Expert Advisory Group Report 2: Building Canada’s Health Data Foundation
Download in PDF format
(2.63 MB, 33 pages)
Organization: Public Health Agency of Canada
Date published: 2021-11-XX
Preface
Canadian governments have invested heavily to advance the use of health data, most often without a clear national vision. Where there has been a vision, the will to see it implemented has not been present. Consequently, benefits from these investments are fragmented and unevenly distributed. In the first report of the Expert Advisory Group (EAG) for the Pan-Canadian Health Data Strategy, we described the systemic barriers that have obstructed success from these investments - including misaligned incentives, poor understanding of health data, and failure to engage the public meaningfully.
COVID-19, while devastating, has conclusively demonstrated the value of standardized national health data, providing a rare, cross-cutting opportunity to leverage the strengths of Canada's federation - its diversity, and leading intellectual capital - to re-assert Canada's position as a world leader in health data collection, exchange, and use. Together, individuals, decision-makers, health workforce leaders, researchers and innovators can deliver better health outcomes for all. This will result in the sustainable health sector that all persons living in Canada need and expect.
A recent Commonwealth Fund report showed that Canada's health service now ranks 10th out of 11 high-income countries in health care performance compared to spending. Another report showed that Canada has been slow to share genomic data to help insights for COVID-19 variants - ranking 48th of 54 countries that have sequenced at least 1000 genomes and last among G20 countries. Many countries ahead of Canada in these rankings recognize that investments in data are a crucial component of health sector transformation and are focusing heavily on data to revitalize their health sectors. Failure to act now risks Canada falling further behind, compromising the quality of services that promote individual and population health, and perpetuating the burden of growing costs.
Canada can deliver better health outcomes and retake its place as a world leader through firm action. This second of three planned reports provides recommendations for a health data strategy, supported by case studies, and an outline for needed actions in the first two years. It promotes a person-centric future state for Canada's health sector driven by data. We provide concrete examples of system benefit if this opportunity is seized and implemented.
By working together, we can align public voice, governance, policy, and standards towards decisive action to achieve better outcomes for individuals, communities, and all of Canada.
Dr. Vivek Goel
Chair, Expert Advisory Group, Pan-Canadian Health Data Strategy
"When facing the greatest public health emergency that this country has tackled for generations, one of the most impactful tools at our disposal was the power of data. With the facts, data, and science at our disposal, we can provide the meaningful and measurable results that the public deserves."
Ministerial Forward from UK Health Data Strategy,
"Data Saves Lives: reshaping health and social care with data", July 2021
Table of contents
- Preface
- Glossary
- Addressing barriers from the Expert Advisory Group's first report
- References
- Members of the Expert Advisory Group
- Contact
"Health lags far behind other sectors in harnessing the potential of data and digital technology, missing the opportunity to save a significant number of lives and billions of dollars."
Health in the 21st Century: Putting Data to Work for Stronger Health Systems, 2019 OECD Report
1. Unleashing health data: The urgent case for action
The challenge
Governments and organizations in Canada must take a consistent approach to collecting, sharing and using health data assets to support health care delivery, public health decision making, economic development and research. The lack of a common, coherent approach for health data across Canada is contributing to lagging health outcomes for people in Canada, escalating sector costs, expanding health inequities and slowing innovation in Canada's health sector. At present, there is:
- no systematic, nor systemic principle-based approach to data use in the health sector;
- no clear accountability in the health sector for its fastest growing asset - data;
- no systemic way to understand public and community health data requirements;
- no strong and coherent governance model for data oversight in the health sector;
- no policy that articulates the duty to share data for the public good while also ensuring it is secure; and
- no common health data terminology to enable effective health data literacy initiatives for health leaders, health workforce and the public.
Currently, the health sector's data governance and management status quo - where data flow is impeded by lack of collaboration and enabling policies - is burdened by subtle but pervasive disincentives to sharing. Investments in health data infrastructure are fragmented and piece-meal, prioritizing short-term needs without consideration for long-term outcomes and potential future uses. A fragmented patchwork of mismanaged and misaligned health data resources results in growing inefficiency, duplicative investments across and within jurisdictions, stifled health sector innovation and significant challenges responding to major public health events such as COVID-19.
As governments move forward in the wake of the pandemic, they must capitalize on domestic and international lessons learned and unleash the power of health data to save and improve lives. Accelerating the transformation of the health sector into the digital world will better meet current demands and set a strong foundation to develop and maintain a sustainable health sector that fulfils future health needs.
Maintaining the status-quo is not an option.
The reward
Health data collection, sharing and use must be optimized through investment in a robust, interoperable foundation that drives benefit for all and balances the need to uphold quality, ethics and privacy. Unleashing the potential of health data while implementing new ways to protect it will launch a new era of health improvement:
- Economies of scale will be achieved through common data policy, workflow and technology;
- Health and wellness will be promoted through data driven population health analyses and integrity of personal health information;
- Individuals will be empowered to achieve their health goals through a person-centric approach to health data;
- Communities will be better protected from public health threats and achieve more equitable outcomes; and
- Canadian health research and management will be delivered on a timely basis and with confidence.
Acting now during this time of profound change will help create a culture of health data cooperation that empowers individuals and communities to achieve their health objectives. High quality, timely, integrated health data saves lives, reduces societal inequities and can help drive recovery from COVID-19.
The time to act is now: Governments, stakeholders, and the public
Governments must collaborate and coordinate to create a new health data foundation for Canada. Trust must be earned so that it can enable sharing of data for health safety, innovation and quality improvement. Without this, health technology investments by borderless vendors and multi-national corporations will continue to expand and fill health data gaps for Canadians, risking further fragmentation and undermining the principles of equity underpinning Canada's health sector. Health data are at risk of being monetised by private companies, where profits are often put before people. Swift and concerted action is needed to ensure that availability and use of health data reflect Canadian values and needs rather than the interests of an online, multi-tier, profit-driven space inconsistent with Canadian values and needs.
Collaborative health data collection, sharing and use has been peripheral to day-to-day health and public health activities. Data are collected and stored by unconnected data custodians, including care providers and administrators. Data are not used effectively due to limitations in sharing between parts of the health sector that fragment personal health information, impacting the immediate benefit of individual clinical care and impeding the integration of data resulting in the failure to identify risks to public health and safety, preventing research,and impairing health sector quality monitoring and improvement.
Going forward, health data are at the heart of today's emerging health priorities - protecting public health, implementing digital health solutions, improving long-term care and improving access to pharmaceuticals. To be successful, health sector decision-makers must work smarter, not harder, in delivering health care and public health interventions. Canada's health sector entities need to become learning organizations - leveraging insights generated through data to promote better and more efficient services that provide excellent value for money.
A Pan-Canadian Health Data Strategy should therefore focus on establishing federated data governance, clear standards for interoperability, an effective policy environment and meaningful engagement with the public to facilitate this change. Together, this will earn the trust of Canadians and allow health data to flourish. All new health investments must require robust health data governance and management that aligns with federated standards to support health sector resilience in the face of future needs and challenges.
Health transformation driven by data
Historically, Canada was recognized as a world leader in the analysis of health data (starting with the Manitoba Centre for Health and Policy Evaluation and Statistics Canada) and as the birthplace of deep learning (an advanced form of Artificial Intelligence). Today, these advances should be synergistically accelerating insight in the health sector. However, systemic barriers are stifling innovation, fragmenting data, impeding health data exchange and impairing health outcomes.
During the early days of COVID-19, Finland, Israel, and South Korea acted promptly, leveraging solutions where citizens access, use and share health records. These solutions improve integrated care, achieve better social outcomes and were powerful assets in the fight against COVID-19.
Health transformations driven by data are underway in the UK, New Zealand, Australia and the US. These countries have recognized the importance of integrated health data and have taken action to harness it effectively. All these countries have adopted a person-centred approach. This means affixing the flow of personal health data to individuals irrespective of location or service. This approach will promote both individual health outcomes, and achieve benefits for communities and the public through population-based analysis.
2. Shared vision and principles for Canada's Health data foundation
Vision for health data in Canada's health sector
In our first report, we explained that a common vision for health data is necessary to act in a coordinated way and achieve common goals. We proposed a vision for health data where, by 2030, all persons in Canada benefit from a strong health data foundation, which would be present within and across jurisdictions in all health settings to foster quality individual careFootnote 1 and public health interventions. Under this vision, the health system would continuously learn from the insights generated by a health data environment that facilitates timely access and interoperability. A broader view of health data would be adopted, whereby it would refer to all data related to health care, public health, population health and health research, inclusive of sociodemographic factors. People in Canada would have meaningful access to their own individual health records, with the recognition that they must be shared to generate comprehensive data for population and public health uses for the benefit of all while also ensuring data are confidential and secure. Public sector governments, health delivery organizations, the private sector and other critical stakeholders would work together to deliver this vision.
Principles to guide the development and implementation of the Health Data Foundation
To effectively implement the health data foundation and achieve the vision, we also proposed a set of common principles that should guide its development. Several key themes were present in the principles. Chief among these was the idea of person-centricity – putting people at the centre of health data governance, policy and architecture and empowering them to be active participants. Similarly, equity was a key theme in these principles. The development of the health data foundation must ensure it promotes better outcomes in a diverse and inclusive way, with particular attention to the needs of racialized minorities and marginalized populations. The health data foundation must also respect First Nations, Inuit, and Métis data sovereignty and address the structural health inequities experienced by Indigenous peoples across Canada. To promote the effective sharing and use of health data, the health data foundation must focus on fostering stewardship that recognizes the moral imperative to share data for the public good while ensuring effective privacy measures are in place. A culture of stewardship would increase data accessibility, by ensuring that Canadians can access their own health information, and that care providers, health managers and decision-makers have access to the information they need for their work. The health data foundation must also be sustainable, by embedding continuous improvement in its pillars. Finally, the transformations needed by our approach to health data require collaboration and coordinated processes between all health sector stakeholders. These processes should build on leading international, domestic and regional data principles, best practices and standards.
In summary, the health data foundation must build towards the shared vision, guided by these principles, to be successful in leveraging data to deliver better health outcomes for individuals, communities and society.
3. Health sector driven by person-centred data by design
Public expectations of the health sector are evolving with advances in data and technology. To unlock the value of data for individuals to achieve their personal health objectives, communities to improve equity, health service managers to ensure high quality and cost-effective care, governments to anticipate public health events and researchers to innovate, the health sector needs to change its approach to data and technology to centre on the individual, rather than on providers.

Figure 3a. 1989: Text description
This image is a visual representation of a health records system from the past.
The title of the image is Past State – 1989 Analog
On the left side of the image is a picture of a patient with a black dotted line beside it representing that the patient lacks access to and control over their personal health information.
On the right side of this image are three bubbles forming a circle. Each of the bubbles contain text. The lower left bubble has text that states "Health Information Exchange" with a picture of a maze. The top bubble states "Personal Health Information" with a picture of a file folder and the lower right bubble states "Population Health Data" with a picture of a filing cabinet. There is a dotted line connecting these bubbles indicating they work together. The bubbles are located far apart, representing the challenges that exist in exchanging information between them. In the centre of the circle is a picture of a person with paper indicating the designated custodian of the information is at the centre of this system. An image of a health care provider is to the left of the "Personal Health Information" bubble indicating that this individual controls the patient's personal health information.
Thirty years ago (Figure 3a), health sector functions were largely analog with the majority of an individual's personal health information being captured and stored by designated custodians in paper charts. This led to the fragmentation of personal health information between different custodians. The ability to exchange or consolidate data for broader health sector insights was slow, manual, inflexible and too often impossible. Service-based health information silos existed at the exclusion of the patient, who often had to repeat their health information as they moved from one custodian to another. Resulting limitations in the ability to exchange and integrate health information potentially compromised both the individual care and population-based functions of the health sector.
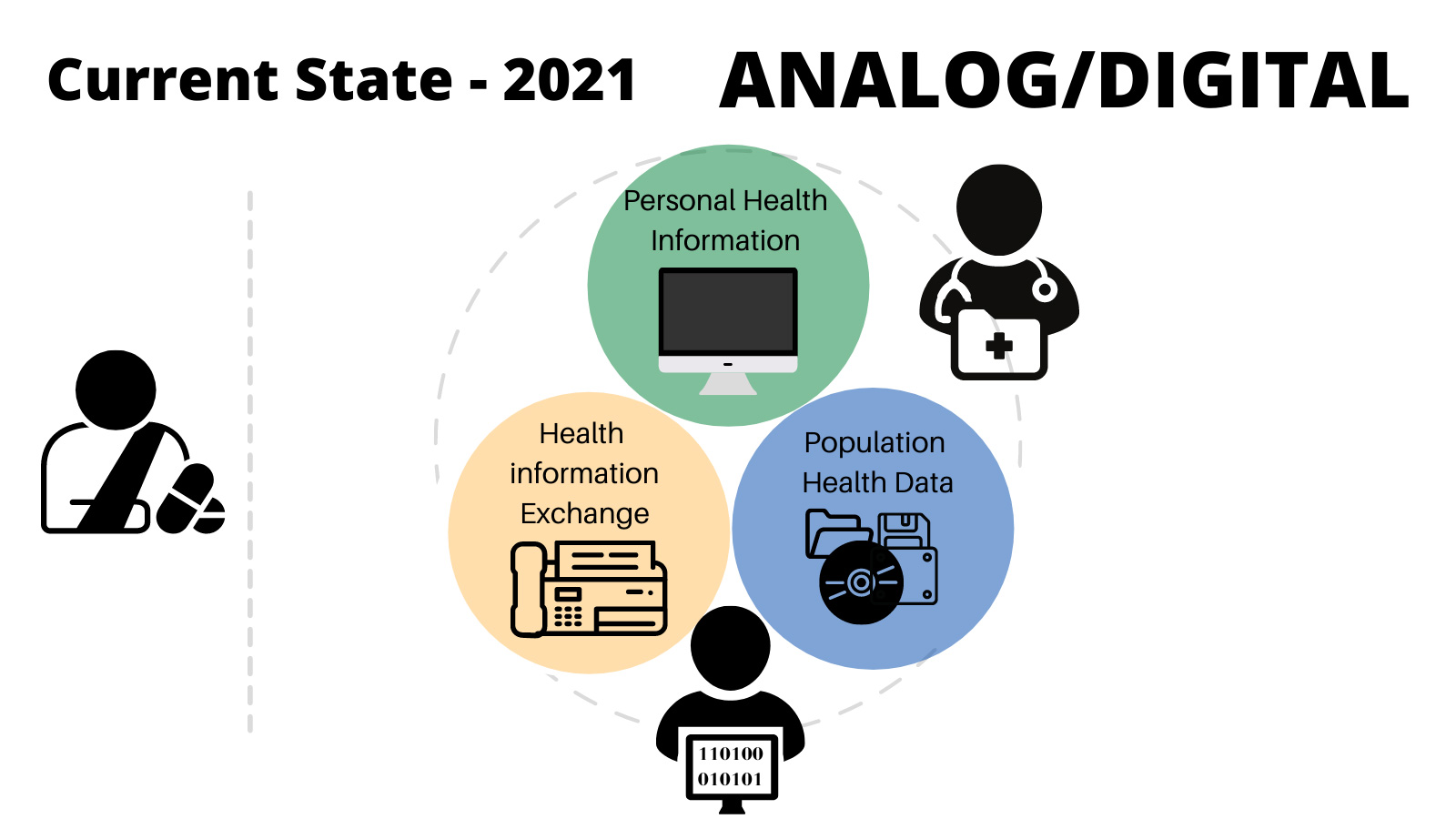
Figure 3b. 2021: Text description
This image is a visual representation of the current health records system.
The title of the image is Current State – 2021 Analog/Digital
On the left side of the image is a picture of a patient with a grey dotted line beside it representing the limited access to and control over their personal health information that the patient has. On the right side of this image are three bubbles forming a circle. Each of the bubbles contain text. The lower left bubble has text that states "Health Information Exchange" with a picture of a fax machine. The top bubble states "Personal Health Information" with a picture of a file computer screen and the lower right bubble states "Population Health Data" with a picture of a diskette and CD-ROM. There is a dotted line surrounding these bubbles indicating they work together. The bubbles are placed closer together compared to Figure 2a which was titled Past State, 1989 Analog, to show that it is now easier to exchange information between groups. In the centre of the circle is a picture of a person on a computer indicating that the designated custodian of the information is at the centre of this system. An image of a health care provider is to the right of the "Personal Health Information" bubble indicating that this individual controls the health information in the system.
Although the health sector has adopted digital technology over the past 30 years (Figure 3b), the policy approach has mostly remained fixed in the custodial paradigm, often perpetuating service-based health information silos that impede the integration of data across clinical service, public health, management and research. Legislation continues to designate care providers as custodians, meaning that patient control of personal health information remains limited. Individuals in some locations do have some access to their health records, but largely in a way that is fragmented between health service providers. Decisions about sharing data are made by custodians on an ad hoc basis, often in a way that is inconsistent and service-centric. Fragmented custodial-based digital platforms that lack data integration necessitate the need for health data to continue to be shared using antiquated and insecure methods like email, fax machine or physical mail. The fragmentation of health information that arises from analogue custodial health information policy compromises both the capacity to provide comprehensive clinical care and to integrate health information for population-based health management and research.
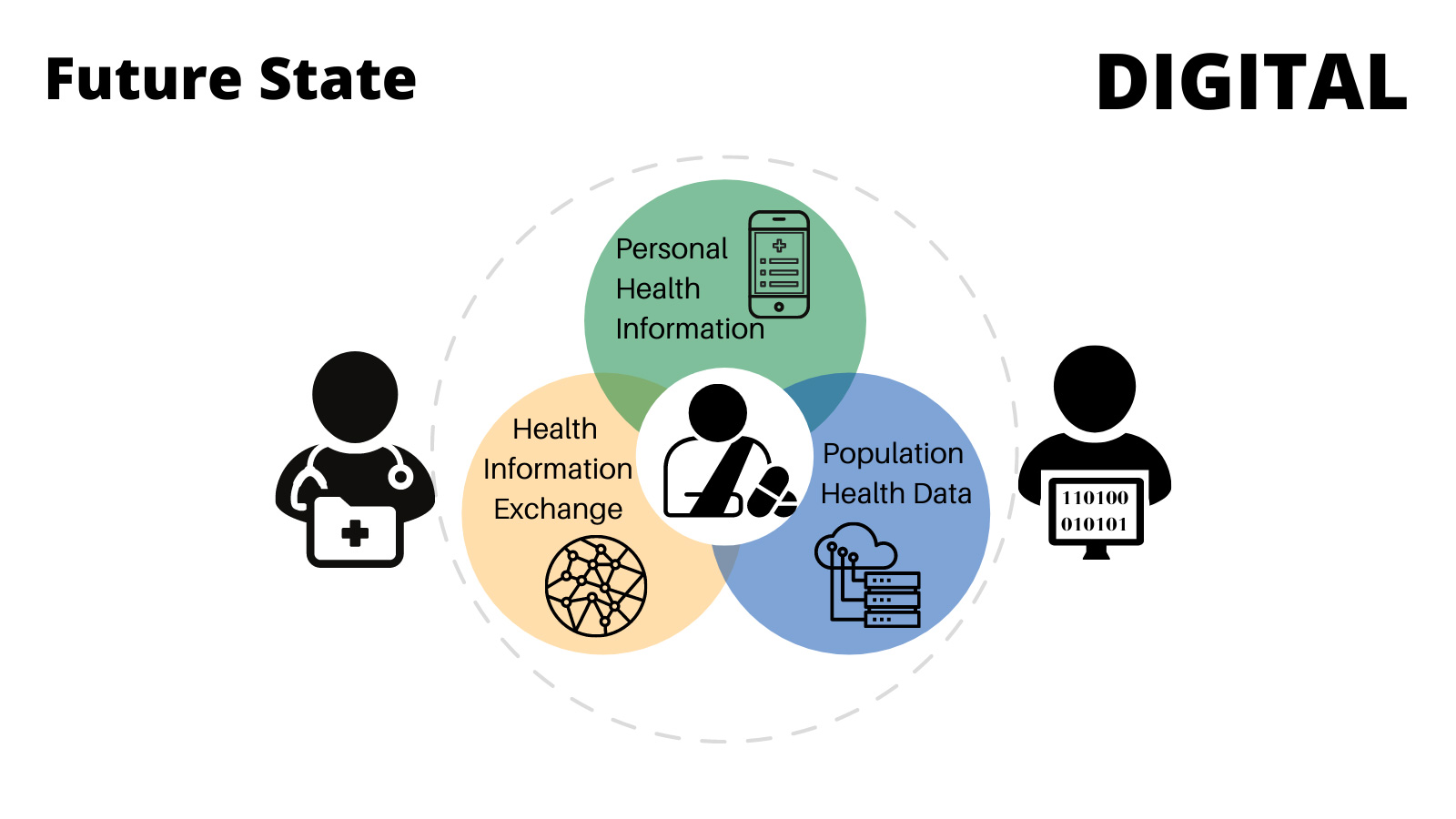
Figure 3c. Future: Text description
This image is a visual representation of the optimized future state of a health records system.
The title of the image is Future State – Digital
In the centre of the image there are three bubbles forming a circle. Each of the bubbles contain text. The lower left bubble has text that states "Health Information Exchange" with a picture of an electronic network. The top bubble states "Personal Health Information" with a picture of a cell phone and the lower right bubble states "Population Health Data" with a picture of a cloud based network. There is a dotted line surrounding these bubbles indicating they work together. The bubbles overlap to show that information exchange between them is seamless. An image of a health care provider is to the left of the three bubbles and an image of a person on a computer is to the right, representing the data steward. These individuals are involved in the collection and exchange of the information but do not have absolute control over it. In the centre of the circle is a picture of the patient, indicating they have access to and control over their information and that their wellbeing and health outcomes are the central concern of this future system design.
A future-oriented approach to health data (Figure 3c) optimizes the promise of health data by establishing digital-age approaches to health data that support:
- The capacity to ensure that all personal health information is collected in a single patient-chart for use by health care providers on a need-to-know basis;
- The seamless exchange of health information between trusted health data stewards; and,
- The capacity to use and to provide duly authorized access to health information by health data stewards, with appropriate levels of access and de-identification, for public good.
This is achieved through person-centric design, whereby all personal health information follows the beneficiary of care throughout their health journey. A person-centric approach to health data obligates health data policy, governance, technology and workflow alignment. Thereby the sector is designed to ensure the right people have the right data at the right time for the right decisions. This networked health approach values adaptability and quality of data to improve health outcomes for all.
An integrated Health Data Foundation: Serving Canada
Person-centred care is a way of thinking and doing things that sees the people using health and social services as equal partners in planning, developing and monitoring care to make sure it meets their needs. This means putting people and their families at the centre of decisions, ensuring a holistic view of them as persons and not body parts or specific diseases, and working alongside professionals to get the best outcome.
An integrated, person-centric health data structure ensures that all health data follows an individual through the course of their life-long care. This obligates health data integration wherever the individual may go; across health services, professional groups and jurisdictions. This is achieved not only through technological integration, but through foundational alignment of data governance, policies, standards, regulation and workflow that allow the seamless movement of health data to support person-centred care and public and population health interventions. When common, forward-looking principles and policies for health data are implemented:
- Individuals have meaningful and timely access to their own health records, improved understanding into why and how their health data are used and have access to evidence-based insights to achieve their personal health objectives;
- Communities have access to insights about their collective health and are able to drive change to achieve greater equity;
- First Nations, Inuit, and Métis Nation data sovereignty is respected, with access to data and the ability to generate impactful insights that support self-determination;
- Health care providers have access on a need-to-know basis to secure data to provide the best possible quality care and proactively allocate resources where needed;
- Public health officials have timely access to the data they require to anticipate, understand and protect against public health threats and drive initiatives to promote public health and wellness;
- Governments and health authorities have timely access to data needed to improve health outcomes, protect against public health threats, manage public health issues, monitor performance and support an innovative health sector that continually learns from its experiences and thereby improves;
- Researchers drive health sector improvement and innovation through access to data to provide timely insights, analysis and solutions to health issues that bring benefits to society, communities and individuals; and
- Private sector technology vendors create new and needed data, technology and care solutions that conform to integrated person-centric health data policy, based on common standards for the benefit of all.
Case study – Advancing person-centric approaches: "One Person, One Record"
Many countries are advancing approaches for "One Person, One Record". The National Health Service in England released "Data saves lives: reshaping health and social care with data"
in July 2021. Citizens in Israel, Finland, and Estonia already enjoy timely access to their health and wellness data. The US passed the 21st Century Cures Act mandating the importance of data portability and utility.
Integrated health records allowed Israel to get early access to COVID-19 vaccines in exchange for anonymized real-world evidence for vaccine effectiveness. Half their population was vaccinated by the middle of February 2021. A peer-reviewed study of vaccine effectiveness was published February 24th, 2021.
Canada had vaccinated half of its population by mid-May – three months later. Insights related to vaccine effectiveness across jurisdictions took much longer to produce due to the fragmentation of data. These delays have cost lives and impaired the ability to re-open Canada's economy.
With decisive action, Canada can halt the negative momentum that risks us falling further behind other leading nations and suffering untold numbers of illnesses and deaths.
Treating health sector data as an asset requires the will to overcome significant institutional, structural, jurisdictional and cultural barriers that obstruct the establishment of a robust health data foundation. This will require a combination of a shared vision, clear governance alignment, accountable leadership, stewardship for interoperability investments, digital-age data policy and standards and meaningful engagement with individuals, communities and Indigenous peoples to deliver outcomes that people in Canada expect.
4. Health Data Foundation components
The health sectorFootnote 2 works collectively to deliver better health outcomes for individuals, communities and society. This includes being ready to respond to a changing threat environment and evolving socio-demographic needs. Better health outcomes and nimble responses to threats rely on informed decision-making by health care providers, policy makers and individuals. This is only possible through a robust health data foundation that provides timely access to quality information that then generates insight.
Countries that have implemented health data strategies have addressed the following five essential components:
- Clear health data accountability and governance;
- Built and sustained trust with the public and communities through meaningful engagement;
- Digital-age health data policies;
- Coherent and regulated interoperability standards; and
- Common language and health sector and public data literacy.
A health data foundation is like urban planning for the health sector
When approving public infrastructure projects, urban planners have a set of foundational principles, guidelines and requirements that help to leverage common resources and support contributions to strengthen and sustain public infrastructure.
This foundation of zoning by-laws and transportation networks provides the framework for a diversity of individual developments. As a result, it allows those projects to deliver value for individuals, their communities and the broader municipality. As the foundation is strengthened, both legacy building and future projects benefit.
The Health Data Foundation will deliver the same benefits for the health sector and will become stronger as new initiatives contribute to the foundation for the benefit of all persons in Canada.
In a Canadian context, these components need to be applied to health sector data across governments, where individual jurisdictions have autonomy to deliver health services and all jurisdictions (including Canada) benefit from seamless health information exchange and collective data and insights that will inform individual care, data policy, public safety and research.
These essential components are the pillars of the health data foundation that must be strengthened and will be the focus of any pan-Canadian health data strategy. A stronger health data foundation will accelerate data initiatives by rebuilding on what already exists and contributing to future initiatives. Future investments in the health sector must draw from and contribute to the health data foundation. This will accelerate their delivery, generate new insights faster and lower the overall cost of health data infrastructure.
The following sections provide details regarding the five components needed to strengthen Canada's health data foundation. Each section includes specific advice and case studies to demonstrate opportunities and benefits that a stronger foundation would provide.
4.1 Clear health data accountability and governance
Recommendation 1: Clarify shared accountability and governance for the creation, implementation, and sustainment of the pan-Canadian health data strategy and health data foundation.
Clear accountability and governance in the health sector for its fastest growing asset – data – is essential. Every health outcome, policy decision and innovation should rely on timely, quality data.
Attempts to establish governance in health data have had little success. Either governance has been too broad – for example, establishing a blueprint for health technology without the incentives or will to follow through on its adoption – or too narrow, where implementation meets local needs without vision, incentive or ability to spread and scale innovation. Effective accountability and governance must learn from past experience – not only ensuring sound privacy protections, but also prioritizing the achievement of better health outcomes and more cost-effective health care from opening up the collection, sharing and use of data.
When accountability and common governance for health data are established, collaboration will:
- Drive the common vision and principles across jurisdictions, the public and other critical stakeholders;
- Enable pan-Canadian decision-making (across federal, provincial and territorial governments) in areas of mutual benefit with effective escalation mechanisms to address new and emerging challenges;
- Define accountability for components of the health data foundation to align within and between jurisdictions to simplify the ability to use what exists and gain contributions for others to use;
- Leverage policies and standards that are working, revise or retire those that are not, address remaining gaps and be agile for future threats;
- Listen to, engage and involve those who are impacted – individuals and communities;
- Respect Indigenous data sovereignty and related principles using a distinctions-based approach;
- Establish goals and take action in a practical step-wise approach and hold each other accountable to follow through while delivering individual data initiatives;
- Invest in sufficient capacity and capability across the health sector to sustain the health data foundation and support data initiatives within and across jurisdictions; and,
- Measure progress independently and be transparent to all stakeholders and the public.
Sophisticated, data-intensive, and seamless: The potential for health data
When digital technology works properly it recedes into the background of lived experience. In the case of health information, the current experience is often foregrounded like a broken hammer that won't drive nails. It is reasonable to expect that person-centric health information by design could be as immersive and beneficial as other services people enjoy.
Take two valuable examples that leverage digital technologies and large-scale data, and which are regulated, pan-Canadian, involve multiple levels of government and the cooperation between public and private entities.
Online banking is person-centric in its design, providing secure money management, financial information and an array of banking services across the country and accessible world-wide. Financial institutions recognized early that these services are client-friendly and mutually beneficial.
Nav Canada controls 18 million Km2 of airspace in Canada, ensuring the safe passage of 3.3 million flights annually by providing data products for air traffic control networks. In the air or on the ground, the background expectation and benefit is safe passage of aircraft.
What these examples suggest is that people's experience of health information could be just as seamless, beneficial and operating in the background as we have come to expect of other sophisticated and data-intensive services.
Duplicating Efforts: Wasted Investment in Health Data
Many investments in health data initiatives in Canada are working in parallel, where initiatives compete, rather than collaborate, towards a common outcome. The result is new silos that impair outcomes, wastefully duplicate effort and contribute to greater health data fragmentation.
Data platforms: Multiple organizations are working on health data platforms with minimal (or no) collaboration on underlying principles, policy and design. As a result, millions of dollars are invested in duplicative ways that will require additional resources to connect silos together. Like other countries, Canada can choose to harmonize on common practices and data models now, simplifying collaboration on health data and delivering more quickly with the same investment.
Data literacy: Several Canadian educational and public sector institutions, independently recognizing the importance of health data literacy, are working on their own unique sets of terminology and curriculum. This will result in students learning different concepts, principles, and language which may lead to mistrust and confusion among learners.
Clear accountability established at high levels can set the bar for essential health data collaboration, optimizing public investments, making progress transparent and allowing jurisdictions and organizations to learn from each other.
4.2 Building and sustaining trust
Recommendation 2: Establish meaningful and ongoing engagement with the public to understand their health data needs and ongoing involvement in decisions on health data collection, sharing and use.
Systemic ways to build trust and identify individual and community requirements for health data are needed. This extends well beyond communicating the benefits of data use and how data are protected.
It is a multi-stage process to earn and sustain trust in the collection, sharing and use of health data, where the public are engaged to help define how the health data foundation should work. First, people must have the opportunity to express their requirements, hopes and concerns regarding health data. Second, the health sector needs to incorporate those requirements into its policies, processes and practices, and demonstrate their implementation. Third, the health sector needs to know whether they have earned the trust of the public and communities. Finally, this cycle needs to be continually refreshed to sustain trust and demonstrate how optimized health data sharing benefits all.
Meaningful relationships with First Nations, Inuit, and Métis are a key element of this component. While core principles for health data include respecting data sovereignty of Indigenous peoples and their related data principles, it is essential to have mutual understanding of what that respect looks like practically. This requires ongoing conversation to establish common understandings.
Building trust through meaningful engagement includes:
- Empowering people in Canada to improve their health outcomes through increased control over, and access to, their personal health information, and awareness about health data, its uses and the responsibility to share;
- Setting standard, permanent and meaningful leadership roles for the public in health data governance structures;
- Establishing public engagement infrastructure for broader public involvement in decisions on health data issues of broad interest at regional, jurisdictional and pan-Canadian scales;
- Incorporating direct (e.g. via assemblies or panels) and indirect (e.g. via polling) engagement to ensure clear and rigorous basis for the views of the general public;
- Supporting collaboration between public engagement forums across Canada; and
- Creating transparent, pro-active two-way communication with the public to help earn and sustain their trust, and demonstrate the value of health data sharing.
Case study – Public trust: A non-negotiable asset
Prioritizing trust with the public and communities is a relatively new idea and there have been missteps.
The UK broke trust with the public with its implementation of "care.data" which was scrapped in 2016. The platform intended to bring personal health records into one place to improve individual health outcomes and drive broad health sector insights. Those in charge of the project failed to adequately explain the benefits of data sharing. They also allowed the toxic possibility that personal data might be accessed by commercial companies. The decision to make patients actively opt out proved to be an additional misjudgment.
In Canada, it will be essential to inform any health data strategy at the beginning with the insights and requirements of the public. This is needed to determine how they want to be empowered with their health data to achieve their personal health objectives, which protections they want in place while their data are collected, shared, used for the public good and supporting equitable health outcomes for all.
4.3 Digital-age health data policies
Recommendation 3: Establish data stewards and structures to identify, share, and adopt pan-Canadian health data policies that are of mutual benefit to all governments.
Digital-age health data policiesFootnote 3 to prioritize data use for the public good while also ensuring it is secure are critical to optimize and sustain health data collection, sharing and appropriate use.
Current data policies are decades old and are grounded in antiquated practices based on custodianship that are not suitable for the digital age. There are also many different approaches to health data policy across jurisdictions, meaning that to engage in pan-Canadian activities or data sharing, even for the public good such as during a pandemic, requires a heavy administration to address variation and meet multiple standards. Often months or years are wasted in trying to assemble data to inform decisions or advance a novel treatment or research. Many times, the efforts required are so burdensome that the project is abandoned.
Health data custodianship, arising from provincial and territorial privacy law and its misinterpretation, provides incentives to some custodians to act in a risk-averse manner that restricts access to authorized individuals and stifles clinical care, decision support and research. Ultimately, custodianship is a provider-control model, which is antithetical to a person-centric approach.
Collectively these kinds of policy approaches have created a 'privacy chill' in Canada, where data sharing happens at the speed of the slowest actor, or not at all, due to misinterpretations of privacy requirements and a failure to incentivize data sharing. This often occurs without consideration for overall desired outcomes and, more importantly, without appreciating the risks of not sharing and using data for innovation and improvement.
Establishing a culture of data stewardship in the health sector through legislative and policy change will address many of these problems. Individuals would be more empowered and involved in the access, sharing, and use of their data. Data stewards would be accountable for ensuring that data are both used for the public good and are protected. This will require an approach to health data policy where we must:
- Abandon the custodial model of health data management and adopt digital age health data policies that are supported by legislation and based on data stewardship that champions data sharing, access, use and protection to uphold:
- Quality of individual patient care;
- Population based data use by health data stewards and those duly authorized;
- Interoperability; and
- Privacy and security
- Embed sufficiently senior level Lead Data Stewards in significant health data organizations to simplify data sharing and protection with other data stewards;
- Establish consistent federal, provincial and territorial health data policies across jurisdictions, learning from past failures;
- Embed review processes for health data policies to ensure ongoing appropriateness and relevance;
Stewardship: Transforming our Approach to Data Management
Data stewards are the evolution of privacy officers and data custodians, and contribute to, collaborate with and leverage other data stewards to promote cohesion. Data Stewardship roles have not yet been clearly defined in Canada. However, their accountabilities could include:
- aligning policy, process and standards across organizations to achieve prioritized health outcomes while protecting the privacy of individuals;
- seeking opportunities to re-use data and leverage existing policy, process or standards;
- contributing health data policy and practices for others to re-use;
- collaborating to adopt common principles and minimize unintentional duplication; and
- communicating with others so that new initiatives are aware of the opportunity to collaborate.
This would be similar to Caldicott guardians appointed in the National Health Service (UK).
'Privacy Chill': Harms individuals, contributes to the brain drain, and hampers pandemic response
The Hippocratic Oath says to "do no harm" and is often cited as the reason to not share data as it may cause harm through a hypothetical privacy breach. This does not consider the harms that may be caused by not sharing data.
For individuals, data are often not available for care in emergencies, and are not easily accessible or portable to meet their needs. Insufficient data are shared to inform health sector safety, quality and equity improvements. Duplicative and redundant tests are ordered due to inability to access previous test results.
Data scientists have migrated to Canada to make a meaningful contribution leveraging Canada's rich data assets, but they then realize that the ability to apply their skills is hampered by the inability to get timely access to data. Further, studies are not completed due to excessive administration to gain access and cleanse disparate data sets.
The 'privacy chill' also hampered Canada's response to COVID-19. Scientists were unable to link crucial data about variants of concern to determine whether the patient with a positive COVID test had been vaccinated, where they were located and other important details that would have benefited insights and not impacted the privacy of the individual. Scientists were not able to develop the detailed insight that could have improved Canada's response and potentially saved lives.
Case study – Modernizing Health Data Policy: Consistent data sharing in the United States
The Sequoia project in the United States is the recognized organization that is fostering interoperability and coherent multi-lateral health data sharing.
In their multi-lateral agreement, they have developed a standard agreement for the minimum requirements for sharing data with other organizations in their network. These minimum requirements reflect what is needed to trust each other and sustain the trust of the public. Accountabilities are clearly identified and methods for escalations and oversight are provided.
Through this simplified protocol, data are shared among peers with trust and speed. Further, they have replaced tens of thousands of bi-lateral data sharing agreements with one omnibus agreement, saving time and money without impairing (and arguably improving) integrity and trust.
4.4 Interoperability by design
Recommendation 4: Empowered by accountable leadership at the highest levels, establish bodies entrusted to identify, share and implement pan-Canadian interoperability standards that are of mutual benefit to all governments, with orchestration across these bodies.
Common data standards for interoperability, including data exchange and content, are the backbone of health data in the health sector and need to be consistently defined, adopted, evolved and sustained.
Many standards – including exchange standards for technologies to communicate with each other, and data standards for personal data such as gender – are adopted on an ad hoc basis, leading to additional costs to connect fragmented data silos, and further costs to maintain those connections. Fragmentation causes delays and additional cost in public health surveillance, necessary research and decisions by health authorities and governments. The absence of common standards leads to decreased data quality, completeness and timeliness, and in some cases to no useable data at all. This contributes to sub-optimal individual health outcomes, impaired public health insights and struggles to innovate. Data sets are too small, different, and disparate to inform pan-Canadian decision-making and contribute internationally.
In addition, current data custodian policies and legislation for health data management in Canada place control and management of personal health information in the hands of designated health service providers and organizations. They emphasize the importance of health data privacy and security, but are silent on health data interoperability and data use for public good. As a consequence, digital health technologies have been deployed on a service-centric basis with little regard to data interoperability or the wider benefits that could be achieved through data sharing. This current custodian framework is promoting a lack of data interoperability, and thereby compromising both individual care and public and population health interventions.
Adopting common interoperability standards would enable individuals to have an integrated health record that follows them throughout their lives and is accessible on a "need to know" basis to any of the health care providers in their "circle of care". This kind of person-centric intelligence avoids burdens on the public as well as individuals – avoiding unnecessary testing and repeated explanations of their health history as they move through care settings, and reducing cost to access and transfer their records. Their health data moves with them, accessible by those who provide care.
These same integrated health records can be used for whole sector intelligence to power research that supports personal health objectives, public health that protects society from future threats and policy that supports continuous improvement across the sector.
Canada has access to multiple, existing data standards. These can be brought together, in the areas of greatest mutual benefit, to establish pan-Canadian standards. Interoperability standards, when implemented must:
- Adopt a model architecture that enables interoperability across jurisdictions;
- Establish data and exchange standards where there is mutual benefit across Canada (including linking across data sets and alignment to international standards);
- Leverage partnerships between provinces, territories and the federal government to affirm the adoption of the model architecture across Canada;
- jurisdictions would develop gap analysis and roadmap to adopt common model architecture;
- Establish an ongoing process to regularly review data and exchange standards for ongoing appropriateness, relevance and dissemination;
- Collect standards that are used and not yet broadly adopted with a process to communicate and share what has been collected (e.g. standards on emerging areas like genomics);
- Communicate clearly and broadly so interoperability standards are easy to find, easy to implement and easy to integrate with other standards; and
- Develop common requirements for procurement of health data and IT solutions, including software solutions that embed interoperability standards.
Case study – Interoperability: Required for whole health sector intelligence
As evidenced during the pandemic, infection status with hospitalizations and with vaccinations are all in separate data silos within many provinces, and are in completely different silos province by province. Methods to link these data siloes together are cumbersome and inefficient.
By contrast, the United Kingdom is able to link health records of 55 million people to test results and vaccination records to develop whole system intelligence to inform its public health measures. They were also able to link to over 800 thousand genomic records to develop insights into the progression of variants.
Without interoperability standards, Canada is unable to generate the critical health intelligence necessary to manage public health crises. Some intelligence gaps are filled by relying on other countries' data and analyses, despite not accurately representing the situation in Canada.
Case study – Lack of interoperability: Disempowers patients, wastes time, and inhibits innovation
More than 2 million Canadians have diabetes. As part of the monitoring of their disease, these patients have regular blood sugar tests at a local blood lab. Many of these labs provide the ability for patients to access the results of these tests online shortly after their test.
Depending on the lab and the lab technician producing the result, a single vial of blood could have as many as 14 different values due to different methodologies, levels of precision and order of magnitude. This makes it difficult for an individual to understand the results, let alone use them for their decisions.
Further, not all labs are interoperable, sometimes sending the results to the patient's doctor by fax. This requires manual data re-entry, which increases risk to the patient in two ways: via a keying error or a privacy breach.
The lack of standards for blood sugar tests wastes time for providers in interpreting the results and may lead to poor health outcomes. Further, any secondary use of the data (such as for research) requires additional time to transform the data onto a comparable scale and often loses precision.
This lack of interoperability standards negatively impacts individuals' ability to be empowered in their care, wastes precious time for health providers and prevents meaningful research and innovation.
4.5 Common language and data literacy
Recommendation 5: Establish a common language for health data and support programs for health data literacy for the public, leaders and health workforces.
Language unifies communities. A common health data terminology for health leaders, health workforces and the public would improve health data literacy and simplify health data policy, standard and decision-making.
Currently, many health data policies are complex and incomprehensible for most people. This results in long negotiations for data access and sharing as significant time is necessary to interpret idiosyncratic terminology. Often, data are not shared as confusion over terminology increases risk for the decision-maker – further contributing to the 'privacy chill'. Without common language, miscommunication may result in data misuse and negatively influence all aspects of health sector performance and public trust.
Improved health data literacy is essential for clear accountability, interoperability standards, health data policy and meaningful engagement with the public and communities. It is also essential for the impactful use of data, evaluating risks and benefits, turning insights into action and building trust among partners. Common language makes it easier to communicate with each other in a way that facilitates trust, accelerates outcomes, and lowers risk of miscommunication.
Common terminology for health data including roles and responsibilities that will enable the development of literacy programs that:
- Communicate the overall vision and strategy for health data to engage the public, leaders and health workforces, using context-based case studies to demonstrate the value of data for the audience;
- Communicate a common code of practice for health data professionals to champion coherent health data policy and interoperability standards;
- Promote the practice of learning health systems where all parts of the health sector continually improve based on their trusted insights; and
- Include health data literacy in school-age curriculum, which is starting to be done in other countries.
Case study – Data literacy: Drives health sector transformation in Finland
In 2018, Finland set an audacious goal to educate 1% of their population on data and the basics of artificial intelligence (AI) to demystify how AI works and the benefits it would create.
A free online course was developed to educate and to increase social license for the use of data by providing clarity on how individuals' data were protected and how data are used to create beneficial outcomes for individuals, communities and Finland's economy.
In 2019, Finland decided to offer the course to all European Union (EU) member states for free, with the goal of training 1% of Europe's population as well. By 2021, approximately 2% of Finnish people had completed the course and over 0.5% of the population of the EU. Finnish people enjoy access to their personal health data (the 2nd most popular website in the country) and are now able to fill their prescriptions while in Estonia or Spain. Health sector transformation is underway and supported by the public.
5. Health Data Foundation: Start building it now
As our governmentsFootnote 4 consider how and when a pan-Canadian health data strategy could be funded and implemented, several things are clear and should be acted on immediately:
- The public must be meaningfully engaged in the health data strategy to ensure that their needs, requirements and aspirations are clearly articulated, understood and respected; and
- Governments must commit to addressing the 'privacy chill' surrounding health data to be able to give their constituents a more targeted, responsive health sector.
These investments will take significant resources, funding and personnel capacity to advance common pan-Canadian goals, stand up provincial/territorial strategies in a collaborative and coordinated manner, and recognize those areas of greatest mutual benefit to standardize, harmonize or coordinate.
| Foundation pillar | Actions |
|---|---|
| Governance | Establish federal-provincial-territorial governance, clarify accountabilities and align with First Nations, Métis and Inuit data governance Establish coordinating secretariats |
| Trust | Engage the public and First Nations, Inuit and Métis to understand their requirements |
| Policy | Develop target health data policies in areas of greatest mutual benefit |
| Interoperability | Develop target health data interoperability standards in areas of greatest mutual benefit |
| Capacity and literacy | Develop target health data terminology and literacy in areas of greatest mutual benefit |
In addition, several prioritized health data projects should be identified to contribute to, and demonstrate the value of, a health data foundation-based approach to implementation. Ideally, the prioritized project would be chosen based on both its availability of data and its ability to contribute to the health data foundation.
Our final report will elaborate these recommendations:
- Governance: Structures necessary to monitor, sustain and evolve the strategy;
- Trust: Structures to meaningfully engage the public and First Nations, Inuit and Metis peoples;
- Policy: Specific policies to be considered; elaboration of model of data stewardship;
- Interoperability: Specific interoperability principles, standards and designs; and
- Capacity and literacy: Specific terminology to be adopted and literacy initiatives to be prioritized.
Immediately, jurisdictions should come together to understand their current state; co-develop policy, interoperability standards and terminology; and agree on priority projects that will start to transform health data in Canada.
6. Conclusion
Canada's response to COVID-19 relied on heroics, ingenuity and immeasurable additional hours of work from many – front-line staff providing compassionate care, public health professionals acting as a steady hand in the face of ambiguity and most of the public who chose to work together for the collective public good.
Heroics are not a sustainable strategy.
Canada needs to make it easy for everyone to have access to the right data at the right time to develop the right insight for health outcomes that benefit individuals, communities and society. This requires overcoming the systemic barriers that have prevented progress with health data.
This report has articulated areas where urgent action is needed to transform Canada's data culture from 'privacy chill' to empowerment, collaboration and innovation. This new approach would prioritize sharing data to achieve health sector outcomes and ensure protection of personal health information. It would incent conscious collaboration across regions, jurisdictions and Canada rather than the fragmented competitive approach that is in place today. It would accelerate initiatives by making it easy to find the excellence that exists to simplify data sharing for generating timely and impactful insights and outcomes.
Together, we can unleash the value of data and improve the health of every person in Canada.
"How governments protect and leverage their national assets in the global technology competition will increasingly determine which countries race ahead in the middle decades of the 21st century. And which ones lag behind…"
Glossary
Data: Observations, narratives or measurements that are captured for possible use as the basis for further analysis, calculation or reasoning.Footnote 5
Data Custodian: As defined in Canadian health legislation, an individual or organization responsible for the secure collection and/or storage of health data and the curation of health data use, disclosure, retention and disposal. Primarily concerned with security and privacy of health data.
Data Steward: An entity or senior government role responsible for assuring the quality, integrity and access arrangements of data and metadata in a manner that is consistent with applicable law, institutional policy and individual permissions. Includes entities and positions that deal primarily with personal health information, and those that deal with other health information.Footnote 6
De-identification: The process of removing or altering data that identifies an individual or could, foreseeably, identify an individual in the future to lower the possibility of re-identification. The degree to which data is de-identified depends upon the sensitivity of the information, what it is being used for and who has access to it.Footnote 7
Health Data: Observations, facts or measurements – captured for possible further analysis, calculation or reasoning – which relate to the physical or mental health status of individuals, health system performance and socio-economic,community and health system characteristics.
Health Information: Health data that have been analyzed or interpreted to provide insight or a narrative related to the physical or mental health status of individuals, health system performance, and socio-economic, community and health system characteristics.
Health Sector: The general set of activities related to Individual-based health, population-based health, health research and education and health management, oversight and governance.
Health Services: Activities related to health, delivered either directly or indirectly to the public, on both an individual level (including primary, secondary and tertiary care) and a population level (disease surveillance, prevention and control; health promotion; reducing health inequity).
Interoperability: The capacity for seamless sharing of health data and information between health sector stakeholders by means of policy, governance,workflow and, especially, technical alignment.
Personal Health Information: Health data or information that is specific to a unique and identified individual.
Information: Data that have already been interpreted, i.e. they have meaning in a specific context.Footnote 8
Addressing barriers from the Expert Advisory Group's first report
| Barrier | Recommendation |
|---|---|
| Lack of trust and clear accountability | Recommendation 1: Clarify shared accountability and governance for the creation, implementation and sustainment of the pan-Canadian health data strategy and health data foundation. |
| A culture of risk aversion | |
| Misaligned incentives and lack of a common vision | |
| Limited public insight and involvement | Recommendation 2: Establish meaningful and ongoing engagement for the public to understand their health data needs and ongoing involvement in decisions on health data collection, sharing and use. |
| Lack of consensus and follow-up on pan-Canadian interoperability | Recommendation 3: Empowered by accountable leadership at the highest levels, establish bodies entrusted to identify, share and implement pan-Canadian interoperability standards that are of mutual benefit to all governments, with orchestration across these bodies. |
| A failure to spread and scale excellence | |
| A reluctance to include conditional requirements | |
| An uncoordinated approach to procuring and implementing | Recommended Action 4: Establish data stewards and structures to identify, share and adopt pan-Canadian health data policies that are of mutual benefit to all governments. |
| Antiquated data policy environment | |
| Inconsistent and insufficient investment in data capacity and capability | |
| Significant data debt | |
| Fiscal pressures | |
| A culture of avoidance | Recommendation 5: Establish a common language for health data and support programs for health data literacy for the public, leaders and health workforces. |
References
Main Text
Canadian Anonymization Network. Practices for Generating Non-identifiable Data.
Available online at https://deidentify.ca/wp-content/uploads/2021/08/CANON-OPC-Project-Final-Report-v9.pdf
Commonwealth Fund. (2021). Mirror, Mirror 2021: Reflecting Poorly.
Available online at https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
Dagan, Noa; Noam Barda; Eldad Kepten; et al. (2021). BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. The New England Journal of Medicine 384(15).
Available online at https://www.nejm.org/doi/10.1056/NEJMoa2101765
Dawson, Philip & Marc-Etienne Ouimette. (September 7, 2021). Tech and geopolitics are on a collision course. Is Canada ready?. The Globe and Mail.
Available online at https://www.theglobeandmail.com/business/commentary/article-tech-and-geopolitics-are-on-a-collision-course-is-canada-ready/
Deckler, Janosch. (2019). Finland's grand AI experiment. Politico EU.
Available online at https://www.politico.eu/article/finland-one-percent-ai-artificial-intelligence-courses-learning-training/
Finnish Ministry of Economic Affairs and Employment. (May 3, 2021). Finalnd's AI course to contribute to digital skills of Europeans across the continent [Press Release].
Available online at https://valtioneuvosto.fi/en/-/1410877/finland-s-ai-course-to-contribute-to-digital-skills-of-europeans-across-the-continent
Global Alliance for Genomics & Health. (2016). Data Sharing Lexicon.
Available online at https://www.ga4gh.org/wp-content/uploads/GA4GH_Data_Sharing_Lexicon_Mar15.pdf
Godlee, Fiona. (2016). What can we salvage from care.data?. The BMJ 354.
Available online at https://www.bmj.com/content/354/bmj.i3907
Health Innovation Network. (2017). What is person-centred care and why is it important? Available online at https://healthinnovationnetwork.com/system/ckeditor_assets/attachments/41/what_is_person-centred_care_and_why_is_it_important.pdf
Kalia, Kishan; Gayatri Saberwal & Gaurav Sharma. (2021). The lag in SARS-CoV-2 genome submissions to GISAID. Nature Biotechnology 39.
Available online at https://www.nature.com/articles/s41587-021-01040-0
Organization of Economic Cooperation and Development. (2019). Health in the 21st Century: Putting Data to Work for Stronger Health Systems.
Available online at https://www.oecd-ilibrary.org/sites/e3b23f8e-en/index.html?itemId=/content/publication/e3b23f8e-en
pan-Canadian Health Data Strategy Expert Advisory Group. (2021). Expert Advisory Group Report 1: Charting a Path toward Ambition. Available online at https://www.canada.ca/en/public-health/corporate/mandate/about-agency/external-advisory-bodies/list/pan-canadian-health-data-strategy-reports-summaries/expert-advisory-group-report-01-charting-path-toward-ambition.html
Statistics Canada. (2018). Health Fact Sheets: Diabetes, 2017.
Available online at https://www150.statcan.gc.ca/n1/pub/82-625-x/2018001/article/54982-eng.htm
UK Caldicott Guadian Council. (n.d.) The Caldicott Guardian's role.
Available online at https://www.ukcgc.uk/caldicott-guardian-role
UK Department of Health and Social Care. (2021) Data saves lives: reshaping health and social care with data (draft).
Available online at https://www.gov.uk/government/publications/data-saves-lives-reshaping-health-and-social-care-with-data-draft/data-saves-lives-reshaping-health-and-social-care-with-data-draft
US Food and Drug Administration. (2020). Regulatory Information: 21st Century Cures Act.
Available online at https://www.fda.gov/regulatory-information/selected-amendments-fdc-act/21st-century-cures-act
Annexes
Dormuth, Colin; Brenda Hemmelgarn; J. Michael Paterson; et al. (2013). Use of high potency statins and rates of admission for acute kidney injury: multicenter, retrospective observational analysis of administrative databases. The BMJ 346.
Available online at https://www.bmj.com/content/346/bmj.f880
Kaiser Permanente Thrive. (July 26, 2018). Electronic Health Records Enabled Kaiser Permanente to Identify Vioxx Concerns. YouTube.
Available online at https://www.youtube.com/watch?v=C0HImCL2m6E
Royal Society of Canada. (2021). Excess All-Cause Mortality During the COVID-19 Epidemic in Canada: An RSC Policy Briefing.
Available online at https://rsc-src.ca/en/covid-19-policy-briefing/excess-all-cause-mortality-during-covid-19-epidemic-in-canada
Sadowski, Jathan. (2021). Everyone should decide how their digital data are used — not just tech companies. Nature – Comment.
Available online at https://www.nature.com/articles/d41586-021-01812-3
Statistics Canada. (2021). Provisional weekly estimates of the number of deaths, expected number of deaths and excess mortality: Interactive Tool.
Available online at https://www150.statcan.gc.ca/n1/pub/71-607-x/71-607-x2020023-eng.htm
Wong, Andrew; Erkin Otles; John Donnelly; et al. (2021). External Validation of a Widely Implemented Proprietary Sepsis Prediction Model in Hospitalized Patients. JAMA Internal Medicine.
Available online at https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2781307
Members of the Expert Advisory Group
Chair
Dr. Vivek Goel
Members
- Dr. Ewan Affleck
- Dr. David Castle
- Dr. Stafford Dean
- Dr. Jonathan Dewar
- Dr. Isabel Fortier
- Mr. Michael Harvey
- Dr. Steven Hoffman
- Dr. Bartha Maria Knoppers
- Ms. Alies Maybee
- Dr. Muhammad Mamdani
- Dr. Kim McGrail
- Mr. Jeff Nesbitt
- Dr. Cory Neudorf
- Ms. Glynda Rees
- Dr. Janet Smylie
- Dr. Gail Tomblin Murphy
- Dr. Graham Tipples
- Dr. Michael Wolfson
Contact
To contact the secretariat directly:
Email: pchds-spcds@phac-aspc.gc.ca
Annex A: Data gap case study: Adverse drug reactions
Pharmaceuticals are one of the most expensive parts of Canadian health care, and drugs are heavily regulated so they are only approved if they are safe and effective, at least when they are being introduced. However, the clinical trials supporting their approval are generally months in duration, and have modest sample sizes compared to the often millions of individuals who will be using each drug. As a result, adverse drug reactions (ADRs) do occur after a drug has been approved. ADRs are detected by Manufacturers (required to report ADRs to Health Canada), observing a problem detected in another country, or by a voluntary system whereby patients or physicians report unusual side effects to Health Canada.
The pain reliver Vioxx is a notorious and stark example where a clear and serious side effect, heart attack, was not found prior to its approval. Moreover, this side effect could not be detected by a voluntary ADR reporting system, since individual physicians typically have patient groups where many were taking Vioxx, and many had heart attacks, but the correlation was not easily seen. The relationship only became clear after the US FDA requested a statistical analysis of millions of Kaiser Permanente patient records where individual data on drug prescriptions and hospital visits for heart attacks were linked.
Health Canada has since funded CIHR to create CNODES, a collaborating centre of the Drug Safety and Effectiveness Network (DSEN). Fortunately, most of its studies have not found any problems. But one of its first studies of high dose statins (a widely prescribed drug to prevent heart attacks) has shown that in these patients, there is a significantly elevated risk of kidney damage.
Because of the still insurmountable restrictions to the inter-provincial flow of the linked health care data, these statistical analyses must be done within provincial silos, and then only in the provinces that even have enough of the needed data. There are major challenges as each province has its own way of defining various data elements, and the best that can be done is to compare the statistical results from each provincial data silo. As a result, the statistical results are under-powered compared to what could be done if these data were not siloed.
Annex B: Data gap case study: Measuring mortality from COVID-19
Ideally, deaths from COVID-19 would be fully and quickly reported on death certificates. But Canada has suffered from major problems in this most fundamental kind of health data, which has been collected by Statistics Canada and its predecessor organization for more than a century: incomplete data including not only the age and sex of the decedent, but also the medical cause of death.
The following two graphs show recent data, first for Canada in 2020, and then for 2021, downloaded from Statistics Canada:
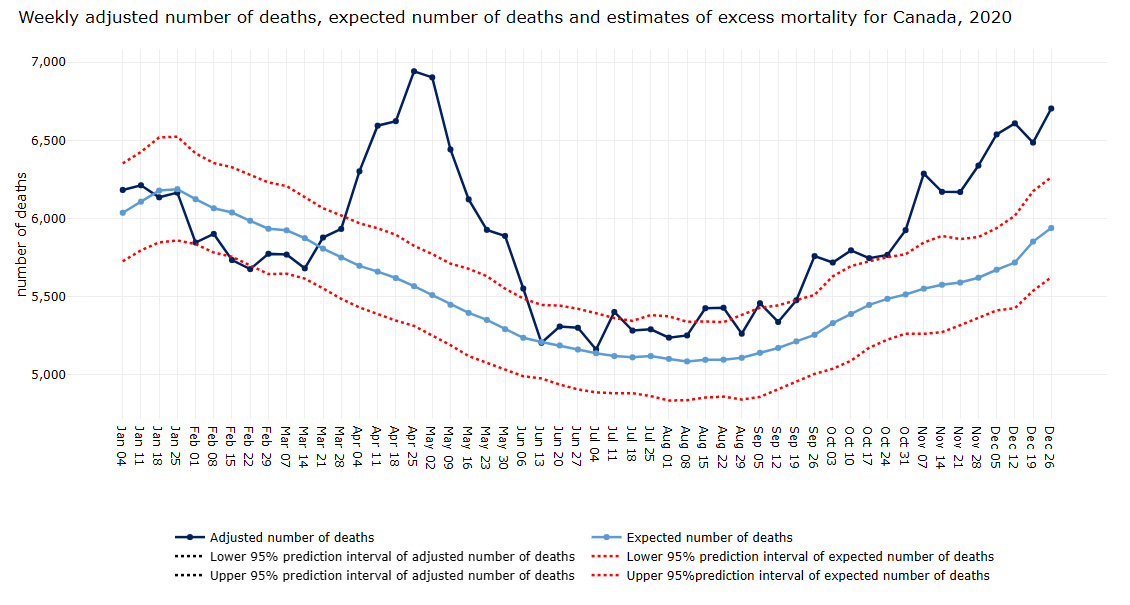
Figure B1: Text description
This image is a graph depicting the adjusted number of deaths, the number of expected deaths and the estimate of excess mortality for Canada on a weekly basis during 2020.
The title of the image is Weekly adjusted number of deaths, expected number of deaths and estimates of excess mortality for Canada, 2020
| Date | Characteristics | Number of deaths |
|---|---|---|
| January 04 | Adjusted number of deaths | 6,183 |
| January 11 | Adjusted number of deaths | 6,213 |
| January 18 | Adjusted number of deaths | 6,136 |
| January 25 | Adjusted number of deaths | 6,166 |
| February 01 | Adjusted number of deaths | 5,847 |
| February 08 | Adjusted number of deaths | 5,902 |
| February 15 | Adjusted number of deaths | 5,735 |
| February 22 | Adjusted number of deaths | 5,677 |
| February 29 | Adjusted number of deaths | 5,775 |
| March 07 | Adjusted number of deaths | 5,769 |
| March 14 | Adjusted number of deaths | 5,681 |
| March 21 | Adjusted number of deaths | 5,878 |
| March 28 | Adjusted number of deaths | 5,933 |
| April 04 | Adjusted number of deaths | 6,301 |
| April 11 | Adjusted number of deaths | 6,593 |
| April 18 | Adjusted number of deaths | 6,622 |
| April 25 | Adjusted number of deaths | 6,941 |
| May 02 | Adjusted number of deaths | 6,901 |
| May 09 | Adjusted number of deaths | 6,441 |
| May 16 | Adjusted number of deaths | 6,121 |
| May 23 | Adjusted number of deaths | 5,926 |
| May 30 | Adjusted number of deaths | 5,886 |
| June 06 | Adjusted number of deaths | 5,549 |
| June 13 | Adjusted number of deaths | 5,201 |
| June 20 | Adjusted number of deaths | 5,304 |
| June 27 | Adjusted number of deaths | 5,296 |
| July 04 | Adjusted number of deaths | 5,157 |
| July 11 | Adjusted number of deaths | 5,396 |
| July 18 | Adjusted number of deaths | 5,278 |
| July 25 | Adjusted number of deaths | 5,285 |
| August 01 | Adjusted number of deaths | 5,232 |
| August 08 | Adjusted number of deaths | 5,246 |
| August 15 | Adjusted number of deaths | 5,418 |
| August 22 | Adjusted number of deaths | 5,421 |
| August 29 | Adjusted number of deaths | 5,255 |
| September 05 | Adjusted number of deaths | 5,451 |
| September 12 | Adjusted number of deaths | 5,330 |
| September 19 | Adjusted number of deaths | 5,468 |
| September 26 | Adjusted number of deaths | 5,748 |
| October 03 | Adjusted number of deaths | 5,707 |
| October 10 | Adjusted number of deaths | 5,783 |
| October 17 | Adjusted number of deaths | 5,731 |
| October 24 | Adjusted number of deaths | 5,751 |
| October 31 | Adjusted number of deaths | 5,908 |
| November 07 | Adjusted number of deaths | 6,268 |
| November 14 | Adjusted number of deaths | 6,151 |
| November 21 | Adjusted number of deaths | 6,147 |
| November 28 | Adjusted number of deaths | 6,314 |
| December 05 | Adjusted number of deaths | 6,510 |
| December 12 | Adjusted number of deaths | 6,578 |
| December 19 | Adjusted number of deaths | 6,453 |
| December 26 | Adjusted number of deaths | 6,667 |
| January 04 | Expected number of deaths | 6,037 |
| January 11 | Expected number of deaths | 6,108 |
| January 18 | Expected number of deaths | 6,179 |
| January 25 | Expected number of deaths | 6,188 |
| February 01 | Expected number of deaths | 6,124 |
| February 08 | Expected number of deaths | 6,066 |
| February 15 | Expected number of deaths | 6,039 |
| February 22 | Expected number of deaths | 5,986 |
| February 29 | Expected number of deaths | 5,935 |
| March 07 | Expected number of deaths | 5,925 |
| March 14 | Expected number of deaths | 5,875 |
| March 21 | Expected number of deaths | 5,808 |
| March 28 | Expected number of deaths | 5,751 |
| April 04 | Expected number of deaths | 5,698 |
| April 11 | Expected number of deaths | 5,661 |
| April 18 | Expected number of deaths | 5,620 |
| April 25 | Expected number of deaths | 5,568 |
| May 02 | Expected number of deaths | 5,511 |
| May 09 | Expected number of deaths | 5,449 |
| May 16 | Expected number of deaths | 5,397 |
| May 23 | Expected number of deaths | 5,352 |
| May 30 | Expected number of deaths | 5,293 |
| June 06 | Expected number of deaths | 5,238 |
| June 13 | Expected number of deaths | 5,211 |
| June 20 | Expected number of deaths | 5,189 |
| June 27 | Expected number of deaths | 5,163 |
| July 04 | Expected number of deaths | 5,139 |
| July 11 | Expected number of deaths | 5,121 |
| July 18 | Expected number of deaths | 5,113 |
| July 25 | Expected number of deaths | 5,121 |
| August 01 | Expected number of deaths | 5,103 |
| August 08 | Expected number of deaths | 5,087 |
| August 15 | Expected number of deaths | 5,097 |
| August 22 | Expected number of deaths | 5,098 |
| August 29 | Expected number of deaths | 5,110 |
| September 05 | Expected number of deaths | 5,142 |
| September 12 | Expected number of deaths | 5,173 |
| September 19 | Expected number of deaths | 5,215 |
| September 26 | Expected number of deaths | 5,257 |
| October 03 | Expected number of deaths | 5,332 |
| October 10 | Expected number of deaths | 5,390 |
| October 17 | Expected number of deaths | 5,448 |
| October 24 | Expected number of deaths | 5,487 |
| October 31 | Expected number of deaths | 5,515 |
| November 07 | Expected number of deaths | 5,552 |
| November 14 | Expected number of deaths | 5,577 |
| November 21 | Expected number of deaths | 5,591 |
| November 28 | Expected number of deaths | 5,622 |
| December 05 | Expected number of deaths | 5,673 |
| December 12 | Expected number of deaths | 5,719 |
| December 19 | Expected number of deaths | 5,853 |
| December 26 | Expected number of deaths | 5,940 |
| January 04 | Lower 95% prediction interval of adjusted number of deaths | 6,183 |
| January 11 | Lower 95% prediction interval of adjusted number of deaths | 6,213 |
| January 18 | Lower 95% prediction interval of adjusted number of deaths | 6,136 |
| January 25 | Lower 95% prediction interval of adjusted number of deaths | 6,166 |
| February 01 | Lower 95% prediction interval of adjusted number of deaths | 5,847 |
| February 08 | Lower 95% prediction interval of adjusted number of deaths | 5,902 |
| February 15 | Lower 95% prediction interval of adjusted number of deaths | 5,734 |
| February 22 | Lower 95% prediction interval of adjusted number of deaths | 5,676 |
| February 29 | Lower 95% prediction interval of adjusted number of deaths | 5,774 |
| March 07 | Lower 95% prediction interval of adjusted number of deaths | 5,768 |
| March 14 | Lower 95% prediction interval of adjusted number of deaths | 5,680 |
| March 21 | Lower 95% prediction interval of adjusted number of deaths | 5,877 |
| March 28 | Lower 95% prediction interval of adjusted number of deaths | 5,933 |
| April 04 | Lower 95% prediction interval of adjusted number of deaths | 6,301 |
| April 11 | Lower 95% prediction interval of adjusted number of deaths | 6,593 |
| April 18 | Lower 95% prediction interval of adjusted number of deaths | 6,622 |
| April 25 | Lower 95% prediction interval of adjusted number of deaths | 6,941 |
| May 02 | Lower 95% prediction interval of adjusted number of deaths | 6,901 |
| May 09 | Lower 95% prediction interval of adjusted number of deaths | 6,441 |
| May 16 | Lower 95% prediction interval of adjusted number of deaths | 6,121 |
| May 23 | Lower 95% prediction interval of adjusted number of deaths | 5,926 |
| May 30 | Lower 95% prediction interval of adjusted number of deaths | 5,886 |
| June 06 | Lower 95% prediction interval of adjusted number of deaths | 5,549 |
| June 13 | Lower 95% prediction interval of adjusted number of deaths | 5,200 |
| June 20 | Lower 95% prediction interval of adjusted number of deaths | 5,303 |
| June 27 | Lower 95% prediction interval of adjusted number of deaths | 5,295 |
| July 04 | Lower 95% prediction interval of adjusted number of deaths | 5,155 |
| July 11 | Lower 95% prediction interval of adjusted number of deaths | 5,393 |
| July 18 | Lower 95% prediction interval of adjusted number of deaths | 5,274 |
| July 25 | Lower 95% prediction interval of adjusted number of deaths | 5,281 |
| August 01 | Lower 95% prediction interval of adjusted number of deaths | 5,227 |
| August 08 | Lower 95% prediction interval of adjusted number of deaths | 5,241 |
| August 15 | Lower 95% prediction interval of adjusted number of deaths | 5,414 |
| August 22 | Lower 95% prediction interval of adjusted number of deaths | 5,415 |
| August 29 | Lower 95% prediction interval of adjusted number of deaths | 5,250 |
| September 05 | Lower 95% prediction interval of adjusted number of deaths | 5,445 |
| September 12 | Lower 95% prediction interval of adjusted number of deaths | 5,324 |
| September 19 | Lower 95% prediction interval of adjusted number of deaths | 5,461 |
| September 26 | Lower 95% prediction interval of adjusted number of deaths | 5,742 |
| October 03 | Lower 95% prediction interval of adjusted number of deaths | 5,700 |
| October 10 | Lower 95% prediction interval of adjusted number of deaths | 5,775 |
| October 17 | Lower 95% prediction interval of adjusted number of deaths | 5,724 |
| October 24 | Lower 95% prediction interval of adjusted number of deaths | 5,744 |
| October 31 | Lower 95% prediction interval of adjusted number of deaths | 5,899 |
| November 07 | Lower 95% prediction interval of adjusted number of deaths | 6,259 |
| November 14 | Lower 95% prediction interval of adjusted number of deaths | 6,141 |
| November 21 | Lower 95% prediction interval of adjusted number of deaths | 6,138 |
| November 28 | Lower 95% prediction interval of adjusted number of deaths | 6,303 |
| December 05 | Lower 95% prediction interval of adjusted number of deaths | 6,499 |
| December 12 | Lower 95% prediction interval of adjusted number of deaths | 6,566 |
| December 19 | Lower 95% prediction interval of adjusted number of deaths | 6,442 |
| December 26 | Lower 95% prediction interval of adjusted number of deaths | 6,655 |
| January 04 | Lower 95% prediction interval of expected number of deaths | 5,727 |
| January 11 | Lower 95% prediction interval of expected number of deaths | 5,797 |
| January 18 | Lower 95% prediction interval of expected number of deaths | 5,848 |
| January 25 | Lower 95% prediction interval of expected number of deaths | 5,860 |
| February 01 | Lower 95% prediction interval of expected number of deaths | 5,837 |
| February 08 | Lower 95% prediction interval of expected number of deaths | 5,783 |
| February 15 | Lower 95% prediction interval of expected number of deaths | 5,756 |
| February 22 | Lower 95% prediction interval of expected number of deaths | 5,702 |
| February 29 | Lower 95% prediction interval of expected number of deaths | 5,645 |
| March 07 | Lower 95% prediction interval of expected number of deaths | 5,648 |
| March 14 | Lower 95% prediction interval of expected number of deaths | 5,616 |
| March 21 | Lower 95% prediction interval of expected number of deaths | 5,554 |
| March 28 | Lower 95% prediction interval of expected number of deaths | 5,487 |
| April 04 | Lower 95% prediction interval of expected number of deaths | 5,432 |
| April 11 | Lower 95% prediction interval of expected number of deaths | 5,390 |
| April 18 | Lower 95% prediction interval of expected number of deaths | 5,348 |
| April 25 | Lower 95% prediction interval of expected number of deaths | 5,314 |
| May 02 | Lower 95% prediction interval of expected number of deaths | 5,254 |
| May 09 | Lower 95% prediction interval of expected number of deaths | 5,191 |
| May 16 | Lower 95% prediction interval of expected number of deaths | 5,121 |
| May 23 | Lower 95% prediction interval of expected number of deaths | 5,078 |
| May 30 | Lower 95% prediction interval of expected number of deaths | 5,038 |
| June 06 | Lower 95% prediction interval of expected number of deaths | 4,992 |
| June 13 | Lower 95% prediction interval of expected number of deaths | 4,978 |
| June 20 | Lower 95% prediction interval of expected number of deaths | 4,939 |
| June 27 | Lower 95% prediction interval of expected number of deaths | 4,908 |
| July 04 | Lower 95% prediction interval of expected number of deaths | 4,889 |
| July 11 | Lower 95% prediction interval of expected number of deaths | 4,883 |
| July 18 | Lower 95% prediction interval of expected number of deaths | 4,884 |
| July 25 | Lower 95% prediction interval of expected number of deaths | 4,865 |
| August 01 | Lower 95% prediction interval of expected number of deaths | 4,837 |
| August 08 | Lower 95% prediction interval of expected number of deaths | 4,839 |
| August 15 | Lower 95% prediction interval of expected number of deaths | 4,856 |
| August 22 | Lower 95% prediction interval of expected number of deaths | 4,862 |
| August 29 | Lower 95% prediction interval of expected number of deaths | 4,843 |
| September 05 | Lower 95% prediction interval of expected number of deaths | 4,860 |
| September 12 | Lower 95% prediction interval of expected number of deaths | 4,907 |
| September 19 | Lower 95% prediction interval of expected number of deaths | 4,958 |
| September 26 | Lower 95% prediction interval of expected number of deaths | 5,007 |
| October 03 | Lower 95% prediction interval of expected number of deaths | 5,040 |
| October 10 | Lower 95% prediction interval of expected number of deaths | 5,091 |
| October 17 | Lower 95% prediction interval of expected number of deaths | 5,174 |
| October 24 | Lower 95% prediction interval of expected number of deaths | 5,226 |
| October 31 | Lower 95% prediction interval of expected number of deaths | 5,264 |
| November 07 | Lower 95% prediction interval of expected number of deaths | 5,263 |
| November 14 | Lower 95% prediction interval of expected number of deaths | 5,274 |
| November 21 | Lower 95% prediction interval of expected number of deaths | 5,318 |
| November 28 | Lower 95% prediction interval of expected number of deaths | 5,366 |
| December 05 | Lower 95% prediction interval of expected number of deaths | 5,413 |
| December 12 | Lower 95% prediction interval of expected number of deaths | 5,427 |
| December 19 | Lower 95% prediction interval of expected number of deaths | 5,538 |
| December 26 | Lower 95% prediction interval of expected number of deaths | 5,625 |
| January 04 | Upper 95% prediction interval of adjusted number of deaths | 6,183 |
| January 11 | Upper 95% prediction interval of adjusted number of deaths | 6,213 |
| January 18 | Upper 95% prediction interval of adjusted number of deaths | 6,136 |
| January 25 | Upper 95% prediction interval of adjusted number of deaths | 6,166 |
| February 01 | Upper 95% prediction interval of adjusted number of deaths | 5,847 |
| February 08 | Upper 95% prediction interval of adjusted number of deaths | 5,902 |
| February 15 | Upper 95% prediction interval of adjusted number of deaths | 5,735 |
| February 22 | Upper 95% prediction interval of adjusted number of deaths | 5,677 |
| February 29 | Upper 95% prediction interval of adjusted number of deaths | 5,775 |
| March 07 | Upper 95% prediction interval of adjusted number of deaths | 5,769 |
| March 14 | Upper 95% prediction interval of adjusted number of deaths | 5,682 |
| March 21 | Upper 95% prediction interval of adjusted number of deaths | 5,879 |
| March 28 | Upper 95% prediction interval of adjusted number of deaths | 5,933 |
| April 04 | Upper 95% prediction interval of adjusted number of deaths | 6,301 |
| April 11 | Upper 95% prediction interval of adjusted number of deaths | 6,593 |
| April 18 | Upper 95% prediction interval of adjusted number of deaths | 6,622 |
| April 25 | Upper 95% prediction interval of adjusted number of deaths | 6,941 |
| May 02 | Upper 95% prediction interval of adjusted number of deaths | 6,901 |
| May 09 | Upper 95% prediction interval of adjusted number of deaths | 6,441 |
| May 16 | Upper 95% prediction interval of adjusted number of deaths | 6,121 |
| May 23 | Upper 95% prediction interval of adjusted number of deaths | 5,926 |
| May 30 | Upper 95% prediction interval of adjusted number of deaths | 5,886 |
| June 06 | Upper 95% prediction interval of adjusted number of deaths | 5,549 |
| June 13 | Upper 95% prediction interval of adjusted number of deaths | 5,201 |
| June 20 | Upper 95% prediction interval of adjusted number of deaths | 5,304 |
| June 27 | Upper 95% prediction interval of adjusted number of deaths | 5,297 |
| July 04 | Upper 95% prediction interval of adjusted number of deaths | 5,157 |
| July 11 | Upper 95% prediction interval of adjusted number of deaths | 5,396 |
| July 18 | Upper 95% prediction interval of adjusted number of deaths | 5,279 |
| July 25 | Upper 95% prediction interval of adjusted number of deaths | 5,287 |
| August 01 | Upper 95% prediction interval of adjusted number of deaths | 5,234 |
| August 08 | Upper 95% prediction interval of adjusted number of deaths | 5,248 |
| August 15 | Upper 95% prediction interval of adjusted number of deaths | 5,422 |
| August 22 | Upper 95% prediction interval of adjusted number of deaths | 5,424 |
| August 29 | Upper 95% prediction interval of adjusted number of deaths | 5,259 |
| September 05 | Upper 95% prediction interval of adjusted number of deaths | 5,455 |
| September 12 | Upper 95% prediction interval of adjusted number of deaths | 5,334 |
| September 19 | Upper 95% prediction interval of adjusted number of deaths | 5,472 |
| September 26 | Upper 95% prediction interval of adjusted number of deaths | 5,754 |
| October 03 | Upper 95% prediction interval of adjusted number of deaths | 5,712 |
| October 10 | Upper 95% prediction interval of adjusted number of deaths | 5,788 |
| October 17 | Upper 95% prediction interval of adjusted number of deaths | 5,737 |
| October 24 | Upper 95% prediction interval of adjusted number of deaths | 5,758 |
| October 31 | Upper 95% prediction interval of adjusted number of deaths | 5,914 |
| November 07 | Upper 95% prediction interval of adjusted number of deaths | 6,275 |
| November 14 | Upper 95% prediction interval of adjusted number of deaths | 6,158 |
| November 21 | Upper 95% prediction interval of adjusted number of deaths | 6,155 |
| November 28 | Upper 95% prediction interval of adjusted number of deaths | 6,322 |
| December 05 | Upper 95% prediction interval of adjusted number of deaths | 6,519 |
| December 12 | Upper 95% prediction interval of adjusted number of deaths | 6,587 |
| December 19 | Upper 95% prediction interval of adjusted number of deaths | 6,464 |
| December 26 | Upper 95% prediction interval of adjusted number of deaths | 6,677 |
| January 04 | Upper 95% prediction interval of expected number of deaths | 6,353 |
| January 11 | Upper 95% prediction interval of expected number of deaths | 6,426 |
| January 18 | Upper 95% prediction interval of expected number of deaths | 6,519 |
| January 25 | Upper 95% prediction interval of expected number of deaths | 6,524 |
| February 01 | Upper 95% prediction interval of expected number of deaths | 6,417 |
| February 08 | Upper 95% prediction interval of expected number of deaths | 6,355 |
| February 15 | Upper 95% prediction interval of expected number of deaths | 6,328 |
| February 22 | Upper 95% prediction interval of expected number of deaths | 6,277 |
| February 29 | Upper 95% prediction interval of expected number of deaths | 6,231 |
| March 07 | Upper 95% prediction interval of expected number of deaths | 6,208 |
| March 14 | Upper 95% prediction interval of expected number of deaths | 6,139 |
| March 21 | Upper 95% prediction interval of expected number of deaths | 6,066 |
| March 28 | Upper 95% prediction interval of expected number of deaths | 6,020 |
| April 04 | Upper 95% prediction interval of expected number of deaths | 5,970 |
| April 11 | Upper 95% prediction interval of expected number of deaths | 5,938 |
| April 18 | Upper 95% prediction interval of expected number of deaths | 5,897 |
| April 25 | Upper 95% prediction interval of expected number of deaths | 5,826 |
| May 02 | Upper 95% prediction interval of expected number of deaths | 5,773 |
| May 09 | Upper 95% prediction interval of expected number of deaths | 5,712 |
| May 16 | Upper 95% prediction interval of expected number of deaths | 5,679 |
| May 23 | Upper 95% prediction interval of expected number of deaths | 5,632 |
| May 30 | Upper 95% prediction interval of expected number of deaths | 5,552 |
| June 06 | Upper 95% prediction interval of expected number of deaths | 5,489 |
| June 13 | Upper 95% prediction interval of expected number of deaths | 5,448 |
| June 20 | Upper 95% prediction interval of expected number of deaths | 5,444 |
| June 27 | Upper 95% prediction interval of expected number of deaths | 5,423 |
| July 04 | Upper 95% prediction interval of expected number of deaths | 5,395 |
| July 11 | Upper 95% prediction interval of expected number of deaths | 5,364 |
| July 18 | Upper 95% prediction interval of expected number of deaths | 5,346 |
| July 25 | Upper 95% prediction interval of expected number of deaths | 5,383 |
| August 01 | Upper 95% prediction interval of expected number of deaths | 5,375 |
| August 08 | Upper 95% prediction interval of expected number of deaths | 5,340 |
| August 15 | Upper 95% prediction interval of expected number of deaths | 5,342 |
| August 22 | Upper 95% prediction interval of expected number of deaths | 5,338 |
| August 29 | Upper 95% prediction interval of expected number of deaths | 5,384 |
| September 05 | Upper 95% prediction interval of expected number of deaths | 5,430 |
| September 12 | Upper 95% prediction interval of expected number of deaths | 5,445 |
| September 19 | Upper 95% prediction interval of expected number of deaths | 5,479 |
| September 26 | Upper 95% prediction interval of expected number of deaths | 5,512 |
| October 03 | Upper 95% prediction interval of expected number of deaths | 5,631 |
| October 10 | Upper 95% prediction interval of expected number of deaths | 5,696 |
| October 17 | Upper 95% prediction interval of expected number of deaths | 5,727 |
| October 24 | Upper 95% prediction interval of expected number of deaths | 5,753 |
| October 31 | Upper 95% prediction interval of expected number of deaths | 5,772 |
| November 07 | Upper 95% prediction interval of expected number of deaths | 5,847 |
| November 14 | Upper 95% prediction interval of expected number of deaths | 5,889 |
| November 21 | Upper 95% prediction interval of expected number of deaths | 5,869 |
| November 28 | Upper 95% prediction interval of expected number of deaths | 5,882 |
| December 05 | Upper 95% prediction interval of expected number of deaths | 5,939 |
| December 12 | Upper 95% prediction interval of expected number of deaths | 6,018 |
| December 19 | Upper 95% prediction interval of expected number of deaths | 6,175 |
| December 26 | Upper 95% prediction interval of expected number of deaths | 6,264 |
The heavy line in the graph above shows a blip representing "excess" deaths from March to June 2020, during the first wave of COVID. Unfortunately, these data do not distinguish whether these excess deaths occurred in the community or in long term care facilities. As a result, it is possible that much of the first wave public health pandemic health policy was misdirected. For example, there has been an unfortunately very long delay in beginning to use rapid testing in schools and the community, leading to many unnecessary deaths.
In addition to this failure to track where COVID deaths were actually occurring, these data suffered from completely unacceptable delays in the submission of death certificates from the provinces to Statistics Canada, as shown in the next graph for 2021.
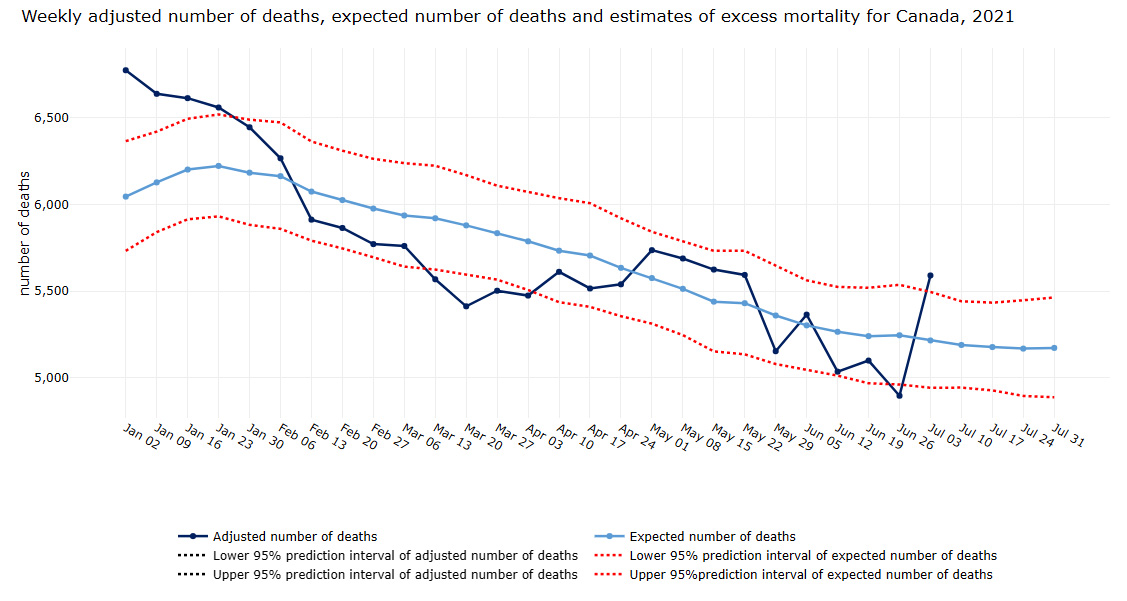
Figure B2: Text description
This image is a graph depicting the adjusted number of deaths, the number of expected deaths and the estimate of excess mortality for Canada on a weekly basis during 2021. The date range for this graph is from January 1 until the week of July 31, 2021.
The title of the image is Weekly adjusted number of deaths, expected number of deaths and estimates of excess mortality for Canada, January to July 2021
| Date | Characteristic | Number of Deaths |
|---|---|---|
| January 02 | Adjusted number of deaths | 6,760 |
| January 09 | Adjusted number of deaths | 6,660 |
| January 16 | Adjusted number of deaths | 6,618 |
| January 23 | Adjusted number of deaths | 6,547 |
| January 30 | Adjusted number of deaths | 6,463 |
| February 06 | Adjusted number of deaths | 6,290 |
| February 13 | Adjusted number of deaths | 5,922 |
| February 20 | Adjusted number of deaths | 5,881 |
| February 27 | Adjusted number of deaths | 5,767 |
| March 06 | Adjusted number of deaths | 5,764 |
| March 13 | Adjusted number of deaths | 5,569 |
| March 20 | Adjusted number of deaths | 5,413 |
| March 27 | Adjusted number of deaths | 5,476 |
| April 03 | Adjusted number of deaths | 5,455 |
| April 10 | Adjusted number of deaths | 5,624 |
| April 17 | Adjusted number of deaths | 5,486 |
| April 24 | Adjusted number of deaths | 5,499 |
| May 01 | Adjusted number of deaths | 5,696 |
| May 08 | Adjusted number of deaths | 5,637 |
| May 15 | Adjusted number of deaths | 5,559 |
| May 22 | Adjusted number of deaths | 5,572 |
| May 29 | Adjusted number of deaths | 5,179 |
| June 05 | Adjusted number of deaths | 5,430 |
| June 12 | Adjusted number of deaths | 5,143 |
| June 19 | Adjusted number of deaths | 5,221 |
| June 26 | Adjusted number of deaths | 5,101 |
| July 03 | Adjusted number of deaths | 5,920 |
| July 10 | Adjusted number of deaths | 4,988 |
| July 17 | Adjusted number of deaths | .. |
| July 24 | Adjusted number of deaths | .. |
| July 31 | Adjusted number of deaths | .. |
| January 02 | Lower 95% prediction interval of adjusted number of deaths | 6,747 |
| January 09 | Lower 95% prediction interval of adjusted number of deaths | 6,647 |
| January 16 | Lower 95% prediction interval of adjusted number of deaths | 6,605 |
| January 23 | Lower 95% prediction interval of adjusted number of deaths | 6,533 |
| January 30 | Lower 95% prediction interval of adjusted number of deaths | 6,448 |
| February 06 | Lower 95% prediction interval of adjusted number of deaths | 6,274 |
| February 13 | Lower 95% prediction interval of adjusted number of deaths | 5,906 |
| February 20 | Lower 95% prediction interval of adjusted number of deaths | 5,864 |
| February 27 | Lower 95% prediction interval of adjusted number of deaths | 5,749 |
| March 06 | Lower 95% prediction interval of adjusted number of deaths | 5,747 |
| March 13 | Lower 95% prediction interval of adjusted number of deaths | 5,550 |
| March 20 | Lower 95% prediction interval of adjusted number of deaths | 5,393 |
| March 27 | Lower 95% prediction interval of adjusted number of deaths | 5,456 |
| April 03 | Lower 95% prediction interval of adjusted number of deaths | 5,433 |
| April 10 | Lower 95% prediction interval of adjusted number of deaths | 5,601 |
| April 17 | Lower 95% prediction interval of adjusted number of deaths | 5,463 |
| April 24 | Lower 95% prediction interval of adjusted number of deaths | 5,473 |
| May 01 | Lower 95% prediction interval of adjusted number of deaths | 5,668 |
| May 08 | Lower 95% prediction interval of adjusted number of deaths | 5,607 |
| May 15 | Lower 95% prediction interval of adjusted number of deaths | 5,529 |
| May 22 | Lower 95% prediction interval of adjusted number of deaths | 5,539 |
| May 29 | Lower 95% prediction interval of adjusted number of deaths | 5,146 |
| June 05 | Lower 95% prediction interval of adjusted number of deaths | 5,395 |
| June 12 | Lower 95% prediction interval of adjusted number of deaths | 5,107 |
| June 19 | Lower 95% prediction interval of adjusted number of deaths | 5,184 |
| June 26 | Lower 95% prediction interval of adjusted number of deaths | 5,063 |
| July 03 | Lower 95% prediction interval of adjusted number of deaths | 5,876 |
| July 10 | Lower 95% prediction interval of adjusted number of deaths | 4,946 |
| July 17 | Lower 95% prediction interval of adjusted number of deaths | .. |
| July 24 | Lower 95% prediction interval of adjusted number of deaths | .. |
| July 31 | Lower 95% prediction interval of adjusted number of deaths | .. |
| January 02 | Upper 95% prediction interval of adjusted number of deaths | 6,771 |
| January 09 | Upper 95% prediction interval of adjusted number of deaths | 6,671 |
| January 16 | Upper 95% prediction interval of adjusted number of deaths | 6,631 |
| January 23 | Upper 95% prediction interval of adjusted number of deaths | 6,561 |
| January 30 | Upper 95% prediction interval of adjusted number of deaths | 6,476 |
| February 06 | Upper 95% prediction interval of adjusted number of deaths | 6,304 |
| February 13 | Upper 95% prediction interval of adjusted number of deaths | 5,935 |
| February 20 | Upper 95% prediction interval of adjusted number of deaths | 5,895 |
| February 27 | Upper 95% prediction interval of adjusted number of deaths | 5,782 |
| March 06 | Upper 95% prediction interval of adjusted number of deaths | 5,781 |
| March 13 | Upper 95% prediction interval of adjusted number of deaths | 5,586 |
| March 20 | Upper 95% prediction interval of adjusted number of deaths | 5,431 |
| March 27 | Upper 95% prediction interval of adjusted number of deaths | 5,496 |
| April 03 | Upper 95% prediction interval of adjusted number of deaths | 5,475 |
| April 10 | Upper 95% prediction interval of adjusted number of deaths | 5,646 |
| April 17 | Upper 95% prediction interval of adjusted number of deaths | 5,509 |
| April 24 | Upper 95% prediction interval of adjusted number of deaths | 5,523 |
| May 01 | Upper 95% prediction interval of adjusted number of deaths | 5,722 |
| May 08 | Upper 95% prediction interval of adjusted number of deaths | 5,664 |
| May 15 | Upper 95% prediction interval of adjusted number of deaths | 5,588 |
| May 22 | Upper 95% prediction interval of adjusted number of deaths | 5,602 |
| May 29 | Upper 95% prediction interval of adjusted number of deaths | 5,210 |
| June 05 | Upper 95% prediction interval of adjusted number of deaths | 5,462 |
| June 12 | Upper 95% prediction interval of adjusted number of deaths | 5,177 |
| June 19 | Upper 95% prediction interval of adjusted number of deaths | 5,258 |
| June 26 | Upper 95% prediction interval of adjusted number of deaths | 5,138 |
| July 03 | Upper 95% prediction interval of adjusted number of deaths | 5,962 |
| July 10 | Upper 95% prediction interval of adjusted number of deaths | 5,028 |
| July 17 | Upper 95% prediction interval of adjusted number of deaths | .. |
| July 24 | Upper 95% prediction interval of adjusted number of deaths | .. |
| July 31 | Upper 95% prediction interval of adjusted number of deaths | .. |
| January 02 | Expected number of deaths | 6,046 |
| January 09 | Expected number of deaths | 6,128 |
| January 16 | Expected number of deaths | 6,202 |
| January 23 | Expected number of deaths | 6,223 |
| January 30 | Expected number of deaths | 6,184 |
| February 06 | Expected number of deaths | 6,164 |
| February 13 | Expected number of deaths | 6,075 |
| February 20 | Expected number of deaths | 6,026 |
| February 27 | Expected number of deaths | 5,977 |
| March 06 | Expected number of deaths | 5,937 |
| March 13 | Expected number of deaths | 5,921 |
| March 20 | Expected number of deaths | 5,880 |
| March 27 | Expected number of deaths | 5,835 |
| April 03 | Expected number of deaths | 5,788 |
| April 10 | Expected number of deaths | 5,734 |
| April 17 | Expected number of deaths | 5,706 |
| April 24 | Expected number of deaths | 5,635 |
| May 01 | Expected number of deaths | 5,576 |
| May 08 | Expected number of deaths | 5,514 |
| May 15 | Expected number of deaths | 5,440 |
| May 22 | Expected number of deaths | 5,431 |
| May 29 | Expected number of deaths | 5,360 |
| June 05 | Expected number of deaths | 5,303 |
| June 12 | Expected number of deaths | 5,266 |
| June 19 | Expected number of deaths | 5,241 |
| June 26 | Expected number of deaths | 5,246 |
| July 03 | Expected number of deaths | 5,216 |
| July 10 | Expected number of deaths | 5,190 |
| July 17 | Expected number of deaths | 5,178 |
| July 24 | Expected number of deaths | 5,169 |
| July 31 | Expected number of deaths | 5,173 |
| January 02 | Lower 95% prediction interval of expected number of deaths | 5,733 |
| January 09 | Lower 95% prediction interval of expected number of deaths | 5,841 |
| January 16 | Lower 95% prediction interval of expected number of deaths | 5,915 |
| January 23 | Lower 95% prediction interval of expected number of deaths | 5,932 |
| January 30 | Lower 95% prediction interval of expected number of deaths | 5,883 |
| February 06 | Lower 95% prediction interval of expected number of deaths | 5,860 |
| February 13 | Lower 95% prediction interval of expected number of deaths | 5,792 |
| February 20 | Lower 95% prediction interval of expected number of deaths | 5,747 |
| February 27 | Lower 95% prediction interval of expected number of deaths | 5,696 |
| March 06 | Lower 95% prediction interval of expected number of deaths | 5,642 |
| March 13 | Lower 95% prediction interval of expected number of deaths | 5,625 |
| March 20 | Lower 95% prediction interval of expected number of deaths | 5,595 |
| March 27 | Lower 95% prediction interval of expected number of deaths | 5,567 |
| April 03 | Lower 95% prediction interval of expected number of deaths | 5,507 |
| April 10 | Lower 95% prediction interval of expected number of deaths | 5,437 |
| April 17 | Lower 95% prediction interval of expected number of deaths | 5,410 |
| April 24 | Lower 95% prediction interval of expected number of deaths | 5,356 |
| May 01 | Lower 95% prediction interval of expected number of deaths | 5,313 |
| May 08 | Lower 95% prediction interval of expected number of deaths | 5,247 |
| May 15 | Lower 95% prediction interval of expected number of deaths | 5,153 |
| May 22 | Lower 95% prediction interval of expected number of deaths | 5,136 |
| May 29 | Lower 95% prediction interval of expected number of deaths | 5,080 |
| June 05 | Lower 95% prediction interval of expected number of deaths | 5,048 |
| June 12 | Lower 95% prediction interval of expected number of deaths | 5,013 |
| June 19 | Lower 95% prediction interval of expected number of deaths | 4,969 |
| June 26 | Lower 95% prediction interval of expected number of deaths | 4,962 |
| July 03 | Lower 95% prediction interval of expected number of deaths | 4,943 |
| July 10 | Lower 95% prediction interval of expected number of deaths | 4,944 |
| July 17 | Lower 95% prediction interval of expected number of deaths | 4,928 |
| July 24 | Lower 95% prediction interval of expected number of deaths | 4,896 |
| July 31 | Lower 95% prediction interval of expected number of deaths | 4,888 |
| January 02 | Upper 95% prediction interval of expected number of deaths | 6,366 |
| January 09 | Upper 95% prediction interval of expected number of deaths | 6,421 |
| January 16 | Upper 95% prediction interval of expected number of deaths | 6,495 |
| January 23 | Upper 95% prediction interval of expected number of deaths | 6,520 |
| January 30 | Upper 95% prediction interval of expected number of deaths | 6,490 |
| February 06 | Upper 95% prediction interval of expected number of deaths | 6,474 |
| February 13 | Upper 95% prediction interval of expected number of deaths | 6,364 |
| February 20 | Upper 95% prediction interval of expected number of deaths | 6,311 |
| February 27 | Upper 95% prediction interval of expected number of deaths | 6,264 |
| March 06 | Upper 95% prediction interval of expected number of deaths | 6,239 |
| March 13 | Upper 95% prediction interval of expected number of deaths | 6,224 |
| March 20 | Upper 95% prediction interval of expected number of deaths | 6,170 |
| March 27 | Upper 95% prediction interval of expected number of deaths | 6,109 |
| April 03 | Upper 95% prediction interval of expected number of deaths | 6,074 |
| April 10 | Upper 95% prediction interval of expected number of deaths | 6,037 |
| April 17 | Upper 95% prediction interval of expected number of deaths | 6,008 |
| April 24 | Upper 95% prediction interval of expected number of deaths | 5,921 |
| May 01 | Upper 95% prediction interval of expected number of deaths | 5,843 |
| May 08 | Upper 95% prediction interval of expected number of deaths | 5,786 |
| May 15 | Upper 95% prediction interval of expected number of deaths | 5,733 |
| May 22 | Upper 95% prediction interval of expected number of deaths | 5,733 |
| May 29 | Upper 95% prediction interval of expected number of deaths | 5,646 |
| June 05 | Upper 95% prediction interval of expected number of deaths | 5,563 |
| June 12 | Upper 95% prediction interval of expected number of deaths | 5,525 |
| June 19 | Upper 95% prediction interval of expected number of deaths | 5,520 |
| June 26 | Upper 95% prediction interval of expected number of deaths | 5,537 |
| July 03 | Upper 95% prediction interval of expected number of deaths | 5,496 |
| July 10 | Upper 95% prediction interval of expected number of deaths | 5,442 |
| July 17 | Upper 95% prediction interval of expected number of deaths | 5,434 |
| July 24 | Upper 95% prediction interval of expected number of deaths | 5,448 |
| July 31 | Upper 95% prediction interval of expected number of deaths | 5,464 |
It is completely implausible that deaths in Canada from January to March 2021 were declining to levels well below Stat Can's 95% confidence band at the end of March 2021. This is stark evidence that the provinces, who are responsible for collecting and sending their death certificates to Statistics Canada, are woefully behind.
There was some improvement in this data since March 2021, as there has been an additional four months for the provinces to send the data to Statistics Canada.
Still, the timeliness and range of information included on death certificates (e.g. whether or not resident in a nursing home) remain completely inadequate, though Statistics Canada is working with the provinces to improve these longstanding problems. While Canadians and much of the world have become accustomed to near instant responses when we want to see if an airplane seat is available anywhere in the world on virtually any flight, the submission of death certificate data is mired in decades old technology and stodgy governance. We echo the first recommendation of a recent Royal Society report, "Mandate weekly preliminary reporting of numbers of deaths due to all causes, in all provinces and territories, to Statistics Canada, similar to other countries."
Annex C: Data gap case study: Using artificial intelligence for prediction in health care
There is a great deal of excitement and enthusiasm about the use of sophisticated statistical methods, including machine learning algorithms and artificial intelligence, to offer a range of health-related predictions. However, these algorithms are often proprietary, so their validity is difficult to assess. In a recent study, a widely used algorithm in the US to predict sepsis, an often fatal complication for hospitalized patients, failed to give an alarm in two-thirds of sepsis cases but also gave numerous false alarms when the patient did not have sepsis. This same system is used by many Canadian hospitals.
From a pan-Canadian perspective, this anecdote reveals a number of major failures. First, even though much of the relevant data exist in order to create a similar made-in-Canada sepsis prediction algorithm, these data reside in separate silos, so it is essentially impossible to create one. Second, as it was produced using primarily data for a non-Canadian population, and this poorly performing and indeed life-threatening algorithm is proprietary, there is no way for Canadian regulators to check its validity for the Canadian population. Third, with the increasing concerns and evidence that such algorithms can perform more poorly for minority and other marginalized populations, the often wide gulf between socio-economic and clinical data silos in Canada mean that any such biases cannot be examined.
In addition to the need to break down the data silos preventing the development of sophisticated health prediction algorithms, there is also a need for complete transparency in the details of how these algorithms construct their predictions. They cannot remain inside proprietary black boxes.
Annex D: Data gap case study: Real-time mobility data
One of the dramatic changes in recent years is the ability to track the geographic mobility of huge segments of the population. This has been enabled by the ubiquity of cell phone ownership, most yielding at least a coarse measure of location from cell towers, and many providing much more detailed locations from the phones' internal GPS.
This tracking capacity has been driven by the business objectives of the major tech companies. Serendipitously, to varying degrees, the current COVID-19 pandemic has spurred researchers and infectious disease modellers to do their best to access these data in order to track the existing spread of the virus, and more importantly, to estimate where it is most likely to surge.
However, as discussed in a recent Nature comment article, this extremely important potential use of these data is most often stymied by the proprietary nature of these data. The large tech and phone companies first decide which data elements on individuals they will collect and link to their locations, then decide which, if any of these data they will make available to various users, and how much they will charge. Moreover, they can change all these decisions at their discretion.
Of course, there are significant ethical and personal privacy issues involved in making any of these data available, at the individual level, outside the firm that has done the primary data collection. But this is equally true for physician visit and diagnostic lab data, where in both cases, most of these data are collected by private sector entities. However, it is widely accepted that for health policy, especially in the midst of a pandemic, these data have crucial public health benefits. As the Nature article indicates, there are widely acceptable means by which these data could be made routinely available for authorized public health uses, especially for tracking infectious diseases.
Footnotes
- Footnote 1
-
Incorporates several dimensions of care including safety, health outcomes, effectiveness, efficiency, equity, person-centred care and timeliness.
- Footnote 2
-
See glossary.
- Footnote 3
-
Policy in this document refers to the set of legislation, regulation, principles, policies, and practices that establish the environment for health.
- Footnote 4
-
Including federal-provincial-territorial Ministers of Health, supported by their First Ministers and Ministers of Finance.
- Footnote 5
-
Adapted from the Global Alliance for Genomics & Health (GA4GH)'s Data Sharing Lexicon.
- Footnote 6
-
From the Global Alliance for Genomics & Health Lexicon.
- Footnote 7
-
Adapted from the GA4GH Data Sharing Lexicon and the Spectrum of Identifiability defined in the Canadian Anonymization Network's report, Practices for Generated Non-identifiable Data.
- Footnote 8
-
From the Global Alliance for Genomics & Health Lexicon.
Page details
- Date modified:
