STI trends and associated risk behaviours in CAF

 Download this article as a PDF
Download this article as a PDF
Published by: The Public Health Agency of Canada
Issue: Volume 46–9: Force Health Protection
Date published: September 3, 2020
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 46–9, September 3, 2020: Force Health Protection
Survey report
Trends in pre-military sexually transmitted infections and associated risk behaviours in Canadian Armed Forces recruits
Heather McCuaig Edge1
Affiliation
1 Directorate Force Health Protection, Canadian Forces Health Services and Directorate Research Personnel and Family Support, Department of National Defence, Ottawa, ON
Correspondence
Suggested citation
McCuaig Edge HJ. Trends in pre-military sexually transmitted infections and associated risk behaviours in Canadian Armed Forces recruits. Can Commun Dis Rep 2020;46(9):272–8. https://doi.org/10.14745/ccdr.v46i09a04
Keywords: sexually transmitted infections, Canadian Armed Forces, military recruits, risk behaviours, condom use, number of sexual partners
Abstract
Background: Sexually transmitted infections (STIs) have historically been problematic for militaries. Recent reports indicating that rates of STIs among young male Canadian Armed Forces (CAF) members are higher than civilians prompted a need to better understand CAF members’ reported rates of STIs and their behavioural risk factors for STIs. This study examined the prevalence of self-reported pre-military sexual behaviours (i.e. number of sexual partners and frequency of condom use) and history of a STI diagnosis among CAF recruits attending basic military training using data collected from the Recruit Health Questionnaire.
Methods: Data came from 50,603 recruits who participated in the survey between 2003 and 2018 (84.9% male, 78.6% Non-Commissioned Member candidates, 64.9% aged between 17 and 24 years).
Results: Among sexually active recruits, the proportions who had more than one sexual partner in the previous year increased from 30.5% in 2003 (95% CI, 27.8–33.4) to 35.5% in 2018 (95% CI, 34.0–37.0). Of recruits who were not in an exclusive relationship at the time, the proportions who reported always using a condom decreased from 50.8% in 2003 (95% CI, 46.4–55.1) to 40.2% in 2018 (95% CI, 38.3–42.2). Overall, 5.5% (95% CI, 5.3–5.7) reported ever having received a STI diagnosis. Demographic differences by age and sex were also found.
Conclusion: These observations provide an indication of the baseline, pre-enlistment STI risk behaviours, and STI history among CAF recruits, and may provide insight into avenues for targeted interventions and health promotion programming, such as education and screening initiatives.
Introduction
Sexually transmitted infections (STIs) have historically been problematic for militariesFootnote 1Footnote 2. For example, reported rates of STIs have been much higher in the United States (US) military population compared with the civilian populationFootnote 3Footnote 4Footnote 5. Recent comparisons between the Canadian general population (CGP) and Canadian Armed Forces (CAF) personnel revealed that while rates of STIs were the same as or lower than civilians in most demographic groups, the rates of STIs among young (i.e. younger than 30 years) male CAF members were almost double those of their civilian counterpartsFootnote 6. A qualitative study revealed that CAF personnel and healthcare providers alike perceived STIs as a problem within CAF, and many indicated that STIs were similarly, or even more, problematic for CAF than for the CGPFootnote 7.
The Public Health Agency of Canada has identified behavioural risk factors associated with STIs; including sexual activity in youth younger than 25 years, new or more than two sexual partners in the previous year, unprotected sex, alcohol or substance use and a history of a STI, among othersFootnote 8. Military members may be at elevated risk for acquiring STIs given the younger age of the majority of personnel, frequent and extended time spent away from home for training or operations, deployments to areas with higher rates of STIs, or elevated rates of risk-taking attitudes and behaviours associated with STIsFootnote 9Footnote 10Footnote 11. Self-reported STI risk behaviours among serving CAF members indicated that almost 21% reported having had two or more sexual partners in the previous 12 months, and of those, only 22% reported always using a condom, while approximately 18% reported never using a condomFootnote 12.
Determining the baseline prevalence and demographic profiles of STI risk behaviours and STI history among new recruits can inform education, screening and intervention practices at the beginning of the military career. Thus, this study examined the prevalence of STI risk behaviours (i.e. number of sexual partners and frequency of condom use) and self-reported pre-military history of a STI diagnosis among CAF recruits attending basic military training (BMT).
Methods
Data for this study were collected between July 2003 and December 2018 using the Recruit Health Questionnaire (RHQ), administered during the first few weeks of BMT at the Canadian Forces Leadership and Recruit School in St-Jean-sur-Richelieu, Québec. All Regular Force Non-Commissioned Member (NCM) and Officer candidates (hereafter collectively referred to as “recruits”) enrolled in BMT were invited to complete the RHQ—a long term, ongoing surveillance study that provides baseline health and lifestyle information about recruits. The RHQ is a voluntary survey that recruits provide written consent to participate in. Participants’ data is linked via service number to health data collected later in their career; thus, data are confidential, not anonymous. Approximately 75% of recruits completed the RHQ. The RHQ study protocol was approved by the Defence Research and Development Canada Human Research Ethics Committee.
The RHQ includes items assessing number of sexual partners in the previous year, frequency of condom use and STI history. Number of sexual partners was assessed with the question “How many different sexual partners have you had in the past 12 months?” with response options of “none,” “one partner,” “two partners,” “three partners” or “four or more”. Frequency of condom use was assessed with the question, “If you were not in an exclusive relationship at the time, how often did you use a condom in the past 12 months?” with response options of “always,” “usually,” “occasionally,” “never” and “not applicable”. The proportion of respondents with a previous STI diagnosis were estimated based on “yes/no” responses to the question, “Have you ever been told by a doctor or nurse that you had a sexually transmitted infection—like chlamydia, gonorrhea, genital herpes, or syphilis?” The procedure of administration and questions related to sexual behaviours and STI history has not changed over the 16-year period.
The data about sexual behaviours and STI history are self-reported and are, thus, subject to recall and social desirability biases, which may result in under or over-reportingFootnote 13. As noted elsewhereFootnote 14, while the impact of social desirability on self-reports of sexual behaviours is difficult to quantify, studies have confirmed the general reliability of responses.
Descriptive analysis of crude proportions along with 95% CIs was examined for each cohort year. Sequential logistic regressions controlling for age and sex were conducted to identify linear and non-linear (i.e. quadratic or cubic) trends over time, with cohort year (or its squared or cubed value) entered as a continuous variable. A trend was detected if the addition of cohort year (or its squared or cubic values) to the model significantly improved the model fit, as indicated by a significant chi-square. Difference tests between cohort years were conducted using z-tests of proportions, while chi-square analyses were conducted to detect demographic differences.
Results
Data were available for 50,603 cases from recruits who participated in the RHQ between July 2003 and December 2018. Respondents were mostly male (84.9%), NCM candidates (78.6%), primarily English-speaking (72.7%) and between 17 and 24 years old when they completed the RHQ (64.9%; M=24.0; SD=5.9).
Trends, 2003–2018
Among sexually active recruits, the proportions who had two or more sexual partners in the previous year increased from 30.5% overall in 2003 (95% CI, 27.8–33.4) to 35.5% overall in 2018 (95% CI, 34.0–37.0; p<0.01; Figure 1). Significant trends, controlling for age and sex, indicated that the number of sexual partners reported by recruits in the previous year have fluctuated between 2003 and 2018 (χ2 (5)=1,344.28; p< 0.001).
Figure 1: Annual overall and sex-specific rates of self-reported number of sexual partners in Canadian Armed Forces recruits, two or more partners in the previous year, 2003–2018
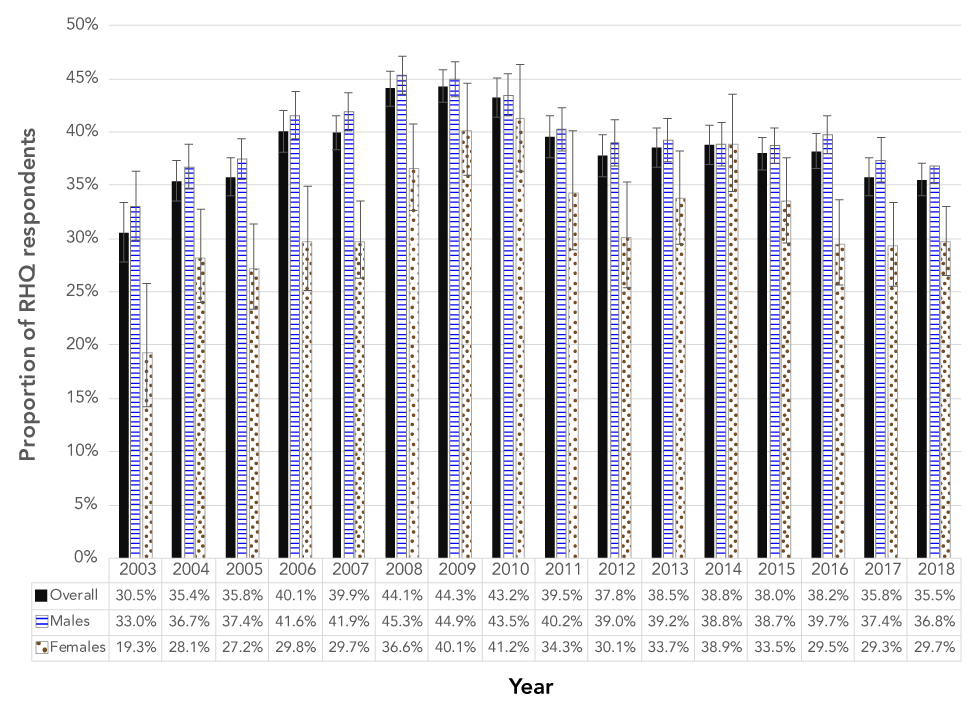
Text description: Figure 1
Figure 1: Annual overall and sex-specific rates of self-reported number of sexual partners in Canadian Armed Forces recruits, two or more partners in the previous year, 2003–2018
The graph shows annual rates of self-reported number of sexual partners in Canadian Armed Forces (CAF) recruits overall and by sex (male versus female) from 2003 to 2018, with error bars representing 95% confidence intervals. The percentages represent those who reported having two or more sexual partners in the year prior to basic training. The overall proportion of sexually active recruits with two or more sexual partners within the last year increased from 2003 (30.5%) to 2009 (44.3%) and gradually decreased from 2010 (43.2%) to 2018 (35.5%). The annual trend was similar for males, whereby rates increased from 2003 (33.0%) to 2008 (45.3%) and decreased from 2009 (44.9%) to 2018 (36.8%). The annual trend for females was more varied: the proportion increased from 2003 (19.3%) to 2010 (41.2%), decreased from 2011 (34.4%) to 2012 (30.1%), increased again from 2013 (33.7%) to 2014 (38.9%), and decreased again from 2015 (33.5%) to 2018 (29.7%). In general, the overall proportion who reported two or more sexual partners increased from 2003 to 2018. With the exception of 2014, more males reported having two or more sexual partners in the last year than females, those these differences by sex were not always statistically significant.
Of recruits who were not in an exclusive relationship at the time, the proportion who reported always using a condom decreased from 50.8% in 2003 (95% CI, 46.4–55.1) to 40.2% in 2018 (95% CI, 38.3–42.2; p< 0.001; data not shown). As depicted in Figure 2, the proportion who reported never using a condom increased from 16.5% in 2003 (95% CI, 13.5–20.0) to 25.7% in 2018 (95% CI, 24.0–27.5; p< 0.001). Respondents who selected “not applicable” were excluded from these analyses, resulting in a reduced n=27,783 for this STI risk behaviour. Significant trends controlling for age and sex were found, indicating that rates of condom use reported by recruits during the previous year have varied significantly over the 16-year period (χ2 (5)=400.70; p< 0.001).
Figure 2: Annual overall and sex-specific rates of self-reported rates of never using a condom in the previous year, for Canadian Armed Forces recruits not in a relationship, 2003–2018
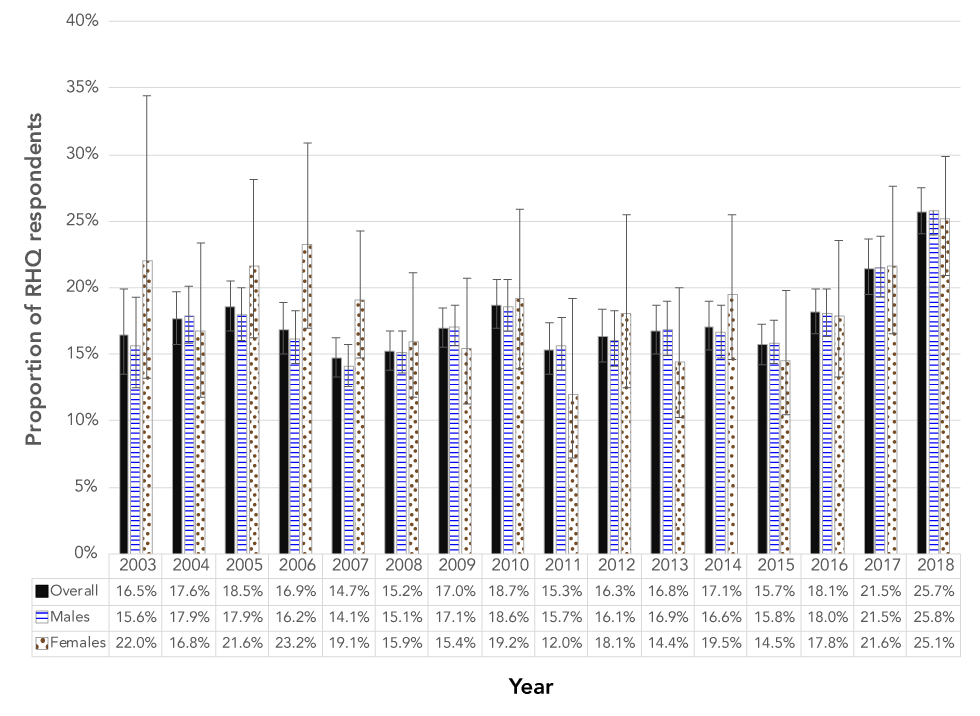
Text description: Figure 2
Figure 2: Annual overall and sex-specific rates of self-reported rates of never using a condom in the previous year, for Canadian Armed Forces recruits not in a relationship, 2003–2018
The graph shows annual overall and sex-specific rates of self-reported condom use in Canadian Armed Forces (CAF) recruits from 2003 to 2018, with error bars representing 95% confidence intervals. The percentages represent those not in a relationship who reported never using a condom in the year prior to basic training. The overall proportion who reported never using a condom increased from 2003 (16.5%) to 2018 (25.7%). This trend was consistent when analyzed by sex. For males, rates increased from 15.6% in 2003 to 25.8% in 2018. For females, rates increased from 22.0% in 2003 to 25.1% in 2018.
Overall, 5.5% (95% CI, 5.3–5.7) of recruits reported ever having received a STI diagnosis (Figure 3). These proportions were not significantly different for the 2003 or 2018 recruit cohorts. There was a significant trend found in the rates of recruits having reported ever having had a STI diagnosis (χ2 (5)=445.18; p< 0.001) after controlling for age and sex, indicating that the rates of reported STI diagnoses varied over the 16-year period.
Figure 3: Annual overall and sex-specific rates of self-reported history of sexual transmitted infections diagnosis in Canadian Armed Forces recruits, 2003–2018
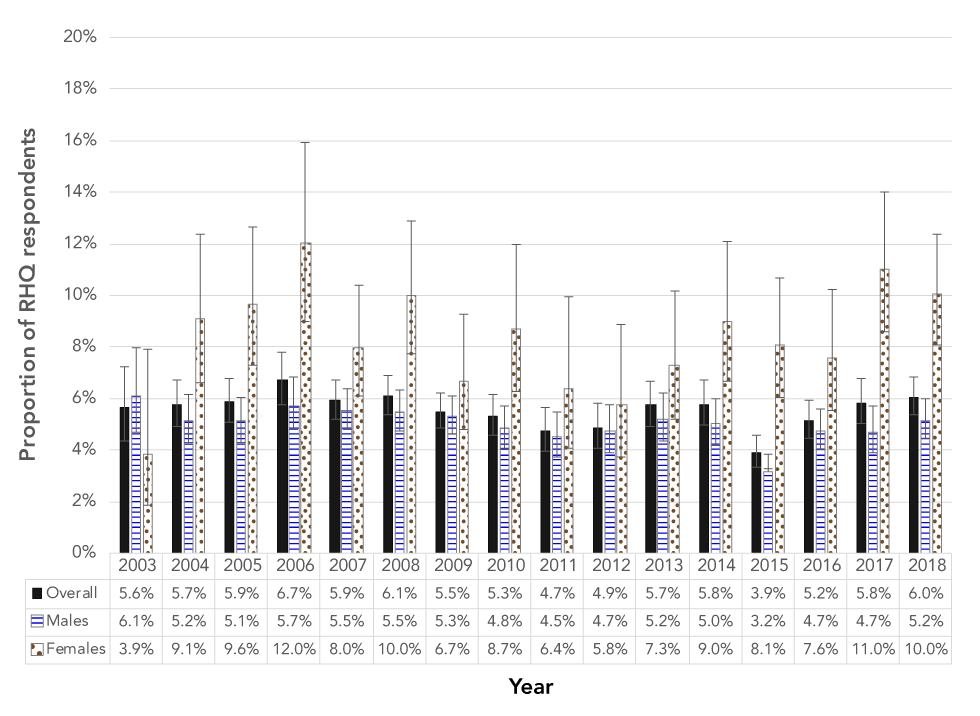
Text description: Figure 3
Figure 3: Annual overall and sex-specific rates of self-reported history of sexual transmitted infections diagnosis in Canadian Armed Forces recruits, 2003–2018
The graph shows annual overall and sex-specific rates of self-reported sexually transmitted infections (STIs) history in Canadian Armed Forces (CAF) recruits from 2003 to 2018, with error bars representing 95% confidence intervals. The proportions represent those who reported a history of STI diagnosis prior to basic training. The overall proportion who reported a STI history increased from 2003 (5.6%) to 2018 (6.0%), but not to a statistically significant degree. For males, rates decreased from 6.1% in 2003 to 5.2% in 2018; whereas for females, rates increased from 3.9% in 2003 to 10.0% in 2018. From 2004 to 2018, females reported more STI diagnoses than males.
Demographic differences
Pooling responses over the 16-year period, demographic differences by sex and age were also found for number of sexual partners, condom use and STI history. As depicted in Figure 4, more male than female recruits reported having two or more sexual partners in the previous year (χ2 (2)=716.75; p<0.001), while more female than male recruits reported a previous STI diagnosis (χ2 (1)=43.44; p< 0.001). Of recruits who were not in an exclusive relationship at the time, more female than male recruits reported always using a condom (data not shown; χ2 (2)=84.93; p< 0.001); however, there were no differences in the proportions of male and female recruits who reported never using a condom.
Figure 4: Sexually transmitted infections history and associated risk behaviours in Canadian Armed Forces recruits, by sex
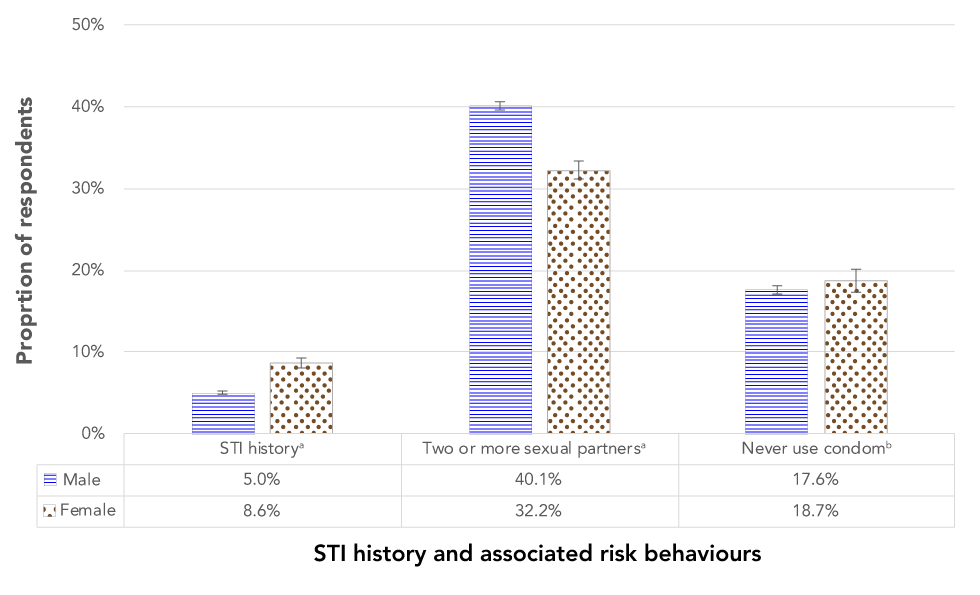
Text description: Figure 4
Figure 4: Sexually transmitted infections history and associated risk behaviours in Canadian Armed Forces recruits, by sex
The graph shows sex-specific rates of self-reported sexually transmitted infections (STIs) history and associated risk behaviours (i.e. two or more sexual partners and never using a condom) in Canadian Armed Forces (CAF) recruits. The proportions represent pooled data collected from 2003 to 2018, with error bars representing 95% confidence intervals. Significantly more female recruits (8.6%) reported a history of STIs than male recruits (5.0%), but significantly more male recruits (40.1%) had two or more sexual partners within the last year than female recruits (32.2%). There was no significant difference between males (17.6%) and females (18.7%) who reported never using a condom.
As depicted in Figure 5, the proportions of reports of having two or more sexual partners in the previous year significantly differed for each age group (χ2 (6)=3,183.48; p< 0.001), with the highest proportion among recruits aged 20 to 24 years. Recruits aged 30 or older who were not in an exclusive relationship had the highest proportion of reports that they never used a condom, with the proportions being significantly lower in each descending age group (χ2 (6)=365.01; p< 0.001). There were proportionally more recruits aged 25 or older who reported a history of a STI diagnosis than younger recruits (χ2 (3)=512.67; p< 0.001), with the youngest group of recruits (i.e. those aged 17 to 19 years) reporting the lowest proportion of STI diagnosis history.
Figure 5: Sexually transmitted infections history and associated risk behaviours by age group in Canadian Armed Forces recruits
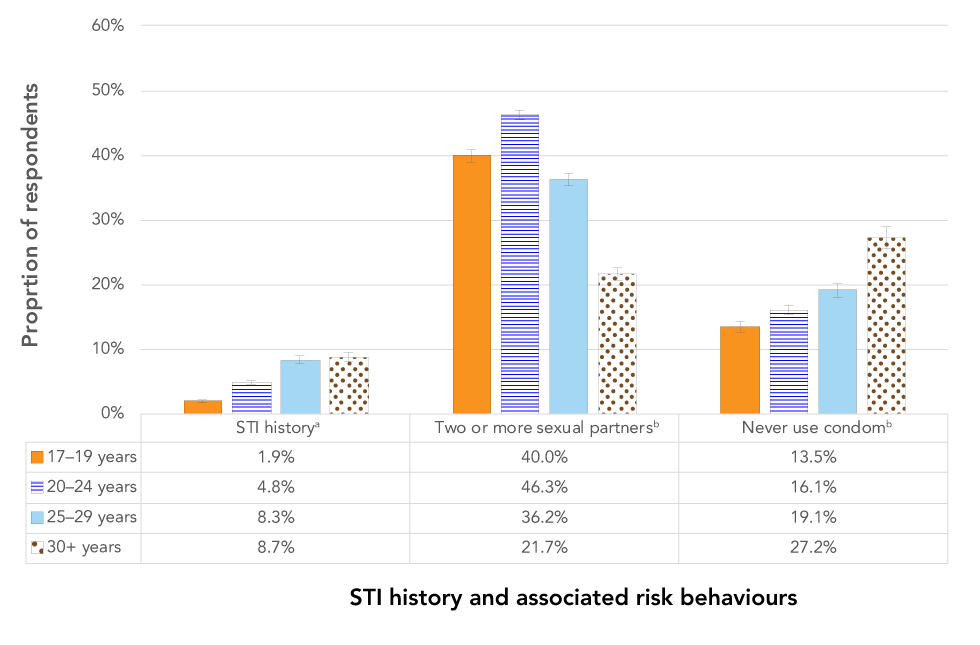
Text description: Figure 5
Figure 5: Sexually transmitted infections history and associated risk behaviours by age group in Canadian Armed Forces recruits
The graph shows age-specific rates of self-reported sexually transmitted infections (STIs) history and associated risk behaviours (i.e. two or more sexual partners and never using a condom) in Canadian Armed Forces (CAF) recruits. The proportions represent pooled data collected from 2003 to 2018, with error bars representing 95% confidence intervals. The analyses were divided by four age groups (17–19 years, 20–24 years, 25–29 years, and 30 years and older). STI history significantly differed by age, with recruits aged 17–19 years reporting the lowest proportion (1.9%) and recruits aged 25 years and older reporting the highest proportions (8.3%–8.7%). Recruits aged 25–29 years and 30 years and older did not significantly differ by STI history. Reports of two or more sexual partners also differed by age: recruits aged 20–24 years reported the highest proportion (46.3%), followed by recruits aged 17–19 years (40.0%), 25–29 years (36.2%), and 30 years and older (21.7%). Never using a condom also significantly increased by age, with recruits aged 17–19 years reporting the lowest proportion (13.5%) and recruits aged 30 years and older reporting the highest proportion (27.2%).
Discussion
Observations from the RHQ concerning the number of sexual partners, frequency of condom use and STI history, suggest that the majority of recruits were not engaging in risky sexual behaviours. However, at least a third of recruits reported having had two or more sexual partners in the year prior to starting BMT. More recently, among those who were not in an exclusive relationship at the time, a quarter of recruits reported never using a condom. From 2003 to 2018, the proportions of recruits reporting multiple sexual partners and never wearing a condom increased. These patterns in STI risk behaviours mirror the recent increases in rates of STIs reported in the general population in CanadaFootnote 15Footnote 16Footnote 17 and in other high-income countriesFootnote 18Footnote 19, and are also consistent with increased risky sexual behaviours among adolescents and adults in the CGPFootnote 14Footnote 20Footnote 21Footnote 22.
While reports of recruits having had a STI diagnosis prior to BMT have remained relatively low, consistently more female than male recruits reported a history of STI diagnosis. This is unsurprising given that, for certain STIs (e.g. chlamydia), women tend to have higher rates of infection than menFootnote 16 and tend to be screened and/or seek health care more regularly, and would, therefore, be more likely to have been diagnosed than menFootnote 23Footnote 24Footnote 25. Moreover, because of their physiology, women are more susceptible than men to acquire STIsFootnote 24.
Differences in the number of sexual partners between men and women were consistent with findings that men tend to report having more sexual partners than womenFootnote 14Footnote 21Footnote 22. This difference may be due to socialization, gender roles or sociocultural norms surrounding sexual behaviours and the reporting thereofFootnote 26. In line with findings from the CGPFootnote 21Footnote 22, the proportion of recruits reporting multiple partners was lower in the older age groups, possibly due to increased likelihood of older recruits being in longer term, monogamous relationships. The largest proportion of recruits reporting multiple partners was among the 20 to 24-year old group, which is the age group with the highest rates of gonorrheaFootnote 17 and chlamydiaFootnote 16 and the third highest rates of infectious syphilis in the CGP in 2015Footnote 15.
Consistent with findings from the CGP that have found that regular condom use declines with ageFootnote 14Footnote 20Footnote 23, a higher proportion of older recruits who were not in an exclusive relationship at the time reported never using a condom, compared with younger recruits. This could be due to the increased use of other contraceptive methods for preventing pregnancy with increased ageFootnote 21; however, these methods do not prevent STIs.
Findings from recruits are consistent with the rates and behaviours found in the CGP; this is unsurprising since recruits were drawn from the CGP and had not yet begun their military careers when the RHQ was administered. The importance of this research for CAF in its efforts to prevent STIs are highlighted by the observed increasing rates of STI risk behaviours, the higher STI rates and risk among military membersFootnote 3Footnote 4Footnote 5Footnote 6Footnote 9Footnote 27 and perceptions of STIs as a problem for CAFFootnote 7. These efforts may be especially important for recruits, who have not yet experienced some of the military situations that may place military personnel at increased risk for acquiring STIs, such as deploymentsFootnote 9Footnote 11, or having higher levels of risk propensityFootnote 28. While the risk for STIs may be elevated for military members, CAF also presents an opportunity for members to more easily access health care for primary and secondary prevention and health promotion programming. Other militaries have implemented programs that have reduced STI rates, such as in US recruit training centers, and have proven effective at increasing STI knowledge and perceived norms for safe sexFootnote 29Footnote 30Footnote 31Footnote 32Footnote 33. These programs included mass screening and programming that included presentations and activities to educate about the transmission, symptoms and prevention of STIs, or emphasized adaptive decision-making skills and communication strategies. Other programs aimed at the general population using digital interventions, online programs and social media have been effective at increasing condom use, knowledge and perceived norms surrounding safe sex, especially among younger individualsFootnote 34Footnote 35Footnote 36. Similar programming and interventions could be implemented in CAF’s BMT program or in other routine training or health promotion activities throughout the military career.
Strengths and limitations
This surveillance report, based on observational data, presents a baseline indication of pre-enlistment STI risk behaviours and STI history among recruits. It provides trend information for 16 years of recruit cohorts, and describes demographic differences in reports of STI history, number of sexual partners in the previous 12 months and frequency of condom use. These findings underscore the rising trends in risky behaviours associated with acquiring STIs in both the CGP and in CAF recruits, as well as provide insight into demographic information about groups of individuals at particular risk for STIs. These data could inform the development of screening tools to identify segments of the recruit population that might benefit from targeted interventions and health promotion programming.
This study and the RHQ are not without limitations. The RHQ data were self-reported; a technique which is prone to social desirability bias, recall bias and subjectivityFootnote 13Footnote 37. In addition, there was no way of assessing the accuracy of responses. Further, we had single item measures asking about sensitive topics. As such, some recruits may have been reluctant to disclose personal information about their sexual history and sexual behaviours, which may have resulted in under-reporting. The requirement for an individual to be in an “exclusive relationship” in the question about frequency of condom use may have resulted in the exclusion of individuals who had been in serially monogamous relationships. These individuals may not have responded, as they considered themselves to be in an “exclusive relationship”, yet the nature of these relationships may expose them to a significant number of sexual partners in a short period of time. Moreover, the current RHQ does not consider sexual identity or sexual preference, which may impact risk behaviours for STIs and intervention strategies. Future research on STI risk behaviours with CAF members should take sexual preference into consideration. Finally, the RHQ is voluntary, so results are based on the subset of recruits who chose to respond rather than the whole population of recruits who trained during this period. Although the overall response rate was high (75.6%), there may be demographic differences between respondents and non-respondents.
Conclusion
Since 2003, risk behaviours for acquiring STIs have increased among recruits, but these rates are consistent with similar increases observed in CGP. Findings from this study provide baseline information about sexual risk behaviours for STIs among CAF population, and a demographic profile of those at higher risk for STIs. These findings may provide insight, especially for CAF, into avenues for targeted interventions and health promotion programming, such as education, primary and secondary prevention and screening initiatives.
Author’s statement
HJME conceived and wrote the article.
Competing interests
None.
Acknowledgements
The author would like to thank the following members of the Canadian Forces Health Services Group and Director General Military Personnel and Analysis for their valuable help and feedback on this article: Dr. D Lu; Cdr K Barnes; Dr. J Lee; G Ivey; S Carlucci; LCol C Rossi and Col P Morissette.
Funding
This project was funded by the Department of National Defence, Canada.
