMIWG) Health Support Services work with individuals, families and communities as they heal from unresolved and intergenerational trauma rooted in their Residential School experience or loss and grief related to MMIWG, through cultural and emotional supports, as well as access to trauma-informed and culturally-safe mental health counselling.
Refugees and other newcomers
Through its Settlement Program, Immigration, Refugees and Citizenship Canada funds service provider organizations to deliver non-clinical mental health-related supports and provide community-based health information for newcomers. The Department also supports capacity building of service providers so they can respond to the needs of vulnerable groups, particularly women, youth, seniors, and refugees.
The Interim Federal Health Program offers limited, temporary health care coverage to resettled refugees, asylum seekers, and other groups, such as victims of human trafficking, and persons detained under the Immigration and Refugee Protection Act, until they become eligible for provincial or territorial health care coverage or, in the case of asylum claimants, leave Canada. This coverage includes a wide range of mental health supports provided by general practitioners, psychiatrists, psychologists, registered psychotherapists, registered counselling therapists, and licensed social workers. Coverage is also provided for prescription drugs, as well as interpretation and translation during counselling sessions.
All Canadians
The Public Health Agency of Canada (PHAC) works to reduce cross-cutting risk factors for mental health issues – including PTSD – such as violence, discrimination, stigma and other forms of trauma that can have lasting impacts on both mental and physical health. PHAC has made strategic investments in community-based projects to improve the physical and mental health of those who have experienced the trauma of family violence. PHAC also led the development of the Federal Framework for Suicide Prevention, published in 2016, which sets out the Government of Canada's guiding principles and strategic objectives in suicide prevention. This initiative is helping to raise awareness and reduce stigma, better connect people to information and resources, and accelerate innovation and research in suicide prevention.
The Government of Canada invests via the Canadian Institutes of Health Research (CIHR) in research on mental health and behavioural conditions such as PTSD, PTSI, suicide, and substance use. CIHR investments in mental health research and behavioural condition research are building the evidence base needed to inform policy-makers and clinicians on how to deliver the most effective mental health services for Canadians, including those living with and impacted by PTSD.
As part of its 2017 Health Accord with provinces and territories, the federal government invested more than $5 billion over ten years in mental health services based on shared principles and health priorities. Additional investments through the Emergency Treatment Fund were rolled out to provinces and territories to deal with an acute need for immediate care and treatments for individuals with substance use disorders.
Statistics Canada collects, analyzes and provides high-quality statistical information on a range of relevant topics that increase our understanding of PTSD, including those related to health, justice, social wellbeing, and special populations. The Statistics Canada Population Health Program collects information on diagnosed chronic conditions in the general population, including mood and anxiety disorders. In partnership with other relevant stakeholders, the Centre for Population Health Data is exploring how Statistics Canada can develop a new suite of projects related to the mental health of Canadians. An initiative to expand the relevance of population health data integrates existing survey data that includes information on PTSD diagnosis to administrative health records and information from the Census.
Other partners and stakeholders who provide PTSD support and services
Mental Health Commission of Canada (MHCC)
The MHCC is a pan-Canadian health organization, funded by the Government of Canada. The MHCC leads the development and dissemination of innovative programs and tools to support the mental health and wellness of Canadians.
The MHCC has played a leadership role in building capacity to advance the mental health of public safety personnel. Through stakeholder collaboration, the MHCC has developed and adapted training tools and resources to enable organizations to adopt comprehensive mental wellness strategies. The Working Mind First Responders, adapted from the CAF Road to Mental Readiness Training, is designed to reduce the stigma of mental illness and address and promote mental health and resiliency in a public safety workplace setting. The Program includes a self-assessment tool and a set of evidenced-based, cognitive behavioural therapy techniques that help individuals cope with stress and improve their mental health and resiliency.
The MHCC also offers its Mental Health First Aid (MHFA) training, at a cost, across Canada. MHFA teaches participants to recognize the signs and symptoms of the most common mental health conditions so they can support individuals who may be showing early signs of a mental health problem or crisis and direct them to appropriate support services.
The MHCC has an educational video series, which showcases stories of individual Canadian public safety personnel from coast to coast who have experienced and overcome mental health challenges, including PTSD. During the past decade, the MHCC has reduced stigma among a variety of target groups (e.g., youth, health care providers, the workforce, and news media and first responder stigma toward opioid users) through its program Opening Minds.
Canadian Institute for Public Safety Research and Treatment (CIPSRT)
CIPSRT's mission is to provide a Canadian knowledge exchange hub for strategic public safety wellness research and analysis by working with public safety leaders and academics from across Canada to translate and mobilize research knowledge that meets the current and future needs of Canadian public safety personnel, their leadership, and their families. Through its national network, CIPSRT responds to the identified needs of public safety personnel by producing or facilitating the evidence necessary for engaging strategies and allocating resources to support high-quality and easily accessible mental health care for all public safety personnel. CIPSRT works to improve the lifetime health and wellbeing of people directly or indirectly related to public safety personnel, including frontline personnel, support personnel, families of personnel, and retired personnel. CIPSRT research focuses on the unique occupational exposures, experiences, and environment encountered by people directly or indirectly related to public safety personnel.
Canadian Institute for Military and Veteran Health Research (CIMVHR)
CIMVHR brings together a network of 43 Canadian university members, ten global affiliates, four philanthropic organizations, three industry partners, several government departments, and more than 1,700 researchers—who are all committed to improving the way that Canada cares for members of the military, Veterans, and their families. As the Canadian hub for military, Veteran and family health research, CIMVHR provides the infrastructure to enable more of Canada's military, Veteran, and family health research requirements to be met by enhancing the accessibility of military, Veteran, and family health research; and engaging with stakeholders to foster collaborations, which enables increased research and improves knowledge translation activities.
CIMVHR also hosts an annual forum to engage thought leaders from government, academia, industry and philanthropic sectors. Issues discussed at the forum include mental disorders, such as PTSD, prevention and treatment of chronic health conditions, suicide prevention, and the transition to civilian life. Since 2018,CIMVHR has collaborated with CIPSRT to include research related to public safety personnel on the agenda. The forum provides an important opportunity for participants to present new research, exchange ideas, share insight, learn and collaborate on the needs of military, Veterans, public safety personnel, and their families.
Provinces and territories
All provinces and territories have mental health strategies, which focus on upstream approaches to mental health care, mental health services, stigma reduction, and treatment. These strategies recognize the impacts of trauma (including intergenerational and historical trauma) on mental health and as a risk factor for substance-related harms and suicide.
Many provinces and territories recognize the impact of PTSD on their workforce and have implemented presumptive legislation for PTSD. Presumptive legislation links a disease or condition that has been evidenced as a hazard associated with a particular occupation and allows for more timely access to services and benefits if diagnosed with the disease or condition.
As of September 2019, presumptive legislation for occupational mental health claims existed in all jurisdictions across Canada aside from Quebec, the Northwest Territories, and Nunavut. While this type of legislation is limited to PTSD in most jurisdictions, they apply to a broader set of psychological injuries in British Columbia, Alberta, Saskatchewan, and Prince Edward Island. Occupations covered by this type of legislation range from first responders (police, firefighters, paramedics) in New Brunswick and the Yukon to public safety personnel (often including correctional officers, nurses, and dispatchers) in British Columbia, Ontario, and Nova Scotia to all occupations in Alberta, Saskatchewan, Manitoba, Prince Edward Island, as well as Newfoundland and Labrador.
Alberta, Ontario, British Columbia, Saskatchewan, and Yukon offer formal support programs for jurors, which allows at least four free counselling sessions if necessary, following a trial. Most other provinces and territories have mechanisms in place to provide support for jurors, but not through a formalized program and the level of support varies by jurisdiction.
Two provinces introduced legislation designating June 27 as PTSD awareness day--Alberta celebrated its first PTSD awareness day on June 27, 2016 and Ontario began in 2019. This day was established to bring awareness to the issue, reduce stigma and recognize those living with PTSD, and the value of lived experience.
Indigenous Organizations
First Nations Mental Wellness Continuum Framework
The First Nations Mental Wellness Continuum Framework (FNMWCF) is a national framework that addresses mental wellness among First Nations in Canada. This framework was developed collaboratively by the Assembly of First Nations, Health Canada's former First Nations and Inuit Health Branch, the National Native Addictions Partnership Foundation, the Native Mental Health Association, and other community mental health leaders.
The FNMWCF is designed to strengthen federal mental wellness programs and appropriately integrate federal, provincial, and territorial programs. The FNMWCF also guides communities to better plan, implement, and coordinate comprehensive responses to mental wellness challenges in ways that are consistent with community priorities.
The FNMWCF is organized around five key themes: culture as a foundation; community development ownership and capacity building; quality care system and competent service delivery; collaboration with partners; and, enhanced flexible funding.Endnote 67
The National Inuit Suicide Prevention Strategy
Launched in 2016 by Inuit Tapiriit Kanatami (ITK), the National Inuit Suicide Prevention Strategy (NISPS) has set out a series of actions and interventions to reduce the high rates of suicide among Inuit. The Strategy promotes a shared understanding of the context and underlying risk factors for suicide in Inuit communities and guides policy at the regional and national levels on evidence-based approaches to suicide prevention.Endnote 68
The NISPS outlines six priorities areas for action and investment: create social equity; create cultural continuity; nurture healthy Inuit children; ensure access to continuum of mental wellness services for Inuit; heal unresolved trauma and grief; and mobilize Inuit knowledge for resilience and suicide prevention.
Although the Strategy focuses on suicide prevention and reducing risk factors, it also intends to build overall resilience and increase protective factors that impact mental wellness. In the priority area related to, "Healing Unresolved Trauma and Grief," the Strategy aims to address the current and ongoing impacts of historical and intergenerational trauma, as well as traumatic losses from suicide and other tragic events. The specific objectives of this priority area include the development of Inuit-specific approaches and resources and services to first responders within communities who may be impacted by exposure to the aftermath of suicide and suicide attempts.
Appendix D – Glossary of terms
A shared understanding of the common terms used to describe psychological trauma
Available from the Canadian Institute for Public Safety Research and Treatment (CIPSRT):
Appendix E - References
Endnotes
- Endnote 1
-
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), fifth edition. Arlington (VA): American Psychiatric Association; 2013.
- Endnote 2
-
Foa E. Effective Treatments for PTSD: Second Edition. New York: The Guilford Press. 2009:606-613.
- Endnote 3
-
Brennstuhl MJ, Tarquinio C, Montel S. Chronic Pain and PTSD: Evolving Views on Their Comorbidity. Perspectives in Psychiatric Care. 2015 October;51(4):295-304.
- Endnote 4
-
Panagioti M, Gooding PA, Triantafyllou K et al. Suicidality and posttraumatic stress disorder (PTSD) in adolescents: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2015; 50: 525.
- Endnote 5
-
Krysinska K, and Lester D. Post-Traumatic Stress Disorder and Suicide Risk: A Systematic Review, Archives of Suicide Research. 2010;14(1):1-23.
- Endnote 6
-
Canadian Institute for Public Safety Research and Treatment (CIPSRT). Glossary of terms: A shared understanding of the common terms used to describe psychological trauma (version 2.0).
- Endnote 7
-
Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Committee on the Assessment of Ongoing Effects in the Treatment of Posttraumatic Stress Disorder; Institute of Medicine. Washington (DC): National Academies Press (US); 2012 Jul 13.
- Endnote 8
- Endnote 9
- Endnote 10
-
Brewin CR, Andrews B, and Valentine JD. Meta-Analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766.
- Endnote 11
- Endnote 12
-
Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Canadian journal of psychiatry. 2014;59(9): 460–467.
- Endnote 13
-
Van Ameringen M, Mancini C, Patterson B, and Boyle MH. Post-traumatic stress disorder in Canada. CNS Neuroscience and Therapeutics CNS. 2008 August 13;14:171-81.
- Endnote 14
-
Statistics Canada. Table 13-10-0465-01: Mental health indicators. Ottawa (ON): Statistics Canada; 2019.
- Endnote 15
-
Weeks M, Park SB, Ghanem S, Plebon-Huff S, Robert AM, MacKay H, and LeBlanc AG. A systematic review of the prevalence of post-traumatic stress disorder reported in Canadian studies. In R. Ricciardelli, R.N. Carleton, S. Bornstein, & A. Hall (Eds.). Handbook of Posttraumatic Stress: Psychosocial, Cultural, and Biological Perspectives. Kentucky (US): Routledge, Taylor & Francis Group; in press.
- Endnote 16
-
Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur J Psychotraumatol. 2017 Sep;8(sup4):1351204.
- Endnote 17
-
Hourani H, Williams J, Bray R, and Kandel D. Gender differences in the expression of PTSD symptoms among active duty military personnel. Journal of Anxiety Disorders. 2014 Dec 4;29:101-108.
- Endnote 18
-
Brady K, Killeen T, Brewerton T, and Lucerini S. Comorbidity of Psychiatric Disorders and Posttraumatic Stress Disorder. J Clin Psychiatry. 2000;61(suppl 7):22-32.
- Endnote 19
-
Manitoba Nurses Unions. Helping Manitoba's wounded healers. Winnipeg (MB): Manitoba Nurses Union; 2015.
- Endnote 20
-
Reichert C. Enough is enough: putting a stop to violence in the health care sector, first edition. Ottawa (ON): The Canadian Federation of Nurses Unions; 2017 June. 44 p.
- Endnote 21
-
Poulin C, Gouliquer L, and McWilliams J. Othering of full-time and volunteer women firefighters in the Canadian fire services. Qualitative Sociology Review – Special Issue. 2019 February. 47 p.
- Endnote 22
-
Sareen J, Afifi TO, and Taillieu T. Deployment-related traumatic events and suicidal behaviour in a nationally representative sample of Canadian Forces Personnel. Can J Psychiatry. 2017 Nov;62(11):795–804.
- Endnote 23
-
Forbes D, Pedlar D,…Heber A,…Jetly R,…Richardson JD,…Thompson JM,…and Wessely S. Treatment of military-related post-traumatic stress disorder: Challenges, innovations, and the way forward. International Review of Psychiatry. 2019 May;31(1):95-110.
- Endnote 24
-
Sareen J, Henriksen C, Bolton S-L, Afifi TO, Stein MB, and Asmundson G. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychological Medicine. 2013;43(1):73-84.
- Endnote 25
-
Pearson C, Zamorski M, Janz T. Mental health of the Canadian Armed Forces. Statistics Canada. Ottawa: Statistics Canada; 2014 November 25. 10 p.
- Endnote 26
-
Sareen J, Cox BJ, Afifi TO, Stein MB, Belik SL, Meadows G, Asmundson GJ. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry. 2007 July; 64(7): 843–852.
- Endnote 27
-
Thompson JM, VanTil L, Zamorski MA, Garber B, Dursun S, Fikretoglu D, et al. Mental health of Canadian Armed Forces Veterans – review of population studies. Journal of Military, Veteran and Family Health. 2016;1:70-86.
- Endnote 28
-
VanTil LD, Sweet J, Poirier A, McKinnon K, Sudom K, Dursun S, Pedlar D. Well-Being of Canadian Regular Force Veterans, Findings from LASS 2016 Survey. Charlottetown (PE): Veterans Affairs Canada Research Directorate; 2017 Jun 23. Technical Report.
- Endnote 29
-
Marmar CR, McCaslin SE, Metzler TJ, Best S, Weiss DS, Fagan J et al. Predictors of posttraumatic stress in police and other first responders. Annals of the New York Academy of Sciences. 2006 Jan 1;1071:1-18.
- Endnote 30
-
Anders J and Kerstin S. Guilt, shame and need for a container: a study of post-traumatic stress among ambulance personnel. Accident and Emergency Nursing. 2004;12(4): 215-223.
- Endnote 31
-
Carleton RN, Afifi TO, Turner S, Taillieu T, Duranceau S, LeBouthillier DM et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry. 2018 Jan;63(1):54-64.
- Endnote 32
-
Bride B. Prevalence of Secondary Traumatic Stress among Social Workers. Social Work. 2007 Jan;52(1):63–70.
- Endnote 33
-
de Boer JC, Lok A, van't Verlaat E, Duivenvoorden HJ, Bakker AB, and Smit BJ. Work-related critical incidents in hospital-based health care providers and the risk of post-traumatic stress symptoms, anxiety, and depression: A meta-analysis. Social Science and Medicine. 2011 July;73(2): 316-326.
- Endnote 34
-
Substance Abuse and Mental Health Services Administration (SAMHSA) Disaster Technical Assistance Center. First Responders: Behavioral Health Concerns, Emergency Response, and Trauma [Supplemental Research Bulletin]. 2018 May.
- Endnote 35
-
Laposa JM, and Alden LE. Posttraumatic stress disorder in the emergency room: exploration of a cognitive model. Behaviour Research and Therapy. 2003;41(1):49-65.
- Endnote 36
-
Report of the Standing Committee on Health. Violence facing health care workers in Canada. Ottawa (ON): Report of the Standing Committee on Health, 42nd Parliament, 1st session; 2019 June.
- Endnote 37
-
Lonergan M, Leclerc M, Descamps M Pigeon S, and Brunet A. Prevalence and severity of trauma- and stressor-related symptoms among jurors: A review. Journal of Criminal Justice. 2016 July 26;47: 51-61.
- Endnote 38
-
Feinstein A, Owen J, Blair N. A hazardous profession: war, journalists, and psychopathology. Am J Psychiatry. 2002 Sep 1;159(9):1570-5.
- Endnote 39
-
Goodleaf S, and Gabriel W. The frontline of revitalization: Influences impacting aboriginal helpers. First Peoples Child and Family Review. 2009;4(2):18-29.
- Endnote 40
-
Centre for Addiction and Mental Health. Police Mental Health: A Discussion Paper. Toronto (ON): Centre for Addiction and Mental Health. 2018. 14 p.
- Endnote 41
-
Brown J and Fraehlich C. Aboriginal Family Services Agencies in High Poverty Urban Neighborhoods: Challenges Experienced by Local Staff. First Peoples Child and Family Review. 2011;6(1):10-27.
- Endnote 42
-
Finklestein M, Stein E, Greene T, Bronstein I, and Solomon Z. Posttraumatic Stress Disorder and Vicarious Trauma in Mental Health Professionals. Health & Social Work. 2015;40(2):25-31.
- Endnote 43
-
Lerias D and Byrne MK. Vicarious traumatization: symptoms and predictors. Stress and Health. 2003 Aug 6;19(3):129–138.
- Endnote 44
-
Minore B, Boone M, Katt M, Kinch P, Birch S, and Mushquash C. The Effects of Nursing Turnover on Continuity of Care in Isolated First Nation Communities. Canadian Journal of Nursing Research. 2005 Jun;37(2):2.
- Endnote 45
-
Bombay A, Matheson K and Anisman H. (2014) The intergenerational effects of Indian Residential Schools: Implications for the concept of historical trauma. Transcultural Psychiatry. 2014;51(3) 320–338.
- Endnote 46
-
National inquiry into Missing and Murdered Indigenous Women and Girls. Reclaiming Power and Place [Final Report on the Internet]. 2019 [cited 2019 Oct]. 1,180 p.
- Endnote 47
-
Aguiar W, and Halseth R. Aboriginal Peoples and Historic Trauma: The Processes of Intergenerational Transmission. Prince George (BC): National Collaborating Centre for Aboriginal Health; 2015. 32p.
- Endnote 48
-
Cutajar MC, Mullen PE, Ogloff JP, Thomas S, Wells D and Spataro J. Psychopathology in a large cohort of sexually abused children followed up to 43 years. Child Abuse and Neglect. 2010 November;34(11):813-822.
- Endnote 49
-
Tang B, Liu X, Liu Y, Xue C, and Zhang L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014 Jun 19;14(623).
- Endnote 50
-
Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467–480.
- Endnote 51
-
Bellamy, S and Hardy C. Post-traumatic Stress Disorder in Aboriginal People in Canada: Review of Risk Factors, the Current State of Knowledge and Directions for Future Research. Prince George (BC): National Collaborating Centre for Aboriginal Health; 2015. 26 p.
- Endnote 52
-
Richmond CAM, Ross NA, and Bernier J. Exploring Indigenous Concepts of Health: The Dimensions of Métis and Inuit Health. Aboriginal Policy Research Consortium International (APRCi) 2007. 115 p.
- Endnote 53
-
Simpson L. Violent victimization of lesbians, gays and bisexuals in Canada. Statistics Canada Catalogue no. 85-002-X. Ottawa (ON): Statistics Canada; 2014.
- Endnote 54
-
Roberts AL, Austin SB, Corliss HL, Vandermorris AK, and Koenen KC. Pervasive Trauma Exposure Among US Sexual Orientation Minority Adults and Risk of Posttraumatic Stress Disorder. Am J Public Health. 2010;100(12):2433-41.
- Endnote 55
-
Bontempo DE, and D'Augelli AR. Effects of at-school victimization and sexual orientation on lesbian, gay, or bisexual youths' health risk behavior. Journal of Adolescent Health. 2002;30(5): 364-374.
- Endnote 56
-
Friedman Mark, Marshal MP, Guadamuz T, Wei C, Wong CF, Saewyc EM, et al. A Meta-Analysis of Disparities in Childhood Sexual Abuse, Parental Physical Abuse, and Peer Victimization Among Sexual Minority and Sexual Nonminority Individuals. Am J Public Health. 2011;101(8):1481-94.
- Endnote 57
-
Mooney M. Recognizing, Treating, and Preventing Trauma in LGBTQ Youth. Journal of Family Strengths. 2017;17(2):16.
- Endnote 58
-
Roberts AL, Rosario M, Corliss, HL, Koenen KC, and Austin SB. Elevated Risk of Posttraumatic Stress in Sexual Minority Youths: Mediation by Childhood Abuse and Gender Nonconformity. American Journal of Public Health. 2012;102(8):1587-1593.
- Endnote 59
-
Ponka D and Wilkinson L. Migration, Health and Survival: International Perspectives. Cheltenham: Edward Elgar Publishing Limited; 2017:88-110.
- Endnote 60
-
Fazel M, Wheeler J, and Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet. 2005;365(9467):1309-14.
- Endnote 61
-
Baddoura C, and Merhi M. PTSD among children and adolescents in the Arab World. The Arab Journal of Psychiatry. 2015;26(2), 129-136.
- Endnote 62
-
Ghumman U, McCord CE, and Chang JE. Posttraumatic stress disorder in Syrian refugees: A review. Canadian Psychology / Psychologie canadienne. 2016;57(4): 246-253.
- Endnote 63
-
Thabet AAM, Abed Y, and Vostanis P. Comorbidity of PTSD and depression among refugee children during war conflict. Journal of Child Psychology and Psychiatry. 2004;45(3):533-542.
- Endnote 64
-
Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, et al. Common mental health problems in immigrants and refugees: general approach in primary care. Canadian Medical Association Journal. 2011 Sep 6;183(12):959–967.
- Endnote 65
-
Bryant RA, Edwards B, Creamer M, O'Donnell M, Forbes D, Felmingham KL, et al. The effect of post-traumatic stress disorder on refugees' parenting and their children's mental health: a cohort study. 2018 May;3(5):249-258.
- Endnote 66
-
Torchalla I, Strehlau V, Li K, Linden IA, Noel F and Krausz M. Posttraumatic Stress Disorder and Substance Use Disorder Comorbidity in Homeless Adults: Prevalence, Correlates, and Sex Differences. Psychology of Addictive Behaviors. 2013 August;28(2):443-452.
- Endnote 67
-
Thunderbird Partnership Foundation. First Nation Mental Wellness Continuum Framework. Bothwell (ON): Thunderbird Partnership Foundation; 2015.
- Endnote 68
-
Inuit Tapiriit Kanatami. The National Inuit Suicide Prevention Strategy. Ottawa (ON): Inuit Tapiriit Kanatami; 2016. 48 p.
Footnotes
- Footnote a
-
While the spelling in the Act has a hyphen (i.e., post-traumatic), the spelling in the Diagnostic and Statistical Manual of Mental Disorders (DSM) does not. For the purposes of this Framework, the DSM spelling (i.e., posttraumatic) will be used, except when referencing the Act specifically.
- Footnote b
- Footnote c
-
For the purpose of this section, frontline workers include public safety personnel, health and social service providers, including mental health care and support.
- Footnote d
- Footnote e
-
https://www.canada.ca/content/dam/dnd-mdn/documents/reports/2017/caf-vac-joint-suicide-prevention-strategy.pdf