HIV among African, Caribbean and Black people in Ontario

 Download this article as a PDF
Download this article as a PDF(323 KB)
Published by: The Public Health Agency of Canada
Issue: CCDR Volume 50-7/8, July/August 2024: Sexual Health
Date published: July/August 2024
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 50-7/8, July/August 2024: Sexual Health
Infographic
Infographic - Text description
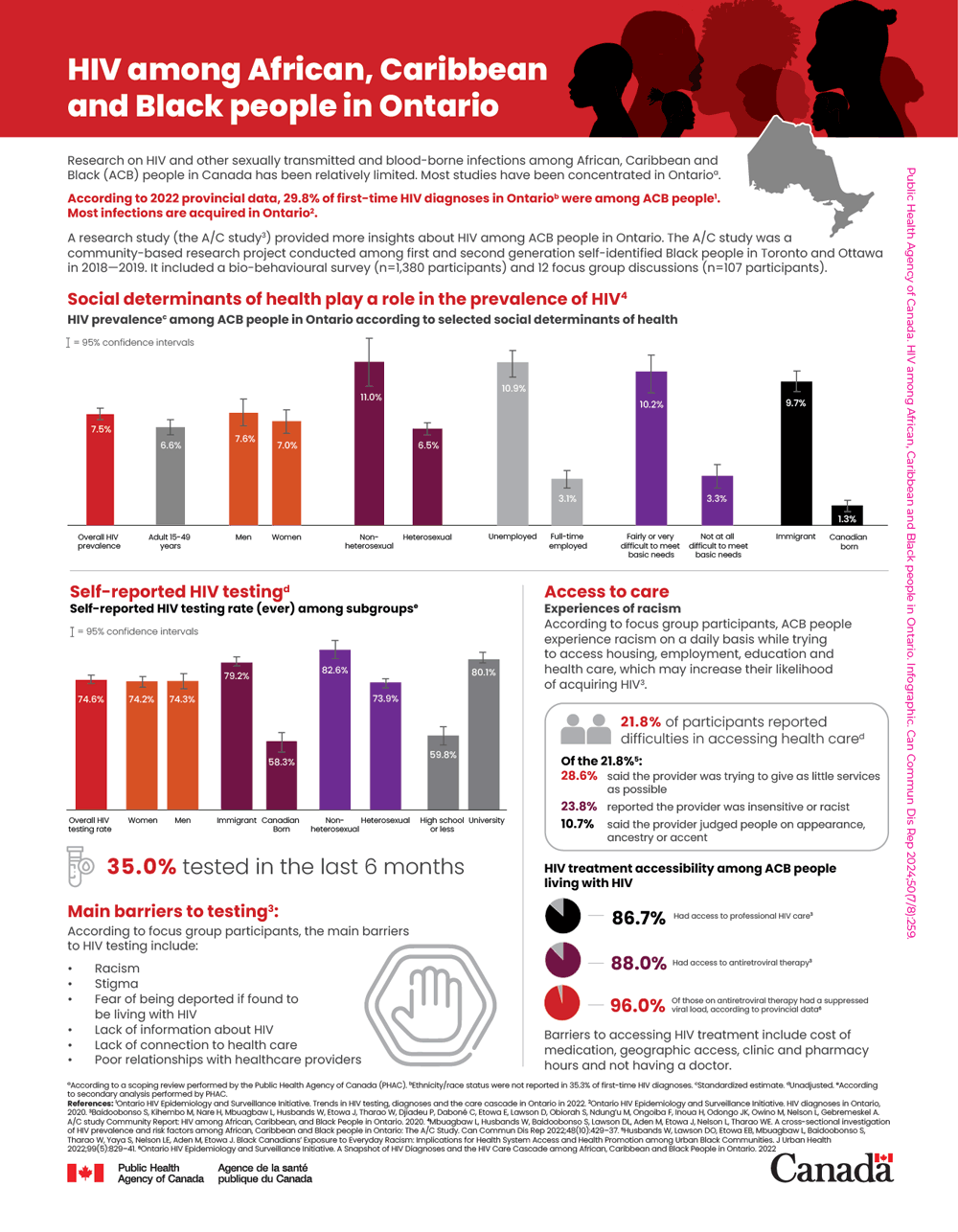
Research on HIV and other sexually transmitted and other blood-borne infections among African, Caribbean and Black (ACB) people in Canada has been relatively limited. Most studies have been concentrated in OntarioFootnote a.
According to 2022 provincial data, 29.8% of first-time HIV diagnoses in OntarioFootnote b were among ACB peopleFootnote 1. Most infections are acquired in OntarioFootnote 2.
A research study (the A/C studyFootnote 3) provided more insights about HIV among ACB people in Ontario. The A/C study was a community-based research project conducted among first and second generation self-identified Black people in Toronto and Ottawa in 2018–2019. It included a bio-behavioural survey (n=1,380 participants) and 12 focus group discussions (n=107 participants).
Social determinants of health play a role in the prevalence of HIVFootnote 4
| Social determinants of health | HIV prevalence | 95% confidential intervals |
|---|---|---|
| Overall HIV prevalence | 7.5% | 7.1%–8.0% |
| Adult 15–49 years | 6.6% | 6.1%–7.1% |
| Men | 7.6% | 6.8%–8.5% |
| Women | 7.0% | 6.3%–7.8% |
| Non-heterosexual | 11.0% | 9.5%–12.6% |
| Heterosexual | 6.5% | 6.0%–7.1% |
| Unemployed | 10.9% | 10.0%–11.8% |
| Full-time employed | 3.1% | 2.6%–3.8% |
| Fairly or very difficult to meet basic needs | 10.2% | 8.9%–11.7% |
| Not at all difficult to meet basic needs | 3.3% | 2.6%–4.1% |
| Immigrant | 9.7% | 9.0%–10.4% |
| Canadian born | 1.3% | 0.9%–1.8% |
Abbreviation: ACB, African, Caribbean and Black |
||
Self-reported HIV testingFootnote d
| Subgroups | HIV test prevalence | 95% confidential intervals |
|---|---|---|
| Overall HIV testing rate | 74.6% | 72.1%–76.9% |
| Women | 74.2% | 71.0%–77.3% |
| Men | 74.3% | 70.0%–78.2% |
| Immigrant | 79.2% | 76.6%–81.7% |
| Canadian-born | 58.3% | 52.3%–64.1% |
| Non-heterosexual | 82.6% | 75.0%–87.9% |
| Heterosexual | 73.9% | 71.1%–76.6% |
| High school or less | 59.8% | 54.2%–65.3% |
| University | 80.1% | 77.0%–83.0% |
- 35.0% tested in the last 6 months
Main barriers to testingFootnote 3
According to focus group participants, the main barriers to HIV testing include:
- Racism
- Stigma
- Fear of being deported if found to be living with HIV
- Lack of information about HIV
- Lack of connection to health care
- Poor relationships with healthcare providers
Access to care
Experiences of racism
According to focus group participants, ACB people experience racism on a daily basis while trying to access housing, employment, education and health care, which may increase their likelihood of acquiring HIVFootnote 3.
- 21.8% of participants reported difficulties in accessing health careFootnote d
Of the 21.8%Footnote 5:
- 28.6% said the provider was trying to give as little services as possible
- 23.8% reported the provider was insensitive or racist
- 10.7% said the provider judged people on appearance, ancestry or accent
HIV treatment accessibility among ACB people living with HIV
- 86.7% had access to professional HIV careFootnote 3
- 88.0% had access to antiretroviral therapyFootnote 3
- 96.0% of those on antiretroviral therapy had a suppressed viral load according to provincial dataFootnote 6
Barriers to accessing HIV treatment include cost of medication, geographic access, clinic and pharmacy hours, and not having a doctor.
Footnotes
- Footnote a
-
According to a scoping review performed by the Public Health Agency of Canada (PHAC)
- Footnote b
-
Ethnicity/race status were not reported in 35.3% of first-time HIV diagnoses
- Footnote c
-
Standardized estimate
- Footnote d
-
Unadjusted
- Footnote e
-
According to secondary analysis performed by PHAC
References
- Footnote 1
-
Ontario HIV Epidemiology and Surveillance Initiative. Trends in HIV testing, diagnoses and the care cascade in Ontario in 2022.
- Footnote 2
-
Ontario HIV Epidemiology and Surveillance Initiative. HIV diagnoses in Ontario, 2020.
- Footnote 3
-
Baidoobonso S, Kihembo M, Nare H, Mbuagbaw L, Husbands W, Etowa J, Tharao W, Djiadeu P, Daboné C, Etowa E, Lawson D, Obiorah S, Ndung'u M, Ongoiba F, Inoua H, Odongo JK, Owino M, Nelson L, Gebremeskel A. A/C study Community Report: HIV among African, Caribbean, and Black People in Ontario. 2020.
- Footnote 4
-
Mbuagbaw L, Husbands W, Baidoobonso S, Lawson DL, Aden M, Etowa J, Nelson L, Tharao WE. A cross-sectional investigation of HIV prevalence and risk factors among African, Caribbean and Black people in Ontario: The A/C Study. Can Commun Dis Rep 2022;48(10):429–37.
- Footnote 5
-
Husbands W, Lawson DO, Etowa EB, Mbuagbaw L, Baidoobonso S, Tharao W, Yaya S, Nelson LE, Aden M, Etowa J. Black Canadians' Exposure to Everyday Racism: Implications for Health System Access and Health Promotion among Urban Black Communities. J Urban Health 2022;99(5):829–41.
- Footnote 6
-
Ontario HIV Epidemiology and Surveillance Initiative. A Snapshot of HIV Diagnoses and the HIV Care Cascade among African, Caribbean and Black People in Ontario. 2022
Public Health Agency of Canada. HIV among African, Caribbean and Black people in Ontario. Infographic. Can Commun Dis Rep 2024;50(7/8):259.
