Challenges to developing a vaccine for respiratory syncytial virus

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 46–4: Respiratory syncytial virus (RSV)
Date published: April 2, 2020
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 46–4, April 2, 2020: Respiratory syncytial virus (RSV)
Research
Overview of the respiratory syncytial virus vaccine candidate pipeline in Canada
April Killikelly1, Matthew Tunis1, Althea House1, Caroline Quach2, Wendy Vaudry3, Dorothy Moore4
Affiliations
1 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
2 Centre Hospitalier Universitaire Sainte-Justine, Université de Montréal, Montreal, QC
3 Stollery Children’s Hospital, University of Alberta, Edmonton, AB
4 McGill University, Montreal, QC
Correspondence
Suggested citation
Killikelly A, Tunis M, House A, Quach C, Vaudry W, Moore D. Overview of the respiratory syncytial virus vaccine candidate pipeline in Canada. Can Commun Dis Rep 2020;46(4):56–61. https://doi.org/10.14745/ccdr.v46i04a01
Keywords: vaccine, National Advisory Committee on Immunization, NACI, immunization, RSV, respiratory syncytial virus
Abstract
A vaccine for respiratory syncytial virus (RSV) has been actively sought for over 60 years due to the health impacts of RSV disease in infants, but currently the only available preventive measure in Canada and elsewhere is limited to passive immunization for high-risk infants and children with a monoclonal antibody.
RSV vaccine development has faced many challenges, including vaccine-induced enhancement of RSV disease in infants. Several key developments in the last decade in the fields of cellular immunology and protein structure have led to new products entering late-stage clinical development. As of July 2019, RSV vaccine development is being pursued by 16 organizations in 121 clinical trials. Five technologies dominate the field of RSV vaccine development, four active immunizing agents (live-attenuated, particle-based, subunit-based and vector-based vaccines) and one new passive immunizing agent (monoclonal antibody). Phase 3 clinical trials of vaccine candidates for pregnant women, infants, children and older adults are under way. The next decade will see a dramatic transformation of the RSV prevention landscape.
Introduction
Respiratory syncytial virus (RSV) infection represents a large burden of disease in Canada and worldwide. The age distribution of RSV disease burden is bimodal, with the greatest impact felt in the first two years of life and in older adults. Annually, RSV disease is estimated to cause 3.4 million hospitalizations and 100,000 deaths globallyFootnote 1. In Canada, the burden of RSV disease and hospitalizations are captured by various surveillance systems. Although preventive and supportive medical interventions exist to prevent or treat RSV, vaccination holds hope as a method to reduce the health and economic burden of RSV.
RSV is an orthopneumovirus in the Pneumoviridae family. It is a negative-sense, single-stranded RNA virus that has 11 proteinsFootnote 2. The F protein on the surface of the viral membrane mediates fusion between the virus and the host cell. Two conformations of F have been defined, prefusion and postfusion. Some neutralizing epitopes are present on both conformations, notably site II targeted by palivizumab. Other neutralizing epitopes are present only on prefusion F, including the sites V (targeted by suptavumab) and ø (targeted by nirsevimab). Without specific stabilization or modification, the F protein will exist in a spectrum of conformations, which will have different antigenic and neutralization profiles. Without stabilization, this immunogen will settle into a postfusion conformation over time.
Two subtypes of RSV have been defined, RSV/A and RSV/B. Subtype A is more prevalent than subtype BFootnote 3. RSV infects cells in the human airway, including polarized, differentiated, ciliated epithelial cells, and causes infection of the upper and lower airways. Severe disease clinically manifests as influenza-like illnesses and lower respiratory tract infection (LRTI), with bronchiolitis the most common severe presentation in young children. Primary RSV infections can result in symptomatic LRTI, a minority of which require hospitalization. Canadian surveillance to capture the RSV burden in different populations is under way.
The only countermeasure currently available for RSV is palivizumab, a monoclonal antibody administered prophylactically to infants and children under two years of age at higher risk for severe infection.
A vaccine against RSV has been sought after for over 60 years for its potential impacts on the health outcomes for various age groups. A shadow was cast over vaccine development in the 1960s when a formalin-inactivated RSV (FI-RSV) vaccine was tested in seronegative children, that is, they were naive to RSV antigens. Instead of inducing protection, immunization resulted in enhanced respiratory disease (ERD) upon subsequent RSV infection, leading to two deathsFootnote 4Footnote 5Footnote 6Footnote 7.
Recently, RSV vaccine development has leveraged advances in understanding of T-cell biology and protein structure as well as a better delineation of different populations at risk for RSV. As of July 2019, 16 organizations were undertaking RSV vaccine development in 121 clinical trials. Vaccine candidates are in development for children, older adults and pregnant women. Phase 3 clinical trials that target pediatric, older adult and maternal populations are under way.
Five technologies dominate the field of RSV vaccine development: four active immunizing agents (live-attenuated, particle-based, subunit-based and vector-based vaccines) and one new passive immunizing agent (i.e. monoclonal antibody). Other trials are in late preclinical and early clinical stages.
The objective of this overview is to summarize the vaccine candidates in the five different vaccine technologies for three target populations and to identify current challenges to developing a vaccine for RSV.
Key Findings
Immunization technologies and strategies
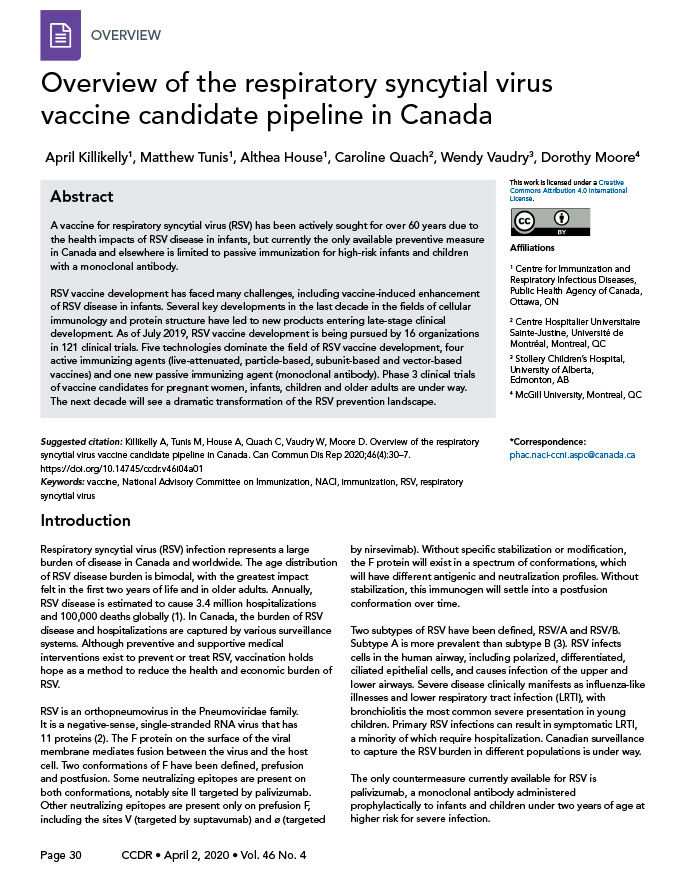
Clinical trials are under way for maternal, pediatric and older adult populations. Based on data collected through July 1, 2019, Figure 1 represents the RSV vaccine products in development for each target population at risk for RSV. Phase 3 clinical trials that target maternal, senior adult and pediatric populations are under way. Below we summarize the developments for each vaccine candidate type, with an emphasis on products in later stages of clinical development (Stage 2 or 3 clinical trials).
Figure 1: Summary of RSV vaccine target populations
Text description: Figure 1
Figure 1: Summary of RSV vaccine target populations
Figure 1 is a flow chart of the various respiratory syncytial virus vaccines and the targeted populations, in their various phases of clinical development. The figure starts with an arrow to identify the targeted populations. The five targeted populations are: pregnant women, infants, children, adults (18–54) and adults over 55 years of age.
Under the pregnant women targeting population are three vaccines in various phases: Phase 1: GlaxoSmithKline, GSK RSV F (GSK3888550A) NCT03674177; Phase 2: GSK RSV F (GSK3003895A) NCT02360475; and Phase 3: Novavax, RSV F Nanoparticle NCT02624947.
Under infants and children targeted population, it has a monthly age marker identifying 1 to 73 months. Immediately below the monthly marker are 12 vaccines in identified in Phase 1. The first phase spans between 4 to 60 months: 1) NIH/NIAID, RSV ∆NS2/∆1313/I1314L NCT01893554, NCT03422237, NCT03227029, NCT03916185. The next five fall between 6 to approximately 54 months: 2) Sanofi RSV D46/NS2/N/ΔM2-2-Hindlll, NCT03099291, NCT03102034; 3) Sanofi, RSV LID ΔM2-2 1030s NCT02952339, NCT02794870; 4) NIH/NIAID, RSV cps2, NCT01852266, NCT01968083; 5) NIH/NIAID, RSV LID ΔM2-2 NCT02040831, NCT02237209; 6) NIH/NIAID, RSV 276 NCT03422237, NCT03227029, NCT03916185. The next five fall between six and 60 months: 7) Sanofi, RSV D46 cp ΔM2-2, NCT02601612; 8) NIH/NIAID, RSV 6120/∆NS1, NCT03596801; 9) NIH/NIAID, RSV 6120/F1/G2/∆NS1, NCT03596801; 10) NIH/NIAID, RSV 6120/∆NS2/1030s, NCT03387137, NCT03916185; 11) NIH/NIAID, RSV MEDI ΔM2-2, NCT01459198 and 12) falls between 24 and 72 months: Novavax RSV F Nanoparticle, NCT02296463.
Under infants and children targeted population, in Phase 2 are six that span between 1 and 24. Between 1 and 8 months: 1) MS&D, MK-1654, NCT03524118. Between 1 and 24 months: 2) AstraZeneca/Sanofi, MEDI-8897, NCT02878330, 3) MedImmune, MEDI-559, NCT00767416. Between 4 and 24 months: 4) MedImmune, MEDI-534, NCT00493285, NCT00686075. Between 6 and 24 months: 5) GSK, ChAd155-RSV, NCT03636906, NCT02927873. Between 12 and 24 months: 6) Janssen, Ad26.RSV.preF, NCT03303625, NCT03606512. There are two vaccines in Phase 3. First one falls between 1 and 8 months: Regeneron, REGN2222, NCT02325791, and the second one falls between 1 and 24 months: MedImmune,MEDI-524, NCT00129766, NCT00121108.
Under the adult 18–54 targeting population are seven companies under Phase 1: 1) Pontificia Univ Catolica de Chile rBCG-N-hRSV, NCT03213405; 2) GSK, RSV F NCT02298179; 3) NIH/NIAID, SeVRSV, NCT03473002; 4) NIH/NIAID/VRC, RSV F DS-Cav1 NCT03049488; 5) Mucosis BV, SynGEM, NCT02958540; 6) Crucell,Ad.RSV.FA2, NCT02561871, NCT02440035; and 7) Vaxart, Ad VXA-RSVf, NCT02830932.
The next two fall between the adults 18–54 and over 55 years. In Phase 1: ReiThera Srl, PanAd3/MVA-RSV NCT01805921 (18−75 years) and in Phase 2: Pfizer, NCT03529773 (18−85 years).
Under the older adults, 55 and over are five vaccines. One in Phase 1: Immunovaccine and VIB, DPX-RSV NCT02472548. Three in Phase 2: 1) Bavarian Nordic, MVA-BN-RSV NCT02873286; 2) GSK, RSV F, NCT03814590; 3) Janssen, Ad26.RSV.preF NCT03339713, NCT03334695. One in Phase 3: Novavax, RSV F Nanoparticle NCT02608502.
Live-attenuated vaccines
Live-attenuated vaccines are versions of RSV that are able to replicate but have been modified to discourage severe disease. They can be created by traditional techniques (i.e. temperature or chemical sensitivity) or by reverse genetics to create an attenuated-replication competent vaccine. The challenge of this technique is to decrease the pathogenicity of the virus but to maintain the replicative function to stimulate immune responses. One of the key downsides, however, is the possibility of partial reversion to wild-type virusFootnote 9.
This technique represents several advantages: possible needle-free delivery by intranasal administration; lack of enhanced diseaseFootnote 10; in the case of intranasal vaccines, replication in the presence of maternal antibodiesFootnote 11; and stimulation of cellular and humoral immunity systemically and locallyFootnote 12. No vaccine candidates of this type have progressed beyond Phase 2 clinical trials. The replicative nature of this type of vaccines and the reduced danger of ERD make it an attractive strategy for seronegative infants.
Vector-based vaccines
Vector-based vaccines are created from components of the RSV virus inserted into a carrier vector, to create a chimeric vector. This chimeric vector replicates according to the carrier vector properties and induces immune responses to both the insert and carrier sequences. The intent is for the carrier vector to enhance responses to the RSV components. This platform is attractive for both pediatric and older adult populations due to the reduced risk of ERD. Unlike live-attenuated vaccines, the chimeric nature of these vectors means there is no risk of reversion to wild-type RSV. In addition, replicating vectors are able to boost the immune responses to the inserted sequences. Several companies are using variations of this platform as RSV vaccine candidates. (See infographic for an overview of the products from each manufacturer).
- Bavarian Nordic (BN) is developing a vector from modified Vaccinia Ankara (MVA) virus, based on the orthopox virus used as a vaccine against smallpox. This vector is used to express several RSV antigens, including wild-type F, G, N, M2-1, and potentially other proteins. This candidate is in the Phase 2 clinical trials of MVA-BN-RSV in older adults [National Clinical Trial (NCT)02873286] for either a one or two-dose strategy via intramuscular route of administration. This trial has demonstrated that this vaccine induces both B and T-cell responses and neutralizing antibodies.
- GlaxoSmithKline (GSK) is developing a nonreplicating vector from Chimpanzee Adenovirus 155 (ChAd155), a simian adenovirus engineered by GSK to produce F, N and M2-1. The version of RSV F protein inserted into this vector lacked the transmembrane domain and the conformation of F is unknown. In adults, this intramuscular vaccine was safe and well-tolerated and induced cellular and humoral immune responses. This vaccine is currently in Phase 2 clinical trials in seropositive infants aged six months and older (NCT03636906). Phase 2 clinical trials in seronegative infants (aged 6–11 months) are in progress.
- Janssen is developing a vector from Adenovirus 26 (Ad26), a human adenovirus, as a carrier vector for prefusion F protein antigens. This vector is being assessed in older adults and infants in Phase 2 clinical trials (NCT03606512; NCT03982199). In seniors, this vector is being assessed alone and in conjunction with a subunit protein (NCT03502707).
Subunit-based vaccines
Subunit-based vaccines are composed of purified viral proteins. They are administered alone or with adjuvant, often as an aqueous solution or emulsion, depending on the route of administration or the adjuvant to boost immune responses. This type of vaccine is expected to predominately induce humoral responses and CD4+ T-cell activationFootnote 13. The lack of CD8+ T-cell responses and the history of ERD necessitates caution in the use of this type of vaccine in seronegative infants. In seropositive populations, including older adults and pregnant women, these types of vaccines represent the opportunity to boost protective antibody responses. Fusion protein or prefusion protein-based vaccines may or may not be synonymous based on their antigenicity profiles and/or features of their high-resolution structures.
- GSK is developing a stabilized prefusion protein vaccine candidate. It is in development for maternal populations and in Phase 2 for older adults (NCT03814590). In Phase 1 testing, the alum adjuvant had no effect on neutralizing antibody responses (NCT02298179). The unadjuvanted product was intended for Phase 2 clinical trial in pregnant women, but it was withdrawn due to issues with protein stability during manufacturing (NCT03191383).
- Janssen is developing a subunit vaccine candidate that is being assessed with and without an adenovirus vaccine. This protein is reported to be in the prefusion conformation. A new candidate of the fusion protein stabilized in its prefusion conformation is now in Phase 2 trials for both the older adult and maternal populations. This program is currently in Phase 1/2 clinical trials (NCT03502707).
Particle-based vaccines
Particle-based vaccines are composed of synthesized nanoscopic particles that present multiple copies of a selected antigen to the immune system. The intent is to boost immunological responses to immunogens by the high copy number and the immune-boosting properties of the particle matrix.
- Novavax developed a recombinant fusion protein particle vaccine with polysorbate 80, ResVax. The conformation of this immunogen was a singly cleaved prefusogenic formFootnote 14. In Phase 1 clinical trials in older populations and pregnant women, ResVax was safe and produced palivizumab-competing antibodiesFootnote 15. However, in Phase 3 clinical trials in older populations, this candidate did not meet the primary outcome (preventing RSV-associated moderate–severe lower respiratory tract disease) or the secondary outcome (reduce all symptomatic respiratory disease due to RSV) (NCT02608502). Currently, a Phase 2 trial is planned to evaluate a reformulation. In Phase 3 clinical trials in pregnant women, this vaccine did not meet its primary objective (prevention of medically significant RSV-related LRTI in young infants) but still demonstrated 39% efficacy in reducing RSV-induced LRTI within the first 90 days of life and in reducing hospitalization by 44%, with the most protection seen if the vaccine was delivered before 33 weeks gestation (NCT02624947).
Monoclonal antibodies
Monoclonal antibodies against RSV have been used as passive immunizing agents. Even once vaccine programs exist, monoclonal antibodies may continue to provide prophylaxis in populations where active immunization will not be effective, such as immunocompromised individuals, or to severely premature infants who receive little or no maternal antibodies. The downside to this technology is that passive antibodies are only protective for as long as they remain in circulation. The passive protection of the passive monoclonal antibody currently available, palivizumab, lasts about a month. New monoclonal antibodies are being developed that could have a higher potency and longer duration of activity.
- AstraZeneca/Sanofi Pasteur is developing nirsevimab (MEDI8897), a recombinant human anti-RSV monoclonal antibody that has been engineered with a triple amino acid substitution in the constant domain to increase its serum half-life. This antibody targets neutralization-sensitive site ø at the apex of the prefusion F protein. One dose of this product could be effective for up to 5–6 months and provide protection for a whole RSV season due to increased potency and increased half-lifeFootnote 16. The increased period of effectiveness for this product could particularly serve to benefit rural and remote communities with reduced access to health care resources and where monthly travel is currently required to obtain palivizumab.
- Regeneron was developing REGN2222 (suptavumab), a monoclonal antibody. This product was fast-tracked from Phase 1 to Phase 3 clinical trials by the Food and Drug Administration in October 2015, but did not meet its primary endpoint of preventing medically attended RSV infection within the first 150 days of life (NCT02325791).
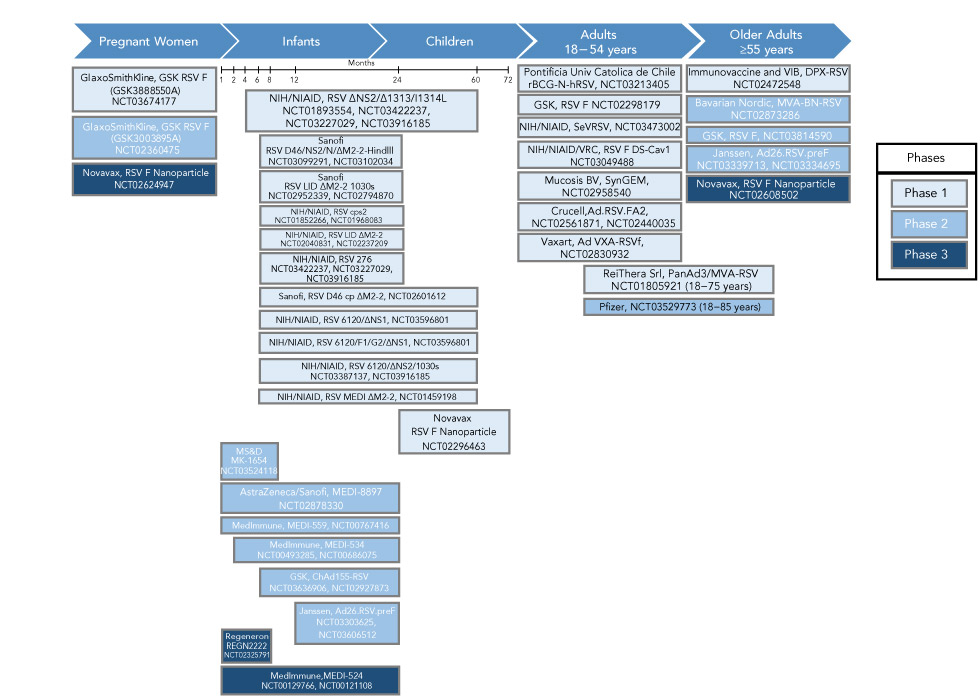
In summary, five different strategies are being pursued to address the challenges of vaccine development for RSV infection. Over 100 trials have been conducted on 38 candidates, and eight new trials were initiated last year alone. Based on data collected through July 1, 2019, Figure 2 describes the timeline of the clinical testing of products in late-stage clinical development. This RSV product development pipeline is becoming increasingly crowded, and it is possible that new vaccines for RSV may be introduced into the Canadian market in the next 2–5 years.
Figure 2: Summary of RSV vaccine products timelineFigure 2 footnote a
Text description: Figure 2
Figure 2: Summary of RSV vaccine products timelineFigure 2 footnote a
Figure 2 is a ten-year timeline flowchart for testing of the RSV vaccine. Below are the phases with the companies that includes the target for each trial with their timelines.
Phase 1
Novavax targeting maternal and older adults 2011–2012
AstraZeneca/Sanofi Pasteur targeting pediatric, two products; one mid 2014 to mid 2015 and second from 2015 through to the end of 2016.
Bavarian Nordic targeting older adults, end of 2015 through to mid 2016.
GaxoSmithKline targeting pediatric, mid 2015 through to mid 2017.
Phase 2
GlaxoSmithKline targeting maternal, one beginning of 2015 through to mid 2016; second from 2016 for a few months and third starting end of 2016 to beginning of 2018. Pediatric starts in 2017 through to the end of 2020. Older adults, mid 2019 through to end of 2020.
Novavax targeting maternal, end of 2012 to mid 2013; second end of 2013 to beginning of 2014; third mid 2014 through to mid 2016. Target older adults one trial end of 2012 through to mid 2014; second trial from end of 2014 through to mid 2016; third end of 2015 through to end of 2016, and fourth beginning of 2017 through to mid 2018.
Janssen Vaccine targeting older adults, end of 2017 through to end of 2018.
Bavarian Nordic targeting older adults, one from end of 2016 through to beginning of 2019.
Phase 3
Novavax, targeting older adults for the year of 2016, maternal from 2016 through to mid 2019.
Challenges to RSV vaccine development
Antigen diversity
A successful vaccine candidate will account for the diversity of antigens presented by RSV in the form of the structural variability of the proteins on the surface of the virus. The protective, neutralizing antibody response to RSV is dominated by antibodies targeting the prefusion F protein on the surface of RSVFootnote 17Footnote 18. Although the genetic sequence of F does not vary substantially between strains of RSV [89% of its sequence is identical in both A and B strainsFootnote 19], amino acids do vary in prefusion specific epitopes. As new products are authorized and make it into broad usage, it will be critical to understand the sero-epidemiological responses at a population level to understand whether prefusion or postfusion antibodies are dominant responses, and whether these demonstrate equivalent protection against both RSV type A and B.
RSV infection dampens the immune response
The second major challenge of RSV vaccine development implicates the cellular and humoral immune responses: RSV infection dampens immune responses. RSV surface and internal proteins can trigger cellular immune responses and antibody-dependant cellular cytotoxicity alongside humoral immune responses. However, several viral mechanisms act to diminish virus-specific proliferative and effector responsesFootnote 20. Even when cellular responses are not dampened by viral mechanisms, they may or may not offer protection. The CD8 T-cell mediated response to RSV is complex and has been associated with both viral clearance and disease pathology, depending on the type and location of the cellsFootnote 21Footnote 22. The response mediated by CD4+ T-cells is also not straightforward as helper T-cell subset 2 biased CD4 responses have been associated with adverse vaccine reactions, yet are needed to induce antibody-mediated responses and other cellular responses, including T-follicular helper cells and effector cellsFootnote 23Footnote 24. The key for vaccine development is to bolster immune responses, despite the dampening effect of RSV, to achieve the aims of the vaccine program: humoral responses may be targeted to prevent infection and cellular responses may be augmented to prevent severe diseaseFootnote 25. Clear definitions of correlates of protection for each of these immune responses are needed to ensure that seroconversion during trials translates to vaccine efficacy.
There are no clear correlates of protection
The third major challenge is the lack of clear correlates of protection for at-risk populations. Natural infection does not induce protection, as evidenced by the fact that 100% of children are infected by age two years but RSV disease recurs across age demographics. Longitudinal studies have demonstrated that children can be naturally reinfected with the same strain of virus, but that the second and subsequent infections are less severeFootnote 26Footnote 27, and there have been similar findings in adultsFootnote 28. Why this is unclear; it may be a combination of low viral immunogenicity or hampered immunological boosting by recurrent infectionsFootnote 29. Current biological markers of protection are humoral, as measured by assays that determine antibody specificity (including the palivizumab-competition assay) and function (neutralization assays). However, this may not be sufficient, as illustrated by the late-stage failure of a monoclonal antibody from Regeneron (suptavumab).
Different correlates of protection may be needed for the two populations at risk for severe RSV disease: infants and older adults. Infants pose a challenge for vaccination as they have underdeveloped immune capabilities. This population may be susceptible to vaccine-induced ERD, as observed in the formalin-inactivated RSV trials. ERD has been attributed to low antibody efficacyFootnote 30 and Th2-biased CD4 immune responsesFootnote 31Footnote 32Footnote 33. The aims of direct and indirect immunization programs for infants includes protection of infection, severe disease and hospitalizationFootnote 34. Discussions are underway in some jurisdictions to define the thresholds of protection in multiple humoral and cellular correlates of protection needed before advancing clinical trials into seronegative populationsFootnote 35.
Older adults face a different challenge in that the immune responses they have developed are waning due to immunosenescence. Immunization in older adults may have different aims and different correlates of protection depending on the health priorities of the jurisdictionFootnote 34. To prevent infection, humoral correlates of protection may be monitored. To prevent severe disease, cellular correlates of protection may be monitored. These two aims are not mutually exclusive, but a vaccine candidate may be better suited at achieving one of the aims over the other. To create a vaccine that is both efficacious and effective, vaccine manufacturers need to consider the public health goals of the vaccine programs and use correlates of protection in preclinical and clinical phases of development that align with these goals.
Discussion
The key to vaccine development will be eliciting an age-appropriate immune response in each target population. Current vaccine strategies are mindful of the history of ERD and the unique immunological characteristics and vulnerability of seronegative children. Live-attenuated and virus-vectored vaccines are two vaccination strategies that are appealing for infants and children, as replicating vaccines do not prime vaccine-enhanced RSV diseaseFootnote 10Footnote 36Footnote 37. Neonates can also acquire immunity against RSV from their mothers. Active transplacental antibody transfer begins at 28–30 weeks gestation, and maternal vaccination to boost anti-RSV response is intended to confer increased infant protection postpartumFootnote 38. Maternal and infant immunization strategies are being pursued to indirectly and directly target the infant population.
Older adults face different challenges in that they are already seropositive but face immunosenescence. To boost the immunological repertoire of this at-risk population, direct and indirect immunization strategies, such as vaccination of children (as with Rotavirus)Footnote 39, may be pursued.
The field of vaccine development for respiratory viruses is rapidly expanding. Technologies tested and proved effective in one field elicit development across the board. Structure-based immunogen design, spurred from publication of the pre-F structure in 2013Footnote 40, has bolstered the development of new RSV vaccines across multiple vaccine platforms (see Figure 2). Technologies to identify and isolate B cells with receptors of interest is enabling the identification of monoclonal antibodies with useful characteristics. Regulatory and production timelines for these products may be faster than for traditional vaccines, putting pressure on expert groups to create guidance within shorter timeframes. mRNA-based vaccines may shorten production timelines further.
Conclusion
Substantial progress has been made in the RSV vaccine development field. Federal, provincial and territorial public health departments in Canada and abroad need to be aware of new products as they are closer to market—how they have addressed the key challenges in RSV vaccine development and how they work to achieve the public health goals for RSV in each jurisdiction.
Authors’ statement
- AK — Writing–original draft, project administration, conceptualization
- MT — Writing–reviewing & editing, conceptualization, supervision
- AH — Writing–reviewing & editing, conceptualization, supervision
- CQ — Writing–reviewing & editing, conceptualization, supervision
- WV — Writing–reviewing & editing, conceptualization, supervision
- DM — Writing–reviewing & editing, conceptualization, supervision
Conflict of interest
None.
Acknowledgements
The authors would also like to acknowledge the significant contribution of N Winters to creation of the figures.
Funding
This work is supported by the Public Health Agency of Canada.
