Evidence synthesis – Mapping social determinants of cognitive health in Canada: a scoping review

HPCDP Journal Home
Published by: The Public Health Agency of Canada
Date published: November 2025
ISSN: 2368-738X
Submit a manuscript
About HPCDP
Browse
Sarah O’ConnorAuthor reference footnote *, RD, MSc; Teodora RigleaAuthor reference footnote *, RN, MSc; Mathilde Lavigne‑Robichaud, PhD; Lucie Lapierre, PhD
https://doi.org/10.24095/hpcdp.45.11/12.01
This article has been peer reviewed.

Recommended Attribution
Evidence synthesis by O’Connor S et al. in the HPCDP Journal licensed under a Creative Commons Attribution 4.0 International License
Author reference
Public Health Capacity and Knowledge Mobilization Unit, Operation and Emergency Management Branch, Public Health Agency of Canada, Montréal, Quebec, Canada
Correspondence
Sarah O’Connor, Public Health Capacity and Knowledge Mobilization Unit, Regulatory, Operation and Emergency Management Branch, Public Health Agency of Canada, Quebec Regional Office, 200, boul. René-Lévesque Ouest, East Tower, Montréal, QC H2Z 1X4; Tel: 418-473-4488; Email: sarah.oconnor@phac-aspc.gc.ca
Suggested citation
O’Connor S, Riglea T, Lavigne-Robichaud M, Lapierre L. Mapping social determinants of cognitive health in Canada: a scoping review. Health Promot Chronic Dis Prev Can. 2025;45(11/12):431-44. https://doi.org/10.24095/hpcdp.45.11/12.01
Abstract
Introduction: We sought to map the literature assessing the associations between the social determinants of health (SDoH) and the cognitive health of adults in Canada.
Methods: We searched the Embase, CENTRAL, Global Health and MEDLINE databases through Ovid, from inception to 20 February 2024, for studies examining associations between SDoH and cognitive health among Canadian adults, irrespective of health or cognitive status.
Results: We identified 159 publications covering 93 studies; 27% (n = 25) had nationwide coverage and 48% (n = 45) were from Ontario or Quebec. Of the 410 associations between SDoH and cognition, 20 were from 6 qualitative studies and 390 from 87 quantitative studies. Education was the most frequently evaluated (46%) of the 29 identified SDoH categories, then social support (24%), household/individual income (19%), marital status (17%), occupation (16%), rural or urban area of residence (16%), living arrangement/household composition (12%) and environmental factors (13%). Two-thirds (67%) of the studies examined various cognitive health constructs, while 41% evaluated dementia (all types). Most of the SDoH were from the settings with which individuals directly interact. SDoH related to environmental exposure or pollution, societal norms, beliefs, values and practices were less frequently evaluated.
Conclusion: This scoping review provides a detailed map of the literature on SDoH and cognitive health in Canada. It highlights the importance of considering a comprehensive range of SDoH and of using diverse data sources and data collection approaches. The results also highlight SDoH that remain largely unexamined and should be prioritized in future research.
Keywords: dementia, social determinants of health, scoping review, Alzheimer disease, cognition, education, social support
Highlights
- The 93 studies we reviewed identified 29 categories of social determinants of health (SDoH) associated with the cognitive health of adults in Canada.
- Education and social support were most frequently examined SDoH.
- Most of the examined SDoH were within people’s immediate environments, while systemic and structural SDoH were less frequently examined.
- Almost half of the studies were conducted in Ontario or Quebec, and there were no data specific to Yukon, the Northwest Territories, Nunavut, Nova Scotia or Prince Edward Island.
- Only two interventional studies evaluated the impact of SDoH on cognitive health, which highlights a gap in the integration of health impact assessments in public health initiatives.
Introduction
Between 2022 and 2023, approximately 487 000 (6.2%) of Canadians aged 65 years and older were living with diagnosed dementia, with 99 000 newly diagnosed during this period.Footnote 1 While the incidence rate of dementia in this age group has been decreasing over the past decade, the overall number of Canadians with dementia is expected to increase because of the aging population.Footnote 2 In response to the urgent need to understand and prevent dementia, the Parliament of Canada passed the National Strategy for Alzheimer’s Disease and Other Dementias ActFootnote 3 in 2017. In 2019, the federal Minister of Health released the first national strategy, A Dementia Strategy for Canada: Together We Aspire,Footnote 4 and subsequently, related annual reports.Footnote 5Footnote 6
In 2024, the Lancet Commission on dementia estimated that 45.3% of dementia cases could be explained by 14 risk factors: 1) less education; 2) hearing loss; 3) high LDL cholesterol; 4) depression; 5) traumatic brain injury; 6) physical inactivity; 7) diabetes; 8) smoking; 9) hypertension; 10) obesity; 11) excessive alcohol use; 12) social isolation; 13) air pollution; and 14) vision loss.Footnote 7 While many of these risk factors can be modified at the individual level, not everyone has access to the resources necessary to address them effectively.Footnote 8Footnote 9 As the Alzheimer Society of Canada noted, “These risk factors are only truly modifiable if the proper supports are provided by our communities, public health agencies and other governmental organizations.”Footnote 8,p.50
Social determinants of health (SDoH)—the conditions in the environments where “people are born, grow, live, work and age”Footnote 10,p.76—profoundly influence people’s exposure to or ability to modify the risk factors identified by the Lancet Commission.Footnote 7Footnote 8 The differences in the distribution of SDoH across subgroups and populations derive from established systemic social, political and economic structures, which lead to socioeconomic and health inequalities and, ultimately, disparities in health outcomes, including cognitive diseases.Footnote 11
The framework proposed by Adkins-Jackson et al.Footnote 11 incorporates Bronfenbrenner’s ecological theoryFootnote 12 to illustrate how SDoH influence the risk of dementias classified as Alzheimer disease. This framework depicts a continuum of embedded and interdependent systems: the microsystem (the settings with which individuals directly interact); the mesosystem (interactions between microsystems); the exosystem (the factors that indirectly influence health, such as climate change); the macrosystem (societal norms, beliefs, values and practices established in the society in which individuals live that influence microsystems); and the chronosystem (exposure to SDoH during the life course)Footnote 11 (see Supplemental Figure 1). As such, key SDoH that influence cognitive health and dementia include the 14 risk factors identified by the Lancet CommissionFootnote 7 as well as neighbourhood deprivation, workplace conditions and occupation, financial and food insecurity, poverty, housing and other factors. These, in turn, are influenced by broader systemic SDoH such as structural racism, discrimination or ageism.Footnote 13
Although Canada’s national dementia strategyFootnote 3 includes prevention as a core objective, it primarily focuses on the individual risk factors identified by the Lancet Commission;Footnote 7 targeting the broader structural determinants of these risk factors is less evident. Given that the interdependence of the SDoH systems can result in a cascade of effects on individuals’ capacity to act upon modifiable risk factors and take action to prevent diseases,Footnote 11 it is essential to consider the structural SDoH that shape health disparities and the incidence of cognitive diseases in Canada. Although interest in the role of SDoH in cognitive health and dementia is increasing,Footnote 8 we do not yet have a comprehensive synthesis of the existing Canadian scientific literature examining associations between SDoH and cognition.
The objective of this scoping review was to map the current state of knowledge on the SDoH that affect cognitive health among adults in Canada.
Methods
This scoping review was conducted according to JBI’s guide for scoping reviewsFootnote 14 and the six-stage approach from Arksey and O’MalleyFootnote 15 and Levac et al.Footnote 16 We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR).Footnote 17 The protocol is available online.
Eligibility criteria
We included studies that assessed all levels of cognitive health status (i.e. healthy cognitive status, mild cognitive impairment or diagnosed dementia [all types]) in samples of adult participants aged 18 years or older or in samples of youth and adults composed mainly (≥ 80%) of adults. No restrictions were imposed on pre-existing health conditions, including diseases that may affect cognitive health. Although we did not include studies that focused on caregivers as the unit of analysis, we included studies in which the presence of caregivers was considered an SDoH for cognitive health.
Only those studies examining populations living in Canada were included. Multicountry studies were included if we could extract results specific to Canada.
We included studies if they evaluated an association between SDoH and at least one aspect of cognitive health. We initially limited SDoH to the World Health Organization definitionFootnote 10 but subsequently expanded our examination to include those identified in the Adkins-Jackson et al. frameworkFootnote 11 and others that may be related to cognitive health.Footnote 18
We excluded studies that assessed individual nonmodifiable risk factors (e.g. age, sex, genotype) or modifiable risk factors (e.g. diet, physical activity, tobacco use, clinical measurements [anthropometric measurements, blood pressure, lipid profile, glucose profile]) without evaluating SDoH. Macrosystem-level risk factors (e.g. gender) were considered to be SDoH if specific or indirect assessments of societal norms, beliefs, values, practices or points of view were conducted (e.g. genderism—the belief that there are only two genders and that a person’s gender should align with their sex as assigned at birth).
Cognitive health is a global concept that includes (but is not limited to) dementia and the overall progression towards dementia. We defined cognitive health broadly as the ability to think clearly, to learn and to remember.Footnote 19 (Definitions for the different cognitive health constructs considered in this scoping review are listed in Supplemental Table 1.) The tools used to evaluate cognitive constructs included self-reported outcomes, standardized or home tests, questionnaires, medical diagnosis screenings and cognitive evaluations (see Supplemental Table 2).
The following constructs were not considered because they are only indirectly associated with cognitive health: mental health or psychiatric conditions (e.g. depression, anxiety, psychosis, schizophrenia or bipolar disorder, attention deficit disorder with or without hyperactivity), intelligence tests, and motor impairments or related diseases (e.g. Parkinson disease, multiple sclerosis).
We included quantitative and qualitative peer-reviewed studies as well as conference abstracts. In quantitative studies, only univariate and multivariate associations where SDoH were considered the main exposure or a predictor were included; SDoH used as adjustment variables were not. Qualitative studies of perceived changes in cognitive health (or symptoms of) in the presence of a specific SDoH were included. We included both empirical and conceptual studies as long as they reported an association between SDoH and cognition. Reviews, government policy documents and protocols were excluded.
There were no restrictions on the year of publication, although conference abstracts were limited to the last 5 years (2019–2024).
Search and study selection
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), Embase, Global Health and MEDLINE biomedical databases through Ovid, from their inception until 20 February 2024, using both indexed and free keywords associated with SDoH, cognitive health and Canadian contexts (see Supplemental Table 3). The search strategy was reviewed and validated by a science librarian.
Citations were imported into Covidence (Veritas Health Innovation, Melbourne, AU) and duplicates were removed. Two reviewers [TR, SO] independently screened the titles, abstracts and full texts of the retrieved studies. Any differences were resolved by other reviewers [MLR, LL]. The search strategy was re-evaluated iteratively. Because of the large number of eligible studies, we restricted the search to biomedical databases only.
Data extraction and charting
Data were extracted by one reviewer [TR or SO] into a pre-piloted data collection form. The following details were collected from each retrieved publication: year of publication, study design, name of the study, sample size and examined SDoH, cognitive health constructs and their associations. As the assessment of the effects of exposures was not an objective, we did not appraise risk of bias.
To avoid overestimating the frequency of associations, we combined articles that used the same cohort and treated them as one study.
Using each study as the unit of analysis, we gathered information on the study participants’ age, sex, rural versus urban area of residence, health conditions, cognitive status at baseline and location in Canada. Identical associations in a single study were combined. In each study, we identified all the associations between individual cognitive health constructs and each given SDoH. Thus, if a study reported on several associations between a specific SDoH and different cognitive health constructs, each association was counted independently of the others. In the case of longitudinal studies with multiple time points, we selected the most recent time point. Measures assessing similar SDoH were combined into the same categories and classified according to the Adkins-Jackson et al. framework.Footnote 11
When SDoH were assessed using indirect measures or proxies, we categorized them with the closest to the SDoH of interest. For example, self-reported race or ethnicity would be categorized in the macrosystem as an indirect measure of potential racism.
We summarized data on SDoH, cognitive health constructs and their associations using frequencies or proportions. Associations reported in qualitative studies are summarized separately.
Results
Search results
Of the 7390 records retrieved, 159 publications were included in this scoping review (see Figure 1). Of these, 158 were in English and 18 had abstracts in French. Articles were published between 1991 and 2024, with 101 published since 2014 and 72 since 2019. The sample sizes for both the qualitative and quantitative studies ranged from 3 to 6538000 participants. Of the included publications, 85 had cross-sectional designs, 49 retrospective or prospective cohort designs, eight case-control or nested case-control designs, six qualitative or mixed designs, six repeated cross-sectional designs, one case-crossover design, one randomized controlled trial, one pre–post design with no control group and one post hoc analysis of a nonrandomized controlled trial. (See Supplemental Table 4 for the details of included publications.)
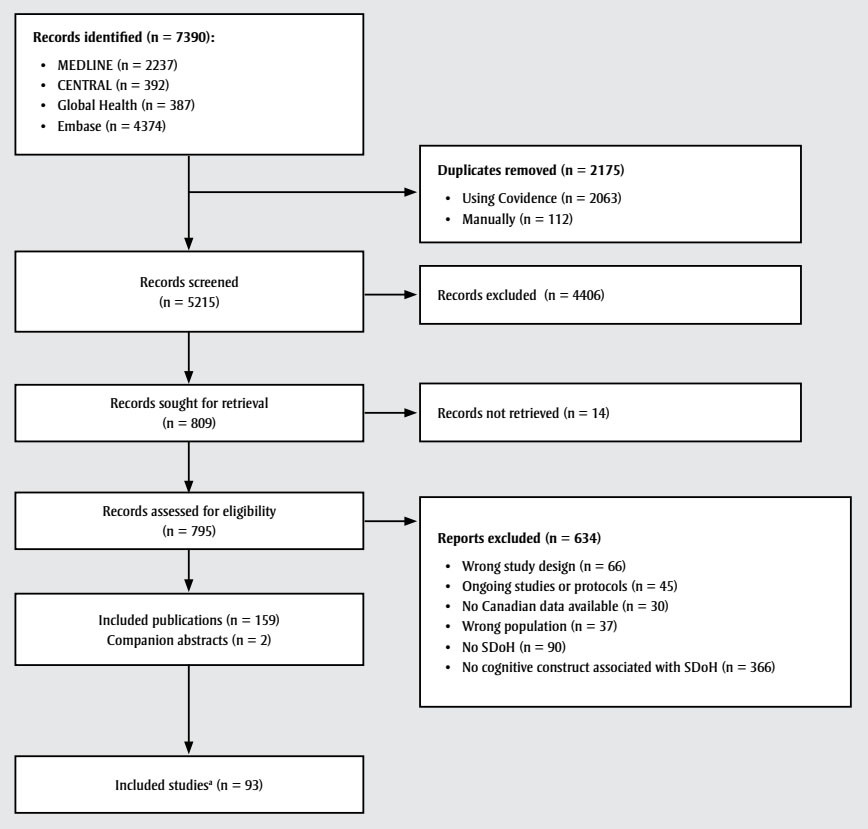
Figure 1: Descriptive text
This figure depicts the process through which studies were identified and selected to be included in this scoping review.
As a first step, n = 7390 records were identified:
- MEDLINE (n = 2237)
- CENTRAL (n = 392)
- Global Health (n = 387)
- Embase (n = 4374)
Of these, n = 2175 duplicates were removed:
- Using Covidence (n = 2063)
- Manually (n = 112)
This left n = 5215 records to be screened. As a result of this screening, n = 4406 records were excluded. The remaining 809 records were sought for retrieval, of which 14 were not retrieved. The remaining 795 records were assessed for eligibility, of which 634 reports were excluded for the following reasons:
- Wrong study design (n = 66)
- Ongoing studies or protocols (n = 45)
- No Canadian data available (n = 30)
- Wrong population (n = 37)
- No SDoH (n = 90)
- No cognitive construct associated with SDoH (n = 366)
This resulted in n = 93 studies included in the scoping review.
Study characteristics
The 159 retrieved publications covered 93 individual studies. Of these, 25 had national coverage or covered multiple provinces, and almost half (n = 45) were conducted in Ontario or Quebec. (See Table 1 for summaries of study participants’ characteristics and the contexts of the retrieved studies; for additional details, see Supplemental Table 5 and 6.)
| Characteristics | n (%)Footnote a |
|---|---|
| Location | |
| Multiple provinces or nationwide coverage | 25 (27) |
| British Columbia | 4 (4) |
| Alberta | 7 (8) |
| Saskatchewan | 4 (4) |
| Manitoba | 2 (2) |
| Ontario | 25 (27) |
| Quebec | 20 (22) |
| New Brunswick | 1 (1) |
| Nova Scotia | 0 |
| Prince Edward Island | 0 |
| Newfoundland and Labrador | 2 (2) |
| Yukon, Northwest Territories and Nunavut | 0 |
| Not reported | 3 (3) |
| Sex of participants | |
| Both | 72 (77) |
| Men | 6 (7) |
| Women | 4 (4) |
| Not reported | 11 (12) |
| Age group | |
| Young adults | 1 (1) |
| Older adults | 36 (39) |
| Adults (no specification) | 56 (60) |
| Main type of data used | |
| Administrative database | 21 (23) |
| Clinical data | 8 (9) |
| Medical records | 4 (4) |
| Survey data | 29 (31) |
| Qualitative data | 6 (6) |
| Mixed | 25 (27) |
| Study population | |
| Ambulatory clinics | 17 (18) |
| Community dwellings | 59 (63) |
| First Nations, Inuit or Métis communities | 3 (3) |
| Emergency departments | 1 (1) |
| Home care settings | 2 (2) |
| Hospital settings | 4 (4) |
| Long-term care facilities | 6 (6) |
| Correctional facilities | 1 (1) |
| Cognitive status at baseline | |
| Cognitively healthy | 17 (18) |
| Cognitive impairment or dementia | 6 (6) |
| Mixed | 30 (32) |
| Not reported | 40 (43) |
We sorted the identified SDoH into 29 categories (see Table 2). A total of 80 studies (86%) assessed microsystem-level SDoH, for example, education (46%), social support (24%), household/individual income (19%), occupation (16%), urban or rural area of residence (16%), marital status (17%) and living arrangement/household composition (12%). Twelve studies (13%) evaluated exposure to environmental pollutants, an exosystem-level SDoH, and 31 (33%) assessed macrosystem-level SDoH, including access to health care (11%), ethnicity (11%), primary language or language barriers (11%) and First Nations, Inuit or Métis identity (4%). Some SDoH were evaluated retrospectively over the lifespan (the chronosystem), the most common being highest educational attainment and past occupational exposure to pollutants. One study assessed the history of childhood maltreatment, and one evaluated perinatal and childhood exposure to mercury. None of the studies retrieved assessed interactions between different microsystems (i.e. the mesosystem).
| SDoHFootnote a | n (%) | ||
|---|---|---|---|
| All studies (n = 93) |
Quantitative studies (n = 87) |
Qualitative studies (n = 6) |
|
| MicrosystemFootnote b | |||
| Education | 43 (46) | 42 (48) | 1 (17) |
| Social support | 22 (24) | 18 (21) | 4 (66) |
| Income | 18 (19) | 18 (21) | 0 |
| Marital status | 16 (17) | 16 (18) | 0 |
| Occupation or employment | 15 (16) | 15 (17) | 0 |
| Area of residence (rural/urban) | 15 (16) | 13 (15) | 2 (33) |
| Immigration status | 11 (12) | 10 (11) | 1 (17) |
| Living arrangement/household composition | 11 (12) | 11 (13) | 0 |
| Built environment | 10 (11) | 10 (11) | 1 (17) |
| Housing | 10 (11) | 9 (10) | 0 |
| Neighbourhood deprivation or socioeconomic status | 8 (9) | 8 (9) | 0 |
| Childhood maltreatment | 6 (6) | 5 (6) | 1 (17) |
| Occupational exposure | 4 (4) | 4 (5) | 0 |
| Loneliness | 4 (4) | 4 (5) | 0 |
| Food security | 1 (1) | 1 (1) | 0 |
| ExosystemFootnote c | |||
| Environmental pollutants | 12 (13) | 12 (14) | 0 |
| MacrosystemFootnote d | |||
| Access to health care | 10 (11) | 8 (9) | 2 (33) |
| Ethnicity | 10 (11) | 10 (11) | 0 |
| Primary language or language barriers | 10 (11) | 9 (10) | 1 (17) |
| First Nations, Inuit or Métis identity | 4 (4) | 3 (3) | 1 (17) |
| Knowledge of cognitive health | 2 (2) | 1 (1) | 1 (17) |
| Policy implementation | 2 (2) | 2 (2) | 0 |
| Religion | 2 (2) | 1 (1) | 1 (17) |
| Sexual orientation | 2 (2) | 2 (2) | 0 |
| Stigma | 2 (2) | 1 (1) | 1 (17) |
| Culture | 1 (1) | 0 | 1 (17) |
| Gender identity or genderism | 1 (1) | 1 (1) | 0 |
| Marginalization | 1 (1) | 1 (1) | 0 |
| Quality of care | 1 (1) | 0 | 1 (17) |
A total of 62 studies assessed either global cognition using, for example, the Mini Mental State Examination, the Montreal Cognitive Assessment (MoCA), the Cognitive Performance Scale, or global cognition composite measures, or a specific cognitive health construct using, for example, tests for executive function, processing speed or memory. A diagnosis of dementia (all types) was an outcome associated with SDoH in 38 studies (see Table 3; for additional information on the SDoH and cognitive constructs evaluated across studies, see Supplemental Table 5).
| Cognitive health constructs | n (%) | ||
|---|---|---|---|
| All studies (n = 93) |
Quantitative studies (n = 87) |
Qualitative studies (n = 6) |
|
| Global cognition and cognitive health constructs | |||
| Global cognitionFootnote a | 47 (51) | 46 (53) | 1 (17) |
| Executive function | 12 (13) | 12 (14) | 0 |
| Processing speed | 9 (10) | 9 (10) | 0 |
| Visuospatial processing | 4 (4) | 4 (5) | 0 |
| Verbal fluency | 7 (8) | 7 (8) | 0 |
| Memory (large) | 17 (18) | 16 (18) | 1 (17) |
| Verbal learning and memory | 9 (10) | 9 (10) | 0 |
| Working memory | 5 (5) | 5 (6) | 0 |
| Prospective memory | 1 (1) | 1 (1) | 0 |
| Verbal comprehension | 1 (1) | 1 (1) | 0 |
| Self-reported cognition, memory or cognitive decline | 11 (12) | 9 (10) | 2 (33) |
| Mild cognitive impairment and dementiaFootnote b | |||
| Dementia (all types) diagnosis | 38 (41) | 35 (40) | 3 (50) |
| Alzheimer disease | 13 (14) | 13 (15) | 0 |
| Vascular dementia | 2 (2) | 2 (2) | 0 |
| Self-reported dementia | 5 (5) | 5 (6) | 0 |
| Death associated with dementia | 2 (2) | 2 (2) | 0 |
| Mild cognitive impairment diagnosis | 10 (11) | 10 (11) | 0 |
| Self-reported healthy aging | 1 (1) | 0 | 1 (17) |
Associations between SDoH and cognition
We identified 410 main associations between SDoH and cognitive health constructs across the 93 individual studies included in this scoping review (see Supplemental Table 6). Of these 410 associations, 87 quantitative analyses reported 390 associations between SDoH categories and cognitive health constructs (see Supplemental Table 4) and six qualitative studies reported 20 descriptive thematic data linking SDoH and cognitive outcomes (see Supplemental Table 5).Footnote 20Footnote 21Footnote 22Footnote 23Footnote 24Footnote 25 We also retrieved two trials that reported on interventions addressing SDoH (access to health care, rural or urban area of residence) and evaluated their impact on cognitive health.Footnote 26Footnote 27
Quantitative studies
Of the 390 associations between SDoH and cognition and dementia in quantitative studies, education was the most frequently studied, followed by social support and household/individual income (see Table 4).
| SDoH | Cognitive health constructs, n | Dementia diagnosis, n | Cognitive impairment diagnosis, n | Death associated with dementia, n | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Global cognitionFootnote a | Memory (all constructs) | Executive function | Verbal fluency | Processing speed | Visuospatial processing | Verbal comprehension | Attention | Dementia (all types)Footnote b | Alzheimer disease | Self-reported dementia | Vascular dementia | |||
| Education | 23 | 8 | 5 | 4 | 4 | 3 | 1 | 1 | 11 | 4 | 3 | 1 | 4 | 1 |
| Social support | 13 | 6 | 5 | 5 | 1 | 1 | 1 | 0 | 6 | 2 | 1 | 0 | 1 | 0 |
| Income | 11 | 3 | 3 | 2 | 0 | 1 | 0 | 0 | 8 | 0 | 0 | 0 | 1 | 1 |
| Occupation or employment | 11 | 3 | 2 | 1 | 2 | 0 | 0 | 0 | 3 | 1 | 1 | 1 | 0 | 2 |
| Marital status | 11 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 5 | 0 | 2 | 0 | 4 | 1 |
| Environmental pollutants | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 9 | 5 | 0 | 0 | 0 | 1 |
| Area of residence (rural/urban) | 5 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 1 | 1 | 1 | 0 | 1 |
| Living arrangement/ household composition | 8 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 4 | 0 | 1 | 0 | 1 | 0 |
| Ethnicity | 7 | 3 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 2 | 0 |
| Immigration status | 6 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 1 | 1 |
| Built environment | 2 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 5 | 2 | 0 | 0 | 0 | 1 |
| Neighbourhood deprivation or socioeconomic status | 3 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 5 | 1 | 0 | 0 | 0 | 0 |
| Access to health care | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 1 | 0 | 2 | 0 |
| Housing | 6 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 |
| Primary language or language barriers | 5 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 3 | 0 | 1 | 0 | 0 | 0 |
| Loneliness | 3 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Occupational exposure | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 3 | 0 | 2 | 0 | 0 |
| Childhood maltreatment | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| Sexual orientation | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| First Nations, Inuit or Métis identity | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Policy implementation | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Gender identity or genderism | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Food security | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Knowledge of cognitive health | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Marginalization | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Religion | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Stigma | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Qualitative studies
The six qualitative studies were conducted in Alberta, Saskatchewan, Ontario and Newfoundland and Labrador with various populations, for example, people living with dementia, caregivers and health care workers, sex workers and Indigenous grandmothers.Footnote 20Footnote 21Footnote 22Footnote 23Footnote 24Footnote 25 Access to health care was the most studied SDoH, followed by social support and area of residence (rural or urban). Macrosystemic SDoH such as stigma, religion, ethnicity, cultural background and maltreatment were also examined (see Table 5).
| Study / Setting | Population | Social determinants of health | Selected quotes |
|---|---|---|---|
| Di Gregorio et al.(2015)Footnote 21 Four communities in northern Ontario |
2 people living with dementia, 15 care partners, 37 health care and social service providers, 17 other community members | Health care service providers’ knowledge and awareness; access to health care; awareness and understanding of dementia; rural environment; community support networks; health and community care services | “Awareness is the first step in which one begins to have knowledge of the phenomenon: in this case, the signs and symptoms of dementia, the available resources, or people who have dementia.” “Despite lack of awareness of the signs and symptoms of dementia, people who were diagnosed with dementia were often more visible in rural environments.” |
| Pace (2020)Footnote 20 NunatuKavut community, Newfoundland and Labrador |
14 adults ≥ 50 years, family caregivers and home care workers | Social support | “Loneliness and isolation were described as risk factors for developing dementia, whereas social contact was seen as protective against cognitive decline. […] Participants described that seeing other people regularly was good for the brain and for mental wellness. Visiting and social gatherings were perceived to spur laughter, storytelling, and reminiscence, which were described as supportive of memory as well as the reinforcement of collective identity and shared experiences.” |
| Baumann et al. (2019)Footnote 22 Urban settings in Toronto, Ontario |
10 sex workers, women (n = 5) and transgendered women (n = 5), aged ≥18 years, in the Worksafe program | Sexual violence | “Some participants […] reported experiencing long-term consequences such as persistent memory loss, noise sensitivity and scars. Tiffany, who was strangled by an acquaintance, has persistent anxiety and memory loss, and shared that she has ‘short-term memory problems right now and [gets] constant headaches’ […]” |
| Bacsu et al. (2020)Footnote 23 Two rural communities in Saskatchewan |
42 adults aged ≥ 60 years | Social support | “Rural older adults identified social engagement as being vital to supporting cognitive health. For instance, an older adult stated, ‘I feel a lot of brain health is due to mingling with others….’ In particular, rural seniors described activities related to two subthemes: technology and social media; and community activities.” |
| Koehn et al. (2016)Footnote 24 Chinese-Canadians in Greater Vancouver, British Columbia; anglophones in Calgary, Alberta; East Indian Canadians in Toronto, Ontario; francophones in Ottawa, Ontario |
29 dementia and caregiver dyads | Access to health care; cultural background; education; immigration status; language barriers; quality of care; religion; social support; stigma | "Also important, however, is that credible sources be knowledgeable about the disease, which is where immigrant-serving agency staff typically fall short, since most lack the education in, and hence understanding of, the symptomology and trajectory of dementia and may not steer the person with dementia in the direction of appropriate services.” |
| Lanting et al. (2011)Footnote 25 Northern communities in Saskatchewan |
Three Indigenous grandmothers | Road access to northern communities (built environment); perceived cultural changes; culturally grounded health care | “[…] these data suggest common core cultural perceptions of aging and dementia identified by a group of [Indigenous] grandmothers. Additionally, perceived changes in culture are thought to underlie the increase in illness among [Indigenous] seniors and to negatively impact the process of aging.” |
Discussion
Impact of SDoH on cognitive outcomes in Canada
Using an ecological framework,Footnote 10 we retrieved 159 publications covering 93 studies that encompassed numerous SDoH and cognitive health outcomes, including established associations (e.g. education, social support) and emerging or less-studied ones (e.g. working conditions, SDoH from the macrosystem).
Our synthesis highlights researchers’ sustained efforts to understand the impact of SDoH on cognitive health in Canada. This scoping review complements existing international reviewsFootnote 28Footnote 29Footnote 30 and is the first to examine a comprehensive range of SDoH in relation to cognitive health in Canada. This synthesis provides information for policy makers and public health authorities on how Canadians’ living, work and aging conditions may affect cognitive outcomes.
Geographical scope and representation of SDoH research
About one-quarter (27%) of the included studies had nationwide coverage, while almost half were conducted in Ontario (27%) or Quebec (22%), the two most populous Canadian provinces. Nationwide studies, especially those with nationally representative samples, are useful for their generalizability and for identifying regional differences in the distribution of SDoH and health outcomes. However, we did not identify any studies conducted in Yukon, the Northwest Territories or Nunavut, and no province-specific findings from Nova Scotia or Prince Edward Island were available outside of multiprovince or nationwide studies. These gaps in the existing research highlight the need to research inadequately studied populations in Canada.
Macrolevel and microlevel determinants and measurement challenges
We found that 86% of the associations were with SDoH categorized in the microsystem, or the individual’s immediate environment, which aligns with the findings of a similar scoping review.Footnote 28 Only one-third (33%) of the associations were with macrosystemic SDoH, which highlights a potential challenge in assessing these upstream, structural SDoH.
The macrosystem, the outermost layer of the embedded systems surrounding the individual, has been described as the realm of the power systems driving SDoH and health disparities and as permeating throughout all other systems.Footnote 11 Although macrosystemic SDoH have been less studied than those from the microsystem, we identified 31 studies assessing diverse macrosystemic SDoH, including knowledge of cognitive health, policy implementation, religion, stigma, sexual orientation and gender identity.
The inclusion of qualitative studies enabled us to identify subjective experiences of SDoH, including stigma, discrimination or other associations with cultural background, ageism and genderism, which can be harder to assess otherwise. Future studies should focus on better ways to assess macrosystemic SDoH.
Established and emerging determinants
We found education and social support to be the most frequently studied SDoH, which aligns with the findings of other reviews.Footnote 28Footnote 29Footnote 30 Social support, especially social engagement, social activities and the quality of relationships with caregivers, has been consistently studied in its relation to the cognitive health of individuals with or at risk for Alzheimer disease and related dementias.Footnote 30 Marital status or loneliness may also play a role in cognitive decline, although the supporting evidence remains weaker than that for social engagement.Footnote 30
Longitudinal studies have also observed education to be a protective factor against dementia-related pathologies, possibly due to greater cognitive reserve.Footnote 6Footnote 31Footnote 32Footnote 33 The role of education in cognitive health is complex, as individuals with higher levels of education generally perform better on neurocognitive tests than those with a lower educational attainment.Footnote 34 Thus, education could be considered either a key predictor or a confounding factor. However, education as a variable was usually self-reported formal education, either educational attainment or years of education, while cognitive stimulation from continuous learning throughout the lifespan remained largely unexamined in longitudinal studies.Footnote 35
The role of occupational factors in cognitive health is increasingly recognized.Footnote 36 Most of the studies in this review focused solely on occupation or employment status, but a few assessed exposure to chemicals or psychosocial hardships during work.Footnote 36Footnote 37Footnote 38Footnote 39Footnote 40Footnote 41Footnote 42Footnote 43Footnote 44Footnote 45Footnote 46Footnote 47 Although many studies have examined exposure to work-related hazards (e.g. exposure to chemicals, work in the mining industry),Footnote 36Footnote 37Footnote 38Footnote 39Footnote 40Footnote 41Footnote 42Footnote 43Footnote 44Footnote 45Footnote 46Footnote 47 the psychosocial aspects of work conditions (e.g. job strain, high psychological demand or low job control perception, job complexity) have only recently been investigated in a handful of studies, with mixed results.Footnote 36Footnote 42Footnote 43Footnote 44Footnote 45
Quebec’s progressive occupational health and safety legislation provides a framework for protecting workers against physical and psychosocial hazards in the workplace, recognizing the broader health impacts that may extend into retirement.Footnote 36Footnote 48 By requiring the assessment of workplace stressors such as job strain, high psychological demand, low job control and job complexity, and by mandating actions to mitigate them, this legislation has the potential to enhance cognitive health as well as cardiovascular and mental health outcomes.Footnote 49Footnote 50 Quebec’s approach recognizes workplace psychosocial stressors as modifiable SDoH that can be addressed through targeted interventions and legislation.Footnote 48Footnote 51
The built and natural environments also play a significant role in cognitive health; protective and risk factors depend on the availability of green spaces, walkable areas, social and physical activities, and other resources. Research conducted in Canada suggests that access to green spaces is associated with lower rates of dementia.Footnote 52Footnote 53 Higher walkability scores are correlated with improved cognitive functioning in aging populations, underscoring the benefits of accessible and active living environments.Footnote 54 Consistent with these findings, Canada’s national dementia strategy promotes community-based physical and social activities, particularly in rural and isolated regions, with built environments designed to support prevention.Footnote 4Footnote 5Footnote 6 By developing accessible environments that encourage people to exercise, create art, play music and similar activities, built spaces can be leveraged to foster cognitive resilience.Footnote 55Footnote 56 Such community-driven programs not only support dementia prevention but also highlight the potential of neighbourhood design as a modifiable SDoH with broad implications for physical, social and cognitive health.Footnote 55Footnote 56
We retrieved only two interventional studies that targeted SDoH and examined their impact on cognitive health.Footnote 26Footnote 27 This underscores the need for better integration of impact assessments in evaluations of public health initiatives on cognitive health in Canada. Future interventional studies could also examine the development of dementia-inclusive initiatives that address inequalities and inequities in SDoH, such as the age-friendly cities and communities proposed by the World Health Organization.Footnote 57
Methodological considerations: self-reported versus ecological data
Most of the SDoH were assessed using self-reported measurements. Obtained through questionnaires or surveys, these are cost-effective and easy ways to assess a wide variety of SDoH from participants’ points of view.Footnote 58 However, self-reports are subject to recall bias and social desirability bias, not least in the context of memory loss and cognitive decline.Footnote 58 In addition, some microsystemic SDoH, such as social support and education, may be more likely to be studied because they are easily assessed through self-reports.
Exosystemic SDoH, such as environmental and occupational exposures, were not as commonly evaluated. These SDoH were more often measured using ecological data such as dissemination areas or postal codes. Several barriers impede the use of ecological data, namely, data access, data linkage and regulatory processes.Footnote 59 Future studies should further explore the potential of using ecological data to examine associations between possible risk factors and cognitive health outcomes.
Strengths and limitations
This scoping review has many strengths, including the exhaustive search strategy and inclusion of various SDoH associated with the full cognitive health spectrum. The focus on populations in Canada is a strength as the results can inform policy makers and health care professionals by providing directly relevant evidence. We have also highlighted opportunities for future research.
This review also has limitations. The focus on published Canadian literature restricted our ability to explore some SDoH because of a lack of external control groups. For example, we were unable to compare national health care systems, public programs or approaches.
We limited the search to biomedical databases because of the large number of eligible studies retrieved, although a search of the grey literature might have identified other relevant publications or interventions and data on other or under-represented populations. In addition, data extraction was conducted by only one reviewer.
We could not combine the information on study designs using the study as the unit of analysis because the various publications describing the same study may have used different study designs. Finally, the various study designs and analytical approaches did not allow for meta-analyses of the associations. Our results may, however, guide the development of future systematic reviews to explore these associations.
Conclusion
This scoping review identified 159 publications covering 93 studies describing associations between SDoH in 29 categories and cognitive health outcomes on the continuum from healthy cognition to dementia. Along with showing diverse associations, we also highlighted the complexity of evaluating social determinants and the value of using a broad range of data sources and data collection approaches within studies for a better coverage of the SDoH. Our findings show the importance of examining a wide range of SDoH, better integrating the chains of influence between SDoH, and designing both targeted and global interventions that would act efficiently upon cognitive health. Future research should also focus on integrating more measures of positive cognitive function and healthy aging to cover this continuum of cognitive health.
Funding
We thank the Centre for Surveillance and Applied Research and the Centre for Health Promotion from the Health Promotion and Chronic Disease Prevention Branch of the Public Health Agency of Canada for their financial support.
Acknowledgements
We thank the Centre for Surveillance and Applied Research and the Centre for Health Promotion in the Health Promotion and Chronic Disease Prevention Branch of the Public Health Agency of Canada for their valuable expertise and feedback; the Public Health Agency of Canada Library for their help in validating the search strategy; and Dominique Parisien from the Public Health Capacity and Knowledge Mobilization Unit, the Regulatory, Operation and Emergency Management Branch of the Public Health Agency of Canada, for her help in the realization of this project and relevant knowledge transfer.
Conflicts of interest
The authors have no conflicts of interest.
Authors’ contributions and statement
- SO: Conceptualization, data curation, formal analysis, investigation, methodology, writing—original draft, writing—review and editing.
- TR: Conceptualization, data curation, formal analysis, investigation, writing—original draft, writing—review and editing.
- MLR: Conceptualization, project administration, supervision, validation, writing—review and editing.
- LL: Conceptualization, project administration, supervision, validation, writing—review and editing.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
 Download in PDF format (257 kB, 14 pages)
Download in PDF format (257 kB, 14 pages)