Chronic Diseases and Injuries in Canada
Chronic Diseases and Injuries in Canada
Volume 31 · Supplement 1 · Fall 2011
Patterns of Health Services Utilization in Rural Canada
Results
National overview: access to and utilization of health care services
Access
According to the HSAS 2000–2001, with the exception of the No MIZ areas, similar proportions of respondents in urban and rural areas reported having a regular family doctor (CMA/CA: 87.3%; Strong, Moderate, Weak MIZ: 88.3% to 90.6%; No MIZ: 76.1%). Among those with no regular family doctor, between 35 % and 61 % of rural residents, compared with 13.2 % of urban residents, reported lack of availability of a family doctor as the reason. Aside from Weak MIZ areas, where significantly more residents reported difficulties in getting routine care (14.8%), similar proportions of respondents in urban and rural areas reported such difficulties (range: 9.7% to 11.6%) (Figure 2). After controlling for sex, age, chronic disease, health behaviours and socio-demographic and economic factors, multivariate analysis indicated that place of residence had an independent effect (odds ratio [OR] = 2.65, 95% CI: 1.51 to 4.64) on not having a family doctor only for No MIZ areas.
Figure 2
Age-standardized proportions of Canadians 15 years of age or over who required access to routine or ongoing health care services, by place of residence, 2000–2001
Figure 2 - Text equivalent
Age-standardized proportions of Canadians 15 years of age or over who required access to routine or ongoing health care services, by place of residence, 2000–2001
According to the HSAS 2000–2001, with the exception of the No MIZ areas, similar proportions of respondents in urban and rural areas reported having a regular family doctor (CMA/CA: 87.3%; Strong, Moderate, Weak MIZ: 88.3% to 90.6%; No MIZ: 76.1%). Between 35.0% and 61.0% of rural residents, compared with 13.2% of urban residents, reported having no family doctor because there were none available. Aside from Weak MIZ areas, where significantly more residents reported difficulties in getting routine care (14.8%), similar proportions of respondents in urban and rural areas reported such difficulties (range: 9.7% to 11.6%).
Data source: Health Services Access Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Significantly greater proportions of HSAS respondents living in Weak MIZ areas reported requiring immediate health care services for minor health problems during the year prior to the survey, compared with their urban counterparts (CMA/CA: 32.9%; Weak MIZ: 39.6%). As well, significantly greater proportions of respondents living in No MIZ areas reported difficulties accessing immediate health services due to lack of availability in the area, lack of availability at the time of day, or transportation problems (CMA/CA: 8.8%; No MIZ: 61.4%) (Figure 3).
Figure 3
Age-standardized proportions of Canadians 15 years of age or over who required access to immediate health services for minor health problems in the past year, by place of residence, 2000–2001
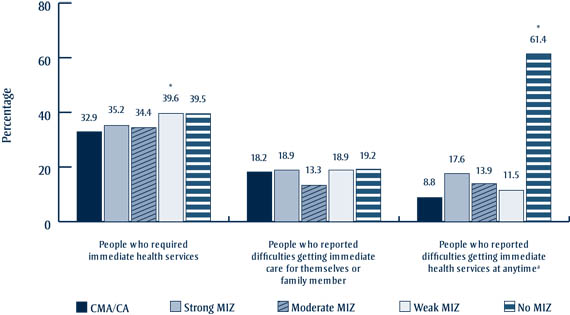
Figure 3 - Text equivalent
Age-standardized proportions of Canadians 15 years of age or over who required access to immediate health services for minor health problems in the past year, by place of residence, 2000–2001
Significantly greater proportions of HSAS respondents living in Weak MIZ areas reported requiring immediate health care services for minor health problems during the year prior to the survey, compared with their urban counterparts (CMA/CA: 32.9%; Weak MIZ: 39.6%). As well, significantly greater proportions of respondents living in No MIZ areas reported difficulties accessing immediate health services due to lack of availability in the area, lack of availability at the time of day, or transportation problems (CMA/CA: 8.8%; No MIZ: 61.4%).
Data source: Health Services Access Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA. a Reasons for not receiving health care: health care services not available in the area; not available at time required; or transportation problems.
Waiting time for specialists and non- emergency surgery
With regard to waiting for specialized care, 57.0% to 77.7% of HSAS respondents reported waiting months for health care services in 2000–2001, and the proportions did not vary significantly according to place of residence (Figure 4). Significantly higher proportions of rural Canadians living in Strong MIZ areas felt that the waiting times were unacceptable, compared with those living in urban areas (CMA/CA: 31.3%; Strong MIZ: 47.5%). The proportion of No MIZ residents reporting unacceptable waiting times was as high as in Strong MIZ areas but did not reach a statistically significant level.
Figure 4
Age-standardized proportions of Canadians 15 years of age or over who reported waiting for months to access specialized and non-emergency surgery, by place of residence, 2000–2001
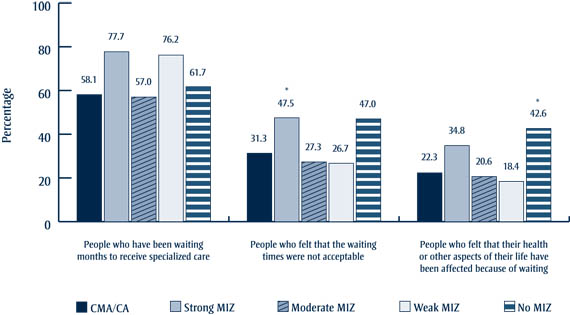
Figure 4 - Text equivalent
Age-standardized proportions of Canadians 15 years of age or over who reported waiting for months to access specialized and non-emergency surgery, by place of residence, 2000–2001
With regard to waiting for specialized care, 57.0% to 77.7% of HSAS respondents reported waiting months for health care services in 2000–2001, and the proportions did not vary significantly according to place of residence (Figure 4). Significantly higher proportions of rural Canadians living in Strong MIZ areas felt that the waiting times were unacceptable, compared with those living in urban areas (CMA/CA: 31.3%; Strong MIZ: 47.5%). The proportion of No MIZ residents reporting unacceptable waiting times was as high as in Strong MIZ areas but did not reach a statistically significant level.
Data source: Health Services Access Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Health care resources and health services utilization
Overall, urban areas had higher FP-to-population ratios than rural areas (10.1 versus 6.9 per 10 000), though in Weak MIZ areas and RST territories (the non-CMA/CA parts of Yukon, the Northwest Territories and Nunavut, i.e. all areas within the Territories outside of Yellowknife and Whitehorse), the ratios were similar to or even higher than in urban areas (10.2 and 14.7 per 10 000, respectively). The differences were much greater with respect to specialist-to-population ratios: 11.0 per 10 000 in urban areas versus 1.0 per 10 000 overall in rural areas (Table 4).
| Number of FPs | FPs per 10 000 (population) | Number of medical and surgical specialists | Specialists per 10 000 (population) | Population estimates | |
|---|---|---|---|---|---|
| CMA/CA | 24 133 | 10.1 | 26 276 | 11.0 | 23 929 310 |
| All MIZ and RST areas | 4 244 | 6.9 | 626 | 1.0 | 6 447 995 |
| Strong MIZ | 533 | 3.5 | 70 | 0.5 | 1 524 335 |
| Moderate MIZ | 1 466 | 6.4 | 172 | 0.8 | 2 283 225 |
| Weak MIZ | 2 008 | 10.2 | 337 | 1.7 | 1 961 235 |
| No MIZ | 156 | 4.6 | 31 | 0.9 | 579 090 |
| RST territoriesb | 81 | 14.7 | 16 | 2.9 | 100 110 |
| Total | 28 377 | 9.5 | 26 902 | 8.9 | 30 377 305 |
| Data source: Southam Medical Database, Canadian Institute for Health Information, 2001. Abbreviations: CA, Census Agglomeration; ,CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone; RST, Rural and Small Town. a Excludes residents and physicians with "no publication" status (see Methodological Notes in the CIHI report Supply, Distribution and Migration of Canadian Physicians, 2003); includes physicians who provide both clinical and/or non-clinical services; includes certificants of the College of Family Physicians of Canada (CFPC), non-CFPC general practitioners, foreign-certified specialists and other non-certified specialists. b The non-CMA/CA parts of Yukon, the Northwest Territories and Nunavut, i.e. all areas within the territories outside of Yellowknife and Whitehorse. |
|||||
CCHS 2000–2001 data show that over 75% of male respondents reported receiving physician care in the 12 months prior to the survey. There were no statistically significant differences according to area of residence in the proportions of men who reported that they had received the services of a family doctor (range: 66.0% to 77.2%), but for medical specialist care in the previous 12 months, men in Moderate and Weak MIZ areas fared worse (8.6% and 7.6%, respectively) than those in urban areas (13.1%) (Figure 5).
Figure 5
Age-standardized proportions of Canadian men 12 years of age or over who reported using physician services in the past 12 months, by type of physician and place of residence, 2000–2001
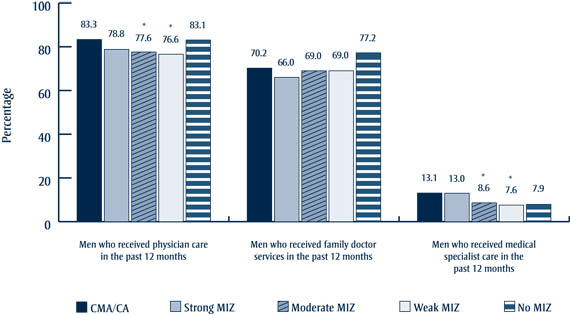
Figure 5 - Text equivalent
Age-standardized proportions of Canadian men 12 years of age or over who reported using physician services in the past 12 months, by type of physician and place of residence, 2000–2001
CCHS 2000–2001 data show that over 75% of male respondents reported receiving physician care in the 12 months prior to the survey. There were no statistically significant differences according to area of residence in the proportions of men who reported that they had received the services of a family doctor (range: 66.0% to 77.2%), but for medical specialist care in the previous 12 months, men in Moderate and Weak MIZ areas fared worse (8.6% and 7.6%, respectively) than those in urban areas (13.1%).
Data source: Canadian Community Health Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
There were no statistically significant differences in the proportions of women who reported receiving care from family doctors, except for a higher proportion of those living in Weak MIZ areas (CMA/CA: 74.6%; Weak MIZ: 78.5%). Among those who reported receiving care from specialists, women living in weak MIZ areas reported significantly lower specialist utilization rates, compared with their urban counterparts (CMA/CA: 15.1%; Weak MIZ: 8.4%) (Figure 6).
Figure 6
Age-standardized proportions of women 12 years of age or over who reported using physician services in the past 12 months, by type of physician and place of residence, Canada, 2000–2001
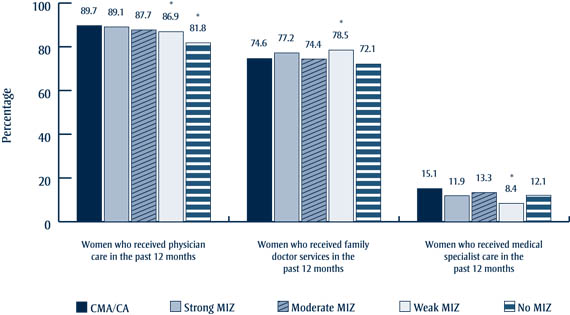
Figure 6 - Text equivalent
Age-standardized proportions of women 12 years of age or over who reported using physician services in the past 12 months, by type of physician and place of residence, Canada, 2000–2001
There were no statistically significant differences in the proportions of women who reported receiving care from family doctors, except for a higher proportion of those living in Weak MIZ areas (CMA/CA: 74.6%; Weak MIZ: 78.5%). Among those who reported receiving care from specialists, women living in weak MIZ areas reported significantly lower specialist utilization rates, compared with their urban counterparts (CMA/CA: 15.1%; Weak MIZ: 8.4%).
Data source: Canadian Community Health Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Among respondents to the CCHS 2000–2001 who reported having consulted a physician in the 12-month period prior to the survey, significantly greater proportions of men in rural areas reported not having consulted a family doctor; a similar pattern held among women, with the exception that there was no statistically significant difference between Strong MIZ areas and urban areas. Among men, similar proportions of rural and urban residents reported four or more consultations with family doctors. A greater proportion of women than men in all geographic categories had visited their family doctor four or more times. Compared with urban areas and with the exception of Strong MIZ areas, fewer men in all rural areas reported having had at least one consultation with other medical doctors. Fewer women in all rural areas reported consulting other medical doctors (Table 5).
| Consultation with a doctor |
CMA/CA | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | |
|---|---|---|---|---|---|---|
| People reporting 0 consultations with a family doctor | Men | 26.5 (25.9–27.2) |
31.6 (29.7–33.4)* |
29.4 (27.9–30.8)* |
29.2 (28.0–30.5)* |
33.6 (29.8–37.5)* |
| Women | 15.3 (14.8–15.8) |
16.5 (15.0–17.9) |
17.4 (16.2–18.6)* |
17.3 (16.3–18.3)* |
20.3 (17.2–23.4)* |
|
| People reporting 4 or more consultations with a family doctor | Men | 23.1 (22.5–23.7) |
21.1 (19.6–22.6) |
22.4 (21.2–23.6) |
24.1 (23.0–25.2) |
23.7 (20.8–26.6) |
| Women | 34.4 (33.8–35.4) |
33.2 (31.4–35.0) |
34.9 (33.5–36.2) |
37.2 (36.0–38.4)* |
38.3 (34.9–41.6) |
|
| People reporting 1 or more consultations with other medical doctors | Men | 24.0 (23.4–24.6) |
23.5 (21.8–25.1) |
20.2 (18.9–21.4)* |
19.0 (17.9–20.0)* |
16.1 (13.4–18.9)* |
| Women | 34.5 (33.9–35.1) |
31.7 (29.9–33.4)* |
29.5 (28.2–30.9)* |
27.1 (26.0–28.3)* |
30.4 (27.0–33.8)* |
|
Data source: Canadian Community Health Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA. |
||||||
According to the CCHS 2000–2001, residents of Moderate, Weak and No MIZ areas were significantly more likely to report a consultation with a nurse than residents of urban areas (Table 6). The proportions that had visited a dentist or received community-based care (i.e. services provided outside a hospital or doctor’s office) in the 12 months before the survey were significantly lower in rural than in urban areas, with the exception of community-based care in No MIZ areas (Table 6).
| Consultations with health care providers | CMA/CA | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | |
|---|---|---|---|---|---|---|
| People reporting 1 or more consultations with nurse | Men | 7.8 (7.4–8.1) |
7.7 (6.7–8.8) |
9.1 (8.2–10.0)* |
10.4 (9.5–11.3)* |
10.5 (8.4–12.6)* |
| Women | 11.6 (11.2–12.0) |
12.5 (11.3–13.8) |
13.1 (12.2–14.1)* |
14.1 (13.3–15.0)* |
20.3 (17.3–23.4)* |
|
| People reported 1 or more consultations with dentist | Men | 59.8 (59.1–60.6) |
54.1 (25.2–56.1)* |
46.6 (45.1–48.2)* |
48.6 (47.2–49.9)* |
44.1 (40.3–47.8)* |
| Women | 64.2 (63.6–64.8) |
58.5 (56.7–60.3)* |
53.6 (52.2–55.1)* |
53.5 (52.3–54.7)* |
45.4 (41.7–49.1)* |
|
| People who received community-based care in the previous 12 months | Men | 15.4 (14.2–16.7) |
9.5 (7.1–12.0)* |
11.1 (8.6–13.6)* |
10.1 (8.1–12.0)* |
10.7 (5.0–16.4) |
| Women | 19.0 (17.9–20.1) |
14.2 (11.6–16.7)* |
12.5 (10.5–14.5)* |
13.6 (11.7–15.4)* |
15.6 (9.7–21.5) |
|
Data source: Canadian Community Health Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA. |
||||||
With respect to hospital care, data from the HMDB for 2001–2002 indicate higher hospitalization rates among all rural residents compared with urban residents, and the differences between urban and all rural areas were all statistically significant (Table 7).
| Sex | CMA/CA | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|
| Men | 67.8 (67.7–68.0) |
72.0 (71.4–72.7)* |
83.8 (83.2–84.4)* |
107.2 (106.5–107.8)* |
116.6 (115.0–118.3)* |
| Women | 88.2 (88.0–88.4) |
98.6 (97.7–99.4)* |
111.1 (110.3–111.8)* |
140.0 (139.2–140.7)* |
161.3 (159.2–163.4)* |
Data source: Hospital Morbidity Database, 2001–2002, Canadian Institute for Health Information. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. a Pan-Canadian totals exclude Quebec because of insufficient geographic coding of source data. * Statistically significant at p < .05; reference group is CMA/CA. |
|||||
The results of the CCHS 2000–2001 agree with these findings: significantly greater proportions of rural residents reported that they had received hospital care in the 12 months prior to the survey. In general, there were few differences in the proportions of people receiving in-patient care, but significantly more rural residents in Strong MIZ (women), Moderate MIZ (men), Weak MIZ (men and women) and No MIZ areas (women) had had outpatient care.
The average lengths of hospital stay increased with increasing age, but decreased with increasing rurality across all age-sex groups. The patterns of lengths of hospital stay among men differed according to age: average lengths of stay for men aged 20 to 44 years were similar in rural and urban areas; men aged 45 to 64 years living in Weak MIZ and No MIZ areas had significantly shorter hospital stays than their urban counterparts; the average lengths of hospital stay among men aged 65 to 74 years living in rural areas were significantly shorter compared with their urban counterparts; and the average lengths of hospital stay for men aged 75 years or more living in all MIZ areas were shorter than for similarly aged men in urban areas (Table 8).
Average lengths of hospital stay among women living in rural areas were shorter than for their urban counterparts, with the shortest lengths of stay reported by those in No MIZ areas. There was one exception to this pattern: no difference was found between women aged 65 to 74 years living in Moderate MIZ areas and those in urban areas (Table 8).
| Age group (years) | Sex | CMA/CA | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|---|
| All ages | Men | 8.58 (7.97–9.18) |
7.43 (6.91–7.95)* |
6.85 (6.58–7.19)* |
6.65 (6.33–6.96)* |
6.29 (5.97–6.60)* |
| Women | 8.28 (7.92–8.64) |
6.87 (6.53–7.21)* |
6.92 (6.63–7.20)* |
6.27 (6.04–6.49)* |
6.17 (5.83–6.50)* |
|
| 20–44 | Men | 5.91 (5.63–6.20) |
5.40 (4.84–5.96) |
5.21 (4.70–5.72) |
5.27 (4.46–6.09) |
5.40 (4.79–6.00) |
| Women | 5.33 (5.07–5.59) |
4.58 (4.17–4.99)* |
4.26 (4.04–4.48)* |
4.30 (3.91–4.69)* |
4.01 (3.71–4.31)* |
|
| 45–64 | Men | 8.24 (7.69–8.79) |
7.17 (6.08–8.26) |
7.21 (6.51–7.91) |
6.43 (6.09–6.76)* |
6.15 (5.64–6.67)* |
| Women | 7.81 (7.38–8.24) |
6.76 (6.21–7.31)* |
6.57 (6.18–6.96)* |
6.02 (5.72–6.32)* |
6.32 (5.81–6.83)* |
|
| 65–74 | Men | 10.7 (9.85–11.6) |
7.98 (7.39–8.58)* |
8.66 (8.03–9.28)* |
7.94 (7.39–8.49)* |
7.55 (6.70–8.41)* |
| Women | 10.9 (10.0–11.8) |
8.23 (7.59–8.87)* |
9.74 (8.24–11.2) |
8.12 (7.29–8.95)* |
8.15 (7.06–9.24)* |
|
| 75+ | Men | 14.5 (13.7–15.2) |
12.6 (11.2–14.1) |
10.46 (9.85–11.06)* |
11.03 (10.1–12.0)* |
9.93 (8.90–11.0)* |
| Women | 16.3 (14.8–17.8) |
12.0 (11.0–13.1)* |
12.2 (11.4–13.0)* |
10.9 (10.2–11.6)* |
10.5 (9.27–11.7)* |
|
Data source: Hospital Morbidity Database, 2001–2002, Canadian Institute for Health Information. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. a Pan-Canadian totals exclude Quebec due to insufficient geographic coding of source data. * Statistically significant at p < .05; reference group is CMA/CA. |
||||||
Multivariate regression analysis of the CCHS 2000–2001 data showed that place of residence had an independent effect on reported hospitalization during the 12 months prior to the survey in all rural categories except Strong MIZ areas. The risks of hospitalization for these rural residents were 10% to 27% greater than for residents of urban areas. Other independent risk factors were being female, having less than high income, having less than a secondary education degree, being in poor health and having a chronic disease. Those who were aged 45 or over, were non-white and smoked all had lower risks of being admitted to hospital. The direction of risk for some factors was different when the analysis was broken down by sex (Table 9).
| Odds ratios (95% confidence intervalsa) | ||||
|---|---|---|---|---|
| Men | Women | All | ||
| Place of residence | CMA/CA | 1.0 | 1.0 | 1.0 |
| Strong MIZ | 1.06 (0.90–1.25) |
1.11 (0.96–1.28) |
1.09 (0.98–1.22) |
|
| Moderate MIZ | 1.10 (0.96–1.25) |
1.10 (0.98–1.22) |
1.10 (1.01–1.20)* |
|
| Weak MIZ | 1.18 (1.04–1.33)* |
1.16 (1.06–1.28)* |
1.18 (1.09–1.27)* |
|
| No MIZ | 1.35 (1.05–1.73)* |
1.16 (0.93–1.45) |
1.27 (1.08–1.49)* |
|
| Sex | Male | 1.0 | ||
| Female | – | – | 1.46 (1.37–1.55)* |
|
| Age | <45 | 1.0 | 1.0 | 1.0 |
| >=45 | 1.36 (1.22–1.52)* |
0.56 (0.52–0.61)* |
0.78 (0.73–0.84)* |
|
| Race | White | 1.0 | 1.0 | 1.0 |
| Non-white | 0.61 (0.48–0.77)* |
0.76 (0.65–0.90)* |
0.70 (0.61–0.81)* |
|
| Incomeb | High | 1.0 | 1.0 | 1.0 |
| Upper high | – | 1.21 (1.07–1.36)* |
1.15 (1.05–1.26)* |
|
| Low middle | 1.21 (1.07–1.37)* |
1.35 (1.19–1.52)* |
1.31 (1.18–1.44)* |
|
| Low | 1.51 (1.29–1.77)* |
1.52 (1.33–1.73)* |
1.49 (1.34–1.66)* |
|
| Education | Post-secondary degree | 1.0 | 1.0 | 1.0 |
| Secondary/some post-secondary | 1.21 (1.04–1.33)* |
0.87 (0.80–0.94)* |
– | |
| Less than secondary | 1.42 (1.25–1.60)* |
– | 1.13 (1.05–1.22)* |
|
| Self-rated health | Good/excellent | 1.0 | 1.0 | 1.0 |
| Poor/fair | 2.66 (2.35–3.00)* |
2.75 (2.51–3.02)* |
2.76 (2.56–2.98)* |
|
| Chronic disease | No | 1.0 | 1.0 | 1.0 |
| Yes | 2.46 (2.22–2.74)* |
1.78 (1.63–1.95)* |
2.00 (1.87–2.14)* |
|
| Smoking | No | 1.0 | 1.0 | |
| Yes | – | 0.90 (0.83–0.98)* |
0.90 (0.84–0.96)* |
|
Data source: Canadian Community Health Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone; –, excluded during modelling. a Confidence intervals were determined using 500 Bootstrap weights to account for the complex survey design. b Income classification was based on total household income and the number of people living in the household. * Statistically significant at p < .05. |
||||
Satisfaction of health services users
The 2000–2001 CCHS asked participants about quality of care and user satisfaction in three types of health services: overall health care, physician care and community-based health care. No statistically significant differences were found between urban and rural populations in the perceived quality of and satisfaction with health care, or in the quality of and satisfaction with physician care. When asked about the quality of community-based health services, a lower proportion of men living in Weak MIZ areas reported the quality of care as poor or fair, compared with men in urban areas (CMA/CA: 24.6%; Weak MIZ: 10.7%). No statistically significant differences were found between women in urban and rural areas on this subject, although a significantly smaller proportion of women living in Weak MIZ areas than those in urban areas were dissatisfied with community-based services (CMA/CA: 12.8%; Weak MIZ: 6.9%) (Table 10).
| Sex | CMA/CA | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | |
|---|---|---|---|---|---|---|
| Overall health care services | ||||||
| People who reported receiving poor/fair quality of health care | Men | 16.3 (15.1–17.6) |
16.1 (13.1–19.1) |
14.1 (11.4–16.8) |
14.5 (12.4–16.6) |
24.2 (15.8–32.6) |
| Women | 15.4 (14.4–16.5) |
12.3 (10.0–14.5) |
13.2 (11.1–15.3) |
14.3 (12.6–16.1) |
17.2 (11.5–22.9) |
|
People who reported being "neither satisfied nor dissatisfied"or "somewhat dissatisfied"with the health care they received |
Men | 13.2 (12.0–14.4) |
13.5 (10.5–16.4) |
12.1 (9.6–14.6) |
13.2 (10.7–15.6) |
8.9 (3.4–14.3) |
| Women | 12.3 (11.3–13.3) |
10.3 (8.1–12.4) |
12.3 (10.1–14.6) |
11.4 (9.7–13.1) |
10.0 (5.2–14.8) |
|
| Physician care | ||||||
| People who reported receiving poor/fair quality of physician care | Men | 11.6 (10.4–12.9) |
11.6 (8.4–14.8) |
9.0 (6.6–11.4) |
9.2 (7.1–11.3) |
13.6 (5.4–21.8) |
| Women | 9.8 (8.9–10.7) |
8.6 (6.5–10.7) |
8.1 (6.3–9.9) |
8.7 (7.2–10.2) |
12.6 (7.1–18.1) |
|
People who reported being "neither satisfied nor dissatisfied"or "somewhat dissatisfied"with the physician care they received |
Men | 7.9 (6.9–8.9) |
8.7 (6.0–11.4) |
6.3 (4.5–8.1) |
5.6 (3.9–7.4) |
10.3 (2.8–17.8) |
| Women | 7.4 (6.6–8.1) |
6.6 (4.6–8.7) |
6.5 (4.5–8.4) |
6.8 (5.3–8.3) |
7.0 (3.1–11.0) |
|
| Community-based care | ||||||
| People who reported receiving poor/fair quality of community-based care in the past 12 months | Men | 24.6 (20.8–28.4) |
21.1 (9.7–32.6) |
13.9 (5.1–22.7) |
10.7 (5.8–15.5)* |
23.7 (13.5–33.8) |
| Women | 20.6 (17.9–23.3) |
16.3 (8.0–24.7) |
14.7 (7.7–21.7) |
12.9 (8.0–17.9) |
14.0 (3.8–24.2) |
|
People who reported being "neither satisfied nor dissatisfied"or "somewhat dissatisfied"with the community-based care they received |
Men | 15.2 (11.7–18.7) |
15.6 (6.0–25.2) |
8.5 (1.0–16.0) |
8.3 (3.3–13.3) |
5.9 (0.1–12.0) |
| Women | 12.8 (10.5–15.0) |
9.3 (3.6–15.0) |
12.9 (6.1–19.8) |
6.9 (3.5–10.2)* |
12.5 (4.0–21.0) |
|
Data source: Health Services Access Survey 2000–2001, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA. |
||||||
Provincial patterns in health care resources and utilization
The findings reported in the previous section are based mostly on self-reported data and are at the national level. In this section, administrative data (such as physician billing data) from three provinces are used to describe rural health services utilization patterns.
Rates of physician visits and hospital admission obtained from physician billing and hospital discharge data were analyzed for Nova Scotia, Ontario and British Columbia. In Ontario and British Columbia, the vast majority of the population lives in urban areas (87% and 86.2%, respectively); in Nova Scotia, on the other hand, 63.3% live in urban areas and 23.4%—almost a quarter of the population—live in Weak and No MIZ areas, as compared with 2.6% in Ontario and 7.2% in British Columbia (Table 11).
| Population and percent distribution (within 2001 boundaries) | ||||||
|---|---|---|---|---|---|---|
| Nova Scotia | Ontario | British Columbia | ||||
| Number | % | Number | % | Number | % | |
| Urban (CMA/CA) | 574 696 | 63.3 | 9 925 949 | 87.0 | 3 369 035 | 86.2 |
| RST areas | 333 311 | 36.7 | 1 484 097 | 13.0 | 538 703 | 13.8 |
| Strong MIZ | 22 209 | 2.4 | 695 979 | 6.1 | 71 044 | 1.8 |
| Moderate MIZ | 98 571 | 10.9 | 489 378 | 4.3 | 188 811 | 4.8 |
| Weak MIZ | 207 881 | 22.9 | 270 527 | 2.4 | 236 892 | 6.1 |
| No MIZ | 4 650 | 0.5 | 28 213 | 0.2 | 41 956 | 1.1 |
| Total population | 908 007 | 11 410 046 | 3 907 738 | |||
| Total area | 55 284 km2 | 1 076 395 km2 | 944 735 km2 | |||
Data sources: Statistics Canada. Census of Population, 2001; Natural Resources Canada. Canada Centre for Remote Sensing, GeoAccess Division, 2001. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone; RST, Rural and Small Town. |
||||||
Nova Scotia
According to CIHI data, between 1991 and 2001, the number of FPs in Nova Scotia increased by only eight, and the FP-to-population ratio decreased in both rural and urban areas. In 2001, there were 11.6 FPs per 10 000 in CMA/CA areas, higher than in any of the rural areas (7.1 per 10 000 in all rural areas combined). From 1997 to 2002, residents of Strong MIZ areas were significantly more likely than urban residents to have visited an FP. According to figure 7, male residents of Strong MIZ area were significantly more likely than urban residents to have visited an FP in the first biennial period (1997-98).
Figure 7
Average annual age-standardized physician-visit rates for family physicians, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002
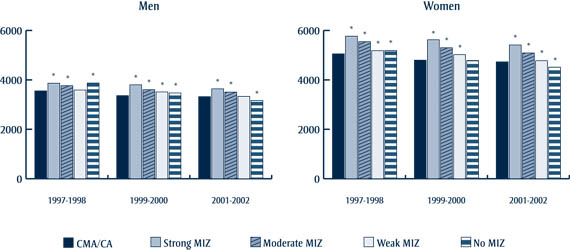
Figure 7 - Text equivalent
Average annual age-standardized physician-visit rates for family physicians, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002
From 1997 to 2002, residents of Strong MIZ areas were significantly more likely than urban residents to have visited an FP. According to figure 7, male residents of Strong MIZ area were significantly more likely than urban residents to have visited an FP in the first biennial period (1997-98).
Data source: Nova Scotia Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
The number of specialists in Nova Scotia increased by 139 between 1991 and 2001, according to CIHI data. The specialist-to-population ratio in urban areas was 13.6 per 10 000 in 2001, as compared with 2.6 per 10 000 in all rural areas combined. Among both men and women, the annual rate of those who had visited a medical specialist over the period 1997–2002 was significantly lower in all rural areas, with a decreasing rate by degree of rurality, with the exception of men in No MIZ areas (Figure 8). In contrast, lower visit rates to surgical specialists were observed for all rural areas except No MIZ areas among men in 1999–2000 and 2001–2002 and No and Moderate MIZ areas among women from 1997 to 2002 (Figure 9).
Figure 8
Average annual age-standardized physician-visit rates for medical specialists, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002
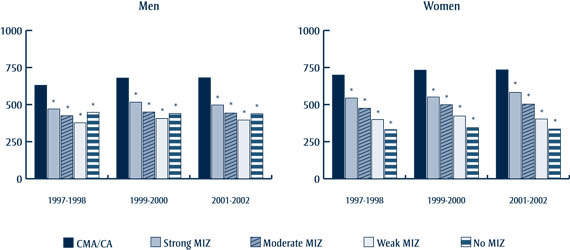
Figure 8 - Text equivalent
Average annual age-standardized physician-visit rates for medical specialists, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002
Among both men and women, the annual rate of those who had visited a medical specialist over the period 1997–2002 was significantly lower in all rural areas, with a decreasing rate by degree of rurality, with the exception of men in No MIZ areas.
Data source: Nova Scotia Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Figure 9
Average annual age-standardized physician-visit rates for surgical specialists, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002

Figure 9 - Text equivalent
Average annual age-standardized physician-visit rates for surgical specialists, per 1000, by place of residence and sex, Nova Scotia, biennial periods, 1997–2002
In contrast, lower visit rates to surgical specialists were observed for all rural areas except No MIZ areas among men in 1999–2000 and 2001–2002 and No and Moderate MIZ areas among women from 1997 to 2002.
Data source: Nova Scotia Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Compared with their urban counterparts, Nova Scotians living in all rural areas had higher all-cause hospital discharge rates in 2001–2002, and these increased with increased degree of rurality (CMA/CA: 89.5 per 1000 for men and 72.8 per 1000 for women; Moderate MIZ: 108.4 per 1000 for men and 87.3 per 1000 for women; No MIZ: 232.3 per 1000 for men and 171.8 per 1000 for women). Lengths of hospital stay during this period were significantly shorter for men in rural areas than men in urban areas (9.01 days in CMA/CA versus 6.39 days in No MIZ); among women the only difference according to area of residence was that those in No MIZ areas spent significantly less time in hospital (6.92 days) than those in urban areas (9.43 days).
Ontario
According to CIHI data, the number of FPs in Ontario decreased by 370 between 1991 and 2001, a decline that affected primarily the urban areas, where the number of FPs per 10 000 fell from 11.0 in 1991 to 9.4 in 1996 and 9.0 in 2001. The corresponding figures per 10 000 for all the MIZ areas combined were 5.9 in 1991, 5.5 in 1996 and 6.3 in 2001. In No MIZ areas, the number increased from 2.1 per 10 000 in 1991 to 5.5 per 10 000 in 2001.
Among men in the various rural areas, the annual rates per 1000 of those who had visited an FP between 1997 and 2002 were similar and significantly lower, on the whole, than among men in urban areas. The rates of FP visits in all rural areas were significantly lower compared with urban areas for both men and women in 2001–2002. Among women in different rural communities, however, with the exception of a decline in No MIZ areas during 2001–2002, the rates increased with greater degree of rurality. Among both men and women, rates of FP visits were significantly lower in Strong MIZ areas than in urban areas throughout the period from 1997 to 2002 (Figure 10).
Figure 10
Average annual age-standardized physician-visit rates for family physicians, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002
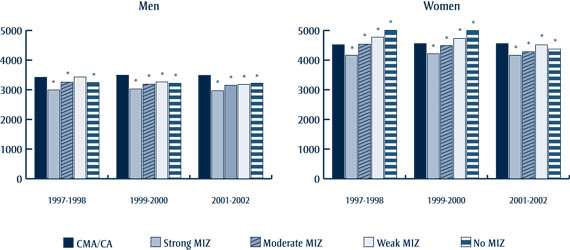
Figure 10 - Text equivalent
Average annual age-standardized physician-visit rates for family physicians, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002
Among men in the various rural areas, the annual rates per 1000 of those who had visited an FP between 1997 and 2002 were similar and significantly lower, on the whole, than among men in urban areas. The rates of FP visits in all rural areas were significantly lower compared with urban areas for both men and women in 2001–2002. Among women in different rural communities, however, with the exception of a decline in No MIZ areas during 2001–2002, the rates increased with greater degree of rurality. Among both men and women, rates of FP visits were significantly lower in Strong MIZ areas than in urban areas throughout the period from 1997 to 2002.
Data source: Ontario Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Between 1991 and 2001, the number of specialists in Ontario increased by 1440, according to CIHI data. The specialist-to-population ratios were stable over time in urban areas (10.6 per 10 000 in 1991, 10.2 in 1996 and 10.6 in 2001) and most of the rural areas (all rural areas combined: 0.7 per 10 000 in 1991, 0.7 in 1996 and 0.9 in 2001). Among both women and men, rates of visit to medical specialists were significantly higher—sometimes twice as high—in urban areas of Ontario than in all rural areas between 1997 and 2002, and generally decreased with increasing degree of rurality (Figure 11). Although visits to surgical specialists also followed this pattern, the rates in No MIZ areas were the highest of all rural areas among women throughout the period from 1997 to 2002 and among men in the period from 2001 to 2002 (Figure 12).
Figure 11
Average annual age-standardized physician-visit rates for medical specialists, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002

Figure 11 - Text equivalent
Average annual age-standardized physician-visit rates for medical specialists, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002
Among both women and men, rates of visit to medical specialists were significantly higher—sometimes twice as high—in urban areas of Ontario than in all rural areas between 1997 and 2002, and generally decreased with increasing degree of rurality.
Data source: Ontario Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
Figure 12
Average annual age-standardized physician-visit rates for surgical specialists, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002
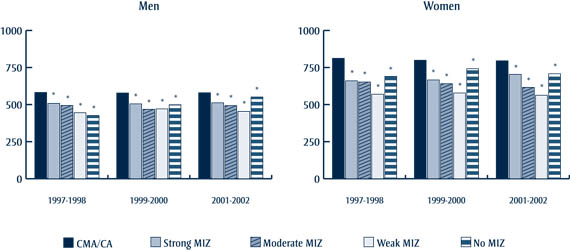
Figure 12 - Text equivalent
Average annual age-standardized physician-visit rates for surgical specialists, per 1000, by place of residence and sex, Ontario, biennial periods, 1997–2002
Although visits to surgical specialists also followed this pattern, the rates in No MIZ areas were the highest of all rural areas among women throughout the period from 1997 to 2002 and among men in the period from 2001 to 2002
Data source: Ontario Physicians Claims files 1997–2002, Statistics Canada. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA.
According to the HMDB, all-cause hospital discharge rates were higher among women than among men in Ontario in 2001–2002. Compared with their urban counterparts, Ontarians living in all rural areas had higher overall hospital discharge rates, and these increased with increasing degree of rurality (men in CMA/CA, 66.4 per 1000 versus 128.6 per 1000 in No MIZ; women in CMA/CA, 86.1 per 1000 versus 178.8 per 1000 in No MIZ). In general, average lengths of hospital stay for men showed no significant differences between rural and urban Ontario in 2001–2002. Among women, those living in Strong and Weak MIZ areas had shorter average lengths of hospital stay than their urban counterparts (CMA/CA: 7.06 days; Strong MIZ: 5.87 days; Moderate MIZ: 6.00 days).
British Columbia
According to CIHI data, the number of FPs in British Columbia increased by 608 in the decade between 1991 and 2001. In urban areas, the ratio of FPs per 10 000 decreased somewhat (from 11.6 in 1991 to 11.0 in 1996 and 11.2 in 2001) but was higher than in all rural areas, with the exception of Weak MIZ areas (12.6 per 10 000 in 2001). During this period, the number of specialists also increased, by 590, and the number per 10 000 was again higher in urban than rural areas (9.6 in urban areas versus 1.6 in all rural areas) in 2001.
With the exception of Strong MIZ areas, where the rates were significantly lower than in urban areas, rural residents had higher hospital discharge rates than their urban counterparts (CMA/CA: 65.4 per 1000 for men, 84.6 per 1000 for women; Moderate MIZ: 70.3 per 1000 for men, 92.2 per 1000 for women; No MIZ: 105.6 per 1000 for men, 151.2 per 1000 for women). Men living in Moderate, Weak and No MIZ areas had significantly shorter lengths of hospital stay than those in urban areas (CMA/CA: 8.04 days; Moderate MIZ: 6.58 days; Weak MIZ: 6.48 days; No MIZ: 5.79 days). Among women, the only difference in lengths of hospital stay according to place of residence was that those in Weak MIZ areas were in hospital for a significantly shorter time (6.06 days) compared with women in urban areas (8.00 days).
Utilization patterns by disease in three provinces
Data on physician visits and hospitalization (age-standardized rates) for selected diseases categories and diseases in Nova Scotia, Ontario and British Columbia in 2001–2002 were used to calculate the relative probabilities of health services utilization in rural areas compared with urban areas. The conditions analyzed were circulatory diseases, cancer, respiratory diseases, musculoskeletal diseases, mental disorders, diseases of the nervous system and sense organs, and diabetes; physician visits and hospitalization for injuries and poisonings were also examined. Not all conditions could be analyzed for each province because of data extraction problems, particularly in British Columbia, where the analysis of physician visits focused on specific diseases as opposed to broad disease categories.Footnote **
Nova Scotia
In Nova Scotia, the patterns of relative risks of physician visits were highly variable but, in general, residents of Strong MIZ areas had higher risks of physician visits, and those in Weak MIZ and No MIZ areas had lower risks. The pattern for residents of Moderate MIZ varied considerably according to each of the six disease categories analyzed and for injuries and poisonings (Table 12).
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Disease category (ICD-9 diagnostic code) | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
| Relative risks of physician visit | ||||||||
| Circulatory disease (390–459) | ↑ | ↓ | ↓ | ↓ | ↑ | ↓ | ↓ | ↓ |
| Cancers/neoplasms (140–239) | ↑ | ↓ | ↓ | --- | --- | ↓ | ↓ | ↓ |
| Respiratory disease (460–519) | ↑ | ↑ | ↓ | ↓ | ↑ | ↑ | ↓ | ↓ |
| Musculoskeletal system disease (710–739) | ↓ | --- | ↓ | ↓ | ↑ | ↑ | ↓ | ↓ |
| Injuries and poisonings (802–894, 959, 977–998) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↓ | --- |
| Mental disorders (290–319) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ |
| Nervous system and sense organs disease (320–389) | ↓ | ↑ | ↓ | ↓ | --- | ↑ | ↓ | ↓ |
| Relative risks of hospitalization | ||||||||
| Circulatory disease (390–459) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Cancers/neoplasms (140–239) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Respiratory disease (460–519) | ↑ | ↑ | ↑ | ↑ | --- | --- | ↑ | ↑ |
| Musculoskeletal system disease (710–739) | ↑ | ↑ | --- | ↑ | ↑ | ↑ | --- | ↑ |
| Injuries and poisonings (802–894, 959, 977–998) | --- | ↑ | ↑ | ↑ | ↑ | ↑ | --- | ↑ |
| Mental disorders (290–319) | --- | ↓ | ↑ | ↑ | --- | ↓ | ↑ | ↑ |
| Nervous system and sense organs disease (320–389) | ↑ | ↑ | --- | ↑ | ↑ | ↑ | ↑ | ↑ |
Data source: Nova Scotia Physician Claims Files, 2001–2002. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. ↑ Statistically higher relative risk at p < .05; ↓ statistically lower relative risk at p < .05; --- no statistical difference at p < .05; reference group is CMA/CA. |
||||||||
Rural Nova Scotians had consistently lower risks of physician visits for mental disorders than their urban counterparts, but consistently higher physician visits for injuries and poisoning, with the exception of women in Weak and No MIZ areas. (Table 13).
| Disease category (ICD-9 diagnostic code) | Sex | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|
| Mental disorders (290–319) | Men | 0.75 (0.73–0.78)* |
0.84 (0.83–0.85)* |
0.70 (0.69–0.71)* |
0.88 (0.82–0.94)* |
| Women | 0.94 (0.92–0.95)* |
0.89 (0.88–0.90)* |
0.73 (0.72–0.74)* |
0.80 (0.76–0.84)* |
|
| Injuries and poisonings (802–894, 959, 977–998) | Men | 1.19 (1.16–1.23)* |
1.18 (1.16–1.19)* |
1.08 (1.06–1.09)* |
1.21 (1.14–1.28)* |
| Women | 1.22 (1.19–1.25)* |
1.11 (1.09–1.12)* |
0.98 (0.97–0.99)* |
0.96 (0.90–1.03) |
|
Data source: Nova Scotia Physician Claims Files, 2001–2002. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA = 1.00. |
|||||
In terms of hospital discharge rates, rural Nova Scotians had higher relative risks of hospitalization compared with urban Nova Scotians, with the exception of mental disorders for which the results were inconsistent, being significantly higher in Weak and No MIZ areas, but lower in Moderate and Strong MIZ areas (Table 14).
| Disease category (ICD-9 diagnostic code) | Sex | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|
| Mental disorders (290–319) | Men | 0.84 (0.65–1.11) |
0.81 (0.68–0.96)* |
1.37 (1.23–1.53)* |
3.69 (2.58–5.29)* |
| Women | 0.83 (0.62–1.11) |
0.83 (0.70–0.98)* |
1.24 (1.11–1.38)* |
7.56 (5.97–9.58)* |
|
Data source: Hospital Morbidity Database, 2001–2002, Canadian Institute for Health Information. Abbreviations: CMA, Census Metropolitan Area; CA, Census Agglomeration; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA = 1.00. |
|||||
Ontario
The patterns with respect to risks of physician visits and hospitalization in Ontario were fairly consistent: rural residents, regardless of sex, were generally less likely to visit a physician than their urban counterparts, though they were more likely to be hospitalized for the same disease categories and for injuries and poisonings (Table 15). However, compared with their urban counterparts, both male and female rural Ontarians were more likely to visit their physician in the case of injuries and poisonings, with the exception of men and women in Strong MIZ area. As you can see, according to Table 16, both men and women in Strong MIZ area were significantly less likely to visit their physician in the case of injuries and poinsonings.
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Disease category (ICD-9 diagnostic code) | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
| Relative risks of physician visit | ||||||||
| Circulatory diseases (390–459) | ↓ | ↓ | ↓ | --- | ↑ | ↓ | ↓ | ↓ |
| Cancers/neoplasms (140–239) | ↓ | ↓ | ↓ | --- | ↓ | ↓ | ↓ | ↑ |
| Respiratory diseases (460–519) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ |
| Musculoskeletal system diseases (710–739) | ↓ | --- | ↓ | ↓ | ↓ | ↓ | ↓ | --- |
| Injuries and poisonings (802–894, 959, 977–998) | ↓ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ |
| Mental disorders (290–319) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ |
| Nervous system and sense organs diseases (320–389) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ |
| Relative risks of hospitalization | ||||||||
| Circulatory diseases (390–459) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Cancers/neoplasms (140–239) | --- | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Respiratory diseases (460–519) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Musculoskeletal system diseases (710–739) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Injuries and poisonings (802–894, 959, 977–998) | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Mental disorders (290–319) | ↓ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ |
| Nervous system and sense organs diseases (320–389) | --- | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. Reference group is CMA/CA = 1.00; ↑ statistically higher relative risk at p < .05; ↓statistically lower relative risk at p < .05; --- no statistical difference at p < .05. |
||||||||
| Disease category (ICD-9 diagnostic code) | Sex | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|
| Injuries and poisonings (802–894, 959, 977–998) | Men | 0.98 (0.98–0.99)* |
1.10 (1.09–1.10)* |
1.15 (1.14–1.16)* |
1.17 (1.15–1.20)* |
| Women | 0.94 (0.94–0.95)* |
1.01 (1.00–1.02)* |
1.06 (1.05–1.07)* |
1.23 (1.20–1.26)* |
|
Data source: Ontario Physician Claims Files, 2001–2002. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. *Statistically significant at p < .05; reference group is CMA/CA = 1.00. |
|||||
Higher risks of hospital discharge were evident among all rural residents, relative to urban residents, for all disease categories, with the exception of mental disorders for both male and female residents in Strong MIZ areas (Table 17).
| Disease category (ICD-9 diagnostic code) | Sex | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ |
|---|---|---|---|---|---|
| Mental disorders (290–319) | Men | 0.82 (0.75–0.90)* |
1.54 (1.46–1.61)* |
1.99 (1.92–2.07)* |
2.79 (2.47–3.15)* |
| Women | 0.82 (0.78–0.87)* |
1.54 (1.46–1.61)* |
1.99 (1.88–2.12)* |
2.79 (2.46–3.16)* |
|
Data source: Hospital Morbidity Database, 2001–2002, Canadian Institute for Health Information. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. * Statistically significant at p < .05; reference group is CMA/CA = 1.00. |
|||||
British Columbia
In general, physician visits were significantly less likely among residents of Strong and Weak MIZ areas than those in urban areas for most diseases examined. Residents of No MIZ areas, however, were more likely to visit a physician for conditions such as stroke, breast cancer, lung cancer, chronic obstructive pulmonary disease, arthritis and diabetes (Table 18). Those living in Weak and No MIZ areas were at significantly greater risk of hospitalization than urban residents, and for certain conditions this was also true for people residing in Moderate MIZ areas. In Strong MIZ areas, the risks of hospitalization were either lower than or the same as that for urban residents.
| Disease category (ICD-9 diagnostic code) | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | Strong MIZ | Moderate MIZ | Weak MIZ | No MIZ | |
| Relative risks of physician visit | ||||||||
| Coronary heart disease (410–414) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | --- |
| Stroke (430–434) | ↓ | ↓ | ↓ | ↑ | --- | ↓ | ↓ | ↑ |
| Breast cancer (174) | n/a | n/a | n/a | n/a | ↓ | ↑ | ↑ | ↑ |
| Lung cancer (162) | --- | ↑ | ↑ | ↑ | --- | ↑ | --- | ↑ |
| Asthma (493) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | --- |
| Chronic obstructive pulmonary disease (490–492, 496) | ↓ | ↓ | ↓ | ↑ | ↓ | ↓ | ↓ | ↑ |
| Rheumatoid arthritis (714) | --- | ↑ | ↓ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Osteoarthritis (715) | ↓ | ↑ | ↓ | ↑ | ↓ | ↑ | ↓ | ↑ |
| Depression (296.2, 296.3, 300.4, 311) | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ |
| Alzheimer's/dementia disorders (331) | ↓ | ↑ | ↓ | --- | ↑ | ↑ | ↓ | ↓ |
| Diabetes (250) | ↓ | ↓ | ↓ | ↑ | ↓ | ↓ | ↓ | ↑ |
| Relative risks of hospitalization | ||||||||
| Circulatory disease (390–459) | --- | --- | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Cancers/neoplasms (140–239) | --- | --- | ↑ | ↑ | --- | ↓ | ↑ | ↑ |
| Respiratory diseases (460–519) | ↓ | --- | ↑ | ↑ | --- | --- | ↑ | ↑ |
| Musculoskeletal system diseases (710–739) | --- | ↑ | ↑ | ↑ | --- | ↑ | ↑ | ↑ |
| Injuries and poisonings (802–894, 959, 977–998) | --- | ↑ | ↑ | ↑ | --- | ↑ | ↑ | ↑ |
| Mental disorders (290–319) | ↓ | ↑ | ↑ | ↑ | ↓ | --- | ↑ | ↑ |
| Nervous system and sense organs diseases (320–389) | ↓ | --- | ↑ | ↑ | --- | --- | ↑ | ↑ |
Data source: British Columbia Physician Claims Files, 2001–2002. Abbreviations: CA, Census Agglomeration; CMA, Census Metropolitan Area; ICD-9, International Statistical Classification of Diseases and Related Health Problems, 9th Revision; MIZ, Metropolitan Influenced Zone. Reference group is CMA/CA = 1.0; ↑ statistically higher relative risk at p < .05; ↓ statistically lower relative risk at p < .05; --- no statistical difference at p < .05. |
||||||||
Health services utilization patterns by MIZ
The patterns of health services utilization in Nova Scotia, Ontario and British Columbia can also be presented by focusing on the similarities and differences between degrees of rurality in relation to the relative risks of physician visits and hospitalization.
Strong MIZ:
- Nova Scotians living in Strong MIZ areas had equal or higher relative risks of physician visits (except for mental disorders and diseases of the musculoskeletal and nervous systems) and equal or higher risks of hospitalization than their urban counterparts for all conditions examined.
- Ontarians living in Strong MIZ areas typically had lower relative risks of physician visits but higher risks of hospitalization than urban Ontarians. One of the few exceptions was women in Strong MIZ areas, who had higher risks of physician visits for circulatory diseases. The risks of hospitalization were higher for all disease categories with the exception of mental disorders. Also, there were no statistically significant differences among men with cancer and with diseases of the nervous system and sense organs.
- British Columbians living in Strong MIZ areas consistently showed lower or equal risks of physician visits for the eleven specific diagnoses examined compared with urban residents, except for women with rheumatoid arthritis or Alzheimer’s disease. The risks of hospitalization were mostly equal or lower, relative to those in urban areas, except for women with circulatory diseases, who were at increased risk.
Moderate and Weak MIZ areas:
- Nova Scotians and British Columbians living in Moderate and Weak MIZ areas showed no consistent patterns in relation to risks of physician visits. There were differences between men and women, and the relative risks varied from one disease category or disease to another in the case of Nova Scotia and British Columbia, respectively. However, Ontarians in Moderate and Weak MIZ areas typically had lower risks of physician visits, with the exception of injuries and poisonings for both men and women.
- On the other hand, residents in Moderate and Weak MIZ areas in all three provinces generally had higher relative risks of hospitalization. The few exceptions were mostly found in Moderate MIZ areas of British Columbia, for both men and women, and in Moderate and Weak MIZ areas of Nova Scotia, especially among women.
No MIZ areas:
- No MIZ areas generally showed risk patterns that were different from those in other types of rural areas. Compared with people residing in CMA or CA, the residents of No MIZ areas in Nova Scotia had lower or similar risks of physician visits (with the exception of injuries and poisonings for men) but higher risks of hospitalization for all of the conditions examined.
- The relative risks of physician visits for Ontarians living in No MIZ areas were lower than or the same as for their urban counterparts, except for injuries and poisonings for both men and women and cancer for women; however, the relative risks of hospitalization were higher for all disease categories for both men and women.
- In British Columbia, no clear patterns emerged for residents in No MIZ areas in relation to the relative risks of physician visits; however, the relative risks of hospitalization were consistently higher than for those in urban areas. These findings are in line with the higher risks of hospitalization in Weak MIZ areas in British Columbia for all of the diseases examined.