COVID-19 outbreak trends in Canada, 2021

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 49-4, April 2023: Children's Health and COVID-19
Date published: April 2023
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 49-4, April 2023: Children's Health and COVID-19
Surveillance
COVID-19 outbreak trends in Canada, 2021
Demy Dam1, Erin McGill1, Anna Bellos1, Cameron Coulby1, Jonathan Edwin1, Rachel McCormick1, Kaitlin Patterson1
Affiliation
1 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
Correspondence
Suggested citation
Dam D, McGill E, Bellos A, Coulby C, Edwin J, McCormick R, Patterson K. COVID-19 outbreak trends in Canada, 2021. Can Commun Dis Rep 2023;49(4):133–44. https://doi.org/10.14745/ccdr.v49i04a06
Keywords: COVID-19, Canada, outbreak, surveillance, outbreak trends, SARS-CoV-2 transmission, public health, respiratory virus
Abstract
Background: In January 2021, the Public Health Agency of Canada launched an outbreak surveillance system, the Canadian COVID-19 Outbreak Surveillance System (CCOSS), with the goal of monitoring incidence and severity of coronavirus disease 2019 (COVID-19) outbreaks across various community settings and complementing case surveillance.
Methods: Seven provinces were included in this report; these provinces submitted weekly cumulative COVID-19 outbreak line lists to CCOSS in 2021. Data includes administrative variables (e.g. date outbreak declared, date outbreak declared over, outbreak identifier), 24 outbreak settings, and number of confirmed cases and outcomes (hospitalization, death). Descriptive analyses for COVID-19 outbreaks across Canada from January 3, 2021, to January 1, 2022, were performed examining trends over time, severity, and outbreak size.
Results: Incidence of outbreaks followed similar trends to case incidence. Outbreaks were most common in school and childcare settings (39%) and industrial/agricultural settings (21%). Outbreak size ranged from 2 to 639 cases per outbreak; the median size was four cases per outbreak. Correctional facilities had the largest median outbreak size with 18 cases per outbreak, followed by long-term care facilities with 10 cases per outbreak. During periods of high case incidence, outbreaks may be under-ascertained due to limited public health capacity, or reporting may be biased towards high-risk settings prioritized for testing. Outbreaks reported to CCOSS were dominated by jurisdictions with the largest populations.
Conclusion: The trends illustrate that COVID-19 outbreaks in 2021 were reported most frequently in community settings such as schools; however, the largest outbreaks occurred in congregate living settings. The information gathered from outbreak surveillance complemented case incidence trends and furthered understanding of COVID-19 in Canada.
Introduction
Context
On January 25, 2020, the first severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was detected in Canada Footnote 1. The World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19), the disease caused by SARS-CoV-2 infection, a pandemic on March 11, 2020 Footnote 2 and COVID-19 rapidly spread across Canada with many cases and deaths associated with outbreak events Footnote 3 Footnote 4. Outbreaks can result in many infections over a short period of time, which has the potential to rapidly increase community transmission through secondary exposures and strain healthcare services Footnote 4.
The Public Health Agency of Canada (PHAC) determined that outbreak surveillance could provide additional data on the COVID-19 epidemic in Canada to help guide the public health response; as a result, PHAC created the Canadian COVID-19 Outbreak Surveillance System (CCOSS) following consultations with provincial and territorial partners. In January 2021, CCOSS launched with seven provinces contributing data: British Columbia (BC), Alberta (AB), Manitoba (MB), Ontario (ON), Québec (QC), Nova Scotia (NS) and Prince Edward Island (PE). These provinces represent 93% of the Canadian population Footnote 5. The remaining Canadian provinces and territories indicated their support for national outbreak surveillance but were unable to participate at that time. Ongoing efforts are underway to integrate interested partners.
Outbreak surveillance has not been commonly conducted for established pathogens at the national level. Very few countries, such as Ireland and the United Kingdom, reported trends on COVID-19 outbreaks Footnote 6 Footnote 7. The implementation of an event-based surveillance system to capture COVID-19 outbreak trends in Canada is novel and different from existing event-based surveillance systems in its timeliness and the level of detail captured.
Objectives
Systematic monitoring of COVID-19 outbreak trends allows for the improved understanding of settings and populations most at risk of experiencing outbreaks and of the relative impact of outbreaks on the burden of COVID-19 in Canada. This federal/provincial/territorial initiative allowed for national outbreak trends to be monitored during the pandemic. Knowledge gained from CCOSS informs public health response in Canada for prevention and control of SARS-CoV-2 transmission in various settings. This report provides a retrospective descriptive analysis of COVID-19 outbreak trends in Canada observed over a one-year period from January 2021 to January 2022.
Methods
Information sources
Data were extracted from the CCOSS database and enhanced with case-level data from the National COVID-19 Case Dataset, both stored in a Postgres database and maintained by PHAC. The CCOSS is a passive event-based surveillance system implemented in January 2021 that aims to systematically monitor the incidence and severity of COVID-19 outbreak events by setting type. Seven provinces were included in this analysis (BC, AB, MB, ON, QC, NS and PE); these provinces submitted cumulative COVID-19 outbreak line lists electronically to CCOSS on a weekly basis in 2021. The surveillance system captures aggregate outbreak-level data on administrative variables (e.g. date outbreak declared, date outbreak declared over, outbreak identifier), 24 outbreak settings and number of confirmed cases and outcomes (hospitalization, death). In 2021, provinces submitted records of outbreaks for a variety of outbreak settings, including but not limited to the following settings of interest: long-term care facilities (LTCF), acute care, school and childcare settings, correctional facilities, congregate living, and industrial settings (Table 1) Footnote 8 Footnote 9.
| Condensed settings | CCOSS outbreak settings |
|---|---|
| Acute care | Acute care setting |
| Congregate living | Congregate living setting (e.g. assisted living, shelters, group homes), retirement residence |
| Correctional facility | Correctional facility |
| Industrial/agricultural | Industrial setting, agri-food processing facility |
| Long-term care facility | Long-term care facility |
| School and childcare | School, daycare, or day camp |
| Other | Community healthcare setting, emergency services, mass gathering event, office, personal care setting, recreational facility, restaurant/bar, retail, social event, transportation, travel/tourism, other specify, workplace unspecified, unknown |
|
|
The National COVID-19 Case Dataset is a non-nominal case-based surveillance system capturing data on case demographics, clinical status and outcomes, exposures, risk factors, vaccination, and variant lineages of COVID-19 cases in Canada. For provinces that provided permission for linkage of outbreak and case data, CCOSS data were linked to the COVID-19 case dataset using unique outbreak identifiers. This linkage allowed PHAC to obtain additional information on outbreak case counts and severe outcomes for outbreaks with missing information and variant lineages.
Definitions
The national definition for COVID-19 outbreaks is as follows: two or more confirmed cases of COVID-19 Footnote 10 epidemiologically linked to a specific setting and/or location, excluding households since household cases may not be declared or managed as an outbreak if the risk of transmission is contained. This definition also excludes cases that are geographically clustered (e.g. in a region, city, or town) but not epidemiologically linked, and cases attributed to community transmission Footnote 10.
To contextualize the impact of each variant of concern (VOC), we utilized the period from VOC introduction to the end of the dominant period. Using data from the National COVID-19 Case Dataset, the case with the earliest episode date was used to define the date of introduction. The date corresponding to the end of the dominant period was identified based on the last date that the proportion of VOC cases accounted for at least 75% of sequenced cases reported. March 2021 to May 2021 corresponded to a period of mixed VOC (Alpha, Beta, Gamma) dominance as no single VOC represented over 75%.
To provide context for the role of COVID-19 vaccines on outbreak incidence, we added a vaccination timeline for the start of the vaccination campaign in priority groups (December 2020) and the dates Health Canada authorized vaccines for individuals aged 12–17 years (May 5, 2021) and 5–11 years (November 19, 2021) and first booster doses (November 9, 2021), understanding that there are variations in the timing of the vaccine rollout in different jurisdictions Footnote 11 Footnote 12 Footnote 13 Footnote 14.
Data quality and missing data
The national COVID-19 outbreak definition was applied to CCOSS data. Denominators for outbreak settings (e.g. number of schools or populations at risk within these settings) were not available; thus, it was not possible to calculate which settings are most at risk of outbreaks from these data, only which settings most commonly report outbreaks. Therefore, calculated proportions of outbreaks by setting are relative to the overall number of outbreaks. The completeness of variables reported in the outbreak line list varied by jurisdiction. In a jurisdiction that did not report on industrial setting outbreaks separately, where possible "workplace unspecified" outbreaks were mapped to "industrial/agricultural" based on information from location names. Case fatality was defined as the proportion of confirmed COVID-19 cases associated with an outbreak that died due to COVID-19. Case fatality was missing for approximately 5% of outbreaks. Duplicate records identified using unique outbreak identifiers were removed.
Data analysis
The CCOSS outbreak settings were grouped for analyses according to Table 1. Settings that represented less than 2% of outbreaks or that were inconsistently reported across provinces were grouped into the "other" category. For reporting purposes, data were aggregated by epidemiological week (Sunday to Saturday) in which the outbreak was declared; therefore, this report covers outbreaks declared during the period of January 3, 2021, to January 1, 2022. Data were extracted on April 29, 2022. Data were cleaned and analyzed using R Statistical Software version 4.0.4. Descriptive statistics on outbreak trends by setting, over time and by case characteristics, such as outbreak size and severe outcomes, were computed.
Results
Outbreak trends by settings
From January 3, 2021, to January 1, 2022, a total of 30,078 outbreaks were reported to CCOSS from the seven contributing provinces (Table 2). Outbreaks were most common in school and childcare settings (39%), followed by industrial/agricultural settings (21%), congregate living settings (8%), LTCF (4%), acute care facilities (4%), and correctional facilities (1%). Twenty-four percent of outbreaks occurred in "other" settings. In Canada, schools are in session from January to June and September to mid-December, and during these periods, school and childcare settings consistently accounted for the largest weekly proportion of outbreaks (Figure 1). This was especially evident from September to December 2021, when children younger than 12 years of age were not yet eligible for COVID-19 vaccination; the proportion of outbreaks with vaccine-eligible populations was smaller during fall of 2021. In school and childcare settings, primary schools accounted for the largest proportion of outbreaks, followed by childcare centres, K–12 schools (combined primary and secondary schools), and secondary schools. In the "other" setting, outbreaks occurring in workplaces of an unspecified type accounted for the largest proportion of outbreaks (Figure 2). In congregate living settings, retirement residences and assisted living/group homes accounted for the largest proportion of outbreaks.
| Setting | Outbreaks n=30,078 |
Cases n=241,335 |
Hospitalizations n=10,252 |
Deaths n=3,988 |
Median size | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | Range | |
| School and childcare | 11,699 | 39 | 73,311 | 30 | 294 | 3 | 7 | <1 | 4 | 2–236 |
| Other | 7,069 | 24 | 39,912 | 17 | 1,031 | 10 | 157 | 4 | 3 | 2–364 |
| Industrial/agricultural | 6,262 | 21 | 38,777 | 16 | 939 | 9 | 103 | 3 | 3 | 2–300 |
| Congregate living setting | 2,508 | 8 | 34,641 | 14 | 2,960 | 29 | 1,098 | 28 | 6 | 2–374 |
| Long-term care facility | 1,267 | 4 | 34,703 | 14 | 885 | 9 | 1,554 | 39 | 10 | 2–342 |
| Acute care | 1,120 | 4 | 12,051 | 5 | 4,073 | 40 | 1,061 | 27 | 7 | 2–112 |
| Correctional facility | 153 | 1 | 7,940 | 3 | 70 | 1 | 8 | <1 | 18 | 2–639 |
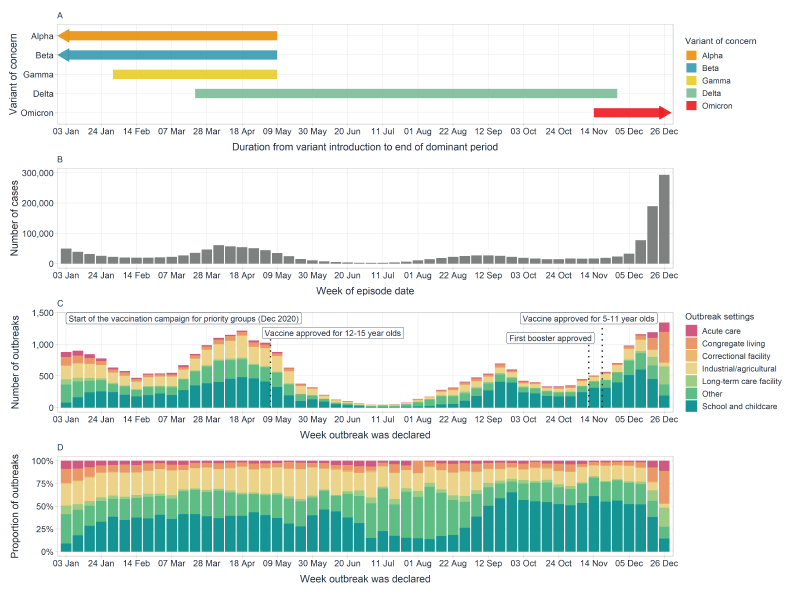
Figure 1 - Text description
Figure 1 displays trends in SARS-CoV-2 variants, all cases incidence, outbreak incidence by setting and proportion of outbreak setting over time. Panel A displays the period of time from when SARS-CoV-2 variants of concern were introduced to the end of their dominance in Canada, which can be contrasted against increases in case and outbreak incidence. Case (Panel B) and outbreak incidence (Panel C) peaks and troughs align over time with large increases noted in March to April 2021 and December 2021. The increase observed in December 2021 aligned with the introduction of Omicron. The proportion of outbreak setting (Panel D) illustrates that a large proportion of outbreaks were in school and childcare facilities, with a decrease in proportion noted during July and early August.
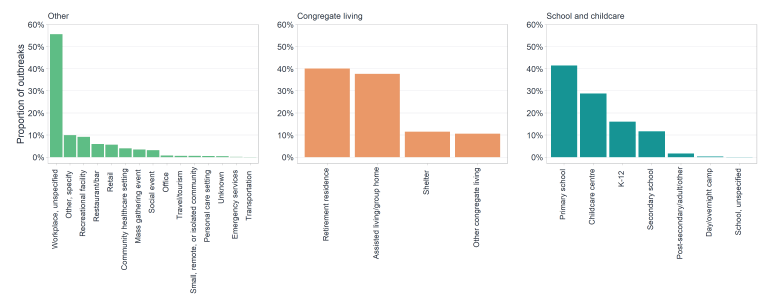
Figure 2 - Text description
Figure 2 illustrates the breakdown of other, congregate living, and school and childcare settings, to demonstrate which sub-settings had the largest proportion of outbreaks. Within the other setting, unspecified workplaces represented the largest proportion of outbreaks. Retirement residences, closely followed by assisted living/group homes represented the largest proportion of outbreaks in congregate living. Within school and childcare settings, primary schools represented the largest proportion of outbreaks.
Temporal outbreak trends
The incidence of outbreaks followed similar trends in reported cases (Figure 1). Waves denoting increasing and decreasing rates of declared outbreaks were largely driven by the introductions of VOCs and the subsequent stabilization of transmission within Canada. The increase in outbreaks in March 2021 was heavily driven by the Alpha variant, although there were also outbreaks involving Beta and Gamma variants. The Delta variant drove the resurgence in the incidence of outbreaks in August 2021, which peaked in late September 2021. The introduction of the Omicron variant in November 2021 led to a significant increase in the incidence of outbreaks but was not proportional to the magnitude of the increase observed in case incidence.
Outbreak trends by case characteristics
A total of 241,335 outbreak-associated cases were reported to CCOSS between January 3, 2021, and January 1, 2022 (Table 2). The distribution of cases by setting was similar to trends in outbreak incidence, with most cases reported in school and childcare settings (30%). Most outbreak-associated hospitalizations were associated with acute care facilities (40%) or congregate living setting (29%) outbreaks. The highest proportions of outbreak-associated deaths were in LTCF (39%), congregate living settings (28%) and acute care facilities (27%). The highest outbreak case fatality was in acute care facilities, with a mean case fatality of 10.7%, followed by LTCF (4.3%) and congregate living settings (2.9%).
The size of outbreaks ranged from 2 to 639 cases per outbreak with a median of four cases per outbreak (Table 2). Correctional facilities (18 cases per outbreak) had the highest median outbreak size followed by LTCF (10 cases per outbreak), acute care facilities (seven cases per outbreak) and congregate living settings (six cases per outbreak). Figure 3 shows that the largest outbreaks were reported in correctional facilities, with more than 18% of outbreaks reporting more than 100 cases, followed by LTCFs (6%).
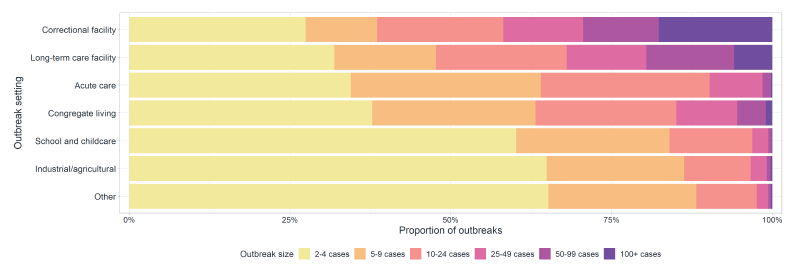
Figure 3 - Text description
Figure 3 displays the proportion of outbreaks by outbreak size across settings. Correctional facilities have the largest proportion of outbreak with 100 cases or more, with most outbreaks having more than 5–9 cases. Long-term care facilities have the second largest proportion of outbreaks with 100 cases or more, while the setting "Other" has the largest proportion of outbreaks with 2–4 cases.
| Condensed settings | 2–4 cases | 5–9 cases | 10–24 cases | 25–49 cases | 50–99 cases | 100+ cases |
|---|---|---|---|---|---|---|
| Correctional facility | 27% | 11% | 20% | 12% | 12% | 18% |
| Long-term care facility | 32% | 16% | 20% | 12% | 14% | 6% |
| Acute care | 34% | 30% | 26% | 8% | 1% | <1% |
| Congregate living | 38% | 25% | 22% | 9% | 4% | 1% |
| School and childcare | 60% | 24% | 13% | 2% | 1% | <1% |
| Industrial/agricultural | 65% | 21% | 10% | 2% | 1% | <1% |
| Other | 65% | 23% | 9% | 2% | <1% | <1% |
Within LTCF, there was a sharp decline in the incidence of outbreak-associated deaths in January 2021 shortly after the COVID-19 vaccine rollout began, for which LTCF was one of the priority settings (Figure 4). Subsequently, incidence of outbreak-associated deaths remained low and relatively stable until the introduction of the Omicron variant in late 2021 which resulted in a rapid increase in cases and deaths (Figure 1, Figure 4).
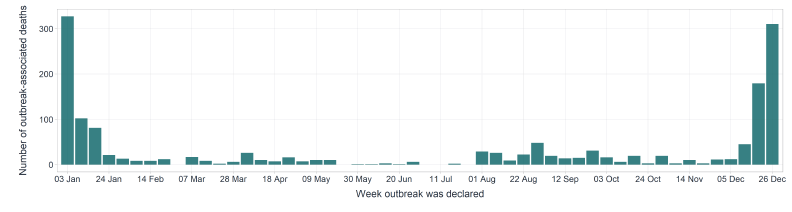
Figure 4 - Text description
Figure 4 illustrates the weekly number of long-term care facility outbreak-associated deaths over time (January 3, 2021 to January 1, 2022). Peaks in long-term care outbreak-associated deaths are observed for the first few weeks in January 2021 and in December 2021. The number of long-term care facility outbreak associated deaths is lowest during the end of May to July 2021.
Discussion
In 2021, 30,078 outbreaks were reported to CCOSS, with the highest proportions being in school and childcare, industrial/agricultural and congregate living settings. Temporal trends for outbreak and case incidence generally aligned; however, a larger relative increase was noted in cases compared to outbreaks in December 2021, following the introduction of the Omicron variant. Settings that experienced the highest severity were acute care and LTCF. The largest outbreaks were reported in correctional facilities and LTCFs, both of which are congregate living settings.
In 2021, the majority of outbreaks reported to CCOSS were in settings considered to be essential services and functions Footnote 15 Footnote 16. The most reported setting was school and childcare settings (39%). There are approximately 15,500 schools in Canada Footnote 17, representing almost 5.7 million students Footnote 18 and 766,200 educators Footnote 17 resulting in a large population at risk. During the Delta-driven resurgence of cases from September to November 2021, when those under 12 years of age were not yet eligible for COVID-19 vaccinations, primary schools experienced the largest increase in the incidence of outbreaks relative to other settings Footnote 19. Despite their large representation, the size of school and childcare outbreaks remained small compared to other settings, with 60% of outbreaks reporting fewer than four cases; severity in this setting remained low throughout 2021, which is consistent with what has been reported in the literature Footnote 20 Footnote 21. Studies conducted globally reported similar findings, whereby outbreak cases were small and transmission risk was low when public health measures were in place (e.g. masking, vaccination, cohorting, physical distancing, screening, testing) Footnote 22 Footnote 23.
The second most reported outbreak setting was "other," which consists of multiple settings aggregated for reporting purposes. "Unspecified workplaces" accounted for the majority of outbreaks in "other" settings. The remaining settings included restaurants, bars, retail and recreational facilities. Outbreak trends in these settings often follow case incidence trends and can contribute to community transmission given the potential for exposure from multiple networks Footnote 24 Footnote 25. However, the reported outbreaks in these settings were lower than may have been expected, potentially as a result of extended lockdown orders for nonessential settings through the course of 2021 and/or lower levels of symptom surveillance and testing compared to essential and high-risk settings Footnote 25 Footnote 26.
Although the incidence of outbreaks was highest in community-type settings (e.g. schools, retail, restaurants), outbreak size was the largest in settings with congregate living, likely due to the communal nature of these settings Footnote 9. Larger outbreak sizes may reflect increased transmissibility in high-risk populations, configuration of settings (e.g. shared bedrooms, communal areas), population dynamics (e.g. rotating staff, transient population, visitors) and outbreak management strategies (e.g. case cohorting, inability to vacate populations) within those settings. Attack rates in dormitories and shelters, both congregate settings, ranged from 1.9%–41.7% Footnote 27 Footnote 28. Denominators were not available for outbreaks submitted to CCOSS; however, high case counts in congregate settings such as retirement residences and shelters suggest attack rates may have been high.
Industrial/agricultural outbreaks accounted for the third-largest proportion of outbreaks (21%). Early in the pandemic, several large outbreaks were reported in industrial/agricultural settings (e.g. meat processing facilities, oil refineries, warehouses), many of which involved temporary foreign workers, immigrant populations and rotational workers Footnote 29 Footnote 30 Footnote 31 Footnote 32 Footnote 33 Footnote 34. Poor ventilation, difficulties maintaining physical distancing, shared transportation and housing, lack of paid sick leave and the rotational nature of the work can lead to rapid transmission of SARS-CoV-2 in certain industrial/agricultural settings—often overlapping with wider marginalized employee populations Footnote 35 Footnote 36. Additionally, many industrial and/or work camp settings involve workers from jurisdictions across Canada, which creates an elevated risk of importation of COVID-19 into the workplace, as well as back into communities in various parts of the country as workers return following rotations. Following broader vaccination rollout in May 2021, including mandatory vaccine policies in some settings, there was a dramatic reduction in the incidence of outbreaks in industrial/agricultural settings; however, this may have been in part due to revised testing strategies and outbreak management. Incidence remained relatively low until the introduction of the Omicron variant in November, which has been shown to escape immunity Footnote 37. The case fatality in this setting was 0.2%, though this could be biased by the healthy worker effect Footnote 38.
The LTCF are settings that experienced devastating impacts as a result of COVID-19 outbreaks Footnote 39 Footnote 40. In Canada, 80% of COVID-19 deaths during the first pandemic wave occurred in LTCF, when COVID-19 vaccines were not yet available Footnote 40. In November 2020, the National Advisory Committee on Immunization (NACI) recommended that the first stage of the COVID-19 vaccine rollout be prioritized to residents and staff of LTCF, among other high-risk settings such as retirement residences and acute care facilities Footnote 41. Jurisdictions across Canada reported high vaccine uptake among this population Footnote 42 Footnote 43 Footnote 44 Footnote 45. As vaccine coverage increased among the LTCF population in early 2021, there was a notable and rapid decrease in the incidence of COVID-19 deaths in this setting, aligning with evidence demonstrating vaccine protection against severe outcomes Footnote 46 Footnote 47 Footnote 48. In December 2021, we observed an increase in the incidence of deaths associated with outbreaks in LTCF, reflecting evidence of a shift in the immunity profile following the introduction of the immuno-evasive Omicron variant in fall of 2021 Footnote 49.
Outbreaks can result in high morbidity and mortality—adding strain to the healthcare system in addition to individual suffering Footnote 50. For COVID-19, the following populations have been identified as higher risk for severe outcomes: older adults (especially those living in congregate settings); people with medical conditions; pregnant people; and communities that experience disproportionate burdens of disease (People of Colour, Indigenous Peoples, refugee populations) Footnote 51. However, details on communities disproportionately impacted by COVID-19 were not available through CCOSS or case data. Within the CCOSS data, congregate living settings and LTCF experienced high case burdens; however, acute care settings had the highest case fatality (10.7%). The highest numbers of deaths were reported in LTCF, followed by congregate living settings and acute care facilities. Other countries, such as France, the United Kingdom, Belgium and Australia, have also noted severe outcomes in these high-risk populations Footnote 52. Mortality rates in LTCF have been higher than those of older adults in community dwellings Footnote 53. An international review found that 19%–72% of deaths during the pandemic occurred in LTCF Footnote 52. High mortality in acute care settings may be due to patients having comorbidities that impacted their clinical outcome Footnote 54. Approximately 90% of deaths in acute care outbreaks were among individuals older than 60 years of age Footnote 54. Interpreting severity for acute care is challenging, as individuals are already hospitalized and death rates may be influenced by underlying health conditions. Similarly, residents of LTCF who become ill have access to care in the facility rather than being hospitalized, complicating the interpretation of nonfatal severity outcomes in this setting. Continuing to monitor COVID-19 outbreaks in LTCF and acute care settings is recommended and aligns with current surveillance practices for other respiratory viruses (e.g. influenza).
Strengths
The CCOSS was rapidly and effectively implemented as a novel initiative in collaboration with federal, provincial and territorial partners in the middle of an emerging infectious disease emergency. PHAC recently conducted an evaluation of CCOSS and found that the surveillance system had good representation, with participating jurisdictions representing 93% of the Canadian population Footnote 5. Data providers consistently submitted outbreak line lists to CCOSS on a weekly basis and as a result, data were very timely. The system is flexible and was able to adapt to the needs of jurisdictions (e.g. multiple methods of data sharing, file types) and changes to data elements and format. Additionally, data were mapped to CCOSS variables by PHAC, which reduced reporting burden on provinces and improved acceptability. Outbreak data from CCOSS can also be linked to case data from the National COVID-19 Case Dataset to obtain information on outbreak-associated cases which further reduced reporting burden for certain jurisdictions, although linkage was not possible for all participating provinces. Variable completeness was excellent for the basic variables (i.e. outbreak identifier, setting, start date, number of cases) required for describing outbreak trends.
The CCOSS processes were efficient, which allowed for the timely dissemination of trends from CCOSS to various audiences in its short weekly surveillance cycle. Outbreak trend data, including outbreak setting, outbreak size and severity, have been used by the Office of the Chief Public Health Officer to provide context to the case incidence and for epidemic planning and modelling Footnote 55. The outbreak data collected from CCOSS has helped inform decisions by NACI around additional vaccine doses for LTCF residents. Epidemiologists from PHAC examined LTCF outbreak trends for several months following the implementation of the second dose of vaccine in LTCF residents (i.e. June to September 2021) to identify any increases in the incidence and size of outbreaks that could indicate waning immunity and the need for an additional vaccine dose.
Outbreaks have not been experienced equally across Canada. Smaller provinces and territories experienced fewer and less varied types of outbreaks compared with more densely populated provinces with large urban centres and/or concentrations of large industrial operations. Field epidemiologists mobilized to assist with the control and investigation of COVID-19 outbreaks in some provinces and territories, and used nationally aggregated outbreak statistics in the context of public health measures to make recommendations suitable to novel yet similar contexts.
Limitations
The accuracy and validity of the data reported to CCOSS by provinces for each outbreak setting are unknown and dependent on public health capacity to identify cases, contact trace, and establish epidemiological links. During periods of high case incidence, outbreaks may be under-ascertained due to limited public health capacity, or where high-risk settings were prioritized for testing. Outbreak size was underestimated in certain settings such as industrial settings, correctional facilities and acute care, where separate outbreaks were administratively recorded by smaller groupings for public health management (e.g. by floor, units, or another identifier). Furthermore, enhanced outbreak management implemented by some jurisdictions during periods with high surges in cases (i.e. the introduction of the Omicron variant) may impact the incidence of outbreaks reported, outbreak size and outbreak declared/end dates.
Only seven provinces of 13 provinces/territories were included in this analysis. The national outbreak analysis presented in this report was highly influenced by three of the most populous provinces in Canada (ON, QC and AB), which submitted the highest number of outbreaks (99%) and covered the greatest number of outbreak settings. Smaller participating jurisdictions and non-participating provincial and territorial jurisdictions may experience outbreak trends that differ from the national picture presented here, which was heavily influenced by the more populous provinces.
In October 2021, AB changed their outbreak definition to between two and 10 cases for certain settings Footnote 56. This would have led to an underreporting of smaller outbreaks in these settings and biased the outbreak size towards larger outbreaks.
Denominators for a number of facilities within a province or health region were not available, and even if they were, it would be difficult to identify how many facilities were affected by outbreaks since some facilities might report multiple outbreaks over time or report outbreaks by units/floors/classes, etc. The lack of denominators by setting and population at risk made it impossible to calculate attack rates for a setting or within a facility.
The data mapping of "workplace unspecified" to industrial/agricultural for jurisdictions that did not report on industrial settings separately may have contributed to non-industrial/agricultural workplaces being included. This could have contributed to an artificial increase in the number of outbreaks reported in this setting.
Conclusion
Nationally aggregated provincial outbreak data permitted trend and additional descriptive analyses to inform our understanding of where COVID-19 outbreaks occur in Canada and support ongoing efforts to reduce transmission in high-risk settings. Outbreak trends illustrated that outbreaks were reported more frequently in certain settings, specifically schools and workplaces; however, congregate living settings were prone to larger outbreaks and acute care settings experienced the highest case fatality. The information gathered from outbreak surveillance complemented case incidence trends and furthered understanding of COVID-19 in Canada. Monitoring COVID-19 outbreaks in high-risk settings such as LTCF, acute care and congregate living aligns with current surveillance practices for other respiratory viruses and continues to be a priority.
Authors' statement
DD — Conceptualization, methodology, software, formal analysis, writing–original draft, writing–review and editing, visualization
EM — Conceptualization, methodology, writing–original draft, writing–review and editing
AB — Conceptualization, writing–review and editing
CC — Conceptualization, writing–review and editing
JE — Conceptualization, writing–review and editing
RM — Conceptualization, supervision, writing–review and editing
KP — Conceptualization, supervision, writing–review and editing
Competing interests
None.
Acknowledgements
We thank the following current and former team members that contributed to the management of the Canadian COVID-19 Outbreak Surveillance System (CCOSS) and CCOSS analyses and products since March 2021: Samara David, Yuhui Xu, Carolyn Dohoo, Krista Wilkinson, Yasmina Tehami, Arzoo Alam, and Meong Jin (Ellie) Joung. We also thank the participating provinces (BC, AB, MB, ON, QC, NS, PE) for collecting and submitting their data to the Public Health Agency of Canada (PHAC) in 2021. Finally, we thank the Data Integration team at PHAC for their conceptualization of the database and ongoing support to integrate submitted data into the database.
Funding
This work was supported by the Public Health Agency of Canada as part of its core mandate.
References
- Footnote 1
-
Sunnybrook Hospital. A look back at Canada's first COVID-19 case. Toronto, ON: SBH; Aug 25, 2020. https://sunnybrook.ca/media/item.asp?page=38&i=2167
- Footnote 2
-
Zhao N, Liu Y, Smargiassi A, Bernatsky S. Tracking the origin of early COVID-19 cases in Canada. Int J Infect Dis 2020;96:506–8. https://doi.org/10.1016/j.ijid.2020.05.046
- Footnote 3
-
Public Health Agency of Canada. COVID-19 data trends. Ottawa, ON: PHAC; May 20, 2022. [Accessed 2022 May 25]. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/epidemiological-economic-research-data.html
- Footnote 4
-
Murti M, Achonu C, Smith BT, Brown KA, Kim JH, Johnson J, Ravindran S, Buchan SA. COVID-19 Workplace Outbreaks by Industry Sector and Their Associated Household Transmission, Ontario, Canada, January to June, 2020. J Occup Environ Med 2021;63(7):574–80. https://doi.org/10.1097/JOM.0000000000002201
- Footnote 5
-
Statistics Canada. Population and dwelling counts: Canada, provinces and territories. Ottawa, ON: StatCan; Feb 2021. [Accessed 2022 May 27]. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810000101
- Footnote 6
-
Health Protection Surveillance Centre. Epidemiology of COVID-19 Outbreaks/Clusters in Ireland Weekly Reports 2022. Dublin (IE): HPSC; 2023. [Accessed 2023 Jan 18]. https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/surveillance/covid-19outbreaksclustersinireland/covid-19outbreaksclustersinirelandweeklyreports2022/
- Footnote 7
-
Government of the United Kingdom. National COVID-19 Surveillance reports. London (UK); Gov’t UK; 2021. [Accessed 2023 Jan 18]. https://www.gov.uk/government/publications/national-covid-19-surveillance-reports#full-publication-update-history
- Footnote 8
-
World Health Organization. Regional Office for the Western Pacific. Actions for consideration in the care and protection of vulnerable population groups for COVID-19. Geneva (CH): WHO; 2021. https://apps.who.int/iris/handle/10665/333043
- Footnote 9
-
Terebuh PD, Egwiekhor AJ, Gullett HL, Fakolade AO, Miracle JE, Ganesh PT, Rose J, Stange KC, Szabo AD, Grisez B, Brennan K, Hrusch S, Napolitano J, Brazile R, Allan T. Characterization of community-wide transmission of SARS-CoV-2 in congregate living settings and local public health-coordinated response during the initial phase of the COVID-19 pandemic. Influenza Other Respir Viruses 2021;15(4):439–45. https://doi.org/10.1111/irv.12819
- Footnote 10
-
Public Health Agency of Canada. National case definition: Coronavirus disease (COVID-19). Ottawa, ON: PHAC; 2022. [Accessed 2022 May 25]. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/national-case-definition.html
- Footnote 11
-
Public Health Agency of Canada. National Advisory Committee on Immunization. Recommendations on the use of COVID-19 vaccine(s). Ottawa, ON: PHAC; Dec 2020. [Accessed 2023 Jan 18]. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines/december-12-2020.html#a6(s)
- Footnote 12
-
Health Canada. Health Canada authorizes use of the Pfizer-BioNTech COVID-19 vaccine in children 12 to 15 years of age. Ottawa, ON: HC; May 5, 2021. [Accessed 2023 Jan 18]. https://www.canada.ca/en/health-canada/news/2021/05/health-canada-authorizes-use-of-the-pfizer-biontech-covid-19-vaccine-in-children-12-to-15-years-of-age.html
- Footnote 13
-
Health Canada. Health Canada authorizes use of Comirnaty (the Pfizer-BioNTech COVID-19 vaccine) in children 5 to 11 years of age. Ottawa, ON: HC; Nov 2021. [Accessed 2023 Jan 18]. https://www.canada.ca/en/health-canada/news/2021/11/health-canada-authorizes-use-of-comirnaty-the-pfizer-biontech-covid-19-vaccine-in-children-5-to-11-years-of-age.html
- Footnote 14
-
Health Canada. Health Canada authorizes the use of the Pfizer-BioNTech Comirnaty COVID-19 vaccine as a booster shot. Ottawa, ON: HC; Nov 2021. [Accessed 2023 Jan 18]. https://www.canada.ca/en/health-canada/news/2021/11/health-canada-authorizes-the-use-of-the-pfizer-biontech-comirnaty-covid-19-vaccine-as-a-booster-shot.html
- Footnote 15
-
Public Health Agency of Canada. COVID-19 epidemiology update: Key updates. Ottawa, ON: PHAC; Oct 2022. [Accessed 2022 Oct 25]. https://health-infobase.canada.ca/covid-19/
- Footnote 16
-
Children’s Mental Health Ontario. Schools are Essential. Toronto, ON: CMHO; April 13, 2021. [Accessed 2022 May 25]. https://cmho.org/schools-are-essential/
- Footnote 17
-
Council of Ministers of Education. Canada. Education in Canada. Toronto, ON: CMEC. [Accessed 2022 May 25]. https://www.cmec.ca/299/education-in-canada-an-overview/index.html#:~:text=Schools%20and%20Enrolments,mixed%20elementary%20and%20secondary%20schools
- Footnote 18
-
Statistics Canada. Elementary–Secondary Education Survey, 2019/2020. Ottawa, ON: StatCan; October 2021. [Accessed 2022 May 25]. https://www150.statcan.gc.ca/n1/daily-quotidien/211014/dq211014c-eng.htm
- Footnote 19
-
Head JR, Andrejko KL, Remais JV. Model-based assessment of SARS-CoV-2 Delta variant transmission dynamics within partially vaccinated K-12 school populations. medRxiv. 2021.08.20.21262389. https://doi.org/10.1101/2021.08.20.21262389
- Footnote 20
-
Drouin O, Hepburn CM, Farrar DS, Baerg K, Chan K, Cyr C, Donner EJ, Embree JE, Farrell C, Forgie S, Giroux R, Kang KT, King M, Laffin M, Luu TM, Orkin J, Papenburg J, Pound CM, Price VE, Purewal R, Sadarangani M, Salvadori MI, Top KA, Viel-Thériault I, Kakkar F, Morris SK; Canadian Paediatric Surveillance Program COVID-19 Study Team. Characteristics of children admitted to hospital with acute SARS-CoV-2 infection in Canada in 2020. CMAJ 2021;193(38):E1483–93. https://doi.org/10.1503/cmaj.210053
- Footnote 21
-
Shekerdemian LS, Mahmood NR, Wolfe KK, Riggs BJ, Ross CE, McKiernan CA, Heidemann SM, Kleinman LC, Sen AI, Hall MW, Priestley MA, McGuire JK, Boukas K, Sharron MP, Burns JP; International COVID-19 PICU Collaborative. Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr 2020;174(9):868–73. https://doi.org/10.1001/jamapediatrics.2020.1948
- Footnote 22
-
Boutzoukas AE, Zimmerman KO, Benjamin DK, DeMuri GP, Kalu IC, Smith MJ, McGann KA, Koval S, Brookhart MA, Butteris SM. Secondary transmission of COVID-19 in K–12 schools: findings from 2 states. Pediatrics 2022;149(12 Suppl 2):e2021054268K. https://doi.org/10.1542/peds.2021-054268K
- Footnote 23
-
Lakha F, King A, Swinkels K, Lee AC. Are schools drivers of COVID-19 infections-an analysis of outbreaks in Colorado, USA in 2020. J Public Health (Oxf) 2022;44(1):e26–35. https://doi.org/10.1093/pubmed/fdab213
- Footnote 24
-
Jin X, Leng Y, Gong E, Xiong S, Yao Y, Vedanthan R, Yang Z, Chen K, Wu C, Yan L. Neighborhood-level public facilities and COVID-19 transmission: A nationwide geospatial study in China. Research Square. 2020. https://doi.org/10.21203/rs.3.rs-117254/v1
- Footnote 25
-
Banholzer N, van Weenen E, Lison A, Cenedese A, Seeliger A, Kratzwald B, Tschernutter D, Salles JP, Bottrighi P, Lehtinen S, Feuerriegel S, Vach W. Estimating the effects of non-pharmaceutical interventions on the number of new infections with COVID-19 during the first epidemic wave. PLoS One 2021;16(6):e0252827. https://doi.org/10.1371/journal.pone.0252827
- Footnote 26
-
Huang X, Shao X, Xing L, Hu Y, Sin DD, Zhang X. The impact of lockdown timing on COVID-19 transmission across US counties. EClinicalMedicine 2021;38:101035. https://doi.org/10.1016/j.eclinm.2021.101035
- Footnote 27
-
Currie DW, Moreno GK, Delahoy MJ, Pray IW, Jovaag A, Braun KM, Cole D, Shechter T, Fajardo GC, Griggs C, Yandell BS, Goldstein S, Bushman D, Segaloff HE, Kelly GP, Pitts C, Lee C, Grande KM, Kita-Yarbro A, Grogan B, Mader S, Baggott J, Bateman AC, Westergaard RP, Tate JE, Friedrich TC, Kirking HL, O’Connor DH, Killerby ME. Interventions to Disrupt Coronavirus Disease Transmission at a University, Wisconsin, USA, August-October 2020. Emerg Infect Dis 2021;27(11):2776–85. https://doi.org/10.3201/eid2711.211306
- Footnote 28
-
Redditt V, Wright V, Rashid M, Male R, Bogoch I. Outbreak of SARS-CoV-2 infection at a large refugee shelter in Toronto, April 2020: a clinical and epidemiologic descriptive analysis. CMAJ Open 2020;8(4):E819–24. https://doi.org/10.9778/cmajo.20200165
- Footnote 29
-
Fabreau GE, Holdbrook L, Peters CE, Ronksley PE, Attaran A, McBrien K, Pottie K. Vaccines alone will not prevent COVID-19 outbreaks among migrant workers-the example of meat processing plants. Clin Microbiol Infect 2022;28(6):773–8. https://doi.org/10.1016/j.cmi.2022.02.004
- Footnote 30
-
Yourex-West H. Why did Canada's two biggest COVID-19 workplace outbreaks get so big, so fast? Global News. 2021 May 31. https://globalnews.ca/news/7902976/why-canada-biggest-covid-19-workplace-outbreaks-so-fast/
- Footnote 31
-
Guardian Law Group. Class Actions and Mass Torts: Cargill Meat Processing Plant Covid-19 Outbreak. https://www.guardian.law/our-services/class-actions-mass-torts/covid-outbreak-at-cargill-limited/
- Footnote 32
-
Yourex-West H. Inside the oilsands site that has seen Canada's largest workplace COVID-19 outbreak. Global News. 2021 May 12. https://globalnews.ca/news/7852937/oil-sands-site-canada-largest-workplace-covid-outbreak/
- Footnote 33
-
Herhalt C. Major Amazon Warehouse ordered closed in Brampton, Ont. due to COVID-19 outbreak inside. Toronto CTV News. 2021 March 12. https://toronto.ctvnews.ca/major-amazon-warehouse-ordered-closed-in-brampton-ont-due-to-covid-19-outbreak-inside-1.5345208
- Footnote 34
-
Aziz T. Federal government to invest $59M to help migrant farm workers. CBC News. 2020 August 1. https://www.cbc.ca/news/canada/windsor/federal-government-59-million-migrant-farm-workers-covid-1.5671468
- Footnote 35
-
Dyal JW, Grant MP, Broadwater K, Bjork A, Waltenburg MA, Gibbins JD, Hale C, Silver M, Fischer M, Steinberg J, Basler CA, Jacobs JR, Kennedy ED, Tomasi S, Trout D, Hornsby-Myers J, Oussayef NL, Delaney LJ, Patel K, Shetty V, Kline KE, Schroeder B, Herlihy RK, House J, Jervis R, Clayton JL, Ortbahn D, Austin C, Berl E, Moore Z, Buss BF, Stover D, Westergaard R, Pray I, DeBolt M, Person A, Gabel J, Kittle TS, Hendren P, Rhea C, Holsinger C, Dunn J, Turabelidze G, Ahmed FS, deFijter S, Pedati CS, Rattay K, Smith EE, Luna-Pinto C, Cooley LA, Saydah S, Preacely ND, Maddox RA, Lundeen E, Goodwin B, Karpathy SE, Griffing S, Jenkins MM, Lowry G, Schwarz RD, Yoder J, Peacock G, Walke HT, Rose DA, Honein MA. COVID-19 Among Workers in Meat and Poultry Processing Facilities - 19 States, April 2020. MMWR Morb Mortal Wkly Rep 2020;69(18):557–61. https://doi.org/10.15585/mmwr.mm6918e3
- Footnote 36
-
Günther T, Czech-Sioli M, Indenbirken D, Robitaille A, Tenhaken P, Exner M, Ottinger M, Fischer N, Grundhoff A, Brinkmann MM. SARS-CoV-2 outbreak investigation in a German meat processing plant. EMBO Mol Med 2020;12(12):e13296. https://doi.org/10.15252/emmm.202013296
- Footnote 37
-
Hu J, Peng P, Cao X, Wu K, Chen J, Wang K, Tang N, Huang AL. Increased immune escape of the new SARS-CoV-2 variant of concern Omicron. Cell Mol Immunol 2022;19(2):293–5. https://doi.org/10.1038/s41423-021-00836-z
- Footnote 38
-
Shah D. Healthy worker effect phenomenon. Indian J Occup Environ Med 2009;13(2):77–9. https://doi.org/10.4103/0019-5278.55123
- Footnote 39
-
Kain D, Stall N, Brown K, McCreight L, Rea E, Kamal M, Brenner J, Verge M, Davies R, Johnstone J. A longitudinal, clinical, and spatial epidemiologic analysis of a large COVID-19 long-term care home outbreak. J Am Med Dir Assoc 2021;22(10):2003–2008.e2. https://doi.org/10.1016/j.jamda.2021.07.021
- Footnote 40
-
Canadian Institute for Health Information. Pandemic Experience in the Long-Term Care Sector: How Does Canada Compare With Other Countries? Ottawa, ON: CIHI; 2020. [Accessed 2023 Jan18]. https://www.cihi.ca/sites/default/files/document/covid-19-rapid-response-long-term-care-snapshot-en.pdf
- Footnote 41
-
Public Health Agency of Canada. National Advisory Committee on Immunization. Preliminary guidance on key populations for early COVID-19 immunization. Ottawa, ON: PHAC; November 2020. [Accessed 2023 Jan18]. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/guidance-key-populations-early-covid-19-immunization.html
- Footnote 42
-
Ministry of Health. British Columbia. Health Sector Information, Analysis and Reporting Division. COVID-19 Vaccination Rates in Long Term Care and Assisted Living Facilities. Vancouver, BC: MOHBC; February 2021. [Accessed 2023 Jan 24]. http://www.bccdc.ca/Health-Info-Site/PublishingImages/health-info/diseases-conditions/covid-19/data/LTC-vaccine-coverage-by-Facility.pdf
- Footnote 43
-
Sinha S, Feil C, Iciaszczyk N. The rollout of the COVID-19 vaccines in care homes in Canada as of 3rd March 2021 update. International Long-Term Care Policy Network. London, ON; CPEC-LSE; 2021. https://ltccovid.org/2021/03/04/the-rollout-of-covid-19-vaccines-in-canadian-long-term-care-homes-3rd-march-2021-update/
- Footnote 44
-
Brown KA, Stall NM, Vanniyasingam T, Buchan SA, Daneman N, Hillmer MP, Hopkins J, Johnstone J, Maltsev A, McGeer A, Sander B, Savage RD, Watts T, Juni P, Rochon PA on behalf of the Congregate Care Setting Working Group and the Ontario SOVID-19 Science Advisory Table. Early impact of Ontario’s COVID-19 vaccine rollout on long-term care home residents and health care workers. Ontario COVID-19 Science Advisory Table (Science Briefs) 2021;2(13). https://doi.org/10.47326/ocsat.2021.02.13.1.0
- Footnote 45
-
Fortin É, De Wals P, Talbot D, Ouakki M, Deceuninck G, Sauvageau C, Gilca R, Kiely M, De Serres G. Impact of the first vaccine dose on COVID-19 and its complications in long-term care facilities and private residences for seniors in Québec, Canada. Can Commun Dis Rep 2022;48(4):164–9. https://doi.org/10.14745/ccdr.v48i04a07
- Footnote 46
-
Shrotri M, Krutikov M, Nacer-Laidi H, Azmi B, Palmer T, Giddings R, Fuller C, Irwin-Singer A, Baynton V, Tut G, Moss P, Hayward A, Copas A, Shallcross L. Duration of vaccine effectiveness against SARS-CoV-2 infection, hospitalisation, and death in residents and staff of long-term care facilities in England (VIVALDI): a prospective cohort study. Lancet Healthy Longev 2022;3(7):e470–80. https://doi.org/10.1016/S2666-7568(22)00147-7
- Footnote 47
-
Moline HL, Whitaker M, Deng L, Rhodes JC, Milucky J, Pham H, Patel K, Anglin O, Reingold A, Chai SJ, Alden NB, Kawasaki B, Meek J, Yousey-Hindes K, Anderson EJ, Farley MM, Ryan PA, Kim S, Nunez VT, Como-Sabetti K, Lynfield R, Sosin DM, McMullen C, Muse A, Barney G, Bennett NM, Bushey S, Shiltz J, Sutton M, Abdullah N, Talbot HK, Schaffner W, Chatelain R, Ortega J, Murthy BP, Zell E, Schrag SJ, Taylor C, Shang N, Verani JR, Havers FP. Effectiveness of COVID-19 Vaccines in Preventing Hospitalization Among Adults Aged ≥65 Years - COVID-NET, 13 States, February-April 2021. MMWR Morb Mortal Wkly Rep 2021;70(32):1088–93. https://doi.org/10.15585/mmwr.mm7032e3
- Footnote 48
-
Lin DY, Gu Y, Xu Y, Wheeler B, Young H, Sunny SK, Moore Z, Zeng D. Association of Primary and Booster Vaccination and Prior Infection With SARS-CoV-2 Infection and Severe COVID-19 Outcomes. JAMA 2022;328(14):1415–26. https://doi.org/10.1001/jama.2022.17876
- Footnote 49
-
Willett BJ, Grove J, MacLean OA, Wilkie C, De Lorenzo G, Furnon W, Cantoni D, Scott S, Logan N, Ashraf S, Manali M, Szemiel A, Cowton V, Vink E, Harvey WT, Davis C, Asamaphan P, Smollett K, Tong L, Orton R, Hughes J, Holland P, Silva V, Pascall DJ, Puxty K, da Silva Filipe A, Yebra G, Shaaban S, Holden MT, Pinto RM, Gunson R, Templeton K, Murcia PR, Patel AH, Klenerman P, Dunachie S, Haughney J, Robertson DL, Palmarini M, Ray S, Thomson EC; PITCH Consortium; COVID-19 Genomics UK (COG-UK) Consortium. SARS-CoV-2 Omicron is an immune escape variant with an altered cell entry pathway. Nat Microbiol 2022;7(8):1161–79. https://doi.org/10.1038/s41564-022-01143-7
- Footnote 50
-
Madhav N, Oppenheim B, Gallivan M, Mulembakani P, Rubin E, Wolfe N. Chapter 17: Pandemics: Risks, Impacts, and Mitigation. In: Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017. https://doi.org/10.1596/978-1-4648-0527-1_ch17
- Footnote 51
-
Centers for Disease Control and Prevention. COVID-19: Understanding Risk. Atlanta (GA): CDC; 2022. [Accessed 2022 May 25]. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html
- Footnote 52
-
Thompson DC, Barbu MG, Beiu C, Popa LG, Mihai MM, Berteanu M, Popescu MN. The impact of COVID-19 pandemic on long-term care facilities worldwide: an overview on international issues. BioMed Res Int 2020;2020:8870249. https://doi.org/10.1155/2020/8870249
- Footnote 53
-
Levin AT, Jylhävä J, Religa D, Shallcross L. COVID-19 prevalence and mortality in longer-term care facilities. Eur J Epidemiol 2022;37(3):227–34. https://doi.org/10.1007/s10654-022-00861-w
- Footnote 54
-
Jarrett M, Schultz S, Lyall J, Wang J, Stier L, De Geronimo M, Nelson K. Clinical Mortality in a Large COVID-19 Cohort: observational Study. J Med Internet Res 2020;22(9):e23565. https://doi.org/10.2196/23565
- Footnote 55
-
Public Health Agency of Canada. Mathematical modelling and COVID-19. Ottawa, ON: PHAC; modified Apr 2022. [Accessed 2022 May 25]. https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/epidemiological-economic-research-data/mathematical-modelling.html
- Footnote 56
-
Government of Alberta. Alberta Public Health Disease Management Guidelines Coronavirus, COVID-19 - Superseded. Alberta Health; November 2021. [Accessed 2023 Jan 30]. https://open.alberta.ca/dataset/a86d7a85-ce89-4e1c-9ec6-d1179674988f/resource/10ac51a3-45a0-438a-b0de-ba5dc6e486de/download/health-disease-management-guidelines-covid-19-2021-11.pdf
