Vaccine hesitancy in Canadian parents
Download in PDF format
(956 KB, 30 pages)
Organization: Public Health Agency of Canada
Date published: 2022-04-04
On this page
- Summary
- Introduction
- Methods
- Results
- Discussion
- Strengths and limitations
- Conclusion
- Acknowledgements
List of Abbreviations
- CATI
- Computer Assisted Telephone Interview
- CCB
- Canadian Child Benefit
- CIRN
- Canadian Immunization Research Network
- CLSC
- Centre local de services communautaires (Local Community Service Centre)
- CNICS
- Childhood National Immunization Coverage Survey
- HBM
- Health Belief Model
- HPV
- Human Papillomavirus
- INSPQ
- Institut National de Santé Publique du Québec
- KAB
- Knowledge, Attitudes, and Beliefs
- NIS
- National Immunization Survey
- PHAC
- Public Health Agency of Canada
- SAGE
- Strategic Advisory Group of Experts
- SIDS
- Sudden Infant Death Syndrome
- VPD
- Vaccine Preventable Diseases
- WHO
- World Health Organization
Summary
This report summarizes the results from the 2017 childhood National Immunization Coverage Survey (cNICS) pertaining to Canadian parents' knowledge, attitudes and beliefs (KAB) towards childhood vaccines. It also provides estimates of vaccine hesitancy prevalence among Canadian parents of two-year-old children.
For the purpose of the present analysis, respondents were considered vaccine-hesitant if they indicated in the survey that they either had refused or hesitated to get their child vaccinated with one or more non-influenza vaccines, or decided to delay vaccination for a reason other than their child having health issues. Vaccine hesitancy and the complete refusal of all vaccines were considered as two different, mutually exclusive events. The analysis of non-vaccination is described in detail in the 2017 cNICS coverage report.Reference footnote 1 Parents who refused all vaccines for their child were not considered as vaccine-hesitant in this report.
Vaccine hesitancy:
- Overall, 17% of parents were considered to be vaccine-hesitant.
- Significant regional variations in the prevalence of vaccine hesitancy were observed (14% to 24%).
Knowledge, Attitudes and Beliefs (KAB) regarding childhood vaccines:
- Most parents strongly believed that childhood vaccines are effective (71%), and help to protect the health of their child (78%) and others in the family (76%) or community (78%).
- One in four respondents (25%) strongly or somewhat agreed that a vaccine can give a serious case of the very same disease it was meant to prevent.
- Almost one third of parents (31%) strongly or somewhat agreed that it is better for children to develop their immunity from natural infections rather than from vaccines.
- There were a number of parents that thought the use of alternative practices can eliminate or replace the need for vaccination. This includes homeopathy or chiropractic (13% strongly or somewhat agreed) or a healthy lifestyle (e.g., nutrition and hygiene) (17% strongly or somewhat agreed).
Source of information on childhood vaccination:
- The source of information most trusted by parents was their medical doctors (really trusted by 43%).
- The most commonly reported sources of information on vaccination were medical doctors (81%), local public health clinic or CLSC (54%) and nurses (50%).
In summary, the estimated prevalence of vaccine hesitancy among Canadian parents of two-year-old children was 17%. Primary health care providers, in particular doctors, were the most trusted sources of information on childhood vaccination. They therefore have an essential role in promoting vaccination uptake and dispelling myths, such as a vaccine can give a serious case of the same disease it is meant to prevent, and it is better for children to develop their immunity from natural infections rather than from vaccines.
Introduction
High vaccination coverage is essential in preventing the transmission of vaccine-preventable diseases (VPD) and reducing morbidity and mortality resulting from these diseases.Reference footnote 2 Vaccination of children is a major public health priority as some infectious diseases are particularly harmful to children. In Canada, young children are routinely vaccinated against diphtheria, pertussis (whooping cough), tetanus, poliomyelitis, Haemophilus influenzae type B (Hib), measles, mumps, rubella, varicella (chickenpox), meningococcal and pneumococcal infections, hepatitis B, influenza, and rotavirus.Reference footnote 3 To ensure children are protected, a high vaccination coverage goal of 95% as part of the National Immunization Strategy objectives for 2016-2021 has been established for all childhood vaccines by two and seven years of age.Reference footnote 4 However, vaccine uptake remains suboptimal in CanadaReference footnote 5 and sporadic outbreaks of measlesReference footnote 6Reference footnote 7 and pertussisReference footnote 8Reference footnote 9Reference footnote 10 continue to occur.
Lack of confidence in the safety and effectiveness of vaccines is a major contributor to some parents' decision not to vaccinate their children. Based on the childhood National Immunization Coverage Survey (cNICS), an estimated 2.4% of Canadian two-year-old children had not received any vaccine in 2017. The main reason for this, mentioned by 54% of non-vaccinating parents, was concern about vaccine safety and 33% were not confident in the usefulness or the effectiveness of vaccines.Reference footnote 1 Compared with vaccine refusers, vaccine-hesitant parents are a larger group who underimmunize their children instead of not immunizing them at all. Vaccine-hesitant parents who decided to refuse or delay certain recommended vaccinations due to lack of confidence in vaccine safety and/or effectiveness, leave their children unprotected from infectious disease at the most vulnerable age. Their choices may in fact, have a larger impact on population immunity than the non-vaccination group. Vaccine hesitancy can be seen as an intermediate attitude between the refusal of all vaccines and the acceptance of all vaccines recommended by public health authorities. A working group convened by the World Health Organization (WHO)'s Strategic Advisory Group of Experts (SAGE) to investigate this phenomenon defined vaccine hesitancy as the "delay in acceptance or refusal of vaccination despite availability of vaccination services"
.Reference footnote 11 A consultation of Canadian experts and healthcare providers, conducted by the Canadian Immunization Research Network (CIRN), led to a broader definition: "the reluctance to receive recommended vaccination because of concerns and doubts about vaccines that may or may not lead to delayed vaccination or refusal of one, many or all vaccines"
.Reference footnote 12
According to the SAGE working group, multiple factors can influence vaccine hesitancy or acceptance. The Complacency, Convenience and Confidence (3Cs) model was created to better understand and group vaccine hesitancy determinants. Complacency exists when there is a low perceived risk from VPD; convenience is the availability and accessibility of vaccination services, including the accessibility of information on vaccines; and confidence is the trust in the safety and effectiveness of vaccines.Reference footnote 11 These factors can interact with each other: for instance, a parent who is not convinced of the usefulness of a vaccine may be more deterred by some inconvenience than a parent who is convinced that vaccines work and are effective.
The prevalence of vaccine hesitancy in Canada was unknown until now. The previous cycles of cNICS included several questions on knowledge, attitudes and beliefs (KAB) towards vaccines, but the information gathered was not sufficient to measure vaccine hesitancy and identify vaccine-hesitant parents. To address this gap, the KAB section of cNICS was re-designed in 2016-2017 with the assistance of a group of expertsFootnote 1 in order to better measure vaccine hesitancy.
This report presents findings from the descriptive analysis of the KAB section of the 2017 cycle of cNICS, including estimates of the prevalence of vaccine hesitancy among Canadian parents of two-year-old children. A better understanding of the scope of vaccine hesitancy and the negative perceptions about vaccines and their origins will guide interventions that can more efficiently address vaccine hesitancy within Canada.
Methods
Data sources
cNICS 2017 was conducted by the Public Health Agency of Canada (PHAC) and Statistics Canada primarily to estimate national uptake for all publicly funded routine childhood vaccinations in Canada. The survey also assessed knowledge, attitudes, and beliefs (KAB) among parents to better understand factors influencing decisions on vaccination for their children. This report presents the results pertaining to parents' KAB about vaccination; coverage estimates from cNICS are described in a separate report.Reference footnote 1 A detailed description of sampling, data collection and data processing methods used in cNICS is available on the Statistics Canada's website.Reference footnote 13
Sampling
The sampling frame of the survey was built using the list of children for whom the ab (CCB) was claimed as of June 2017. This list is estimated to include 96% of Canadian children. Children aged two, seven, fourteen or seventeen years as of March 1, 2017, were eligible for inclusion in the survey. Children were randomly selected from the sampling frame by Statistics Canada. The sampling method ensured that only one eligible child from each household was selected. Children were selected by strata defined by gender, age, provinces and territories. Sampling weights were assigned to each respondent in order for estimates to be nationally representative of the Canadian population as of March 2017. The weights were adjusted for non-response bias.
The target population for the KAB analysis consisted of parents of Canadian children aged two years, except for institutionalized children and First Nations children living on reserve. The reason to restrict the analysis to one age group only was to ensure a homogeneous population with respect to the vaccines and number of doses recommended and offered to their children. In addition, the two-year-old age group was used because it had by far and away the largest sample size, which permitted a more comprehensive analysis at the provincial and territorial level.
Data collection and processing
Data were collected through a computer assisted telephone interview (CATI) during which the person most knowledgeable about the child's vaccinations, usually a parent or guardian (hereafter referred to as the respondent or parent), provided information about vaccines their child had received and answered questions regarding their knowledge, attitudes and beliefs about childhood vaccination.
The 2017 cNICS questionnaire was developed by Statistics Canada and PHAC. The entire questionnaire was also reviewed and tested by Statistics Canada's Questionnaire Design Resource Centre before being used.
The questionnaire included several blocks of questions collecting information about parents' KAB regarding immunization. Questions in the first two KAB blocks were asked only to respondents who provided a positive answer to the very first question of the survey "Has your child ever been vaccinated?"
, to which the respondents were not allowed to refuse to answer or respond "I don't know"
. In the first KAB block, those who had vaccinated their child at least once were asked "Have you ever decided not to immunize your child with a particular vaccine" with the possibility to answer "Yes"
, "No"
, and "I don't know"
. Those who answered "Yes"
were then asked which vaccine(s) they decided not to give to the child (Figure 1). Parents could answer this question by naming either antigens (e.g., measles, pertussis) or vaccines (e.g., MMR, DTaP).
In the next block, respondents were asked "Have you ever been reluctant or hesitated to get a vaccination for your child?"
with the possibility to answer "Yes"
, "No"
, and "I don't know"
. Parents or guardians who answered "Yes"
to this question were asked to identify the vaccine(s) they were reluctant to get for their child, the reasons why they hesitated and finally, what made them decide to have their child vaccinated despite their initial reluctance. Then, parents were also asked "Have you ever decided to delay any vaccines for your child?"
with the possibility to answer "Yes"
, "No"
and "I don't know"
. Those who answered "Yes"
were asked to choose the reasons why they decided to delay some vaccines for their child.
In the third KAB block, respondents were asked 15 questions to measure their KAB about vaccination using a 4-point Likert scale with the possibility to answer "I don't know"
. For each of the 15 statements, respondents were asked to state if they strongly agreed, somewhat agreed, somewhat disagreed or strongly disagreed with statements such as "Childhood vaccines are safe"
, "Vaccines help to protect my child's health"
, and "In general, I am concerned about the potential side effects from vaccines."
In the final KAB block, respondents were asked to what extent do they trust the sources of information on vaccination using a 4-point Likert scale ranging from "Really trust"
to "Do not trust at all"
, with the possibility to answer "I don't know"
. Then, the fourth KAB block finished by asking parents where they seek information on vaccination for their child (Figure 1).
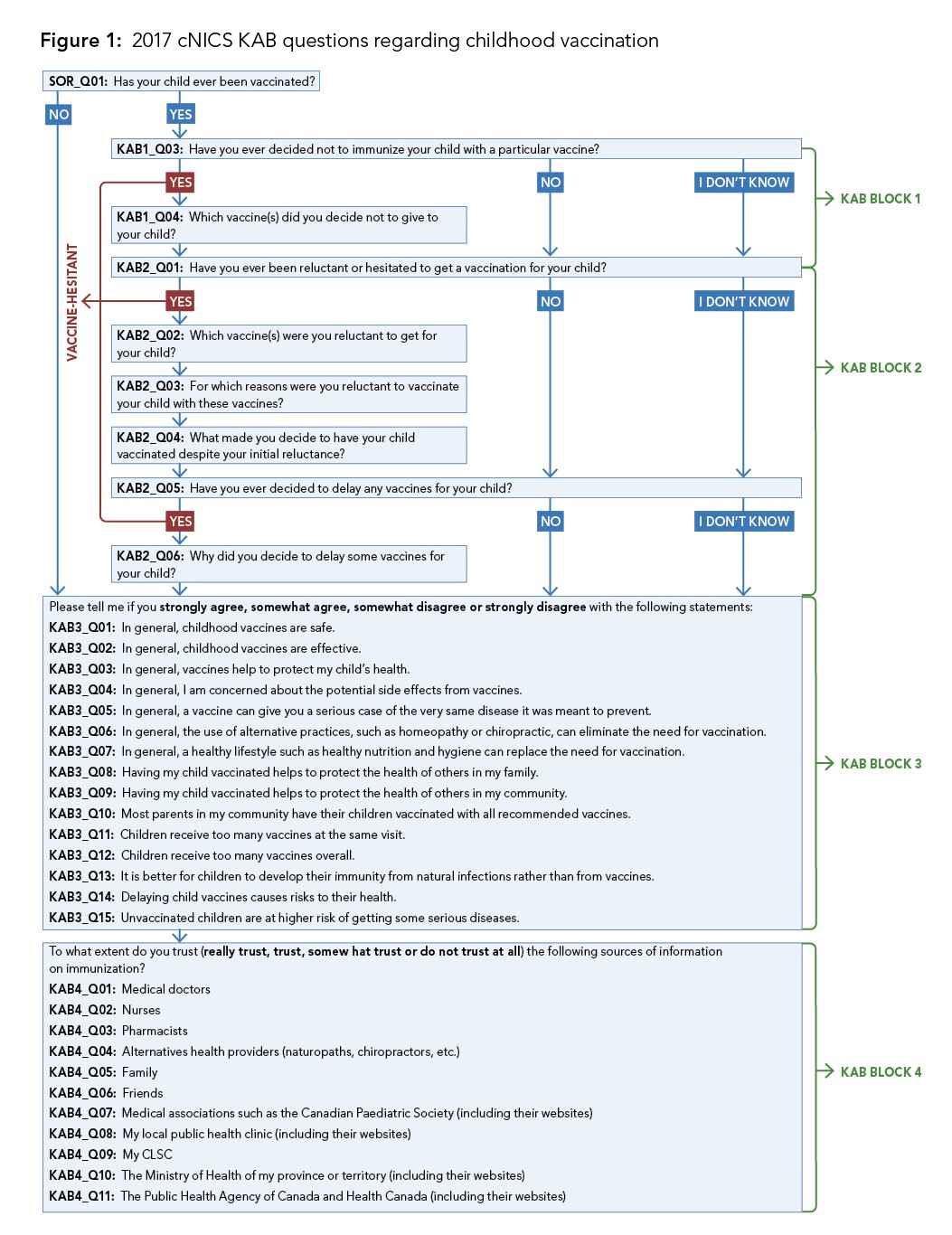
Figure 1 - Text description
- SOR_Q01: Has your child ever been vaccinated?
- Yes – go to KAB Block 1
- No – go to KAB Block 3
KAB Block 1:
- KAB1_Q03: Have you ever decided not to immunize your child with a particular vaccine?
- YesFigure * – go to KAB1_Q04
- No/I don't know – go to KAB Block 2
- KAB1_Q04: Which vaccine(s) did you decide not to give to your child?
KAB Block 2:
- KAB2_Q01: Have you ever been reluctant or hesitated to get a vaccination for your child?
- YesFigure * – go to KAB2_Q02
- No/I don't know – go to KAB2_Q05
- KAB2_Q02: Which vaccine(s) were you reluctant to get for your child?
- KAB2_Q03: For which reasons were you reluctant to vaccinate your child with these vaccines?
- KAB2_Q04: What made you decide to have your child vaccinated despite your initial reluctance?
- KAB2_Q05: Have you ever decided to delay any vaccines for your child?
- YesFigure * – go to KAB2_Q06
- No/I don't know – go to KAB Block 3
- KAB2_Q06: Why did you decide to delay some vaccines for your child?
KAB Block 3:
- Please tell me if you strongly agree, somewhat agree, somewhat disagree or strongly disagree with the following statements:
- KAB3_Q01: In general, childhood vaccines are safe.
- KAB3_Q02: In general, childhood vaccines are effective.
- KAB3_Q03: In general, vaccines help to protect my child's health.
- KAB3_Q04: In general, I am concerned about the potential side effects from vaccines.
- KAB3_Q05: In general, a vaccine can give you a serious case of the very same disease it was meant to prevent.
- KAB3_Q06: In general, the use of alternative practices, such as homeopathy or chiropractic, can eliminate the need for vaccination.
- KAB3_Q07: In general, a healthy lifestyle such as healthy nutrition and hygiene can replace the need for vaccination.
- KAB3_Q08: Having my child vaccinated helps to protect the health of others in my family.
- KAB3_Q09: Having my child vaccinated helps to protect the health of others in my community.
- KAB3_Q10: Most parents in my community have their children vaccinated with all recommended vaccines.
- KAB3_Q11: Children receive too many vaccines at the same visit.
- KAB3_Q12: Children receive too many vaccines overall.
- KAB3_Q13: It is better for children to develop their immunity from natural infections rather than from vaccines.
- KAB3_Q14: Delaying child vaccines causes risks to their health.
- KAB3_Q15: Unvaccinated children are at higher risk of getting some serious diseases.
KAB Block 4:
- To what extent do you trust (really trust, trust, somewhat trust or do not trust at all) the following sources of information on immunization?
- KAB4_Q01: Medical doctors
- KAB4_Q02: Nurses
- KAB4_Q03: Pharmacists
- KAB4_Q04: Alternatives health providers (naturopaths, chiropractors, etc.)
- KAB4_Q05: Family
- KAB4_Q06: Friends
- KAB4_Q07: Medical associations such as the Canadian Paediatric Society (including their websites)
- KAB4_Q08: My local public health clinic (including their websites)
- KAB4_Q09: My CLSC
- KAB4_Q10: The Ministry of Health of my province or territory (including their websites)
- KAB4_Q11: The Public Health Agency of Canada and Health Canada (including their websites)
Data analysis
cNICS is primarily aimed at measuring vaccination coverage. Therefore, any person able to provide information on the vaccination of the selected child can be accepted as a respondent. However, for the analysis of KAB it is important to focus on those respondents who are most likely to be the ones making decisions regarding the child's vaccination. For this reason the analysis includes only respondents who identified themselves as a biological parent, an adoptive parent or a step-parent to the selected child.
Of the 6,502 two-year-old surveyed children, 6,463 (99%) had a biological parent, adoptive parent or step-parent as their respondent, whereas 39 (1%) had another person (e.g., older sibling, or grandparent). Only the former were included in the analysis.
A vaccine hesitancy variable was created based on vaccine refusal, reluctance and delays. Those parents who have ever refused or been reluctant to get their child vaccinated for a particular vaccine (other than influenza vaccine), or ever decided to delay any vaccines for a reason other than their child having health issues were considered as vaccine-hesitant. The refusal of influenza vaccine only, or reluctance about this vaccine only was not included in the definition of vaccine hesitancy because not all provinces and territories include influenza vaccine in their childhood immunization schedule, each province and territory has designed and adopted its own approach to immunizing their population regarding this vaccine, and the importance of influenza vaccine may be perceived differently among parents from different regions.Reference footnote 14 Parents who never refused or hesitated to get their child vaccinated, but decided to delay vaccination due to child's health issues only, were not considered as vaccine-hesitant because this includes postponing a vaccination appointment for a sick child until he or she gets better, which is not vaccine hesitancy.
As per Statistics Canada rules on data confidentiality and disclosure analysis, tables of results should not contain cells with less than 10 observations. As a result, the response categories "Religious reasons" and "Philosophical reasons" were combined together for the question about why parents were reluctant to vaccinate their child. For the same reason, due to small numbers of observations in the non-vaccination group, Newfoundland and Labrador, Prince Edward Island, Nova Scotia and New Brunswick were grouped together into the "Atlantic region"; and those in the three territories (Yukon, Northwest Territories, Nunavut) were grouped into the "Northern region".
Analysis was completed using SAS 9.4. Based on collected KAB information, the parental vaccine hesitancy rate was calculated as the proportion of parents (birth, step or adoptive) that had refused partially, delayed or hesitated to immunize their child. The denominator of the vaccine hesitancy rate were all parents of a two-year-old child, including parents whose child had not received any vaccine. Those who refused to answer or answered "I don't know" to a given question of the survey were excluded from the rate calculation for this question. For this reason, the total number presented in the result tables were less than 6,463.
Variance and 95% confidence intervals were estimated using the bootstrap method.Reference footnote 15 The precision of the estimate was determined by the coefficient of variation. Estimates with a coefficient of variation from 16.6% to 33.3% indicated higher sampling error and are to be interpreted with caution. Estimates with a coefficient of variation greater than 33.3% or based on a count less than 10 were considered unreliable and therefore are not reported.
All estimates presented in this report are weighted.
Results
The overall response rate in cNICS 2017 for parents of children aged two years was 62%. A total of 6,463 parents (biological, adoptive or step parents) of two-year-old children that responded to the KAB questions were included for analysis. However, some parents declined to answer specific questions, leading to lower response rates for these questions.
Vaccine refusals
Overall, 92% of parents had never refused a vaccine other than influenza for their child. About 6% had refused at least one vaccine other than influenza, leaving 2% of parents who had refused all vaccines for their child (Table 1.1). Vaccines most frequently refused among respondents who refused any vaccine other than influenza were rotavirus (40%) and varicella (29%) vaccines. Non-vaccination is described in detail in the 2017 cNICS coverage report.Reference footnote 13
| Response (n = 6,446) | % (95% CI) |
|---|---|
| Never refused any vaccine | 81.6 (80.1-83.0) |
| Refused influenza only | 10.5 (9.4-11.7) |
| Refused any vaccine other than influenzaTable 1.1 footnote * | 5.5 (4.7-6.4) |
| Refused all vaccines | 2.4 (1.8-3.0) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Reluctance to vaccinate
Among those parents whose child had received at least one vaccine, a large majority (88%) had never been reluctant to get a vaccination for their child, or had been reluctant towards the influenza vaccine only. However, there were still 10% of parents that had been initially reluctant to vaccinate their child with at least one vaccine (other than influenza) but ended up having their child vaccinated (Table 2.1). The vaccines that parents were most reluctant towards were measles-containing vaccines (MMR and MMRV), the varicella vaccine and the rotavirus vaccine (29%, 25% and 23%, respectively).
| Response (n = 6,447) | % (95% CI) |
|---|---|
| Never being reluctant | 85.4 (84.1-86.8) |
| Reluctant to influenza only | 2.6 (1.9-3.2) |
| Reluctant to vaccine other than influenzaTable 2.1 footnote * | 9.6 (8.5-10.8) |
| Refused all vaccines | 2.4 (1.8-3.0) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Among those parents who had been initially reluctant to vaccinate their child with a non-influenza vaccine (10%), the most common reason for being reluctant to vaccinate their child was concern about the risk of side effects of vaccines (62% of reluctant respondents). 16% of the reluctant respondents did not consider the vaccines necessary for their child, and 12% of the reluctant respondents did not feel confident in the effectiveness of the vaccines. 2% of parents were reluctant to vaccinate their child because of religious or philosophical reasons (Table 2.2).
| Response (n = 535)Table 2.2 footnote * | % (95% CI) |
|---|---|
| Concerns about the risk of side effects of vaccines | 61.9 (55.5-68.2) |
| Did not consider it necessary for my child | 16.2 (11.0-21.3) |
| Not confident in the effectiveness of vaccines | 11.5 (7.4-15.6) |
| Religious or philosophical reasons | 1.9 (0.5-3.3) |
| Other | 29.6 (23.7-35.5) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
The most common reason for parents to decide to have their child vaccinated despite their initial reluctance was because of advice from their doctor or health care professional (27%). The other main reasons cited were to protect the child from disease (22%), and the perception that the benefits of getting the vaccines for their child outweighed the risks (16%) (Table 2.3).
| Response (n = 528)Table 2.3 footnote * | % (95% CI) |
|---|---|
| Advice from my doctor or health care professional | 27.1 (21.2-33.0) |
| To protect him/her from disease | 21.7 (16.2-27.2) |
| Benefits outweigh risks | 16.5 (11.5-21.4) |
| Need it for day care or school entry | 6.2 (2.9-9.5) |
| Advice from a friend or a family member | 4.1 (1.5-6.6) |
| I fear I may regret it later if I don't | 2.6 (0.2-5.1) |
| To protect others from disease | 2.3 (0.3-4.2) |
| Other | 18.8 (13.4-24.1) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Delayed vaccination
Among parents whose child had been vaccinated, 13% had decided to delay at least one vaccine. (Table 3.1)
| Response (n = 6,446) | % (95% CI) |
|---|---|
| No | 85.1 (83.7-86.6) |
| Yes | 12.5 (11.3-13.8) |
| Refused all vaccines | 2.4 (1.8-3.0) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
More than half of the parents who delayed their child's vaccination(s) (54%) reported having done so because of an issue related to the health of their child, and 18% of the parents delayed vaccination because they thought that their child was too young to be vaccinated (Table 3.2).
| Response (n = 821) | % (95% CI) |
|---|---|
| My child had a health issue | 54.3 (48.7-59.9) |
| My child was too young to receive vaccines | 18.3 (13.8-22.7) |
| Too many vaccines at the same time | 9.4 (5.8-12.9) |
| Needed more time to decide | 5.9 (3.4-8.3) |
| Other | 20.1 (15.7-24.5) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
In total, 4% of respondents had never refused or hesitated to get their child vaccinated, and only delayed vaccination because of their child's health issues. These parents were excluded from the estimate of vaccine hesitancy in the study (Table 3.3).
| Response (n = 6,446) | % (95% CI) |
|---|---|
| Never delayed any vaccines | 85.1 (83.7-86.6) |
| Delayed due to child's health issues only | 4.3 (3.5-5.1) |
| Delayed because of other reasonsTable 3.3 footnote * | 8.2 (7.1- 9.3) |
| Refused all vaccines | 2.4 (1.8-3.0) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Prevalence of vaccine hesitancy
Overall, 17% of parents were considered as vaccine-hesitant. They had either refused, or been reluctant towards at least one vaccine other than influenza, or delayed one or more vaccines for reasons other than their child had a health issue. Parents who had refused or been reluctant to influenza vaccine were counted in the non-hesitant group. Parents who only delayed vaccination due to child's health issue without refusing or hesitating to get any vaccines for their child, were also included in the non-hesitant group. However, parents who selected more than one reason for delaying a child's vaccination were considered as vaccine-hesitant (Table 4.1).
| Response (n = 6,438) | % (95% CI) |
|---|---|
| Non-hesitant | 80.2 (78.7-81.8) |
| Hesitant | 17.4 (15.9-18.9) |
| Refused all vaccines | 2.4 (1.8-3.0) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Significant regional variations in the prevalence of vaccine hesitancy were also observed. Quebec had the highest proportion of vaccine-hesitant parents (24%), whereas Alberta had the lowest (14%) (Table 4.2).
| Region | Refuse all % (95% CI) |
Hesitant % (95% CI) |
Non-hesitant % (95% CI) |
n |
|---|---|---|---|---|
| Atlantic region | 1.4 (0.8-1.9) | 15.6 (13.9-17.4) | 83.0 (81.2-84.8) | 2,145 |
| Quebec | 3.0 (1.6-4.3) | 23.9 (20.5-27.3) | 73.1 (69.5-76.7) | 628 |
| Ontario | 1.7 (0.7-2.7) | 15.6 (12.8-18.5) | 82.7 (79.7-85.6) | 636 |
| Manitoba | 3.4 (1.9-4.8) | 15.7 (12.6-18.7) | 81.0 (77.7-84.3) | 553 |
| Saskatchewan | 2.8 (1.3-4.2) | 15.3 (11.8-18.7) | 82.0 (77.8-86.2) | 564 |
| Alberta | 2.0 (0.9-3.2) | 14.3 (11.6-17.1) | 83.6 (80.7-86.6) | 622 |
| British Columbia | 3.9 (2.3-5.6) | 16.2 (12.9-19.4) | 79.9 (76.6-83.3) | 578 |
| Northern region | 1.8 (0.7-2.9) | 21.9 (18.4-25.3) | 76.3 (72.8-79.8) | 712 |
| Total | n = 132 | n = 1,092 | n = 5,214 | 6,438 |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. Note: Due to the small number of observations (n < 10) in the 'refuse all' category, some provinces and territories were combined. Atlantic region includes Newfoundland and Labrador, Prince Edward Island, Nova Scotia and New Brunswick; Northern region includes Yukon, Northwest Territories and Nunavut. |
||||
Knowledge, attitudes and beliefs regarding vaccines organized by Health Belief Model (HBM) dimensions
The Health Belief Model (HBM) can be used to understand beliefs and perceptions of threats, benefits and barriers about childhood vaccination, and guide the choice of interventions for parents who refuse or hesitate to vaccinate their child. Perceived threats refer to an individual's joint perception of susceptibility to a disease (i.e., the likelihood of contracting it) and severity of the disease (i.e., the possibility of severe symptoms or serious consequences of contracting an illness). Perceived benefits refer to an individual's belief in potential benefits of getting vaccinated, primarily being protected from diseases; this includes the confidence in the effectiveness of vaccines. Perceived barriers are the perception about the potential negative aspects of getting vaccinated such as concerns about vaccine safety and side effects.Reference footnote 16Reference footnote 17 Studies have shown that the perceived threat of diseases encourages vaccine uptake and people were more likely to get vaccinated if they perceived more benefits than barriers from vaccination.Reference footnote 16Reference footnote 17Reference footnote 18Reference footnote 19 The perceived threat and effectiveness of vaccination differ from one illness to another.Reference footnote 18 Some stimulus is necessary to trigger the decision-making process and activate an individual's readiness to seek vaccination, which is called cues to action.Reference footnote 16Reference footnote 17 A health care provider's recommendation and a belief that vaccination is a social norm were found to be effective cues to action.Reference footnote 16Reference footnote 20
Two KAB statements assessed the perceived threat dimension. Although most parents recognized the threat that not vaccinating posed to their child's health (87% strongly or somewhat agreed), 31% of parents strongly or somewhat disagreed that delaying childhood vaccines presented a risk (Table 5.1).
Four statements were related to a person's perceived benefits of childhood vaccination, whereas three statements were linked to the absence of such benefits. The majority of respondents of two-year-old children strongly believed that childhood vaccines are effective (71%), and help to protect the health of their child (78%) and others in the family (76%) or community (78%). However, 13% of parents strongly or somewhat agreed that the use of alternative health practices (such as naturopathy) can eliminate the need for vaccination, and 17% thought that lifestyle choices such as healthy nutrition and good hygiene can replace the need for vaccination. More than a third of parents (31%) strongly or somewhat believed that it is better for children to develop their immunity from natural infections rather than from vaccines (Table 5.1).
Four statements were associated with the presence of perceived barriers and one statement was related to the absence of such barriers. The results indicated that the most important barrier to getting a child vaccinated was a concern about potential side effects from vaccines (52% strongly or somewhat agreed). Despite 94% of parents strongly or somewhat agreeing that childhood vaccines are safe, one in four (25% strongly or somewhat agreed) still believed that a vaccine can give their child a serious case of the disease it was meant to prevent. Moreover, 35% (strongly or somewhat agreed) of respondents felt that children receive too many vaccines at the same visit, and 22% thought that children receive too many vaccines overall (Table 5.1).
In addition, one statement in the cue to action category on social norms was asked to parents in order to measure whether they believe other parents in their communities are vaccinating their children. The results showed that 94% of respondents strongly or somewhat agreed that most parents in their community have their children vaccinated with all recommended vaccines (Table 5.1). Social norms can be supportive of vaccination by encouraging behaviour perceived as 'normal', the 'right thing' to do and socially responsible. Conversely, not vaccinating one's child may be perceived as irresponsible and evidence of bad parenting.Reference footnote 20Reference footnote 21
| Health belief constructs | Strongly agree % (95% CI) |
Somewhat agree % (95% CI) |
Somewhat disagree % (95% CI) |
Strongly disagree % (95% CI) |
n | |
|---|---|---|---|---|---|---|
| Perceived threats | Unvaccinated children are at higher risk of getting some serious diseases. | 63.5 (61.4-65.5) | 23.2 (21.5-25.0) | 7.3 (6.1-8.4) | 6.0 (4.9-7.2) | 6,286 |
| Delaying child vaccines causes risks to their health. | 37.0 (35.0-39.0) | 31.5 (29.5-33.6) | 19.8 (18.1-21.5) | 11.7 (10.2-13.2) | 6,093 | |
| Perceived benefits (presence/absence) | In general, childhood vaccines are effective. | 71.1 (69.1-73.1) | 25.4 (23.6-27.1) | 2.6 (1.9-3.3) | 1.0 (0.6-1.4) | 6,359 |
| In general, vaccines help to protect my child's health. | 78.1 (76.4-79.8) | 18.6 (17.1-20.1) | 2.4 (1.7-3.0) | 1.0 (0.6-1.3) | 6,410 | |
| Having my child vaccinated helps to protect the health of others in my family. | 76.1 (74.3-78.0) | 18.1 (16.6-19.6) | 3.7 (2.9-4.4) | 2.0 (1.5-2.6) | 6,377 | |
| Having my child vaccinated helps to protect the health of others in my community. | 78.0 (76.2-79.7) | 17.5 (16.0-18.9) | 3.0 (2.3-3.7) | 1.6 (1.1-2.1) | 6,380 | |
| In general, the use of alternative practices, such as homeopathy or chiropractic, can eliminate the need for vaccination. | 3.7 (2.8-4.6) | 9.5 (8.2-10.9) | 23.9 (22.0-25.8) | 62.9 (60.0-65.8) | 5,916 | |
| In general, a healthy lifestyle such as healthy nutrition and hygiene can replace the need for vaccination. | 6.5 (5.3-7.8) | 10.9 (9.3-12.5) | 21.4 (19.8-22.9) | 61.2 (58.4-63.9) | 6,324 | |
| It is better for children to develop their immunity from natural infections rather than from vaccines. | 10.2 (8.4-12.1) | 20.6 (18.8-22.5) | 28.3 (26.5-30.1) | 40.9 (38.2-43.6) | 6,150 | |
| Perceived barriers (presence/absence) | In general, I am concerned about the potential side effects from vaccines. | 20.1 (18.3-21.8) | 32.2 (30.4-34.1) | 24.4 (22.7-26.1) | 23.3 (21.7-25.0) | 6,376 |
| In general, a vaccine can give you a serious case of the very same disease it was meant to prevent. | 8.2 (6.8-9.7) | 17.0 (15.3-18.6) | 30.5 (28.7-32.3) | 44.3 (42.0-46.6) | 5,972 | |
| Children receive too many vaccines at the same visit. | 12.5 (11.1-13.8) | 22.9 (21.3-24.5) | 31.8 (29.9-33.7) | 32.9 (31.0-34.7) | 6,232 | |
| Children receive too many vaccines overall. | 9.1 (7.7-10.5) | 13.2 (11.7-14.6) | 29.9 (28.1-31.7) | 47.8 (45.6-50.0) | 6,233 | |
| In general, childhood vaccines are safe. | 66.6 (64.7-68.6) | 27.8 (26.1-29.5) | 3.5 (2.7-4.3) | 2.1 (1.4-2.8) | 6,402 | |
| Cue to action | Most parents in my community have their children vaccinated with all recommended vaccines. | 53.3 (50.9-55.7) | 40.3 (37.7-43.0) | 4.7 (3.9-5.6) | 1.6 (1.0-2.2) | 5,426 |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
||||||
Sources of information on vaccination
In the last KAB section, parents were asked to what extent they trust the 10 different sources of information on vaccination. The source of information most trusted by parents was their medical doctors (really trusted by 43% and trusted by 39%). Most of the parents somewhat trust the information on vaccination provided from alternative health providers, family and friends (49%, 44% and 50%, respectively). For the other sources of information, such as nurses, pharmacists, local public health clinics or CLSC, etc., most of respondents selected the category "Trust" (Table 6.1).
| Response | Really trust % (95% CI) |
Trust % (95% CI) |
Somewhat trust % (95% CI) |
Do not trust at all % (95% CI) |
n |
|---|---|---|---|---|---|
| Medical doctors | 43.4 (41.0-45.8) | 38.9 (36.9-40.8) | 15.6 (14.1-17.0) | 2.2 (1.5-2.9) | 6,390 |
| Nurses | 36.2 (33.5-38.8) | 39.9 (38.0-41.8) | 20.9 (19.1-22.6) | 3.1 (2.1-4.0) | 6,384 |
| Pharmacists | 29.3 (26.8-31.8) | 40.0 (38.2-41.8) | 25.8 (23.8-27.9) | 4.8 (3.8-5.8) | 6,347 |
| Alternative health providers | 4.2 (3.3-5.1) | 19.8 (18.1-21.4) | 48.5 (46.1-50.8) | 27.5 (25.7-29.3) | 6,052 |
| Family | 9.7 (8.6-10.9) | 25.1 (23.4-26.8) | 44.3 (41.9-46.6) | 20.9 (19.2-22.5) | 6,307 |
| Friends | 3.2 (2.6-3.8) | 20.2 (18.6-21.8) | 50.3 (48.2-52.4) | 26.3 (24.2-28.4) | 6,308 |
| Medical associations such as the Canadian Paediatric Society | 34.5 (31.7-37.2) | 41.2 (38.8-43.6) | 21.1 (19.5-22.7) | 3.3 (2.4-4.1) | 6,194 |
| Local public health clinics or CLSC | 32.2 (29.8-34.5) | 43.5 (41.6-45.4) | 20.9 (19.2-22.6) | 3.4 (2.6-4.2) | 6,290 |
| The Ministry of Health of my province or territory | 30.9 (28.7-33.1) | 44.1 (42.0-46.1) | 21.0 (19.5-22.6) | 4.0 (3.2-4.9) | 6,205 |
| The Public Health Agency of Canada and Health Canada | 35.9 (33.6-38.2) | 44.1 (42.0-46.2) | 17.7 (16.3-19.2) | 2.3 (1.6-2.9) | 6,269 |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|||||
Finally, parents were asked where they seek information on vaccination for their child. The most commonly reported sources of information on vaccination were medical doctors (81%), local public health clinics or CLSC (54%) and nurses (50%) (Table 6.2).
| Response (n = 6,386) | % (95% CI) |
|---|---|
| Medical doctors | 81.4 (79.9-82.9) |
| Local public health clinics or CLSC | 53.5 (51.7-55.4) |
| Nurses | 50.1 (48.1-52.0) |
| The Public Health Agency of Canada and Health Canada | 40.2 (38.1-42.3) |
| Medical associations such as the Canadian Paediatric Society | 35.3 (33.2-37.3) |
| The Ministry of Health of my province or territory | 35.1 (33.1-37.1) |
| Family | 25.1 (23.4-26.8) |
| Pharmacists | 23.4 (21.8-25.0) |
| Friends | 19.2 (17.8-20.7) |
| Social media | 10.7 (9.4-12.0) |
| Alternative health providers | 8.4 (7.3-9.5) |
| I do not seek information on immunization | 2.2 (1.6-2.7) |
| Other | 8.2 (7.1-9.2) |
n = number of respondents (unweighted) excluding those who did not provide a valid answer. |
|
Discussion
This report presents findings from cNICS regarding knowledge, attitudes and beliefs towards childhood vaccination and the prevalence of vaccine hesitancy in a large and representative sample of Canadian parents of children aged two years. The results indicated that 17% of Canadian parents of two-year-old children are hesitant to vaccinate their children. In France, a 2016 study reported a higher prevalence of vaccine hesitancy among parents of 0 to 9 years old children with 43% considered as vaccine-hesitant according to the SAGE group's definition.Reference footnote 22 Similarly, in a 2014 Quebec cross-sectional survey on vaccination against seasonal influenza and pneumococcal infections, which also included analysis pertaining to parents' KAB about vaccination, 21% of parents of children aged 2 months to 17 years of age were hesitant to vaccinate their child but eventually accepted the vaccines.Reference footnote 23 A vaccine hesitancy prevalence of 32% was also observed by another large population-based survey in Quebec in 2019.Reference footnote 24 Vaccines most commonly mentioned were influenza vaccine, varicella, human papilloma virus (HPV) and rotavirus.Reference footnote 24 However, owing to differences in survey methodology and analysis, these estimates of vaccine hesitancy prevalence are not comparable to the 24% of vaccine-hesitant parents observed in Quebec in the 2017 cNICS survey (Table 4.2).
Over one in ten parents (13%) had decided to delay at least one recommended vaccine, while 6% refused at least one vaccine other than influenza for their child. The proportions found in this survey are nearly half of those found in data collected in the 2011 National Immunization Survey (NIS) for children between 19 and 35 months of age in the United States, where 27% of parents had delayed and 15% had refused recommended vaccines (including the seasonal influenza vaccine).Reference footnote 25 Parents who refused and delayed vaccination were more likely to report that reasons for their decision included concerns about vaccine effectiveness and side effects, or because they heard or read negative things about vaccines in the media.Reference footnote 25Reference footnote 26
This iteration of the cNICS found that the reasons for being reluctant to vaccinate were very similar to the reasons of parents who decided not to vaccinate their child at all.Reference footnote 1 The most commonly reported reason for not vaccinating or being reluctant to vaccinate was a concern about the risk of side effects of vaccinesReference footnote 1, However, the questions asked in cNICS did not distinguish whether the respondents were concerned about local reactions (e.g. swelling, redness), possible rare side effects (e.g. seizure, severe allergic reaction, and intussusception), or unfounded myths or false information such as vaccines causing autism and sudden infant death syndrome (SIDS). Similar results about the source of vaccine hesitancy were demonstrated in the 2014 Quebec survey where the main reasons for being hesitant were fears of side effects and low perceptions of vulnerability to and severity of the diseases.Reference footnote 23
In cNICS 2017, the results showed that advice from a doctor or health care professional was the most common reason for parents to decide to have their child vaccinated despite their own initial reluctance. This suggests that promotional messaging for childhood vaccination from physicians and health care providers remains an important strategy to increase vaccine uptake. Though in the 2014 Quebec survey, the desire to protect one's child against diseases and feelings of social pressure were the reasons most frequently reported for the ultimate decision to vaccinate.Reference footnote 23
The majority of parents acknowledged the threat of not vaccinating their child, which might encourage vaccine uptake with respect to the psychosocial domains of the Health Belief Model. However, about one third of parents did not recognize the potential harm of delaying vaccines for their child. More effective messaging in vaccine promotion is needed to emphasize the importance of getting children vaccinated on-time, since younger children are often at increased risk for illness and death related to infectious diseases. Delaying vaccines may leave them unprotected at ages with a high risk of contracting several VPDs.Reference footnote 27 Despite the fact that more than half of respondents were concerned about the potential side effects from vaccines, in general, a higher proportion of parents agreed with statements about the perceived benefits rather than the perceived barriers for childhood vaccination. Although a minority perceived no benefits from vaccination, more than one third of respondents believed in the myth that immunity from natural infections is "better" than immunity from vaccines. In reality, vaccines use harmless attenuated or inactivated virus or bacteria to trigger the body's natural immune response and provide long-term protection against a disease, without the risk of getting the disease.Reference footnote 28 Recent research suggests that natural measles virus infections may lead to long-term immune response impairment, whereas vaccination with live measles vaccines do not elicit such an outcome.Reference footnote 29Reference footnote 30 Ongoing efforts to maintain and improve vaccination coverage needs to target those with vaccine safety concerns and educate individuals about the benefits of vaccination.
Strengths and limitations
As with any large scale survey, the 2017 cNICS has several strengths and limitations that must be considered when interpreting the results of the survey.
The major strength of the survey was the sufficiently large sample size. cNICS used random sampling from a comprehensive sampling frame (the list of CCB) which is believed to include 96% of Canadian children. Furthermore, Statistics Canada has applied sound calibration of weight to ensure the estimates are representative of all Canadian children. This allows a representative sample to be collected on a national and provincial/territorial level and analysis of under-vaccinated populations.
There are some limitations with the study that need to be acknowledged. First, the total response rate of cNICS 2017 for two-year-old children was 62%, with 38% of parents contacted refusing to participate. The possibility of non-response bias should be taken into consideration. However, the response rate was higher than those of comparable surveys carried out by Institut National de Santé Publique du Québec (INSPQ) and Santé publique France (the French national public health agency), at 50% and 52% respectively.Reference footnote 22Reference footnote 31 Nevertheless, as with any survey, the results were subject to sampling error and risks of non-response bias. To mitigate them, rigorous quality assurance mechanisms were applied across all steps of the statistical process.
Moreover, the survey was designed primarily to measure vaccine coverage and the methodology used may not be ideal for measuring vaccine hesitancy. The targeted respondents were those most knowledgeable of the child's vaccination information, who may or may not be the one making decisions about vaccination. To mitigate this, we included in the analysis only those who were most likely to make decisions regarding their child's vaccination, which included biological parents, adoptive parents and step-parents. In addition, since only one parent was interviewed, it is important to consider that the parents of a child may hold different views about vaccination. The vaccination or non-vaccination of a child may therefore result from a compromise between the parents, or from one parent acting against the will of the other. In such cases, assuming a child's partial, refused, or delayed vaccination as a surrogate of parental hesitancy may be inaccurate.
Sometimes, in order to capture all possible answers for a particular question in the survey, the answer categories could be less specific. For example, for parents who stated their child had health issues as the reason for delaying vaccination, it would be difficult to determine if the health problems were important enough to delay the vaccination and for how long they had delayed the vaccination.
cNICS also shares the usual limitations of surveys based on self-reporting which may be subject to recall bias that can drive the true rate of vaccine hesitancy in either direction, or to social desirability bias, which may lead to an under-estimation of vaccine hesitancy rates.
Similar to many other Statistics Canada surveys, cNICS excluded First Nations on-reserve communities and institutionalized children, and interviews were conducted in English or French, excluding children with parents that are not fluent in either official language. Furthermore, children in the child welfare system were not included on the CCB frame, since foster parents cannot claim the CCB for the children under their care. Instead, the government pays the children's special allowances directly to the foster parents, which are the same amount as the CCB. These populations may have differences in KAB regarding vaccination and access or utilization of healthcare services from that of other Canadian children.
In addition, some changes have been made to the design and methodology for cNICS 2017 in order to better measure parents' knowledge, attitudes and beliefs regarding vaccination. In previous iterations of cNICS (2011-2015), respondents of children never vaccinated were not asked any KAB related questions. The exclusion of those parents most adverse to vaccination biased the results on KAB towards vaccination. Therefore, results of the KAB questions from cNICS 2017 are relatively more representative, but they cannot be compared directly with the results from previous iterations of cNICS conducted between 2011 and 2015.
Conclusion
The prevalence of vaccine hesitancy among Canadian parents estimated from the 2017 cNICS was 17%. Significant regional variations in the prevalence of vaccine hesitancy were observed (14% to 24%). The main reason cited for being hesitant to vaccinate their child was concern about the risk of side effects of vaccines. Although most of the parents agreed that childhood vaccines are effective and help to protect the health of their child and others in the family and community, one quarter of respondents falsely believed that a vaccine can give a serious case of the very same disease it was meant to prevent, and one third mistakenly thought that it is better for children to develop their immunity from natural infections rather than from vaccines. The advice from doctors or health care professionals was the main trigger for parents to have their child vaccinated despite initial reluctance. Nurses were also main trusted sources of information on childhood vaccination. Thus, primary health care providers play a key role in driving vaccine acceptance, dispelling the vaccine-related myths and encouraging vaccination uptake.
Further research is needed to better understand why and how these beliefs are formed and the impact they have on parental decisions regarding vaccination. A better understanding of the scope of vaccine hesitancy and the negative perceptions about vaccines and their origins will guide interventions that can more effectively address vaccine hesitancy within Canada.
Acknowledgements
The Public Health Agency of Canada (PHAC) is grateful to all the individuals who contributed to the development of this report, including the following.
Re-design of the knowledge, attitude, and belief component of the cNICS 2017 questionnaire
Heidi Larson (London School of Hygiene and Tropical Medicine), Eve Dubé (Université Laval), Noni MacDonald (Dalhousie University), Richard Carpiano (University of British Columbia), Saad Omer (Emory University) and Glen Nowak (University of Georgia)
Lyne Cantin, Nicolas Gilbert (PHAC)
Michele Hardy, Serge Legault, John Hoover (Statistics Canada)
Coordination of data collection
Isabelle Lévesque, Jackie Kokaua, Cindy Bennett, Camélia St-Denis (Statistics Canada)
Data Analysis
Ruoke Chen, Christopher Bell, Eugénie Samson (PHAC)
Report Writing
Ruoke Chen, Nicolas Gilbert
Review
Eve Dubé (Institut national de santé publique du Québec), Holly Witteman and Hina Hakim (Université Laval)
Christopher Bell, Martine Dubuc, Julie Wiens, Shainoor Ismail, Kendra Hardy (PHAC)
Isabelle Lévesque, Jackie Kokaua, Camélia St-Denis, Carole Morin (Statistics Canada)
