COVID-19 and multisystem inflammatory syndrome in hospitalized children

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 49-4, April 2023: Children's Health and COVID-19
Date published: April 2023
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 49-4, April 2023: Children's Health and COVID-19
Overview
Resource use and disease severity of children hospitalized for COVID-19 versus multisystem inflammatory syndrome in children (MIS-C) in Canada
Daniel Farrar1, Charlotte Moore Hepburn2,3, Olivier Drouin4,5, Tala El Tal6, Marie-Paule Morin7, Roberta Berard8, Melanie King9, Melanie Laffin Thibodeau9, Krista Baerg10,11, Guillaume Beaudoin-Bussières12, Camille Beaufils7, Terri-Lyn Bennett13, Susanne Benseler14,15, Kevin Chan16,17,18, Claude Cyr19, Nagib Dahdah20, Elizabeth Donner16,21, Joanne Embree22,23, Catherine Farrell24, Andrés Finzi12, Sarah Forgie25,26, Ryan Giroux27, Kristopher Kang28, Bianca Lang29, Ronald Laxer6,16, Brian McCrindle30, Julia Orkin2,31, Jesse Papenburg32,33, Catherine Pound34, Victoria Price35, Jean-Phillippe Proulx-Gauthier36, Rupeena Purewal10,37, Manish Sadarangani28,38, Marina Salvadori13, Roseline Thibeault39, Karina Top40, Isabelle Viel-Thériault39, Elie Haddad7, Rosie Scuccimarri41, Rae Yeung6,42,43, Fatima Kakkar44, Shaun Morris1,16,45,46 on behalf of the Canadian Paediatric Surveillance Program COVID-19 Study Team
Affiliations
1 Centre for Global Child Health, The Hospital for Sick Children, Toronto, ON
2 Division of Paediatric Medicine, The Hospital for Sick Children, Toronto, ON
3 Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON
4 Division of General Paediatrics, Department of Paediatrics, CHU Sainte-Justine, Montréal, QC
5 Department of Social and Preventive Medicine, School of Public Health, Université de Montréal, Montréal, QC
6 Division of Rheumatology, Department of Paediatrics, The Hospital for Sick Children, University of Toronto, ON
7 Division of Paediatric Rheumatology-Immunology, CHU Sainte-Justine, Department of Paediatrics, University of Montreal, Montréal, QC
8 Division of Rheumatology, Department of Paediatrics, Children's Hospital at London Health Sciences Centre, London, ON
9 Canadian Paediatric Surveillance Program, Canadian Paediatric Society, Ottawa, ON
10 Department of Paediatrics, University of Saskatchewan, Saskatoon, SK
11 Division of General Paediatrics, Jim Pattison Children's Hospital, Saskatchewan Health Authority, Saskatoon, SK
12 Centre de Recherche du CHUM et Département de Microbiologie, Infectiologie et Immunologie, Université de Montréal, Montréal, QC
13 Public Health Agency of Canada, Ottawa, ON
14 Alberta Children's Hospital Research Institute, Cumming School of Medicine, University of Calgary, Calgary, AB
15 Division of Rheumatology, Department of Paediatrics, Alberta Children's Hospital, University of Calgary, Calgary, AB
16 Department of Paediatrics, Temerty Faculty of Medicine, University of Toronto, Toronto, ON
17 Department of Children's and Women's Health, Trillium Health Partners, Mississauga, ON
18 Institute for Better Health, Trillium Health Partners, Mississauga, ON
19 Service de Soins Intensifs Pédiatriques, Centre Hospitalier Universitaire de Sherbrooke, Sherbrooke, QC
20 Division of Paediatric Cardiology, CHU Sainte-Justine, Department of Paediatrics, University of Montréal, Montréal, QC
21 Division of Neurology, The Hospital for Sick Children, Toronto, ON
22 Department of Paediatrics and Child Health, University of Manitoba, Winnipeg, MB
23 Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB
24 Division of Paediatric Intensive Care, Department of Paediatrics, CHU Sainte-Justine, Montréal, QC
25 Division of Infectious Diseases, Department of Paediatrics, University of Alberta, Edmonton, AB
26 Stollery Children's Hospital, Edmonton, AB
27 Women's and Children's Health Program, St. Michael's Hospital, Unity Health Toronto, Toronto, ON
28 Department of Paediatrics, University of British Columbia, Vancouver, BC
29 Division of Rheumatology, Department of Paediatrics, Dalhousie University, Halifax, NS
30 The Labatt Family Heart Centre, The Hospital for Sick Children, Department of Paediatrics, University of Toronto, Toronto, ON
31 Child Health Evaluative Sciences, The Hospital for Sick Children, Toronto, ON
32 Division of Paediatric Infectious Diseases, Department of Paediatrics, Montreal Children's Hospital, Montréal, QC
33 Division of Microbiology, Department of Clinical Laboratory Medicine, McGill University Health Centre, Montréal, QC
34 Division of Consulting Paediatrics, Department of Paediatrics, Children's Hospital of Eastern Ontario, Ottawa, ON
35 Division of Paediatric Hematology/Oncology, Department of Paediatrics, Dalhousie University, Halifax, NS
36 Division of Paediatric Rheumatology, Department of Paediatrics, CHU de Québec-Université Laval, Québec City, QC
37 Division of Paediatric Infectious Diseases, Jim Pattison Children's Hospital, Saskatchewan Health Authority, Saskatoon, SK
38 Vaccine Evaluation Center, BC Children's Hospital Research Institute, Vancouver, BC
39 Division of Infectious Diseases, Department of Paediatrics, CHU de Québec-Université Laval, Québec City, QC
40 Department of Paediatrics, Dalhousie University, Halifax, NS
41 Division of Paediatric Rheumatology, Montreal Children's Hospital and McGill University Health Centre, Montréal, QC
42 Cell Biology Program, The Hospital for Sick Children, Toronto, ON
43 Department of Immunology and Institute of Medical Science, University of Toronto, Toronto, ON
44 Division of Infectious Diseases, CHU Sainte-Justine, Montréal, QC
45 Division of Infectious Diseases, The Hospital for Sick Children, Toronto, ON
46 Clinical Public Health, Dalla Lana School of Public Health, University of Toronto, Toronto, ON
Correspondence
Suggested citation
Farrar DS, Moore Hepburn C, Drouin O, El Tal T, Morin M-P, Berard RA, King M, Laffin Thibodeau M, Baerg K, Beaudoin-Bussières G, Beaufils C, Bennett T-L, Benseler SM, Chan K, Cyr C, Dahdah N, Donner EJ, Embree JE, Farrell C, Finzi A, Forgie S, Giroux R, Kang KT, Lang B, Laxer RM, McCrindle BW, Orkin J, Papenburg J, Pound CM, Price VE, Proulx-Gauthier J-P, Purewal R, Sadarangani M, Salvadori MI, Thibeault R, Top KA, Viel-Thériault I, Haddad E, Scuccimarri R, Yeung RSM, Kakkar F, Morris SK on behalf of the Canadian Paediatric Surveillance Program COVID-19 Study Team. Resource use and disease severity of children hospitalized for COVID-19 versus multisystem inflammatory syndrome in children (MIS-C) in Canada. Can Commun Dis Rep 2023;49(4):103–12. https://doi.org/10.14745/ccdr.v49i04a03
Keywords: COVID-19, intensive care, multisystem inflammatory syndrome in children, MIS-C, paediatrics, hospitalizations, resource use, surveillance, SARS-CoV-2
Abstract
Background: Direct comparisons of paediatric hospitalizations for acute coronavirus disease 2019 (COVID-19) and multisystem inflammatory syndrome in children (MIS-C) can inform health system planning. We describe the absolute and relative hospital burden of acute paediatric COVID-19 and MIS-C in Canada.
Methods: This national prospective study was conducted via the Canadian Paediatric Surveillance Program from March 2020–May 2021. Children younger than 18 years old and hospitalized for acute COVID-19 or MIS-C were included in the analysis. Outcomes included supplemental oxygen (low-flow oxygen or high-flow nasal cannula), ventilation (non-invasive or conventional mechanical), vasopressors, paediatric intensive care unit (PICU) admission, or death. Adjusted risk differences (aRD) and 95% confidence intervals (CI) were calculated to identify factors associated with each diagnosis.
Results: Overall, we identified 330 children hospitalized for acute COVID-19 (including five deaths) and 208 hospitalized for MIS-C (including zero deaths); PICU admission was required for 49.5% of MIS-C hospitalizations versus 18.2% of acute COVID-19 hospitalizations (aRD 20.3; 95% CI, 9.9–30.8). Resource use differed by age, with children younger than one year hospitalized more often for acute COVID-19 (aRD 43.4% versus MIS-C; 95% CI, 37.7–49.1) and more children 5–11 years hospitalized for MIS-C (aRD 38.9% vs. acute COVID-19; 95% CI, 31.0–46.9).
Conclusion: While there were more hospitalizations and deaths from acute paediatric COVID-19, MIS-C cases were more severe, requiring more intensive care and vasopressor support. Our findings suggest that both acute COVID-19 and MIS-C should be considered when assessing the overall burden of severe acute respiratory syndrome coronavirus 2 in hospitalized children.
Introduction
Along with hospitalization for acute coronavirus disease 2019 (COVID-19), multisystem inflammatory syndrome in children (MIS-C) has emerged as a serious yet infrequent complication of paediatric severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Though MIS-C was first described in the United Kingdom in April 2020, to date, few studies have directly compared characteristics and outcomes associated with these two diagnoses Footnote 1 Footnote 2 Footnote 3 Footnote 4. Case series describing MIS-C indicate higher proportions of severe disease relative to acute COVID-19, despite much lower incidence of MIS-C in the community, estimated at 316 cases per million SARS-CoV-2 infections among those younger than 21 years of age Footnote 5 Footnote 6 Footnote 7. Differences in the associated use of hospital resources (e.g. ventilation or hemodynamic support requiring intensive care) between these two disease entities are not well known and may have implications for future paediatric pandemic planning. We aimed to describe the absolute and relative hospital burden of acute paediatric COVID-19 infection and MIS-C during the first fifteen months of the pandemic in Canada, prior to the emergence of the Omicron variant and the approval of SARS-CoV-2 vaccines for use in children.
Methods
We conducted a national prospective study via the Canadian Paediatric Surveillance Program (CPSP) from March 2020–May 2021, during which time ancestral SARS-CoV-2 lineages and later the Alpha (B.1.1.7) variant of concern were dominant. The CPSP is a public health surveillance network that includes more than 2,800 paediatricians and paediatric subspecialists across Canada, who were surveyed weekly and asked to voluntarily report any incident cases to this study. In addition to the survey report, study co-investigators from 13 university health centres across Canada actively reported all cases from their institutions. Cases of children younger than 18 years of age and hospitalized with acute SARS-CoV-2 infection or paediatric inflammatory multisystem syndrome (PIMS) were eligible to be reported. While cases were reported based on a surveillance definition of PIMS, we applied a post-hoc case definition of MIS-C according to the World Health Organization Footnote 8. By definition, all patients with MIS-C had a documented linkage to SARS-CoV-2 (i.e. positive polymerase chain reaction, rapid antigen or serology test, or a close contact with microbiologically confirmed SARS-CoV-2). For all SARS-CoV-2 hospitalizations, the reporting physician indicated whether the hospitalization was due to acute COVID-19 or if incidental infection was identified upon routine screening; this was confirmed by dual case adjudication by the study team to ensure consistency. We therefore compared two mutually exclusive groups for this analysis: children hospitalized for acute COVID-19 versus children hospitalized for MIS-C. Further details regarding the study design are described elsewhere, and surveillance definitions are available Footnote 9 Footnote 10 Footnote 11.
Baseline characteristics and severity outcomes were ascertained for both case definitions using a standardized case report form. Severity outcomes included requirements for supplemental oxygen (either low-flow oxygen or high-flow nasal cannula), ventilation (either non-invasive, conventional mechanical or high-frequency oscillatory ventilation), vasopressors, paediatric intensive care unit (PICU) admissions or death. Characteristics were summarized using medians, interquartile ranges (IQR), frequencies and percentages. Frequencies between one and four were reported as "fewer than five" while some larger frequencies were presented as ranges to prevent back calculation, in accordance with CPSP privacy policy. Adjusted risk differences (aRD) were calculated to identify factors associated with each diagnosis, adjusting for age, sex, presence of one or more comorbid conditions, and the timing of hospitalization (classified in five three-month periods from March 2020–May 2021). Differences in continuous variables (i.e. age and PICU length of stay) were assessed using Wilcoxon rank-sum tests. The temporal lag (in weeks) between all Canadian SARS-CoV-2 case counts (ascertained from the Public Health Agency of Canada) Footnote 12 and hospitalizations reported to CPSP were assessed using Spearman's rank correlation coefficient. The p-values <0.05 were considered statistically significant. Analyses were conducted in Stata v17.0 Footnote 13.
Results
Overall, 330 children hospitalized for acute COVID-19 and 208 hospitalized for MIS-C were reported during the surveillance period (Figure 1, Table 1). The median age among acute COVID-19 patients (1.9 years; IQR 0.1–13.3) was significantly younger than those with MIS-C (8.1 years; IQR 4.2–11.6; p<0.001). More children younger than one year of age were hospitalized for acute COVID-19 than with MIS-C (aRD 43.4%; 95% CI, 37.7–49.1), while more children aged 5–11 years were hospitalized for MIS-C than acute COVID-19 (aRD 38.9%; 95% CI, 31.0–46.9). Chronic comorbid conditions were more common amongst acute COVID-19 patients (43.0% vs. 15.9% with MIS-C; aRD 38.0%; 95% CI, 31.0–45.1).
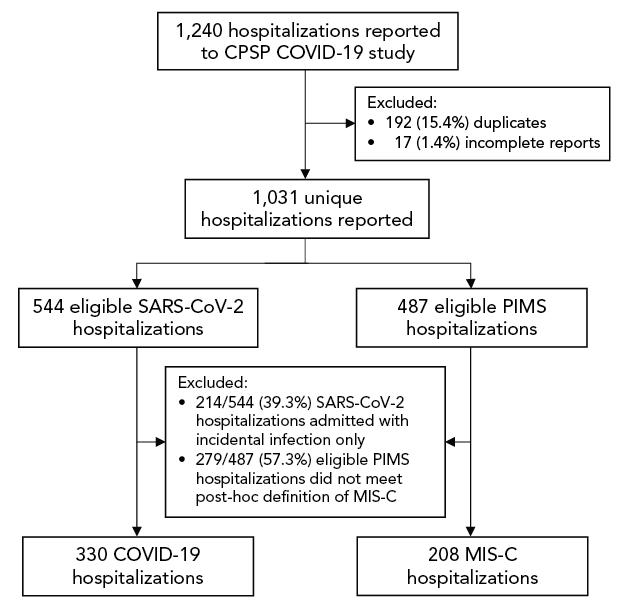
Figure 1 - Text description
The flowchart describes the flow of case reports submitted to the Canadian Paediatric Surveillance Program (CPSP) COVID-19 study, and how they were processed to reach the final analysis sample size. Overall, the CPSP COVID-19 study received 1,240 case reports of hospitalized children which were eligible to be analyzed in this study. Among these case reports, 192 (15.4%) duplicates and 17 (1.4%) incomplete reports were removed. Therefore, 1,031 unique hospitalizations with complete reports were reported and included 544 eligible hospitalizations of SARS-CoV-2 hospitalizations and 487 eligible hospitalizations of paediatric inflammatory multisystem syndrome (PIMS). From these subtotals, 214/544 (39.3%) SARS-CoV-2 hospitalizations were excluded because they were admitted with incidental infection only, while 279/487 (57.3%) PIMS hospitalizations were excluded because they did not meet the post hoc case definition of multisystem inflammatory syndrome in children (MIS-C). Therefore, the analysis included 330 COVID-19 hospitalizations and 208 MIS-C hospitalizations.
| Characteristic | Diagnosis | aRDFootnote a, % | 95% CI | p-value | |
|---|---|---|---|---|---|
| COVID-19 | MIS-C | ||||
| Total hospitalizations, NFootnote b | 330 | 208 | - | - | - |
| Age (years), median (IQR)Footnote c | 1.9 (0.1–13.3) | 8.1 (4.2–11.6) | - | - | <0.001 |
| Age (years), n (%) | |||||
| Younger than 1 | 140 (42.4) | 9 (4.3) | 43.4 | 37.7–49.1 | <0.001 |
| 1–4 | 68 (20.6) | 52 (25.0) | −2.9 | −10.4–4.6 | 0.45 |
| 5–11 | 30 (9.1) | 98 (47.1) | −38.9 | −46.9–−31.0 | <0.001 |
| 12–17 | 92 (27.9) | 49 (23.6) | −1.6 | −9.6–6.4 | 0.69 |
| Sex, n (%) | |||||
| Female | 145 (43.9) | 76 (36.5) | 6.2 | −4.9–17.3 | 0.27 |
| Male | 185 (56.1) | 132 (63.5) | −6.2 | −17.3–4.9 | 0.27 |
| Comorbid conditions, n (%)Footnote d | |||||
| None/unknown | 188 (57.0) | 175 (84.1) | −38.0 | −45.1–−31.0 | <0.001 |
| 1 or more | 142 (43.0) | 33 (15.9) | 38.0 | 31.0–45.1 | <0.001 |
| Population group, n (%) | |||||
| White | 75 (22.7) | 63 (30.3) | −12.4 | −22.8–−2.0 | 0.02 |
| South Asian | 40 (12.1) | 25 (12.0) | 1.4 | −6.0–8.7 | 0.71 |
| Arab/West Asian | 39 (11.8) | 16 (7.7) | 4.4 | −2.3–11.1 | 0.20 |
| Black | 39 (11.8) | 29 (13.9) | −2.2 | −9.5–5.1 | 0.56 |
| Indigenous | 28 (8.5) | 9 (4.3) | 4.8 | −0.6–10.3 | 0.08 |
| East/Southeast Asian | 18 (5.5) | 12 (5.8) | 3.0 | −2.2–8.1 | 0.26 |
| Latin American | 5 (1.5) | 18 (8.7) | −7.5 | −13.3–−1.7 | 0.01 |
| Unknown | 92 (27.9) | 49 (23.6) | - | - | - |
|
|||||
The PICU admission was required for 49.5% of MIS-C hospitalizations versus 18.2% of acute COVID-19 hospitalizations (aRD 20.3; 95% CI 9.9–30.8), though the proportion of children younger than five years of age admitted to PICU was similar (19.7% vs. 15.4%; Table 2). The median length of PICU stay was one day greater for acute COVID-19 (four days; IQR 2–7) than MIS-C (three days; IQR 2–4; p=0.04). Vasopressor use was more common for MIS-C than acute COVID-19 at all ages (35.6% vs. 2.4%; aRD 23.1%; 95% CI, 15.8–30.4). The proportion of all patients requiring supplemental oxygen and mechanical ventilation were similar (24.6% and 10.9% for acute COVID-19 vs. 30.3% and 9.6% for MIS-C, respectively). Five deaths due to acute COVID-19 were reported versus zero due to MIS-C.
| OutcomeFootnote a | Diagnosis | aRDFootnote b, % | 95% CI | p-value | |
|---|---|---|---|---|---|
| COVID-19 | MIS-C | ||||
| All hospitalizations | |||||
| Supplemental oxygen | 81/330 (24.6) | 63/208 (30.3) | −5.6 | −15.2–3.9 | 0.25 |
| Ventilation | 36/330 (10.9) | 20/208 (9.6) | 1.7 | −4.9–8.2 | 0.62 |
| Vasopressors | 8/330 (2.4) | 74/208 (35.6) | −23.1 | −30.4–−15.8 | <0.001 |
| PICU admission | 60/330 (18.2) | 103/208 (49.5) | −20.3 | −30.8–−9.9 | <0.001 |
| PICU length of stay (days) | 4 (2–7 days) | 3 (2–4 days) | - | - | 0.04 |
| ECMO | 0/330 (0.0) | 0/208 (0.0) | - | - | - |
| Death | 5/330 (1.5) | 0/208 (0.0) | - | - | - |
| Age younger than 5 years | |||||
| Supplemental oxygen | 36/208 (17.3) | 10/61 (16.4) | −0.1 | −13.0–12.6 | 0.98 |
| Ventilation | 18–21/208 (8.7–10.1)Footnote c | Fewer than 5/61 (fewer than 8.2) |
12.8 | 7.0–18.5 | <0.001 |
| Vasopressors | 5–7/208 (2.4–3.4)Footnote c | 8/61 (13.1) | −4.7 | −12.1–2.6 | 0.21 |
| PICU admission | 32/208 (15.4) | 12/61 (19.7) | 2.5 | −8.8–13.8 | 0.66 |
| PICU length of stay (days) | 4 (2–6 days) | 3 (1–3 days) | - | - | 0.02 |
| Age 5–11 years | |||||
| Supplemental oxygen | 8/30 (26.7) | 37/98 (37.8) | −12.9 | −35.0–9.3 | 0.25 |
| Ventilation | Fewer than 5/30 (fewer than 16.7) |
7–10/98 (7.1–10.2)Footnote c | −9.8 | −18.5–−1.1 | 0.03 |
| Vasopressors | 0/30 (0.0) | 42/98 (42.9) | - | - | - |
| PICU admission | 7/30 (23.3) | 61/98 (62.2) | −34.5 | −57.7–−11.3 | 0.004 |
| PICU length of stay (days) | 2 (1–9 days) | 3 (2–4 days) | - | - | 0.68 |
| Age 12–17 years | |||||
| Supplemental oxygen | 37/92 (40.2) | 16/49 (32.7) | −9.2 | −27.2–8.9 | 0.32 |
| Ventilation | 11–14/92 (12.0–15.2)Footnote c | 6–9/49 (12.2–18.4)Footnote c | −6.9 | −25.1–11.3 | 0.46 |
| Vasopressors | Fewer than 5/92 (fewer than 5.4) |
24/49 (49.0) | −43.5 | −63.3–−23.8 | <0.001 |
| PICU admission | 21/92 (22.8) | 30/49 (61.2) | −38.1 | −57.2–−19.0 | <0.001 |
| PICU length of stay (days) | 6 (3–8 days) | 4 (2–5 days) | - | - | 0.11 |
|
|||||
Acute paediatric COVID-19 hospitalization trends lagged behind all Canadian SARS-CoV-2 infection waves by one week (Spearman's ρ=0.89), versus a lag of six weeks for MIS-C hospitalizations (Spearman's ρ=0.82; Figure 2).
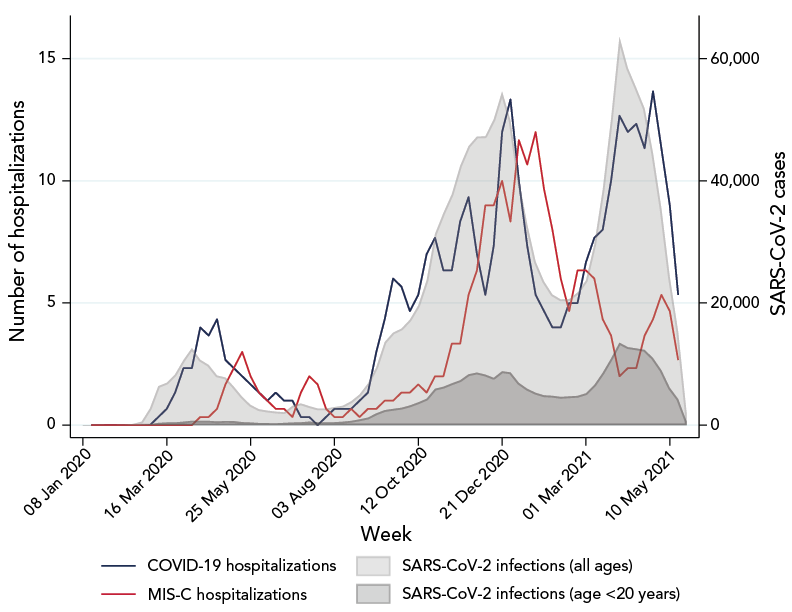
Figure 2 - Text description
The graph shows the number of COVID-19 and MIS-C hospitalizations among children younger than 18 years old by calendar week, as included in this study. These data are presented as three-week moving averages of the number of weekly hospitalizations. These data are then overlayed with the number of SARS-CoV-2 infections across Canada, separately amongst all ages and then amongst ages younger than 20 years, as publicly reported by the Public Health Agency of Canada. The x-axis ranges from January 8, 2020 to May 31, 2021, using calendar week units. The number of hospitalizations and infections in January and February 2020 all begin at or near zero, and thereafter increase gradually, reaching a first peak in spring 2020. Specifically, SARS-CoV-2 infections peaked at 12,609 weekly infections during the week of April 6, COVID-19 hospitalizations peaked at 4.3 average weekly hospitalizations during the week of April 27, and MIS-C hospitalizations peaked at 3.0 average weekly hospitalizations during the week of May 18. The number of infections and hospitalizations again begin to increase in fall 2020 and increase to a peak of 54,608 SARS-CoV-2 infections the week of December 21, a peak of 13.3 average COVID-19 hospitalizations the week of December 28, and a peak of 12.0 average MIS-C hospitalizations the week of January 18, 2021. After a steep decline in infections and hospitalizations in early 2021, SARS-CoV-2 infections and COVID-19 hospitalizations increase again. Specifically, SARS-CoV-2 infections peaked at 63,517 weekly infections during the week of March 29 and COVID-19 hospitalizations peaked at 13.7 average weekly hospitalizations during the week of April 26. MIS-C hospitalizations do not increase as quickly during this wave of the pandemic. Trends in SARS-CoV-2 infections among people younger than 20 years follow the same temporal pattern as all SARS-CoV-2 infections.
Discussion
Understanding the severity and associated in-hospital resource use required to manage acute paediatric COVID-19 and MIS-C is necessary to anticipate acute health system needs, and to make informed decisions regarding preventative measures including SARS-CoV-2 vaccination. Based on national surveillance data from March 2020 to May 2021, acute COVID-19 was found to have resulted in more paediatric hospitalizations and deaths and longer PICU stays, while MIS-C resulted in more PICU admissions and more frequent need for hemodynamic support. In this study, half of hospitalized MIS-C patients required intensive care, consistent with prior studies from the United Kingdom (44%) and the United States (64%) during the first year of the pandemic Footnote 14 Footnote 15. While PICU admissions among MIS-C patients were often initiated due to shock, these patients were likely stabilized rapidly with immune modulation and vasopressor support. This may explain the shorter PICU stays relative to patients with acute COVID-19, who typically require PICU admission due to respiratory distress and/or exacerbation of chronic comorbid conditions (e.g. neurologic or respiratory disease). The higher vasopressor and intensive care requirements for MIS-C, with similar rates of respiratory support requirements, are consistent with multiple United States studies Footnote 2 Footnote 16. A small number of acute COVID-19-related deaths were reported versus no MIS-C-related deaths, in part due to complications from chronic comorbid conditions among children with severe COVID-19 Footnote 17.
Despite comparable absolute rates of overall in-hospital resource use, there were important age differences in disease severity and the ensuing strategies used to support these patients. Infants (i.e. younger than one year old) rarely required hospitalization for MIS-C, presenting with lower rates of shock, coagulopathy and myocarditis relative to older children Footnote 11 Footnote 18. Conversely, infants were the most commonly hospitalized age group for acute COVID-19, in part due to the routine practice of admitting febrile infants for investigations and empiric treatment Footnote 19. Meanwhile, the requirement for hemodynamic support among children five years of age and older with MIS-C (43–49%) likely led to the high proportion of PICU admission among this age group relative to acute COVID-19, in keeping with other published literature Footnote 3.
While our study period ended prior to dominance of the Delta and Omicron lineages, these and future SARS-CoV-2 lineages may affect the relative in-hospital burden of acute COVID-19 infection and MIS-C. Studies from Denmark and Israel have found the incidence of MIS-C during Omicron waves fell to one tenth that of prior waves, after accounting for vaccination status Footnote 20 Footnote 21. Declines in the proportion of MIS-C patients admitted to PICU have also been observed (e.g. 61% during pre-Delta waves to 52% during the Delta wave in the United States Footnote 22; 49% during Delta waves to 21% during Omicron waves in Israel Footnote 21), though this may also reflect increased physician knowledge of MIS-C and refinement of supportive and treatment strategies. Uptake of paediatric and adolescent SARS-CoV-2 vaccines may also alter the relative in-hospital burden of disease, having shown effectiveness against both severe COVID-19 and MIS-C Footnote 23 Footnote 24.
Limitations
There are several limitations to this study. First, the voluntary nature of CPSP reporting means that not all paediatric hospitalizations in Canada were identified. The number of hospitalizations reported in this study may therefore differ from provincial reports, which use administrative data. Moreover, the limited availability of molecular and serologic testing during the early pandemic likely resulted in some cases failing to meet the case definition of MIS-C. Data were also collected prior to emergence of the Delta and Omicron variants, and before implementation of paediatric and adolescent SARS-CoV-2 vaccine programs. The PICU admission criteria may have differed by age, centre and diagnosis. Nevertheless, this study provided a unique opportunity to compare children hospitalized for acute COVID-19 infection and MIS-C using data ascertained with the same surveillance methods, timeframe and patient population, with physician case review to ensure all reported cases met the case definitions.
Conclusion
Our findings suggest that both acute COVID-19 and MIS-C need to be considered when assessing the overall burden of SARS-CoV-2 in hospitalized children, and have implications for future pandemic planning with respect to hospital resource use. Given the high proportion of children requiring PICU support for MIS-C, in tandem with the limited number of specialized hospital beds, it is clear these resources need to be anticipated for future pandemic waves. Moreover, given the low overall rates of vaccination among children younger than 12 years of age Footnote 25, awareness of disease severity from both acute COVID-19 and MIS-C may inform parents and policymakers in their decision-making regarding paediatric vaccines.
Authors' statement
DSF — Conceptualization, methodology, validation, formal analysis, investigation, data curation, writing (original draft)
CMH — Conceptualization, methodology, validation, investigation, writing (review & editing), supervision, funding acquisition
OD — Investigation, writing (review & editing)
TET — Investigation, writing (review & editing)
MPM — Investigation, writing (review & editing)
RAB — Investigation, writing (review & editing)
MK — Validation, investigation, data curation, writing (review & editing)
MLT — Methodology, validation, investigation, data curation, writing (review & editing), project administration
KB — Investigation, writing (review & editing)
GBB — Investigation, writing (review & editing)
CB — Investigation, writing (review & editing)
TLB — Investigation, writing (review & editing)
SMB — Investigation, writing (review & editing)
KC — Investigation, writing (review & editing)
CC — Investigation, writing (review & editing)
ND — Investigation, writing (review & editing)
EJD — Investigation, writing (review & editing)
JEE — Investigation, writing (review & editing)
CF — Investigation, writing (review & editing)
AF — Investigation, writing (review & editing)
SF — Investigation, writing (review & editing)
RG — Investigation, writing (review & editing)
KTK — Investigation, writing (review & editing)
BL — Investigation, writing (review & editing)
RML — Investigation, writing (review & editing)
BWM — Investigation, writing (review & editing)
JO — Investigation, writing (review & editing)
JP — Investigation, writing (review & editing)
CMP — Investigation, writing (review & editing)
VEP — Investigation, writing (review & editing)
JPPG — Investigation, writing (review & editing)
RP — Investigation, writing (review & editing)
MS — Investigation, writing (review & editing)
MIS — Investigation, writing (review & editing)
RP — Investigation, writing (review & editing)
KAT — Investigation, writing (review & editing)
IVT — Investigation, writing (review & editing)
EH — Conceptualization, investigation, writing (review & editing), supervision
RS — Conceptualization, investigation, writing (review & editing), supervision
RSMY — Conceptualization, investigation, writing (review & editing), supervision
FK — Conceptualization, methodology, investigation, writing (review & editing), supervision
SKM — Conceptualization, methodology, investigation, writing (review & editing), supervision
CPSP COVID-19 Study Team — Investigation, writing (review & editing)
F Kakkar and S Morris were co-senior authors.
Competing interests
CMH is the Director of Children's Mental Health of Ontario, and the Director of Medical Affairs for the Canadian Paediatric Society and Canadian Paediatric Surveillance Program. MPM has received consulting fees from Sobin and Abbvie and payment for expert testimony from the Canadian Medical Protective Association. RAB has received honoraria and participated in advisory boards with SOBI, Roche, Amgen, and AbbVie. KB served as Past President of the Community Paediatrics Section of the Canadian Paediatric Society and has received royalties from Brush Education. TLB is an employee of the Public Health Agency of Canada (PHAC). KC is Chair of the Acute Care Committee of the Canadian Paediatric Society and is past-president of the Emergency Medicine Section of the Canadian Paediatric Society. EJD is Chair of the Scientific Research Committee and a director of Epilepsy Canada. She is also a member of Partners Against Mortality in Epilepsy and the advisory boards of Cardiol, Pendopharm and Stoke Therapeutics. CF is Chair of the Scientific Steering Committee for the Canadian Paediatric Surveillance Program, former Chair of the Specialty Committee in Paediatrics of the Royal College of Physicians and Surgeons of Canada, former president of the Canadian Paediatric Society, and member of the Executive as Secretary of the Canadian Critical Care Society. She has received reimbursement for travel expenses from Canadian Paediatric Society and the Royal College of Physicians and Surgeons of Canada. She has also received an honorarium for a presentation at a continuing education conference from the Université de Sherbrooke. SF is the President of the Association of Medical Microbiology and Infectious Disease Canada and has received consulting fees from Toronto Metropolitan University. RML has received honoraria for serving as a consultant to Sobi, Novartis, Sanofi, and Eli Lilly, as chair for data monitoring committees for Eli Lilly and Novartis, and from the Canadian Rheumatology Association. JP has received consultant fees from AbbVie, honoraria from AbbVie, AstraZeneca and Seegene, and he received respiratory virus testing materials from Seegene for his institution. He has participated in ad hoc advisory board meetings for AbbVie and Merck and is a voting member of the National Advisory Committee on Immunization. RP is a consultant for Verity Pharmaceuticals. MS is supported via salary awards from the BC Children's Hospital Foundation and the Michael Smith Foundation for Health Research and has been an investigator on projects funded by GlaxoSmithKline, Merck, Moderna, Pfizer, Sanofi-Pasteur, Seqirus, Symvivo and VBI Vaccines. All funds have been paid to his institute, and he has not received any personal payments. MIS is an employee of the Public Health Agency of Canada. EH has participated in advisory board meetings of CSL-Behring and Takeda, data safety monitoring boards of Rocket Pharmaceutical and Jasper Therapeutics, and has patent applications with Immugenia and Immune Biosolutions. RS has received honoraria and served on an advisory board and as a consultant with Novartis, honoraria from Canadian Rheumatology Association, is a board member for Rheumatology for All, and her institution receives funding from Bristol Myers Squibb for a patient registry for which she is Principal Investigator. RSMY has received grant funding from CFI, CIHR, Genome Canada, PHAC and the COVID-19 Immunity Task Force, and The Arthritis Society; is a member of the Science and Industry Advisory Committee at Genome Canada and Medical Advisory Board at Kawasaki Disease Canada; and a member of a data safety monitoring board for a study on IL-1 inhibitors for Kawasaki Disease. FK has received honoraria for presentations given to the Association des Pédiatres du Québec and receives CMV testing kits from Altona Diagnostics. SKM has received honoraria for lectures from GlaxoSmithKline, was a member of ad hoc advisory boards for Pfizer Canada and Sanofi Pasteur, and is an investigator on an investigator led grant from Pfizer. DSF, OD, TET, MK, and MLT have no conflicts of interest to report.
Funding
Financial support for the Canadian Paediatric Surveillance Program (CPSP) was received from the Public Health Agency of Canada (PHAC). The CPSP is governed by an independent Scientific Steering Committee (SSC) comprised of individuals from both the Canadian Paediatric Society and PHAC. Members of the SSC reviewed and approved the study design. Individuals from PHAC, CPS, and the SSC participated in interpretation of the data. The final report was provided to PHAC for review, though the study team maintained scientific independence and authors were under no obligation to accept or incorporate changes to the manuscript.
References
- Footnote 1
-
Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020;395(10237):1607–8. https://doi.org/10.1016/S0140-6736(20)31094-1
- Footnote 2
-
Feldstein LR, Tenforde MW, Friedman KG, Newhams M, Rose EB, Dapul H, Soma VL, Maddux AB, Mourani PM, Bowens C, Maamari M, Hall MW, Riggs BJ, Giuliano JS Jr, Singh AR, Li S, Kong M, Schuster JE, McLaughlin GE, Schwartz SP, Walker TC, Loftis LL, Hobbs CV, Halasa NB, Doymaz S, Babbitt CJ, Hume JR, Gertz SJ, Irby K, Clouser KN, Cvijanovich NZ, Bradford TT, Smith LS, Heidemann SM, Zackai SP, Wellnitz K, Nofziger RA, Horwitz SM, Carroll RW, Rowan CM, Tarquinio KM, Mack EH, Fitzgerald JC, Coates BM, Jackson AM, Young CC, Son MB, Patel MM, Newburger JW, Randolph AG; Overcoming COVID-19 Investigators. Characteristics and Outcomes of US Children and Adolescents With Multisystem Inflammatory Syndrome in Children (MIS-C) Compared With Severe Acute COVID-19. JAMA 2021;325(11):1074–87. https://doi.org/10.1001/jama.2021.2091
- Footnote 3
-
Martin B, DeWitt PE, Russell S, Anand A, Bradwell KR, Bremer C, Gabriel D, Girvin AT, Hajagos JG, McMurry JA, Neumann AJ, Pfaff ER, Walden A, Wooldridge JT, Yoo YJ, Saltz J, Gersing KR, Chute CG, Haendel MA, Moffitt R, Bennett TD. Characteristics, Outcomes, and Severity Risk Factors Associated With SARS-CoV-2 Infection Among Children in the US National COVID Cohort Collaborative. JAMA Netw Open 2022;5(2):e2143151. https://doi.org/10.1001/jamanetworkopen.2021.43151
- Footnote 4
-
Godfred-Cato S, Abrams JY, Balachandran N, Jaggi P, Jones K, Rostad CA, Lu AT, Fan L, Jabbar A, Anderson EJ, Kao CM, Hunstad DA, Rosenberg RB, Zafferani MJ, Ede KC, Ballan W, Laham FR, Beltran Y, Bryant B, Meng L, Hammett TA, Oster ME, Bamrah Morris S, Belay ED. Distinguishing Multisystem Inflammatory Syndrome in Children From COVID-19, Kawasaki Disease and Toxic Shock Syndrome. Pediatr Infect Dis J 2022;41(4):315–23. https://doi.org/10.1097/INF.0000000000003449
- Footnote 5
-
Hoste L, Van Paemel R, Haerynck F. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur J Pediatr 2021;180(7):2019–34. https://doi.org/10.1007/s00431-021-03993-5
- Footnote 6
-
Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, Gupta A. Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation. Paediatr Respir Rev 2021;38:51–7. https://doi.org/10.1016/j.prrv.2020.08.001
- Footnote 7
-
Payne AB, Gilani Z, Godfred-Cato S, Belay ED, Feldstein LR, Patel MM, Randolph AG, Newhams M, Thomas D, Magleby R, Hsu K, Burns M, Dufort E, Maxted A, Pietrowski M, Longenberger A, Bidol S, Henderson J, Sosa L, Edmundson A, Tobin-D'Angelo M, Edison L, Heidemann S, Singh AR, Giuliano JS Jr, Kleinman LC, Tarquinio KM, Walsh RF, Fitzgerald JC, Clouser KN, Gertz SJ, Carroll RW, Carroll CL, Hoots BE, Reed C, Dahlgren FS, Oster ME, Pierce TJ, Curns AT, Langley GE, Campbell AP, Balachandran N, Murray TS, Burkholder C, Brancard T, Lifshitz J, Leach D, Charpie I, Tice C, Coffin SE, Perella D, Jones K, Marohn KL, Yager PH, Fernandes ND, Flori HR, Koncicki ML, Walker KS, Di Pentima MC, Li S, Horwitz SM, Gaur S, Coffey DC, Harwayne-Gidansky I, Hymes SR, Thomas NJ, Ackerman KG, Cholette JM; MIS-C Incidence Authorship Group. Incidence of Multisystem Inflammatory Syndrome in Children Among US Persons Infected With SARS-CoV-2. JAMA Netw Open 2021;4(6):e2116420. https://doi.org/10.1001/jamanetworkopen.2021.16420
- Footnote 8
-
World Health Organization. Multisystem inflammatory syndrome in children and adolescents with COVID-19: Scientific Brief. Geneva (CH): WHO; 2020. [Accessed 2021 May 3]. https://www.who.int/publications/i/item/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19
- Footnote 9
-
Drouin O, Hepburn CM, Farrar DS, Baerg K, Chan K, Cyr C, Donner EJ, Embree JE, Farrell C, Forgie S, Giroux R, Kang KT, King M, Laffin M, Luu TM, Orkin J, Papenburg J, Pound CM, Price VE, Purewal R, Sadarangani M, Salvadori MI, Top KA, Viel-Thériault I, Kakkar F, Morris SK; Canadian Paediatric Surveillance Program COVID-19 Study Team. Characteristics of children admitted to hospital with acute SARS-CoV-2 infection in Canada in 2020. CMAJ 2021;193(38):E1483–93. https://doi.org/10.1503/cmaj.210053
- Footnote 10
-
Farrar DS, Drouin O, Moore Hepburn C, Baerg K, Chan K, Cyr C, Donner EJ, Embree JE, Farrell C, Forgie S, Giroux R, Kang KT, King M, Laffin Thibodeau M, Orkin J, Ouldali N, Papenburg J, Pound CM, Price VE, Proulx-Gauthier JP, Purewal R, Ricci C, Sadarangani M, Salvadori MI, Thibeault R, Top KA, Viel-Thériault I, Kakkar F, Morris SK. Risk factors for severe COVID-19 in hospitalized children in Canada: A national prospective study from March 2020-May 2021. Lancet Reg Health Am 2022;15:100337. https://doi.org/10.1016/j.lana.2022.100337
- Footnote 11
-
El Tal T, Morin MP, Morris SK, Farrar DS, Berard RA, Kakkar F, Moore Hepburn C, Baerg K, Beaufils C, Bennett T-L, Benseler SM, Beaudoin-Bussieres G, Chan K, Cyr C, Dahdah N, Donner EJ, Drouin O, Edjoc R, Eljaouhari M, Embree JE, Farrell C, Finzi A, Forgie S, Giroux R, Kang KT, King M, Laffin Thibodeau M, Lang B, Laxer RM, Luu TM, McCrindle BW, Orkin J, Papenburg J, Pound CM, Price VE, Proulx Gautier J-P, Purewal R, Sadarangani M, Salvadori MI, Thibeault R, Top KA, Viel-Theriault I, Haddad E, Scuccimarri R, Yeung RSM. Epidemiology and role of SARS-CoV-2 Linkage in Paediatric Inflammatory Multisystem Syndrome (PIMS): A Canadian Paediatric Surveillance Program National Prospective Study. medRxiv 2022.05.27.22275613. https://doi.org/10.1101/2022.05.27.22275613
- Footnote 12
-
Public Health Agency of Canada. COVID-19 epidemiology update: Key updates. Ottawa, ON: PHAC; 2023. https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html
- Footnote 13
-
StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC; 2021. https://www.stata.com/
- Footnote 14
-
Flood J, Shingleton J, Bennett E, Walker B, Amin-Chowdhury Z, Oligbu G, Avis J, Lynn RM, Davis P, Bharucha T, Pain CE, Jyothish D, Whittaker E, Dwarakanathan B, Wood R, Williams C, Swann O, Semple MG, Ramsay ME, Jones CE, Ramanan AV, Gent N, Ladhani SN. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS): Prospective, national surveillance, United Kingdom and Ireland, 2020. Lancet Reg Health Eur 2021;3:100075. https://doi.org/10.1016/j.lanepe.2021.100075
- Footnote 15
-
Godfred-Cato S, Bryant B, Leung J, Oster ME, Conklin L, Abrams J, Roguski K, Wallace B, Prezzato E, Koumans EH, Lee EH, Geevarughese A, Lash MK, Reilly KH, Pulver WP, Thomas D, Feder KA, Hsu KK, Plipat N, Richardson G, Reid H, Lim S, Schmitz A, Pierce T, Hrapcak S, Datta D, Morris SB, Clarke K, Belay E; California MIS-C Response Team. COVID-19-Associated Multisystem Inflammatory Syndrome in Children - United States, March-July 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1074–80. https://doi.org/10.15585/mmwr.mm6932e2
- Footnote 16
-
Tripathi S, Gist KM, Bjornstad EC, Kashyap R, Boman K, Chiotos K, Gharpure VP, Dapul H, Sayed IA, Kuehne J, Heneghan JA, Gupta M, Khandhar PB, Menon S, Gupta N, Kumar VK, Retford L, Zimmerman J, Bhalala US; Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group. Coronavirus Disease 2019-Associated PICU Admissions: A Report From the Society of Critical Care Medicine Discovery Network Viral Infection and Respiratory Illness Universal Study Registry. Pediatr Crit Care Med 2021;22(7):603–15. https://doi.org/10.1097/PCC.0000000000002760
- Footnote 17
-
McCormick DW, Richardson LC, Young PR, Viens LJ, Gould CV, Kimball A, Pindyck T, Rosenblum HG, Siegel DA, Vu QM, Komatsu K, Venkat H, Openshaw JJ, Kawasaki B, Siniscalchi AJ, Gumke M, Leapley A, Tobin-D'Angelo M, Kauerauf J, Reid H, White K, Ahmed FS, Richardson G, Hand J, Kirkey K, Larson L, Byers P, Garcia A, Ojo M, Zamcheck A, Lash MK, Lee EH, Reilly KH, Wilson E, de Fijter S, Naqvi OH, Harduar-Morano L, Burch AK, Lewis A, Kolsin J, Pont SJ, Barbeau B, Bixler D, Reagan-Steiner S, Koumans EH; Pediatric Mortality Investigation Team. Deaths in Children and Adolescents Associated With COVID-19 and MIS-C in the United States. Pediatrics 2021;148(5):e2021052273. https://doi.org/10.1542/peds.2021-052273
- Footnote 18
-
Godfred-Cato S, Tsang CA, Giovanni J, Abrams J, Oster ME, Lee EH, Lash MK, Le Marchand C, Liu CY, Newhouse CN, Richardson G, Murray MT, Lim S, Haupt TE, Hartley A, Sosa LE, Ngamsnga K, Garcia A, Datta D, Belay ED. Multisystem Inflammatory Syndrome in Infants <12 months of Age, United States, May 2020-January 2021. Pediatr Infect Dis J 2021;40(7):601–5. https://doi.org/10.1097/INF.0000000000003149
- Footnote 19
-
Burstein B, Gravel J, Aronson PL, Neuman MI; Pediatric Emergency Research Canada (PERC). Emergency department and inpatient clinical decision tools for the management of febrile young infants among tertiary paediatric centres across Canada. Paediatr Child Health 2019;24(3):e142–54. https://doi.org/10.1093/pch/pxy126
- Footnote 20
-
Holm M, Espenhain L, Glenthøj J, Schmidt LS, Nordly SB, Hartling UB, Nygaard U. Risk and Phenotype of Multisystem Inflammatory Syndrome in Vaccinated and Unvaccinated Danish Children Before and During the Omicron Wave. JAMA Pediatr 2022;176(8):821–3. https://doi.org/10.1001/jamapediatrics.2022.2206
- Footnote 21
-
Levy N, Koppel JH, Kaplan O, Yechiam H, Shahar-Nissan K, Cohen NK, Shavit I. Severity and Incidence of Multisystem Inflammatory Syndrome in Children During 3 SARS-CoV-2 Pandemic Waves in Israel. JAMA 2022;327(24):2452–4. https://doi.org/10.1001/jama.2022.8025
- Footnote 22
-
Miller AD, Yousaf AR, Bornstein E, Wu MJ, Lindsey K, Melgar M, Oster ME, Zambrano LD, Campbell AP. Multisystem Inflammatory Syndrome in Children During Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Delta and Omicron Variant Circulation-United States, July 2021-January 2022. Clin Infect Dis 2022;75 Suppl 2:S303–7. https://doi.org/10.1093/cid/ciac471
- Footnote 23
-
Olson SM, Newhams MM, Halasa NB, Price AM, Boom JA, Sahni LC, Irby K, Walker TC, Schwartz SP, Pannaraj PS, Maddux AB, Bradford TT, Nofziger RA, Boutselis BJ, Cullimore ML, Mack EH, Schuster JE, Gertz SJ, Cvijanovich NZ, Kong M, Cameron MA, Staat MA, Levy ER, Chatani BM, Chiotos K, Zambrano LD, Campbell AP, Patel MM, Randolph AG; Overcoming COVID-19 Investigators. Effectiveness of Pfizer-BioNTech mRNA Vaccination Against COVID-19 Hospitalization Among Persons Aged 12-18 Years - United States, June-September 2021. MMWR Morb Mortal Wkly Rep 2021;70(42):1483–8. https://doi.org/10.15585/mmwr.mm7042e1
- Footnote 24
-
Zambrano LD, Newhams MM, Olson SM, Halasa NB, Price AM, Boom JA, Sahni LC, Kamidani S, Tarquinio KM, Maddux AB, Heidemann SM, Bhumbra SS, Bline KE, Nofziger RA, Hobbs CV, Bradford TT, Cvijanovich NZ, Irby K, Mack EH, Cullimore ML, Pannaraj PS, Kong M, Walker TC, Gertz SJ, Michelson KN, Cameron MA, Chiotos K, Maamari M, Schuster JE, Orzel AO, Patel MM, Campbell AP, Randolph AG; Overcoming COVID-19 Investigators. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA Vaccination Against Multisystem Inflammatory Syndrome in Children Among Persons Aged 12-18 Years - United States, July-December 2021. MMWR Morb Mortal Wkly Rep 2022;71(2):52–8. https://doi.org/10.15585/mmwr.mm7102e1
- Footnote 25
-
Public Health Agency of Canada. Canadian COVID-19 vaccination in Canada. Vaccination coverage. Ottawa, ON: PHAC; 2022. https://health-infobase.canada.ca/covid-19/vaccination-coverage/
