COVID-19 outbreak in Saskatchewan

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 48-4, April 2022: First Nations Health
Date published: April 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-4, April 2022: First Nations Health
Outbreak
Multijurisdictional outbreak of COVID-19 associated with a wake/funeral event in a northern Saskatchewan First Nations community
Nnamdi Ndubuka1, Sabyasachi Gupta1, Rim Zayed2, Brian Quinn2, Moliehi Khaketla2, Elaine Chan3, Kristyn Franklin4, Erin McGill4
Affiliations
1 Northern Inter-Tribal Health Authority Inc., Prince Albert, SK
2 Saskatchewan Health Authority, La Ronge, SK
3 Alberta Health (Public Health Officer placement), Edmonton, AB
4 Public Health Agency of Canada, Ottawa, ON
Correspondence
Suggested citation
Ndubuka N, Gupta S, Zayed R, Quinn B, Khaketla M, Chan E, Franklin K, McGill E. Multijurisdictional outbreak of COVID-19 associated with a wake/funeral event in a northern Saskatchewan First Nations community. Can Commun Dis Rep 2022;48(4):140–5. https://doi.org/10.14745/ccdr.v48i04a04
Keywords: COVID-19, SARS-CoV-2, outbreak, Indigenous community, mass gathering, funeral
Abstract
Background: Sixty-eight laboratory-confirmed cases of the coronavirus disease 2019 (COVID-19) (12 in Alberta [AB], 56 in Saskatchewan [SK]) were linked to a gathering at a hospital in Alberta on June 1–4, 2020, and a wake/funeral in a First Nations community in northern Saskatchewan on June 9–11, 2020.
Objective: The objectives were to provide a comprehensive description of the epidemiology of the outbreak and describe the chains of transmission to inform the hypothesis that there were multiple introductions of COVID-19 at the wake/funeral.
Methods: Case investigation and contact tracing was conducted by local public health in AB and SK. The Public Health Agency of Canada conducted a centralized case analysis. An epidemic curve and a Gantt chart for period of communicability were created to support or refute whether there had been multiple introductions of COVID-19 at the wake/funeral.
Results: Illness onset dates ranged from May 31 to July 1, 2020. Ages ranged from 2 to 80 years (median age=43 years). Five cases were hospitalized; there were no deaths. The available case exposure information supports the hypothesis that there had been multiple introductions of COVID-19 at the wake/funeral. Public health authorities in AB and SK declared the outbreak over on July 20, 2020; based on two incubation periods (i.e. 28 days) following the illness onset of the last primary case.
Conclusion: During multijurisdictional outbreaks, data sharing, coordination across health authorities and centralized analysis is essential to understanding the events that lead to the outbreak and possible hypotheses around chains of transmission.
Introduction
An outbreak of coronavirus disease 2019 (COVID-19) occurred in two Indigenous communities in northern Alberta (AB) and northern Saskatchewan (SK) in 2020. Sixteen individuals from AB and SK, including the index case (SK), visited a hospital in Edmonton, AB, on June 1–4. Nine of these individuals later travelled to an Indigenous community in northern Saskatchewan for a wake/funeral that was held on June 9–11. A large number of people attended the wake/funeral, including individuals from Indigenous communities in northern AB, where the deceased resided (whose death was unrelated to COVID-19). The index case and a household member hosted the wake indoors at their home on June 9–10. Public health measures, including physical distancing and masking, were not strictly observed at all times. The funeral ceremony took place in a church on June 11; 140 people attended these events.
The events on June 9–11 are refer to as "wake/funeral" because transmission and acquisition potentially occurred at either of these closely connected occasions and the investigation could not discern which of the 140 attendees came to which of the two events.
The objective of this report is to comprehensively describe the epidemiology of this COVID-19 outbreak using all cases and to describe the chains of transmission. It is important to highlight the value of collaborative interjurisdictional investigations in outbreaks; data sharing across jurisdictions can reveal associations that might not be uncovered during separate investigations.
Methods
Overview
Rapid point-of-care (POC) and polymerase chain reaction (PCR) testing are available to members of the northern Indigenous communities. Sufficient test kits are supplied to initiate testing for close contacts and exposed people, as the communities are remote. Samples are sent to the SK provincial laboratory for confirmation.
Saskatchewan public health was first alerted to an emerging outbreak when the index case was hospitalized on June 11, 2020. The individual was tested by rapid POC test on June 7, and the positive PCR test occurred on June 12. Saskatchewan public health launched its investigation and began contact tracing on June 11.
On June 11, Northern Inter-Tribal Health Authority (NITHA) public health in SK declared an outbreak of COVID-19 and launched an investigation. NITHA declared the outbreak over on July 20, 2020, based on two incubation periods (i.e. 28 days) following the illness onset of the last primary case.
Definitions
The definitions used during this outbreak investigation and in this report are as shown in Table 1.
| Item | Definition |
|---|---|
| Primary outbreak case |
|
| Secondary outbreak case |
|
| Outbreak setting/siteTable 1 footnote a |
|
| Close contactTable 1 footnote b | A person who had direct contact with a primary or secondary outbreak case during the case's period of communicability because they
|
| Incubation period | Up to 14 days from exposure to onset of symptoms. The maximum incubation period of 14 days is used as a proxy for the likely exposure period |
| Period of communicability | For symptomatic individuals: 2 days prior to onset of symptoms and 10 days post onset of symptoms or symptom resolution, whichever is longer For asymptomatic individuals: 2 days prior to specimen collection date and 10 days post specimen collection date |
The AB, SK and the Public Health Agency of Canada (PHAC) collaborated on the minimum set of data elements required to provide an epidemiological description of cases and describe the chains of transmission. Case-level line lists were shared with PHAC for centralized analysis. Data were received for 68 PCR-confirmed cases.
Investigations
Case investigation and contact tracing was conducted by public health nurses and trained case investigators from AB and SK using the standard COVID-19 case report form agreed upon by all provinces/territories in Canada. Most of the interviews were conducted in-person because reaching individuals by phone was difficult. Local Indigenous outreach workers helped with translation as needed. Community leaders, including the First Nations Chief and Council, worked closely with Indigenous Services Canada, Alberta Health, NITHA and Saskatchewan Health Authority throughout the investigation.
Alberta public health laboratory genetically sequenced the isolates and found the SARS-CoV-2 lineage to be identical for them all. Centralized genomic analysis comparing AB and SK isolates was not completed.
Epidemiologic and statistical analyses
Case demographics, including age, sex and severity of illness, were summarized. An epidemic curve was generated based on illness onset date (or earliest date based on the date sequence: onset date, specimen collection date and positive laboratory test result date).
A Gantt chart with the cases' periods of communicability was overlaid with exposure information. As specific linkages between cases based on case identifier were not available, it was not possible to produce a social network analysis.
Because the exposure information did not include date of attendance at the wake and funeral, we assumed that cases were present on all three days (June 9–11). Travel dates were not available; the assumption that AB cases were in SK on June 8–11 is based on information from AB.
Interventions
The First Nations community in northern SK imposed travel restrictions that permitted essential travel only. Curfew was in effect from 11 p.m. to 7 a.m. daily, and groceries and essential supplies were delivered to minimize travel. Local public health issued a precautionary health advisory, as the attendance list for these events were not available. Anyone in attendance at an outbreak setting/site was advised to immediately self-isolate and self-monitor for symptoms of COVID-19 for 14 days and to call community health centre for evaluation and direction. Local radio broadcast key messages translated into the local language. Local radio and social media promoted public health strategies, such as the use of nonmedical face masks, physical distancing, personal hygiene measures and participating in responsible gatherings.
NITHA and the Saskatchewan Health Authority established rapid POC and PCR door-to-door and drive-through testing options. Isolation trailers were made available to ensure adherence to isolation requirements. Public health detention orders and warning letters were issued to individuals not complying with the self-isolation requirement.
Contact tracing and mass testing were also conducted in the First Nations community in northern AB. Accommodations for isolation/quarantine were made available for individuals returning to AB from SK following the wake/funeral.
Investigation findings
Descriptive epidemiology
There were three settings where transmission may have occurred. The first setting was the hospital visit in AB (June 1–4); of the 16 visitors, 9 (AB=7, SK=2) later tested positive for COVID-19. Of the 9 hospital visitors who tested positive, 8 attended the wake and funeral.
The second and third settings were the wake/funeral in the northern Saskatchewan First Nations community (June 9–11). Of the 140 attendees, 44 (AB=11, SK=33) later tested positive, an attack rate of 31%.
In total, 68 PCR-confirmed cases of COVID-19, including secondary cases (AB=12, SK=56), were identified as part of this outbreak (Figure 1 and Table 2). A large proportion of cases (38%) remained asymptomatic throughout their period of communicability.
Figure 1: Epidemic curve of laboratory-confirmed SARS-CoV-2 cases by episode dateFigure 1 footnote a from two northern Indigenous communities linked to a wake/funeral in northern Saskatchewan, May 31 to July 20, 2020 (N=68)
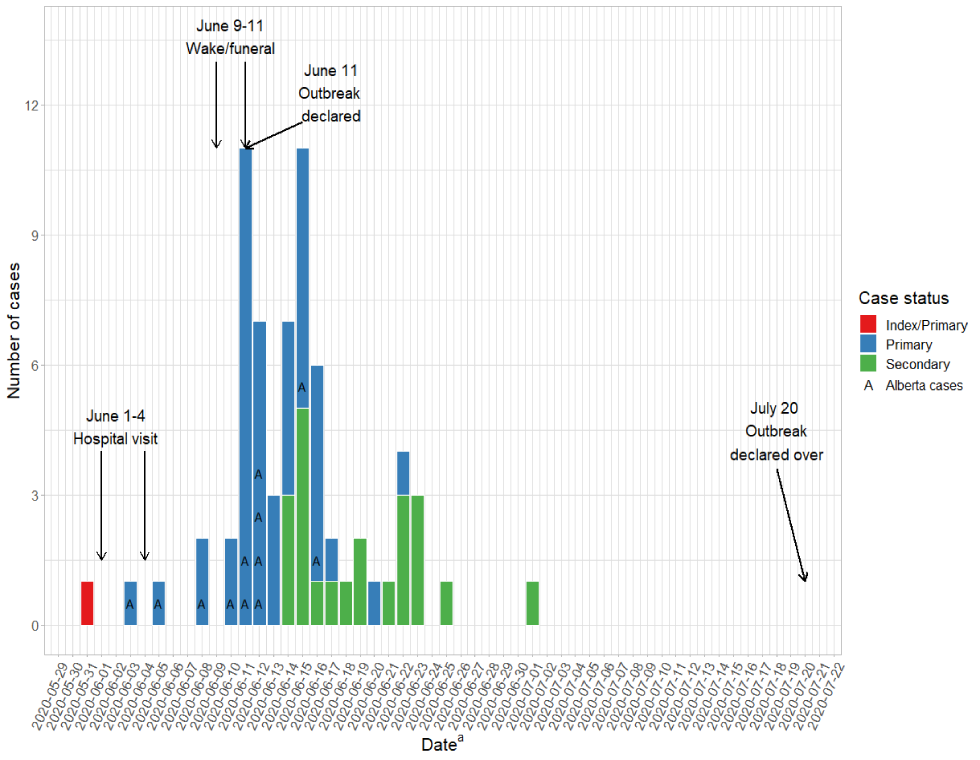
Text description: Figure 1
The graph shows the number of laboratory-confirmed COVID-19 cases linked to the wake/funeral outbreak from May 31 to July 20, 2020. Following the hospital visits between June 1–4, 2020, the number of cases increased until June 15, 2020, with case counts ranging from one to eleven. The majority of primary cases were identified between May 31 and June 16, 2020. Case counts decreased after June 15, 2020, and the outbreak was declared over on July 20, 2020.
| Characteristics | Description | Outcome |
|---|---|---|
| Breakdown by case status | Primary, n | 45 (AB=12, SK=33) |
| Secondary, n | 23 (SK) | |
| Episode dates | Earliest date (illness onset, positive specimen collection date or date of first positive test result) | May 31–July 1, 2020 |
| Demographics | Median age, years (range) | 43 (range: 2–80) |
| Female gender, n (%) | 34/68 (50%) | |
| Asymptomatic casesTable 1 footnote a | Cases that never developed symptoms, n | 26/68 (38%) |
| Case severity | Hospitalizations, n (% cases hospitalized) | 5 (7%) |
| ICU admissions, n (% hospitalizations admitted to ICU) | 1 (20%) | |
| Deaths, n | 0 | |
Ancillary analyses
The first transmission likely occurred in the hospital in AB. Nine cases (AB=7, SK=2) reported visiting the deceased (non-COVID-19-related death) in the hospital in AB between June 1 and June 4. During the visit, three of the cases were within their period of communicability and two were symptomatic (Figure 2). The two SK cases stayed together at a hotel in AB; one was the index case from SK. Seven of the AB cases reported close contact with the two individuals from SK.
Figure 2: Gantt chart of the period of communicability for all SARS-CoV-2 outbreak cases from two northern Indigenous communities linked to a wake/funeral in northern Saskatchewan, May 31 to July 20, 2020 (N=68)
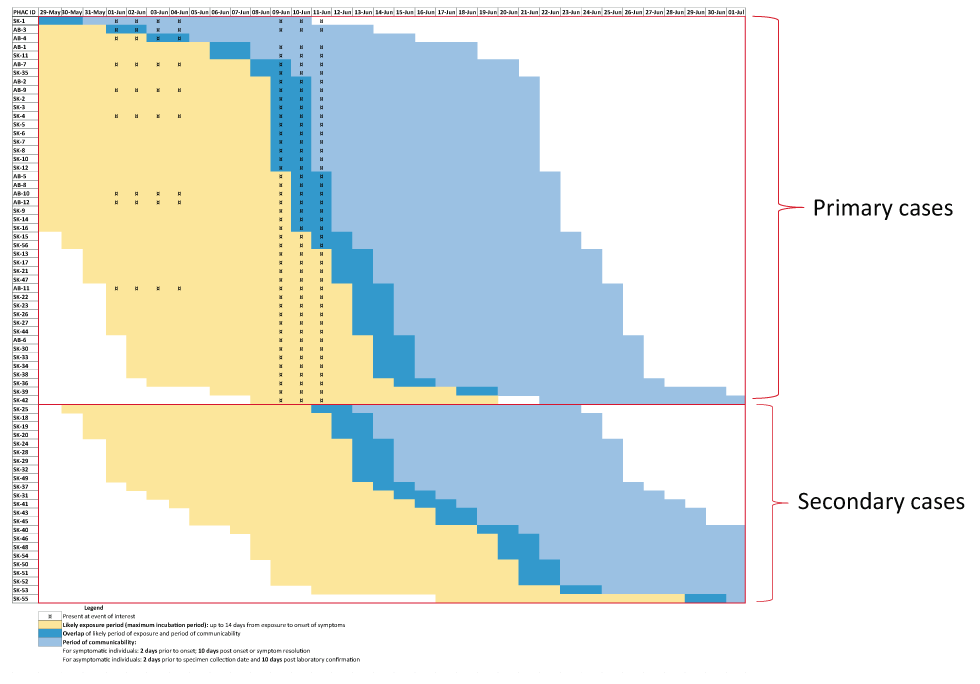
Text description: Figure 2
The Gantt chart illustrates cases, their case status and event attendance, over time (May 31-July 20, 2020). Attendance for the hospital and wake/funeral exposure events is noted for each case. The cases' exposure period, period of communicability and the overlap between likely period of exposure and period of communicability are denoted by colours and hatching. The figure shows the wave of cases that ensued following these transmission events and how inclusion of the hospital event is imperative to explaining the likely period of exposure among secondary cases.
On June 8, 12 AB cases travelled to SK for the wake/funeral in a convoy of six vehicles. Only one AB case (AB-4) did not attend any of the events in SK, because that person was ill, likely with COVID-19; however, that case was not tested until June 14.
The second and third most likely transmission settings were the wake/funeral in SK. Forty-four cases attended the wake/funeral and 26 were in their period of communicability (Figure 2). These 26 individuals may have all potentially infected others with COVID-19. Based on onset date, 9 individuals (AB=5, SK=4) may have been symptomatic during the wake/funeral; 5 had visited the hospital (Figure 2).
There were 23 secondary cases who reported close contact with a known case linked to one of the outbreak settings, although they were not present themselves.
Complications
Five cases were hospitalized and one was admitted to the intensive care unit (ICU). No deaths were associated with this outbreak (Table 2).
Discussion
Key results
The centralized analysis suggested that the hospital visit in AB was critical to transmission, as three individuals were in their period of communicability during the visit and close contact occurred between the AB and SK visitors. Furthermore, if the hospital event was excluded, a subset of the secondary outbreak cases identified could not be explained based on the likely period of exposure (the maximum incubation period of 14 days is used as a proxy for the likely exposure period) and the period of communicability for COVID-19Footnote 1.
The data supported the hypothesis of multiple introductions of COVID-19 at the wake/funeral. There were 26 individuals in their period of communicability and 9 may have been symptomatic based on onset date.
A large proportion of the cases remained asymptomatic throughout their period of communicability (38%). Also, a notable proportion of cases were asymptomatic when tested (n=16/68; 24%) but developed symptoms later, indicative of a rapid outbreak response.
Comparison
In Canada, there has been media coverage of COVID-19 outbreaks linked to funerals/memorial services and other mass gathering eventsFootnote 2Footnote 3Footnote 4.
South Africa reported that physical distancing (or "social distancing") guidelines are not always observed in many parts of the country, especially during funeralsFootnote 5. In the Eastern Cape Province, 80% of all cases were linked to burial ceremoniesFootnote 3. Cultural practices during burial ceremonies and lack of adherence to physical distancing protocols present an opportunity for transmissionFootnote 5. Jaja et al. recommend that, in order to reduce spread of COVID-19, religious and cultural activities should be restricted and only immediate family members be allowed to bury their loved onesFootnote 5.
Early in the pandemic, the United States identified a multifamily cluster linked to gatherings, including a funeralFootnote 6. An individual with mild respiratory symptoms, later confirmed as a case, attended the funeral and a meal with family members of the deceasedFootnote 6. The index case transmitted their infection to 10 other people, none of whom were household contactsFootnote 6. This funeral cluster occurred before physical distancing policies were implemented, and they support the recommendations to avoid gatherings and illustrate the importance of physical distancingFootnote 6.
Outbreak response
Outbreak response was timely; the outbreak was identified and the investigation launched on June 11, the day of the funeral. Public health employed multiple interventions, including imposing a curfew and travel restrictions to reduce the spread of COVID-19, both within the community and to surrounding communities, and supported the residents by bringing essential supplies into the community. The public health interventions were widely accessible—door-to-door or drive-through testing, messaging in the local languages and provision of isolation accommodations.
NITHA and Saskatchewan Health Authority have always benefited from a strong collaborative working relationship, and the organizations meet regularly to share information and discuss public health measures. Partnership with the Ministry of Health in Saskatchewan and PHAC, to coordinate with the Ministry of Health in Alberta, resulted in agreement on outbreak management, response and communication. Local, trusted or Indigenous nurses led the interviews and door-to-door initiatives to increase community uptake.
The investigation faced many challenges: the multijurisdictional nature of the outbreak, barriers to gathering data and contextual issues specific to the population.
Multiple public health organizations with different jurisdictions, including Indigenous population health needed to be involved to take into account that the cases lived in various geographic and administrative regions in two provinces. This required significant coordination. The pandemic response had put a strain on public health resources, making it difficult to find a convenient time for outbreak investigation partners to convene.
The lack of an attendance list for the wake/funeral made it difficult to notify individuals of their potential exposure. This has informed subsequent recommendations that event organizers maintain attendee lists for contact tracing.
There are many sensitivities related with sharing information between provinces and publicly about the affected Indigenous people. Trust issues remain between cases and investigators, including fear of stigma and/or discrimination, which made it difficult to obtain an accurate history. The transience of many community members added another layer of complexity. There were also cases who refused to isolate.
The investigation focused on forward contact tracing, and the role the hospital visits may have played in transmission was only identified during the centralized retrospective analysis. The subsequent outbreak investigation highlighted the value of backwards contact tracingFootnote 7.
Conclusion
The retrospective centralized analysis supported the hypothesis that there were multiple introductions of COVID-19 at the wake/funeral. As many as 26 attendees were in their period of communicability; 9 may have been symptomatic based on onset date at the time of the event. Public health measures including masking and physical distancing were not strictly adhered to during the wake, although people who dropped in to pay their respects at the funeral did wear masks (none of whom were cases). The attack rate for the wake/funeral was 31% (44/140), which emphasizes the importance of protective measures at gatherings. The outbreak investigation also illustrated the importance of centralized analysis for multijurisdictional outbreaks. Information sharing is essential when gathering the details required to understand the events leading up to an outbreak and the hypotheses around chains of transmission.
Authors' statement
- NM — Investigation, conceptualization, supervision, validation, writing–review & editing
- SG — Investigation, conceptualization, data curation, validation, writing–review & editing
- RZ — Investigation, conceptualization, data curation, validation, writing–review & editing
- BQ — Investigation, conceptualization, validation, writing–review & editing
- MK — Investigation, conceptualization, validation, writing–review & editing
- EC — Investigation, conceptualization, data curation, validation, writing–review & editing
- KF — Supervision, conceptualization, validation, writing–review & editing
- EM — Conceptualization, formal analysis, visualization, writing–original draft, writing–review & editing
Competing interests
None.
Acknowledgements
The authors gratefully acknowledge Northern Inter-Tribal Health Authority, Saskatchewan Health Authority and partner communities and colleagues from Alberta for their cooperation and contribution to this article.
Funding
The outbreak investigation did not receive research funding.
