Evidence synthesis – Timing of sedentary behaviour and access to sedentary activities in the bedroom and their association with sleep quality and duration in children and youth: a systematic review

HPCDP Journal Home
Published by: The Public Health Agency of Canada
Date published: April 2022
ISSN: 2368-738X
Submit a manuscript
About HPCDP
Browse
Previous | Table of Contents | Next
Travis J. Saunders, PhDAuthor reference footnote 1; Travis McIsaac, MScAuthor reference footnote 1; Jenny Campbell, BScAuthor reference footnote 1; Kevin Douillette, BScAuthor reference footnote 1; Ian Janssen, PhDAuthor reference footnote 2Author reference footnote 3; Jennifer R. Tomasone, PhDAuthor reference footnote 2; Amanda Ross-White, MLISAuthor reference footnote 4; Stephanie A. Prince, PhDAuthor reference footnote 5Author reference footnote 6; Jean-Philippe Chaput, PhDAuthor reference footnote 7
https://doi.org/10.24095/hpcdp.42.4.03
This article has been peer reviewed.
Author references
Correspondence
Travis Saunders, Department of Applied Human Sciences, University of Prince Edward Island, Charlottetown, PE C1A 4P3; Tel: 902-566-0641; Email: trsaunders@upei.ca
Suggested citation
Saunders TJ, McIsaac T, Campbell J, Douillette K, Janssen I, Tomasone JR, Ross-White A, Prince SA, Chaput JP. Timing of sedentary behaviour and access to sedentary activities in the bedroom and their association with sleep quality and duration in children and youth: a systematic review. Health Promot Chronic Dis Prev Can. 2022;42(4):139-49. https://doi.org/10.24095/hpcdp.42.4.03
Abstract
Background: The purpose of this study was to systematically review the relationship between the timing of sedentary behaviours and access to sedentary activities in the bedroom with sleep duration and quality in children and youth. A secondary purpose was to examine whether these relationships differ when comparing screen-based and non-screen-based sedentary activities.
Methods: We searched four databases for peer-reviewed studies published between 1 January 2010 and 19 January 2021. Risk of bias assessment for each study and certainty of evidence were assessed using the GRADE framework.
Results: We identified 44 eligible papers reporting data from 42 separate datasets and including 239 267 participants. Evening participation in screen-based sedentary behaviours and access to screen-based devices in the bedroom were associated with reduced sleep duration and quality. Daytime screen use was also associated with reduced sleep duration, although this was examined in relatively few studies. Whether performed during the day or night, non-screen-based sedentary behaviours were not consistently associated with sleep duration or quality. The quality of evidence was rated as low to very low for all outcomes.
Conclusion: In order to maximize sleep duration and quality, children and youth should be encouraged to minimize screen time in the evening and remove screens from bedrooms. (PROSPERO registration no.: CRD42020189082)
Keywords: sedentary behaviour, screen time, sleep duration, sleep quality, timing, systematic review, youth, public health
Highlights
- Using screen-based devices in the evening and access to screen-based devices in the bedroom were associated with reduced sleep duration and quality.
- Findings were based primarily on observational studies, using self-report methodologies.
- Children and youth should be encouraged to minimize the use of screen-based devices before bed and remove screens from bedrooms.
Introduction
Sedentary behaviours (waking behaviours characterized by an energy expenditure of 1.5 or less metabolic equivalents while in a sitting, reclining or lying posture)Footnote 1 are linked with numerous important health outcomes among school-aged children and youth.Footnote 2 While screen-based sedentary behaviours are often associated with detrimental health outcomes, non-screen-based sedentary behaviours such as reading typically show null or even beneficial associations with health.Footnote 3Footnote 4
In a 2016 systematic review of 235 studies, Carson et al.Footnote 4 reported that higher durations and frequencies of screen time were associated with unfavourable body composition, behavioural conduct, fitness, self-esteem and clustered cardiometabolic risk. In contrast, reading and homework were positively associated with academic achievement.Footnote 4 Other recent systematic reviews and meta-analyses report that higher levels of screen-based sedentary behaviours are also associated with increased risk of depression,Footnote 5Footnote 6 although questions remain regarding the magnitude of this relationship.Footnote 7
Inadequate sleep duration and quality likely mediate the relationship between screen-based sedentary behaviour and health outcomes.Footnote 8 Longer sleep duration is associated with favourable body composition, emotional regulation, academic achievement and quality of life.Footnote 9 A systematic review reported that 90% of studies examined found that screen time is associated with poor sleep outcomes (primarily shorter and delayed sleep) among children and youth.Footnote 10 Reductions in total daily screen time are also associated with small increases in sleep duration among children and youth.Footnote 11
A number of mechanisms have been suggested to explain these associations, the most obvious being time displacement; more time using screens means less time for other behaviours, including sleep.Footnote 10Footnote 12 Other mechanisms include increased arousal and negative effects on circadian rhythms.Footnote 10Footnote 13 Limited evidence has also suggested that interactive screen time (e.g. using a computer, smartphone or video game console) is more consistently associated with poor sleep than more passive forms of screen time (e.g. television viewing).Footnote 10
Based on these suggested mechanisms, it is plausible that the timing of screen-based sedentary behaviours may have a greater impact on sleep than total daily volume. A meta-analysis by Carter et al.Footnote 14 reported a strong and consistent association between bedtime use of smartphones and tablets with deleterious sleep quantity (odds ratio [OR] = 2.17; 95% confidence interval [CI]: 1.42–3.32) and quality (OR = 1.46; 95% CI: 1.14–1.88). Not surprisingly, it is common to recommend that children and youth avoid screens in the hour(s) before bed and limit using screen-based devices in the bedroom.Footnote 10Footnote 13Footnote 15Footnote 16
While this evidence suggests that the timing of sedentary behaviour may be associated with sleep quality and duration, several key questions remain. Although previous reviews have examined the impact of screen use in the bedroom, or immediately preceding sleep, to date none have compared this with the impact of screen use during other periods of the day or with the impact of non-screen-based sedentary behaviours during these same periods. It is therefore unclear whether the relationship between evening screen use and sleep differs markedly from that of daytime screen use. It is also unclear whether non-screen-based sedentary behaviour such as reading a book or doing paper-based homework show similar or different associations with sleep. These are important research gaps, as they preclude specific public health recommendations related to sedentary behaviour and sleep.
The purpose of this study was to systematically review the relationship between the timing of sedentary behaviours and access to sedentary activities in the bedroom with sleep duration and quality in children and youth. A secondary purpose was to examine whether these relationships differ based on the mode of sedentary behaviour (i.e. screen based and non-screen based).
Methods
Protocol and registration
This systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO; Registration no. CRD42020189082) and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.Footnote 17 Methods are presented below using the Population, Intervention/Exposure, Comparison/Control and Outcome (PICO) framework.
Eligibility criteria
Population
The population of interest was apparently healthy children and youth aged 5 to 17.99 years. Studies with participants outside of this age range were included if participants aged 5 to 17.99 were reported separately or if the mean age fell within this range. Studies exclusively targeting disease-specific populations (e.g. children with diabetes, children with congenital heart defects) or patients with sleep disorders were excluded.
Intervention/exposure
The intervention or exposure was the timing of sedentary behaviour as well as access to both screen-based and non-screen-based sedentary activities in the bedroom. Sedentary behaviours were defined as any waking behaviour characterized by low energy expenditure and a sitting, reclining or lying posture.Footnote 1 This included measures of time spent sitting as well as screen-based sedentary behaviours (e.g. watching TV, playing video games, accessing social media, reading an ebook) and non-screen-based sedentary behaviours (e.g. reading a print book, listening to music, playing board games).
Sedentary behaviour timing refers to the time of day that sedentary behaviours occur. The timing may be reported as time of day or time relative to bedtime. Studies were eligible if they included device-measured (e.g. using an inclinometer, actigraph unit/accelerometer) or self-reported (e.g. questionnaire) measures of sedentary behaviour timing or both. Studies were also included if they reported the presence of objects used to engage in screen-based or non-screen-based sedentary activities in the bedroom. For experimental studies, the interventions must have targeted sedentary behaviour timing or presence of sedentary activities exclusively and not multiple health behaviours (e.g. both sedentary behaviour and diet or sedentary behaviour and physical activity).
Comparison/control
Various levels of sedentary behaviour timing/access to sedentary activities in the bedroom were used for comparison. However, a comparator or control group was not required for inclusion.
Outcomes
This systematic review had two outcomes: sleep duration (e.g. hours per night, hours per 24-hour period), and sleep quality, which included the following measures: sleep onset latency, sleep efficiency (% of time in bed spent sleeping), waking after sleep onset, waking up too early, sleeping restlessly, difficulty falling asleep, insomnia symptoms and overall sleep quality.
Study designs
All study designs, except case studies, were eligible for inclusion, but only published or in-press English or French language peer-reviewed studies were eligible; all grey literature (e.g. book chapters, dissertations, conference abstracts) were excluded. For longitudinal studies, any length of follow-up was allowed, but there must have been at least one measure of sleep timing at 5 to 17 years of age. Because we initially identified a large number of small cross-sectional studies, we set the minimum sample size for cross-sectional studies to 1000 midway through the review. This threshold is consistent with previous systematic reviews in this field.Footnote 9 There were no sample size limitations for longitudinal or experimental studies.
Information sources and search strategy
A comprehensive search strategy was developed by a research librarian (AR-W). Four bibliographic databases were searched: Ovid MEDLINE, Ovid Embase, Ovid PsycINFO and EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL). Searches were conducted on 19 January 2021. All studies had to have been published on or since 1 January 2010; these dates were chosen to manage scope and to focus on the most recent body of evidence.
The search strategy is shown in Supplementary Table 1.
We also searched the reference lists of all review studies identified during level 2 screening for additional relevant studies.
Data extraction
To remove duplicates, bibliographic records were extracted and imported into EndNote software (Clarivate, Philadelphia, PA, US). During level 1 screening, two reviewers (any combination of JC, TM, SP or TJS), working independently, screened titles and abstracts of potentially relevant articles using Covidence (Veritas Health Innovation, Melbourne, AU). We obtained full-text copies of the articles that met initial screening criteria. During level 2 screening, two reviewers (any combination of JC, TM, SP, KD or TJS), working independently, examined all the full-text articles. Any discrepancies were resolved via discussion until consensus was reached.
A reviewer (TM) extracted the relevant data using a customized Google Form, and another (TJS) verified the data. Authors’ and journal names were not blinded when the reviewers were extracting data. The extracted information included descriptive study characteristics (e.g. author, publication year, study design, country, sample size, age, sex), intervention/exposure, outcome(s), results and confounders. Where studies reported multiple models, the reviewers extracted results from the most fully adjusted model, including both the direction and statistical significance of any associations.
Risk of bias and study quality assessment
Using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework,Footnote 18 we systematically examined the quality of primary research contributing to each health indicator and assessed the overall quality and risk of bias of the evidence across health indicators. We completed the risk of bias assessment for individual intervention studies according to methods described in the Cochrane Handbook.Footnote 19 GRADE does not have a tool for assessing risk of bias in observational studies, but does recommend the types of characteristics to examine.Footnote 18 For individual observational studies, we assessed selection bias, performance bias, selective reporting bias, detection bias, attrition bias and other biases (e.g. inadequate control for key confounders). Risk of bias for individual studies was assessed by one reviewer (TM) and verified by another (TJS). According to the GRADE framework, randomized controlled trials start with a quality of evidence rating of “high”; all other designs start at a rating of “low.”Footnote 18 The quality of evidence can be downgraded if there are limitations across studies as a result of risk of bias (operationalized as ≥50% of studies showing high risk of bias for a given outcome), inconsistency, indirectness, imprecision or other factors.Footnote 18 The quality can be upgraded if there are no serious limitations, as well as a large magnitude of effect or evidence of a dose–response relationship.Footnote 18
Results
Description of studies
A total of 3548 studies were identified through database searches, leaving 2999 after duplicates were removed. After title and abstract screening, 803 papers underwent full-text review. Of these, 42 met all inclusion criteria. Searching the reference lists of all reviews identified at level 2 screening identified 132 potentially relevant papers, of which 2 met the inclusion criteria. This left a total of 44 papers, reporting on 42 individual datasets. (See Figure 1 for the PRISMA flow diagramFootnote 17.)
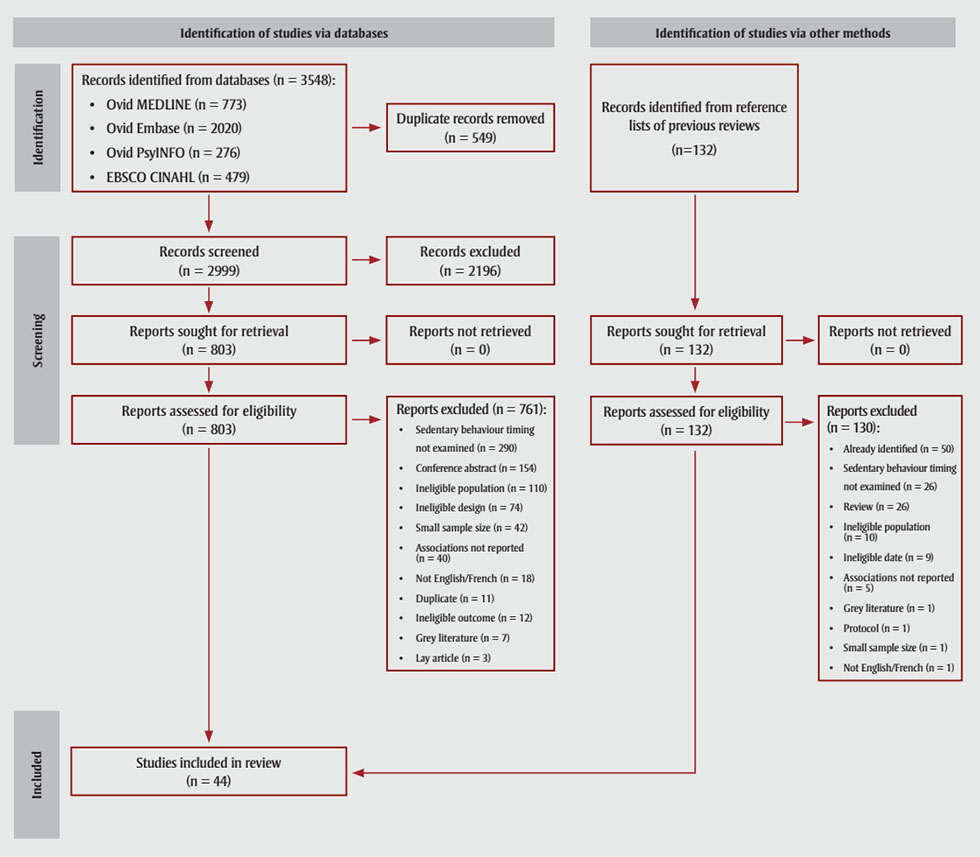
Figure 1 - Text description
This figure depicts the PRISMA flow diagram for selection of studies in this systematic review.
3548 records were identified from databases:
- Ovid MEDLINE (n = 773)
- Ovid EMBASE (n = 2020)
- Ovid PsyINFO (n = 276)
- EBSCO CINAHL (n = 479)
Of these 549 duplicate records were removed. A total of 2999 records were screened, which resulted in 2196 records being excluded. 803 reports were thus sought for retrieval (n = 0 reports not retrieved), and 803 reports were assessed for eligibility. Of these, 761 were excluded for the following reasons:
- Sedentary behaviour timing not examined (n = 290)
- Conference abstracts (n = 154)
- Ineligible population (n = 110)
- Ineligible design (n = 74)
- Small sample size (n = 42)
- Associations not reported (n = 40)
- Not English/French (n = 18)
- Duplicate (n = 11)
- Ineligible outcome (n = 12)
- Grey literature (n = 7)
- Lay article (n = 3)
Additionally, 132 records were identified via other methods (in this case, from reference lists of previous reviews). Of those, 132 reports were sought for retrieval (n = 0 reports not retrieved), and 132 reports were assessed for eligibility. Of those, 130 reports were excluded for the following reasons:
- Already identified (n = 50)
- Sedentary behaviour timing not examined (n = 26)
- Review (n = 26)
- Ineligible population (n = 10)
- Ineligible date (n = 9)
- Associations not reported (n = 5)
- Grey literature (n = 1)
- Protocol (n = 1)
- Small sample size (n = 1)
- Not English/French (n = 1)
In the end, this resulted in n = 44 studies included in this review.
Abbreviation : PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The most common reasons for excluding an article at level 1 full-text screening was that the study failed to measure or report sedentary behaviour timing (n = 290), it was a conference abstract (n = 154) or that it examined ineligible populations (n = 110). Forty-three cross-sectional studies that met other inclusion criteria were excluded because the sample size was less than 1000. A list of reasons for excluding individual papers is in Supplementary Table 2. Quality of evidence for each outcome are presented in Table 1, and a high-level summary of findings is presented in Table 2.
| Health outcome | Study design | No. of studies | No. of participants | Quality assessment indicator | Quality | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk of bias | Inconsistency | Indirectness | Imprecision | Large magnitude of effect | Dose response | |||||
| Sleep duration | ||||||||||
| Sedentary timing | Nonrandomized trials | 4 | 71 | High risk of selection bias | Low | Low | Low | No | No | Very low |
| Observational studies | 21 | 208 801 | Low risk of bias | Low | Low | Low | No | No | Low | |
| Presence of sedentary behaviours in bedroom | Nonrandomized trials | 0 | 0 | NA | NA | NA | NA | NA | NA | NA |
| Observational studies | 15 | 36 711 | Low risk of bias | Low | Low | Low | No | No | Low | |
| Sleep quality | ||||||||||
| Sedentary timing | Nonrandomized trials | 8 | 361 | High risk of selection bias | High | Low | Low | No | No | Very low |
| Observational studies | 12 | 154 836 | Low risk of bias | Low | Low | Low | No | No | Low | |
| Presence of sedentary behaviours in bedroom | Nonrandomized trials | 0 | 0 | NA | NA | NA | NA | NA | NA | NA |
| Observational studies | 5 | 11 154 | Low risk of bias | Low | Low | Low | No | No | Low | |
Abbreviations: NA, not applicable; no., number. |
||||||||||
| Sleep outcome | No. of studies | No. of participants | Quality of evidence | Summary of findings |
|---|---|---|---|---|
| Sleep duration | 34 | 233 067 | Very low | Evening screen use is negatively associated with sleep duration |
| Reducing evening screen use may increase sleep duration | ||||
| Presence of screen-based devices in the bedroom may be associated with reduced sleep duration | ||||
| Sleep quality | 22 | 160 686 | Low | Evening screen use and presence of screens in the bedroom are negatively associated with sleep quality |
| Reducing evening screen use may increase sleep quality | ||||
Abbreviation: No., number. |
||||
Characteristics of the individual studies included in this review are in Supplementary Tables 3–6 and risk of bias assessments of individual studies are in Supplementary Tables 7–10. We identified 28 cross-sectional studies, 6 longitudinal studies lasting between 1 and 3 years, and 8 nonrandomized intervention studies lasting 1 to 14 days.
Sedentary behaviour was self- or parent-reported in 36 studies, device-measured in 1 study, and intervened upon by the research team in 5 nonrandomized intervention studies. Sleep duration and quality were device-measured in 7 of the 8 intervention studies and 1 of the 34 observational studies. Sedentary behaviour timing was categorized in a variety of ways across studies, including “morning,” “after school,” “dinner time,” “after dinner,” “before bedtime/sleep,” “at night,” “before and/or after lights out,” “last hour before bed” and “in bed,” as well as the specific time of use/last use. For this review, “morning,” “after school” and “dinner time” were considered daytime, and all other time points, evening.
Thirty-one studies examined the impact of sedentary behaviour timing, while 16 studies examined the impact of sedentary behaviours in the bedroom (5 studies included both). Sleep duration was assessed in 34 studies, and sleep quality in 23, with 16 studies examining both eligible outcomes. Across all studies, there were 239 267 participants from 23 countries. Mean ages ranged from 5.3 to 17.4 years.
Data synthesis
Because the heterogeneity in study design, measurement of sedentary behaviour and sleep, and statistical analyses precluding the use of meta-analyses, we present our results as a narrative synthesis.
Sedentary behaviour timing and sleep duration
Four nonrandomized intervention studiesFootnote 20Footnote 21Footnote 22Footnote 23 examined the relationship between sedentary behaviour timing and sleep duration. One 2-week-long intervention reported that reducing total screen time after 9 p.m. increased sleep duration by 17 ± 2 minutes.Footnote 20 Another 1-week-long intervention found that reducing mobile phone use in the hour before bed led to sleep lasting 21 minutes longer each night.Footnote 21 An intervention lasting a single night reported a negative correlation between video game time and sleep duration (r = −0.92; p < 0.05),Footnote 22 while another single-night intervention reported that playing video games for 150 minutes reduced sleep duration by 27 ± 12 minutes, compared to effects of playing the same game for 50 minutes.Footnote 23
Quality of evidence was rated as very low for these experimental studies because of the lack of randomized trials, concerns related to bias and lack of evidence of large effects or dose–response relationships.
One longitudinal study lasting 3 years reported that, in comparison to those who did not use screens at any time after dinner, those who used screens after dinner had significant reductions in sleep duration (β = −0.10; 95% CI: −0.18, −0.02; p = 0.01).Footnote 24 However, there was no significant association between changes in screen use after dinner and changes in sleep duration (β = −0.08; 95% CI: −0.16, 0.01; p = 0.07). A longitudinal study that lasted 2 years reported that watching TV/using video games before bedtime was associated with reduced sleep duration (β = −0.04; 95% CI: −0.05, −0.12; p < 0.05).Footnote 25
Nineteen cross-sectional studies examined the relationship between sedentary behaviour timing and sleep durationFootnote 26Footnote 27Footnote 28Footnote 29Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 36Footnote 37Footnote 38Footnote 39Footnote 40Footnote 41Footnote 42Footnote 43Footnote 44, 2 of which looked only at daytime sedentary behaviourFootnote 39Footnote 44. Evening screen use was negatively associated with sleep in 15/17 studiesFootnote 26Footnote 27Footnote 28Footnote 29Footnote 30Footnote 31Footnote 32Footnote 33Footnote 34Footnote 35Footnote 37Footnote 40Footnote 41Footnote 42Footnote 43, positively associated with sleep in 1/17 studyFootnote 38, and showed one or more null associations in 5/17 studiesFootnote 28Footnote 36Footnote 40Footnote 41Footnote 42. Several studies reported associations for multiple modalities of screen use.
All 3 of the studies that examined daytime screen use reported negative associations with sleep duration.Footnote 33Footnote 39Footnote 44 One study reported that daytime homework/reading was negatively associated with sleep durationFootnote 39, while another reported no associationFootnote 30.
Apart from video game use, the associations between evening screen use and deleterious sleep duration were consistent across devices. The majority of studies reported that sleep duration was negatively associated with evening use of smartphones (8/10 studies)Footnote 26Footnote 27Footnote 28Footnote 29Footnote 33Footnote 34Footnote 35Footnote 40 total screen time (6/8 studies)Footnote 30Footnote 33Footnote 34Footnote 40Footnote 42Footnote 43, watching TV (5/6 studies)Footnote 29Footnote 32Footnote 33Footnote 34Footnote 42, texting/instant messaging (6/6 studies)Footnote 27Footnote 28Footnote 31Footnote 35Footnote 37Footnote 42, using a computer (3/3 studies)Footnote 32Footnote 33Footnote 41 and accessing the Internet (3/3 studies)Footnote 28Footnote 29Footnote 42, but not video games (1/4 studies)Footnote 33.
In terms of non-screen-based sedentary behaviours, 1 study reported a positive association between evening homework/reading and sleep durationFootnote 30, while 2 studies reported no associationFootnote 29Footnote 43. Listening to music on a phone or MP3 player in the evening was negatively associated with sleep duration in 2/2 studiesFootnote 28Footnote 33, while listening to the radio was not associated with sleep duration in 1/1 studiesFootnote 41. Two cross-sectional studies examined the relationship between evening screen use in bed and sleep durationFootnote 30Footnote 41. Of these, one reported that adolescents with the lowest self-reported sleep were more likely to report screen use in bedFootnote 30; the other reported that self-reported sleep duration was lower among adolescents who used computers, but not other screen-based devices, in bed “almost every night” or more oftenFootnote 41.
Quality of evidence was rated as low for all observational studies because of the lack of large effects or dose–response relationships.
Access to sedentary activities in the bedroom and sleep duration
Three longitudinalFootnote 25Footnote 46Footnote 47 and 12 cross-sectionalFootnote 41Footnote 42Footnote 43Footnote 44Footnote 45Footnote 48Footnote 49Footnote 50Footnote 51Footnote 52Footnote 53Footnote 54 studies examined the relationship between access to sedentary activities in the bedroom and sleep duration. The longitudinal studies provided mixed results: Cespedes et al.Footnote 45 found that the presence of a TV in the bedroom was associated with reduced sleep duration; King et al.Footnote 23 reported no association between bedroom screens and sleep duration; and Nuutinen et al.Footnote 46 reported that having a TV in the bedroom was negatively associated with weekend sleep duration among boys, and positively associated with weekend sleep duration among girls, with no significant associations observed between having a TV or computer in the bedroom and weekday sleep in either gender.
In the cross-sectional studies, associations between the use of screens in the bedroom and deleterious sleep duration were observed for computers (3/4 studies)Footnote 41Footnote 42Footnote 44 and all screen-based devices (3/3 studies)Footnote 40Footnote 42Footnote 52, with inconsistent results observed for TV watching (negative association observed for at least one analysis in 5/11 studies)Footnote 42Footnote 47Footnote 50Footnote 52Footnote 53, playing video games (negative association in 1/2 studies)Footnote 42 and using cell phones (negative association in 1/2 studies)Footnote 42.
The quality of evidence was rated as low; although bias was not a concern, there was no evidence of large magnitude of effect or dose–response relationships.
Sedentary behaviour timing and sleep quality
Eight nonrandomized intervention studies and 12 observational studies examined the relationship between sedentary behaviour timing and sleep quality. One intervention asked participants to avoid using screens after 9 p.m. on school nights for 2 weeksFootnote 20. Compared to baseline, this intervention resulted in earlier sleep onset on school nights, by 20 minutes, with no change in sleep efficiencyFootnote 20. The other interventions lasted one night; they reported significant associations between evening screen use and sleep onset latency (negative in 2/6 studies)Footnote 23Footnote 54, sleep efficiency (negative in 2/3 studies)Footnote 23Footnote 55, number of arousals per hour (negative in 1/1 studies)Footnote 55 but not waking after sleep onset (0/1 studies)Footnote 55.
One intervention study also reported that exposure to violent video games before bed reduced overall sleep quality for those with low exposure to games in daily life (≤1 hour/day), but not for those with high exposure (≥3 hours/day)Footnote 56.
Of the 6 interventions investigating device-measured sleep qualityFootnote 20Footnote 22Footnote 23Footnote 54Footnote 55Footnote 57, 4 reported negative associations between evening screen use and at least one outcome Footnote 20Footnote 23Footnote 54Footnote 55. The quality of evidence for intervention studies was rated as very low because of the lack of randomized trials, high risk of selection bias and inconsistency of results, with no evidence of large effects or dose–response relationship.
Two longitudinal studies examined the relationship between timing of sedentary behaviour and sleep quality over 1 yearFootnote 58 and 3 yearsFootnote 59. Foerster et al.Footnote 58 reported that adolescents woken by their phone were more likely to develop restless sleep and problems falling asleep than those who were not woken up by their phone. Similarly, Vernon et al.Footnote 59 reported that nighttime phone use was also associated with poor sleep quality.
The relationship between timing and sleep quality was also assessed in 10 cross-sectional studiesFootnote 32Footnote 33Footnote 34Footnote 35Footnote 37Footnote 39Footnote 40Footnote 43Footnote 60Footnote 61. The use of screen-based devices in the evening was negatively associated with measures of sleep quality in 7/9 studiesFootnote 33Footnote 34Footnote 35Footnote 37Footnote 40Footnote 60Footnote 61, positively associated with sleep quality in 1/9 studiesFootnote 34 and demonstrated null associations in 3/9 studiesFootnote 32Footnote 34Footnote 43. (Several studies reported associations for multiple measures of sleep quality.)
Daytime screen use was negatively associated with measures of sleep quality in 2/2 studiesFootnote 33Footnote 39 or had null associations in 1/2 studiesFootnote 39.
Overall sleep quality was negatively associated with evening screen use in 3/4 studiesFootnote 35Footnote 40Footnote 61, but was not associated with reading in 1/1 studiesFootnote 43. Sleep onset latency was positively associated with evening screen use in 2/3 studiesFootnote 33Footnote 60, negatively associated with evening screen use in 1/3 studiesFootnote 34 and positively associated with daytime screen use in 1/1 studiesFootnote 33. Sleep efficiency was negatively associated with evening screen access/use in 1/1 studiesFootnote 40. Insomnia symptoms were positively associated with evening screen use in 2/2 studiesFootnote 35Footnote 37. Waking up too early, difficulty falling asleep and sleeping restlessly were all positively associated with evening screen use in 1/1 studiesFootnote 34. Waking after sleep onsetFootnote 34 and frequency of sleep disturbancesFootnote 32 were not associated with evening screen use in 1/1 studies.
After-school homework and mobile phone use were positively associated with difficulty maintaining sleep in Grades 6 to 8 (but not Grades 4 to 5) and were not associated with difficulty falling asleep in either age group in 1/1 studiesFootnote 39.
The quality of evidence for these observational studies was rated as low, as there was a low risk of bias with no evidence of large effects or dose–response relationships.
Access to sedentary activities in the bedroom and sleep quality
Of the 5 cross-sectional studiesFootnote 40Footnote 43Footnote 52Footnote 53Footnote 61 that examined the relationship between access to screen-based devices in the bedroom and sleep quality, 4/5 reported negative associations between the presence of electronic screens in the bedroom and at least one measure of sleep qualityFootnote 40Footnote 43Footnote 52Footnote 61, and 1/5 reported only null associationsFootnote 53. Overall sleep quality was negatively associated with the presence of screen-based devices in the bedroom in 3/3 studiesFootnote 40Footnote 43Footnote 61, while both sleep efficiencyFootnote 40 and perceived insufficient sleepFootnote 52 were negatively associated with screen-based sedentary behaviours in 1/1 studies. Sleep onset insomnia was not associated with the presence of screens in the bedroom in 1/1 studiesFootnote 53.
The quality of evidence for these cross-sectional studies was rated as low; although risk of bias was low, there was no evidence of large effects or dose–response relationship.
Discussion
The purpose of this study was to systematically review the relationship between the timing of sedentary behaviours and access to sedentary activities in the bedroom with sleep duration and quality in children and youth. Our findings suggest that evening screen use and access to screen-based devices in the bedroom are associated with reduced sleep duration and quality in this age group. Intervention-based studies suggest that reducing evening screen use may lead to improved sleep duration and quality, although most interventions only examined a single night’s sleep. In the 2 studies lasting 1 week or longer, restricting evening screen use resulted in a roughly 20-minute increase in each night’s sleepFootnote 20Footnote 21, suggesting that the impacts may be clinically meaningful.
A secondary purpose of this review was to examine whether these relationships differ based on the mode of sedentary behaviour. In contrast to screen-based sedentary behaviours, our results suggest that reading and doing homework are not consistently associated with sleep duration or quality in this age group. Although only 3 studies reported on listening to music, 2 studies reported that listening to music on a cell phone or MP3 player was negatively associated with sleep durationFootnote 30Footnote 33, whereas listening to the radio was not associated with sleep durationFootnote 41.
Taken together, these findings suggest that screen-based sedentary behaviours are more likely to negatively impact sleep duration and quality, although relatively few studies examined the impact of non-screen-based sedentary behaviours. In contrast to previous researchFootnote 10, we found that, with the exception of video games, both interactive (e.g. computers, phones) and passive (e.g. TV viewing) forms of screen use were consistently associated with reduced sleep duration.
Compared to evening screen use, far fewer studies examined the impact of daytime use on sleep durationFootnote 33Footnote 39Footnote 44 or qualityFootnote 33Footnote 39; only one study examined associations between both daytime and evening sedentary behaviours and sleep duration or qualityFootnote 33. However, all these studies reported deleterious relationships between daytime screen use and at least one measure of sleep duration or quality. This is in line with previous research that found that total screen time is consistently associated with poorer sleep outcomes among children and youthFootnote 10. Unfortunately, the timing of sedentary behaviour was measured in various ways across studies, using broad descriptions such as “morning,” “after school” or “before bedtime.” This evidence gap makes it impossible to identify the optimal “cooling off” period prior to sleep. Further research is needed to directly compare the impact of sedentary behaviour during different periods of the day and night, as well as to examine the optimal interval between screen use and bedtime.
Our findings do suggest that children and youth are likely to benefit from following the recommendations of the American Academy of PediatricsFootnote 15 and Canadian Pediatric SocietyFootnote 16, both of which include removing screens from bedrooms and avoiding screens for at least 1 hour before bed. Although the current findings are based on very low quality evidence, meeting these recommendations will likely still benefit sleep, with very low risk of harm. Removing screens from bedrooms is particularly important because bedroom screen use is most likely to directly displace or delay sleep. This may also be easier than reducing screen time during other periods of the day, when parents have less control over screen use. It is important that schools and teachers help to support students in limiting their evening screen time, by limiting the volume and frequency of screen-based homework that must be completed each day.
Although we cannot rule out the possibility of a bidirectional relationship, the evidence included in this review does not suggest that changes in sleep duration or quality lead to increases in evening screen use. Of the longitudinal studies we identify in the review, none reported that reductions in sleep quality or duration predicted subsequent increases in evening screen time. Further, the intervention studies included suggest that increases in evening screen use are associated with subsequent reductions in sleep duration and quality. Future studies should specifically investigate the directionality of the relationship between sedentary behaviour timing and sleep outcomes.
Strengths and limitations
This review has a number of strengths and limitations. We used a comprehensive search strategy, included all study designs, assessed risk of bias within studies and used the GRADE approach to determine the certainty of evidence across studies. However, GRADE takes a conservative approach, with all study designs other than randomized trials starting as “low quality” by default.Footnote 18
All the cross-sectional studies (but not longitudinal or intervention studies) had to have a minimum of 1000 participants, which may have limited the number of included studies for some outcomes. Restricting inclusion to larger cross-sectional studies increases the likelihood of detecting a true effectFootnote 62, and the large number of included studies (n = 44) and participants (n = 239 267) increased the confidence in our findings. The studies excluded because of small sample size had altogether 17 603 eligible participants, which represents just 7% of participants in the papers in this review.
Our search strategy did not include grey literature and we did not contact content experts, although we believe this would be unlikely to impact our overall findings. Our review also identified relatively few intervention studies.
The studies did not differentiate between recreational and school-related screen time; nor did they indicate whether homework was screen or paper based. Future studies should employ randomized intervention studies to better understand the chronic impact of reductions in evening screen use, and to examine the associations between sleep and both recreational and school-related screen time.
All the observational studies in our review measured self- or parent-reported sedentary behaviour; using objective measures of sedentary behaviour timing would improve the quality of future research. Because of the heterogeneity in the included studies, we were unable to perform meta-analyses, which also precluded a formal assessment of publication bias or investigation of whether relationships varied by age or gender. However, only including studies published in the last 10 years could have partly mitigated the risk of publication bias, as many more journals publish null findings in recent years.
Finally, our review was limited to English and French language peer-reviewed papers, although available evidence suggests these restrictions are unlikely to impact our findingsFootnote 63Footnote 64.
Conclusion
Our results suggest that engaging in screen-based sedentary behaviours in the evening and access to screen-based devices in the bedroom are associated with reduced sleep duration and quality among school-aged children and youth. In contrast, there were no consistent associations between non-screen-based sedentary behaviours and sleep duration or quality in this age group. In order to maximize sleep duration and quality, children and youth should minimize screen time prior to bedtime and remove screens from their bedrooms.
Acknowledgements
TJS was supported by the Jeanne and J.-Louis Lévesque Professorship in Nutrisciences and Health.
Registration of the protocol
PROSPERO registration no. CRD42020189082, available online.
Conflicts of interests
TJS has received honorariums for public presentations on the health impact of sedentary behaviour. The other authors have no conflicts to declare.
Authors’ contributions and statement
TJS, TM, JC, SAP and KD screened the papers.
TM and TJS extracted the data and performed the risk of bias and GRADE assessments.
TJS drafted the final version of the manuscript.
All authors were involved in the conception of the study, and all authors reviewed and approved the final version for publication.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
