
 Download this article as a PDF
Download this article as a PDF Published by: The Public Health Agency of Canada
Issue: Volume 48-2/3, February/March 2022: Syphilis Resurgence in Canada
Date published: February/March 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-2/3, February/March 2022: Syphilis Resurgence in Canada
Eyewitness
Delayed diagnosis of maternal and congenital syphilis: An unrecognized epidemic?
Zachary Dionisopoulos1, Fatima Kakkar2, Ana C Blanchard2
Affiliations
1 Paediatrics Residency Program, Department of Paediatrics, CHU Sainte-Justine, Université de Montréal, Montréal, QC
2 Division of Infectious Diseases, Department of Paediatrics, CHU Sainte-Justine, Université de Montréal, Montréal, QC
Correspondence
Suggested citation
Dionisopoulos Z, Kakkar F, Blanchard AC. Delayed diagnosis of maternal and congenital syphilis: An unrecognized epidemic? Can Commun Dis Rep 2022;48(2/3):115–8. https://doi.org/10.14745/ccdr.v48i23a10
Keywords: syphilis, sexually transmitted infections, pregnancy, congenital infection, epidemiology
Abstract
Syphilis is an infection caused by Treponema pallidum spirochetes. The diagnosis of this sexually transmitted disease may be missed, partly due to the painless nature of genital ulcers in its primary stage. Women in Canada are screened for syphilis in their first trimester of pregnancy, but late pregnancy testing is not done in all provinces to date; therefore, undetected vertical transmission of syphilis may occur. This case emphasizes the importance of recognizing congenital syphilis in infants and young children with unexplained growth problems and biochemical and hematological abnormalities. Congenital syphilis remains a rare diagnosis, but in the context of increased syphilis rates in Canada during recent years, clinicians should consider this diagnosis in infants presenting with compatible clinical manifestations.
Introduction
Congenital syphilis can be challenging to diagnose, as it may mimic other conditions. In addition, clinicians may not consider congenital syphilis due to the rarity of this diagnosis and because women are screened for syphilis in first trimester of pregnancy. Here, we report the case of an infant with intrauterine growth restriction (IUGR) and known congenital cytomegalovirus infection who presented with persistent anemia, thrombocytopenia and liver enzyme elevation. This case highlights the need to have a high index of suspicion in infants presenting with these findings and raises important questions about the need for third trimester screening in pregnant women in Canada.
Case
A two-month-old infant was admitted to hospital for evaluation of bicytopenia and hepatitis in September 2021. He was born to a G1P1 21-year-old-mother. In the first trimester, she had negative HIV, hepatitis B and C virus and syphilis serologies. She was rubella immune and had negative chlamydia and gonorrhea urine screens. The pregnancy was complicated by oligohydramnios and IUGR in the third trimester. The baby was born prematurely at 35+1/7 weeks of gestation by vaginal delivery, with Apgar scores of 9-10-10. Birth parameters confirmed IUGR with a birth weight of 1,910 kg (z score -1.48, centile 6.97), a length of 46 cm (z score -0.09, centile 46.47) and a head circumference of 31 cm (z score -0.86, centile 19.53). As part of his IUGR workup, salivary and urine cytomegalovirus (CMV) polymerase chain reaction (PCR) tests were done at day zero and day five of life and were found to be positive at 33,884,416 and 3,801,894 copies/mL respectively. The infant had a normal complete blood count and liver enzyme panel at that time. A transfontanellar ultrasound showed small colloidal parenchymal cysts in the right caudate nucleus of unknown origin, without intracranial calcifications. A cerebral magnetic resonance imaging was normal. Ophthalmological and audiological exams were normal. Valganciclovir was initiated at a dose of 16 mg/kg/dose twice daily, with a plan to complete six months of therapy. He was discharged home at 38+4/7 weeks.
On follow-up at six weeks of age, the infant was found to have a hemoglobin level of 66 g/L, a platelet count of 77x109/L and a white blood count of 10x109/L. His alanine aminotransferase level was 253 U/L, aspartate aminotransferase was 254 U/L, gamma-glutamyl transferase was 256 U/L, alkaline phosphatase level was 690 U/L, albumin was 29 g/L and his coagulogram was normal. The anemia and liver enzyme abnormalities were thought to be due to valganciclovir toxicity so treatment was held. He was seen in the clinic a week later without improvement of his blood work findings; therefore, he was admitted to the Paediatrics ward for further investigation.
On admission, he was afebrile and well overall. On physical exam, he had hepatosplenomegaly and mild diffuse desquamation. He was irritable, but consolable. An extensive workup was done including blood and urine cultures, nasopharyngeal multiplex viral PCR, Epstein Barr virus, parvovirus B19, adenovirus, herpes simplex virus and CMV blood PCRs—all results were negative. He required a packed red blood cell transfusion as his hemoglobin had dropped to 57 g/L.
After 10 days in hospital, the infant developed a new onset low grade fever. Given the persistent unexplained anemia, a bone marrow aspirate was planned. On repeat questioning of the mother alone for possible infectious symptoms, she described for the first-time flu-like symptoms following delivery, as well as a sore throat and genital lesions. In addition, she presented at the time of repeat questioning a bilateral erythematous scaling papular palmar rash (Figure 1) on physical examination, which had appeared in the previous three weeks. Syphilis serologies were immediately ordered on the patient and his mother. They both had strongly-positive syphilis enzyme immunoassays and rapid plasma reagin of 1:64. A lumbar puncture was performed on the infant, with the cerebrospinal fluid analysis showing normal white and red blood cell counts, glucose and protein profiles as well as a negative Venereal Disease Research Laboratory test. A cerebral magnetic resonance imaging was repeated and was normal. A skeletal survey was not conclusive for congenital syphilis, but slightly enhanced periosteal reactions were noted along both femurs and the right tibia (Figure 2). Placental examination showed only one area of villitis of unknown significance, and no spirochetes were seen on immunochemistry stains.
Figure 1: Bilateral erythematous scaling papular palmar rash, woman with secondary syphilis, Montréal, 2021

Text description: Figure 1
This photograph shows a bilateral erythematous scaling papular palmar rash in the mother of the patient. She had this rash for three weeks at the time that it was observed and photographed. She reported that it had been oozing clear fluid initially but had become dry for several days.
Figure 2: Radiograph of the right femurFigure 2 Footnote a of an infant with congenital syphilis, Montréal, 2021
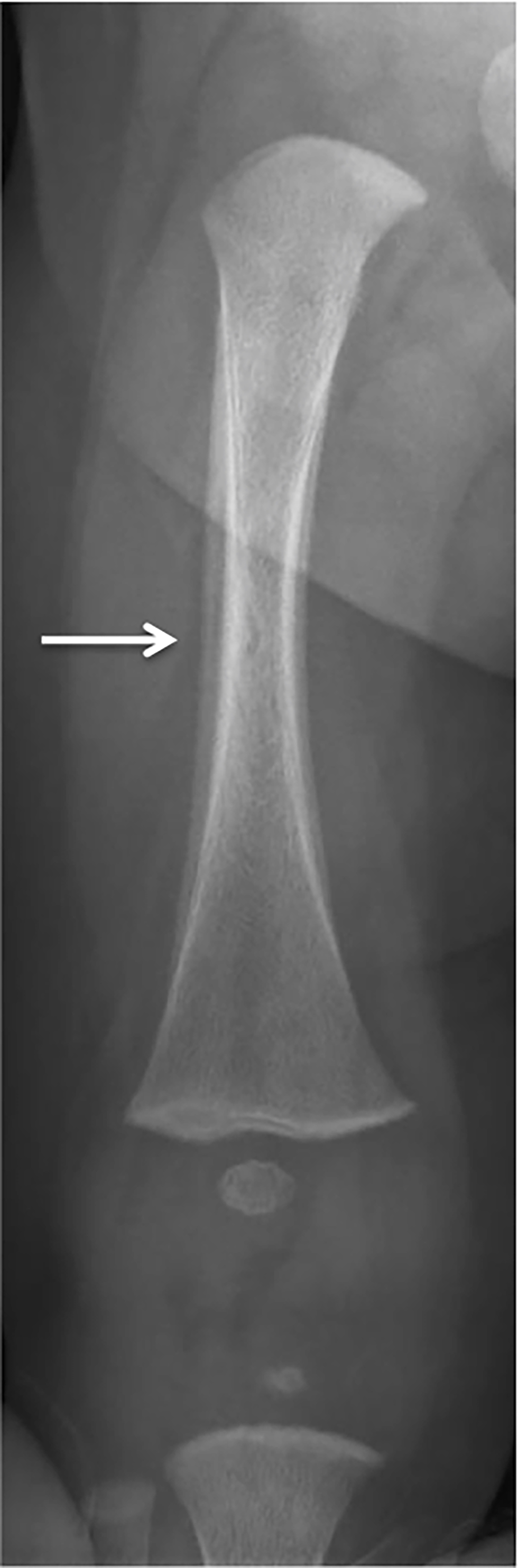
Text description: Figure 2
A skeletal survey performed at 68 days of life showed periosteal reactions along both femurs, as well as the right tibia, that were more than physiologic for the patient’s age. No bone destruction was seen, but the zones of provisional calcification were dense.
The infant was treated with a 10-day course of intravenous penicillin G, with rapid resolution of his fever and his bloodwork abnormalities. A repeat rapid plasma reagin at the end of treatment was 1:32. The patient was discharged with follow-up in the Congenital Infection Clinic. His mother was referred to an adult infectious diseases clinic, where she received appropriate treatment and serological follow-up.
Discussion
The rate of syphilis in Canada increased by 85.6%, from 5.0 to 9.3 cases per 100,000 population, from 2010 to 2015. Although this rate was higher in males than in females and was thought to be largely attributable to men who have sex with men, there was a 27.8% increase among females with individuals aged 20–39 years having the highest ratesFootnote 1. In a recent report, national rates of syphilis increased by 124% between 2016 and 2020, with the largest increase occurring among females (740%). Nearly a third of cases occurred in women (versus only 8% in 2016)Footnote 2. In addition, the incidence of congenital syphilis has been rising in recent years in Canada, with cases increasing from 2.5 per 100,000 women aged 15–39 years in 2016 to 39.7 per 100,000 women aged 15–39 years in 2020Footnote 2. This alarming rise in syphilis amongst Canadian women and their infants calls for urgent attention, as has already been recently reported in the United States and Australia (3,4). The Canadian Paediatric Surveillance Program has recently began a cross-sectional study across Canada to describe the epidemiology of congenital syphilis, identify risk factors in mothers of affected children and describe the investigation and management of these childrenFootnote 5.
Congenital syphilis occurs through vertical transmission, during pregnancy and/or birth. It may have severe consequences for the infant, including sensorineural hearing loss, neurodevelopmental disorders, musculoskeletal deformity or deathFootnote 6. The risk of transmission varies from 10% to up to than 80% depending on the mother’s stage of disease, with a higher risk of transmission in primary and secondary stagesFootnote 6. With appropriate treatment in pregnancy, the risk of congenital syphilis decreases to 1%–2%Footnote 7. Although syphilis is routinely tested for in first trimester of pregnancy, serological testing of pregnant women later in pregnancy is not currently a widespread practice across Canada. This is typically done in a targeted fashion for high-risk settings, of which the definitions may vary. Third trimester screening has been implemented in 2019 in British Columbia, due to the occurrence of two severe congenital syphilis casesFootnote 8.
Infants may be completely asymptomatic at birthFootnote 9; however, a wide array of clinical manifestations may occur in the context of congenital infection, including prematurity, small stature for gestational age, anemia, thrombocytopenia, hepatosplenomegaly and osteitisFootnote 9. Paediatricians and family doctors should be aware of these clinical manifestations, promptly suspect congenital syphilis, obtain investigations and provide rapid management to prevent late-onset disease and complications. A detailed history of symptoms and epidemiological risk factors should be obtained from mothers in complete confidentiality, as illustrated in this case, so that the opportunity for diagnosis is not missed. All children with clinical or serological evidence of congenital syphilis should be treated with penicillin G for 10 to 14 days, depending on severity of their disease. Clinical and serological follow-up of all children potentially exposed to syphilis in utero is requiredFootnote 9.
Of note, coinfection with CMV and syphilis in newborns remains largely undescribed in the literature. As CMV is increasingly recognized as a leading cause of congenital infection, it may be more frequently detected; therefore, there may be more cases of coinfection described in the future. The impact of coinfection on the long-term clinical outcomes of affected infants will warrant further research.
Conclusion
This case highlights the importance of considering congenital syphilis in young infants with unexplained hepatosplenomegaly, hematological and biochemical abnormalities, despite negative first trimester screening during pregnancy. Surveillance initiatives, such as that led by the Canadian Paediatric Surveillance Program, are useful to characterize the epidemiology and severity of congenital syphilis which is potentially underdiagnosed in Canadian youth. With the current resurgence of syphilis in Canada, third trimester testing of pregnant women may be considered by public health policy makers in different provinces and territories.
Authors’ statement
All authors were involved in the management of the patient: ZD and ACB made the diagnosis and provided initial management and counselling And FK provided long-term clinical follow-up and management. ZD wrote the initial draft of the manuscript. ACB oversaw manuscript preparation and revisions. All authors read and approved the final manuscript.
The content and view expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests
None.
Acknowledgements
The authors would like to thank the mother of the patient, who accepted that this data be shared with the scientific community to raise awareness about syphilis.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
