Recommended use of palivizumab to reduce complications of respiratory syncytial virus infection in infants
Download the alternative format
(PDF format, 1.4 MB, 151 pages)
Organization: Public Health Agency of Canada
Published: June 1, 2022
Published: June 1, 2022
On this page
- Preamble
- Summary of information contained in this NACI statement
- Introduction
- Methods
- Epidemiology
- Product
- Economics
- Ethics, equity, feasibility and acceptability considerations
- Recommendations
- Research priorities
- Surveillance issues
- Abbreviations
- Acknowledgements
- Appendix A: Current criteria for receipt of Palivizumab in Canadian provinces and territories and internationally
- Appendix B: Palivizumab safety
- Appendix C: Palivizumab effectiveness: additional data table
- References
Preamble
The National Advisory Committee on Immunization (NACI) provides the Public Health Agency of Canada (PHAC) with ongoing and timely medical, scientific, and public health advice relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the systematic consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be systematically considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Not all NACI Statements will require in-depth analyses of all programmatic factors. While systematic consideration of programmatic factors will be conducted using evidence-informed tools to identify distinct issues that could impact decision-making for recommendation development, only distinct issues identified as being specific to the vaccine or vaccine-preventable disease will be included.
PHAC acknowledges that the advice and recommendations set out in this statement are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC's Policy on Conflict of Interest, including yearly declaration of potential conflict of interest.
Summary of information contained in this NACI statement
The following highlights key information for immunization providers. Please refer to the remainder of the Statement for details.
1. What
-
Respiratory syncytial virus disease
Respiratory syncytial virus (RSV) causes yearly outbreaks of respiratory tract disease, in Canada from late fall to early spring. It is the most common cause of lower respiratory tract illness in young children worldwide. While many infections are simple colds, children less than 2 years of age are at risk of severe disease such as bronchiolitis or pneumonia and may be hospitalized. Underlying health conditions, especially premature birth, chronic lung disease and congenital heart disease (CHD) redispose to severe RSV illness. Reinfections occur throughout life as infection produces only partial and temporary immunity, although reinfections are usually milder than the initial one.
-
Palivizumab
At present there is no vaccine available to prevent RSV. The only means of prophylaxis against RSV disease is temporary passive protection with the monoclonal antibody preparation Palivizumab (SynagisTM). Palivizumab (PVZ) has only been studied in children less than 2 years of age with underlying health conditions. Efficacy in early studies was 38-78% in different patient groups, and further studies, mainly observational, showed wide variation in effect with some studies showing no benefit. PVZ has been used for over 2 decades in many countries and has a good safety record, with very rare cases of anaphylaxis being the major serious adverse event (SAE) It is an expensive product, with wide ranging estimates of cost-effectiveness (or value for money). Estimated incremental effectiveness ratios (ICERs) ranged from less than $1,000 per quality-adjusted life year (ALY) to over 2 million dollars per QALY in various scenarios. In various high risk groups, 64% to 100% of estimates were < $50,000 per QALY. In rare scenarios it may be dominant (i.e. less costly and more effective). RSV vaccines are currently under study.
2. Who
NACI makes the following recommendations for public health program level decision-making:
- PVZ should be offered to premature infants of < 30 weeks gestational age (wGA) and < 6 months of age at onset of or during the RSV season; children aged < 24 months with chronic lung disease of prematurity who require ongoing oxygen therapy within the 6 months preceding or during the RSV season; infants aged < 12 months with haemodynamically significant CHD and infants born at < 36 wGA and age < 6 months old living in remote northern Inuit communities who would require air transport for hospitalization. For children with both CHD and chronic lung disease, recommendations for chronic lung disease should be followed.
- PVZ may be considered for premature infants of 30-32 wGA and age <3 months who are at high risk for exposure to RSV; selected children <24 months of age with severe chronic lung disease due to cystic fibrosis or other etiology who require ongoing oxygen therapy or assisted ventilation in the 6 months preceding or during the RSV season; infants <12 months of age with haemodynamically significant chronic cardiopathy other than congenital; children aged 12-24 months awaiting heart transplant or having received a heart transplant within 6 months of onset of the RSV season; and children aged <24 months with severe immunodeficiency. It may also be considered for term infants aged <6 months living in remote Inuit communities with very high rates of hospitalization for RSV among term infants and for infants of < 36 weeks gestational age and age <6 months living in other remote communities with high rates of hospitalization for RSV and where air transport would be required for hospitalization. PVZ may be considered when all other measures to control a RSV outbreak in a NICU have failed.
- PVZ should not be offered to otherwise healthy infants born at or after 33 wGA; or to siblings in multiple births who do not otherwise qualify for prophylaxis. It should not be offered routinely for children <24 months of age with cystic fibrosis; for children <24 months of age with Down syndrome without other criteria for PVZ; or for healthy term infants living in remote northern Inuit communities, unless hospitalization rates for RSV are very high. It should not be used for the prevention of recurrent wheezing or asthma in the absence of other indications.
- PVZ should not be given to prevent hospital-associated RSV infection in eligible children who remain in hospital. It may be considered when all other measures have failed to control an RSV outbreak in a neonatal intensive care unit.
Since in Canada PVZ is not readily available for purchase, no specific recommendations are made for individual-level decision making.
3. How
- The dose of PVZ is 15 mg/kg by intramuscular injection, starting with the onset of the local RSV season. Eligible children who are in hospital should receive their first dose on discharge (or within 48-72 hr before discharge to facilitate vial sharing). The interval between the first and second doses should be 21-28 days and between subsequent doses 28-35 days, for a maximum of 4 doses.
- An extra dose should be given after cardiac bypass or extracorporeal membrane oxygenation. An extra dose may be considered in remote Northern areas where RSV outbreaks may continue longer than is usual elsewhere.
- PVZ should be discontinued for the season if a child is hospitalized for RSV infection.
- If feasible, clinics or appointments should be organized to facilitate vial sharing, to reduce costs.
- PVZ is contraindicated in individuals with known significant hypersensitivity reaction to PVZ or any component of the product (humanized monoclonal antibody, glycine, histidine). Moderate to severe illness, with or without fever, is a reason to consider deferring PVZ, to avoid superimposing adverse effects from PVZ on the underlying illness, or mistakenly identifying a manifestation of the underlying illness as a complication of PVZ. The decision to delay PVZ depends on the severity and etiology of the underlying disease. Minor illnesses such as the common cold, with or without fever, are not contraindications to use of PVZ.
- PVZ contains antibody only against RSV and may be co-administered with any other live or inactivated vaccines.
4. Why
PVZ is recommended for infants and young children with health conditions that make them more vulnerable to severe RSV disease requiring hospitalization and possibly admission to an intensive care unit and mechanical ventilation.
Although the risk of severe RSV disease is reduced, PVZ does not prevent all hospitalizations for RSV. It is thought to prevent 40 to 80% of hospitalizations, depending on age and underlying health condition. Therefore other means of protection against RSV (limiting exposure of high risk children to persons with cough and colds, appropriate hand hygiene, preventing exposure to cigarette smoke) are important.
Although any young child may be hospitalized with RSV, most will not have severe illness. PVZ is not recommended for children at lower risk of severe disease, in some instances because of cost, in others because of lack of information about whether it will work.
Introduction
Respiratory syncytial virus (RSV) is the most common cause of lower respiratory tract illness in young children worldwideFootnote 1 Footnote 2.
At present the only immunizing agent available for the prevention of serious RSV disease is PVZ, a monoclonal anti-RSV antibody. Several active vaccine candidates are currently undergoing clinical trials in infants, pregnant women and adultsFootnote 3. RSV vaccines will not be addressed in this Statement.
In June 2002, Health Canada approved PVZ (SynagisTM) for the prevention of serious lower respiratory tract disease caused by RSV in infants at high risk of serious RSV disease. In 2003, the National Advisory Committee on Immunization (NACI) published recommendations on the use of PVZ or the prevention of RSV diseaseFootnote 4. At that time, NACI recommended PVZ be used during the RSV season for premature infants (less than or equal to 32 weeks' gestational age (wGA) who would be less than six months of chronological age at the start of RSV season, children less than 24 months of age with chronic lung disease of prematurity (CLD) requiring oxygen and/or medical therapy in the previous six months or other pulmonary disorders requiring oxygen therapy, and children less than 24 months of age with hemodynamically significant congenital heart disease (hsCHD). PVZ prophylaxis could also be considered for children born at less than 35 wGA who are less than 6 months of age at the start of RSV season and who live in remote northern communitiesFootnote 4. Since the 2003 statement, NACI recommendations have been modified in the Canadian Immunization Guide (CIG) but no new Statement has been issued. From 2013, in addition to the above recommendations, the CIG stated that PVZ prophylaxis may benefit selected infants between 33 and 35 wGA who are less than 6 months of age at the start of the RSV season and may be considered for infants in this gestational age group who live in rural or remote communities according to an assessment of access to medical care (e.g., requirement for air transportation to hospital facilities) and other factors known to increase risk. In addition, PVZ prophylaxis should be considered for all Inuit children in northern remote communities who are younger than 6 months of age at the start of RSV season, regardless of wGA.
Since the publication of the NACI statement in 2003, there have been a series of updated PVZ guidance documents published by expert committees including the American Academy of Pediatrics (AAP) in 2009 and 2014Footnote 5 Footnote 6 Footnote 7 and the Canadian Paediatric Society (CPS) in 2015Footnote 8 which have made PVZ prophylaxis recommendations that differ significantly from the 2003 NACI guidance and highlight the need to reassess NACI’s recommendations. A summary of current criteria for PVZ eligibility in Canadian provinces and territories and in ten other northern hemisphere countries, “Recommendations for use of Palivizumab in Canada and internationally”, is presented in Appendix A.
The purpose of this document is to update previous NACI recommendations for the use of PVZ, taking into consideration recent data on burden of illness due to RSV disease, the efficacy and effectiveness of PVZ in infants at risk of more severe RSV disease and economic implications of PVZ use.
Guidance Objective:
The objective of this advisory committee statement is to review evidence and develop guidance on strategies to prevent severe consequences of RSV infection in children at high risk of severe RSV disease by administration of monoclonal antibody.
Methods
NACI's recommendation development process is described in detail elsewhereFootnote 9 .
In brief, the broad stages in the preparation of this NACI advisory committee statement included:
- Knowledge synthesis
- Synthesis of the body of evidence of benefits and harms, considering the quality of the synthesized evidence and magnitude and certainty of effects observed across the studies
- Translation of evidence into recommendations.
Further information on NACI's evidence-based methods is available in: Evidence-Based Recommendations for Immunization: Methods of the NACI, January 2009, CCDR.
To meet the objective of this Statement, three systematic literature reviews were carried out using standard NACI methodology:
-
The burden of RSV disease in young children in high-income countries comparable to Canada
An initial search of the literature from 2000 to February 2017 retrieved 2389 records. Because of the large number of records, further assessment was limited to systematic reviews of which 6, with ratings of 6 to 7 (average) using A Measurement Tool to Assess Systematic Reviews (AMSTAR)Footnote 10, were retained; there were none with higher ratings. These reviews included literature from 1995 to 2015.
A second search of the literature from 2014 to September 2018 yielded 1022 records, of which 29 were retained for final quality assessment and data extraction. The start date was chosen to provide data from the time of the 2014 AAP change in recommendation for PVZ use. Two reviewers independently assessed the risk of bias (ROB) for each study, using a modified tool based on the Quality Assessment Tool for Observational Cohort and Cross-sectional Studies and the Quality in Prognosis Studies (QUIPS). For within-study comparisons, two reviewers independently assessed the certainty of evidence for each outcome (as high, moderate, low, or very low), using the principles of Grading of Recommendations Assessment, Development and Evaluation (GRADE). Disagreements were resolved through consensus. Details of methodology and results of this search are presented in the manuscript by Wingert et al 2021Footnote 11 and summarized in Sections III.1 and III.2 of this Statement.
A third search, using the same strategy, of literature from September 1, 2018 to July 29, 2020 identified an additional 699 records, with 14 retained for quality assessment and data extraction.
Because search of the more recent literature did not provide data on some issues for which recommendations were needed, relevant earlier references identified in the systematic reviews or in the papers accepted from the 2014-2018 search were assessed. Fifteen studies were retained for quality assessment. Information from these studies and from the 2018-2020 search are presented in Section III.1 and III.2 of this document.
-
The effectiveness of PVZ prophylaxis on reducing the complications associated with RSV in infants
For details of methodology and results in the document “NACI Literature Review on the Effects of PVZ Prophylaxis on Reducing the Complications Associated with Respiratory Syncytial Virus in Infants” which will be forthcoming. Data are summarized in Section IV.2 of this StatementFootnote 12.
-
The cost-effectiveness of PVZ prophylaxis for RSV
For details of methodology and results see “Cost-Effectiveness of PVZ Prophylaxis for Respiratory Syncytial Virus (RSV): A Systematic Review.” Data are summarized in Section V.1 of this Statement.
In addition to these systematic reviews, other literature searches included:
- An environmental scan of recommendations for use of PVZ in Canadian provinces and territories and in other Northern hemisphere countries
- A rapid literature review on the safety of PVZ
- Informal literature reviews when information was needed to address specific questions.
Results of (4) and (5) are added to this document as Appendices A and B. Information and data from the informal reviews (6) are presented in the text of this document.
In order to develop comprehensive, appropriate immunization program recommendations, NACI considers a number of factors. In addition to critically appraising evidence on burden of disease and vaccine characteristics such as safety, efficacy, immunogenicity and effectiveness, NACI uses a published, peer-reviewed framework and evidence-informed tools to ensure that issues related to ethics, equity, feasibility, and acceptability (EEFA) are systematically assessed and integrated into its guidanceFootnote 13. The NACI Secretariat applied this framework with accompanying evidence-informed tools (Ethics Integrated Filters, Equity Matrix, Feasibility Matrix, Acceptability Matrix) to systematically consider these programmatic factors for the development of clear, comprehensive, appropriate recommendations for timely, transparent decision-making. For details on the development and application of NACI’s EEFA Framework and evidence-informed tools (including the Ethics Integrated Filters, Equity Matrix, Feasibility Matrix, and Acceptability Matrix), please see https://doi.org/10.1016/j.vaccine.2020.05.051.
For this Statement, NACI reviewed the key questions for the systematic literature reviews as proposed by the RSV Working Group. Following literature searches and critical appraisal of individual studies, proposed recommendations for PVZ use were developed. The RSV Working Group chair and PHAC medical specialist presented the evidence and proposed recommendations to NACI on February 5, 2020. Following thorough review of the evidence and consultation at the NACI meetings of February 5, 2020, September 24, 2020 and October 22, 2021, the committee voted on specific recommendations. The description of relevant considerations, rationale for specific decisions, and knowledge gaps are described in the text.
Epidemiology
RSV is an enveloped RNA virus belong to the family Paramyxoviridae. There are 2 subgroups based on differences in the G surface protein, and numerous genotypes within these subgroups. Humans are the only source of infection and transmission occurs from direct or indirect exposure to respiratory secretions containing the virusFootnote 14.
RSV infects almost all infants by 2 years of ageFootnote 1 Footnote 2. The most common clinical presentations of RSV in young children requiring hospitalization are bronchiolitis (an acute lower respiratory tract infection associated with tachypnea, cough, and wheezing), and pneumoniaFootnote 14 Footnote 15. Primary infection does not confer complete protective immunity. Reinfections occur throughout life but are usually less severe, mainly presenting as upper respiratory tract illness in older children and adultsFootnote 14.
Hospitalization rates are highest in children < 1 year of age and especially in the first 2 months of lifeFootnote 16. Hospitalization rates per 1000 children per year in high income countries are reported as 26.3 (95% CI 22.8, 30.2), 11.3 (95% CI 6.1, 20.9) and 1.4 (95% CI 0.9, 2.0) for age groups 0-5 months, 6-11 months and 12-59 months respectivelyFootnote 2. In Canada, similar rates of 20, 10.2, and 4.8 per 1000 per year are reported for children aged < 6 monthsFootnote 15, <1year, and 1-3 years, respectivelyFootnote 17. In Ontario, 9% of annual hospital admissions of children <1 year of age were attributed to RSVFootnote 17. The case-fatality rate in high income countries is usually <0.5%, with higher rates in infants with co-morbiditiesFootnote 1 Footnote 18. Eighty-two percent of deaths in one Canadian study were in children with underlying risk factors for severe RSV diseaseFootnote 19.
Most children less than 2 years of age hospitalized with RSV infection have no co-morbiditiesFootnote 1 Footnote 17, but higher rates and durations of hospitalization and more intensive care unit admissions have been reported in premature infants and in those with CLD or CHDFootnote 1 Footnote 8 Footnote 17. Children with other lung diseases not associated with prematurity such as cystic fibrosisFootnote 20 or with other chronic conditions including immunodeficiencyFootnote 21 Footnote 22 and children living in indigenous communities in the far northFootnote 23 may also be at increased risk of severe RSV disease. RSV is being increasingly recognized as an important cause of morbidity and mortality in the elderlyFootnote 24.
In temperate climates, RSV causes epidemics every winter. In Canada the RSV season typically begins in October or November and lasts until April or May, with most cases occurring in December through MarchFootnote 25. Studies of temporal trends in RSV hospitalization rates have shown conflicting results, likely due to differences in testing policies, sensitivity of diagnostic tests used, and criteria for hospitalizationFootnote 1. One recent US study reported decreased RSV hospitalization rates from 1997 to 2012 for all infants and for infants with CLD and high risk CHD but not for other high risk infantsFootnote 26.III.1 Burden of disease in specific high risk groups
Data from the burden of RSV illness systematic review performed for the development of this statement are summarized and integrated into the relevant sections below. In view of the small numbers of articles identified and heterogeneity in the methodology used and outcomes studied, the interpretation of the findings must be viewed with caution. Information from earlier studies and from the 2018-2020 literature review is also presented here.
III.1.1 Preterm infants without CHD or CLD
IIII.1.1.1 Hospitalization
Risk of hospitalization for RSV infection increases with lower gestational age. In a prospective population-based study of young children hospitalized with laboratory confirmed RSV lower respiratory tract disease from 2000-2005, Hall et al. reported RSV hospitalization (RSVH) rates per 1000 infants < 24 months of age of 19.3, 18.7, 6.3, 6.9, and 5.3 for gestational ages of <29, 29-31, 32-34,≥ 35 weeks and term infants respectively. In their study, 38% of the infants had other high risk conditions and 20% received PVZFootnote 16.
The systematic literature review on the burden of RSV disease in young children (BODsr), limited to publications from 2014 to September 2018, and the 2020 updated review yielded no studies of burden of RSV illness in premature infants of <29 wGA. Data from studies of less premature infants are summarized here.
In study-level comparisons, one study of moderate to low certainty of evidence (COE) found similar RSVH rates for infants of 29-32 wGA and 33-36 wGA during their first RSV season (RR 1.20, 95% CI 0.92, 1.56)Footnote 27. Another, also rated as moderate to low COE, found a relative risk of RSVH of 2.05 (95% CI 1.89, 2.22) between infants of 33-36 wGA and term infants age <24 monthsFootnote 28. Very low COE was found for RSVH in one study of infants <33 wGA compared to term infants in their first RSV season (RR 3.88, 95% CI 1.13, 13.30)Footnote 29.
Single arm pooled proportions for RSVH (Table 1) were 5.1%, 2.8%, 3.3% and 4.1 for infants of 29 to <33 wGAFootnote 27 Footnote 29 32-34 wGAFootnote 30, 32/33 to 35 wGAFootnote 27 Footnote 28 Footnote 30 Footnote 31 Footnote 32 Footnote 33 Footnote 34 Footnote 35 and 35 wGAFootnote 30 respectively. RSVH rate for healthy term infants was 1.2%. Three of four studies in this group reported RSVH during the first year of life (0.8% to 1.5%) Footnote 29 Footnote 36 Footnote 37, and one study reported RSVH to age 24 months (1.3%)Footnote 28.
| wGA | % RSVH | 95% CI | No. studies | Risk of bias |
|---|---|---|---|---|
| 29 - <33Footnote 27 Footnote 29 | 5.1 | 4.0, 6.3 | 2 | Moderate |
| 32 - 34Footnote 30 | 2.8 | 1.6, 4.0 | 1 | High |
| 32/33 – 35 Footnote 27 Footnote 28 Footnote 30 Footnote 31 Footnote 32 Footnote 33 Footnote 34 Footnote 35 | 3.3 | 2.7, 4.1 | 8 | Moderate (5), High (3) |
| 35Footnote 30 | 4.1 | 2.8, 5.4 | 1 | High |
| Healthy term Footnote 28 Footnote 29 Footnote 36 Footnote 37 | 1.2 | 1.1, 1.2 | 4 | Moderate |
Between-study comparisons using pooled data (all assessed by GRADE at very low COE due to the indirect nature of the evidence) showed RR for RSVH for premature infants versus term infants of 4.3 (95% CI 3.7, 4.8, p=0.000) for infants of 29-32 to <33 wGA and 2.8 (95% CI 2.5, 3.1, p=0.000) for infants of 32-35 wGA. Actual risk differences were 3.9% (95% CI 2.7, 5.1) and 2.1% (95% CI 1.4, 2.8) respectively.
The 2020 literature update identified two studies that reported on RSVH in otherwise healthy premature infants. In a multinational RCT assessing efficacy of nirsevimab (a new monoclonal antibody active against RSV), RSVH rates in the 150 days following administration of placebo were 4.3% and 4.0 % in infants of ≥29 to ≤32 wGA and > 32 wGA respectively (ROB low)Footnote 38. RSVH rate during RSV season was 3.4% in infants of 33-35 wGA in a 2015-2017 retrospective cohort study in Quebec by Papenburg et al. (ROB moderate)Footnote 39. In addition, a systematic review, rated by AMSTAR as average, reported on seven observational prospective studies carried out between 2000 and 2008. The pooled RSVH rate for otherwise healthy infants of 33-<35 wGA was 3.4% or 5.5 per 100 patient-seasonsFootnote 40.
Earlier literature was reviewed for data about more severely premature infants. RSVH rates for infants during their first RSV season in the placebo arm of a 1996-1997 PVZ RCT were (% and 95% CI) 10.0 (2.8, 23.7), 7.7 (3.6, 14.1), 10.1 (5.1, 17.3) and 8.2 (3.1, 17) for gestational ages of <29, 29-32, 32-35, and 33-35 weeks respectively (ROB low)Footnote 41. In a historical cohort study from the pre- PVZ era, Stevens et al. reported RSVH rates to 1 year corrected age in premature infants without CLD of 10.2%, 8.6%, 6.8%, and 4.3% for infants of ≤ 26, 27-28, >28-30 and >30-32 weeks of gestational age (wGA) respectively. For all infants of ≤ 30 wGA, RSVH rate was 8.1% (ROB moderate)Footnote 42 Boyce et al., using Tennessee Medicaid data from 1989-93, estimated RSVH rates in the first 6 months of life of 93.8, 81.8 and 79.8 per 1000 children for infants of ≤ 28, 29 to <33 and 33 to <36 wGA respectively and 44.1 per 1000 children for low risk infants (term infants without CLD or CHD or other chronic disease). Hospitalization rates in the second 6 months of life were 46.1, 50 and 34.5 per 1000 children for those of ≤ 28, 29 to <33 and 33 to 36 wGA respectively and 15 for low risk infants (ROB moderate)Footnote 43. Other observational studies, ROB lowFootnote 44 or moderate Footnote 45 Footnote 46 Footnote 47, have reported RSVH rates of 10.4%, 7.7%, 13% and 13.5% in the first year of life for infants born at <29, <28, <29 or ≤30 wGA without other co-morbidities. These early preterm infants receive little or no maternal antibody and their narrower airway passages increase their vulnerability to the effects of RSV infection.
Infants of 29-32 wGA are also at increased risk of RSVH in comparison to healthy term infants but RSVH rates are lower than those for more premature infants, at 5.7 to 9.9% in their first RSV season (ROB moderate)Footnote 45 Footnote 46. Infants of 32 or 33 to 35 wGA have reported RSVH rates of 2.8 to 6.5% in their first year of life or first RSV season (ROB moderate)Footnote 45 Footnote 48. In the study of Boyce et al., RSVH rates for premature infants in the second 6 months of life were similar to those for low risk term infants in the first 6 months (ROB moderate)Footnote 43. In another study, RSVH rates for preterm infants of 32-34 of wGA (20% of whom received PVZ), were similar to those of 1 month old term infants by 4.2 - 4.5 months of age (ROB moderate)Footnote 49.
Chronological age is an important risk factor for RSVH (ROB moderate) Footnote 16 Footnote 43 Footnote 49 with overall RSVH rates highest at age <3 monthsFootnote 16.
III.1.1.2 Length of stay for RSVH
From the BODsr, study-level comparison of length of hospital stay (LOS) was available in two studies. In one, of moderate to low COE, the mean difference in LOS between infants age <24 months of 33-36 wGA and term infants was 1.0 day (95% CI 0.88, 1.12)Footnote 28 while in the other, of very low COE, the mean difference in LOS between infants age <12 months of 29-32 wGA and 33-35 wGA was 4.0 days (95% CI 1.54, 6.46)Footnote 50.
Mean LOS from pooled single arm studies were 10 days, 7.7 days, 5.5 days, 4.5 days and 7 days, for 29 to 32 wGAFootnote 50, 29 to 34/35 wGAFootnote 50 Footnote 51, 33-34 wGAFootnote 28 Footnote 50, 32/33 to 35 wGAFootnote 28 Footnote 30 Footnote 33 and 35 wGAFootnote 50 respectively. LOS for healthy term infants was 3.5 days Footnote 28 Footnote 37 Footnote 52 Footnote 53. (Table 2)
| wGA | Mean LOS (days) | 95% CI | No. studies | Risk of bias |
|---|---|---|---|---|
| 29 - 32Footnote 50 | 10.0 | 7.7,12.3 | 1 | Moderate |
| 29-34/35Footnote 50 Footnote 51 | 7.7 | 6.1,9.2 | 2 | Moderate |
| 33 - 34Footnote 28 Footnote 50 | 5.5 | 0.6-10.4 | 2 | Moderate, Low |
| 32/33 - 35 Footnote 28 Footnote 30 Footnote 33 | 4.5 | 2.3-6.8 | 3 | Moderate (1), Low (2) |
| 35Footnote 50 | 7.0 | 4.9-9.1 | 1 | Moderate |
| Healthy termFootnote 28 Footnote 37 Footnote 52 Footnote 53 | 3.5 | 2.3,4.7 | 4 | High (1), Moderate (2), Low (1) |
Between-study comparisons (all at very low COE) using pooled data showed mean differences in LOS between premature versus term infants of 6.5 days (95% CI 3.9, 9.1, p<0.000), 1.0 days (95% CI -8.6, 10.6) and 4.2 days (95% CI -5.3, 13.7) for infants of 29-32 wGA, 32/33-35 wGA, and 29-35 wGA respectively.
The 2020 literature update identified three studies that reported this outcome. Median LOS was 7.0 days (range 2-20) in 29-<36 wGA infants (ROB low)Footnote 38 and 7.0 days (IQR 3-12) in 29-34 wGA infants (ROB moderate)Footnote 54. Anderson et al. reported median LOS of 6 (IQR 3-11), 5 (IQR 3-10) and 5 (IQR 3-8) days in infants of 29-32 wGA, 33-34 wGA and 35 wGA respectively (ROB low)Footnote 55. In addition, and for comparison, four studies reported LOS for healthy term infants. Median LOS was 4 days (range 1-23) (ROB moderate)Footnote 56 and 1.9 days (IQR 1.1-2.9) (ROB low)Footnote 57. Mean (SD) LOS was 5 (2.2) days (ROB moderate)Footnote 58 and 5.9 (2.99), 5.4 (2.89) and 5.84 (3.13) days for different RSV genotypes in a study by Midulla et al. (ROB low)Footnote 59.
In earlier literature, premature infants have also been reported to have longer median hospital stays than term infantsFootnote 60. In a prospective cohort study in 2008-9, infants of 28 to < 33 wGA with confirmed RSVH had a mean LOS of 7.2 ± 3.3 days (ROB low)Footnote 61.
III.1.1.3. ICU admission and mechanical ventilation
In the BODsr, one study looked at ICU admission, ICU LOS, mechanical ventilation (MV) and duration of MV in infants of 29-32 versus 33-35 wGA. There was no significant difference in any of these parameters (low to very low COE)Footnote 50.
Single arm pooled proportions of patients hospitalized for RSV that were admitted to ICU were 51.7, 19.1, 31.5 and 13.9 for infants of 29-32 wGAFootnote 50, 32-34 wGAFootnote 30, 32-35 wGA Footnote 30 Footnote 35 Footnote 50 and 35 wGAFootnote 30, respectively. Rate of ICU admission for hospitalized healthy term infants was 15.8% Footnote 37 Footnote 52 Footnote 53. (Table 3)
| wGA | % ICU | 95% CI | No. studies | Risk of bias |
|---|---|---|---|---|
| 29 - 32Footnote 50 | 51.7 | 41.3, 62.1 | 1 | Moderate |
| 33 - 34Footnote 30 | 19.1 | 2.3, 35.8 | 1 | Moderate |
| 32 - 35 Footnote 30 Footnote 35 Footnote 50 | 31.5 | 13.1, 53.6 | 3 | Moderate (2) Low (1) |
| 35Footnote 30 | 13.9 | 2.6, 25.2 | 1 | Moderate |
| Healthy termFootnote 37 Footnote 52 Footnote 53 | 15.8 | 5.4, 30.0 | 3 | Moderate (2), High (1) |
Between-study comparisons (all at very low COE) using pooled data showed RR for ICU admission among hospitalized premature versus term infants of 3.3 (95% CI 1.9, 5.7, p=0.000), 2.0 (95% CI 1.0, 4.0, p=0.000) and 3.3 (95% CI 1.9, 5.6, p=0.000) for infants of 29-32 wGA, 32-35 wGA, 29-35 wGA respectively. Actual risk differences were 35.9% (95% CI 19.8, 52.0, p=0.000), 15.7% (95% CI -8.0, 39.4, p=0.194) and 36.2% (95% CI 22.5, 49.9, p=0.000) respectively.
For ICU LOS, single arm pooled data showed ICU LOS of 9.0, 7.0, and 6.7 for infants of 29-32 wGAFootnote 50, 29-34/35 wGAFootnote 50 Footnote 51 and 33-35 wGAFootnote 35 Footnote 50 respectively. There were no studies showing ICU LOS stay for healthy term infants. (Table 4)
| wGA | Mean LOS (days) | 95% CI | No. studies | Risk of bias |
|---|---|---|---|---|
| 29 - 32Footnote 50 | 9.0 | 7.0, 11.0 | 1 | Moderate |
| 29 – 34/35Footnote 50 Footnote 51 | 7.0 | 4.7, 9.2 | 2 | Moderate |
| 33 - 35Footnote 35 Footnote 50 | 6.7 | 5.5, 8.0 | 2 | Moderate, Low |
Single arm pooled proportions of hospitalized patients that underwent MV were 27.0%, 22% and 14.0 for infants of 29-32 wGAFootnote 50, 29-34/35 wGAFootnote 50 Footnote 51, 32/33-35 wGA Footnote 30 Footnote 35 Footnote 50, respectively. MV rate for healthy term infants was 14.0%Footnote 52 Footnote 53. (Table 5)
| wGA | % MV | 95% CI | No. studies | Risk of bias |
|---|---|---|---|---|
| 29 - 32Footnote 50 | 27.0 | 17.8, 36.2 | 1 | Moderate |
| 29-34/35Footnote 50 Footnote 51 | 22.0 | 18.0, 26.0 | 2 | Moderate |
| 32/33 - 35Footnote 30 Footnote 35 Footnote 50 | 14.0 | 10.0, 18.0 | -3 | Moderate (2), Low |
| Healthy termFootnote 52 Footnote 53 | 14.0 | 9.0-21.0 | 2 | Moderate, High |
Between-study comparisons (all at very low COE) using pooled data showed RR for MV among hospitalized premature versus term infants of 1.9 (95% CI 1.4, 2.6, p<0.000), 2.3 (95% CI 1.8, 2.9, p<0.000) and 1.0 (95% CI 0.76, 1.32, p<-.000) for infants of 29-32 wGA, 29-35 wGA and 33-35 wGA respectively. Actual risk differences were 13.0% (2.0, 24.0, p=0.020), 18.0% (9.9, 26.1, p=0.000) and 0.00% (-7.2, 7.2, p=1.000) respectively.
Mean duration of MV from pooled single arm studies was 10 days (95% CI 7.6, 12.4), 8.6 days (95% CI 7.3, 9.8) and 6.5 days (95% CI 3.5, 9.4) for infants of 29-32 wGA (one study, ROB moderate)Footnote 50, 29-35 wGA (two studies, moderate ROB)Footnote 50 Footnote 51 and 33-35 wGA (two studies, ROB moderate, low)Footnote 35,Footnote 50 respectively. There were no studies reporting duration of MV for healthy term infants.
The 2020 literature search update identified three studies that reported on ICU admission. ICU care among infants with RSVH was 25% of infants of 29-<35 wGA (ROB low)Footnote 38, 64.2% of infants of 29-34 wGA (ROB moderate)Footnote 54 and 48%, 46% and 49% of infants of 28-32, 33-34, and 35 wGA respectively (ROB low).Footnote 55 Six studies reported on ICU care for healthy term infants. Percentages were 29%Footnote 57, 43.3%Footnote 62, 20%Footnote 63 and 9%Footnote 59 in studies of ROB low and 3.4%Footnote 56 and 2%Footnote 58 in studies of moderate ROB.
Median (IQR) ICU LOS was 6 days in infants of 29-34 wGA (ROB moderate)Footnote 54 and 6 (3-11) 5 (3-10) and 5 (3-6) days for infants of 29-32, 33-34 and 35 wGA respectively (ROB low)Footnote 55. For healthy term infants median ICU LOS was reported as 4 days (IQR 3, 7.6) (ROB low)Footnote 57 and 0 days (range 0-15) (moderate ROB)Footnote 56.
MV among infants with RSVH was 5% for infants of 29-<35 wGA (ROB low)Footnote 38, 31.8% for infants of 29-34 wGA (moderate ROB)Footnote 54, and 22%, 20% and 15% for infants of 28-32, 33-34, and 35 wGA respectively (ROB low)Footnote 55.
In earlier literature, premature infants have also been reported to have an increased risk for ICU admission compared to term infantsFootnote 60. In a prospective cohort study in 2008-9, 5.9% of infants of 28 to < 33 wGA required admission to the ICU (ROB low)Footnote 61. A later systematic review of studies from 2000-2014, rated as average by AMSTAR, of infants of 33-35 wGA without comorbidities reported that 22.2% of infants required ICU admission for a median of 8.3 days and 12.7% required MV for a median of 4.8 daysFootnote 40. Younger age is associated with higher rates of ICU admission. In a report of infants of 32-35 wGA, no infants >6 months of age required intensive care, but 14% of those aged 3 to <6 months and 27% of those aged < 3 months were admitted to ICU (actual ages)Footnote 64.
III.1.1.4. Mortality
In a meta-analysis of studies from 1990-2007, all-cause mortality during their first RSV season was 0.99% and 0.13% for infants of ≤32 wGA and 32-35 wGA respectively. RSV attributable mortality was 0.03% for the two groups combined (AMSTAR rating average)Footnote 65. In another systematic review of literature from 1975 to 2011, the weighted mean case fatality rate for children aged ≤ 24 months hospitalized with RSV was 1.2% (range, 0–8.3%; median, 0%; n = 10) for preterm infants <37 wGA versus a weighted mean of 0.2% (range 0-1.5%; median, 0.0%; n = 6) for children with no risk factors for severe RSV (AMSTAR rating poor)Footnote 66. In the BODsr, one study of very low COE reported one death attributed to RSV in infants of 29-32 wGA and no deaths in the 33-35 wGA group, not significantly differentFootnote 50.
III.1.1.5. Risk scores
While prematurity of any degree may increase risk of RSV hospitalization to some extent, providing prophylaxis for all is not feasible. In Canada 7.7-8.0% of births annually are of < 37 wGAFootnote 67 and it has been estimated that 5% of the birth cohort may be born at 32-35 wGAFootnote 34. Risk scores have been developed in attempts to identify otherwise healthy premature infants of > 29-30 wGA or > 32 wGA who are at significantly increased risk of severe RSV disease, which are currently used in several Canadian provinces and territories and internationally (see Appendix A below). The risk factors identified as significant and used in these risk scores vary widely. The validity of such scores, especially those validated with data from several years ago or from different geographical settings, has been questioned Footnote 7 Footnote 34 Footnote 68 Footnote 69 Footnote 70 Footnote 71.
Young chronological age during the RSV season is the most consistent risk factor identified. Other factors include environmental and host factors that increase risk of exposure to RSV or of more severe RSV disease. The risk of RSV hospitalization associated with these individual factors has been difficult to determine because of inconsistent results in different studies. Most environmental and host factors increase the risk for RSVH only slightly and their individual contribution to the burden of RSV disease is limitedFootnote 7 Footnote 70. In a multiple logistic-regression analyses of risk factors which included male gender, child care attendance, smoke exposure, lack of breastfeeding, and other children in the house, only preterm birth and young chronologic age independently correlated with more severe RSV disease after adjusting for other covariatesFootnote 69.
III.1.2 Chronic lung disease of prematurity and other chronic lung diseases
CLD has been defined by the AAP as "born at gestational age of <32 weeks with need for supplemental O2 for at least the first 28 days after birth"Footnote 6. Some studies defined CLD as the need for O2 at 36 weeks post conceptual age. The BODsr and the 2020 updated literature search did not identify any studies of this risk group.
In a systematic review of data to December 2015, rated average by AMSTAR, RSVH rates for children with CLD in the first 2 years of life without prophylaxis were 12-21% with a weighted mean of 16.8%. CLD was associated with a higher rate of RSVH than other high-risk groups and was a significant independent risk factor for RSVH with odds ratios of 2.2 to 7.2Footnote 72. The Canadian Paediatric Society statement reported RSVH of 6.0 to 22.6 % in studies carried out between 1995 and 2009Footnote 8.
RSVH rate of 16.8% in the first year of life was reported in a 1992-6 retrospective cohort study (ROB moderate)Footnote 42. RSVH rate was 12.8% for children ≤ 24 months of age with CLD in the control arm of a PVZ RCT (ROB moderate)Footnote 48 and 15.7 % for children within 12 months of initial discharge in the control arm of a PVZ observational study (ROB moderate)Footnote 44. A 1989-93 study reported higher rates in the first year of life than in the second (38.8% vs. 7.3%) (ROB moderate)Footnote 43. Winterstein et al. compared RSVH rates in infants with CLD and in healthy term infants with siblings. The peak RSVH rate for those with CLD was 15.3 /1000 patient-seasons at age 9 months. The RSVH rate for infants with CLD at 18.5 months was similar to that of healthy term infants aged 1 month (9/1000 patient-seasons)Footnote 73. In that study, 42.7% of the infants with CLD had received PVZ.
There are limited data on outcomes other than hospitalization. In the systematic review of Paes, rated by AMSTAR as average, the mean length of hospital stay for RSV was 4-11 days, with one study reporting 29% of those hospitalized admitted to ICU and 24% undergoing mechanical ventilationFootnote 72. In the retrospective cohort study of Stevens et al. (ROB low) the mean LOS was 9.4 days and 9.1% were admitted to ICUFootnote 42. A meta-analysis, rated by AMSTAR as average, reported an all-cause mortality rate of 0.34% during the first RSV seasonFootnote 74. In a systematic review of literature from 1975 to 2011, the weighted mean case fatality rate for infants age ≤ 24 months hospitalized with RSV was 4.1% (range, 0–10.5%; median, 7.0%; n = 6) for children with CLD (rated by AMSTAR as poor)Footnote 66.
Data on RSV risk in children with chronic lung disease of etiology other than prematurity are limited. The BODsr identified two studies. Increased rates of RSVH were reported in infants < 24 months old with congenital cystic lung disease (CCLD) (8.3%, 95% CI 0.5, 16.2)Footnote 75 (ROB moderate) and in children with chronic interstitial lung disease (chILD) receiving corticosteroids (30%, 95% CI 9.9, 50.1)Footnote 76 (ROB high). In between-study comparisons (all at very low COE), RR for RSVH in comparison to term infants Footnote 28 Footnote 29 Footnote 36 Footnote 37 (all ROB moderate) were 6.9 (95% CI 5.3, 8.9, p=0.000) for CCLD, and 25.0 (95% CI 14.3, 43.6 p=0.000) for chILD. Actual risk differences were 7.1% (95% CI 1.5, 12.7 p=0.013) for CCLD and 28.8(95% CI 8.7, 48.9, p=0.005) for chILD. Mean LOS was 11.25 days (95% CI 9.29, 13.21) for CCLD (ROB low), and 6 days (95% CI -0.6, 12.6) for chILD (ROB moderate). In between-study comparisons (very low COE), mean differences in LOS versus term infants were 7.8 days (95% CI -1.8, 17.3, p<0.112) for CCLD and 2.5 days (95% CI -4.2, 9.2 p=0.465) for chILD. None of the patients in these two studies were admitted to ICU because of RSV.
In an earlier report, Kristensen et al. reported RSVH rates for children age < 24 months with chILD (27.3%), congenital lung malformations (13.7%), other congenital airway abnormalities (8.3%, 9.3%) and some neuromuscular conditions that affect ability to clear airway secretions (9.9%-15.9%), while the overall rate in the population of this age was 2.8% (ROB moderate)Footnote 21.
III.1.3 Cystic fibrosis
The BODsr identified two studies of infants with cystic fibrosis (CF). Pooled proportion for RSVH was 12.3% (95% CI 1.3, 30.8) (ROB high)Footnote 77 Footnote 78. In between-study comparisons, RR for RSVH in comparison to term infants was 10.3 (95% CI 3.3, 31.6, p<0.000) and actual risk difference was 11.1% (95% CI -3.7, 25.9, p=0.140). One study, with a small number of admissions, reported a mean LOS of 47.00 (12.53, 81.47) (ROB moderate) much higher than in previously published studies but not commented on by the authorsFootnote 77. The other study (moderate ROB) reported a mean LOS of 10 daysFootnote 78. Due to a lack of data (standard deviation not reported by Groves et al), pooling was not conducted from these studies for this outcome.In the study of Bjornson, the proportion of the population at risk that was admitted to ICU because of RSV was 2.4% (95% CI -0.9, 5.6) (ROB moderate)Footnote 77. Of the 5 admitted to hospital, 2 were admitted to ICU (40%) and one required mechanical ventilation. Mean duration of ICU admission was 5.00 days (95% CI -2.84, 12.84) (ROB moderate)Footnote 77. The other study did not report on ICU admissionsFootnote 78.
Earlier reports also indicate that RSVH occurs more frequently in children with cystic fibrosis than in healthy children. In a systematic review rated as average by AMSTAR, rates of RSVH were 6.4-18.1%, 2.5-4.3 times higher than in healthy children. Average LOS was 2-11 days and ICU admission was reported in 12.5 % (1 of 8 hospitalized patients)Footnote 22. Another systematic review of PVZ prophylaxis in cystic fibrosis, rated as good by AMSTAR, reported RSVH rates in patients not receiving PVZ of 7.5-11.7%Footnote 20.
III.1.4 Congenital heart disease
Children with hsCHD were at high risk of RSV morbidity and mortality in the era when corrective surgery was usually delayed. As repair early in infancy became the norm, the risk of severe RSV disease is expected to have decreased although data to support this are sparse. A US study showed decreasing RSVH rates before PVZ prophylaxis was recommended for this group of patientsFootnote 79.
The BODsr identified one study of children with hsCHD. Using combined data from 1997 and 2000, RSVH incidence per 1000 births of infants with hsCHD was 23 (95% CI 20, 26) (ROB moderate)Footnote 79. Between-study comparison with RSVH rates for healthy term infants could not be made. For other reported hospitalization-related outcomes, only combined data including years after PVZ became available was presented, and therefore these outcomes were excluded from analysis.
In earlier studies, a systematic review of data from 1995 to 2015, rated as average by AMSTAR, reported RSVH rates of 3.8 to 10.2 % in children < 2 years of age with hsCHDFootnote 65. The Canadian Paediatric Society statement reported RSVH rates of 1.3 to 15% in studies carried out between 1992 and 2008Footnote 8.
RSVH rates decreases with age. Rates in the placebo arm of a 1998-2002 RCT were 9.7% for all infants (< 24 months old), 12.2% for infants < 6 months old, 7.3% for those 6 to 12 months old and 4.3% for those 1-2 years old (ROB low)Footnote 80. In observational studies, the RSV hospitalization rate in infants with hsCHD is also significantly higher in those aged <12 months than in those aged 12-24 months. In the study identified in the BODsr, reporting on RSVH in the USA from 1997 to 2012 and spanning the pre and post PVZ eras, 85% of hospitalizations occurred in the 1st year of lifeFootnote 79. Chiu et al. in Taiwan in 2005-10 reported RSVH rates of 4.8% and 2.1% with cyanotic and acyanotic hsCHD respectively in the first year of life and 0.9% and 0.56% in the second year (ROB moderate)Footnote 81. Resch reported a 9.6% hospitalization rate in 2004-08 study including children with hsCHD and non-hemodynamically significant CHD, some of whom received PVZ, with 56 of 58 infections occurring in the 1st year of lifeFootnote 82. In a study of children with CHD (not necessarily hemodynamically significant) using Medicaid data from 1989-93, estimated RSVH rate was 9.2% in the 1st year and 1.8% in the 2nd year (ROB moderate)Footnote 43.
In the systematic review of Checchia, median LOS for RSVH for children with hsCHD was 7 to 9.7 days. The proportion of hospitalised patients admitted to ICU was 30.4 - 46%, median ICU LOS was 10 days and the proportion receiving mechanical ventilation was 30%Footnote 65. In the placebo arm of the1998-2002 RCT, mean LOS was 13.3 days, 38.1% of those hospitalized were admitted to ICU for a mean of 19.2 days and 22.2% required MV for a mean of 25.3 days (ROB low)Footnote 80. In the study of Chu, children with hsCHD (with or without PVZ prophylaxis) hospitalized for RSV had longer mean hospital LOS (12.1 versus 3.4 days, p<0.001), higher rates of MV (21.9% vs 2.3%, p<0.001) and higher rates of respiratory syncytial virus-associated mortality (2.8 versus 0.1%, p<0.001) when compared with children without hsCHDFootnote 79.
Feltes et al. reported RSV-related deaths among hospitalized infants with hsCHD of 0.6% (ROB low)Footnote 80. In a meta-analysis of studies from 1990 to 2007 all-cause mortality rate in the first RSV season was 4.17% and RSV-attributable mortality was 0.62% (AMSTAR rating average)Footnote 74. In a systematic review of literature from 1975 to 2011, the weighted mean case fatality rate for infants age ≤ 24 months hospitalized with RSV was 5.2% (range, 2.0–37.0%; median, 5.9%; n = 7) for children with CHD (AMSTAR rating poor)Footnote 66.
III.1.5 Down syndrome
There is evidence that children with Down syndrome have a higher risk of RSVH than healthy children. This increase is partially explained by co-morbidities such as CHD, CLD or prematurity. Excluding children with these comorbidities, risk remains increased. Possible explanations for this include anatomic abnormalities of the upper respiratory tract, airway malacia, swallowing dysfunction, hypotonia and immune dysfunctionFootnote 83.
The BODsr did not identify any studies of children with Down syndrome that were limited to those < 2 years of age. A single observational study of moderate COE comparing RSV outcomes in children with Down syndrome and healthy children < 3 years of age was identified. For children with Down sndrome and no other risk factors for severe RSV, RSVH rate was reported to be 2%, vs 1.1% in healthy controls, but the RSVH data had some inconsistencies and could not be further assessed. The median LOS was 5 days versus 2 days for healthy controls (mean difference 3.00 days, 95% CI 1.95, 4.05) (low COE)Footnote 84.
A meta-analysis published in 2018 of studies to May 2017, rated by AMSTAR as average, reported a pooled odds ratio (OR) for RSVH in comparison with healthy controls of 8.69 (95% CI 7.33, 10.30) for all cases of Down syndrome and a pooled OR of 16.66 (95% CI 7.22, 38.46) when only studies that excluded children with other known risk factors for severe RSV were included (2 studies). Actual RSVH rates in this subgroup were 7.6 and 9.7%. Children with Down syndrome, including those with known risk factors for severe RSV, had increased LOS (pooled mean difference 4.73 days; 95% CI 2.12, 7.33), oxygen requirement (pooled OR 6.53; 95% CI 2.22, 19.19); ICU admission (pooled OR: 2.56 95% CI 1.17, 5.59) and need for mechanical ventilation (pooled OR 4.56; 95% CI 2.17, 9.58) and RSV associated mortality rate (pooled OR 9.4; 95% CI 2.26, 39.15) vs control infants without Down syndromeFootnote 83. The authors report that in the single study that included only infants with no other risk factors, there was no mortality and LOS, oxygen need, ICU admission and mechanical ventilation did not differ from those reported for the whole group. An earlier systematic review (1995-2015), rated by AMSTAR as average, reported RSVH rates of 3.6 – 13.5% in infants with Down syndrome and no other known risk factors for severe RSV. Risk ratio vs healthy infants was 3.5-10.5 and average LOS was 4-5 daysFootnote 22.
III.1.6. Immunocompromised children
RSV can cause significant morbidity and mortality in immunocompromised children. Serum and secretory antibodies are important in preventing RSV infection and T cells are required to efficiently clear the virus. There is very little population based data on the burden of RSV disease in this group. Although most infections occur in young children, immunocompromised older children and adults are also at risk of severe RSV disease and death. Morbidity varies by severity of immunocompromisedFootnote 22.
The BODsr identified two studies of immunocompromised children. A USA multicenter study in 2004-2012 reported on RSV hospitalization in liver transplant recipients <18 years of ageFootnote 85. Multivariate analyses identified age <2 years at transplant as a predictor of RSVH (p<0.001). RSVH rate in the first 2 years post- transplant (for all aged <18 years) was 5.3% (95% CI 4.4, 6.2) (ROB moderate). Between-study comparisons (all at very low COE) showed a RR for RSVH of 4.4 (95% CI 4.0, 4.9, p<0.000) versus healthy term infants. Actual risk difference was 4.1% (95% CI 3.2, 5.04, p=0.000). The proportion of hospitalized patients that were admitted to ICU was 22.2% (95% CI 15.2, 29.2) (ROB low). RR for ICU admission among those hospitalized for RSV was 1.4 (95% CI 0.8, 2.5, p=0.242, very low COE) versus healthy term infants. Actual risk difference was 6.4% (95% CI -7.8, 20.6, p=0.375; very low COE). Of those admitted to hospital, 10.4 % (95% CI 5.2, 15.5), received MV (ROB low). RR for MV amongst those admitted to hospital was 0.7 (95% CI 0.5, 1.1, p=0.156) versus healthy term infants, with actual risk difference of -3.6% (95% CI -11.5, 4.3, p=0.372, all at very low COE)Footnote 85.
The second study was of RSV infections in children less than 18 years of age with sickle cell disease. This single center retrospective study reported a RSVH rate of 63 per 1000 person-years (95% CI 44, 87) for children < 2 years of age (ROB moderate). Other outcomes (LOS, ICU admission, mechanical ventilation), were reported only for all children aged less than 18 years and did not differ significantly from those of healthy term infants age < 2 yearsFootnote 86.
An earlier systematic review, rated as average by AMSTAR, reported that most RSV infections in haematopoietic stem cell and solid organ transplant recipients occur in the first 2 years after transplant. Immunocompromised children < 2 years of age with RSVH had a median LOS of 7 and 10 days, with ICU admission occurring in 13% and 19.1% and intubation and/or mechanical ventilation in 3% and 14.3%. Overall, case fatality rates were 0% and 4.8%Footnote 22. In a Danish study of children less than 2 years old, carried out in 1997-2003, rates of first hospitalization for RSV were 21.3% in children with congenital immunodeficiencies and 8.4% in children with cancer, while the overall rate in the population of this age was 2.8%. Duration of hospitalization was not increased (ROB moderate)Footnote 21.
El Saleeby et al. reported on RSV infections in 58 individuals aged < 21 years with cancer in Tennessee between 1997 and 2005. In multivariate analysis, age ≤ 2 years and absolute lymphocyte counts of < 100/mm3 at the time of RSV infection were found to be independent predictors of the development of LRTI, with OR of 9.84 (95% CI 1.95, 49.8) and 7.17 (95% CI 1.17, 44.03) respectively. These factors were also significantly associated with deathFootnote 87. In a Seattle study of HSCT recipients, the majority of whom were adults, absolute lymphocyte count of ≤100 / mm3 at the time of symptom onset was a risk factor for RSV disease progressionFootnote 88.
III.1.7 Children residing in remote communities
The BODsr identified two studies of infants in remote communities. Data from the two studies were not pooled due to differences in study design and patient populations.
One study of infants living in Canadian northern Inuit communities, carried out in 2009, (about 20% of the birth cohort, with or without prematurity or co-morbidities) reported an overall RSVH rate of 66.9 admissions per 1000 live births per year among children <1 year of age (ROB high), with regional RSVH rates of 2.0% in the Northwest Territories, 7.5% in Nunavut, and 17.6% in Nunavik. In different areas of Nunavut rates were 19.5%, 9.1% and 3.7%Footnote 23.
The second was a study of healthy term Native American infants living on reservations in southwestern USAFootnote 89. The RSVH rate was 12.8% (95% CI 10.1, 15.5) (ROB high). In between-study comparisons (very low COE), RR for RSVH was 10.7 (95% CI 9.4, 12.1, p<0.000). Actual risk difference was 11.6% (95% CI 8.9, 14.3, p=0.000). Mean LOS was 4.7 days (95% CI 4.2, 5.2) (ROB moderate). Mean difference in LOS versus healthy term infants was 1.2 days (95% CI -0.10, 2.5), p<0.802, very low COE). The proportion of hospitalized patients that were admitted to the ICU (ROB moderate) was 6.3% (95% CI 1.0, 11.6). RR for ICU admission was 0.4 (95% CI 0.04, 1.2, p=0.091). The actual risk difference was -9.5% (95% CI -22.9, 3.9, p=0.164). Mean ICU LOS 5.2 days (95% CI 2.1, 8.3) (ROB moderate). Mechanical ventilation was required for 2.5% of hospitalized patients (95% CI 0.9, 5.9) (ROB moderate) for a mean duration of 6.5 days (95% CI 3.6, 9.4) (ROB moderate).
The 2020 literature search update did not identify any studies of populations living in remote communities. Subsequent to that search, results of a recent observational study from Nunavik, Quebec became available (ROB high)Footnote 90. RSVH rates for 2013-2019 was 5.0% for all infants < 1 year of age (7.3% after adjustment for possible under detection by rapid antigen test compared to PCR), a much lower rate than that reported in 2009Footnote 91.
Previous studies indicate that children living in remote northern Inuit communities have high rates of RSV infection. In 2002, 16.6% of Baffin Island infants less than 1 year of age were admitted to Baffin Regional Hospital for RSV (ROB moderate). Rates ranged from 6.3% for infants from Iqaluit to 34.9% for infants from high risk rural communities. For infants of less than 6 months of age, overall RSVH rate was 25% and was 51% in high risk communitiesFootnote 91. Singleton et al. reported the YK district of Alaska as having the highest rate of RSVH in the world, with 43.9% of premature infants and 14.8% of term infants < 1 year of age hospitalized annually in the pre-PVZ era (ROB high)Footnote 92. These rates are many fold higher than the overall rates of 1-2% for term infants reported in developed countries and the infected infants frequently require air transfer to community hospitals or to tertiary care institutions.
Data on the burden of RSV illness in children living in other aboriginal communities in North America is very limitedFootnote 93 and there is no information for other remote communities.
III.1.8 Other high risk infants
The BODsr and the 2020 literature search update did not identify any additional groups at risk for severe RSV disease.
III.2 RSV infection and long term sequelae: recurrent wheezing, asthma and pulmonary function
Several studies have shown RSV LRTI in early life to be associated with recurrent wheezing in childhood. Some studies suggest that post RSV recurrent wheezing is transient, with wheezing decreasing to background levels over the first decadeFootnote 94. Whether RSV in infancy predisposes to the development of asthma, or if infants genetically predisposed to develop asthma are at increased risk of severe RSV disease in infancy, is not knownFootnote 95 but there is some indirect evidence for the latter. In a prospective cohort of healthy term newborns, infants who later developed severe RSV infection and post-RSV wheezing had lower results on pulmonary function tests in the neonatal period than those that did notFootnote 36, and another study showed bronchial hyper-responsiveness in otherwise healthy term neonates who later developed severe bronchiolitisFootnote 96. Genetic factors predisposing to severe RSV have been describedFootnote 94 Footnote 95. An association between early rhinovirus infection and asthma has been reportedFootnote 95, as well as an association between asthma and the frequency of respiratory viral infections in early life rather than any specific etiologyFootnote 97. A recent World Health Organization review determined that the evidence is inconclusive in establishing a causal association between RSV lower respiratory tract infection and recurrent wheezing in childhood or asthma and that the evidence does not establish that RSV monoclonal antibody will have a substantial effect on these outcomesFootnote 98.
The BODsr identified 6 studies that assessed long term respiratory sequelae of RSV infection in infancy.
A study of children born at 32-35 wGA with or without RSVH at < 12 months of age found small increases in the proportions with parent or physician reported simple wheeze (< 3 episodes within 12 months) (RR 1.4, 95% CI 1.15, 1.60, absolute increase 18%), parent or physician reported recurrent wheezing (≥3 episodes in 12 months) (RR 1.70, 95% CI 1.27, 2.29, absolute increase 19%), or physician reported severe wheeze (≥ 1 hospitalizations or ≥3 medically-attended episodes or on medication for wheeze for 3 consecutive months or 5 cumulative months) (RR 1.59, 95% CI 1.13, 2.24, absolute increase 14%) from 2 to 6 years of age. There was little to no difference in wheezing during the sixth year, with RR 1.16 (95% CI 0.70, 1.93), RR 1.28 (95% CI 0.71, 2.32) and RR 0.91(95% CI 0.44, 1.88) for simple, recurrent and severe wheezing respectively. There was a small increase in bronchodilator use (RR 1.48, 95% CI 1.23, 1.77, absolute increase 8%), inhaled corticosteroid use (RR 1.65, 95% CI 1.13, 2.40, absolute increase 10%) and oral corticosteroid use (RR 1.71, 95% CI 1.06., 2.74, absolute increase of 8%, and a larger increase in leukotriene antagonist use (RR 2.52, 95% CI 1.43, 4.42, absolute increase 10% from 2 to 6 years of age (COE low for all outcomes)Footnote 32.
A study compared infants born at < 33 wGA versus at term for wheezing in the year following RSVH. There was no significant difference in simple, recurrent or severe wheeze between the two groups (RR 0.54, 95% CI 0.18-1.55; RR 0.80, 95% CI 0.04, 16.14; RR 0.00, 95% CI -0.34, 0.34 respectively but numbers with RSV were small) (very low COE)Footnote 29.
A study of wheezing in the first year of life in healthy term infants with RSV infection who did or did not require hospitalization found little or no difference in parent-reported days with wheeze per month between the two groups (mean difference 0.70; 95% CI -0.94, 2.34) (very low COE)Footnote 36.
Relative risk for physician diagnosed asthma at age 7 years among healthy term infants born to mothers with asthma who had RSV versus another respiratory infection in the first year of life was RR 2.33 (95% CI 1.35, 4.05, absolute increase 15%, OR 2.82, 95% CI 1.38, 5.77, p=0.005). After adjustment for the total number of respiratory infections the OR was 1.26, (95% CI 0.54, 2.91, p=0.59 (COE very low)Footnote 97.
There was no difference in physician diagnosed asthma at age 28-31 years in individuals who were born at term and did or did not have RSVH at age < 24 months (RR 1.82, 95% CI 0.84, 3.94) (COE very low). There was an increase in self-reported bronchodilator use (RR 2.17, 95% CI 1.08, 4.34) and no difference in self-reported inhaled corticosteroid use (RR 1.56 95% CI 0.62, 3.89) (COE very low)Footnote 99.
Some studies also addressed pulmonary function. There was little to no difference in the proportion of children born at 32-35 wGA with Force Expiratory Volume in one minute (FEV1) Z score ranking of -2 or -1 in the sixth year of life among those who did or did not have RSVH at age < 12 months (RR 0.83, 95% CI 0.45, 1.53) (COE low).Footnote 32
Infants with or without RSVH at age < 24 months were evaluated at age 17-20 or 28-31 years. Pre-bronchodilator, there was a small decrease in mean percent of predicted FEV1 (mean difference -7.63, 95% CI -11.35, -3.91) and in the mean percent of predicted Forced Vital Capacity (FVC) (mean difference -4.74, 95% CI -7.80, -1.67) (COE low). There was little or no difference in the mean percent of predicted FEV1/FVC (mean difference -3.20, 95% CI -9.07, 2.67) or the mean percent of predicted Maximum Expiratory Flow after 50% of expired FVC (MEF50) (mean difference -4.00 95% CI -14.95, 6.95) (COE very low)Footnote 99 Footnote 100. There was little to no difference in the change in mean percent predicted FEV1 (mean difference 0.81, 95% CI -0.67, 2.30) (COE low) after administration of bronchodilator. There was very uncertain evidence on the change in mean percent predicted FVC (mean difference 0.60, 95% CI -0.67, 1.87) (COE very low), FEV1/FVC (mean difference -0.20 95% CI -2.71, 2.31) and the change in mean percent of predicted MEF50 (mean difference 3.70, 95% CI -5.42, 12.82) after administration of bronchodilator (COE very low).There was little or no difference for fractional exhaled nitrous oxide between those with or without RSVH at age < 24 month (mean difference -1.00 95% CI -14.49, 12.49) (COE low)Footnote 99 Footnote 100.
Single arm data showed rates of recurrent wheezing after RSVH in infancy of 12.4% (95% CI 6.3, 18.5; ROB moderate) for parent-reported or physician-diagnosed recurrent wheezing and 8.0% (95% CI 3.0, 13.0) for physician diagnosed severe wheezing at age 6 yrFootnote 32. In other studies rates of physician-diagnosed asthma after RSVH in the first year of life were 26.9% (95% CI 14.9, 39.0; ROB low) at age 7 yrFootnote 97, and 23.3% (95% CI 10.6, 35.9; ROB moderate) at age 28-31 yrFootnote 99.
The 2020 literature review update identified two studies that looked at long term recurrent wheezing or asthma. In a prospective birth cohort study, premature infants of 32-25 wGA were followed up at 6 years of age for parent-reported wheeze within the previous 12 months. Wheeze was reported for 27.7% of children with RSVH in infancy versus 17.6% for those without RSVH (OR 1.80, 95% CI 1.11, 2.85). After adjustment for confounding factors, OR was 1.89 (95% CI 1.06, 3.32). When stratified by atopic predisposition (defined as atopic disease in at least one parent), the difference was significant only for the group without atopic predisposition (ROB high)Footnote 101.
A retrospective matched cohort study of term infants without hsCHD, congenital lung disease or respiratory tract anomalies who did or did not have RSV infection in the first year of life assessed asthma or reactive airway disorder, identified from administrative claims databases, in the first 5 years of life. Cumulative incidence of asthma or reactive airway disorder for children with or without a history of RSV infection was 25.2% vs 11.4%, aOR (95% CI) 2.6 (2.5, 2.9), p<0.0001; 35.4% vs 16.7%, aOR 2.8 (2.6, 2.9), p<0.0001; and 24.4% vs 12.7%, aOR 2.2 (2.0, 2.4), p<0.0001 in three administrative databases (ROB high)Footnote 102.
III.3 RSV Reinfection
Reinfections with RSV occur throughout life. Naturally acquired immunity does not protect against subsequent infection, although it may modify disease severity with the initial infection usually being the most severe infection during childhood Footnote 103 Footnote 104 Footnote 105. In addition, two antigenically distinct RSV subgroups, A and B, may circulate during the same season Footnote 105 Footnote 106. In a study of 30 infants under 2 years of age with bronchopulmonary dysplasia (BPD), one child had two RSVH in the same season (3.3%)Footnote 107. Two prospective studies from Spain of children born at ≤ 32 weeks gestation reported recurrent RSVH in the same season in 6/584 (1.0%) and 9/999 (0.9%) of patientsFootnote 108 Footnote 109. For these reasons, previous statements from NACIFootnote 4 and AAPFootnote 5 recommended continuation of PVZ if an infant had a breakthrough RSV infection while receiving prophylaxis.
However, more recent data suggest that repeat RSV infections in the same season are rare. A study of 240 premature infants of <28 wGA or birth weight <1000 g in Denmark identified only 1 child with two RSVH in the same season (0.4%)Footnote 110. In a placebo-controlled trial of PVZ in children with CHD, only 0.39% of children (3 of 648 in the placebo group and 2 of 639 who received PVZ) had more than 1 RSVH in the same seasonFootnote 80. In another study of 429 premature infants followed for 1 year, there were no RSV reinfectionsFootnote 111. A study in an outpatient setting identified 726 RSV lower respiratory tract infections among children younger than 5 years over 8 successive RSV seasons. There were 56 reinfections but only one occurred during the same seasonFootnote 112. In another outpatient study of children less than 5 years of age, of 1802 children with RSV respiratory tract infections over 2 seasons only 1 had two infections in the same season, one of RSV-A and one of RSV-BFootnote 113. Because of the rarity of repeat infections in the same season, the AAP (2014)Footnote 6 and CPS (2015)Footnote 8 now recommend that if a child experiences a breakthrough RSVH while receiving PVZ, monthly prophylaxis should be discontinued.
III.4 RSV infection risk and siblings of multiple births
In a case-control study of preterm infants with BPD, fourteen sets of twins and two sets of triplets were matched with 34 singleton infants for date of birth and gestational age. The risk of developing RSV illness was significantly higher in multiple-birth infants than in singletons (53% vs 24%; p=0.01), as were the rate of RSVH (32% vs 18%; p=0.05) and the rate of RSV pneumonia (24% vs. 6%, p=0.05). After controlling for confounders in a matched logistic multiple regression analysis, multiple birth was still significantly associated only with the development of pneumonia (p=0.048)Footnote 114. In another study, Resch and colleagues retrospectively evaluated rates of hospitalization due to respiratory illness in 435 premature infants of 29–36 weeks gestation without chronic lung disease. They found that multiple birth was associated with RSVH (55% vs. 15%, p=0.013). Multivariate analysis to consider confounding factors was not doneFootnote 115.
In contrast, two larger prospective studies of risk factors linked to RSVH, involving a total of 2326 premature infants, found similar proportions of infants of multiple births in the groups with RSVH and in the control groupsFootnote 71 Footnote 116.
In a retrospective study of infants hospitalized with RSV bronchiolitis, twins represented 7.6 % (66/875) of hospitalizations. Of the 53 pairs of twins with at least one twin with RSVH, if one twin was hospitalized the other had a 34% chance of also being hospitalized with bronchiolitis (24% chance of being hospitalized with RSV positive bronchiolitis) during the same period. However, infants in the twin group were younger and had lower gestational age than singletons. In multivariate analysis, being born a twin was not a significant risk factor for RSV disease severityFootnote 117.
III.5 Healthcare associated RSV infections
RSV is frequently transmitted in hospitals, including in neonatal intensive care unitsFootnote 118. The available data indicates that RSV infection rates during the birth hospitalization do not differ among infants who receive PVZ prophylaxis while in the neonatal unit compared with those who receive PVZ starting at hospital discharge Footnote 119 Footnote 120 Footnote 121. These studies were rated as fair (Harris criteria)Footnote 122. The 2003 NACI statement on PVZ did not address the issue of administration of PVZ to in-patientsFootnote 4. The 2014 AAP Statement states that infants in a neonatal unit who qualify for prophylaxis may receive a dose 48-72 hours before discharge home or promptly after dischargeFootnote 6. The CPS states that for eligible infants being discharged home for the first time during RSV season, PVZ should be started just before dischargeFootnote 8. The United Kingdom's Green Book states that infants in neonatal units who are in the appropriate risk groups should begin PVZ 24 to 48 hours before being discharged.Footnote 123 To avoid wastage when vials are being opened daily for single infants about to be discharged, coordinating administrations to three times weekly has been suggestedFootnote 121.
PVZ has frequently been used to control RSV outbreaks in neonatal units. In some instances PVZ was administered to all exposed infants Footnote 118 Footnote 124 Footnote 125 Footnote 126 Footnote 127, in others only to those would have qualified for PVZ as outpatients Footnote 118 Footnote 127 Footnote 128. PVZ was started after other infection control measures had failed in some outbreaksFootnote 118 Footnote 124, and at the time of recognition of the outbreak in others Footnote 118 Footnote 125 Footnote 126 Footnote 127 Footnote 128. The incremental role played by PVZ in control of these outbreaks could not be determinedFootnote 118. PVZ may be useful when other measures have failed to control an outbreak or when it is anticipated that adherence to infection control recommendations will be poorFootnote 118 Footnote 126.
Although not addressed in the AAP 2014 or the CPS statements, the 2009 AAP PVZ statement indicates that infants who have begun PVZ prophylaxis earlier in the season and are hospitalized on the date when a dose is due should receive that dose as scheduledFootnote 5. Likewise the UK Green Book states that those infants that have begun a course of PVZ but are subsequently hospitalized should continue to receive it whilst they remain in hospitalFootnote 123.
Product
IV.1 Preparation authorized for use in Canada
The only product currently authorized for use in Canada for prevention of serious RSV disease is PVZ (Synagis®, AbbVie AstraZeneca, Mississauga, Ontario). PVZ is a humanized monoclonal antibody (IgG1κ) produced by recombinant DNA technology, directed to an epitope in the A antigenic site of the F protein of RSV, a surface protein that is highly conserved among RSV isolates. It is a composite of 95% human and 5% murine amino acid sequencesFootnote 129. It was authorized for use in Canada in 2002.
PVZ solution for injection is available in 50 mg/0.5 ml and 100 mg/1 ml single use vials. Non-medicinal ingredients included are chloride, glycine, histidine and water for injectionFootnote 129.
IV.2 Efficacy and effectiveness
Studies of the efficacy and effectiveness of PVZ in preventing severe consequences of RSV infection in children at high risk of severe RSV disease are reported in the document "NACI Literature Review on the Effects of PVZ Prophylaxis on Reducing the Complications Associated with Respiratory Syncytial Virus in Infants" which will be forthcoming. Results are summarized below. In mixed populations of infants at risk of severe RSV infection, PVZ prophylaxis is associated with reductions of 38 - 86% in the risk of RSV-associated hospital admissions, with number needed to treat (NNT) to prevent one hospitalization of 2 to 24. Differences in the health conditions of the mixed populations preclude definitive conclusions about relative benefits for different patient groups. Studies of mixed populations will not be discussed further here, but are included in the Literature Review which will be forthcoming.
IV.2.1 Premature infants without infantile chronic lung disease
IV.2.1.1 RSV-associated hospitalizations
Twelve studies examined the effect of PVZ prophylaxis on RSVH in premature infants without CLD: a systematic review and meta-analysis of average qualityFootnote 74, four RCT reports of goodFootnote 41 Footnote 48 or average qualityFootnote 111 Footnote 130, six observational cohort studies of either goodFootnote 131, average or fair Footnote 27 Footnote 44 Footnote 49, or poorFootnote 47 Footnote 132 quality and one case-control study of fair qualityFootnote 133.
The systematic review and meta-analysis of studies from 1990 to 2007 found that compared to no prophylaxis, PVZ use was associated with 72% fewer RSVH in infants born at ≤32 wGA and 74% fewer in infants born at 32–35 wGAFootnote 74. The IMPACT RCT, carried out in 1996, reported a 78% decrease in rate of hospitalization for RSV in premature infants aged ≤ 6 months without CLD who received PVZ, with a NNT of 16Footnote 48. The decrease was 47% for infants ≤ 32 wGA and 72% for those 32-35 wGAFootnote 48. Notario et al. further analyzed the data from the IMpact study by gestational age groups. PVZ resulted in significant reductions in hospitalization rates for infants of 28-31 wGA (73%), 29-32 wGA (80%), 32-34 wGA (82%), and 32-35 wGA (82%), but not for those <29 wGA or 33-35 wGA. The numbers in these two latter groups were smallFootnote 41. NNT ranged from 13 to 21 and decreased with increased gestational age. A similar significant protective effect of PVZ prophylaxis was found in a later RCT of infants 33–35 wGA enrolled in 2008-10 (82%. NNT 24)Footnote 111and a small RCT of infants born at ≤32 wGA enrolled in 2009-11 (OR 0.26, NNT 5)Footnote 130.
In the prospective case-control study rated as fair quality, conducted from 2002 to 2006, PVZ effectiveness for prevention of RSVH was 74% of 29-35 wGA infants. Effectiveness was not observed in those < 29 wGA but the numbers were smallFootnote 133.
Observational cohort studies had conflicting results about the impact of PVZ prophylaxis on RSVH in premature infants. A retrospective cohort study of fair quality of children born in 2012-2015 found a 38% lower RSVH rate in the first RSV season in infants 29–32 wGA who received PVZ compared to infants receiving no prophylaxis (NNT 53), but no statistically significant difference in RSVH in infants 33–36 wGA who did and did not receive PVZ prophylaxis. However, numbers of children prescribed PVZ and adherence to PVZ prophylaxis in the latter group were lowFootnote 27.
In an observational study rated fair quality, PVZ prophylaxis did not significantly reduce RSVH rate for infants of ≤ 28 wGA without CLD enrolled between 2011-2013 compared with a historic control group born in 2000-2008Footnote 44. However, the sample sizes were small.
PVZ was not significantly effective in cohorts of children born at 32–35 wGA in 2002-3 in a study rated as good qualityFootnote 131. Another cohort study of infants born at 32-34 wGA from 1995-2004, rated as fair quality, found a significant reduction in RSVH in Texas (OR=0.45, 95% CI 0.26, 0.78, p=0.005) but not in Florida (OR=0.81, 95% CI 0.42, 1.58, p=.54)Footnote 49.
In a study rated as poor quality, PVZ prophylaxis was found to significantly reduce RSVH in a cohort of children born at ≤30 wGA in 1999-2004 (1.1 % vs 13.6%, NNT 9)Footnote 47.
In summary, there is good evidence, based on early RTC, of the efficacy of PVZ in premature infants of 28-35 wGA. The conflicting results of observational studies on infants of 32-36 wGA are difficult to explain, but may in part be due to differences in study design, adherence, location and era. Three studies, one of good and two of fair quality, suggested lack of effect in infants of < 29 wGA but this may be the result of small numbers of infants without CLD in this very premature group Footnote 41 Footnote 44 Footnote 133. One observational study of poor quality supported a protective effect in infants of ≤ 30 wGA. In general, it appears there is evidence in support of the effectiveness of PVZ in reducing RSVH in children born prematurely, although the level of prematurity at which PVZ is most effective is not clear from the data.
IV.2.1.2. Mortality
The only study that examined all-cause mortality was a systematic review and meta-analysis of average quality by Checchia et al.. In infants born at ≤32 wGA. PVZ recipients had a significantly reduced risk of all-cause mortality (OR=0.25, 95% CI 0.13, 0.49, p<0.001) compared to recipients of placebo or no intervention, while in infants born at 32–35 weeks' GA, the difference was not significant (OR=0.22, 95% CI 0.03, 1.89, p=0.085)Footnote 74.
It is possible that there may be a differential impact of PVZ prophylaxis on all-cause mortality in this population, showing a protective effect in infants born at ≤32 weeks' GA, but not at lesser levels of prematurity (32–35 weeks' GA). However, these findings are based upon few studies which may have been underpowered to detect difference in mortality in the less premature infants.
IV.2.1.3 Long term sequelae
IV.2.1.3.1 Recurrent wheezing and atopic asthma
Six reports examined the effect of PVZ prophylaxis on the risk of wheezing in the first few years of life: Two reports of average or fair quality from a RCTFootnote 111 Footnote 134 and four reports from two cohort studies of goodFootnote 135, average or fairFootnote 136 Footnote 137 and poorFootnote 138 quality. One studyFootnote 111 investigated parent-reported wheezing only, while the other five investigated physician-diagnosed or both parent-reported and physician-diagnosed wheezing. Three studies found that PVZ prophylaxis in otherwise healthy premature infants born at 33–35 wGAFootnote 111 Footnote 138 or ≤35 wGAFootnote 136, resulted in a significant reduction (46-66%) in the risk of wheezing in children in the first year of lifeFootnote 111, up to age 3Footnote 138, or up to 2 years after enrollment at age ≤36 monthsFootnote 136.
In another report from the cohort study of Simoes et al., children who had received PVZ prophylaxis had a significantly decreased incidence of physician-diagnosed wheezing 24-months after study enrollment and a significantly longer time to a third physician-diagnosed wheezing episode compared to children receiving no intervention, but only in children without a family history of asthma or atopy. There was no significant difference in these outcomes in children with a family history of asthma or atopyFootnote 135.
A follow-up of the cohort of children born at 33–35 wGA initially assessed for wheezing at age 3 yearsFootnote 138 found that children who had received PVZ prophylaxis had reduced rates of physician-diagnosed recurrent wheezing during the first 6 years of life compared to children who had not received prophylaxis. However, this association was found only in the subgroups of children with a family history of allergy. The authors distinguished atopic asthma (recurrent wheezing and elevated IgE) from recurrent wheezing and found rates of atopic asthma were similar in children who received PVZ and those who did not, regardless of family history of allergyFootnote 137. On follow-up at age 6 years of the infants enrolled in the Blanken et al. RCT, the difference between PVZ and placebo recipients was significant only for those with parent reported infrequent wheeze (1-3 episodes per year). There was no significant difference in physician diagnosed asthma or the use of asthma medication in the previous 12 months and pulmonary function at 6 years of age did not differ between the groupsFootnote 134.
It appears PVZ may have a consistent impact in reducing the incidence of recurrent wheezing in young children in the first few years of life, but the findings are contradictory as to the relative impact of PVZ versus a family history of atopy on subsequent recurrent wheezing in older children. It also is not clear from these studies at what level of prematurity PVZ may be most effective in having a long term impact. The NNT to prevent one case of recurrent wheezing was 7-8 in infants of 32-35 or 33-35 wGA Footnote 111 Footnote 136 Footnote 137 Footnote 138, 10 for 29-32 wGAFootnote 136 and 15 for < 29 wGAFootnote 136.
IV.2.1.3.2 Growth parameters
One cohort study of fair quality assessed parameters of growth at 6 years of age in children born at 33–35 wGAFootnote 137. The study found no significant differences in weight, height or body mass index between children who received PVZ and children did not.
IV.2.2 Premature infants with infantile chronic lung disease
IV.2.2.1 RSV-associated hospitalizations
Five studies examined this outcome. A good quality RCT of children born at ≤35 wGA and ≤24 months of age with BPD, carried out in 1996, found that PVZ recipients had a reduced risk of RSV-associated hospitalization compared to infants who received placebo (RR=0.61, 95% CI 0.40, 0.95; NNT 21)Footnote 48. In an observational study rated as fair, PVZ prophylaxis reduced RSVH rate by 86% (NNT 13) in the first 6 months after initial hospital discharge for infants with CLD enrolled between 2011 and 2013 compared with a historic control group born in 2000-2008. By gestational age, reduction was significant for those of ≤28 wGA (89%, NNT 12) and not those 29-35 wGA, but numbers in the latter group were smallFootnote 44. An earlier prospective observational cohort study of poor quality of infants born at ≤32 wGA, carried out in 1999-2002, found PVZ prophylaxis to be associated with a reduced risk of RSVH (RR=0.15, 95% CI 0.05, 0.49, p<0.01; NNT 3) in the 1st RSVFootnote 139. Another prospective observational study of poor quality that included children up to 24 months of age with CLD also reported reduced risk of RSVH (RR=0.28, 95% CI 0.14, 0.58, p<0.007; NNT 8)Footnote 46. In a prospective case-control study, rated as fair quality, of infants ≤35 wGA and <12 months or 12-24 months of age, conducted from 2002 to 2006, there was no significant reduction in hospitalization rateFootnote 133.
The results suggest that PVZ prophylaxis provides a reduction in the risk of RSV-associated hospital admissions in this population, but the influence of gestational age on this benefit is not clear.
IV.2.2.2 Mortality
A meta-analysis of average quality showed no observed effect of PVZ vs no intervention/placebo on all-cause mortality for preterm CLD (0.22% vs. 0.34%; Peto OR, 0.83; 95% CI 0.13, 5.25), but there were only 3 events in the prophylaxis group and 2 events in the placebo/no intervention groupFootnote 74.
IV.2.3 Children with cystic fibrosis
IV.2.3.1. RSV-associated Hospitalizations
Six studies examined this outcome. A systematic review rated of good quality identified one RCT carried out in 1998-2001. The study found no significant difference in RSVH in children with cystic fibrosis who received either PVZ prophylaxis or placebo (RR 1.02 (95% CI 0.06, 16.09). However only one child in each group was hospitalized due to RSVFootnote 140 Footnote 141. One small observational study of fair quality found that historical controls from 1997-2002 who did not receive PVZ were more likely to have RSVH compared to children who received PVZ from 2003-2007 (21.3% vs 4.4%, p=0.027; NNT 6)Footnote 78. Three other observational studies found no significant difference in RSVH between PVZ recipients and controls. In the study by Bjornson et al, carried out from 2000-2017 and rated as fair, hospitalization rate was 2.7% for PVZ recipients and 6.0 % for controls (p=0.20). After adjustment for confounding factors, the hospitalization rate for RSV was still not significantly less in children who received PVZ than in those who did not. However there was a significantly reduced rate of hospitalization for respiratory illness in the PVZ recipients, and overall testing rate for RSV was low at 53%Footnote 77. A large study from 1999-2006, of poor qualityFootnote 142, and a small study of PVZ recipients from 2001-05 with historical controls from 1997-2000, also of poor qualityFootnote 143 did not find a significant benefit of PVZ prophylaxis compared to no intervention on subsequent RSVH. A case control study of fair quality, carried out in 2001-12, found no significant reduction in RSVH between the PVZ (5%) and control (2.9%) groupsFootnote 144.
No conclusions on the effectiveness of PVZ prophylaxis in reducing the risk of RSVH in children with cystic fibrosis can be drawn from the findings of these studies. Only the observational study of Groves et al. found a significant preventive effect of PVZ prophylaxis on RSVHFootnote 78. The rate of RSVH in the control group in that study was very high and the number of participants was small. Most studies had small numbers and may have been underpowered to detect an effect. The exception was the large study of Winterstein et al, which used a health care provider administrative databaseFootnote 142. It may be that some children with cystic fibrosis, e.g, those with significant chronic lung disease in the first 1 or 2 years of life, may benefit.
IV.2.3.2 Additional Hospital Outcomes due to RSV
IV.2.3.2.1 Length of hospital stay due to RSV
One observational cohort study of fair quality examined the effect of PVZ on the duration of hospitalization due to RSV in children with cystic fibrosis. The mean duration of hospitalization was significantly less in the PVZ recipients (5.7 ± 2.4 days) than in the controls (47 ± 39 days), p=0.048Footnote 77. An earlier small historical cohort study of poor quality found no significant difference in the median number of days of RSVH in PVZ recipients (11, interquartile range: 3–14) compared to children receiving placebo (13, IQR: 2–14) (OR=0.46, 95% CI 0.16, 1.31)Footnote 143.
At present, with the results of a single small study of poor assessed quality that may not have been sufficiently powered to detect a difference, no firm conclusions can be drawn on the effect of PVZ prophylaxis on the duration of RSVH in children with cystic fibrosis.
IV.2.3.2.2. Admission to intensive care unit due to RSV
One study assessed this outcome. None of 183 PVZ recipients and 2 of 84 controls were admitted to ICU because of RSV. Of patients hospitalized for RSV, 2 of 5 patients in the control group required ICU admissionFootnote 77.
IV.2.3.2.3 Use of respiratory support due to RSV
Robinson et al examined the effect of PVZ prophylaxis on the use of oxygen therapy due to RSV in children with cystic fibrosis. No significant difference between the groups was found in the need for oxygen therapy; however, the number of outcomes was small (PVZ prophylaxis group, n=1; placebo intervention group, n=0)Footnote 140. In the study of Bjornson, increased respiratory support, either MV or oxygen therapy, was required by 2.2 % of PVZ recipients and 1.2% of the control group (p=0.58)Footnote 77. In the study of Buchs, no patients required supplemental oxygen or MVFootnote 144.
IV.2.3.3 All-cause Mortality
The RCT study examined the effectiveness of PVZ prophylaxis in reducing all-cause mortality in children with cystic fibrosis. However, as there were no deaths identified in either group during the 6 months of follow-up during the study, no conclusion can be drawn about the effect of PVZ prophylaxis on this outcomeFootnote 140. A larger cohort study by Fink et al. also reported no difference in all-cause mortality before age 2 years between those who did or did not receive PVZFootnote 145.
IV.2.3.4. Long-term Sequelae
IV.2.3.4.1 Lung function
A small historical cohort study of fair quality found no significant difference in lung function (as assessed by measurement of FEV1) between children with cystic fibrosis who had and had not received PVZ was found on follow-up assessments at 6 years of ageFootnote 78. The cohort study by Fink et al., rated as of poor quality, also found no difference in FEV1 at age 7 years between those who did or did not receive PVZFootnote 145.
IV.2.3.4.2 Growth parameters
The RCT found no significant differences between the PVZ and placebo groups at 12 month follow-up with respect to weight gain or weight to height ratioFootnote 140. A small historical cohort study found no significant differences in growth parameters (weight, height, body mass index) at 6 years of age between children who did and did not receive PVZ prophylaxisFootnote 78. The case control study of Buchs et al, also found no significant difference between PVZ recipients and controls in growth in the first 3 years of lifeFootnote 144.
IV.2.3.4.3 P. aeruginosa and S aureus colonization
The RCT found no statistically significant differences in the numbers of children with P. aeruginosa airway colonization in children receiving PVZ compared to those receiving placebo at 12 months follow-up.Footnote 140 In the study by Groves et al, the median time to a first isolate of P. aeruginosa was significantly shorter in PVZ recipients than in non-recipients and the relative risk of a first isolate during the study period was also significantly increased in PVZ recipients. However, at follow-up at 6 years of age there was no significant difference in chronic P. aeruginosa colonization rates between the two groupsFootnote 78. Buchs et al, reported that PVZ prophylaxis had no significant effect on age at first colonization with P. aeruginosa or S. aureus or in the proportion of children colonized with P. aeruginosa by age 3 years. The proportion of infants colonized with S. aureus by age 3 years was significantly increased in the PVZ recipients (97%) in comparison to controls (85%)Footnote 144. Fink et al. also reported no difference in time to first P. aeruginosa colonization between those with or without PVZ prophylaxisFootnote 145.
The results from the these studies appear consistent with no significant differences in the longer term sequelae examined between children with cystic fibrosis who have and have not received PVZ prophylaxis. However, the number of children studied was small.
IV.2.4 Children with hemodynamically significant congenital heart disease
IV.2.4.1. RSV hospitalizations (RSVH)
Five studies examined the efficacy or effectiveness of PVZ prophylaxis in children with hsCHD. A good quality RCT carried out in 1998-2002Footnote 80 found that children with hsCHD and ≤24 months of age at the start of the RSV season who received PVZ prophylaxis had a significant relative decrease in RSVH compared to children receiving placebo (RD=45%, p=0.003; NNT 23). This was statistically significant in children with acyanotic CHD (RD=58%, p=0.003; NNT 15), but not in children with cyanotic CHD (RD=29%, p=0.285). An observational cohort study of fair quality of infants < 1 year of age, with PVZ recipients in 2013-2015 followed prospectively and controls from 2010-15 identified retrospectively found a significant reduction of 49% (NNT 45) for all cases and 65% (NNT 31) for the subgroup with cyanotic hsCHD but a non-significant reduction of 35% for those with acyanotic diseaseFootnote 146. A significant relative risk of 0.28 (72% reduction, NNT 7) in hospitalization for all cases of hsCHD < 1 year of age was reported in a small observational study of fair quality with PVZ recipients enrolled between 2014-16 and historical controls born in 2007-09Footnote 147. An earlier poor quality observational cohort study with PVZ recipients from 2003-07 and historical controls born 1998-03 did not find PVZ prophylaxis to result in a significant reduction in RSVH compared to no intervention in children with CHD who were born at ≤36 w GA and ≤24 months of age at the start of the RSV season (RR=0.58, 95% CI 0.21, 1.65), but the RSVH rate in the control population was very low (2.9%)Footnote 148. In a prospective case-control study of fair quality, carried out from 2002-6, significant PVZ effectiveness was not observed, either in the first or the second year of lifeFootnote 133.
These studies show conflicting results on the protective effect of PVZ on RSVH in infants with hsCHD. The two studies that did not show a significant effectFootnote 133 Footnote 148 had smaller numbers of participants than two larger studies that showed 45-49% risk reductionFootnote 80 Footnote 146. One of these studies showed significant protection in children with cyanotic heart disease but not in those with acyanotic heart diseaseFootnote 146, but the other showed the oppositeFootnote 80. The reasons for these discrepancies are not evident but may be due to inadequate sample size to detect a difference in the subgroups.
IV.2.4.2. Additional Hospital Outcomes Due To RSV
IV.2.4.2.1. Length of hospital stay due to RSV
The RCT involving children with hsCHD and ≤24 months of age found PVZ recipients to have a significant relative decrease in the total number of RSVH days/100 children compared to placebo recipients (RD=56%, p=0.003)Footnote 80. For those admitted to hospital because of RSV, mean LOS was 10.8 days for PVZ recipients and 13.3 days for placebo, not significantly different. In the study of Chiu et al, the LOS was not significantly different in patients who did or did not receive PVZ, either for the total group or for those with cyanotic or acyanotic hsCHDFootnote 146.
IV.2.4.2.2 Admission to and length of stay in intensive care unit due to RSV
The RCT of children with hsCHD aged ≤24 months reported that compared to placebo recipients, PVZ recipients had a relative decrease in the number of admissions to ICU but the reduction was not significant (RD=46%, p=0.094)Footnote 80. In the observational cohort studies, Chiu et al, reported no significance differences in rates of admission to ICU in those who received PVZ and those who did not, either for the total group or for those with cyanotic or acyanotic hsCHD, and Harris et al also found no significant difference in rate of admission to ICU. In the three studies, the proportions of infants hospitalized for RSV who required ICU admission were also not significantly different in the groups that received PVZ and those that did notFootnote 80 Footnote 146 Footnote 148.
In the RCT the total number of days/100 children in an ICU due to RSV did not differ significantly between PVZ and placebo recipientsFootnote 80. In the cohort study of Harris, mean ICU LOS decreased from 14.9 to 10 days but the difference was not significantFootnote 148.
IV.2.4.2.3 Use of mechanical ventilation (MV) due to RSV
The RCT by Feltes et al. found no significant difference in the use of MV, reported as total days/100 children, between children with hsCHD and ≤24 months of age at the start of the RSV season who received PVZ compared to placebo recipients (RD=41%, p=0.282)Footnote 80.
IV.2.4.2.4. Duration of oxygen therapy due to RSV
The RCT found that compared to placebo, children who received PVZ prophylaxis had significantly less total days/100 children on oxygen therapy (RD=73%, p=0.014)Footnote 80.
These results suggest that for children with hsCHD who are hospitalized with RSV infection, having received PVZ does not affect the severity of illness, as manifested by hospital LOS, ICU admission, ICU LOS, or need for MV, although the number of studies is small.
IV.2.4.3 All-cause mortality
Both the RCT by Feltes et al. and the cohort study by Harris et al. examined all-cause mortality in this populationFootnote 80 Footnote 148. In the RCT, there was no significant difference in all-cause mortality between children with hsCHD and ≤24 months of age at the start of the RSV season who received PVZ compared to placebo recipients. The Harris et al. study reported one death in the no intervention group and no deaths in PVZ prophylaxis group.
The RCT reported deaths from RSV in 2 of 639 PVZ recipients and 4 of 648 controls (p=0.46)Footnote 80.
IV.2.5 Children with Down syndrome
IV.2.5.1 RSV-associated Hospitalizations
Three studies examined the effect of PVZ prophylaxis in reducing RSVH in infants with Down syndrome. A small observational cohort study of fair quality of children carried out in 2012-14 found that hospitalization rate for children with Down syndrome without other criteria for PVZ prophylaxis was not significantly different in those who received PVZ and those who did not (3% vs 15%, p=0.075)Footnote 149. An earlier, larger cohort study, of poor quality, compared children in Canada with Down syndrome who received PVZ from 2005-2012 with children from a Dutch Down syndrome registry born from 2003-05 who did not receive PVZFootnote 150. After adjusting for hsCHD, insignificant CHD, gestational age, and birth weight, the analysis found that compared to no intervention receipt of PVZ was associated with a statistically significantly 72% reduction in RSVH (IRR=3.63 95% CI 1.52, 8.67, p=0.002; NNT 12). Significant reduction in hospitalization was also found when the analysis was restricted to children with at least one standard risk criteria for RSV prophylaxis (hsCHD, born at ≤35 wGA, CLD) (IRR 3.39 (1.02–11.25)). However, when the analysis was restricted to children with no standard RSV risk criteria, the difference in RSVH between children receiving PVZ prophylaxis and children receiving no intervention was not significant (IRR=6.57 95% CI 0.70, 62.16). The third study, rated as good, reported a decrease in overall RSVH after PVZ prophylaxis was approved in Japan for all children with Down syndrome. For all children, the adjusted odds ratio (aOR) for those receiving PVZ was 0.41 (95% CI 0.18, 0.92, p=0.03) but there were no differences in RSVH in the groups without hsCHD (aOR 0.43, 95% CI 0.04, 4.26, p=0.47) or without additional risk factors for RSVH (aOR 0.68, 95% CI 0.06–7.73, p=0.75)Footnote 151.
IV.2.5.2 Additional Hospital Outcomes Due To RSV
IV.2.5.2.1 Duration of hospital stay due to RSV
The observational study of Yi et al. study found that there was no significant difference in average number of days of hospital stay due to RSV in PVZ recipients compared to children receiving no intervention (6.4 versus 12.4 days, p=0.48)Footnote 150.
IV.2.5.2.2. Admission to and duration of stay in intensive care unit due to RSV
The observational study of Yi et al reported that none of the 532 children who received PVZ prophylaxis were admitted to an ICU, while in the 233 without PVZ there were 4 admissions to an ICU (p=0.0085). The average LOS in ICU was 10.3 daysFootnote 150.
IV.2.5.2.3 Use and duration of mechanical ventilation (MV) due to RSV
The Yi et al. study also had no children who received PVZ prophylaxis requiring MV, while in the group without PVZ there were 4 children who required MV (p=0.0085). The average duration of MV was 10.3 dayFootnote 150.
IV.2.5.2.4 Use and duration of oxygen therapy due to RSV
The Yi et al. study found that children who received PVZ prophylaxis had significantly less use of supplemental oxygen therapy (2/532, 0.004% versus 19/233, 0.08%, p<0.001) and fewer average number of days of use of oxygen therapy (4 versus 13.7 days, p=0.046) compared to children who did not receive PVZFootnote 150.
The significance of the results from these studies, one of poor qualityFootnote 150 and the other involving very few childrenFootnote 149, is unclear, but suggests that PVZ may not benefit children with Down syndrome who do not have other conditions that may warrant PVZ administration. Further studies would be required before conclusions can be drawn on the benefit of PVZ in this population.
IV.2.6 Infants residing in remote communities
IV.2.6.1 RSV-associated hospitalizations
There were two cohort studies of poor quality that examined this outcomeFootnote 92 Footnote 152. The Banerji et al. study included Inuit children from Nunavut, Canada who were born at either <36 wGA and/or had significant cardiac or respiratory disease and were <6 months of age at the start of the 2009-10 RSV season. Children who received PVZ had significantly fewer RSVH (2/91, 2.2%) compared to PVZ eligible children receiving no intervention (5/10, 50%) (OR=0.04, 95% CI 0.008, 0.26, p=0.0005). The number needed to treat to prevent one RSVH was 2Footnote 152. As not all PVZ eligible infants were identified, the actual reduction rate is likely to be less than that reported. In the study by Singleton et al., RSVH were assessed in Alaskan Aboriginal children before and after introduction of a PVZ program for high risk infants in 1998.There was a significant reduction in RSVH in infants born at ≤36 wGA (relative rate 0.34, 95% CI 0.17, 0.68, p<0.001). After the PVZ program introduction, among high risk infants the rate of first RSVH was 0.55 per 1000 PVZ protected days and 1.07 per 1000 unprotected days (relative rate 0.52; 95% CI 0.28, 0.93). The number needed to treat to prevent one RSVH was 4Footnote 92.
Although Inuit infants residing in remote northern communities are known to be at high risk of RSVHFootnote 23, data on PVZ effectiveness to prevent hospitalization in this group is very limited. After completion of the PVZ effectiveness literature review, the results of a program providing PVZ prophylaxis to healthy term infants less than 3 months of age during RSV season in Nunavik, Quebec became availableFootnote 90. The quality of the study was rated as fair. Between November 2016 and June 2019, 73% of 646 eligible healthy term infants received some PVZ but only 37% received all recommended doses on time. PVZ effectiveness was assessed by 1) comparing RSVH in infants who received all doses of PVZ on time and those who received no PVZ and 2) comparing RSVH during PVZ-protected and unprotected days. RSVH occurred in 10/237 infants (4.2%) who received PVZ and in 7/177 (4.0%) of those who did not. PVZ direct effectiveness was calculated to be -6.7% with wide 95% CI of -174.8, 85.5. RSVH rates were 37.6/100,000 PVZ-protected days and 39.1/100,000 unprotected days, for a direct protective effect of 3.8% with 95% CI -1167.6, 64.9. Limitations of the study included small numbers of RSVH, wide variation in RSVH in different years, and a high rate of co-infections with other respiratory viruses. For details, see the Data Table in Appendix C.
IV.2.7. Impact of changes in recommendations for PVZ prophylaxis.
Several studies were identified in the literature search on burden of RSV illness that described the impact of the 2014 AAP revised recommendations for PVZ use on RSVH by analyses of sequential time periods before and after implementation of the revised recommendationsFootnote 6. These studies did not meet the criteria for the literature review because children who did or did not receive PVZ were not identified, but are summarized here.
In a single tertiary center study from North Dakota, the rate of RSVH per 1,000 children <24 months old was 5.37 in the pre-2014 guideline period (2012-13 and 2013-14 seasons) and 5.78 in the post-2014 guideline period (2014-2015 season) (rate difference of +0.4, 95% CI −1.2, +2, p=0.622). The number of RSV admissions was 194. The number of doses of PVZ administered per 1000 children <24 months of age was 21.7 in the pre-2014 guideline period and 10.3 doses in the post-2014 guideline period, a reduction of 11.4 doses (95% CI 14.3, 8.4, p<0.001)Footnote 153.
Another single center study from Milwaukee looked at numbers of RSVH in infants less than 1 year old born at ≥29-35 wGA and the proportions of all RSV admissions that were in this gestational age group 2 seasons before and two after implementation of the 2014 AAP guidelines (2012-2017). The number of RSVH was 91.There were no significant differences in the number of admissions or the proportion of admissions in this gestational age group before and after implementation of the new guidelines. Duration of hospitalization increased from a median of 5.86 days before to a median of 7.86 days (p=0.02) after implementation but there was no difference in need for ICU, supplemental oxygen, or MVFootnote 154.
A single center study from Ohio looked at RSVH in infants <12 months old before and after implementation of the 2014 guidelines. Of 1063 RSVH, infants born at 290/7-346/7 wGA accounted for 7.1% (34/482) in the 2013-4 season and 9.8% (57/581) in 2014-5 season (not significantly different). Infants of 29-34 wGA who were <6 months old constituted 3.5% (17/482) of RSVH in 2013-14 versus 7.1% (41/581) in 2014-15 (p=0.01). Among 290/7-346/7 wGA otherwise healthy infants who were <3 months old, oxygen administration (40.0% vs 78.9%; p=0.05), pediatric ICU admission (30.0% vs 68.4%; p=0.04), MV (10.0% vs 52.6%; 0.04), duration of hospitalization (1.8 vs 8.8 days; p=0.04) were all higher in 2014-15. No differences in morbidity were observed between 2013-14 and 2014-15 in premature infants aged 3 to <6 or 6 to <12 months. PVZ eligibility decreased from 32.3% in 2013-14 to 1.8% in 2014-15 (p<0.001)Footnote 51.
A large study used commercial and Medicaid databases to assess infants born between July 1, 2011 and June 30, 2016. Infants were categorized as preterm or term and hospitalizations for RSV for infants aged < 6 months identified. Rate ratios comparing hospitalization rates for preterm and term infants were calculated. Seasonal rate ratios prior to the guidance change for preterm versus term infants ranged from 1.6 to 3.4. After the guidance change, seasonal rate ratios ranged from 2.6 to 5.6. In 2014 to 2016, the risk associated with prematurity of 29-34 wGA versus term birth was significantly higher than in 2012 to 2014 (2.00, p<0.0001 for commercially insured infants and 1.46, p<0.0001 for Medicaid insured infants, p<0.0001). PVZ use decreased by 74-97% in different wGA and age groupsFootnote 155.
An earlier study using similar databases assessed PVZ use and RSVH rates among preterm infants of 29-36 wGA during the 2014–2015 season with rates in the 2013–2014 season. PVZ prophylaxis utilization in infants 29 to 34wGA decreased by 62 to 95% (p< 0.01) in the 2014–2015 season relative to the 2013–2014 season. Compared with the 2013–2014 season, RSVH rates increased in the 2014–2015 season by 2.7-fold (p=0.02) and 1.4-fold (p=0.03) for infants 29 to 34wGA aged <3 months with commercial and Medicaid insurance, respectively. No significant differences were observed for those aged 3-6 monthsFootnote 156.
Another study investigated the effect of the change in recommendations for children with hsCHD. The 2014 AAP guidelines recommended PVZ prophylaxis for those in the first year of life whereas previous guidelines recommended prophylaxis for those < 2 years of age. A US national administrative healthcare database was reviewed to identify children age < 24 months with CHD admitted with RSV in the 2012-2014 and 2014-2016 RSV seasons. There were 644 RSV admissions in the 2012-13 and 2013-2014 seasons and 625 in the 2014-15 and 2015-2016 seasons. There was no change in LOS, ICU admission rate, or in-hospital mortality for children 13–24 months old with CHD after the change in recommendations. There were no deaths in 13–24 month olds, regardless of era. The population studied was not limited to those with hsCHDFootnote 157.
Following publication of the revised recommendations from the AAP in 2014, Italy implemented similar limitations for PVZ use for otherwise healthy premature infants in the fall of 2016. In a population of 284,902 children aged <2 years in one region of Italy, the number of RSVH was 1729. Following the change in policy a reduction in the number of RSVH from 6.3/1000 (95% CI 6.0, 6.7) to 5.5/1000 (95% CI 5.0, 5.9) was observed. There was no significant difference in wGA or age on admission of children admitted with RSV in the 2 seasons before and the season after the change in policy. The number of prescriptions for PVZ decreased by 48% after the change in policyFootnote 158.
A retrospective review of RSVH of children ≤ 1 years of age over three consecutive RSV seasons (2014-15, 2015-16, 2016–2017) was carried out in single tertiary center in Italy. Total RSV admissions for the 3 seasons was 366. The proportion that were preterm increased in the 3 seasons from 6.6%, to 7.3%, to 9.2%, respectively for the 29 - < 36 wGA group, and from 5.1% to 6.4% to 8.3%, respectively, for the 33 - < 36 wGA subgroup. These increases were not statistically significant but sample size was smallFootnote 159.
Another retrospective cohort study of RSVH among infants born at 29-35 wGA in the season before (2015–2016) or after (2016–2017) the introduction of more restricted recommendations for PVZ was conducted in three neonatal ICUs in Italy. There were 262 infants enrolled in 2015-16 and 274 in 2016-17. RSVH occurred in 1.9 and 5.1% in infants in 2015-16 and 2016-17 respectively (odds ratio 2.77; 95% CI 0.98, 7.8, p=0.045. The proportion of infants not receiving PVZ increased significantly from 63.7% in 2015-16 to 80.6% in 2016-17 (p< 0.0001)Footnote 160.
In summary, there is little population-based data on the effect of the 2014 change in AAP recommendations on RSVH of premature infants of 29 to 35/36 wGA. One small single center study reported no difference in overall RSVH rates. A large administrative database study showed a 1.4 to 2.7 fold increase in RSVH rates in premature infants aged < 3 months. Other studies looked at the proportions of children admitted with RSV who were of 29-35 wGA. Two single center studies showed no difference in this proportion. One showed no difference in morbidity of those admitted, while the other reported a shift towards younger age, and higher morbidity in those admitted who were < 3 months old but not in older infants. Another large database study compared ratios of premature to term infants among those admitted with RSV and reported an increase of 1.5 to 2 fold. One study of children with CHD aged 13-24 months showed no increase in morbidity in those hospitalized with RSV. A similar policy change was made in Italy. Two studies there showed no significant impact while a third reported a 2.7 fold increase in RSVH rates in infants of 29 to <36 wGA. However there are important variations in RSVH rates from 1 season to another, and these studies covered only 1 or 2 seasons before and after policy change.
IV.3 Immunogenicity
IV.3.1 PVZ levels
PVZ is a passive immunizing agent. A PVZ serum concentration of ≥ 30 ug/mL was shown to reduce replication of RSV in the lungs of the cotton rat by 99%Footnote 161. Based on this data, ≥40 ug/mL was chosen arbitrarily as the preferred target trough level in clinical trials in infantsFootnote 48 Footnote 80 Footnote 162. In these studies, 5 doses of 15 mg/kg were given at intervals of 30 days. A pharmacokinetic computer model based on data from 22 clinical trials suggested that this schedule would provide levels above the target trough for 6 monthsFootnote 163.
The half-life of PVZ is 19-27 daysFootnote 164. Trough PVZ levels increase with sequential doses. Mean ± SD trough serum concentrations 30 days after 15 mg/kg doses one, two, three, and four were 37±21 ug/mL, 57± 41 ug/mL, 68±51 ug/mL, and 72±50 ug/mL, respectivelyFootnote 165. In a study of PVZ in children with CHD, serum concentrations (mean ±SD) before the second and fifth doses were 55.5 ±19 ug/mL and 90.8 ±35 ug/mL. In 139 patients who underwent cardiac bypass, PVZ levels measured just before and the day after bypass were 98.0 ±52 ug/mL and 41.4 ±33 ug/mL, respectively, a decrease of 58% (p=0.0001)Footnote 80. Previous NACI guidance and the AAP state that for children with CHD who will continue to require prophylaxis, a 15 mg/kg dose of PVZ should be given after cardiac bypassFootnote 4 Footnote 6. The AAP also suggests that if prophylaxis is still indicated, an extra 15 mg/kg dose be considered at the conclusion of extracorporeal membrane oxygenationFootnote 6.
The possibility of giving fewer than 5 doses of PVZ has been explored. A recent modeling study predicted that levels of 30 to 40 ug/mL would be maintained for 181 days if doses 1 and 2 were given 29 days apart and the subsequent 3 doses 38 days apart. With only 4 doses these levels would be maintained for 143 daysFootnote 166. The CPS recommends that programs should administer a maximum of 3 to 5 doses, with 4 doses probably being sufficient in all risk groups if PVZ is started only when there is RSV activity in the community, especially if doses 2, 3, and 4 are given 38 days apartFootnote 8.
However, administration at 38 day intervals is more complex to implement and may result in more wastage; an interval of 35 days may be more practical. A program in British Columbia gave 4 doses of PVZ with interval of 21-28 days between the first 2 doses and 28-35 days between subsequent doses. RSVH occurred in 10 of 666 infants (1.5 %). All were PVZ breakthrough cases with the exception of one set of twins who were hospitalized 65 days after the 4th dose. Eighteen others (2.7%) were hospitalized for bronchiolitis while receiving PVZ but not tested for RSV. A 3-dose schedule was provided for 514 lower risk children born at 29 to <35 wGA and without chronic lung or CHD. One child was admitted for RSV while receiving PVZ and another was admitted 58 days after the 3rd doseFootnote 167.
A further cohort study of 391 children with CHD in British Columbia who received 4 doses of PVZ 2012 through 2016 showed an admission rate for proven or potential (not tested) RSV lower respiratory tract infection of 6.2 per 100 PVZ approvalsFootnote 168, a rate similar to the 5.3% observed in PVZ recipients in a clinical trial of 5 monthly doses in children with CHD (respiratory illnesses that were not tested for RSV were excluded)Footnote 80. Only one child had RSVH more than 30 days following the last dose of PVZ. In another study, protective neutralizing antibody levels (defined as neutralization titre (NT95) of ≥ 1 in 12 dilution) were present at an average of 55 days (range 28-105 days) after the final dose of PVZ. Protective neutralizing antibody levels were also found in 54% of control infants aged 4-11 months who did not receive PVZ, suggesting that humoral response to subclinical RSV infections may contribute to neutralizing titers that persist after PVZ administrationFootnote 169.
Concern has been expressed about the substantial inter- and intra- individual variability in PVZ levelsFootnote 163 Footnote 165 and implications for protection if fewer PVZ doses or longer dose intervals are used. Low trough levels after the first dose has led to suggestions for a shorter interval between the first and second dosesFootnote 170. Troughs of <40 ug/ml after the first dose were reported in 33% of recipientsFootnote 164. In one report, 46% of breakthrough RSV infections occurred in the interval after the first doseFootnote 171 but this high rate has not been replicated in other studies. A retrospective review of 42 patients hospitalized with RSV despite PVZ showing a correlation between lower PVZ levels and admission to an ICU. Mean levels were 47.2 ug/mL in those who required ICU care and 98.7 ug/mL in those who did not (p< 0.0001). In multivariate analysis in the above study, including potential confounding factors, the only parameter associated with ICU admission was PVZ levelFootnote 172.
IV.3.2. Dose Schedules and RSV Seasonality
The annual "RSV season" is the period during which the risk of acquiring RSV is sufficiently high to warrant prophylaxis of high risk infants. The season usually starts in October or November in Canada and ends in April or May, with most cases occurring in December through March. The duration of the annual RSV season varies with year and location, and was reported as varying from 13 to 23 weeks in various locations in the USAFootnote 7 and from 90 to 181 days in Hamilton, OntarioFootnote 173. Because 5 monthly doses should provide protective levels for > 6 months, a maximum of 5 doses is recommended by the AAPFootnote 6. Use of PVZ can be optimized if local virology laboratory data are used to determine when to begin prophylaxisFootnote 173. Where such data are unavailable, the start date may be determined by paediatric RSVH data, or based on previous seasons. In some areas, 4 monthly doses may be sufficientFootnote 174. In Canada, some programs start routinely in November or December and others use local laboratory and hospitalization data to define the RSV season (see Appendix A). The latter may be more complicated to implement than using fixed dates but may make more efficient use of the product.
Occasional RSVH may be expected before or after the main season in some areas, but maximum benefit from prophylaxis will be achieved during the peak of the season.
IV.4 Safety
PVZ is generally considered to be a safe product. Since the description of adverse events (AEs) in the NACI 2003 PVZ statementFootnote 4 there have been no safety alerts, but the number of infants exposed to PVZ has risen considerably. NACI determined that this warranted a new assessment of PVZ safety data. A rapid literature search of publications from 2003 onwards and a review of data from the Canadian Vigilance Program were performed. The full report on PVZ Safety is attached to this document as Appendix B, below.
IV.4.1 Rapid literature review
Nine RCTs, two population based cohort studies, 26 descriptive reports from registries or cohorts, and 2 case reports were identified. The most commonly reported AE considered related to PVZ were injection site reactions, fever, nervousness or irritability, cough, rhinitis, and diarrhea. PVZ related serious adverse events (SAEs) were very rare, reported in 1% or less of recipients, with most studies reporting none. Most were hypersensitivity reactions. Three reports of anaphylaxis were identified. PVZ discontinuation because of AEs occurred in 0-2.3% of recipients. There were no deaths attributable to PVZ. Repeated injections of a humanized monoclonal antibody raised concern for the development of immune mediated disease. Studies showed no increased risk of autoimmune disease or atopy in children exposed to PVZ.
IV.4.2 Data from the Canada vigilance program
A review of AEs reported to the Canada Vigilance Program, Health Canada, identified 259 case reports of AE following PVZ, with 237 classified as serious. The most frequent events were respiratory at 137 (53%), of which 113 were infections, mainly reported because of PVZ product failure, followed by hypersensitivity reactions at 23 (9%). Other events reported are expected complications of the underlying conditions for which PVZ is recommended and are consistent with those reported in the product monograph. The role of PVZ in these AEs is unknown as causality was not assessed.
IV.5 Vaccine administration
PVZ is given at a dose of 15 mg/kg of body weight by intramuscular injection.
For dose intervals and numbers of doses see Immunogenicity, Section IV.3, above.
IV.6 Storage requirements
PVZ should be stored between +2 and +8°C in its original container. It should not be frozen. Vials are for single use and do not contain a preservative.
If an entire vial (50 mg or 100 mg) is not required for a patient's monthly injection, physicians should arrange for more than one patient to receive PVZ within 6 hoursFootnote 4 or on that same clinic dayFootnote 175 in order to minimize product wastage. Opened vials containing product not used within 6 hours should be discarded and not stored. Weekly clinics for eligible infants in a specific locality facilitate efficient use with minimal wastage.
IV.7 Simultaneous administration with other vaccines
PVZ is an antibody directed specifically against RSV and does not contain other antibodies or human serum. It is not expected to interfere with the immune response to live or inactivated vaccines Footnote 7 Footnote 129. Children receiving PVZ should receive all routine childhood vaccines and any other vaccines that may be indicated because of underlying health conditions, following recommended schedules.
IV.8 Contraindications and precautions
Contraindications
Significant hypersensitivity to any component of PVZ is a contraindication to use of this product.
Precautions
Minor illnesses such as the common cold, with or without fever, are not contraindications to use of PVZ. Moderate to severe illness, with or without fever, is a reason to consider deferring PVZ, to avoid superimposing adverse effects from PVZ on the underlying illness, or mistakenly identifying a manifestation of the underlying illness as a complication of PVZ. The decision to delay PVZ depends on the severity and etiology of the underlying disease.
Economics
V.1 Systematic review
A systematic review of the cost-effectiveness of PVZ prophylaxis for RSV was conducted. Studies carried out in OECD countries and published from 2000 to 2018 were reviewed. The original review has been publishedFootnote 176. For the purposes of NACI's decision-making, changes to the reporting and discussion were made to the original review, and can be found as a NACI Supplement entitled "Cost-Effectiveness of PVZ for Respiratory Syncytial Virus (RSV): A Systematic Review" which will be forthcoming. Changes include currency reported in Canadian dollars, a section on Canadian studies, alternate subgroups reported, and additional commentary. Results from the supplement are summarized here. Of 28 studies included in the final analysis, 20 were cost-utility analyses and 8 were cost-effectiveness analyses. Two economic evaluations were trial-basedFootnote 177 Footnote 178, and the rest were considered model-based. Studies were conducted in the US (n=6), Canada (n=5), Netherlands (n=3), the United Kingdom (n=3), Spain (n=3), Austria (n=2), Germany (n=2), and Italy, Mexico, New Zealand, and Sweden (1 each). Base-case analyses were conducted from a health system payer perspective (n=15) or a societal perspective (n=13). Eight of the payer perspective studies performed additional analyses from a societal perspective. The majority of studies were industry sponsored (n=17, 61%). Cost-effectiveness outcomes were reported as ICERs, mostly represented as the incremental cost per additional QALY (n=20) and cost per hospitalization avoided (n=6). ICERs were adjusted to 2017 Canadian dollars (CAD).
PVZ prophylaxis ranged from being a dominant strategy (i.e. less costly and more effective) to having an ICER of $2,975,489/QALY. The wide variation in ICERs depended on the perspective, study setting, population, local RSV epidemiology, healthcare system, and key model input parameters such as rate of reduction in RSVH (39%-96%), estimated RSV-related mortality (1%-8.1%), PVZ costs ($1,099-$2,198 per 100-mg vial), dosage schedules, and vial usage.
V.1.1 Economic evaluations with outcomes expressed in cost per QALY
Data are summarized in Tables 1 and 2. For studies reporting cost-effectiveness in terms of cost per QALY from a health system payer perspective, there were 22 cost-effectiveness estimates for preterm infants, ranging between $6,216 per QALY and $938,623 per QALY Footnote 82 Footnote 179 Footnote 180 Footnote 181 Footnote 182 Footnote 183 Footnote 184 Footnote 185 Footnote 186 Footnote 187 Footnote 188. The subgroups with the next highest numbers of estimates were (i) preterm infants stratified by risk factor scores Footnote 185 Footnote 186 Footnote 187, (ii) infants with CHD Footnote 82 Footnote 179 Footnote 181 Footnote 182 Footnote 190 Footnote 191 Footnote 192, and (iii) infants with CLD Footnote 82 Footnote 181 Footnote 182 Footnote 187 Footnote 191. The proportion of reported cost-effectiveness estimates that fall below different thresholds is shown in Table 1. The largest agreement among reported estimates falling below the commonly used threshold of $50,000/QALY were infants with CLD (n =6 out of 6 studies), preterm infants (n=18/22), and infants with CHD (n=8/10). For premature infants no specific trend was detected between wGA and the ICER. From a societal perspective, PVZ prophylaxis was considered a dominant strategy (i.e. less costly and more effective) in some instances for preterm infants Footnote 183 Footnote 193 Footnote 194 Footnote 195, term infants in the Canadian ArcticFootnote 196, and infants with CHDFootnote 182. However, there was high heterogeneity in the study design and model parameters among reviewed studies including those that reported PVZ prophylaxis to be a dominant strategy. There does not appear to be a common driver for dominance of PVZ prophylaxis. In other scenarios, ICERs <$200,000/QALY were observed. Generally, one would expect ICERs from a societal perspective to be lower than those from a payer perspective, but this trend was not observed. Payer and societal perspective estimates frequently came from different studies and there was heterogeneity in model designs and differences between setting-specific costs and RSV epidemiology that may account for larger ICERs under a societal perspective.
Twelve of these studies were industry sponsored. It was noted that 50% of all estimates of <$200,000/QALY and 19% of all estimates of >$200,000/QALY were from studies funded by industry (S. Mac personal communication Mar 2019).
| Health Conditions | ||||||||
|---|---|---|---|---|---|---|---|---|
| CLD | CHD | Preterm | Preterm with CLD | Preterm with risk factorsFootnote * | CF | Canadian ArticFootnote ** | ||
| All infants | High risk areas | |||||||
| Payer perspective | ||||||||
| Number of estimates | 6 | 10 | 22 | 4 | 14 | 2 | 6 | 2 |
| ICER (Minimum) | 4,786 | 11,668 | 6,216 | 15,202 | 215 | 167,107 | Dominant | Dominant |
| ICER (Maximum) | 46,821 | 164,946 | 938,623 | 131,874 | 205,563 | 693,105 | 178,057 | 391 |
| Proportion of estimates that are dominant | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.17 | 0.50 |
| Proportion of estimates CE below $50,000/QALY | 1.00 | 0.80 | 0.82 | 0.75 | 0.64 | 0.0 | 0.67 | 1.00 |
| Proportion of estimates CE below $100,000/QALY | 1.00 | 0.90 | 0.86 | 0.75 | 0.86 | 0.0 | 0.67 | 1.00 |
| Proportion of estimates CE below $200,000/QALY | 1.00 | 1.00 | 0.91 | 1.00 | 0.92 | 0.50 | 1.00 | 1.00 |
| Societal perspective | ||||||||
| Number of estimates | 1 | 8 | 23 | 3 | 6 | 0 | 6 | 2 |
| ICER (Minimum) | 28,529 | Dominant | Dominant | 18,717 | 21,931 | N/A | Dominant | Dominant |
| ICER (Maximum) | 28,529 | 209,666 | 2,975,489 | 138,282 | 635,172 | N/A | 175,291 | Dominant |
| Proportion of estimates that are dominant | 0.0 | 0.13 | 0.13 | 0.0 | 0.0 | N/A | 0.17 | 1.00 |
| Proportion of estimates CE below$50,000/QALY | 1.00 | 0.63 | 0.39 | 0.67 | 0.17 | N/A | 0.67 | 1.00 |
| Proportion of estimates CE below $100,000/QALY | 1.00 | 0.63 | 0.48 | 0.67 | 0.50 | N/A | 0.67 | 1.00 |
| Proportion of estimates CE below $200,000/QALY | 1.00 | 0.88 | 0.52 | 1.00 | 0.67 | N/A | 1.00 | 1.00 |
All ICERs are reported in 2017 Canadian dollars (CAD) / QALY. Dominant = less costly and more effective CLD, chronic lung disease; CHD, CHD; CF cystic fibrosis N/A: Not available |
||||||||
|
ICERS: Preterm by Gestational Age in weeks (wGA) | ||||||
|---|---|---|---|---|---|---|---|
| 26-28 | < 29 | 29-30 | 29-32 | < 32 | < 33 | 32-35 | |
| Payer perspective | |||||||
| Number of estimates | N/A | 3 | N/A | 3 | 2 | 3 | 6 |
| ICER (Minimum) | N/A | 6,216 | N/A | 9,989 | 12,710 | 16,434 | 26,170 |
| ICER (Maximum) | N/A | 24,009 | N/A | 58,872 | 25,065 | 42,730 | 919,073 |
| Proportion of estimates that are dominant | N/A | 0.00 | N/A | 0.00 | 0.00 | 0.00 | 0.00 |
| Proportion of estimates CE below $50,000/QALY | N/A | 1.00 | N/A | 0.67 | 1.00 | 1.00 | 0.67 |
| Proportion of estimates CE below $100,000/QALY | N/A | 1.00 | N/A | 1.00 | 1.00 | 1.00 | 0.67 |
| Proportion of estimates CE below $200,000/QALY | N/A | 1.00 | N/A | 1.00 | 1.00 | 1.00 | 0.83 |
| Societal perspective | |||||||
| Number of estimates | 4 | 5 | 2 | N/A | 3 | N/A | 4 |
| ICER (Minimum) | 165,301 | 22,765 | 449,264 | N/A | Dominant | N/A | 32,390 |
| ICER (Maximum) | 2,406,619 | 1,359,641 | 1,083,976 | N/A | Dominant | N/A | 338,823 |
| Proportion of estimates that are dominant | 0.00 | 0.00 | 0.00 | N/A | 1.00 | N/A | 0.00 |
| Proportion of estimates CE below$50,000/QALY | 0.00 | 0.40 | 0.00 | N/A | 1.00 | N/A | 0.75 |
| Proportion of estimates CE below $100,000/QALY | 0.00 | 0.80 | 0.00 | N/A | 1.00 | N/A | 0.75 |
| Proportion of estimates CE below $200,000/QALY | 0.25 | 0.80 | 0.00 | N/A | 1.00 | N/A | 0.75 |
All ICERs are reported in 2017 Canadian dollars (CAD) / QALY. Dominant = less costly and more effective N/A: Not available |
|||||||
V.1.2 Economic Evaluations with Outcomes Expressed in Costs per Hospitalizations Avoided
Six studies reported cost-effectiveness in terms of cost per hospitalizations avoided (HA) Footnote 179 Footnote 197 Footnote 198 Footnote 199 Footnote 200 Footnote 201. A study of healthy term infants in different regions of the Canadian Arctic compared two scenarios of PVZ prophylaxis for infants who were less than 6 months of age, from a payer perspective. The ICER ranged from being dominant (i.e. less costly and more effective) in specific Arctic regions to $593,250/HA in the Northwest TerritoriesFootnote 197. Also from the payer perspective, a Florida study of preterm infants (<32 wGA), term infants with CHD, CLD, combinations of all three groups and infants with no indications for PVZ) reported ICERs between $413,127/HA (preterm infants) and $2,924,911/HA (infants with no indication)Footnote 201.
From a societal perspective, a study from the Netherlands of preterm infants (< 28 wGA) with additional risk factors (BPD, male sex, birth weight < 2,500 grams) found ICERs ranging between $24,875/HA and $1,572,268/HA depending on the month of the prophylaxisFootnote 198. In a study from Germany of preterm infants (<35 wGA) with additional risk factors, from a societal perspective ICERs ranged between $11,821/HA and $364,462/HA for preterm infants with CLD and risk factors and preterm male infants without CLD and with no siblings in school, respectivelyFootnote 199. A New Zealand study analyzed cost-effectiveness of prophylaxis in preterm infants (<28, 29-31 wGA) with or without CLD from a societal perspective. The ICERs ranged from $33,376/HA for preterm infants discharged home on oxygen, to $37,213/HA for infants ≤ 28 wGA with no CLD, to $193,859/HA for preterm (29-31 wGA) infants with CLDFootnote 200.
V.1.3 Economic Evaluations with Outcomes Expressed In Other Ratios
An economic evaluation on term infants with CHD in western Canada found that from a societal perspective, the base-case ICER was $18,155 per one day of hospitalization avoidedFootnote 148. A study of preterm infants (< 32 wGA) or with CLD or significant CHD in France found that from a societal perspective, the base-case ICER was $43,856/Life year (LY) gained and $33,450/LY gained for preterm infants with CLD and preterm infants with CHD, respectively. From a payer perspective, the ICER was $16,368/LY gained for infants with CLDFootnote 202. In a study of preterm infants with CLD in the US, the model used a reduction in incidence of RSV infection, ranging from 50% ($66,494 per RSV infection episode avoided) to 83% reduction (PVZ prophylaxis a dominant strategy, i.e. less costly and more effective) from a payer perspectiveFootnote 178.
V.1.4 Economic Evaluations in Canadian Settings
There were five economic evaluations conducted in Canadian settings Footnote 148 Footnote 186 Footnote 189 Footnote 196 Footnote 197. Populations studied were term infants from the Canadian ArcticFootnote 196 Footnote 197, preterm infantsFootnote 186, infants with CFFootnote 189, and infants with CHDFootnote 148. These studies assumed 4.5 to 6 doses of PVZ per RSV season at a cost of $1,599 - $1,718 (2017 CAD) per 100 mg of PVZ. In the above studies, the effectiveness of PVZ was measured in reduction in RSVH, which ranged between 42% and 96%. Mortality rates were incorporated into two models, at 1% and 8.1%Footnote 186 Footnote 196. Sequelae were incorporated into two models (in one sequelae of RSV infection, the other sequelae associated with CF)Footnote 186 Footnote 189. The most influential parameters on the cost-effectiveness outcomes in the five Canadian studies were: RSVH ratesFootnote 196 Footnote 197, cost of PVZFootnote 148 Footnote 189, and cost for hospitalization Footnote 196 Footnote 197, which includes inpatient medical costs and transportation costs to the medical centre.
In the Canadian Arctic, PVZ prophylaxis was considered cost-effective for some subgroups of infants as PVZ can prevent the high costs of hospitalizations related to transportation costs. This was especially the case for settings where baseline RSVH rates were high. From a payer perspective, PVZ can be considered cost-effective under commonly used thresholds for all Baffin Island term infants < 1 year of age ($46,151/QALY) or < 6 months of age ($11,925/QALY), all term infants < 1 year of age in rural areas ($28,965/QALY), infants < 1 year of age in high-risk rural areas ($391/QALY), and infants < 6 months of age in rural areas or in high-risk rural areas (dominant). However, it was not cost-effective for infants < 1 year of age ($178,057/QALY) or < 6 months of age ($120,817/QALY) residing in IqaluitFootnote 196. ICERs were not cost-effective in the city because PVZ did not prevent transportation costs associated with an RSVH. From a societal perspective, ICERs were slightly lower but followed a similar trend. Banerji et al. included term infants from eight Arctic regions: the Northwest Territories, Nunavut, Nunavut without Iqaluit, the three sub-regions of Nunavut (Kitikmeot, Kivalliq and Qikiqtaaluk), the Qikiqtaaluk Region without Iqaluit, and Nunavik (northern Quebec); and reported costs per HA in two separate scenarios: prophylaxis until the end of the RSV season (scenario A) and prophylaxis until 5 months of age (scenario B). PVZ prophylaxis was a dominant strategy (i.e. less costly and more effective) in Kitikmeot (scenarios A and B) and Kivalliq (scenario B); $24,981/HA in Kivalliq (scenario A); $5,042/HA (scenario B) and $31,104/HA (scenario A) in Nunavut without Iqaluit; $15,829/HA (scenario B) and $45,060/HA (scenario A) in Nunavut; $16,979/HA (scenario B) $32,899/HA (scenario A) in Nunavik. In all other regions, ICERs were greater than $100,000/HAFootnote 197. There was much variation in ICERs by region. PVZ tended to be cost-effective at a threshold of $50,000/QALY in regions with higher RSVH rates (range: 97.8 to 296.1 RSV admissions per 1,000 in Nunavik, Kivalliq region, Kitikmeot region, and Nunavut), whereas PVZ tended to be not cost-effective at a threshold of $100,000/QALY in regions with lower RSVH rates (range: 16.6 to 49.4 RSV admissions per 1,000 in the Northwest Territories and Qikiqtaaluk region)Footnote 197.
From the payer perspective, PVZ was considered cost-effective under commonly used thresholds for preterm infants of 32-35 weeks GA ($20,814/QALY including asthma as a consequence of RSV infection and $35,119/QALY excluding asthma). Using two sets of risk factor scores, ICERs were $251/QALY and $5,906/QALY for infants with high scores (high risk), $29,901/QALY and $38,566/QALY with medium scores, and > $50,000/QALY ($92,649 - $919,073) for lower scores or no risk factorsFootnote 186. For infants less than 24 months of age with CF, PVZ was determined unlikely to be cost-effective from a payer perspective ($693,105/QALY for all and $167,107/QALY for high risk infants)Footnote 189. In the study of PVZ cost-effectiveness in children < 24 months of age with CHD, from a societal perspective the ICER was $18,155/day of hospitalization avoided and considered unlikely to be cost-effectiveFootnote 148.
These latter three studies may be generalizable to most Canadian provinces given they used PVZ costs ($1,468 - $1,505 per 100 mg vial, original costs) similar to those in other Canadian provinces, dosing schedules close to 5 injections per season (4.5 to 5.39 vials per season), healthcare costs from British Columbia and Ontario, and included model parameters of relevance to the Canadian healthcare system. Studies of cost-effectiveness of PVZ prophylaxis for infants from smaller Canadian provinces (e.g. Maritimes provinces) were lacking.
| Authors, Year | Population | Dosage (per season) |
Cost per unit (Unadjusted) | Hospitalization | Mortality | RSV-Sequelae included? | ||
|---|---|---|---|---|---|---|---|---|
| PVZ | No PVZ | Reduction (%) | ||||||
| Tamet al., 2009Footnote 196 | Baffin Island Term infants | 5 doses | Vial unit cost: NR; $220/kg infant |
1.4 - 11.4% | 6.3 - 51.2% | 78%Table 8 Footnote a | 1% (both groups) | No |
| Banerji et al., 2016Footnote 23 | Canadian Arctic Term infants |
6 doses (maximum) | Vial unit cost: NR; $226/kg infant | NR | NR | 96% | NR | No |
| Smartet al., 2010Footnote 186 | Premature 32-35 wGA | 5.39 vials | 50mg: $752 100mg: $1,505 |
1.8% | 10.0% | NR (82% back calculation) | 3.9% (both groups)Table 8 Footnote b | Yes / No (asthma) |
| McGirr et al., 2017Footnote 189 | Cystic fibrosis age <24 months | 5 doses | 100mg: $1,505 | 1.7% (assuming 55% reduction)Table 8 Footnote c | 3.8% | 55% | NR (Used CF-related death) | Yes (cystic fibrosis progression) |
| Harris et al., 2011Footnote 148 | CHD age <24 months | 4.5 doses | 100mg: $1,468 | 1.7% | 2.9% | NR (42% back calculation) | NR 0.2% (1/41, no PVZ); 0% (0/292, PVZ) |
No |
NR: not reported |
||||||||
V.1.5 Heterogeneity in Results: Key Parameters
The most frequently reported influential parameters affecting the ICER were the RSVH rates and cost of PVZ used. Reduction in RSVH varied drastically between 39% and 96% depending on the population of interest, and the source of the data. The cost of a 100mg vial of PVZ also ranged between $1,099 and $2,198 (2017 CAD). However, vial usage and dosage scheme only affected the ICERs in fourFootnote 181 Footnote 183 Footnote 195 Footnote 200, and three studiesFootnote 185 Footnote 187 Footnote 200, respectively. In studies addressing drug wastage, ICERs fluctuated up to 50% depending on the assumed vial usage. In a New Zealand study, assuming no vial sharing (entire 100 mg vial is used per injection) increased cost per case averted by up to 50% (i.e. worse value for money)Footnote 200, while another study in Spain concluded a lower ICER (i.e. better value for money) when 50-mg vials were used instead of 100mgFootnote 183. It has been suggested in the literature that vial usage efficiency can be achieved for PVZFootnote 203. Discounting was also frequently reported as being influential on the ICER. Discount rates varied across studies (3-5%). Currently Canadian guidelines recommend a discount rate of 1.5% for costs and outcomesFootnote 204.
V.1.6 Generalizability of Included Studies to Canadian Setting
Most study results may be broadly generalizable to the Canadian healthcare system since these were economic evaluations conducted in OECD countries with healthcare components similar to CanadaFootnote 205. The only exceptions were the six studies from the US. Choice of payer or societal perspective may influence the costs and the benefits included in the analysis. Among the studies that used a societal perspective, the following costs outside of the healthcare system were considered: time loss from work due to asthma; indirect costs of nosocomial infections; travel costs (i.e. hotel, transportation); productivity loss (i.e. caregiving, leisure, future productivity of children); and school absenteeism.
From three Canadian studies, the cost per 100-mg vial of PVZ used in models was between $1,599 and $1,718 (2017 CAD). Models from the UK used a lower PVZ cost of $1,099 to $1,240 per 100-mg vial, and costs in the remaining studies (with the exception of those from the US) were between $1,386 and $2,035 (2017 CAD). The number of doses per season ranged between 3.88 and 6 doses. In the subset of countries with similar healthcare structure to Canada, almost all models assumed five doses of PVZ per season, except for Resch et al. (Austria)Footnote 82, Nuijten et al., Sanchez-Luna et al., and Schmidt et al. (all from Spain), where the average number of doses was 4 per seasonFootnote 183 Footnote 185 Footnote 195.
Despite the similarities in PVZ prophylaxis cost and dosage schedule, estimated reduction rates of RSVH varied from 39% to 96% depending on the infant population, and literature referenced. Sixty-eight percent of the studies (S. Mac personal communication June 2019) used the IMPACT-RSV trial for some of their model parameters, a trial that included Canadian children and concluded that reduction in RSVH was 78% for preterm infants, 39% for children with CLD and 55% overall. While the subgroup of Canadian subjects in that study showed a 40% overall reduction in RSVH, the trend was similar to that seen in US (56%), and UK subjects (64%)Footnote 48. It is noted that the IMPACT-RSV trial was carried out in 1996 and that with changes in the management of prematurity, CLD and CHD, as well as RSV infection, model parameters based on that study may not be appropriate today.
V.2 Cost-effectiveness study in Nunavik, Quebec
In addition to the studies in the systematic review, preliminary results of a cost-effectiveness study in the region of Nunavik, Northern Quebec were reported to NACI on March 13, 2019 (R. Gilca, Institut national de santé publique de Québec, personal communication, Nov. 18 2020)Footnote 206. Starting in the 2016-17 season, healthy full-term infants <3 months of age at the start of the RSV season or born during the RSV season became eligible for up to 3 doses of PVZ. For the 2017-18 season, infants meeting these criteria were eligible for up to 5 doses. The objectives were to estimate the healthcare cost of RSVH in the targeted population and the cost of the PVZ program, and to estimate cost per hospitalization averted.
The analysis below is based on the first 2 years of the program. It is being updated to include 4 years of data and will be published. The conclusions remain unchanged.
| Date | Incidence of RSVH per 100 000 patient-days | EffectivenessTable 9 Footnote * | |
|---|---|---|---|
| Unprotected | PVZ - Protected | ||
| 2017 | |||
| January 1 to April 30 | 58.1 | 37.5 | 35.5% |
| January 1 to May 31 | 45.5 | 33.8 | 25.7% |
| 2018 | |||
| January 1 to May 31 | 22.5 | 14.5 | 35.6% |
| January 1 to June 30 | 17.8 | 13.0 | 27.3% |
|
|||
| Scenarios / hypotheses | Averted costs: (average cost in absence of program, 2014-2016 = $156,914) |
2017 | 2018 | ||||
|---|---|---|---|---|---|---|---|
| total costs for program | ratio spent/averted | ROI | total costs for program | ratio spent /averted | ROI | ||
| 1. PVZ effectiveness = 36%Footnote *; cost reduction is proportional to effectiveness | $55,861 | $291,533 | 5 | 0.19 | $369,641 | 7 | 0.15 |
| 2. All observed reduction in 2017 is due to PVZ (reduction=89%)Footnote ** | $139,395 | $291,533 | 2 | 0.48 | $369,641 | 3 | 0.38 |
| 3. All observed reduction in 2018 is due to PVZ (reduction=71%)Footnote ** | $112,040 | $291,533 | 3 | 0.38 | $369,641 | 3 | 0.30 |
ROI: return on investment |
|||||||
The program costs far exceeded hospitalization and transportation costs. To be cost-neutral, the program would need to prevent 9 to 11 hospitalizations per year (total program costs / average 2014-2016 cost per hospitalization = $33,600). Such a high number of hospitalizations has not been observed in this population (average for 2014-2016 = 7 hospitalizations)
There are several limitations to this study, including the small population size, with approximately 220 healthy term infants born between October 1 and June 30 annually, and scattered across many very small communities. The number of hospitalizations of healthy full-term 0-2-month-old infants from Nunavik was low (lower than previously anticipated) and highly variable from year to year. The total costs for hospitalization and transportation are therefore also highly variable. The program cost is similar from year to year. The cost of PVZ is the main component but administration cost is not negligible (>$135/dose). Effectiveness of PVZ to prevent RSVH was low. Many hospitalized infants had co-infections with other viruses. There were also issues of social acceptability and compliance with the PVZ program.
Ethics, equity, feasibility and acceptability (EEFA) considerations
The peer-reviewed EEFA FrameworkFootnote 13 was applied to this guidance to ensure the systematic consideration of factors critical for comprehensive immunization program decision-making and successful implementation of recommendations. The use of this EEFA Framework empowers the committee to review and balance all of the available evidence and transparently summarize their rationale for appropriate, timely recommendations. The evidence-informed tools associated with the framework (Ethics Integrated Filters, Equity Matrix, Feasibility Matrix, Acceptability Matrix) ensure that issues related to EEFA of expert committee guidance are systematically and adequately integrated.
Ethics considerations
To support ethics deliberation and decision-making, NACI's Ethics Integrated Filters for core ethical dimensions (respect for persons and communities, beneficence and non-maleficence, justice, trust) and procedural ethical dimensions (accountability, inclusiveness, responsibility, responsiveness, transparency) were applied. NACI followed its established methodology, standard operating procedures (SOP), and conflict of interest guidelines to ensure a robust analysis of evidence, with transparency about knowns and unknowns, as well as certainty of evidence, and to maintain stakeholder trust. In order to respect the right to exercise informed choice, NACI reviewed the best, current evidence available for groups of infants and children at risk of RSV and summarized it for stakeholders throughout this guidance document, including recent data on burden of illness due to RSV disease, the efficacy and effectiveness of PVZ in infants at risk of more severe RSV disease and economic implications of PVZ use. NACI also considered evidence for minimizing the risk of harm and maximizing benefits for all potential key populations in their deliberations. These findings should be interpreted with caution given that some potential concerns were identified regarding availability of evidence; small numbers of articles were identified for some risk groups and situations and there was significant heterogeneity in methodology used and the outcomes studied. Furthermore, with no evidence of lowered mortality rates from RSV or of long term benefit from PVZ, the high cost of PVZ prophylaxis programs must also be balanced against costs of other health care interventions if these other interventions may be compromised by provision of PVZ programs. Therefore, NACI will continue to monitor the evidence related to use of PVZ in different groups, including the cost-effectiveness of PVZ programs and alternative dosage schedules and newer products which may be more cost-effective and will update the statement and its recommendations as needed.
Equity considerations
NACI reviewed the epidemiology of RSV and the results of the systematic review on the burden of RSV disease in young children in high-income countries comparable to Canada (summarized in Section III) to identify distinct inequities associated with COVID-19, potential reasons for these inequities, and suggested interventions to reduce inequities and improve access to vaccine when it becomes available.
The risk of severe RSV illness is influenced by gestational age at birth, underlying health conditions, and age. As it is not feasible to provide PVZ prophylaxis to all infants at some increased risk of RSV disease, in principle it should be provided to high risk groups at equivalent risk of severe disease. Specific recommendations are needed for selective PVZ prophylaxis for identifiable high-risk subgroups of infants and children who are more vulnerable than others to the adverse effects of RSV infection, and whose risk of severe outcome are within a similar range and for whom PVZ prophylaxis has been shown to be effective. However, the limited nature and heterogeneity of the data available makes assessment of degree of risk somewhat arbitrary. For certain very rare conditions, risk of severe RSV illness may be high but epidemiologic data are not available, and the number of children with certain rare diseases may not be sufficient for PVZ effectiveness to be studied. In these circumstances, extrapolation may be made from data on conditions of pathophysiological similarity with documented increased risk of RSV and where PVZ has been shown to be effective. In most provinces and territories, physicians may request PVZ by exception for children that do not meet specific criteria for PVZ. While this permits flexibility for use in children with rare conditions, it may also introduce inequity. Those making requests for exceptions and those assessing these requests must do so fairly, to avoid inequity.
Infants living in remote northern Inuit communities and other remote rural communities may also be at increased risk of severe outcomes resulting from RSV infection. Limited local access to medical care may necessitate medical evacuations requiring air transportation to hospital facilities. Therefore, additional resources may be needed for provision of PVZ prophylaxis and for monitoring and follow-up of infants living in remote locations. PVZ prophylaxis should also be provided as close to home as possible given that the number and frequency of visits over a short period of time and the strict injection intervals may be a barrier for families due to out-of-pocket expenses if the family has to travel some distance to receive PVZ and/or take time off work for these visits. In these cases, assistance may need to be given to some families so that they can benefit from the PVZ prophylaxis program. NACI will continue to monitor the evidence related to severity of RSV disease in infants with pre-existing conditions and in infants living in remote northern Inuit communities and other remote rural communities.
Feasibility considerations
Provision of PVZ prophylaxis is complex and integration into existing active vaccination programs is not feasible due to the dosing schedule and the seasonal nature of the disease. In particular, the need for multiple injections over a short time period may create scheduling challenges; up to 4 doses must be given at 28-35 day intervals during the period that the local annual RSV outbreak is underway. Unlike vaccines, PVZ dose depends on weight and precise timing of visits for PVZ administration is crucial for appropriate protection and it is not possible to combine all visits with visits for other vaccines or routine child care. Additionally, PVZ is provided in multi-dose vials which, once opened, must be used within 6 hours or discarded and wasted. Vial sharing may be difficult in smaller communities where very few children are candidates for PVZ, further increasing the cost. Therefore, important considerations for the implementation of a new PVZ prophylaxis program include limiting prophylaxis to those groups at highest risk of severe outcomes, scheduling specific PVZ clinics during the RSV season, recognizing the potential impact on existing local programs, and involving of local care givers in planning for program implementation.
Acceptability considerations
Very limited acceptability data are currently available specific to PVZ prophylaxis and the perception of RSV disease in parents or guardians of high risk infants. Likely barriers to acceptability and adherence include:
- The number and frequency of visits, especially if families have to travel some distance to receive prophylaxis and it is not possible to combine visits for PVZ with visits for other vaccines or routine health care needs.
- Out-of-pocket expenses if appointments require long-distance travel to the treatment center and time away from work.
- Lack of knowledge about the risk of RSV infection in high risk children.
There is some evidence indicating that Indigenous populations in Canada are at higher risk of non-adherence than non-Indigenous populations and that acceptance is lower in remote northern populationsFootnote 207 Footnote 208. Nurses and midwives working with a population in the Canadian North have also expressed concerns regarding lack of data about the efficacy and safety of PVZ in healthy term infantsFootnote 207. Low acceptability of PVZ prophylaxis by families may result in decreased adherence to PVZ schedules and diminish effectivenessFootnote 209. Therefore, implementation of a new program should include ongoing education of local health care providers, families and guardians of infants for whom PVZ is indicated, and their active involvement in planning of the intervention. Provision of PVZ in local clinics as close to home as is feasible and sufficient resources to provide assistance for families who may need some additional support to be able to travel to the clinic are also important considerations.
Recommendations
Following the thorough review of available evidence summarized above, as well as the systematic assessment of ethics, equity, feasibility and acceptability considerations with the peer-reviewed EEFA Framework, NACI makes the following evidence-informed recommendations.
Recommendations for public health program level decision-making
(i.e. provinces/territories making decisions for publicly funded immunization programs)
In considering these recommendations and for the purposes of publicly funded program implementation, provinces and territories may take into account local programmatic factors (e.g. current programs, resources). Recognizing that there are differences in operational contexts across Canada, jurisdictions may wish to refer to the Management Options Table below for a summary of the relative merits of vaccinating different high risk groups, if prioritization of targeted immunization programs is required for implementation.
1. Preterm infants without CHD or CLD:
Recommendation 1.1: NACI recommends that PVZ should be offered to infants born at < 30 weeks, 0 days gestation and aged < 6 months at the onset of or during the RSV season. (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend PVZ use in this population (Grade B evidence).
Recommendation 1.2: NACI recommends that PVZ may be considered for infants of 30 to 32 weeks, 6 days gestation aged < 3 months at the onset of or during the RSV season if they are at high risk of exposure to RSV from day care attendance or presence of another preschool child or children in the home. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Recommendation 1.3: NACI recommends that PVZ should not be offered to otherwise healthy infants born at or after 33 weeks, 0 days gestation (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend against PVZ use in this population (Grade C evidence).
Summary of evidence and rationale:
- There is good evidence that risk of RSVH is higher in premature infants born at lower gestational age, with reported rates of 7.7 to 13.6% in the first year of life for those of < 28 or < 29 wGAFootnote 41 Footnote 42 Footnote 43 Footnote 44 Footnote 45 Footnote 46 Footnote 47. These infants receive little or no maternal antibody and their narrower airway passages increase their vulnerability to the effects of RSV infection.
- There is good evidence that infants of 30-32 wGA are also at increased risk of RSVH in comparison to term infants but hospitalization rates are lower, at 5.1 in the systematic review of publications from 2014-2018 (BODsr) (see Section III.1.1), 5.7 – 9.9% in earlier literature Footnote 41 Footnote 42 Footnote 43 Footnote 45 Footnote 46 and 4.3 % in a more recent studyFootnote 38. There is fair evidence that RSVH rates for infants of 29-32 and 33-35 wGA are 4.6 and 2.8 times higher than in term infants, respectively (Section III.1.1). Earlier studies show inconsistent evidence on the risk of RSVH in infants of 32-35 wGA. Rates of 2.85 to 6.5% in the first year of life or first RSV season have been reported Footnote 40 Footnote 45 Footnote 48, while two more recent studies reported rates of 4.0 and 3.4%Footnote 38 Footnote 39. RSVH rate for healthy term infants in the BODsr was 1.2%.
- There is fair evidence that premature infants hospitalized for RSV have a longer LOS than term infants, with mean difference in LOS between premature and term infants of 7.97 days for infants of 29-32 wGA and 1.06 days for infants of 32/33-35 wGA. There is fair evidence that premature infants with RSVH have a higher rate of ICU admission than term infants, with RR of 4.0 for infants of 29-32 wGA and 3.0 for 32-35 wGA. There is fair evidence that premature infants of 29-35 wGA with RSVH have a higher rate of MV than term infants, with RR of 1.9 for infants of 29-32 wGA and 1.2 for 33-35 wGA.(Section III.1.1)
- There is fair evidence that chronological age is an important risk factor for RSVH, with most infections occurring in the first 2-3 months of lifeFootnote 16 Footnote 49.
- There is insufficient evidence of the effectiveness of PVZ in reducing risk of RSVH in premature infants born at < 30 wGA. three studies, two rated as good and one as fair, did not show a significant effect on RSVH in this group, but the numbers of participants were small (total 228 for the three studies). One larger study of premature infants born at ≤30 wGA, rated as poor quality, showed a reduction of 92% with NNT of 9.
- There is good evidence that PVZ is effective in reducing RSVH rates by 38-80% in premature infants of ≤32 wGA without CLD or hsCHD (NNT 53, 5, 17).
- There is conflicting evidence about the effect of PVZ on RSVH rates in premature infants born at 32-35 wGA without CLD or hsCHD. Two RCT and one observational study showed reductions of 55-82% (NNT 22, 24) and 55%, while 3 observational studies did not show a significant effect.
- There is fair evidence (one systematic review) of an association between PVZ receipt and lower all-cause mortality in infants born at ≤ 32 wGA but no evidence for an effect of PVZ on RSV specific mortalityFootnote 74.
- ICERs for preterm infants were < $50,000 per QALY in 82% of estimates (payer perspective) and were dominant (i.e. less costly and more effective) in infants of < 32 wGA (societal perspective). No specific trend was detected between wGA thresholds and ICERs, but numbers of estimates in the wGA groups were small. ICERs were <$50,000/QALY in 100% of estimates for infants of < 29wGA, 67% for 29-32 wGA, 100% for <32 wGA and for < 33 wGA and 67% for 32-35 wGA (payer perspective). In one Canadian study, ICERs were < $50,000 per QALY for infants of 32-35 wGA with high or moderate RSV risk scores (payer perspective).
- Although burden of illness is higher in infants of 30-35 wGA than in term infants and there is good evidence of PVZ effectiveness for those of 30-32 wGA, cost is of concern for PVZ use in these older gestational age groups. In Canada it is estimated that 8% of infants are born prematurelyFootnote 67, and that 5% of the birth cohort may be born at 32-35 wGAFootnote 34. Recommendations are based on providing prophylaxis for the premature infants at highest risk.
Recommendation 1.4: NACI recommends that PVZ should not be offered to infants or siblings of multiple births who do not otherwise qualify for prophylaxis. (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend against PVZ use in this population (Grade C evidence).
Summary of evidence and rationale:
- Most studies of twins and other multiple births have reported similar risks of RSVH in infants of multiple and singleton births, either withoutFootnote 71 Footnote 116 or afterFootnote 114 Footnote 117 adjustment for confounding factors.
- One study reported a higher rate of RSVH in infants of multiple births but potential confounding factors were not consideredFootnote 115.
- There are no data on PVZ use in this group.
- Evidence is based on review of key studies, without formal quality appraisal.
2. Chronic Lung Disease of Prematurity and other chronic lung diseases
Recommendation 2.1: NACI recommends that PVZ should be offered to infants with chronic lung disease of prematurity (defined as born at ≤32 wGA and need for supplemental O2 >21% for at least the first 28 days after birth) who are <24 months of age at the onset on the RSV season and have required ongoing supplemental O2 therapy in the 6 months prior to the onset of or during the RSV season. (Strong NACI Recommendation)
NACI concludes that there is good evidence to recommend PVZ use in this population (Grade A evidence).
Summary of evidence and rationale:
- RSVH rate for infants with CLD of prematurity in the first 2 years of life is high (12-21%) Footnote 42 Footnote 44 Footnote 48 Footnote 72. For hospitalized patients, high rates of ICU admission (29%) and MV (24%) have been reportedFootnote 72.
- There is good evidence that PVZ reduces RSVH in infants of ≤ 35 wGA with CLD age < 24 m (RD 39%, NNT 21)Footnote 48. There is fair evidence that PVZ reduces the rate of RSVH in infants with CLD during their first 6 months post initial discharge (RD 86% NNT13)Footnote 44 and poor evidence in infants with CLD aged < 6 m at onset of RSV season (RD 85%, 72%; NNT 3, 8)Footnote 46 Footnote 139. There is insufficient evidence of the effect of PVZ in infants with CLD aged < 12 months or 6-12 months. There is no evidence concerning the effect of PVZ on other hospitalization-related outcomes or RSV long term sequelae in infants with CLD. There is insufficient evidence that PVZ has an effect on all-cause mortality or RSV related mortality in children with CLD as numbers studied are insufficient to detect an effectFootnote 74.
- Studies on cost-effectiveness of PVZ prophylaxis reported ICERs of < $50,000 per QALY in all estimates (payer or society perspective); ICERs for infants discharged home on oxygen were < $50,000 per hospitalization avoided, and < $50,000 per life year gained.
Recommendation 2.2: NACI recommends that PVZ may be considered for children < 24 months of age with severe chronic lung disease of other etiology (e.g. congenital cystic lung disease, chronic interstitial lung disease, congenital lung malformations, congenital airway abnormalities or neuromuscular conditions affecting ability to clear airway secretions) or who require home respiratory support (e.g. supplemental O2, mechanical ventilation, continuous positive airway pressure, tracheostomy) if requiring ongoing supplemental O2 or assisted ventilation in the 6 months prior to the onset of or during the RSV season. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There is fair evidence for increased rates of RSVH in infants with chronic lung disease of etiology other than prematurity (congenital cystic lung disease 8.3%, chronic interstitial lung disease 30%, congenital lung and airway malformations 8.3-13.7%, and some neuromuscular conditions that affect ability to clear airway secretions 9.9-15.9%v Footnote 21 Footnote 75 Footnote 76.
- There is no evidence concerning the effect of PVZ on RSV disease in these conditions.
- It is postulated that infants with CLD of severity comparable to CLD of prematurity may benefit from PVZ.
3. Cystic fibrosis:
Recommendation 3.1: NACI recommends that PVZ should not be offered routinely to children < 24 months of age with cystic fibrosis. (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend against routine PVZ use in this population (Grade D evidence).
Summary of evidence and rationale:
- RSVH occurs more frequently in children with CF than in healthy children. RSVH in the systematic review was 12.3% (Section III.1.3). There are limited data about other hospitalization related outcomes.
- There is inconsistent evidence on the effect of routine administration of PVZ to infants with CF on RSVH, with all but one study showing no effect Footnote 77 Footnote 78 Footnote 140 Footnote 142 Footnote 143 Footnote 144.
- There is fair evidence that routine administration of PVZ to infants with CF does not significantly affect long term pulmonary function, growth or airway bacterial colonization Footnote 78 Footnote 140 Footnote 144 Footnote 145.
- One Canadian study estimated an ICER of over $600,000 per QALY (payer perspective) for routine PVZ prophylaxis in infants with cystic fibrosisFootnote 189.
Recommendation 3.2: NACI recommends that PVZ may be considered for children < 24 months of age with cystic fibrosis who have severe chronic lung disease as defined by need for ongoing supplemental oxygen in the 6 months prior to the onset of or during the RSV season. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend use in this population. (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There is no evidence on the burden of RSV illness in the subgroup of infants with CF with severe chronic lung disease in infancy.
- There is no evidence concerning the effect of PVZ prophylaxis on RSV disease in this subgroup.
- It is postulated that infants with CF lung disease of severity comparable to CLD of prematurity may benefit from PVZ.
4. Congenital heart disease and other chronic cardiopathy:
Recommendation 4.1: NACI recommends that PVZ should be offered to infants with haemodynamically significant CHD (as assessed by a paediatric cardiologist) who are < 1 year of age at the onset of the RSV season. (Strong NACI Recommendation)
NACI concludes that there is good evidence to recommend PVZ use in this population (Grade A evidence)
Summary of evidence and rationale:
- There is good evidence that children < 24 months of age with hsCHD are at increased risk for RSVH with rates of 2.3-10.2% reportedFootnote 65 Footnote 79 Footnote 80.
- There is good evidence that the RSVH rates for infants with CHD is significantly higher in the first year of life than the second yearFootnote 43 Footnote 79 Footnote 81.
- There is good evidence that PVZ reduces the risk of RSVH in children with hsCHD aged < 24 months (RD 45%, NNT 23)Footnote 80. There is good evidence that PVZ reduces the risk of RSVH in children with hsCHD aged < 6 months (RD 51%, NNT 16) and fair evidence in children aged <12 months (RD 49%-72%, NNT 45, 7)Footnote 44 Footnote 80 Footnote 147. There is good evidence that PVZ reduces the overall number of days of hospitalization for RSV in children with hsCHDFootnote 80 but not the LOS for those admitted with RSVFootnote 80 Footnote 146, and good evidence that PVZ does not affect the proportion of hospitalized children admitted to ICU, the duration of ICU stay, or the proportion requiring MVFootnote 80 Footnote 146 Footnote 148. There is insufficient evidence on the effect of PVZ on all-cause mortality or RSV mortality in children with hsCHDFootnote 80 Footnote 148.
- Studies on cost-effectiveness of PVZ prophylaxis reported ICERs of < $50,000 per QALY in 80% of estimates (payer perspective) and 63% of estimates (societal perspective). An ICER of $18,155 per day of hospitalization avoided was estimated in a Canadian studyFootnote 148.
Recommendation 4.2: NACI recommends that PVZ may be considered for infants < 1 year of age at the onset of the RSV season who have haemodynamically significant chronic cardiopathy (as assessed by a paediatric cardiologist) of other etiology. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There is no evidence about the burden of RSV illness or the use of PVZ in this group.
- It is postulated that infants with cardiac dysfunction of severity similar to that of children with haemodynamically significant CHD may benefit from PVZ.
Recommendation 4.3: NACI recommends that PVZ may be considered for children 12-24 months of age at the onset of the RSV season if they are awaiting heart transplantation or have received a heart transplant in the previous 6 months. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There is no evidence about the burden of RSV illness or the use of PVZ in this group.
- It is postulated that these infants will have severe cardiac dysfunction and will likely receive immunosuppressive therapy during the RSV season and that they may benefit from PVZ.
Recommendation 4.4: NACI recommends that for children with both haemodynamically significant CHD and chronic lung disease, recommendations for chronic lung disease (above) should be followed. (Strong NACI Recommendation)
NACI concludes that there is insufficient evidence to support a recommendation for this population (Grade I evidence)
Summary of evidence and rationale:
- There are no data on burden of RSV illness or effectiveness of PVZ for this group.
- Chronic lung disease may warrant prophylaxis for a second RSV season whereas hsCHD alone usually will not.
5. Down syndrome:
Recommendation 5.1: NACI recommends that PVZ should not be offered routinely to children < 24 months of age with Down syndrome. (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend against routine PVZ use in this population (Grade D evidence).
Summary of evidence and rationale:
- RSVH occurs more frequently in children with Down syndrome without hsCHD, CLD or prematurity than in healthy children. There are limited data about other hospitalization related outcomesFootnote 22 Footnote 83.
- Three studies of PVZ prophylaxis in infants with Down syndrome and without hsCHD, CLD or prematurity showed no effect on RSVH Footnote 149 Footnote 150 Footnote 151.
Recommendation 5.2: NACI recommends that PVZ should be offered to children with Down syndrome who qualify for prophylaxis because of hsCHD, chronic lung disease, prematurity or immunodeficiency. (Strong NACI Recommendation)
NACI concludes that there is fair evidence to recommend PVZ use in this population (Grade B evidence).
Summary of evidence and rationale:
- See evidence for hsCHD, chronic lung disease, prematurity or immunodeficiency, above.
- One study found reduction in RSVH rates in infants with Down syndrome who met standard criteria for receipt of PVZFootnote 150.
6. Immunocompromised Children:
Recommendation 6.1: NACI recommends that PVZ may be considered for children <24 months of age who are severely immunocompromised. (Discretionary NACI Recommendation)
NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There are little population based data on the burden of RSV disease in immunocompromised children. Increased rates of RSVH have been reported in children <24 months old with primary immunodeficiencies (21.3%) and cancer (8.4%)Footnote 21.
- Limited data suggests that children aged ≤24 months and those with absolute lymphocyte counts of < 100 / mm3 are at highest risk of severe RSV disease Footnote 85 Footnote 87 Footnote 88.
- No studies were identified that assessed the effectiveness of PVZ prophylaxis in immunocompromised children.
7. Children Residing in Remote Communities
Recommendation 7.1: NACI recommends that PVZ should be offered to children <36 wGA and < 6 months of age living in remote northern Inuit communities who would require air transport for hospitalization. (Strong NACI recommendation)
NACI concludes that there is fair evidence to recommend PVZ use in this population (Grade B evidence).
Summary of evidence and rationale:
- There is good evidence that premature infants living in remote northern Inuit communities have very high rates of RSVH and frequently require air transfer to tertiary care institutionsFootnote 23 Footnote 91 Footnote 92.
- There is poor quality evidence of the effectiveness of PVZ on RSVH rates in premature Inuit infants (NNT 4, 2)Footnote 92 Footnote 152.
Recommendation 7.2: NACI recommends that PVZ should not be routinely offered to healthy full term infants living in remote northern Inuit communities. (Strong NACI Recommendation)
- NACI concludes that there insufficient evidence to recommend routine PVZ prophylaxis in this population. (Grade I evidence). Therefore this recommendation is based on expert opinion. NACI will continue to monitor the evidence as it evolves.
Summary of evidence and rationale:
- Rates of RSVH in such communities vary widely by community and by year Footnote 23 Footnote 90 Footnote 91 Footnote 92.
- There is one study of fair quality showing no effect of PVZ prophylaxis on RSVH in healthy full term infants living in a northern Inuit population in Canada with rate of RSVH in all infants < 1 year of age of 5%Footnote 90.
- A qualitative study of PVZ prophylaxis in healthy full term infants living in one northern Inuit population in Canada identified significant acceptability and feasibility issuesFootnote 207.
Recommendation 7.3: NACI recommends that PVZ prophylaxis may be considered for healthy full term infants aged <6 months at the onset of, or during, the RSV season living in remote northern Inuit communities with documented very high RSV hospitalization rates for term infants. (Discretionary NACI Recommendation)
- NACI concludes that there is insufficient evidence to make a recommendation for or against PVZ use in healthy term infants living in remote northern Inuit communities with very high RSV hospitalization rates (Grade I evidence). Therefore, this recommendation is based on expert opinion, with consideration of the high burden of illness in these communities and need for air transport if hospitalization or specialized ambulatory care is required. NACI will continue to monitor the evidence as it evolves.
Summary of evidence and rationale:
- Term infants living in some remote northern Inuit communities have very high rates of RSVH and frequently require air transfer to tertiary care institutionsFootnote 23 Footnote 91 Footnote 92. Rates of RSVH as high as 20% to 50% of all live births have been reported in some remote communities.
- There are no studies of PVZ prophylaxis in healthy term infants living in remote northern Inuit communities with very high RSVH rates.
- Studies of cost-effectiveness of PVZ prophylaxis estimated ICERs of < $50,000 per QALY for term infants residing in select communities in the Eastern Canadian Arctic with high RSV hospitalization rates, whereas PVZ was dominant (i.e. less costly and more effective) in other select communities. However, these estimates used data for PVZ effectiveness from premature infants and effectiveness in term infants is yet to be establishedFootnote 196.
- A qualitative study of PVZ prophylaxis in healthy full term infants living in one northern Inuit population in Canada identified significant acceptability and feasibility challengesFootnote 207.
Recommendation 7.4: NACI recommends that PVZ may be considered for infants < 36 wGA and age < 6 months living in other remote communities with documented high rates of hospitalization for RSV who would require air transport for hospitalization. (Discretionary NACI Recommendation)
- NACI concludes that there is insufficient evidence to recommend PVZ use in this population (Grade I evidence). Therefore this recommendation is based on expert opinion.
Summary of evidence and rationale:
- There is limited evidence on the burden of RSV disease in infants living in other remote aboriginal communities in North America and no evidence for those in other remote communities.
- There is no evidence on the effect of PVZ on RSV disease in these communities. One study of motavizumab, another RSV monoclonal antibody, reported a 87% relative reduction in risk of RSVH in healthy term Native American infants living on reservations in southwestern USAFootnote 89.
8. Prevention of Subsequent Recurrent Wheezing
Recommendation 8.1: NACI recommends that PVZ should not be used for the prevention of recurrent wheezing or asthma in the absence of other indications. (Strong NACI Recommendation)
- NACI concludes that there is insufficient evidence to recommend PVZ use for prevention of this outcome (Grade I evidence). Therefore this recommendation is based on expert opinion.
Summary of evidence and rationale:
- It is not known whether RSV in infancy predisposes to the development of asthma, or if infants genetically predisposed to develop asthma are at increased risk of severe RSV disease requiring RSVH in infancy, is not known.
- Recurrent wheezing in childhood occurs in healthy term infants hospitalized for RSV in infancy in proportions similar to those reported for infants at high risk of RSVH in infancyFootnote 29.
- Although PVZ administration to infants born at < 36 wGA has an impact on physician diagnosed recurrent wheezing in the first 1- 6 years of life (NNT 3 to 15), findings are contradictory as to PVZ effectiveness in the absence or presence of a family history of atopy Footnote 111 Footnote 134 Footnote 135 Footnote 136 Footnote 137 Footnote 138.
- There are no data on the effect of early receipt of PVZ on subsequent wheezing or asthma in children over 7 years of age or in adults.
9. Use of PVZ in hospitalized infants
Recommendation 9.1: NACI recommends that PVZ should not routinely be used to control or prevent RSV infections in neonatal intensive care (NICU) or other hospital units. (Strong NACI Recommendation)
- NACI concludes that there is fair evidence to recommend against PVZ use in this population (Grade D evidence).
Summary of evidence and rationale:
- Studies showed that RSV infection rates in NICU did not differ when infants received PVZ prophylaxis in the NICU or starting at hospital discharge Footnote 119 Footnote 120 Footnote 121.
Recommendation 9.2: NACI recommends that PVZ prophylaxis may be considered when all other measures to control an RSV outbreak in a NICU have failed. (Discretionary NACI Recommendation)
- NACI concludes that there is insufficient evidence to recommend PVZ use in this situation (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- PVZ, in addition to other infection control measures, has been used to control NICU outbreaks, but the specific role played by PVZ is unclear Footnote 118 Footnote 124 Footnote 125 Footnote 126 Footnote 127 Footnote 128.
Recommendation 9.3: NACI recommends that infants who qualify for PVZ prophylaxis and are discharged from hospital during RSV season should receive their first dose 48-72 hours before discharge home if possible, or promptly after discharge. (Strong NACI Recommendation)
- NACI concludes that there is insufficient evidence to recommend PVZ use in this situation (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- Administering the first dose before discharge avoids the need of a visit to a health care facility soon after discharge and may improve adherence.
- In hospital, to avoid wastage when vials are opened for individual infants, administration may be coordinated to 3 times weekly.
Recommendation 9.4: NACI recommends that an infant who has begun PVZ prophylaxis earlier in the season and is re-hospitalized on the date when a dose is due should receive that dose as scheduled, providing that the admitting institution is able to supply PVZ when due. (Strong NACI Recommendation)
- NACI concludes that there is insufficient evidence to recommend PVZ use in this situation (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- Keeping to the child's existing PVZ schedule avoids the need to reschedule appointments and may improve adherence.
10. PVZ dosing:
Recommendation 10.1: NACI recommends that PVZ should be given at a dose of 15 mg/kg by intramuscular injection. The first dose should be given at the onset of the current RSV season, as determined by local laboratory data or pediatric hospitalization data. If these data are not available in a timely fashion, the start date may be pre-determined based on dates of previous local RSV seasons. The interval between the first and second doses should be 21-28 days and between further doses should be 28-35 days. (Strong NACI Recommendation)
- NACI concludes that there is fair evidence for this PVZ schedule (Grade B evidence).
Summary of evidence and rationale:
- A dose of 15 mg/kg every 30 days resulted in target serum PVZ levels assumed to be protective based on animal studiesFootnote 162.
- Longer dose intervals have been used based on a PVZ half-life of 19-27 days and observed accumulation of PVZ after the second dose Footnote 48 Footnote 164 Footnote 166 Footnote 167.
- Evidence is based on review of key studies, without formal quality appraisal.
Recommendation 10.2: NACI recommends that a maximum of 4 doses should be administered, with the following exceptions: (Strong NACI Recommendation)
- If a child undergoes cardiac bypass and will continue to need PVZ after surgery, a dose should be given as soon as feasible after bypass
- If a child undergoes extracorporeal membrane oxygenation and will continue to require PVZ, a dose should be given at conclusion of the procedure
- An extra dose may also be considered in remote Northern areas where RSV outbreaks may continue longer than is usual elsewhere
- NACI concludes that there is insufficient evidence to determine the optimum number of PVZ doses (Grade I evidence). Therefore, this recommendation is based on expert opinion.
Summary of evidence and rationale:
- Studies suggest that 4 doses are sufficient to provide protection throughout the usual RSV season Footnote 166 Footnote 167 Footnote 168 Footnote 169.
- A study of children undergoing cardiac bypass reported a 58% decrease in PVZ level after bypassFootnote 80. It is assumed that extracorporeal membrane oxygenation may have a similar effectFootnote 6.
- Dose sparing can be achieved by:
- Starting PVZ only when the local RSV season has begunFootnote 173 Footnote 174;
- Favoring the longer interval between doses after dose 2;
- Organizing clinics or appointments for PVZ administration that facilitate vial sharing.
- Evidence is based on review of key studies, without formal quality appraisal.
Recommendation 10.3: NACI recommends that PVZ should be discontinued for the season if a child is hospitalized because of RSV infection. (Strong NACI Recommendation). NACI concludes that there is fair evidence that recurrent severe RSV infections in a single season are rare (Grade B evidence).
Summary of evidence and rationale:
- Reported rates of second episodes of RSVH in the same season vary from in 0% to 1.0% of the cohort studied Footnote 80 Footnote 108 Footnote 109 Footnote 110 Footnote 111, except for a rate of 3.3% in a very small study in 1988Footnote 107.
- Evidence is based on review of key studies, without formal quality appraisal.
Recommendations for individual level decision-making
(For example, individuals wishing to prevent RSV disease or a clinician wishing to advise individual patients with conditions not currently included in public health programs about preventing RSV).
PVZ is not readily available for private purchase in Canada, is costly, and cost may or may not be reimbursed by private insurance plans. No specific recommendations are made for individual level decision-making.
The recommendations provided above may be applied to public health program level decision-making. See the Management Options Table, below.
Management options table
(Recommendations for public health program level decision-making).
Various options for the use of PVZ, and the decision on which options are preferable will depend on the considerations listed below:
| Options | Considerations | Decision Points |
|---|---|---|
Cohorts at risk: |
PVZ, a monoclonal antibody that provides temporary passive protection against severe RSV infection, is the only prophylaxis presently available. PVZ has only been investigated in children < 24 months old with underlying conditions putting them at increased risk for severe RSV illness and is not recommended for healthy term infants or for individuals over 24 months old. |
Epidemiology Risk of severe RSV illness is influenced by gestational age at birth, underlying health conditions, and age. Infants are at highest risk of severe RSV disease in their 1st RSV season and especially at age < 3 months.
RSV causes yearly epidemics from winter to early spring
Safety PVZ is safe, with few adverse effects other than transient local reactions. two cases of anaphylaxis were reported after more than 2,000,000 doses of PVZ administered. Economics: PVZ is costly, and the main cost of prophylaxis programs is the product itself. Studies reported a wide range of ICERs depending on the population, setting, baseline hospitalization rates, as well as model structure and study design. Estimated ICERs of <$50,000 per QALY have been reported in selected scenarios but dominant (i.e. less costly and more effective) in very few. Unlike vaccines, PVZ dose varies with weight. Once opened, a vial must be used that day or discarded.
With no evidence of lowered mortality rates from RSV or of long term benefit from PVZ, the high cost of PVZ prophylaxis must be balanced against costs of other health care interventions if these interventions may be compromised by provision of PVZ programs. |
1. Otherwise healthy premature infants: |
Otherwise healthy premature infants have increased risk of severe RSV infection in comparison with term infants. Risk of hospitalization is highest in those < 30 wGA (7.7 to 13%) although also increased in those of 29-32 and 33-35 wGA (4.6 and 2-3 times that of term infants). PVZ was effective in preventing hospitalization in studies of infants of ≤32 wGA (rate decrease 38-74%, NNT 9 to 54 in different studies). For infants of 32-35 wGA rate decreases of 72-83% with NNT of 12-14 were reported but some studies showed no effect. Studies specific to infants of < 29 wGA did not show an effect but numbers studied were very small. In Canada 7.7-8% of births are at < 37 wGA and an estimated 5% are 32-35 wGA. Cost-effectiveness studies of PVZ prophylaxis for otherwise healthy premature infants reported ICERs from $6,216/QALY to $938,623/QALY with a trend towards greater ICERs with increasing gestational age. No estimates were dominant (i.e. less costly and more effective) and 82% of estimates showed ICERs of <$50,000/QALY. |
|
2. Children with chronic lung disease of prematurity or of other etiology: Use of PVZ may be individualized depending on the severity of the chronic lung disease (e.g. oxygen dependence) |
Children with CLD of prematurity have a 12-21% risk of hospitalization for RSV. PVZ is effective to prevent hospitalization (rate reduction 39% and NNT 21 in the first 2 years of life, 86%, NNT 13 in the first year). There are data on increased rates of RSV hospitalization in chronic lung disease of other etiologies but PVZ has not been investigated. There are data that children with cystic fibrosis have an increased risk of RSV hospitalization but studies to date suggest that PVZ is not protective. Cost-effectiveness of PVZ prophylaxis for children with chronic lung disease of prematurity reported ICERs from $4,786/QALY to $46,821/QALY. No estimates were dominant (i.e. less costly and more effective). |
|
3. Children with haemodynamically significant CHD or haemodynamically significant heart disease of other etiology: Use of PVZ may be individualized depending on the severity of the cardiac dysfunction |
Children with haemodynamically significant CHD have a 9.7 % risk of hospitalization for RSV, with almost all infections occurring in the first year of life. PVZ is effective to prevent hospitalization (rate reduction 45-72%, NNT 7-45) in most studies, although two small studies showed no effect. There are no data on RSV disease and PVZ use in children with haemodynamically significant heart disease of other etiology. Cost-effectiveness of PVZ prophylaxis for children with haemodynamically significant CHD reported ICERs from $11,668/QALY to $164,946/QALY. No estimates were dominant (i.e. less costly and more effective) and 80% of estimates showed costs of < $50,000/QALY. |
|
4. Down syndrome, Immunocompromised and other chronic conditions |
Recommendations are based on PVZ effectiveness and risk of severe RSV disease in different risk groups. For certain very rare conditions, risk of severe RSV illness may be high but epidemiologic data are not available. Likewise, the number of children with certain rare diseases is not sufficient for PVZ effectiveness to be studied. In these circumstances, extrapolation may be made from data on conditions of pathophysiological similarity with documented increased risk of RSV and PVZ effectiveness. No studies of cost-effectiveness of PVZ prophylaxis were identified for these populations. |
|
5. Use of PVZ for preterm infants of <37 wGA or for term infants living in remote Inuit communities Use of PVZ in term infants may be based on local rates of hospitalization of term infants with RSV and costs of transport to distant hospitals |
Studies indicate that children living in some remote Inuit communities, including term infants, are at high risk of RSV hospitalization. Limited data suggests that PVZ reduces RSV hospitalization of infants of <37 wGA living in remote Inuit communities (rate reduction 96%, 66%, NNT 2,4). One study offering PVZ to term Inuit infants in an area where baseline rate of RSVH was not very high showed no effect. Canadian modelling has suggested that PVZ prophylaxis for term infants may be dominant (i.e. less costly and more effective) in remote Inuit communities with very high baseline RSV hospitalization rates. ICERs were <$50,000/QALY in 75% of estimates, but efficacy was based on studies of preterm infants |
|
6. Use of PVZ for term infants living in other remote aboriginal or other remote communities Use of PVZ in term infants may be based on local rates of hospitalization of term infants with RSV and costs of transport to distant hospitals |
Limited data suggest that RSV hospitalization rates may be increased in other isolated aboriginal communities. There are no data from Canada. There are no data on PVZ use in these communities. |
Research priorities
Research to address the following outstanding questions is encouraged:
- Serological correlate of protection:
- Determination of the minimum antibody level required to protect against severe RSV infection in humans and development of a commercially available test for RSV antibody would permit more judicious use of costly monoclonal antibody products, as many infants will develop natural antibody during their first or second year of life.
- RSV monoclonal antibody efficacy/effectiveness in infants living in remote communities, especially in Inuit infants in the far North:
- There is (good) evidence of a high burden of RSV disease in Inuit infants in the far North but limited data on the effectiveness of PVZ to prevent hospitalization and the need for air transfer.
- Burden of RSV disease in infants with Down syndrome and efficacy/effectiveness of RSV monoclonal antibody to prevent hospitalization in this population:
- The literature suggests that infants with Down syndrome without recognized clinical criteria for PVZ prophylaxis may have high rates of RSV hospitalization. The reasons for this susceptibility are not clear but may relate to immunodeficiency in this population. There is very limited data on the use of PVZ infants with Down syndrome.
- Efficacy/effectiveness of RSV monoclonal antibody in otherwise healthy premature infants born at < 29 wGA:
- Studies of the efficacy/effectiveness of PVZ prophylaxis in severely premature infants of < 29 wGA failed to show protection, but the numbers of infants studied were very small. Such studies could not be done in countries where PVZ is now recommended for these infants. Note that UK and Switzerland do not recommend PVZ for healthy premature infants.
Surveillance issues
Epidemiology:
- Development of a RSV surveillance system with data for each province and territory, analogous to FluWatch, could provide timely data on which to determine when RSV monoclonal antibody prophylaxis programs should most efficiently begin and end.
- Studies of the burden of severe RSV disease in immunocompromised populations, stratified by age group (especially focusing on those ≤ 2 years of age) and by severity of immunosuppression (especially focusing on those with antibody deficiencies, as these individuals may not benefit from RSV vaccines in the future and thus may continue to warrant RSV monoclonal passive prophylaxis).
Ranking individual studies, strength of recommendations, grade of evidence
| Level | Description |
|---|---|
| I | Evidence from randomized controlled trial(s). |
| II-1 | Evidence from controlled trial(s) without randomization. |
| II-2 | Evidence from cohort or case-control analytic studies, preferably from more than one centre or research group using clinical outcome measures of vaccine efficacy. |
| II-3 | Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence. |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees. |
| Quality Rating | Description |
|---|---|
Good |
A study (including meta-analyses or systematic reviews) that meets all design- specific criteriaTable 12 Footnote * well. |
Fair |
A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criterionTable 12 Footnote * but has no known "fatal flaw". |
Poor |
A study (including meta-analyses or systematic reviews) that has at least one design-specificTable 12 Footnote * "fatal flaw", or an accumulation of lesser flaws to the extent that the results of the study are not deemed able to inform recommendations. |
|
|
| Strength of naci recommendation | Grade of evidence |
|---|---|
| Based on factors not isolated to strength of evidence (e.g. public health need) | Based on assessment of the body of evidence (as summarized in the Summary of Evidence Table, Table 1, where the level and quality of individual studies is assessed) |
| Strong "should/should not be offered"
|
A – good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making | |
| Discretionary "may be considered"
|
A – good evidence to recommend |
| B – fair evidence to recommend | |
| C – conflicting evidence, however other factors may influence decision-making | |
| D – fair evidence to recommend against | |
| E – good evidence to recommend against | |
| I – insufficient evidence (in quality or quantity), however other factors may influence decision-making |
List of abbreviations
- AAP
- American Academy of Pediatrics
- AEs
- Adverse events
- AMSTAR
- A Measurement Tool to Assess Systematic Reviews
- ARCHE
- Alberta Research Centre for Health Evidence
- BODsr
- Burden of RSV disease in young children
- BPD
- Bronchopulmonary dysplasia
- CAD
- Canadian dollars
- CCLD
- Congenital cystic lung disease
- CF
- Cystic fibrosis
- CHD
- Congenital heart disease
- CHILD
- Chronic interstitial lung disease
- CI
- Confidence interval
- CIG
- Canadian Immunization Guide
- CLD
- Chronic lung disease
- COE
- Certainty of evidence
- CPS
- Canadian Paediatric Society
- EEFA
- Ethics, equity, feasibility, and acceptability
- FEV1
- Force Expiratory Volume in one minute
- FVC
- Forced Vital Capacity
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HA
- Hospitalizations avoided
- hsCHD
- Hemodynamically significant congenital heart disease
- ICER
- Incremental cost-effectiveness ratio
- IQR
- Interquartile range
- IRR
- Incidence rate ratio
- LOS
- Length of hospital stay
- LY
- Life year
- MEF
- Maximum Expiratory Flow
- MV
- Mechanical ventilation
- NACI
- National Advisory Committee on Immunization
- NICU
- Neonatal intensive care (unit?)
- NNT
- Number needed to treat
- NT
- Neutralization titre
- NVK
- Dutch Association for Pediatrics
- O2
- Oxygen
- OR
- Odds ratio
- PHAC
- Public Health Agency of Canada
- PT
- Provinces and territories
- PVZ
- Palivizumab
- QALY
- Quality-adjusted life year
- QUIPS
- Quality in Prognosis Studies
- RD
- Risk difference
- ROB
- Risk of bias
- RSV
- Respiratory syncytial virus
- RSVH
- RSV hospitalization
- SAE
- Serious adverse event
- SD
- Standard deviation
- SENeo
- Spanish Neonatology Society
- SOP
- Standard operating procedures
- wGA
- Weeks gestational age
Acknowledgments
This statement was prepared by: D Moore, A Sinilaite, R Stirling, MW Yeung on behalf of the NACI RSV Working Group and approved by NACI.
NACI gratefully acknowledges the contribution of: P Doyon-Plourde, S Duschesne-Belanger, E Poirier, A House, SJ Ismail, A Sumner, C Tremblay, MC Tunis, V Mouajou Feujio, L Zhao, A Killikelly, N St-Pierre as well as the research team at the Alberta Research Centre for Health Evidence (ARCHE), including J Pillay, A Wingert, and L Hartling
NACI RSV Working Group
Members: D Moore (Chair), M Salvadori, V Dubey, J Papenburg, J Robinson
Former Members: S Gantt, W Vaudry
PHAC Participants: S Duschesne-Belanger, A Killikelly, R Pless, A Sinilaite, R Stirling, A Sumner, MC Tunis, MY Yeung, and L Zhao
NACI
Members: S Deeks (Chair), R Harrison (Vice-Chair), J Bettinger, N Brousseau, P De Wals, E Dubé, V Dubey, K Hildebrand, K Klein, J Papenburg, C Rotstein, B Sander, S Smith, and S Wilson.
Former member: C Quach (Chair)
Liaison representatives: LM Bucci (Canadian Public Health Association), E Castillo (Society of Obstetricians and Gynaecologists of Canada), A Cohn (Centers for Disease Control and Prevention, United States), L Dupuis (Canadian Nurses Association), J Emili (College of Family Physicians of Canada), D Fell (Canadian Association for Immunization Research and Evaluation), M Lavoie (Council of Chief Medical Officers of Health), D Moore (Canadian Paediatric Society), Dr. M Naus (Canadian Immunization Committee), A Pham-Huy (Association of Medical Microbiology and Infectious Disease Canada), P Emberley (Canadian Pharmacists Association), L Bill (Canadian Indigenous Nurses Association), and Dr. S Funnel (Indigenous Physicians Association of Canada). Ex-officio representatives: K Robinson (Marketed Health Products Directorate, HC), E Henry (Centre for Immunization and Respiratory Infectious Diseases [CIRID], PHAC), M Lacroix (Public Health Ethics Consultative Group, PHAC), S Ogunnaike-Cooke (CIRID, PHAC), C Lourenco (Biologic and Radiopharmaceutical Drugs Directorate, Health Canada), G Poliquin (National Microbiology Laboratory, PHAC), V Beswick-Escanlar (National Defence and the Canadian Armed Forces), and T Wong (First Nations and Inuit Health Branch, Indigenous Services Canada).
Appendix A: Current criteria for receipt of Palivizumab in Canadian provinces and territories and internationally
Eligibility criteria for PVZ (PVZ) prophylaxis were obtained from all Canadian provinces and territories and from 10 northern hemisphere countries. Data are summarized in the table below.
Canada:
Premature infants without chronic lung disease or hemodynamically significant congenital heart disease (hsCHD)
NACI in 2003 recommended PVZ prophylaxis for infants of ≤ 32 weeks gestational age (wGA) and age < 6 months at the start of the RSV season. The current Canadian Immunization Guide (CIG) states that selected infants of 33-35 wGA may also benefit, based on local considerations. The Canadian Paediatric Society (CPS) in 2015 stated that it is reasonable but not essential to offer prophylaxis to premature infants born at < 30 wGA and aged <6 months.
Six provinces and territories (PT) followed the current CIG recommendations for infants ≤ 32 wGA and selected infants of 33-35 wGA (AB, MB, NB, NT, ON, SK). All 6 PT used defined risk scores to determine eligibility for this group, but the risk criteria and scoring systems used varied across all PT. Two PT offered prophylaxis for those ≤ 29 wGA and for those 29-35 wGA with risk factors (BC, YT). One territory offered PVZ for all < 36 wGA (NU).Only one province followed the NACI recommendation (QC). Three provinces followed the CPS recommendation of prophylaxis for those < 30 wGA (NL, NS, PE).
Chronic lung disease of prematurity (CLD) and other chronic lung conditions
In 2003, NACI recommended PVZ for children age < 24 months at the start of the RSV season with CLD requiring therapy in the previous 6 months or with other pulmonary disorders requiring oxygen therapy, while the current CIG only mentions children with CLD. CPS recommends prophylaxis for those with CLD of age < 12 months at the start of the RSV season who require ongoing treatment, but for their second RSV season only if still requiring supplemental oxygen or weaned off oxygen in the previous 3 months. Children with cystic fibrosis, upper airway obstruction, or chronic pulmonary disorders other than CLD should not be offered prophylaxis routinely, but it may be considered for those < 24 months old who are on home oxygen or have had a prolonged hospitalization for severe pulmonary disease.
Eight PT followed the NACI recommendation of prophylaxis for children with CLD (AB, MB, NB, NS, ON, PE, QC, SK) while in three PT infants were eligible only to age 12 months (BC, NL, YT). In one territory all infants with CLD and age < 12 months old and those 12-24 months requiring treatment the previous 3 months were eligible (NU) while in another selected infants with CHD who were < 36 wGA and age < 24 months were eligible only a case-by-case basis (NT).
Nine PT provided prophylaxis for other chronic pulmonary conditions for infants of age <24 months (8) or <12 months (1), with some PT requiring individual assessment. Conditions included cystic fibrosis (7), congenital lung or airway abnormalities (4), and neuromuscular conditions affecting ability to clear airway secretions (5). Other conditions included were requirement for home respiratory support (O2, mechanical ventilation, tracheostomy, CPAP) and other severe pulmonary disability.
Congenital heart disease
NACI in 2003 and the current CIG recommend prophylaxis for children with hsCHD and age < 24 months. CPS recommends prophylaxis for those of age <12 months only.
Six PT offered prophylaxis for children with hsCHD aged < 24 months (AB, NB, NT, NS, PE, SK), 4 for those < 12 months and for 12-24 months after individual assessment (BC, MB, ON, YK). Three limited prophylaxis to the first 12 months (NL, NU, QC).
Other clinical conditions:
CPS states that prophylaxis may be considered for children < 24 months old with Down syndrome or immunodeficiency if they are on home oxygen, have had a prolonged hospitalization for severe pulmonary disease, or are severely immunocompromised.
Ten PT listed other clinical criteria for prophylaxis, some requiring individual assessment. Seven offered prophylaxis for Down syndrome (1 requiring additional comorbidity); eight for immunodeficiency (degree of severity varied), and one for neuromuscular conditions without mention of clearance of respiratory secretions.
In four PT, prophylaxis was offered to siblings of a multiple birth if one sibling qualified for prophylaxis (AB, BC, ON, YK), in all but one (ON) only if infants were premature. In one province, all infants of a multiple birth (other than twins), who were of ≤ 356/7 wGA and < 3 months old were eligible for prophylaxis (AB). In another, a twin of an approved child may be eligible after assessment (NT).
In all but two PT (NB, YK), protocols stated that other medical conditions may be considered on request after individual assessment.
Remote areas:
Five provinces had specific criteria for children living in remote Northern areas (MB, NL, ON, QC, SK) while 4 other PT (AB, BC, NT, YT) considered remote areas in risk scores. One territory offered PVZ for all < 36 wGA (NU). Most included infants of ≤36 wGA and < 6 months of age. One included term infants of < 3 months age (QC).
Defining RSV season and PVZ Dosing:
In six PT (AB, BC, ON, SK, YT, NT) the period for RSV prophylaxis was based on local RSV epidemiology and in five (NL, NS, PE, QC, NU) fixed dates were used. No information was found for two PT.
The recommended interval between doses of PVZ was 28 days in six PT (NS, NU, NT, PE, QC,SK) and monthly in one (NB). In AB the recommended intervals were 28 days in Northern AB but 21 days for the second dose and 28 days for subsequent doses in Southern AB. BC and ON, the recommended intervals were 21-28 days for the second dose and 28-35 days for subsequent doses while in NL the recommended interval for the second dose was 28 days and for subsequent doses 35 days. In YK the interval for the second dose was 18-24 days and the subsequent doses 28-30 days. The recommended interval in MB was 28 days up to the fourth dose, 35 days between doses 4 and 5 and 42 days between doses 5 and 6.
The maximum number of doses was 5 in 7 PT (AB, NB, NS, PE, ON, QC, SK), 6 in one (MB), 6 with extension based on local epidemiology in one (NU), and 4 in one (NL). In BC the maximum number of doses was 4 for infants of < 29 wGA and those with CLD or hsCHD, and 3 for premature infants of ≥29 wGA and no CLD or hsCHD. Two did not state a maximum (YK, NT).
International:
Premature infants without chronic lung disease or hemodynamically significant congenial heart disease (hsCHD).
Three countries used gestational age alone with varying wGA limits: < 26 (Sweden), < 29 (US) and <32 (Netherlands). Four countries (Austria, Germany, Italy, Spain) recommended prophylaxis for all infants below a specific wGA (< 28 to <31), and for less premature infants (up to 34 to 36 wGA) using risk scores. Three countries (France, Switzerland, UK) did not provide prophylaxis for prematurity alone.
Chronic lung disease of prematurity (CLD) and other chronic lung conditions
All 10 countries recommended prophylaxis for infants with chronic lung disease of prematurity. Eight countries, all but Switzerland and the UK, included those age < 24 months requiring treatment in the previous 6 months, with 5 of these including all infants < 12 months and one including all infants < 6 months old regardless of treatment. Switzerland recommended prophylaxis only for those < 1 year old. The UK recommended prophylaxis using a gestational age and chronological age grid which encompassed infants of ≤ 34 wGA and age 9 to 1.5 months.
Eight countries, all but France and Spain, also recommended prophylaxis for children aged < 1 or < 2 years with other pulmonary conditions, either routinely or on individual assessment. These included cystic fibrosis in 5 countries, neuromuscular conditions interfering with clearing of respiratory secretions in 2, congenital anomalies of the respiratory tract or lung in 4, and other conditions such as chronic pulmonary conditions requiring long term need for oxygen therapy, mechanical ventilation or tracheostomy.
Congenital heart disease
All ten countries recommended prophylaxis for infants with significant CHD, to age 2 years in France, Spain, and Netherlands, for the first year of life only in Italy, Sweden, Switzerland, and for the first year with consideration of extension to the second year in the US. Germany recommended prophylaxis to age 6 months, with individual consideration for age 6-12 months. The UK included infants of ≤26 to ≤32 wGA and age 1.5 to 6 months based on a grid using these two parameters. Austria recommended prophylaxis until surgical correction or heart transplantation, regardless of age.
Other clinical conditions:
Other clinical conditions were considered after individual assessment in eight countries (all but France and Spain). These included immunodeficiency of varying degrees in all eight, neurological or neuromuscular conditions without mention of clearance of respiratory secretions in Austria, Germany, Sweden, and Switzerland, trisomy 21 in Italy and Switzerland, and chromosomal abnormalities or storage diseases in Sweden.
Abbreviations: AB Alberta; BC British Columbia; MB Manitoba; NB New Brunswick; NL Newfoundland and Labrador; NT Northwest Territories; NS Nova Scotia; NU Nunavut; ON Ontario: PE Prince Edward Island; QC Quebec; SK Saskatchewan; YT Yukon; US United States; UK United Kingdom
| Jurisdiction | Group | Other Footnote * | ||
|---|---|---|---|---|
| Preterm infants w/o CLD | Children with respiratory disease | Children with heart disease | ||
NACI (2003) |
"Recommends" |
"Recommends" |
"Recommends" |
"May be considered" |
CIG (2013) |
"Recommends" Selected infants born 33 to 35 wGA and <6 m old at start of local RSV season may benefit; decision based on local considerations. |
"Recommends" |
"Recommends" |
"May be considered" "Should be considered" |
CPS (2015) |
"Reasonable but not essential to offer": |
"Should receive": Second RSV season if still on supplemental O2 or weaned off during the past 3 m "May be considered" |
"Should receive" |
"Should be offered" "Consideration may be given": Term Inuit infants < 6 m old if live in communities with persistent high RSV hospitalization rates "May be considered: |
Alberta |
≤ 286/7 wGA born after May 31, 2020 290/7- 326/7 wGA, born after Sep 30, 2020 330/7- 356/7 wGA born after Oct 31, 2020 AND a risk score of >55 Premature: 330/7- 356/7 wGA otherwise healthy AND twin/ Premature: Multiple birth (excluding twins) ≤ 356/7 wGA and born after Sep 30, 2020 |
≤356/7 wGA and age <2 yr old as of Dec 1, 2020 with CLD (home O2 after May 31, 2020 or on long term prophylaxis or recent exacerbation needing systemic steroids) Tracheostomy age < 2 yr Dec 1, 2020. May be considered:
|
<2 years of age Dec 1, 2020 with severe hsCHD (list of eligible and non-eligible conditions provided; referrals reviewed by cardiologist) |
Trisomy 21 age < 1yr as of Dec 1 2020 Significant immunodeficiency:
Neuromuscular disorders: Exception with no age restriction: spinal muscular atrophy type 1 weighing less than 15 kg Other children < 24 months of age may be considered on an individual basis |
British Columbia |
< 29 wGA and discharged home on or after Sep 1, 2020 29 - 346/7 wGA and discharged home on or after Oct 1, 2020 AND with a risk factor score of ≥42 points < 35 wGA AND multiple of an approved child AND born on or after Nov 1 2019 (i.e., < 1 year old at RSV season start) |
Ex premature with BPD/CLD (O2 or CPAP at > 28 d of age) and born on or after Nov 1 2019 AND requiring continuous O2 on or after Jul 1, 2020 Other:
|
hsCHD and <1 year old on Nov 1, 2020 Significant cardiopulmonary disability (i.e., pulmonary hypertension, cardiac palliation, other) and born on or |
Trisomy 21 born on or after Apr 1, 2020 Requires adjudication:
|
Manitoba |
<33 wGA and age <6 m at start of RSV season 33-35 wGA born after Oct 31, 2020 AND live or will reside in remote Northern community 33-35 wGA with risk score ≥65 will be considered |
<24 months of age with BPD who have received O2 therapy within 6 m preceding start of RSV season |
< 12 m old with hsCHD as assessed by Paediatric Cardiology. Referral through Paediatric Cardiology |
Other children < 24 months of age may be considered on an individual basis |
New Brunswick (2020-21) |
Should be considered for infants < 320/7 wGA and age ≤ 6 m at beginning of RSV season (born on or after Jun 1, 2020) 321/7 to 35 wGA AND risk score is >49 |
Should be considered for children ≤ 24 m old with CLD/BPD AND who have required O2 or medical therapy within 6 m preceding RSV season (i.e. Jun –Nov 2020) Reviewed on a case by case basis: |
Should be considered for children < 24 m old with hsCHD (requiring corrective surgery or on cardiac medication for haemodynamic considerations |
Reviewed on a case by case basis: Down syndrome after discussion with the family; <12 m old will be approved |
Newfoundland and Labrador (2020-21) |
≤ 300/7 wGA and age ≤ 6 m at start of RSV season (i.e. must be born on or after Jun 1, 2020) |
≤ 300/7 wGA and age ≤ 6 m age with CLD/BPD at start of RSV season (i.e. must be born on or after Jun 1, 020) ≤ 12 m old with CLD/BPD AND who have required O2 and /or medical therapy within 6 m preceding RSV season (i.e. after Jun 1, 2020) |
≤ 12 m old with cyanotic or acyanotic hsCHD (requiring corrective surgery or who are on cardiac medication for hemodynamic consideration) as determined by pediatric cardiologist |
≤ 360/7 wGA and < 6 m old at start of RSV season AND who live in isolated or remote northern communities should definitely be considered for prophylaxis, based on access to medical care and other factors known to increase risk (must be born on or after Jun 1, 2020) Other children may be considered on an individual basis |
Northwest Territories |
Premature ≤326/7 wGA and < 6 m old as of Dec 1, 2020 (born after May 31, 2020) May be eligible, will be assessed: |
May be eligible, will be assessed:
|
May be eligible, will be assessed: |
May be eligible, will be assessed:
Other children may be considered on an individual basis |
Nova Scotia, PEI |
≤300/7 wGA and ≤6 m old (i.e. must be born on or after Jun 1,2020) |
≤300/7 wGA with BPD/CLD and ≤6 m old (i.e. must be born on or after Jun 1, 2020) <24 m old with BPD/CLD AND who have required O2 and/or medical therapy within 6 m preceding RSV season (i.e. Jun 1 – Nov, 2020) Requiring consultation:
|
≤24 m old with hsCHD (L-R shunt requiring medication, CHD with surgery pending, ongoing cyanosis), Determined by a pediatric cardiologist |
Requiring consultation:
Other children may be considered on an individual basis |
Nunavut |
≤356/7 wGA and ≤6 m old at start of or during RSV season (born Jul 1 or later) |
<12 m old at start of RSV season with CLD (need for O2 at 36 wGA) currently requiring ongoing supplemental O2 and/or medical treatment (diuretics, bronchodilators, steroids) <24 m old at start of RSV season with BPD requiring ongoing supplemental O2 OR weaned off supplemental O2 in the past 3 months May be considered for children < 24 months with:
only if on home O2 or have had prolonged hospitalization for severe pulmonary disease |
hsCHD < 12 m old at beginning of RSV season (CHD with requirement for supplemental O2 and/or ongoing medical therapy) |
May be considered for children < 24 m old with
Other children may be considered on an individual basis |
Ontario |
≤32 wGA and age ≤ 6 m at start of, or during, local RSV season 33 – 35 completed wGA and age ≤ 6 m at start of or during local RSV season, who DO NOT live in isolated communities AND Risk Score of 49 - 100 33 – 35 completed wGA and aged ≤ 6 m at start of or during local RSV season, and who LIVE IN isolated communities defined by lack of immediate access to medical care (< 30 min, level I hospital) and/or inability to access pediatric services in a timely manner (<90 minutes) |
<24 m old with BPD who required O2 and/or medical therapy for CLD within 6 m preceding RSV season |
<12 m old with cyanotic or acyanotic hsCHD; requiring corrective surgery or on cardiac medication for congestive heart failure or diagnosed with moderate to severe pulmonary hypertension Children 12-24 m old with ongoing hsCHD will be considered on a case-by-case basis Cardiac consultation required |
Children < 24 m old with Down syndrome Siblings of a multiple birth if one child qualifies for prophylaxis Other children may be considered on an individual basis |
Quebec |
<33 wGA age < 6 m at start of RSV season |
Premature <24 m of age at start of RSV season with BPD (defined by need for O2 therapy persisting until at least 28 days of life and gestational age ≥36 weeks) Term, <24 m of age at start of RSV season AND < 24 m old at start of RSV season AND
|
<1 yr old at start of RSV season with CHD, cardiomyopathy or myocarditis that results in clinically significant hemodynamic consequences Must be requested by pediatric cardiologist) |
< 24 m at start of RSV season with HSCT, stem cell or solid organ transplant in the 6 months preceding or during RSV season ≤36 wGA < 6 m old at onset or during RSV season, resident in Nunavik Term infants < 3 m old at onset or during RSV season, resident in Nunavik (under review) Other children may be considered on an individual basis |
Saskatchewan (2020-21) |
< 30 wGA born on or after Jun 1, 2020 < 36 wGA born during current RSV season (Nov – Feb), AND risk score ≥60 < 36 wGA gestation born during current RSV season that are living in or north of La Ronge. |
< 2 yr old with BPD/CLD AND who have required O2 within 6 months preceding the RSV season < 1 yr old with cystic fibrosis |
< 2 yr old with hsCHD as assessed by pediatric cardiology |
Other children may be considered on an individual basis |
Yukon |
< 290/7 wGA and discharged home on or after Sep 1, 2020 290/7 - 346/7 wGA and discharged home on or after Oct 1, 2020 AND risk factors score > 41 Multiple of approved child AND qualifying twin qualifies under prematurity |
Premature with BPD/CLD (oxygen or CPAP for more than 28 d) and born on or after Nov 1 2019 AND on continuous oxygen on or after Jul 1 2020 Tracheostomy / continuous home oxygen / ventilation on or after Nov 1 2020 and born on or after Nov 1 2018 Progressive neuromuscular disease with inability to clear secretions and born on or after Nov 1 2018 (adjudication required) Significant pulmonary disability (pulmonary malformations, severe BPD, symptomatic cystic fibrosis, other) and born on or after Nov 1 2018 (adjudication required) |
Hemodynamically significant CHD and born on or after Nov 1 2019 (clinical details and supporting cardiologist required) Significant cardiopulmonary disability (pulmonary hypertension, cardiac palliation, other) and born on or after Nov 1, 2018 (adjudication required) |
Trisomy 21 born on or after Apr 1, 2020 Severe immunodeficiency (e.g., stem cell transplantation) and born on or after Nov 1 2018 |
BPD: bronchopulmonary dysplasia; CLD: chronic lung disease; CPAP: continuous positive airway pressure; |
||||
| Risk Factor | Alberta (score >55) |
British Columbia (score ≥42) |
Manitoba (score ≥65) |
New Brunswick (score ≥49) |
Northwest Territories (score ≥55 |
Ontario (score ≥49) |
Saskatchewan (score ≥60) |
Yukon (score >41) |
|---|---|---|---|---|---|---|---|---|
| Birth month | √ (Nov-Feb) | N/A | √ (Nov-Mar) | √ (Nov-Jan) 25 |
N/A | √ (Nov-Jan) 25 | √ (Nov- Feb) 27 | N/A |
| Infant or sibling attends daycare | N/A | N/A | √ | √ 17 | N/A | N/A | N/A | N/A |
| Infant or sibling ≤ 4 yr old attends daycare | √ | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Infant or sibling ≤ 4 yr old attends daycare ≥ 3 half-days per week | N/A | N/A | N/A | N/A | √ 19 | N/A | N/A | N/A |
| Infant or siblings attend daycare ≥ 20 hr/wk or kindergarten/preschool ≥ 3 half-days /week | N/A | N/A | N/A | N/A | N/A | N/A | √ 19 | N/A |
| Infant will attend daycare regularly during first 3 m after discharge | N/A | √ 22 | N/A | N/A | N/A | N/A | N/A | √ 22 |
| Infant to attend daycare OR siblings in day care or kindergarten during this winter | N/A | N/A | N/A | N/A | N/A | √ 17 | N/A | N/A |
| Infant attends home or facility-based group | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| >5 individuals in the home, including the applicant and multiples of applicant | √ | √ 12 | √ | √ 13 | √ 15 | √ 13 | √ 15 | √ 12 |
| Other child < 5 yr old in household (not incl. multiples of applicant) | N/A | √ 14 | N/A | N/A | N/A | N/A | N/A | √ 14 |
| Discharged home Dec-Feb | N/A | √ (to Mar in Northern Health Regions) 20 | N/A | N/A | N/A | N/A | N/A | √ 20 |
| Discharged home Nov or Mar | N/A | √ (to Apr in Northern Health Regions) 10 | N/A | N/A | N/A | N/A | N/A | √ 10 |
| Discharged home Nov-Feb | N/A | N/A | N/A | N/A | √ 27 | N/A | N/A | N/A |
| GA 29-306/7 wks | N/A | √ 10 | N/A | N/A | N/A | N/A | N/A | √ 10 |
| Small for GA (birth weight < tenth percentile for GA) | √ | N/A | √ | √ 12 | √ 14 | √ 12 | √ 14 | √ 8 |
| Small for GA (birth weight ≤ tenth percentile for GA | N/A | √ 8 | N/A | N/A | N/A | N/A | N/A | N/A |
| Male | √ | N/A | √ | √ 11 | √ 13 | √ 11 | √ 13 | N/A |
| Male (all), or female not receiving human milk | N/A | √ 8 | N/A | N/A | N/A | N/A | N/A | √ 8 |
| Immediate family (mother, father, siblings) all without eczema | N/A | N/A | √ | √ 12 | N/A | √ 12 | N/A | N/A |
| 2 or more smokers in the household | √ | √ 8 | √ | √ 10 | N/A | N/A | N/A | √ 8 |
| Smoker(s) in the household | N/A | N/A | N/A | N/A | √ 13 | √ 10 | √ 12 | N/A |
| Lives more than 2 hr from nearest hospital that provides bronchiolitis treatment | √ | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Lives more than 1 hr by road from nearest hospital that provides bronchiolitis treatment | N/A | N/A | N/A | N/A | √ 20 | N/A | N/A | N/A |
| Remote location with no permanent road access | √ | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Remote location 100 km or 1 hr ground transport from hospital/point of pediatric care | N/A | √ 10 | N/A | N/A | N/A | N/A | N/A | N/A |
| Remote residence (Yukon is considered remote) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | √ 10 |
N/A: Not available |
||||||||
| Jurisdiction | Group | |||
|---|---|---|---|---|
| Preterm infants | Children with lung disease | Children with heart disease | Other | |
Austria |
< 28 wGA and age ≤ 12 m |
BPD age < 2 yr and requiring therapy in the last 6 months |
hsCHD until corrected or transplanted |
May be considered; |
France |
- |
≤ 32 wGA, age < 6 m at onset of RSV season and respiratory disease (requiring > 28 d of O2 in neonatal period) |
< 2 yr old with hsCHD |
N/A |
Germany |
May be given: |
Should receive: Underlying syndrome or neurological condition with CLD |
Should receive: May receive: |
May be considered: Should receive: |
Italy |
< 29 wGA and age ≤12 m |
BPD age ≤ 12 m with BPD (defined as need for O2 therapy for ≥ 28 d after birth) BPD age 1-2 yr and requiring treatment in the previous 6 m |
< 1 yr old with severe CHD (cyanotic heart disease prior to surgery or after a palliative procedure, on therapy for congestive heart failure and scheduled to undergo surgery, moderate to severe pulmonary hypertension, surgically repaired CHD still needing therapy for congestive heart failure, infants awaiting heart transplantation or in the post-transplantation period. |
To consider: Immunodeficiency, Down syndrome |
Spain |
≤ 286/7 wGA and age < 9 m 29-316/7wGA and age < 6 m 321/7 to 346/7 wGA and age < 6 m if risk factors present |
CLD and age < 2 yr requiring treatment in the previous 6 months |
hsCHD and age < 2 yr requiring treatment in the previous 12 months |
N/A |
Sweden |
< 26 wGA and age < 6 months |
BPD and age < 12 m requiring O2 treatment in the previous 6 m Severe CLD age < 12 m (esophageal atresia, diaphragmatic hernia, malformations in trachea, bronchus and / or lung |
CHD and age < 12 m and hemodynamically significant heart failure, pronounced pulmonary hypertension, cardiomyopathy with pronounced heart failure |
May be considered on an individual basis: |
Switzerland |
Not recommended |
BPD age < 1 yr age < 24 m with cystic fibrosis, or anatomical lung malformations may be considered in selected cases, |
May be considered: |
Others: |
The Netherlands |
< 32 wGA and age < 6 m |
< 1 yr old with BPD or pulmonary hypertension < 1 yr old with serious lung pathology from cystic fibrosis |
hsCHD age < 2 yr |
Selected: |
UK |
Not warranted for prematurity alone |
Pre-term infants who have moderate or severe BPD (defined as preterm infants with compatible x-ray changes who continue to receive supplemental O2 or respiratory support at 36 weeks post-menstrual age. The following should be offered prophylaxis: b) Infants with respiratory diseases who are not necessarily pre-term but who remain in O2 at start of RSV season, including:
those receiving long term ventilation at onset of season if age < 24 m and additional co-pathology as reflected by oxygen dependency |
Preterm infants with Cyanotic or acyanotic CHD plus significant co-morbidities particularly if multiple organ systems are involved |
< 24 m old with SCID unable to mount either T-cell responses or produce antibody - until immune reconstituted. |
USA 2014 |
"May be administered" in text; summary says "Recommended" < 290/7 wGA and <12 m old at start of RSV season |
"May be considered" in text; summary says "Recommended" <320/7 wGA with CLD of prematurity (defined as requirement for >21% oxygen for at least the first 28 days after birth, first yr of life. Second yr: Consideration only if above plus continued need for medical support (steroid, diuretic, O2) in 6 m before start of second RSV season. May be considered: Cystic fibrosis with CLD or nutritional compromise in first yr of life; may be considered in second yr if previously hospitalized for pulmonary exacerbation or abnormal chest x-ray or CT that persists when stable; weight for length < tenth percentile |
"May benefit from". Summary says "may administer" to certain infants with hsCHD Age < 1 yr at onset of RSV season with hsCHD (with consultation with a pediatric cardiologist) " may be considered": age < 2 yr and undergoing cardiac transplantation during the RSV season |
Other: May be considered: Insufficient data to justify: Selection may differ in Alaska native infants based on local epidemiology Not recommended for prevention of asthma |
N/A: Not available |
||||
Sources:
Canada:
- National Advisory Committee on Immunization. Statement on the recommended use of monoclonal anti-RSV antibody (PVZ). CCDR 2003;29. ACS-7,8.
- Public Health Agency of Canada. Canadian Immunization Guide: Part 5 - Passive Immunization.
https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-5-passive-immunization.html - Robinson JL, Le Saux N, Canadian Paediatric Society Infectious Diseases and Immunization Committee. Preventing hospitalizations for respiratory syncytial virus. Paediatr Child Health 2015;20(6):321.26
- Alberta Health Services: https://www.albertahealthservices.ca/assets/info/hp/rsv/if-hp-rsv-criteria.pdf; https://www.albertahealthservices.ca/frm-18957.pdf
- British Columbia Provincial Health Services Authority:
https://www.childhealthbc.ca/sites/default/files/b.c.-rsv-manual-2020-21v2.pdf - Manitoba Children's Hospital: Personal communication
- New Brunswick Department of Health: Personal communication
- Newfoundland and Labrador Eastern Health: Personal communication
- Northwest Territories:
https://www.hss.gov.nt.ca/professionals/en/services/seasonal-rsv-prophylaxis-synagis%C2%AE-program-package-2020-2021 - Nova Scotia IWK Health Centre
https://www.iwk.nshealth.ca/PVZ/provincial-guidelines/indications-for-use - Nunavut Department of Health:
https://www.gov.nu.ca/sites/default/files/11.0_specialized_and_annual_immunization_protocols_december_2020.pdf - Prince Edward Island: Personal communication (using Nova Scotia protocol)
- Ontario Ministry of Health:
https://www.health.gov.on.ca/en/pro/programs/drugs/funded_drug/pdf/rsv_season2020-2021.pdf - Hema-Quebec: https://www.hema-quebec.qc.ca/userfiles/file/media/francais/hopitaux/20-030.pdf
- Saskatchewan Health Authority: https://www.saskatoonhealthregion.ca/locations_services/Services/Childrens-Services/RSV-Program/Pages/Forms.aspx
- Yukon Health and Social Service: https://yukon.ca/sites/yukon.ca/files/hss/hss-imgs/Section_5_-_immunization_of_special_populations_october_2020.pdf
International:
Austria, Austrian Society for Pediatrics and Adolescent Medicine:
- Resch B, Manzoni P, Lanari M et al. Severe respiratory syncytial virus (RSV) infection in infants with neuromuscular diseases and immune deficiency syndromes. Paediatr Respir Rev. 2009;10:148–53.
- Österreichische Gesellschaft für Kinder- und Jugendheilkunde (ÖGKJ). Konsensuspapier zur prophylaxe der RSV-infektion mit PVZ und post-RSV-atemwegserkrankung Monatsschr Kinderheilkd 2008:156:381-383. https://doi.org/10.1007/s00112-008-1722-y
- Resch B, Bramreiter VS, Kurath-Koller S, Freidl T, Urlesberger B. Respiratory syncytial virus associated hospitalizations in preterm infants of 29 to 32 weeks gestational age using a risk score tool for PVZ prophylaxis. Eur J Clin Microbiol Infect Dis (2017) 36:1057–1062.
France, Haute autorité de santé Commission de la transparence:
- https://www.has-sante.fr/portail/upload/docs/evamed/CT-15884_SYNAGIS_QD_INS_Avis2_CT15884.pdf accessed Mar 22 2021
Germany, German Society for Pediatric Infectiology:
- https://www.awmf.org/uploads/tx_szleitlinien/048-012l_S2k_Prophylaxe-von-schweren_RSV-Erkrankungen-Risikokindern-PVZ_2018-11.pdf accessed Mar 22 2021
Italy, Italia Medicine Agency:
- Bollani L, Baraldi E, Chirico G, et al. Revised recommendations concerning PVZ prophylaxis for respiratory syncytial virus (RSV). Ital J Pediatr 2015;15:97.
- Belleudi V, Trotta F, Pinnarelli L, et al. Neonatal outcomes following new reimbursement limitations on PVZ in Italy Arch Dis Child 2018;103:1163–1167.
Spain, Standards Committee of the Spanish Neonatology Society:
- Figueras Aloy J, Quero J, Comité de Estándares de la Sociedad Española de Neonatología. Recommendations for the prevention of respiratory syncytial virus infections. An Pediatr (Barc) 2005;63(4):357-62.
- Figueras Aloy J, Carbonell Estrany X, Comité de Estándares de la Sociedad Española de Neonatología. Recommendations for the use of PVZ in the prevention of respiratory syncytial virus infection in late preterm infants (321 to 350 weeks of gestation). An Pediatr (Barc) 2010;73 (2) 2010:98.e1-98.e4.
- Figueras Aloy J, Carbonell Estrany X, Comité de Estándares de la SENeo. Update of recommendations on the use of PVZ as prophylaxis in RSV infections. An Pediatr (Barc) 2015;82(3):199.e1-199.e2
Sweden, Medical Products Agency:
- http://www.lakemedelsverket.se/malgrupp/Halso---sjukvard/Behandlings--rekommendationer/Behandlingsrekommendation---listan/RSV-infektioner/ Accessed Mar 22 2021
Switzerland, Interdisciplinary Working Group:
- Agyemana P, Barazzoneb C, Hammerb J et al. Prävention von RSV-Infektionen mit dem humanisierten monoklonalen Antikörper PVZ. Swiss Med Forum 2017; 17(28-29):611-614.
The Netherlands, Dutch Association for Pediatrics; Ministry of Health
- Ministry of Health, Wellness and Sport (reimbursement). https://zoek.officielebekendmakingen.nl/stcrt-2006-218-p29-SC77527.pdf accessed Mar 21, 2021.
- Whelan B, Musters E, Murray A et al. Review of the home care programmes for respiratory syncytial virus (RSV) prophylaxis in Ireland and The Netherlands. Drugs Ther Perspect 2016;32:119–130
United Kingdom, Public Health England:
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/458469/Green_Book_Chapter_27a_v2_0W.PDF Assessed Mar 22, 2021
United States, American Academy of Pediatrics:
- Committee on Infectious Diseases and Bronchiolitis Guidelines Committee. Updated guidance for PVZ prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014;134:415–420
Appendix B: Palivizumab safety
Table of contents
- Introduction
- Methods
- 3. Results
- Summary
- Table A: Search strategy and results
- Table B: Level of evidence based on research design and quality (internal validity) rating of evidence
- Table C: Summary of evidence related to safety of PVZ
Introduction
PVZ (PVZ) is considered to be a safe product. Since the description of adverse events (AEs) in the NACI 2003 PVZ statementFootnote 4 there have been no safety alerts, but the number of infants exposed to PVZ has risen considerably. NACI determined that this warranted a new assessment of PVZ safety data, and that a rapid literature search and a review of data from the Canadian Vigilance ProgramFootnote 210 would be performed.
Methods
2.1. Rapid literature review
A rapid literature review of the safety of PVZ was conducted using the following sources:
- A systematic review of PVZ safety published in 2013 (rated average by AMSTAR) was used to identify studies published before 2013Footnote 211. These studies were reviewed.
- A literature search, based on the research question below, was conducted. The search strategy was developed with a Health Canada librarian (LG), included publications from 2013 onwards and was performed on April 24, 2019. The detailed search strategy is presented below. Because of time constraints, the literature search was limited to two bibliographic databases (MEDLINE and EMBASE)
- Studies cited in the references obtained in the search that were not included in (1) or (2) were also reviewed.
Screening, eligibility assessment, data extraction and quality assessment were completed by a single reviewer. A data summary table with ratings of the quality of the evidence using NACI's standard methodology (Table B) was produced (Table C). Results from the accepted studies were synthesized narratively.
Research question: What is the safety of PVZ use in humans?
P (population): human (no age restriction)
I (intervention): PVZ administered intramuscularly
C (comparison): placebo, other monoclonal antibody, or none
O (outcome): adverse events
Identification of eligible studies:
Articles retrieved in the Health Canada literature search were loaded into RefWorks (ProQuest LLC, Ann Arbor, MI) and uploaded to DistillerSR (Evidence Partners, Ottawa, Canada). Duplicate records were removed. Records were screened by title and abstract. The full texts for articles that were relevant based on the inclusion and exclusion criteria, or that had insufficient information to exclude, were retrieved and assessed for eligibility through full-text screening.
Studies were included if they met the following criteria:
- The study involved administration of PVZ intramuscularly to children.
- The study presented data on safety or AE. (If PVZ was administered but these were not mentioned in the abstract, the study was nevertheless included for full text review as studies could include safety data without reference in the abstract).
Studies were excluded if they met one or more of the following criteria:
- The study did not provide data on AE or safety
- PVZ was not administered intramuscularly
- The study was in a language other than English or French
- The study was non-human
- The article was an editorial or an opinion.
- The study presented only secondary research (systematic reviews were accepted).
2.2. Data from the Canada vigilance program
The Canada Vigilance Program (CVP) is Health Canada's post-market surveillance program within the Marketed Health Products Directorate (MHPD) that collects and assesses reports of suspected adverse reactions to health products. The purpose of the CVP is to detect possible safety signals of adverse reactions associated with health products. Adverse reaction reports are suspected associations which reflect the opinion or observation of the individual reporter and does not reflect any Health Canada assessment of association between the health product and the reaction. Inclusion of a particular reaction does not necessarily mean that it was caused by the suspected health product. A serious adverse event (SAE) means that an event required in-patient hospitalization or prolongation of existing hospitalization, caused congenital malformation, resulted in persistent or significant disability or incapacity, was life-threatening or resulted in death. Other important medical events that may jeopardize the patient or may require intervention may also be considered serious.
Reports to CVP to Dec 31, 2018 were downloaded on April 5, 2019. The MHPD also performs periodic safety reviews if safety signals arise (MedEffect™ Canada). No safety reviews were warranted.
3. Results
3.1. Literature review
3.1.1. Randomized controlled trials
Nine double blind RCTs were identified. Four were placebo controlledFootnote 48 Footnote 80 Footnote 111 Footnote 140 Footnote 141, two compared lyophilized and liquid forms of PVZ Footnote 212 Footnote 213 and three compared PVZ to otavizumab (MVZ) (another monoclonal antibody directed against respiratory syncytial virus that was not licensed Footnote 214 Footnote 215 Footnote 216. Quality for seven was rated as good while oneFootnote 111 was rated as fair. The ninth was a conference abstract assessed in a systematic review that included additional information and was rated as good.
In the initial PVZ IMPACT RCT of children born at ≤ 35 weeks gestational age (wGA) and aged ≤ 6 months or age ≤ 24 months with bronchopulmonary dysplasia (BPD), rates of AE reported by the blinded investigator as potentially related to the study drug were similar in the PVZ and placebo groups (11% and 10% respectively). There were no significant differences in types of AE, including injection site reactions. There were no SAE. Discontinuation of PVZ because of AE was rare (0.3%). There were 4 (0.4%) deaths in the PVZ group and 5 (1%) with placebo for reasons judged unrelated to the study drug. The number of infants receiving PVZ was 1002Footnote 48.
An RCT of children ≤ 24 months old with hemodynamically significant CHD (hsCHD) reported similar overall rates of AE (96% vs 97%) and AE judged related to study drug by the blinded investigator (7.2% vs 6.9%) in PVZ and placebo groups respectively. There were more SAE in the placebo group (63% vs 55%, p=0.005) but RSV hospitalizations were included as SAE. SAE judged related to study drug were rare (0 and 0.5% in PVZ and placebo groups). There were no drug discontinuations because of AE. Deaths occurred in 3.3% in the PVZ group and 4.2% in the placebo group but none were attributed to study drugs. The number of infants receiving PVZ was 639Footnote 80.
Results of an RCT of PVZ in children <2 years old with cystic fibrosis were presented as a conference abstractFootnote 141 and was the only study in a later systematic reviewFootnote 140. There were no significant differences in overall rates of AE, SAE, rates of AE related to study drug (5.4% vs 4.4%) or SAE related to study drug (0 vs 2.1%) with PVZ vs placebo respectively. PVZ was discontinued because of SAE in one case. There were no deaths. The number of children receiving PVZ was 92.
An RCT of otherwise healthy premature infants born at 33-35 wGA and aged ≤ 6 months reported only hospitalizations and deaths as AE. Hospitalization rates were higher with placebo than with PVZ (21.9% vs 12.6%, p=0.04) but when hospitalizations for RSV were removed the difference was not significant (19.1% vs 14.0% for placebo vs PVZ). There were no deaths. The number of infants receiving PVZ was 214Footnote 111.
Two RCTs comparing lyophilized and liquid preparations of PVZ in children with chronic lung disease age ≤ 24 months or born at ≤ 35 wGA and age ≤ 6 monthsFootnote 212 or infants born at ≤ 35 wGAFootnote 213 found no significant differences in overall rates of AEFootnote 213 or SAEFootnote 212 Footnote 213. SAE occurred in 5.9% and 2.6% of lyophilized PVZ recipients and 8.5% and 3.3% of liquid PVZ recipients in the two studies but none were judged related to the study drugs. There was one death in a child who received lyophilized PVZ that was deemed not related to the study drugFootnote 212. The total numbers of infants exposed to PVZ were 413 Footnote 212 and 305 Footnote 213.
In an RCT of PVZ vs MVZ in preterm infants of ≤ 35 wGA and aged ≤ 6 months or aged ≤ 24 months with chronic lung disease, overall rates of AE and SAE were similar. AE observed in the PVZ group included skin and subcutaneous disorders in 18.5%; injection site reactions in 2.7%, psychiatric conditions (restlessness, sleepiness, unsettled, irritability) in 2.9%. AE considered as possible cutaneous hypersensitivity reactions occurred in 0.2% of PVZ recipients. There were no cases of anaphylaxis. The rate of SAE in the PVZ group was 15.3%. Relationship of AE to study drug was not ascertained. PVZ was discontinued because of AE in 0.3%. Mortality rate was 0.1% with PVZ and no deaths were considered related to PVZ. The number of children receiving PVZ was 3298Footnote 214. A second study of PVZ versus MVZ included children aged ≤ 24 months with hsCHD. Overall rates of AE and SAE were similar with the two products. In the PVZ group, AE and SAE judged related to study drug occurred in 8.8% and 1.0% respectively. PVZ was discontinued in one patient (0.2%) due to a macular rash. Mortality rate was 1.6% with no deaths related to the study drug. The number of children receiving PVZ was 612Footnote 216. A third study of PVZ versus MVZ in preterm infants of ≤ 35 wGA and aged ≤ 6 months or aged ≤ 24 months with chronic lung disease used a crossover design, reporting AEs for each drug before and after crossover. The rate of AE related to PVZ was 9.3%. There were no SAE related to PVZ. PVZ was discontinued because of AE in one case (0.6%). There were no deaths. The number of children receiving PVZ was 161Footnote 215.
3.1.2 Population-based cohort studies
Two population based cohort studies, rated as good quality, were carried out in Sweden and Denmark using national health registers to investigate specific events occurring in PVZ recipients versus the rest of the population. The age-adjusted population was 1,351,265 of which 1192 children received PVZ. The first study looked at the incidence of autoimmune disease, which was not significantly increased in PVZ recipients with rates of 0.54% in Swedish and 0.60% in Danish children not exposed to PVZ and 0.76% in PVZ recipients; adjusted hazard ratio (HR) 1.54, 95% CI 0.80, 2.95Footnote 217. The second study investigated atopy. There was an increased risk of asthma with PVZ exposure (HR 1.49, 95% CI 1.32, 1.68), but after post-hoc analysis using a propensity score to balance confounding factors this was no longer significant (HR 0.91; 95% CI 0.56, 1.48). There was no increased risk of atopic dermatitis (HR 1.18; 95% CI 0.94, 1.48) or allergic rhinoconjunctivitis (HR 1.14; 95% CI 0.92, 1.42)Footnote 218.
3.1.3 Prospective registries and cohort studies
The Canadian RSV Evaluation Study of PVZ (CARESS) registry described SAE reported in 13,025 PVZ recipients (born at ≤ 35 wGA or with hsCHD or BPD or other complex medical conditions) who received 57,392 doses of PVZ from 2008 through 2013. Hospitalizations for respiratory tract infections were excluded. There were 62 SAE in 52 infants. The incidence of SAE considered possibly or probably related to PVZ was 2.8 per 10,000 patient-months or 2.4 per 10,000 doses, with 14 SAEs occurring in 6 patients (0.05%). All were suggestive of hypersensitivity reactions and recurred with subsequent doses in the 4 children who were re-challenged: generalized erythema and bronchospasm after second and third doses; generalized urticaria soon after third dose; facial erythema 5 minutes post injection; localized rash near injection site after second and third doses; and prolonged vomiting and nasal congestion after each of 4 doses in 2 infants. PVZ was discontinued in these 6 patients and in another 14, 3 of whom were hospitalized for respiratory tract infections and 11 with AE that did not qualify as SAE (rash on thigh, gastrointestinal upset, fussiness, and "unwell"). There were 5 deaths, unrelated to PVZFootnote 170. In an earlier report of data in the CARESS registry from 2005-2009, 5286 children received 19,485 doses of PVZ. There were 61 SAE of which 56 were hospitalizations for respiratory infections. No details about the other 5 SAE were presented. PVZ was discontinued in 1.7% of recipients because of AE. There were 5 deaths deemed probably not or not related to PVZFootnote 219. A review of CARESS data to 2010 reported 8 deaths, none related to PVZFootnote 220. Data from CARESS combined with a prospective cohort from Italy were reported for 2001-2014. In 14,468 PVZ recipients, 15 SAE related to PVZ were reported in 7 patients (0.05%). All 15 SAEs were hypersensitivity reactions. These results overlap with those of Chen, aboveFootnote 221.
Data from the German PVZ registry, from 2002-2007, indicated that 10,686 subjects received 49,608 doses of PVZ. SAE possibly or probably related to PVZ occurred in 10 subjects (0.09%), a rate of 2 per 10,000 doses). SAE were dyspnea or cyanosis with or without fever (4), As well as rash, thrombocytopenia, osteomyelitis, seizure, hypo-responsiveness, and fever with restlessness. There were 3 deaths, one unrelated to PVZ and two not assessableFootnote 222. A later publication reported data from the same registry for 2009-2016, when 12,729 subjects received 63,572 doses. SAE probably related to PVZ were reported in 8 cases (0.06%), or 1.3 per 10,000 doses. These events were described as breathing cessation (2), rash, rash with fever, urticaria, agitation, erythema at injection site, and acute restriction of leg mobility (1 each). There were 9 deaths, none related to PVZFootnote 223.
An international prospective observational study from 15 northern hemisphere countries reported on 565 infants with prematurity (≤ 35 wGA) and age ≤ 6 months or age ≤ 24 months with BPD who received PVZ in 1998-9. Forty-five infants had one or more AE, of which 39 had 40 AE considered related to PVZ (7%). The most common related AE were injection site reactions (12), fever (8), diarrhea (4) and nervousness or irritability (4). None were SAE. PVZ was discontinued because of AE in 11 cases, 3 of which were considered to be possibly or probably related to PVZ: oxygen desaturation immediately after injection, abdominal and peripheral edema, and gastroenteritis. There were 2 deaths, unrelated to PVZFootnote 224. An international prospective observational study from 17 European countries and Saudi Arabia studied 285 preterm infants of 29-32 wGA aged ≤ 6 months who received PVZ in 2000-2001. There were 7 AE (fever, enteritis, bronchitis, rhinitis, cough, bacterial pneumonia, conjunctivitis) judged related to PVZ in 5 patients (2.5%), of which one (bacterial pneumonia) was an SAE (0.35%). In addition, a case of RSV bronchiolitis was classed as an SAE possibly related to PVZ. PVZ was discontinued in 2 cases due to AE, one of which (fever) was considered as probably related to PVZ. There were no deathsFootnote 225. An international prospective observational study from 7 Latin American countries reported on 459 recipients of PVZ (born at ≤ 35 wGA or with BPD or hsCHD) in 2011-12. There were 1165 AE. A total of 135 SAE occurred in 102 patients but none were considered related to PVZ. There were 3 deaths unrelated to PVZFootnote 226.
A multicenter prospective observational study from France reported on data from 516 children who received PVZ for prematurity (≤ 32 wGA with BPD and age ≤ 6 months or ≤ 35 wGA with BPD and age < 2 yr) in 1999-2000. There were 15 AE judged potentially related to PVZ: apnea (n=3) fever (n=3) injection site pain (n=2) hyperventilation (n=2) and asthenia, vomiting, bronchitis, cough, urticaria (1 case each). There no SAE. There were 10 deaths, none attributed to PVZFootnote 227. A later multicenter prospective observational study from France reported on SAE in 1371 recipients of 6257 doses of PVZ. There were no SAE judged related to PVZ. There were 6 deaths, none attributable to PVZFootnote 228. A multicenter prospective observational study from Japan followed 304 children aged < 24 months who received PVZ in 2013-15 and who were immunocompromised or had Down syndrome. A total of 220 AE occurred in 99 children, of which 33 AE in 25 children (8%) were considered possibly related to PVZ: (pneumonia (3), RSV infection (3), other infections (11), upper respiratory tract inflammation (5), asthma (1), diarrhea (2), and miscellaneous (8). Eighty-nine SAE occurred in 53 patients. Of these, 8 SAE in 7 patients (2.3%) were considered related to PVZ (pneumonia (4), RSV infection (2) and bronchitis and upper respiratory tract inflammation (1 each). For another 5 SAE in 4 patients (septic shock, device-related infection, asthma, drug related liver injury, nephroblastoma), the relationship to PVZ was considered to be indeterminable. PVZ was discontinued because of AE in 7 patientsFootnote 229. A multicenter prospective observational study from Spain of 1919 premature infants of ≤ 32 weeks GA and age ≤ 6 months reported no deaths related to PVZFootnote 46.
In 7 smaller prospective observational studies, a total of 560 infants received PVZ; no SAE related to PVZ were reported Footnote 44 Footnote 230 Footnote 231 Footnote 232 Footnote 233 Footnote 234 Footnote 235.
A multicenter retrospective observational study from Poland reported on 3241 PVZ doses in 1021 children. There were 108 AE in 84 recipients (8.2%), the most common being nervousness (40), fever (24), injection site reactions (15), diarrhea (4), vomiting (4). Whether any AE were SAE and the relationship to PVZ were not reported, nor were deaths or PVZ discontinuations because of AEFootnote 236. A descriptive retrospective / prospective single center study from Qatar reported no AE and no deaths attributable to PVZ in 429 premature infants of ≤ 35 wGA and aged ≤ 6 months or age ≤ 2 years with CLD or hsCHDFootnote 237. A retrospective multicenter study of 187 children in Canada with cystic fibrosis aged < 2 years reported no SAE related to PVZFootnote 77. A retrospective single center cohort study of 75 preterm infants born at ≤ 35 wGA aged < 2 years with chronic lung disease in Korea reported 3 injection site reactions and no systematic, respiratory or gastrointestinal events symptomsFootnote 238.
Two studies of children receiving PVZ for one or 2 seasons found no difference in frequency or types of AE in the first versus the second season, but the numbers of subjects were small (first season 103; second season 119)Footnote 231 Footnote 232.
3.1.4 Case reports of serious adverse events attributed to PVZ
A case report described non-fatal anaphylaxis of onset 20 minutes after a dose of PVZ.Footnote 239 The child had received 5 doses of PVZ the previous season and one previous dose in the current season). Anaphylaxis has rarely been reported. The manufacturers in 2002 reported 2 cases of anaphylaxis after administration of 2,000,000 doses of PVZFootnote 240.
In another case report a child developed apnea, bradycardia and oxygen desaturation 8 hours after the first dose of PVZ. The child was found to have parainfluenza virus 1 and rhinovirus/enterovirus in a nasopharyngeal swab. Review of data reported to the Drug Commission of the German Medical Association from 1998 to 2017 revealed 93 reports of apnea/bradycardia, desaturations or cardiorespiratory event after PVZ administration, of which all but 29 were associated with a concurrent infection. There were 3 fatal cases of cardiorespiratory events within 48 hours of PVZ, all without concomitant infection but all with severe CHD. The authors concluded that there was insufficient information to assess the association of cardiorespiratory events after PVZ administrationFootnote 241.
3.1.5 Detection and clinical significance of anti-PVZ antibodies:
In an early study, antibody to PVZ was detected in 1.2 % of PVZ and 2.8% of placebo recipients, suggesting that the binding of PVZ to antibody was non-specificFootnote 48. In subsequent studies, anti-PVZ antibody has been detected in 1.5-5.9% of PVZ recipients Footnote 212 Footnote 213 Footnote 216 Footnote 230 Footnote 231 Footnote 232. Antibody was generally present transiently and at low levels and there was no boosting with subsequent doses or differences in responses between the first and second year of PVZ exposureFootnote 231 Footnote 232. Anti-PVZ antibody was not associated with presence or type of AE events including potentially immune-mediated reactions, and did not affect PVZ levels.
3.2 Data from the Canada vigilance program
There were 259 unique case reports of AE following PVZ administration to Dec. 31, 2018, of which 237 were considered serious. The most frequent events were respiratory at 137 (53%), of which 113 were infections (mainly reported because of PVZ product failure), followed by hypersensitivity reactions at 23 (9%). Other events reported are expected complications of the underlying conditions for which PVZ is recommended and are consistent with those reported in the product monograph. The role of PVZ in these AE is unknown as causality was not assessed.
Summary
The most commonly reported AE considered related to PVZ were injection site reactions, fever, nervousness or irritability, cough, rhinitis, and diarrhea. PVZ related SAE were rare, reported in 1% or less of recipients with most studies reporting none. Most were hypersensitivity reactions. Three reports of anaphylaxis were identified. PVZ discontinuation because of AE occurred in 0-2.3% of recipients. There were no deaths attributable to PVZ.
Repeated injections of a humanized monoclonal antibody raises concern for the development of immune mediated disease Footnote 217 Footnote 242. Studies showed no increased risk of autoimmune disease or atopy in children exposed to PVZ.
Table A: Search strategy and Results
Medline
Database(s): Ovid MEDLINE(R) ALL 1946 to April 23, 2019
Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | PVZ/ | 688 |
| 2 | exp antibodies, monoclonal/ and (respiratory syncytial virus vaccines/ or respiratory syncytial virus, human/ or respiratory syncytial virus infections/) | 863 |
| 3 | (PVZ* or medi 493 or monoclonal antibody medi-493 or monoclonal antibody medi 493 or monoclonal antibody medi493 or medi-493 or medi493 or synagis or abbosynagis or synagys or ((respiratory syncytial virus* or rsv) adj5 monoclonal*)).ti,kf,kw. | 600 |
| 4 | (PVZ* or medi 493 or monoclonal antibody medi-493 or monoclonal antibody medi 493 or monoclonal antibody medi493 or medi-493 or medi493 or synagis or abbosynagis or synagys or ((respiratory syncytial virus* or rsv) adj5 monoclonal*)).ab. /freq=2 | 556 |
| 5 | 1 or 2 or 3 or 4 [PVZ] | 1141 |
| 6 | death/ or exp "drug-related side effects and adverse reactions"/ or exp product surveillance, postmarketing/ or risk assessment/ or risk factors/ or exp safety/ or abnormalities, drug-induced/ or exp toxicity tests/ or allergens/ or exp hypersensitivity/ or exp mutagenesis/ or exp food-drug interactions/ or exp herb-drug interactions/ or drug fatality/ | 1755435 |
| 7 | (postmarketing or post marketing or adverse or anaphyla* or complication? or dermatit* or hypersensitiv* or harm or harms or harmful or intoleran* or tolera* or toxic* or urticaria or poison* or cardiotox* or cytotox* or dermatotox* or dermotox* or embryotox* or fetotox* or genotox* or hepatotox* or immunotox* or maternotox* or nephrotox* or neurotox* or ototoxic* or iatrogen* or teratogen* or mutagen* or carcin* or death* or fatal* or hazard* or lethal* or "life-threatening" or mortal* or safe or safety or unsafe or ((side or unintended or unintentional or unwanted or unexpected or undesirable or serious* or severe or allergic or allergy) adj3 (effect* or event* or impact* or interaction* or outcome* or react* or response*))).ti,kf,kw. | 1746562 |
| 8 | (postmarketing or post marketing or adverse or anaphyla* or complication? or dermatit* or hypersensitiv* or harm or harms or harmful or intoleran* or tolera* or toxic* or urticaria or poison* or cardiotox* or cytotox* or dermatotox* or dermotox* or embryotox* or fetotox* or genotox* or hepatotox* or immunotox* or maternotox* or nephrotox* or neurotox* or ototoxic* or iatrogen* or teratogen* or mutagen* or carcin* or death* or fatal* or hazard* or lethal* or "life-threatening" or mortal* or safe or safety or unsafe or ((side or unintended or unintentional or unwanted or unexpected or undesirable or serious* or severe or allergic or allergy) adj3 (effect* or event* or impact* or interaction* or outcome* or react* or response*))).ab. /freq=2 | 2287607 |
| 9 | 6 or 7 or 8 [adverse events] | 4455565 |
| 10 | 5 and 9 | 398 |
| 11 | limit 10 to yr = "2013 - Current" | 150 |
Embase
Database(s): Embase 1974 to 2019 April 23
Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | *PVZ/ | 817 |
| 2 | *monoclonal antibody/ and (*respiratory syncytial virus infection/ or *respiratory syncytial virus vaccine/ or exp *human respiratory syncytial virus/) | 48 |
| 3 | (PVZ* or medi 493 or monoclonal antibody medi-493 or monoclonal antibody medi 493 or monoclonal antibody medi493 or medi-493 or medi493 or synagis or abbosynagis or synagys or ((respiratory syncytial virus* or rsv) adj5 monoclonal*)).ti,kw. | 934 |
| 4 | (PVZ* or medi 493 or monoclonal antibody medi-493 or monoclonal antibody medi 493 or monoclonal antibody medi493 or medi-493 or medi493 or synagis or abbosynagis or synagys or ((respiratory syncytial virus* or rsv) adj5 monoclonal*)).ab. /freq=2 | 808 |
| 5 | 1 or 2 or 3 or 4 [PVZ] | 1317 |
| 6 | exp *death/ or *drug safety/ or exp *postmarketing surveillance/ or *risk assessment/ or *risk factor/ or *safety/ or *developmental toxicity/ or exp *reproductive toxicity/ or exp *toxicity assay/ or exp *toxicity testing/ or exp *toxicology/ or exp *"toxicity and intoxication"/ or exp *toxicological parameters/ or exp *toxic substance/ or exp *allergenicity/ or exp *carcinogenicity/ or exp *mutagenicity/ or exp *mutagenesis/ or exp *drug contraindication/ or *drug effect/ or exp *adverse drug reaction/ or exp *"drug toxicity and intoxication"/ or *food drug interaction/ or *herb drug interaction/ or exp *side effect/ | 1204250 |
| 7 | (postmarketing or post marketing or adverse or anaphyla* or complication? or dermatit* or hypersensitiv* or harm or harms or harmful or intoleran* or tolera* or toxic* or urticaria or poison* or cardiotox* or cytotox* or dermatotox* or dermotox* or embryotox* or fetotox* or genotox* or hepatotox* or immunotox* or maternotox* or nephrotox* or neurotox* or ototoxic* or iatrogen* or teratogen* or mutagen* or carcin* or death* or fatal* or hazard* or lethal* or "life-threatening" or mortal* or safe or safety or unsafe or ((side or unintended or unintentional or unwanted or unexpected or undesirable or serious* or severe or allergic or allergy) adj3 (effect* or event* or impact* or interaction* or outcome* or react* or response*))).ti,kw. | 2146080 |
| 8 | (postmarketing or post marketing or adverse or anaphyla* or complication? or dermatit* or hypersensitiv* or harm or harms or harmful or intoleran* or tolera* or toxic* or urticaria or poison* or cardiotox* or cytotox* or dermatotox* or dermotox* or embryotox* or fetotox* or genotox* or hepatotox* or immunotox* or maternotox* or nephrotox* or neurotox* or ototoxic* or iatrogen* or teratogen* or mutagen* or carcin* or death* or fatal* or hazard* or lethal* or "life-threatening" or mortal* or safe or safety or unsafe or ((side or unintended or unintentional or unwanted or unexpected or undesirable or serious* or severe or allergic or allergy) adj3 (effect* or event* or impact* or interaction* or outcome* or react* or response*))).ab. /freq=2 | 3293097 |
| 9 | 6 or 7 or 8 [adverse events] | 4866691 |
| 10 | 5 and 9 | 302 |
| 11 | limit 10 to yr = "2013 - Current" | 131 |
Figure 1: PRISMA flow diagram of the study selection process for the literature review on the safety of PVZ
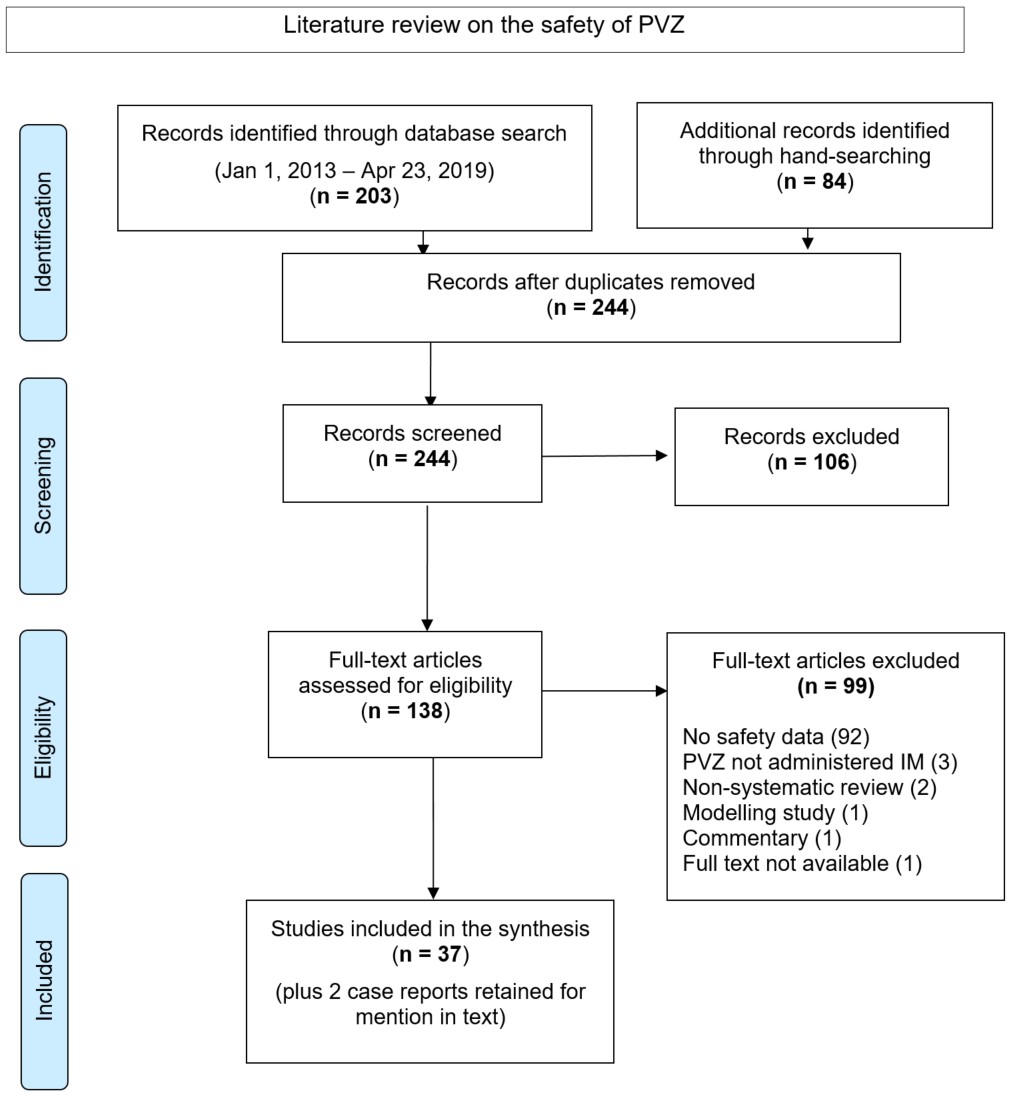
Figure 1: Text description
Abbreviations: PRISMA, preferred reporting items for systematic review and meta-analyses; PVZ, palivizumab; IM, intramuscular injection.
The PRISMA flow diagram describes the process by which articles were selected for the literature review on the safety of PVZ. The process is broken down into four stages: Identification, Screening, Eligibility and Included.
Stage 1: Identification
- 203 records were identified through the January 1, 2013 − April 23, 2019 database search, 84 records were identified through hand-searching.
- 244 records remained after duplicates were removed.
Stage 2: Screening
- 224 records were then screened.
- Of these 224 records, 106 records were excluded.
Stage 3: Eligibility
- 138 full-text articles were assessed for eligibility.
- Of these 138 full-text articles, 99 were excluded. The exclusion breakdown is as follows: 92 did not report on safety data, 3 did not report on PVZ given by intramuscular injection, 2 were non-systematic reviews, 1 was a modelling study, 1 was a commentary and for 1 study the full-text was not available.
Stage 4: Included
- 37 articles were included.
- 2 case reports were retrained for mention in text.
Table B: Level of evidence based on research design and quality (internal validity) rating of evidence
| Level | Description |
|---|---|
| I | Evidence from randomized controlled trial(s). |
| II-1 | Evidence from controlled trial(s) without randomization. |
| II-2 | Evidence from cohort or case-control analytic studies, preferably from more than one centre or research group using clinical outcome measures of vaccine efficacy. |
| II-3 | Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence. |
| III | Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees. |
| Quality Rating | Description |
|---|---|
| Good | A study (including meta-analyses or systematic reviews) that meets all design- specific criteriaTable B2 Footnote * well. |
| Fair | A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criterionTable B2 Footnote * but has no known "fatal flaw". |
| Poor | A study (including meta-analyses or systematic reviews) that has at least one design-specificTable B2 Footnote * "fatal flaw", or an accumulation of lesser flaws to the extent that the results of the study are not deemed able to inform recommendations. |
|
|
Table C: Summary of evidence related to safety of PVZ
Order of listing: Systematic reviews (alphabetically), followed by individual studies in descending order according to Level of Evidence, then Quality of Evidence, then alphabetically
| Study details | Summary | ||||
|---|---|---|---|---|---|
| Study | Study design | Participants | Summary of key findings | Level of evidence | Quality |
Robinson et al 2016Footnote 140 Funding of original RCT: Industry Funding of review: |
Systematic review of RCT: one RCT found 1998-2001 Randomized 1:1 to PVZ 15 mg/kg or placebo monthly x 5 months |
Children with cystic fibrosis aged < 2 years PVZ: 92 96% received all 5 doses |
Only one RCT found: Cohen et al 2005. Authors of systematic review obtained additional information from authors. Followed 150 d (30 days after last dose) Number of children with an event: Any AE: Related AE: Any SAE: Related SAE: No details of events provided |
I |
Good Assessed using |
Wegzyn et al., 2014Footnote 211 Funded by AbbVie Inc. |
Systematic review of randomized controlled trials and prospective observational studies 1996-2013 PVZ (PVZ) prophylaxis versus no intervention |
Children born at ≤35 wGA OR with chronic lung disease or CHD |
Systematic review without meta-analysis. Individual studies of PVZ safety identified in this review are presented separately in this table, by author. Please see elsewhere in this table for the findings from the following studies:
(data from the systematic review not used) |
No rating under NACI methods |
Average Assessed using AMSTAR) |
NBlanken et al., 2013Footnote 111 Funding: |
RCT Apr 2008-Dec 2010 Randomized 1:1 to PVZ 15 mg/kg or placebo during winter season. |
Otherwise healthy preterm infants 33 - 35 wGA and age ≤6 months at start of RSV season PVZ: 214 Median injections = 4 in each group. |
Followed to age 1 year (parents kept daily logs) Hospitalizations Number of children hospitalized RSV infection Other respiratory illness Gastroenteritis Surgery Failure to thrive Other Number of non-RSV hospitalizations * p=0.04 ** p= 0.16 |
I |
Fair (Limited AE ascertainment) |
Carbonell-Estrany et al 2010Footnote 214 Sponsor: MedImmune |
RCT Nov 2004-May 2006 RSV seasons Randomized 1:1 to 15 mg/kg PVZ or motavizumab at 30 day intervals |
Preterm ≤ 35 wkGA and age ≤ 6 months old OR PVZ: 3298 Motavizumab: 3315 |
Followed up for 150 days after randomization (30 d after last scheduled dose) Event: ≥1 AE Psychiatric disorders * Skin and subcutaneous disorders *** Injection site reactions ≥1 AE, level 3 as the highest severity ≥1 level 4 AE ≥1 SAE ≥1 AE resulting in discontinuation of drug |
I |
Good Relation of AE to study drug not stated |
Feltes et al 2003Footnote 80 Supported by MedImmune |
RCT 1998-2002 Randomized 1:1 to PVZ (15 mg/kg) or placebo every 30 days for 5 doses |
Infants age ≤24 months with PVZ: 639 Placebo: 648 |
Followed 150 d (30 d after last scheduled dose). Any adverse change in child's medical condition reported and assessed by blinded investigator for relation to study drug. AE and SAE defined. 3.3% PVZ, 4.2% placebo died; none attributed to PVZ. Adverse event category: Adverse event category: No. of AE Adverse event category: No. of children with AE Adverse event category: cardiovascular Adverse event category: respiratory system Adverse event category: Requiring medical intervention Adverse event category: Serious adverse event Adverse event category: Fatalities Adverse event category: Related AE Adverse event category: Related AE resulting in permanent discontinuation Adverse event category: Related SAE * When serious AEs reported during RSV hospitalizations were removed from the analysis, the P value was 0.043 |
I |
Good |
Feltes et al 2011Footnote 216 Supported by MedImmune |
RCT Noninferiority study of motavizumab vs PVZ Randomized 1:1 to 15 mg/kg PVZ or MVZ every 30 days for 5 doses |
Children age ≤ 24 mo with Motavizumab: 624 |
Followed 150 d (30 d after last dose). Any adverse change in child's medical condition reported and assessed by blinded investigator for relation to study drug. AE and SAE defined. Outcome n (%): ≥ 1 AE: ≥ 1 Related AE: ≥ 1 SAE: ≥ 1 related SAE: ≥ 1 related AE resulting in discontinuation of study drug: Deaths**: * maculopapular rash |
I |
Good |
Fernandez et al 2010Footnote 215 Funded by MedImmune |
RTC 2006-7 Motavizumab (M) or PVZ (P) |
Preterm ≤35 wGAk and age ≤6 months OR MMPPP: 83 PPMMM:84 MMMMM: 93 (data for last group not extracted) |
Followed from randomization through study day 150 AE (n): MVZ Subjects with ≥ 1 AE: MVZ ≥ 1 related AE : MVZ ≥ 1 SAE: MVZ ≥ 1 related SAE: MVZ AE resulting in discontinuation: MVZ Death: MVZ * staphylococcal scalded skin syndrome |
I |
Good |
IMPACT-RSV Study Group 1998Footnote 48 Funding: not stated; contributions from MedImmune |
RCT 1996–1997 RSV season Randomized 2:1 to PVZ 15 mg/kg or placebo every 30 days; total of 5 doses |
Children born at ≤35 wGA and age ≤ 6 months at start of RSV season |
Followed for 150 days from randomization (30 days after the last scheduled injection) Number of children reporting AE judged by the blinded investigator to be related to the study drug: placebo (10%) PVZ (11%). Discontinuation of injections for AEs related to PVZ was rare (0.3%). Injection site reactions included erythema, pain, induration/swelling, bruising. These were generally mild and of short duration; none was serious. Event Fever: Nervousness: Injection site reaction: Diarrhea: Rash: AST increased: URI: Liver function abnormal†: ALT increased: Vomiting: Cough: Rhinitis: Abbreviations: AST, aspartate aminotransferase; URI, upper respiratory |
I |
Good |
Makari et al 2014Footnote 212 Funding MedImmune |
RTC 2005-2007 Randomized 1:1 to 15 mg/kg PVZ |
Children with CLD age ≤ 24 months OR born at ≤ 35 wGA and age ≤ 6 months 211: liquid |
Monitored to day 150 (only SAE reported) SAE (n, 9%) Subjects with ≥1 SAE: SAE: bronchiolitis: respiratory distress: other resp: viral Infection: other infection: gastroenteritis: dehydration: malformations: seizures: miscellaneous *: * Inguinal hernia (2), umbilical hernia, failure to thrive, anal fissure, gastroesophageal reflux, hydronephrosis (1 each) |
I |
Good |
Robbie et al 2014Footnote 213 Supported by MedImmune |
Phase 2 RCT crossover design USA (21 sites) Randomized 1:1 to 15 mg/kg liquid PVZ or lyophilized PVZ day 0; crossed over to the alternate formulation on day 30, one dose |
Premature Liquid PVZ day 0: 75 |
Followed 30 days after each study dose. (After day 60, received lyophilized PVZ for remainder of season). AE, n (%) Infants with ≥ AE: Number of AE: AE related to PVZ: Fever: Injection: Pneumonia: Infants with ≥ SAE: Number of SAE: RSV: Fever: gastrointestinal: pneumonia: Apnea: Dehydration : UTI: SAE related to PVZ: |
I |
Good |
Haerskjold et al 2016Footnote 217 Funded by AbbVie |
Population-based cohort study 1999-2010 |
1,351,265 children Exposed to PVZ: (prematurity, BPD, HSCHD) Average PVZ doses: Sweden 5.4 |
Followed to Dec 31 2010 in Denmark and Dec 31 2011 in Sweden. The risk of autoimmune disease was not significantly increased after PVZ exposure (hazard ratio adjusted for age and country: 1.54; 95 % confidence interval 0.80–2.95). Not exposed: 0.54% Swedish and 0.60% Danish children developed autoimmune disease Exposed: 9 of 1192 developed autoimmune disease (0.76%). Celiac disease (4), diabetes mellitus (2) inflammatory bowel disease (2), juvenile arthritis (1) |
II-2 |
Good |
Haerskjold et al 2017Footnote 218 Funded by AbbVie |
Population-based cohort study 1999-2010 Data from national health registers |
1,351,265 children Exposed to PVZ: (prematurity, BPD, HSCHD) Average PVZ doses: |
Followed to 4 years of age or end of study, whichever came first |
II-2 |
Good |
Abushahin et al 2018Footnote 237 Funding not stated |
Descriptive single center cohort study PVZ 15 mg/kg monthly for 3-5 doses |
Born ≤ 35 wGA and <6 months of age OR ≤ 35 wGA and ≤ 2 years old with BPD or hsCHD n= 429 |
Followed monthly while receiving PVZ and for 30 days after last dose AE (anaphylaxis, fever, erythema, swelling, rash, cough, wheezing, vomiting, and/ or diarrhea) within 7 d of injection recorded No AE and no deaths related to PVZ. |
III |
N/A |
al-Alaiyan et al 2015Footnote 230 Funded by AbbVie |
Prospective Single center observational PVZ 15 mg/kg every 25-30 days for 7 doses |
Children ≤35 wGA and ≤6 months old OR chronic lung disease and ≤24 months old N= 17 |
Followed every 25-30 days for 7 months Total 7 AE in 5 patients (27.8%); 6 SAE in 4 patients SAE: Bronchiolitis: 3 (1RSV positive, 2 RSV negative); pneumonia:1 chest infection: 2 (both RSV negative) |
III |
N/A |
Bjornson et al 2018Footnote 77 Funded by AbbVie |
Retrospective multicenter observational comparative cohort Alberta province-wide (2 centers) 2000-2017 PVZ 15 mg/kg monthly |
267 children <2 yr old with cystic fibrosis 183 PVZ recipients Mean 4.4 ± 1.5 injections 84 did not receive PVZ |
Review of medical records No SAEs were related to PVZ |
III |
N/A AE mentioned in abstract and methods but not in results |
Borecka et al 2016Footnote 236 Funded by AbbVie |
Retrospective observational multicentre registry Poland 2008-9, 2009-10 |
2008-9: 2009-10: 1021 children 3241 doses avg 3.2 ± 1.04 |
Review of medical records 75.5% of children received all of their expected injections Overall: 108 AE / 3241 doses (3.33%) |
III |
N/A Methods of follow-up for AE and definitions of AE not stated |
Castillo et al 2017Footnote 226 Funded AbbVie |
Prospective international observational noncomparative study |
Born at ≤35 w GA OR with BPD OR hsCHD 458 children Total 1744 doses (avg 3.8 ± 1.3 doses) |
Monthly visits while on PVZ; monthly phone calls for one year after first PVZ dose. 397 completed one year follow-up. 1165 AE. |
III |
N/A |
Chang et al 2010Footnote 238 Funding not stated |
Retrospective cohort |
Born ≤ 35 wGA with chronic lung disease and age <2 years n=75 |
No information about follow-up. AE not defined AE within 7 days after injection recorded Erythema and swelling at the injection site was noted in 3 patients, and subsided |
III |
N/A |
Chen JJ et al. 2015Footnote 170 Funded by AbbVie, MedImmune |
Prospective Multicenter Canada RSV seasons 2008-2013 PVZ 15 mg/kg at interval of |
Premature ≤35 wGA Total = 13,025 57,392 doses 92.7% (±16.1%) of expected injections given |
Active surveillance for SAE, followed monthly until 30 days after last dose of PVZ. Infants with PVZ related SAE: Age (m): 18 Age (m): 0.7 Age (m): 0.7 Age (m): 2.4 Age (m): 7.3 Age (m): 18 |
III |
N/A |
Chi et al 2014Footnote 44 Funding: Grants from Mackay Memorial Hospital, Taipei, Taiwan and the Taiwan |
Prospective single center observational non-comparative study Taiwan 2011-2013 PVZ 15 mg/kg monthly for 6 doses |
Infants ≤ 28 wGA: 108 Total 127 718 doses |
Followed monthly while receiving PVZ and by telephone to 12 months after first dose 46 AE Local: erythema: Pain: Systemic: fever: cough: rhinorrhea: vomiting: diarrhea: irritability: |
III |
N/A |
Groothuis 2001Footnote 224 Funded: Abbott Laboratories |
Prospective International observational non-comparative study 15 northern hemisphere countries) Nov 1998 – Mar 1999 |
Preterm ≤35 wGA, age ≤6 months OR BPD, age ≤24 months requiring medical intervention < within last 6 months 565 enrolled, 530 completed study |
Followed for a maximum of 150 days (30 days after final dose). Discontinued for AE: 11 cases. 3 possibly or probably related to PVZ: (oxygen desaturation immediately after third dose; gastroenteritis; abdominal and peripheral edema) ≥ 1 AE:254 ≥ 1 Related AE Number of related AE More common related AE: Injection site reaction Fever:8 / 530 Diarrhea Nervousness/irritability Related SAE |
III |
N/A |
Groothuis 2003Footnote 225 Support: Abbot Laboratories |
Prospective International Europe (17 countries) and Saudi Arabia Oct 2000-Ap 2001 |
Preterm 29-32 wGA without CLD age < 6 months at enrollment 285 enrolled 24 did not complete |
Seen monthly and 30 days after last dose. PVZ discontinued because of AE in 2: GI disorder with peripheral edema and apnea, moderate severity, not related to PVZ; fever lasting 15 hr after 3rd PVZ dose, moderate severity, probably related to PVZ Most common AE: rhinitis (18%), cough (10%), fever 7%, diarrhea, bronchiolitis, pharyngitis (5% each). Majority mild-moderate. Event: Fever Event: Enteritis Event: Bronchitis and rhinitis Event: Cough Event: Bacterial pneumonia and conjunctivitis |
III |
N/A |
Kashiwagi et al 2018Footnote 229 Funded by AbbVie |
Prospective Multicenter post marketing surveillance Dec 2013-Dec 2015 PVZ 15 mg/kg monthly during RSV season |
Children age < 24 months receiving PVZ. |
Followed to 30 d after last dose AE: 220 (99 patients). 33 (25 patients) considered adverse drug reactions (ADR) ADR: 33 in 25 patients (pneumonia 3, rsv infection 3, other infections 11, upper respiratory tract inflammation 5, asthma 1, diarrhea 2, misc 8) SADR: 13 in 11 patients: Discontinued for AE in 7. One death (septic shock) mentioned but overall number of deaths not stated. |
III |
N/A |
Lacaze- Masmonteil et al 2002Footnote 227 Funding not stated. Abbott France acknowledged |
Prospective Multicenter France Sept 1999-Jan 2000 PVZ 15 mg/kg monthly during RSV season |
Premature ≤ 32 wGA with BPD and age < 6 m 547 enrolled; 516 received at least 1 dose |
Followed to 30 d after last dose of PVZ 10 deaths (1.9%): (acute respiratory failure children with severe chronic lung disease of the newborn (5), obstruction of tracheotomy cannula (2), intraoperative cardiac arrest, pertussis, cardiocirculatory failure (1 each). There were 15 AE judged by physician as potentially related to PVZ. : AE: Apnea AE: Fever AE: Pain at injection site AE: Hyperventilation AE: Asthenia AE: Vomiting AE: Bronchitis AE: Cough worsening AE: Urticaria Total events: |
III |
N/A |
Lacaze-Masmonteil et al 2003Footnote 231 Supported by Abbott Laboratories |
Prospective International observational study Europe and Canada 1999-2000 RSV season PVZ 15 mg/kg every 25-30 days to maximum 5 doses |
Children age ≤ 2 yr born at ≤35 wGA with BPD AND requiring medical management in previous 6 months OR judged by the investigator to be at risk for serious RSV infection |
Comparison of events in first season vs second season of PVZ No deaths occurred during the study Number of subjects ≥1 AE *: ≥1 SAE **: AE with probable or possible relationship to PVZ: Fever: Infection: Injection site reaction: Diarrhoea: Anorexia: Epistaxis: Ataxia: SAE: * The majority of AE were mild or moderate in severity (90%) and considered |
III |
N/A |
Manzoni et al 2017Footnote 221 Funded by AbbVie |
Prospective International Canada (CARESS) and Italy (number of sites not stated) 2001-2014 PVZ 15 mg/kg monthly during RSV season |
Infants born at ≤35 wGA and infants with chronic diseases and eligible for PVZ N= 14,468 |
Follow-up monthly 15 SAE in 7 patients. All hypersensitivity reactions. SAE in another 49 patients not PVZ related. Considerable overlap with data from CHEN above. |
III |
N/A Significant overlap with data from Chen et al |
Mitchell et al 2011Footnote 219 Funding: Abbott Laboratories |
Prospective Multicenter Canada |
Children eligible for PVZ: 5286 Prematurity only: 3741 19,485 doses (3.7 ± 1.5) |
Followed monthly to end of RSV season 61 SAE, 56 = hospitalizations due to respiratory infection). |
III |
N/A Limited detail on followup, no definition of AE, no details of AE |
Mori et al 2014Footnote 234 Supported by AbbVie Inc. |
Prospective Multicenter non-comparative study Oct 2011 – Mar 2012 PVZ 15 mg/kg at |
Children age ≤24 months with 28 subjects mean of 6.2 doses |
Followed to 30 days after last dose. Most frequent AE, occurring in ≥10% of subjects, were upper respiratory tract infection, gastroenteritis and eczema. Most SAEs were considered to be mild or moderate. Subjects experiencing ≥ one AE Subjects experiencing ≥ one SAE Bronchitis Gastroenteritis Encephalopathy, gastric perforation SAE at least possibly related to PVZ AE leading to discontinuation AE leading to death * Encephalopathy 104 d (after 4th dose of PVZ) |
III |
N/A Little information on follow-up |
Null et al 2005Footnote 232 Contributions from MedImmune |
Prospective observational study of subjects from prior RCT USA multicenter (6) 1997-98 RSV season PVZ 15 mg/kg dose every 30 days; total of 5 doses |
Participants: From RCT IMPACT 1998 1st yr Second yr |
Open-label follow-up to IMPACT study: Second season prophylaxis No deaths AE related to PVZ: Injection site pain (mild): Mild-moderate elevation AST or ALT: Fever: |
III |
N/A |
Paes et al 2012Footnote 220 Funding: Abbott Laboratories |
Prospective Multicenter registry 2006-2010 RSV seasons |
Premature 22,465 doses |
Follow-up telephone interviews monthly until the end of the RSV season. If hospitalized, hospital records were reviewed. 8 infants died over the course of the study for causes thought not directly related to PVZ. |
III |
N/A Overlap with data from Chen |
Pedraz 2003Footnote 46 Funding: Abbott Laboratories |
Observational multicenter prospective non interventional cohort study Spain 2000-2002 |
Preterms ≤32 wGA and age ≤ 6 months N= 1919 |
Followed monthly while on PVZ |
III |
N/A |
Pinquier et al 2009Footnote 228 Funded by Abbott Laboratories |
Prospective Multicenter observational non-comparative study France PVZ 15 mg/kg every 31± 6 days |
1371 children: premature ≤ 35 wGA: 878 6257 doses |
Followed one year after first injection. Chart review plus telephone at 4,8 and 12 months and visit at 12 months 6 deaths (underlying cardio-respiratory conditions (3), NEC (1), cause not stated, both with CHD (2). No death attributed to PVZ 30 SAE reported by investigators as probably related to PVZ (24 from one center). Mainly respiratory and ORL symptoms. Anonymous review of these 30 by evaluation committee concluded no relation to PVZ. No discontinuation because of AE |
III |
N/A Definitions of AE not stated, no details on types of AE |
Saez-Llorens et al 1998Footnote 235 Funding not stated |
Multinational observational non-comparative dose-escalation study Year of study not stated PVZ 5 mg/kg, 10 mg/kg and 15 mg/kg |
Infants born at ≤ 35 wgA and age ≤ 6 months OR with BPD and age ≤ 24 months 5 mg/kg (11) (2 to 5 doses at 30 day intervals; total of 190 doses) |
Followed days 2, 14, and 30 after dosing. 2 deaths unrelated to PVZ 3 patients had AE judged by the investigators as possibly related to study drug: |
III |
N/A |
Saji 2005Footnote 243 Funding not mentioned |
Survey |
Infants with CHD Avg 3.0 ±1.4 doses |
Questionnaire to institutions using PVZ. No details of follow-up or definitions of AE. Not classed for severity or seriousness 9 AE in 5 patients. |
III |
N/A Questionnaire not available; Discrepancies in AE data between text and table Data not included in text above |
Simon 2011Footnote 222 Supported by Abbott GmbH & Co. Germany |
Prospective Multicenter observational Registry 2002-2007 PVZ 15 mg/kg/dose monthly during RSV season. |
10,686 recipients 49,608 doses |
Followed to 4 weeks after the last dose SAE in 22 patients (0.21%). 3 deaths: SIDS; fever with diarrhoea and respiratory distress; cardiac arrest in a child with complex CHD, Assessed as not probably not related to PVZ (1) and not assessable (2) |
III |
N/A SAE not defined |
Simon 2018 (Klin Padiatr)Footnote 223 Funded by AbbVie Deutschland GmbH & Co, |
Prospective Multicenter Observational Germany 2009-2016 PVZ 15 mg/kg/dose monthly during RSV season. |
12,729 recipients (premature, BPD, HDCHD) Only data from the 1st season for each child reported 63,572 doses Avg 5.0 doses per patient |
Observed during PVZ treatment and until June 30 of that RSV season. 668 SAE reported (105 per 10,000 doses) Probable relationship to PVZ: 8 cases (1.3 per 10,000 doses): 9 deaths. None related to PVZ. |
III |
N/A |
Simon et al 2018 (Euro J Ped)Footnote 244 Supported by AbbVie GmbH |
Prospective Multicenter (Registry) 2009-2016 15 mg/kg PVZ monthly during RSV season |
Infants with Down syndrome age <25 months: 249 Average 5.0 doses |
Follow-up not described Down syndrome: Excluding RSV-related hospitalizations, most SAEs (n = 20) were hospitalizations for RTI without detection of RSV. No SAE was causally related to PVZ |
III |
N/A Follow-up procedure not clear; Limited data on SAE Data not included in text above |
Turti et al 2012Footnote 233 |
Prospective, Multicenter 2009-10 |
100 children who met criteria for high risk of severe RSV infection Total = 100 |
Followed monthly and 30 and 100 days after last dose of PVZ One discontinuation because of non-serious atopic dermatitis. AE: AE possibly related to PVZ: Rhinitis : Atopic dermatitis (mild): SAE: SAE possibly related to PVZ: * in 44 subjects |
III |
N/A |
Appendix C: Palivizumab effectiveness: additional data table
| Study details | Summary | ||||
|---|---|---|---|---|---|
| Study | Study design | Participants | Summary of key findings | Level of evidence | Quality |
Gilca et al 2020AppC Footnote ‡ Supported by the Ministère de la Santé et des Services sociaux du Québec |
Retrospective cohort study Multicenter (Nunavik, Quebec); 3 centers Nov 1, 2013 to June 31 2019 PZV effectiveness to prevent RSV hospitalization PVZ every 28 days to a maximum of 3 doses first season of intervention, up to 5 doses for subsequent 2 seasons. RSV diagnosed by rapid antigen detection tests (RADT) (97% both pre-intervention and during intervention) and/or PCR (24% pre-intervention, 73% during intervention) |
Whole cohort of infants age < 1 yr (born Nov 2012 to June 2019): Intervention period: HFT < 3 months old at start of RSV season or born during RSV season, followed to age <1 yr: 469 (73% of eligible infants) received PVZ |
Over six seasons, RSVH rates 50.2/1000 in all infants < 1 yr old (72.6/1000 after adjustment * for under detection). Intervention period: Direct PVZ effectiveness in HFT infants estimated by comparing the incidence of RSV hospitalizations There was no difference in RSVH in the groups who did or did not receive PVZ or during PVZ-protected or unprotected days: Infants who received no PVZ: Infants who received all PVZ doses on time: Unprotected days **: PVZ-protected days **: * 1 - relative risk protected/unprotected x 100% |
II-2 |
FairAppC Footnote † Sensitivity analyses were done by considering the wash-out period as days with PVZ protection or as days without PVZ protection; PVZ effectiveness was essentially unchanged. Small number of cases, wide variation in numbers of RSVH in different years. Co-infections with other respiratory viruses were frequent in both protected and unprotected infants |
|
|||||
Footnotes
- Footnote 1
-
Bont L, Checchia PA, Fauroux B, et al. Defining the Epidemiology and Burden of Severe Respiratory Syncytial Virus Infection among Infants and Children in Western Countries. Infectious Diseases and Therapy. 2016 Aug 1;5(3):271-98. doi: 10.1007/s40121-016-0123-0.
- Footnote 2
-
Shi T, McAllister DA, O'Brien KL, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. The Lancet. 2017 Sep 2;390(10098):946-58. doi: 10.1016/S0140-6736(17)30938-8.
- Footnote 3
-
Mazur NI, Higgins D, Nunes MC, et al. The Respiratory Syncytial Virus Vaccine Landscape: lessons from the graveyard and promising candidates. Lancet Infect Dis. 2018 Oct;18(10):e295-311 doi: 10.1016/S1473-3099(18)30292-5.
- Footnote 4
-
National Advisory Committee on Immunization. Statement on The Recommended Use Of Monoclonal Anti-RSV Antibody (PVZ). Canada Com Dis Rep = Releve des maladies transmissibles au Canada JID - 9303729 2003 [Internet]. Ottawa (ON) : Public Health Agency of Canada; 2003 Sep 15 [cited 2022 May 10]. Available from: https://pubmed.ncbi.nlm.nih.gov/14524195/.
- Footnote 5
-
Committee on Infectious Diseases. From the American Academy of Pediatrics: Policy Statements--Modified Recommendations for Use of PVZ for Prevention of Respiratory Syncytial Virus Infections. Pediatrics. 2009 Dec;124(6):1694-701. doi: 10.1542/peds.2009-2345.
- Footnote 6
-
American Academy of Pediatrics Committee on Infectious Diseases; American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated Guidance for PVZ Prophylaxis among Infants and Young Children at Increased Risk of Hospitalization for Respiratory Syncytial Virus Infection. Pediatrics. JID – 0376422. 2014 Aug;134(2):415-20. doi: 10.1542/peds.2014-1666.
- Footnote 7
-
American Academy of Pediatrics Committee on Infectious Diseases; American Academy of Pediatrics Bronchiolitis Guidelines Committee. Technical Report. Updated Guidance for PVZ Prophylaxis among Infants and Young Children at Increased Risk of Hospitalization for Respiratory Syncytial Virus Infection. Pediatrics. JID – 0376422. 2014 Aug;134(2):e620-38. doi: 10.1542/peds.2014-1665.
- Footnote 8
-
Robinson J.L., Saux N.L. Preventing Hospitalizations for Respiratory Syncytial Virus Infection [Internet]. Ottawa (ON): Canadian Pedeatric Society; Infectious Disease and Immunization Committee; 2015 Sep 8;20:321-6. [cited 2022 May 10] Available from: https://cps.ca/documents/position/preventing-hospitalizations-for-rsv-infections.
- Footnote 9
-
Ismail SJ, Langley JM, Harris TM, et al. Canada's National Advisory Committee on Immunization (NACI): Evidence-Based Decision-Making on Vaccines and Immunization. Vaccine. 2010 Apr 19;28:A58-A63. doi:10.1016/j.vaccine.2010.02.035.
- Footnote 10
-
Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: A Measurement Tool to Assess the Methodological Quality of Systematic Reviews. BMC Medical Research Methodology. 2007 Feb 15;7. https://doi.org/10.1186/1471-2288-7-10.
- Footnote 11
-
Wingert A, Pillay J, Moore DL, et al. Burden of Illness in Infants and Young Children Hospitalised for Respiratory Syncythial Virus. Can Commun Dis Rep. 2021 Sep 10;47(9):381-396. doi: 10.14745/ccdr.v47i09a05.
- Footnote 12
-
National Advisory Committee on Immunization. NACI Literature Review on the Effects of PVZ Prophylaxis on Reducing the Complications Associated with Respiratory Syncytial Virus in Infants. 2021.
- Footnote 13
-
Ismail SJ, Hardy K, Tunis MC, et al. A Framework for the Systematic Consideration of Ethics, Equity, Feasibility, and Acceptability in Vaccine Program Recommendations. Vaccine. 2020 Aug 10;38(36):5861. doi:10.1016/j.vaccine.2020.05.051.
- Footnote 14
-
American Academy of Pediatrics, Committee on Infectious Diseases. Red Book (2018): Report of the Committee on Infectious Diseases, 31st Edition [Internet]. Itasca (IL): American Academy of Pediatrics 2018:2018:682-692 [cited 2022 May 10]. Available from: https://seciss.facmed.unam.mx/wp-content/uploads/2021/02/Red-Book-31th-Edition.pdf.
- Footnote 15
-
Schanzer DL, Langley JM, Tam TW. Hospitalization Attributable to Influenza and Other Viral Respiratory Illnesses in Canadian Children. The Pediatric Infectious Disease Journal. 2006 Sep 1;25(9):795–800. doi: 10.1097/01.inf.0000232632.86800.8c.
- Footnote 16
-
Hall C, Weinberg G, Blumkin A, et al. Respiratory Syncytial Virus-Associated Hospitalizations among Children Less than 24 Months of Age. Pediatrics. 2013 Aug;132(2):e341-8 http://dx.doi.org/10.1542/peds.2013-0303.
- Footnote 17
-
Pisesky A, Benchimol EI, Wong CA, et al. Incidence of Hospitalization for Respiratory Syncytial Virus Infection amongst Children in Ontario, Canada: A Population-Based Study Using Validated Health Administrative Data. PLoS ONE. 2016 Mar 9;11(3):e0150416. doi: 10.1371/journal.pone.0150416.
- Footnote 18
-
Scheltema NM, Gentile A, Lucion F, et al. Global Respiratory Syncytial Virus-Associated Mortality in Young Children (RSV GOLD): A Retrospective Case Series. Lancet Glob Health. 2017 Oct 5;5(10):e984-e991. doi: 10.1016/S2214-109X(17)30344-3.
- Footnote 19
-
Tam J, Papenburg J, Fanella S, et al. Pediatric Investigators Collaborative Network on Infections in Canada Study of Respiratory Syncytial Virus-Associated Deaths in Pediatric Patients in Canada, 2003-2013. Clin Infect Dis. 2019 Jan 1;68(1):113-9. http://dx.doi.org/10.1093/cid/ciy413.
- Footnote 20
-
Kua KP, Lee S. Systematic Review of the Safety and Efficacy of PVZ among Infants and Young Children with Cystic Fibrosis. Pharmacotherapy. 2017 Jun;37(6):755-69. http://dx.doi.org/10.1002/phar.1936.
- Footnote 21
-
Kristensen K., Hjuler T., Ravn H., et al. Chronic Diseases, Chromosomal Abnormalities, and Congenital Malformations as Risk Factors for Respiratory Syncytial Virus Hospitalization: A Population-Based Cohort Study. Clin Infect Dis. 2012 Mar;54(6):810-7. http://dx.doi.org/10.1093/cid/cir928.
- Footnote 22
-
Manzoni P, Figueras-Aloy J, Simoes EAF, et al. Defining the Incidence and Associated Morbidity and Mortality of Severe Respiratory Syncytial Virus Infection among Children with Chronic Diseases. Infectious diseases and therapy. 2017 Sep;6(3):383-411. doi: 10.1007/s40121-017-0160-3.
- Footnote 23
-
Banerji A, Panzov V, Young M, et al. Hospital Admissions for Lower Respiratory Tract Infections among Infants in the Canadian Arctic: A Cohort Study. CMAJ Open. 2016 Oct 18;4(4):E615-22. https://dx.doi.org/10.9778/cmajo.20150051.
- Footnote 24
-
Shi T, Denouel A, Tietjen AK, et al. Global Disease Burden Estimates of Respiratory Syncytial Virus-Associated Acute Respiratory Infection in Older Adults in 2015: A Systematic Review and Meta-Analysis. J Infect Dis. 2020 Oct 7;222:S577-S583. doi: 10.1093/infdis/jiz059.
- Footnote 25
-
Centre for Immunization and Respiratory Infectious Diseases (CIRID). Respiratory Virus Detections in Canada 2014-2021 [Internet]. Ottawa (ON): Public Health Agency of Canada. [cited 2022 May 10]. Available from: https://www.canada.ca/en/public-health/services/surveillance/respiratory-virus-detections-canada.html.
- Footnote 26
-
Doucette A, Jiang XH, Fryzek J, et al. Trends in Respiratory Syncytial Virus and Bronchiolitis Hospitalization Rates in High-Risk Infants in a United States Nationally Representative Database, 1997-2012. PLoS ONE. 2016 Apr 6;11(4):e0152208. doi: 10.1371/journal.pone.0152208.
- Footnote 27
-
Farber HJ, Buckwold FJ, Lachman B, et al. Observed Effectiveness of PVZ for 29-36-Week Gestation Infants. Pediatrics. 2016 Aug;138(2):e20160627. doi: 10.1542/peds.2016-0627.
- Footnote 28
-
Helfrich AM, Nylund CM, Eberly MD, et al. Healthy Late-Preterm Infants Born 33-36+6 Weeks Gestational Age have Higher Risk for Respiratory Syncytial Virus Hospitalization. Early Hum Dev. 2015 Sep;91(9):541-6. doi: 10.1016/j.earlhumdev.2015.06.009.
- Footnote 29
-
Fauroux B, Gouyon JB, Roze JC, et al. Respiratory Morbidity of Preterm Infants of Less Than 33 Weeks Gestation without Bronchopulmonary Dysplasia: A 12-Month Follow-Up of the CASTOR Study Cohort. Epidemiol Infect. 2014 Jul;142(7):1362-74. doi: 10.1017/S0950268813001738.
- Footnote 30
-
Ambrose CS, Anderson EJ, Simoes EAF, et al. Respiratory Syncytial Virus Disease in Preterm Infants in the US Born at 32-35 Weeks Gestation not Receiving Immunoprophylaxis. Pediatr Infect Dis J. 2014 Jun;33(6):576-82. doi: 10.1097/INF.0000000000000219.
- Footnote 31
-
Blanken MO, Korsten K, Achten NB, et al. Population-Attributable Risk of Risk Factors for Recurrent Wheezing in Moderate Preterm Infants During the First Year of Life. Paediatr Perinat Epidemiol. 2016 Jul;30(4):376-85. doi:10.1111/ppe.12295.
- Footnote 32
-
Carbonell-Estrany X, Perez-Yarza EG, Garcia LS, et al. Long-Term Burden and Respiratory Effects of Respiratory Syncytial Virus Hospitalization in Preterm Infants-The SPRING Study. PLoS ONE. 2015 May 8;10(5):e0125422. doi:10.1371/journal.pone.0125422.
- Footnote 33
-
Korsten K, Blanken MO, Nibbelke EE, et al. Prediction Model of RSV-Hospitalization in Late Preterm Infants: An Update and Validation Study. Early Hum Dev. 2016 Apr;95:35-40. doi: 10.1016/j.earlhumdev.2016.01.020.
- Footnote 34
-
Ryan VMJ, Langley JM, Dodds L, et al. Estimating Respiratory Syncytial Virus-Associated Hospitalization in the First Year of Life Among Infants Born at 32-35 Weeks of Gestation. Pediatr Infect Dis J. 2016 Aug;35(8):851-855. doi: 10.1097/INF.0000000000001186.
- Footnote 35
-
Straňák Z, Saliba E, Kosma P, et al. Predictors of RSV LRTI Hospitalization in Infants Born at 33 to 35 Weeks Gestational Age: A Large Multinational Study (PONI). PLoS ONE. 2016 Jun 16;11(6):e0157446. doi: 10.1371/journal.pone.0157446.
- Footnote 36
-
Zomer-Kooijker K, Uiterwaal CSPM, van der Gugten AC, et al. Decreased Lung Function Precedes Severe Respiratory Syncytial Virus Infection and Post-Respiratory Syncytial Virus Wheeze in Term Infants. Eur Respir J. 2014 Sep;44(3):666-74. doi: 10.1183/09031936.00009314.
- Footnote 37
-
McLaurin KK, Farr AM, Wade SW, et al. Respiratory Syncytial Virus Hospitalization Outcomes and Costs of Full-Term and Preterm Infants. J Perinatol. 2016 Nov;36(11):990-6. doi: 10.1038/jp.2016.113.
- Footnote 38
-
Griffin MP, Yuan Y, Takas T, et al. Single-Dose Nirsevimab for Prevention of RSV in Preterm Infants. N Engl J Med. 2020 Jul;30(5);383:415-425. doi: 10.1056/NEJMoa1913556.
- Footnote 39
-
Papenburg J, Defoy I, Massé E, et al. Impact of the Withdrawal of PVZ Immunoprophylaxis on the Incidence of Respiratory Syncytial Virus (RSV) Hospitalizations Among Infants Born at 33 to 35 Weeks' Gestational Age in the Province of Quebec, Canada: The RSV-Quebec Study. Pediatric Infect Dis Soc. 2021 Apr 3;10(3):237-244. doi: 10.1093/jpids/piaa046.
- Footnote 40
-
Anderson EJ, Carbonell-Estrany X, Blanken M, et al. Burden of Severe Respiratory Syncytial Virus Disease among 33-35 Weeks' Gestational Age Infants Born During Multiple Respiratory Syncytial Virus Seasons. Pediatr Infect Dis J. 2017a Feb;36(2):160-7. doi: 10.1097/INF.0000000000001377.
- Footnote 41
-
Notario G, Vo P, Gooch K, et al. Respiratory Syncytial Virus-Related Hospitalization in Premature Infants Without Bronchopulmonary Dysplasia: Subgroup Efficacy Analysis of the IMpact-RSV Trial by Gestational Age Group. Pediatric Health Med Ther. 2014 May 30;2014(5):43-48. https://doi.org/10.2147/PHMT.S59572.
- Footnote 42
-
Stevens TP, Sinkin RA, Hall CB, et al. Respiratory Syncytial Virus and Premature Infants Born at 32 Weeks' Gestation or Earlier: Hospitalization and Economic Implications of Prophylaxis. Arch Pediatr Adolesc Med. 2000 Jan;154:55-61. [cited 2022 May 10]. Available from: https://jamanetwork.com/journals/jamapediatrics/fullarticle/348500.
- Footnote 43
-
Boyce TG, Mellen BG, Mitchel EF J, et al. Rates of Hospitalization for Respiratory Syncytial Virus Infection among Children in Medicaid. J Pediatr. 2000 Dec;137(6):865-70 doi:10.1067/mpd.2000.110531.
- Footnote 44
-
Chi H, Hsu CH, Chang JH, et al. A Novel Six Consecutive Monthly Doses of PVZ Prophylaxis Protocol for the Prevention of Respiratory Syncytial Virus Infection in High-Risk Preterm Infants in Taiwan. PLoS One. 2014 Jun 27;9(6):e100981. doi: 10.1371/journal.pone.0100981.
- Footnote 45
-
Park HW, Lee BS, Kim AR, et al. Epidemiology of Respiratory Syncytial Virus Infection in Infants Born at Less than Thirty-Five Weeks of Gestational Age. Pediatr Infect Dis J. 2012 Aug;31(8):e99-e104. doi: 10.1097/INF.0b013e318257f619.
- Footnote 46
-
Pedraz C, Carbonell-Estrany X, Figueras-Aloy J, et al. Effect of PVZ prophylaxis in decreasing respiratory syncytial virus hospitalizations in premature infants. Pediatr Infect Dis J. 2003 Sep;22(9):823-7. doi: 10.1097/01.inf.0000086403.50417.7c.
- Footnote 47
-
Grimaldi M, Gouyon B, Sagot P, et al. PVZ Efficacy in Preterm Infants with Gestational Age <30 Weeks without Bronchopulmonary Dysplasia. Pediatr Pulmonol. 2007 Mar;42(3):189-92. doi: 10.1002/ppul.20503.
- Footnote 48
-
IMpact-RSV. PVZ, a Humanized Respiratory Syncytial Virus Monoclonal Antibody, Reduces Hospitalization from Respiratory Syncytial Virus Infection in High-Risk Infants. The IMpact-RSV Study Group. Pediatrics. 1998 Sep;102(3):531-537. [cited 2022 May 10]. Available from: https://pubmed.ncbi.nlm.nih.gov/9724660.
- Footnote 49
-
Winterstein AG, Knox CA, Kubilis P, et al. Appropriateness of Age Thresholds for Respiratory Syncytial Virus Immunoprophylaxis in Moderate-Preterm Infants - A Cohort Study. JAMA Pediatr. 2013 Dec;167(12):1118-24. doi: 10.1001/jamapediatrics.2013.2636.
- Footnote 50
-
Anderson EJ, Krilov LR, DeVincenzo JP, et al. SENTINEL1: An Observational Study of Respiratory Syncytial Virus Hospitalizations among U.S. Infants Born At 29 to 35 Weeks' Gestational Age Not Receiving Immunoprophylaxis. Am J Perinatol. 2017 Jan;34(1):51-51. doi: 10.1055/s-0036-1584147.
- Footnote 51
-
Rajah B, Sánchez PJ, Garcia-Maurino C, et al. Impact of the Updated Guidance for PVZ Prophylaxis against Respiratory Syncytial Virus Infection: A Single Center Experience. J Pediatr. 2017 Feb;181:183-8. doi: 10.1016/j.jpeds.2016.10.074.
- Footnote 52
-
Luchsinger V, Ampuero S, Palomino MA, et al. Comparison of Virological Profiles of Respiratory Syncytial Virus and Rhinovirus in Acute Lower Tract Respiratory Infections in Very Young Chilean Infants, According To Their Clinical Outcome. J Clin Virol. 2014 Sep;61(1):138-44. doi: 10.1016/j.jcv.2014.06.004.
- Footnote 53
-
Caserta MT, Qiu X, Tesini B, et al. Development of a Global Respiratory Severity Score for Respiratory Syncytial Virus Infection in Infants. J Infect Dis. 2017 Mar 1;215(5):750-6. doi: 10.1093/infdis/jiw624.
- Footnote 54
-
Fergie J, Suh M, Jiang X, et al. Respiratory Syncytial Virus and All-Cause Bronchiolitis Hospitalizations among Preterm Infants Using the Pediatric Health Information System (PHIS). J Infect Dis. 2020 Jul 21;225(7):1197-1204. doi: 10.1093/infdis/jiaa435.
- Footnote 55
-
Anderson EJ, DeVincenzo JP, Simões EAF, et al. SENTINEL1: 2-Season Study of Respiratory Syncytial Virus Hospitalizations among U.S. Infants Born at 29 to 35 Weeks' Gestational Age Not Receiving Immunoprophylaxis. Am J Perinatol. 2020 Mar;37(4):421-9. doi: 10.1055/s-0039-1681014
- Footnote 56
-
Jang MJ, Kim YJ, Hong S, et al. Positive Association of Breastfeeding on Respiratory Syncytial Virus Infection in Hospitalized Infants: A Multicenter Retrospective Study. Korean J Pediatr. 2020 Apr;63(4):135-40. doi: 10.3345/kjp.2019.00402.
- Footnote 57
-
Garcia-Mauriño C, Moore-Clingenpeel M, Thomas J et al. Viral Load Dynamics and Clinical Disease Severity in Infants with Respiratory Syncytial Virus Infection. J Infect Dis. 2019 Apr 19;219(8):1207-15. doi: 10.1093/infdis/jiy655.
- Footnote 58
-
Oz-Alcalay L, Ashkenazi S, Glatman-Freedman A, et al. Hospitalization for Respiratory Syncytial Virus Bronchiolitis in the PVZ Prophylaxis Era: Need for Reconsideration of Preventive Timing and Eligibility. Isr Med Assoc J. 2019 Feb 1;21:110-5 [cited 2022 May 10]. Available from: https://www.semanticscholar.org/paper/Hospitalization-for-Respiratory-Syncytial-Virus-in-Oz-Alcalay- Ashkenazi/eb2d8bda758bc528cd2ffaeaaedb4d7145481905
- Footnote 59
-
Midulla F, Nenna R, Scagnolari C, et al. How Respiratory Syncytial Virus Genotypes Influence the Clinical Course in Infants Hospitalized for Bronchiolitis. J Infect Dis. 2019 Jan 29;219(4):526-34. doi: 10.1093/infdis/jiy496.
- Footnote 60
-
Figueras-Aloy J, Manzoni P, Paes B, et al. Defining the Risk and Associated Morbidity and Mortality of Severe Respiratory Syncytial Virus Infection Among Preterm Infants Without Chronic Lung Disease or CHD. Infect Dis Ther. 2016 Dec;5(4):417-52. doi: 10.1007/s40121-016-0130-1.
- Footnote 61
-
Gouyon JB, Roze JC, Guillermet-Fromentin C, et al. Hospitalizations for Respiratory Syncytial Virus Bronchiolitis in Preterm Infants at <33 Weeks Gestation without Bronchopulmonary Dysplasia: The CASTOR Study. Epidemiol Infect. 2013 Apr;141(4):816-26. http://dx.doi.org/10.1017/S0950268812001069.
- Footnote 62
-
Vu LD, Siefker D, Jones TL, et al. Elevated Levels of Type 2 Respiratory Innate Lymphoid Cells In Human Infants with Severe Respiratory Syncytial Virus Bronchiolitis. Am J Respir Crit Care Med. 2019 Nov 27;200(11):1414-23. http://dx.doi.org/10.1164/rccm.201812-2366OC.
- Footnote 63
-
Rodriguez-Gonzalez M, Perez-Reviriego AA, Castellano-Martinez A, et al. Left Ventricular Dysfunction and Plasmatic NT-Probnp are Associated with Adverse Evolution in Respiratory Syncytial Virus Bronchiolitis. Diagn. 2019 Jul 27;9(3):85. doi: 10.3390/diagnostics9030085.
- Footnote 64
-
Simões EAF, Ambrose CS, Wu X, et al. Intensive Care Unit Admission Rates for Respiratory Syncytial Virus Infection as a Function of Age in Preterm Infants Born at 32-35-Week Gestation and Not Receiving Immunoprophylaxis. Pediatr Infect Dis J. 2015 Mar;34(3):331. doi: 10.1097/INF.0000000000000566.
- Footnote 65
-
Checchia PA, Paes B, Bont L, et al. Defining the Risk and Associated Morbidity and Mortality of Severe Respiratory Syncytial Virus Infection among Infants with Congenital Heart Disease. Infect Dis Ther. 2017 Mar;6(1):37-56. doi: 10.1007/s40121-016-0142-x.
- Footnote 66
-
Szabo SM, Gooch KL, Bibby MM, et al. The Risk of Mortality among Young Children Hospitalized for Severe Respiratory Syncytial Virus Infection. Paediatr Respir Rev. 2013 Jan;13:Suppl 2:S1-S8. doi: 10.1016/S1526-0542(12)00095-4.
- Footnote 67
-
Statistics Canada. Table: 13-10-0425-01 Live Births, by Weeks of Gestation https://doi.org/10.25318/1310042501-eng.
- Footnote 68
-
Pignotti MS, Leo MC, Pugi A, et al. Consensus Conference on the Appropriateness of PVZ Prophylaxis in Respiratory Syncytial Virus Disease. Pediatr Pulmonol. 2016 Oct;51(10):1088-96. doi: 10.1002/ppul.23561.
- Footnote 69
-
Hall CB, Weinberg GA, Iwane MK, et al. The Burden of Respiratory Syncytial Virus Infection in Young Children. N Engl J Med. 2009;360(6):588-98. doi: 10.1056/NEJMoa0804877
- Footnote 70
-
Meissner HC, Bocchini JA, Brady MT, et al. The Role of Immunoprophylaxis in the Reduction of Disease Attributable to Respiratory Syncytial Virus. Pediatrics. 2009 Dec;124(6):1676-9. doi: 10.1542/peds.2009-2346.
- Footnote 71
-
Figueras-Aloy J, Carbonell-Estrany X, Quero-Jimenez J, et al. Flip-2 Study: Risk Factors Linked to Respiratory Syncytial Virus Infection Requiring Hospitalization in Premature Infants Born in Spain at a Gestational Age of 32 to 35 Weeks. Pediatr Infect Dis J. 2008 Sep;27(9):788-93. doi: 10.1097/INF.0b013e3181710990.
- Footnote 72
-
Paes B, Fauroux B, Figueras-Aloy J, et al. Defining the Risk and Associated Morbidity and Mortality of Severe Respiratory Syncytial Virus Infection Among Infants with Chronic Lung Disease. Infect Dis Ther. 2016 Dec;5(4):453-471. doi: 10.1007/s40121-016-0137-7.
- Footnote 73
-
Winterstein AG, Choi Y, Meissner HC. Association of Age with Risk of Hospitalization for Respiratory Syncytial Virus in Preterm Infants with Chronic Lung Disease. JAMA Pediatr. 2018;172(2):154-60. doi: 10.1001/jamapediatrics.2017.3792.
- Footnote 74
-
Checchia PA, Nalysnyk L, Fernandes AW, et al. Mortality and Morbidity among Infants at High Risk for Severe Respiratory Syncytial Virus Infection Receiving Prophylaxis with PVZ: A Systematic Literature Review and Meta-Analysis. Crit Care Med. 2011 Sep;12(5):580-8. doi: 10.1097/PCC.0b013e3182070990
- Footnote 75
-
Hama I, Takahashi S, Nakamura T, et al. Risk of Respiratory Syncytial Virus Infection in Infants with Congenital Cystic Lung Disease. Pediatrics International. 2015 Apr;57(2):253-7. doi: 10.1111/ped.12544.
- Footnote 76
-
Drummond D, Thumerelle C, Reix P, et al. Effectiveness of PVZ in Children with Childhood Interstitial Lung Disease: The French Experience. Pediatr Pulmonol. 2016 Jul;51(7):688-95. doi: 10.1002/ppul.23354.
- Footnote 77
-
Bjornson C, Chan P, Li A, et al. PVZ Prophylaxis for Respiratory Syncytial Virus in Infants with Cystic Fibrosis: Is there a Need? Eur J Clin Microbiol Infect Dis. 2018 Jun;37(6):1113-8. doi: 10.1007/s10096-018-3225-7.
- Footnote 78
-
Groves HE, Jenkins L, Macfarlane M, et al. Efficacy and Long-Term Outcomes of PVZ Prophylaxis to Prevent Respiratory Syncytial Virus Infection in Infants with Cystic Fibrosis in Northern Ireland. Pediatr Pulmonol. 2016 Apr;51(4):379-85. doi: 10.1002/ppul.23376.
- Footnote 79
-
Chu PY, Hornik CP, Li JS, et al. Respiratory Syncytial Virus Hospitalisation Trends in Children with Haemodynamically Significant Heart Disease, 1997-2012. Cardiol Young. 2017 Jan;27(1):16-25. doi: 10.1017/S1047951116000470.
- Footnote 80
-
Feltes TF, Cabalka AK, Meissner HC, et al. PVZ prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003 Oct;143(4):532-40. doi: 10.1067/s0022-3476(03)00454-2.
- Footnote 81
-
Chiu SN, Shao PL, Chen HC, et al. Risk of Respiratory Syncytial Virus Infection in Cyanotic Congenital Heart Disease in a Subtropical Area. J Pediatr. 2016 Apr;171:25-30e1. doi: 10.1016/j.jpeds.2015.12.029.
- Footnote 82
-
Resch B, Sommer C, Nuijten MJC, et al. Cost-Effectiveness of PVZ for Respiratory Syncytial Virus Infection in High-Risk Children, Based On Long-Term Epidemiologic Data from Austria. Pediatr Infect Dis J, 2012 Jan;31(1):e1-8. doi: 10.1097/INF.0b013e318235455b.
- Footnote 83
-
Beckhaus AA, Castro-Rodriguez JA. Down syndrome and the Risk of Severe RSV Infection: A Meta-Analysis. Pediatrics. 2018 Sep 1;142(3):e20180225. doi: 10.1542/peds.2018-0225.
- Footnote 84
-
Stagliano DR, Nylund CM, Eide MB, et al. Children with Down syndrome are High-Risk for Severe Respiratory Syncytial Virus Disease. J Pediatr. 2015 Mar;166(3):703-9. doi: 10.1016/j.jpeds.2014.11.058.
- Footnote 85
-
Feldman AG, Sundaram SS, Beaty BL, et al. Hospitalizations for Respiratory Syncytial Virus and Vaccine-Preventable Infections in the First 2 Years after Pediatric Liver Transplant. J Pediatr. 2017 Mar;182:232,238.e1. doi: 10.1016/j.jpeds.2016.12.021.
- Footnote 86
-
Sadreameli SC, Reller ME, Bundy DG, et al. Respiratory Syncytial Virus and Seasonal Influenza Cause Similar Illnesses in Children with Sickle Cell Disease. Pediatr Blood Cancer. 2014 May;61(5):875-8. doi: 10.1002/pbc.24887.
- Footnote 87
-
El Saleeby CM, Somes GW, DeVincenzo JP, et al. Risk Factors for Severe Respiratory Syncytial Virus Disease in Children with Cancer: The Importance of Lymphopenia and Young Age. Pediatrics. 2008 Feb;121(2):235-243. doi: 10.1542/peds.2007-1102.
- Footnote 88
-
Kim YJ, Guthrie KA, Waghmare A, et al. Respiratory Syncytial Virus in Hematopoietic Cell Transplant Recipients: Factors Determining Progression to Lower Respiratory Tract Disease. J Infect Dis. 2014 Apr 15;209(8):1195-204. doi: 10.1093/infdis/jit832.
- Footnote 89
-
O'Brien KL, Chandran A, Weatherholtz R, et al. Efficacy of Motavizumab for the Prevention of Respiratory Syncytial Virus Disease in Healthy Native American Infants: A Phase 3 Randomised Double-Blind Placebo-Controlled Trial. Lancet Infect Dis. 2015 Dec;15(12):1398-408. doi: 10.1016/S1473-3099(15)00247-9.
- Footnote 90
-
Gilca R, Billard MN, Zafack J, et al. Effectiveness of PVZ Immunoprophylaxis to Prevent Respiratory Syncytial Virus Hospitalizations in Healthy Full-Term <6-Month-Old Infants from the Circumpolar Region of Nunavik, Quebec, Canada. Prev Med Rep. 2020 Dec;20:101180. doi: 10.1016/j.pmedr.2020.101180.
- Footnote 91
-
Banerji A, Lanctot KL, Paes BA, et al. Comparison of the Cost of Hospitalization for Respiratory Syncytial Virus Disease Versus PVZ Prophylaxis in Canadian Inuit Infants. Pediatr Infect Dis J. 2009 Aug;28(8):702-6. doi: 10.1097/INF.0b013e31819df78e.
- Footnote 92
-
Singleton R, Dooley L, Bruden D, et al. Impact of PVZ Prophylaxis on Respiratory Syncytial Virus Hospitalizations in High Risk Alaska Native Infants. Pediatr Infect Dis J. 2003 Jun;22(6):540-5. http://dx.doi.org/10.1097/00006454-200306000-00010.
- Footnote 93
-
Kim L, Rha B, Abramson JS, et al. Identifying Gaps in Respiratory Syncytial Virus Disease Epidemiology in the United States Prior to the Introduction of Vaccines. CID. 2017 Sep 15;65(6):1020-5. doi: 10.1093/cid/cix432.
- Footnote 94
-
Fauroux B, Simoes EAF, Checchia PA, et al. The Burden and Long-Term Respiratory Morbidity Associated with Respiratory Syncytial Virus Infection in Early Childhood. Infect Dis Ther. 2017 Jun;6(2):173-97. doi:10.1007/s40121-017-0151-4.
- Footnote 95
-
Groves HE SM. Respiratory Syncytial Virus and Asthma Inception: Cause and Effect, or Shared Susceptibility?. J Infect Dis. 2019 Jul 19;220(4):547-549. doi: 10.1093/infdis/jiy672.
- Footnote 96
-
Chawes BLK, Poorisrisak P, Johnston SL, et al. Neonatal Bronchial Hyperresponsiveness Precedes Acute Severe Viral Bronchiolitis in Infants. J Allergy Clin Immunol. 2012 Aug;130(2):354-61. doi: 10.1016/j.jaci.2012.04.045.
- Footnote 97
-
Bonnelykke K, Vissing NH, Sevelsted A, et al. Association Between Respiratory Infections in Early Life and Later Asthma is Independent of Virus Type. J Allergy Clin Immunol. 2015 Jul;136(1):81-6. doi: 10.1016/j.jaci.2015.02.024.
- Footnote 98
-
Driscoll AJ, Arshad SH, Bont L, et al. Does Respiratory Syncytial Virus Lower Respiratory Illness in Early Life Cause Recurrent Wheeze of Early Childhood and Asthma? Critical Review of the Evidence and Guidance for Future Studies from a World Health Organization-Sponsored Meeting. Vaccine. 2020 Mar 4;38(11):2435-48. doi: 10.1016/j.vaccine.2020.01.020.
- Footnote 99
-
Backman K, Piippo-Savolainen E, Ollikainen H, et al. Adults Face Increased Asthma Risk After Infant RSV Bronchiolitis and Reduced Respiratory Health-Related Quality of Life After RSV Pneumonia. Acta Paediatr. 2014 Aug;103(8):850-5. doi: 10.1111/apa.12662.
- Footnote 100
-
Backman K, Ollikainen H, Piippo-Savolainen E, et al. Asthma and Lung Function in Adulthood after a Viral Wheezing Episode in Early Childhood. Clin Exp Allergy. 2018 Feb;48(2):138-46. doi: 10.1111/cea.13062.
- Footnote 101
-
Korsten K, Blanken MO, Buiteman BJM, et al. RSV Hospitalization in Infancy Increases the Risk of Current Wheeze at Age 6 in Late Preterm Born Children without Atopic Predisposition. Eur J Pediatr. 2019 Aprl;178(4):455-62. doi: 10.1007/s00431-018-03309-0.
- Footnote 102
-
Mejias A, Wu B, Tandon N, et al. Risk of Childhood Wheeze and Asthma after Respiratory Syncytial Virus Infection in Full-Term Infants. Pediatr Allergy Immunol. 2020 Jan;31(1):47-56. doi: 10.1111/pai.13131.
- Footnote 103
-
Henderson FW, Collier AM, Clyde WA Jr, et al. Respiratory-Syncytial-Virus Infections, Reinfections and Immunity. A Prospective, Longitudinal Study in Young Children. N Engl J Med. 1979 Mar 8;300(10):530-4. doi: 10.1056/NEJM197903083001004.
- Footnote 104
-
Glezen WP, Taber LH, Frank AL, et al. Risk of Primary Infection and Reinfection with Respiratory Syncytial Virus. Am J Dis Child. 1986 Jun;140(6):543-6. doi: 10.1001/archpedi.1986.02140200053026.
- Footnote 105
-
Hall CB. Respiratory Syncytial Virus and Parainfluenza Virus. N Engl J Med. 2001 Jun 21;344(25):1917-28. doi: 10.1056/NEJM200106213442507.
- Footnote 106
-
Pangesti KNA, Abd El Ghany M, Walsh MG, et al. Molecular Epidemiology of Respiratory Syncytial Virus. Rev Med Virol. 2018 Mar;28(2):1002/rmv.1968. doi: 10.1002/rmv.1968.
- Footnote 107
-
Groothuis JR, Gutierrez KM, Lauer BA. Respiratory Syncytial Virus Infection in Children with Bronchopulmonary Dysplasia. Pediatrics. 1988 Aug;82(2):199-203. [cited 2022 May 10]. Available from: https://pubmed.ncbi.nlm.nih.gov/3399292/.
- Footnote 108
-
Carbonell-Estrany X, Quero J, Bustos G, et al. Rehospitalization Because of Respiratory Syncytial Virus Infection in Premature Infants Younger than 33 Weeks of Gestation: A Prospective Study. Pediatr Infect Dis J. 2000 Jul;19(7):592-7. doi: 10.1097/00006454-200007000-00002.
- Footnote 109
-
Carbonell-Estrany X, Quero J, The IRIS Study Group. Hospitalization Rates for Respiratory Syncytial Virus Infection in Premature Infants Born During Two Consecutive Seasons. Pediatr Infect Dis J. 2001 Sep;20(9):874-9. doi: 10.1097/00006454-200109000-00010.
- Footnote 110
-
Pedersen O, Herskind AM, Kamper J, et al. Rehospitalization for Respiratory Syncytial Virus Infection in Infants with Extremely Low Gestational Age or Birthweight in Denmark. Acta Paediatr Jpn Overs Ed. 2003;92(2):240-2. doi: 10.1111/j.1651-2227.2003.tb00533.x.
- Footnote 111
-
Blanken MO, Rovers MM, Molenaar JM, et al. Respiratory Syncytial Virus and Recurrent Wheeze in Healthy Preterm Infants. N Engl J Med. 2013 May 9;368:1791-9. doi: 10.1056/NEJMoa1211917.
- Footnote 112
-
Yamaguchi M, Sano Y, Dapat IC, et al. High Frequency of Repeated Infections due to Emerging Genotypes of Human Respiratory Syncytial Viruses among Children During Eight Successive Epidemic Seasons in Japan. J Clin Microbiol. 2011 Mar;49(3):1034-40. doi: 10.1128/JCM.02132-10.
- Footnote 113
-
Okamoto M, Dapat CP, Sandagon AMD, et al. Molecular Characterization of Respiratory Syncytial Virus in Children with Repeated Infections with Subgroup B in the Philippines. J Infect Dis. 2018 Aug 24;218(7):1045-53. doi: 10.1093/infdis/jiy256.
- Footnote 114
-
Simões EA, King SJ, Lehr MV, et al. Preterm Twins and Triplets. A High-Risk Group for Severe Respiratory Syncytial Virus Infection. Am J Dis Child. 1993 Mar;147(3):303-6. doi: 10.1001/archpedi.1993.02160270065020.
- Footnote 115
-
Resch B, Pasnocht A, Gusenleitner W, et al. Rehospitalisations for Respiratory Disease and Respiratory Syncytial Virus Infection in Preterm Infants Of 29-36 Weeks Gestational Age. J Infect. 2005 Jun;50(5):397-403. doi:10.1016/j.jinf.2004.06.015.
- Footnote 116
-
Figueras-Aloy J, Carbonell-Estrany X, Quero J, et al. Case-Control Study of the Risk Factors Linked to Respiratory Syncytial Virus Infection Requiring Hospitalization in Premature Infants Born at a Gestational Age of 33-35 Weeks in Spain. Pediatr Infect Dis J. 2004 Sep;23(9):815-20. doi: 10.1097/01.inf.0000136869.21397.6b.
- Footnote 117
-
Dotan M, Ashkenazi-Hoffnung L, Samra Z, et al. Hospitalization for Respiratory Syncytial Virus Bronchiolitis and Disease Severity in Twins. Isr Med Assoc J. 2013;15:701-4. [cited 2022 May 10]. Available from: https://www.ima.org.il/MedicineIMAJ/viewarticle.aspx?year=2013&month=11&page=701.
- Footnote 118
-
Groothuis J, Bauman J, Malinoski F, et al. Strategies for Prevention of RSV Nosocomial Infection. J Perinatol. 2008 May;28(5):319-23. doi: 10.1038/jp.2008.37.
- Footnote 119
-
Katz BZ, Sullivan C. Respiratory Syncytial Virus Prophylaxis in a Tertiary Care Neonatal Intensive Care Unit. Pediatr Infect Dis J. 2009 Sep;28(9):842,844. doi: 10.1097/INF.0b013e3181a0ad01.
- Footnote 120
-
Ohler KH, Pham JT. Comparison of the Timing of Initial Prophylactic PVZ Dosing on Hospitalization of Neonates for Respiratory Syncytial Virus. Am J Health Syst Pharm. 2013 Aug 1;70(15):1342-6. doi: 10.2146/ajhp120526.
- Footnote 121
-
Zembles TN, Gaertner KM, Gutzeit MF, et al. Implementation of American Academy of Pediatrics Guidelines for PVZ Prophylaxis in a Pediatric Hospital. Am J Health-Syst Pharm. 2016 Mar 15;73(6):405-8. doi:10.2146/ajhp150499.
- Footnote 122
-
Harris RP, Helfand M, Woolf SH, et al. Current Methods of the Us Preventive Services Task Force: A Review Of The Process. Am J Prev Med. 2001 Apr;20:21-35. doi: 10.1016/s0749-3797(01)00261-6.
- Footnote 123
-
Public Health England. The Green Book Part 2: The Diseases, Vaccinations and Vaccines. Chapter 27a: Respiratory Syncytial Virus. 2015. [cited 2022 May 10]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/458469/Green_Book_Chapter_27a_v2_0W.PDF.
- Footnote 124
-
Abadesso C, Almeida HI, Virella D, et al. Use of PVZ to Control an Outbreak of Syncytial Respiratory Virus in a Neonatal Intensive Care Unit. J Hosp Infect. 2004 Sep;58(1):38-41. doi: 10.1016/j.jhin.2004.04.024.
- Footnote 125
-
Silva CdeA, Dias L, Baltieri SR, et al. Respiratory Syncytial Virus Outbreak in Neonatal Intensive Care Unit: Impact of Infection Control Measures plus PVZ Use. Antimicrob Resist Infect Control. 2012 May 2;1:16. doi:10.1186/2047-2994-1-16.
- Footnote 126
-
Hammoud MS, Al-Taiar A, Raina A, et al. Use of PVZ with Other Infection Control Measures to Control Respiratory Syncytial Virus Outbreaks in Neonatal Care Units. J Trop Pediatr. 2016 Oct;62(5):409-14. doi:10.1093/tropej/fmw025
- Footnote 127
-
Silva DG, Almeida FJ, Arnoni MV, et al. First Report of Two Consecutive Respiratory Syncytial Virus Outbreaks by the Novel Genotypes On-1 and Na-2 in a Neonatal Intensive Care Unit. J Pediatr. 2020 Mar-Apr;96(2):233-9. doi: 10.1016/j.jped.2018.10.014.
- Footnote 128
-
Dizdar EA, Aydemir C, Erdeve O, et al. Respiratory Syncytial Virus Outbreak Defined by Rapid Screening in a Neonatal Intensive Care Unit. J Hosp Infect. 2010 Aug;75(4):292,294. doi: 10.1016/j.jhin.2010.01.013.
- Footnote 129
-
AbbVie Corporation. SYNAGIS Product Monograph. 2018. [cited 2022 May 10]. Available from: https://www.abbvie.ca/content/dam/abbvie-dotcom/ca/en/documents/products/SYNAGIS_PM_EN.pdf.
- Footnote 130
-
Tavsu I, Gursoy T, Dirman S, et al. PVZ Prophylaxis: Does it have Any Influence on the Growth and Development of the Infants? Am J Perinatol. 2014 Sep;31(8):667-72. doi: 10.1055/s-0033-1356485.
- Footnote 131
-
Wegner S, Vann JJ, Liu G, et al. Direct Cost Analyses of PVZ Treatment in a Cohort of At-Risk Children: Evidence from the North Carolina Medicaid Program. Pediatrics. 2004 Dec;114(6):1612-9. doi: 10.1542/peds.2004-0959.
- Footnote 132
-
Mitchell I, Tough S, Gillis L, et al. Beyond Randomized Controlled Trials: A "Real Life" Experience of Respiratory Syncytial Virus Infection Prevention in Infancy with and without PVZ. Pediatr Pulmonol. 2006 Dec;41(12):1167-74. doi: 10.1002/ppul.20507.
- Footnote 133
-
Anderson EJ, Carosone-Link P, Yogev R, et al. Effectiveness of PVZ in High-Risk Infants and Children: A Propensity Score Weighted Regression Analysis. Pediatr Infect Dis J. 2017b Aug;36(8):699-704. doi: 10.1097/INF.0000000000001533.
- Footnote 134
-
Scheltema NM, Nibbelke EE, Pouw J, et al. Respiratory Syncytial Virus Prevention and Asthma in Healthy Preterm Infants: A Randomised Controlled Trial. Lancet Respir Med. 2018 Apr;6(4):257-64. doi: 10.1016/S2213-2600%2818%2930055-9.
- Footnote 135
-
Simões EAF, Carbonell-Estrany X, Rieger CHL, et al. The Effect of Respiratory Syncytial Virus on Subsequent Recurrent Wheezing in Atopic and Nonatopic Children. J Allergy Clin Immunol. 2010 Aug;126(2):256-62. doi: 10.1016/j.jaci.2010.05.026.
- Footnote 136
-
Simões EA, Groothuis JR, Carbonell-Estrany X, et al. PVZ Prophylaxis, Respiratory Syncytial Virus, and Subsequent Recurrent Wheezing. J Pediatr. 2007 Jul;151(1):34,42.e1. doi: 10.1016/j.jpeds.2007.02.032.
- Footnote 137
-
Mochizuki H, Kusuda S, Okada K, et al. PVZ Prophylaxis in Preterm Infants and Subsequent Recurrent Wheezing: Six-Year Follow-Up Study. Am J Respir Crit Care Med. 2017 Jul 1;196(1):29-38. doi: 10.1164/rccm.201609-1812OC.
- Footnote 138
-
Yoshihara S, Kusuda S, Mochizuki H, et al. Effect of PVZ Prophylaxis on Subsequent Recurrent Wheezing in Preterm Infants. Pediatrics. 2013 Nov;132(5):811-8. doi: 10.1542/peds.2013-0982.
- Footnote 139
-
Grimaldi M, Gouyon B, Michaut F, et al. Severe Respiratory Syncytial Virus Bronchiolitis: Epidemiologic Variations Associated with the Initiation of PVZ in Severely Premature Infants with Bronchopulmonary Dysplasia. Pediatr Infect Dis J. 2004 Dec;23:1081-5. doi: 10.1097/01.inf.0000145406.74341.c7.
- Footnote 140
-
Robinson KA, Odelola OA, Saldanha IJ. PVZ for Prophylaxis against Respiratory Syncytial Virus Infection in Children with Cystic Fibrosis. Cochrane Database Syst Rev. 2016 Jul;2016(7):CD007743. doi: 10.1002/14651858.CD007743.pub6.
- Footnote 141
-
Cohen AH, Boron ML, Dingivan C. A Phase IV Study of the Safety of Synagis®(PVZ) for Prophylaxis of Respiratory Syncytial Virus Disease in Children with Cystic Fibrosis [Poster presented at the American Thoracic Society International Conference, May 20-25, 2005 in San Diego, CA]. 2005
- Footnote 142
-
Winterstein AG, Eworuke E, Xu D, et al. PVZ Immunoprophylaxis Effectiveness in Children with Cystic Fibrosis. Pediatr Pulmonol. 2013 Sep;48(9):874-84. doi:10.1002/ppul.22711.
- Footnote 143
-
Giebels K, Marcotte JE, Podoba J. Prophylaxis against Respiratory Syncytial Virus in Young Children with Cystic Fibrosis. Pediatr Pulmonol. 2008 Feb;43(2):169-74. doi:10.1002/ppul.20751.
- Footnote 144
-
Buchs C, Dalphin ML, Sanchez S. PVZ Prophylaxis in Infants with Cystic Fibrosis does not Delay First Isolation of Pseudomonas Aeruginosa or Staphylococcus Aureus. Eur J Pediatr. 2017 May 16;176(7):891-7. doi: 10.1007/s00431-017-2926-8.
- Footnote 145
-
Fink AK, Graff G, Byington CL. PVZ and Long-term Outcomes in Cystic Fibrosis. Pediatrics. 2019 Jul;144(1):e20183495. doi: 10.1542/peds.2018-3495.
- Footnote 146
-
Chiu SN, Wang JN, Fu YC, et al. Efficacy of a Novel PVZ Prophylaxis Protocol for Respiratory Syncytial Virus Infection in Congenital Heart Disease: A Multicenter Study. J Pediatr. 2018;195:108,114.e1. doi: 10.1016/j.jpeds.2017.11.044.
- Footnote 147
-
Soraiz MG, Andrés SB, Castro SB, et al. PVZ in Infants Less than 1 Year with Hemodynamically Significant Congenital Heart Disease in Argentina a Comparative Study with Historical Control Group. Cardiology in the Young: 2017 Supplement 4. WCPCCS 2017:Abstract P2182 -S165-6.
- Footnote 148
-
Harris KC, Anis AH, Crosby MC, et al. Economic Evaluation of PVZ in Children With Congenital Heart Disease: A Canadian Perspective. Can J Cardiol. 2011;27:523.e11,523.e15. doi:10.1016/j.cjca.2010.12.064.
- Footnote 149
-
Sanchez-Luna M, Medrano C, Lirio J, et al. Down syndrome as Risk Factor for Respiratory Syncytial Virus Hospitalization: A Prospective Multicenter Epidemiological Study. Influenza Other Respi Viruses. 2017 Mar;11(2):157-64. doi: 10.1111/irv.12431.
- Footnote 150
-
Yi H, Lanctôt KL, Bont L, et al. Respiratory Syncytial Virus Prophylaxis in Down syndrome: A Prospective Cohort Study. Pediatrics. 2014 Jun;133(6):1031-7. doi: 10.1542/peds.2013-3916.
- Footnote 151
-
Kimura T, Takeuchi M, Kawakami K. Utilization and Efficacy of PVZ for Children with Down syndrome. Pediatr Int. 2020 Jan;62:677-82. doi: 10.1111/ped.14157.
- Footnote 152
-
Banerji A, Panzov V, Young M, et al. The Real-Life Effectiveness of PVZ for Reducing Hospital Admissions for Respiratory Syncytial Virus in Infants Residing in Nunavut. Can Respir J. 2014 May-Jun;21:185-9. doi: 10.1155/2014/941367.
- Footnote 153
-
Grindeland CJ, Mauriello CT, Leedahl DD, et al. Association between Updated Guideline-Based PVZ Administration and Hospitalizations for Respiratory Syncytial Virus Infections. Pediatr Infect Dis J. 2016 Jul;35(7):728-32. doi: 10.1097/INF.0000000000001150.
- Footnote 154
-
Zembles TN, Bushee GM, Willoughby RE, et al. Impact of American Academy of Pediatrics PVZ Guidance for Children >=29 and <35 Weeks of Gestational Age. J Pediatr. 2019 Jun;209:125-9. doi: 10.1016/j.jpeds.2019.02.020.
- Footnote 155
-
Goldstein M, Krilov LR, Fergie J, et al. Respiratory Syncytial Virus Hospitalizations among US. Preterm Infants Compared with Term Infants before and after the 2014 American Academy of Pediatrics Guidance on Immunoprophylaxis: 2012-2016. Am J Perinatol. 2018 Dec;35(14):1433-42. doi: 10.1055/s-0038-1660466.
- Footnote 156
-
Kong AM, Krilov LR, Fergie J, et al. The 2014-2015 National Impact of the 2014 American Academy of Pediatrics Guidance for Respiratory Syncytial Virus Immunoprophylaxis on Preterm Infants Born in the United States. Am J Perinatol. 2018 Jan;35(2):192-200. doi: 10.1055/s-0037-1606352.
- Footnote 157
-
Walpert AS, Thomas ID, Lowe MC, et al. RSV Prophylaxis Guideline Changes and Outcomes in Children with Congenital Heart Disease. Congenital Heart Disease. 2018 May;13(3):428-31. doi: 10.1111/chd.12590.
- Footnote 158
-
Belleudi V, Trotta F, Pinnarelli L, et al. Neonatal Outcomes Following New Reimbursement Limitations on PVZ in Italy. Arch Dis Child. 2018 Dec;103(12):1163-7. doi: 10.1136/archdischild-2018-315349.
- Footnote 159
-
Capizzi A, Silvestri M, Orsi A, et al. The Impact of the Recent Aap Changes in PVZ Authorization on Rsv-Induced Bronchiolitis Severity and Incidence. Italian J Pediatr. 2017 Aug 14;43:71. https://doi.org/10.1186/s13052-017-0390-8
- Footnote 160
-
Priante E, Tavella E, Girardi E, et al. Restricted PVZ Recommendations and the Impact on RSV Hospitalizations among Infants Born at > 29 Weeks of Gestational Age: An Italian Multicenter Study. Am J Perinatol. 2019 Jul;36(S 02):S77-82. doi: 10.1055/s-0039-1691771.
- Footnote 161
-
Johnson S, Oliver C, Prince GA, et al. Development of a Humanized Monoclonal Antibody (Medi-493) with Potent In Vitro and In Vivo Activity against Respiratory Syncytial Virus. J Infect Dis. 1997 Nov;176(5):1215-24. doi: 10.1086/514115.
- Footnote 162
-
Subramanian KN, Weisman LE, Rhodes T, et al. Safety, Tolerance and Pharmacokinetics of a Humanized Monoclonal Antibody to Respiratory Syncytial Virus in Premature Infants and Infants with Bronchopulmonary Dysplasia. MEDI-493 Study Group. Pediatr Infect Dis J. 1998 Feb;17(2):110-5. doi: 10.1097/00006454-199802000-00006.
- Footnote 163
-
Robbie GJ, Zhao L, Mondick J, et al. Population Pharmacokinetics of PVZ, a Humanized Anti-Respiratory Syncytial Virus Monoclonal Antibody, in Adults and Children [Published Correction Appears in Antimicrob Agents Chemother. 2012 Oct;56(10):5431]. Antimicrob Agents Chemother. 2012 Sep;56(9):4927-36. doi: 10.1128/AAC.06446-11.
- Footnote 164
-
Fenton C, Scott LI, Plosker GL. PVZ: A Review of Its Use as Prophylaxis for Serious Respiratnnory Syncytial Virus Infection. Pediatr Drugs. 2004;6(3):177-97. doi: 10.2165/00148581-200406030-00004.
- Footnote 165
-
La Via WV, Notario GF, Yu X-Qiang, et al. Three Monthly Doses of PVZ are Not Adequate for 5-Month Protection: A Population Pharmacokinetic Analysis. Pulm Pharmacol Ther. 2013 Dec;26:666e-671. doi: 10.1016/j.pupt.2013.03.007.
- Footnote 166
-
Gutfraind A, Galvani AP, Meyers LA, et al. Efficacy and Optimization of PVZ Injection Regimens against Respiratory Syncytial Virus Infection. JAMA Pediatr. 2015 Apr;169(4):341-8. doi: 10.1001/jamapediatrics.2014.3804.
- Footnote 167
-
Lavoie PM, Solimano A, Taylor R, et al. Outcomes of Respiratory Syncytial Virus Immunoprophylaxis in Infants Using an Abbreviated Dosing Regimen of PVZ. JAMA Pediatr. 2016 Feb;170(2):174-6. doi: 10.1001/jamapediatrics.2015.3235.
- Footnote 168
-
Claydon J, Popescu CR, Shaiba L, et al. Outcomes Related to Respiratory Syncytial Virus with an Abbreviated PVZ Regimen in Children with Congenital Heart Disease: A Descriptive Analysis. CMAJ OPEN. 2019 Feb 18;7(1):E88-93. doi: 10.9778/cmajo.20180167.
- Footnote 169
-
Claydon J, Sur A, Callejas A, et al. Respiratory Syncytial Virus-Neutralizing Serum Antibody Titers in Infants Following PVZ Prophylaxis with an Abbreviated Dosing Regimen. PLoS ONE. 2017 Apr 24;12(4):e0176152. doi: 10.1371/journal.pone.0176152.
- Footnote 170
-
Chen JJ, Chan P, Paes B, et al. Serious Adverse Events in the Canadian Registry of Children Receiving PVZ (CARESS) for Respiratory Syncytial Virus Prevention. PLoS ONE. 2015 Aug 3;10(8):e0134711. doi: 10.1371/journal.pone.0134711.
- Footnote 171
-
Parnes C, Guillermin J, Habersang R, et al. PVZ Prophylaxis of Respiratory Syncytial Virus Disease in 2000-2001: Results from the PVZ Outcomes Registry. Pediatr Pulmonol. 2003 Jun;35(6):484-9. doi: 10.1002/ppul.10288.
- Footnote 172
-
Forbes ML, Kumar VR, Yogev R, et al. Serum PVZ Level is Associated with Decreased Severity of Respiratory Syncytial Virus Disease in High-Risk Infants. Human Vaccines & Immunotherapeutics. 2014;10(10):2789-94. doi: 10.4161/hv.29635.
- Footnote 173
-
Paes BA, Craig C, Pigott W, et al. Seasonal Respiratory Syncytial Virus Prophylaxis Based on Predetermined Dates Versus Regional Surveillance Data. Pediatr Infect Dis J. 2013 Sep;32(9):e360-4. doi: 10.1097/INF0b013e31829479d3.
- Footnote 174
-
Weinberger DM, Warren JL, Steiner CA, et al. Reduced-Dose Schedule of Prophylaxis Based on Local Data Provides Near-Optimal Protection Against Respiratory Syncytial Virus. Clin Infect Dis. 2015 Aug 15;61(4):506-14. doi: 10.1093/cid/civ331.
- Footnote 175
-
Key Immunization Information Storage and Handling of Immunizing Agents: Handling of vaccines: Canadian Immunization Guide, Part 1 [Internet]. Ottawa (ON): Public Health Agency of Canada; 2021 Jun 11 [cited 2022 May 10]. Available at: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-1-key-immunization-information/page-9-storage-handling-immunizing-agents.html#p1c8a2.
- Footnote 176
-
Mac S, Sumner A, Duchesne-Belanger S, et al. Cost-Effectiveness of PVZ for Respiratory Syncytial Virus: A Systematic Review. Pediatrics. 2019 May;143(5):e20184064. doi: 10.1542/peds.2018-4064.
- Footnote 177
-
Blanken MO, Frederix GW, Nibbelke EE, et al. Cost-Effectiveness of Rule-Based Immunoprophylaxis Against Respiratory Syncytial Virus Infections in Preterm Infants. Eur J Pediatr. 2018 Jan;177(1):133-44. doi: 10.1007/s00431-017-3046-1.
- Footnote 178
-
Lofland JH, O'Connor JP, Chatterton ML, et al. PVZ for Respiratory Syncytial Virus Prophylaxis in High-Risk Infants: A Cost-Effectiveness Analysis. Clin Ther. 2000 Nov;22(11):1357-69. doi: 10.1016/s0149-2918(00)83032-5.
- Footnote 179
-
Wang D, Cummins C, Bayliss S, et al. Immunoprophylaxis Against Respiratory Syncytial Virus (RSV) with PVZ in Children: A Systematic Review and Economic Evaluation. Health Technol Assess. 2008 Dec;12(36):iii, ix-x, 1-86. doi: 10.3310/hta12360.
- Footnote 180
-
Neovius K, Buesch K, Sandstrom K, et al. Cost-Effectiveness Analysis of PVZ as Respiratory Syncytial Virus Prophylaxis in Preterm Infants in Sweden. Acta Paediatr Int J Paediatr. 2011 Oct;100(10):1306-14. doi: 10.1111/j.1651-2227.2011.02309.x.
- Footnote 181
-
Nuijten MJC, Wittenberg W, Lebmeier M. Cost Effectiveness of PVZ for Respiratory Syncytial Virus Prophylaxis in High-Risk Children: A UK Analysis. Pharmacoeconomics. 2007;25(1):55-71. doi: 10.2165/00019053-200725010-00006.
- Footnote 182
-
Nuijten M, Lebmeier M, Wittenberg W. Cost Effectiveness of PVZ for RSV Prevention in High-Risk Children in the Netherlands. J Med Econ. 2009a;12(4):291-300. doi: 10.3111/13696990903316961.
- Footnote 183
-
Nuijten MJ, Wittenberg W. Cost Effectiveness of PVZ in Spain: An Analysis Using Observational Data. Eur J Heal Econ. 2010 Feb;11(1):105-15. doi: 10.1007/s10198-009-0206-x.
- Footnote 184
-
Salinas-Escudero G, Martínez-Valverde S, Reyes-López A, et al. Cost-Effectiveness Analysis of the Use of PVZ in the Prophylaxis of Preterm Patients in Mexico. Salud Publica Mex. 2012 Jan-Feb;54(1):47-59. [cited 2022 May 10]. Available from: https://pubmed.ncbi.nlm.nih.gov/22286828/.
- Footnote 185
-
Sanchez-Luna M, Burgos-Pol R, Oyagüez I, et al. Cost-Utility Analysis of PVZ for Respiratory Syncytial Virus Infection Prophylaxis in Preterm Infants: Update Based on the Clinical Evidence in Spain. BMC Infect Dis. 2017 Oct 17;17(1):1-11. doi: 10.1186/s12879-017-2803-0.
- Footnote 186
-
Smart KA, Paes BA, Lanctt KL. Changing Costs and the Impact on RSV Prophylaxis. J Med Econ. 2010;13(4):705-8. doi: 10.3111/13696998.2010.535577.
- Footnote 187
-
Chirico G, Ravasio R, Sbarigia U. Cost-Utility Analysis of PVZ in Italy: Results from a Simulation Model in the Prophylaxis of Respiratory Syncytial Virus Infection (RSV) Among High-Risk Preterm Infants. Ital J Pediatr. 2009 Feb 25;35:1-12. doi: 10.1186/1824-7288-35-4.
- Footnote 188
-
Elhassan NO, Sorbero MES, Hall CB, et al. Cost-Effectiveness Analysis of PVZ in Premature Infants without Chronic Lung Disease. Arch Pediatr Adolesc Med. 2006 Oct;160(10):1070-6. doi: 10.1001/archpedi.160.10.1070.
- Footnote 189
-
McGirr AA, Schwartz KL, Allen U, et al. The Cost-Effectiveness of PVZ in Infants with Cystic Fibrosis in the Canadian Setting: A Decision Analysis Model. Hum Vaccines Immunother. 2017 Mar 4;13(3):599-606. doi: 10.1080/21645515.2016.1235670.
- Footnote 190
-
Nuijten M, Lebmeier M, Wittenberg W. Cost Effectiveness of PVZ in Children with Congenital Heart Disease in Germany. J Med Econ. 2009b;12(4):301-8. doi: 10.3111/13696990903347172.
- Footnote 191
-
Bentley A, Filipovic I, Gooch K, et al. A Cost-Effectiveness Analysis of Respiratory Syncytial Virus (RSV) Prophylaxis in Infants in the United Kingdom. Health Econ Rev 2013;3:1-12 doi: 10.1136/thoraxjnl-2011-201054c.170.
- Footnote 192
-
Yount LE, Mahle WT. Economic Analysis of PVZ in Infants with Congenital Heart Disease. Pediatrics. 2004 Dec;114(6):1606-11. doi: 10.1542/peds.2004-0224.
- Footnote 193
-
Weiner LB, Masaquel AS, Polak MJ, et al. Cost-Effectiveness Analysis of PVZ among Pre-Term Infant Populations Covered By Medicaid in the United States. J Med Econ. 2012;15(5):997-1018. doi: 10.3111/13696998.2012.672942.
- Footnote 194
-
Mahadevia PJ, Masaquel AS, Polak MJ, et al. Cost Utility of PVZ Prophylaxis among Pre-Term Infants in the United States: A National Policy Perspective. J Med Econ. 2012 May 10;15(5):987-96. doi: 10.3111/13696998.2012.690013.
- Footnote 195
-
Schmidt R, Majer I, García Román N, et al. PVZ in the Prevention of Severe Respiratory Syncytial Virus Infection in Children with Congenital Heart Disease; A Novel Cost-Utility Modeling Study Reflecting Evidence-Based Clinical Pathways in Spain. Health Econ Rev. 2017 Dec 19;7:47. doi: 10.1186/s13561-017-0181-3.
- Footnote 196
-
Tam DY, Banerji A, Paes BA, et al. The Cost Effectiveness of PVZ in Term Inuit Infants in the Eastern Canadian Arctic. J Med Econ. 2009;12(4):361-70. doi: 10.3111/13696990903442155.
- Footnote 197
-
Banerji A, Ng K, Moraes TJ, et al. Cost-Effectiveness of PVZ Compared to No Prophylaxis in Term Infants Residing in the Canadian Arctic. CMAJ Open. 2016 Oct-Dec;4(4):E623-33. doi: 10.9778/cmajo.20150052.
- Footnote 198
-
Rietveld E, Steyerberg EW, Polder JJ, et al. Passive Immunisation against Respiratory Syncytial Virus: A Cost-Effectiveness Analysis. Arch Dis Child. 2010 Jul;95(7):493-8. doi: 10.1136/adc.2008.155556
- Footnote 199
-
Roeckl-Wiedmann I, Liese JG, Grill E, et al. Economic Evaluation of Possible Prevention of RSV-Related Hospitalizations in Premature Infants in Germany. Eur J Pediatr. 2003 Apr;162(4):237-44. doi: 10.1007/s00431-002-1106-6.
- Footnote 200
-
Vogel AM, McKinlay MJ, Ashton T, et al. Cost-Effectiveness of PVZ in New Zealand. J Paediatr Child Health. 2002 Aug;38(4):352-7. doi: 10.1046/j.1440-1754.2002.00790.x.
- Footnote 201
-
Hampp C, Kauf TL, Saidi AS, et al. Cost-Effectiveness of Respiratory Syncytial Virus Prophylaxis in Various Indications. Arch Pediatr Adolesc Med. 2011 Jun;165(6):498-505. doi: 10.1001/archpediatrics.2010.298.
- Footnote 202
-
Hascoet JM, Fagnani F, Charlemagne A, et al. Methodological Aspects of Economic Evaluation in Pediatrics: Illustration by RSV Infection Prophylaxis in the French Setting. Arch Pediatr. 2008 Dec;15(12):1739-48. doi: 10.1016/j.arcped.2008.09.024.
- Footnote 203
-
Seeler RA, Schatz B. PVZ (Synagis)--Cohorting Babies to Reduce Waste. Pediatrics. 1999 Nov;104(5 Pt 1):1170-1. doi: 10.1542/peds.104.5.1170.
- Footnote 204
-
CADTH Methods and Guidelines. Guidelines for the Economic Evaluation of Health Technologies: Canada 4th Edition [Internet]. Ottawa (ON): CADTH; 2017 May;1-76 [cited 2022 May 10]. Available from: https://www.cadth.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf.
- Footnote 205
-
Mossialos E, Wenzl M, London School of Economics and Political Science, et al. 2015 International Profiles of Health Care Systems: JANUARY 2016 [Internet]. New York (NY): The Commonwealth Fund; 2016 Jan;1-180 [cited 2022 May 10]. Available from: https://www.commonwealthfund.org/publications/fund-reports/2016/jan/international-profiles-health-care-systems-2015.
- Footnote 206
-
Gilca R. Institut National de Santé Publique de Québec. Personal Communication.
- Footnote 207
-
Lorcy A, Gilca R, Dubé E, et al. Feasibility and Ethical Issues: Experiences and Concerns of Healthcare Workers Regarding a New RSV Prophylaxis Programme in Nunavik, Quebec. Int J Circumpolar Health. 2020 Dec;79(1):1742564. doi: 10.1080/22423982.2020.1742564.
- Footnote 208
-
Hui C, Paes B, Papenburg J, et al. PVZ Adherence and Outcomes in Canadian Aboriginal Children. Pediatr Infect Dis J. 2016 Nov;35(11):1187-93. doi: 10.1097/INF.0000000000001282.
- Footnote 209
-
Wong S.K., Li A., Lanctot K.L., et al. Adherence and Outcomes: A Systematic Review of PVZ Utilization. Expert Rev Respir Med. 2018 Jan;12(1):27-42. doi: 10.1080/17476348.2018.1401926.
- Footnote 210
-
Canada Vigilance Program [Internet]. Ottawa (ON): Health Canada; 2018 Jul 12[cited 2019 Apr 5]. Available from: https://www.canada.ca/en/health-canada/services/drugs-health-products/medeffect-canada/canada-vigilance-program.html.
- Footnote 211
-
Wegzyn C, Toh LK, Notario G, et al. Safety and Effectiveness of PVZ in Children at High Risk of Serious Disease Due to Respiratory Syncytial Virus Infection: A Systematic Review. Infect Dis Ther. 2014 Dec;3(2):133-58. doi: 10.1007/s40121-014-0046-6.
- Footnote 212
-
Makari D, Jensen KM, Harris B, et al. Randomized, Double-Blind Study of the Safety of the Liquid Versus Lyophilized Formulation of PVZ in Premature Infants and Children with Chronic Lung Disease of Prematurity. Infect Dis Ther. 2014 Dec;3(2):339-47. doi: 10.1007/s40121-014-0033-y.
- Footnote 213
-
Robbie GJ, Makari D, Harris B. Randomized, Double-Blind Study of the Pharmacokinetics and Safety of PVZ Liquid Formulation Compared with Lyophilized Formulation. Infect Dis Ther. 2014 Dec;3(2):203-14. doi: 10.1007/s40121-014-0042-x.
- Footnote 214
-
Carbonell-Estrany X, Simões EAF, Dagan R, et al. Motavizumab for Prophylaxis of Respiratory Syncytial Virus in High-Risk Children: A Noninferiority Trial. Pediatrics. 2010 Jan;125(1):e35-51. doi: 10.1542/peds.2008-1036.
- Footnote 215
-
Fernandez P, Trenholme A, Abarca K, et al. A phase 2, Randomized, Double-Blind Safety and Pharmacokinetic Assessment of Respiratory Syncytial Virus (RSV) Prophylaxis with Motavizumab and PVZ Administered in the Same Season. BMC Pediatr. 2010 Jun 3;10:38. doi: 10.1186/1471-2431-10-38.
- Footnote 216
-
Feltes TF, Sondheimer HM, Tulloh RM, et al. Randomized Controlled Trial of Motavizumab Versus PVZ for the Prophylaxis of Serious Respiratory Syncytial Virus Disease in Children with Hemodynamically Significant Congenital Heart Disease. Pediatr Res. 2011 Aug;70(2):186-91. doi: 10.1203/PDR.0b013e318220a553.
- Footnote 217
-
Haerskjold A, Linder M, Henriksen L, et al. PVZ Exposure and the Risk of Autoimmune Disease: A Cross-National Cohort Study. Paediatr Drugs. 2016 Dec;18(6):435-41. doi: 10.1007/s40272-016-0191-3.
- Footnote 218
-
Haerskjold A, Stokholm L, Linder M, et al. PVZ Exposure and the Risk of Atopic Dermatitis, Asthma and Allergic Rhinoconjunctivitis: A Cross-National, Population-Based Cohort Study. Paediatr Drugs. 2017 Apr;19(2):155-64. doi: 10.1007/s40272-017-0215-7.
- Footnote 219
-
Mitchell I, Paes BA, Li A, et al. CARESS: The Canadian Registry of PVZ. Pediatr Infect Dis J. 2011 Feb;30:651-5. doi: 10.1097/INF.0b013e31821146f7.
- Footnote 220
-
Paes B, Mitchell I, Li A, et al. Respiratory Hospitalizations and Respiratory Syncytial Virus Prophylaxis in Special Populations. Eur J Pediatr. 2012 May;171(5):833-41. doi: 10.1007/s00431-011-1654-8.
- Footnote 221
-
Manzoni P, Paes B, Lanctôt KL, et al. Outcomes of Infants Receiving PVZ Prophylaxis for Respiratory Syncytial Virus in Canada and Italy: An International, Prospective Cohort Study. Pediatr Infect Dis J. 2017 Jan;36(1):2-8. doi: 10.1097/INF.0000000000001340.
- Footnote 222
-
Simon A, Nowak H, Sterz R. Use of PVZ in Germany: Data from 2002-2007. Klin Padiatr. 2011 Sep;223(5):292-8. doi: 10.1055/s-0030-1270515.
- Footnote 223
-
Simon A, Gehrmann S, Wagenpfeil G, et al. Use of PVZ in Germany - Report from the German SynagisTM Registry 2009 - 2016. Klin Padiatr. 2018 Sep;230(5):263-9. doi: 10.1055/a-0595-7771.
- Footnote 224
-
Groothuis JR. Safety and Tolerance of PVZ Administration in a Large Northern Hemisphere Trial. Northern Hemisphere Expanded Access Study Group. Pediatr Infect Dis J. 2001 Jun;20(6):628-30. doi: 10.1097/00006454-200106000-00018.
- Footnote 225
-
Groothuis JR. Safety of PVZ in Preterm Infants 29 to 32 Weeks' Gestational Age Without Chronic Lung Disease to Prevent Serious Respiratory Syncytial Virus Infection. Eur J Clin Microbiol Infect Dis. 2003 Jul;22(7):414-7. doi: 10.1007/s10096-003-0961-z.
- Footnote 226
-
Castillo LM, Bugarin G, Arias JC. One-Year Observational Study of PVZ Prophylaxis on Infants at Risk for Respiratory Syncytial Virus Infection in Latin America. Eur J Clin Microbiol Infect Dis. 2017 Sep-Oct;93(5):467-74. doi: 10.1016/j.jped.2016.11.006.
- Footnote 227
-
Lacaze-Masmonteil T, Roze JC, Fauroux B. Incidence of Respiratory Syncytial Virus-Related Hospitalizations in High-Risk Children: Follow-Up of a National Cohort of Infants Treated with PVZ as RSV Prophylaxis. Pediatr Pulmonol. 2002 Sep;34(3):181-8. doi: 10.1002/ppul.10175.
- Footnote 228
-
Pinquier D, Gouyon JB, Fauroux B, et al. Modalités d'Utilisation, Tolérance et Benefice du PVZ dans la Prévention des Infections à VRS en France : Saison 2005–2006 [PVZ Immunoprophylaxis: Use in Clinical Practice, Safety and Beneficial Effects in France]. Arch Pediatr. 2009 Nov;16(11):1443-52. doi: 10.1016/j.arcped.2009.08.008.
- Footnote 229
-
Kashiwagi T, Okada Y, Nomoto K. PVZ Prophylaxis against Respiratory Syncytial Virus Infection in Children with Immunocompromised Conditions or Down syndrome: A Multicenter, Post-Marketing Surveillance in Japan. Pediatr Drugs. 2018 Feb;20(1):97-104. doi: 10.1007/s40272-017-0264-y.
- Footnote 230
-
Al-Alaiyan S, Pollack P, Notario GF. Safety and Pharmacokinetics of Extended Use of PVZ in Saudi Arabian Infants and Children. Drugs in Context. 2015 Feb 27;4:212270. doi: 10.7573/dic.212270.
- Footnote 231
-
Lacaze-Masmonteil T, Seidenberg J, Mitchell I, et al. Evaluation of the Safety of PVZ in the Second Season of Exposure in Young Children at Risk for Severe Respiratory Syncytial Virus Infection. Drug Saf. 2003;26(4):283-91. doi: 10.2165/00002018-200326040-00005.
- Footnote 232
-
Null D Jr, Pollara B, Dennehy PH, et al. Safety and Immunogenicity of PVZ (Synagis) Administered for Two Seasons. Pediatr Infect Dis J. 2005 Nov;24(11):1021-3. doi: 10.1097/01.inf.0000183938.33484.bd.
- Footnote 233
-
Turti TV, Baibarina EN, Degtiareva EA, et al. A Prospective, Open-Label, Non-Comparative Study of PVZ Prophylaxis in Children at High Risk of Serious Respiratory Syncytial Virus Disease in the Russian Federation. BMC Res Notes. 2012 Sep 4;5:484. doi: 10.1186/1756-0500-5-484.
- Footnote 234
-
Mori M, Onodera M, Morimoto A, et al. PVZ use in Japanese Infants and Children with Immunocompromised Conditions. Pediatr Infect Dis J. 2014 Nov;33(11):1183-5. doi: 10.1097/INF.0000000000000392.
- Footnote 235
-
Sáez-Llorens X, Castaño E, Null D, et al. Safety and Pharmacokinetics of an Intramuscular Humanized Monoclonal Antibody to Respiratory Syncytial Virus in Premature Infants and Infants with Bronchopulmonary Dysplasia. The MEDI-493 Study Group. Pediatr Infect Dis J. 1998 Sep;17(9):787-91. doi: 10.1097/00006454-199809000-00007.
- Footnote 236
-
Borecka R, Lauterbach R, Helwich E. Factors Related to Compliance with PVZ Prophylaxis for Respiratory Syncytial Virus (RSV) Infection - Data from Poland. Med Wieku Rozwoj. 2016;20(3):181-90. [cited 2022 May 10]. Available from: https://pubmed.ncbi.nlm.nih. gov/27941187/.
- Footnote 237
-
Abushahin A, Janahi I, Tuffaha A. Effectiveness of PVZ Immunoprophylaxis in Preterm Infants against Respiratory Syncytial Virus Disease in Qatar. Int J Gen Med. 2018 Jan 31;11:41-6. doi: 10.2147/IJGM.S156078.
- Footnote 238
-
Chang SG, Park MS, Yu JE. Outcomes of PVZ Prophylaxis for Respiratory Syncytial Virus Infection in Preterm Children with Bronchopulmonary Dysplasia at a Single Hospital in Korea from 2005 to 2009. J Korean Med Sci. 2010 Feb;25(2):251-6. doi: 10.3346/jkms.2010.25.2.251.
- Footnote 239
-
Savitz J, Geaney C, Banks TA. A Case of Anaphylaxis to PVZ. Ann Allergy Asthma Immunol. 2014 Aug;113(2):236-7. doi: 10.1016/j.anai.2014.06.006.
- Footnote 240
-
Resch B. Product Review on the Monoclonal Antibody PVZ for Prevention of Respiratory Syncytial Virus Infection. Hum Vaccin Immunother. 2017 Sep 2;13(9):2138-49. doi: 10.1080/21645515.2017.1337614.
- Footnote 241
-
Tenenbaum T, Drechsel-Bäuerle U, Oberle D. Cardiorespiratory Events After Monoclonal Antibody Prophylaxis With PVZ. Pediatr Infect Dis J. 2018 Nov;37(11):e281-2. doi: 10.1097/INF.0000000000002017.
- Footnote 242
-
Pérez-De-Lis M, Retamozo S, Flores-Chávez A, et al. Autoimmune diseases induced by biological agents. A review of 12,731 cases (BIOGEAS Registry). Expert Opin Drug Saf. 2017 Nov;16(11):1255-71. doi: 10.1080/14740338.2017.1372421.
- Footnote 243
-
Saji T, Nakazawa M, Harada K. Safety and Efficacy of PVZ Prophylaxis in Children with Congenital Heart Disease. Pediatr Internat. 2005 Aug;47(4):397-403. doi: 10.1111/j.1442-200x.2005.02089.x.
- Footnote 244
-
Simon A, Gehrmann S, Wagenpfeil G, et al. PVZ Use in Infants with Down syndrome - Report from the German SynagisTM Registry 2009-2016. Eur J Pediatr. 2018 Jun;177(6):903-11. doi: 10.1007/s00431-018-3142-x.