Syphilis in Canada, 2011–2020

 Download this article as a PDF
Download this article as a PDF Published by: The Public Health Agency of Canada
Issue: Volume 48-2/3, February/March 2022: Syphilis Resurgence in Canada
Date published: February/March 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-2/3, February/March 2022: Syphilis Resurgence in Canada
Surveillance
Rising syphilis rates in Canada, 2011–2020
Josephine Aho1, Cassandra Lybeck1, Ashorkor Tetteh1, Carmen Issa1, Fiona Kouyoumdjian2, Jason Wong3,4, Alexandrea Anderson1, Nashira Popovic1
Affiliations
1 Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada, Ottawa, ON
2 Ontario Ministry of Health, Toronto, ON
3 BC Centre for Disease Control, Vancouver, BC
4 School of Population and Public Health, Faculty of Medicine, University of British Columbia, Vancouver, BC
Correspondence
Suggested citation
Aho J, Lybeck C, Tetteh A, Issa C, Kouyoumdjian F, Wong J, Anderson A, Popovic N. Rising syphilis rates in Canada, 2011–2020. Can Comm Dis Rep 2022;48(2/3):52–60. https://doi.org/10.14745/ccdr.v48i23a01
Keywords: infectious syphilis, congenital syphilis, surveillance, gbMSM, heterosexual females, pregnant individuals, Canada
Abstract
Background: Syphilis rates are of public health concern in Canada, with multiple jurisdictions reporting outbreaks over the past five years. The objective of this article is to describe trends in infectious and congenital syphilis in Canada 2011–2020.
Methods: Routine surveillance of syphilis is conducted through the Canadian Notifiable Disease Surveillance System (CNDSS). In response to rising rates of syphilis, all provinces and territories (P/Ts) have also submitted enhanced surveillance data on infectious syphilis to the Public Health Agency of Canada through the Syphilis Outbreak Investigation Coordinating Committee (SOICC) starting in 2018. Descriptive analyses of CNDSS and SOICC surveillance data 2011–2020 by age, sex, pregnancy status, male sexual orientation and P/Ts were performed.
Results: The national rate of infectious syphilis increased from 5.1 per 100,000 population in 2011 to 24.7 per 100,000 population in 2020.The rates increased in almost all P/Ts, with the Prairie provinces reporting the greatest relative increases from 2016 to 2020 (more than 400%). Rates in males were consistently higher than rates in females over the past 10 years; however, from 2016 to 2020, rates among females increased by 773%, compared with 73% among males. Although the proportion of cases who self-identify as gay, bisexual and other men who have sex with men decreased from 54% to 38% between 2018 and 2020, they still represent a high proportion of cases (according to data from eight P/Ts). From 2016 to 2020, rates of infectious syphilis increased in every age group, especially in females aged 15–39 years. Confirmed early congenital syphilis cases for 2020 increased considerably from prior years, with 50 cases reported in 2020, compared with 4 cases in 2016.
Conclusion: Infectious and congenital syphilis rates are a growing concern in Canada and the nature of the syphilis epidemics across Canada appears to be evolving, as evidenced by recent trends. More data and research are needed to better understand the drivers associated with the recent changes in the epidemiology of syphilis in Canada.
Introduction
Syphilis is the third most reported notifiable sexually transmitted infection in Canada, after chlamydia and gonorrhea. A bacterial infection caused by Treponema pallidum subspecies pallidum, syphilis is primarily transmitted through genital, anal/or oral sexual contact and can also be vertically transmitted to the fetus during pregnancy or to the neonate at delivery. Syphilis can easily and effectively be treated with penicillin, but left untreated it can progress through several different stages: primary; secondary; early latent; late latent; and tertiary syphilis. Syphilis is only infectious during the first three stages of infection (primary, secondary or early latent), which occur within the first year. Acute neurosyphilis can also develop during this time. At more advanced disease stages, syphilis can lead to serious health consequences such as neurological, cardiovascular or musculoskeletal complications. Congenital syphilis, which is syphilis transmitted in utero, can have severe debilitating effects and can lead to stillbirth or neonatal deathFootnote 1.
Following a long period of declining syphilis rates since the 1940s, Canada announced in 1998 a national goal of maintaining syphilis rates below 0.5 per 100,000 populationFootnote 2. In 2016, the World Health Organization released global targets for reducing the health impact of sexually transmitted infections by 2030, which included a 90% reduction in rates of syphilis globally and a threshold of 50 or fewer cases of congenital syphilis per 100,000 live births in 80% of countriesFootnote 3. The Government of Canada has endorsed these global targetsFootnote 4.
In Canada, rates of infectious syphilis started to increase steadily in the early 2000s, with substantial increases after 2017. Cases of congenital syphilis also increased during the same period. Ten Canadian jurisdictions have reported province and territory-wide or regional outbreaks in the past few yearsFootnote 1. In July 2019, in response to rising rates of syphilis across jurisdictions in Canada, the Public Health Agency of Canada (PHAC), in collaboration with all provinces and territories (P/Ts), established a federal, provincial and territorial Syphilis Outbreak Investigation Coordinating Committee (SOICC). The aim of SOICC is to share information on the epidemiology of syphilis and best practices and challenges on responses to rate increases. All P/Ts share enhanced surveillance data on confirmed infectious syphilis and confirmed early congenital syphilis case counts directly with PHAC as part of the activities of the SOICC.
In this article, we describe recent trends in infectious and congenital syphilis rates in Canada using surveillance data from 2011–2020.
Methods
Data sources
Since 1924, provincial and territorial health authorities have routinely provided data on laboratory-confirmed cases of syphilis to PHAC through the Canadian Notifiable Disease Surveillance System (CNDSS)Footnote 5. While all stages of syphilis are notifiable, only confirmed infectious cases and confirmed early congenital cases were included in our analysis. National case definitions of all syphilis stages as well as congenital syphilis can be found onlineFootnote 6.
Case variables submitted to CNDSS included sex, age at time of diagnosis, year of diagnosis and province or territory of diagnosis, while variables submitted to the SOICC also included male sexual orientation and pregnancy status. All P/Ts submitted data on sex, age and year of diagnosis to CNDSS and the SOICC. Newfoundland and Labrador's data were stratified by age and by sex but not by age and sex concurrently. Male sexual orientation and pregnancy data were reported consistently to the SOICC for 2018 to 2020 by British Columbia, Alberta, Saskatchewan, Ontario, New Brunswick, Nova Scotia, Yukon and the Northwest Territories. These eight P/Ts represented 72% of the Canadian population. Confirmed early congenital syphilis cases (less than two years after birth) did not include stillbirths.
Data for the years prior to the SOICC data collection (2011–2017) were extracted from CNDSS while data from 2018 to 2020 were collected via the SOICC. Twelve P/Ts submitted data for the full calendar year of 2020, and one province (Newfoundland and Labrador) provided partial counts for 2020; thus, annual counts for 2020 for this province were extrapolated.
Data analysis
Case counts, proportions and rates are presented overall and by sex, male sexual orientation, age group and P/T. Counts of cases of pregnant individuals are also presented. For reporting P/Ts, the proportion of missing data for sex and age did not exceed 1%, while it ranged from 0% to 18% for male sexual orientation and pregnancy data. The rates of confirmed infectious and confirmed early congenital syphilis were calculated using reported case counts as numerators and Statistics Canada population and live birth estimates, last updated in July 2020, as denominators. Reported rates were calculated per 100,000 population and included overall annual rates as well as sex, age group and P/T-specific rates. Descriptive analyses were performed using R version 4.0.2Footnote 7Footnote 8Footnote 9 and Microsoft Excel. Observed trends based on small numbers must be interpreted with caution, as rates based on small numbers are more prone to fluctuation over time.
Results
Since 2011, there has been a consistent increase in the number of confirmed infectious syphilis cases reported, except for a slight decline in 2020 (Figure 1). The highest increases were observed in 2018 and 2019 (50% and 45% yearly increases, respectively), corresponding to the highest numbers of cases and rates recorded in the last 10 years. There were an estimated 9,382 cases in 2020, corresponding to a rate of 24.7 per 100,000 population (Figure 1). This reflects a 385% increase in rates compared to the 2011 rate of 5.1 per 100,000 population.
Figure 1: Total number of cases and sex-specific rates of infectious syphilis in Canada by year, 2011–2020
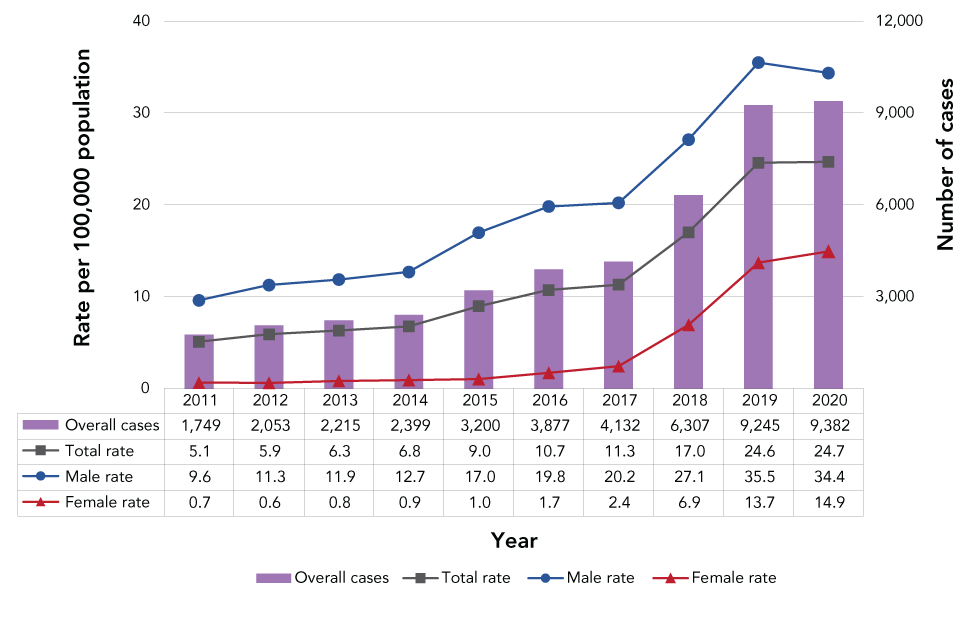
Text description: Figure 1
| Year | Total rate | Male rate | Female rate | Number of infectious syphilis cases |
|---|---|---|---|---|
| 2011 | 5.1 | 9.6 | 0.7 | 1,749 |
| 2012 | 5.9 | 11.3 | 0.6 | 2,053 |
| 2013 | 6.3 | 11.9 | 0.8 | 2,215 |
| 2014 | 6.8 | 12.7 | 0.9 | 2,399 |
| 2015 | 9.0 | 17.0 | 1.0 | 3,200 |
| 2016 | 10.7 | 19.8 | 1.7 | 3,877 |
| 2017 | 11.3 | 20.2 | 2.4 | 4,132 |
| 2018 | 17.0 | 27.1 | 6.9 | 6,307 |
| 2019 | 24.6 | 35.5 | 13.7 | 9,245 |
| 2020 | 24.7 | 34.4 | 14.9 | 9,382 |
Rates of infectious syphilis increased among males and females, but faster in females
In the past decade, the annual rate of infectious syphilis has consistently been higher in males, compared with females (Figure 1). Rates of infectious syphilis increased in both males and females over 2011–2020; however, the magnitude of the rise has been more pronounced in females, especially in the past five years. From 2016 to 2020, while rates increased by 73% in males, they increased by 773% in females. Nonetheless, in 2020, the rate in males remained higher compared with females at 34.4 per 100,000 population and 14.9 per 100,000, respectively.
The proportion of all infectious syphilis cases reported in females has also considerably increased. The national proportion of infectious syphilis cases among females was 6% in 2011 and remained under 10% until 2017. In 2019 and 2020, the proportion of all infectious syphilis cases reported among females was 28% and 30% respectively. In 2020, P/Ts with the highest proportions of female cases were Saskatchewan (51%), Manitoba (49%) and Alberta (43%). Although with low case counts (50 cases or fewer), Nunavut also reported a high proportion of female cases (60%). British Columbia, Ontario and Québec reported the lowest proportions of female cases in 2020 (less than or equal to 15%).
Proportion of infectious syphilis cases still highest among gay, bisexual and other men who have sex with men, but declining
The eight P/Ts that reported male sexual orientation accounted for 71% of all male cases reported in the country in 2020. Based on 2020 data provided by these P/Ts, 38% of all infectious syphilis cases were reported among gay, bisexual and other men who have sex with men (gbMSM), and 25% were reported among heterosexual males. In comparison, in 2018, the same eight P/Ts reported a proportion of 54% of cases identifying as gbMSM and 24% as heterosexual males.
Rates of infectious syphilis increased faster in young adults
Overall, rates of infectious syphilis have been increasing between 2011 and 2019 in almost all age group but remained relatively unchanged from 2019 to 2020 (Figure 2). The highest rate in 2020 was observed in those aged 25–29 years (69.8 per 100,000 population).
Figure 2: Rate of infectious syphilis in males and females per 100,000 by age group in Canada, 2011–2020Figure 2 Footnote aFigure 2 Footnote b
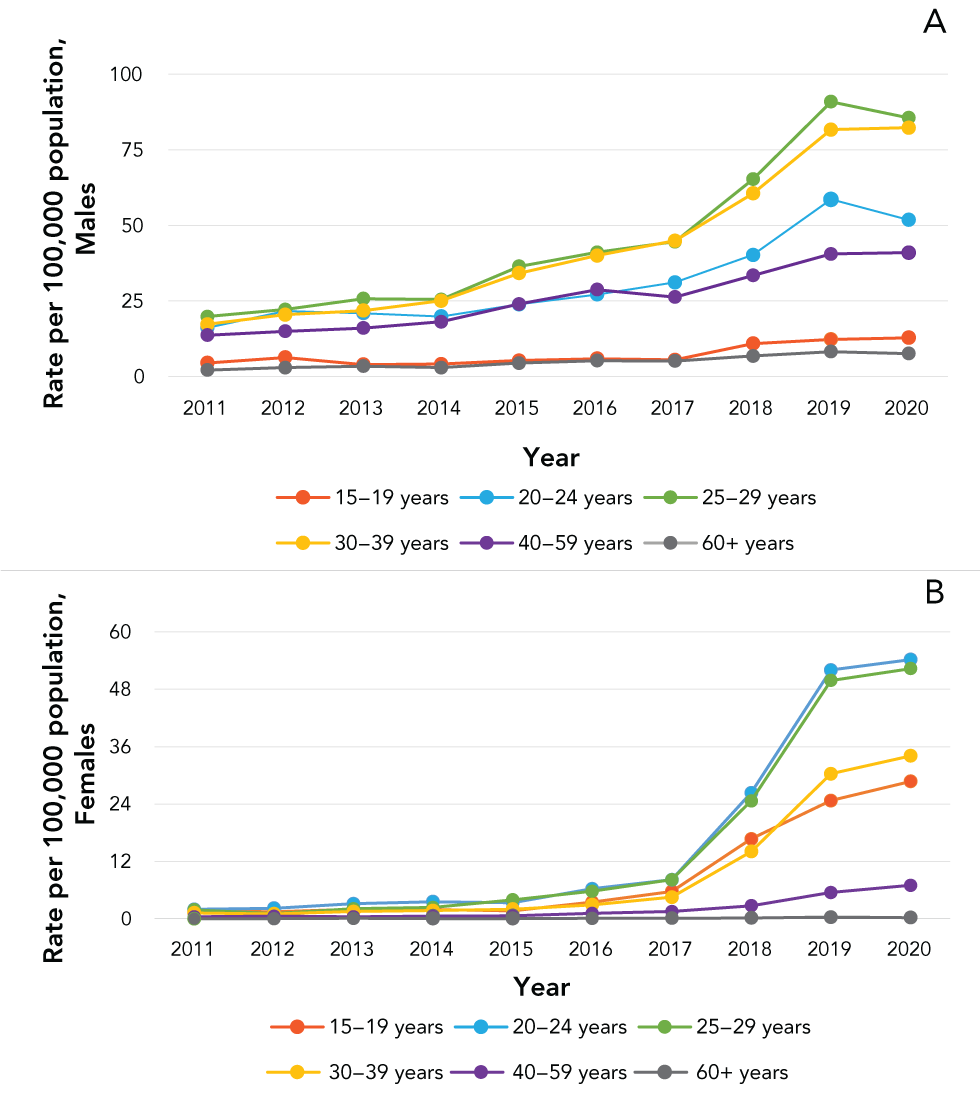
Text description: Figure 2
| Year | 15–19 years | 20–24 years | 25–29 years | 30–39 years | 40–59 years | 60+ years |
|---|---|---|---|---|---|---|
| 2011 | 4.5 | 16.1 | 19.8 | 17.3 | 13.6 | 2.1 |
| 2012 | 6.3 | 21.6 | 22.2 | 20.5 | 15.0 | 2.9 |
| 2013 | 4.0 | 20.9 | 25.7 | 21.8 | 16.0 | 3.4 |
| 2014 | 4.1 | 19.9 | 25.5 | 25.0 | 18.1 | 2.9 |
| 2015 | 5.3 | 23.9 | 36.4 | 34.2 | 24.0 | 4.4 |
| 2016 | 5.9 | 27.1 | 41.1 | 40.0 | 28.7 | 5.2 |
| 2017 | 5.5 | 31.1 | 44.6 | 44.9 | 26.3 | 5.1 |
| 2018 | 10.9 | 40.2 | 65.3 | 60.6 | 33.4 | 6.8 |
| 2019 | 12.3 | 58.6 | 90.9 | 81.6 | 40.5 | 8.2 |
| 2020 | 12.8 | 51.8 | 85.5 | 82.3 | 41.0 | 7.6 |
| Year | 15–19 years | 20–24 years | 25–29 years | 30–39 years | 40–59 years | 60+ years |
|---|---|---|---|---|---|---|
| 2011 | 1.7 | 2.0 | 1.9 | 1.2 | 0.4 | 0.0 |
| 2012 | 1.5 | 2.2 | 1.1 | 1.0 | 0.5 | 0.0 |
| 2013 | 2.0 | 3.1 | 2.1 | 1.5 | 0.4 | 0.1 |
| 2014 | 2.0 | 3.6 | 2.4 | 1.7 | 0.6 | 0.0 |
| 2015 | 1.7 | 3.4 | 3.9 | 2.0 | 0.6 | 0.0 |
| 2016 | 3.5 | 6.3 | 5.7 | 2.9 | 1.1 | 0.1 |
| 2017 | 5.7 | 8.2 | 8.2 | 4.5 | 1.5 | 0.1 |
| 2018 | 16.7 | 26.3 | 24.6 | 14.1 | 2.7 | 0.2 |
| 2019 | 24.7 | 52.0 | 49.8 | 30.3 | 5.5 | 0.4 |
| 2020 | 28.7 | 54.2 | 52.3 | 34.1 | 7.0 | 0.3 |
Rates among males were consistently highest in all years (2011–2020) in those aged 25–29 years (85.5 per 100,000 population in 2020), followed closely by those aged 30–39 years (82.3 per 100,000 population in 2020) (Figure 2A).
Rates of infectious syphilis in females were highest in younger age groups compared with their male counterparts (Figure 2B). Until 2017, there was a steady increase in rates of infectious syphilis in females, primarily in those aged 15–39 years. In 2018, rates in females in this age range tripled (increasing by over 200% from the previous year). In 2020, the highest rates of infectious syphilis in females were observed in those aged 20–24 years (54.2 per 100,000 population). Although only slightly higher than the rates observed in males (51.8 per 100,000 population), this is the first time in the period of interest (2011–2020) that female rates in this age group have surpassed males. The second highest rate of infectious syphilis among females was reported in females aged 25–29 years (52.3 per 100,000 population).
The proportion of all infectious syphilis cases that was reported in females aged 15–39 years has also increased rapidly. In 2011, 5.2% of all cases were reported in females aged 15–39 years, increasing five-fold to approximately a quarter (26%) of cases in 2020. From 2016 to 2020 (Figure 2B), an 858% increase in rates of infectious syphilis was observed in females aged 15–39 years. In 2020, females aged 15–39 represented 87% of all female cases.
Rates of infectious syphilis are increasing in almost all provinces and territories
In 2011, nine P/Ts reported cases of infectious syphilis, with rates ranging from 1.0 per 100,000 population in Newfoundland and Labrador to 7.8 per 100,000 population in Québec. Since then, there has been a steady rate increase in most P/Ts, with large increases observed in 2017 and 2018. From 2016 to 2020, the Prairie provinces reported the greatest relative increases (more than 400%). In most P/Ts, the highest rates of infectious syphilis reported in the last 10 years occurred in 2019. The P/Ts with the highest rates of infectious syphilis in 2019 were Nunavut (266.7 per 100,000 population), Manitoba (136.7 per 100,000 population), the Northwest Territories (97.7 per 100,000 population), Alberta (51.9 per 100,000 population) and Saskatchewan (33.7 per 100,000 population). Rates declined from 2019 to 2020 in Manitoba, the Northwest Territories and Nunavut but increased in Alberta and Saskatchewan (Figure 3).
Figure 3: Rates of reported infectious syphilis cases in Canada, by province and territory, 2020
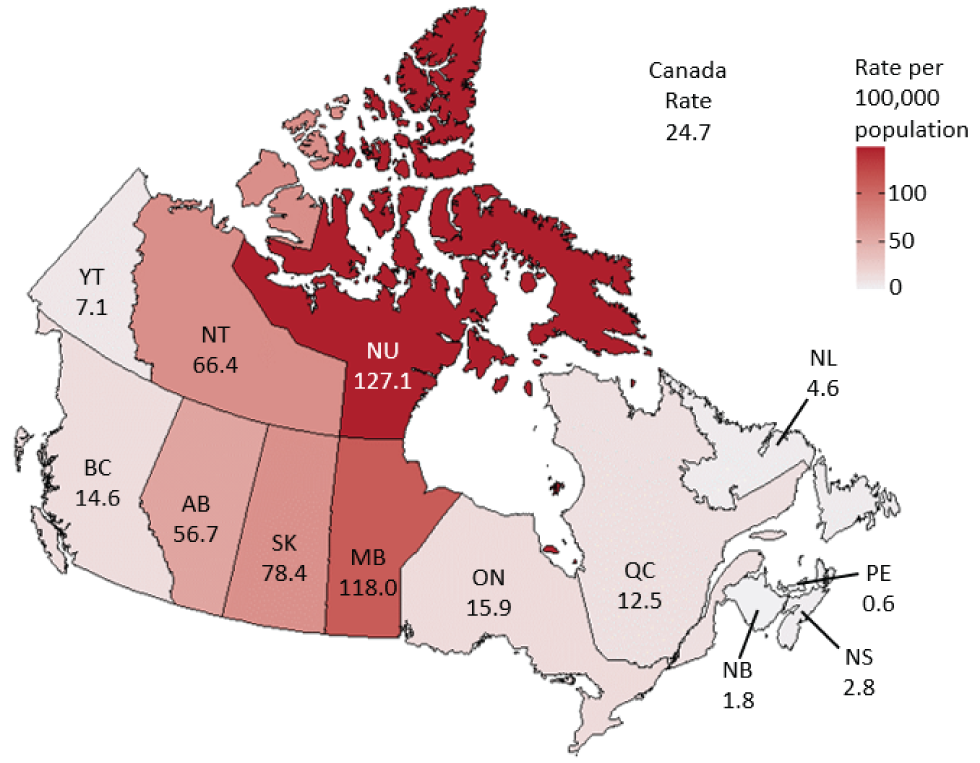
Text description: Figure 3
| Province/territory | Rate |
|---|---|
| BC | 14.6 |
| AB | 56.7 |
| SK | 78.4 |
| MB | 118.0 |
| ON | 15.9 |
| QC | 12.5 |
| NB | 1.8 |
| NS | 2.8 |
| NL | 4.6 |
| PE | 0.6 |
| YT | 7.1 |
| NT | 66.4 |
| NU | 127.1 |
| Canada | 24.7 |
Early congenital syphilis cases also on the rise
The reported number of confirmed early congenital syphilis cases has increased over the last 10 years in Canada (Figure 4). From 2011 to 2017, 10 or fewer cases of confirmed early congenital syphilis were observed per year. Reported cases of confirmed early congenital syphilis more than doubled between 2017 and 2018, from 7 cases in 2017 to 17 cases in 2018. In 2019 and 2020, total case counts increased to 53 and 50, respectively, corresponding to a rate of 14.2 per 100,000 live births in 2019 and 13.4 per 100,000 live births in 2020.
Figure 4: Number and rate of reported confirmed early congenital syphilis cases per 100,000 live births in Canada, 2011–2020
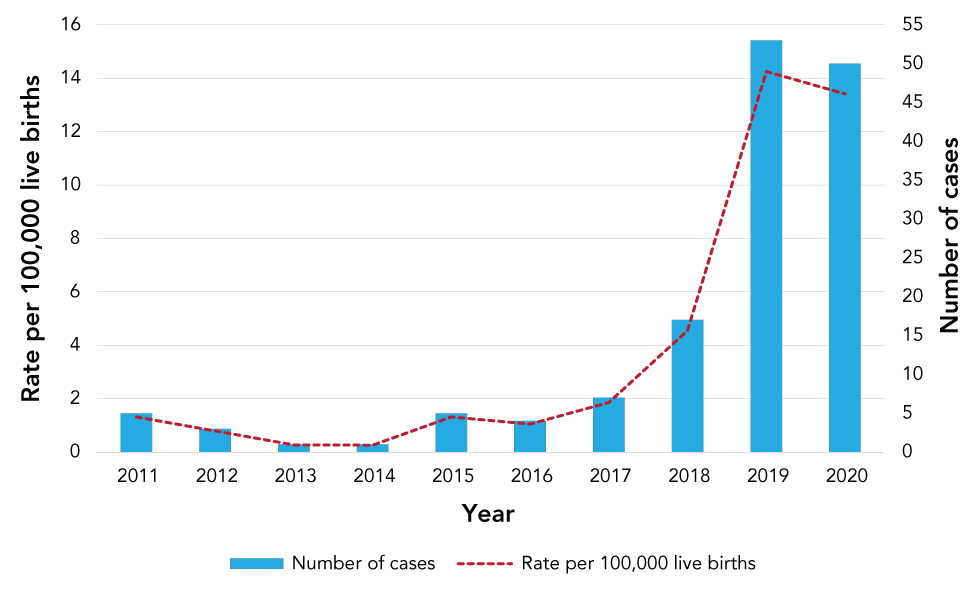
Text description: Figure 4
| Year | Number of cases | Rate per 100,000 live births |
|---|---|---|
| 2011 | 5 | 1.3 |
| 2012 | 3 | 0.8 |
| 2013 | 1 | 0.3 |
| 2014 | 1 | 0.3 |
| 2015 | 5 | 1.3 |
| 2016 | 4 | 1.0 |
| 2017 | 7 | 1.9 |
| 2018 | 17 | 4.5 |
| 2019 | 53 | 14.2 |
| 2020 | 50 | 13.4 |
In 2019, Alberta and Manitoba reported 79% of all confirmed early congenital syphilis cases in Canada, while other P/Ts reported three or fewer congenital cases. In 2020, the majority (86%) of all confirmed early congenital syphilis cases reported were observed in Alberta, Manitoba and Saskatchewan. These P/Ts also had the highest rates of infectious syphilis among females aged 15–39 years.
In the eight P/Ts that submitted data on pregnancy status, there were 230 cases of infectious syphilis reported among pregnant individuals in 2020. The same P/Ts reported 71 cases of infectious syphilis in pregnant individuals in 2018 and 133 cases in 2019.
Discussion
Rates of infectious syphilis in Canada have increased substantially in the past decade and especially since 2017. Similar to the United States (US), the United Kingdom and Australia, the majority of cases (based on partial data) in Canada have occurred among males, especially among gbMSMFootnote 10Footnote 11Footnote 12. However, while rates in Canada have remained higher among males than females, rates of infectious syphilis among females have risen quickly in recent years. Similar trends have also been observed in other countries. The US, the United Kingdom and Australia have all reported rising rates of infectious syphilis, with rates increasing more than 175% between 2015 and 2019, and rates in females increasing faster than in malesFootnote 10Footnote 11Footnote 12.
The reasons for the ongoing high rates of syphilis among males, and particularly among gbMSM, and the more recent increases among heterosexual populations, remain unclear as data on sexual behaviours and key populations are incomplete in national surveillance. Social and structural determinants of health and health inequities undoubtedly play a crucial role in the inequitable occurrence of syphilis across different populationsFootnote 1Footnote 13. These determinants include housing instability, experiences of violence, lack of access to culturally appropriate care, and experiences of stigma, discrimination and racism, particularly within the healthcare systemFootnote 1Footnote 14Footnote 15Footnote 16Footnote 17Footnote 18Footnote 19.
Available evidence from Canada and the US suggests that substance use may potentially help explain the recent trends in syphilis rates. Substance use, including opioids and crystal methamphetamine (“crystal meth”), has become more frequent in recent yearsFootnote 20Footnote 21Footnote 22Footnote 23. While the prevalence of crystal meth use is low overall in Canada (less than 1% of the general population and 11 times lower than in the US), its availability, use and related harms have dramatically increased since 2013Footnote 20. Crystal meth use can influence decision-making on safer sex practicesFootnote 24Footnote 25. Among gbMSM, chemsex, which is the use of substances (such as crystal meth) to prolong and intensify sexual experiences, has been described as a major trendFootnote 24Footnote 26Footnote 27. Among other behaviours, injection drug use and problematic alcohol use in gbMSM have been shown to increase the risk of syphilis and human immunodeficiency virus coinfectionFootnote 28Footnote 29Footnote 30. Crystal meth use was also reported in a heterosexual outbreak in Winnipeg in 2017–2018 and identified as a driver in 2019 during the syphilis outbreak in SaskatchewanFootnote 16Footnote 31. Recent data from the US similarly show associations between crystal meth and opioid use and syphilis outbreaks in heterosexual populationsFootnote 32Footnote 33Footnote 34.
In the last 10 years, females aged 15–39 years accounted for an average of 96% of live births in CanadaFootnote 35. From 2016 to 2020, an almost 10-fold increase in infectious syphilis cases (858%) was reported in females aged 15–39 years, with this group representing 87% of all female syphilis cases in 2020. The increase in infectious syphilis cases among this age cohort of females has led to subsequent increases in congenital syphilis in Canada. Record-high numbers of confirmed early congenital syphilis cases were reported in 2019 and 2020 (at least 50 cases in each year, compared with 10 or fewer cases up until 2017). This is the highest number of confirmed early congenital syphilis cases reported since congenital syphilis became reportable in 1993. The US also experienced a similar situation with 1,870 reported cases of congenital syphilis in 2019, a 291% increase from 2015Footnote 10. Females face unique challenges in early diagnosis due to anatomical or biological differences that may make primary lesions take longer to identifyFootnote 1. This may play a role in delaying early testing and access to care. It is worth noting that some jurisdictions have changed their clinical practice guidelines around prenatal screening over the past decade, to increase the frequency of testing for syphilis over the course of a pregnancyFootnote 36Footnote 37Footnote 38Footnote 39Footnote 40Footnote 41Footnote 42. This change in guidelines might have resulted in more consistent and more frequent screening for syphilis—and greater detection of cases—in pregnant individuals, and females of reproductive age in general, compared to males. In addition, US studies indicated that potential factors associated with increasing rates of syphilis during pregnancy and of congenital syphilis included lack of access to prenatal care and missed opportunities for timely and effective treatment of pregnant individualsFootnote 43Footnote 44.
Various structural barriers, including lower income, insecure housing and rural or remote residence, have been associated with syphilis infection, especially during pregnancyFootnote 1Footnote 36Footnote 45Footnote 46Footnote 47. In addition, systemic discrimination, racism and stigmatization in healthcare settings due to substance use may contribute to mistrust of healthcare systems and serve as barriers to care for individuals with syphilisFootnote 1Footnote 13Footnote 43Footnote 48Footnote 49. At least one province has anecdotally reported more frequent diagnoses of latent stages, indicating missed diagnoses at earlier stages of infection possibly linked to structural barriers to care. Rapid tests that can be performed at the site of patient care, such as point-of-care tests, may play an important role in the control of syphilis in remote or marginalized populationsFootnote 50Footnote 51. However, no point-of-care tests for syphilis diagnosis have been licensed in CanadaFootnote 1Footnote 52.
The rates of infectious syphilis reported in this article may underestimate true rates, as individuals living with the infection may not necessarily access health care or sexually transmitted and bloodborne infections (STBBI) services for testing. This underestimation may especially have occurred during the coronavirus disease 2019 (COVID-19) pandemic as a result of public health measures to control the pandemic limiting access to and provision of STBBI services. As the pandemic was declared in March 2020, the decreases observed in 2020 may not reflect the true incidence. An online survey conducted by PHAC in 2021 indicated that the COVID-19 pandemic has impacted STBBI detection and responseFootnote 53. The survey reported that the pandemic led to a decrease in demand for and the ability to deliver STBBI prevention, testing and treatment services but an increase in demand for harm-reduction and drug-treatment servicesFootnote 53. The impact of the pandemic on STBBI surveillance has also been reported in other countries, highlighting decreased screening and testing and limited resources, which resulted in underdiagnosis and underreportingFootnote 54Footnote 55Footnote 56.
Given the disruption in services and reports of increased substance use, the impact of the pandemic on the true incidence of syphilis is yet to be seen. This may be reflected in 2021 and 2022 national surveillance data depending on how the COVID-19 pandemic evolves and its related impact on STBBI screening and testingFootnote 53Footnote 57. It is important to note that there are limitations in the enhanced national surveillance system, such as incomplete data on variables such as male sexual orientation and substance use (the latter not presented in this article due to high levels of missing data), which are not collected systematically and consistently across jurisdictions. In addition, data collection and research on other social determinants of health including ethnicity and Indigeneity data would be instrumental in better understanding the epidemics, although data collection on ethno-cultural identity is still controversial. Nonetheless, there is a growing consensus, especially emerging from lessons learned during the COVID-19 pandemic, that disaggregated data are important to better describe epidemics and appropriately target interventionsFootnote 58Footnote 59Footnote 60.
Conclusion
This article provides a national picture of the syphilis epidemic in Canada over the past 10 years and discusses potential factors associated with the considerable recent increases in syphilis rates. Syphilis incidence has surged over time and the nature of epidemics across Canada appear to vary and evolve, with a persisting impact on gbMSM and an increasing number of outbreaks in heterosexual men and women. The number of congenital syphilis cases has also risen significantly. Greater understanding of the social, structural and behavioural factors affecting syphilis could help identify opportunities for interventions using a syndemic approach. More research is needed to understand the full extent of syphilis and its associated determinants in Canada. Such evidence could inform efforts to reduce the health impact of STBBI and to reach the World Health Organization's global target for reducing syphilis incidence by 2030.
Authors' statement
JA — Conceptualization, writing–original draft, writing–review and editing, supervision
CL — Data curation, validation, visualization, data analysis, literature review, writing–original draft, writing–review and editing
AT — Writing–original draft, literature review, writing–review and editing, validation
CI — Data collection and curation, validation, data analysis, literature review, writing–original draft, writing–review and editing
FK — Writing–review and editing
JW — Writing–review and editing
AA — Data collection, writing–review and editing
NP — Conceptualization, writing–review and editing
Competing interests
None.
Acknowledgements
The authors thank B Ephrem, G Gravel, M-A Leblanc, R Naraine, M Sabourin, S Sabourin, R Tsang and J Wu for their perspectives, advice, and edits while reviewing this manuscript. The authors are also grateful to S Thomas for contributing to the initial abstract, to J Sandhu for assisting with reference management, and to the Health Canada and Public Health Agency of Canada library team for assisting with the manuscript's literature search. Finally, we are grateful to all provinces and territories for their contributions to building the national portrait of enhanced surveillance data on syphilis in Canada from 2011–2020 and for their review of the manuscript.
Funding
This work was supported by the Public Health Agency of Canada.
