Evidence-informed policy brief – Substance use and related harms in the context of COVID-19: a conceptual model
Health Promotion and Chronic Disease Prevention in Canada
Tell us what you think
Help us improve our products, answer our quick survey.
Aganeta Enns, MScAuthor reference footnote 1; Adena Pinto, BScAuthor reference footnote 1Author reference footnote 2; Jeyasakthi Venugopal, MPHAuthor reference footnote 1Author reference footnote 3; Vera Grywacheski, MPHAuthor reference footnote 1; Mihaela Gheorghe, MScAuthor reference footnote 1; Tanya Kakkar, MPHAuthor reference footnote 1; Noushon Farmanara, MScPHAuthor reference footnote 1; Bhumika Deb, MPHAuthor reference footnote 1; Amy Noon, MScAuthor reference footnote 1; Heather Orpana, PhDAuthor reference footnote 1Author reference footnote 2
https://doi.org/10.24095/hpcdp.40.11/12.03
(Published September 16, 2020)
This article has been peer reviewed.
Correspondence: Aganeta Enns, 785 Carling Ave, Ottawa, ON K1A 0K9; Tel: 343-551-4367; Email: aganeta.enns@canada.ca
Abstract
As the effects of COVID-19 have been unfolding, growing attention has been paid to the intersection of COVID-19 and substance use and the related harms. However, there are few theories and little empirical evidence to guide investigations in this area. To advance this emerging area of inquiry, we present a conceptual model that synthesizes evidence, information and knowledge on substance use and related harms in the context of the pandemic. The conceptual model offers a visual representation of the connections between the pandemic and substance use and related harms, and can be used to identify areas for future research.
Keywords: COVID-19, coronavirus, substance use, substance-related harms, opioids, conceptual model
Highlights
- As of June 2020, substance use and related harms in the context of a pandemic remained largely uninvestigated.
- The COVID-19 pandemic may impact how Canadians use substances and may present specific challenges and harms among people who use substances.
- The conceptual model in this paper offers a synthesis of evidence, information and knowledge of the concepts and associations relevant to substance use and harms in the context of the pandemic.
- Relevant concepts were synthesized into five interrelated domains that can be used to identify areas for future research into substance use and related harms in the context of COVID-19: substance use as a means of coping; changes in social support and networks; availability and accessibility of services; increased risk of COVID-19 transmission among people who use substances; and increased risk of severe outcomes.
Introduction
In March 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) a pandemic.Footnote 1 In response, Canada has implemented significant public health measures to reduce transmission.Footnote 2 Studies on the effects of physical distancing and self-isolation suggest that people may be changing how they use substances—alcohol,Footnote 3 opioidsFootnote 4Footnote 5Footnote 6Footnote 7 and cigarettesFootnote 7—as a result of the COVID-19 pandemic. Moreover, the pandemic and associated secondary effectsFootnote * may present unique challenges, such as decreased access to services and safe supplies of substances, and increased risk of substance-related harms.Footnote 3Footnote 4Footnote 5Footnote 6Footnote 7
The COVID-19 pandemic is an unprecedented event in modern history. The limited evidence that can be drawn from previous pandemics, for example, the severe acute respiratory syndrome (SARS) outbreak of 2003, may not be representative of current circumstances. A rapidly evolving area of investigation has been of substance use and related harms in the context of the pandemic. Despite a growing number of editorials and media reports,Footnote 3Footnote 4Footnote 5Footnote 6Footnote 7 there are few theories and little empirical evidence to guide future research.
A conceptual model is a diagram of “linkages among a set of concepts believed to be related to a particular public health problem.”Footnote 8 This type of model is particularly useful when there is little existing empirical evidence and formal theory. Model development involves summarizing and integrating the knowledge available from the scientific literature and from the experience of experts and professionals. Conceptual models can guide future research by providing potentially pertinent concepts and guiding hypotheses to be tested on the potential relationships between concepts.Footnote 8
The objective of this paper is to present a conceptual model of the possible effects of the COVID-19 pandemic on substance use and related harms. This model was developed primarily with a focus on opioids and other illegal drugs; however, alcohol and cannabis use were also considered. This model can be used to generate specific research questions and hypotheses that can then be tested through rigorous methods. The model can be updated and refined as evidence emerges.
Model development
While there is no standardized methodology for developing a conceptual model, we used the general approach to model development described by Earp and EnnettFootnote 8 to guide the development process. Earp and Ennett’s approach is a well-established and widely cited and adapted method of conceptual model development.Footnote 9Footnote 10 The overarching process of model development involves determining the scope of the model, identifying concepts or variables that relate to the issue of interest and explicating potential relationships between concepts.Footnote 8Footnote 9
The scope of the model presented in this paper includes substance use and related harms as they pertain to the COVID-19 pandemic. We developed the model through an iterative process of literature review, discussion within the research group and consultation with public health professionals and experts. Model development was led by a researcher (AE) with experience in qualitative research and thematic analysis.
We developed the first version of the model by summarizing a list of potentially relevant concepts and conducting a literature review of these concepts in published and grey literature sources. Beginning in March 2020, we searched the peer-reviewed literature in MEDLINE and the World Health Organization COVID literature database for English-language original research articles, reviews and editorials/commentaries. We then searched pre-print databases and grey literature sources. As the focus on the conceptual model is an emerging area of investigation, with limited high quality literature to rely on, we expanded the search to include expert opinion and media reports to support generating potential concepts to include in the model. The members of the research group discussed the list of concepts and the potential relationships between them, and revised these based on the results of the literature review. We then drafted the visual model and circulated it for discussion and revision within the research group.
To obtain rapid feedback, we invited professionals with expertise in substance use and related harms surveillance, research, policy and program to critically review the draft of the visual model and accompanying text descriptions and to comment. We gave these professionals a spreadsheet to document comments and questions on each domain as well as to provide feedback on the overall model. Using the feedback, we refined the conceptual model and circulated the revised model and text descriptions to the research group and to the experts who had provided feedback on the model for confirmation and additional feedback. The conceptual model was developed between March and May 2020.
This model should be considered a first version that may be revised and expanded as the pandemic and its effects continue to unfold, new areas of concern and investigation emerge, and research evidence becomes available.
Conceptual model
The conceptual model (Figure 1) provides a visual representation of how intersecting factors associated with the COVID-19 pandemic affect harms in people who use substances. The model has five main interrelated domains:
- substance use as a means of coping;
- changes in social support and networks;
- changes in availability and accessibility of services related to substance use and harms;
- increased risk of COVID-19 transmission among people who use substances; and
- increased risk of severe outcomes among people who use substances.
Figure 1. Conceptual model for substance use and related harms in the context of COVID-19
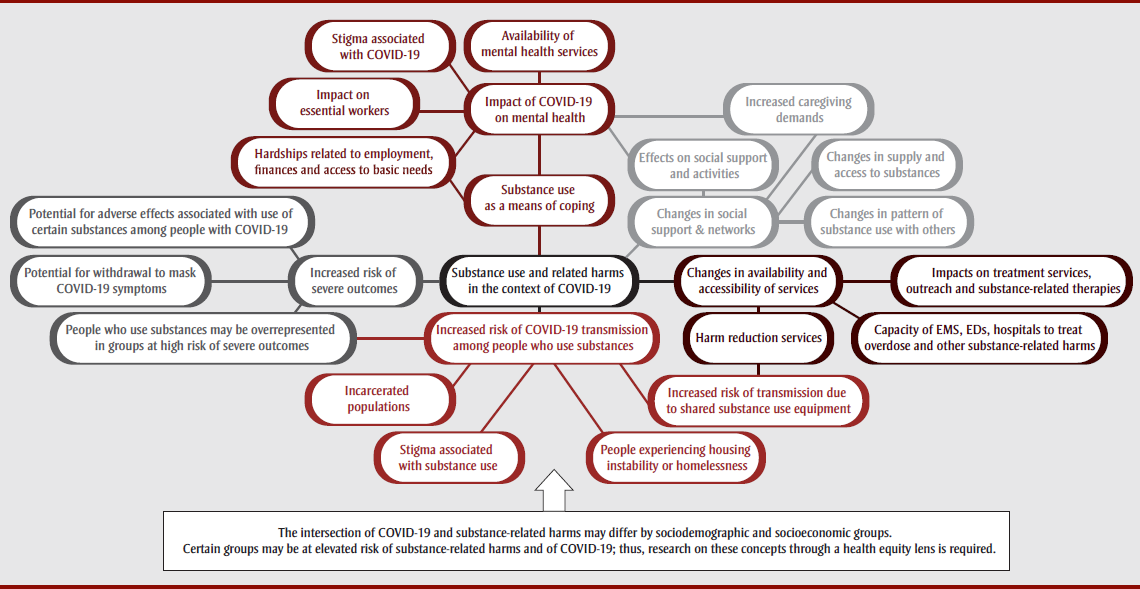
Text description: Figure 1
Figure 1. Conceptual model for substance use and related harms in the context of COVID-19
| Assigned ID | Cluster | Subheading? | Connects to | Text |
|---|---|---|---|---|
| CENT | N/A | Main heading / Central element | LBH, PH, DBH, LGH, DGH | Substance use and related harms in the context of COVID-19 |
| LBH | Light blue | Yes | CENT, LB1, LB2 | Substance use as a means of coping |
| LB1 | Light blue | No | LBH, LB2 | Hardships related to employment, finances and access to basic needs |
| LB2 | Light blue | No | LBH, LB1, LB3, LB4, LB5, P1, P2 | Impact of COVID-19 on mental health |
| LB3 | Light blue | No | LB2 | Impact on essential workers |
| LB4 | Light blue | No | LB2 | Stigma associated with COVID-19 |
| LB5 | Light blue | No | LB2 | Availability of mental health services |
| PH | Purple | Yes | CENT, P1, P2, P3, P4 | Changes in social support & networks |
| P1 | Purple | No | PH, LB2 | Effects on social support and activities |
| P2 | Purple | No | PH, LB2 | Increased caregiving demands |
| P3 | Purple | No | PH | Changes in supply and access to substances |
| P4 | Purple | No | PH | Change in patterns of substance use with others |
| DBH | Dark blue | Yes | CENT, DB1, DB2, DB3 | Changes in availability and accessibility of services |
| DB1 | Dark blue | No | DBH | Impacts on treatment services, outreach and substance-related therapies |
| DB2 | Dark blue | No | DBH | Capacity of EMS, EDs, hospitals to treat overdose and other substance-related harms |
| DB3 | Dark blue | No | DBH, LG1 | Harm reduction services |
| LGH | Light green | Yes | CENT, LG1, LG2, LG3, LG4, DG1 | Increased risk of COVID-19 transmission among people who use substances |
| LG1 | Light green | No | LGH, DB3 | Increased risk of transmission due to shared substance use equipment |
| LG2 | Light green | No | LGH | People experiencing housing instability or homelessness |
| LG3 | Light green | No | LGH | Stigma associated with substance use |
| LG4 | Light green | No | LGH | Incarcerated populations |
| DGH | Dark green | Yes | CENT, DG1, DG2, DG3 | Increased risk of severe outcomes |
| DG1 | Dark green | No | DGH, LGH | People who use substances may be overrepresented in groups at high risk of severe outcomes |
| DG2 | Dark green | No | DGH | Potential for withdrawal to mask COVID-19 symptoms |
| DG3 | Dark green | No | DGH | Potential for adverse effects associated with use of certain substances among people with COVID-19 |
Note: The intersection of COVID-19 and substance-related harms may differ by sociodemographic and socioeconomic groups. Certain groups may be at elevated risk of substance-related harms and of COVID-19; thus, research on these concepts through a health equity lens is required.
The domains likely intersect and interact, which may increase the risk of harms in many cases. Moreover, the concepts and relationships may differ between sociodemographic and socioeconomic groups (e.g. by sex, gender, age, ethnicity, racialization, income or occupation) as not all groups and communities in Canada are equally affected by COVID-19 or substance-related harms. While literature has emerged on the disproportionate effects of COVID-19 in the United States and how the pandemic has exacerbated health inequalities,Footnote 11 as of June 2020, there was little evidence available on the Canadian context.
Substance use as a means of coping
The COVID-19 pandemic has affected many facets of daily life. People may turn to substances to cope with distress and other secondary effects of COVID-19, such as boredom and changes in routine. A survey of 1036 adults in Canada conducted between March 30 and April 2, 2020, found that a quarter of people aged 35 to 54 years reported increased alcohol consumption during the pandemic outbreak.Footnote 12
Impact of COVID-19 on mental health
Recognition of how the pandemic may directly and indirectly affect mental health is growing. Symptoms of stress, anxiety and depression associated with the pandemic have been observed in the general population.Footnote 13 Fewer people aged 15 and older reported excellent or very good mental health during the period from March 30 to April 2, 2020, compared to 2018 estimates.Footnote 14 The survey revealed that younger adults (aged 15 to 24) were particularly affected, with 62% reporting excellent or very good mental health in 2018 compared to just 42% during the pandemic;Footnote 14 thus, this age group may also be at higher risk of using substances to cope.
The number of people experiencing distress may be increasing for reasons directly related to COVID-19, that is, diagnosis with infection and/or risk of transmission. But more people may be experiencing distress due to the secondary effects of the pandemic, for example, economic impacts or changes to health care services. Participants in a United Kingdom survey reported increased anxiety, depression, stress and concerns about the effects of physical distancing and the practical implications, such as financial impacts, on their well-being.Footnote 15
Stigma associated with COVID-19
Experiences of social stigma related to COVID-19 may contribute to poor mental health outcomes in some populations. For example, stereotyping and prejudiced messaging in the media, such as using terms that link COVID-19 to China (e.g., “China virus”), may fuel discrimination and stigmatization.Footnote 16 Older adultsFootnote 17, health care workers and people who have tested positive for COVID-19 and their families are among the groups who also potentially face stigma.Footnote 18 Increased distress and other impacts on mental health can result in increased use of substances.Footnote 19
Hardships related to employment, finances and access to basic needs
Many people across the country have faced hardships as a result of the decline in employment between February and April, 2020.Footnote 20 In April 2020, approximately 5.5 million Canadians either lost their employment or were working substantially reduced hours.Footnote 20 Employment decreased more sharply among recent immigrants than among people born in Canada. Moreover, compared with men, women had higher rates of unemployment in the early months of the pandemic.Footnote 20
For some, the pandemic has resulted in having to work from home, changes to their regular schedules and boredom. A 2020 survey published by the Canadian Centre on Substance Use and Addiction found that schedule changes and boredom were two of the top three reasons given for increased alcohol and cannabis use.Footnote 12 The third reason most often cited was stress. Note that this survey was conducted over 3 days early in the outbreak, and the situation has evolved since then. Job loss or insecurity and continued financial hardships and related issues, such as food and housing insecurity, may have resulted in increased stress.
Impact on essential workers
Workers who have continued to provide essential services may be at increased risk of exposure to COVID-19 at their physical workplaces and transmission of the virus. Essential workers include people employed in health care, transportation and food and those services necessary for the basic functioning of society. These workers may face demands and challenges associated with implementing new and evolving protocols related to COVID-19. Essential workers may be at increased risk of depression, anxiety and distress,Footnote 21 which increases the likelihood of substance use.
Availability of mental health services
The capacity of mental health services, including the availability and accessibility of trained personnel and infrastructure, may be affected during the pandemic. Demand for services may increase as people try to cope with stressors associated with COVID-19. Many service providers have transitioned to telehealth services.Footnote 22 This may be a barrier to people who do not have consistent access to phones, computers or private space, for example. If mental health needs are not met because of these limitations, people may turn to substances as a coping behaviour.Footnote 19
Changes in social support and networks
Effects on social support and activities
Physical distancing, closures of recreation and community facilities, limits on cultural and religious gatherings and other secondary effects of COVID-19 may affect access to social supports and resources for coping with stress. This could result in people feeling isolated and/or bored.Footnote 23 Restrictions or service alterations, such as changes in end-of-life care and funeral arrangements, may also affect the supports available to people who lose a family member or friend during the pandemic. Decreased social support and isolation may be associated with distress and increased use of substances to cope.Footnote 24Footnote 25 Lack of support or social isolation may disproportionately affect some, for example, people living in retirement homes or long-term care facilities that have limited visitors, people living alone and essential workers who may have to spend extended time away from family.
When people are overcoming a substance use disorder, social support, including informal supports and peer-support group meetings, may be a crucial facet of their recovery.Footnote 9 The secondary effects of COVID-19 may affect access to such social supports. Support groups may be facilitated through web-based platforms, but people who have barriers to accessing technology may not be able to benefit from this type of support.
Increased caregiving demands
Childcare and caregiving demands may increase because of daycare and school closures and changes in access to support and care resulting from physical distancing. In addition, many people will be caring for sick or distressed loved ones during the pandemic. The impacts of these demands will not be equal across sociodemographic groups; for example, a disproportionately high number of caregivers are women.Footnote 26 Thus, sex and other factors that affect health inequalities should be considered while examining these issues.Footnote 26
Quality of care and risk of infection for caregivers may also be of particular concern.
These changes in caregiving demands may increase distress and the use of substances to cope.
Changes in patterns of substance use with others
Patterns of substance use, including where people use and who they use substances with, may change due to the need for physical distancing and other secondary effects of COVID-19. Reduction or closure of harm reduction services may also affect patterns of substance use. If people are following physical distancing guidelines, they may be using substances alone, increasing the risk of death if they overdose.Footnote 27 People may also be driven to use in public places, which may result in increased risk of harm, anxiety and likelihood of arrest and possible incarceration.Footnote 28
Changes in supply and access to substances
International travel limitations and reduced travel between Canadian provinces and territories has affected supply chains of illegal substances.Footnote 29Footnote 30 In addition, COVID-19 risk reduction measures such as physical distancing and self-isolation may also have affected access. Limited supplies may change the potency or composition of the illegal drugs that are available.Footnote 31 Changes in supply and access may also pose as a barrier to COVID-19 risk reduction measures. For example, individuals seeking new sources may not be able to practise physical distancing.
If access to substances is limited, there may be an increase in the number of people who go through withdrawal and an increase in instances of people starting to use new or unfamiliar but more readily available substances.Footnote 31 Interruptions in supply can affect a person’s tolerance, increasing the risk of overdose when substances do become available. The risk of overdose may be greater if potency is increased or substances are contaminated.
Some jurisdictions have seen increases in overdoses since the beginning of the pandemic. In June 2020, British Columbia recorded the highest number of illicit drug toxicity deaths to date as well as an increase in the number of cases that involved high concentrations of fentanyl.Footnote 32 Note that there may be geographical differences in supply dynamics and how provinces, territories and municipalities are working to mitigate these issues.
For legal substances such as alcohol and cannabis, some provinces and territories made changes to existing regulations about the sale of these substances. While most licensed establishments were closed for in-person dining and drinking during the initial period of restrictive measures, other actions increased access to alcohol. For example, licensed restaurants in Ontario were allowed to sell alcohol with takeout and delivery orders, and to sell spirits at a lower price with these orders.Footnote 33 Delivery of cannabis by licensed retail stores was also allowed in Ontario in March, but was discontinued in July.Footnote 34
Changes in availability and accessibility of services related to substance use and harms
Impacts on treatment services, outreach and substance-related therapies
The COVID-19 pandemic may affect the availability and accessibility of certain treatment services for substance use disorders.Footnote 4Footnote 5 Many providers have shifted to telehealth outpatient services and wait times may be affected. People who made use of outreach services for substance use and related harms may be affected during the pandemic. Service reductions in outreach programs may take place due to personnel or infrastructure limitations.
The implications of COVID-19 on opioid agonist therapies have been discussed in commentaries, media reports and in regard to policy.Footnote 4Footnote 5 As these therapies are typically administered in-person on a regimented basis, the pandemic may disrupt therapy for people who are in isolation or afraid to leave their home. As mentioned above, jurisdictions have responded in different ways to mitigate issues to do with the safe supply of substances. For example, British Columbia has increased efforts to provide a safe supply of substances to reduce harms during the pandemic.Footnote 35 The safe supply approach involves prescribing and dispensing pharmaceutical-grade medications as an alternative to the unregulated street supply of substances to people who are at risk of harms such as an overdose.Footnote 36
Harm reduction services
Harm reduction services sites, including safe consumption sites, may reduce their hours, limit the number of people they can serve or close temporarily during the COVID-19 pandemic.Footnote 37 Service reductions may involve limiting the number of available consumption booths to take into account physical distancing measures and accommodating reductions in staff because of their need to self-isolate or quarantine. Programs that provide harm reduction supplies (e.g. sterile equipment) and distribute naloxone may face closures, reduced hours and/or other service restrictionsFootnote 38 that limit the number of people that they can serve.
Capacity of hospitals, emergency departments, first responders to treat overdose and other substance-related harms
If hospitals or first responders become overwhelmed as a result of pandemic-related patient intake, their capacity to respond to and provide treatment for overdoses and other substance-related harms may be limited.Footnote † Moreover, some people may choose to delay treatment, avoid accessing health care services or abstain from calling emergency services due to fears associated with COVID-19.
Drug-related overdoses may be treated differently due to COVID-19. Opioid poisonings (overdoses) are typically treated by administering naloxone and immediately providing oxygen, either through a mask or rescue breathing. First responders may no longer be able to give oxygen this way because of the risk of COVID-19 transmission.Footnote 29 Moreover, some first responders have stopped administering naloxone in a nasal spray due to the risk of COVID-19 transmission through nasal droplets,Footnote 39 although as of June 2020, we found no reports of changes to practices of administering naloxone by injection.
Some people who overdose require ventilators to survive. Should a situation occur where demand for ventilators is overwhelmed due to COVID-19, only a limited number of ventilators may be available.Footnote †
Increased risk of COVID-19 transmission among people who use substances
Increased risk of transmission due to shared substance use equipment
Sharing substance use equipment (e.g. pipes, joints, vaping devices or alcohol containers) increases the risk of virus transmission. (This is linked to the “availability of harm reduction services” domain, as the availability and accessibility of harm reduction services, such as sterile supply programs, may impact access to clean equipment and consequently, risk of transmission.)
Stigma associated with substance use
Stigmatizing substance use stems from erroneous beliefs that people with substance use disorders are to blame for their conditions or are dangerous or reckless, and that substance use is a choice or matter of will power. Experiences related to stigma may act as a barrier to accessing health and social services.Footnote 40 People who use substances may also receive poorer quality health care services or engage in harmful behaviours or coping methods (e.g. avoidance of health care or more or more frequent substance use).
Outcomes associated with the stigmatization of people who use substances may be exacerbated during the pandemic and may impede access to care and uptake of COVID-19 risk reduction measures.Footnote 6Footnote 12Footnote 41 People who use substances are likely to experience multiple forms of stigmas (i.e. targeted toward their health conditions, characteristics, sex/gender or gender identity, racialized identity, age, ability or language). Complex intersections between multiple stigmas can further affect health.Footnote 40
Incarcerated populations
People who use substances tend to be overrepresented in incarcerated populations, and substance use is common in prison populations in Canada.Footnote 42 Incarcerated populations are at increased risk of disease transmission during the pandemic and face unique challenges when implementing risk reduction measures.Footnote 7Footnote 43 For example, the aging prison population, issues of crowding within cells and the high prevalence of substance use and associated comorbidities may elevate the risk of COVID-19 infection and likelihood of severe outcomes.Footnote 43
People experiencing homelessness, instability or inadequate housing
People who use substances may be more likely to experience housing instability or homelessness. Individuals who rely on shelters, shared or overcrowded accommodations or public places are less likely to have regular access to hygiene supplies and may not be able to practise physical distancing. They are at higher risk of acquiring and transmitting COVID-19. In addition, they may face barriers to implemented risk reduction measures.Footnote 44 Service reductions due to the pandemic and limiting capacity at shelters may serve as a barrier to accessing shelter, hygiene facilities and safe places to use substances. This would likely increase the risks of both infection and overdose. Moreover, this population often has worse access to health services, experiences higher rates of substance use and may be less likely to engage in harm reduction measures (e.g. using sterile drug equipment).Footnote 44
Increased risk of severe outcomes among people who use substances
People who use substances may be overrepresented in groups at high risk of severe outcomes
Several pre-existing health conditions are risk factors for severe outcomes among people diagnosed with COVID-19.Footnote 45 Many of the conditions that have been identified as risk factors also disproportionately affect people who use substances: chronic lung disease, cardiovascular disease and weakened immune system.Footnote 45Footnote 46
As mentioned in the section “Substance use as a means of coping,” effects of the pandemic may contribute to increased substance use. In addition, use of certain substances may increase the risk of severe illness among people diagnosed with COVID-19: the use of certain substances may weaken the immune system and the use of long-acting and immunosuppressive opioids, such as methadone or fentanyl, has been associated with increased risks of respiratory infections.Footnote 47
Abrupt discontinuation of opioids, which can trigger withdrawal, has also been associated with an elevated risk of serious infection,Footnote 48 meaning that disruptions in access to opioids during the pandemic may exacerbate the risk of COVID-19 infection.
Chronic alcohol consumption has also been associated with weakened immune function and even moderate consumption has been linked with increased risk of infection.Footnote 49
Potential for adverse effects associated with use of certain substances among people with COVID-19
Among those infected with COVID-19, people who use substances may be susceptible to complications and more severe outcomes. Opioid use increases risk of respiratory infections that, in turn, increases the risk of disease complications and severe outcomes.Footnote 7 Methamphetamine use may also increase the risk of severe COVID-19 outcomes, as its use can lead to pulmonary damage and/or affect immune function.Footnote 7Footnote 50 Examining potential adverse effects of methamphetamine use among people with COVID-19 may be an important area of investigation as the prevalence of methamphetamine use is rising in North America.Footnote 50
Due to the harmful effects on lung health, smoking and vaping may also increase the risk of severe COVID-19 infection.Footnote 7 However, these associations have not yet been substantiated and further investigation is needed.
Poly-substance use may impact disease outcomes and could interact with risk factors, including older age or having one or more chronic conditions, for severe outcomes related to COVID-19.
In addition to the potential for substance use to affect the severity of COVID-19 outcomes, the effects of COVID-19 on respiratory function could affect the risk of opioid overdose. Chronic respiratory disease has been associated with greater risk of opioid overdose hospitalizations and mortality.Footnote 51Footnote 52 Similarly, diminished lung capacity caused by COVID-19 infection may further increase harms.Footnote 7 Coupled with the potential changes in drug supplies and reduced availability of certain harm reduction and treatment services, as described above, the risk of overdose may be particularly high for some people who use substances during the pandemic.
Potential for withdrawal to mask COVID-19 symptoms
COVID-19 symptoms such as fever and difficulty breathing could be mistaken for withdrawal symptoms among people who use substances. Changes in the circulating drug supply and available services as a result of the pandemic may increase the number of people experiencing withdrawal. There may also be less oversight of these issues due to limitations to the accessibility or availability of services during the pandemic.
Implications for research
The secondary effects of the COVID-19 pandemic is a rapidly evolving topic. This conceptual model of substance-related harms and COVID-19 offers guidance for future areas of investigation where there is currently a dearth of empirical evidence.
As this area of investigation is emerging, few original peer-reviewed studies and reviews were available. Therefore we also included commentaries and non-reviewed sources to inform the development of the model. While the quality of evidence informing this conceptual model is limited, the inclusion of a variety of evidence sources, including peer-reviewed original research, allowed for a rapid and in-depth examination of this emerging area. While conceptual models are not intended to specify how or where to target interventions,Footnote 14 the information provided in this paper may help to identify areas where research could support intervention efforts.
The present model suggests that COVID-19 and its secondary effects may have far-reaching implications for how people use substances in Canada and the unique harms to which they are exposed. Given this, research on these topics is needed to confirm or disprove the proposed relationships.
The model presented five interrelated domains of concepts that highlight potential associations of interest. Empirical evidence on changes in patterns of substance use in response to the mental health and social effects of the pandemic is needed. Substance use and exposure to related harms may be affected by changes in social support, safe access to substances and access to services. Risk of COVID-19 infection among people who use substances, as well as severe outcomes among people diagnosed with COVID-19, should be monitored to elucidate how substance use, including poly-substance use, contribute to disease outcomes.
The relationships posited in this model likely intersect with sociodemographic or socioeconomic factors, as certain populations are at elevated risk for both substance-related harms and COVID-19. Research into how the intersection between the pandemic and substance-related harms affects different communities and groups across Canada is needed to document health inequalities and inequities.
Conclusion
In this paper we presented a model that illustrated relevant interrelated concepts in the emerging area of substance use and related harms in the context of the COVID-19 pandemic. The conceptual model synthesized information from a variety of sources—including peer-reviewed literature, opinion pieces and commentaries, grey literature and expert opinion and perspectives on substance use and related harms during the COVID-19 pandemic—to summarize the available material and generate future research directions.
The full effects of the pandemic on substance use and related harms have likely not yet been realized. Evidence is needed to elucidate the relationships shown in the conceptual model to better understand these issues as they unfold and to guide future research and considerations for policy and programs during the pandemic.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Authors’ contributions and statement
AE and HO conceived of the project. AE, AP, JV and VG conducted the literature review. AE led the development of the conceptual model. AP, JV, VG, MG, NF, TK, BD, AN and HO contributed to the development of the model. AE drafted the article. All authors critically revised the article.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.