Opioid-related poisoning and anoxic brain injury in Canada: a descriptive analysis of hospitalization data
Canada is currently experiencing an overdose crisis. While this crisis involves a wide range of substances, opioids continue to play a major role in harms and deaths. The Public Health Agency of Canada (PHAC), in collaboration with the provincial and territorial (PT) offices of Chief Coroners and Chief Medical Examiners, PT public health and health partners, and Emergency Medical Services data providers, releases quarterly reports on apparent opioid toxicity deaths and Emergency Medical Services responses for suspected opioid-related overdoses. PHAC also collaborates with Health Canada to report on hospitalizations for opioid-related poisonings (overdoses) using hospital administrative data from the Canadian Institute for Health Information (CIHI).
When a person experiences an opioid-related poisoning, their normal breathing rate is decreased, resulting in a loss of blood circulation and oxygen supply to the brain.Reference 1 Without enough oxygen, brain cells begin to deteriorate rapidly leading to potential anoxic brain injury. Depending on the individual, their medical history, type of opioid(s) and substances involved, severity of the poisoning, and time to treatment, anoxic brain injury can result in coma or death.Reference 2,Reference 3,Reference 4 Effects of anoxic brain injury vary between individuals and can include organ failure, nerve damage, paralysis, memory loss, mental disorientation, diminished motor skills, reduced physical and cognitive functioning, and behavioural changes.Reference 5 Currently, there are limited data available for opioid-related anoxic brain injuries in Canada.Reference 6,Reference 7,Reference 8
The objective of this analysis is to describe the pattern of co-diagnosed anoxic brain injury among opioid-related poisoning hospitalizations in Canada (excluding Quebec). This report examines the co-diagnosis of anoxic brain injury, that is, a diagnosis received for anoxic brain injury during the same hospital stay for the opioid poisoning. Data are presented for the time period between April 1, 2019 and March 31, 2020, and examine patterns by patient demographics (age and sex), hospitalization characteristics and outcomes (length of stay, intensive care, discharge disposition), and the context of the poisoning (which substances were involved and the location in which the poisoning occurred).
Definitions in this report
Opioid-related poisoning: opioid poisoning harm (overdose) resulting from use of opioids in an intentional, accidental or unknown manner. Opioid poisonings may involve non-pharmaceutical opioids, pharmaceutical opioids, or both. Pharmaceutical opioids refer to opioids that were manufactured by a pharmaceutical company and approved for medical purposes in humans. Pharmaceutical opioids can be obtained by a personal prescription or by other means.
Anoxic brain injury: a type of non-traumatic brain injury (or damage) caused by a lack of oxygen supply to the brain. The severity of injury depends on the amount of time the brain goes without sufficient oxygen supply and can vary between people. In practice, the term is sometimes used interchangeably with hypoxic brain injury.
Key findings
Opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury
Between April 2019 and March 2020, for Canada (excluding Quebec), there were a total of 4,433 opioid-related poisoning hospitalizations. Overall, 4.2% (n=187) of opioid-related poisonings during this time period had a co-diagnosis of anoxic brain injury recorded during their hospital stay.
By sex and age
The majority of opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury were among males (67%). However, a more similar proportion of males (53%) and females (47%) was observed among hospitalizations without co-diagnosed anoxic brain injury (Figure 1).

Figure 1 - Text description
| Opioid-related Poisoning Hospitalization | Male, % (N) | Female, % (N) |
|---|---|---|
| With Co-Diagnosed Anoxic Brain Injury | 67% (125) | 33% (62) |
| Without Co-Diagnosed Anoxic Brain Injury | 53% (2253) | 47% (1992) |
Data source Discharge Abstract Database (DAD), fiscal year 2019/2020, Canadian Institute for Health Information (CIHI). |
||
Note ‘Other sex’ is excluded due to low numbers. Refer to the limitations section for more information regarding sex and gender data in the DAD. |
||
Overall, opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury consisted of a younger population compared to those without anoxic brain injury (Figure 2). For both males and females with co-diagnosed anoxic brain injury, the median age was 36 years. In comparison, opioid-related poisoning hospitalizations without co-diagnosed anoxic brain injury were among older individuals, with a median age of 50 years for females and 42 years for males.

Figure 2 - Text description
| Opioid-related Poisoning Hospitalization | Median age in years among males | Median age in years among females |
|---|---|---|
| With Co-Diagnosed Anoxic Brain Injury | 36 | 36 |
| Without Co-Diagnosed Anoxic Brain Injury | 42 | 50 |
Data source Discharge Abstract Database (DAD), fiscal year 2019/2020, Canadian Institute for Health Information (CIHI). |
||
Note ‘Other sex’ is excluded due to low numbers. Refer to the limitations section for more information regarding sex and gender data in the DAD. |
||
By hospitalization characteristics and outcomes
Length of stay
The total length of stay in hospital, including the number of days the patient was in acute care and alternative level of care, if applicable, was longer for opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury. Patients who experienced opioid-related poisonings with co-diagnosed anoxic brain injury stayed in hospital for an average of 20.1 days (median = 5 days), compared to an average of 7.3 days (median = 3 days) for those without co-diagnosed anoxic brain injury.Footnote a
Intensive care
The intensive care unit (ICU) is an organized system to provide specialized medical care to patients who are critically ill, and allow for enhanced monitoring and life support,Reference 9 which could involve mechanical ventilation to help a person breathe if they are unable to do so on their own. The majority (94%) of opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury were admitted to the ICU, compared to 37% of those without co-diagnosed anoxic brain injury.
Discharge disposition
Discharge disposition, that is, where the patient was discharged to or the status of the patient on discharge, varied between hospitalizations with and without anoxic brain injury (Figure 3). The majority (70%) of opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury indicated the patient died in hospital, compared to only 3% of those without co-diagnosed anoxic brain injury. However, a similar percentage of opioid-related poisoning hospitalizations with (20%) or without (19%) co-diagnosed anoxic brain injury resulted in the patient being transferred, for instance, to specialty hospitals for inpatient rehabilitation, long-term care with 24-hour nursing, mental health or addiction treatment centres, or to assisted living and supportive housing.
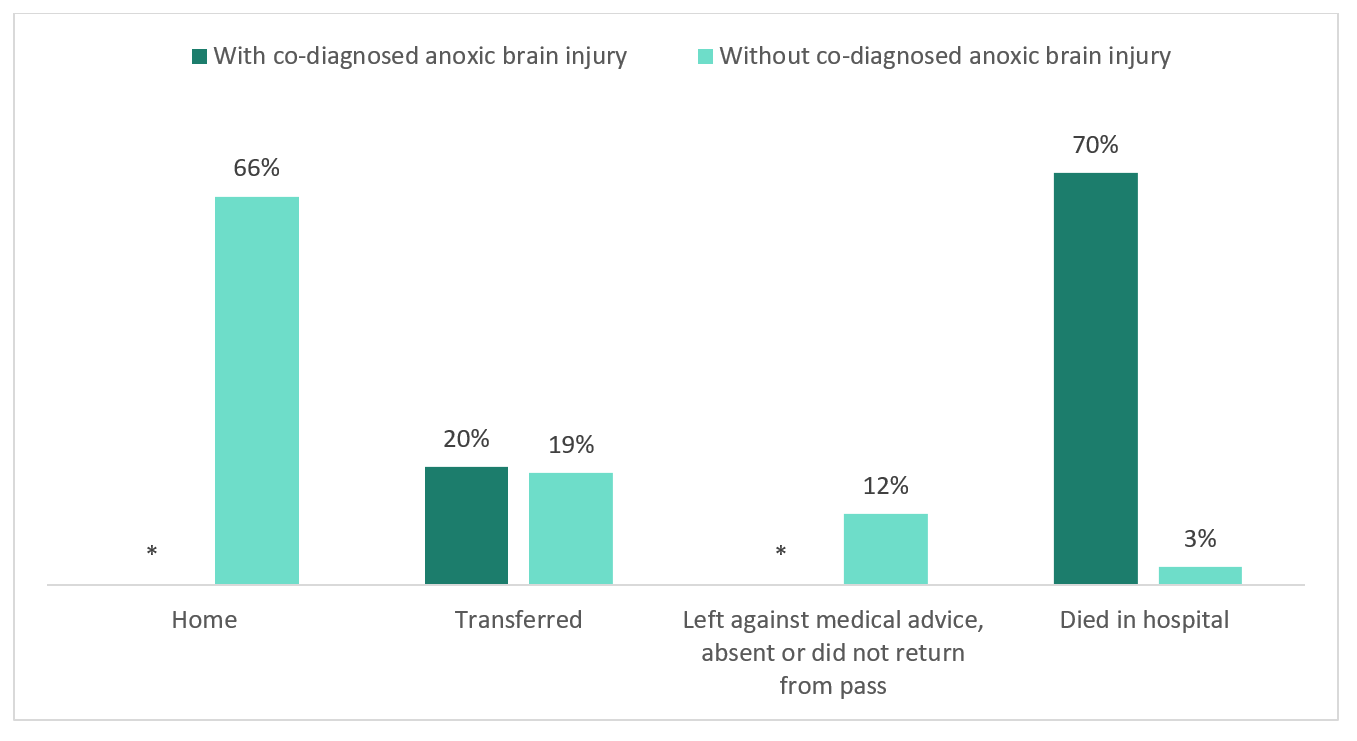
Figure 3 - Text description
| Opioid-related Poisoning Hospitalization | Discharged home, % (N) | Transferred to another facility, % (N) | Left against medical advice, absent or did not return from pass, % (N) | Died in hospital, % (N) |
|---|---|---|---|---|
| With Co-Diagnosed Anoxic Brain Injury | Suppressed | 20% (38) | Suppressed | 70% (130) |
| Without Co-Diagnosed Anoxic Brain Injury | 66% (2794) | 19% (809) | 12% (514) | 3% (129) |
Data source Discharge Abstract Database (DAD), fiscal year 2019/2020, Canadian Institute for Health Information (CIHI). |
||||
Note *Counts less than five have been suppressed as per CIHI privacy guidelines. |
||||
Substances involved and context of poisoning
Type of opioid involved
When examining the type of opioid(s) involved in the poisoning, differences were observed for those with and without anoxic brain injury (Figure 4). For opioid-related poisoning hospitalizations co-diagnosed with anoxic brain injury, fentanyl and its derivatives were the most common type of opioid involved, with half of hospitalizations (50%) indicating its presence. In comparison, fentanyl and its derivatives were less common among opioid-related poisonings without co-diagnosed anoxic brain injury, with only 20% of these hospitalizations indicating its presence. While fentanyl was more commonly observed among opioid-related hospitalizations co-diagnosed to have anoxic brain injury, other opioid types were more prevalent among those without anoxic brain injury. Overall, for opioid-related poisoning hospitalizations without co-diagnosed anoxic brain injury, the following types of opioids were more commonly involved: tramadol, methadone, oxycodone, hydromorphone, morphine, and codeine. Of note, it was not possible to determine which poisonings were a result of pharmaceutical opioids, non-pharmaceutical opioids, or a combination of both. Multiple types of opioids and non-opioid substances may be involved in any given poisoning. Refer to the technical notes and Appendix A for the methodology used to identify types of opioid-related poisoning hospitalizations.
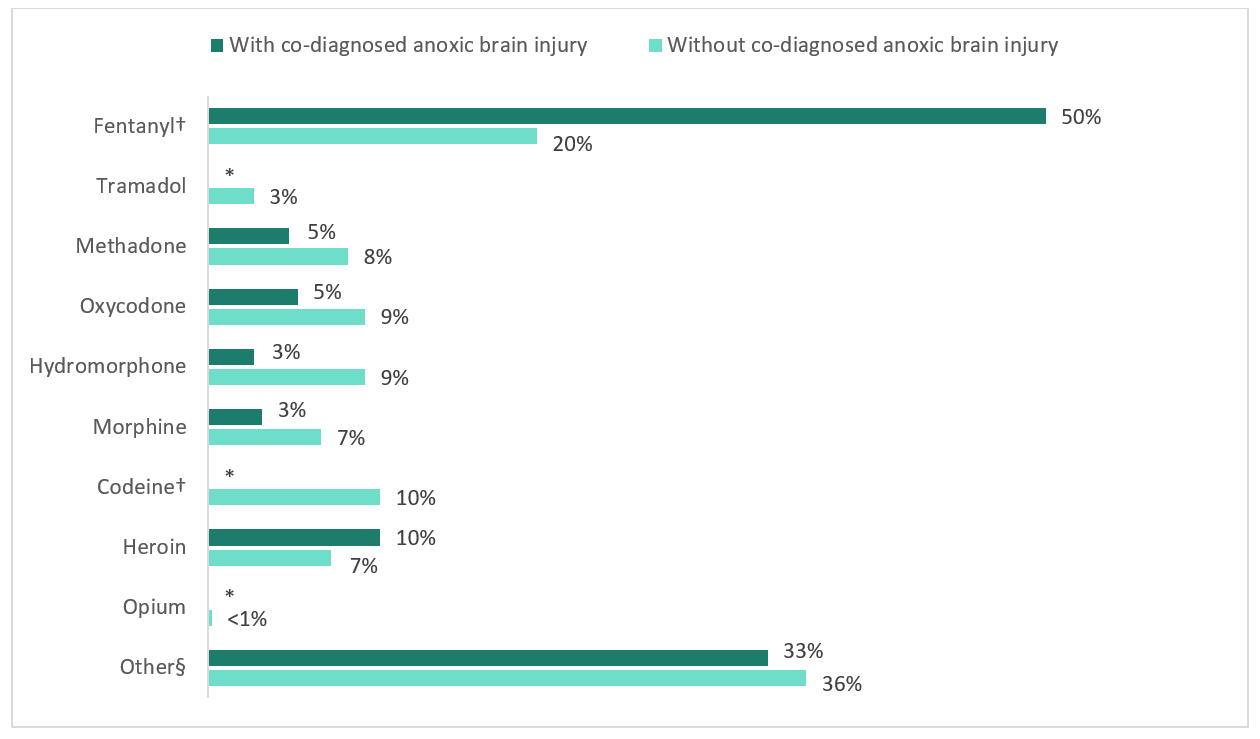
Figure 4 - Text description
| Opioid-related Poisoning Hospitalization |
Fentanyl†, % (N) |
Tramadol, % (N) |
Methadone, % (N) |
Oxycodone, % (N) |
Hydromor -phone, % (N) |
Morphine, % (N) |
Codeine†, % (N) |
Heroin, % (N) |
Opium, % (N) |
Other§, % (N) |
|---|---|---|---|---|---|---|---|---|---|---|
| With Co-Diagnosed Anoxic Brain Injury |
50% (93) | Suppressed | 5% (9) | 5% (10) | 3% (5) | 3% (6) | Suppressed | 10% (19) | Suppressed | 33% (62) |
| Without Co-Diagnosed Anoxic Brain Injury |
20% (829) | 3% (115) | 8% (354) | 9% (396) | 9% (395) | 7% (285) | 10% (431) | 7% (310) | <1% (7) | 36% (1507) |
Data source Discharge Abstract Database (DAD), fiscal year 2019/2020, Canadian Institute for Health Information (CIHI). |
||||||||||
Notes
|
||||||||||
Multiple drug poisoning involving non-opioid substances
Opioid-related poisonings that involved another non-opioid substance(s) were more common among those with anoxic brain injury. Overall, 45% of opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury involved a co-occurring poisoning from a non-opioid substance(s), compared to only one-third (33%) of opioid-related poisonings without co-diagnosed anoxic brain injury.
With respect to specific types of non-opioid substances involved, differing patterns were observed for those with and without co-diagnosed anoxic brain injury (Figure 5). Overall, co-occurring poisonings with stimulants (e.g., cocaine, methamphetamine), were more common among opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury compared to those without, 36% and 18% respectively. Cannabis was also more common among opioid-related poisonings with co-diagnosed anoxic brain injury compared to those without (7% vs. 3%, respectively). Co-poisoning with alcohol was similar for those with and without anoxic brain injury, however opioid-related poisoning hospitalizations without co-diagnosed anoxic brain injury consisted of a higher percentage of co-poisonings with other depressants (e.g. sedatives and benzodiazepines). Refer to the technical notes and Appendix B for the methodology used to identify co-occurring poisonings from non-opioid substances. Of note, it may be possible that multiple substances could have contributed to anoxic brain injury.
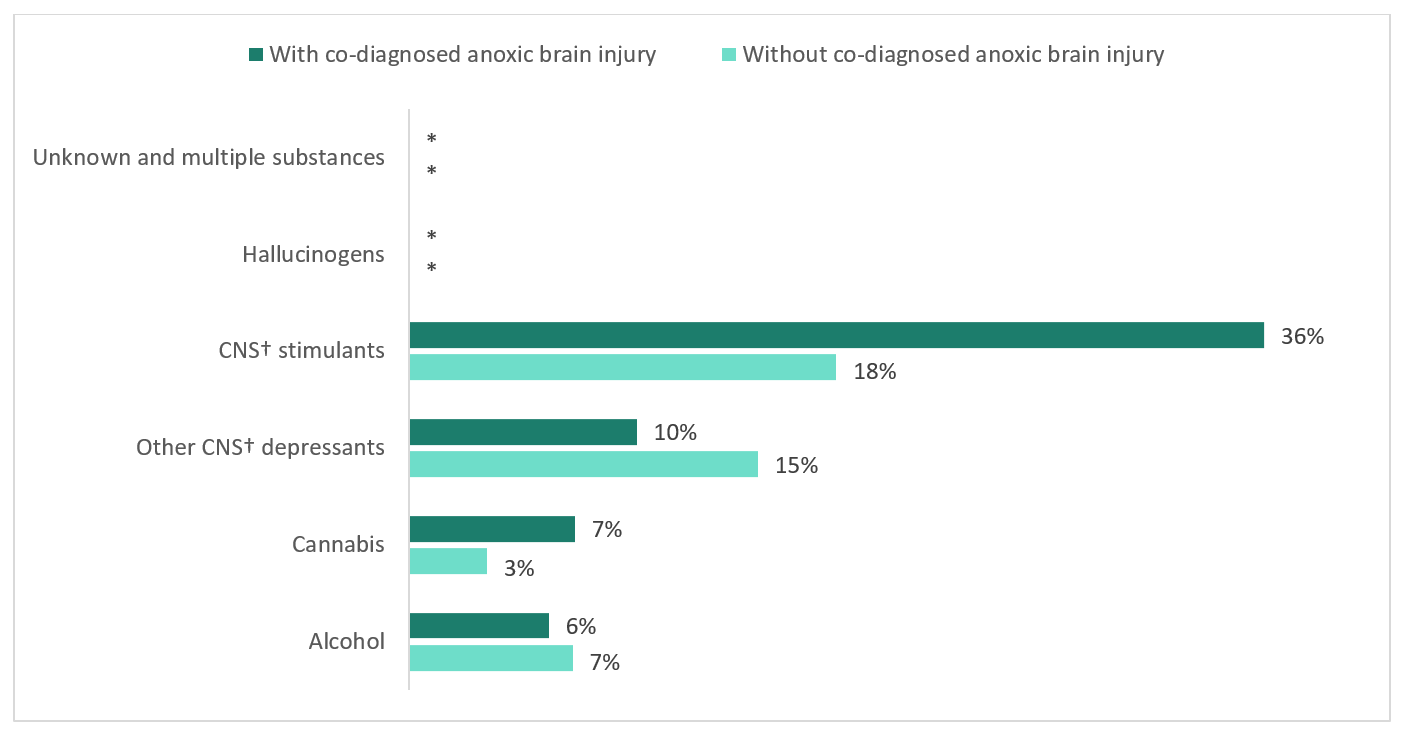
Figure 5 - Text description
| Opioid-related Poisoning Hospitalization | Involved unknown and multiple substances, % (N) | Involved hallucinogens, % (N) | Involved CNS† stimulants, % (N) | Involved other CNS† depressants, % (N) | Involved cannabis, % (N) | Involved alcohol, % (N) |
|---|---|---|---|---|---|---|
| With Co-Diagnosed Anoxic Brain Injury | Suppressed | Suppressed | 36% (78) | 10% (18) | 7% (13) | 6% (11) |
| Without Co-Diagnosed Anoxic Brain Injury | Suppressed | Suppressed | 18% (867) | 15% (626) | 3% (138) | 7% (294) |
Data source Discharge Abstract Database (DAD), fiscal year 2019/2020, Canadian Institute for Health Information (CIHI). |
||||||
Notes
|
||||||
Place of occurrence
Roughly the same proportion of opioid-related poisoning hospitalizations with and without co-diagnosed anoxic brain injury indicated the patient experienced the poisoning at a home or residential institution, 52% and 54% respectively. The remaining experienced the poisoning in another location, such as a public area, street, or service area.
In summary
Canada continues to experience a national overdose crisis. Furthering our understanding of opioid-related harms, including the long-term impact of opioid-related poisonings, can help inform comprehensive clinical and public health actions to address the crisis.
When a person experiences an opioid-related poisoning, their brain may not receive enough oxygenReference 1 which can lead to an anoxic brain injury. Reference 2,Reference 3,Reference 4 Early intervention, including the administration of naloxone, is essential to reverse the symptoms of an opioid-related poisoning and reduce the risk of an anoxic brain injury.Reference 10 Anoxic brain injury is often an under-recognized consequence of opioid-related poisonings, and for those who survive, the lasting effects can include significant changes to physical, cognitive, and behavioural functioning which may warrant additional supports.Reference 8
This report revealed that roughly 4% of hospitalizations for opioid-related poisonings are co-diagnosed to have anoxic brain injury. Among opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury, there was a higher proportion of males, younger individuals, and involvement of fentanyl or its derivatives, compared to opioid-related poisoning hospitalizations without co-diagnosed anoxic brain injury. Hospitalizations for opioid-related poisonings that indicated the person experienced a multiple drug poisoning with another non-opioid substance(s), notably involving stimulants (e.g., cocaine, methamphetamine), were also more common among those co-diagnosed with anoxic brain injury. These findings highlight the importance for healthcare professionals, researchers and policy makers, to consider how the long-term impact of opioid-related harms may vary between different populations and with respect to the type and context of substance use.
Further research is needed to better understand the long-term impacts of opioid-related harms, such as those related to physical and cognitive impairments, chronic conditions, mental health, as well as broader impacts on individuals, families, and communities. The Government of Canada will continue to improve data and analysis to inform strategies and interventions to reduce opioid-related harms across the country.
Acknowledgements
We would like to acknowledge the Canadian Institute for Health Information (CIHI) for collecting and providing the data used for reporting opioid-related hospitalizations.
Disclaimer
Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the authors, and not necessarily those of the Canadian Institute for Health Information (CIHI).
Suggested Citation
Opioid-related poisoning and anoxic brain injury in Canada: a descriptive analysis of hospitalization data. Ottawa: Public Health Agency of Canada; March 2021
Technical notes
Methodology
Data from CIHI's Discharge Abstract Database (DAD) for the fiscal year April 1, 2019 to March 31, 2020 were analyzed for this report. This analysis was limited to acute inpatient hospitalizations, which are nationally representative across Canada, with the exception of Quebec. This analysis presents the number of acute inpatient hospitalizations for opioid-related poisonings, it does not reflect the number of patients who were hospitalized in the analysis year. It is possible some patients may have been hospitalized more than once for an opioid-related poisoning.
The International Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA) is used in the DAD to capture diagnoses from the patient's hospitalization. It is the national standard for reporting morbidity statistics. More information on the DAD and ICD-10-CA coding can be found on CIHI's website.
A complete listing of all ICD-10-CA diagnosis codes used to identify opioid-related poisonings and co-occurring poisonings from non-opioid substances presented in this report can be found in Appendix A and Appendix B, respectively. Information on opioid poisonings are extracted from patient charts by trained coders, which may be based on patient self-report and/or toxicological analysis. The methodology for this report was adapted from CIHI’s Opioid-related Harms in Canada report and Hospital Stays for Harm Caused by Substance Use indicator in their Your Health System data tool.
Opioid-related poisoning records with and without a corresponding ICD-10-CA code of G93.1 “anoxic brain damage, not else where classified”, were identified to create two groups for analyses:
- opioid-related poisoning hospitalizations with co-diagnosed anoxic brain injury and;
- opioid-related poisoning hospitalizations without co-diagnosed anoxic brain injury.
Analyses were restricted to the following significant diagnosis types for both groups:
- Most responsible diagnosis ("M")
- Pre-admit comorbidity ("1")
- Post-admit comorbidity ("2")
- Service transfer diagnosis ("W", "X", and "Y")
These significant diagnosis types capture hospitalizations in which the poisoning and anoxic brain injury was considered influential to the time spent in hospital and treatment received by the patient while there. Secondary diagnoses that do not meet the criteria for significance were excluded.
For poisonings, a diagnosis prefix of "Q", indicating unconfirmed diagnoses or query diagnoses recorded by the physician, were excluded from these analyses. For all analyses, records indicating the patient was admitted to the facility as a cadaveric donor and or a stillbirth were excluded.
Limitations
General notes
- It is possible some diagnoses for anoxic brain injury were not captured, such as milder cases, or some people may have received a delayed diagnosis. As this analysis examined co-diagnoses for anoxic brain injury during the same hospitalization for opioid-related poisoning, the data presented may reflect underreporting.
- Anoxic brain injury was the focus for this analysis, however it is important to note that there are other forms of brain injury which may be associated with opioid use, such as toxic leukoencephalopathy, whereby injury occurs to the brain’s white matter from exposure to a variety of agents.Reference 11 Although rarer, acute toxic leukoencephalopathy can sometimes mimic anoxic brain injury following opioid-related poisoning and it should be considered in patients who present without an identifiable period where they lacked oxygen.Reference 12 Of note, there were 17 patients in the study population with a co-diagnosis of toxic encephalopathy identified by ICD-10-CA code “G92”.
- This analysis was not longitudinal in nature, and it did not assess baseline brain status or potential pre-existing issues. The cumulative impact of opioid-related harms and anoxic brain injury is not known.
- It was not possible to determine which poisonings were a result of pharmaceutical opioids, non-pharmaceutical opioids, or a combination of both. It was also not possible to determine whether co-poisonings were a result of intended polysubstance use or if substances unknowingly contained other substances.
- The DAD captures patients discharged from hospital. Patients who were still hospitalized during the analysis year are not captured in this report.
- Data released by provinces and territories may differ from the data provided in this report due to the availability of updated data, differences in the type of data reported, the use of alternate age groupings, differences in time periods presented and/or population estimates used for calculations, etc.
Data on sex
- At the time of this analysis, no data was available in relation to gender identity. In the DAD, data on sex is typically recorded based on biological determination or legal documentation. Although an 'other' sex group was available, the counts were too low to include in this report. Therefore, the 'other' sex group was retained in the overall analyses, but excluded from all analyses by sex to avoid disclosure.
Data suppression
Values representing less than five hospitalizations are suppressed according to CIHI's privacy guidelines.
Appendix A
| Opioid-related poisonings | ICD-10-CA Code description |
|---|---|
| T40.0 | Poisoning by opium |
| T40.1 | Poisoning by heroin |
| T40.2 | Poisoning by other opioids |
| T40.20 | Poisoning by codeine and derivatives |
| T40.21 | Poisoning by morphine |
| T40.22 | Poisoning by hydromorphone |
| T40.23 | Poisoning by oxycodone |
| T40.28 | Poisoning by other opioids not elsewhere classifiedTable Footnote * |
| T40.3 | Poisoning by methadone |
| T40.4 | Poisoning by other synthetic narcotics |
| T40.40 | Poisoning by fentanyl and derivatives |
| T40.41 | Poisoning by tramadol |
| T40.48 | Poisoning by other synthetic narcotics not elsewhere classifiedsTable Footnote * |
| T40.6 | Poisoning by other and unspecified narcoticsTable Footnote * |
|
|
Appendix B
| Poisoning from non-opioid substance | ICD-10-CA Code Descriptions |
|---|---|
| Alcohol |
|
| Cannabis |
|
| Other central nervous system (CNS) depressants |
|
| Central nervous system (CNS) stimulants |
|
| Hallucinogens |
|
| Unknown and multiple substances |
|
References
- Reference 1
-
Solis Jr E, Cameron-Burr KT, Kiyatkin EA. Heroin contaminated with fentanyl dramatically enhances brain hypoxia and induces brain hypothermia. eneuro. 2017 Sep;4(5). doi: 10.1523/ENEURO.0323-17.2017
- Reference 2
-
Dolinak D. Opioid toxicity. Academic forensic pathology. 2017 Mar;7(1):19-35. doi: 10.23907/2017.003
- Reference 3
-
Kiyatkin EA. Respiratory depression and brain hypoxia induced by opioid drugs: morphine, oxycodone, heroin, and fentanyl. Neuropharmacology. 2019 Jun 1;151:219-26. doi: 10.1016/j.neuropharm.2019.02.008
- Reference 4
-
Davis MP, Behm B. Reasons to avoid fentanyl. Annals of Palliative Medicine. 2020 Mar 3;9(2):611-24. doi: 10.21037/apm.2020.01.12
- Reference 5
-
Zibbell J, Howard J, Clarke S, et al. Non-Fatal Opioid Overdose and Associated Health Outcomes: Final Summary Report. Office of the Assistant Secretary for Planning and Evaluation. 2019. Available from: https://aspe.hhs.gov/basic-report/non-fatal-opioid-overdose-and-associated-health-outcomes-final-summary-report
- Reference 6
-
Pfister GJ, Burkes RM, Guinn B, et al. Opioid overdose leading to intensive care unit admission: epidemiology and outcomes. Journal of critical care. 2016 Oct 1;35:29-32. doi: 10.1016/j.jcrc.2016.04.022
- Reference 7
-
Morrow RL, Bassett K, Maclure M, et al. Outcomes associated with hospital admissions for accidental opioid overdose in British Columbia: a retrospective cohort study. BMJ open. 2019 May 1;9(5):e025567. doi: 10.1136/bmjopen-2018-025567
- Reference 8
-
O'Brien P, Todd J. Hypoxic brain injury following heroin overdose. Brain Impairment. 2009 Sep;10(2):169. doi:10.1375/brim.10.2.169
- Reference 9
-
Marshall JC, Bosco L, Adhikari NK, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. Journal of critical care. 2017 Feb 1;37:270-6. doi: 10.1016/j.jcrc.2016.07.015
- Reference 10
-
Government of Canada. Naloxone [Internet]. 2019 [cited February 23, 2021]. Available from: https://www.canada.ca/en/health-canada/services/substance-use/problematic-prescription-drug-use/opioids/naloxone.html
- Reference 11
-
Filley CM, Kleinschmidt-DeMasters BK. Toxic Leukoencephalopathy. The New England Journal of Medicine. 2001 Aug 9;345:425-432. doi: 10.1056/NEJM200108093450606
- Reference 12
-
Achamallah N, Wright RS, Fried J. Chasing the wrong dragon: A new presentation of heroin-induced toxic leukoencephalopathy mimicking anoxic brain injury. J Intensive Care Soc. 2018 May 10; 20(1):80-85. doi: 10.1177/1751143718774714
Footnotes
- Footnote a
-
Average and median express the central or typical value in a set of data. The average measure is equal to the sum of all the values in the dataset divided by the number of values in the set. The median measure is determined by ranking the data set from smallest to largest, and then identifying the middle value of the entire dataset